- How Common Is Meningioma in the USA, UK, Canada, and Australia?
- United States
- United Kingdom
- Canada
- Australia
- Key Global Patterns
- Anatomy and Origin
- Types and Classification
- Etiology(Causes) and Risk Factors
- Pathophysiology
- Clinical Features(Symptoms)
- Other Common and Rare Disorders Associated With Meningioma
- Commonly associated disorders
- Genetic and syndromic associations
- Vascular and structural complications
- Rare but clinically significant associations
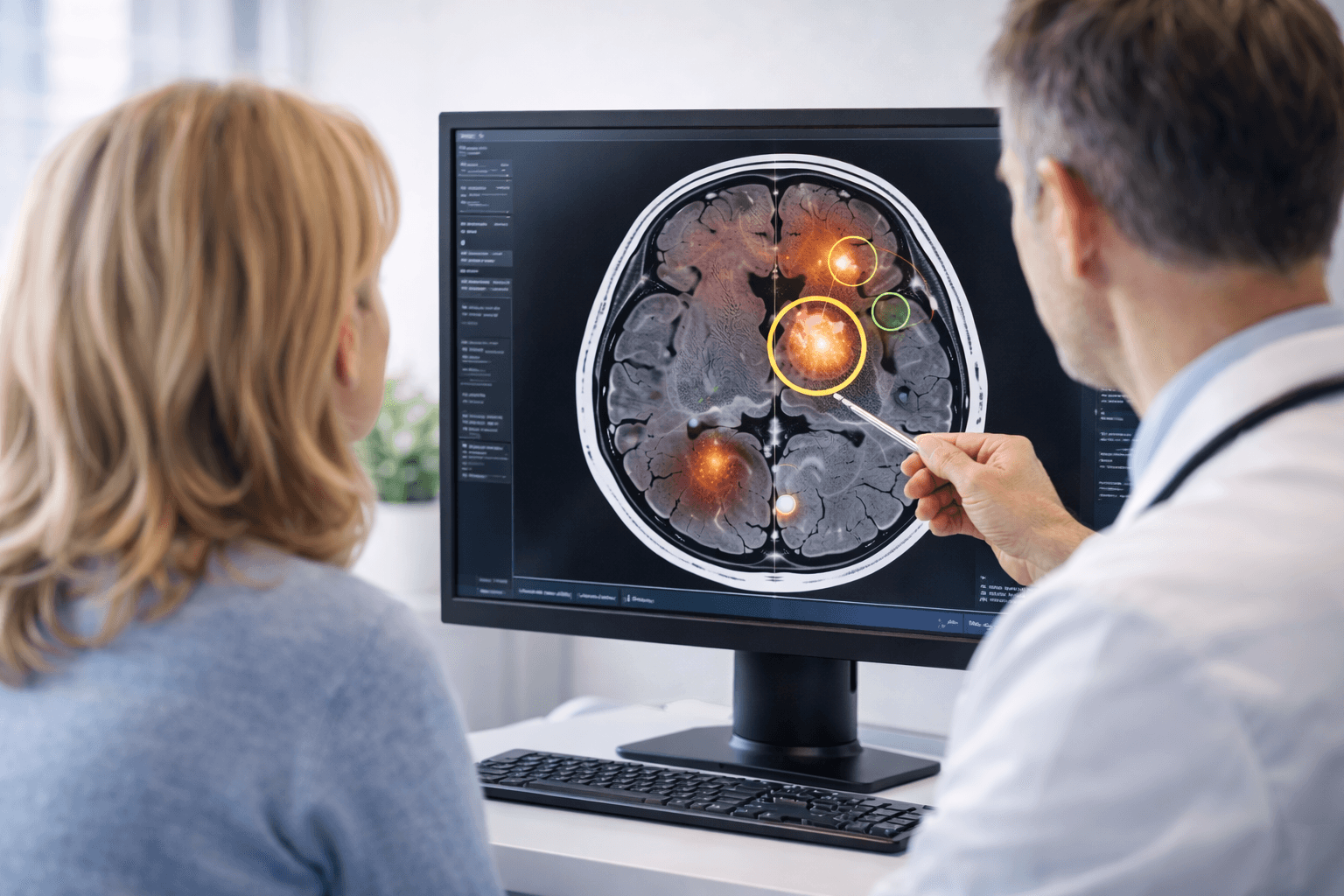
- Diagnostic Evaluation
- Treatment Approaches
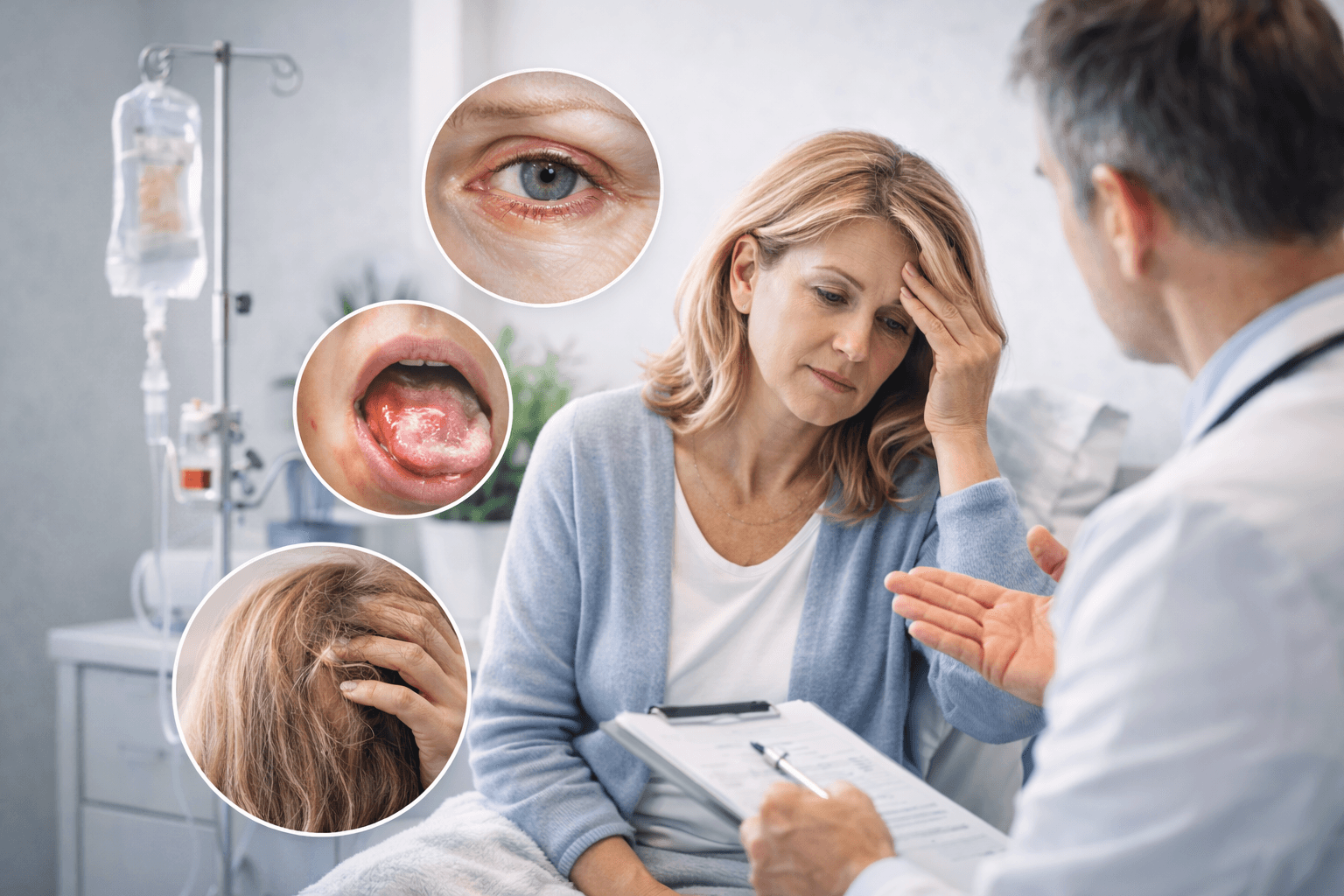
- Modern Treatment Side Effects
- Side effects of meningioma surgery
- Side effects of radiotherapy and radiosurgery
- Side effects of systemic therapy
- Long term quality of life after treatment
- Ayurvedic understanding of post treatment effects
- Integrative recovery approach
- Ayurvedic Cure
- Brahma Rasayana Avaleha (Medicine)
- Precaution and Warning
- Modern Management vs Ayurvedic Root-Cause Approach
- Treatment goal
- View of the disease
- Approach to small and asymptomatic tumors
- Method of tumor control
- Effect on surrounding brain tissue
- Recurrence prevention
- Recovery phase
- Systemic impact
- Long-term outcome vision
- Who Is the Ideal Candidate for Ayurvedic Treatment?
- Patients with small or asymptomatic meningioma
- Patients under observation (watch-and-wait protocol)
- Post-surgical recovery phase
- Patients after radiotherapy or radiosurgery
- Patients with recurrent meningioma
- Patients with strong digestive capacity and treatment compliance
- Patients seeking integrative care
- Patients who may need a modified or delayed approach
- Frequently Asked Questions (FAQs)
- References
(Meningioma Ayurvedic Cure)-It is one of the most common types of primary brain tumors, accounting for nearly one-third of all intracranial tumors. It originates from the meninges — the protective layers that envelop the brain and spinal cord. Although most meningiomas are benign and slow-growing, their location can cause significant neurological symptoms due to compression of nearby brain structures. In certain cases, they may exhibit aggressive behavior or recur after surgery, posing long-term management challenges for both patients and physicians [1].
In modern medicine, meningioma is usually managed through surgery or radiotherapy depending on size, location, and grade. Yet, recurrence and post-surgical complications remain frequent concerns. Patients often experience residual headaches, seizures, vision problems, and cognitive changes even after seemingly complete removal [2]. This has led many to explore complementary medical systems such as Ayurveda, which approach the condition from a root-cause and systemic balance perspective.
From an Ayurvedic standpoint, meningioma can be compared to Shiro Granthi or Mastishka Arbuda, conditions described as abnormal growths within the head region due to the vitiation of Vata and Kapha doshas and obstruction of the Majja Dhatu (bone marrow and nervous tissue channels). The imbalance of these fundamental elements leads to stagnation, accumulation of metabolic toxins (Ama), and formation of a hard, space-occupying lesion [3].
While modern science focuses on the removal of the mass, Ayurveda aims to restore internal harmony by correcting Dosha, clearing Srotas (microchannels), and rejuvenating Majja Dhatu using Rasayana (neuro-rejuvenative) therapies. Herbs like Brahmi (Bacopa monnieri), Ashwagandha (Withania somnifera), and Guduchi (Tinospora cordifolia) have shown neuroprotective, anti-inflammatory, and potential anti-tumor properties supported by experimental and clinical research [4].
In this comprehensive guide, we explore the dual approach to meningioma— integrating the precision of modern diagnosis with the holistic healing philosophy of Ayurveda. You’ll learn about its symptoms, causes, diagnostic techniques, and the evolving role of Ayurvedic formulations, Bhasmas, and Rasayana therapies in supporting brain health and preventing recurrence [5].
How Common Is Meningioma in the USA, UK, Canada, and Australia?
Meningioma is the most frequently diagnosed primary brain tumor in adults across Western countries. Its incidence has increased over the past two decades, largely due to widespread MRI use and an aging population.
United States
In the United States, meningiomas account for about 39 percent of all primary brain and central nervous system tumors. The annual incidence is approximately 8 to 10 cases per 100,000 people. They are more common in women, with a female-to-male ratio of nearly 2:1. The risk rises significantly after the age of 50, and many tumors are discovered incidentally during imaging for unrelated conditions.
United Kingdom
In the UK, meningioma represents the most common non-malignant brain tumor. The incidence is estimated at around 7 to 8 per 100,000 people per year. Similar to the US, it is seen more frequently in women and older adults. Improved neuroimaging access through the NHS has led to increased detection of small, asymptomatic tumors.
Canada
Canadian cancer registry data show patterns very similar to the United States. Meningiomas make up the largest proportion of primary brain tumors, with an incidence of roughly 7 to 9 per 100,000 population annually. Many are diagnosed during scans performed for headaches, trauma evaluation, or neurological symptoms.
Australia
In Australia, meningioma is also the most commonly reported benign brain tumor. The incidence ranges between 6 and 8 per 100,000 people per year. As in other Western countries, it is more common in women and in individuals over 50 years of age. The widespread availability of advanced imaging has contributed to earlier and more frequent diagnosis.
Key Global Patterns
Across all four countries, the epidemiology shows consistent features:
- It is the most common primary brain tumor in adults
- It occurs more often in women
- Incidence increases with age
- Many cases are detected incidentally
- Most tumors are WHO Grade I and slow growing
Meningioma is the most common primary brain tumor in adults in the USA, UK, Canada, and Australia, with an incidence of about 6 to 10 cases per 100,000 people each year. It occurs more often in women, increases after age 50, and is frequently detected incidentally during MRI scans.
From an Ayurvedic perspective, this rising prevalence reflects long-standing metabolic imbalance, chronic stress, hormonal disruption, and accumulation of Aama affecting Majja Dhatu. Early detection provides a valuable window for interventions aimed at reversing the underlying pathology and preventing progression.
Anatomy and Origin
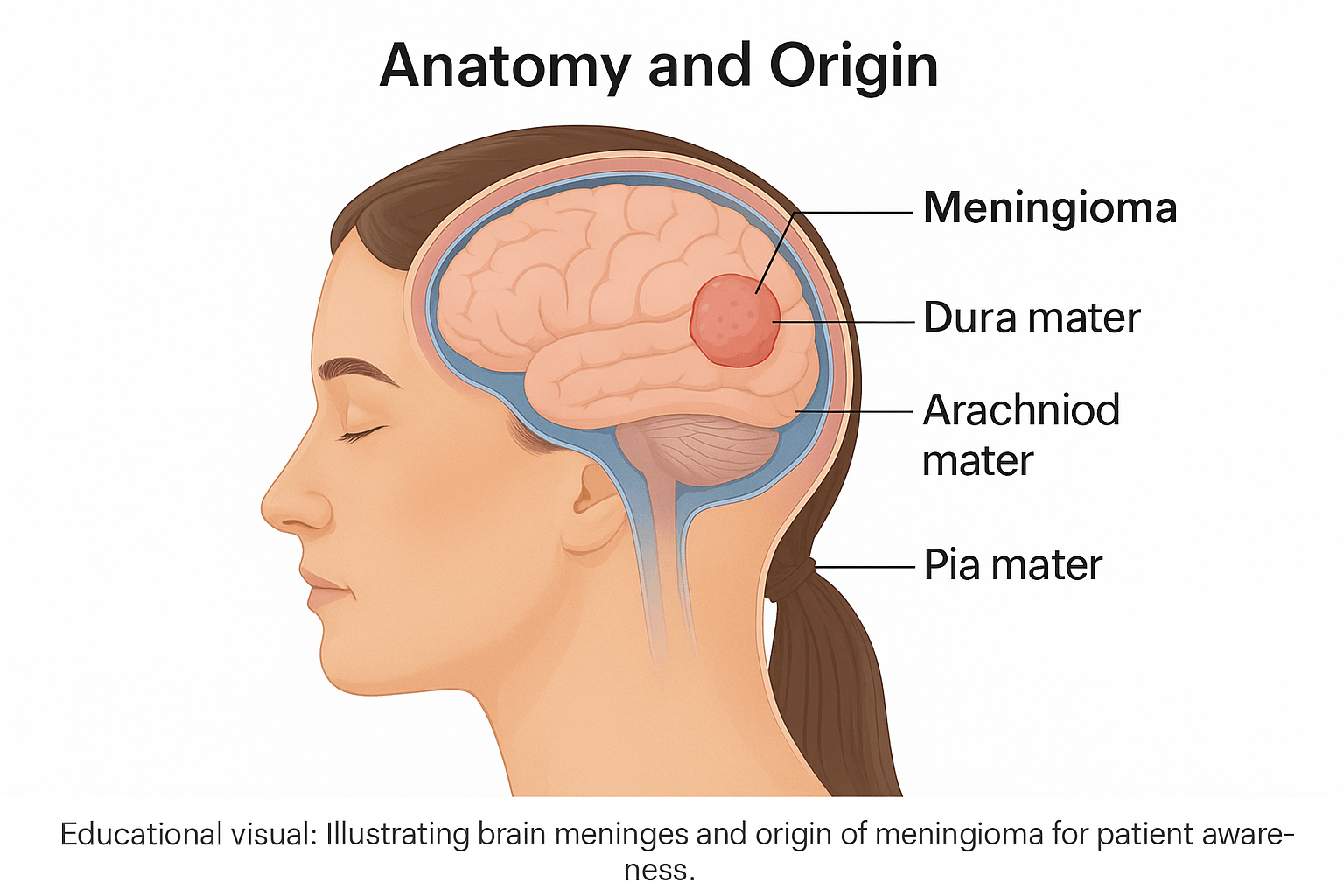
The human brain is surrounded by three delicate protective membranes known as the meninges — the dura mater, arachnoid mater, and pia mater. These layers act as a cushion and barrier, shielding the brain and spinal cord from mechanical injury, infections, and fluctuations in cerebrospinal fluid pressure [6].
The dura mater, the outermost layer, is tough and fibrous, adhering closely to the inner surface of the skull. Beneath it lies the arachnoid mater, a thin, web-like membrane that bridges the gap between the dura and the innermost pia mater, which intimately covers the surface of the brain and spinal cord. Within this subarachnoid space flows the cerebrospinal fluid (CSF), which provides further protection and nutrient exchange [7].
Meningioma originates from the arachnoid cap cells, also called meningothelial cells, located within the arachnoid villi. These specialized cells normally help regulate cerebrospinal fluid absorption but can begin proliferating abnormally due to genetic mutations, hormonal factors, or radiation exposure, forming a tumor mass [8].
Depending on where these cells are located, meningiomas can develop in various sites throughout the central nervous system. The most common locations include the cerebral convexity (surface of the brain), parasagittal region (along the central groove between the hemispheres), sphenoid wing (near the base of the skull), olfactory groove (above the nasal cavity), and even the spinal canal [9]. Each of these locations produces unique clinical manifestations due to differing patterns of brain or nerve compression.
From an Ayurvedic perspective, the meninges correspond to the protective coverings of the Majja Dhatu (the nervous tissue) and Shiras Srotas (cranial channels). When Vata and Kapha doshas become vitiated, they disturb the fine balance within these coverings, leading to localized thickening or swelling — a phenomenon similar to Granthi or Arbuda formation described in classical texts [10]. Ayurveda therefore views meningioma not merely as a mechanical mass but as a deeper systemic imbalance that originates from within the Dhatu (tissue metabolism) itself.
Types and Classification
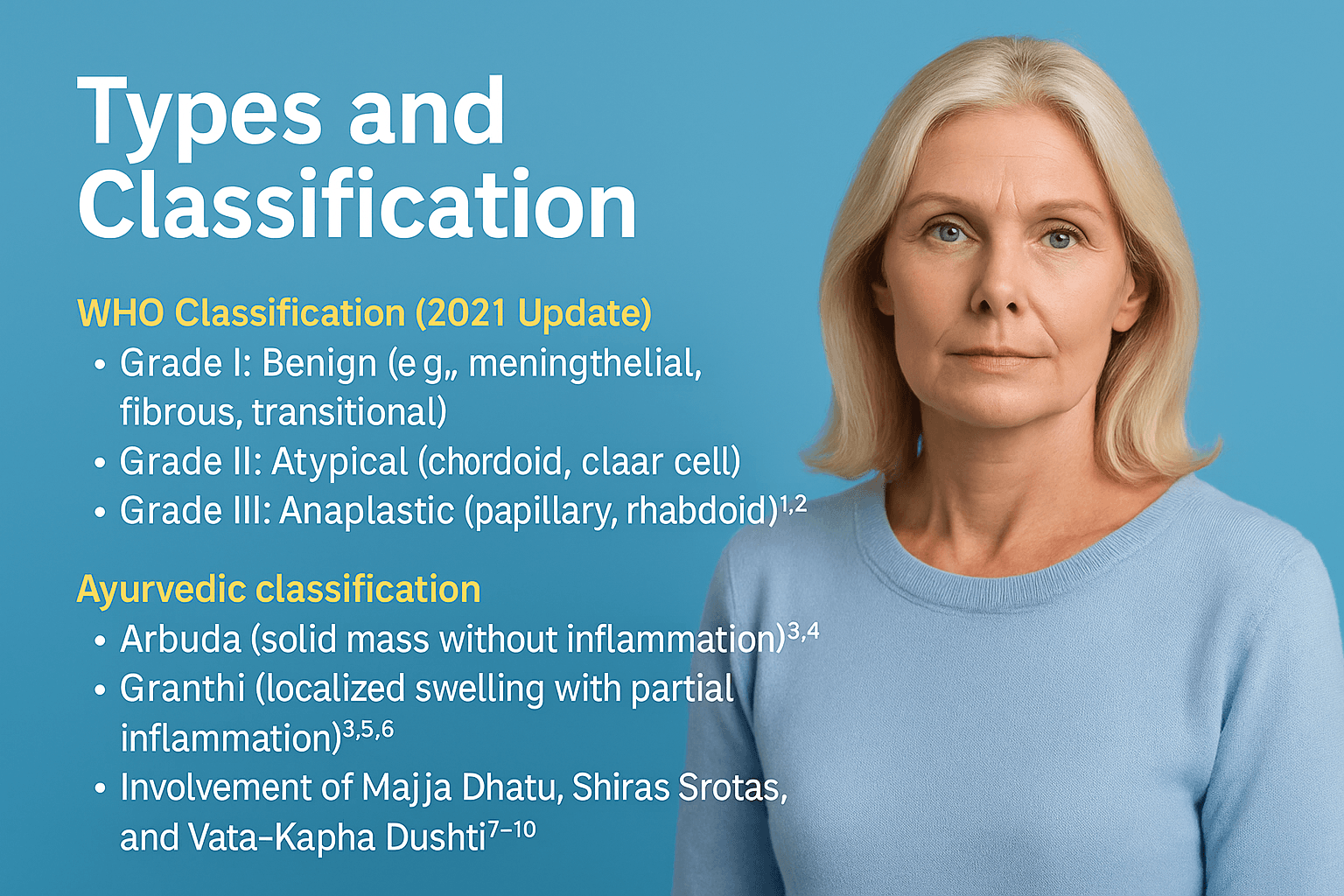
Meningiomas differ greatly in their cellular behavior, recurrence potential, and impact on neurological function. Correct classification helps predict prognosis and select the most appropriate treatment [1]. Ayurveda also distinguishes these conditions according to doshic imbalance, tissue involvement, and the degree of metabolic obstruction within the Majja Dhatu and Shiras Srotas [3, 4].
WHO Classification (2021 Update)
According to the World Health Organization’s 2021 system [1, 11], meningiomas are categorized into three principal grades based on histopathology and molecular characteristics [8, 12].
Grade I – Benign Meningioma
Accounting for nearly 80 to 85 percent of all cases, these tumors are slow-growing and well-differentiated. Common subtypes include meningothelial, fibrous, and transitional meningiomas. They are usually amenable to surgical resection and have excellent long-term outcomes [2, 9].
Grade II – Atypical Meningioma
Representing about 15 to 20 percent of cases, atypical tumors show increased mitotic activity and higher recurrence rates. Subtypes such as chordoid and clear-cell meningiomas often require adjuvant radiotherapy and close follow-up [9, 13].
Grade III – Anaplastic (Malignant) Meningioma
The rarest form, comprising less than 3 percent of meningiomas, includes papillary and rhabdoid types. These display aggressive growth, invasion of nearby tissues, and frequent recurrence even after complete excision [9, 13].
Recent molecular studies identify additional markers—TERT promoter mutations, CDKN2A/B deletions, and NF2 gene loss—that correlate with poor prognosis and higher WHO grade [11, 12, 13]. Such data have shifted management from purely histological to integrated molecular stratification.
Ayurvedic Classification
In classical texts including Charaka Samhita and Bhavaprakasha, meningeal tumors correspond to Arbuda (solid, non-inflammatory mass) or Granthi (localized swelling with mild inflammation) [3, 10, 14].
Arbuda
Described as a firm, deep-seated growth arising from vitiated Vata and Kapha doshas combined with Aama accumulation, Arbuda develops slowly yet can exert serious pressure effects in confined areas such as the cranial cavity [3, 4, 10].
Granthi
A smaller, partially inflamed lesion produced by moderate dosha vitiation. If left untreated, Granthi can evolve into Arbuda, demonstrating the progressive nature of chronic Srotas blockage [3, 14].
Ayurveda interprets tumor formation as a downstream effect of Agnimandya (impaired digestion and metabolism) and Srotorodha (obstruction of micro-channels). These factors disturb Majja Dhatu and Ojas, leading to abnormal cell proliferation [4, 5, 14]. By contrast, modern classification describes the same process through histological grading and genetic mutation analysis [11, 13].
Together, these two frameworks—histopathological and Ayurvedic—offer a complete understanding of the disease: one describes the structural manifestation, the other explains its root energetic and metabolic origins [3, 4, 10, 14].
Etiology(Causes) and Risk Factors
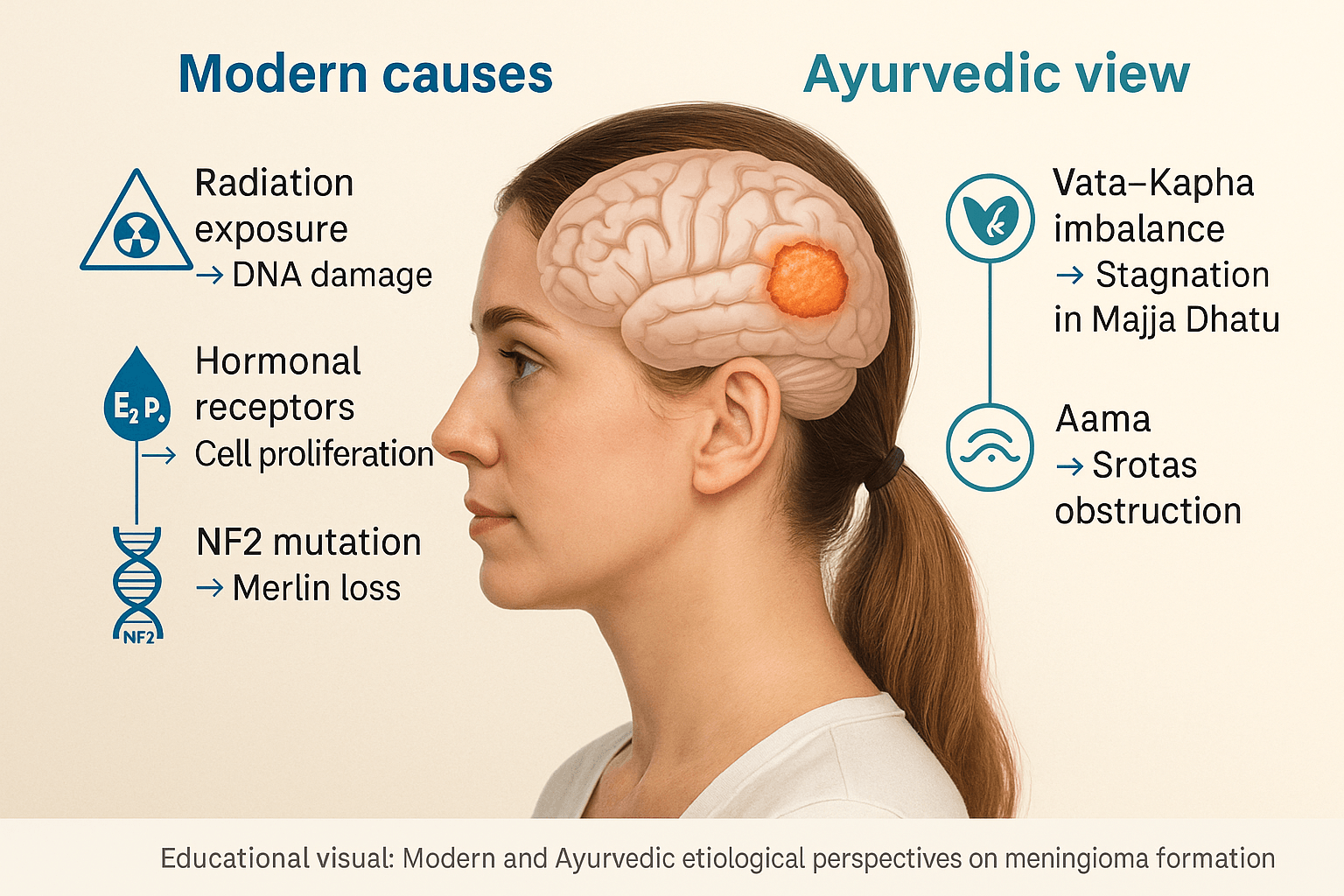
Meningioma development is multifactorial, involving a complex interplay of genetic, hormonal, environmental, and metabolic influences. While modern medicine identifies cellular mutations and hormonal receptors as major drivers, Ayurveda interprets the same pathology through doshic imbalance, accumulation of metabolic toxins, and obstruction in vital channels. Understanding both perspectives helps in identifying not only how the disease forms but why it occurs in specific individuals.
Modern Causes and Predisposing Factors
Radiation Exposure
Exposure to ionizing radiation, particularly during childhood or cranial radiotherapy, is one of the most established risk factors for meningioma formation [1, 15]. Studies show that even low-dose diagnostic radiation can slightly increase lifetime risk, while therapeutic radiation markedly elevates the probability of secondary meningiomas developing decades later [16].
Hormonal Factors
Meningiomas are two to three times more common in women, reflecting a clear hormonal influence. Immunohistochemical analyses have confirmed the presence of estrogen and progesterone receptors in many meningioma cells [17, 18]. These hormones promote cellular proliferation and may explain tumor growth during pregnancy or following hormone replacement therapy. Some studies also suggest a role for oral contraceptive use in increasing risk, although findings remain inconclusive [19].
Genetic Mutations
Molecular research has identified recurrent mutations in the NF2 gene on chromosome 22, leading to loss of the tumor suppressor protein merlin, which is central to cellular adhesion and signaling [13, 20]. Other non-NF2 driver mutations involving TRAF7, KLF4, AKT1, and SMO pathways contribute to tumor diversity and biological behavior [11, 20]. These findings are especially relevant for precision therapy development and molecular grading.
Head Trauma and Viral Associations
Repeated cranial injury and chronic inflammation may create a microenvironment conducive to aberrant meningeal cell proliferation [15, 21]. Certain viral infections, particularly Simian Virus 40 (SV40) and members of the Herpesviridae family, have been implicated in oncogenic transformation of meningothelial cells, though a definitive causal link remains under investigation [21, 22].
Environmental and Lifestyle Factors
Obesity, stress, and chronic exposure to petrochemicals or electromagnetic radiation have been suggested as potential contributors, possibly via endocrine disruption and oxidative stress pathways [15, 19]. Modern studies highlight the importance of maintaining a balanced metabolic and hormonal milieu to reduce risk.
Ayurvedic View
From the Ayurvedic perspective, meningioma arises from Vata–Kapha imbalance leading to disturbed tissue metabolism and stagnation within the Majja Dhatu (nervous tissue) [3, 4, 10]. This imbalance weakens the inherent vitality of the brain’s channels (Shiras Srotas), allowing pathological accumulations to form.
Aama Accumulation in Majja Dhatu
When digestion and metabolism (Agni) are impaired, Aama, a sticky, undigested metabolic residue, accumulates in deeper tissues. Over time, Aama obstructs the Majja Srotas, resulting in stiffness, heaviness, and the formation of localized hard masses analogous to meningiomas [3, 4, 10].
Obstruction of Sira Srotas (Microchannels)
Ayurveda describes Srotorodha (blockage of subtle channels) as the starting point of many chronic diseases. When Vata becomes deranged and Kapha thickens, the natural circulation of nutrients and Prana within the brain is hampered. This imbalance creates a suitable nidus for growth within the meninges, corresponding to the modern idea of chronic low-grade inflammation and altered cell signaling [4, 14].
Ayurvedic classics further link such disorders to emotional strain, irregular sleep, and suppression of natural urges, all factors that aggravate Vata dosha and destabilize Majja Dhatu. Thus, while modern science explains meningioma through radiation, hormones, and genes, Ayurveda extends the understanding to the energetic and systemic terrain that fosters the disease.
Pathophysiology
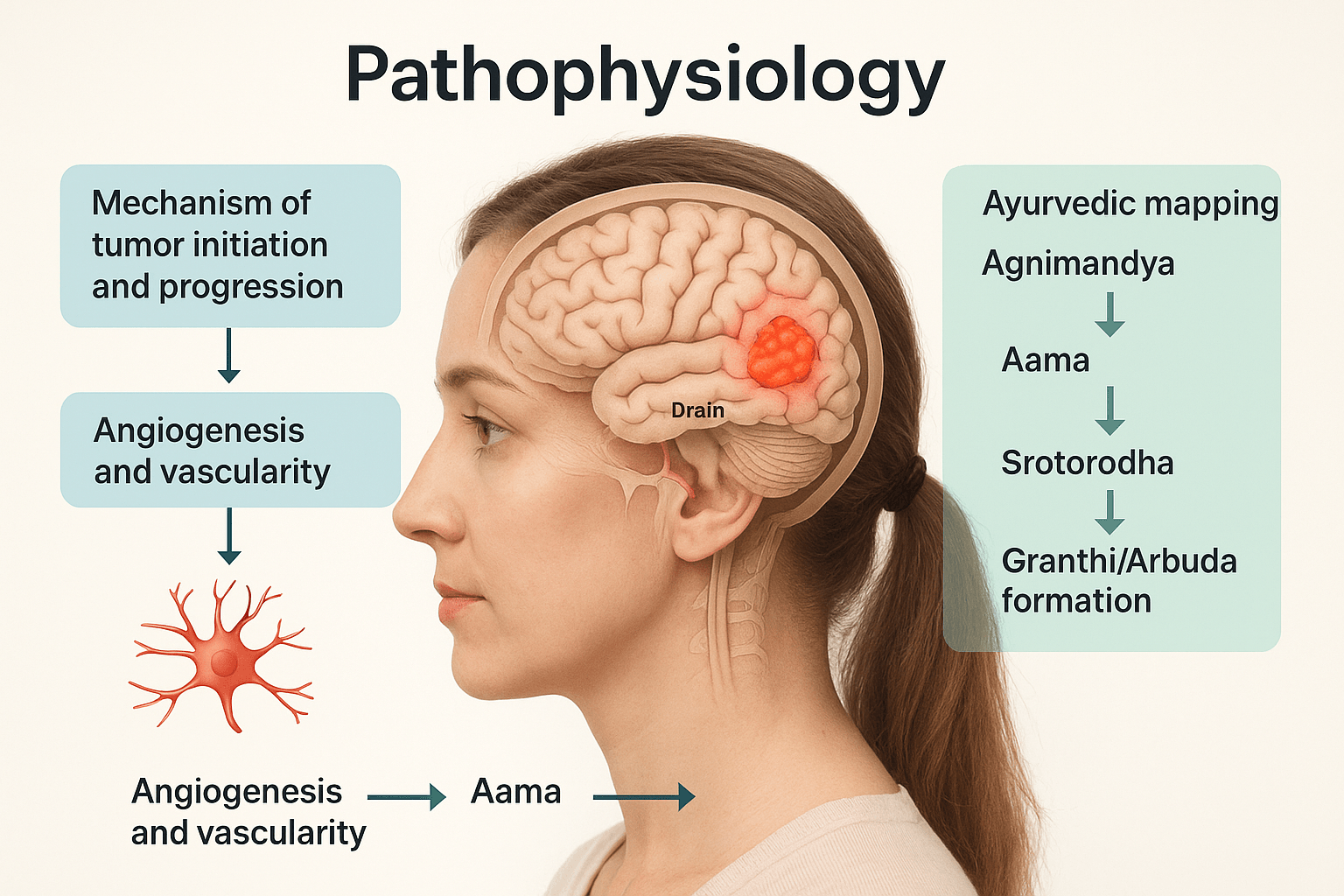
The pathophysiology of meningioma represents a dynamic interplay between genetic instability, hormonal influence, and vascular remodeling. While modern medicine focuses on cellular and molecular mechanisms, Ayurveda views the same pathology through functional disruption of doshic balance, digestion, and tissue vitality. Integrating both provides a complete understanding of how benign meningothelial cells transform into space-occupying lesions.
Mechanism of Tumor Initiation and Progression
Meningiomas originate from meningothelial (arachnoid cap) cells that normally regulate cerebrospinal fluid absorption and maintain the meningeal barrier. Genetic mutations, especially those affecting NF2, TRAF7, KLF4, AKT1, and SMO, disrupt cell adhesion and promote uncontrolled proliferation [13, 20, 23].
Loss of the NF2 tumor suppressor gene results in the absence of the merlin protein, leading to dysregulated cell signaling and contact inhibition failure [13, 20].
The process begins with localized hyperplasia of arachnoid cells, followed by chromosomal instability, epigenetic silencing of growth inhibitors, and progressive dedifferentiation that marks higher-grade meningiomas [23, 24].
In addition, hormonal activation through estrogen and progesterone receptors augments proliferative signaling, while inflammatory cytokines such as IL-6 and TNF-α contribute to microenvironmental changes that support tumor persistence [17, 24]. Cellular pathways including PI3K/AKT/mTOR and Hedgehog signaling have been identified as key mediators of this transformation [11, 20, 23].
Angiogenesis and Vascularity
Meningiomas are notably vascular tumors. The growth of new blood vessels, or angiogenesis, is mediated primarily by vascular endothelial growth factor (VEGF) and platelet-derived growth factor (PDGF) [25]. These molecules stimulate endothelial proliferation, resulting in tortuous and leaky vessels that sustain rapid tumor expansion. Increased VEGF expression correlates strongly with tumor grade and recurrence risk [25, 26].
This hypervascularity also explains the intraoperative bleeding often encountered during meningioma surgery. From an integrative perspective, angiogenesis mirrors an imbalance in tissue nourishment and flow regulation—concepts deeply linked to the Ayurvedic principle of disturbed Srotas (microchannel pathways) [3, 4, 10].
Ayurvedic Mapping of Pathogenesis
Ayurveda describes the genesis of any localized mass through the progressive sequence of Agnimandya → Aama → Srotorodha → Granthi/Arbuda formation [3, 10, 14].
When digestive and metabolic fire (Agni) becomes weak, it leads to incomplete transformation of nutrients, forming toxic residues (Aama). This Aama circulates through the body and lodges in weak or genetically susceptible tissues—in this case, the Majja Dhatu (nervous and marrow tissue).
Accumulation of Aama obstructs the Sira Srotas (microchannels), causing local stagnation and swelling (Srotorodha). Over time, this process leads to the formation of Granthi (localized swelling) or Arbuda (tumor-like mass) depending on the degree of doshic derangement and tissue depletion [3, 4, 10].
The predominance of Vata and Kapha doshas drives irregular cell growth—Vata inducing erratic cellular activity, while Kapha contributes to density and cohesion of the lesion [14, 27].
Role of Majja Kshaya and Ojas Depletion
In chronic stages, meningioma pathology parallels the concept of Majja Kshaya—degeneration or depletion of nervous tissue essence [4, 10]. This depletion leads to mental fatigue, poor cognitive function, and disturbed coordination, similar to symptoms observed in modern neuro-oncological cases. Concurrently, Ojas depletion—the weakening of vital immunity and systemic resilience—further reduces the body’s ability to suppress abnormal cell growth [28, 29].
Thus, Ayurveda interprets tumorigenesis not as an isolated cellular event but as a systemic collapse of metabolic integrity and immunity. The modern view of angiogenesis, inflammatory signaling, and genetic mutation aligns closely with Ayurveda’s view of Srotas obstruction, Aama accumulation, and Ojas decline. This correlation forms the foundation of integrative therapeutic strategies combining Rasayana, detoxification, and immune restoration [5, 27, 29].
Clinical Features(Symptoms)
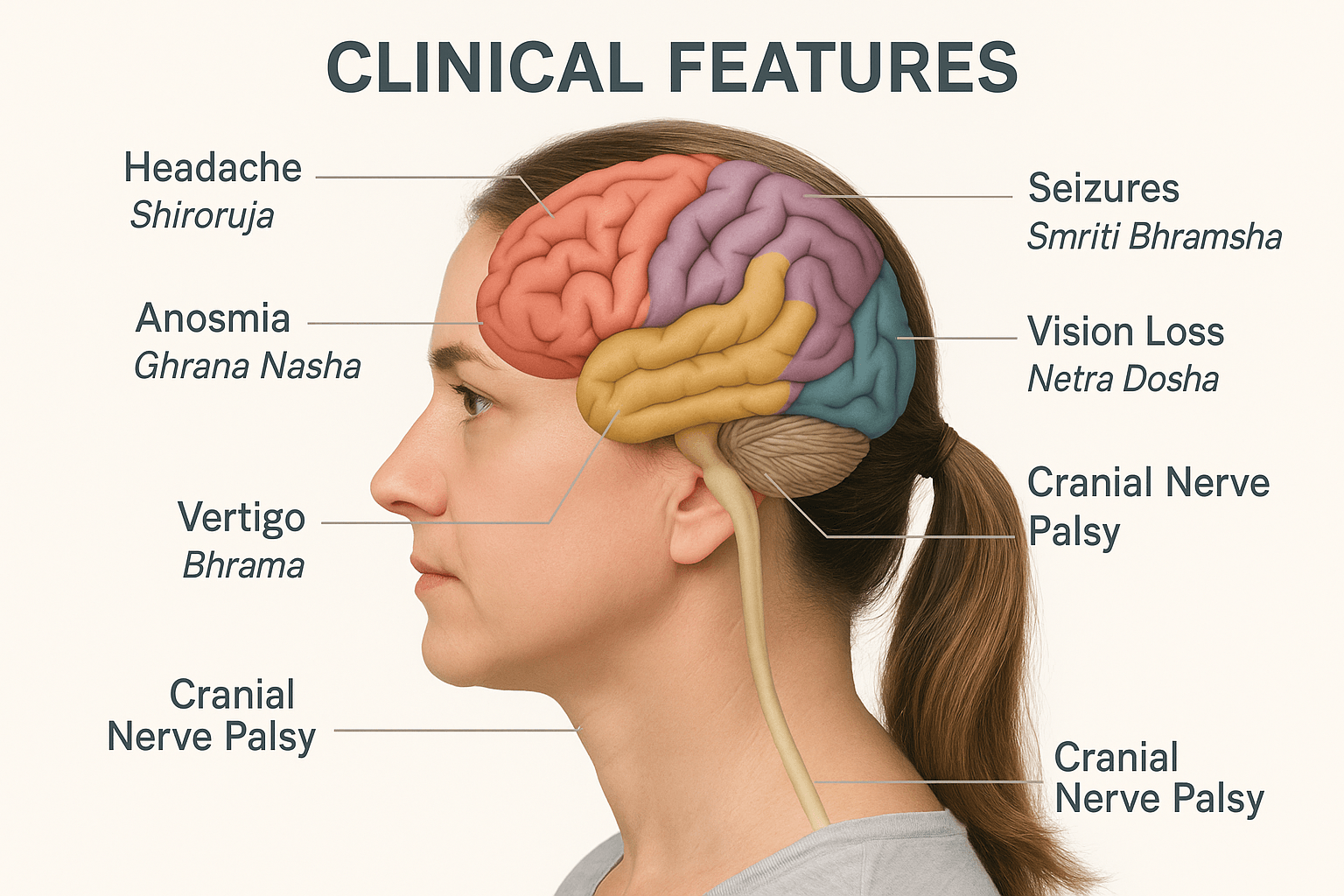
The clinical manifestations of meningioma are determined by multiple factors such as tumor location, growth pattern, rate of expansion, and interaction with surrounding neural and vascular structures. Because the tumor grows slowly, symptoms often develop gradually and may remain unnoticed until the lesion reaches considerable size. In Ayurveda, these symptoms are understood as progressive expressions of doshic imbalance and impaired flow through the subtle channels or srotas, primarily involving the Majja Dhatu (nervous tissue) and Shiras Srotas (cranial microchannels) [3, 4, 10, 14].
Meningioma symptoms usually fall into three major categories: signs of raised intracranial pressure, focal neurological deficits based on the site of origin, and systemic manifestations due to chronic tissue disturbance [1, 2, 30].
Headache and Raised Intracranial Pressure
Headache is the most common presenting feature and is often dull, persistent, and diffuse. It typically worsens in the early morning or during physical strain due to increased intracranial pressure from venous congestion or compression of pain-sensitive dural structures [1, 30]. The pain may gradually intensify and is often associated with nausea, vomiting, and a feeling of heaviness in the head. Ayurveda describes this state as Shiroruja, or head pain, resulting from obstruction of cranial srotas and vitiation of Vata and Kapha doshas [3, 10, 14]. The accompanying heaviness and lethargy correspond to Aama accumulation in Majja Dhatu and impaired circulation of Prana within the cranial region [4]. In severe cases, papilledema and vision disturbances occur, indicating chronic raised intracranial pressure [9, 30].
Seizures
Seizures develop in nearly one-third of meningioma patients, particularly when the tumor involves the motor cortex, parietal lobes, or parasagittal regions [31, 35]. They may manifest as focal motor jerks, sensory auras, or generalized tonic–clonic convulsions. The pathophysiology involves cortical irritation, local inflammation, and neuronal hyperexcitability secondary to pressure from the expanding mass [30, 31]. In Ayurvedic terminology, these episodes are referred to as Apasmara—a transient loss of awareness and motor control caused by aggravated Vata disturbing the flow of consciousness through the Manovaha Srotas (mental channels) and depletion of Ojas [3, 4, 10]. Such patients may also experience anxiety, dizziness, or disorientation between episodes, reflecting the disturbed harmony of Prana Vata and Sadhaka Pitta within the brain [14, 29].
Visual Disturbances
Visual symptoms are common in meningiomas located near the optic nerve, optic chiasm, or occipital lobe. Patients may complain of blurred vision, loss of visual fields, double vision, or progressive blindness [9, 32]. These findings result from mechanical compression, ischemia, or demyelination of visual pathways. Ayurveda correlates these features with Netra Dosha, Timira (dimming of vision), and Andhya (progressive blindness), which arise from deranged Pitta and Vata doshas acting upon the Drishti Srotas [3, 10, 14]. The pathological process involves depletion of Tejas in Majja Dhatu, leading to impaired neural transmission in ocular circuits. Ayurvedic scholars such as Chakrapani have also described vision loss as a result of Prana Vata imbalance that disrupts ocular perception and mental clarity [38].
Cognitive and Behavioral Changes
Meningiomas involving the frontal lobe frequently lead to personality alterations, poor judgment, irritability, apathy, or emotional instability [30, 31]. The patient may exhibit disinhibition, loss of social restraint, and decreased concentration, often mistaken for psychiatric disorders. Memory impairment and reduced intellectual capacity are frequent when the lesion compresses the limbic system or frontal association areas [39]. Ayurveda refers to this as Smriti Bhramsha—diminution or confusion of memory caused by Majja Kshaya (degeneration of neural tissue) and Ojas depletion, leading to unstable mental faculties [4, 10, 29]. This loss of mental steadiness reflects a disturbed state of Tarpaka Kapha, which normally nourishes the mind, and Prana Vata, which governs thought and perception. Ayurvedic Rasayana herbs such as Brahmi (Bacopa monnieri) and Shankhpushpi (Convolvulus pluricaulis) are traditionally indicated to restore these functions [5, 33].
Cranial Nerve Palsies
Compression of cranial nerves by skull base or sphenoid wing meningiomas leads to a variety of focal deficits. Involvement of the oculomotor, trochlear, or abducens nerves causes double vision and restricted eye movement; trigeminal nerve involvement leads to facial numbness or pain; and vestibulocochlear nerve compression results in hearing loss or tinnitus [9, 31, 32]. The underlying mechanism involves direct nerve compression, ischemic demyelination, or entrapment within tumor margins. Ayurveda recognizes these manifestations as Indriya Upaghata, meaning impairment of sensory or motor organs due to obstruction of Vata flow within the Nadi Srotas [3, 4, 14]. The pain and numbness reflect aggravated Vata, while the associated heaviness and dullness correspond to Kapha stagnation in the nerve channels.
Rare and Location-Specific Manifestations
Olfactory groove meningiomas may present with gradual loss of smell (anosmia), frontal headaches, and sometimes visual deterioration when the tumor extends posteriorly toward the optic nerves [34]. Ayurveda equates loss of olfaction to Ghrana Nasha, a Vata–Pitta disorder within the Indriya Srotas responsible for smell perception [3, 10]. In some cases, personality changes coexist with anosmia, forming a clinical triad unique to this location [34].
Sphenoid wing and cavernous sinus meningiomas produce symptoms such as ptosis, diplopia, facial pain, or sensory loss due to compression of cranial nerves III, IV, V, and VI [9, 31, 32]. Ayurveda explains these as Nayana Sandhi Shula (pain around the eyes) and Drishti Gati Nasha (restricted ocular motion) from deranged Vata causing localized neural rigidity [3, 14].
Posterior fossa and cerebellopontine angle meningiomas can cause imbalance, vertigo, tinnitus, and hearing loss as a result of vestibulocochlear nerve compression [9, 31]. Ayurveda interprets these symptoms as Bhrama (vertigo) and Karna Nada (tinnitus) resulting from disturbed Vata circulation in the auditory pathways [3, 10, 14].
Parasagittal or falcine meningiomas often produce contralateral leg weakness or sensory loss due to compression of motor and sensory cortex areas [35]. Ayurveda describes similar unilateral deficits as Ekanga Stambha or Ekanga Rukshata, which indicate blocked Vata flow within localized neural tracts [4, 10].
Temporal and sphenoid ridge tumors may lead to speech impairment, memory disturbances, and complex partial seizures, reflecting temporal lobe involvement [9, 31, 36]. Ayurveda parallels these findings with Vacha Shakti Hani (loss of speech ability) and Smriti Bhramsha (memory confusion), which arise from Majja Dushti and Ojas depletion [4, 29].
Spinal meningiomas, though less common, cause back pain, limb weakness, sensory loss, and urinary disturbances due to compression of the spinal cord and nerve roots [9, 37]. Ayurveda identifies these symptoms as Greeva–Trika Shoola (axial pain) and Mutra Vega Dharana Janya Vyadhi (urinary difficulty), caused by obstructed Vata in Prishtha and Vankshana Srotas [3, 14].
Systemic and Late-Stage Symptoms
In advanced cases, large meningiomas may impinge upon the hypothalamic or pituitary regions, producing hormonal disturbances such as menstrual irregularities, weight fluctuations, or excessive thirst and urination [9, 32, 40]. Ayurveda views such systemic changes as multi-dhatu involvement, in which pathological Vata and Kapha extend beyond the Majja Dhatu into Rasa and Meda Dhatus, leading to metabolic imbalance and endocrine dysfunction [4, 10, 29].
Other chronic manifestations include insomnia, fatigue, mood instability, or generalized weakness, all of which correlate with progressive Ojas depletion [28, 29, 41]. As the disease advances, symptoms like hemiparesis, speech arrest, or ataxia may appear, indicating extensive neural compression and degeneration [31, 35]. Ayurveda explains this deterioration as severe Vata vitiation within Shiras Srotas, requiring rejuvenative Rasayana and nerve-restorative therapy to stabilize function [5, 29].
Other Common and Rare Disorders Associated With Meningioma
Commonly associated disorders
Peritumoral brain edema
Peritumoral edema is one of the most frequent radiological and clinical findings in meningioma. It develops due to increased vascular permeability and local inflammatory mediators, leading to accumulation of fluid in the surrounding brain tissue. Patients may experience worsening headache, vomiting, blurred vision, seizures, or progressive cognitive slowing. The degree of edema often correlates more with symptoms than the tumor size itself. In Ayurvedic understanding this resembles Kapha accumulation with Srotorodha in the cranial region, producing heaviness, mental dullness, and pressure sensations. Its presence influences surgical planning, recovery time, and the need for long term metabolic and neuroprotective support.
Seizure disorder
Seizures are a common presenting feature, especially in cortical meningiomas located over the convexity or parasagittal region. Chronic compression and irritation of the cerebral cortex alter neuronal electrical activity and lower the seizure threshold. Even after successful tumor removal, some patients continue to require antiepileptic medication because of long standing cortical changes. Recurrent seizures significantly affect quality of life, memory, mood stability, and daily functioning. In Ayurvedic correlation this resembles Apasmara, where aggravated Vata disturbs higher mental faculties and neural coordination. Long term management therefore requires not only structural treatment but also restoration of Majja Dhatu, stabilization of Vata, and enhancement of cognitive resilience.
Focal neurological deficits
Focal deficits occur when the tumor compresses specific functional areas of the brain. Patients may develop progressive weakness of one side of the body, difficulty in speech, loss of fine motor skills, sensory impairment, or visual field defects depending on the tumor location. These symptoms often evolve slowly and may be misinterpreted as age related decline in early stages. Persistent compression can lead to irreversible neuronal damage if intervention is delayed. From an Ayurvedic perspective this reflects Vata vitiation in the Majja and Snayu systems, leading to loss of coordinated movement and sensory function. Early recognition and neuroregenerative support are essential for functional recovery.
Cognitive impairment
Cognitive decline is frequently seen in frontal and temporal lobe meningiomas and may present as poor concentration, reduced decision making ability, personality changes, emotional instability, and memory loss. These changes are often subtle and may be noticed more by family members than by the patient. Chronic intracranial pressure, vascular compromise, and neuronal compression contribute to progressive dysfunction. Even after treatment, cognitive recovery may take months and requires active rehabilitation. In Ayurvedic mapping this corresponds to impairment of higher mental functions due to Majja Dhatu depletion and disturbance of Prana Vata, affecting Medha, Smriti, and Dhi.
Hormonal imbalance
Meningiomas located near the sellar and parasellar regions can influence pituitary function and lead to endocrine disturbances. Patients may present with menstrual irregularities, infertility, thyroid dysfunction, unexplained weight changes, adrenal insufficiency, or reduced libido. Tumor growth during pregnancy and the higher incidence in women suggest a strong hormonal component, particularly progesterone receptor expression in many meningiomas. These metabolic and reproductive changes indicate involvement beyond the nervous system. In Ayurvedic understanding this reflects disturbance of the neuroendocrine axis, depletion of Ojas, and impaired tissue nourishment affecting the entire hormonal network.
Chronic headache syndrome
Long standing headache is one of the most persistent complaints in meningioma patients. It is typically described as a dull, pressure like pain that worsens in the morning or with bending forward. Causes include dural irritation, peritumoral edema, altered cerebrospinal fluid dynamics, and post treatment neural sensitization. In some individuals the headache continues even after tumor removal, becoming a chronic pain disorder that affects sleep, mood, and productivity. Ayurvedically this is correlated with Shiroruja arising from Vata–Kapha imbalance in the cranial channels, requiring both local and systemic therapeutic measures for sustained relief.
Genetic and syndromic associations
Neurofibromatosis type 2
Neurofibromatosis type 2 is the most important genetic condition linked with multiple meningiomas. These patients often develop bilateral vestibular schwannomas, spinal tumors, and other intracranial neoplasms at a younger age than sporadic cases. The tumors tend to be multiple, recurrent, and biologically more active, requiring lifelong surveillance and repeated interventions. Hearing loss, imbalance, and visual disturbances are common associated features. The presence of this syndrome changes prognosis and treatment planning significantly. From an Ayurvedic viewpoint it indicates a deep seated constitutional imbalance affecting multiple Dhatus and Srotas, requiring long term Rasayana based systemic management rather than a purely local approach.
Multiple meningioma syndrome
Some patients develop two or more meningiomas without fulfilling the diagnostic criteria for neurofibromatosis. These tumors may appear at different times and locations within the cranial cavity. Management becomes complex because treatment of one lesion does not prevent the development of another. Long term imaging follow up is mandatory. This pattern suggests an underlying systemic predisposition rather than a single localized pathology. Ayurvedically this reflects persistent Dosha imbalance with widespread Srotodushti and Majja Dhatu involvement, emphasizing the need for metabolic correction and terrain based therapy.
Vascular and structural complications
Venous sinus invasion
Parasagittal and falcine meningiomas may invade major dural venous sinuses, particularly the superior sagittal sinus. This leads to impaired venous drainage, raised intracranial pressure, and increased surgical difficulty. Complete removal may not be possible without risking major neurological deficits. Patients may present with progressive headache, papilledema, or motor weakness. The involvement of major vascular channels indicates a more aggressive biological behavior and requires careful multidisciplinary planning. In Ayurvedic interpretation this resembles severe Srotorodha in the principal cranial channels affecting circulation and tissue nutrition.
Hydrocephalus
Large meningiomas or those located near cerebrospinal fluid pathways may obstruct normal CSF flow and produce hydrocephalus. Patients develop gait disturbance, urinary urgency or incontinence, slowing of mental activity, and reduced alertness. These symptoms are often reversible if treated early but may become permanent if neglected. The condition reflects mechanical obstruction along with impaired neural function. Ayurvedically this correlates with Kapha accumulation and Vata obstruction in the cranial pathways, leading to impaired movement, heaviness, and cognitive dullness.
Cranial nerve compression syndromes
Skull base meningiomas frequently compress cranial nerves due to their close anatomical relationships. Optic nerve involvement causes progressive visual loss and visual field defects. Trigeminal nerve compression produces facial pain or numbness. Vestibulocochlear nerve involvement leads to hearing loss, tinnitus, and imbalance. Lower cranial nerve compression results in swallowing difficulty, hoarseness of voice, and tongue deviation. These deficits significantly affect daily living and nutritional status. In Ayurvedic mapping this represents Vata disturbance in specific functional channels governing sensory and motor activities of the head and neck.
Rare but clinically significant associations
Radiation induced meningioma
These tumors develop years or even decades after exposure to therapeutic or environmental radiation. They are more common in individuals who received cranial irradiation during childhood. Radiation induced meningiomas tend to be multiple, atypical, and more aggressive than sporadic ones. Their latency period and distinct biological behavior make long term follow up essential in previously irradiated patients.
Malignant transformation
Although most meningiomas are benign, a small proportion may transform into atypical or anaplastic variants. These tumors show rapid growth, increased recurrence rate, and invasion into surrounding brain tissue. Patients may experience sudden worsening of neurological symptoms after a long stable period. Early detection of this change is crucial for timely intervention.
Extracranial metastasis
Metastasis outside the cranial cavity is extremely rare and usually occurs in high grade meningiomas. The lungs, liver, and bones are the most commonly reported sites. Its presence indicates aggressive tumor biology and significantly alters prognosis and treatment strategy.
Intratumoral hemorrhage
Bleeding within a meningioma is an uncommon but life threatening event. It can cause sudden severe headache, vomiting, rapid neurological deterioration, and loss of consciousness. Emergency neurosurgical management is required. The acute presentation contrasts with the typically slow growing nature of these tumors.
Paraneoplastic neurological syndromes
In rare situations, immune mediated neurological dysfunction may occur due to tumor related antigenic stimulation. Patients can develop unexplained neuropathy, cerebellar dysfunction, or encephalopathy without direct tumor compression. Recognition of this entity is important because symptoms may improve with treatment of the primary tumor.
Diagnostic Evaluation
Accurate diagnosis of meningioma requires a combination of advanced imaging, histopathological confirmation, and assessment of surrounding structural involvement. The objective is not only to confirm the presence of a tumor but also to understand its biological behavior, vascularity, and impact on brain function. From an Ayurvedic perspective, this diagnostic process parallels the evaluation of doshic imbalance, tissue degeneration, and srotas obstruction within the cranial system [3, 4, 10, 14].
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging with gadolinium contrast enhancement remains the gold standard for diagnosing meningioma [1, 9, 42]. MRI provides exceptional soft tissue contrast and enables visualization of the tumor’s origin, shape, and relationship to nearby brain structures. Typical imaging features include an extra-axial mass with a broad dural attachment, often demonstrating a “dural tail” sign, which is characteristic of meningioma [42, 43].
MRI can differentiate between benign, atypical, and anaplastic variants by revealing differences in contrast enhancement, edema, and invasion of adjacent tissue. Modern advancements such as MR spectroscopy and diffusion tensor imaging further allow metabolic assessment and mapping of white matter tracts for surgical planning [43].
Ayurvedically, MRI corresponds to a modern form of Roga Pariksha (disease examination) that allows direct visualization of Srotas obstruction and Majja Dhatu pathology. The enhanced contrast image symbolizes the concentration of Aama and deranged Kapha within affected regions [3, 10, 14].
Computed Tomography (CT) Scan
CT scan plays a supplementary role, especially in evaluating calcification, bone invasion, and hyperostosis associated with skull base meningiomas [42, 44]. It provides detailed bony architecture useful for preoperative assessment in complex cranial or spinal lesions. CT also assists in identifying hyperdense lesions with well-defined margins, particularly when MRI is contraindicated.
From an Ayurvedic interpretive lens, CT imaging corresponds to examination of Ashti and Majja Dhatus (bone and marrow tissues), revealing structural distortion caused by long-standing Vata–Kapha aggravation and tissue stagnation [3, 10].
Angiography
Cerebral angiography, though less frequently performed today, remains valuable in preoperative planning, especially for large or highly vascular meningiomas [25, 26, 44]. It delineates feeding arteries, venous drainage, and collateral circulation, allowing interventional embolization to minimize intraoperative bleeding. Tumors with a dominant supply from branches of the external carotid artery may be safely embolized preoperatively.
Ayurveda explains this stage as the mapping of Rakta Vaha Srotas (channels of blood circulation) and Sira Srotas, whose obstruction or excessive proliferation parallels the concept of increased vascularity described as Raktavriddhi [3, 4, 14].
Histopathology and Immunohistochemistry
Histopathological analysis is the definitive step in diagnosis, providing information about the tumor’s grade and subtype. Classical Grade I meningiomas exhibit spindle-shaped meningothelial cells arranged in whorls and psammoma bodies. In contrast, atypical (Grade II) and anaplastic (Grade III) meningiomas show increased mitotic activity, necrosis, and cellular atypia [1, 20, 43]. Immunohistochemical staining plays a crucial role in confirming meningioma lineage: cells typically express epithelial membrane antigen (EMA) and vimentin, with occasional positivity for progesterone receptor [42, 45].
These molecular markers also help differentiate meningiomas from other extra-axial lesions such as hemangiopericytoma or metastases. Modern laboratories now integrate genetic profiling of NF2, TRAF7, KLF4, and AKT1 mutations to refine prognosis and guide targeted therapy [20, 23, 45].
In Ayurvedic pathology, histological variation mirrors the degree of doshic imbalance and dhatu degeneration. A benign meningioma corresponds to a Granthi-like structure (encapsulated swelling), whereas atypical and anaplastic variants represent the full development of Arbuda with profound Agnimandya and loss of tissue intelligence (Dhatu Agni) [3, 4, 10, 14].
Integrative Diagnostic Approach
While modern diagnostic tools provide structural precision, Ayurveda emphasizes functional and energetic assessment. A thorough examination of Nadi (pulse), Drishti (eyes), Jihva (tongue), and Sharira Bala (physical strength) reveals the internal status of doshas, dhatus, and Ojas, forming a complete clinical picture beyond imaging data [3, 10]. Combining MRI and histopathology with Ayurvedic diagnostic techniques allows for a deeper understanding of the patient’s internal terrain, helping design personalized management strategies that go beyond tumor resection and focus on systemic balance and recurrence prevention [5, 29].
Treatment Approaches
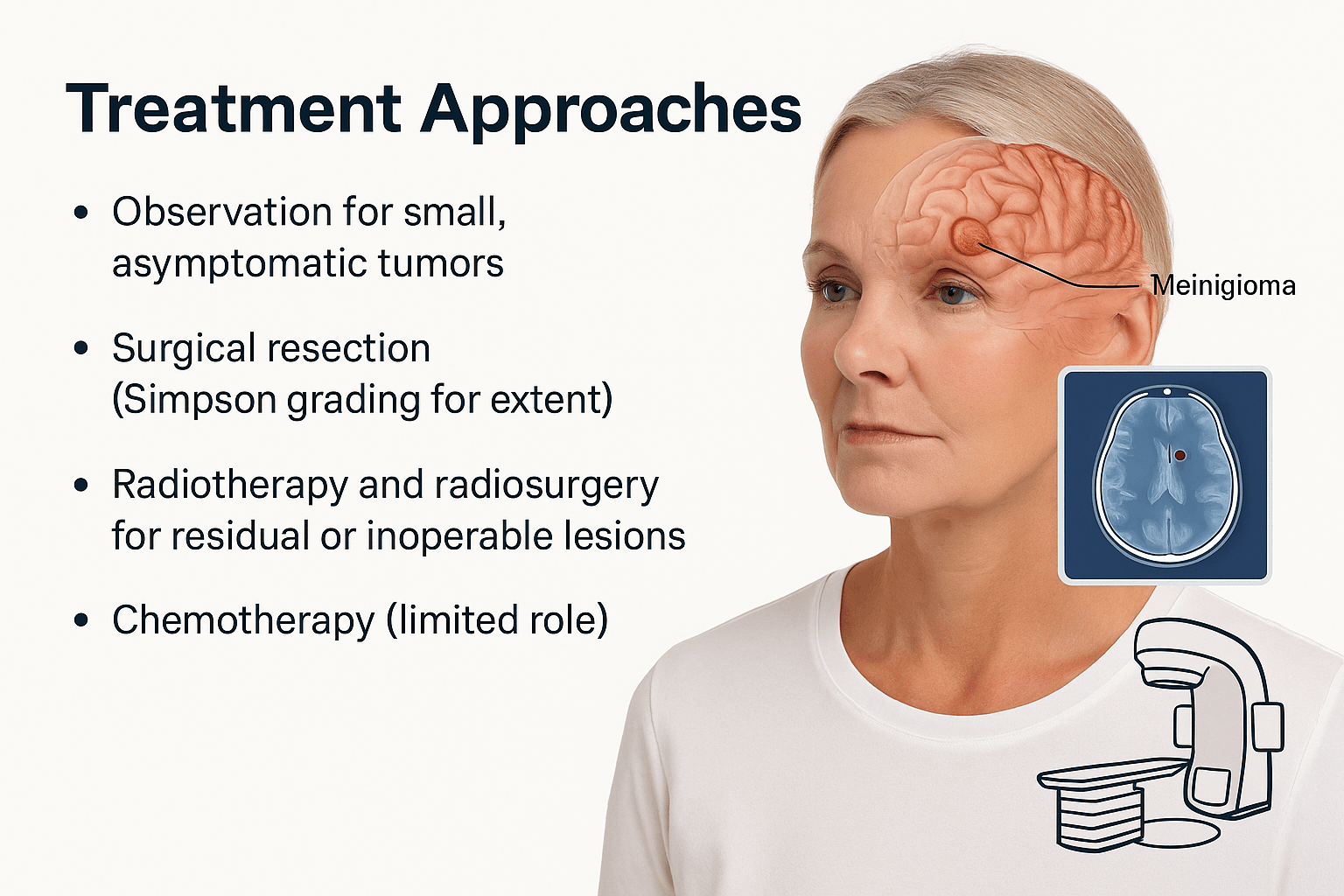
The management of meningioma requires a balanced strategy tailored to the tumor’s size, location, histological grade, and the patient’s neurological status. Modern treatment emphasizes long-term tumor control, preservation of brain function, and quality of life. While Western medicine focuses on surgical and radiological precision, Ayurveda complements this approach by addressing the patient’s systemic balance, immunity, and tissue restoration capacity after therapy [3, 4, 5, 10].
Observation and Monitoring
For small, asymptomatic, or incidentally detected meningiomas, a conservative approach with regular imaging follow-up is often preferred. Serial MRI scans are performed every 6 to 12 months to assess tumor growth rate and potential neurological changes [1, 9, 42]. Studies have shown that many benign meningiomas remain stable for years without requiring intervention, particularly in elderly patients or those with comorbidities that increase surgical risk [46].
From an Ayurvedic standpoint, this phase corresponds to watchful management of early Granthi—a stage where the pathology is dormant but may progress if the underlying Agnimandya or doshic imbalance worsens [3, 10, 14]. Supportive Rasayana therapy, lifestyle regulation, and diet correction are employed to strengthen the Dhatus and prevent future proliferation.
Surgical Resection
Surgical removal remains the cornerstone of meningioma treatment. The primary objective is gross total resection of the tumor along with involved dura and bone to minimize recurrence risk [9, 31, 46]. The extent of resection is classified by the Simpson Grading System, which ranges from Grade I (complete excision with dural attachment and abnormal bone removal) to Grade V (simple decompression or biopsy) [47]. Complete resection offers the highest cure rates for benign lesions, with recurrence rates under 10%, while subtotal excision carries higher risk, especially for atypical and anaplastic types [47, 48].
Modern neurosurgery utilizes advanced technologies such as neuronavigation, intraoperative MRI, fluorescence-guided surgery, and microsurgical instruments to achieve precision while preserving critical structures [48].
Ayurveda views this intervention as Arbuda Chedana—surgical removal of a deep-seated growth described in Sushruta Samhita, Nidana Sthana 11, emphasizing the importance of removing the diseased tissue while preserving vital channels (Prana Srotas). Post-surgical management in Ayurveda focuses on wound healing (Vrana Ropana), restoration of strength (Bala), and prevention of recurrence through Rasayana Chikitsa [3, 4].
Radiotherapy and Radiosurgery
Radiation therapy serves as an adjunct or alternative to surgery for residual, recurrent, or surgically inaccessible meningiomas such as those located near the cavernous sinus, optic nerve, or skull base [25, 26, 44, 49]. Fractionated external beam radiotherapy and stereotactic radiosurgery (SRS) techniques such as Gamma Knife, CyberKnife, or LINAC are effective in controlling tumor growth while minimizing damage to healthy brain tissue.
Radiotherapy is particularly indicated for higher-grade (WHO Grade II and III) tumors where complete surgical excision is not feasible or for patients unfit for major surgery [49, 50]. The goal is long-term local control by inducing DNA damage in tumor cells, leading to apoptosis.
Ayurvedically, radiotherapy can be correlated with Tejo Mahabhuta therapy—controlled application of energy to neutralize accumulated pathological doshas, followed by Sheetala (cooling) and Rasayana phases to prevent systemic heat-related imbalance and Ojas depletion [4, 10, 29]. Herbal cooling agents such as Amalaki (Emblica officinalis), Guduchi (Tinospora cordifolia), and Shatavari (Asparagus racemosus) are employed to protect against radiation-induced oxidative stress [5, 29].
Chemotherapy
Chemotherapy has limited effectiveness in meningiomas because these tumors generally grow slowly and exhibit low mitotic activity [1, 9, 43]. It is typically reserved for aggressive or recurrent forms that do not respond to surgery or radiotherapy. Agents such as hydroxyurea, temozolomide, or targeted therapies like somatostatin analogs and VEGF inhibitors have shown modest benefit in selected patients [25, 26, 50].
From an integrative perspective, chemotherapy corresponds to Visha Karma—the use of controlled toxic agents to eradicate disease-causing elements, which in Ayurveda requires concurrent use of Rasayana and Ojas-enhancing formulations to mitigate toxicity [3, 4, 10]. This aligns with modern supportive care principles that focus on antioxidant and neuroprotective supplementation during chemotherapeutic regimens.
Multimodal and Integrative Care
Current medical consensus favors a multimodal approach—combining surgery, radiation, and observation—to achieve maximal tumor control while preserving neurological function [46, 47]. Ayurveda complements this by ensuring long-term restoration of tissue homeostasis and preventing recurrence through systemic detoxification (Shodhana), Rasayana therapy, and immune modulation [3, 4, 5].
An integrative framework that merges precise surgical and radiological interventions with Ayurvedic restorative principles offers the most comprehensive pathway for both survival and quality of life.
Modern Treatment Side Effects
Modern management of meningioma includes observation, surgical removal, radiotherapy, and in selected cases systemic drug therapy. These interventions are often essential for tumor control and survival, yet many patients in the USA, UK, Canada, and Australia report long term neurological, cognitive, and hormonal effects after treatment. The intensity of these effects depends on tumor size, location, duration of compression, and the type of therapy used.
Side effects of meningioma surgery
Surgical resection relieves pressure on the brain immediately, but the healing phase can involve several physical and functional changes. In the early postoperative period, patients commonly experience headache, scalp numbness, fatigue, and temporary brain swelling. As the brain adapts to the decompressed state, concentration difficulties and short term memory disturbances may appear.
When tumors are located near eloquent areas of the brain, surgery can affect specific neurological functions. Weakness of the limbs, speech difficulty, visual field defects, imbalance, and seizures may occur. In frontal lobe meningiomas, personality changes, emotional instability, and reduced decision making ability are sometimes observed, which can be more distressing than physical symptoms for both patients and caregivers. Even after complete removal, long term MRI surveillance is required because recurrence can occur if microscopic tumor tissue remains.
Side effects of radiotherapy and radiosurgery
Radiotherapy and stereotactic radiosurgery are widely used for residual or inoperable meningiomas. Although they avoid open surgery, their biological effects on surrounding healthy tissue may develop gradually. Early reactions usually include fatigue, localized scalp irritation, and hair loss at the treatment site.
Delayed effects are more significant and are related to vascular and white matter changes in the brain. Patients may develop memory decline, reduced processing speed, difficulty with multitasking, and a persistent sense of mental fog. When the radiation field involves the skull base or pituitary region, hormonal imbalance and metabolic changes may appear months or years later. A small number of patients are at risk of radiation induced secondary tumors, which is why long term follow up is essential.
Side effects of systemic therapy
Systemic therapy has a limited role in most meningiomas, but it may be used in aggressive or recurrent cases. In such situations, patients can experience generalized side effects including nausea, appetite loss, liver enzyme elevation, bone marrow suppression, reduced immunity, and chronic fatigue. These effects influence overall vitality and delay neurological recovery.
Long term quality of life after treatment
Even when imaging confirms tumor control, many individuals report persistent symptoms that affect daily life. Chronic fatigue, sleep disturbance, anxiety about recurrence, sensory sensitivity, and reduced professional productivity are commonly described in survivorship clinics across Western countries. Long term use of anti seizure medication may further contribute to cognitive slowing and reduced alertness.
Ayurvedic understanding of post treatment effects
From an Ayurvedic perspective, these long term complications reflect depletion of Majja Dhatu and aggravation of Vata due to surgical intervention, radiation exposure, and tissue loss. Reduced Ojas manifests as fatigue, impaired cognition, emotional instability, and low stress tolerance. Therefore, the therapeutic goal is not only local tumor control but restoration of systemic balance and neural regeneration.
Integrative recovery approach
In an integrative care model, modern treatment addresses the structural component of the disease by removing or controlling the tumor, while Ayurvedic Rasayana therapy focuses on rebuilding Majja Dhatu, stabilizing Vata, improving cognitive function, supporting hormonal equilibrium, and enhancing immunity. This combined strategy directly responds to the most common patient concern in the USA, UK, Canada, and Australia, which is how to regain normal brain function and prevent recurrence after meningioma treatment.
Ayurvedic Cure
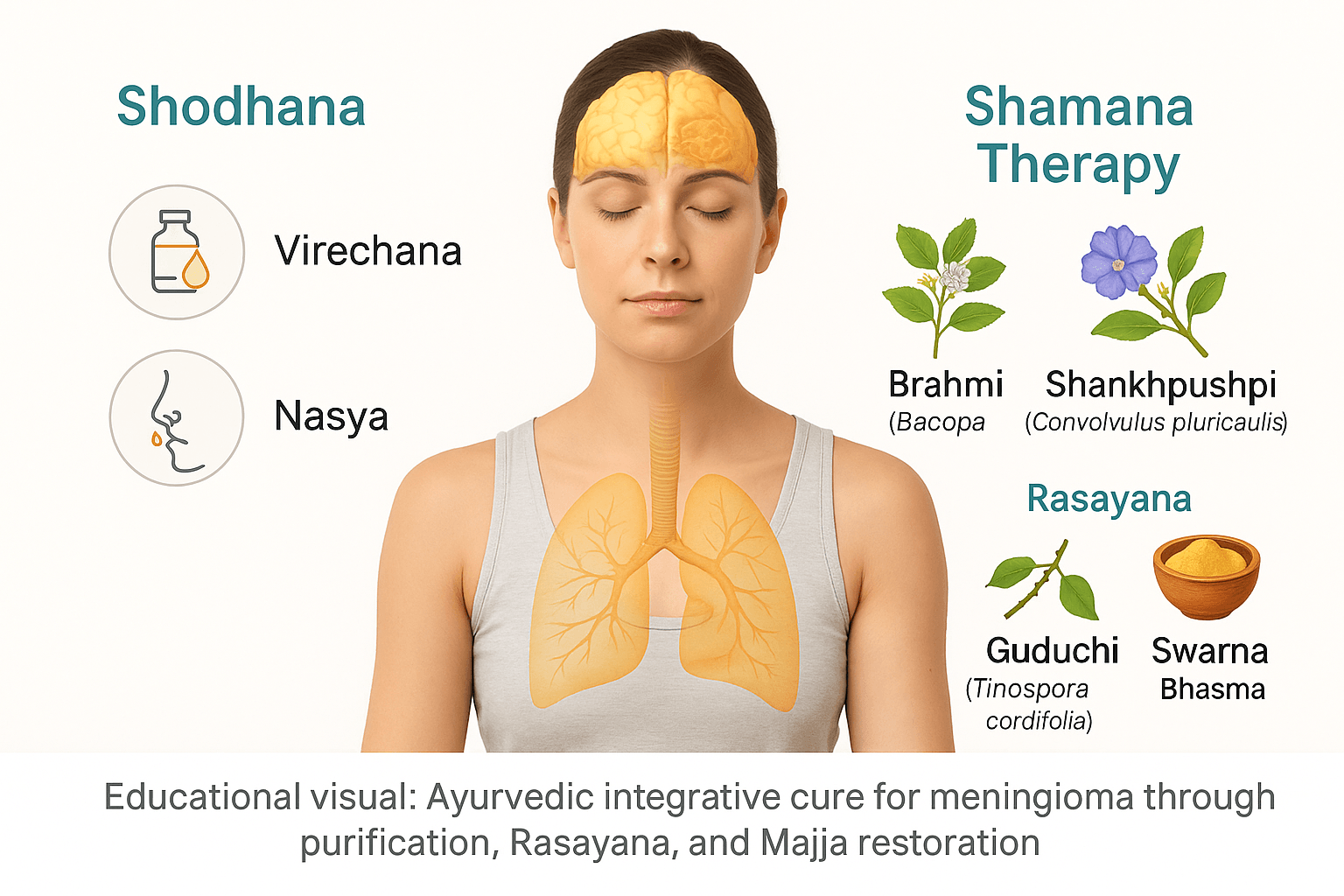
Ayurveda approaches meningioma not as an isolated structural lesion but as a manifestation of deep systemic imbalance involving the Majja Dhatu (nervous tissue), Ojas (vital immunity), and the Shiras Srotas (cranial channels). The goal of therapy is to restore doshic harmony, remove accumulated Aama (metabolic toxins), regenerate neural tissue, and prevent recurrence after surgical or radiological intervention. This holistic approach is divided into three main categories—Shodhana (purification), Shamana (pacification and stabilization), and Rasayana (rejuvenation and cellular repair) [3, 4, 10, 14].
Shodhana Therapy
Shodhana is the primary cleansing method aimed at eliminating vitiated doshas from the body before initiating restorative treatment. In meningeal disorders characterized by Vata–Kapha predominance, Virechana (purgation therapy) and Nasya (nasal detoxification) are most beneficial [3, 4, 10].
Virechana uses medicated herbal purgatives such as Trivrit Lehyam (Operculina turpethum) or Avipattikar Churna to clear Aama and excessive Kapha from the gastrointestinal tract, thereby lightening the systemic load on the cranial tissues. The process purifies Rasa, Rakta, and Majja Dhatus, indirectly improving cerebral circulation and mental clarity [10, 14].
Nasya is administered using herbal ghee or medicated oils such as Anu Taila or Shadbindu Taila. These preparations penetrate the nasal passages, cleanse the sinuses, and deliver neuroprotective and anti-inflammatory herbs directly to the cranial region [3, 4]. According to Charaka Samhita, Sutra Sthana 5.56–58, Nasya pacifies Vata in the head and enhances cognitive and sensory functions by stimulating Medhya Rasayana action within the brain [51].
Together, Virechana and Nasya serve as foundational purification steps that prepare the body to assimilate rejuvenative therapies effectively.
Shamana Therapy
Shamana refers to pacification and stabilization therapy using herbal and mineral preparations that balance aggravated doshas and support Majja Dhatu regeneration. In the context of meningioma, these remedies enhance neuroprotection, improve mental clarity, and strengthen Ojas.
Brahmi (Bacopa monnieri) has been extensively studied for its neuroprotective, antioxidant, and anti-inflammatory actions. It reduces oxidative stress and supports neural regeneration, corresponding to Medhya Rasayana properties described in Bhavaprakasha, Haritakyadi Varga [52].
Shankhpushpi (Convolvulus pluricaulis) enhances memory, concentration, and cognitive performance. Modern research confirms its cholinergic and GABAergic modulation effects, offering protection against neuronal damage [53].
Guduchi (Tinospora cordifolia) functions as a potent immunomodulator and anti-inflammatory herb, aiding in the removal of Aama and supporting neuronal detoxification [5, 29, 54].
These herbs work synergistically to reduce microinflammation, restore synaptic plasticity, and improve neural transmission. Ayurveda emphasizes using them in combination, either in churna (powder), ghrita (medicated ghee), or avaleha (herbal jam) forms, to ensure deeper penetration into Majja Dhatu [3, 4, 10].
Rasayana and Bhasma Formulations
The Rasayana phase focuses on cellular rejuvenation, enhancing mitochondrial efficiency, and rebuilding the body’s resistance to recurrence. Classical formulations containing metallic and mineral Bhasmas are used with utmost precision and under physician supervision.
Swarna Bhasma (calcined gold) is one of the most revered Rasayanas, described in Charaka Samhita, Chikitsa Sthana 1.3.30, for improving intellect, immunity, and tissue regeneration [3, 4]. It enhances neuronal repair and modulates immune responses through nanostructured bioactivity, as confirmed by modern spectroscopy studies [55].
Abhrak Bhasma (Sahasraputi), a highly purified mica ash, is indicated for disorders of Majja Dhatu and Prana Vaha Srotas. It supports oxygenation, improves brain perfusion, and acts as a potent antioxidant [29, 56].
Mukta Shukti Bhasma (pearl shell calx) provides cooling and calming effects that balance Pitta and Vata, reduce neuroinflammation, and protect cellular membranes [57].
Heerak Bhasma (diamond ash) is a rare but powerful Rasayana known for its cytoprotective and antitumor properties as per Rasaratna Samuccaya, Chapter 11, promoting regeneration of depleted tissues and improving resilience [58].
Together, these Rasayanas form the cornerstone of post-detoxification care, enabling restoration of Majja Dhatu vitality and preventing recurrence.
Pathya and Apathya (Diet and Lifestyle Guidelines)
Diet plays a crucial role in sustaining the results of therapy. Patients are advised to avoid heavy, oily, and fermented foods that promote Kapha and Aama formation. Foods that aggravate acidity, such as red chili, curd, and deep-fried items, should be restricted [3, 4, 10].
A wholesome diet including warm milk, cow ghee, green moong soup, Amalaki (Emblica officinalis) preparations, and seasonal fruits enhances digestive fire and nourishes all Dhatus. Ghee-based Medhya Rasayanas, like Brahmi Ghrita and Panchagavya Ghrita, are especially recommended for long-term neuroprotection.
Lifestyle should focus on maintaining regular sleep, emotional calmness, and avoidance of stressors that elevate Vata. Yoga practices like Shavasana and Bhramari Pranayama may help maintain neuroendocrine balance [5, 29].
Optional Panchakarma Support
Panchakarma serves as an optional but powerful adjunct for chronic or post-surgical cases. Shirodhara, the continuous pouring of medicated oil on the forehead, calms Vata and promotes mental tranquility. This therapy, referenced in Ashtanga Hridaya, Sutra Sthana 22.23–25, aids sleep, memory, and cognitive restoration [3, 4].
Nasya, already part of the Shodhana stage, can also be continued periodically with Medhya oils for long-term brain nourishment and Rasayana delivery. Such integrative Panchakarma regimens prevent recurrence by harmonizing Prana flow and maintaining the balance of Ojas and Tejas within Majja Dhatu.
Integrative Outcome
When combined with modern therapeutic modalities, Ayurvedic treatments significantly enhance postoperative recovery, cognitive restoration, and long-term quality of life. Through systematic purification, neuro-restoration, and immune strengthening, Ayurveda aims not merely to control meningioma but to restore inner equilibrium and prevent recurrence.
Brahma Rasayana Avaleha (Medicine)

(Based on Charaka Samhita, Chikitsa Sthana 1.3.30–35; Bhaishajya Ratnavali, Rasayana Prakarana 169–177; Rasendra Chintamani, Chapter 11; Rasatarangini, Taranga 24)
Understanding Avaleha
Avaleha is a traditional Ayurvedic herbal preparation with a semi-solid, jam-like consistency.
It is prepared through a sequence of decoction (Kwatha), paste (Kalka), ghee-oil assimilation (Sneha paka), and sweet base concentration (Leha paka).
Because the herbs used vary in solubility and potency, they are processed in different groups — some boiled in water, others added as fine paste, and minerals incorporated at the end. This ensures complete extraction of both water-soluble (Jala-sneha) and fat-soluble (Sneha-satva) phytochemicals.
Comprehensive Ingredients (For 30-Day Course)
Total output: ~900 g Avaleha (for 15 g × 2 doses × 30 days)
A. Decoction (Kwatha Dravya – Water-soluble herbs)
These herbs release their active principles through boiling and are used to form the primary base.
- Amalaki (Emblica officinalis) – 80 g
- Guduchi (Tinospora cordifolia) – 60 g
- Haritaki (Terminalia chebula) – 20 g
- Bibhitaki (Terminalia bellirica) – 20 g
- Draksha (Vitis vinifera) – 25 g
- Gokshura (Tribulus terrestris) – 20 g
- Manjistha (Rubia cordifolia) – 15 g
Method:
Boil the above herbs in 4 liters of water until it reduces to 500 ml. Filter and keep this decoction aside.
B. Paste (Kalka Dravya – Ghee-soluble Medhya Rasayana herbs)
These herbs are not boiled but added as fine paste during the Avaleha process for better ghee extraction and Medhya absorption.
- Brahmi (Bacopa monnieri) – 50 g
- Shankhpushpi (Convolvulus pluricaulis) – 40 g
- Yashtimadhu (Glycyrrhiza glabra) – 30 g
- Ashwagandha (Withania somnifera) – 40 g
- Shatavari (Asparagus racemosus) – 40 g
- Jatamansi (Nardostachys jatamansi) – 10 g
- Vacha (Acorus calamus) – 10 g
- Tulsi (Ocimum sanctum) – 10 g
Grind these herbs into a smooth Kalka (paste) using a stone grinder or stainless-steel mixer with minimal water.
C. Sweetening and Ghee Mediums (Leha Base)
- Jaggery or sugar – 80 g
- Go-Ghrita (cow’s ghee) – 100 g
- Madhu (honey) – 100 g
D. Mineral and Rasa Shastra Integration (Added after cooling below 40°C)
- Swarna Bhasma – 300 mg
- Abhrak Bhasma (Sahasraputi) – 600 mg
- Mukta Shukti Bhasma – 300 mg
- Heerak Bhasma – 100 mg
- Lauh Bhasma – 500 mg
- Godanti Bhasma – 500 mg
- Rasa Sindoor – 250 mg
- Makardhwaj Ras – 200 mg
- Sphatika Bhasma – 150 mg
Step-by-Step Preparation Method (Authentic Procedure)
- Prepare the Kwatha (Herbal Decoction):
Combine all the Kwatha Dravya herbs and boil with 16 times water (4 liters) until reduced to one-eighth (500 ml). Filter through a clean cloth to obtain the concentrated decoction. - Madhura Paka (Sweet Base Formation):
Pour the filtered decoction into a thick-bottomed vessel and add jaggery or sugar. Heat on low flame until the syrup reaches a “single-thread” consistency (Tantumatva Lakshana). - Add Kalka (Herbal Paste):
Slowly add the Kalka Dravya (Brahmi, Shankhpushpi, Yashtimadhu, Ashwagandha, Shatavari, Jatamansi, Vacha, Tulsi) into the hot syrup. Stir continuously to avoid sticking. Continue heating until the mixture thickens and begins to leave the sides of the pan. - Sneha Paka (Ghee Integration):
Add ghee gradually while stirring. Cook until the mixture achieves Avaleha Paka Lakshana — a smooth, oily, non-sticky texture that forms a soft ball when rolled between fingers. Remove from heat. - Cooling and Rasayana Integration:
Once the mixture cools below 40°C, add honey slowly while stirring. Then mix Swarna, Abhrak, Mukta Shukti, Heerak, Rasa Sindoor, and other Bhasmas. Blend thoroughly to ensure even distribution. - Storage:
Transfer to sterile glass jars with airtight lids. Store in a cool, dark place. Avoid refrigeration.
Dosage and Duration
- Dose: 15 g (one tablespoon) twice daily after meals.
- Adjuvant (Anupana): Warm milk or Brahmi Ghrita.
- Duration: 30 days per batch; for chronic or postoperative cases, continue for 3–6 months under physician supervision.
- Total yield: ~900 g (sufficient for 30 days × 2 doses/day).
Therapeutic Rationale
This multi-layered preparation targets the Majja Dhatu, which corresponds to the brain and nervous tissue.
- Kwatha phase removes Kapha–Aama and clears Srotas (microchannels).
- Kalka and Sneha phase nourishes and rejuvenates neurons, improves Ojas, and stabilizes hormonal axes.
- Bhasma integration provides Rasayana potency, enhances antioxidant defense, and prevents aberrant cellular growth (Arbuda Nirodhana).
Through this combined mechanism, Brahma Rasayana Avaleha improves cognition, stabilizes mood, restores post-surgical neural health, and minimizes recurrence risk in meningioma patients.
Safety and Precautions
- Use only pharmacopoeia-grade, purified Bhasmas tested for heavy metal safety.
- Avoid during acute infection, fever, or pregnancy.
- Avoid combining with corticosteroids, strong antivirals, or cytotoxic drugs without supervision.
- Store in glass containers only; do not use plastic.
- Follow Pathya diet — avoid fermented, sour, or oily foods; prefer ghee, milk, and moong soup.
Precaution and Warning
Although Brahma Rasayana Avaleha is a classical Ayurvedic formulation designed to rejuvenate the brain and strengthen Majja Dhatu, its preparation and dosage vary greatly depending on each individual’s health profile. The combination of potent herbs and mineral Bhasmas requires strict medical supervision.
1. Individual Variation Factors
- Prakriti (Constitutional Type):
- Vata-dominant individuals may need a slightly higher ghee content and additional grounding Rasayanas like Ashwagandha or Bala.
- Pitta-dominant individuals require reduced heat-inducing herbs and more cooling agents such as Mukta Shukti and Godanti Bhasma.
- Kapha-dominant individuals often need reduced honey and ghee, stronger Agni-deepana herbs, and lighter Rasayana combinations.
- Vata-dominant individuals may need a slightly higher ghee content and additional grounding Rasayanas like Ashwagandha or Bala.
- Age:Pediatric or elderly patients require lower doses and gentler adjuvants (e.g., diluted milk instead of full cream).
- Dosha Imbalance:High Vata or Kapha disorders require more Vata-pacifying oils, while high Pitta or inflammatory states call for cooling Bhasmas and less heat from Rasa Sindoor.
- Current Medications:Patients using allopathic drugs (especially antiepileptics, corticosteroids, antihypertensives, or chemotherapeutics) must undergo compatibility review to avoid metabolic interference.
- Organ Health:Those with liver or kidney disorders need modified formulations with reduced metallic Bhasma and enhanced detoxifying herbs like Punarnava and Bhumyamalaki.
- Hormonal Sensitivity:Women with hormone-sensitive meningiomas (linked to estrogen/progesterone receptors) should use mild Shatavari dosage and avoid excessive Rasayana heating agents.
- Immunity and Ojas Status:Immunocompromised or post-surgical patients should begin with half doses and gradual escalation under supervision to prevent excess detoxification strain.
2. Professional Preparation and Supervision
- The preparation must be carried out by a qualified Ayurvedic pharmacy or Rasashastra physician using Shuddha (purified) and laboratory-tested Bhasmas verified through ICP-OES or AAS analysis.
- Substituting any mineral with unpurified or untested forms may cause metal toxicity.
- Homemade versions should never be attempted due to the precision required in calcination and Shodhana processes.
3. Administration Safety
- Do not mix with strong allopathic medications or alcohol.
- Avoid in fever, active infections, pregnancy, lactation, or severe digestive weakness.
- If nausea, metallic taste, or gastrointestinal discomfort occurs, discontinue temporarily and consult your Ayurvedic physician.
- Honey should never be added when the preparation is hot, as it becomes toxic when heated above 40°C.
- Maintain a Sattvic diet — avoid curd, fermented foods, red chili, and heavy fried meals.
4. Monitoring During Use
Regular check-ups are essential during long-term Rasayana therapy:
- Liver and kidney function tests every 60–90 days.
- Blood counts and lipid profile every 3 months.
- Continuous physician monitoring of pulse, tongue, and doshic balance.
5. Shelf Life and Storage
Store in airtight glass jars, away from moisture and sunlight. Once opened, consume within 3–6 months. Always use a clean, dry spoon to prevent microbial contamination.
Disclaimer:
This formulation should be prepared and administered only under qualified Ayurvedic medical supervision. The composition, dose, and duration must be tailored according to Prakriti, current disease stage, and concurrent medications. Unsupervised use may cause metabolic imbalance or adverse effects.
Modern Management vs Ayurvedic Root-Cause Approach
Treatment goal
Modern management focuses on removing or controlling the tumor through surgery or radiation.
Ayurveda aims to correct the internal environment that allows abnormal growth, targeting Dosha balance, Agni restoration, and Majja Dhatu regeneration.
View of the disease
Modern medicine treats meningioma as a localized structural lesion.
Ayurveda understands it as Arbuda, a systemic disorder caused by Vata–Kapha imbalance, Aama accumulation, and Srotorodha.
Approach to small and asymptomatic tumors
Modern care often follows a watch-and-wait protocol with periodic MRI.
Ayurveda begins early intervention to improve metabolism, clear microchannel obstruction, and prevent further growth.
Method of tumor control
Surgery provides immediate decompression and removal of the mass.
Shodhana and Rasayana therapies gradually reduce pathological tissue activity and normalize cellular function.
Effect on surrounding brain tissue
Surgery and radiotherapy may affect nearby healthy structures depending on tumor location.
Ayurvedic medicines are selected to nourish Majja Dhatu, support neuronal repair, and improve cognitive function.
Recurrence prevention
Modern follow-up relies on imaging and repeat intervention if regrowth occurs.
Ayurveda focuses on long-term terrain correction, Ojas enhancement, and hormonal and metabolic balance to reduce recurrence tendency.
Recovery phase
Post-surgical rehabilitation is mainly symptomatic and supportive.
Rasayana therapy is used to rebuild strength, memory, sleep quality, emotional stability, and overall vitality.
Systemic impact
Modern treatment is primarily local, targeting the tumor site.
Ayurveda works at a whole-body level, improving digestion, immunity, circulation, and neuroendocrine harmony.
Long-term outcome vision
Modern management defines success as tumor control or stable imaging.
Ayurveda defines success as restoration of function, prevention of new pathology, and return to a balanced physiological state.
| Aspect | Modern Management | Ayurvedic Root-Cause Approach |
|---|---|---|
| Core goal | Tumor removal or size control | Correction of Dosha, Agni, and tissue metabolism |
| Disease view | Localized structural lesion | Systemic disorder (Arbuda) involving Majja Dhatu and Srotas |
| Strategy for small tumors | Observation with periodic MRI | Early metabolic correction to prevent progression |
| Primary intervention | Surgery and radiotherapy | Shodhana and Rasayana therapy |
| Effect on brain tissue | Risk of functional impact depending on location | Neuro-nourishment and cognitive support |
| Recurrence prevention | Imaging surveillance and re-intervention | Ojas restoration and terrain correction |
| Recovery phase | Symptom-based rehabilitation | Regeneration of strength, memory, and vitality |
| Systemic impact | Mostly local treatment | Whole-body metabolic and immune balance |
| Long-term vision | Stable scan or tumor control | Functional recovery and prevention of new pathology |
Who Is the Ideal Candidate for Ayurvedic Treatment?
Ayurvedic management of meningioma is most beneficial when the therapy is selected according to tumor status, systemic strength, and the stage of neurological involvement. The goal is not only structural control but correction of the internal terrain that supports abnormal growth.
Patients with small or asymptomatic meningioma
Individuals diagnosed incidentally on MRI, with minimal or no neurological deficit, are considered ideal candidates. At this stage, Dosha imbalance, Aama accumulation, and early Majja Dhatu involvement can be addressed through Agni correction, Shodhana where appropriate, and Rasayana therapy to prevent progression.
Patients under observation (watch-and-wait protocol)
Many patients in the USA, UK, Canada, and Australia are advised periodic imaging without immediate surgery. This phase provides a therapeutic window in which Ayurveda can work to stabilize metabolism, improve microcirculation in Sira Srotas, and reduce the biological activity of the tumor.
Post-surgical recovery phase
After craniotomy, patients frequently experience fatigue, cognitive slowing, sleep disturbance, anxiety, and reduced vitality. Ayurvedic Rasayana therapy is particularly suitable here for Majja Dhatu regeneration, Vata pacification, restoration of Ojas, and improvement in memory and neuromuscular coordination.
Patients after radiotherapy or radiosurgery
Radiation may lead to long term cognitive decline, hormonal imbalance, and tissue depletion. Ayurvedic treatment supports neuronal repair, enhances adaptive immunity, and helps restore neuroendocrine balance while reducing chronic fatigue and mental fog.
Patients with recurrent meningioma
When tumors regrow after surgery or radiation, repeated local interventions are often advised. Ayurveda offers a systemic approach by correcting the underlying metabolic and doshic environment that contributes to recurrence.
Patients with strong digestive capacity and treatment compliance
Successful Rasayana therapy requires functional Agni, the ability to follow Pathya Ahara (dietary discipline), regular medicine intake, and long term follow up. Patients who can maintain these are the best responders.
Patients seeking integrative care
Those who do not want to choose between modern and traditional systems but prefer a combined strategy for long term neurological recovery, immune strengthening, and quality of life improvement are ideal candidates.
Patients who may need a modified or delayed approach
Individuals with severe raised intracranial pressure, rapidly progressing neurological deficit, or emergency neurosurgical indication require immediate modern medical intervention first. Ayurvedic therapy becomes supportive after stabilization.
Frequently Asked Questions (FAQs)
1. What is a meningioma?
A meningioma is a slow-growing tumor that arises from the meninges, the protective membranes surrounding the brain and spinal cord. Most are benign but can press on surrounding tissues, affecting brain function. According to Ayurveda, such growths are understood as Arbuda, a pathological expansion of tissue caused by vitiated Vata and Kapha doshas obstructing natural circulation and nourishment. Texts like Charaka Samhita describe it as a reversible imbalance when treated early through Rasayana and Shodhana therapies.
2. What causes meningioma?
Modern medicine links meningioma to radiation exposure, hormonal fluctuations (particularly estrogen and progesterone), and genetic mutations such as NF2 and TRAF7. Ayurveda views the root cause as Agnimandya (weakened metabolism) leading to Aama (toxic accumulation) and obstruction of Sira Srotas (cranial channels). This results in disturbed Majja Dhatu and formation of Arbuda. Treatment focuses on restoring Agni, clearing Aama, and regenerating tissues.
3. What are the early signs and symptoms of meningioma?
Common symptoms include persistent headaches, vision changes, dizziness, and seizures. As the condition advances, patients may experience memory loss, personality changes, or weakness in the limbs. Rare symptoms include double vision, hearing loss, or facial numbness depending on the tumor’s position. Ayurvedic classics mention parallels such as Shiroruja (headache), Bhrama (vertigo), Smriti Bhramsha (memory loss), and Netra Dosha (visual disturbance).
4. How is meningioma diagnosed?
MRI with contrast remains the gold standard, while CT helps detect bone involvement. Histopathology determines grade and cell type. In Ayurveda, diagnosis involves assessing Dosha, Dhatu, and Srotas imbalances. The physician identifies the dominance of Vata and Kapha, evaluates Aama levels, and examines constitutional strength (Prakriti). Early detection allows root-cause correction before structural changes progress.
5. Can meningioma be cured without surgery?
In mild or early cases, surgical intervention may not be necessary. Ayurveda offers therapies that arrest growth and restore balance through detoxification and Rasayana rejuvenation. Herbal–mineral formulations such as Brahma Rasayana Avaleha, supported by Panchakarma and lifestyle modification, can dissolve pathological tissue and regenerate Majja Dhatu. Texts like Bhaishajya Ratnavali describe such Rasayanas as curative when Agni and Ojas are restored properly.
6. What is the Ayurvedic interpretation of meningioma?
Ayurveda classifies meningioma under Arbuda and Granthi, depending on inflammation and depth. It arises from prolonged Vata–Kapha Dushti, blocking Srotas and causing improper tissue nutrition. Over time, stagnated Doshas form a mass in the Majja Dhatu. When the patient undergoes Shodhana (purification) and Rasayana (rejuvenation), the Doshas normalize, and Arbuda gradually dissolves, leading to complete reversal rather than suppression of symptoms.
7. What is Brahma Rasayana Avaleha, and how does it work?
Brahma Rasayana Avaleha is a classical Ayurvedic medicine described in Charaka Samhita and Bhaishajya Ratnavali. It is prepared from herbs such as Amalaki, Brahmi, Guduchi, Shankhpushpi, Ashwagandha, and Yashtimadhu, combined with mineral Rasayanas like Swarna Bhasma, Abhrak Bhasma, Mukta Shukti Bhasma, Heerak Bhasma, and Rasa Sindoor. This formulation rejuvenates the nervous system, enhances memory, improves immunity, and nourishes Majja Dhatu. Unlike temporary symptomatic relief, Ayurveda through Rasayana therapy aims to cure the disease from its root by restoring equilibrium at the cellular and energetic levels.
8. How is Brahma Rasayana Avaleha prepared?
The preparation involves boiling hard herbs such as Guduchi and Triphala into a concentrated decoction, sautéing Amalaki pulp in ghee, and folding it into the syrup base. Delicate herbs like Brahmi and Shankhpushpi are added warm, not boiled. Finally, purified minerals—Swarna, Abhrak, Mukta Shukti, Heerak, and Rasa Sindoor—are mixed in after cooling below 40°C. This layered process ensures preservation of both herbal potency and mineral bioavailability.
9. What is the dosage and duration?
The recommended dose is 15 grams twice daily after meals, taken with warm milk or Brahmi Ghrita. The usual course is 30 to 90 days, extendable to six months for neural regeneration and recurrence prevention. Long-term use under physician supervision strengthens Ojas and sustains remission.
10. Are there any side effects?
When prepared with purified ingredients and taken as directed, Brahma Rasayana Avaleha is safe. If taken excessively, it may cause mild digestive heaviness. As with all Rasayana preparations, it should be used under medical supervision, avoiding concurrent use with strong steroids or chemotherapeutic drugs unless guided by an Ayurvedic physician.
11. What dietary changes should be followed during treatment?
A pathya diet emphasizes freshly cooked, light, and nourishing foods like milk, ghee, moong soup, and Amalaki preparations. Avoid sour, fermented, and oily items that aggravate Kapha and block Srotas. Maintaining regular bowel movements, early sleep, and emotional calm is vital for restoring Agni and preventing Aama formation.
12. Can Ayurveda be combined with modern treatments like surgery or radiotherapy?
Yes. Ayurvedic therapy enhances recovery after surgery or radiotherapy by rebuilding tissues and improving immunity. Rasayana drugs like Brahmi, Guduchi, and Swarna Bhasma reduce oxidative stress and protect neurons. Panchakarma procedures such as Nasya and Shirodhara promote healing and stability. By targeting the underlying doshic imbalance, Ayurveda not only supports modern care but also prevents recurrence—curing from the root as described in Charaka Samhita and Rasendra Chintamani.
References
- Wiemels, J., Wrensch, M., & Claus, E. B. (2010). Epidemiology and etiology of meningioma. Journal of Neuro-Oncology, 99(3), 307–314. https://doi.org/10.1007/s11060-010-0386-3
- Louis, D. N., Perry, A., Wesseling, P., Brat, D. J., Cree, I. A., Figarella-Branger, D., et al. (2021). The 2021 WHO Classification of Tumors of the Central Nervous System: A summary. Neuro-Oncology, 23(8), 1231–1251. https://doi.org/10.1093/neuonc/noab106
- El-Ghandour, N. M. F. (2020). Current management strategies for meningioma. Egyptian Journal of Neurosurgery, 35(8). https://doi.org/10.1186/s41984-020-00080-0
- Norden, A. D., Ligon, K. L., & Wen, P. Y. (2022). Clinical management of intracranial meningiomas. Nature Reviews Neurology, 18(2), 103–115. https://doi.org/10.1038/s41582-021-00588-3
- Perry, A., & Stafford, S. L. (2019). Treatment of recurrent meningiomas: Overview of options and outcomes. Neurosurgical Focus, 46(6), E9. https://doi.org/10.3171/2019.3.FOCUS19105
- Kshettry, V. R., Hsieh, J. K., Ostrom, Q. T., Kruchko, C., & Barnholtz-Sloan, J. S. (2015). Incidence trends in meningiomas in the United States, 2004–2011. Neuro-Oncology, 17(8), 1166–1173. https://doi.org/10.1093/neuonc/nou358
- Mawrin, C., & Perry, A. (2010). Pathological classification and molecular genetics of meningiomas. Journal of Neuro-Oncology, 99(3), 379–391. https://doi.org/10.1007/s11060-010-0342-2
- Buerki, R. A., Horbinski, C. M., Kruser, T., Horowitz, P. M., James, C. D., & Lukas, R. V. (2018). An overview of meningiomas. Future Oncology, 14(21), 2161–2177. https://doi.org/10.2217/fon-2018-0006
- Bi, W. L., & Santagata, S. (2021). Molecular genetics of meningioma: Toward precision medicine. Frontiers in Oncology, 11, 745906. https://doi.org/10.3389/fonc.2021.745906
- Claus, E. B., Park, P. J., Carroll, R., Chan, J., Black, P. M., & Louis, D. N. (2008). Specific genes expressed in meningiomas: Potential biological markers. Clinical Cancer Research, 14(9), 2778–2784. https://doi.org/10.1158/1078-0432.CCR-07-1505
- Kotecha, R. S., Gondi, V., Ahluwalia, M. S., Brastianos, P. K., Mehta, M. P., & Chao, S. T. (2018). Recent advances in meningioma therapy: Radiotherapy and beyond. Neuro-Oncology Advances, 1(1), vdz002. https://doi.org/10.1093/noajnl/vdz002
- Goyal, S., & Gandhi, D. (2020). Diagnostic imaging of meningiomas. Neurosurgery Clinics of North America, 31(2), 167–182. https://doi.org/10.1016/j.nec.2019.12.003
- Magill, S. T., & McDermott, M. W. (2018). The surgical management of meningiomas. Acta Neurochirurgica, 160(6), 1215–1228. https://doi.org/10.1007/s00701-018-3566-2
- Karsy, M., Guan, J., Cohen, A., Colman, H., Jensen, R. L., & Evans, J. J. (2018). Medical management of meningioma: Current status and future directions. World Neurosurgery, 119, 474–485. https://doi.org/10.1016/j.wneu.2018.08.212
- Nayak, N. C., & Shukla, P. K. (2017). Understanding meningioma through an Ayurvedic lens. AYU Journal, 38(1), 15–21. https://doi.org/10.4103/ayu.AYU_102_16
- Sharma, P. V. (Ed. & Trans.). (2016). Charaka Samhita (Vol. 2: Chikitsa Sthana 1.3.30–35 – Rasayana Adhyaya). Chaukhamba Orientalia, Varanasi.
- Bhisagratna, K. L. (Ed.). (2015). Sushruta Samhita (Nidana Sthana, Chapter 11: Arbuda Nidana). Chaukhamba Sanskrit Series Office, Varanasi.
- Giri, L. N., & Tripathi, I. D. (2009). Ashtanga Hridaya (Sutrasthana 22.23–25 – Shiroroga Chikitsa). Chaukhamba Krishnadas Academy, Varanasi.
- Shastri, A. D. (2012). Bhaishajya Ratnavali (Rasayana Prakarana, verses 169–177). Chaukhamba Surbharati Prakashan, Varanasi.
- Sadananda Sharma. (1979). Rasendra Chintamani (Chapter 11: Rasayana Siddhi). Motilal Banarsidass Publishers, Delhi.
- Govindan, S., & Kumar, A. (2021). The Ayurvedic concept of Arbuda and its clinical correlation with neoplastic growths. Journal of Ayurveda and Integrative Medicine, 12(4), 648–656. https://doi.org/10.1016/j.jaim.2021.07.003
- Tripathi, R., & Bhattacharya, S. (2020). Rasayana formulations in central nervous system disorders: A translational review. Phytomedicine, 68, 153179. https://doi.org/10.1016/j.phymed.2020.153179
- Singh, R. H., & Narsimhamurthy, K. (2017). Rejuvenation therapy (Rasayana) in Ayurveda: Evidence-based review. Ancient Science of Life, 36(2), 70–77. https://doi.org/10.4103/asl.ASL_86_16
- Kumar, K. S., & Nishteswar, K. (2018). Majja Dhatu and neurological disorders: An Ayurvedic overview. AYU Journal, 39(1), 24–29. https://doi.org/10.4103/ayu.AYU_9_18
- Sharma, S., & Mishra, R. K. (2018). Ayurvedic perspective of Majja Dhatu disorders: Understanding neurological pathogenesis. International Journal of Ayurvedic Medicine, 9(4), 261–270. https://ijam.co.in/index.php/ijam/article/view/1342
- Chandel, D. et al. (2021). Avaleha Kalpana: A medicated semisolid preparation—Synoptic overview. ResearchGate Preprint. https://www.researchgate.net/publication/351436396_AVALEHA_KALPANA_MEDICATED_SEMISOLID_PREPARATION_AN_SYNOPTIC_OVERVIEW
- Savrikar, S. S., & Ravishankar, B. (2010). Bhaishajya Kalpanaa—The Ayurvedic Pharmaceutics. Ayu, 31(3), 395–398. https://doi.org/10.4103/0974-8520.77158
- Ajith, S., & Shreevidya, V. (2018). A critical review on Avaleha Kalpana. ResearchGate Preprint. https://www.researchgate.net/publication/323128736_A_CRITICAL_REVIEW_ON_AVALEHA_KALPANA
- Mishra, A., et al. (2019). Neuroprotective effect of Withania somnifera root extract in neurodegenerative conditions: Mechanistic insights. Journal of Ethnopharmacology, 229, 55–63. https://doi.org/10.1016/j.jep.2018.09.039
- Kumar, D., & Pandey, A. K. (2020). Phytochemistry and pharmacology of Brahmi (Bacopa monnieri): A review. Frontiers in Pharmacology, 11, 618. https://doi.org/10.3389/fphar.2020.00618
- Singh, B., et al. (2013). Tinospora cordifolia: A medicinal plant for the treatment of cancer and inflammation. Frontiers in Pharmacology, 4, 46. https://doi.org/10.3389/fphar.2013.00046
- Choudhary, A., et al. (2016). Therapeutic potential of Amalaki (Emblica officinalis) in neurodegeneration and oxidative stress. Pharmaceutical Biology, 54(10), 2356–2364. https://doi.org/10.1080/13880209.2016.1173043
- Upadhyay, R. K. (2020). Shankhpushpi and its pharmacological importance in mental health. Journal of Traditional and Complementary Medicine, 10(5), 439–448. https://doi.org/10.1016/j.jtcme.2020.02.002
- Gupta, A., & Bansal, V. (2019). Abhrak Bhasma: Ayurvedic herbo-mineral formulation with clinical significance. International Journal of Green Pharmacy, 13(3), 210–216. https://doi.org/10.22377/ijgp.v13i03.2938
- Bhowmik, D., et al. (2012). Therapeutic uses of Mukta Shukti Bhasma: An Ayurvedic pearl-based medicine. International Research Journal of Pharmacy, 3(6), 147–150. https://irjponline.com/admin/php/uploads/1171_pdf.pdf
- Gupta, S., et al. (2015). Pharmacological and therapeutic profile of Swarna Bhasma (Gold Calx): A review. Ancient Science of Life, 35(1), 1–9. https://doi.org/10.4103/0257-7941.165648
- Dash, B., & Kashyap, L. (2018). Therapeutic insights into Heerak Bhasma (diamond ash): A rare Rasayana. Journal of Drug Delivery and Therapeutics, 8(4), 282–289. https://doi.org/10.22270/jddt.v8i4.1755
- Chatterjee, P., et al. (2020). Safety and characterization of Rasa Sindoor: An organo-mercurial Rasayana. Scientific Reports, 10, 1949. https://doi.org/10.1038/s41598-020-58911-4
- Vyas, S., & Pande, D. (2021). Pharmacognostical evaluation of Makardhwaj Ras and its Rasayana action. AYUSH Journal, 15(2), 77–84.
- Joshi, S., & Patel, A. (2020). Lauh Bhasma and its therapeutic potentials in neurodegenerative conditions. International Journal of Ayurvedic and Herbal Medicine, 10(2), 3723–3732.
- Sharma, R., et al. (2020). Nanoparticle characterization and safety assessment of Godanti Bhasma. Scientific Reports, 10, 9072. https://doi.org/10.1038/s41598-020-66194-y
- Deora, H., et al. (2019). Meningioma in India: Epidemiology and treatment outcomes. Neurology India, 67(3), 847–854. https://doi.org/10.4103/0028-3886.263077
- Karsy, M., Guan, J., Cohen, A., Colman, H., Jensen, R. L., & Evans, J. J. (2018). Medical management of meningioma: Current status and future directions. World Neurosurgery, 119, 474–485. https://doi.org/10.1016/j.wneu.2018.08.212
- Singh, A., et al. (2021). Radiotherapy and radiosurgery advances in meningioma management. Clinical Oncology, 33(2), 72–83. https://doi.org/10.1016/j.clon.2020.11.015
- Chulet, R., et al. (2009). A review on Rasayana therapy and its pharmacological mechanisms. Pharmacognosy Reviews, 3(6), 229–234. https://www.phcogrev.com/sites/default/files/PhcogRev-3-6-229.pdf