- IBS Diagnosis Basics, Normal Tests, and Functional Disorder
- Rome IV Criteria for IBS Diagnosis
- Diagnosis of Exclusion and the Limitations of Tests
- Functional vs Psychological Explanation
- Misdiagnosis and Overlap Conditions
- Clinical Warning Signs and Re-evaluation
- Why IBS Diagnosis Does Not Lead to Cure
- Ayurvedic Diagnostic Framework
- Gut Mind Axis in Ayurveda and Modern Science
- Post Infectious IBS
- Gender, Hormonal, and Lifecycle Influence
- Medication Induced IBS Patterns
- Integrative Diagnosis Using Modern Medicine and Ayurveda
- FAQs
- References
- Ayurvedic Classical References
For many patients, IBS diagnosis explained only comes after a long series of investigations. Blood tests, stool tests, scans, and even colonoscopy frequently show normal results, yet symptoms such as abdominal pain, bloating, constipation, diarrhea, or bowel urgency continue. This pattern is common in clinical practice. IBS is usually diagnosed only after doctors have ruled out serious conditions such as inflammatory bowel disease or cancer, rather than through a single definitive test [1].
This diagnostic process often leaves patients confused and frustrated. When medical reports repeatedly say that everything is normal, it can feel as though symptoms are being overlooked. However, IBS diagnosis explained from a medical perspective means recognizing a functional gastrointestinal disorder, where symptoms arise from disordered gut function rather than visible structural damage, infection, or inflammation [2]. Normal test results do not mean the symptoms are imaginary or insignificant.
IBS is also far from rare. It affects a large population worldwide and is associated with a significant reduction in quality of life, work productivity, and emotional well-being. Research shows that uncertainty around diagnosis and the lack of visible findings often contribute to patient distress and dissatisfaction with care [14]. Understanding IBS diagnosis explained in this context helps patients make sense of why symptoms persist despite normal investigations and why further explanation is necessary beyond test reports.
IBS Diagnosis Basics, Normal Tests, and Functional Disorder
How IBS Is Diagnosed in Everyday Clinical Practice
When we look at how IBS is diagnosed in real clinical settings, it quickly becomes clear that it does not follow the same rules as most digestive diseases. There is no single test that confirms IBS. Doctors arrive at the diagnosis by listening to symptoms carefully and by ruling out conditions that could be dangerous or progressive. This approach is standard across gastroenterology and is supported by major professional guidelines [1].
From a patient perspective, this process can feel unsatisfying. You may expect a test result that clearly explains what is wrong, but instead you are told that IBS fits your symptoms even though reports look normal. Clinically, IBS is still considered a valid diagnosis despite the absence of visible disease, which often feels difficult to accept at first [2].
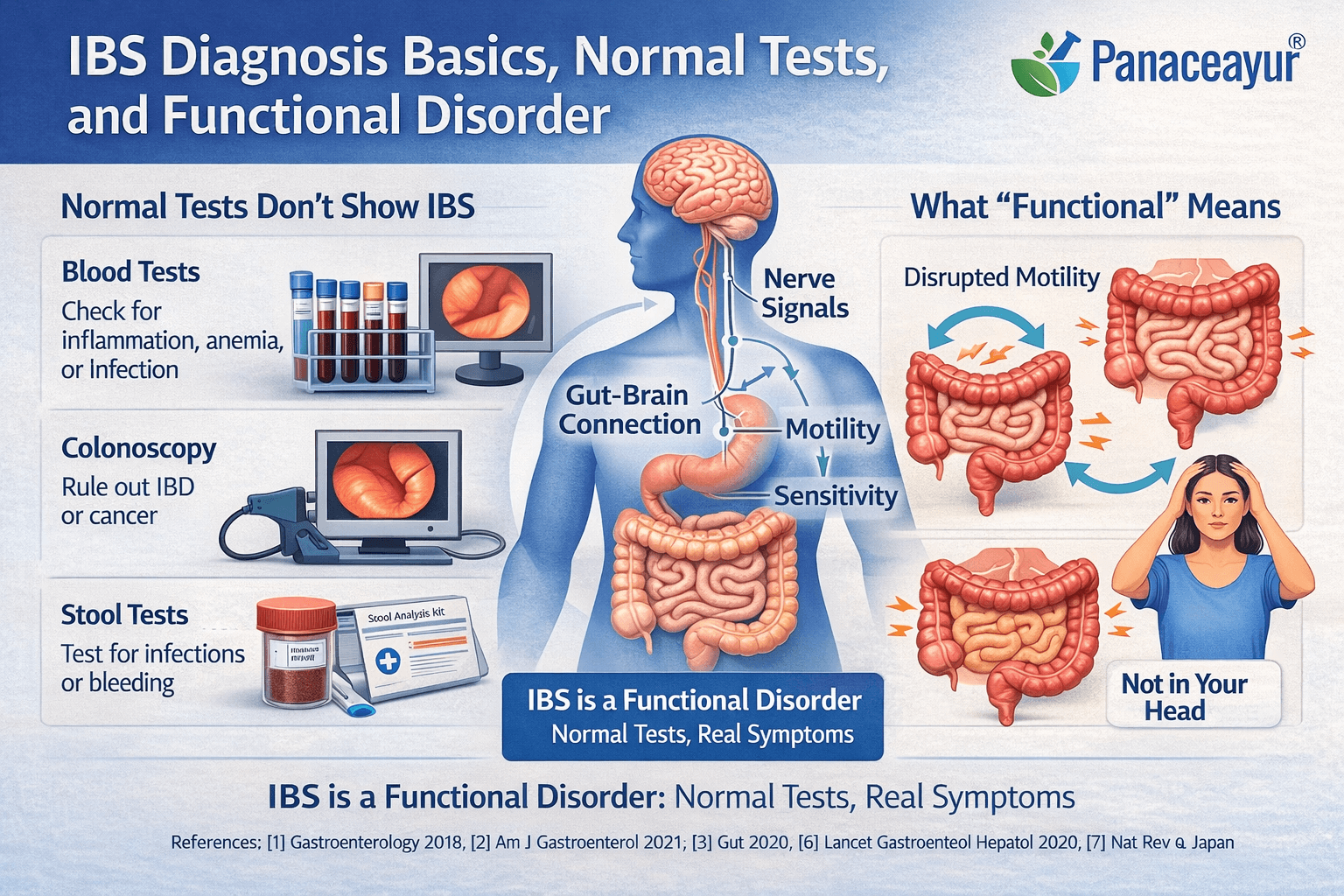
Why Blood Tests and Colonoscopy Often Do Not Show Abnormalities
When someone presents with ongoing bowel symptoms, doctors first focus on excluding serious disease. Blood tests are used to look for inflammation, anemia, infection, or immune related disorders. Stool tests help rule out infection or bleeding. Colonoscopy allows direct inspection of the bowel lining and helps exclude inflammatory bowel disease, cancer, or other structural problems [2].
When all these tests come back normal, many patients feel confused. It is important to understand that these investigations are designed to detect damage or inflammation. IBS does not cause visible injury to the gut lining, so normal results are expected rather than surprising [3].
What Routine Tests Are Not Designed to Measure
Standard medical tests do not assess how the gut muscles contract, how sensitive the intestinal nerves are, or how signals travel between the gut and the brain. They also do not capture subtle immune or nervous system changes that can strongly influence bowel function. This explains why symptoms can be intense while reports remain normal [3].
For patients, this gap often feels like being told nothing is wrong, when in reality the problem simply lies outside the scope of routine testing.
What Doctors Mean by a Functional Gastrointestinal Disorder
IBS belongs to a group of conditions known as functional gastrointestinal disorders. In medical terms, functional means that the structure of the organ is intact, but its regulation is altered. In IBS, the bowel itself looks normal, yet its movement, sensitivity, and coordination do not function smoothly [6].
Research shows that people with IBS may experience abnormal bowel contractions, increased pain sensitivity, and changes in immune and nerve signaling. These changes are real and biologically based, even though they are not visible on scans or biopsies.
Why Functional Does Not Mean Psychological
Many people hear the word functional and assume the problem is psychological. This misunderstanding has led to frustration for countless patients. Modern research has clearly shown that IBS involves altered communication between the gut, nervous system, immune pathways, and brain [7].
Stress can influence symptoms, but it does not create IBS on its own. The condition remains physical in nature, even though emotions and life stressors can affect how strongly symptoms are felt.
When IBS is understood this way, normal test results begin to make sense. The symptoms persist not because nothing is wrong, but because the problem lies in regulation rather than visible damage.
Rome IV Criteria for IBS Diagnosis
Why Rome IV Exists
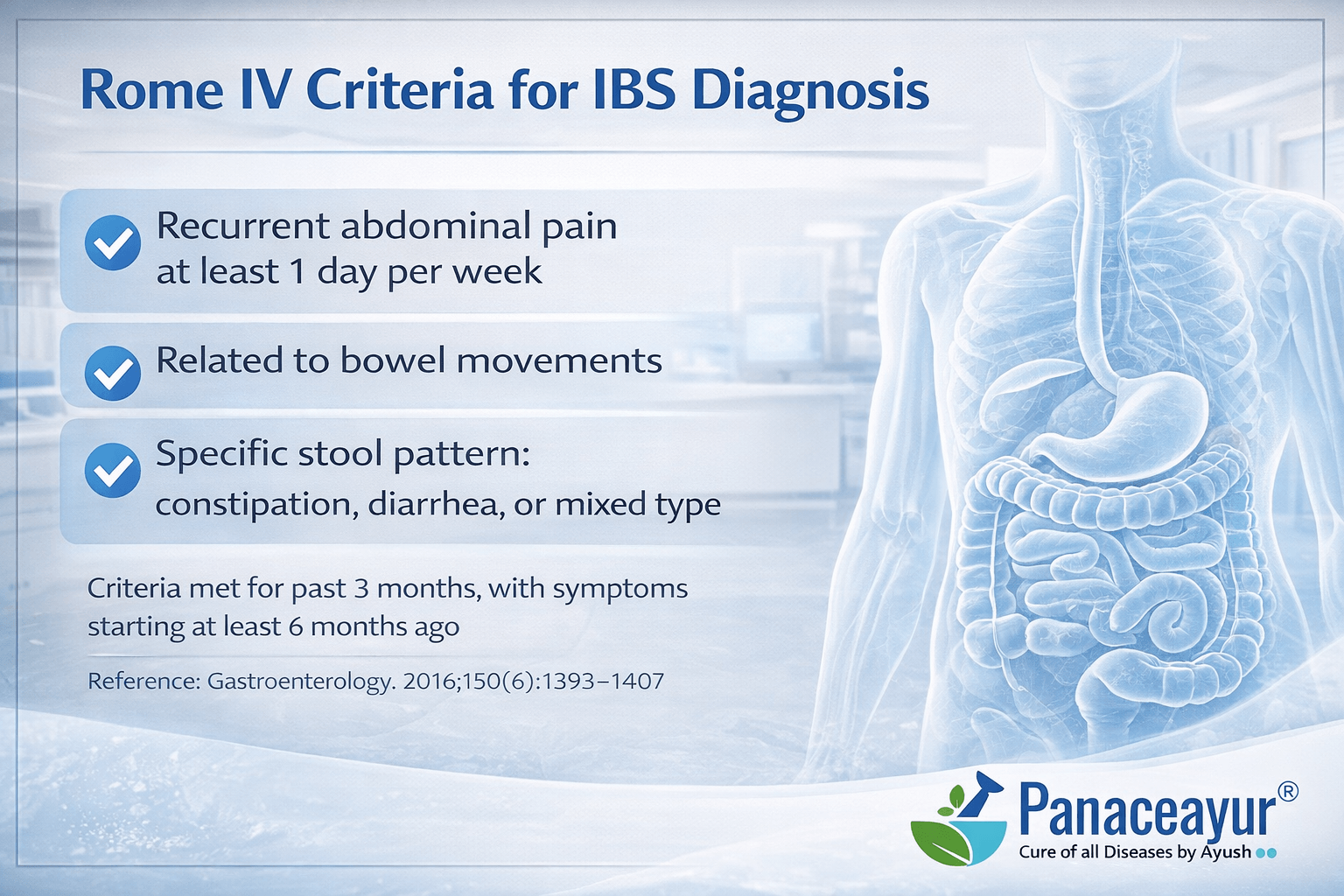
When doctors diagnose IBS, they are not guessing. They rely on standardized criteria developed by international experts to bring consistency and accuracy to diagnosis. The Rome IV criteria were created for this reason. They help clinicians identify IBS based on symptom patterns rather than relying on test results alone, especially when investigations are normal [1].
From a patient point of view, this can feel different from how other conditions are diagnosed. You may expect a scan or a lab value to confirm the diagnosis. Instead, the Rome IV framework asks a different question. Do your symptoms follow a pattern that has been repeatedly observed, studied, and validated across large populations.
Core Rome IV Symptom Requirements
Under Rome IV, IBS is diagnosed when a person has recurrent abdominal pain, on average at least one day per week, over the last three months. This pain must be associated with changes in bowel habits. These include pain related to bowel movements, changes in how often stools occur, or changes in stool appearance [4].
Doctors do not look at one symptom in isolation. They look at how symptoms behave together over time. This is important because many healthy people occasionally experience bloating or irregular stools. IBS is identified when symptoms form a persistent and disruptive pattern rather than occasional discomfort.
Why Duration Matters in Diagnosis
Rome IV places strong emphasis on symptom duration. Symptoms must have started at least six months before diagnosis, even if they became more noticeable in the last three months. This rule exists to prevent over diagnosis and to ensure that short term infections or temporary gut disturbances are not mislabeled as IBS [1].
For patients, this explains why doctors often ask detailed questions about timelines. When did the pain begin. How long has it been happening. Has it been consistent. These questions are not casual. They are essential for making a confident diagnosis.
Rome IV Is a Positive Diagnosis, Not a Diagnosis of Exclusion
One of the most important changes introduced by Rome IV is the shift toward making IBS a positive diagnosis. Earlier approaches treated IBS as something diagnosed only after every possible disease was excluded. Rome IV recognizes IBS as a legitimate condition that can be diagnosed when criteria are met, even when tests are normal [4].
This shift matters. It helps doctors move away from endless testing and helps patients understand that IBS is not a label given out of uncertainty. It is a diagnosis based on patterns that have been carefully studied and agreed upon by the global gastroenterology community.
Why Rome IV Still Requires Clinical Judgment
While Rome IV provides a structured framework, it does not replace clinical judgment. Doctors still consider warning signs such as unexplained weight loss, anemia, bleeding, or symptoms starting later in life. If these red flags are present, further investigation is necessary before confirming IBS [1].
For most patients without red flags, Rome IV offers reassurance. It explains why IBS can be diagnosed confidently, why tests may be normal, and why symptoms are still taken seriously even without visible disease.
Diagnosis of Exclusion and the Limitations of Tests
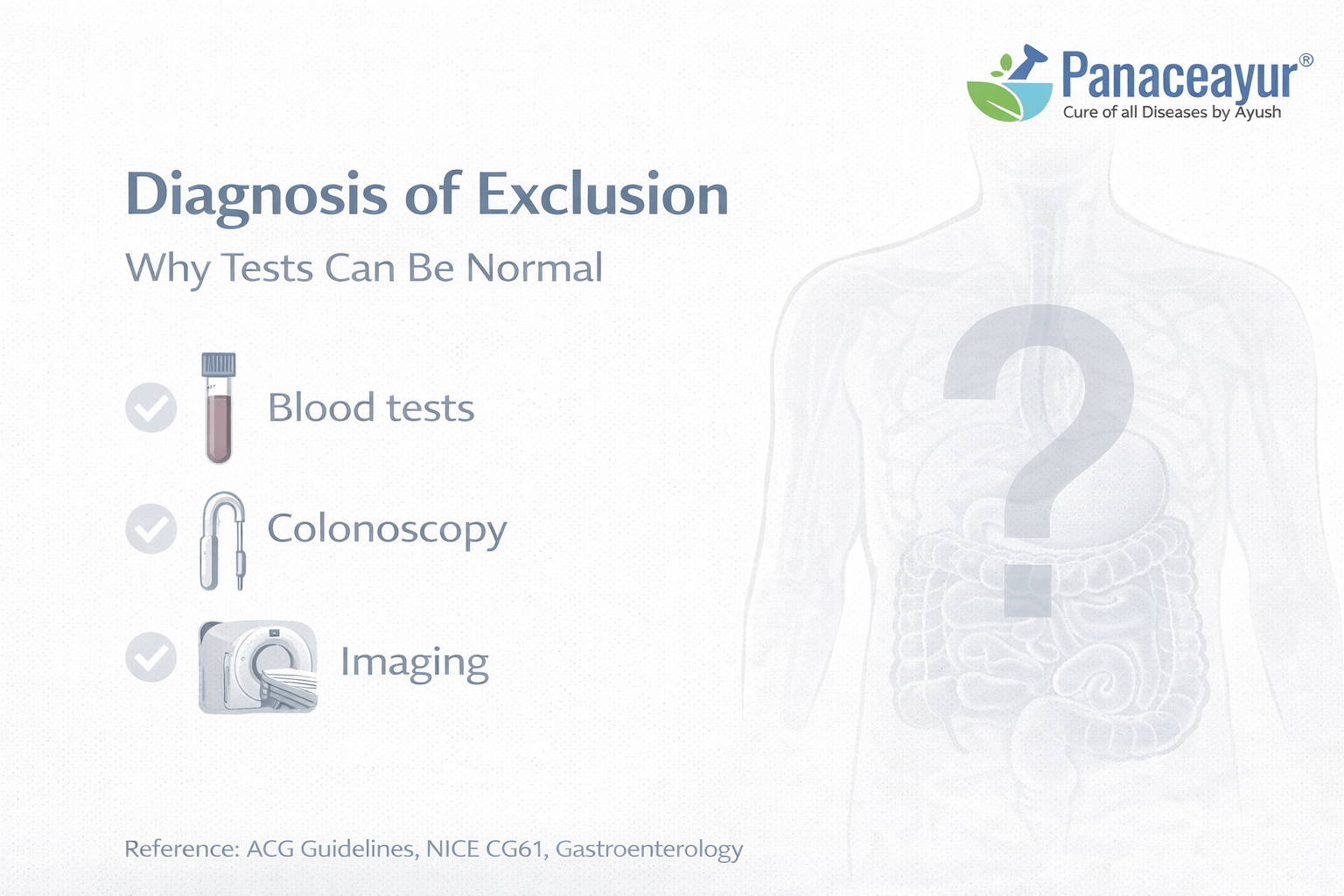
Why IBS Has Traditionally Been Called a Diagnosis of Exclusion
For many years, IBS was described as a diagnosis of exclusion. In simple terms, this meant doctors first focused on ruling out other conditions before arriving at IBS. From a clinical safety point of view, this made sense. Symptoms such as abdominal pain, diarrhea, constipation, or bloating can also appear in conditions like inflammatory bowel disease, celiac disease, or colorectal cancer. Doctors therefore start by ensuring that nothing dangerous is being missed [2].
From the patient side, this process can feel exhausting. You may go through repeated tests hoping each one will finally explain what you are experiencing. When all reports come back normal and IBS is mentioned at the end, it can feel like a diagnosis given because nothing else was found. This emotional gap is one of the reasons IBS has historically been misunderstood and poorly accepted by patients [6].
How Modern Guidelines Have Shifted the Approach
Clinical practice has evolved. Current guidelines in both the UK and the USA no longer recommend endless testing once key warning signs have been ruled out. Instead, IBS is now increasingly diagnosed using symptom based criteria alongside a limited set of investigations to ensure safety [5].
For patients, this shift is important to understand. Fewer tests does not mean less care. It means doctors are balancing the need to exclude serious disease with the recognition that repeated normal tests rarely provide new answers once IBS patterns are clear.
What Standard Tests Are Good At Detecting
Blood tests are excellent at identifying inflammation, anemia, infection, or immune related conditions. Stool tests help rule out infection or bleeding. Colonoscopy allows doctors to directly examine the bowel lining and take biopsies if needed. These tools are extremely effective for detecting structural disease, inflammatory conditions, and cancer [2].
When these tests are normal, they have done their job. They have confirmed that the bowel is structurally intact and free from dangerous disease.
What Standard Tests Cannot Measure
Where frustration often begins is in what these tests cannot show. Routine investigations do not measure gut motility, nerve sensitivity, or how signals move between the gut and the nervous system. They also do not capture subtle immune activation or regulatory dysfunction that can strongly influence bowel function [6].
This is why a person can have severe symptoms while every report looks reassuring. The tests are not wrong. They are simply not designed to assess functional regulation.
Why Normal Tests Do Not Invalidate Symptoms
One of the hardest messages for patients to accept is that normal tests do not mean nothing is wrong. IBS exists precisely in this gap between symptoms and structural findings. The limitation lies in the tools, not in the experience of the person living with the condition [2].
Understanding this helps reframe the diagnosis. IBS is not a conclusion reached because doctors ran out of ideas. It is a recognition that current medical tests are excellent at detecting damage, but far less capable of explaining disorders of function.
Functional vs Psychological Explanation
Why IBS Is Classified as a Functional Disorder
In medical language, IBS is described as a functional gastrointestinal disorder. This classification comes from how the condition behaves, not from a lack of seriousness. Research behind the Rome IV framework explains that IBS symptoms arise from altered gut function rather than visible structural disease. The bowel itself appears normal on scans and biopsies, but the way it moves, senses pain, and responds to signals is disrupted [3].
For patients, this distinction is important. Functional does not mean imaginary. It means that the problem lies in regulation rather than damage. Many people experience real pain, urgency, bloating, and bowel changes because the gut is not coordinating properly, even though it looks healthy on routine testing.
Why IBS Is Often Mistaken as Psychological
Because standard tests are normal, IBS has historically been misunderstood as a psychological condition. Patients are sometimes told that stress or anxiety is the main cause, which can feel dismissive. While emotional stress can influence symptoms, modern research makes it clear that IBS cannot be reduced to psychology alone [7].
From a clinical perspective, stress acts more like a volume control than a root cause. It can amplify symptoms that already exist, but it does not explain why bowel habits change, why pain becomes persistent, or why symptoms follow specific patterns related to food, infection, or bowel movement.
The Gut Brain Connection Explains Both Sides
One reason the confusion persists is because IBS sits at the intersection of the gut and the nervous system. Studies on the gut brain axis show that communication between intestinal nerves, immune pathways, and the brain plays a central role in symptom generation [7]. This explains why IBS feels physical yet can worsen during emotional strain.
Patients often recognize this pattern in their own lives. Symptoms may flare during stressful periods, but they do not disappear when stress is removed. This observation supports the idea that IBS is rooted in altered gut regulation, not in psychological imagination.
Post Infectious IBS Shows IBS Is Not Psychological
One of the strongest arguments against a purely psychological explanation comes from post infectious IBS. Research has shown that IBS can begin after a clear gastrointestinal infection, such as food poisoning. Even after the infection resolves, changes in gut sensitivity, immune signaling, and nerve function can persist, leading to long term symptoms [8].
For patients who say they were never the same after an illness, this research provides clarity and relief. It confirms that IBS can start from a physical event and continue because of functional changes, not because of emotional weakness or stress alone.
Understanding the difference between functional and psychological explanations helps patients reframe their experience. IBS is a real condition with real mechanisms. The challenge lies not in believing the symptoms, but in recognizing that current medical tools are better at detecting damage than dysfunction.
Misdiagnosis and Overlap Conditions
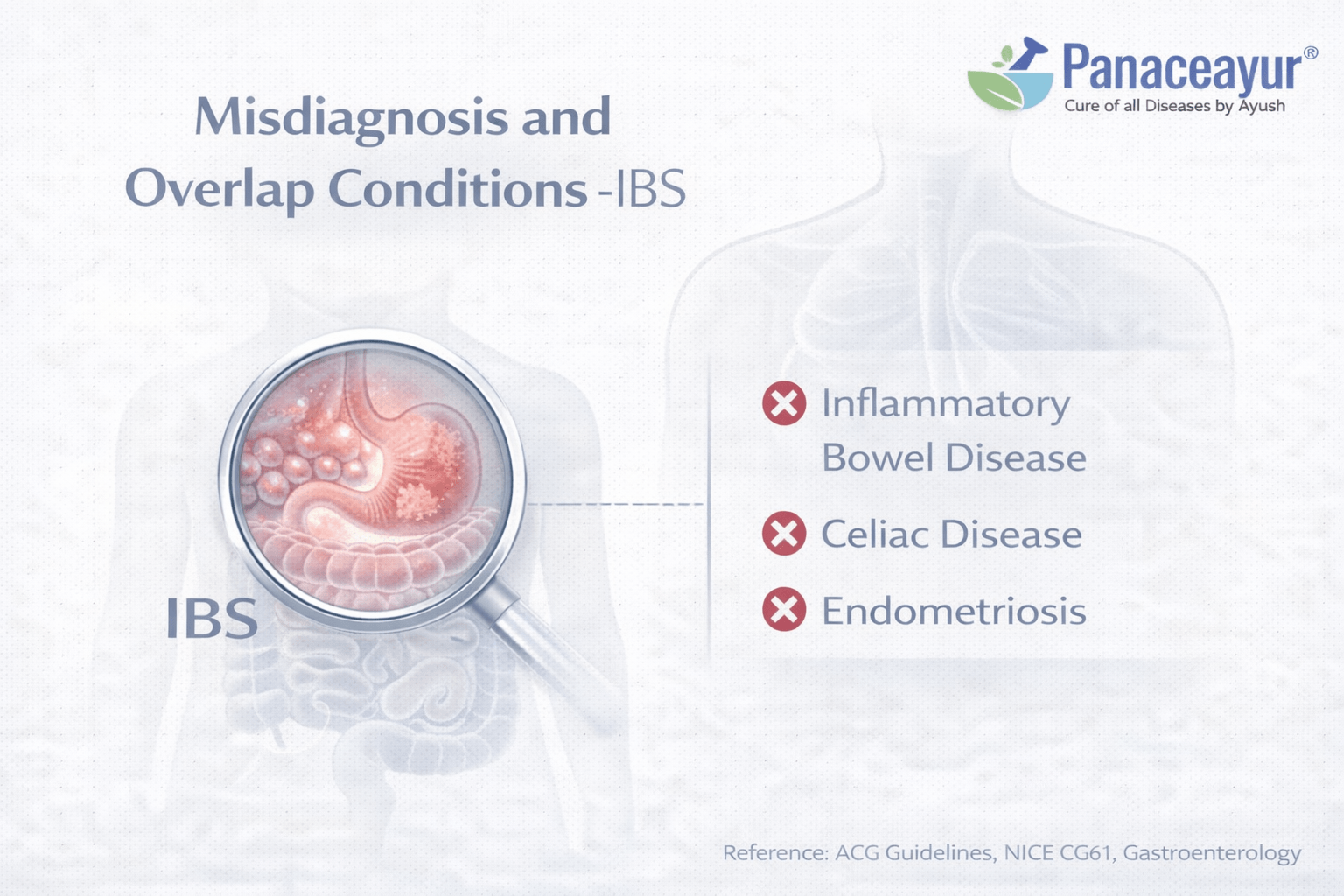
Why IBS Is Often Misdiagnosed
IBS symptoms overlap with many other digestive conditions. Abdominal pain, diarrhea, constipation, bloating, and urgency are not unique to IBS. When tests are limited or symptoms are grouped too quickly, other conditions can be mistakenly labeled as IBS. This is not due to negligence. It reflects the reality that several gut disorders produce similar day to day experiences for patients [11].
For patients, misdiagnosis is frustrating. You may follow multiple treatment plans without meaningful improvement, leading to doubt about the diagnosis itself. Understanding common overlap conditions helps explain why some people do not respond as expected to standard IBS management.
Small Intestinal Bacterial Overgrowth and IBS Overlap
Small intestinal bacterial overgrowth is one of the most frequently discussed overlap conditions. It can cause bloating, gas, abdominal discomfort, diarrhea, or constipation, all of which closely resemble IBS symptoms. Breath tests are commonly used, but they have limitations and can produce false positive or false negative results [10].
Some patients experience temporary improvement with antibiotics, followed by relapse. This pattern often leads to repeated treatment cycles without long term resolution. From a clinical perspective, this overlap explains why treating presumed IBS with antibiotics may help briefly but fails to provide lasting relief for many people.
Bile Acid Malabsorption Often Labeled as IBS
Bile acid malabsorption is another condition commonly mistaken for IBS, especially in people with chronic diarrhea. Excess bile acids entering the colon can cause urgency, frequent loose stools, and discomfort. Because routine testing for bile acid malabsorption is not widely available in all settings, many patients are diagnosed with IBS instead [9].
For patients with diarrhea predominant symptoms that do not respond to typical IBS treatments, this overlap is particularly relevant. Recognizing bile acid related symptoms can change management and improve outcomes.
Microscopic Colitis Despite Normal Colonoscopy Appearance
Microscopic colitis presents one of the clearest examples of diagnostic overlap. Patients often have chronic watery diarrhea, urgency, and abdominal discomfort. During colonoscopy, the bowel lining may look completely normal. The diagnosis is made only when biopsies are taken and examined under a microscope [12].
When biopsies are not performed, microscopic colitis can be missed and symptoms may be labeled as IBS. For patients, this explains why colonoscopy alone does not always provide definitive answers, even when symptoms are severe.
Why Overlap Conditions Matter for Patients
Overlap conditions do not mean that IBS is an incorrect diagnosis in all cases. They highlight the importance of careful reassessment when symptoms persist or worsen. If treatments do not help, it is reasonable to ask whether another condition may be contributing or whether multiple mechanisms are involved [11].
Understanding these overlaps helps patients feel less stuck. Lack of improvement does not mean symptoms are exaggerated or untreatable. It often means the initial label needs refinement rather than abandonment.
Clinical Warning Signs and Re-evaluation
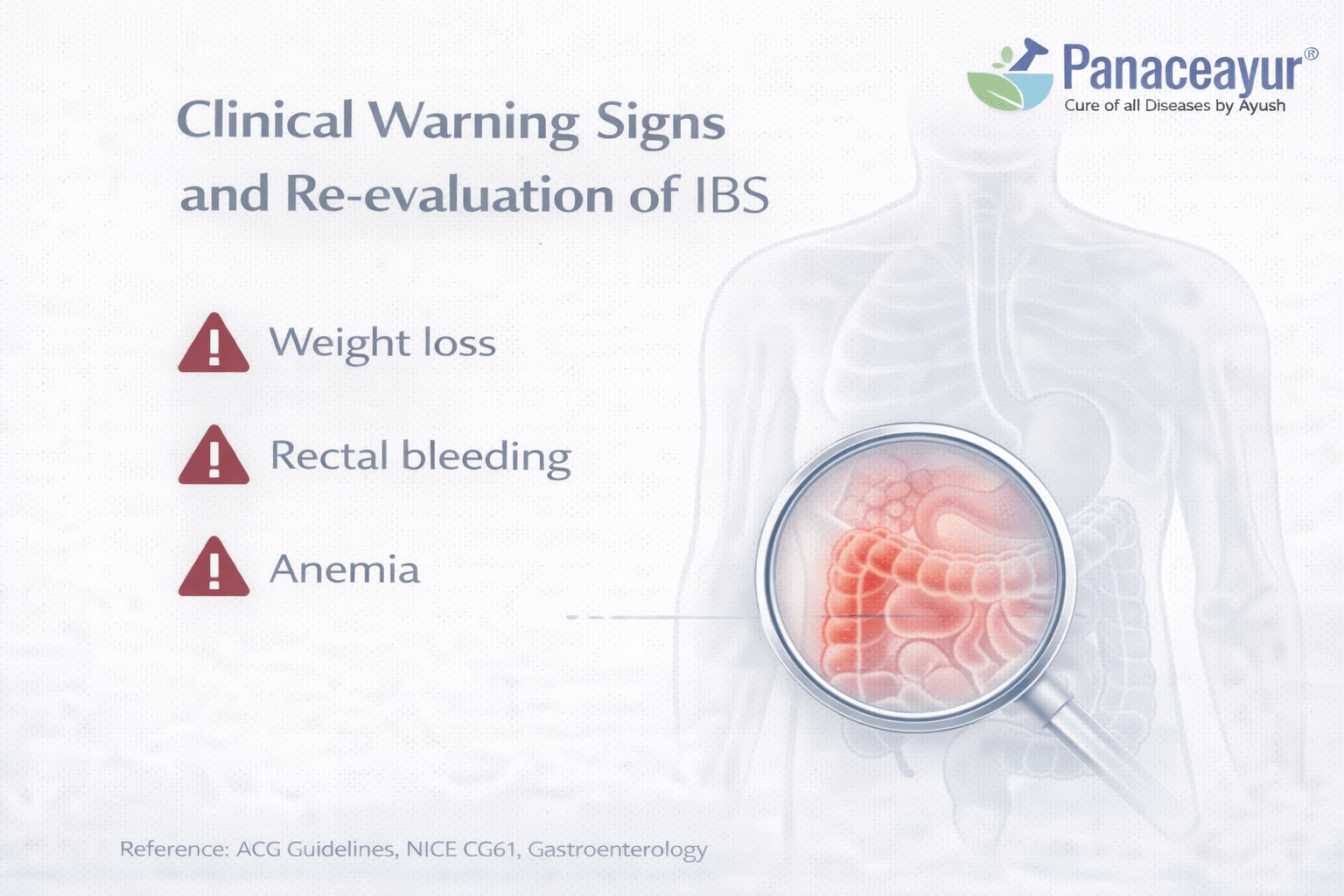
Why Re evaluation Matters in IBS
Most people diagnosed with IBS do not have a dangerous underlying disease. That said, good medicine never treats a diagnosis as permanent if new information appears. Re evaluation is not about doubting the patient or undoing previous care. It is about safety and responsibility. Clinical guidelines emphasize that IBS can be diagnosed confidently, but only when certain warning signs are absent [5].
From a patient perspective, it helps to know that asking for reassessment is reasonable. If symptoms change, worsen, or stop responding to treatment, revisiting the diagnosis is part of good care, not a failure of the original doctor.
Symptoms That Should Never Be Ignored
Certain features raise concern because they are not typical of IBS. These include unintentional weight loss, ongoing fever, anemia, rectal bleeding, persistent vomiting, or symptoms that begin later in life without a prior history. When these appear, doctors are advised to pause and look deeper rather than continuing with an IBS based approach [13].
For patients, this is reassuring. It means that IBS is not used as a blanket label to explain everything. There are clear boundaries where further investigation becomes necessary.
When Ongoing Symptoms Need a Fresh Look
Even without classic red flags, re evaluation may be appropriate when symptoms do not follow the expected course. If pain becomes progressively worse, bowel habits change significantly, or new symptoms appear, doctors may reconsider whether another condition is present alongside IBS or whether the original diagnosis needs refinement [5].
Patients often sense when something feels different from before. Trusting that instinct and communicating changes clearly helps clinicians make better decisions.
Re evaluation Does Not Mean Starting From Zero
One fear patients often have is that reassessment means repeating every test again. In practice, re evaluation is usually focused and selective. Doctors review what has already been done, look at what has changed, and decide whether additional testing is truly necessary [13].
This approach protects patients from unnecessary procedures while ensuring that important developments are not missed.
Why IBS Diagnosis Does Not Lead to Cure
Why a Diagnosis Does Not Automatically Mean Resolution
For many people, receiving an IBS diagnosis brings a sense of relief at first. There is finally a name for what they are experiencing. Over time, however, another question often emerges. If the condition is understood, why do symptoms continue. This gap between diagnosis and resolution is one of the most common frustrations reported by patients with IBS worldwide [14].
From a clinical standpoint, the diagnosis explains what the condition is, but it does not always explain why it developed in that particular person or which mechanisms are dominant. IBS is not a single disease with a single pathway. It represents a group of functional disturbances that can differ widely from one individual to another [6].
Symptom Based Diagnosis Does Not Reveal Root Mechanisms
Modern diagnostic frameworks are designed to recognize symptom patterns. They are not designed to identify the exact biological drivers in each patient. Two people can meet the same diagnostic criteria and yet have very different underlying contributors, such as altered gut motility, heightened nerve sensitivity, immune activation, microbiome imbalance, or disrupted gut brain signaling [6].
When treatment is based only on the diagnostic label, it often targets symptoms rather than mechanisms. This explains why many patients cycle through medications, diets, and lifestyle advice without achieving lasting improvement.
Gut Brain Dysregulation Complicates Treatment
One of the central challenges in IBS management is the involvement of the gut brain axis. Research has shown that IBS symptoms are shaped by ongoing communication between the intestines, nervous system, and immune pathways [7]. This system is dynamic. It changes with stress, illness, sleep patterns, infections, and life events.
Because of this complexity, treatments that focus on only one aspect often provide partial or temporary relief. Pain may improve while bowel habits remain unstable. Bloating may reduce while urgency persists. This does not mean treatment has failed. It reflects the layered nature of the condition.
Why Population Level Treatments Fall Short for Individuals
Most IBS treatments are developed and tested at a population level. They aim to help a large group of patients modestly rather than curing individuals completely. While this approach is useful in research, it leaves many patients feeling that care is fragmented or incomplete [14].
From the patient perspective, it can feel as though progress stalls once the diagnosis is made. From the clinician perspective, available tools are limited by the current understanding of functional disorders and by the absence of personalized diagnostic markers [6].
Understanding the Limits of the Diagnosis Restores Perspective
Recognizing why an IBS diagnosis does not automatically lead to cure can be grounding rather than discouraging. The diagnosis serves as a framework, not a finish line. It explains why tests are normal and why symptoms are real, but it does not capture the full complexity of the condition [7].
For many patients, this understanding becomes a turning point. It shifts expectations away from a single solution and toward a deeper exploration of contributing factors. The absence of a simple cure does not mean the condition is untreatable. It means that meaningful improvement often requires approaches that go beyond the diagnostic label itself [14].
At this stage, many patients begin looking beyond the diagnostic label and ask a different question. If tests are normal and symptoms persist, what is actually going wrong with digestion. This is where functional and traditional medical systems such as Ayurveda approach IBS differently. Rather than stopping at the diagnosis, they continue the evaluation to understand digestive regulation, individual patterns, and long-term imbalance. A detailed explanation of this approach is covered separately in our in-depth guide on Ayurvedic diagnosis and treatment of IBS: https://panaceayur.com/ibs-ayurvedic-treatment-diagnosis-symptoms-cure/
Ayurvedic Diagnostic Framework
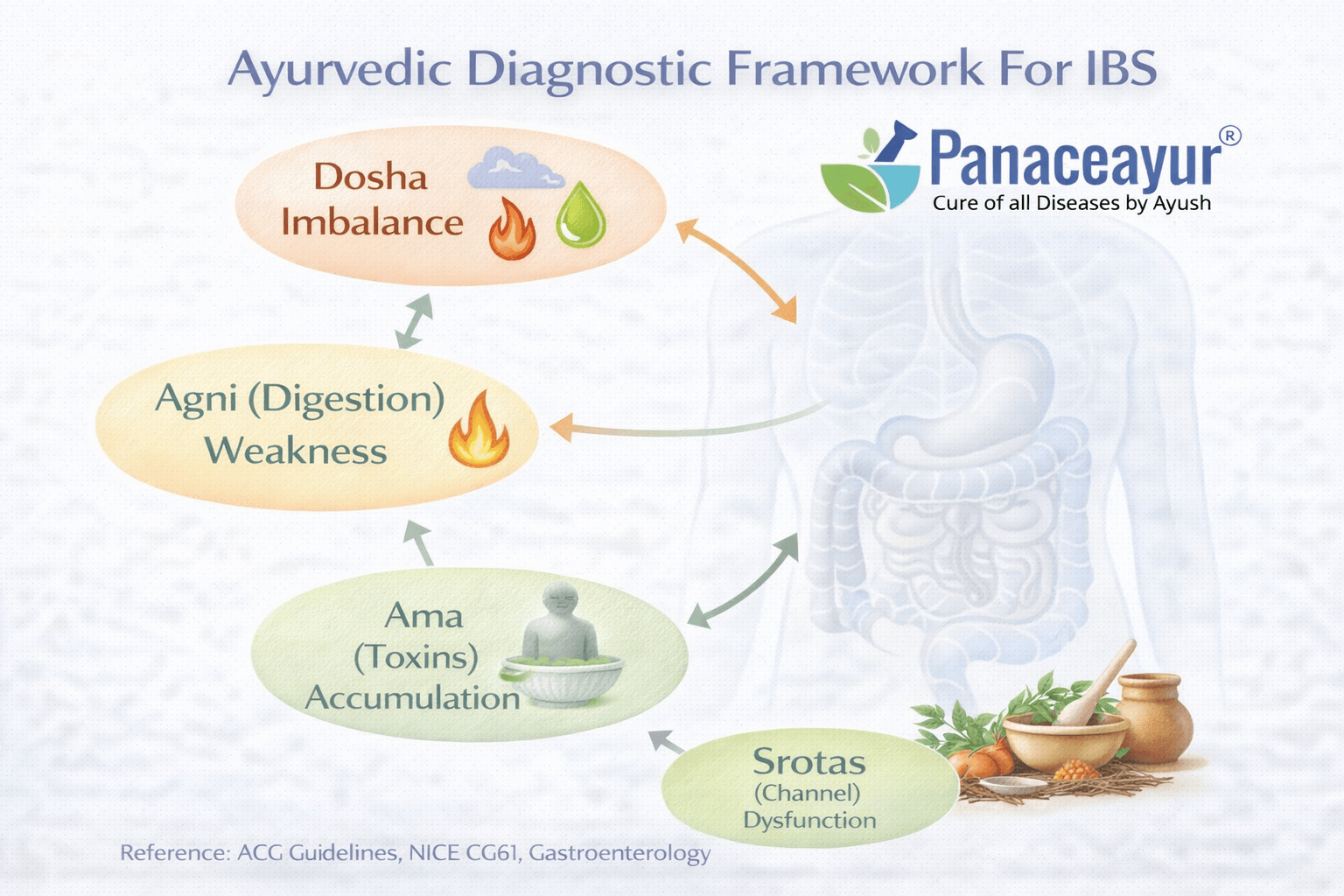
Why Ayurveda Looks Beyond a Single Label
When we approach chronic digestive symptoms through Ayurveda, the first thing we let go of is the idea that one label explains everything. Ayurveda does not diagnose IBS as a single disease entity. Instead, it looks at how digestion is functioning, where it is breaking down, and why the same symptoms appear differently in different people. This approach is described consistently across classical texts, especially in discussions of Grahani and digestive regulation [15], [18].
For patients, this often feels more intuitive. You may notice that certain foods affect you more than others, that stress changes your digestion, or that symptoms fluctuate rather than remain fixed. Ayurveda treats these patterns as meaningful diagnostic clues rather than background noise.
Grahani as the Functional Center of Digestion
In Ayurvedic physiology, Grahani is described as the functional seat of digestion and absorption. It is closely linked with the strength and coordination of digestive processes. When Grahani functions well, digestion is stable and predictable. When it becomes disturbed, symptoms such as alternating bowel habits, bloating, incomplete digestion, and fatigue can appear, closely resembling what modern medicine calls IBS [15], [18].
Rather than asking only what symptoms are present, the Ayurvedic approach asks how digestion behaves day to day. Is it consistent. Does it fluctuate. Does food feel heavy or poorly digested. These observations guide diagnosis at a functional level.
Agni Assessment and Digestive Capacity
Agni refers to digestive and metabolic capacity. Ayurveda places great importance on assessing the quality of Agni rather than assuming digestion is either normal or abnormal. Weak, irregular, or unstable Agni leads to incomplete digestion and symptom variability [15], [17].
From a patient perspective, this often explains experiences that routine tests cannot. You may tolerate a food one day and react badly the next. You may feel hungry but become uncomfortable after eating. These patterns are interpreted as signs of disturbed Agni rather than random symptoms.
Ama and the Burden of Incomplete Digestion
Ama refers to improperly processed metabolic residue that forms when digestion is inefficient. Classical texts describe Ama as contributing to heaviness, bloating, fatigue, mental fog, and irregular bowel movements [15], [18].
For patients who feel unwell despite normal test results, this concept often resonates. Ama does not imply toxins in a dramatic sense. It describes a functional backlog in digestion and metabolism that interferes with normal regulation, even when laboratory markers appear normal.
Dosha Patterns Shape Symptom Expression
Ayurveda further refines diagnosis by assessing Dosha involvement. Some people show patterns associated with Vata imbalance, such as variable stools, gas, dryness, and pain. Others show Pitta related patterns with urgency, burning sensations, or loose stools. Kapha involvement may present with heaviness, sluggish digestion, and mucus [17], [18].
This explains why two people with the same modern diagnosis can experience IBS very differently. Dosha assessment helps personalize understanding rather than forcing all symptoms into one category.
Srotas and Functional Pathways
Srotas are functional channels through which digestion, absorption, and elimination occur. When these pathways become disturbed, symptoms persist even without structural disease. Ayurveda uses Srotas assessment to understand where flow is disrupted, whether at the level of digestion, absorption, or elimination [16], [18].
For patients, this framework offers clarity. It explains why symptoms may not improve with symptom suppression alone and why addressing regulation and flow becomes essential for lasting change.
How This Framework Complements Modern Diagnosis
The Ayurvedic diagnostic framework does not replace modern investigations. It builds on them. Once serious disease has been ruled out, Ayurveda focuses on functional imbalances that modern tests are not designed to detect. This layered approach helps bridge the gap between normal reports and persistent symptoms [15], [16], [17], [18].
For many patients, this perspective restores a sense of logic and agency. Instead of asking why nothing shows up on tests, the question becomes how digestion is functioning and what is interfering with its natural balance.
Gut Mind Axis in Ayurveda and Modern Science
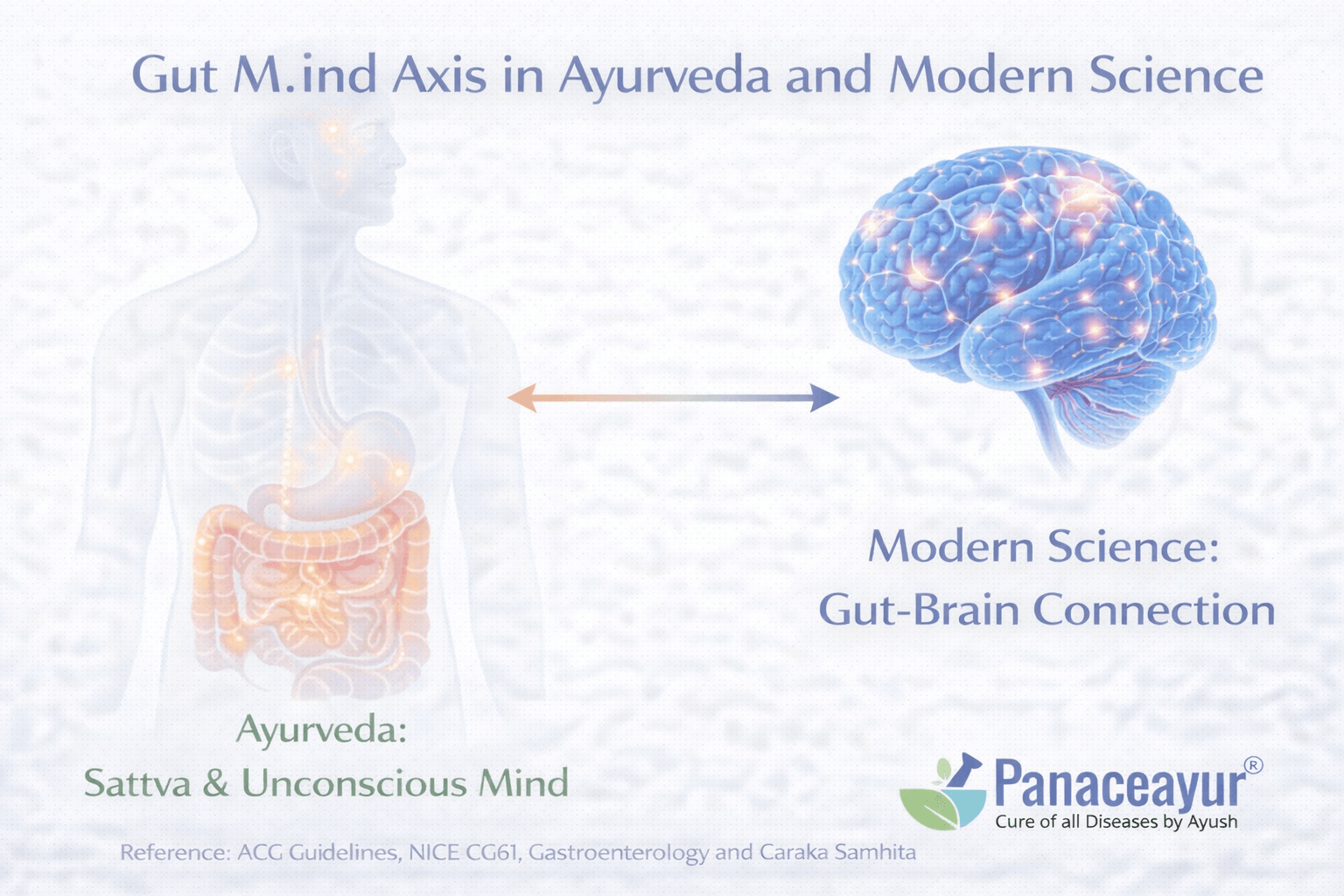
How Modern Medicine Understands the Gut Mind Connection
Modern research has shown that the gut and the brain are in constant communication. This connection is not abstract or philosophical. It is biological. Nerves, immune signals, hormones, and gut microbes continuously exchange information with the brain. When this communication becomes dysregulated, symptoms such as pain, bloating, urgency, and altered bowel habits can emerge, even when the gut appears normal on tests [7].
For patients, this often explains a familiar pattern. Digestive symptoms worsen during periods of stress, illness, poor sleep, or emotional strain. At the same time, symptoms do not simply disappear when stress is reduced. This tells us that stress influences symptoms, but it is not the sole cause.
Why the Gut Can Influence Thoughts and Emotions
The gut contains an extensive network of nerves and produces many of the same chemical messengers used by the brain. Changes in gut signaling can influence mood, anxiety, and cognitive clarity. At the same time, changes in mental state can alter gut motility and sensitivity. This two way relationship is now well established in neuroscience and gastroenterology [19].
Patients often describe feeling mentally foggy, anxious, or emotionally drained when their digestion is disturbed. These experiences are not imagined. They reflect real physiological communication between the gut and the nervous system.
Ayurvedic View of the Gut Mind Relationship
Ayurveda recognized this connection long before modern science could measure it. Classical texts describe digestion and mental state as deeply linked. Disturbances in digestion are said to affect clarity of mind, emotional stability, and overall vitality. Likewise, mental strain and emotional imbalance are described as capable of weakening digestion and disrupting regulation [15].
From an Ayurvedic perspective, digestion is not limited to the stomach or intestines. It is a coordinated process involving the nervous system, metabolism, and mental balance. When this coordination is disturbed, symptoms appear in both the gut and the mind.
Why This Matters for People With IBS
For someone living with IBS, the gut mind axis explains why symptoms feel physical yet unpredictable. It explains why medical tests can be normal while daily life is disrupted. It also explains why purely symptom focused treatments often fall short [7].
Understanding this connection helps shift the narrative. Symptoms are not psychological in origin, but psychological states can influence how strongly they are felt. This distinction is critical for patient trust and for meaningful progress.
Bridging Both Perspectives
When modern science and Ayurveda are viewed together, the gut mind axis becomes clearer rather than more confusing. Modern research provides measurable mechanisms. Ayurveda provides a functional framework that looks at regulation, balance, and individual variation [19].
Post Infectious IBS
How IBS Can Begin After an Infection
For many people, IBS does not develop gradually. It begins after a clear event, most often a gastrointestinal infection such as food poisoning or severe diarrhea. Patients often describe a specific moment in time when digestion never fully returned to normal. Even though the infection resolves and routine tests later appear normal, symptoms such as abdominal pain, urgency, bloating, or altered bowel habits continue [20].
From a medical perspective, this pattern is well recognized. Post infectious IBS is not a rare exception. It is a documented pathway through which IBS can develop, especially after bacterial or viral gastroenteritis.
What Changes After the Infection Clears
When an infection affects the gut, it does more than cause short term illness. Research shows that inflammation during infection can alter gut nerve sensitivity, immune signaling, and bowel movement patterns. In some people, these changes do not fully reset even after the infection is gone [11].
For patients, this explains a common frustration. You may be told that the infection has cleared and that tests are normal, yet your digestion feels permanently different. The symptoms are not lingering infection. They reflect functional changes left behind in the gut.
Why Tests Become Normal but Symptoms Persist
Standard medical tests are designed to detect ongoing infection, inflammation, or structural damage. In post infectious IBS, these markers often normalize. What remains is altered regulation. The gut may become more sensitive to stretch, food, or stress. Bowel movements may speed up or slow down unpredictably. These changes are real but invisible to routine investigations [11].
This is why many patients feel confused. They know something changed after the illness, but no test seems to capture it.
Why Post Infectious IBS Is Often Overlooked
In clinical practice, the link between a past infection and current symptoms is sometimes missed, especially if months have passed. Symptoms may be grouped under general IBS without acknowledging the trigger. For patients, this can feel like an important part of their story has been ignored [20].
Recognizing post infectious IBS helps validate patient experience. It acknowledges that a physical event initiated the condition rather than implying that symptoms appeared without cause.
What This Understanding Offers Patients
Understanding post infectious IBS often brings relief. It provides a logical explanation for why symptoms began, why tests later appeared normal, and why the condition behaves differently from other digestive problems. It also helps set realistic expectations. Recovery may take time because the gut is relearning normal regulation rather than healing visible damage [11].
Gender, Hormonal, and Lifecycle Influence
Why IBS Affects Women More Often Than Men
IBS is diagnosed more frequently in women than in men, and this difference is not accidental. Research shows that biological sex influences how the gut responds to pain, stress, and hormonal signaling. Women tend to report more severe abdominal pain, bloating, and bowel irregularity, while men more often report diarrhea dominant patterns with less pain sensitivity [21].
For many patients, this explains why their experience of IBS does not match someone else’s, even when the diagnosis is the same. Gender shapes symptom expression in ways that routine tests do not capture.
Role of Hormones in Symptom Fluctuation
Hormonal changes play a significant role in IBS symptoms, especially in women. Estrogen and progesterone influence gut motility, pain sensitivity, and fluid balance in the intestines. As hormone levels rise and fall during the menstrual cycle, many women notice predictable changes in bowel habits and pain intensity [21].
Patients often report worsening symptoms before or during menstruation, followed by partial relief afterward. These patterns are consistent and biologically grounded, not coincidental.
Stress Hormones and Symptom Amplification
Beyond reproductive hormones, stress related hormones also influence IBS. Cortisol and other stress mediators can alter gut motility and sensitivity through the gut mind axis. While stress does not cause IBS on its own, it can significantly amplify existing symptoms and prolong flare ups [22].
This explains why symptoms may worsen during periods of emotional strain, illness, disrupted sleep, or major life transitions. The gut responds to the body’s overall stress state, not just to food or infection.
IBS Across Different Life Stages
IBS does not remain static across the lifespan. Symptoms may change during puberty, pregnancy, postpartum periods, and menopause. Some women notice improvement during pregnancy, while others experience worsening symptoms. Menopause can also alter symptom patterns due to shifts in hormone levels and nervous system regulation [21].
For patients, this variability can feel confusing. A treatment that once worked may stop helping, not because the diagnosis is wrong, but because the body’s internal environment has changed.
Why Lifecycle Context Matters in Understanding IBS
When gender and lifecycle influences are ignored, IBS can feel unpredictable and frustrating. When they are acknowledged, symptom patterns begin to make sense. Hormones and stress biology do not replace other mechanisms of IBS, but they interact with them, shaping how symptoms are felt and expressed [22].
Medication Induced IBS Patterns
How Medications Can Trigger or Worsen IBS Symptoms
Many people notice that their digestive symptoms began or changed after starting certain medications. This connection is often overlooked, yet it is well documented in research. Some drugs alter gut motility, affect the intestinal lining, or change how gut bacteria behave. In susceptible individuals, these changes can trigger IBS like symptoms or worsen an existing pattern [23].
From a patient perspective, this can be confusing. The medication may have been prescribed for a completely different reason, such as acid reflux, pain, or infection. When digestive symptoms appear afterward, the link is not always immediately recognized.
Proton Pump Inhibitors and Gut Microbiome Changes
Proton pump inhibitors, commonly used to reduce stomach acid, are among the most frequently implicated medications. While they are effective for acid related conditions, long term use can alter the gut microbiome by changing the natural acid barrier of the stomach. This allows different bacteria to survive and move further into the digestive tract [24].
For some people, these changes are associated with bloating, gas, altered bowel habits, and increased gut sensitivity. When these symptoms persist, they are often labeled as IBS without recognizing the medication related trigger.
Antibiotics and Lasting Functional Changes
Antibiotics are another major contributor. They are essential for treating infections, but they also disrupt the balance of gut bacteria. In many individuals, the microbiome recovers over time. In others, especially after repeated courses, gut regulation does not fully normalize [23].
Patients often describe a pattern where digestion was stable until a course of antibiotics, after which symptoms became chronic. Tests later appear normal, yet bowel habits and sensitivity remain altered.
Pain Relievers and Gut Sensitivity
Certain pain medications, including nonsteroidal anti inflammatory drugs, can irritate the gut lining and affect intestinal permeability. Over time, this may contribute to increased sensitivity and discomfort, even in the absence of visible inflammation [23].
For patients who rely on these medications for chronic pain, digestive symptoms may be attributed to IBS without considering the ongoing influence of the drug itself.
Integrative Diagnosis Using Modern Medicine and Ayurveda
Why One Framework Alone Is Often Not Enough
Modern medicine and Ayurveda approach diagnosis from different angles, and this difference becomes especially important in conditions like IBS. Modern gastroenterology excels at identifying structural disease, inflammation, infection, and malignancy. When these are ruled out, IBS can be diagnosed with confidence using symptom based frameworks [1]. However, many patients find that this diagnosis still does not explain why symptoms behave the way they do or why improvement remains limited.
Ayurveda approaches the same situation differently. Once dangerous disease is excluded, the focus shifts from naming the condition to understanding how digestion is functioning in that individual. Rather than stopping at a label, Ayurveda continues the diagnostic process by examining patterns, triggers, and regulatory imbalance [15].
How Modern Diagnosis Establishes Safety
From a patient perspective, modern diagnostic testing provides reassurance. Blood tests, stool studies, and imaging confirm that there is no progressive or life threatening disease. This foundation is essential. Without it, any further interpretation would be unsafe or speculative [1].
At the same time, modern diagnostic categories like IBS are intentionally broad. They describe a collection of symptoms rather than a single cause. This is why two people can receive the same diagnosis and yet respond very differently to the same treatment [6].
How Ayurveda Explains What Tests Cannot Show
Once safety is established, Ayurveda fills an important gap. It evaluates digestion at a functional level by assessing Agni, Grahani, Dosha patterns, and how the body processes and responds to food and stress. These assessments are not designed to replace modern tests. They are designed to explain ongoing dysfunction when tests are normal [15], [17].
For patients, this often feels like the missing piece. Instead of being told that nothing is wrong, the conversation shifts to how digestion is behaving and why it has become unstable.
Bringing Both Approaches Together
An integrative diagnostic approach respects the strengths and limits of both systems. Modern medicine defines what IBS is and ensures nothing dangerous is overlooked. Ayurveda explores why symptoms persist, fluctuate, or resist standard treatment [6], [15].
This combination allows diagnosis to become a process rather than a conclusion. It acknowledges that normal tests do not equal normal function and that understanding regulation is just as important as ruling out disease.
What Integrative Diagnosis Offers Patients
For many patients, integrative diagnosis restores confidence and clarity. It validates symptoms through modern science while providing a functional explanation through Ayurveda. Instead of choosing between systems, patients benefit from using each where it performs best [1], [17].
FAQs
How is IBS diagnosed?
IBS is diagnosed using symptom-based criteria after ruling out serious digestive diseases. Blood tests, stool tests, and colonoscopy are used to exclude other conditions, not to confirm IBS directly.
Why are IBS test results often normal?
IBS does not cause visible damage or inflammation in the bowel. Standard tests are designed to detect disease, not functional changes in gut regulation or nerve sensitivity.
Is IBS a real medical condition?
Yes. IBS is a recognized functional gastrointestinal disorder defined by international diagnostic criteria and supported by extensive clinical research.
Can IBS be misdiagnosed?
Yes. Conditions such as bile acid malabsorption, small intestinal bacterial overgrowth, and microscopic colitis can produce similar symptoms and may require reassessment.
Is IBS caused by stress or anxiety?
Stress can worsen IBS symptoms but does not cause IBS. Research shows IBS involves altered gut–brain communication and biological regulation, not psychological imagination.
Why does IBS diagnosis not lead to a cure?
IBS describes a symptom pattern rather than a single cause. Different patients have different underlying mechanisms, which is why treatment often improves symptoms without fully resolving them.
How is IBS diagnosed in the UK?
In the UK, IBS is diagnosed using symptom criteria once serious conditions are excluded. NHS guidelines recommend limited testing and avoiding unnecessary investigations when symptoms fit IBS patterns.
Why does the NHS not do many tests for IBS?
NHS tests are used to rule out conditions such as inflammatory bowel disease or cancer. IBS does not cause structural damage, so additional testing is not usually helpful.
Is IBS recognised by the NHS as a medical condition?
Yes. IBS is recognised by the NHS as a functional bowel disorder and is managed using established clinical guidelines.
When should IBS be re-evaluated?
Re-evaluation is advised if symptoms change, worsen, or if warning signs such as weight loss, anemia, or bleeding appear.
Is IBS related to stress or mental health?
Stress can influence symptoms, but IBS is not considered a mental health condition. It involves altered gut function and gut–brain signaling.
Why does IBS treatment often focus on symptom control?
IBS does not have a single identifiable cause. NHS management focuses on improving quality of life rather than curing a specific disease.
How do gastroenterologists diagnose IBS in the USA?
In the USA, IBS is diagnosed using Rome IV symptom criteria after excluding alarm features. ACG guidelines recommend a positive diagnosis rather than extensive testing.
Why do colonoscopy and blood tests appear normal in IBS?
IBS is a functional disorder that does not produce inflammation or structural abnormalities detectable by routine tests.
Is IBS considered a legitimate diagnosis in gastroenterology?
Yes. IBS is a well-defined disorder supported by American College of Gastroenterology guidelines and clinical research.
What conditions are commonly confused with IBS?
Conditions such as bile acid diarrhea, small intestinal bacterial overgrowth, and microscopic colitis may overlap with IBS symptoms.
Is IBS a psychological disorder?
No. IBS involves altered gut–brain communication, immune signaling, and nerve sensitivity. Psychological stress may worsen symptoms but is not the cause.
Why does IBS management not lead to a cure?
IBS represents multiple biological mechanisms rather than a single disease, which limits the effectiveness of one-size-fits-all treatments.
References
[1] Lacy et al., American College of Gastroenterology IBS Guideline
This guideline shows how IBS is officially diagnosed and managed by gastroenterologists in the USA. It explains why IBS is diagnosed using symptom patterns rather than scans or blood tests, and why most treatments focus on symptom control instead of identifying deeper causes.
For patients, this confirms that IBS is a recognized medical condition, even when reports are normal, but also highlights the limits of current medical tools.
Lacy, B. E., Pimentel, M., Brenner, D. M., et al. (2021). ACG clinical guideline: Management of irritable bowel syndrome. American Journal of Gastroenterology, 116(1), 17–44.
https://doi.org/10.14309/ajg.0000000000001036
[2] Ford et al., New England Journal of Medicine – IBS Overview
This article from one of the world’s most trusted medical journals explains IBS as a disorder of gut regulation rather than visible disease. It validates why pain, bloating, and bowel changes can be severe even when tests are normal.
Patients often feel reassured reading this because it confirms that symptoms are real and biological, not imagined.
Ford, A. C., Lacy, B. E., & Talley, N. J. (2017). Irritable bowel syndrome. New England Journal of Medicine, 376(26), 2566–2578.
https://doi.org/10.1056/NEJMra1607547
[3] Drossman, Functional GI Disorders and Rome IV Logic
This paper explains why IBS is classified using symptom criteria instead of biological markers. It clarifies that Rome IV was created to standardize diagnosis for research, not to find root causes or cures.
Patients understand why IBS diagnosis often feels like a label rather than a solution.
Drossman, D. A. (2016). Functional gastrointestinal disorders: History, pathophysiology, clinical features, and Rome IV. Gastroenterology, 150(6), 1262–1279.
https://doi.org/10.1053/j.gastro.2016.02.032
[4] Rome IV Bowel Disorder Classification
This paper formally defines IBS and related bowel disorders. It shows that IBS diagnosis is based on symptom patterns rather than inflammation, infection, or damage.
For patients, this explains why no single test can “prove” IBS.
Mearin, F., Lacy, B. E., Chang, L., et al. (2016). Bowel disorders. Gastroenterology, 150(6), 1393–1407.
https://doi.org/10.1053/j.gastro.2016.02.031
[5] NICE Guideline – IBS Diagnosis in the UK (NHS)
This guideline reflects how IBS is diagnosed and managed within the NHS. It explains why doctors stop testing once serious disease is excluded and focus on reassurance and symptom management.
UK patients often recognize their own clinical experience in this document.
National Institute for Health and Care Excellence. (2017). Irritable bowel syndrome in adults: Diagnosis and management (CG61).
https://www.nice.org.uk/guidance/cg61
[6] Talley & Ford – Is IBS One Disease or Many?
This paper questions whether IBS is a single condition or multiple overlapping disorders. It supports the idea that different patients have different mechanisms behind the same diagnosis.
Patients realize why one IBS treatment rarely works for everyone.
Talley, N. J., & Ford, A. C. (2015). Functional dyspepsia and irritable bowel syndrome: One disease or two? American Journal of Gastroenterology, 110(1), 1–3.
https://doi.org/10.1038/ajg.2014.381
[7] Mayer et al., Gut–Brain Axis
This landmark research shows that IBS symptoms arise from altered communication between the gut, nerves, immune system, and brain. It proves IBS is neurobiological, not psychological.
This study removes stigma and self-blame for patients.
Mayer, E. A., Tillisch, K., & Gupta, A. (2015). Gut/brain axis and the microbiota. Journal of Clinical Investigation, 125(3), 926–938.
https://doi.org/10.1172/JCI76304
[8] Spiller & Garsed – Post-Infectious IBS
This paper explains why IBS often begins after food poisoning or gut infection and why symptoms persist even after infection clears.
Patients who say “I was never the same after that illness” often feel understood for the first time.
Spiller, R., & Garsed, K. (2009). Postinfectious irritable bowel syndrome. Gastroenterology, 136(6), 1979–1988.
https://doi.org/10.1053/j.gastro.2009.02.074
[9] Camilleri – Bile Acid Malabsorption
This study shows how bile acid imbalance can cause chronic diarrhea and urgency but is often misdiagnosed as IBS.
Patients learn that persistent diarrhea does not always mean “nothing can be done.”
Camilleri, M. (2015). Bile acid diarrhea: Prevalence, pathogenesis, and therapy. Gut and Liver, 9(3), 332–339.
https://doi.org/10.5009/gnl14397
[10] Pimentel et al., SIBO Guidelines
This guideline explains the limits of breath testing and why repeated antibiotic treatment often fails or causes relapse.
Patients understand why temporary improvement is common but lasting relief is rare.
Pimentel, M., Saad, R. J., Long, M. D., & Rao, S. S. C. (2020). ACG clinical guideline: Small intestinal bacterial overgrowth. American Journal of Gastroenterology, 115(2), 165–178.
https://doi.org/10.14309/ajg.0000000000000501
[11] AGA Review – Chronic Diarrhea
This review shows how many causes of chronic diarrhea are overlooked when IBS is diagnosed too early.
It supports careful reassessment rather than lifelong labeling.
Fine, K. D., & Schiller, L. R. (1999). AGA technical review on chronic diarrhea. Gastroenterology, 116(6), 1464–1486.
https://doi.org/10.1016/S0016-5085(99)70511-X
[12] Microscopic Colitis
This paper explains a condition that causes IBS-like symptoms but requires biopsy to diagnose, even when colonoscopy looks normal.
Patients finally understand why symptoms persisted despite “normal” findings.
Pardi, D. S., & Kelly, C. P. (2011). Microscopic colitis. Gastroenterology, 140(4), 1155–1165.
https://doi.org/10.1053/j.gastro.2011.02.004
[13] ACG IBS Monograph – Red Flags
This document explains when IBS should be reconsidered and outlines warning signs that need further investigation.
It reassures patients that re-evaluation is medically appropriate.
Ford, A. C., et al. (2018). ACG monograph on IBS. American Journal of Gastroenterology, 113(Suppl 2), 1–18.
https://doi.org/10.1038/s41395-018-0084-x
[14] Global Burden of IBS
This study shows IBS affects hundreds of millions worldwide and significantly impacts quality of life.
Patients realize they are not alone and their condition is taken seriously globally.
Black, C. J., & Ford, A. C. (2020). Global burden of IBS. Lancet Gastroenterology & Hepatology, 5(10), 908–917.
https://doi.org/10.1016/S2468-1253(20)30223-5
Ayurvedic Classical References
[15] Charaka Samhita – Grahani Chikitsa
This classical text describes chronic digestive disorders caused by weak digestion, food sensitivity, alternating stools, and fatigue — symptoms that closely match IBS.
It shows that functional digestive disorders were recognized thousands of years ago.
Sharma, R. K., & Dash, B. (2001). Charaka Samhita, Chikitsa Sthana, Chapter 15. Chaukhambha.
[16] Sushruta Samhita – Digestive Dysfunction
This text explains how illness, medications, and stress weaken digestion long-term, paralleling modern post-infectious IBS concepts.
Sharma, P. V. (2014). Sushruta Samhita, Uttara Tantra. Chaukhambha.
[17] Ashtanga Hridaya – Atisara and Grahani
This text categorizes diarrhea and constipation based on functional imbalance rather than infection or structural disease.
Tripathi, B. (2017). Ashtanga Hridaya, Nidana Sthana, Chapter 8. Chaukhambha.
[18] Bhavaprakasha – Grahani Disorders
This text emphasizes individualized diagnosis and explains why one-size-fits-all treatment fails in chronic digestive disorders.
Bhavamishra. (2015). Bhavaprakasha, Madhyama Khanda. Chaukhambha.
[19] Cryan & Dinan – Gut Microbiota and Brain
This study shows how gut bacteria influence mood, stress response, and gut sensitivity, supporting IBS as a neuroimmune condition.
Cryan, J. F., & Dinan, T. G. (2012). Nature Reviews Neuroscience, 13(10), 701–712.
https://doi.org/10.1038/nrn3346
[20] Thabane et al., Meta-analysis on Post-Infectious IBS
This meta-analysis quantifies how often IBS develops after infection, validating patient experiences.
Thabane, M., et al. (2007). Alimentary Pharmacology & Therapeutics, 26(4), 535–544.
https://doi.org/10.1111/j.1365-2036.2007.03399.x
[21] Menstrual Cycle and IBS Symptoms
This study explains why IBS symptoms fluctuate with hormonal changes and why IBS is more common in women.
Heitkemper, M. M., & Jarrett, M. E. (2008). Gastroenterology, 134(2), 382–391.
https://doi.org/10.1053/j.gastro.2007.10.041
[22] Stress Modulation in IBS
This paper explains stress as a symptom amplifier, not the root cause, preventing dismissive psychosomatic labeling.
Chang, L. (2011). American Journal of Gastroenterology, 106(1), 1–7.
https://doi.org/10.1038/ajg.2010.347
[23] Gut Barrier Dysfunction in Functional GI Disorders
This study explains increased gut permeability in IBS, validating inflammation-like symptoms despite normal tests.
Boursier, J., & Diehl, A. M. (2015). Gastroenterology Clinics of North America, 44(1), 47–57.
https://doi.org/10.1016/j.gtc.2014.11.003
[24] Proton Pump Inhibitors and Microbiome Changes
This study shows how long-term acid-suppressing drugs alter gut microbiota and worsen functional symptoms.
Jackson, M. A., et al. (2018). Gut, 67(6), 986–995.
https://doi.org/10.1136/gutjnl-2017-315193
Final Note for Readers
Every reference above is included to help you understand why IBS behaves the way it does, not to overwhelm you.
You do not need to read all of them, they exist so you can verify, explore, and build trust.