- IBS C Constipation Predominant Irritable Bowel Syndrome
- IBS D Diarrhea Predominant Irritable Bowel Syndrome
- IBS M Mixed Type Irritable Bowel Syndrome
- IBS U Unclassified Irritable Bowel Syndrome
- How IBS Subtypes Differ Clinically
- Can IBS Type Change Over Time
- Which IBS Type Is Most Severe
- How Doctors Identify IBS Subtype
- Medical Review and Diagnostic Guidance
- Why Correct IBS Classification Matters
- Frequently Asked Questions About IBS Types
- References
What IBS Types Mean in Clinical Practice
IBS types refer to the way irritable bowel syndrome is classified based on a person’s dominant bowel habit and symptom pattern. Doctors recognize IBS as a functional gut brain disorder, meaning the problem lies in how the brain and digestive system communicate rather than in visible damage to the intestines. Because symptoms vary from person to person, IBS types help explain why two individuals with the same diagnosis can experience very different digestive problems [1][6].
Irritable bowel syndrome presents differently in each person, which is why understanding symptom patterns is essential. If you are looking for a complete explanation of symptoms, diagnosis, and long term healing approach, you can read the full Irritable Bowel Syndrome Ayurvedic diagnosis and Cure guide here. https://panaceayur.com/ibs-ayurvedic-treatment-diagnosis-symptoms-cure/
How IBS Types Reflect Gut and Brain Interaction
Each of the IBS types represents a different expression of altered gut brain signaling. In some people, intestinal movement slows down and leads to constipation. In others, the gut becomes overactive, resulting in frequent loose stools. For many, the bowel pattern alternates unpredictably. These variations occur because the nervous system, gut sensitivity, and motility respond differently in each person, which is why IBS types can shift over time based on stress, hormones, infections, or lifestyle factors [6][9].
Why IBS Types Are Defined by Symptoms Rather Than Tests
IBS types are defined by symptom patterns instead of blood tests or scans because standard investigations often appear normal in people with IBS. Clinicians rely on internationally accepted diagnostic frameworks such as the Rome IV criteria, which classify IBS types according to stool form and frequency. This symptom based approach allows doctors to better understand how IBS behaves in your body and to tailor evaluation and treatment decisions more accurately [1][9].
Why Stool Pattern Matters in IBS Diagnosis
Stool Pattern as the Core Diagnostic Signal
In irritable bowel syndrome, stool pattern is one of the most reliable indicators doctors use to understand how the condition behaves in your body. Unlike many digestive diseases where blood tests or scans reveal inflammation or damage, IBS is diagnosed by observing how your bowel habits change over time. Stool consistency and frequency reflect how quickly or slowly the intestines are moving and how the gut nervous system is responding, which makes stool pattern central to identifying IBS types accurately [1][6].
How Stool Pattern Reflects Gut and Brain Communication
The speed at which stool moves through the intestines is controlled by the interaction between the gut and the brain. When this communication is altered, stool may become hard and infrequent, loose and urgent, or fluctuate between the two. These patterns are not random. They reflect differences in intestinal motility, nerve sensitivity, and stress response unique to each person. By paying attention to stool pattern, doctors gain insight into how strongly gut brain signaling is disrupted and in which direction it is leaning [6][9].
Why Stool Pattern Is More Useful Than Single Symptoms
Abdominal pain, bloating, and gas are common across all IBS types, but stool pattern helps distinguish one type from another. Two people may both report pain and discomfort, yet one experiences chronic constipation while the other has frequent diarrhea. Stool pattern provides a consistent, measurable way to classify IBS when other symptoms overlap. This is why international diagnostic systems such as the Rome IV criteria rely heavily on stool form and bowel habit trends rather than isolated symptoms [1][9].
How Doctors Use Stool Pattern to Avoid Misdiagnosis
Tracking stool pattern over weeks or months helps doctors differentiate IBS from other digestive conditions that may appear similar at first. Persistent changes in stool without alarm signs support an IBS diagnosis, while patterns that include bleeding, weight loss, or nighttime symptoms prompt further investigation. By focusing on stool pattern, clinicians reduce unnecessary testing while still ensuring that serious conditions are not overlooked. This approach balances patient safety with accurate diagnosis in everyday clinical practice [1][6][11].
IBS C Constipation Predominant Irritable Bowel Syndrome
Core Symptom Pattern in IBS C
IBS C is defined by constipation as the dominant bowel habit along with recurrent abdominal discomfort. If you have this IBS type, you may notice infrequent bowel movements, hard or pellet like stools, and the need to strain excessively during defecation. Many patients describe a persistent feeling that the bowel has not emptied completely, even after using the toilet. Clinicians rely on these stool pattern features to identify IBS C, as outlined in internationally accepted diagnostic frameworks such as the Rome IV criteria [1][11].
Associated Digestive and Systemic Features
Beyond constipation itself, IBS C often comes with significant bloating and visible abdominal distension. You may feel tightness or pressure in the lower abdomen that improves only partially after a bowel movement. Gas retention is common, not because of excess gas production alone, but because slowed intestinal movement traps gas within the bowel. Research also shows that people with IBS C frequently experience heightened gut sensitivity, meaning normal intestinal activity can feel uncomfortable or painful [3][6][12].
How IBS C Affects Daily Life
Living with IBS C can have a subtle but persistent impact on daily functioning. You may feel sluggish, heavy, or mentally fatigued, especially on days when bowel movements are absent. Travel, dehydration, long periods of sitting, and changes in routine often worsen symptoms. Many patients report planning their day around bathroom availability or avoiding social situations due to discomfort and bloating. Studies evaluating quality of life consistently show that IBS C significantly affects physical comfort, emotional well being, and overall productivity, even when symptoms appear mild on the surface [3][10].
Why IBS C Is Not Just Simple Constipation
It is important to understand that IBS C is not the same as occasional or lifestyle related constipation. In IBS C, constipation occurs alongside altered gut brain signaling, which affects motility, sensation, and stress response. This explains why laxatives alone often provide incomplete relief and why symptoms tend to recur. Recognizing IBS C as a distinct IBS type helps doctors avoid oversimplifying the condition and supports a more accurate, individualized approach to diagnosis and care [1][6][11].
Irritable bowel syndrome presents differently in each person, which is why understanding symptom patterns is essential. If you are looking for a complete explanation of symptoms, diagnosis, and long term healing approach, you can read the full Irritable Bowel Syndrome Ayurvedic diagnosis and cure guide here.
IBS D Diarrhea Predominant Irritable Bowel Syndrome
Core Symptom Pattern in IBS D
IBS D is characterized by diarrhea as the dominant bowel habit along with recurring abdominal discomfort. If you have this IBS type, you may experience frequent loose or watery stools, an urgent need to use the toilet, and multiple bowel movements within a short period of time, especially in the morning. Many patients describe a constant fear of urgency, which can feel difficult to control. Doctors identify IBS D by observing these stool patterns over time, as defined by symptom based diagnostic frameworks such as the Rome IV criteria [1][11].
Associated Digestive and Systemic Features
Along with diarrhea, IBS D is often associated with cramp like abdominal pain that improves temporarily after a bowel movement. You may notice burning or irritation around the rectal area due to frequent stool passage. Fatigue is also common, partly because rapid bowel movements can disrupt fluid balance and leave you feeling drained. Research shows that people with IBS D frequently have increased gut sensitivity, meaning even normal intestinal contractions can trigger pain or discomfort [4][6][5].
How IBS D Affects Daily Life
IBS D can significantly affect daily routines and emotional well being. You may avoid eating before travel, meetings, or social events out of concern that symptoms will flare suddenly. Many patients report heightened anxiety linked to the unpredictability of bowel habits, which can further intensify gut symptoms through the gut brain connection. Studies assessing quality of life demonstrate that IBS D often leads to social withdrawal, reduced work productivity, and ongoing stress related to symptom control [5][10].
Why IBS D Is More Than Frequent Diarrhea
It is important to understand that IBS D is not simply a problem of having frequent stools. In this IBS type, altered gut brain signaling plays a central role, affecting intestinal speed, pain perception, and stress responsiveness. This explains why anti diarrheal medications alone may not fully resolve symptoms and why episodes often return during periods of emotional or physical stress. Recognizing IBS D as a distinct IBS type allows clinicians to better understand its underlying mechanisms and avoid mistaking it for infection or inflammatory disease when routine tests appear normal [1][6][9].
IBS M Mixed Type Irritable Bowel Syndrome
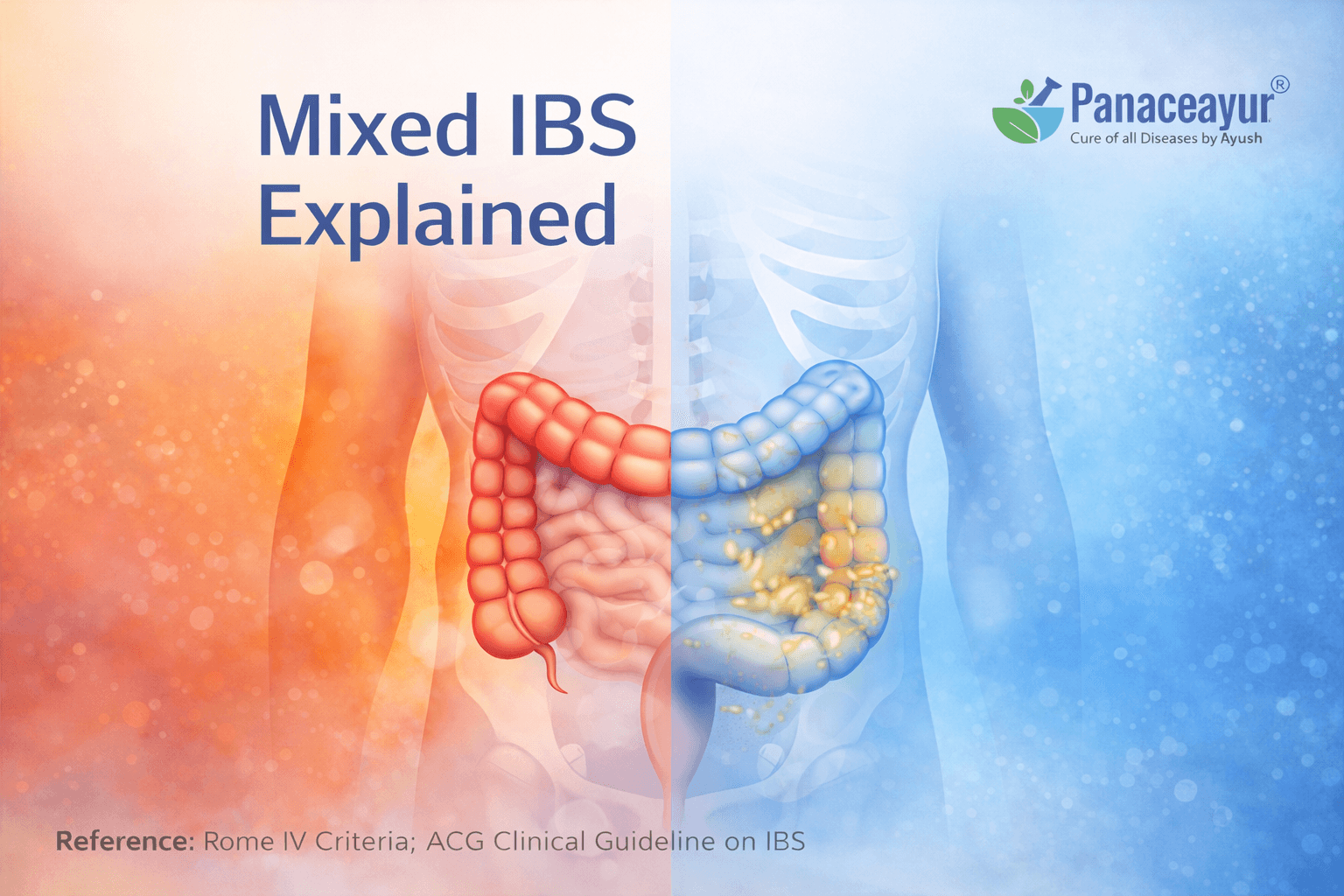
Core Symptom Pattern in IBS M
IBS M is defined by a mixed bowel pattern in which constipation and diarrhea alternate over time. If you have this IBS type, you may experience periods of hard infrequent stools followed by episodes of loose or urgent bowel movements. These changes are not random and usually occur in cycles that can shift over weeks or months. Doctors recognize IBS M when neither constipation nor diarrhea clearly dominates, making symptom tracking over time especially important for accurate classification [1][6][9].
Associated Digestive and Systemic Features
Along with alternating bowel habits, IBS M is commonly associated with significant bloating, abdominal discomfort, and variable pain intensity. You may notice that pain feels different from day to day, sometimes dull and heavy during constipated phases and cramp like during diarrheal phases. Many people with IBS M also report sleep disturbance, fatigue, and heightened sensitivity to stress. Research suggests that these fluctuating symptoms reflect instability in gut brain signaling rather than a single fixed digestive abnormality [5][6][12].
How IBS M Affects Daily Life
Living with IBS M can feel particularly frustrating because symptoms are unpredictable. You may plan your routine around one bowel pattern only to find that it suddenly changes. This uncertainty often affects confidence in social and work settings, as you may not know whether constipation or urgency will dominate on a given day. Quality of life studies show that people with IBS M frequently report a high symptom burden because they experience challenges associated with both constipation and diarrhea, rather than just one pattern [6][10].
Why IBS M Is Often Perceived as the Most Disruptive IBS Type
IBS M is often perceived as more disruptive because it reflects a highly sensitive and reactive gut brain system. Instead of remaining locked into one pattern, the digestive system shifts between extremes based on stress, hormonal changes, infections, diet, or routine disruptions. This explains why treatment responses may vary and why symptoms can feel difficult to predict or control. Understanding IBS M as a distinct IBS type helps clinicians recognize the need for flexible, individualized evaluation rather than a one size fits all approach [1][5][9].
IBS U Unclassified Irritable Bowel Syndrome
Core Symptom Pattern in IBS U
IBS U refers to irritable bowel syndrome symptoms that do not clearly fit into constipation predominant, diarrhea predominant, or mixed patterns. If you fall into this category, you may experience abdominal discomfort, bloating, or irregular bowel habits, but without a consistent stool pattern that meets the criteria for other IBS types. Doctors use the IBS U classification when symptoms are present yet remain inconsistent over time, making this an important category rather than a vague or meaningless label [1][7].
Associated Digestive and Systemic Features
People with IBS U often report non specific digestive complaints such as intermittent bloating, mild abdominal pain, or occasional changes in stool form that fluctuate without a clear pattern. Systemic symptoms such as fatigue or stress sensitivity may also be present, even when bowel habits seem relatively normal. Research indicates that IBS U can reflect early or evolving gut brain dysfunction, where symptom patterns have not yet stabilized into a recognizable IBS type [7][9].
How IBS U Affects Daily Life
Although IBS U may appear less severe on paper, it can still affect daily comfort and confidence. You may feel uncertain about your symptoms because they do not follow a predictable pattern, which can lead to repeated medical visits or frustration with inconclusive answers. Some patients report dismissing their symptoms initially, only to realize over time that digestive discomfort continues to interfere with concentration, sleep, or stress tolerance. Quality of life impact can be subtle but persistent, especially when symptoms remain unexplained [7][10].
Why IBS U Should Not Be Ignored
IBS U is often an early stage or transitional form of irritable bowel syndrome rather than a final diagnosis. Over time, stool patterns may shift toward constipation predominant, diarrhea predominant, or mixed forms. Recognizing IBS U allows clinicians to monitor symptom evolution and avoid premature labeling or unnecessary interventions. Understanding this IBS type also helps patients appreciate that their symptoms are valid, even if they do not yet fit neatly into other categories [1][7][9].
How IBS Subtypes Differ Clinically
Differences in Bowel Behavior Rather Than Disease Severity
Although IBS is a single diagnostic condition, its subtypes differ mainly in how the bowel behaves rather than in how serious the disease is. IBS C, IBS D, IBS M, and IBS U are not separate diseases. They are different expressions of the same underlying gut brain disorder. What changes from one person to another is the direction and stability of bowel movement patterns, which is why two individuals with IBS can have very different daily experiences despite sharing the same diagnosis [1][6].
IBS C Versus IBS D in Real Life
In IBS C, the bowel tends to move slowly, leading to infrequent and hard stools, bloating, and a sensation of fullness. In IBS D, the bowel moves too quickly, resulting in urgency, loose stools, and fear of accidents. While both groups experience abdominal discomfort, the timing and triggers differ. IBS C symptoms often worsen with dehydration and inactivity, while IBS D symptoms are more likely to flare after meals, during stress, or early in the day. These contrasting patterns help clinicians distinguish between subtypes even when pain and bloating overlap [1][6][11].
How IBS M Differs From Stable IBS Types
IBS M stands apart because it lacks consistency. Instead of remaining fixed in a constipation or diarrhea pattern, the bowel alternates between extremes. This fluctuation reflects instability in gut brain signaling rather than a single dominant motility issue. Clinically, IBS M can be harder to classify and manage because symptom patterns shift over time. Patients often feel confused when treatments that help one phase worsen the other, which is why careful symptom tracking is essential in this subtype [5][6][9].
Where IBS U Fits in the Clinical Spectrum
IBS U occupies an important place in the clinical spectrum of IBS. It includes patients whose symptoms are real but do not yet meet formal criteria for other subtypes. Rather than being a weak diagnosis, IBS U often represents an early or evolving phase of IBS. Over time, bowel patterns may become more defined and shift into IBS C, IBS D, or IBS M. Recognizing IBS U helps clinicians avoid mislabeling symptoms while maintaining appropriate follow up [1][7][9].
Why IBS Subtypes Can Overlap and Change
IBS subtypes are not fixed labels for life. Stress, infections, hormonal changes, medications, and shifts in gut microbiota can all influence bowel behavior. This is why a person may start with IBS U, move into IBS D during a stressful period, and later develop IBS C. Understanding these overlaps helps patients and doctors view IBS as a dynamic condition rather than a static diagnosis, reducing confusion and unrealistic expectations [5][9][12].
Can IBS Type Change Over Time
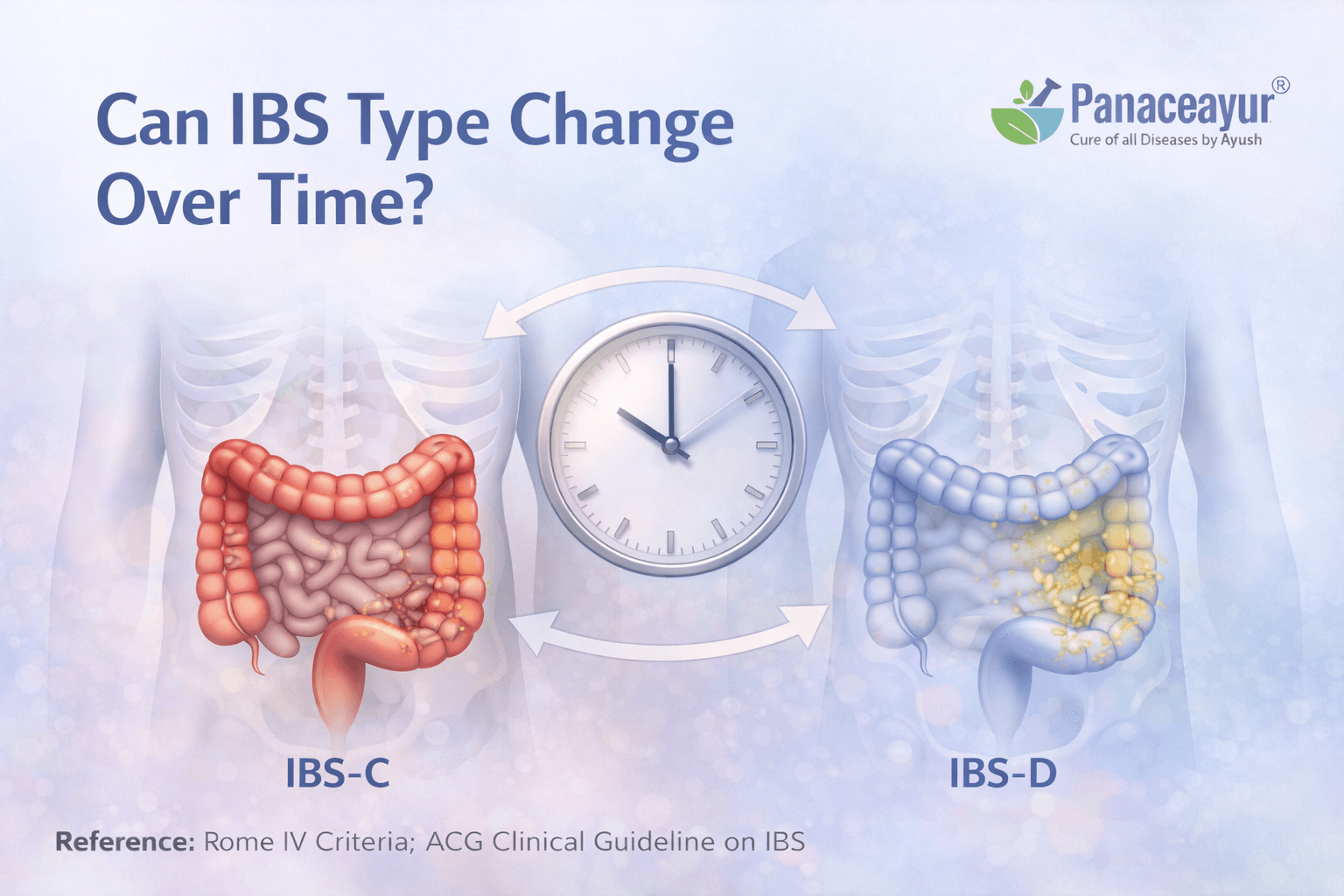
Why IBS Is a Dynamic Condition Rather Than a Fixed Label
IBS is not a static condition, and the type you experience today may not remain the same in the future. Many patients notice that their bowel pattern changes over months or years. This happens because IBS is driven by functional changes in gut brain communication rather than permanent damage to the intestines. When the factors influencing this communication shift, symptoms can also change direction, moving from constipation to diarrhea or alternating between both [6][9].
Role of Stress and the Nervous System
Stress plays a major role in shaping IBS symptoms and subtype changes. The gut and brain are closely connected through the nervous system, and emotional stress can directly alter intestinal movement and sensitivity. During prolonged stress, some people develop faster bowel transit and IBS D type symptoms, while others experience slowed movement and IBS C patterns. When stress levels change, bowel behavior often shifts with it, explaining why IBS types are not permanent for many individuals [5][9].
Influence of Hormones and Life Stages
Hormonal changes can also influence IBS type over time. Many patients report changes in bowel habits during phases such as puberty, pregnancy, postpartum periods, or menopause. Hormones affect gut motility and pain perception, which can tilt symptoms toward constipation, diarrhea, or fluctuation. This is one reason IBS M is commonly seen during transitional life stages rather than remaining stable long term [6][9].
Impact of Infections, Diet, and Medications
Gut infections, even after they resolve, can alter intestinal sensitivity and movement, sometimes leading to a shift in IBS type. Certain medications, dietary changes, or prolonged antibiotic use may also influence gut function and microbiota balance. These factors can push symptoms toward a different bowel pattern, reinforcing the idea that IBS types reflect current gut behavior rather than a permanent diagnosis [9][12].
What This Means for You as a Patient
Understanding that IBS type can change helps set realistic expectations. If your symptoms shift, it does not mean your diagnosis was wrong or that something new has suddenly gone wrong. It means your gut brain system is responding differently to internal or external influences. Recognizing this flexibility allows doctors to reassess symptoms over time and adjust evaluation strategies accordingly, rather than locking you into a single IBS type indefinitely [1][6].
Which IBS Type Is Most Severe
Severity in IBS Is About Impact, Not the Label
When people ask which IBS type is the most severe, doctors do not answer based on the subtype name alone. IBS severity is determined by how much the symptoms affect your daily life, emotional well being, and ability to function, rather than whether you have IBS C, IBS D, IBS M, or IBS U. Two people with the same IBS type can experience very different levels of discomfort and disruption, which is why severity is considered on an individual basis [6][10].
Why IBS M Is Often Experienced as More Burdensome
IBS M is often perceived as more severe by patients because it combines challenges seen in both constipation and diarrhea. You may feel physically uncomfortable during constipated phases and anxious or restricted during diarrheal phases. This unpredictability can be mentally exhausting, as you may not know which symptoms will dominate on a given day. Quality of life studies show that people with IBS M frequently report a higher overall symptom burden due to constant fluctuation rather than symptom intensity alone [6][9][10].
IBS D and Quality of Life Disruption
IBS D can feel particularly severe because of urgency and the fear of losing bowel control. Even when pain is moderate, the constant need to locate a restroom can limit travel, work performance, and social interaction. Many patients report planning their lives around bathroom access, which significantly affects independence and confidence. Research consistently links IBS D with higher anxiety levels and greater social avoidance compared to other IBS types [5][10].
IBS C and Chronic Discomfort Over Time
IBS C is sometimes underestimated in terms of severity because it may appear less urgent than diarrhea. However, chronic bloating, abdominal fullness, and difficulty passing stool can cause persistent discomfort that wears down physical and mental resilience over time. Patients often describe feeling heavy, slow, or uncomfortable for days at a stretch, which can affect concentration, mood, and productivity. Long term quality of life impact in IBS C is well documented, even when symptoms are not dramatic [3][10].
Why IBS U Severity Is Often Overlooked
IBS U is frequently assumed to be mild, but this is not always the case. The lack of a clear pattern can lead to uncertainty, repeated medical consultations, and frustration. Some patients feel dismissed because their symptoms do not fit neatly into defined categories, which can increase stress and symptom awareness. Severity in IBS U often comes from unpredictability and lack of clarity rather than symptom intensity alone [7][10].
What Doctors Actually Assess When Judging Severity
Clinicians assess IBS severity by looking at symptom frequency, pain intensity, impact on sleep, emotional distress, and daily functioning. The subtype provides useful information, but it does not determine how serious the condition feels to you. Understanding this helps patients avoid comparing themselves to others and encourages a more personalized view of IBS, where management decisions are guided by lived experience rather than labels [6][11].
How Doctors Identify IBS Subtype
Why Diagnosis Starts With Listening to Your Symptoms
Doctors identify IBS subtype primarily by listening carefully to how you describe your bowel habits over time. Unlike conditions that can be diagnosed with a single blood test or scan, IBS requires a detailed symptom history. Clinicians focus on the pattern of bowel movements, the relationship between abdominal discomfort and defecation, and how symptoms behave across weeks or months. This patient centered approach reflects the functional nature of IBS and places your lived experience at the core of diagnosis [1][6].
Role of Stool Pattern Tracking in Clinical Evaluation
Stool pattern tracking plays a central role in identifying IBS subtype. Doctors often ask you to describe stool form, frequency, and consistency using everyday language rather than medical jargon. Some clinicians recommend keeping a brief symptom diary to capture trends over time. This helps distinguish whether constipation, diarrhea, or mixed patterns dominate most days. Consistency across time is more important than isolated episodes, which is why short term changes do not automatically redefine IBS type [1][9].
Use of Rome IV Criteria in Subtype Classification
The Rome IV criteria provide a standardized framework that doctors use worldwide to classify IBS and its subtypes. According to these criteria, IBS is diagnosed when recurrent abdominal pain is associated with changes in stool frequency or form. Subtypes are then defined based on the proportion of bowel movements that are hard, loose, or mixed. This method ensures that IBS subtyping is grounded in reproducible symptom patterns rather than subjective impressions [1][6][9].
Why Tests Are Used to Exclude Other Conditions
Although IBS itself does not show abnormalities on routine tests, doctors may still order investigations to rule out other conditions that can mimic IBS symptoms. Blood tests, stool studies, or imaging are used selectively based on age, symptom severity, and warning signs. The goal is not to confirm IBS through testing, but to ensure that inflammatory, infectious, or structural diseases are not missed. Once these conditions are excluded, IBS subtype classification becomes more reliable [8][11].
How Doctors Reassess IBS Type Over Time
IBS subtype is not always determined once and for all at the first visit. Doctors often reassess bowel patterns during follow up visits, especially if symptoms change. A person initially classified as IBS U may later meet criteria for IBS C, IBS D, or IBS M. This ongoing reassessment reflects the dynamic nature of IBS and helps ensure that clinical decisions remain aligned with current symptom behavior rather than past labels [1][6][9].
Medical Review and Diagnostic Guidance
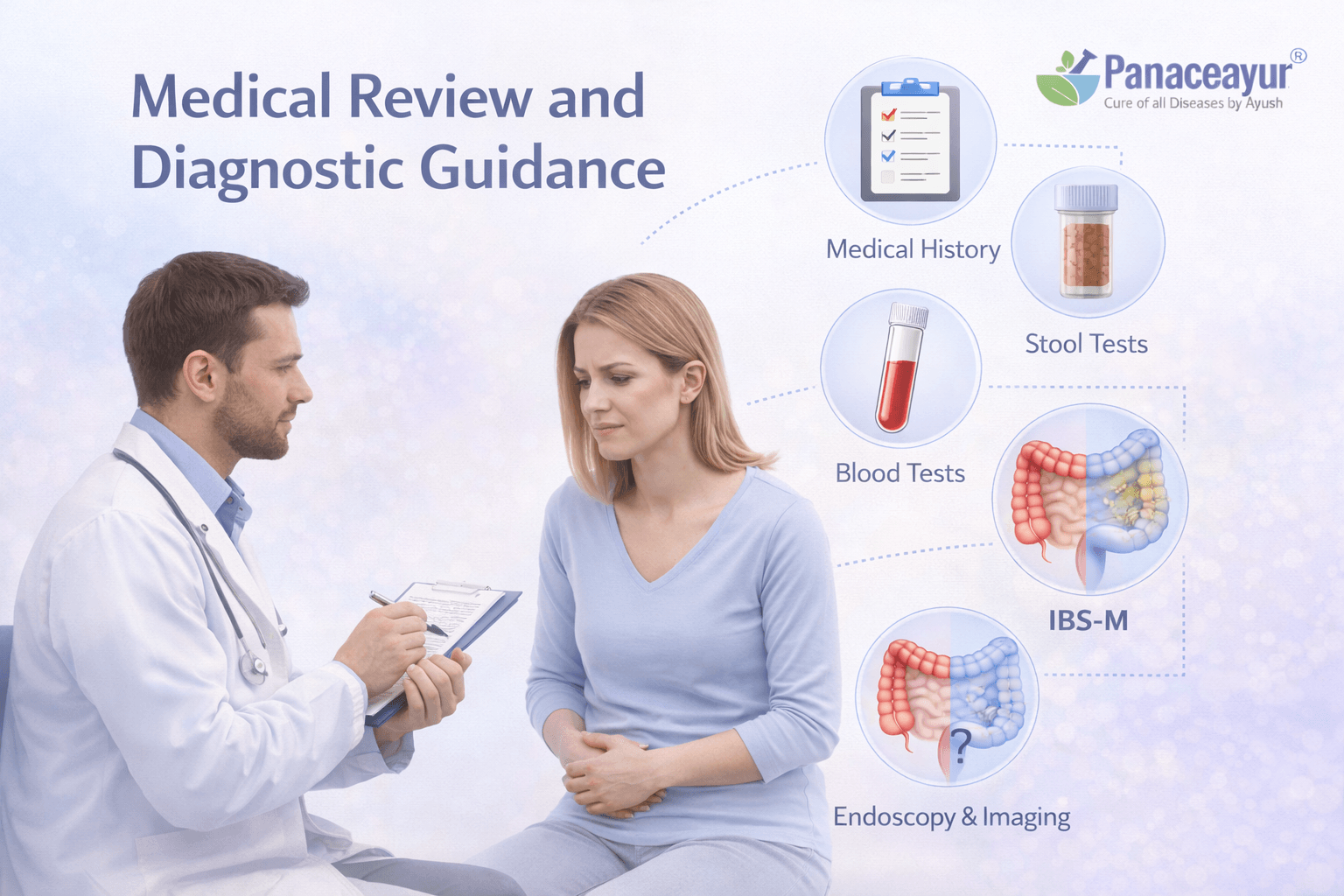
IBS Is a Diagnosis of Exclusion, Not Assumption
Doctors do not diagnose irritable bowel syndrome by assumption or by ruling in symptoms alone. IBS is considered a diagnosis of exclusion, meaning other medical conditions that can cause similar digestive symptoms must first be reasonably ruled out. This approach protects patients from missed diagnoses and ensures that IBS is identified only when no structural, inflammatory, or infectious disease explains the symptoms. International guidelines emphasize that a careful clinical evaluation is the foundation of safe IBS diagnosis [8][11].
How Clinicians Decide When Further Testing Is Needed
Not every person with IBS symptoms requires extensive testing. Doctors assess age, symptom duration, family history, and overall health before deciding on investigations. In younger individuals without concerning features, a detailed history and symptom pattern analysis may be sufficient. In other cases, targeted tests such as blood work or stool analysis are used to exclude conditions like inflammatory bowel disease, celiac disease, or chronic infection. This selective approach avoids unnecessary procedures while maintaining diagnostic accuracy [11].
Warning Signs That Require Additional Evaluation
Certain symptoms signal the need for further medical evaluation beyond routine IBS assessment. These include unintentional weight loss, rectal bleeding, anemia, fever, persistent nighttime symptoms, or a family history of serious gastrointestinal disease. When such features are present, doctors expand the diagnostic workup to ensure that IBS is not masking another condition. Recognizing these warning signs helps maintain patient safety and reinforces that IBS should never be diagnosed casually [8][11].
Why Normal Test Results Still Matter in IBS
Patients often feel confused or frustrated when test results return normal despite ongoing symptoms. In IBS, normal investigations are not a dismissal of symptoms but an important part of diagnosis. They confirm the absence of structural disease and support the understanding that symptoms arise from altered gut brain function. This reassurance can reduce anxiety, which itself plays a role in symptom severity and persistence [6][9].
The Role of Ongoing Medical Review
IBS management does not end with a single diagnosis. Doctors continue to review symptoms over time, especially if patterns change or new concerns arise. Regular follow up allows clinicians to reassess IBS subtype, monitor quality of life impact, and revisit diagnostic considerations if needed. This ongoing review reflects best clinical practice and acknowledges that IBS is a dynamic condition requiring attentive, patient centered care [1][6][11].
Why Correct IBS Classification Matters
Accurate Classification Shapes Clinical Decision Making
Correctly identifying IBS type helps doctors understand how your digestive system is behaving at a functional level. IBS C, IBS D, IBS M, and IBS U reflect different patterns of bowel movement and gut sensitivity, and these patterns influence how symptoms present day to day. When classification is accurate, clinicians can interpret symptoms more clearly and avoid confusing IBS with other digestive disorders that may require different evaluation pathways [1][6].
Preventing Treatment Mismatch and Frustration
One of the most common reasons patients feel that IBS care is ineffective is treatment mismatch. Approaches that may help diarrhea predominant symptoms can worsen constipation, and strategies aimed at constipation may aggravate urgency or loose stools. Correct IBS classification reduces this risk by aligning evaluation and management strategies with the dominant bowel pattern. This prevents unnecessary trial and error and helps patients feel that their symptoms are being understood rather than generalized [6][11].
Improving Symptom Monitoring and Long Term Outcomes
When IBS is classified correctly, both patients and doctors can track symptom changes more meaningfully over time. You can recognize whether shifts in bowel habits represent a temporary flare or a true change in IBS type. This shared understanding improves communication during follow up visits and allows earlier adjustment when symptoms evolve. Research shows that structured symptom monitoring is associated with better long term symptom control and patient confidence [1][9].
Supporting Realistic Expectations and Patient Confidence
Clear classification helps patients develop realistic expectations about their condition. Understanding that IBS types can change reduces fear when symptoms shift and prevents unnecessary alarm. It also reinforces that IBS is a functional condition influenced by stress, lifestyle, and physiological changes rather than a progressive structural disease. This perspective supports psychological reassurance, which is a key component of long term symptom stability [6][10].
Guiding Ongoing Review Rather Than Fixed Labels
Correct IBS classification does not lock a patient into a permanent category. Instead, it provides a clinical reference point that can be reassessed as symptoms change. Doctors use IBS types as flexible guides rather than rigid labels, revisiting classification during follow up when bowel patterns evolve. This adaptive approach reflects modern gastroenterology practice and acknowledges the dynamic nature of gut brain interaction in IBS [1][6][9].
IBS types help explain symptom patterns, but they are only one part of the condition. To understand IBS fully from symptoms to diagnosis and long term healing strategy, explore the complete IBS Ayurvedic overview and care guide.
Frequently Asked Questions About IBS Types
How are IBS types defined
IBS types are defined by the bowel habit that occurs most often over time. Doctors evaluate whether constipation, diarrhea, or alternating patterns dominate and classify IBS accordingly. This approach reflects functional behavior of the gut rather than disease severity.
What symptoms are used to classify IBS
IBS classification is based on stool consistency, bowel movement frequency, and the relationship between abdominal discomfort and defecation. These features are assessed across several weeks to identify the predominant pattern.
Can a person have more than one IBS type
A
Person may experience features of different IBS types at different times. Classification is based on the pattern that is most consistent during a given period rather than on isolated episodes.
Is unclassified IBS a valid diagnosis
Unclassified IBS is a recognized category used when symptoms meet criteria for IBS but bowel habits do not clearly match other types. It is often used when symptoms are inconsistent or evolving.
Does IBS type affect medical evaluation
IBS type helps guide clinical assessment by indicating how the bowel is functioning. However, all IBS types require evaluation to rule out conditions that may cause similar symptoms.
Are IBS types permanent
IBS types are not fixed. Doctors reassess bowel patterns during follow up visits and may update classification if symptoms change over time.
Is IBS diagnosed differently in each type
The diagnostic process is the same for all IBS types. Classification occurs after IBS is diagnosed based on symptom criteria and exclusion of other conditions.
Do IBS types indicate disease progression
IBS types do not represent stages of disease progression. They describe symptom patterns rather than worsening or improvement of the condition.
Why does my bowel pattern change so often with IBS
People with IBS often notice that their symptoms do not stay the same, shifting between constipation, diarrhea, or mixed patterns. Many wonder what causes these changes and whether they signal a change in the underlying condition.
Can stress really make IBS worse or change my subtype
Stress is one of the most commonly discussed triggers in IBS communities. Users often want to know whether emotional or work related stress can shift bowel habits and lead to alternating symptoms.
What foods are most likely to trigger symptoms in different IBS types
Instead of generic diet advice, readers today want subtype specific guidance: which foods tend to worsen constipation predominant symptoms versus diarrhea predominant symptoms?
How do I tell if my symptoms are IBS C, IBS D, or something else
This question moves beyond definitions and taps into real uncertainty users have when symptoms overlap, especially when they have both constipation and diarrhea at different times.
Is it normal for IBS symptoms to feel unpredictable even when tests are normal
Many users report confusion when their medical tests come back normal but symptoms persist or vary day to day. This addresses a core Discover intent: “Why is this happening to me?”
Can changing my routine or travel trigger a flare in IBS symptoms
Travel and routine disruption are among the top search triggers for IBS sufferers. Users want specifics on why disruptions affect bowel habits and how to manage that.
What’s the difference between IBS and food intolerances like lactose sensitivity
There is heavy search overlap between IBS and food intolerance symptoms. Patients want clarity on how IBS types differ from intolerance or allergy related patterns.
Why does IBS seem worse after sleeping poorly or having anxiety
Sleep and mental health are highly searched triggers for IBS symptom severity. Users seek direct links between sleep quality, anxiety, and bowel habits.
References
[1] Drossman, D. A., & Hasler, W. L. (2016). Rome IV functional gastrointestinal disorders: Disorders of gut–brain interaction. Gastroenterology, 150(6), 1257–1261.
https://doi.org/10.1053/j.gastro.2016.03.035
https://www.romecriteria.org
[2] Oka, P., Parr, H., Barberio, B., Black, C. J., Savarino, E. V., & Ford, A. C. (2020). Global prevalence of irritable bowel syndrome according to Rome III and Rome IV criteria: A systematic review and meta-analysis. The Lancet Gastroenterology & Hepatology, 5(10), 908–917.
https://doi.org/10.1016/S2468-1253(20)30217-X
[3] Chey, W. D., Lembo, A. J., & Lavins, B. J. (2015). Linaclotide for irritable bowel syndrome with constipation: A randomized, controlled trial. The American Journal of Gastroenterology, 110(2), 251–259.
https://doi.org/10.1038/ajg.2014.361
[4] Camilleri, M. (2012). Management of the irritable bowel syndrome. Gastroenterology, 143(5), 1146–1148.
https://doi.org/10.1053/j.gastro.2012.09.004
[5] Mayer, E. A., Tillisch, K., & Gupta, A. (2015). Gut–brain axis and the microbiota. Journal of Clinical Investigation, 125(3), 926–938.
https://doi.org/10.1172/JCI76304
[6] Ford, A. C., Lacy, B. E., & Talley, N. J. (2017). Irritable bowel syndrome. New England Journal of Medicine, 376(26), 2566–2578.
https://doi.org/10.1056/NEJMra1607547
[7] Whitehead, W. E., Palsson, O., & Jones, K. R. (2002). Systematic review of the comorbidity of irritable bowel syndrome with other disorders. The American Journal of Gastroenterology, 97(11), 2767–2776.
https://doi.org/10.1111/j.1572-0241.2002.07028.x
[8] Lacy, B. E., Mearin, F., Chang, L., Chey, W. D., Lembo, A. J., Simrén, M., & Spiller, R. (2016). Bowel disorders. Gastroenterology, 150(6), 1393–1407.
https://doi.org/10.1053/j.gastro.2016.02.031
[9] Holtmann, G. J., Ford, A. C., & Talley, N. J. (2016). Pathophysiology of irritable bowel syndrome. The Lancet Gastroenterology & Hepatology, 1(2), 133–146.
https://doi.org/10.1016/S2468-1253(16)30023-1
[10] Gralnek, I. M., Hays, R. D., Kilbourne, A., Naliboff, B., & Mayer, E. A. (2000). The impact of irritable bowel syndrome on health-related quality of life. Digestive Diseases and Sciences, 45(4), 699–709.
https://doi.org/10.1023/A:1005544205474
[11] Lacy, B. E., Pimentel, M., Brenner, D. M., Chey, W. D., Keefer, L. A., Long, M. D., & Rao, S. S. C. (2021). ACG clinical guideline: Management of irritable bowel syndrome. The American Journal of Gastroenterology, 116(1), 17–44.
https://journals.lww.com/ajg/fulltext/2021/01000/acg_clinical_guideline__management_of.11.aspx
[12] Simrén, M., Barbara, G., Flint, H. J., Spiegel, B. M., Spiller, R. C., Vanner, S., Verdu, E. F., Whorwell, P. J., & Zoetendal, E. G. (2013). Intestinal microbiota in functional bowel disorders: A Rome Foundation report. Gut, 62(1), 159–176.
https://doi.org/10.1136/gutjnl-2012-302167