- Quick Answer-How IBS Differs in Men and Women
- IBS Symptoms Common in Both Sexes
- IBS Symptoms More Common in Men
- Hormones and IBS-What Estrogen and Progesterone Do to the Gut
- The Gut Brain Axis- Stress Response Differences by Sex
- Ayurveda View- Grahani, Agni, Apana Vayu, and Sex Specific Patterns
- Why Symptoms Vary Even Within the Same Sex
- Red Flags-When It Is Not IBS
- What to Track for Faster Diagnosis
- FAQs
- Reference
IBS symptoms in men and women differ because hormones, gut movement, pain sensitivity, and stress response do not work the same way in every body [3]. When we look at women with IBS, we often see constipation, bloating, and stronger abdominal pain, while men more commonly experience diarrhea, urgency, and bowel changes linked to stress [4]. If you are a woman, hormonal fluctuations such as changes in estrogen and progesterone can slow digestion and increase gut sensitivity, which explains why IBS symptoms often worsen around the menstrual cycle or other hormonal transitions [9]. These biological differences combine with emotional stress, lifestyle habits, and nervous system responses, so they experience IBS symptoms differently even though the diagnosis is the same [3][4].
IBS symptoms in men and women can look very different, but they all fall under the same functional digestive disorder that affects how the gut works rather than causing physical damage. To understand symptoms, diagnosis, and long term outcomes clearly, it is important to view IBS through a comprehensive framework that integrates modern gastroenterology with classical digestive science, as explained in IBS Ayurvedic treatment diagnosis symptoms cure.
Quick Answer-How IBS Differs in Men and Women
Quick answer
Women with IBS more often report constipation, bloating, and symptom flares around menstruation due to hormone linked changes in motility and pain sensitivity. Men more often report diarrhea, urgency, and stress linked bowel changes, and may underreport pain or delay care. IBS varies because hormones, gut brain signaling, microbiome patterns, diet, sleep, and stress interact differently in each person.
Biological Differences That Shape IBS Symptoms
IBS symptoms in men and women differ primarily because hormones, nervous system signaling, and digestive motility do not function identically in every body [3]. From a clinical perspective, doctors consistently observe that women tend to experience slower bowel movement, increased bloating, and stronger abdominal pain, while men more often show faster bowel transit with diarrhea or urgency [4]. These differences are not random but are rooted in measurable biological mechanisms.
The Role of Hormones in Symptom Patterns
Hormonal regulation plays a central role in explaining why IBS symptoms in men and women feel so different [9]. In women, estrogen and progesterone influence how quickly the intestines move and how sensitively the gut responds to stretching and gas. If you are a woman, this is why IBS symptoms often worsen around menstruation or during other hormonal shifts, even when diet and lifestyle remain unchanged [9]. In men, relative hormonal stability means bowel symptoms are less cyclic and more closely linked to stress and external triggers [3].
Differences in Pain Perception and Stress Response
Another key difference lies in how pain and stress are processed [3]. Women with IBS often report higher pain sensitivity and greater abdominal discomfort, even when bowel changes are mild [4]. Men, on the other hand, may experience significant bowel urgency or loose stools with less reported pain. If you are a patient, this can sometimes make it confusing, because the severity of symptoms does not always match how much pain is felt.
Why the Same Diagnosis Feels Different
Although IBS is diagnosed using the same clinical criteria, they experience it differently because hormones, gut movement, emotional stress, and nervous system responses interact uniquely in each person [3][4]. This explains why one patient struggles mainly with constipation and bloating, while another struggles with diarrhea and urgency, even though both are told they have IBS. Recognizing these differences helps patients understand their symptoms and helps clinicians choose more personalized treatment approaches.
IBS Symptoms Common in Both Sexes
Core Digestive Symptoms Seen in Most Patients
When we examine IBS symptoms in men and women, several core digestive complaints appear consistently in both sexes, regardless of age or hormonal background [1][2]. Most patients experience recurring abdominal discomfort or pain that is closely linked to bowel movements. If you live with IBS, you may notice that pain improves after passing stool or sometimes intensifies when bowel movements are delayed. Clinicians consider this pain bowel relationship a defining feature of IBS in both men and women, and it plays a central role in diagnosis [1].
Changes in Bowel Habits That Affect Everyone
Altered bowel habits are a hallmark of IBS symptoms in both sexes [1][3]. Some people experience constipation, others diarrhea, and many fluctuate between the two patterns over time. What matters clinically is not only how often stools occur but also the loss of predictability in bowel function. If you are a patient, this unpredictability often leads to anxiety around meals, work schedules, and travel, even when symptoms are moderate [3].
Bloating Gas and Abdominal Fullness
Bloating and abdominal fullness are among the most frequently reported IBS symptoms in men and women [3]. Many patients describe a sensation of abdominal tightness or visible distension that worsens after eating or as the day progresses. From a medical perspective, this bloating is not always caused by excess gas alone. Instead, it reflects altered gut sensitivity and abnormal coordination of intestinal muscles. If you feel uncomfortable even after small meals, this experience is common across both sexes with IBS [3].
Sensation of Incomplete Bowel Evacuation
Another symptom shared by both men and women is the persistent feeling that bowel movements are incomplete [1][2]. Patients often report ongoing pressure or the urge to pass stool even after using the restroom. Doctors recognize this as a functional symptom rather than evidence of physical obstruction. If you experience this regularly, it helps explain why IBS can feel physically draining and emotionally frustrating, even when medical tests appear normal [1].
Chronic Course and Fluctuating Symptoms
IBS symptoms in men and women typically follow a chronic but fluctuating course rather than a stable pattern [1][3]. Symptoms may improve for weeks or months and then return without an obvious trigger. If you are managing IBS, this variability can make it difficult to judge whether a treatment is truly effective. Clinicians understand this waxing and waning nature as a core characteristic of IBS, which is why long term symptom awareness and realistic expectations are essential parts of care [1][3].
IBS Constipation Bloating and Pelvic Pressure
How Constipation Presents in Women With IBS
In women, IBS constipation often develops gradually and becomes a persistent pattern rather than an occasional symptom [4][7]. Doctors commonly observe infrequent bowel movements, hard stools, and prolonged straining. If you are experiencing this pattern, you may feel that bowel movements never feel fully complete, even after repeated attempts. Clinically, this happens because intestinal movement slows down and the colon becomes more sensitive to stool retention, a feature seen more often in women than in men [7][9].
Bloating That Progresses Through the Day
Bloating in IBS is not just a sensation of gas but a complex functional response of the gut [7][9]. Many women report that their abdomen feels relatively normal in the morning but becomes increasingly distended by afternoon or evening. If you notice that clothes feel tighter as the day progresses, this experience is common in IBS. Research shows that this bloating is linked to abnormal gut muscle coordination and heightened visceral sensitivity rather than excess gas alone [7].
Pelvic Pressure and Lower Abdominal Heaviness
Pelvic pressure is a frequently overlooked IBS symptom in women [4][7]. Instead of sharp pain, many women describe a sense of heaviness, fullness, or downward pressure in the lower abdomen and pelvic region. If you feel discomfort that resembles gynecological pressure rather than intestinal pain, this can still be part of IBS. Clinicians recognize that constipation and delayed stool passage can increase pressure within the pelvic floor and lower bowel, creating these sensations [7][9].
Why These Symptoms Often Occur Together
Constipation, bloating, and pelvic pressure often appear together because they share the same underlying mechanisms [4][9]. Slowed bowel movement leads to stool accumulation, which increases intestinal stretching and sensitivity. In women, hormonal influences further amplify this response, making the gut more reactive to normal digestive processes. If you experience all three symptoms simultaneously, it does not mean your condition is worsening structurally, but rather that functional regulation of the gut is disturbed [4][9].
Impact on Daily Life and Quality of Living
These combined symptoms can significantly affect daily functioning and emotional well being [3][4]. Women often report fatigue, frustration, and reduced confidence in social or work settings due to unpredictable bowel habits and visible bloating. If you find yourself planning your day around bowel movements or avoiding certain situations, this impact is a recognized part of IBS and deserves clinical attention, not dismissal [3][4].
Menstrual Cycle Triggers and Why Symptoms Flare
Hormonal Fluctuations and Digestive Timing
Many women notice that IBS symptoms change across the menstrual cycle, and this pattern is well explained by hormonal physiology [9][10]. Estrogen and progesterone levels rise and fall throughout the month, and these hormones directly influence how quickly the intestines move and how strongly the gut senses pressure and stretching. When progesterone levels increase, digestion tends to slow. If you are prone to IBS constipation, this slowing can lead to harder stools, bloating, and discomfort during certain phases of the cycle [9].
Increased Gut Sensitivity Before Menstruation
In the days leading up to menstruation, many women experience heightened abdominal sensitivity [9][10]. Even normal amounts of gas or stool can trigger pain or a feeling of pressure. If you find that your IBS symptoms feel more intense without a major change in diet, this increased sensitivity helps explain why symptoms flare. Clinicians recognize that hormonal shifts lower the pain threshold in the gut, making everyday digestive activity feel more uncomfortable [9].
Changes in Bowel Pattern During Menstruation
During menstruation itself, bowel habits may change abruptly [10][4]. Some women who usually experience constipation notice looser stools, while others experience worsening constipation and cramping. If this happens to you, it reflects the interaction between hormonal signaling and prostaglandins, which influence both uterine contractions and intestinal movement. Doctors understand that these bowel changes are functional and cycle related rather than signs of disease progression [10].
Emotional Stress and Symptom Amplification
The menstrual cycle can also affect mood, stress tolerance, and emotional regulation, which in turn influences IBS symptoms [3][4]. If you notice that anxiety or emotional sensitivity increases around your cycle, this stress response can further amplify gut discomfort. From a clinical perspective, this mind body interaction explains why IBS flares often feel more overwhelming during certain times of the month, even when bowel changes are mild [3].
Why Tracking the Cycle Helps Symptom Control
Understanding the link between the menstrual cycle and IBS symptoms empowers patients and clinicians alike [9][4]. If you track your symptoms alongside your cycle, patterns often become clear within a few months. This awareness helps explain why symptoms flare predictably and reassures you that these changes are driven by hormonal regulation rather than new pathology. Clinicians use this information to guide dietary adjustments, stress management, and treatment timing more effectively [9][4].
Pregnancy and Postpartum IBS Changes
Digestive Changes During Pregnancy
During pregnancy, many women notice changes in IBS symptoms due to hormonal shifts and physical adaptations in the body [9][3]. Rising progesterone levels slow intestinal movement, which can worsen constipation, bloating, and abdominal fullness. If you are pregnant and already prone to IBS constipation, you may find that bowel movements become less frequent and discomfort increases even without dietary changes. Clinicians understand that these changes are functional and related to normal pregnancy physiology rather than disease progression [3].
Increased Abdominal Sensitivity and Discomfort
Pregnancy can also alter how the gut senses pressure and stretching [9]. As the uterus expands, space within the abdominal cavity changes, and the intestines become more sensitive to normal digestive activity. If you experience abdominal discomfort that feels different from typical IBS pain, this heightened sensitivity helps explain why symptoms may feel unfamiliar during pregnancy. Doctors carefully differentiate these sensations from warning signs to ensure both maternal and fetal safety [3].
Variability of IBS Symptoms Across Trimesters
IBS symptoms do not behave the same way throughout pregnancy [9][4]. Some women notice symptom improvement in early pregnancy, while others experience worsening constipation or bloating later as hormonal levels peak and physical pressure increases. If your symptoms fluctuate from trimester to trimester, this variability is expected and reflects the changing balance between hormones, gut movement, and nervous system signaling [4].
Postpartum Hormonal Shifts and Bowel Regulation
After childbirth, IBS symptoms may change again as hormone levels rapidly adjust [9][3]. The sudden drop in progesterone and estrogen can alter bowel patterns, sometimes leading to loose stools, urgency, or renewed abdominal discomfort. If you notice that IBS symptoms return or change form after delivery, clinicians recognize this as part of postpartum physiological adjustment rather than a new digestive disorder [3].
Emotional Stress Sleep Disruption and IBS After Delivery
The postpartum period often involves sleep deprivation, emotional stress, and changes in daily routine, all of which can influence IBS symptoms [3][4]. If you are caring for a newborn, stress related gut responses may intensify bowel irregularity or pain sensitivity. From a clinical standpoint, this explains why IBS management after pregnancy often focuses on stress regulation, gentle dietary support, and realistic expectations rather than aggressive intervention [3][4].
Perimenopause and Menopause Changes
Hormonal Transitions and Digestive Regulation
During perimenopause and menopause, many women notice clear changes in IBS symptoms as estrogen and progesterone levels become irregular and then decline [9][4]. These hormones play a key role in regulating bowel movement and gut sensitivity. When their levels fluctuate, intestinal movement can become less predictable. If you are entering this stage of life, you may notice new constipation, increased bloating, or changes in stool consistency even if your IBS was previously stable [9].
Shifts in Pain Sensitivity and Abdominal Discomfort
Hormonal decline during menopause can also affect how the nervous system processes pain [3][4]. Some women report that abdominal discomfort feels different than before, sometimes less cramp like and more diffuse or persistent. If you feel that your pain threshold has changed, this is not unusual. Clinicians understand that reduced estrogen can alter gut brain signaling, making the digestive system either more sensitive or, in some cases, less responsive to pain cues [3][4].
Changes in Bowel Pattern and Bloating
Perimenopause is often marked by irregular bowel habits [9][4]. You may experience alternating constipation and looser stools without a clear dietary trigger. Bloating can also become more prominent, particularly later in the day. From a clinical perspective, these changes reflect altered gut motility and fluid balance rather than structural disease. If you are concerned that IBS is worsening, doctors typically first consider hormonal influence before pursuing extensive testing [9].
Role of Stress Sleep and Metabolic Changes
This life stage often brings changes in sleep quality, stress levels, and metabolism, all of which influence IBS symptoms [3]. If you are dealing with hot flashes, poor sleep, or increased stress, these factors can indirectly worsen bowel irregularity and abdominal discomfort. Clinicians recognize that IBS symptoms during perimenopause and menopause often reflect the combined effect of hormonal change and nervous system strain rather than a single digestive cause [3].
Why Symptoms May Improve for Some Women
Interestingly, not all women experience worsening IBS during menopause [4]. Some report symptom improvement once hormonal fluctuations settle and cycles stop completely. If this happens to you, it suggests that hormonal variability rather than hormone absence was driving earlier flares. Doctors consider this pattern normal and reassuring, reinforcing that IBS symptoms can evolve across life stages rather than follow a fixed course [4].
IBS Symptoms More Common in Men
Diarrhea Dominant Bowel Pattern
When clinicians examine IBS symptoms in men and women, men are more likely to present with diarrhea dominant bowel patterns [4][8]. Men with IBS often report frequent loose stools, sudden urgency, and the need to use the restroom shortly after meals. If you are a man experiencing these symptoms, you may notice that bowel movements feel rapid and difficult to control rather than painful. From a medical perspective, this pattern reflects faster intestinal transit and a different stress related gut response compared to constipation dominant IBS [4].
Urgency and Post Meal Bowel Changes
Bowel urgency is a prominent feature of IBS in men [8][11]. Many men describe a strong and immediate need to pass stool, particularly after eating or during stressful situations. If you find that meals trigger an urgent bowel response, this is a well recognized IBS pattern rather than a sign of infection or structural disease. Doctors understand that this response is driven by heightened gut reflexes and altered communication between the digestive system and the nervous system [11].
Less Prominent Pain but Greater Functional Disruption
Men with IBS often report less abdominal pain compared to women, even when bowel disturbance is significant [7][8]. Instead of pain, symptoms such as urgency, loose stools, and unpredictability dominate daily life. If you feel that your IBS affects your schedule and confidence more than it causes pain, this presentation is common in men. Clinicians recognize that differences in pain perception and reporting play a role in how IBS manifests across sexes [7].
Strong Link Between Stress and Bowel Symptoms
Stress related bowel changes are particularly common in men with IBS [11][12]. Mental pressure, work demands, or emotional strain can quickly translate into diarrhea or urgency. If you notice that stressful days worsen your symptoms even when diet remains unchanged, this connection reflects the influence of the gut brain axis. Doctors view this stress bowel response as a core mechanism in IBS rather than a psychological weakness [11][12].
Delayed Reporting and Underdiagnosis in Men
Men are more likely to delay seeking medical care for IBS symptoms [7][4]. Many tolerate symptoms for years, assuming they are due to diet or stress alone. If you have ignored symptoms because they seem manageable or embarrassing, this delay can contribute to underdiagnosis and prolonged discomfort. Clinicians emphasize that recognizing and addressing IBS early can improve quality of life and prevent unnecessary anxiety about bowel health [7][4].
IBS Diarrhea Urgency and Post Meal Loose Stools
How Diarrhea Presents in Men With IBS
In men, IBS diarrhea often presents as frequent loose stools rather than continuous abdominal pain [4][8]. Bowel movements may occur several times a day, especially after meals or during stressful periods. If you are experiencing this pattern, stools may be loose or watery without signs of infection. Clinicians recognize this as a functional disturbance of bowel movement speed rather than inflammation or structural disease [4].
Urgency and Loss of Bowel Control Sensation
Urgency is one of the most disruptive IBS symptoms reported by men [8][11]. Many men describe a sudden and intense need to use the restroom, sometimes with little warning. If you feel anxious about being far from a restroom, this reaction is common in IBS diarrhea dominant patterns. Doctors understand that this urgency is driven by heightened reflex activity in the colon and altered nerve signaling between the gut and the brain [11].
Post Meal Loose Stools and Gastrocolic Reflex
Loose stools occurring shortly after eating are frequently reported by men with IBS [11][3]. This response is linked to an exaggerated gastrocolic reflex, which normally signals the colon to move after food intake. If you notice that meals trigger rapid bowel movements regardless of food type, this exaggerated reflex helps explain why symptoms appear so quickly. Clinicians consider this response functional and stress sensitive rather than a sign of food intolerance alone [3].
Limited Pain but High Daily Disruption
Unlike constipation dominant patterns, IBS diarrhea in men may involve minimal abdominal pain [7][8]. Instead, the primary burden comes from unpredictability and urgency. If you feel that IBS interferes with work, travel, or social plans more than it causes pain, this experience aligns with common male IBS patterns. Doctors recognize that pain perception differences influence how symptoms are reported rather than how severe the bowel dysfunction truly is [7].
Emotional Stress and Symptom Escalation
Stress plays a strong role in triggering diarrhea and urgency in men with IBS [11][12]. Mental pressure, deadlines, or emotional strain can rapidly activate bowel reflexes. If your symptoms worsen during stressful situations even without dietary changes, this reflects gut brain communication rather than weakness or lack of control. Clinicians view stress management as a legitimate and necessary part of IBS care for men [11][12].
Why Men Report Less Pain and Seek Care Later
Differences in Pain Perception and Reporting
Men with IBS often report less abdominal pain even when bowel disturbance is significant [7][8]. This does not mean the digestive dysfunction is milder. Research shows that differences in pain perception and pain reporting play a role. If you are a man with IBS, you may notice urgency or loose stools without strong pain signals, which can make symptoms feel less alarming at first. Clinicians understand that biological and neurological factors influence how pain signals from the gut are processed and communicated [7].
Focus on Bowel Function Rather Than Discomfort
Many men tend to focus more on bowel function than on discomfort [4][8]. Instead of describing pain, they often emphasize urgency, frequency, or disruption to daily routine. If you feel that your main concern is managing restroom access rather than pain relief, this pattern is common. Doctors recognize that this difference in symptom emphasis can delay IBS recognition because pain is often assumed to be the primary indicator of digestive disease [4].
Social and Cultural Factors Influencing Care Seeking
Social and cultural expectations also influence how men respond to chronic digestive symptoms [7][4]. Men are more likely to normalize symptoms, attribute them to stress or diet, or avoid discussing bowel issues altogether. If you have a tendency to tolerate symptoms silently or avoid medical consultation, this behavior contributes to later diagnosis. Clinicians acknowledge that these patterns are common and do not reflect lack of severity or importance of the condition [7].
Delayed Evaluation and Underdiagnosis
Because pain is less prominent and symptoms are often minimized, men frequently seek care later in the course of IBS [4][8]. By the time they consult a doctor, symptoms may have already affected work, travel, or mental well being. If you recognize that you have adjusted your lifestyle around bowel habits without seeking help, this delay is a known contributor to underdiagnosis in men. Doctors emphasize that earlier evaluation can reduce uncertainty and improve symptom management [4].
Impact on Long Term Quality of Life
Seeking care later can prolong discomfort and increase stress related symptom amplification [3][11]. When IBS remains unaddressed, ongoing bowel unpredictability may heighten anxiety and further disrupt gut function. If you seek care earlier, clinicians can provide reassurance, rule out serious conditions, and guide appropriate management strategies. Understanding why men often delay care helps normalize this experience and encourages timely medical attention [3][11].
Hormones and IBS-What Estrogen and Progesterone Do to the Gut
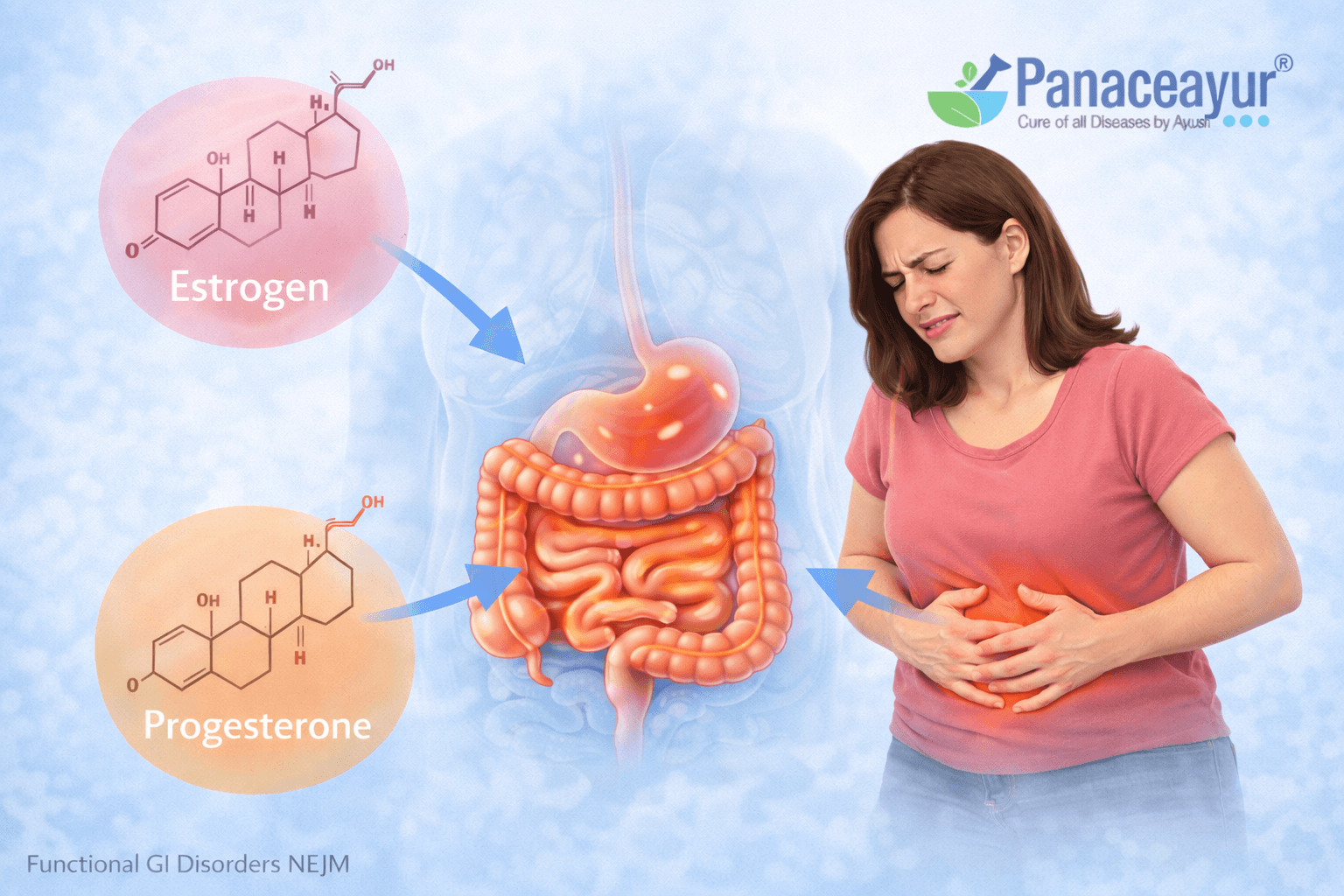
How Estrogen Influences Gut Movement and Sensitivity
Estrogen plays a significant role in regulating how the digestive system functions, particularly in women with IBS [9][4]. This hormone affects intestinal muscle contraction and how the gut senses stretching and pressure. When estrogen levels are higher, gut sensitivity often increases, meaning normal digestive activity can feel uncomfortable or painful. If you notice that your IBS symptoms intensify during certain phases of your cycle, estrogen related changes in gut sensitivity are a key reason behind this pattern [9].
The Slowing Effect of Progesterone on Digestion
Progesterone has a well recognized slowing effect on bowel movement [9][10]. It relaxes smooth muscle in the digestive tract, which can delay stool passage and contribute to constipation. If you are prone to IBS constipation, you may notice that symptoms worsen when progesterone levels rise. Clinicians understand that this hormone driven slowing of digestion increases stool retention, gas buildup, and abdominal fullness without indicating structural disease [10].
Hormonal Impact on the Gut Brain Communication
Both estrogen and progesterone influence communication between the gut and the brain [3][9]. These hormones interact with neurotransmitters such as serotonin, which plays a major role in regulating bowel movement and pain perception. If you experience IBS symptoms that fluctuate with mood or stress, hormonal modulation of gut brain signaling helps explain why emotional states can directly affect digestive comfort [3].
Why Hormonal Changes Create Symptom Fluctuations
IBS symptoms often fluctuate rather than remain constant, and hormonal variation is a major contributor to this instability [9][4]. If hormone levels rise and fall rapidly, the gut may struggle to maintain consistent movement and sensitivity thresholds. This explains why symptoms can improve for weeks and then suddenly flare without a clear dietary trigger. Clinicians view this variability as a functional response to hormonal regulation rather than a sign of disease progression [4].
How Hormonal Effects Differ Between Men and Women
While men also produce estrogen and progesterone in smaller amounts, the magnitude of hormonal fluctuation is far greater in women [9][3]. This difference explains why IBS symptoms in men tend to be less cyclic and more closely linked to stress or lifestyle factors. If you are comparing symptom patterns between men and women, hormonal influence provides a clear biological explanation for why women often experience more pronounced variability across time [3][9].
The Gut Brain Axis- Stress Response Differences by Sex
How the Gut Brain Axis Shapes IBS Symptoms
The gut brain axis refers to the continuous communication between the digestive system and the nervous system, and it plays a central role in IBS symptoms in men and women [11][12]. Signals travel in both directions, meaning stress can alter bowel function and gut activity can influence mood and emotional state. If you notice that stress affects your digestion almost immediately, this connection explains why IBS is not limited to the gut alone but involves the entire nervous system [11].
Stress Response Patterns in Women With IBS
Women with IBS often show a heightened gut response to emotional stress [3][4]. Stress can increase gut sensitivity, slow bowel movement, or intensify bloating and pain perception. If you are a woman, you may notice that emotional strain leads to stronger abdominal discomfort even when bowel movements do not change dramatically. Clinicians understand that hormonal modulation combined with nervous system sensitivity amplifies the stress response in the digestive tract [4][9].
Stress Driven Bowel Changes in Men
In men, stress tends to trigger bowel movement changes rather than pain [11][8]. Many men experience diarrhea, urgency, or frequent bowel movements during periods of mental pressure or workload stress. If you find that stressful situations send you to the restroom quickly, this reaction reflects a faster gut response rather than increased pain sensitivity. Doctors recognize this as a stress mediated bowel reflex driven by gut brain signaling [11].
Role of Anxiety and Emotional Processing
Anxiety and emotional processing influence IBS symptoms differently in men and women [13][3]. Women with IBS are more likely to experience symptom amplification linked to anxiety or emotional overload, while men may experience functional disruption without overt emotional distress. If you feel that emotions affect your gut even when you try to ignore them, this mind body interaction is a recognized feature of IBS and not a personal weakness [13].
Why Stress Management Matters for Both Sexes
Although stress manifests differently, it is a critical driver of IBS symptoms in both men and women [11][12]. If stress remains unaddressed, repeated gut brain activation can reinforce symptom cycles and make IBS more persistent. Clinicians emphasize that understanding your personal stress response helps explain symptom triggers and supports more effective long term management strategies. Recognizing these differences allows patients to approach IBS with clarity rather than confusion or self blame [11][12].
Ayurveda View- Grahani, Agni, Apana Vayu, and Sex Specific Patterns
Grahani as Described in Classical Ayurveda
Ayurveda describes conditions resembling IBS under the disease entity known as Grahani, which arises from impairment of Agni, the digestive fire [17][18]. Charaka Samhita clearly states:
“Agnimandye tu grahani dosha bhavanti sarvashah”
Charaka Samhita, Chikitsa Sthana, Grahani Chikitsa Adhyaya
This shloka explains that when Agni becomes weak or irregular, Grahani disorders develop in various forms. In practical terms, if digestion becomes inconsistent, food is not properly transformed, leading to irregular stool formation, gas, bloating, abdominal discomfort, and alternating bowel habits. If you experience these symptoms without any structural disease, Ayurveda recognizes this as a functional digestive disorder rooted in Agni dysfunction rather than organ damage [17].
Role of Agni in Stool Formation and Digestive Stability
Charaka further explains the central role of Agni in regulating bowel consistency and rhythm:
“Agni balam hi dehanam balam agni prabhavakam”
Charaka Samhita, Chikitsa Sthana
This shloka emphasizes that digestive strength determines overall bodily stability. When Agni is balanced, digestion is complete and stools are well formed. When Agni fluctuates, stools may become hard, loose, or irregular. If you notice unpredictable bowel habits despite eating similar foods, Ayurveda attributes this variability to unstable Agni, which closely mirrors modern observations of altered gut motility and sensitivity in IBS [17][3].
Apana Vayu and Control of Bowel Elimination
Ayurveda identifies Apana Vayu as the primary regulator of elimination and pelvic function [17][19]. Charaka describes Apana Vayu as follows:
“Apano adhogati karma mala mutra shukra nishkramah”
Charaka Samhita, Sutra Sthana
This shloka explains that Apana Vayu governs downward movement, including defecation and pelvic functions. When Apana Vayu becomes disturbed, symptoms such as constipation, urgency, incomplete evacuation, and pelvic pressure arise. If you experience difficulty passing stool or persistent heaviness in the lower abdomen, Ayurveda considers Apana Vayu imbalance a key contributor, aligning with modern concepts of altered colonic motility and pelvic floor coordination [17].
Female Pattern: Raja Kala, Apana Vayu, and Digestive Sensitivity
Ayurveda places special emphasis on digestive changes in women during hormonal phases [17][19]. Classical texts explain that Vata naturally increases during Raja Kala, the menstrual phase. Charaka states:
“Raja kale vata prakopo bhavati”
Charaka Samhita, Sharira Sthana
This means that during menstruation, Vata dosha naturally aggravates. If you are a woman, this Vata increase can disturb Apana Vayu, leading to constipation, bloating, pelvic discomfort, and heightened gut sensitivity. This Ayurvedic explanation closely parallels modern findings that estrogen and progesterone fluctuations alter gut motility and pain perception during the menstrual cycle [9].
Male Pattern: Pitta Vata Influence and Atisara Tendency
In men, Ayurveda more commonly associates IBS like symptoms with combined Pitta and Vata imbalance [18][19]. Bhavaprakasha describes digestive disturbances linked to heat and instability:
“Pittanubandhi vata atisaram janayati”
Bhavaprakasha, Grahani and Atisara Adhyaya
This shloka explains that when Pitta combines with Vata, loose stools and urgency may occur. If you are a man experiencing diarrhea, urgency, or bowel changes triggered by stress, irregular meals, or stimulants, Ayurveda interprets this as Pitta heat disturbing Vata movement. This aligns with modern observations that men more often present with diarrhea dominant IBS patterns linked to stress response [4][8].
Why Ayurveda Emphasizes Sex Specific Digestive Patterns
Ayurveda repeatedly states that disease expression varies according to individual constitution, sex, age, and strength [17][18]. Charaka summarizes this principle clearly:
“Purusham purusham vikshya”
Charaka Samhita, Sutra Sthana
This shloka means that treatment and interpretation must be individualized for each person. If two people have IBS but experience very different symptoms, Ayurveda considers this expected rather than contradictory. Sex specific physiology, hormonal rhythms, and dosha predominance shape how Grahani manifests. This individualized framework explains why uniform treatment often fails and why restoring Agni and balancing Apana Vayu according to sex specific patterns remains central to Ayurvedic digestive care [17][18].
Grahani as the IBS Framework in Charaka Samhita Text Book
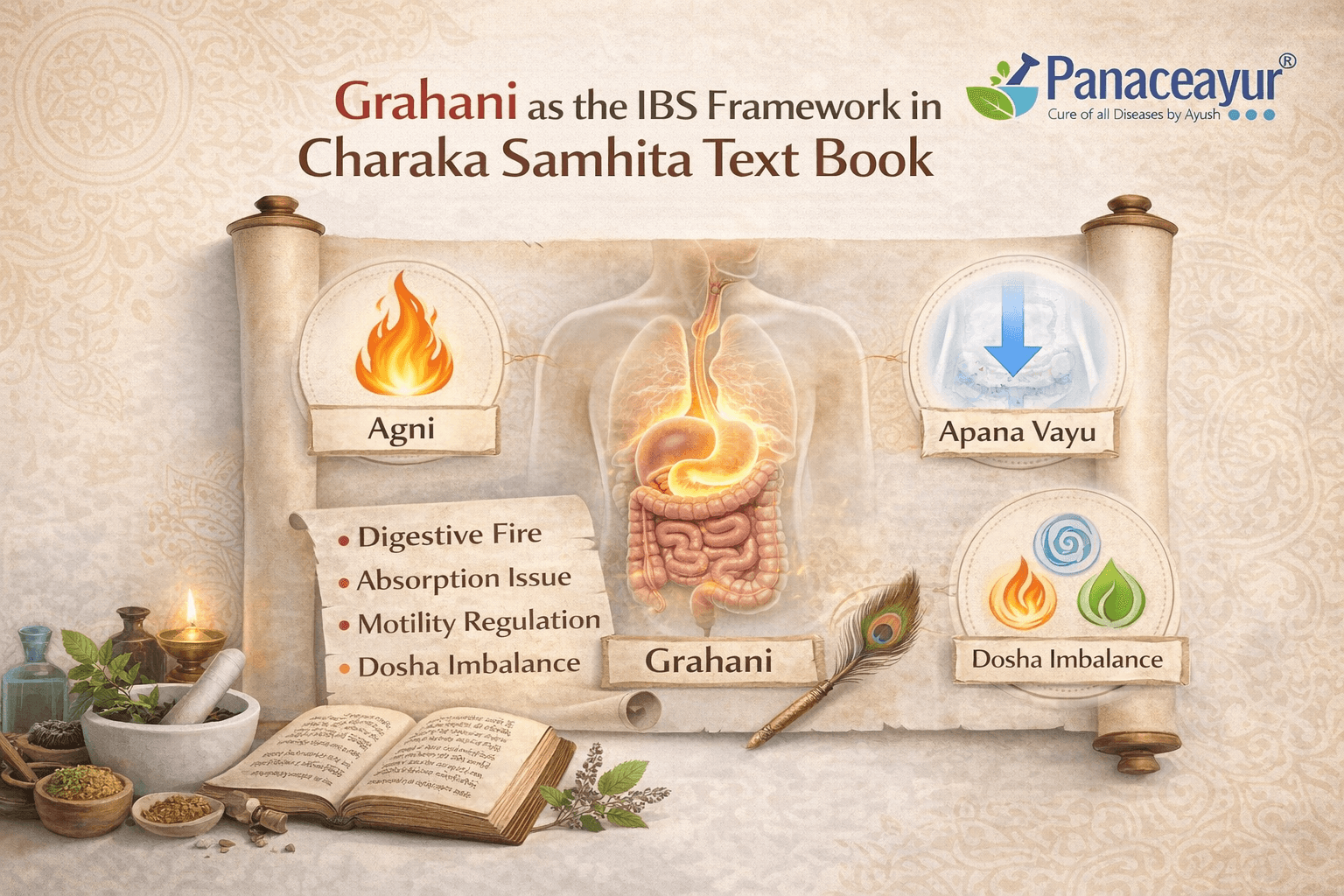
How Charaka Samhita Defines Grahani
In Charaka Samhita, conditions resembling IBS are explained under Grahani, which is described not as a structural disease but as a functional disorder arising from impairment of Agni [17]. Charaka clearly states:
“Grahani doshah agni dushti nimittajah”
Charaka Samhita, Chikitsa Sthana, Grahani Chikitsa Adhyaya
This shloka explains that Grahani disorders originate from dysfunction of digestive fire. In simple terms, when digestion becomes weak, irregular, or unstable, the intestines fail to process food properly. If you experience abdominal discomfort, bloating, gas, irregular stools, or alternating constipation and diarrhea without detectable disease, Ayurveda recognizes this pattern as Grahani rather than a disease of the intestine itself [17].
Agni Dysfunction as the Root Cause
Charaka repeatedly emphasizes that Agni governs digestion, absorption, and elimination [17][18]. One of the most important principles states:
“Agnimandyaat bhavanti vyadhayah sarvashah”
Charaka Samhita, Sutra Sthana
This shloka means that impaired Agni gives rise to multiple diseases. In the context of Grahani, weakened or irregular Agni leads to incomplete digestion, formation of improperly processed food residues, and erratic bowel habits. If you notice that the same food sometimes causes constipation and at other times loose stools, Ayurveda explains this variability as fluctuating Agni rather than random intolerance [17].
Stool Irregularity and Digestive Instability
Charaka describes that in Grahani, stools may be formed, loose, sticky, or delayed depending on the state of Agni and dosha involvement [17]. A classical description explains:
“Kadachit baddham kadachit dravam mala pravrittih”
Charaka Samhita, Chikitsa Sthana
This shloka directly mirrors the modern description of IBS where stool consistency alternates unpredictably. If you experience days of constipation followed by episodes of loose stools, this is a classical Grahani presentation described thousands of years ago. Ayurveda views this instability as functional dysregulation rather than inflammation or obstruction [17][3].
Abdominal Pain Bloating and Weakness in Grahani
Charaka also lists symptoms such as abdominal pain, distension, heaviness, fatigue, and loss of digestive confidence in Grahani [17][18]. These features arise because improperly digested food disrupts normal intestinal movement and sensitivity. If you feel bloated after small meals or experience weakness along with bowel irregularity, Ayurveda considers these hallmark features of Grahani rather than separate conditions [17].
Why Grahani Aligns Closely With Modern IBS
From a modern perspective, IBS is classified as a functional bowel disorder characterized by altered gut motility, visceral hypersensitivity, and brain gut interaction [3][11]. Ayurveda reaches the same conclusion through the lens of Agni and Grahani. Both systems recognize that symptoms arise without visible damage and fluctuate based on stress, diet, and internal regulation. If you are searching for a framework that explains why tests appear normal despite persistent symptoms, Grahani provides a coherent classical explanation that aligns closely with modern IBS understanding [17][3].
Women- Apana Vayu, Raja Kala, Constipation and Bloating
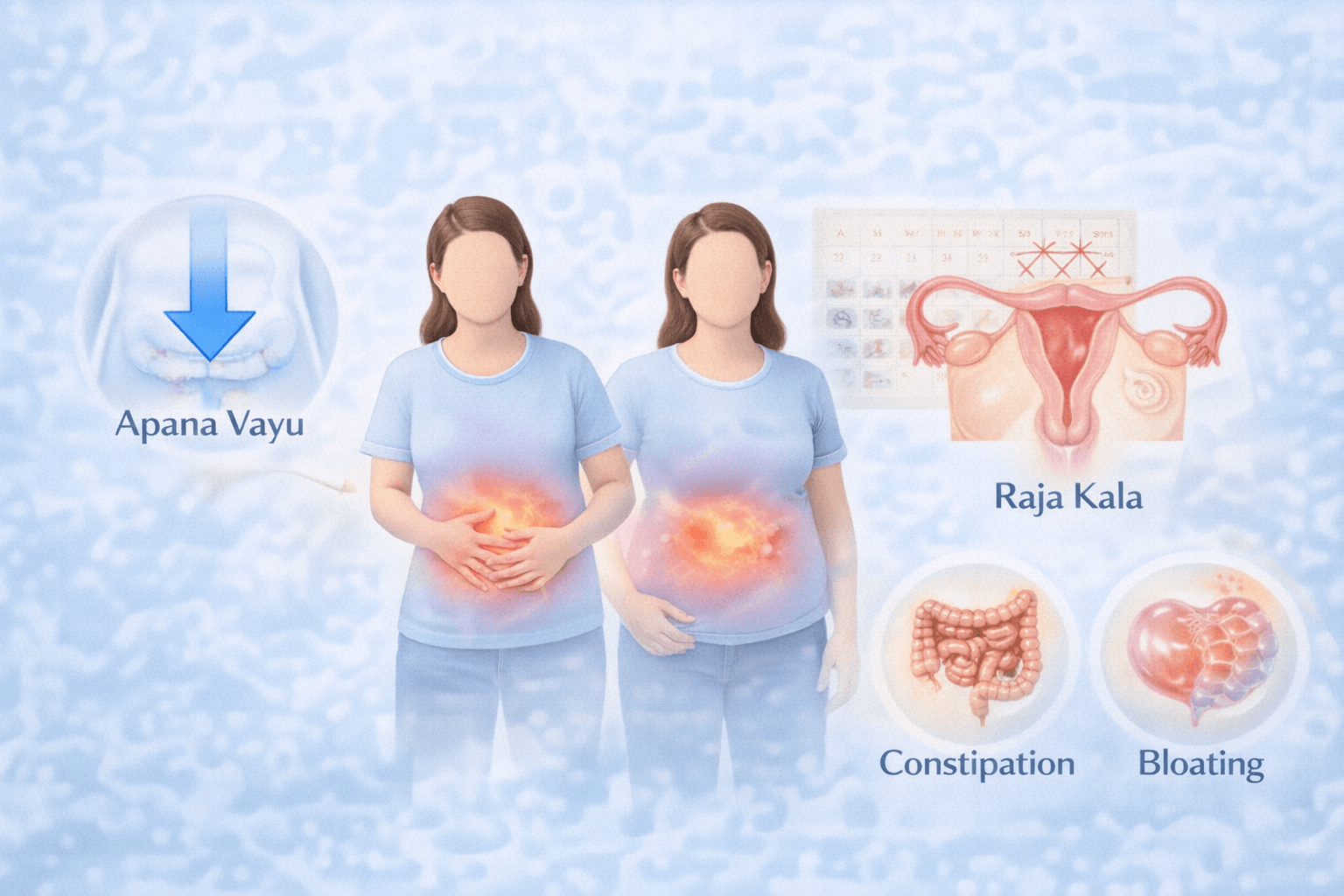
Apana Vayu as the Regulator of Female Bowel Function
In Ayurveda, Apana Vayu governs all downward movements in the body, including defecation, pelvic circulation, and reproductive functions [17]. Charaka Samhita defines the role of Apana Vayu as:
“Apano adhogati karma mala mutra artava nishkramah”
Charaka Samhita, Sutra Sthana
This shloka explains that Apana Vayu controls elimination of stool, urine, and menstrual flow. If you are a woman experiencing constipation, difficulty passing stool, or a persistent sense of heaviness in the lower abdomen, Ayurveda interprets this as disturbed Apana Vayu. When Apana Vayu loses its normal downward flow, bowel movements slow, stool becomes dry or hard, and bloating develops due to improper evacuation [17].
Raja Kala and Natural Vata Aggravation
Ayurvedic texts clearly describe that Vata dosha naturally increases during Raja Kala, the menstrual phase [17]. Charaka states:
“Raja kale vata vriddhir bhavati”
Charaka Samhita, Sharira Sthana
This means that during menstruation, Vata increases physiologically. If you are a woman with IBS like symptoms, this natural rise in Vata can disturb Apana Vayu further, leading to constipation, bloating, abdominal tightness, and pelvic discomfort around the menstrual period. Ayurveda considers this a predictable physiological vulnerability rather than a disease process [17][9].
Why Constipation Is More Common in Women
Constipation is more frequently observed in women because Apana Vayu and hormonal cycles are closely linked [4][17]. When Apana Vayu is disturbed, stool propulsion slows and evacuation becomes incomplete. If you notice that bowel movements feel more difficult or less satisfying around your cycle, Ayurveda explains this through Vata predominance in the pelvic region. Modern medicine similarly observes slower colonic transit in women, particularly during certain hormonal phases, supporting this classical explanation [9].
Bloating and Abdominal Distension Explained Through Ayurveda
Bloating in women is not described in Ayurveda as excess gas alone but as impaired movement of Vata within the intestines [17][19]. Bhavaprakasha explains that when Vata becomes obstructed in the digestive tract, abdominal distension and discomfort arise:
“Vata avarane udaram adhmanam cha jayate”
Bhavaprakasha, Grahani Adhyaya
If you experience visible abdominal distension that worsens through the day, Ayurveda views this as trapped or improperly directed Vata rather than overeating or intolerance. Constipation and bloating often occur together because stool retention increases pressure and further disrupts Apana Vayu movement [17].
Interaction of Hormones and Apana Vayu
Ayurveda acknowledges that reproductive physiology directly influences digestion in women [17]. During Raja Kala, hormonal fluctuations increase Vata sensitivity, which amplifies bloating and constipation. If you are tracking your symptoms and notice monthly patterns, this interaction between hormones and Apana Vayu provides a coherent explanation. Modern research confirms that estrogen and progesterone fluctuations alter gut motility and visceral sensitivity, reinforcing the classical Ayurvedic framework [9].
Why These Symptoms Feel More Intense in Women
Women often report that constipation and bloating feel more distressing and uncomfortable compared to men [4][7]. Ayurveda explains this through increased Vata sensitivity in the pelvic and abdominal regions, combined with heightened gut perception. If you feel that even mild digestive disruption causes significant discomfort, this heightened sensitivity is a recognized physiological pattern rather than exaggeration or anxiety [17][4].
This Ayurvedic interpretation helps you understand why constipation and bloating cluster together in women with IBS and why these symptoms often fluctuate with the menstrual cycle rather than appearing randomly.
Men-Pitta Vata Patterns, Atisara Tendency, and Lifestyle Triggers
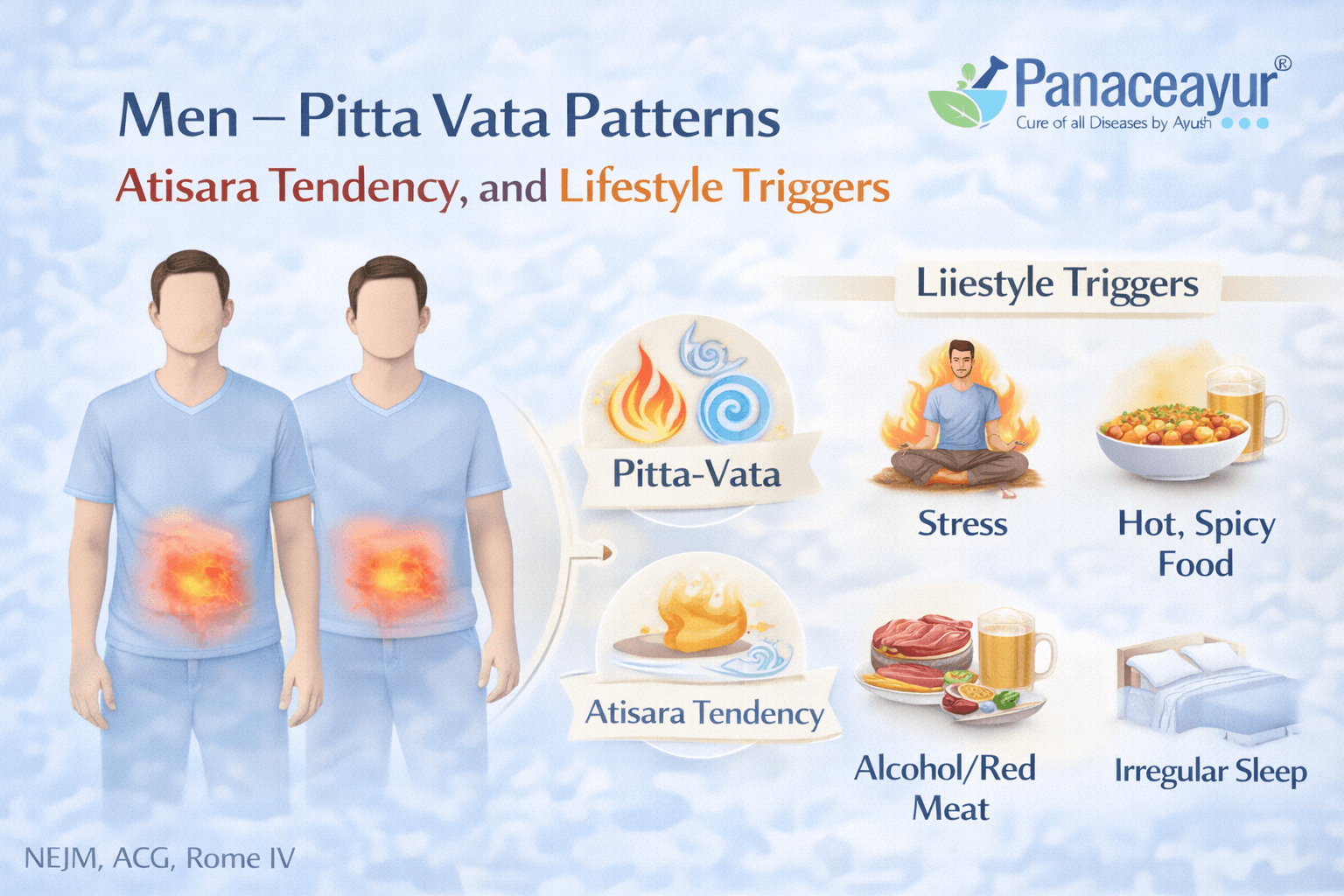
Pitta Vata Dominance in Male Digestive Patterns
In Ayurveda, men with IBS like symptoms are more commonly described as having a combined Pitta Vata imbalance rather than isolated Apana Vayu disturbance [18][19]. Pitta governs heat, metabolism, and digestive enzymes, while Vata governs movement and regulation. When these two doshas become disturbed together, digestion becomes fast, irregular, and unstable. If you are a man experiencing loose stools, urgency, or burning sensations, Ayurveda explains this as excessive digestive heat combined with uncontrolled bowel movement [19].
Bhavaprakasha describes this interaction clearly:
“Pittanubandhi vata atisaram janayati”
Bhavaprakasha, Atisara Adhyaya
This shloka explains that when Vata is aggravated in association with Pitta, diarrhea like conditions arise. In practical terms, stool passes too quickly through the intestines, leading to loose consistency, urgency, and incomplete absorption.
Atisara Tendency and IBS Diarrhea Patterns
Ayurveda uses the term Atisara to describe conditions involving frequent loose stools [19]. While IBS is not identical to infectious diarrhea, Charaka and Bhavaprakasha describe noninfectious Atisara patterns driven by dosha imbalance rather than pathogens. If you experience recurrent loose stools without fever, blood, or acute illness, Ayurveda considers this a functional Atisara tendency rooted in Pitta Vata disturbance rather than an acute disease [17][19].
Charaka states:
“Na cha sarvah atisaro agantukah”
Charaka Samhita, Chikitsa Sthana
This shloka clarifies that not all diarrhea arises from external causes. Many cases originate from internal imbalance, which aligns closely with the modern understanding of IBS diarrhea dominant patterns [4][8].
Role of Digestive Heat and Rapid Gut Movement
In men, stronger digestive fire combined with Pitta aggravation can accelerate intestinal movement [17][18]. If you notice that meals trigger immediate bowel urgency, Ayurveda explains this as excessive digestive heat pushing contents downward too rapidly. Vata then carries this heat through the intestines without proper regulation, resulting in loose stools and urgency. This mirrors modern observations of an exaggerated gastrocolic reflex in men with IBS diarrhea [11].
Lifestyle Triggers That Aggravate Pitta Vata
Ayurvedic texts repeatedly emphasize that lifestyle plays a decisive role in triggering Pitta Vata imbalance [17][19]. Irregular meals, excessive spicy or oily foods, alcohol, caffeine, sleep deprivation, and chronic mental stress all increase Pitta heat and destabilize Vata movement. If you are a man whose IBS symptoms worsen during periods of work pressure, irregular eating, or stimulant use, Ayurveda interprets this as lifestyle driven dosha aggravation rather than inherent weakness of the gut [19].
Charaka cautions:
“Vishamashana ratinam grahani doshah vardhate”
Charaka Samhita, Chikitsa Sthana
This shloka explains that irregular eating habits aggravate Grahani disorders. In modern terms, inconsistent meal timing and dietary excess directly destabilize bowel rhythm and sensitivity.
Why Men Experience Less Pain but More Urgency
Ayurveda explains that Pitta driven digestive disturbance tends to produce heat and movement rather than heaviness or blockage [18][19]. As a result, men often experience urgency and loose stools with relatively less abdominal pain compared to constipation dominant patterns. If you feel that your symptoms disrupt daily routine more than they cause pain, this presentation aligns with classical descriptions of Pitta Vata dominant Grahani and Atisara tendencies [19].
Classical and Modern Alignment
The Ayurvedic description of Pitta Vata driven Atisara closely parallels modern IBS diarrhea dominant presentations seen more commonly in men [4][8]. Both systems recognize that symptoms are functional, stress sensitive, and strongly influenced by lifestyle rather than structural disease. This convergence strengthens the validity of using Grahani and Atisara frameworks to understand male IBS patterns in a clinically meaningful way [17][4].
Why Symptoms Vary Even Within the Same Sex
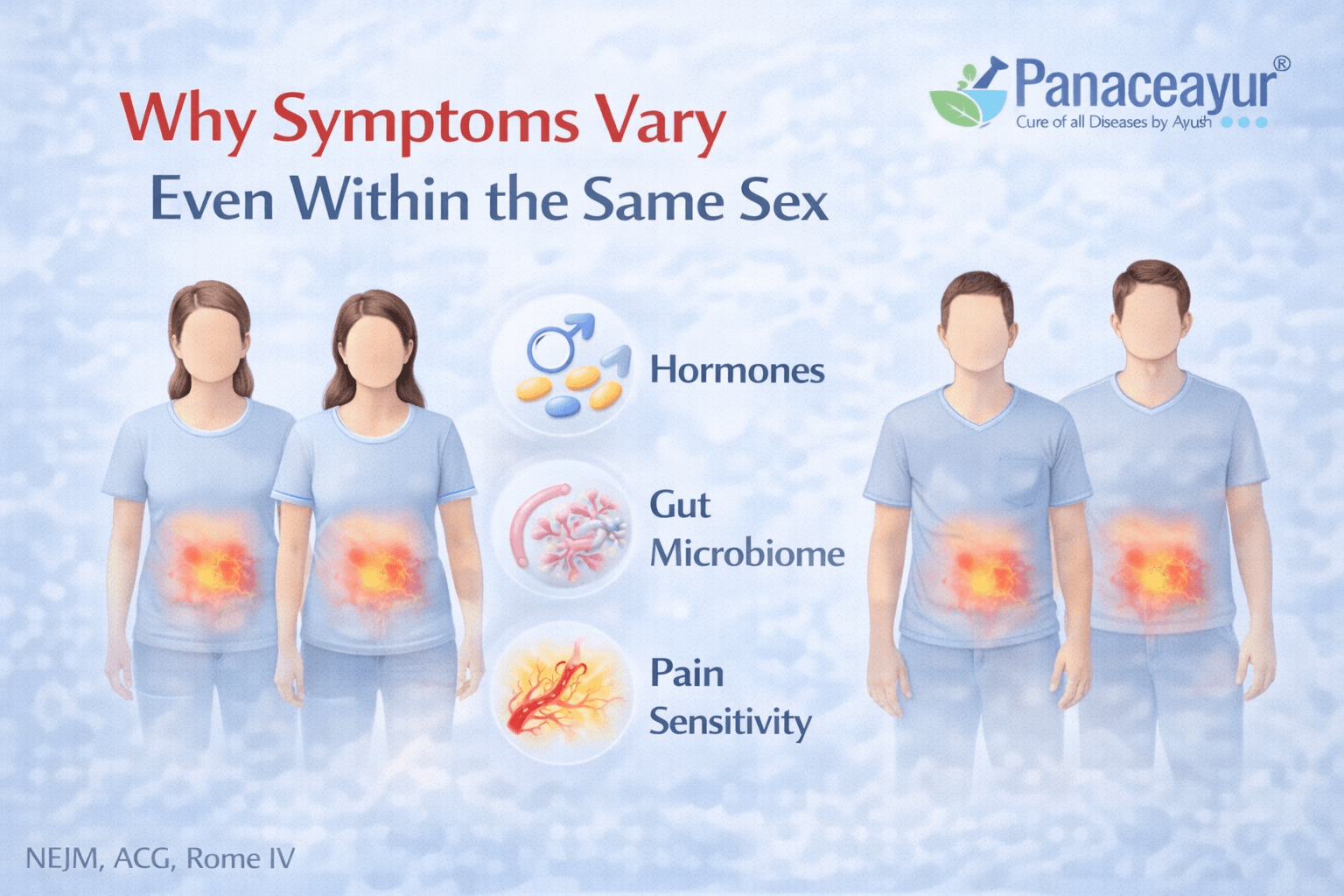
Differences in Digestive Strength and Agni Stability
Even within the same sex, IBS symptoms do not appear in a uniform way because digestive strength, described in Ayurveda as Agni, varies from person to person [17][18]. Two women or two men may eat similar foods yet respond very differently. If your digestion feels sensitive and unpredictable, Ayurveda explains this as unstable Agni rather than a fixed disease pattern. Modern medicine similarly recognizes variability in gut motility and sensitivity among IBS patients, even when diagnostic criteria are identical [3][11].
Individual Nervous System Sensitivity and Stress Response
The way each person responds to stress strongly influences IBS symptoms [11][12]. Some individuals develop bowel urgency during stress, while others experience constipation or abdominal pain. If you notice that emotional pressure immediately affects your digestion, this reflects heightened gut brain communication. Even within the same sex, nervous system sensitivity differs, which explains why stress triggers diarrhea in one person and bloating in another [11][13].
Hormonal Variability Beyond Biological Sex
Hormonal influence does not operate identically in all men or all women [9][4]. Hormone levels, receptor sensitivity, life stage, and prior health conditions modify how the gut responds. If you are a woman, two people with similar menstrual cycles may still experience very different IBS patterns. If you are a man, variations in stress hormones and metabolic regulation can still shape bowel behavior. Clinicians recognize that hormonal effects are individualized rather than uniform [9][3].
Differences in Gut Sensitivity and Pain Perception
Pain perception varies widely between individuals, even within the same sex [7][8]. Some people experience strong discomfort from minor bowel changes, while others tolerate significant bowel disturbance with little pain. If your symptoms feel intense despite mild bowel changes, this reflects visceral hypersensitivity rather than disease severity. Modern research confirms that IBS severity is often determined by sensory processing rather than measurable gut damage [7][11].
Role of Microbiome and Immune Response
The gut microbiome differs significantly between individuals and contributes to symptom variation [14][12]. Two people of the same sex may have completely different microbial compositions, influencing gas production, bowel movement speed, and immune signaling. If you react strongly to certain foods while another person does not, this difference often reflects microbiome variation rather than intolerance alone. Clinicians increasingly recognize microbiome diversity as a key reason IBS symptoms vary so widely [14].
Lifestyle Patterns and Daily Habits
Daily habits strongly influence IBS expression [17][19]. Sleep quality, meal timing, physical activity, caffeine use, and stress management shape digestive rhythm. If your symptoms worsen during irregular routines, Ayurveda explains this as Vata disturbance caused by lifestyle inconsistency. Modern medicine echoes this by recognizing circadian rhythm disruption and behavioral triggers as important IBS modifiers [3][17].
Why One Diagnosis Leads to Many Experiences
IBS is diagnosed using the same criteria, yet they experience it differently because digestion, hormones, nervous system response, microbiome, and lifestyle interact uniquely in each body [3][4][17]. If you have wondered why your symptoms do not match someone else with IBS, this variability is expected rather than unusual. Both Ayurveda and modern gastroenterology agree that IBS is a functional condition shaped by individual physiology rather than a single uniform disease [17][3].
Red Flags-When It Is Not IBS
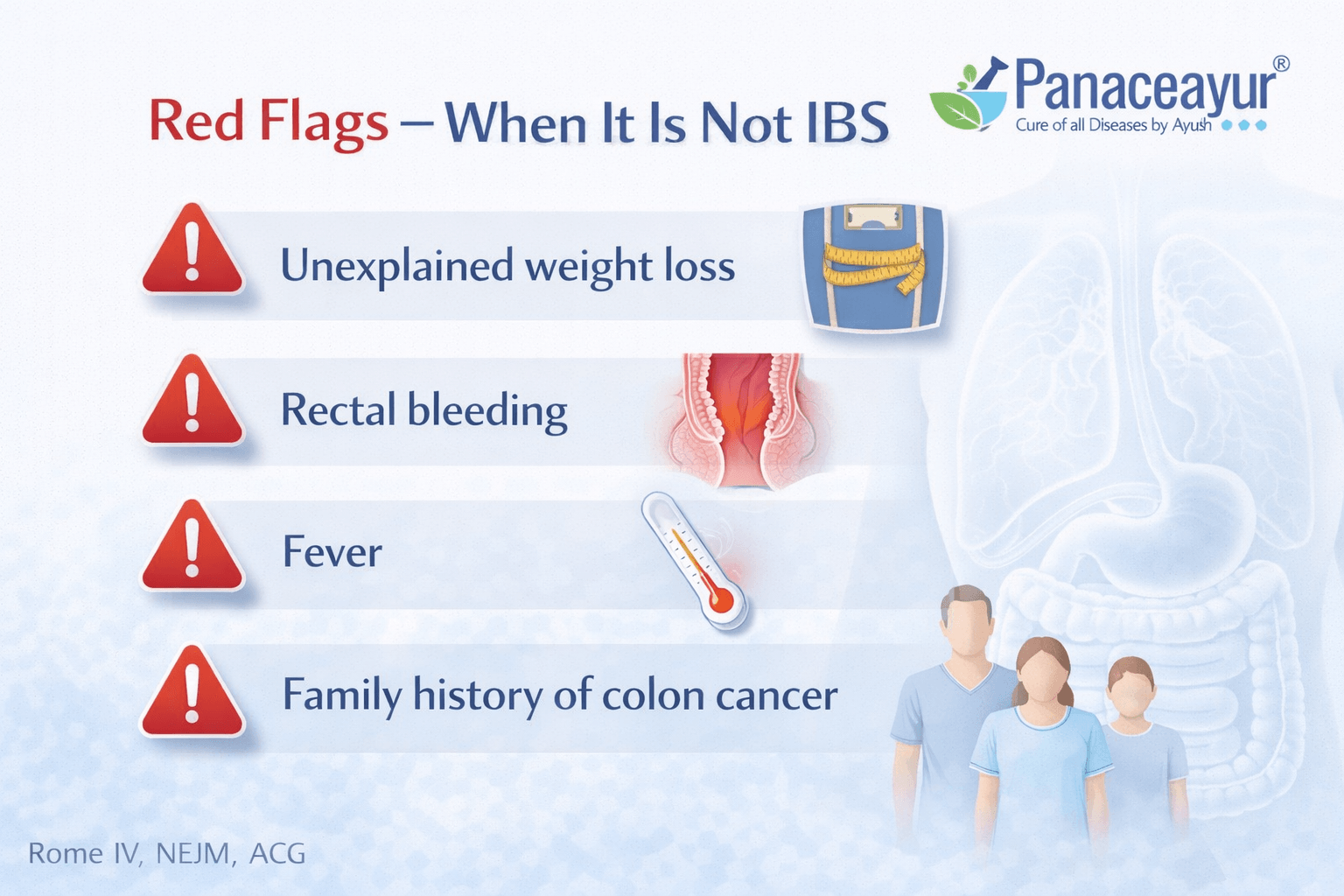
Why Red Flags Matter in Digestive Symptoms
Irritable Bowel Syndrome is classified as a functional gastrointestinal disorder, which means it does not cause structural damage, ongoing inflammation, bleeding, or progressive tissue injury [1][3]. Because of this, certain symptoms are considered red flags and should never be attributed to IBS without proper medical evaluation. If you or a clinician overlook these warning signs, serious underlying conditions may be missed. International guidelines clearly state that IBS should be diagnosed only after these red flags are carefully excluded [1][2][15].
Blood in Stool or Black Tarry Stools
Visible blood in the stool or black, tarry stools are not features of IBS [3][15][16]. IBS does not cause gastrointestinal bleeding. If you notice blood mixed with stool, blood on toilet paper, or dark stools, this requires immediate medical attention. Clinicians consider possibilities such as inflammatory bowel disease, colorectal polyps, infections, hemorrhoids, or malignancy. This warning sign is especially important in adults over the age of forty or in anyone with additional risk factors [15][16].
Unintentional Weight Loss Fatigue or Anemia
Unexplained weight loss, persistent fatigue, or laboratory evidence of anemia are inconsistent with IBS [1][3][15]. While IBS symptoms may fluctuate and affect appetite temporarily, they do not cause progressive nutritional depletion or systemic weakness. If you experience ongoing weight loss or feel persistently exhausted, clinicians must evaluate for conditions such as celiac disease, inflammatory bowel disease, chronic infections, or cancer rather than assuming IBS [3][15].
Nocturnal Symptoms That Disrupt Sleep
Symptoms that wake a person from sleep are another important red flag [15][16]. IBS symptoms are usually linked to meals, stress, or bowel movements and are uncommon during deep sleep. If you experience diarrhea or abdominal pain that regularly wakes you at night, this suggests an organic disease process rather than a functional disorder. Clinicians view nocturnal symptoms as a strong reason to pursue further diagnostic testing [15].
New Onset of Symptoms After Midlife
The appearance of IBS-like symptoms for the first time after the age of fifty requires careful assessment [3][15]. Although IBS can persist into older age, new onset symptoms later in life are more likely to reflect structural or inflammatory disease. If you develop bowel changes for the first time in midlife or later, doctors prioritize ruling out malignancy, inflammatory conditions, or other age-related gastrointestinal disorders before considering IBS [3][15].
Persistent Fever Vomiting or Severe Progressive Pain
IBS does not cause persistent fever, recurrent vomiting, or severe abdominal pain that progressively worsens [1][3][16]. IBS-related pain is typically relieved at least partially after bowel movements. If pain continues to intensify, is unrelated to defecation, or is accompanied by fever or vomiting, it should not be labeled as IBS. Clinicians interpret these features as indicators of infection, obstruction, inflammation, or other serious pathology [16].
Family History of Serious Gastrointestinal Disease
A family history of inflammatory bowel disease, colorectal cancer, or celiac disease increases the need for thorough evaluation [15][16]. If you have close relatives with these conditions, symptoms that resemble IBS warrant additional testing. Clinicians consider genetic and immune-mediated risk factors when deciding how extensively to investigate bowel symptoms, even if they initially appear functional [15].
Clinical Safety and Diagnostic Responsibility
From a safety perspective, international guidelines emphasize that IBS is a diagnosis of exclusion in the presence of red flags [1][2][3][15]. Symptom-based criteria such as Rome IV are applied only after warning signs have been ruled out in the appropriate clinical context. If you are being evaluated for IBS, it is appropriate and responsible for clinicians to ask detailed questions, order tests when indicated, and avoid labeling symptoms as IBS prematurely [1][15].
This careful approach protects patients and ensures that IBS is diagnosed accurately rather than used as a default explanation for symptoms that may signal a more serious condition.
What to Track for Faster Diagnosis
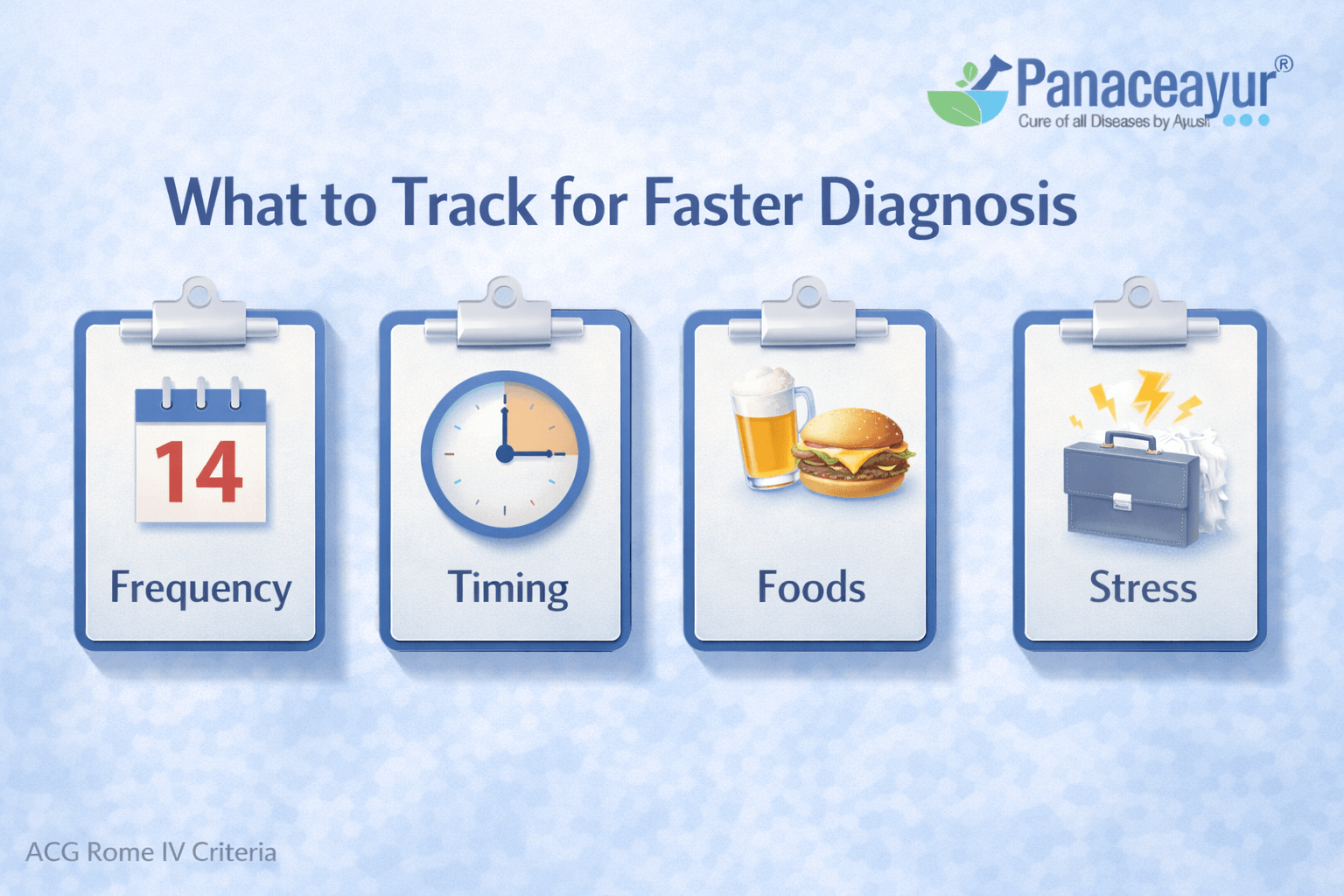
Symptom Timing and Frequency
Tracking when symptoms occur is one of the most effective ways to speed up an accurate diagnosis [1][3]. IBS symptoms are defined by their relationship to bowel movements, meals, and stress. If you record when abdominal discomfort begins, how long it lasts, and how often it appears, clinicians can more easily distinguish IBS from other gastrointestinal disorders. Noting whether pain improves or worsens after bowel movements is particularly important, as this pattern is central to symptom based diagnostic criteria [1].
Stool Frequency and Stool Form
Recording stool frequency and stool form provides critical diagnostic information [1][2][3]. IBS is characterized by changes in stool consistency, not just how often stools occur. If you track whether stools are hard, loose, or variable over time, doctors can better classify the IBS subtype and rule out inflammatory or infectious causes. Consistency over weeks rather than isolated episodes carries the most diagnostic value [2].
Relationship Between Symptoms and Meals
Meal related symptom patterns help clinicians understand gut motility and reflex activity [3][11]. If you notice that symptoms appear shortly after eating, worsen after large meals, or are triggered by irregular meal timing, this information is highly relevant. IBS symptoms often reflect an exaggerated digestive response rather than food allergy or intolerance. Tracking meal timing and portion size is often more useful than listing individual foods alone [3].
Stress Emotional State and Sleep Quality
Stress and emotional state strongly influence IBS symptoms through the gut brain axis [11][12]. If you track stressful events, emotional strain, or sleep disruption alongside digestive symptoms, clear patterns often emerge. Many patients notice that symptoms worsen during periods of anxiety or poor sleep even when diet remains unchanged. Clinicians rely on this information to understand symptom triggers and avoid unnecessary testing [11].
Menstrual Cycle and Hormonal Changes
For women, tracking the menstrual cycle is especially important [9][4]. If symptoms worsen predictably before or during menstruation, this supports a functional diagnosis influenced by hormonal regulation rather than structural disease. Recording cycle timing alongside bowel symptoms allows clinicians to interpret constipation, bloating, or pain flares more accurately and reduces diagnostic uncertainty [9].
Nocturnal Symptoms and Alarm Features
Recording whether symptoms occur during sleep helps identify red flags [15][16]. IBS symptoms are uncommon at night. If you experience pain or diarrhea that wakes you from sleep, this information should be communicated clearly to your doctor. Tracking the presence or absence of nocturnal symptoms helps clinicians decide when further investigation is necessary [15].
Response to Bowel Movements
IBS pain typically improves at least partially after defecation [1][3]. If you note whether pain relief follows bowel movements, this detail supports a functional diagnosis. Pain that does not change after defecation raises concern for other conditions. Clinicians use this response pattern as a key diagnostic distinction [1].
Duration and Symptom Persistence
IBS is a chronic condition with symptoms present for months rather than days [1][2]. Tracking how long symptoms have been occurring helps rule out acute infections or transient digestive disturbances. If symptoms have been present for several months with a fluctuating course, this pattern aligns with IBS rather than short term gastrointestinal illness [2].
Why Accurate Tracking Matters
When you bring structured symptom tracking to a consultation, clinicians can apply diagnostic criteria more confidently and avoid unnecessary tests [1][3][15]. Accurate records shorten the diagnostic process, reduce anxiety, and help ensure that IBS is diagnosed appropriately only after red flags are excluded. This collaborative approach improves safety and leads to clearer treatment planning [3][15].
When IBS symptoms are viewed through the Ayurvedic lens of Grahani, Agni, and dosha balance, treatment shifts from symptom suppression to functional restoration. This individualized approach focuses on correcting digestive strength, bowel rhythm, and stress response, which is explained step by step in the Ayurvedic treatment approach for IBS.
FAQs
Can IBS symptoms change over time in the same person
Yes, IBS symptoms can change over time, even in the same individual. You may experience constipation dominant symptoms for months and later notice diarrhea or mixed bowel patterns. Clinicians understand that IBS is a functional condition influenced by stress, hormones, lifestyle, and nervous system regulation, so symptom patterns are expected to fluctuate rather than remain fixed.
Why do IBS symptoms feel worse during stress
Stress directly affects the gut through the gut brain axis. If you notice that emotional pressure quickly triggers bowel changes, pain, or urgency, this is not imagined. Stress alters gut movement, gut sensitivity, and digestive signaling, which can intensify IBS symptoms even when diet remains unchanged.
Can IBS symptoms occur without abdominal pain
Yes, IBS symptoms can occur with minimal or no abdominal pain, especially in men. Some people mainly experience urgency, loose stools, bloating, or bowel unpredictability. While abdominal pain is an important diagnostic feature, clinicians recognize that pain intensity varies widely and does not always reflect how disruptive symptoms are in daily life.
Do hormones really affect IBS symptoms
Hormones play a significant role in IBS symptoms, particularly in women. Estrogen and progesterone influence bowel movement speed and gut sensitivity. If your symptoms worsen around menstruation, pregnancy, or menopause, hormonal regulation is a well established biological factor rather than coincidence.
Is IBS dangerous or does it damage the intestines
IBS does not cause structural damage, bleeding, inflammation, or cancer. It is a functional disorder, meaning symptoms arise from how the gut functions rather than from tissue injury. However, IBS can significantly affect quality of life, which is why accurate diagnosis and proper management are important.
How do doctors distinguish IBS from serious diseases
Clinicians rely on symptom patterns combined with careful screening for warning signs. If features such as blood in stool, unexplained weight loss, anemia, or nighttime symptoms are absent, IBS can often be diagnosed without extensive testing. When these warning signs are present, further evaluation is necessary.
Can IBS be diagnosed with a single test
There is no single test that confirms IBS. Diagnosis is based on symptom history, duration, and the exclusion of red flags. Medical tests are used selectively to rule out other conditions rather than to prove IBS itself.
Why do two people with IBS have completely different symptoms
IBS symptoms vary because digestion, hormones, stress response, gut sensitivity, microbiome composition, and daily habits differ from person to person. If your symptoms do not match someone else with IBS, this variability is expected and recognized by both modern gastroenterology and Ayurvedic medicine.
Reference
[1] Rome IV, Lacy et al., Gastroenterology 2016, bowel disorders and IBS definition
https://doi.org/10.1053/j.gastro.2016.02.031
[2] Rome Foundation, Rome IV criteria summary page
[3] Ford, Lacy, Talley, IBS review, NEJM 2017
https://www.nejm.org/doi/full/10.1056/NEJMra1607547
[4] Kim and Kim, sex gender differences in IBS, JNM 2018
https://www.jnmjournal.org/journal/view.html?doi=10.5056/jnm18082
[5] Lovell and Ford, global prevalence meta analysis, CGH 2012
https://doi.org/10.1016/j.cgh.2012.02.029
[6] Canavan et al., IBS epidemiology, Clinical Epidemiology 2014
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4049690
[7] Chang et al., gender and patient perspective in IBS, Gastroenterology 2006
https://doi.org/10.1053/j.gastro.2005.09.071
[8] Adeyemo and Chang, gender differences review, JNM 2008
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3271257
[9] Meleine and Matricon, hormones and mechanisms, WJG 2014
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4051914
[10] Houghton et al., menstrual cycle and IBS, AJG 2002
https://doi.org/10.1111/j.1572-0241.2002.05692.x
[11] Mayer et al., systems view of IBS, gut brain axis, Gastroenterology 2015
https://doi.org/10.1053/j.gastro.2015.07.052
[12] Mayer et al., gut brain axis and microbiota, JCI 2015
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4362121
[13] Fond et al., anxiety and depression in IBS meta analysis, CGH 2014
https://doi.org/10.1016/j.cgh.2013.12.032
[14] Simren et al., microbiota in functional bowel disorders, Gut 2013
https://gut.bmj.com/content/62/1/159
[15] NICE guideline CG61 IBS in adults
https://www.nice.org.uk/guidance/cg61
[16] Mayo Clinic, IBS overview and warning signs
https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome
[17] Charaka Samhita, Chikitsa Sthana, Grahani Chikitsa Adhyaya
https://www.carakasamhitaonline.com/index.php?title=Grahani_Chikitsa
[18] Ashtanga Hridaya, Grahani Chikitsa Adhyaya, standard editions in print
[19] Bhavaprakasha, relevant Grahani, Agni, Atisara references, standard editions in print