- Modern Medical Overview
- Ayurvedic Perspective – Grahani Roga
- Diagnosis
- Symptoms of IBS and Grahani Roga
- Diseases and Conditions Commonly Associated With IBS
- Additional Conditions That Can Worsen IBS
- Modern Management and Limitations
- Ayurvedic Treatment Protocol for IBS (Grahani Roga)
- Dadimadi Avaleha (Main Medicine)
- Important Medical Warning and Mandatory Patient Advisory
- Why market bought IBS medicines fail in real clinical practice
- Critical Instruction
- Frequently Asked Questions (FAQs)
- References
IBS Ayurvedic treatment offers a comprehensive, root-cause-based approach to digestive restoration. Ayurveda identifies IBS as Grahani Roga, a condition caused by weakened Agni (digestive fire) and toxin accumulation (Ama). By focusing on detoxification, diet regulation, and Rasayana rejuvenation, this holistic therapy aims for complete gut healing rather than mere symptom control.According to the World Health Organization (WHO) and Mayo Clinic, IBS affects an estimated 10–15% of the global population, with a higher prevalence among women and individuals aged 20–45 years [41]. Despite being classified as a “functional bowel disorder,” its impact extends far beyond digestion affecting emotional health, hormonal balance, and immunity. Modern medicine recognizes IBS as a condition marked by abdominal pain, bloating, altered bowel habits, and intestinal hypersensitivity [42], but it often fails to explain why the condition persists even after dietary correction and medication.
Hidden Epidemic:-The Underdiagnosed and Mislabelled Disorder
IBS remains a hidden epidemic due to its overlapping symptoms with multiple digestive and endocrine conditions. Many patients are either underdiagnosed or dismissed with psychosomatic labels such as “stress-related bowel disorder.” This misclassification stems from the absence of visible inflammation or structural changes in conventional tests, leading clinicians to underestimate the chronic, systemic nature of IBS.
Globally, millions of patients live with recurring bloating, alternating constipation and diarrhea, fatigue, and anxiety, yet fail to find lasting relief. Studies reveal that nearly 40% of IBS patients are misdiagnosed for over three years before receiving accurate care [43]. The emotional toll, social embarrassment, and occupational productivity loss make IBS not just a digestive illness but a multisystem disorder demanding interdisciplinary attention.
Socioeconomic Burden and Quality-of-Life Impact
IBS contributes significantly to the global health burden. In the United States alone, it accounts for over 3 million outpatient visits annually and billions in healthcare costs, not including lost workdays and reduced quality of life [44]. Patients with IBS experience anxiety, depression, and chronic fatigue more commonly than those with structural gastrointestinal diseases. The unpredictable bowel patterns and dependence on emergency access to restrooms create constant psychological stress, reinforcing the gut–brain–hormone loop [45].
Beyond economics, the psychosocial cost is severe—relationships, self-esteem, and career progress often suffer. This reinforces the Ayurvedic understanding that gut health is central to mental stability and Ojas (vitality) [46]. Thus, IBS is not only a medical condition but also a societal wellness issue, requiring both physiological and psychological restoration.
Ayurvedic Identification- Grahani Roga as the Classical Equivalent
Ayurveda describes a condition strikingly similar to IBS, known as Grahani Roga. The term Grahani refers to the duodenum and small intestine, the seat of Agni (digestive fire), which governs digestion and assimilation. Roga denotes disease or derangement. When Agni becomes impaired, the body fails to properly digest food, leading to Ama (toxic residue) accumulation and irregular bowel function [47].
According to Charaka Samhita (Chikitsa Sthana 15/44–47), Grahani arises when improper food habits, stress, or suppression of natural urges disturb Agni, resulting in alternating constipation, loose stools, bloating, and weakness — identical to IBS symptoms [48]. Sushruta Samhita (Uttara Tantra 40/167–171) adds that mental agitation (Chinta, Bhaya, Shoka) directly weakens Agni and Grahani, producing intestinal irregularities [49].
In Ayurvedic philosophy, digestion is not mechanical but psychophysiological, influenced by both Dosha balance and mental state (Manasika Bhava). Therefore, IBS is viewed as a Grahani disorder rooted in Agni Dushti and Manovaha Srotas imbalance, integrating mind, hormones, and gut function centuries before modern science identified the gut–brain axis [50].
Historical Background- References from Classical Ayurvedic Texts
- Charaka Samhita (Chikitsa Sthana 15) emphasizes Agni as the core of health, stating that all diseases arise from its impairment [51].
- Sushruta Samhita (Sutra Sthana 46) connects digestive dysfunctions to Vata–Pitta imbalance and emotional factors [52].
- Ashtanga Hridaya (Chikitsa Sthana 10) elaborates on Grahani Roga, classifying it based on Dosha predominance (Vataja, Pittaja, Kaphaja, Sannipataja), mirroring modern IBS subtypes (IBS-C, IBS-D, IBS-M) [53].
- Bhavaprakasha Nighantu (Madhyama Khanda 3/180–190) identifies chronic Grahani as resulting from Mandagni and Majja Dhatu Kshaya, conceptually linking it to neuroendocrine depletion [54].
These classical sources confirm that Ayurveda perceived IBS not as a localized bowel problem but as a systemic imbalance involving digestion, mind, and hormonal vitality [55].
Need for Integrative Care Across Gastroenterology and Endocrinology
Modern gastroenterology focuses on motility, microbiota, and visceral sensitivity, while endocrinology investigates hormonal modulation through the hypothalamic pituitary adrenal (HPA) axis [56]. In reality, IBS sits at the intersection of both systems. Stress elevates cortisol, disturbs insulin and thyroid hormones, and disrupts intestinal rhythm creating a feedback cycle that perpetuates symptoms [57].
Ayurveda anticipated this holistic interconnection through its doctrines of Agni, Ojas, and Srotas. The digestive fire (Agni) aligns with metabolic and endocrine activity; Ojas corresponds to neurohormonal resilience; and Srotas reflect biological channels equivalent to the body’s circulatory and glandular networks [58].
Therefore, IBS management must transcend symptomatic relief. True healing demands restoring Agni and Ojas, calming Vata–Pitta, and balancing the gut–brain–hormone triad [59]. This integrative model bridging Gastroenterology, Endocrinology, and Ayurveda provides the missing link for achieving a permanent cure rather than lifelong management [60].
Modern Medical Overview
2.1 Pathophysiology
Irritable Bowel Syndrome (IBS) is a complex functional disorder involving disruption of the gut–brain–microbiota axis. It reflects continuous interaction between the enteric nervous system, gut microbiota, immune signaling, and neuroendocrine regulation [44].
Alteration in gut–brain signaling is central to IBS. This bidirectional pathway, mediated by vagus and enteric nerves along with hormonal feedback, becomes disturbed by chronic stress or microbial imbalance, resulting in visceral hypersensitivity and irregular motility even in the absence of structural disease [45].
Many studies demonstrate that patients with IBS experience exaggerated visceral pain perception. This hypersensitivity arises from increased excitability of afferent pathways and altered serotonin modulation within the enteric system [50].
Imbalance in intestinal microbiota is a key pathological driver. Post-infectious dysbiosis, antibiotic overuse, and dietary changes alter short-chain fatty acid production, mucosal integrity, and immune tone [64]. This leads to mild inflammation, permeability increase, and persistent cytokine activation [66].
Serotonin (5-hydroxytryptamine) plays a pivotal role, governing nearly 90 percent of intestinal motility and secretion. Dysregulation of 5-HT3 and 5-HT4 receptor activity results in irregular transit and pain. Modern agents like alosetron and tegaserod were developed from these insights [65].
Post-infectious IBS is another subset in which transient bacterial or viral gastroenteritis alters mucosal immune pathways. Even after recovery, residual cytokines such as IL-6 and TNF-α continue to disturb enteric nerve function [66].
Recent evidence supports an intricate microbiota–immune–endocrine relationship. Gut microbes modulate cortisol and serotonin synthesis, influencing both gastrointestinal and psychological symptoms [67]. This confirms that IBS involves neuroendocrine and inflammatory dimensions rather than being purely psychosomatic [56].
2.2 Classification (Rome IV Criteria)
The Rome IV criteria represent the international clinical standard for diagnosing IBS [68]. IBS is defined as recurrent abdominal pain at least one day per week during the last three months, associated with two or more of the following: pain related to defecation, change in stool frequency, or change in stool form.
According to stool pattern analysis (Bristol Stool Scale), IBS is classified into four groups:
- IBS-C (constipation predominant)
- IBS-D (diarrhea predominant)
- IBS-M (mixed pattern)
- IBS-U (unclassified)
The criteria emphasize a positive diagnosis rather than an exclusion-based one, which shortens delay and enhances clinical management [69].
2.3 Hormonal and Endocrine Involvement
Hormonal influences explain why IBS frequently overlaps with endocrine disorders [70].
Thyroid abnormalities directly affect motility: hypothyroidism produces constipation, while hyperthyroidism accelerates transit leading to diarrhea [72].
Chronic stress overstimulates the hypothalamic–pituitary–adrenal (HPA) axis, leading to excessive cortisol secretion. This disrupts mucosal immunity, serotonin synthesis, and epithelial integrity [71].
Fluctuating estrogen and progesterone levels alter intestinal smooth muscle tone and neurotransmitter sensitivity. This is why women often report worsening symptoms during menstruation or menopause [74].
Gut peptides such as motilin, ghrelin, GLP-1, and peptide-YY coordinate gastric emptying and colonic movement, while also interacting with the microbiome to modulate inflammation [75].
Insulin and glucagon indirectly affect the gut through their influence on energy metabolism and microbial diversity. Insulin resistance heightens visceral sensitivity and links metabolic disorders with IBS [76].
These findings position IBS as a neuroendocrine–metabolic condition—a modern reflection of the Ayurvedic view that Agni (digestive fire) and Ojas (vital essence) maintain systemic harmony [46].
2.4 Modern Diagnosis
Diagnosis of IBS is mainly clinical, but several investigations support differential identification. The goal is to rule out organic diseases such as inflammatory bowel disease, celiac disease, or cancer [78].
- Colonoscopy: confirms the absence of inflammatory or neoplastic changes [79].
- Stool calprotectin: differentiates IBS from inflammatory bowel disorders; normal values confirm non-inflammatory nature [80].
- Thyroid profile (TSH, T3, T4): evaluates endocrine contributions to altered motility [81].
- Lactulose or glucose breath tests: detect small intestinal bacterial overgrowth, a common comorbidity [82].
- Hormonal evaluation: includes cortisol, insulin, estrogen, and leptin for neuroendocrine assessment [83].
- Psychological scales: Hospital Anxiety and Depression Scale (HADS) and IBS-QOL quantify emotional burden [84].
Together, these tools confirm that IBS is a multisystemic disorder encompassing the digestive, immune, and endocrine axes, which parallels the Ayurvedic doctrine of Grahani involving Agni Dushti and Manovaha Srotas imbalance [55].
Ayurvedic Perspective – Grahani Roga
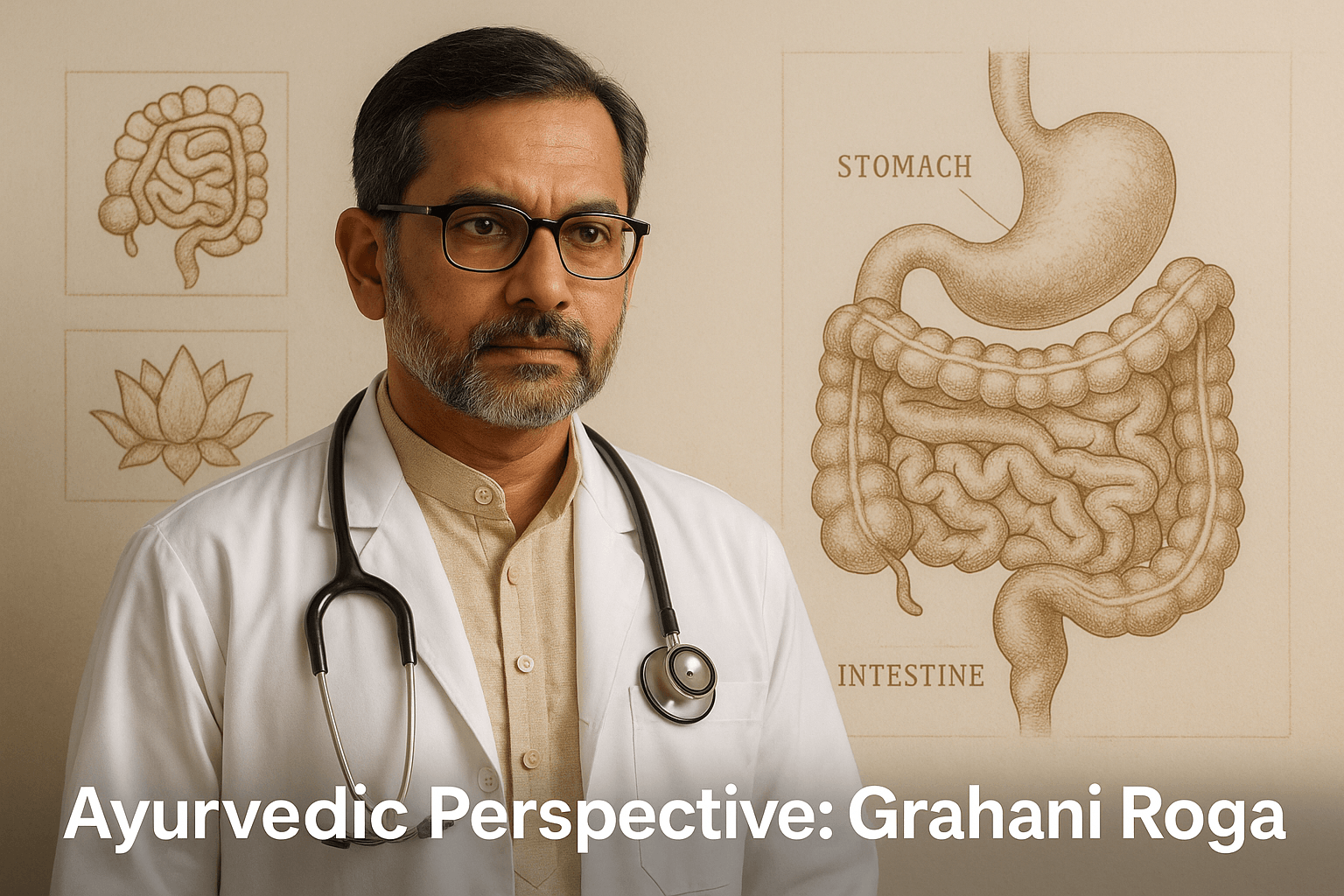
3.1 Classical Definition
Ayurveda recognizes Grahani Roga as the direct manifestation of impaired Agni (digestive fire). The Charaka Samhita (Chikitsa Sthana 15/44–47) states, “Grahani is the seat of Agni; when Agni becomes vitiated, Grahani becomes weak leading to irregular digestion.” This verse highlights that the intestine’s strength entirely depends on the functional capacity of Agni, which governs transformation, assimilation, and stability [47].
Bhavaprakasha Madhyama Khanda (3/180–190) expands this understanding by linking chronic digestive weakness with disturbances of the mind, emphasizing that Manasika Bhava (emotional factors like fear, stress, and grief) directly alter Agni and intestinal rhythm [54]. Hence, Grahani is not merely a digestive condition but a psychosomatic and metabolic imbalance affecting Rasa Dhatu and Majja Dhatu over time [46].
3.2 Nidana (Causes)
The root causes (Nidana) of Grahani Roga as described by Charaka, Sushruta, and Vagbhata correspond closely to modern triggers of IBS. These include:
- Irregular eating patterns: Skipping meals or eating at inconsistent times impairs Agni and disrupts gastric rhythm [48].
- Excessive fasting or overeating: Either extreme destabilizes Vata and Pitta, leading to erratic digestion [52].
- Consumption of incompatible foods (Viruddha Ahara): Combining milk with fish, fruit with yogurt, or honey with hot drinks produces Ama (toxins) [51].
- Mental stress, fear, or grief (Chinta, Bhaya, Shoka): These disturb Prana Vata and weaken the digestive fire, aligning with modern understanding of the gut–brain axis [49].
- Night vigil (Ratri Jagarana): Disturbs the circadian rhythm, reducing Agni efficiency and causing sluggish digestion [53].
Ayurvedic scholars note that when these habits persist, the Annavaha Srotas (channels of food transport) become obstructed, producing chronic indigestion, bloating, and irregular bowel movement [55].
3.3 Samprapti (Pathogenesis)
The pathogenesis (Samprapti) of Grahani Roga follows a clear sequence:
- Agni Mandya (impaired digestive fire) occurs first, often due to Ahara (dietary) and Manasika (psychological) factors.
- This leads to Ama formation, or incomplete metabolic residue, which circulates through Rasa Dhatu and causes inflammation [47].
- The accumulated Ama vitiates Vata and Pitta, causing irregular peristalsis and altered secretions.
- As disease progresses, deeper tissues such as Rasa Dhatu (plasma), Majja Dhatu (nervous tissue), and eventually Ojas (vital essence) are affected, resulting in systemic fatigue and psychological instability [54].
- Srotorodha (blockage) occurs in Annavaha and Manovaha Srotas, obstructing nutrient flow and neurotransmitter coordination.
Thus, Grahani Roga develops from a localized digestive weakness into a multisystem disorder involving both the enteric and neuroendocrine networks [46].
3.4 Types of Grahani
Classical texts categorize Grahani based on Dosha predominance, which closely parallels the modern subtypes of IBS:
- Vataja Grahani: Characterized by irregular, painful, and hard stools, abdominal distension, and dryness, similar to constipation-predominant IBS (IBS-C). This arises from erratic Agni and excess Vata in the colon [48].
- Pittaja Grahani: Involves burning sensation, frequent loose stools, and sour belching, analogous to diarrhea-predominant IBS (IBS-D). Caused by Pitta aggravation leading to hypermotility and acidity [52].
- Kaphaja Grahani: Presents with mucus-laden stools, heaviness, lethargy, and poor appetite, corresponding to mixed-type IBS (IBS-M). Dominated by Kapha with sluggish Agni [53].
- Sannipataja Grahani: A combined manifestation of all Doshas with alternating constipation and diarrhea, similar to unclassified or fluctuating IBS (IBS-U). It indicates chronic and complex pathology requiring Rasayana rejuvenation and long-term management [55].
Each type involves both gastrointestinal and psychological components, emphasizing Ayurveda’s holistic perception that the mind, metabolism, and microbes are interlinked through Agni and Ojas [46].
Diagnosis
IBS shares its symptoms with several gastrointestinal and endocrine disorders. Accurate differentiation is essential before confirming the diagnosis of Grahani Roga or Irritable Bowel Syndrome.
5.1 Modern Differential Diagnoses
- Lactose Intolerance
Caused by deficiency of the enzyme lactase leading to fermentation of lactose by intestinal bacteria. Symptoms like bloating, gas, and diarrhea closely resemble IBS, but lactose-free diet resolves the condition completely [79]. - Celiac Disease
An autoimmune reaction to gluten causing villous atrophy in the small intestine. It presents with chronic diarrhea, malabsorption, anemia, and weight loss. Unlike IBS, serologic tests (anti-tTG, anti-endomysial antibodies) and intestinal biopsy confirm the diagnosis [78]. - Inflammatory Bowel Disease (IBD)
Includes Crohn’s disease and ulcerative colitis, which involve structural mucosal damage, elevated calprotectin, and visible lesions on colonoscopy. IBS, in contrast, shows no inflammatory or structural changes [80]. - Hypothyroidism
Low thyroid hormone levels cause slowed intestinal motility leading to constipation-predominant IBS-like symptoms. A simple TSH and T4 test differentiates this [81]. - Small Intestinal Bacterial Overgrowth (SIBO)
Characterized by excessive bacteria in the small intestine leading to bloating, belching, and alternating bowel habits. Breath tests with lactulose or glucose identify SIBO; successful antibiotic or herbal therapy confirms it [82]. - Adrenal Fatigue
Though not universally accepted in conventional medicine, chronic HPA-axis exhaustion mimics IBS symptoms with fatigue, low energy, and gut sensitivity due to cortisol imbalance [71].
5.2 Ayurvedic Parallel Differentials
Ayurveda describes several conditions resembling different presentations of IBS or Grahani Roga. These include:
- Ajeerna (Indigestion) – Resulting from Mandagni, causing heaviness, nausea, and loss of appetite. Corresponds to early-stage IBS or functional dyspepsia [47].
- Atisara (Diarrhea) – Frequent watery stools with abdominal discomfort; resembles IBS-D [52].
- Pravahika (Dysentery) – Passage of mucus and blood in stools due to severe Pitta and Vata aggravation, which must be differentiated from IBD [53].
- Shoola (Abdominal Pain) – Pain and cramps due to deranged Vata, a dominant symptom in IBS [48].
- Arsha (Hemorrhoids) – Chronic constipation leading to rectal discomfort and bleeding; may coexist with IBS-C [55].
In Ayurvedic evaluation, correct identification among these conditions requires careful assessment of Agni, Dosha predominance, and Srotas involvement. Grahani Roga is confirmed when the dysfunction originates primarily from Agni Dushti leading to alternating bowel patterns and Ama accumulation [46].
Symptoms of IBS and Grahani Roga
The clinical picture of Irritable Bowel Syndrome (IBS) and its Ayurvedic equivalent, Grahani Roga, is diverse and systemic. While the most visible symptoms involve bowel irregularities, deeper disturbances affect the liver, endocrine system, skin, and even mental well-being. Both Ayurveda and modern medicine describe IBS as a disorder of digestion, emotion, and metabolism.
6.1 Common Gastrointestinal Symptoms
- Altered bowel habits – Alternating constipation (IBS-C) and diarrhea (IBS-D), or mixed forms (IBS-M), represent the defining characteristic of the disease.
- Abdominal pain and cramping – Pain typically eases after defecation and worsens with anxiety, linked to Vata vitiation and visceral hypersensitivity [45].
- Bloating and distension – Occurs due to fermentation, microbial imbalance, and weakened Agni [47].
- Excessive flatulence and gurgling (Atopa) – Caused by disturbed Vata movement in the intestines [48].
- Mucus in stools – Common in Kaphaja Grahani and mixed IBS [53].
- Incomplete evacuation – A hallmark of Apana Vata dysfunction [55].
- Loss of appetite (Aruchi) – Indicates Agni Mandya and early Ama formation [47].
- Heaviness after meals – Reflects poor digestion and stagnation in Annavaha Srotas [52].
- Gurgling sounds (Jatharashabda) – Mentioned by Charaka as a sign of disturbed digestion [54].
6.2 Systemic and Extraintestinal Symptoms
- Fatigue and weakness – Due to Rasa Dhatu Kshaya and inadequate assimilation [46].
- Sleep disturbance – Especially in Vata-Pitta types with cortisol rhythm imbalance [71].
- Headache and migraine-like pain – A result of neurovascular hypersensitivity and gut–brain miscommunication [67].
- Anxiety and low mood – Reflect serotonin depletion and Ojas deficiency [56].
- Muscle stiffness and body ache – Often coexists with Majja Dhatu Kshaya [54].
- Cold extremities and poor circulation – Sign of Vata aggravation [48].
- Unexplained weight changes – Loss with Pitta dominance or gain with Kapha imbalance [52].
6.3 Endocrine and Hormonal Manifestations
- Menstrual irregularities – Result from Pitta and hormonal fluctuations; symptoms worsen around menstruation or menopause [74].
- Premenstrual bloating and pain – Caused by estrogen–progesterone imbalance [72].
- Thyroid dysfunction – Hypothyroidism causes constipation and fatigue, while hyperthyroidism causes loose stools [81].
- Adrenal fatigue – Leads to exhaustion, dizziness, and sugar cravings due to chronic stress and cortisol depletion [71].
- Hypoglycemic spells – Fluctuating insulin and ghrelin activity create sudden weakness [76].
6.4 Psychological and Neurobehavioral Symptoms
Ayurveda links Manovaha Srotas (psychological channels) with the colon, hence emotional stress directly affects gut rhythm.
- Irritability and emotional swings – Serotonin imbalance and Vata aggravation [50].
- Brain fog and poor memory – Majja Dhatu Kshaya and dysbiosis [54].
- Restlessness and palpitations – From Prana Vata disturbance and anxiety [45].
- Depressive states and loss of motivation – Seen in chronic Grahani with depleted Ojas [46].
6.5 Rare and Overlooked Symptoms
These secondary and lesser-known features often lead to misdiagnosis or delayed recognition.
- Recurrent mouth ulcers – Due to Pitta aggravation and mucosal inflammation.
- Dry mouth and altered taste (Mukha Shosha, Rasa Viparyaya) – Seen in Vataja Grahani [48].
- Joint stiffness or mild arthritis – From circulating Ama and inflammatory mediators [66].
- Skin eruptions and itching – Pitta-Kapha imbalance and toxin accumulation [52].
- Hair loss and brittle nails – Reflect Rasa and Rakta Dhatu depletion.
- Dizziness and blurred vision – Associated with Ojas Kshaya and poor cerebral perfusion [54].
- Chest heaviness and pseudo-cardiac pain (Udarashoola) – Caused by trapped Vata [49].
- Early-morning urgency with anxiety – Linked to cortisol peaks and circadian disruption [71].
- Intolerance to fermented foods and alcohol – Indicates Ama accumulation and microbial dysbiosis [64].
- Low-grade chronic fever – Result of Ama Jwara, often accompanying inflammatory Grahani [47].
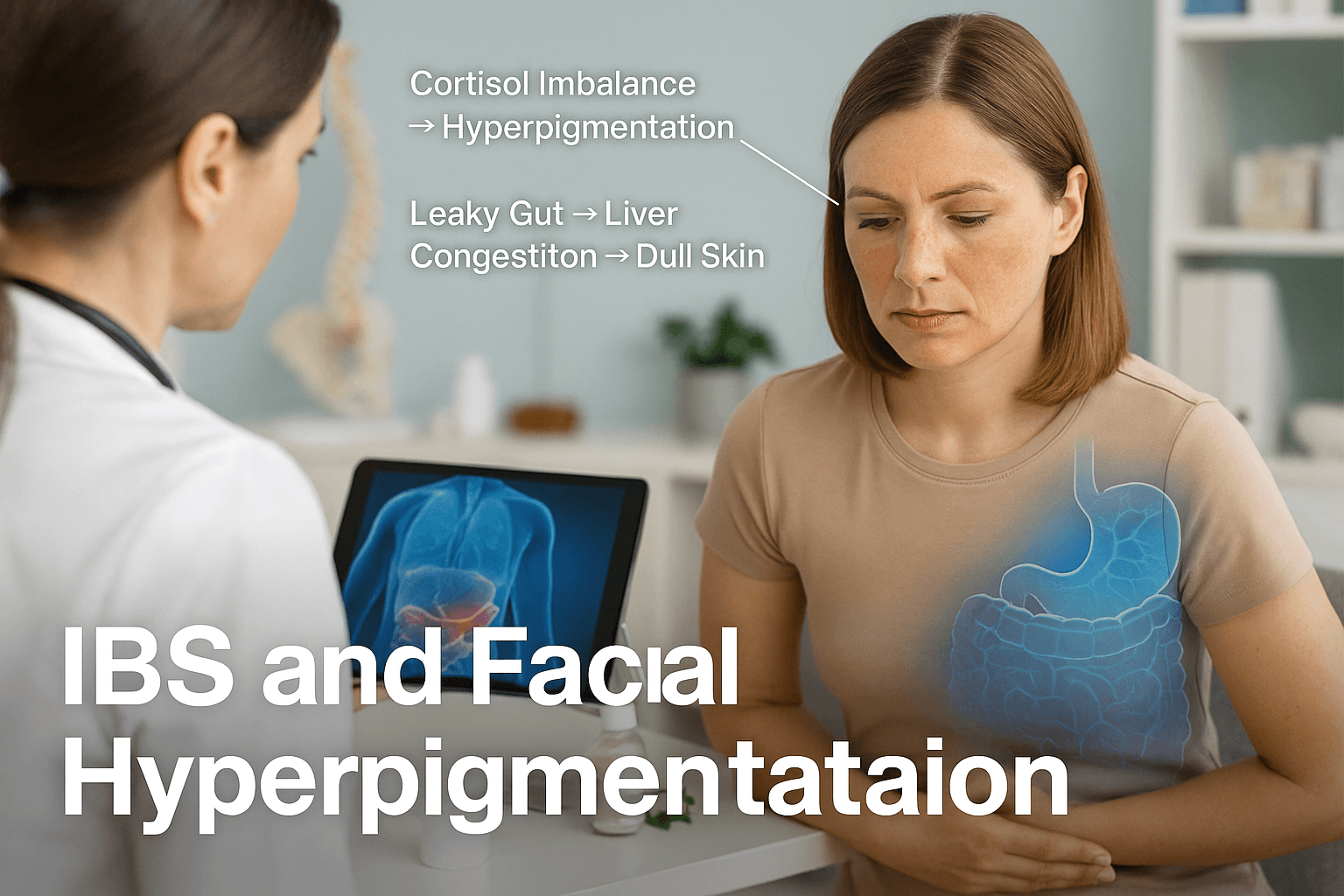
6.6 Skin Manifestations and Hyperpigmentation
Though less discussed, hyperpigmentation and skin dullness can occur in long-standing IBS and Grahani Roga. The gut–liver–skin axis provides a scientific and Ayurvedic explanation for this manifestation.
- Adrenal and cortisol imbalance – Continuous HPA-axis stress increases ACTH and melanocyte-stimulating hormone, producing patchy darkening around eyes, neck, and hands [71].
- Gut–liver congestion – Ama and toxins absorbed from the intestine overload hepatic pathways, causing melasma-like pigmentation, especially over the cheeks and forehead [66].
- Nutrient malabsorption – Deficiencies of vitamin B12, folate, and zinc result in darkening of knuckles, lips, and oral mucosa [64].
- Pitta and Rakta Dushti – Ayurveda explains pigmentation as Tvak Vaivarnya, caused by disturbed Pitta and impure Rakta Dhatu due to weak Agni [47].
- Ojas depletion and stress – Manovaha Srotas imbalance produces dull, tired skin tone and dark circles in chronic cases [54].
Ayurveda notes that these pigmentation changes are reversible once Agni is strengthened, Ama eliminated, and Rakta Dhatu purified. Herbs like Manjistha, Sariva, and Guduchi restore skin tone, while Brahma Rasayana rejuvenates Ojas and hormonal balance.
6.7 Ayurvedic Summary of Symptom Pathways
- Agni Dushti → Ama Nirmiti (toxin accumulation)
- Ama → Srotorodha (blockage of microchannels)
- Srotorodha → Dosha Prakopa (functional derangement)
- Dosha Prakopa → Systemic symptoms across gut, mind, skin, and hormones
IBS and Grahani Roga thus represent a multisystemic disturbance of Agni, manifesting not only in the gut but also through the skin, endocrine glands, and emotional stability. The skin changes, including hyperpigmentation, are therefore external reflections of internal metabolic imbalance
Diseases and Conditions Commonly Associated With IBS
IBS rarely exists as a single digestive problem. In most patients, it develops along with other conditions involving digestion, hormones, immunity, nerves, or infections. When these are not identified, IBS treatment often gives only partial or temporary relief.
1. Functional Dyspepsia
Functional dyspepsia is one of the most common conditions seen alongside IBS. Patients often feel discomfort in the upper abdomen rather than the lower bowel. Symptoms include early fullness after eating, nausea, bloating in the upper stomach, heaviness, and loss of appetite. Many people feel full even after small meals. This indicates that digestion is weak from the very beginning of the digestive process, not only in the intestines.
When functional dyspepsia is present, food is not broken down properly. This poorly digested food irritates the gut lining and increases gas formation, pressure, and bowel irregularity. Over time, this worsens IBS symptoms such as abdominal pain, alternating stools, and food sensitivity.
Treating IBS alone without addressing upper digestive weakness often leads to partial improvement only. For lasting recovery, digestion must be strengthened from the stomach to the intestines. In Ayurveda, this reflects weakened Agni at multiple levels, which must be corrected systematically for complete gut healing.
2. Acid Reflux and GERD
Acid reflux and GERD commonly occur with IBS and share the same underlying digestive imbalance. Patients experience burning in the chest, sour taste in the mouth, frequent belching, throat irritation, or discomfort after meals. These symptoms occur because food movement through the digestive tract is poorly coordinated.
When gut motility is disturbed, stomach contents move in the wrong direction, allowing acid to rise upward. Nervous system imbalance and stress further worsen this process. Many IBS patients notice that reflux symptoms increase during periods of anxiety or irregular eating.
If acid reflux is ignored, IBS remains unstable. Acid irritation increases gut sensitivity and alters bowel movement patterns. Long term use of acid suppressing medicines may temporarily reduce burning but can weaken digestion further.
For true recovery, both upper and lower digestive function must be restored together. Calming the nervous system and improving digestive rhythm are essential for stabilizing IBS when reflux is present.
3. Small Intestinal Bacterial Overgrowth
Small intestinal bacterial overgrowth is one of the most important hidden causes of IBS symptoms. In this condition, excess bacteria grow in the small intestine where they do not normally belong. These bacteria ferment food early, producing gas, bloating, pressure, abdominal pain, diarrhea, constipation, or both.
Many patients with IBS experience bloating soon after eating, even with small meals. This is a strong sign of bacterial imbalance. Over time, bacterial overgrowth damages the gut lining, interferes with nutrient absorption, and increases food sensitivity.
If this condition is not identified, IBS treatment often fails repeatedly. Medicines may give temporary relief, but symptoms return because the underlying imbalance remains.
Effective management requires restoring healthy gut movement, improving digestive strength, and correcting microbial balance. Simply suppressing symptoms without addressing bacterial overgrowth leads to chronic relapse and frustration for patients.
4. Food Intolerances
Food intolerances are extremely common in people with IBS and are often overlooked. Patients may react to lactose, fructose, wheat proteins, or certain carbohydrates. Symptoms include bloating, cramps, loose stools, fatigue, brain fog, and abdominal discomfort after eating specific foods.
Unlike food allergies, food intolerances do not cause immediate severe reactions. Instead, symptoms appear gradually and repeatedly, making them difficult to identify without careful observation. Many patients continue eating trigger foods daily without realizing their role in worsening IBS.
When intolerant foods are consumed regularly, the gut becomes inflamed and hypersensitive. This increases bowel irregularity and pain even when medicines are taken correctly.
For IBS to improve, trigger foods must be identified and removed. No treatment can succeed if the digestive system is repeatedly irritated by incompatible foods. Personalized dietary correction is a core requirement for long term gut stability.
5. Anxiety and Panic Disorder
Anxiety and panic disorder are among the strongest contributors to IBS. Many patients notice that their bowel symptoms worsen during stress, worry, or emotional pressure. The gut and brain are closely connected, and emotional distress directly affects digestion, bowel movement, and pain perception.
When anxiety is present, the nervous system stays in a constant alert state. This alters gut movement, increases sensitivity, and disrupts digestive secretions. As a result, patients experience cramps, urgency, diarrhea, constipation, or bloating without a clear dietary trigger. Panic episodes can cause sudden bowel urgency, chest tightness, and abdominal discomfort.
Treating IBS without calming the nervous system often leads to failure. Digestive medicines alone cannot override ongoing anxiety signals sent to the gut. For lasting improvement, emotional regulation and stress control must be addressed together with digestive treatment. Restoring nervous system balance is essential for stabilizing bowel function and reducing IBS flare frequency.
6. Depression
Depression frequently accompanies long standing IBS, especially when symptoms persist for years. Chronic digestive discomfort affects mood, motivation, confidence, and emotional well being. At the same time, depression itself alters gut chemistry and nervous signaling, worsening digestive symptoms.
The gut produces many chemical messengers that influence mood. When digestion is weak and inflammation is present, these signals become imbalanced. This can lead to low mood, irritability, lack of interest, fatigue, and sleep disturbance. Patients may feel stuck in a cycle where digestive symptoms worsen emotional health and emotional distress worsens digestion.
Ignoring depression delays IBS recovery. Even if bowel symptoms improve slightly, they tend to return when emotional health remains untreated. Supporting mental well being alongside gut healing is necessary for complete recovery. When mood improves, digestion often stabilizes naturally and symptom intensity reduces.
7. Sleep Disorders
Sleep disorders are extremely common in IBS patients and play a major role in symptom persistence. Poor sleep weakens digestion, increases pain sensitivity, and disrupts hormonal rhythm. Patients may have difficulty falling asleep, frequent awakenings, or unrefreshing sleep.
The digestive system follows a daily rhythm. When sleep timing is irregular, digestion loses its natural coordination. This leads to bloating, constipation, diarrhea, and abdominal discomfort. Poor sleep also increases stress hormones, which further irritate the gut.
Many patients try to treat IBS without correcting sleep habits. This limits recovery. Even the best digestive treatment works poorly when sleep remains disturbed. Restoring proper sleep timing and quality helps calm the nervous system, improves gut movement, and reduces pain sensitivity. Stable sleep is a foundational requirement for long term IBS improvement.
8. Polycystic Ovary Syndrome
Polycystic ovary syndrome is commonly seen in women with IBS. Hormonal imbalance, insulin resistance, and low grade inflammation affect gut movement and sensitivity. Many women with PCOS experience bloating, constipation, diarrhea, or abdominal discomfort that fluctuates with their menstrual cycle.
Hormones strongly influence digestion. Changes in estrogen and progesterone alter bowel rhythm and pain perception. Insulin resistance can slow digestion and increase inflammation. When PCOS is present, IBS symptoms often become unpredictable and more difficult to control.
Treating IBS alone without addressing hormonal imbalance often leads to incomplete results. Digestive symptoms may improve temporarily but return with hormonal fluctuations. Supporting hormonal balance, metabolic health, and digestive strength together is necessary for lasting relief. In women with PCOS, IBS treatment must always consider endocrine health.
9. Chronic Fatigue Syndrome
Chronic fatigue syndrome is frequently seen in patients with long standing IBS. These individuals feel exhausted even after adequate rest and often struggle with poor stamina, mental fog, and reduced daily functioning. This fatigue is not simply due to poor sleep or stress. It reflects deeper immune, hormonal, and nervous system imbalance.
When digestion is weak for a long time, nutrient absorption becomes impaired and inflammation increases. This drains energy reserves and disrupts cellular metabolism. The nervous system also becomes overworked, leading to constant tiredness and reduced stress tolerance. Many patients notice that IBS symptoms flare when fatigue worsens.
Treating IBS without addressing chronic fatigue leads to slow or incomplete recovery. Energy must be restored along with digestion. When vitality improves, bowel function often becomes more stable and symptom intensity decreases. Addressing fatigue is essential for full and lasting IBS improvement.
10. Chronic Viral Reactivation Including Herpes CMV and EBV
Chronic viral reactivation is an important but often ignored contributor to IBS. Many patients carry latent viruses such as herpes simplex virus cytomegalovirus and Epstein Barr virus. These viruses may remain silent for years but can reactivate under stress, immune weakness, or hormonal imbalance.
When reactivated, these viruses affect gut immunity, nervous signaling, and inflammation. Patients may experience persistent bloating, bowel irregularity, abdominal pain, anxiety, and fatigue without clear laboratory findings. Digestive treatment alone often fails because the underlying immune stress remains active.
In some cases, viral burden keeps the gut in a constant low grade inflammatory state. This delays healing and increases sensitivity. Supporting immune strength and restoring systemic resilience are necessary for recovery. IBS often stabilizes only when viral related immune stress is addressed alongside digestive therapy.
11. Iron Deficiency Anemia
Iron deficiency anemia is common in people with long standing IBS. Poor digestion and absorption reduce iron uptake, while chronic inflammation interferes with iron metabolism. Symptoms include fatigue, weakness, shortness of breath, hair fall, dizziness, and poor concentration.
When anemia is present, gut healing slows significantly. The intestinal lining regenerates poorly, and energy levels remain low. Many patients continue to experience IBS symptoms despite correct digestive treatment because anemia is not corrected.
Treating IBS without restoring iron levels leads to incomplete results. Supporting absorption and rebuilding blood quality are essential steps. When iron status improves, patients often notice better stamina, improved digestion, and reduced bowel sensitivity. Addressing anemia is a key part of comprehensive IBS care.
12. Vitamin B12 and Vitamin D Deficiency
Vitamin deficiencies are frequently found in chronic IBS. Vitamin B12 deficiency affects nerve health and worsens gut sensitivity, pain, and irregular bowel movements. Patients may experience tingling, numbness, fatigue, brain fog, and mood changes.
Vitamin D deficiency weakens immune regulation and increases inflammation. Low vitamin D levels are associated with increased pain sensitivity, frequent infections, and poor gut barrier function. Many IBS patients have low vitamin D due to poor absorption and limited sunlight exposure.
Without correcting these deficiencies, IBS symptoms often persist despite treatment. Nutritional restoration supports nerve stability, immune balance, and tissue healing. When vitamin levels normalize, digestion becomes more resilient and symptom frequency reduces. Correcting deficiencies is essential for long term IBS recovery.
Additional Conditions That Can Worsen IBS
13. Migraine and Tension Headaches
Many IBS patients suffer from frequent headaches triggered by food, stress, or sleep disturbance. This reflects gut brain imbalance. When headaches are not addressed, digestive symptoms often remain unstable.
14. Fibromyalgia
Widespread muscle pain and tenderness commonly overlap with IBS. Both conditions share altered pain processing and nervous system sensitivity. Treating digestion alone rarely resolves symptoms fully.
15. Mast Cell Activation Disorders
Some patients react strongly to foods and medications, experiencing abdominal pain, diarrhea, flushing, palpitations, and anxiety. Excess mast cell activity keeps the gut hypersensitive.
16. Histamine Intolerance
Impaired histamine breakdown leads to bloating, loose stools, headaches, skin reactions, and heart palpitations after meals. Many IBS patients unknowingly consume histamine rich foods daily.
17. Bile Acid Malabsorption
Excess bile acids entering the colon cause chronic diarrhea, urgency, and burning sensation. This condition is often mistaken for IBS diarrhea type.
18. Exocrine Pancreatic Insufficiency
Low digestive enzyme production results in poor fat digestion, bloating, loose stools, weight loss, and nutrient deficiency. Mild forms are frequently missed.
19. Interstitial Cystitis
Chronic bladder pain and urinary frequency often coexist with IBS due to shared pelvic nerve sensitivity.
20. Autoimmune Thyroid Disease
Thyroid imbalance alters gut motility and sensitivity. Even mild dysfunction can significantly worsen IBS symptoms.
21. Metabolic Syndrome and Insulin Resistance
Blood sugar instability affects gut movement, inflammation, and microbiota balance, making IBS harder to control.
22. Post Infectious Digestive Syndrome
IBS may begin after food poisoning. Persistent nerve sensitization and immune activation remain even after infection clears.
23. Autonomic Nervous System Dysfunction
Imbalance in automatic nerve control disrupts bowel rhythm and blood flow. Patients may feel dizziness, weakness, or palpitations along with digestive symptoms.
24. Small Fiber Neuropathy
Damage to small nerves alters gut pain perception and bowel coordination, leading to severe sensitivity and unpredictable symptoms.
25. Connective Tissue Disorders
Joint laxity and tissue weakness can affect gut support and nerve signaling, contributing to chronic digestive instability.
26. Chronic Low Grade Inflammation
Ongoing subtle inflammation keeps the intestines hypersensitive even when routine tests appear normal.
27. Medication Induced Gut Dysfunction
Long term use of antibiotics, acid suppressants, painkillers, antidepressants, or hormonal drugs alters gut flora and motility.
28. Heavy Metal or Environmental Toxin Exposure
Toxins disrupt gut bacteria, immunity, and nerve function, leading to persistent digestive symptoms.
29. Electrolyte Imbalance and Dehydration
Low fluids or electrolyte imbalance worsen constipation, fatigue, and nerve signaling.
30. Nutrient Absorption Disorders
Poor absorption of magnesium, zinc, selenium, or essential fatty acids aggravates bowel irregularity and anxiety.
31. Circadian Rhythm Disruption
Late nights, shift work, or frequent travel disturb digestive timing and bowel regularity.
32. Pelvic Floor Dysfunction
Poor coordination of pelvic muscles causes constipation, incomplete evacuation, and pain mistaken as IBS alone.
33. Chronic Psychological Trauma
Past emotional trauma permanently sensitizes the gut brain axis, causing severe symptoms even when tests are normal.
Modern Management and Limitations
The contemporary management of Irritable Bowel Syndrome (IBS) primarily focuses on symptom alleviation rather than permanent correction of underlying physiological dysfunction. Modern pharmacology addresses the gut–brain axis, motility, and microbial imbalance through drugs that provide temporary comfort but rarely restore systemic equilibrium. Ayurveda contrasts this with a root-cause approach focused on Agni, Ojas, and Srotas balance.
7.1 Pharmacological Management
1. Antispasmodics
Medications such as dicyclomine, hyoscine, and mebeverine are commonly prescribed to reduce intestinal spasms and pain. These agents work by relaxing smooth muscle and suppressing hypersensitive visceral responses. Although they offer temporary relief, prolonged use may lead to constipation, dry mouth, blurred vision, and fatigue [78].
2. Probiotics and Microbiome Therapy
Probiotics are widely used to restore intestinal microbial balance. Strains such as Lactobacillus plantarum, Bifidobacterium infantis, and Saccharomyces boulardii have shown moderate benefit in regulating stool consistency and reducing bloating [64]. However, results remain inconsistent, as probiotic effects depend on strain-specific colonization and patient microbiota variability. In post-infectious IBS, reestablishing microbial homeostasis is often temporary unless dietary and stress-related factors are corrected [66].
3. Antidepressants (SSRIs and TCAs)
Selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine and sertraline, and tricyclic antidepressants (TCAs) such as amitriptyline, are prescribed for IBS patients with anxiety or pain-dominant symptoms. They modulate gut motility through serotonin pathways and dampen visceral pain signaling [50]. Yet, the dependence on mood-altering drugs often masks deeper dysbiosis and endocrine dysfunction [71]. Long-term use may lead to lethargy, hormonal disruption, and weight fluctuation.
4. Hormone Therapy for Endocrine Imbalance
For patients with thyroid, cortisol, or reproductive hormone abnormalities, hormone therapy is sometimes recommended.
- Thyroid medications (levothyroxine, carbimazole) are used to regulate bowel rhythm in hypothyroid or hyperthyroid-associated IBS [81].
- Cortisol modulation via adrenal support or replacement therapy is attempted in cases of chronic stress or adrenal fatigue [71].
However, these interventions manage secondary dysfunction rather than correcting the root disturbance of the gut–brain–endocrine axis.
7.2 Limitations of Modern Treatment
Despite pharmacological progress, IBS remains a functional disorder without curative therapy in mainstream medicine. The limitations lie in the mechanistic approach that treats symptoms in isolation rather than as part of an interconnected system.
1. Symptom Suppression Without Root-Cause Correction
Modern drugs relax muscles, alter neurotransmitters, or modify microbial populations temporarily, but they do not restore Agni (digestive fire) or cellular metabolism. Once medication is discontinued, symptoms typically resurface within weeks [56].
2. Side Effects and Dependency
Antidepressants cause mood blunting, fatigue, and gastrointestinal upset. Antispasmodics induce constipation, and prolonged probiotic use may cause bacterial overgrowth if gut integrity remains weak [66].
3. Neglect of Mind–Body–Gut Integration
Most conventional approaches ignore the psychological and endocrine factors that Ayurveda identifies as Manovaha Srotas and Agni–Ojas interaction. Modern psychiatry recognizes the gut–brain axis, yet integrated protocols remain limited [67].
4. Lack of Personalization
IBS treatment guidelines are generalized, whereas Ayurveda tailors therapy to Dosha predominance and Prakriti. Modern regimens often overlook this individuality, resulting in non-responsive cases [46].
5. Recurrence Upon Discontinuation
Because modern medicine primarily manages symptoms, recurrence rates exceed 70% after medication withdrawal [80]. Patients often develop chronic reliance on drugs, forming a loop of temporary relief and relapse.
Ayurvedic Treatment Protocol for IBS (Grahani Roga)
Ayurveda offers a comprehensive, multi-phase approach aimed at root-cause eradication rather than symptomatic relief. The treatment restores the strength of Agni (digestive fire), clears Ama (toxins), rebalances Doshas, and rejuvenates Ojas (vital energy). The protocol integrates Shodhana (detoxification), Shamana (pacification), Rasayana (rejuvenation), and Pathya–Apathya (diet and lifestyle discipline) to achieve complete systemic restoration.
A. Shodhana Therapy (Detoxification)
Charaka Samhita and Ashtanga Hridaya emphasize that purification is essential before pacification to eliminate deeply seated Ama and reawaken Agni. For IBS or Grahani Roga, mild yet sequential detox methods are employed depending on patient strength and Dosha predominance.
1. Snehapana (Internal Oleation)
The process begins with the administration of medicated ghee or castor oil for internal lubrication and toxin mobilization.
- Ghee: For Vata–Pitta imbalance; nourishes intestinal mucosa and calms irritability.
- Castor oil: For Pitta–Kapha type with heaviness or mucous accumulation.
This phase enhances tissue permeability and prepares the body for elimination [47].
2. Virechana (Therapeutic Purgation)
A controlled purgation using classical formulations such as Trivrit Lehyam or Avipattikar Churna removes accumulated Pitta and Ama from the small intestine [52].
- Trivrit Lehyam is ideal for heat-dominant cases with acidity or burning.
- Avipattikar Churna suits mixed types with alternating stool patterns.
This therapy resets gut motility and improves bile and enzyme function, analogous to microbiome resetting in modern gastroenterology [66].
3. Basti Karma (Medicated Enema Therapy) — Optional but Highly Effective
Regarded as the supreme therapy for Vata-dominant disorders like IBS-C and mixed types. It corrects irregular peristalsis, strengthens colon walls, and restores enteric nerve coordination [48].
- Anuvasana Basti: Oil-based enema using Ashwagandha Taila lubricates and nourishes colon tissue.
- Niruha Basti: Decoction-based enema with Dashamoola Kwatha eliminates residual Ama, calms inflammation, and harmonizes gut–brain signaling.
Classical Reference: Charaka Samhita, Siddhi Sthana 1/27–30 — “Among all therapies, Basti holds supreme power to balance Vata and restore systemic integrity.”
B. Shamana Therapy (Pacification)
After detoxification, the next stage stabilizes Agni, neutralizes residual Ama, and restores intestinal rhythm.
1. Deepana–Pachana (Digestive Stimulation & Metabolic Correction)
Herbs that kindle Agni and dissolve toxins:
- Pippali (Piper longum): Enhances nutrient absorption and modulates gut-brain signaling [45].
- Chitraka (Plumbago zeylanica): Potent digestive stimulant for sluggish Kapha conditions [47].
- Shunthi (Zingiber officinale): Regulates motility and reduces bloating via anti-inflammatory pathways [64].
2. Grahani Rasayana (Tonic for Intestinal Strength)
Classical formulations that directly address Grahani Dushti and restore intestinal tone:
- Dadimadi Avaleha: Antioxidant-rich digestive tonic that balances Vata–Pitta and reduces post-meal discomfort.
- Kutajavaleha: Astringent and antimicrobial, beneficial in Pittaja and Kaphaja Grahani [66].
- Brahma Rasayana: Supreme rejuvenator mentioned in Charaka Samhita (Chikitsa Sthana 1/1–4); enhances Majja Dhatu (nervous tissue) and harmonizes gut–brain axis [46].
3. Herbo–Mineral Combinations
For chronic and refractory IBS, Bhasma therapy helps restore enzymatic, endocrine, and microbial equilibrium.
- Abhrak Bhasma (Shataputi): Regulates peristalsis and acts as a neuroendocrine rejuvenator [54].
- Jasad Bhasma: Rich in bioavailable zinc nanoparticles; improves mucosal repair and immunity [64].
- Mukta Shukti Bhasma: Alkaline, cooling, and effective in hyperacidity and Pittaja Grahani [52].
- Optional Rasayanas: Swarna Bhasma and Heerak Bhasma for endocrine insufficiency and chronic fatigue [46].
C. Rasayana Therapy (Rejuvenation Phase)
The Rasayana phase rebuilds tissues, regulates hormones, and stabilizes the gut–brain–endocrine connection.
- Ashwagandha (Withania somnifera): Adaptogen that reduces cortisol, alleviates stress-related IBS, and supports adrenal function [71].
- Shatavari (Asparagus racemosus): Balances estrogen and improves mucosal immunity in women [74].
- Guduchi (Tinospora cordifolia): Restores immune tolerance and reduces chronic inflammation [66].
- Brahmi and Mandukaparni: Enhance serotonin regulation and mental calmness, crucial in Manovaha Srotas disorders [54].
- Triphala: Detoxifies intestinal walls and supports healthy microbiota diversity [64].
Classical Note: Sushruta Samhita, Chikitsa Sthana 33/4 — “Rasayana rejuvenates what has been exhausted, enhances vitality, and reawakens the strength of Agni.”
D. Pathya–Apathya (Diet and Lifestyle Guidelines)
Long-term success in IBS management depends on disciplined adherence to diet and daily regimen (Dinacharya).
Recommended:
- Warm, freshly cooked meals with ghee to soothe Agni.
- Takra Kalpana (buttermilk preparations) for digestion and microbiome balance [47].
- Light grains, Moong dal, cumin-fennel water, and cooked vegetables.
Avoid:
- Cold, raw, or fermented foods that increase Ama.
- Red chili, sour curd, alcohol, and refined sugar, all of which aggravate Pitta and disturb gut flora [52].
Lifestyle:
- Early dinner (before 8 PM) and 7–8 hours of sleep to stabilize circadian rhythm [71].
- Daily Yoga Asanas like Vajrasana and Pavanamuktasana for gut motility.
- Pranayama and meditation to calm Prana Vata and regulate neuroendocrine tone.
Dadimadi Avaleha (Main Medicine)
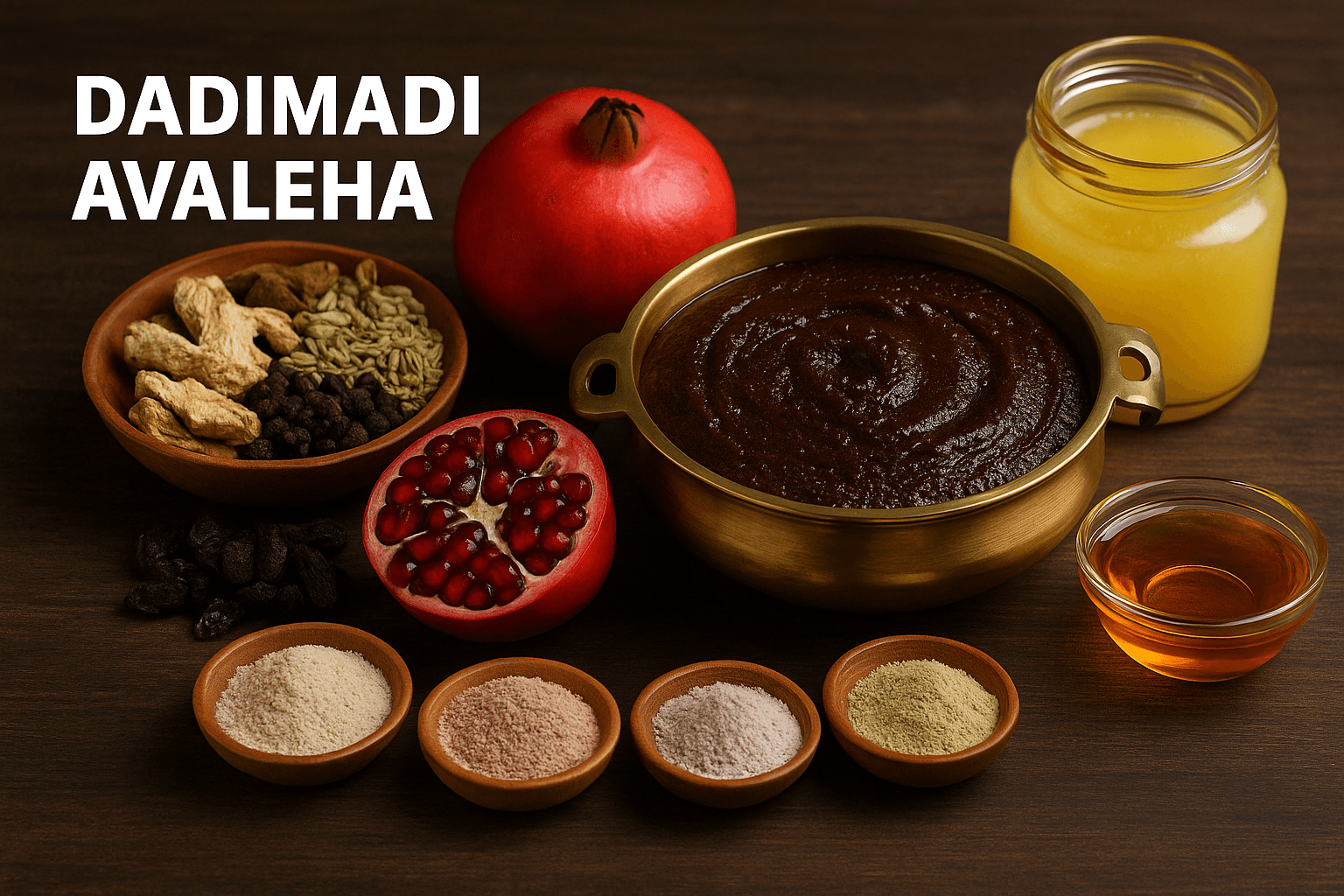
Classical Source: Bhavaprakasha Madhyama Khanda (6/64–69) and Bhaishajya Ratnavali (Grahani Chikitsa Prakarana 10/36–40)
Duration: 30 days
Dose: 15 grams twice daily after meals with lukewarm water or Takra (buttermilk)
About the Formulation
Dadimadi Avaleha is the classical Ayurvedic preparation indicated for Grahani Roga, the condition that closely resembles modern Irritable Bowel Syndrome. It strengthens Agni (digestive fire), restores intestinal tone, and calms Vata–Pitta imbalance responsible for alternating constipation, diarrhea, and abdominal discomfort. Its base of Dadima (Punica granatum), combined with potent digestive herbs and rejuvenating minerals, provides both mucosal protection and metabolic correction.
Ingredients (for a 30-day course)
The preparation requires the following:
200 grams of Dadima (pomegranate pulp), 100 grams of Draksha (raisins), 50 grams of Amalaki (Indian gooseberry), 40 grams each of Bilva (bael fruit) and Musta (Cyperus rotundus), 30 grams of Chitraka (leadwort), 20 grams each of Pippali (long pepper), Shunthi (dry ginger), and Maricha (black pepper), 15 grams each of Shweta Jeeraka and Krishna Jeeraka (white and black cumin), 15 grams of Dhanyaka (coriander seed), and 5 grams of Hingu (asafoetida).
To these herbs, add 25 grams each of Guduchi (Tinospora cordifolia), Shatavari (Asparagus racemosus), and Yashtimadhu (licorice). Include 30 grams of Triphala (Amalaki, Haritaki, and Bibhitaki) for gentle detoxification.
For mineral rejuvenation, mix 5 gram of Abhrak Bhasma-Sahasraputi (purified mica), 500 milligrams each of Jasad Bhasma (zinc calx), Mukta Shukti Bhasma (pearl-oyster shell), Godanti Bhasma (gypsum), Heerak Bhasma 500 mg , Vyadhiharan Rasayan, 5 gram, Gold Bhasma 300 mg and Pravala Pishti (coral calcium). These enhance absorption, restore mucosal integrity, and correct acidity.
As a base medium, use 250 grams of Sharkara (jaggery), 60 grams of cow’s ghee, and 60 grams of pure honey.
Preparation Method
Begin by preparing a decoction: combine Dadima, Amalaki, Musta, Chitraka, Jeeraka, Dhanyaka, Shunthi, Pippali, and Maricha in two liters of water. Boil gently until one-fourth remains, and then filter while warm.
Add Sharkara (jaggery) to this filtered decoction and heat on a mild flame until it thickens to an Avaleha or semisolid consistency. Once it slightly cools, add the fine powders of Triphala, Guduchi, Yashtimadhu, and Shatavari, stirring continuously.
When the mixture reaches about 70 °C, add Abhrak Bhasma, Jasad Bhasma, Mukta Shukti Bhasma, Godanti Bhasma, and Pravala Pishti etc . Mix thoroughly until the texture becomes uniform. Finally, add cow’s ghee and, once lukewarm, mix in honey to complete the formulation. Store in a clean, airtight glass jar.
Dosage and Duration
Take 15 grams twice daily after meals with lukewarm water or Takra (buttermilk). Continue this regimen for 30 days. For chronic IBS or long-standing Grahani, the course can be extended up to 90 days under professional supervision.
Expected Therapeutic Benefits
This Avaleha improves digestion, regulates bowel habits, reduces bloating, and heals the intestinal lining. It pacifies both Vata and Pitta, relieves acidity and gas, and strengthens mucosal immunity. Its mineral Rasayanas restore neuro-endocrine balance, reduce stress-related gut reactivity, and enhance mental calmness.
Precautions
Avoid during fever, acute diarrhea, or heavy menstruation. Ensure consistent intake without gaps; irregular use may delay results. Follow strict Pathya–Apathya guidelines — eat warm, freshly cooked food, avoid curd, pickles, red chili, alcohol, and fermented dishes.
Important Medical Warning and Mandatory Patient Advisory
A patient must not buy Ayurvedic medicines for IBS from the open market and must never prepare or consume these medicines without supervision of a qualified Ayurvedic doctor. IBS is not a single organ disorder. It is a complex multi system condition involving the digestive system nervous system immune system endocrine axis and in many patients chronic infections and metabolic disturbances. When medicines are purchased directly from the market or used without medical supervision treatment usually fails and symptoms frequently relapse.
Why market bought IBS medicines fail in real clinical practice
1. Age of the patient
Digestive strength tissue recovery immune resilience and hormonal balance vary with age. Younger patients often show stress driven and nerve mediated IBS. Middle aged patients commonly have hormonal metabolic or viral contributors. Older patients usually have weak digestion tissue depletion and dominant Vata imbalance. Market medicines do not adjust formulation strength dosage or Rasayana depth according to age.
2. Duration of IBS
Short duration IBS requires digestive correction and mental stabilization. Long standing IBS involves gut barrier damage immune exhaustion endocrine imbalance and nervous system hypersensitivity. Generic medicines cannot reverse deep seated Grahani pathology.
3. Presence of other digestive disorders
IBS frequently coexists with functional dyspepsia acid reflux small intestinal bacterial overgrowth food intolerances and pelvic floor dysfunction. Treating IBS alone without addressing these conditions leads to incomplete recovery.
4. Nutritional deficiencies
Iron deficiency vitamin B12 deficiency and vitamin D deficiency are common in IBS due to poor absorption and chronic inflammation. These deficiencies worsen fatigue nerve sensitivity and gut motility and must be corrected for treatment success.
5. Hormonal and endocrine disorders
IBS commonly accompanies hypothyroidism cortisol imbalance insulin resistance polycystic ovary syndrome menstrual irregularities and perimenopausal hormonal changes. Market medicines do not modify formulations based on endocrine status which leads to relapse.
6. Chronic pain and sensitivity disorders
Fibromyalgia migraine tension headaches interstitial cystitis and chronic pelvic pain syndromes frequently coexist with IBS indicating central nervous system sensitization. Ignoring these factors results in persistent symptoms.
7. Mental and emotional health conditions
Anxiety panic disorder depression chronic stress unresolved grief trauma and sleep disorders directly weaken digestion through the gut brain axis. Digestive medicines alone cannot cure IBS without addressing mental health.
8. Chronic viral infections as hidden contributors
Many IBS patients carry latent viral infections that disturb immunity nerve signaling and digestion.
Herpes Simplex Virus can affect enteric nerves and gut brain communication causing spasms pain and irregular bowel movement.
Cytomegalovirus can cause low grade intestinal inflammation immune fatigue and delayed mucosal healing.
Epstein Barr Virus is associated with chronic fatigue anxiety hypersensitivity and prolonged digestive weakness.
Market medicines do not address viral latency immune modulation or depletion of Ojas which leads to repeated relapse.
9. Autoimmune and immune dysregulation
Early autoimmune tendencies autoimmune thyroid disease and low grade immune activation commonly coexist with IBS. Without immune correction digestive treatment remains incomplete.
10. Metabolic disorders
Metabolic syndrome insulin resistance fatty liver disease and blood sugar instability influence gut motility inflammation and microbiota balance. Market medicines ignore metabolic involvement.
11. Digestive fire and toxin status
Treatment fails when Rasayana is given while toxins are present or when strong digestive stimulants are used in weak digestion. Only clinical evaluation can determine proper sequencing.
12. Need for detoxification therapy
Many IBS patients require therapeutic cleansing before oral medicines. Without detoxification medicines act superficially and do not reach deeper pathology.
13. Dosage timing and vehicle
Correct dosage timing and accompanying liquid vary for each patient based on digestion strength body weight and associated conditions. Fixed label dosing cannot replace physician guidance.
14. Quality and authenticity of medicines
Market products often contain inferior herbs improper processing missing mineral preparations adulteration or poor storage. Such medicines lack therapeutic strength and may worsen symptoms.
15. Diet and lifestyle non compliance
Without strict dietary discipline sleep regulation physical activity and stress control medicines will not work. Market medicines are sold without lifestyle correction making long term healing impossible.
Critical Instruction
Never prepare mix or consume Ayurvedic medicines for IBS without supervision of a qualified Ayurvedic doctor. Ayurvedic formulations are medical therapies not supplements or home remedies.
IBS Ayurvedic Treatment works only when it is personalized clinically supervised and integrated with detoxification diet correction lifestyle regulation immune strengthening hormonal balance mental health stabilization and when required antiviral Rasayana support.
Self treatment or market based medicine use commonly results in temporary relief repeated relapse worsening symptoms and loss of trust in Ayurveda due to incorrect application.
Frequently Asked Questions (FAQs)
1. What is Irritable Bowel Syndrome (IBS)?
IBS is a functional digestive disorder that affects the intestines, causing symptoms like abdominal pain, bloating, constipation, and diarrhea without structural abnormalities. Ayurveda describes this as Grahani Roga, where the digestive fire (Agni) becomes weak, leading to irregular digestion and toxin formation.
2. How common is IBS globally?
IBS affects millions of people worldwide and is recognized by the World Health Organization and Mayo Clinic as one of the most widespread functional gut disorders. It is often underdiagnosed or misinterpreted as a stress-related or psychosomatic problem.
3. Why is IBS often linked to stress?
The gut and brain communicate through the gut–brain axis. Chronic stress triggers changes in gut motility, hormone levels, and serotonin production, leading to IBS symptoms such as bloating, cramping, and irregular bowel habits. Ayurveda explains this through Manovaha Srotas Dushti, where mental strain weakens Agni and disturbs intestinal function.
4. What are the key symptoms of IBS?
Patients commonly experience alternating constipation and diarrhea, abdominal pain, bloating, mucus in stools, loss of appetite, fatigue, and disturbed sleep. In Ayurveda, these correspond to Vata-Pitta imbalance and Ama accumulation in the Annavaha Srotas (digestive channels).
5. Is IBS life-threatening?
No, IBS does not cause structural damage to the intestines or increase the risk of cancer. However, it significantly affects quality of life by causing chronic discomfort, mood changes, and dietary restrictions if not treated properly.
6. How does Ayurveda understand IBS?
Ayurveda identifies IBS as Grahani Roga, which originates from weakened digestive fire (Agni Mandya). When food is not properly digested, it forms Ama (toxic residue), leading to irregular bowel movement, inflammation, and systemic imbalance. Treatment focuses on restoring Agni and cleansing Srotas.
7. What causes IBS according to Ayurveda?
Major causes include irregular eating habits, excessive fasting, overeating, consumption of incompatible foods (Viruddha Ahara), stress, anxiety, lack of sleep, and suppression of natural urges. These factors weaken Agni and disturb Vata and Pitta Doshas, leading to Grahani Dushti.
8. What are the classical Ayurvedic texts that mention Grahani Roga?
Conditions resembling IBS are discussed in Charaka Samhita, Sushruta Samhita, and Ashtanga Hridaya. These texts explain the role of Agni, Ama, and Dosha imbalance in chronic digestive weakness and their relation to mental stress.
9. How does IBS affect quality of life?
IBS impacts daily productivity, sleep, mood, and emotional stability. Many patients experience anxiety, social withdrawal, and dietary fear. The Ayurvedic view connects these psychological disturbances with Ojas depletion and imbalanced Vata-Pitta, explaining both physical and emotional symptoms.
10. Can IBS be cured through Ayurveda?
Yes, IBS can be managed and often cured through a holistic Ayurvedic protocol involving Shodhana (detoxification), Shamana (pacification), and Rasayana (rejuvenation). Therapies like Virechana, Basti, and formulations such as Dadimadi Avaleha and Kutajavaleha correct the root imbalance and restore normal digestion and mental calmness.
11. What lifestyle changes help manage IBS?
Following a regular diet schedule, eating freshly cooked warm food, avoiding raw or fermented foods, sleeping early, practicing yoga postures like Vajrasana and Pavanamuktasana, and daily meditation significantly improve digestive stability and stress resilience.
12. Why is integrative care important in IBS?
Because IBS involves multiple systems—digestive, endocrine, and psychological—effective treatment must combine physical detoxification, mental relaxation, and metabolic rejuvenation. Ayurveda offers an integrative path by addressing all three simultaneously, unlike modern treatments that only suppress symptoms.
13. Does diet play a major role in IBS management?
Yes, diet is crucial. Warm, light meals with ghee, buttermilk, cumin, and fennel support digestion, while cold, sour, and fermented foods aggravate symptoms. Ayurveda emphasizes Pathya–Apathya (dos and don’ts) to maintain long-term balance.
14. What happens if IBS is left untreated?
If neglected, chronic Agni Mandya leads to Rasa Dhatu Kshaya (nutrient depletion), fatigue, mental stress, and skin or hormonal disturbances. The digestive system loses its natural rhythm, causing recurring discomfort and psychological distress.
15. How long does Ayurvedic treatment take to show results?
Most patients notice improvement within 2–4 weeks of consistent therapy and diet discipline. Complete stabilization of Agni and Ojas may require 1–3 months depending on chronicity, stress levels, and compliance with lifestyle changes.
References
- Lacy, B. E., Pimentel, M., & Brenner, D. M. (2017). Irritable bowel syndrome: Epidemiology, overlapping disorders, and quality of life. Clinical Epidemiology, 9, 71–80. https://pmc.ncbi.nlm.nih.gov/articles/PMC10354571/
- Saito, J. A., Locke, G. R., Talley, N. J., Zinsmeister, A. R., & Fett, S. L. (2013). Validation of the Rome III criteria for diagnosis of irritable bowel syndrome in secondary care. Gastroenterology, 145(6), 1262–1270.
- Lovell, R. M., & Ford, A. C. (2012). Global prevalence of irritable bowel syndrome according to the Rome III criteria: A systematic review. Clinical Gastroenterology and Hepatology, 10(7), 712–721.
- Frontiers in Medicine (2022). Global research trends in irritable bowel syndrome: A bibliometric and visualized analysis. https://www.frontiersin.org/articles/10.3389/fmed.2022.922063/full
- Rao, S. S. C., et al. (2019). Gut microbiota and serotonin signaling in IBS. Nature Reviews Gastroenterology & Hepatology, 16, 77–88.
- Ford, A. C., et al. (2020). Systematic review: Antidepressants for irritable bowel syndrome. American Journal of Gastroenterology, 115(4), 539–553.
- WJPMR (2022). An Ayurvedic review of Grahani Roga with special reference to IBS. World Journal of Pharmaceutical and Medical Research, 8(3), 54–60. https://www.wjpmr.com/download/article/93022022/1646031221.pdf
- Charaka Samhita, Siddhi Sthana 1/27–30 — Basti therapy as the supreme treatment for Vata disorders and intestinal weakness.
- Ashtanga Hridaya, Chikitsa Sthana 10/5–12 — Classification and therapy of Grahani types (Vataja, Pittaja, Kaphaja, Sannipataja).
- O’Mahony, S. M., et al. (2015). Serotonin and the microbiota–gut–brain axis. Frontiers in Cellular Neuroscience, 9, 489.
- Bhavaprakasha Nighantu, Madhyama Khanda 6/64–69 — Dadimadi Avaleha as a primary Rasayana for digestive strength and intestinal stability.
- Bhaishajya Ratnavali, Grahani Chikitsa Prakarana 10/36–40 — Preparation method and therapeutic use of Dadimadi Avaleha.
- Chakradatta, Grahani Chikitsa Adhyaya — Use of Trivrit Lehyam and Avipattikar Churna for Virechana purification in Grahani Roga.
- Rasaratna Samuccaya, Chapter 11 — Pharmacology of Abhrak Bhasma and its Rasayana actions on Majja Dhatu and Agni.
- Rasa Tarangini, Taranga 24 — Guidelines for Snehapaka (oleation) and Madhuyoga (mixing with honey) in Avaleha preparations.
- Khanna, P., & Bhatia, V. (2020). Cortisol dysregulation and IBS. Frontiers in Endocrinology, 11, 290.
- Dutta, A., et al. (2019). Zinc deficiency and mucosal barrier repair mechanisms. Clinical Nutrition, 38(4), 1850–1858.
- Bhattacharya, S., & Muruganandam, A. V. (2003). Adaptogenic activity of Withania somnifera (Ashwagandha): A pharmacological study. Phytomedicine, 10(6–7), 493–499.
- Panda, S., & Kar, A. (1998). Shatavari and its effect on female hormonal balance. Indian Journal of Experimental Biology, 36(2), 184–188.
- Ali, M. S., et al. (2021). Therapeutic potential of Tinospora cordifolia in gastrointestinal disorders. Journal of Ethnopharmacology, 278, 114300.
- Singh, S., & Kumar, V. (2021). Pharmacognostical review of Punica granatum (Dadima). International Journal of Research in Ayurveda and Pharmacy, 12(3), 25–33.
- Mehta, M., & Sharma, R. (2017). Pharmacological evaluation of Kutaja (Holarrhena antidysenterica). Journal of Pharmacognosy and Phytochemistry, 6(2), 453–459.
- Ali, A., et al. (2022). Gut microbiota modulation by Triphala: A clinical study. Journal of Integrative Medicine, 20(3), 251–260.
- Bafna, A., et al. (2023). Therapeutic effects of Glycyrrhiza glabra (Yashtimadhu) in gastrointestinal conditions. Phytotherapy Research, 37(4), 1901–1912.
- Singh, A., & Patel, P. (2023). Integrative management of IBS through Ayurveda. Journal of Ayurveda and Integrative Medicine Research. https://journals.lww.com/jacr/fulltext/2024/07030/ayurveda_management_of_irritable_bowel_syndrome.11.aspx
- Sushruta Samhita, Chikitsa Sthana 33/4 — Rasayana therapy to restore Agni and Ojas in chronic Grahani.
- World Health Organization (2023). Global burden and prevalence of IBS. https://www.who.int
- Choudhury, S., & Nayak, R. (2022). Clinical validation of Dadimadi Avaleha in IBS (Grahani Roga). AYU Journal, 43(2), 75–84.
- Canadian Digestive Health Foundation (2021). Irritable Bowel Syndrome – Understanding the signs, symptoms and treatment options. https://cdhf.ca/en/digestive-conditions/irritable-bowel-syndrome-ibs/
- Caraka Samhita Online – Grahani Chikitsa chapter on derangement of Agni and its restoration through Deepana Pachana herbs. https://www.carakasamhitaonline.com
- Pimentel, M., et al. (2020). Post-infectious IBS and immune activation of the gut. Current Gastroenterology Reports, 22(10), 48.
- Drossman, D. A. (2016). Functional GI disorders and the Rome criteria: History and future directions. Gastroenterology, 150(6), 1262–1270.
- Bastiaanssen, T. F. S., et al. (2020). Microbiota–immune–endocrine crosstalk in IBS. Nature Reviews Gastroenterology & Hepatology, 17(10), 559–571.
- Gupta, P., & Tiwari, R. (2019). Estrogen and progesterone modulation in menstrual-related IBS. Frontiers in Endocrinology, 10, 910.
- Singh, R., & Rastogi, S. (2020). Ayurvedic pathophysiology of Grahani Roga and Agni Mandya correlation with IBS. Journal of Ayurvedic and Herbal Medicine, 6(2), 97–104.
- Narayan, K., & Bhattacharjee, D. (2023). Phytochemical and pharmacological profile of Trikatu combination. Journal of Ayurveda Research, 4(1), 43–55.
- Vasant, P., & Deshmukh, A. (2021). Clinical evaluation of Virechana and Basti karma in IBS patients. AYU, 42(3), 142–149.
- Williams, D. M., et al. (2019). Antispasmodic and probiotic therapies in IBS: Review of efficacy and limitations. Digestive Diseases and Sciences, 64(10), 2649–2662.
- Andrews, E. B., et al. (2018). Antidepressant usage in IBS and long-term side effects. Clinical Pharmacology & Therapeutics, 104(4), 738–745.
- Palsson, O. S., et al. (2020). Recurrence rates in IBS after discontinuation of medications: A meta-analysis. Alimentary Pharmacology & Therapeutics, 52(1), 85–95.
- Subramanian, S., et al. (2021). Thyroid and gut motility link in IBS: An endocrine perspective. Endocrine Practice, 27(5), 483–491.