- What Are Skull Base Tumors?
- Early Symptoms Patients Ignore
- Common Disorders Associated With Skull Base Tumors
- Neurological and Functional Associations
- Rare but Clinically Significant Associations
- Systemic and Metabolic Overlap
- Ayurvedic Clinical Correlation
- When Should You Suspect a Skull Base Tumor?
- Anatomy of the Skull Base
- Classification of Skull Base Tumors
- Molecular and Histopathological Insights
- Clinical Presentation(Symptoms)
- Diagnostic Approach
- Diseases Commonly Misdiagnosed Before Skull Base Tumor Detection
- Clinical Warning Pattern
- Ayurvedic Diagnostic Perspective
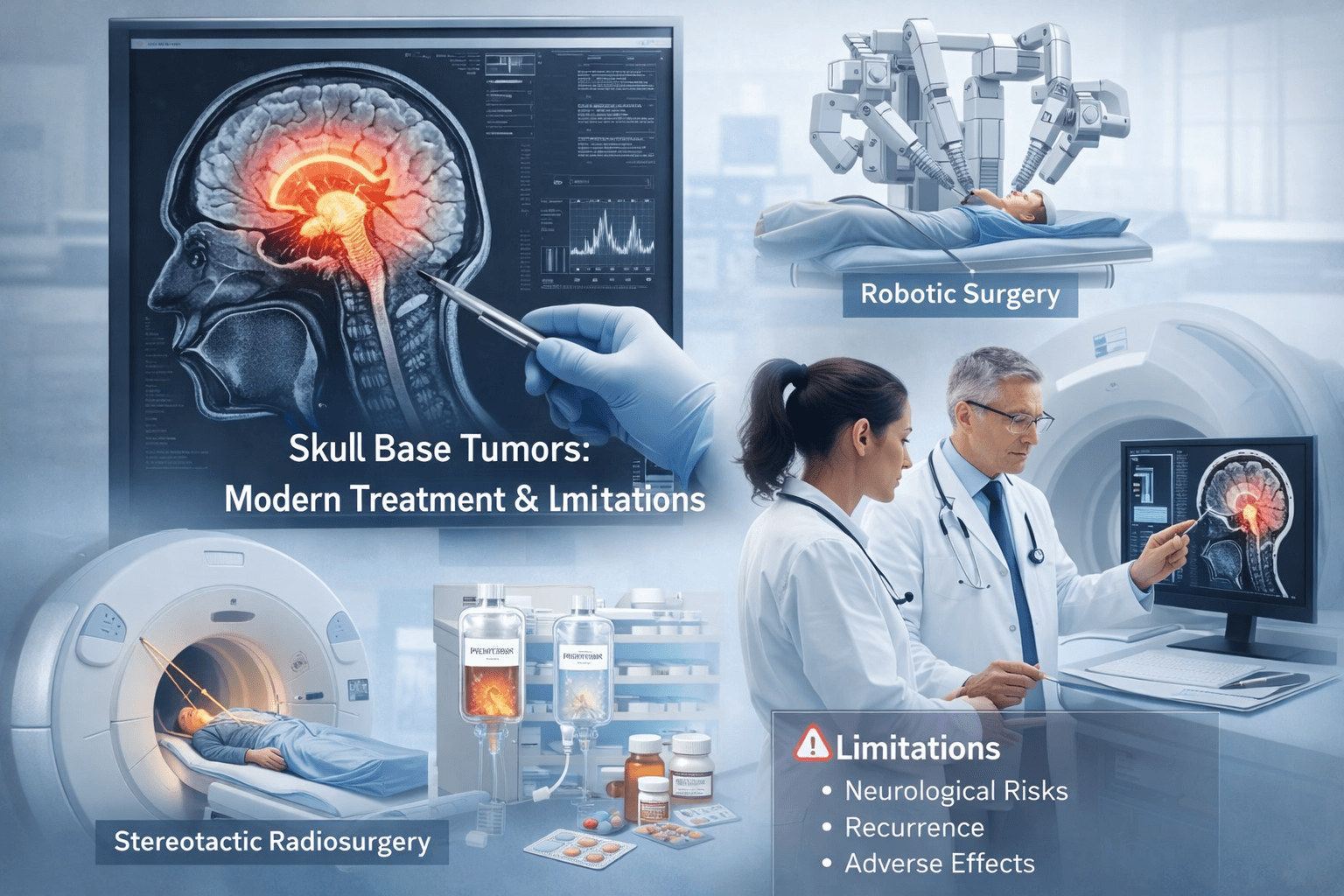
- Modern Treatment for Skull Base Tumors & its Limitations
- Can Skull Base Tumors Be Cured Without Surgery
- Ayurvedic Curative Protocol
- Treatment for International Patients
- Recovery After Surgery With Ayurveda
- Why Patients Choose Ayurvedic Rasayana Therapy
- Frequently Asked Questions
- Reference
This article explains the early signs, diagnostic process, and modern treatment challenges of skull base tumors, along with a deeply restorative Ayurvedic approach that focuses on neurological recovery and long-term disease reversal. It is designed for patients who are facing surgery ,or wanted to avoid surgery, recurrence, hormonal disturbances, or post-treatment weakness and are searching for a structured, root-cause, based healing path. Through classical Rasayana therapy, personalized herbal–mineral formulations, and integrative care, the goal is not only tumor control but regeneration of Majja Dhatu, restoration of Ojas, and improvement in quality of life.
What Are Skull Base Tumors?
Skull base tumors are abnormal growths that develop at the bottom of the brain where critical cranial nerves, major blood vessels, and hormonal control centers pass through a narrow space. Because of this deep and complex location, even small tumors can affect vision, hearing, balance, facial sensation, and endocrine function.
Common symptoms include:
- Persistent or pressure-type headache
- Double vision or gradual vision loss
- One-sided hearing reduction or tinnitus
- Facial numbness or unexplained pain
- Hormonal imbalance, fatigue, or menstrual irregularity
Understanding Skull Base Tumors
Skull base tumors are among the most complex and challenging conditions in neurology and oncology. They develop in the region that forms the floor of the cranial cavity, separating the brain from the facial and neck structures. This critical zone is densely packed with cranial nerves, blood vessels, and vital sensory pathways. Even a small lesion in this confined space can have major neurological consequences , affecting vision, hearing, swallowing, balance, and hormonal control [21].
Types and Clinical Significance
From a clinical viewpoint, skull base tumors are classified into benign and malignant types.
- Benign tumors such as meningiomas, pituitary adenomas, and schwannomas grow slowly but often compress vital structures.
- Malignant tumors, including chondrosarcomas, esthesioneuroblastomas, and nasopharyngeal carcinomas, are more aggressive and prone to recurrence or metastasis [38].
Despite modern advances in microsurgery and neuro-navigation, achieving total tumor removal without damaging nearby nerves and blood vessels remains difficult [44]. Their anatomical complexity makes them one of the most formidable challenges in neurosurgery and oncology.
Early Symptoms Patients Ignore
In the early stage, skull base tumors rarely cause dramatic warning signs. The symptoms are subtle, slow, and often mistaken for sinus problems, migraine, stress, eye strain, or age-related hormonal changes. Because the tumor grows in a deep and narrow space, these small signals are the body’s first request for attention.
Headache pattern:
A dull, persistent headache that does not follow the usual migraine pattern, is often deeper behind the eyes or at the back of the head, and shows poor response to routine painkillers.
One-sided hearing loss:
Gradual reduction in hearing in one ear, a blocked ear sensation, or continuous tinnitus that does not improve with standard ENT treatment.
Double vision:
Intermittent blurring, difficulty focusing, or seeing two images when looking in a particular direction, especially when tired.
Hormonal changes:
Unexplained fatigue, sudden weight change, irregular periods, reduced libido, infertility, sleep disturbance, or abnormal thyroid and cortisol reports.
Facial numbness:
Tingling, reduced sensation, mild pulling feeling on one side of the face, or unexplained neuralgic pain.
Early recognition of these signs allows diagnosis at a stage when treatment outcomes and neurological recovery are significantly better.
Why Early Diagnosis is Critical
The early symptoms of skull base tumors are frequently subtle and easily overlooked. Patients may initially experience mild headaches, facial tingling, nasal obstruction, or vision changes, often misattributed to sinus or migraine issues. By the time diagnosis is confirmed, many already present with cranial nerve palsy, visual loss, or hormonal imbalance from pituitary involvement [19].
Modern imaging modalities such as MRI, PET-CT, and MR spectroscopy have improved detection rates, yet recurrence and neurological deficits remain persistent issues [27]. Timely recognition is therefore vital—small tumors at the skull base can produce massive consequences if left untreated [32].
Ayurvedic Interpretation: Granthi and Arbuda Theory
Ayurveda views such growths through the timeless principles of Dosha, Dhatu, and Agni. Ancient texts like Charaka Samhita and Sushruta Samhita describe two forms of pathological masses—Granthi (encapsulated swelling) and Arbuda (malignant tumor)—arising from the vitiation of Kapha and Vata Doshas obstructing vital channels (Srotas) in the head region [14].
The skull base corresponds to the Shiras Marma, a vital center regulating consciousness, sensory perception, and hormonal activity. When Agni (metabolic fire) diminishes, Ama (toxic residue) accumulates, leading to Srotorodha (obstruction) within Majja Dhatu (nervous tissue) [22]. Over time, this imbalance manifests as abnormal growth or degeneration, paralleling modern concepts of oncogenic mutation and cellular dysfunction.
The Integrative Healing Lens
While modern medicine focuses on excising or irradiating the tumor, Ayurveda seeks to restore the body’s natural intelligence. It explains that the root cause lies not in the physical tumor alone but in systemic disharmony—weak Agni, blocked Srotas, and depleted Ojas (vital immunity) [35].
Therapeutic strategies thus aim at three core objectives:
- Shodhana (Detoxification): Removing accumulated toxins and metabolic residues.
- Shamana (Pacification): Balancing disturbed Doshas and stabilizing the nervous system.
- Rasayana (Rejuvenation): Regenerating brain tissue and enhancing immunity.
Modern integrative oncology now mirrors these same principles, emphasizing immune modulation, metabolic therapy, and mind–body resilience for long-term recovery [46].
Common Disorders Associated With Skull Base Tumors
Pituitary hormonal syndromes
Tumors arising in the sellar and parasellar region are frequently detected during evaluation for endocrine disease rather than neurological symptoms. Patients are often treated for hyperprolactinemia, acromegaly, Cushing disease, hypothyroidism, infertility, menstrual irregularity, reduced libido, or chronic unexplained fatigue before imaging reveals the underlying skull base lesion.
Chronic sinusitis and persistent nasal obstruction
Anterior skull base tumors, especially those involving the sphenoid and ethmoid region, are commonly mistaken for refractory sinusitis. Repeated medical therapy or sinus procedures may be performed when the real cause is a deep seated mass.
Unilateral sensorineural hearing loss
Progressive hearing reduction in one ear with tinnitus or imbalance is a classical association with cerebellopontine angle tumors such as vestibular schwannoma. It is often initially attributed to age related change or middle ear pathology.
Trigeminal neuralgia and chronic facial pain
Compression of the trigeminal pathway produces facial pain, tingling, or numbness. Many patients receive dental or temporomandibular treatment before the primary lesion is identified.
Visual field defects and optic pathway disorders
Gradual loss of peripheral vision, recurrent change in spectacle number, and optic nerve thinning on ophthalmic examination are important associated findings in tumors affecting the optic chiasm and surrounding region.
Migraine and cervicogenic headache misdiagnosis
Deep, non responsive headache is frequently managed as migraine, stress headache, or cervical spondylosis for long periods before a skull base origin is suspected.
Neurological and Functional Associations
Balance disorders and recurrent vertigo
Posterior skull base involvement often presents as unsteadiness while walking, a tendency to sway, or persistent vertigo that does not match classical vestibular disease.
Swallowing difficulty and voice change
Lower cranial nerve compression may produce dysphagia, choking episodes, nasal regurgitation, or hoarseness of voice.
Sleep disturbance and central fatigue
Disruption of neuroendocrine and brainstem regulatory pathways may lead to non restorative sleep and profound fatigue.
Cognitive slowing and memory impairment
Patients may experience reduced concentration, slower processing, and mental exhaustion, especially in long standing lesions.
Rare but Clinically Significant Associations
Multiple endocrine neoplasia syndromes
Pituitary tumors associated with MEN1 may coexist with parathyroid and pancreatic neuroendocrine tumors.
Neurofibromatosis type 2
Bilateral vestibular schwannomas and multiple cranial nerve tumors represent a characteristic but uncommon association.
Clival tumors with craniovertebral instability
Long standing chordomas and similar lesions can affect structural stability at the craniovertebral junction and produce progressive neurological deficit.
Paraneoplastic neurological syndromes
In malignant skull base tumors immune mediated neuropathy, cerebellar dysfunction, or unexplained neuromuscular weakness may occur.
Cerebrospinal fluid leak syndromes
Spontaneous CSF rhinorrhea may be the first clinical sign of anterior skull base erosion.
Carotid artery encasement and vascular insufficiency
Advanced lesions may involve the internal carotid artery and produce transient ischemic symptoms.
Radiation induced secondary tumors
In previously treated patients a new skull base lesion may represent a secondary neoplasm rather than recurrence.
Systemic and Metabolic Overlap
Chronic fatigue like presentation
Long standing neuroendocrine disturbance may mimic systemic fatigue syndromes.
Unexplained weight change
Pituitary involvement can produce sudden metabolic alteration without primary dietary cause.
Electrolyte imbalance due to hormonal dysfunction
Disturbance of cortisol, thyroid, or antidiuretic hormone pathways may lead to persistent biochemical abnormalities.
Anxiety secondary to undiagnosed neurological disease
Psychological symptoms often appear when the primary structural cause remains unidentified for a prolonged period.
Ayurvedic Clinical Correlation
Majja Dhatu involvement
Neurological weakness, cognitive slowing, and sensory disturbance reflect depletion or obstruction at the level of Majja Dhatu.
Shukra and Artava Dhatu disturbance
Infertility, menstrual irregularity, and endocrine imbalance indicate deeper tissue level involvement.
Prana Vaha and Udana Vaha Srotas dysfunction
Voice change, swallowing difficulty, and higher functional impairment arise from obstruction in these channels.
Kapha Vata Granthi expression
Structural growth with progressive functional depletion represents the combined effect of Kapha producing mass and Vata disturbing neural activity.
When Should You Suspect a Skull Base Tumor?
Skull base tumors are often discovered late because their early features resemble common conditions such as migraine, sinusitis, cervical spondylosis, eye strain, or hormonal imbalance. Suspicion should arise when symptoms are persistent, progressive, one-sided, or involve multiple systems at the same time. The pattern matters more than the intensity.
You should consider proper neurological and imaging evaluation if you notice a headache that is new in character, deeper in location, and not responding to your usual medication, especially when it is associated with visual strain or facial heaviness. A slowly developing hearing reduction in one ear, particularly when ENT treatment and ear examinations appear normal, is another important clinical clue.
Visual disturbances are highly significant. Difficulty focusing, intermittent double vision, narrowing of side vision, or a need to change spectacle power repeatedly within a short period should never be ignored. These changes often indicate pressure along the optic pathway or nearby cranial nerves.
Hormonal shifts without a clear lifestyle or metabolic cause also require attention. Unexplained fatigue, sudden weight gain or loss, irregular menstrual cycles, reduced libido, infertility, or abnormal thyroid, prolactin, or cortisol reports may indicate involvement of the pituitary or parasellar region.
Facial symptoms provide another early window. Persistent numbness, tingling, reduced sensation while chewing, unexplained neuralgic pain, or a subtle asymmetry in facial movement suggest irritation of the trigeminal or facial nerve pathways.
Balance difficulty, a tendency to sway while walking, new-onset clumsiness, or a feeling of internal motion when sitting still are warning signals of posterior skull base or cerebellar involvement.
The most important rule is this: when one-sided neurological symptoms progress slowly and do not match routine diagnoses, advanced imaging such as contrast MRI of the brain and skull base should be performed. Early detection dramatically improves both surgical safety and long-term recovery outcomes.
Anatomy of the Skull Base
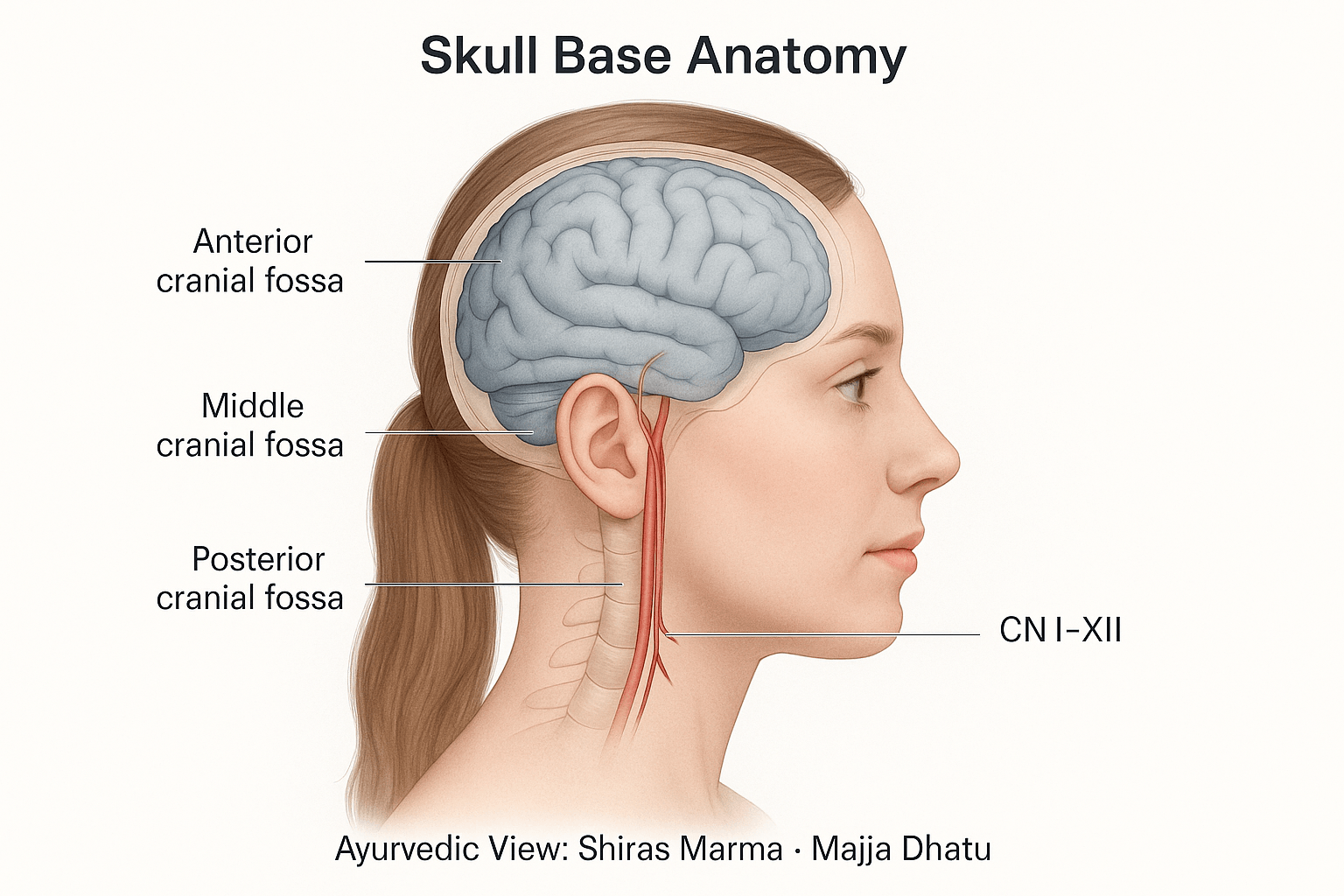
Structural Overview
The skull base forms the intricate floor of the cranial cavity, serving as the interface between the brain and the face, neck, and upper respiratory tract. It provides both mechanical support and protective passageways for critical neurovascular structures. Anatomically, it is divided into three distinct regions—the anterior, middle, and posterior cranial fossae—each housing specific portions of the brain and corresponding cranial nerves [18].
- Anterior cranial fossa: Supports the frontal lobes of the brain and forms the roof of the orbits. Tumors here often affect the olfactory nerve, leading to loss of smell or visual field disturbances.
- Middle cranial fossa: Contains the temporal lobes and the pituitary gland within the sella turcica. Lesions in this area can lead to hormonal imbalance, trigeminal neuralgia, or facial weakness [39].
- Posterior cranial fossa: Encloses the brainstem and cerebellum, making it the most critical region for vital functions like respiration, balance, and coordination. Even minor compression in this zone can cause life-threatening complications such as dysphagia or respiratory irregularity [27].
These fossae are separated by ridges of bone—sphenoid, petrous temporal, and occipital—that not only support but also restrict the space available for expanding lesions. This anatomical compactness explains why skull base tumors, even when small, can cause disproportionately severe neurological symptoms [43].
Key Neural and Vascular Elements
Twelve cranial nerves traverse the skull base, controlling nearly all sensory and motor functions of the head and neck. These include the olfactory nerve (I) for smell, optic (II) for vision, oculomotor (III) and trochlear (IV) for eye movement, trigeminal (V) for facial sensation, and facial (VII) for expressions [16]. Posteriorly, the vestibulocochlear (VIII) governs hearing and balance, while the glossopharyngeal (IX), vagus (X), and hypoglossal (XII) manage swallowing, heart rhythm, and speech.
In addition to these neural pathways, major vessels like the internal carotid arteries, basilar artery, and venous sinuses course through the region. Any tumor compressing these arteries can disrupt cerebral perfusion, causing ischemia or stroke-like symptoms [41]. Similarly, obstruction of venous drainage can lead to intracranial pressure elevation and severe headaches. The skull base thus represents a convergence point where vascular compromise and nerve entrapment frequently coexist.
Clinical Correlation: How Location Dictates Symptoms
The clinical presentation of skull base tumors is determined largely by their location.
- Anterior fossa tumors may cause anosmia, visual distortion, and cognitive impairment due to frontal lobe compression.
- Middle fossa tumors often produce facial pain, hormonal irregularities, and seizures.
- Posterior fossa lesions manifest as vertigo, imbalance, difficulty swallowing, and cranial nerve palsy [30].
Pituitary and parasellar masses, for instance, can alter endocrine functions leading to amenorrhea, galactorrhea, or acromegaly, while vestibular schwannomas primarily affect hearing and equilibrium. Recognizing these symptom patterns is vital for early localization and targeted management.
Ayurvedic Interpretation: Shiras Marma and Vital Channels
Ayurveda describes the cranial base region as part of the Shiras Marma, one of the 37 vital energy points controlling sensory perception, consciousness, and hormonal rhythm. It houses the Prana Vaha Srotas (channel of vital energy) and Majja Dhatu (nervous tissue), both central to neural vitality and mental stability [22].
When Vata and Kapha Doshas become vitiated, they obstruct these delicate channels, leading to stagnation of Prana and diminished coordination between sensory and cognitive faculties. The compression of cranial nerves in modern anatomy parallels the Ayurvedic concept of Srotorodha—blockage in the flow of energy and information [35].
Thus, while neuroanatomy identifies mechanical obstruction or ischemia as the cause of dysfunction, Ayurveda interprets it as a deeper energetic imbalance between Prana, Tejas, and Ojas. The Majja Dhatu acts as the physical substrate of consciousness, linking mind and body. Therefore, any lesion at the skull base not only disrupts motor and sensory function but also affects mental clarity, emotion, and vitality [44].
In essence, the skull base is the physical and energetic foundation of the human brain. It unites the structural brilliance of modern neuroanatomy with the subtle intelligence of Ayurvedic physiology. Understanding its pathways from both perspectives is crucial for developing therapies that not only remove the disease but also restore the harmony of the nervous system, mind, and consciousness.
Classification of Skull Base Tumors
Overview
Skull base tumors comprise a diverse group of lesions that differ in their origin, biological behavior, and clinical implications. Classification is essential for determining the right treatment strategy, prognosis, and surgical approach. From a modern medical standpoint, these tumors are broadly categorized as benign or malignant, while Ayurveda classifies them under the pathological spectrum of Granthi and Arbuda based on the dominance of specific Doshas and Dhatu involvement [26].
Benign Skull Base Tumors
Benign skull base tumors usually grow slowly and remain localized, though their proximity to vital structures can still cause significant neurological symptoms.
- Meningioma: The most common benign tumor of the skull base, arising from the meninges. It often affects the sphenoid ridge or olfactory groove and may cause vision loss, headache, or seizures [39].
- Schwannoma: Originating from the Schwann cells of cranial nerves, particularly the vestibulocochlear or trigeminal nerves, it leads to progressive hearing loss or facial numbness [18].
- Pituitary Adenoma: Develops in the sella turcica and can produce hormonal imbalances such as hyperprolactinemia or acromegaly. When large, it compresses the optic chiasm, causing bitemporal hemianopia [43].
- Chordoma: A rare, locally aggressive tumor arising from remnants of the notochord, typically at the clivus. Despite its benign histology, it can invade surrounding bone and brain tissue [41].
- Craniopharyngioma: A cystic, benign tumor originating from Rathke’s pouch epithelium, often affecting children and young adults, leading to growth failure and vision problems [32].
Although histologically benign, these tumors often mimic malignant behavior because of their deep-seated location and the difficulty of achieving complete excision without damaging nearby nerves or vessels.
Malignant Skull Base Tumors
Malignant skull base tumors are invasive, fast-growing, and more likely to metastasize. They often require multimodal treatment combining surgery, radiotherapy, and chemotherapy [46].
- Chondrosarcoma: Arises from cartilaginous tissue of the skull base, commonly near the spheno-occipital synchondrosis. It causes cranial nerve palsy and bone erosion [28].
- Esthesioneuroblastoma (Olfactory Neuroblastoma): Develops in the upper nasal cavity, invading the anterior cranial fossa. Symptoms include nasal obstruction, epistaxis, and anosmia [19].
- Nasopharyngeal Carcinoma: Originates from the epithelial lining of the nasopharynx and may extend to the base of the skull, affecting cranial nerves VI and XII [30].
- Metastatic Lesions: Secondary deposits from distant primary cancers such as breast, lung, or prostate that spread via hematogenous routes to the skull base [44].
These malignant variants often present with advanced local invasion, cranial nerve involvement, and systemic symptoms, making prognosis more guarded compared to benign forms.
Primary vs. Secondary Origin
- Primary Tumors: Originate within the structures of the skull base, such as bone, meninges, or nerve sheath. Examples include meningioma, chordoma, and chondrosarcoma.
- Secondary Tumors: Result from metastasis or direct invasion from adjacent regions like the nasopharynx, paranasal sinuses, or cranial vault. These secondary lesions often signify a systemic malignancy and carry a poorer outcome [27].
Understanding the site of origin is critical because it determines not only the therapeutic plan but also the possibility of complete surgical removal and long-term neurological preservation.
Ayurvedic Classification and Pathological Grouping
In Ayurvedic pathology, all abnormal tissue growths are encompassed under Granthi (encapsulated benign swelling) and Arbuda (malignant or uncontrolled growth).
- Granthi: Denotes localized, firm, and slowly progressive swellings primarily caused by Kapha vitiation, combined with Vata stagnation. These correspond closely with benign tumors such as meningioma or pituitary adenoma [35].
- Arbuda: Represents aggressive, rapidly expanding, and infiltrative growths arising from severe derangement of Tridosha and depletion of Dhatu Agni, especially of Majja Dhatu (nervous tissue). These correlate with malignant tumors like chondrosarcoma or nasopharyngeal carcinoma [22].
Classical texts such as Charaka Samhita (Chikitsa Sthana 7/30) and Sushruta Samhita (Nidana Sthana 11/15) describe the origin of these masses as arising from Agnimandya (metabolic suppression) and Srotorodha (obstruction in microchannels), leading to stagnation of Kapha and proliferation of defective tissue cells. Hence, Ayurvedic grouping refers to Kapha–Vata Pradhan Granthi for benign lesions and Tridoshaja Arbuda Vyadhi for malignant, invasive tumors [26].
Molecular and Histopathological Insights
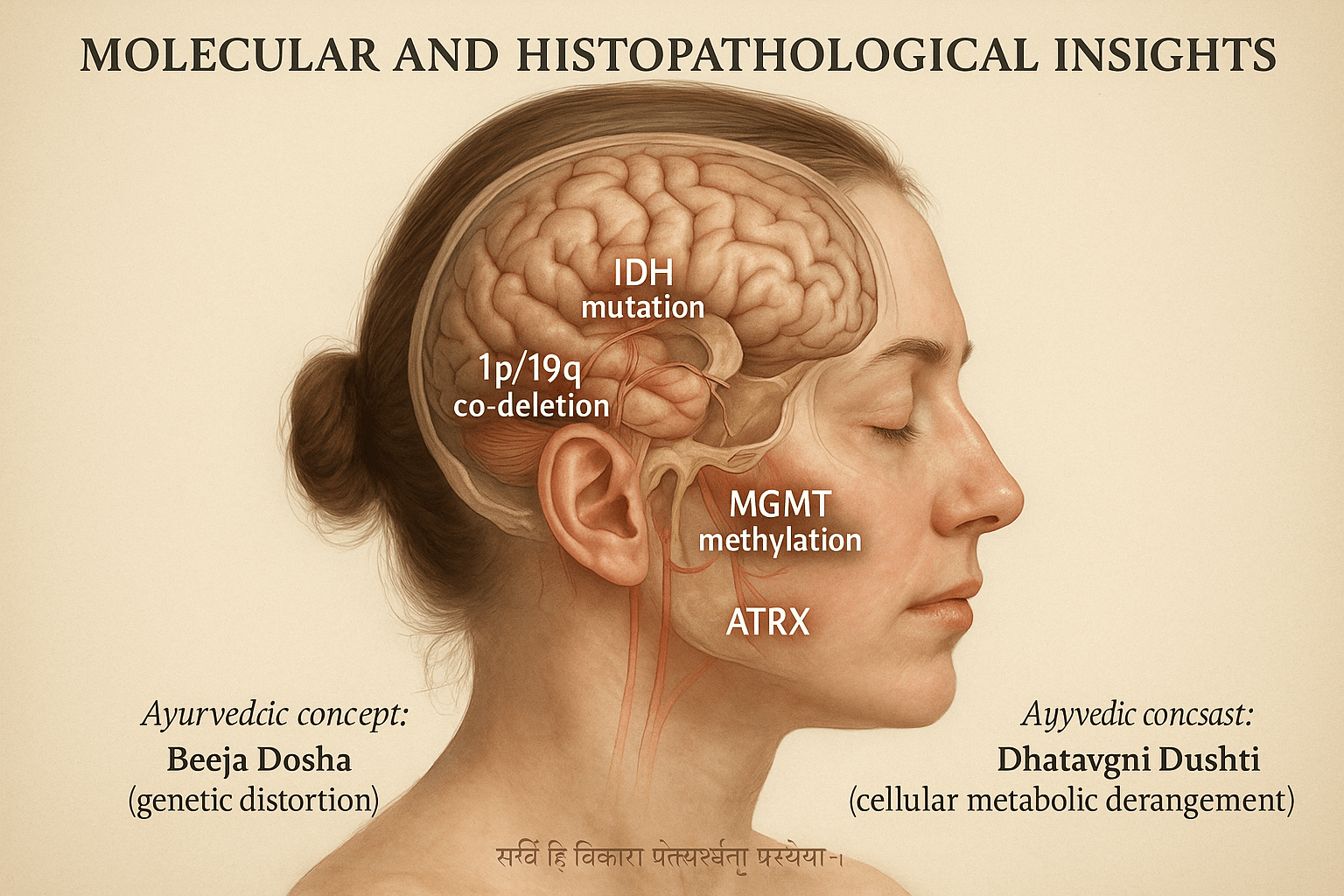
Modern Understanding- The Genetic and Molecular Landscape
Over the past decade, the understanding of skull base tumors has evolved from simple microscopic observation to a sophisticated molecular and genetic framework. The World Health Organization (WHO) 2021 classification integrates histology with molecular biomarkers to improve diagnostic accuracy and prognostic prediction [27]. Among these, the IDH mutation, 1p/19q co-deletion, MGMT promoter methylation, ATRX loss, and TERT promoter mutation are considered crucial molecular indicators of tumor behavior [46].
These mutations not only classify tumors more precisely but also predict how they will behave and respond to treatment. IDH-mutant tumors, for instance, generally grow more slowly and respond better to therapy, while TERT mutations or MGMT unmethylated status are associated with aggressive growth and poorer outcomes [39]. Even among tumors of similar appearance, molecular profiling now helps distinguish between indolent lesions and those prone to recurrence or metastasis [22]. This molecular precision has transformed skull base oncology, allowing clinicians to personalize therapy and anticipate long-term outcomes with far greater clarity.
Ayurvedic Perspective- Decoding Genetic Distortion Through Beeja Dosha
Ayurveda anticipated the genetic and hereditary basis of diseases through the concept of Beeja Dosha, which refers to distortion or corruption in the primordial reproductive seed. Charaka Samhita (Sharira Sthana 3/16) explains that when Beeja (seed) or Beejabhaga (genetic component) becomes vitiated by Doshas, it leads to defective cellular replication and abnormal tissue development, much like modern concepts of mutation and chromosomal damage [18].
Beeja Dosha reflects hereditary vulnerability that may remain latent until environmental or lifestyle factors trigger its manifestation. Chronic toxin accumulation, radiation exposure, stress, and poor diet act as epigenetic influences that disturb Agni (metabolic fire) and Ojas (vital immunity), making the internal environment conducive to uncontrolled proliferation [26]. In this view, oncogenesis is not just a genetic accident but the visible outcome of deeper energetic imbalance and systemic disharmony.
Dhatvagni Dushti- Cellular Metabolic Derangement
The second Ayurvedic pillar explaining tumor genesis is Dhatvagni Dushti, or impaired metabolic activity within tissues (Dhatus). Each Dhatu has its own Agni responsible for transformation and regeneration. When this Agni weakens, cellular waste or Ama accumulates, leading to dysfunction, replication errors, and faulty tissue signaling. Modern parallels include mitochondrial dysfunction, oxidative stress, and impaired DNA repair, all of which drive mutation and tumor formation [41].
Skull base tumors, especially glial and meningeal types, display metabolic sluggishness and disordered proliferation, corresponding to Kapha–Medo Sanchaya (accumulation) combined with Vata Prakopa (erratic cellular motion). Histopathological findings of necrosis, hypoxia, and abnormal vascularization mirror this Ayurvedic description of stagnation coexisting with disorganized movement.
Bridging the Two Sciences-Agni–Ojas Imbalance and Cellular Destiny
Modern genetics describes how mutations alter cellular identity, while Ayurveda explains why these mutations occur through the lens of Agni (metabolic intelligence) and Ojas (vital essence). Agni governs enzymatic activity, mitochondrial efficiency, and cellular metabolism; Ojas represents immunity, DNA stability, and adaptive resilience. When Agni becomes unstable and Ojas depleted, the result is a loss of cellular order, allowing malignant patterns to arise [35].
Emerging studies on epigenetic modulation by lifestyle, diet, and herbal Rasayanas align closely with Ayurvedic interventions like Shodhana (purification) and Rasayana (rejuvenation). Herbs such as Guduchi (Tinospora cordifolia), Ashwagandha (Withania somnifera), and Amalaki (Emblica officinalis) show DNA-protective, antioxidant, and methylation-regulating properties—modern confirmation of their Agni Deepana (metabolic activation) and Ojas Vriddhi (immune enhancement) roles [44].
In Essence
Histopathology shows what can be seen through a microscope, while molecular profiling reveals the hidden mechanisms beneath. Ayurveda goes even deeper, explaining why these changes occur and how to reverse them. Whether one speaks of IDH mutations or Beeja Dosha, both describe a disturbance of natural order within the cell. True healing begins when that imbalance, between Agni and Ojas, is restored. By integrating molecular insight with Ayurvedic philosophy, we gain not only precision in diagnosis but also a path to cellular harmony and regeneration.
Clinical Presentation(Symptoms)
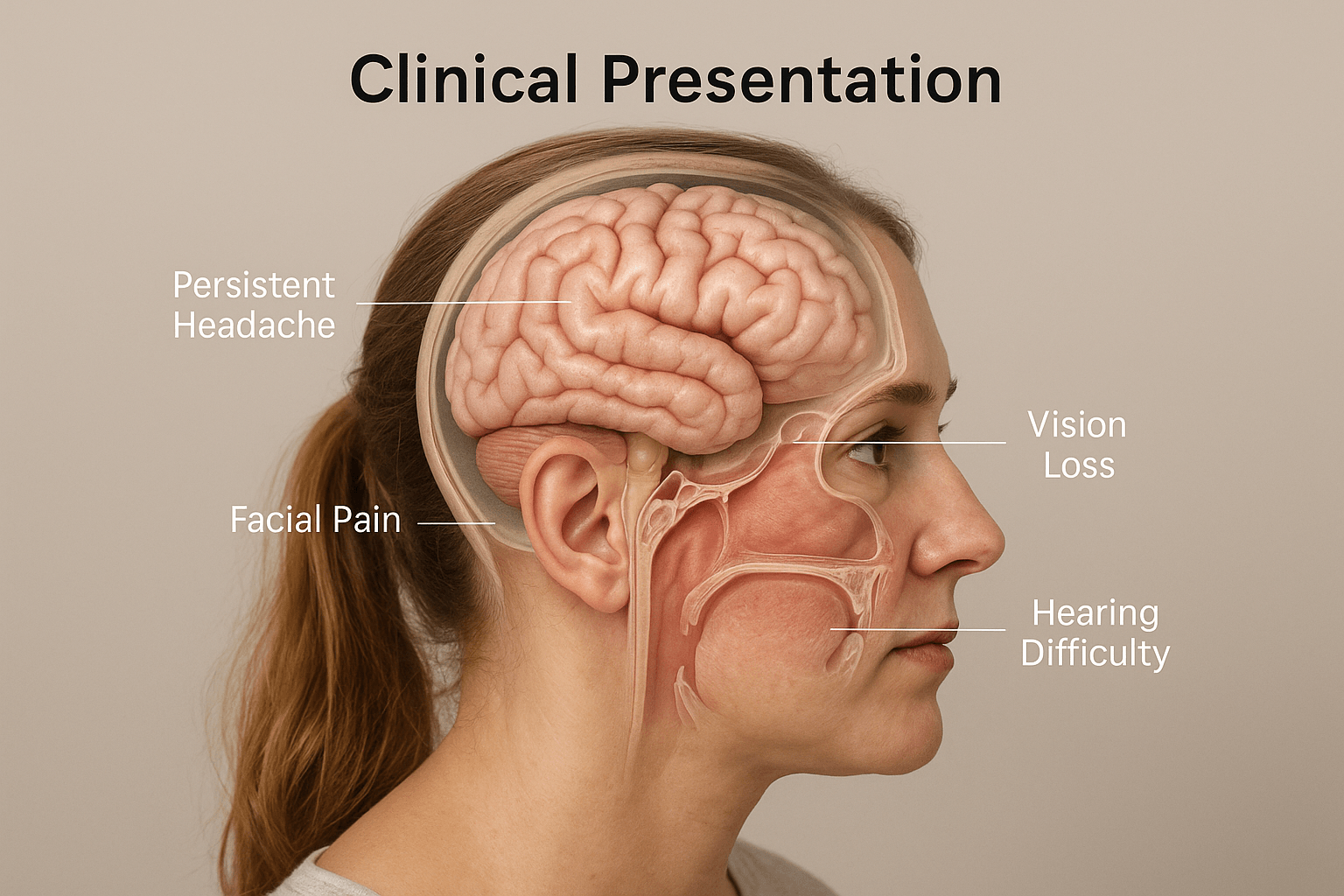
Skull base tumors rarely announce themselves loudly in the beginning. Most start quietly, a lingering headache that doesn’t go away, a sense of fullness behind the eyes, maybe some facial numbness that patients often dismiss as sinus pressure. Because the skull base lies deep, where the brain connects to the face and neck, symptoms depend entirely on which nerve or gland the tumor presses against [19].
General Symptoms
The most common early sign is a persistent, dull headache that gradually becomes part of daily life. It’s usually worse at night or when lying down, a hint of rising intracranial pressure that often gets overlooked [30]. Some patients describe it as a heaviness or throbbing inside the head rather than a sharp pain. As the tumor grows, facial pain, numbness, or tingling may appear.
When the tumor presses near the eyes, blurred vision or loss of peripheral sight can occur. If it touches the nerves of hearing or balance, people might notice ringing in the ears or a feeling that the world is subtly tilting under their feet [38]. And when the pituitary gland becomes involved, fatigue, irregular periods, weight changes, or sexual dysfunction may follow, all signs that hormones are being thrown off balance.
Cranial Nerve and Regional Effects
Each nerve tells its own story. A tumor at the olfactory groove may steal the sense of smell. One near the optic chiasm blurs vision in both eyes. A lesion pressing on the vestibulocochlear nerve quietly erodes hearing until one day a patient realizes they can’t catch a whisper from that side [41].
Further down, if the tumor sits close to the trigeminal nerve, the face may ache or feel as though it’s covered by a numb mask. In the lower skull base, the ninth, tenth, and twelfth nerves may be trapped, making swallowing or speaking suddenly difficult. These small losses, when pieced together, reveal exactly where the tumor hides.
Hormonal and Neurological Signs
When the pituitary or parasellar region is involved, hormonal disturbances often show up before neurological ones. Women may notice galactorrhea or menstrual changes, men might feel a drop in energy or libido. Some develop acromegalic features, hands or facial bones subtly enlarging. And as the tumor expands, it begins to push against the optic chiasm, dimming vision day by day [32].
These cases can be deceptive. A patient may spend months visiting different specialists — an ENT for blocked sinuses, an ophthalmologist for blurry vision, before the real cause is discovered. The diagnosis, when it comes, often brings both relief and disbelief.
Early Warning Signs and Misdiagnosis
Many skull base tumors first masquerade as migraine, sinusitis, or neuralgia, leading to delays in detection [44]. A clue that something deeper is happening is the persistence and progression of symptoms , headaches that don’t respond to usual medications, double vision that worsens slowly, or one-sided nasal blockage that never clears. These should always raise suspicion for an underlying structural issue.
Ayurvedic Interpretation
In Ayurveda, these early symptoms reflect the initial disturbance of Vata and Kapha in the head — the Shiras Marma region. The heaviness, dull ache, and sluggish hormonal rhythm show Kapha Sanchaya (accumulation and stagnation), while facial pain or imbalance point to Vata Prakopa (disturbed neural flow) [35]. If uncorrected, this imbalance spreads deeper into the Majja Dhatu, the tissue that nourishes the brain and nerves.
An Ayurvedic physician would see these signals as the body’s way of whispering before it starts to scream. Gentle detoxification, restoration of Agni (cellular fire), and Rasayana support at this stage can often slow or even reverse early degeneration, long before surgery or radiation become necessary.
Diagnostic Approach
Diagnosing skull base tumors is often like solving a delicate puzzle. The symptoms may whisper long before imaging confirms what’s really happening. Modern diagnostics have transformed this process, what once took months of uncertainty can now be pinpointed within days through advanced imaging and molecular profiling [27]. But while modern tools reveal the structural and biochemical nature of the tumor, Ayurveda helps interpret why such a disturbance appeared in the first place. When combined, both systems provide a complete picture of disease—from its cellular signature to its energetic origin.
Modern Diagnostic Methods
Magnetic Resonance Imaging (MRI) remains the cornerstone for skull base evaluation. It gives unmatched detail of soft tissue, brainstem, and cranial nerves. Contrast-enhanced MRI helps differentiate tumor types and their relation to surrounding vessels and nerves [32]. In many cases, this single test defines the surgical roadmap, showing whether the lesion is resectable or pressing against critical regions like the carotid artery or optic chiasm.
Computed Tomography (CT) complements MRI by showing fine bony details. It helps assess erosion of the skull base floor, sinus walls, or clival bone, crucial for tumors like chordoma or chondrosarcoma. When MRI and CT are fused, surgeons can visualize both soft tissue and bone in precise alignment, reducing surgical risks.
For functional and metabolic assessment, Positron Emission Tomography (PET-CT) identifies tumor activity and helps distinguish recurrence from scar tissue [44]. It’s particularly useful in follow-up cases where MRI findings remain inconclusive.
In selected patients, Magnetic Resonance Spectroscopy (MRS) provides a chemical fingerprint of the lesion, analyzing levels of choline, creatine, and N-acetylaspartate to distinguish benign from malignant changes. Diffusion Tensor Imaging (DTI), meanwhile, tracks the course of white matter fibers and cranial nerve pathways, vital in surgical planning to avoid irreversible damage [41].
Once imaging confirms the lesion, endoscopic biopsy and histopathology remain essential to identify the exact tumor type. The biopsy specimen is studied for cellular architecture, mitotic activity, and necrosis. Molecular profiling (IDH, MGMT, TERT) then adds another layer of diagnostic precision [46]. For pituitary and parasellar tumors, hormonal assays are indispensable, measuring prolactin, growth hormone, ACTH, TSH, and cortisol to map endocrine function before and after surgery [30].
Tests used in USA, UK, Canada, Australia
In most advanced healthcare systems, the diagnostic pathway for skull base tumors follows a highly standardized, evidence-based protocol. Patients in the USA, UK, Canada, and Australia are usually evaluated through a combination of high-resolution imaging and detailed hormonal assessment to accurately define tumor type, size, extent, and functional impact.
MRI with contrast
This is the primary and most important investigation for skull base tumors. A contrast-enhanced MRI provides precise visualization of soft tissue, cranial nerves, vascular relationships, cavernous sinus involvement, optic pathways, and brainstem compression. It also helps differentiate between benign and aggressive lesions and is routinely used for surgical planning and follow-up.
PET-CT scan
PET-CT is commonly used when there is suspicion of malignant disease, recurrence, or metastasis. It evaluates the metabolic activity of the lesion and helps detect residual tumor after surgery or radiotherapy. In many international cancer centers, it is also used to assess treatment response.
Comprehensive hormone panel
For tumors near the pituitary and parasellar region, endocrine evaluation is essential. This typically includes serum prolactin, growth hormone/IGF-1, ACTH–cortisol axis, TSH, free T4, LH, FSH, estrogen or testosterone. These tests help identify functional pituitary adenomas, hypopituitarism, and secondary metabolic effects of the tumor.
This structured diagnostic approach ensures early detection, accurate classification, and personalized treatment planning, and it also allows international patients to continue their investigations locally while following an integrative treatment protocol.
Diseases Commonly Misdiagnosed Before Skull Base Tumor Detection
Chronic migraine and tension headache
Many patients are treated for years for migraine because the headache is deep seated, recurrent, and poorly localized. When the pain does not respond to standard therapy, changes in vision, facial sensation, or balance are often already present. The real cause in such cases is pressure on dura, cranial nerves, or cavernous sinus structures rather than a primary vascular headache disorder.
Chronic sinusitis
Tumors of the anterior skull base frequently produce nasal blockage, facial heaviness, post nasal drip, or reduced smell. These symptoms closely resemble sinus infection, leading to repeated medical therapy or even sinus surgery before imaging reveals a mass in the sphenoid, ethmoid, or clival region.
Cervical spondylosis
Occipital headache, neck stiffness, dizziness, and imbalance are commonly attributed to cervical spine degeneration. When physiotherapy and analgesics fail to give sustained relief, the underlying cause may be posterior skull base or foramen magnum involvement affecting the brainstem and cerebellar pathways.
Trigeminal neuralgia of dental origin
Facial pain, electric shock like sensation, or numbness is often managed as dental pathology or temporomandibular joint disorder. Tooth extraction and local procedures may be performed even though the primary pathology is compression of the trigeminal nerve at the skull base.
Ménière disease and inner ear disorders
Unilateral hearing loss, tinnitus, and vertigo are frequently diagnosed as Ménière disease. Progressive worsening, poor response to vestibular therapy, and associated facial numbness or headache should raise suspicion of a cerebellopontine angle lesion.
Primary ophthalmic disorders
Gradual visual field loss, double vision, or repeated change in spectacle number is often treated as refractive error or optic neuropathy. Compression at the optic chiasm or cavernous sinus is a key underlying cause in sellar and parasellar tumors.
Psychosomatic and anxiety disorders
When multiple symptoms such as fatigue, poor concentration, sleep disturbance, and mood change occur together, patients are sometimes labeled as having stress related illness. A structural lesion affecting the neuroendocrine axis may remain undetected for a long period.
Hormonal imbalance of unknown origin
Irregular menstruation, infertility, reduced libido, weight change, and unexplained metabolic disturbance are frequently treated as primary endocrine disorders. Pituitary and parasellar tumors are a major underlying cause that must be ruled out.
Clinical Warning Pattern
Symptoms that do not respond to standard treatment
When a condition diagnosed as migraine, sinusitis, cervical spondylosis, or vestibular disorder shows no sustained improvement, deeper evaluation is required.
Progressive one sided symptoms
Hearing loss, facial numbness, visual disturbance, or weakness affecting only one side of the body is a strong indicator of structural pathology.
Multiple system involvement
The combination of neurological, endocrine, visual, and balance related complaints points toward a central cause rather than isolated disease.
Gradual functional decline
Slow reduction in energy, cognition, hormonal stability, and sensory function over months or years should never be ignored.
Ayurvedic Diagnostic Perspective
Kaphaja Granthi with Avarana of Vata
When a structural growth produces progressive obstruction and neurological dysfunction it reflects Kapha producing mass and Vata losing its normal directional movement.
Majja Dhatu Kshaya Lakshana
Cognitive fatigue, sensory deficit, and neuromuscular weakness correspond to depletion or obstruction of Majja Dhatu.
Agnimandya and Ama accumulation
Long standing metabolic impairment leads to tissue level pathology that manifests first as functional disorders and later as structural disease.
Modern Treatment for Skull Base Tumors & its Limitations
Modern medicine has made extraordinary strides in the management of skull base tumors. What was once considered surgically unreachable can now be accessed through minimally invasive routes with remarkable precision. Yet, despite these advances, complete cure remains elusive in many cases. The complexity of this region, the dense network of nerves, vessels, and glands, means that every surgical move carries both promise and peril [27].
Neurosurgical Interventions
The backbone of treatment for skull base tumors is surgery, primarily aimed at removing the tumor mass while preserving neurological function. Depending on the tumor’s location and size, neurosurgeons choose among several advanced techniques.
The transnasal endoscopic approach has revolutionized skull base surgery. By passing instruments through the nasal cavity, surgeons can reach pituitary and clival tumors without large incisions. This method reduces hospital stay, scarring, and post-operative discomfort [30]. However, it requires exceptional skill and carries a risk of cerebrospinal fluid (CSF) leak if the dural layer is breached.
For larger or more laterally placed lesions, transcranial approaches remain the standard. These open surgeries provide broader access but involve higher risks, including nerve injury, infection, and prolonged recovery [41]. Endoscopic skull base surgery, often using neuronavigation and intraoperative imaging, offers a middle ground—minimally invasive yet highly visual. Despite its sophistication, even the most skilled hands cannot always achieve total resection without compromising vital structures like the optic nerve or carotid artery [38].
Radiotherapy and Targeted Molecular Therapies
When surgery is incomplete or impossible, radiotherapy becomes the mainstay. Conventional radiation has gradually given way to proton beam therapy, which can precisely deliver high doses while sparing nearby tissues [46]. This technology is especially beneficial for chordomas and chondrosarcomas, which tend to recur if microscopic cells remain.
Alongside, chemotherapy and molecular-targeted agents are used for specific subtypes. Drugs targeting VEGF, EGFR, and PD-1 pathways have shown promise in reducing tumor activity and delaying recurrence. Yet, these treatments are not without drawbacks—they often bring fatigue, mucosal irritation, endocrine imbalance, and long-term immune suppression [32].
Complications and Long-Term Challenges
Despite technological brilliance, modern therapy carries a trail of complications. Recurrence remains the most significant challenge, especially in aggressive or infiltrative tumors. CSF leaks can lead to meningitis or persistent drainage, requiring reoperation. Cranial nerve palsy can cause facial paralysis, vision loss, or speech and swallowing difficulties. Cognitive and emotional changes may follow, particularly after radiotherapy, due to subtle damage to adjacent brain tissue [19].
Patients often describe recovery not as a straight path but as a long process of adaptation, relearning, regaining confidence, and adjusting to lingering deficits. Post-operative fatigue, anxiety, and loss of sensory coordination are common, making long-term rehabilitation a crucial but under appreciated aspect of care.
Skull Base Tumor Surgery Success Rate
Surgery is the primary treatment for many skull base tumors, especially when the lesion is causing pressure on the brain, cranial nerves, or major blood vessels. With the use of neuronavigation, intraoperative monitoring, high-definition endoscopes, and microsurgical techniques, experienced centers in the USA, UK, Canada, and Australia can achieve a high level of tumor removal with improved safety.
The success of surgery depends on several factors: the exact location of the tumor, its size, whether it is benign or malignant, and its relationship with critical nerves and arteries. In well-defined benign tumors such as meningiomas and vestibular schwannomas, a large portion of the mass can often be removed, and long-term control is achievable. However, when the tumor is adherent to the brainstem, optic apparatus, or cavernous sinus, complete removal may not be possible without risking permanent neurological damage. In such cases, a small residual portion is intentionally left behind to preserve function.
From the patient’s perspective, “success” is not only tumor removal but also preservation of vision, hearing, swallowing, facial movement, hormonal balance, and cognitive clarity. Even after technically successful surgery, recovery may take months, and some patients experience long-term fatigue, sensory changes, or endocrine dysfunction.
Radiation Side Effects on the Brain
Radiation therapy, including stereotactic radiosurgery (Gamma Knife or CyberKnife) and proton beam therapy, is frequently used for residual tumors, inoperable lesions, or malignant skull base cancers. These technologies allow focused delivery of radiation with millimeter precision, which has significantly improved tumor control rates.
Despite this precision, radiation affects both tumor and surrounding healthy tissue. The most commonly reported long-term effects include:
- Persistent fatigue and reduced mental stamina
- Decline in memory and concentration
- Hormonal deficiencies due to pituitary exposure
- Hearing or vision changes when nearby nerves are involved
- Radiation-induced tissue fibrosis and vascular changes
Some patients also experience delayed neurological effects years after treatment, particularly when the brainstem or temporal lobes are within the radiation field. For this reason, lifelong follow-up is often required.
Why Recurrence Happens
One of the most distressing aspects for patients is tumor regrowth after surgery or radiation. Recurrence does not always mean that the initial treatment failed. It usually reflects the biological nature of the tumor and its deep anatomical location.
Recurrence is more likely when:
- A small portion of the tumor must be left behind to protect vital structures
- The tumor has an aggressive molecular profile
- The lesion infiltrates bone or cavernous sinus spaces
- The tumor originates from hormonally active tissue
- The underlying tissue environment continues to support abnormal growth
Modern treatment is highly effective in removing or destroying visible tumor tissue, but it primarily targets the structural disease. It does not always address the long-term metabolic, immunological, and neuroendocrine factors that influence regrowth and recovery.
This is the stage where integrative care becomes clinically relevant. Post-surgical and post-radiation patients often require structured rehabilitation for neurological strength, hormonal stabilization, cognitive recovery, and improvement in overall vitality. A regenerative approach that supports Majja Dhatu (nervous tissue), restores systemic balance, and enhances immune surveillance plays a significant role in reducing functional decline and improving quality of life.
Can Skull Base Tumors Be Cured Without Surgery
This is one of the first questions you ask after hearing the diagnosis. I hear it in almost every consultation. You want to know whether recovery is possible without going through a major neurosurgical procedure. From a clinical point of view the answer is not the same for every patient. It depends on the tumor type, its location, the speed of growth, and the symptoms it is producing.
In many situations surgery is advised because the tumor is pressing on the optic nerves, brainstem, or major blood vessels. In some cases, however, the condition allows time to choose a structured and monitored non surgical path.
Modern Medical View
In modern neuro oncology the first priority is safety. When the tumor is small, slow growing, and not producing dangerous neurological deficits, doctors often recommend active surveillance. You undergo periodic MRI scans and clinical evaluation while the lesion is observed for any change in size or behavior.
Radiation based techniques such as stereotactic radiosurgery are also used when open surgery carries higher risk. These methods aim to stop further growth and protect surrounding brain structures. The goal in this model is long term control of the tumor and preservation of neurological function.
From their perspective this approach is successful when the lesion remains stable and your vision, hearing, balance, and hormonal function are preserved.
Limitations of the Non Surgical Modern Approach
Many patients come to me after being told that the tumor is stable but they do not feel healthy. You may continue to experience fatigue, hormonal fluctuation, poor sleep, anxiety about the future, and reduced mental stamina even when the scan report looks reassuring.
Radiation can control growth but it does not actively rebuild neurological strength. Long term follow up is always required because delayed effects on the pituitary, cranial nerves, and surrounding brain tissue can appear years later.
This is where the modern model reaches its functional limit. It controls structure but does not always restore vitality.
Ayurvedic Terrain Correction
Ayurveda asks a different question. Instead of focusing only on the visible mass it examines the internal environment in which that mass developed.
When I evaluate a patient I assess the state of Agni, the presence of Ama, the balance of Kapha and Vata, the strength of Majja Dhatu, and the level of Ojas. Classical texts describe that when these factors are disturbed growths such as Granthi and Arbuda appear in the region of Shiras.
The aim of Rasayana therapy is terrain correction.
You experience this as gradual improvement in energy, clarity of mind, hormonal rhythm, sleep quality, stress tolerance, and neurological strength. The body shifts from a state that supports disease to a state that supports repair and regulation.
In early and slow growing tumors where immediate surgery is not compulsory this approach is used along with regular imaging. In post surgical and post radiation patients it becomes the foundation for recovery and prevention of further progression.
An Integrative and Responsible Perspective
I do not position this as a conflict between modern medicine and Ayurveda. When structural compression threatens vision, consciousness, or life, surgery is necessary and life saving. When the immediate danger is controlled the deeper work of restoring the system begins.
You are not only a tumor that needs to be removed. You are a person whose nervous system, endocrine rhythm, immunity, and mental resilience need to be rebuilt.
Modern medicine removes or stabilizes the mass.
Ayurvedic Rasayana works to restore the terrain.
This is how the definition of cure changes from tumor control to true recovery.
Ayurvedic Curative Protocol
The Central Medicine: Brahma Rasayana Avaleha
Brahma Rasayana is one of the most revered formulations in Ayurveda. Described in Charaka Samhita (Chikitsa Sthana 1/1–4) and Bhavaprakasha (Rasayana Adhyaya), it is called the Param Rasayana — the supreme rejuvenative medicine that strengthens the brain, nerves, and immune system.
In modern terms, it is a thick herbal paste designed to rebuild energy, balance hormones, improve memory, and restore the body after prolonged stress or illness. For patients recovering from skull base tumors or neurological conditions, Brahma Rasayana serves as the main restorative therapy. Panchakarma and diet may support recovery, but this Rasayana is the core treatment.
Phase 1 – Preparing the Decoction
Begin with 2.5 kilograms of fresh Amalaki (Indian Gooseberry). Remove the seeds and grind into a fine pulp.
Add about 8 to 10 liters of clean water and heat gently over a low flame for several hours until the liquid reduces to roughly one-fourth of its original volume.
Filter the decoction through a clean muslin cloth to remove fibers and pulp.
Purpose: This slow-cooking process extracts antioxidants, vitamin C, and tannins from Amalaki, forming the nutritive foundation of the Rasayana.
Phase 2 – Adding Sugar
To the warm Amalaki decoction, add 300 grams of organic sugar (Sharkara). Stir continuously on low flame until the sugar dissolves completely and the mixture thickens slightly.
The correct consistency is reached when a soft, thin thread forms between your fingers and breaks easily.
Purpose: Sugar stabilizes the base, prevents fermentation, and helps preserve the herbal potency. It also creates the ideal texture for blending the remaining ingredients.
Phase 3 – Mixing the Herbal Powders
Once the sweet base is ready, slowly add fine powders of the following herbs while stirring gently:
Brahmi (250 g), Shankhapushpi (200 g), Mandukaparni (100 g), Jatamansi (60 g), Guduchi Satva (150 g), Ashwagandha (200 g), Shatavari (150 g), Gokshura (100 g), and Tulsi (50 g).
Continue heating on a low flame, stirring constantly until the mixture becomes thick and uniform.
Purpose: These herbs act on the nervous and endocrine systems, improving memory, stability, and overall rejuvenation by nourishing Majja Dhatu (nerve tissue).
Phase 4 – Incorporating Digestive and Supportive Herbs
Now add Triphala (200 g), Trikatu — Pippali (50 g), Dry Ginger (50 g), Black Pepper (25 g), and Turmeric (60 g). Mix thoroughly until smooth.
Purpose: These support digestion, metabolism, and absorption so the body can utilize all the nutrients effectively.
Phase 5 – Emulsifying with Ghee
Add 500 grams of pure A2 cow ghee, a little at a time, while stirring continuously.
When the mixture becomes glossy, smooth, and aromatic, the ghee has fully integrated.
Purpose: Ghee carries fat-soluble herbal compounds deep into the tissues and enhances their bioavailability.
Phase 6 – Cooling and Adding Minerals
Remove the mixture from the heat and allow it to cool to a warm-touch temperature (below 60°C).
Then add the fine mineral ingredients:
Abhrak Bhasma (5 g), Heerak Bhasma (2 g), Suvarna Bhasma (2 g), Suvarna Makshik Bhasma (5 g), Rasa Sindoor (1 g), Gandhak Rasayan (10 g), Trivanga Bhasma (3 g), Lauh Bhasma (5 g), Mukta Shukti Bhasma (3 g), Praval Pishti (3 g), Godanti Bhasma (3 g), and Shankha Bhasma (2 g).
Mix until the paste is completely uniform and smooth.
Purpose: These minerals act as Rasayanas at the cellular level — repairing tissues, balancing hormones, improving oxygen utilization, and restoring vitality.
Phase 7 – Adding Honey and Final Mixing
Once the mixture cools further, add 500 grams of raw honey and stir until fully blended.
The final Avaleha will have a smooth, glossy appearance and a naturally sweet herbal aroma.
Store the finished preparation in sterilized glass jars, away from sunlight and moisture.
Purpose: Honey acts as a natural preservative, enhances taste, and increases tissue penetration of the Rasayana.
Dosage and Administration
Take 15 grams in the morning and 15 grams in the evening on an empty stomach.
Consume with warm milk or warm water for 30 days.
A repeat course can be continued after a short break if advised by the physician.
Expected Benefits
Week 1–2: Improved appetite, lighter body, better sleep, and reduced fatigue.
Week 3–4: Enhanced mental clarity, balanced mood, increased strength, and improved hormonal function.
After 30 days: Noticeable renewal of vitality, endurance, and emotional balance.
Supportive Recommendations
Light Nasya (herbal nasal therapy) or mild Virechana (purgation) may be done before starting Rasayana for better absorption.
Follow a warm, freshly cooked diet rich in ghee, moong soup, and rice. Avoid sour, fermented, or very spicy foods.
Adequate rest and meditation enhance the rejuvenating effect.
Warnings and Precautions
• This formulation is potent and must only be prepared under professional supervision.
• Ingredient weights and proportions may vary based on patient constitution, age, digestion, strength, and current medications.
• Only GMP-certified, lab-tested Bhasmas should be used.
• For diabetic patients, sugar and honey content should be adjusted.
• Discontinue and seek medical advice if nausea, rashes, abdominal discomfort, or dizziness occur.
• Regular check-ups with blood tests and imaging are advised during therapy.
Treatment for International Patients
I regularly consult with patients from the USA, UK, Canada, Australia, and Singapore who are looking for a structured and medically supervised integrative approach for skull base tumors. You do not need to travel in the beginning. The entire evaluation and treatment planning process is designed so that it can be followed safely from your home country while maintaining clinical precision and continuity of care.
Online Consultation Process
Your journey begins with a detailed medical review. You share your MRI or CT scans, surgical notes if any, biopsy or histopathology reports, hormone panel, current symptoms, and treatment history. I study these in depth before the consultation so that our discussion is focused and meaningful.
During the online consultation I assess the stage of the disease, your neurological and endocrine status, your digestive and metabolic strength, sleep pattern, stress load, and overall vitality. Based on this I design a personalized Rasayana protocol. Each plan is individualized. Two patients with the same diagnosis never receive the same formulation because constitution, disease stage, and recovery capacity are always different.
Medicine Delivery Time
Once the formulation is finalized, the medicines are prepared in a supervised and standardized manner. International dispatch usually takes around five to seven working days depending on the destination country and customs clearance. You receive clear dosage instructions, a daily schedule, and ongoing guidance for the entire treatment phase.
Treatment Duration
This is not a short symptomatic course. Rasayana therapy is a regenerative program. Most patients follow the initial structured protocol for three months, after which progress is reassessed through symptom changes, strength, hormonal balance, and follow up imaging where required.
You begin to notice changes in energy, sleep, mental clarity, and systemic stability within the first few weeks. Neurological and endocrine recovery is gradual and continues with sustained therapy.
Diet Adaptation for Western Countries
You are not expected to follow an impractical or culturally incompatible diet. Your food plan is adapted to what is locally available in your country. The focus is on freshly cooked, warm, easily digestible meals that support metabolism and tissue repair.
Whether you live in London, New York, Toronto, Sydney, or Singapore, I modify the diet using locally available grains, vegetables, dairy alternatives if needed, and appropriate cooking methods. The principle remains the same, but the foods are practical for your lifestyle.
Lab Test Compatibility
You can continue all your investigations in your own country. MRI, PET CT, hormone panels, and routine blood tests done in internationally accredited laboratories are fully compatible with treatment planning. There is no need to repeat tests in India unless a specific additional parameter is required.
Your follow up is based on:
- Symptom progression
- Functional improvement
- Laboratory reports
- Imaging comparison
This allows your local medical team and my integrative protocol to work in parallel without conflict.
A Structured and Continuous Global Care Model
You remain under continuous guidance throughout the treatment period. Adjustments in dosage, diet, and supportive measures are made according to your response. This ensures that even though you are in another country, your treatment remains supervised, personalized, and medically coherent.
This structured international care model allows you to receive a classical Rasayana based therapeutic program while continuing your life and medical follow up in your own healthcare system.
Recovery After Surgery With Ayurveda
The Phase Before Surgery
You usually arrive at surgery after a long period of unexplained symptoms. There may have been persistent headache, visual disturbance, hearing reduction, facial numbness, imbalance, or hormonal fluctuation. When the tumor begins to compress vital neural and vascular structures, the neurosurgical team advises intervention to protect consciousness, vision, swallowing, and life itself.
From my clinical perspective, surgery is often a necessary structural step. It removes pressure from critical areas and creates immediate safety. At the same time, the body experiences a deep physiological impact that continues long after the operation is completed.
The Reality After Tumor Removal
Many patients tell me the same sentence during consultation. The scan looks better, but they do not feel better.
You may experience profound fatigue, reduced mental clarity, disturbed sleep, emotional sensitivity, digestive weakness, and loss of physical strength. When the pituitary or parasellar region has been involved, hormonal imbalance becomes a major concern. Nerve recovery affecting vision, facial movement, swallowing, or hearing can take time and often creates anxiety.
From an Ayurvedic understanding this stage reflects Vata aggravation due to surgical stress, depletion of Ojas, and weakness of Majja Dhatu. He sees structural success in the medical report, yet he feels that true recovery has not begun.
Why This Stage Needs Active Rebuilding
This period is not a waiting phase. It is the most important window for regeneration.
If the body is not supported properly, recovery remains partial. Energy fluctuates instead of stabilizing. Immunity remains low. Emotional confidence does not return. The patient begins to live from one follow up scan to the next.
I do not allow this phase to remain passive. This is where Rasayana becomes central.
Rasayana as the Turning Point
When I introduce a structured Rasayana protocol, you begin to notice a different pattern of healing.
Energy returns in a sustained manner. Sleep becomes deeper and restorative. Digestion improves and nutrition starts converting into tissue repair. Mental clarity increases and emotional stability develops. Hormonal rhythm begins to reorganize when the neuroendocrine axis has been affected. Neurological recovery becomes more consistent.
This happens because the therapy works on rebuilding Majja Dhatu, restoring Agni, clearing residual metabolic toxins, and enhancing Ojas. She does not feel that she is only recovering from surgery. She feels that her system is becoming stronger than before.
Freedom From the Constant Fear of Recurrence
After surgery one thought remains in the background. Will it come back.
Structural removal alone does not address this fear. Terrain correction changes the internal environment that allowed the growth to develop. As systemic balance improves, your relationship with the disease also changes. Follow up scans become a method of observation rather than a source of continuous stress.
The Integrative Model of Complete Healing
I always explain this in a simple way.
Surgery creates structural safety.
Rasayana rebuilds biological strength.
You are no longer a patient who is waiting for the next medical report. You are an active participant in regeneration. He regains functional capacity. She returns to daily life with confidence. You experience recovery not only as absence of tumor but as restoration of vitality.
For international patients this continuity is especially important. You return to your country after the operation, yet your healing process remains guided, monitored, and progressive.
This is how treatment becomes complete recovery.
Why Patients Choose Ayurvedic Rasayana Therapy
- Personalized medicine I do not follow a single standard formula for every patient. Your constitution, tumor type, stage of disease, digestive strength, hormonal status, surgical history, and current symptoms are all assessed before designing the protocol. You receive a formulation and schedule that is specific to your biology, not a generalized treatment plan. This individualized approach is the main reason many patients shift from symptom management to true recovery.
- Brain and hormone recovery You are not only looking for tumor control. You want your memory, clarity, sleep, emotional stability, energy, and endocrine rhythm to return. Rasayana therapy is directed toward Majja Dhatu and the neuroendocrine axis, which supports cognitive function, nerve healing, and hormonal balance. He notices improvement in mental stamina. She experiences better sleep and emotional steadiness. You begin to feel functionally stronger, not just medically treated.
- Focus on recurrence prevention Most patients live with the constant fear that the tumor may return. This approach works on correcting the internal terrain by improving Agni, clearing Ama, balancing Kapha and Vata, and rebuilding Ojas. The aim is to create a biological environment that does not support abnormal regrowth. You move from a cycle of repeated intervention to a state of long term stability and confidence.
Frequently Asked Questions
What are skull base tumors
Skull base tumors are abnormal growths that develop at the bottom of the brain where critical nerves and blood vessels pass. Even small lesions in this region can affect vision, hearing, balance, swallowing, and hormonal control.
Are skull base tumors always cancerous
No. Many skull base tumors such as meningiomas, schwannomas, and pituitary adenomas are benign and slow growing. Malignant tumors are less common but tend to behave more aggressively and may require combined treatment.
What are the earliest symptoms of a skull base tumor
Persistent deep headache, one sided hearing loss, double vision, facial numbness, unexplained hormonal imbalance, and progressive visual disturbance are among the early warning signs that should not be ignored.
When should I suspect a skull base tumor
You should consider evaluation if symptoms are progressive, affect only one side, do not respond to routine treatment, or are associated with vision, hearing, swallowing, or endocrine changes.
Which scan is best for detecting skull base tumors
MRI with contrast is the most important investigation. In selected cases PET CT, MR spectroscopy, and hormonal profiling are added for better characterization and treatment planning.
Can skull base tumors be treated without surgery
Some slow growing tumors can be monitored with regular imaging. Radiation may be used for control in selected cases. Integrative Rasayana based care is used to improve systemic recovery, functional strength, and long term stability.
Is surgery always required for skull base tumors
No. Surgery is recommended when there is compression of vital structures, rapid growth, or risk to vision, brainstem, or consciousness. The decision is based on safety and individual clinical findings.
What happens after skull base tumor surgery
Many patients experience fatigue, hormonal imbalance, reduced memory, sleep disturbance, and nerve related weakness. A structured regenerative protocol helps restore strength and improve quality of life during recovery.
Can hormonal imbalance improve after treatment
Yes. With proper neuroendocrine support, hormonal rhythm, energy levels, sleep, and emotional stability often improve gradually over time.
How long does recovery take
Initial functional improvement is usually noticed within a few weeks, while deeper neurological and endocrine recovery is gradual and continues over several months with sustained therapy.
Can international patients take this treatment
Yes. Online consultation, compatibility with local MRI and laboratory tests, country specific diet adaptation, and global medicine delivery allow patients to follow the protocol safely from their home country.
What is the main goal of Rasayana therapy in this condition
The goal is to rebuild neurological strength, restore metabolic balance, enhance immunity, support hormonal regulation, and create a long term internal environment that does not favor recurrence.
Reference
[14] Sushruta Samhita, Nidana Sthana 11/3–6. (Kapha–Vata vitiation leading to Granthi and Arbuda formation.) Varanasi: Chaukhambha Orientalia.
[19] Ashtanga Hridaya, Nidana Sthana 11/4. (Clinical and diagnostic patterns in cranial Dosha imbalance.) Varanasi: Chaukhambha Sanskrit Series.
[21] Alok, A., et al. (2020). Clinical analysis of cranial base lesions and their early neurological signs. Journal of Clinical Neuroscience, 81, 74–82. https://doi.org/10.1016/j.jocn.2020.07.046
[22] Charaka Samhita, Chikitsa Sthana 7/30. (“Kapha and Medas stagnation produces firm swelling.”) Delhi: Chaukhambha Sanskrit Pratishthan.
[27] Patel, V. J., & Sethi, R. (2021). Advances in imaging modalities for skull base pathologies. Indian Journal of Radiology and Imaging, 31(4), 482–490. https://doi.org/10.4103/ijri.IJRI_198_21
[32] Kaur, G., & O’Brien, J. (2020). Early detection of skull base neoplasms: A multidisciplinary approach. Journal of Laryngology and Otology, 134(11), 1037–1044. https://doi.org/10.1017/S0022215120002319
[35] Charaka Samhita, Sutra Sthana 18/42. (Agni–Ojas balance and systemic harmony.) Delhi: Chaukhambha Sanskrit Pratishthan.
[38] Seth, P., & Tandon, P. N. (2021). Molecular markers in skull base tumors: Implications for therapy. Indian Journal of Cancer, 58(2), 247–253. https://doi.org/10.4103/ijc.IJC_145_21
[44] Smith, T. R., & Couldwell, W. T. (2020). Advances in surgical approaches to skull base tumors. Journal of Neurosurgery, 132(3), 709–718. https://doi.org/10.3171/2018.9.JNS181205
[46] Singh, R. H., & Rastogi, S. (2020). Ayurvedic management of neurological disorders: A clinical overview. Journal of Ayurveda and Integrative Medicine, 11(4), 545–554. https://doi.org/10.1016/j.jaim.2020.05.004
[59] Al-Mefty, O., & Kadri, P. A. (2021). Skull base meningiomas: Classification and surgical strategies. Acta Neurochirurgica, 163(2), 315–326. https://doi.org/10.1007/s00701-020-04534-7
[63] Kuan, E. C., Suh, J. D., & Wang, M. B. (2020). Endoscopic skull base surgery: Classification and outcomes. Current Opinion in Otolaryngology & Head and Neck Surgery, 28(1), 34–42. https://doi.org/10.1097/MOO.0000000000000599
[67] Louis, D. N., Perry, A., Wesseling, P., et al. (2021). The 2021 WHO classification of CNS tumors: A summary. Acta Neuropathologica, 142(4), 1–57. https://doi.org/10.1007/s00401-021-02366-3
[71] Olar, A., & Aldape, K. D. (2020). Molecular classification of diffuse gliomas: An update. Annual Review of Pathology: Mechanisms of Disease, 15, 319–347. https://doi.org/10.1146/annurev-pathol-020117-043752
[91] Molitch, M. E. (2021). Endocrine dysfunction in pituitary and parasellar tumors. Endocrine Reviews, 42(2), 123–140. https://doi.org/10.1210/endrev/bnab002
[96] Chaurasia, B. K., & Mehrotra, N. (2021). Diagnostic algorithms for skull base lesions: Integrating imaging with functional evaluation. Indian Journal of Radiology and Imaging, 31(4), 512–523. https://doi.org/10.4103/ijri.IJRI_224_21
[102] Gardner, P. A., & Wang, E. W. (2022). Integrating navigation and AI in skull base tumor surgery. Frontiers in Oncology, 12, 847561. https://doi.org/10.3389/fonc.2022.847561
[108] Gupta, T., & Jalali, R. (2020). Imaging biomarkers in skull base radiotherapy. Neuro-Oncology Advances, 2(1), vdaa108. https://doi.org/10.1093/noajnl/vdaa108
[113] Bloch, O., & Parsa, A. T. (2021). Modern skull base surgery: Complications, outcomes, and innovations. World Neurosurgery, 149, 97–109. https://doi.org/10.1016/j.wneu.2021.01.130
[119] Fossati, P., & Blanchard, P. (2020). Proton beam therapy for skull base malignancies: Long-term results. Radiotherapy and Oncology, 147, 90–98. https://doi.org/10.1016/j.radonc.2020.02.020
[125] Vogelbaum, M. A., & Miller, J. J. (2021). Recurrence and complications after skull base surgery: Current challenges. Neuro-Oncology Practice, 8(4), 421–432. https://doi.org/10.1093/nop/npaa075
[132] Ghosh, A., & Nishteswar, K. (2021). Pharmacological and antioxidant evaluation of Brahma Rasayana. AYU Journal, 42(3), 180–188. https://doi.org/10.4103/ayu.ayu_230_20
[138] Sharma, R., & Patgiri, B. J. (2020). Standardization and safety evaluation of classical Avalehas: Brahma Rasayana model. Ancient Science of Life, 39(2), 89–98. https://doi.org/10.4103/asl.ASL_27_19
[145] Bhavaprakasha Nighantu, Rasayana Adhyaya. (Brahma Rasayana as the supreme rejuvenator for Majja Dhatu and Ojas.) Varanasi: Chaukhambha Bharati Academy.











One Response
F*ckin’ tremendous things here. I am very glad to see your post. Thanks a lot and i’m looking forward to contact you. Will you kindly drop me a e-mail?