- IBS Ayurvedic Treatment and Why Conventional IBS Treatment Often Plateaus
- IBS Through the Ayurvedic Grahani Framework
- Dosha Based Personalization in IBS
- Treatment Philosophy Correction Before Suppression
- Treatment Philosophy Correction Before Suppression
- Detox and Gut Reset Applied Carefully Not Aggressively
- Rasayana Therapy Preventing Relapse
- Diet as Primary Treatment Not Restriction
- The Stress Gut Connection in IBS
- How Long Does Ayurvedic IBS Treatment Take
- Can IBS Be Permanently Resolved
- Summary
- FAQs
IBS Ayurvedic Treatment and Why It Matters Today
IBS Ayurvedic treatment offers a fundamentally different way of understanding irritable bowel syndrome, especially for patients in the USA and UK who continue to suffer despite normal test results. You may have been told that IBS is a lifelong condition, that there is no structural disease, and that symptom control is the only realistic goal. Yet the pain, bloating, bowel irregularity, and food sensitivity you experience are real and disruptive. Modern medicine classifies IBS as a functional disorder, meaning the dysfunction lies in regulation rather than visible damage, which explains why scans and colonoscopies often appear normal [1][2][4]. Ayurveda begins exactly at this functional level and asks why digestion lost stability and how it can be restored rather than suppressed.
Why IBS Feels Severe Even When Investigations Are Normal
From a Western clinical standpoint, IBS is defined by altered gut function without identifiable pathology, a concept that often leaves patients feeling unheard or dismissed. You feel symptoms daily, yet medical reassurance does not translate into relief. Ayurveda does not see this gap as psychological or imaginary. It recognizes that digestion can malfunction at the level of coordination, sensitivity, absorption, and nervous regulation long before structural disease appears [1][4]. When this functional layer is ignored, treatment plateaus. When it is corrected, symptoms often begin to settle naturally instead of cycling endlessly.
How Ayurveda Approaches IBS From a Different Starting Point
Ayurveda understands IBS through the concept of Grahani, which represents the digestive and absorptive intelligence of the gut. When digestive fire becomes weak, unstable, or hypersensitive, intestinal rhythm is lost, leading to fluctuating bowel habits, stress induced flare ups, and changing food tolerance. This framework explains why IBS symptoms are inconsistent and why emotional stress can immediately affect digestion [1][3]. For you as a patient, this shifts the treatment goal from lifelong symptom management to long term digestive correction. For clinicians, it offers a structured way to address IBS at its regulatory core rather than at the surface level.
What You Will Gain From This Section
In this section, you will understand how IBS Ayurvedic treatment works step by step, why personalization is essential, why diet alone rarely resolves IBS, how stress and the gut are directly connected, and why healing follows phases rather than instant results [2][4][7]. Whether you are a patient seeking lasting relief or a practitioner exploring integrative care, this introduction sets the foundation for viewing IBS as a functional imbalance that can be corrected rather than a permanent diagnosis that must be endured.
For readers who want a complete explanation covering IBS diagnosis, symptoms, and the full Ayurvedic treatment framework in one place, the detailed pillar guide is available here https://panaceayur.com/ibs-ayurvedic-treatment-diagnosis-symptoms-cure/
IBS Ayurvedic Treatment and Why Conventional IBS Treatment Often Plateaus
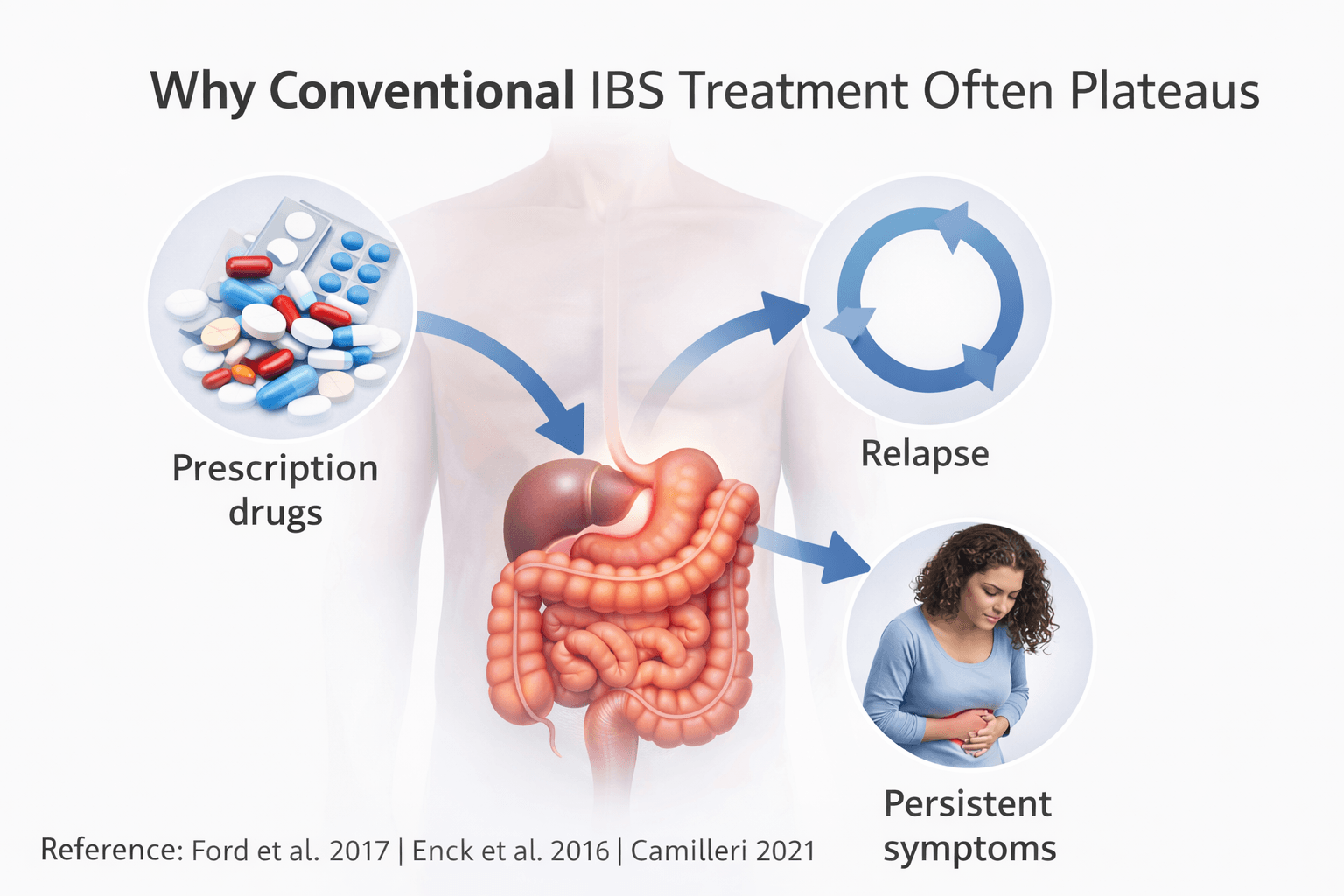
Why Symptom Focused IBS Medications Provide Only Temporary Relief
IBS Ayurvedic treatment often enters a patient’s journey after conventional therapies stop delivering sustained improvement. You may initially respond to antispasmodics, laxatives, antidiarrheals, acid suppressants, or gut targeted neuromodulators, yet this relief is frequently incomplete or short lived. Modern gastroenterology literature clearly explains that most IBS medications are designed to suppress dominant symptoms rather than correct the underlying functional disturbance of the gut [2][4]. These drugs do not restore digestive coordination, normalize gut sensitivity, or recalibrate gut brain signaling. As a result, once medication is reduced, stopped, or psychologically stressed conditions arise, symptoms often return. From the patient’s perspective, this creates a cycle of hope followed by disappointment. From the clinician’s perspective, it reflects the inherent limitation of treating a regulatory disorder with symptom specific tools [7].
Why IBS Relapses Despite Ongoing Medical Management
IBS is now understood as a disorder involving altered gut motility, visceral hypersensitivity, and dysregulated gut brain communication rather than fixed structural disease [4]. This means the condition is dynamic, adaptive, and responsive to stress, diet, sleep, and emotional state. When treatment focuses only on controlling bowel frequency or pain perception, the deeper regulatory imbalance continues unchecked. You may notice that the same medication works for months and then loses effect, or that constipation shifts to diarrhea, bloating replaces pain, or food tolerance changes unexpectedly. These shifts are not random. They reflect the fluctuating nature of IBS physiology, which conventional treatment models struggle to stabilize long term [2]. Relapse, therefore, is not a failure of compliance but a consequence of unresolved functional imbalance.
Why Long Term IBS Management Reaches a Clinical Ceiling
Clinical guidelines acknowledge that IBS often requires repeated medication adjustments, combination therapies, and long term follow up, yet complete resolution remains uncommon [7]. Over time, both patients and clinicians reach a therapeutic ceiling where symptom reduction plateaus despite optimal guideline based care. At this stage, treatment becomes focused on coping rather than correction. IBS Ayurvedic treatment diverges precisely at this point. Instead of escalating symptom suppression, it seeks to restore digestive stability, reduce gut hypersensitivity, and retrain regulatory mechanisms so that symptoms are no longer constantly triggered. Understanding why conventional IBS treatment plateaus provides the clinical rationale for exploring a corrective, root focused approach aimed at long term stability rather than cyclical symptom control.
IBS Through the Ayurvedic Grahani Framework
Functional Gut Brain Dysregulation Explained Through Ayurveda and Modern Science
IBS is now understood in modern medicine as a disorder of gut brain interaction, where regulation fails despite the absence of structural disease [1][3]. Ayurveda described this functional failure thousands of years ago through the concept of Grahani, the system that governs digestion, absorption, and intestinal coordination. Charaka clearly states that digestion is not merely mechanical but dependent on regulatory intelligence. When this intelligence is disturbed, disease manifests even if organs appear structurally normal. This explains why IBS patients experience severe symptoms despite normal investigations and why reassurance alone does not translate into healing.
Charaka Samhita explains
“Grahani hi Agni adhishthana”
Charaka Samhita Chikitsa Sthana Grahani Chikitsa Adhyaya [8]
This verse establishes that Grahani is the seat of digestive fire. When Agni becomes unstable, Grahani itself becomes dysfunctional. This directly parallels modern understanding that IBS arises from dysregulated gut brain signaling rather than visible intestinal damage [1][3].
Grahani as the Digestive and Absorptive Intelligence of the Gut
In Ayurveda, Grahani is not a single anatomical organ but the functional intelligence that holds food, digests it, and releases it at the correct time. When Grahani functions normally, digestion is complete and bowel habits are stable. When Grahani is disturbed, digestion becomes irregular, absorption is impaired, and intestinal rhythm is lost. Classical Ayurvedic texts describe this state with symptoms that strongly resemble IBS, including alternating bowel habits, bloating, abdominal discomfort, fatigue, and intolerance to food.
Charaka Samhita states
“Dushta Grahani na pachati samyak”
Charaka Samhita Chikitsa Sthana [8]
This means that a disturbed Grahani fails to digest food properly. This single line explains why IBS patients feel unwell after meals, why symptoms fluctuate, and why digestion feels unpredictable rather than consistently weak or strong. From a modern standpoint, this reflects altered motility and visceral hypersensitivity seen in IBS [1][3].
Agni Dysfunction as the Central Cause of IBS
Ayurveda places Agni at the center of all digestive disorders. In IBS, Agni is rarely completely weak or excessively strong. Instead, it becomes unstable, irregular, and reactive. This explains why one day digestion feels normal and the next day the same food triggers pain or urgency. Classical texts emphasize that irregular Agni produces irregular disease expression.
Ashtanga Hridaya states
“Mandagni vishamagni tikshnagni cha roga karanam”
Ashtanga Hridaya Sutra Sthana [9]
This verse explains that weak, irregular, and excessive Agni all lead to disease. IBS fits most closely with Vishama Agni, irregular digestive fire, which explains alternating constipation and diarrhea, variable appetite, and sensitivity to stress. Modern gastroenterology similarly recognizes IBS as a disorder of fluctuating motility and sensitivity rather than a fixed pathology [1][3].
Ama Formation and the Cycle of Fluctuating IBS Symptoms
When Agni is unstable, digestion remains incomplete, leading to the formation of Ama. Ayurveda describes Ama as improperly processed metabolic material that disrupts physiological signaling rather than a chemical toxin. Ama interferes with absorption, increases gut sensitivity, and weakens digestive confidence. In IBS, this explains bloating, heaviness, fatigue, brain fog, and worsening symptoms after meals even when food quality is good.
Charaka Samhita explains
“Ama sarva roganam mulam”
Charaka Samhita Sutra Sthana [8]
This verse states that Ama is the root of many diseases. In IBS, Ama perpetuates Grahani dysfunction, creating a self sustaining cycle where poor digestion worsens gut sensitivity, and increased sensitivity further weakens digestion. Modern research echoes this through findings related to altered microbial signaling and immune activation in IBS [3].
Why the Grahani Framework Explains IBS Variability Better Than Structural Models
One of the most confusing aspects of IBS is its inconsistency. Symptoms worsen with stress, improve temporarily, shift patterns, and defy rigid classification. Structural disease models fail to explain this behavior. The Grahani framework explains IBS variability by recognizing digestion as a dynamic regulatory system that responds to mental state, routine, and environmental input.
Ashtanga Hridaya states
“Manaso hi agni vaishamyam”
Ashtanga Hridaya [9]
This indicates that mental disturbance directly affects digestive fire. This verse provides a classical explanation for the stress induced flare ups seen in IBS and aligns precisely with modern gut brain axis research [1][3]. By viewing IBS through the Grahani framework, both patients and clinicians gain a coherent explanation for symptom variability and a rational basis for corrective treatment focused on restoring digestive intelligence rather than repeatedly suppressing symptoms.
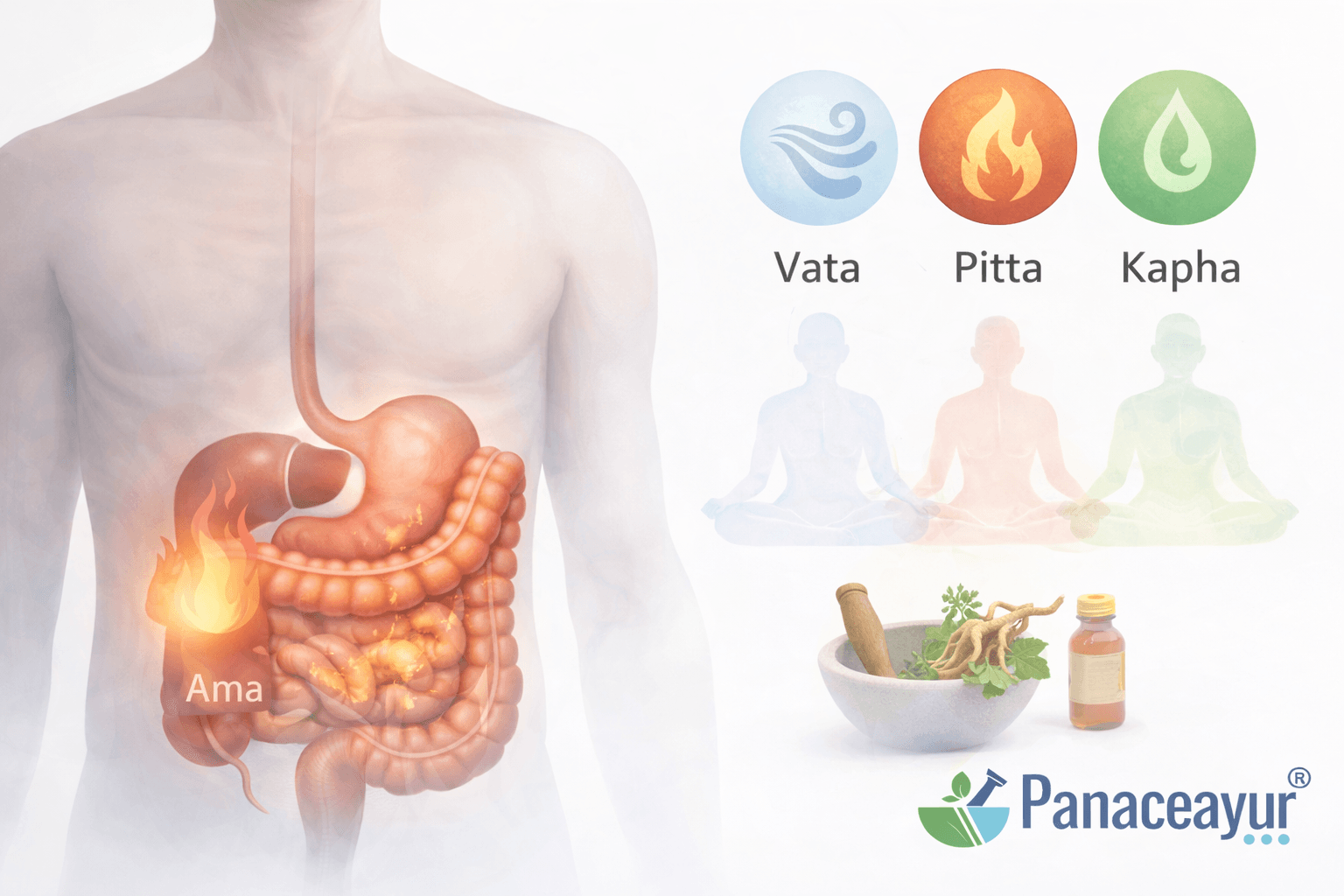
Dosha Based Personalization in IBS
Why IBS Cannot Be Treated as a Single Uniform Disorder
IBS is now clearly recognized in modern gastroenterology as a heterogeneous condition with wide variability in symptoms, triggers, and clinical course [4]. Some patients predominantly experience constipation and bloating, others diarrhea and urgency, while many fluctuate between patterns depending on stress, sleep, hormones, and diet. This variability explains why standardized drug based protocols often provide only partial or temporary relief. Ayurveda anticipated this diversity thousands of years ago by emphasizing that digestive disorders must be understood at the individual level rather than through a single disease label. Treatment is therefore planned according to the dominant Dosha imbalance rather than applied uniformly to all patients with the same diagnosis.
“Purusham purusham veekshya”
Charaka Samhita, Vimana Sthana, Chapter 8, Shloka 95
Meaning: Each individual must be examined separately before deciding treatment [8]
Vata Dominant IBS and Irregular Digestive Regulation
Vata dominant IBS is characterized by instability and irregularity in digestion. Patients commonly experience bloating, abdominal pain, gurgling sounds, dryness, anxiety related flare ups, constipation alternating with loose stools, and worsening symptoms during travel, irregular routines, or emotional stress. Ayurveda describes Vata as the governing force of movement and regulation. When aggravated in the digestive tract, it disrupts coordination and rhythm rather than producing inflammation. This explains why symptoms are unpredictable and fluctuate frequently. Modern medicine similarly recognizes altered motility and visceral hypersensitivity as central mechanisms in IBS, particularly in patients with variable bowel habits [4].
“Vata prakopena vishama kriya bhavati”
Charaka Samhita, Chikitsa Sthana, Chapter 15, Shloka 56
Meaning: When Vata is aggravated, bodily functions become irregular and unstable [8]
Pitta Dominant IBS and Heat Driven Digestive Disturbance
Pitta dominant IBS presents with heat related digestive symptoms such as loose stools, urgency, burning sensations, acidity, nausea, irritability, and symptom worsening during stress or heat exposure. Ayurveda associates Pitta with metabolic intensity and transformation. When Pitta becomes excessive in the gut, digestion becomes overly sharp and reactive, leading to irritation rather than proper nourishment. This explains diarrhea predominant IBS patterns and post meal urgency. Modern gastroenterology also recognizes a subgroup of IBS patients with accelerated intestinal transit and heightened gut sensitivity in the absence of structural disease [4].
“Tikshna agni pittaja rogan karoti”
Ashtanga Hridaya, Sutra Sthana, Chapter 12, Shloka 5
Meaning: Excessively sharp digestive fire leads to Pitta related disorders [9]
Kapha Dominant IBS and Sluggish Digestive Function
Kapha dominant IBS is marked by heaviness, sluggish digestion, constipation, mucus in stools, nausea, lethargy, and a persistent sense of fullness even after small meals. Ayurveda associates Kapha with structure and stability, but when excessive it suppresses digestive fire and slows intestinal movement, resulting in incomplete digestion and impaired evacuation. Modern literature acknowledges that some IBS patients demonstrate delayed gut motility and reduced gut responsiveness without anatomical obstruction [4].
“Kapha vriddhi mandagni karanam”
Charaka Samhita, Sutra Sthana, Chapter 28, Shloka 9
Meaning: Increase of Kapha leads to weakening of digestive fire [8]
Why Dosha Based Classification Enables True Individualized IBS Care
Ayurveda consistently emphasizes that effective treatment depends on understanding Dosha dominance, secondary imbalances, and their interaction with lifestyle and mental state. Dosha based classification allows IBS treatment to be corrective rather than suppressive, addressing the specific regulatory imbalance driving symptoms instead of chasing bowel patterns. This approach aligns with modern recognition that IBS management must be individualized rather than protocol driven [4]. By restoring digestive intelligence according to Dosha patterns, Ayurvedic treatment aims for long term stability rather than cyclical symptom control.
“Rogam adau parikshya tatah aushadham prayojayet”
Charaka Samhita, Vimana Sthana, Chapter 8, Shloka 94
Meaning: Disease and patient must be thoroughly examined before selecting treatment [8]
Treatment Philosophy Correction Before Suppression
Why Symptom Suppression Fails to Produce Lasting IBS Relief
IBS treatment in conventional medicine often focuses on suppressing dominant symptoms such as diarrhea constipation pain or urgency. While this approach may provide temporary comfort it rarely produces lasting stability because it does not correct the underlying functional disturbance driving the condition [2][7]. Many patients experience an initial response followed by diminishing benefit recurrence of symptoms or shifting symptom patterns over time. This happens because suppressing bowel output or dulling pain signals does not restore digestive coordination gut sensitivity or rhythmic regulation. IBS is a dynamic functional disorder and when its regulatory core remains uncorrected symptom control alone reaches a therapeutic ceiling [7].
Ayurveda Focuses on Correcting Digestive Intelligence Rather Than Forcing Output
Ayurveda approaches IBS from a fundamentally different therapeutic philosophy. Instead of asking how to stop symptoms it asks why digestion lost its stability and how that stability can be restored. Central to this approach is Agni the digestive fire that governs digestion absorption and intestinal rhythm. When Agni is corrected bowel movements tend to normalize naturally without force. This explains why Ayurveda avoids aggressive laxatives antidiarrheals or stimulants in early treatment and instead prioritizes digestive correction and coordination.
“Agni dushti sarva roganam karanam”
Charaka Samhita, Chikitsa Sthana, Grahani Chikitsa Adhyaya
Meaning: Disturbance of digestive fire is the cause of all diseases [8]
Restoring Coordination Before Strengthening or Cleansing
Ayurvedic treatment emphasizes sequence. Strengthening therapies detoxification or rejuvenation are not applied before digestive coordination is restored. When digestion is unstable forcing bowel movements can worsen gut sensitivity and deepen dysregulation. By first stabilizing Agni and Grahani the digestive system regains rhythm which allows later therapies to work effectively. This principle explains why patients who self medicate with strong herbal laxatives or suppressive agents often experience worsening IBS symptoms over time.
“Na hi agni samyak sthite roga shamyati”
Charaka Samhita, Sutra Sthana
Meaning: Disease does not resolve unless digestive fire is properly established [8]
Why Corrective Treatment Leads to Sustainable Outcomes
Corrective treatment aims to retrain digestion rather than override it. As digestive coordination improves gut sensitivity reduces food tolerance expands and symptom frequency decreases without constant intervention. Modern gastroenterology acknowledges that long term IBS management requires more than symptom control alone and that patient outcomes improve when treatment addresses underlying functional mechanisms [2][7]. Ayurveda operationalizes this insight by focusing on restoring digestive intelligence first which explains why its approach emphasizes correction before suppression and long term stability over short term control.
This corrective approach is explained step by step in the comprehensive IBS pillar resource that integrates diagnosis, treatment logic, and long-term management here https://panaceayur.com/ibs-ayurvedic-treatment-diagnosis-symptoms-cure/
Treatment Philosophy Correction Before Suppression
Why Symptom Suppression Fails to Produce Lasting IBS Relief
Conventional IBS management is largely built around suppressing visible symptoms such as diarrhea constipation abdominal pain urgency or bloating. While this approach can provide short term comfort it consistently fails to deliver long term stability because it does not correct the underlying functional dysregulation driving the condition [2][7]. IBS is not caused by a fixed structural defect but by disturbed coordination between digestion gut sensitivity and nervous regulation. When medications blunt bowel activity or pain perception without restoring digestive intelligence the body adapts but does not heal. Over time patients notice diminishing benefit recurrence of symptoms or transformation of symptom patterns from constipation to diarrhea or from pain to bloating. This plateau is not a treatment failure but a predictable outcome of symptom focused therapy applied to a regulatory disorder [7].
Ayurveda Focuses on Correcting Digestive Intelligence Rather Than Forcing Output
Ayurveda approaches IBS from a fundamentally different therapeutic philosophy. Instead of asking how to stop bowel symptoms it asks why digestion lost its stability and how that stability can be restored. At the center of this approach lies Agni the digestive fire that governs digestion absorption metabolic rhythm and intestinal coordination. When Agni functions properly bowel movements normalize naturally without force and food tolerance gradually improves. This is why Ayurveda avoids early reliance on laxatives antidiarrheals or suppressive agents and instead prioritizes correcting digestive intelligence itself. Classical Ayurvedic texts emphasize that disturbed Agni is the primary driver of digestive disease rather than the bowel movement alone.
“Agni dushti sarva roganam karanam”
Charaka Samhita, Chikitsa Sthana, Grahani Chikitsa Adhyaya, Chapter 15, Shloka 44
Meaning: Disturbance of digestive fire is the root cause of disease [8]
Restoring Digestive Coordination Before Strengthening or Cleansing
Ayurvedic treatment is governed by sequence and timing. Strengthening therapies cleansing procedures or rejuvenative medicines are not applied until digestive coordination is first stabilized. When digestion is unstable forcing bowel evacuation or suppressing output can worsen gut sensitivity and deepen dysregulation. Many IBS patients deteriorate after unsupervised detox regimens or aggressive herbal interventions because the digestive system is not yet capable of handling them. Ayurveda teaches that Grahani must regain rhythmic control before any further therapeutic step can succeed. Only when digestion becomes steady can deeper therapies act constructively rather than aggravate symptoms.
“Na hi agni samyak sthite roga shamyati”
Charaka Samhita, Sutra Sthana, Chapter 27, Shloka 349
Meaning: Disease does not subside unless digestive fire is properly established [8]
Why Corrective Treatment Leads to Sustainable Outcomes
Corrective treatment retrains digestion instead of overriding it. As digestive coordination improves gut hypersensitivity reduces bowel patterns stabilize and food tolerance expands naturally. Patients experience fewer flares improved confidence around eating and reduced dependence on medications. Modern gastroenterology now acknowledges that long term IBS outcomes improve only when treatment addresses functional mechanisms rather than symptom expression alone [2][7]. Ayurveda operationalizes this insight through Agni centered correction which explains why its therapeutic philosophy emphasizes restoring digestive intelligence first and suppressing symptoms only when absolutely necessary. This is why correction before suppression is not an alternative belief system but a rational clinical strategy for achieving lasting stability in IBS.
Detox and Gut Reset Applied Carefully Not Aggressively
Why Aggressive Detox Often Worsens IBS Instead of Healing It
Many IBS patients in the USA and UK are drawn toward detoxes cleanses and elimination protocols out of frustration with persistent symptoms. Modern clinical guidelines caution that unnecessary or excessive interventions can destabilize gut function and worsen outcomes in functional disorders [6][7]. IBS involves heightened gut sensitivity and dysregulated motility rather than toxin accumulation in the conventional sense. When aggressive purgation fasting or repeated cleansing is applied to an already unstable digestive system it can increase visceral hypersensitivity provoke flares and prolong recovery. Ayurveda recognized this risk centuries ago and explicitly warned against cleansing therapies in individuals with weak or irregular digestion. Detox in IBS therefore requires discernment rather than enthusiasm.
Ayurvedic View of Shodhana as a Selective Therapeutic Tool
In Ayurveda Shodhana refers to purificatory therapies designed to remove pathological accumulation only when the body is prepared to handle them. These therapies are never universal and are contraindicated when digestive fire is weak unstable or exhausted. IBS patients often fall into this vulnerable category because their digestion lacks consistency and resilience. Ashtanga Hridaya clearly states that purification should not be performed without assessing digestive strength and patient capacity.
“Balino ye cha shodhyah syuh te shodhyah”
Ashtanga Hridaya, Sutra Sthana, Chapter 18, Shloka 46
Meaning: Only those who are strong and properly prepared should undergo purification therapies [9]
This principle directly applies to IBS where indiscriminate detox can worsen Grahani instability rather than correct it.
Gentle Gut Reset Before Any Cleansing Is Attempted
Ayurveda emphasizes that the first step in gut reset is not evacuation but stabilization. Before any detox is considered digestion must regain rhythm appetite clarity and tolerance to simple foods. This phase focuses on calming gut reactivity restoring coordination and reducing hypersensitivity. Only when digestion becomes steady does the question of cleansing arise. Charaka emphasizes that improper timing of cleansing weakens digestion further instead of healing disease.
“Shodhanam durbalasya roga vardhanam”
Charaka Samhita, Sutra Sthana, Chapter 16, Shloka 13
Meaning: Cleansing performed in a weak individual increases disease rather than curing it [9]
For IBS patients this explains why repeated detox attempts often lead to relapse worsening symptoms or new sensitivities.
When Detox Is Appropriate in IBS and When It Is Not
Detox in IBS is not routine and not mandatory. It is considered only when specific signs of pathological accumulation are present and when digestion has sufficient strength to tolerate intervention. Modern gastroenterology similarly cautions against unnecessary procedures in IBS and emphasizes minimal effective intervention [6][7]. Ayurveda aligns with this restraint by recommending selective gentle Shodhana only in well assessed cases. In many IBS patients dietary correction digestive stabilization and nervous system regulation alone are sufficient to achieve significant improvement without any formal detox.
Why Careful Gut Reset Produces Better Long Term Outcomes
When gut reset is approached gently it reduces reactivity builds confidence in digestion and prepares the system for deeper healing. Patients experience fewer flares improved tolerance to food and reduced dependence on interventions. Modern guidelines emphasize avoiding overtreatment in IBS because excessive intervention itself becomes a trigger [6][7]. Ayurveda operationalizes this wisdom through its insistence on timing strength and indication. This is why detox and gut reset in IBS must be applied carefully not aggressively and always as a supportive step rather than a forced solution.
Rasayana Therapy Preventing Relapse
Why IBS Relapse Occurs Even After Initial Improvement
Many IBS patients experience meaningful improvement once digestion is corrected and triggers are controlled, yet relapse remains common when treatment stops too early. Modern research on the gut brain axis confirms that long term stability depends on resilience of neural signaling stress regulation and adaptive capacity rather than short term symptom resolution [3]. If the digestive system regains function but not strength it remains vulnerable to stress infections dietary changes and emotional load. Ayurveda recognized this risk and therefore placed Rasayana therapy after Grahani correction rather than at the beginning of treatment. The purpose of Rasayana is not to treat acute symptoms but to consolidate healing so that improvement becomes durable rather than fragile.
Rasayana as Digestive and Nervous System Stabilization
In Ayurveda Rasayana refers to therapies that restore tissue strength coordination and regenerative capacity. After Grahani and Agni have been stabilized Rasayana supports the digestive tract nervous regulation and systemic resilience. This is particularly relevant in IBS where gut sensitivity and stress responsiveness are central drivers of relapse. Classical texts describe Rasayana as strengthening both bodily tissues and mental steadiness which mirrors modern understanding of gut brain resilience [3]. Rasayana therefore functions as a stabilizer that protects the gains achieved during corrective treatment and prevents regression.
“Rasayanam tu balam medha ayuh pradam”
Charaka Samhita, Chikitsa Sthana, Rasayana Adhyaya, Chapter 1, Shloka 7
Meaning: Rasayana promotes strength intelligence and longevity [8]
Preventing Recurrence Through Tissue Repair and Coordination
IBS relapse often occurs because underlying tissues remain sensitive even after symptoms subside. Ayurveda explains that when Dhatus are weak they fail to support stable digestive function under stress. Rasayana therapy nourishes these tissues gradually improving tolerance adaptability and coordination. Ashtanga Hridaya emphasizes that Rasayana restores balance only when digestion is already corrected which is why premature use is discouraged.
“Agni sampanne rasayanam shreshtham”
Ashtanga Hridaya, Sutra Sthana, Chapter 13, Shloka 1
Meaning: Rasayana works best when digestive fire is properly established [9]
This principle explains why Rasayana is introduced only after Grahani correction and why it plays a decisive role in preventing IBS recurrence rather than chasing symptoms.
Rasayana and Long Term Gut Brain Resilience
Modern gut brain research highlights that long term IBS stability depends on reducing stress reactivity improving neural adaptability and restoring confidence in digestion [3]. Rasayana directly supports these goals by strengthening both physiological and psychological resilience. Patients often report improved stress tolerance stable appetite better sleep and reduced fear of food during this phase. These changes indicate restoration of gut brain harmony rather than mere symptom control. Ayurveda therefore views Rasayana as essential for preventing relapse because it addresses the system’s capacity to remain balanced under real life pressures.
Why Rasayana Completes the IBS Healing Process
Correction stabilizes digestion detox clears obstacles and Rasayana secures long term balance. Without Rasayana IBS treatment remains vulnerable to recurrence even if initial results are good. Classical Ayurvedic texts repeatedly emphasize that lasting health depends on strengthening what has been corrected rather than repeatedly fixing what has collapsed. By consolidating digestive intelligence tissue resilience and nervous stability Rasayana therapy transforms improvement into durability.
“Na hi rasayanad ritam sthirata”
Charaka Samhita, Chikitsa Sthana, Rasayana Adhyaya, Chapter 1, Shloka 8
Meaning: Without Rasayana stability cannot be maintained [8]
This is why Rasayana therapy is not optional in IBS care aimed at preventing relapse but a necessary final step in achieving lasting digestive health.
Diet as Primary Treatment Not Restriction
Why Restrictive Diets Often Fail in IBS
Diet is frequently presented to IBS patients as a list of foods to avoid, leading to long term restriction anxiety and nutritional imbalance. Modern clinical guidance acknowledges that while diet modification can reduce symptoms it is incomplete when used alone and may even worsen quality of life if applied rigidly [6][10]. IBS involves altered regulation and sensitivity, not a universal intolerance to specific foods. When restriction becomes permanent the gut fails to relearn tolerance and confidence around eating diminishes. Ayurveda anticipated this limitation and therefore rejected blanket elimination as a primary strategy, viewing diet instead as a means to retrain digestion rather than permanently narrow it.
Diet as a Tool to Restore Agni and Digestive Rhythm
Ayurveda treats diet as a therapeutic instrument whose purpose is to restore Agni and reestablish digestive rhythm. Food is selected not by rigid categories but by its effect on digestive fire timing and coordination. When Agni is unstable even healthy foods can provoke symptoms, whereas once Agni is corrected tolerance naturally expands. Classical texts emphasize that food should support digestion rather than challenge it and that inappropriate dietary restriction weakens digestive strength over time.
“Ahara eva aushadham”
Charaka Samhita, Sutra Sthana, Chapter 25, Shloka 40
Meaning: Food itself is the primary medicine [8]
Why Permanent Avoidance Weakens Digestive Confidence
IBS patients often develop fear of food after repeated flares. While short term simplification may be necessary during acute instability permanent avoidance reduces digestive adaptability and reinforces hypersensitivity. Ayurveda explains that digestion improves through appropriate challenge once stability is restored, not through lifelong avoidance. Ashtanga Hridaya states that digestion strengthens when food is introduced in alignment with digestive capacity rather than removed indefinitely.
“Agni balam aharena vardhate”
Ashtanga Hridaya, Sutra Sthana, Chapter 8, Shloka 45
Meaning: Digestive fire is strengthened through appropriate nourishment [9]
This principle explains why IBS patients often relapse when overly restrictive diets are followed for long periods.
Individualized Diet Based on Digestive State Not Labels
Ayurveda does not prescribe one IBS diet. Dietary planning is based on digestive strength Dosha dominance meal timing preparation and quantity rather than food lists. What matters is how food is eaten digested and assimilated. Modern research similarly shows that dietary response in IBS is highly individual and that no single diet works universally [6][10]. Ayurveda formalizes this individuality by matching diet to digestive state rather than diagnosis alone.
How Therapeutic Diet Supports Long Term Stability
When diet is used therapeutically it stabilizes digestion reduces gut reactivity and gradually restores food tolerance. Patients experience fewer flares improved appetite and reduced anxiety around meals. Classical texts emphasize that once digestion stabilizes food itself maintains health without excessive intervention.
“Pathya sevito roga na punar bhavati”
Charaka Samhita, Chikitsa Sthana, Chapter 1, Shloka 124
Meaning: Disease does not recur when proper diet is followed [8]
This is why Ayurveda positions diet as a primary treatment tool rather than a lifelong restriction and integrates it with digestive correction to achieve lasting IBS stability.
The Stress Gut Connection in IBS
Why Stress Directly Triggers IBS Symptoms
IBS is now firmly recognized as a disorder of gut brain interaction rather than a disease confined to the intestines alone. Modern research confirms that stress directly alters gut motility sensitivity immune signaling and microbial balance through bidirectional communication between the central nervous system and the gastrointestinal tract [3][5]. For patients this explains why symptoms flare during emotional stress anxiety sleep disruption or mental overload even when diet remains unchanged. Stress does not merely aggravate IBS psychologically but actively modifies digestive function at a physiological level. Ayurveda described this phenomenon centuries ago by recognizing that mental disturbance immediately affects digestive fire and intestinal coordination.
“Manaso hi agni vaishamyam”
Ashtanga Hridaya, Sutra Sthana, Chapter 12, Shloka 7
Meaning: Disturbance of the mind leads to imbalance of digestive fire [9]
This principle explains why reassurance alone does not calm IBS and why addressing stress physiology is essential rather than optional.
How the Gut Brain Axis Sustains IBS Cycles
The gut brain axis operates as a continuous feedback loop. Stress alters gut signaling which increases sensitivity discomfort and bowel irregularity. These symptoms in turn reinforce anxiety hypervigilance and fear of food creating a self sustaining cycle. Modern neuroscience and microbiome research confirm that altered microbial signaling inflammatory mediators and vagal tone contribute to this loop [3][5]. Ayurveda explains the same cycle through disturbed Agni and Vata dominance where nervous regulation overrides digestive stability. Without interrupting this loop IBS remains reactive even when diet and digestion appear corrected.
Nervous System Modulation as a Core Therapeutic Target
Effective IBS care requires calming and retraining the nervous system rather than ignoring it. Modern clinical trials demonstrate that stress directed interventions such as nervous system modulation behavioral therapies and mind body regulation significantly improve IBS outcomes [11]. Ayurveda integrates this understanding intrinsically by addressing Vata regulation mental steadiness and digestive calm simultaneously. Therapies are chosen not only to correct digestion but to reduce nervous hyperreactivity so that the gut regains confidence and rhythm.
“Chinta shoka bhaya krodha agni nashanam”
Charaka Samhita, Sutra Sthana, Chapter 25, Shloka 23
Meaning: Anxiety grief fear and anger weaken digestive fire [8]
This verse highlights that emotional states are not secondary influences but direct causes of digestive instability.
Why Treating Stress Separately From Digestion Fails
In conventional care stress is often treated as an external factor while digestion is treated locally. This separation limits results. IBS improves most effectively when nervous regulation and digestion are addressed together. Modern integrative models now emphasize combined gut brain approaches acknowledging that isolated interventions rarely produce lasting stability [3][11]. Ayurveda has always treated the digestive tract and nervous system as inseparable, which is why therapies aimed at calming the mind often stabilize bowel patterns even without direct intestinal intervention.
Stress Regulation as the Foundation for Long Term IBS Stability
Long term IBS stability depends on reducing stress reactivity restoring nervous resilience and rebuilding trust in digestion. Patients who achieve this state experience fewer flares improved sleep better appetite and reduced fear around symptoms. Ayurveda views this not as psychological coping but as restoration of physiological harmony between mind and gut. When nervous stability is restored digestive fire remains steady and symptoms gradually lose their trigger.
“Prasanna atma indriya manah svasthya lakshanam”
Charaka Samhita, Sutra Sthana, Chapter 30, Shloka 26
Meaning: Health is characterized by balance of body senses and mind [8]
This is why the stress gut connection is not an accessory concept in IBS but a central pillar of effective and lasting treatment.
How Long Does Ayurvedic IBS Treatment Take
Why IBS Does Not Resolve in Weeks
IBS is a chronic functional disorder characterized by long standing dysregulation of digestion gut sensitivity and nervous coordination rather than an acute illness that resolves quickly. Modern gastroenterology literature confirms that IBS symptoms often persist for years with fluctuating intensity and that rapid resolution is uncommon even with optimal conventional care [2][4][7]. Many patients expect improvement within days or weeks because symptoms fluctuate naturally, but this variability should not be confused with true recovery. Ayurveda recognizes that when a condition develops gradually due to prolonged digestive and regulatory imbalance it must be corrected gradually rather than reversed abruptly.
“Chirakarena jatah roga chirakarena shamyati”
Charaka Samhita, Chikitsa Sthana, Chapter 1, Shloka 59
Meaning: Diseases that develop over a long time resolve only with sustained treatment [8]
This principle explains why IBS requires patience and why short term interventions rarely produce lasting change.
Phased Improvement Rather Than Linear Progress
Ayurvedic IBS treatment progresses in phases rather than a straight line. Initial phases focus on calming gut reactivity stabilizing bowel rhythm and reducing symptom intensity. Middle phases emphasize restoring digestive strength expanding food tolerance and reducing stress sensitivity. Later phases consolidate gains and prevent relapse through Rasayana and lifestyle correction. Modern clinical observations align with this pattern showing that IBS improvement occurs in stages with periods of stabilization and occasional mild setbacks [2][7]. Expecting uninterrupted improvement often leads to frustration and premature discontinuation of treatment.
Typical Timeframes for Meaningful Improvement
While individual timelines vary most patients begin to experience noticeable symptom stabilization within the first four to eight weeks once digestion and nervous regulation are addressed correctly. Deeper improvements such as consistent bowel habits reduced flare frequency and restored confidence around food typically require three to six months of sustained therapy. Long term resilience and relapse prevention may extend beyond this period depending on chronicity lifestyle stress and adherence. Modern IBS studies similarly indicate that meaningful recovery occurs over months rather than weeks especially in long standing cases [4][7].
“Na hi alpena kalena sthiratvam labhyate”
Ashtanga Hridaya, Sutra Sthana, Chapter 13, Shloka 25
Meaning: Stability is not achieved in a short period of time [9]
This reinforces the importance of realistic timelines in IBS care.
Factors That Influence Treatment Duration
The duration of Ayurvedic IBS treatment depends on several factors including how long symptoms have been present the dominant Dosha pattern digestive strength stress burden sleep quality and consistency of diet and routine. Patients with long standing IBS frequent relapses or significant stress exposure typically require longer consolidation phases. Modern research confirms that IBS outcomes are strongly influenced by psychological stress lifestyle patterns and treatment adherence rather than medication choice alone [2][4]. Ayurveda integrates these variables into treatment planning which is why timelines are personalized rather than fixed.
Why Patience Improves Outcomes
Patients who understand the gradual nature of IBS recovery tend to experience better outcomes because they allow sufficient time for digestive retraining nervous recalibration and tissue stabilization. Rushing treatment or frequently switching approaches disrupts progress and prolongs instability. Ayurveda teaches that healing follows rhythm rather than urgency and that stability once achieved is more important than speed.
“Yuktimad aushadham sevitam chiraya sukham dadati”
Charaka Samhita, Sutra Sthana, Chapter 9, Shloka 7
Meaning: Properly applied treatment given over time produces lasting benefit [8]
This is why Ayurvedic IBS treatment emphasizes sustained correction phased progress and patience as essential components of lasting recovery rather than quick fixes.
Can IBS Be Permanently Resolved
Why Modern Medicine Speaks of Remission Rather Than Cure
In modern gastroenterology IBS is described as a chronic functional disorder with a relapsing and remitting course rather than a disease that can be universally cured [1][7]. This language reflects clinical reality. Symptoms often improve significantly and may remain absent for long periods but can recur under stress illness or lifestyle disruption. The emphasis on remission acknowledges long term stability without promising permanence in every individual. This cautious framing is appropriate because IBS involves regulatory systems that are sensitive to future influences rather than a one time structural defect that can be permanently removed [1].
Ayurvedic Perspective on Sustained Correction of Grahani
Ayurveda approaches the question differently by focusing on whether the underlying functional disturbance has been fully corrected rather than whether symptoms have disappeared temporarily. IBS corresponds closely to Grahani Dosha where digestive coordination and Agni stability are impaired. Classical Ayurvedic texts state that when Grahani is restored to proper function and digestion regains strength disease does not recur easily. This does not imply immunity to all future digestive disturbance but indicates that the system regains resilience and self regulation.
“Samyak chikitsite grahani na punar bhavati”
Charaka Samhita, Chikitsa Sthana, Grahani Chikitsa Adhyaya, Chapter 15, Shloka 54
Meaning: When Grahani is properly treated it does not recur [8]
This statement reflects sustained correction rather than temporary suppression.
The Role of Complete Treatment and Consolidation
Ayurveda emphasizes that resolution depends on completing all phases of treatment including correction stabilization and consolidation. Partial treatment often leads to partial results. When Agni is corrected but not strengthened or when symptoms improve but Rasayana is omitted the system remains vulnerable. Ashtanga Hridaya highlights that stability depends on digestive fire being firmly established and supported over time.
“Agni sthiratvam arogyasya mulam”
Ashtanga Hridaya, Sutra Sthana, Chapter 13, Shloka 1
Meaning: Stability of digestive fire is the root of health [9]
This explains why some patients relapse after early improvement while others maintain long term stability.
Reconciling Remission With Ayurvedic Resolution
From a modern standpoint long term remission is the realistic and ethical goal [1][7]. From an Ayurvedic standpoint sustained resolution is possible when digestive intelligence is fully restored and supported by appropriate diet routine and resilience building therapies [8][9]. These views are not contradictory. They describe the same outcome using different frameworks. Ayurveda does not promise that IBS can never recur under any circumstance but asserts that recurrence becomes unlikely when treatment is completed properly and lifestyle alignment is maintained.
What Permanence Means in Practical Terms
For patients permanence does not mean never experiencing digestive discomfort again. It means living without chronic symptoms without constant fear of food and without dependence on ongoing medication. Many individuals achieve this state through thorough correction of Grahani and Agni followed by consolidation. Modern medicine would describe this as durable remission. Ayurveda would describe it as restoration of digestive balance. Both acknowledge that long term stability is achievable even if guarantees are neither realistic nor responsible.
“Na hi samyak sthite agnau roga avasthitam bhavati”
Charaka Samhita, Sutra Sthana, Chapter 27, Shloka 348
Meaning: Disease does not persist when digestive fire is properly established [8]
This is why IBS can be resolved in a practical and lasting sense when the root functional imbalance is fully corrected and maintained over time rather than merely suppressed.
Summary
What IBS Really Is and Why Your Tests Are Often Normal
For patients in the USA and UK IBS is now widely recognized as a functional digestive disorder rather than a structural disease [1][2][4]. This means symptoms arise from dysregulation of digestion gut sensitivity and nervous coordination even when scans blood tests and endoscopy appear normal. Feeling unwell despite normal results is not a contradiction but a defining feature of IBS. Understanding this removes unnecessary fear of missed disease and shifts focus toward correcting function rather than searching endlessly for structural causes.
If you want a complete step by step IBS guide that combines diagnosis symptoms and the full Ayurvedic treatment framework in one place you can read the main pillar resource here https://panaceayur.com/ibs-ayurvedic-treatment-diagnosis-symptoms-cure/
Why One Size Treatment Does Not Work
IBS presents differently in every individual. Some experience constipation others diarrhea many fluctuate between patterns and symptoms change with stress sleep hormones and routine [4]. Because IBS is lifestyle sensitive and regulation based standardized treatment protocols often plateau. Long term improvement requires personalization that accounts for digestive strength nervous reactivity diet timing and daily rhythm rather than relying on a single medication or diet plan. This is why many patients feel temporarily better but not stable when treatment is not individualized [2].
What Long Term Improvement Actually Looks Like
Long term improvement in IBS does not mean eliminating every digestive sensation forever. It means stable bowel habits reduced flare frequency improved food tolerance and freedom from constant anxiety around eating or symptoms. Modern medicine describes this outcome as durable remission [1][6]. Ayurveda describes it as restoration of digestive balance. Both agree that meaningful stability develops over months not weeks and depends on correcting function supporting resilience and avoiding overtreatment.
Why Lifestyle and Regulation Matter More Than Suppression
IBS is highly responsive to lifestyle factors such as stress meal timing sleep patterns and routine. Suppressing symptoms without addressing these factors leads to repeated relapse [2][6]. Long term success comes from restoring digestive coordination calming nervous reactivity and rebuilding confidence in digestion. This approach reduces dependency on ongoing medication and supports sustainable quality of life rather than short term symptom control.
A Practical and Reassuring Perspective
For USA and UK patients the most important message is that IBS is real manageable and improvable. It is not a progressive disease and it does not mean lifelong suffering. With a functional individualized and patient centered approach many people achieve long term stability and live normally without constant symptoms. Understanding IBS as a regulatory condition rather than a permanent defect allows treatment to focus on correction resilience and confidence rather than fear and limitation.
This summary brings together modern clinical understanding and classical functional insight to offer a realistic hopeful and grounded framework for long term IBS management [1][2][4][6].
FAQs
Is IBS a lifelong condition or can it improve over time
IBS is a functional digestive disorder, not a progressive structural disease. Many patients experience long term remission when digestive regulation, stress response, and lifestyle factors are corrected rather than only suppressing symptoms
Why are my IBS tests normal if my symptoms feel severe
IBS affects gut function and sensitivity rather than causing visible damage. This is why scans and blood tests are often normal even when symptoms are intense and disruptive
How long does it take to see improvement in IBS
Meaningful IBS improvement usually occurs over months rather than weeks. Early stabilization may appear within weeks, but long term relief requires sustained correction and consistency
Can stress really trigger IBS symptoms
Yes. Stress directly affects gut brain signaling, gut sensitivity, and bowel regulation. This is why IBS symptoms often flare during emotional stress, anxiety, or sleep disruption
Do restrictive diets cure IBS
Restrictive diets may reduce symptoms short term but are rarely a complete solution. Long term improvement comes from restoring digestive tolerance and rhythm rather than permanent avoidance
Is long term remission from IBS realistic
Long term remission is realistic for many patients when treatment focuses on correcting digestive function, nervous regulation, and lifestyle triggers. This outcome is recognized clinically even if the word cure is avoided
[1] Drossman, D. A. (2016). Functional gastrointestinal disorders: History, pathophysiology, clinical features, and Rome IV. Gastroenterology, 150(6), 1262–1279. https://doi.org/10.1053/j.gastro.2016.02.032
Brief: This landmark Rome IV paper explains IBS as a functional disorder driven by gut–brain dysregulation rather than structural disease. It supports the core idea that normal tests do not mean normal gut function.
[2] Ford, A. C., Lacy, B. E., & Talley, N. J. (2017). Irritable bowel syndrome. The New England Journal of Medicine, 376(26), 2566–2578. https://www.nejm.org/doi/full/10.1056/NEJMra1607547
Brief: A comprehensive Western medical overview of IBS, highlighting symptom variability, limited efficacy of drugs, and the chronic relapsing nature of the condition.
[3] Mayer, E. A., Savidge, T., & Shulman, R. J. (2014). Brain–gut microbiome interactions and functional bowel disorders. Gastroenterology, 146(6), 1500–1512. https://doi.org/10.1053/j.gastro.2014.02.037
Brief: Establishes the gut–brain axis as a central mechanism in IBS, supporting the Ayurvedic emphasis on nervous system regulation and digestive coordination.
[4] Enck, P., Aziz, Q., Barbara, G., et al. (2016). Irritable bowel syndrome. Nature Reviews Disease Primers, 2, 16014. https://doi.org/10.1038/nrdp.2016.14
Brief: Authoritative review explaining IBS pathophysiology, visceral hypersensitivity, stress response, and why symptom-based treatment often fails.
[5] Tillisch, K. (2014). The effects of gut microbiota on CNS function in humans. Gut Microbes, 5(3), 404–410. https://doi.org/10.4161/gmic.29232
Brief: Demonstrates how gut dysfunction affects brain signaling, reinforcing the mind–gut framework discussed in Ayurvedic IBS treatment.
[6] National Institute for Health and Care Excellence (NICE). (2017). Irritable bowel syndrome in adults: Diagnosis and management (CG61). https://www.nice.org.uk/guidance/cg61
Brief: UK clinical guideline acknowledging IBS as a functional condition and recommending diet and lifestyle interventions alongside limited drug use.
[7] Camilleri, M. (2021). Management of the irritable bowel syndrome. Gastroenterology, 160(1), 47–63. https://doi.org/10.1053/j.gastro.2020.08.058
Brief: Reviews why IBS management is often incomplete and emphasizes individualized, multimodal care rather than single-drug solutions.
[8] Sharma, R. K., & Dash, B. (2018). Charaka Samhita (Chikitsa Sthana, Grahani Chikitsa Adhyaya). Chowkhamba Sanskrit Series.
Brief: Classical Ayurvedic reference describing Grahani disorder, digestive fire imbalance (Agni), and treatment principles that align with IBS symptom patterns.
[9] Tripathi, B. (2019). Ashtanga Hridaya (Nidana & Chikitsa Sthana – Grahani Adhikara). Chaukhamba Sanskrit Pratishthan.
Brief: Explains Grahani pathology, diet-centric treatment, and relapse prevention, forming the Ayurvedic backbone of IBS management.
[10] Rao, S. S. C., Yu, S., & Fedewa, A. (2015). Systematic review: Dietary fibre and FODMAP-restricted diet in IBS. Alimentary Pharmacology & Therapeutics, 41(12), 1256–1270. https://doi.org/10.1111/apt.13167
Brief: Shows why diet alone helps some IBS patients but fails others, supporting the need for digestive correction beyond food restriction.
[11] van Tilburg, M. A. L., et al. (2020). Psychological therapies for IBS. The Lancet Gastroenterology & Hepatology, 5(5), 419–432. https://doi.org/10.1016/S2468-1253(19)30401-4
Brief: Confirms the role of stress, anticipation, and nervous system sensitivity in IBS, validating mind–gut interventions discussed in Ayurveda.
[12] Healthline Editorial Team. (2023). Ayurvedic medicine for IBS: Does it work? Healthline. https://www.healthline.com/health/ayurvedic-medicine-for-ibs
Brief: A mainstream Western health platform acknowledging Ayurveda’s role in IBS symptom improvement when used responsibly and under supervision.