- Herpes Blood Test Accuracy and Reliability Explained
- How Accurate Is a Herpes Blood Test Really?
- Can a Herpes IgG Test Be Negative and Still Turn Positive Later?
- Types of Herpes Blood Tests
- Scientific Basis of Testing
- Indications for Ordering a Blood Test
- Indications for Ordering a Blood Test
- Interpretation of Results
- Accuracy, Pitfalls, and Limitations
- Alternative and Complementary Diagnostic Approaches
- Frequently Asked Questions About Herpes Blood Tests
- References
Herpes Blood Test Accuracy and Reliability Explained
A herpes blood test can be reliable, but only when it is done at the correct time and interpreted properly. Many people receive confusing results because they test too early, rely on the wrong marker, or are not told about the antibody window period. This leads to false negatives, unnecessary anxiety, and incorrect reassurance.
Herpes blood tests do not look for the virus itself. Instead, they measure how your immune system responds to the virus. Because antibodies take time to develop, timing plays a critical role in accuracy. Understanding this is essential before trusting a negative or positive report.
How Accurate Is a Herpes Blood Test Really?
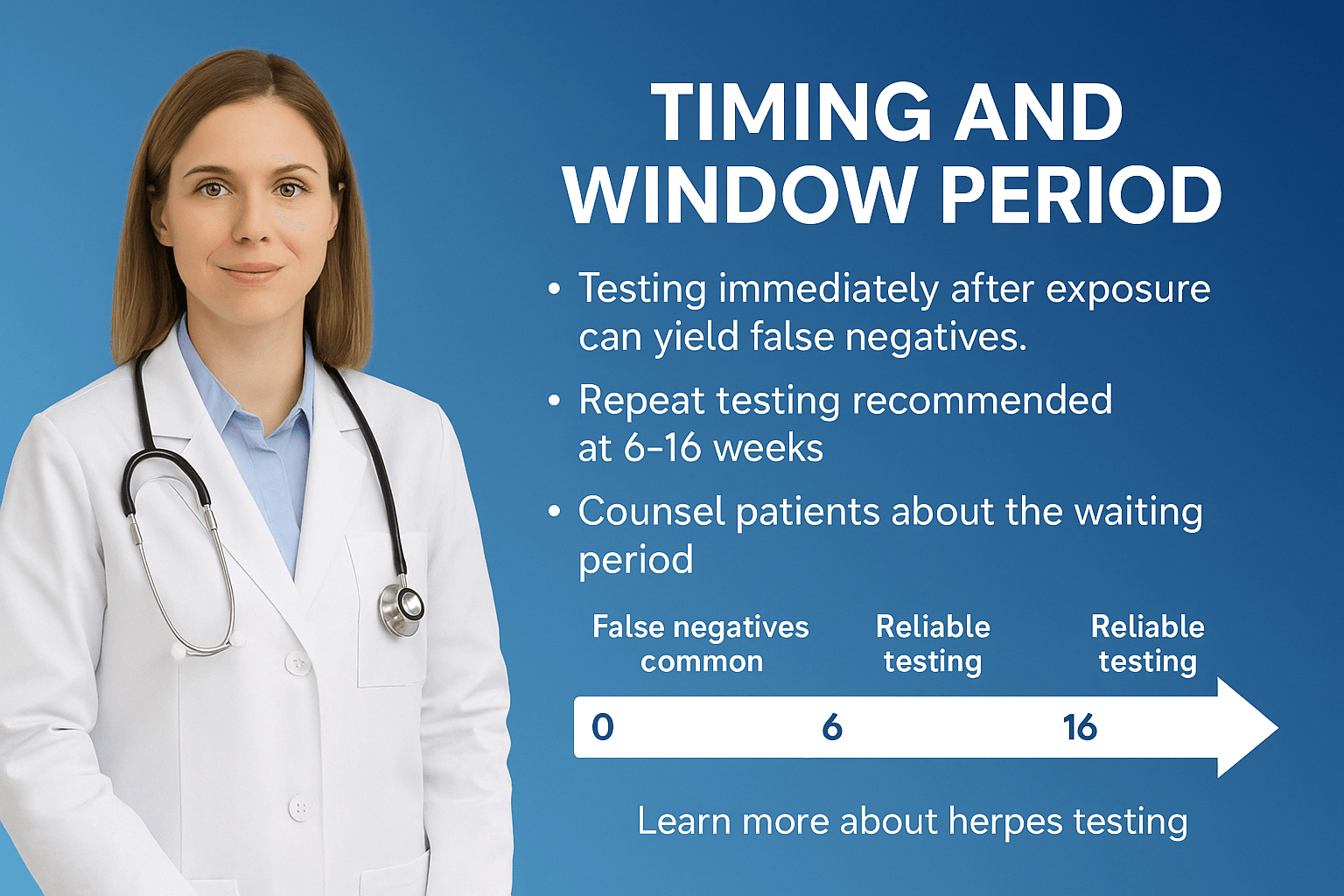
Herpes blood test accuracy depends on three main factors: the type of test used, how long after exposure the test was done, and whether the result is interpreted with proper context.
IgG antibody tests are the most reliable for detecting past herpes infection, but they are not accurate in the early weeks after exposure. Testing during this window period is the most common reason for false negative results. A negative test does not always mean absence of infection if done too early.
A Herpes blood test is one of the most important tools for early and accurate detection of herpes simplex virus (HSV) infection, ensuring proper clinical management and reducing silent transmission within populations [1]. Many individuals remain undiagnosed because their symptoms are mild, atypical, or entirely absent, yet they continue to carry and spread the virus unknowingly [2]. By providing a reliable method of confirming infection even in the absence of visible sores, blood testing has become an essential diagnostic step for both patients and healthcare providers.
One of the greatest advantages of herpes blood testing lies in its ability to differentiate between HSV-1 and HSV-2. Historically, HSV-1 has been linked with oral lesions and HSV-2 with genital disease, but modern evidence shows both viruses can infect either site. This distinction is clinically significant since HSV-2 is associated with more frequent recurrences, higher asymptomatic shedding, and greater complications in pregnancy [3]. Type-specific serological assays based on glycoprotein G antigens have dramatically improved accuracy, allowing physicians to offer personalized counseling, prognosis, and treatment strategies [4].
Blood testing also plays a critical role when no lesions are available for swab or PCR analysis. In such cases, antibody detection offers a retrospective view of exposure, revealing whether infection has occurred in the past [5]. This is particularly valuable for high-risk groups such as pregnant women, immunocompromised individuals, and partners of HSV-positive patients, where hidden infection can have serious medical and emotional consequences [6].
Can a Herpes IgG Test Be Negative and Still Turn Positive Later?
Yes. This is one of the most misunderstood aspects of herpes testing.
IgG antibodies usually take several weeks to appear. In many people, they are not detectable until 8 to 12 weeks after exposure. In some cases, especially if immunity is stressed, it may take up to 16 weeks. This means an early negative result does not rule out herpes.
Types of Herpes Blood Tests
IgG Test (Type-Specific, Glycoprotein G-Based)
The HSV IgG blood test is the most reliable and commonly recommended herpes test for patients. This test looks for IgG antibodies, which your immune system produces after being infected with herpes simplex virus. Unlike older tests, it uses a very specific marker called glycoprotein G (gG) that is unique for HSV-1 and HSV-2. That means it can tell you not only if you have herpes, but also which type you carry.
- When it becomes positive: IgG antibodies usually appear about 3–12 weeks after exposure. If you test too soon, it might be negative even though you are infected.
- What the results mean:
- A positive HSV-1 IgG usually means you were exposed at some point, often in childhood, but it can also mean genital HSV-1 if you got it through sexual contact.
- A positive HSV-2 IgG almost always means genital herpes, even if you never had symptoms.
- Why it matters: Knowing your HSV type can help you understand your risk of recurrences, the chance of passing it to a partner, and—if you are pregnant—what steps need to be taken to protect the baby [7]
[8].
IgM Test (Limitations and Cross-Reactivity)
The HSV IgM test is sometimes marketed as a way to find “new” or “recent” infections, but in reality it is not trustworthy. IgM antibodies can appear not only during the first outbreak, but also during recurrences years later. Even worse, this test often mistakes antibodies from other herpes family viruses (like EBV or CMV) for herpes, leading to false positives [9] [10].
- Why patients should be cautious: Many people receive a positive IgM test and believe they have herpes when they may not. This can cause unnecessary fear, relationship stress, and even incorrect treatment.
- What experts recommend: Most specialists no longer advise using IgM tests for herpes diagnosis. If your doctor offers you an IgM test, ask specifically for a type-specific IgG instead.
Western Blot (University of Washington Standard)
The Western blot test is considered the gold standard for herpes testing. Developed at the University of Washington, it looks for multiple different antibodies to HSV, making it the most accurate test available.
- When it’s used: If your IgG test comes back unclear (“equivocal”) or you received conflicting results, the Western blot can give you a final answer.
- Why patients rarely get it: It is more expensive, requires sending samples to specialized labs, and takes longer to receive results [11] [12].
- What to expect: This test is highly reliable and can provide peace of mind when other tests leave uncertainty—something many patients find worth the extra effort.
ELISA and Chemiluminescent Immunoassays
These are automated laboratory tests used in most hospitals and diagnostic labs worldwide. ELISA and CLIA are both designed to detect HSV IgG antibodies quickly and in large numbers of patients.
- Advantages: They are relatively affordable, widely available, and provide results within a few days.
- Limitations: Depending on the lab and the kit used, results can sometimes be “equivocal” or borderline. In such cases, patients are usually advised to repeat the test after a few weeks or confirm with a Western blot [[13]] [14].
- For patients: If your report says “equivocal,” it doesn’t mean positive or negative. It simply means the antibody level was too close to the cutoff, and a repeat test is needed.
Rapid Point-of-Care Tests
For patients who need immediate answers, some clinics offer rapid herpes blood tests. These are finger-prick tests or small blood samples that can give results in 20–30 minutes.
- Where they are used: Sexual health clinics, emergency visits, or prenatal care settings where quick decisions are needed.
- Pros: Immediate results, no waiting for lab reports.
- Cons: They may not be as accurate as standard IgG tests. A positive result often needs confirmation with a full laboratory test [15]
[16]. - For patients: If you take a rapid test and it is positive, do not panic. Ask your doctor to confirm it with a laboratory IgG or Western blot for certainty.
Patient Takeaway
- Best first choice: HSV IgG type-specific test (accurate, widely available).
- Avoid: HSV IgM test (misleading, not recommended).
- For certainty: Western blot (gold standard, but limited access).
- Routine lab tests: ELISA/CLIA (standard hospital methods).
- Immediate answers: Rapid point-of-care tests (screening, confirm if positive).
IgM Test (Limitations, Cross-Reactivity, and Misuse)
The HSV IgM test is still offered in many laboratories, but experts agree it is misleading and clinically unnecessary. IgM antibodies can appear both during a first infection and during recurrences years later, which means they cannot prove a “new” infection. In addition, this test often cross-reacts with other herpes family viruses, such as Epstein–Barr virus (EBV) or cytomegalovirus (CMV), producing false positives [17] [18].
For patients, this can cause unnecessary emotional distress, strained relationships, and inappropriate treatment. Despite its poor reliability, the IgM test continues to be sold because it is a revenue generator for labs, diagnostic companies, and other healthcare stakeholders. It is cheap to run, quick to report, and easy to market as a “recent infection test,” even though it does not provide medically meaningful answers.
- Why patients should be cautious: A positive IgM does not confirm herpes, and many people have been misdiagnosed due to this flawed test.
- What to do instead: Always ask for a type-specific IgG blood test. If results are uncertain, request confirmation with a Western blot.
Scientific Basis of Testing
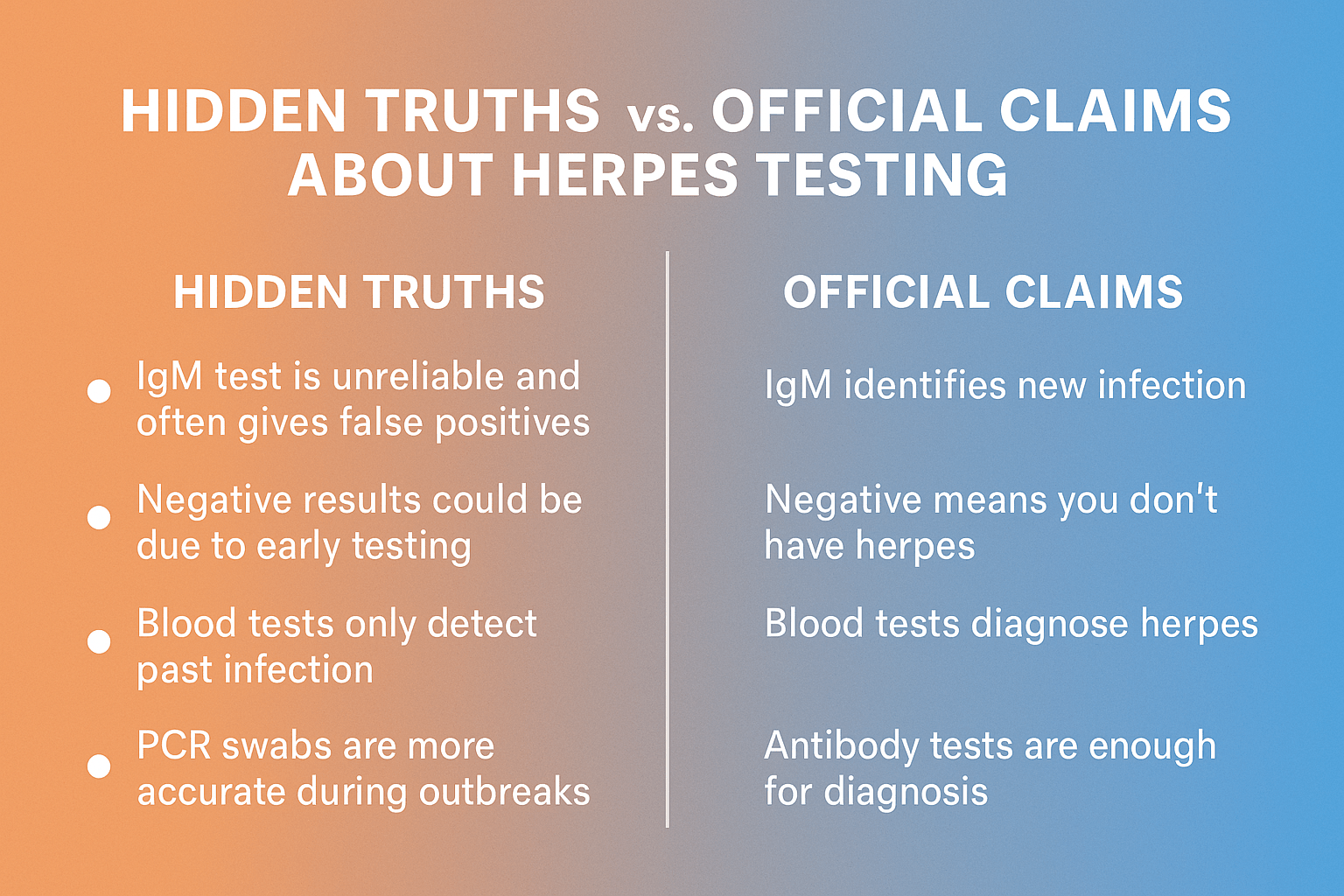
Herpes blood testing is built on the science of antibody detection. Instead of searching for the virus directly, these tests look at how the immune system responds to herpes infection. This principle explains both the power and the limitations of blood testing—and also exposes truths that many patients are not told.
Antibody Formation Timelines
- IgM Antibodies
IgM is the first line of defense produced after infection. In theory, it appears 7–14 days after exposure. But in practice, the story is far more complex. IgM often appears again during recurrent outbreaks, sometimes years later, which destroys its usefulness as a marker of “new” infection [19]. Worse, it cross-reacts with other herpes family viruses like EBV or CMV, which means people can test “positive” without actually having HSV [20].
Hidden truth: Many commercial labs still sell IgM tests, and some physicians continue ordering them despite clear guidelines advising against it. This misleads patients, causing panic, unnecessary stigma, and sometimes incorrect treatment. The persistence of this practice is partly due to profit incentives and the slow update of lab protocols. - IgG Antibodies
IgG antibodies appear 3–12 weeks after infection and then stay for life [21]. A positive IgG test is the most reliable evidence of exposure. However, it cannot reveal when you were infected, nor can it prove whether you are experiencing an outbreak at the moment [22].
Lesser-known fact: Not all IgG tests are created equal. Some “type-specific” assays still show up as equivocal or cross-react in a small percentage of patients. False negatives are also possible in the early weeks, leading to confusion. This is why many specialists recommend retesting at 16 weeks if exposure was recent [23]..
Why Blood Tests Detect Past vs Active Infection Differently
Antibody tests measure the memory of your immune system, not the virus itself. That’s why:
- You can have no sores but test positive (because your body remembers the infection).
- You can be recently infected but test negative (because antibodies have not formed yet).
Hidden truth: Many patients mistakenly believe that a blood test can reveal whether they are contagious at that moment. In reality, it cannot. A person may test positive on IgG but have no active shedding, or vice versa. This mismatch is why herpes transmission is so misunderstood in relationships [24].
Antibody Detection vs Viral DNA Detection (PCR)
- Antibody tests (IgG/IgM): Detect the immune response. Best for diagnosing silent or past infections.
- PCR (Polymerase Chain Reaction): Detects the virus’s genetic material (DNA) directly. Best for confirming an active infection or clarifying confusing cases.
Lesser-known fact: PCR can detect very small amounts of viral DNA—even when sores are healing or not visible. This makes it far superior to older culture methods. However, PCR is more expensive and not always offered outside of advanced clinics [25].
Hidden truth: Some labs and doctors downplay PCR because it is more costly and less profitable for routine screening. Instead, they push antibody testing, even though PCR could provide patients with better answers during outbreaks.
Additional Hidden Truths and Overlooked Details
- False sense of certainty: Many patients assume a negative blood test means they are “clear.” In truth, testing too soon can miss infection. Doctors rarely explain the window period properly, leaving patients with false reassurance.
- Psychological burden: A positive IgG test does not mean you are infectious every day. Yet many patients are told simply “you have herpes,” without counseling on asymptomatic shedding patterns. This fuels stigma more than the infection itself [26].
- Variation between labs: Commercial test kits vary in sensitivity and specificity. Some international labs still use outdated assays. Patients rarely know which test they received or its reliability rating.
- Research bias: Most testing algorithms were developed around Western patient populations. Data on antibody timelines in African and Asian populations suggest slightly different kinetics, yet this is rarely acknowledged in standard guidelines [27].
- Ayurvedic lens: From an integrative perspective, antibody testing aligns with the concept of Rakta and Shukra Dhatu memory—once disturbed, the “imprint” remains. Ayurveda acknowledges this long-lasting immune memory, but emphasizes that true cure lies in correcting the underlying imbalance, not merely detecting antibodies.
Patient Takeaway
Herpes blood tests provide valuable information, but they are often misunderstood or misrepresented.
- IgM is unreliable and should generally be avoided.
- IgG is the most useful but only proves past exposure.
- PCR is the best option for confirming active infection, though less accessible.
- Patients should ask not only for their results but also about which test was used, when it was performed, and whether retesting is necessary.
Indications for Ordering a Blood Test
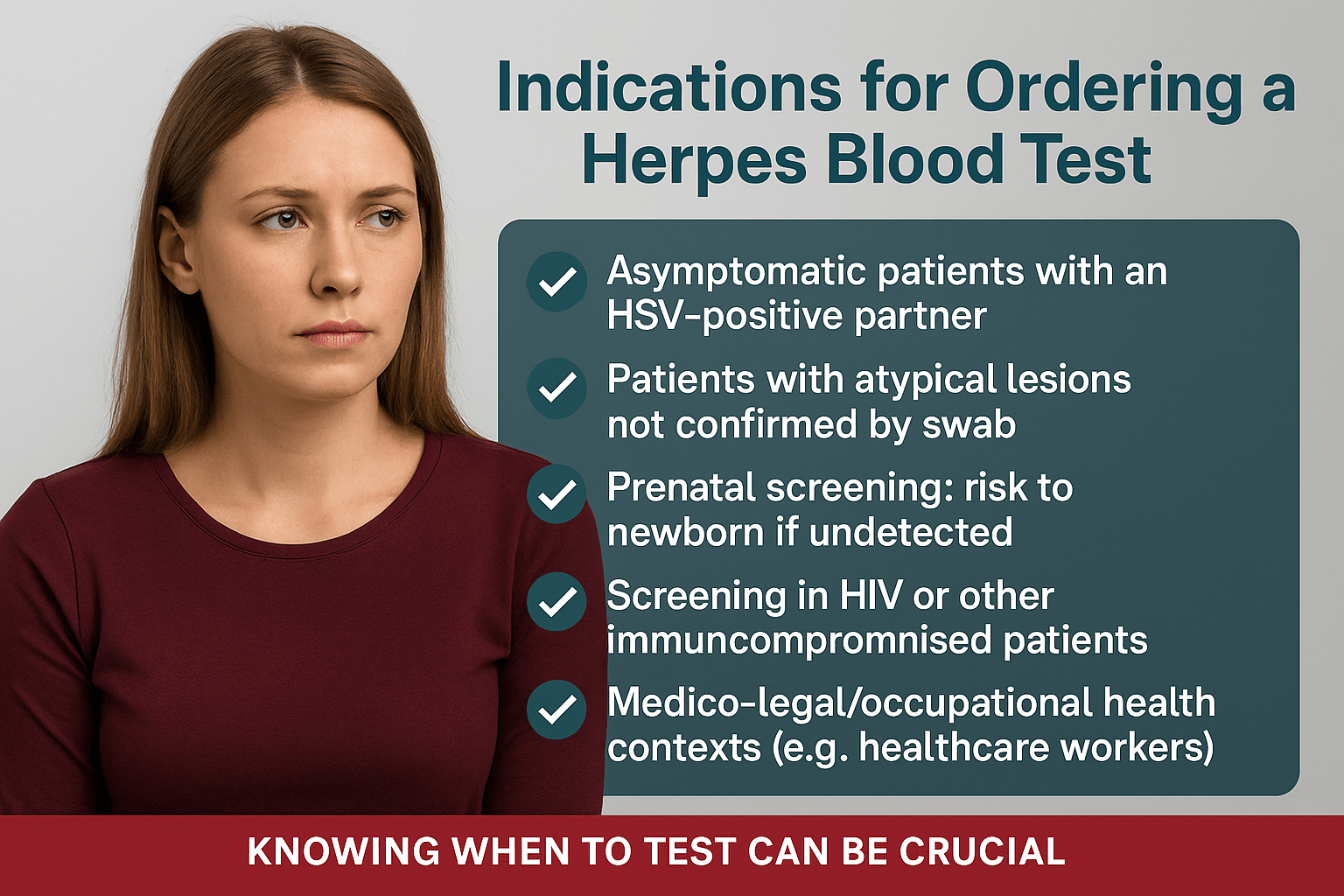
Herpes blood testing is not performed in every case. In fact, most doctors rely first on swab-based PCR tests when sores are visible. However, there are specific scenarios where a blood test becomes critical.
Asymptomatic Patients with an HSV-Positive Partner
One of the most common situations is when a person has no symptoms but their partner has tested positive for herpes. Since herpes can spread even without visible sores through asymptomatic shedding, many patients seek clarity about their own status [28]. In such cases, a type-specific IgG blood test is the most reliable way to detect prior exposure.
Hidden truth: Many couples are told that if there are no symptoms, testing is unnecessary. This is misleading—silent carriers account for a large share of herpes transmission worldwide [29].
Patients with Atypical Lesions Not Confirmed by Swab
Sometimes patients present with rashes, cuts, or sores that do not look like the “classic” herpes blister. Swab results may come back inconclusive. For these individuals, an antibody test helps determine if herpes is the underlying cause, or if another condition (like eczema, yeast infection, or trauma) is responsible [30].
Prenatal Screening (Risk to the Newborn if Undetected)
In pregnancy, undetected herpes can pose a serious risk to the baby. Neonatal herpes, though rare, can be life-threatening. If a pregnant woman has a partner with herpes, or has a history of unexplained genital symptoms, doctors often recommend blood testing to identify silent infection
[31].
Lesser-known fact: Routine herpes screening in pregnancy is not standard in most countries, even though undiagnosed HSV-2 infection can be dangerous at delivery. This gap is partly due to cost and debate about whether widespread testing is “worth it,” but for individual mothers, the consequences of missed diagnosis can be profound [32].
Screening in HIV or Other Immunocompromised Patients
For people with HIV, cancer, organ transplants, or other immune-compromising conditions, herpes can behave more aggressively and increase the risk of other infections. In these patients, blood testing provides crucial information, allowing preventive or suppressive treatment if needed [33].
Hidden truth: Studies show that HSV-2 infection increases both the risk of acquiring HIV and the rate of HIV progression. Despite this, herpes testing is not routinely included in HIV care protocols in many parts of the world [34].
Medico-Legal and Occupational Health Contexts
Certain occupations—such as healthcare workers, surgeons, and caregivers for newborns—may require herpes testing in medico-legal settings or occupational screenings. In such cases, blood testing provides documented evidence of exposure. This is particularly important in malpractice cases, disputes about transmission, or when patients seek legal clarity in relationships [35].
Lesser-known fact: Some courts have accepted HSV IgG test results as evidence in paternity or transmission disputes, though the tests cannot establish when the infection was acquired or from whom. This often creates legal gray zones that patients are rarely warned about.
Patient Takeaway
A herpes blood test is most valuable when:
- You are at risk but have no symptoms.
- You have unclear or atypical skin lesions.
- You are pregnant and at possible risk.
- You have HIV or are immunocompromised.
- You are in legal, occupational, or relationship contexts where proof of exposure matters.
Indications for Ordering a Blood Test
Herpes blood testing is not performed in every case. In fact, most doctors rely first on swab-based PCR tests when sores are visible. However, there are specific scenarios where a blood test becomes critical.
Asymptomatic Patients with an HSV-Positive Partner
One of the most common situations is when a person has no symptoms but their partner has tested positive for herpes. Since herpes can spread even without visible sores through asymptomatic shedding, many patients seek clarity about their own status [36]. In such cases, a type-specific IgG blood test is the most reliable way to detect prior exposure.
Hidden truth: Many couples are told that if there are no symptoms, testing is unnecessary. This is misleading—silent carriers account for a large share of herpes transmission worldwide [37].
Patients with Atypical Lesions Not Confirmed by Swab
Sometimes patients present with rashes, cuts, or sores that do not look like the “classic” herpes blister. Swab results may come back inconclusive. For these individuals, an antibody test helps determine if herpes is the underlying cause, or if another condition (like eczema, yeast infection, or trauma) is responsible [38].
Prenatal Screening (Risk to the Newborn if Undetected)
In pregnancy, undetected herpes can pose a serious risk to the baby. Neonatal herpes, though rare, can be life-threatening. If a pregnant woman has a partner with herpes, or has a history of unexplained genital symptoms, doctors often recommend blood testing to identify silent infection
[39].
Lesser-known fact: Routine herpes screening in pregnancy is not standard in most countries, even though undiagnosed HSV-2 infection can be dangerous at delivery. This gap is partly due to cost and debate about whether widespread testing is “worth it,” but for individual mothers, the consequences of missed diagnosis can be profound [40].
Screening in HIV or Other Immunocompromised Patients
For people with HIV, cancer, organ transplants, or other immune-compromising conditions, herpes can behave more aggressively and increase the risk of other infections. In these patients, blood testing provides crucial information, allowing preventive or suppressive treatment if needed
[41].
Hidden truth: Studies show that HSV-2 infection increases both the risk of acquiring HIV and the rate of HIV progression. Despite this, herpes testing is not routinely included in HIV care protocols in many parts of the world [42].
Medico-Legal and Occupational Health Contexts
Certain occupations—such as healthcare workers, surgeons, and caregivers for newborns—may require herpes testing in medico-legal settings or occupational screenings. In such cases, blood testing provides documented evidence of exposure. This is particularly important in malpractice cases, disputes about transmission, or when patients seek legal clarity in relationships [43].
Lesser-known fact: Some courts have accepted HSV IgG test results as evidence in paternity or transmission disputes, though the tests cannot establish when the infection was acquired or from whom. This often creates legal gray zones that patients are rarely warned about.
Patient Takeaway
A herpes blood test is most valuable when:
- You are at risk but have no symptoms.
- You have unclear or atypical skin lesions.
- You are pregnant and at possible risk.
- You have HIV or are immunocompromised.
- You are in legal, occupational, or relationship contexts where proof of exposure matters.
Interpretation of Results
What a Positive Test Means
If your test shows positive for HSV-1 IgG, it means your body has come in contact with herpes simplex virus type 1. Most people pick this up in childhood as cold sores, but it can also cause genital herpes. The blood test cannot tell you where the virus is in your body—only that your immune system has seen it before.
A positive HSV-2 IgG result usually means genital herpes. This type is important to recognize because it tends to come back more often, sheds silently when you feel fine, and can create risks in pregnancy. If your test is positive for HSV-2, your doctor will usually talk with you about management and prevention steps.
When the Test Is Negative but Symptoms Are Present
Sometimes people have classic sores or itching but their test comes back negative. This often happens if the test is done too soon after exposure. Your body may need up to 12–16 weeks to build enough antibodies to show up on a blood test. If you have symptoms but a negative result, the best approach is:
- Retest later, after the 12–16 week window.
- If sores are present, ask for a swab PCR test, which looks for the virus itself rather than antibodies.
Equivocal or “Borderline” Results
If your results fall into the “equivocal” or “borderline” range, it means the antibody level isn’t high enough to be clearly positive but isn’t negative either. This can happen if the infection is new or simply because of test variability. In this case, doctors usually recommend:
- Repeating the test in 4–6 weeks.
- If doubt remains, ordering a Western Blot test. This is the most accurate herpes blood test, though it’s available only at specialized labs.
Why IgM Is Not the Answer
Many people are offered an IgM test, but it causes more confusion than clarity. IgM can show up both during new infections and during flare-ups years later. It also reacts to other viruses in the herpes family, like mono (EBV) or CMV. Because of this, a positive IgM result doesn’t prove you have herpes, and a negative result doesn’t rule it out. That’s why most experts say IgG is the only reliable antibody test for herpes.
Bottom Line
- HSV-1 positive: Past exposure, may be oral or genital.
- HSV-2 positive: Usually genital herpes, requires counseling and prevention steps.
- Negative with symptoms: Retest later or ask for PCR.
- Equivocal: Retest or confirm with Western Blot.
- IgM: Not recommended—too many false results.
Accuracy, Pitfalls, and Limitations
Sensitivity and Specificity
Herpes blood tests are fairly accurate but not perfect. Type-specific IgG tests based on glycoprotein G usually have sensitivity between 92–99 percent and specificity of 96–99 percent once the infection is established. However, their accuracy drops if the test is done too early or if the antibody levels fall into the borderline range [44]. The Western Blot test is regarded as the gold standard because of its very high specificity and is often used when results are unclear, though it is more costly and less accessible [45]. Rapid point-of-care tests can deliver quick answers but are less accurate than laboratory-based IgG and usually require confirmation if positive [46]. IgM assays, still offered in many labs, are unreliable because of low specificity and frequent false positives, and they are not recommended as a stand-alone test [47].
Cross-Reactivity
False positives can happen because of cross-reactivity with other herpesviruses. IgM tests are especially prone to confusion with antibodies against cytomegalovirus (CMV) or Epstein–Barr virus (EBV), which can lead to misleading results [48]. Even IgG tests, though more specific, can sometimes misclassify results in early or borderline cases, especially in patients with unusual immune responses [49].
Laboratory Variability
Not all tests are the same. Different laboratories and brands use different antigens, cutoffs, and calibration methods, which means the same sample may yield different values in different settings
[50]. Variability is also seen across countries because laboratories operate under different quality standards and population prevalence rates, which can affect predictive value [51]. Testing too soon—within six weeks of exposure—reduces the sensitivity of any assay and increases the risk of false negatives [52]. Repeating the test on the same platform reduces variability, and unresolved cases may need confirmation with Western Blot [53].
Psychological Burden
Testing for herpes does not only carry medical implications but also emotional weight. A false positive or a poorly explained positive result can trigger anxiety, shame, and conflict in relationships. This is a frequent problem when IgM is misused [54]. Patients often benefit from clear explanations about the timing of antibody development, the meaning of IgG positivity, and the reality of asymptomatic shedding, which helps reduce stigma and unnecessary fear [55].
Ethical Duty to Counsel
There is an ethical responsibility to ensure patients understand what their results mean. Informed consent should cover what the test can and cannot reveal, the possibility of false positives or negatives, and the need for follow-up testing when results are equivocal. Counseling should also include emotional support and practical advice, otherwise the test result itself may cause more harm than benefit [56].
Alternative and Complementary Diagnostic Approaches
Herpes blood tests are powerful for detecting past infection, but they cannot always confirm whether the virus is active. In many situations, doctors rely on other tests that look directly for the virus itself.
PCR: Direct Viral DNA Detection
Polymerase chain reaction, or PCR, is now considered the gold standard for diagnosing an active herpes infection. Instead of looking for antibodies, PCR detects the virus’s DNA directly. This makes it extremely sensitive and specific, even if only a tiny amount of virus is present [57]. It is especially valuable during fresh outbreaks, in newborns suspected of having neonatal herpes, or in people with weakened immune systems. PCR can also tell whether the infection is HSV-1 or HSV-2 with high accuracy. The main limitation is cost and availability, since not all clinics have access to PCR.
Viral Culture
Before PCR, viral culture was the standard test. It involves swabbing fluid from a blister and trying to grow the virus in the lab. This method works only if the sores are very fresh—within the first 48 hours. Once the blister starts to heal, the virus becomes much harder to detect [58]. Culture is still used in some labs, but its sensitivity is much lower than PCR, especially for recurrent infections.
Direct Fluorescent Antibody (DFA)
DFA is a quicker test that uses fluorescent dye to bind to herpes antigens in lesion samples. Under a microscope, the virus lights up if present. While faster than culture, DFA is not as accurate as PCR, which has largely replaced it in modern practice [59].
Tzanck Smear (Obsolete)
The Tzanck smear is one of the oldest herpes tests. A sample is scraped from the base of a sore, and under the microscope, large multinucleated cells can suggest herpes. However, it cannot distinguish between HSV and other viruses like varicella-zoster. Because of this lack of specificity, the Tzanck smear is now considered obsolete and is rarely recommended [60].
Putting It Together
For patients, this means that different tests answer different questions. Blood tests are best for detecting whether you have ever been exposed to the virus, even if you have no symptoms. PCR is the most accurate test if you want to know whether the virus is active right now. Viral culture and DFA may still be used in some settings but have more limitations. The Tzanck smear, though historic, should not be relied upon in modern diagnosis [61].
Frequently Asked Questions About Herpes Blood Tests
How accurate is a herpes blood test?
A herpes blood test can be accurate when done at the correct time. Type-specific IgG tests reliably detect past infection, but accuracy is reduced if testing is done too early after exposure.
Can a herpes blood test be negative even if I have symptoms?
Yes. This usually happens during the early window period, before antibodies have fully developed. In such cases, repeat testing or PCR from active sores is advised.
Can a negative herpes blood test later turn positive?
Yes. If the first test was done too early, antibodies may not have been detectable. Repeat testing at 12 to 16 weeks often explains this change.
Can herpes blood tests give false positive results?
False positives can occur, especially with IgM tests or borderline IgG values. Confirmatory testing and proper interpretation are important before drawing conclusions.
Which herpes blood test is the most reliable?
Type-specific IgG tests are the most reliable for identifying past infection. Western Blot is used when results are unclear, while PCR is best for active outbreaks.
Is a herpes blood test useful if I have no symptoms?
Yes. Many people with herpes never develop visible sores. Blood testing can still identify past exposure and help clarify infection status.
References
All Source
- Corey, L., & Wald, A. (2009). Genital herpes. The New England Journal of Medicine, 361(14), 1376–1385. https://doi.org/10.1056/NEJMra0807633 ↩
- Patel, R., Kennedy, O. J., Clarke, E., Geretti, A., Nilsen, A., & Lautenschlager, S. (2017). 2017 European guidelines for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716. https://doi.org/10.1111/jdv.14361 ↩
- Gupta, R., Warren, T., & Wald, A. (2007). Genital herpes. The Lancet, 370(9605), 2127–2137. https://doi.org/10.1016/S0140-6736(07)61908-4 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩
- LeGoff, J., Pere, H., & Bélec, L. (2014). Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virology Journal, 11(1), 83. https://doi.org/10.1186/1743-422X-11-83 ↩
- Ashley-Morrow, R., Nollkamper, J., Robinson, N. J., Bishop, N., & Smith, J. (2004). Performance of focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Microbiology, 42(9), 4193–4197. https://doi.org/10.1128/JCM.42.9.4193-4197.2004 ↩
- Gupta, R., Warren, T., & Wald, A. (2007). Genital herpes. The Lancet, 370(9605), 2127–2137. https://doi.org/10.1016/S0140-6736(07)61908-4 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩
- LeGoff, J., Pere, H., & Bélec, L. (2014). Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virology Journal, 11(1), 83. https://doi.org/10.1186/1743-422X-11-83 ↩
- Ashley-Morrow, R., Nollkamper, J., Robinson, N. J., Bishop, N., & Smith, J. (2004). Performance of focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Microbiology, 42(9), 4193–4197. https://doi.org/10.1128/JCM.42.9.4193-4197.2004 ↩
- Patel, R., Kennedy, O. J., Clarke, E., Geretti, A., Nilsen, A., & Lautenschlager, S. (2017). 2017 European guidelines for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716. https://doi.org/10.1111/jdv.14361 ↩
- Corey, L., & Wald, A. (2009). Genital herpes. The New England Journal of Medicine, 361(14), 1376–1385. https://doi.org/10.1056/NEJMra0807633 ↩
- Morrow, R. A., Friedrich, D., & Krantz, E. (2003). Performance of the Focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Virology, 26(2), 153–160. https://doi.org/10.1016/S1386-6532(02)00252-9 ↩
- Wald, A., Ashley-Morrow, R., & Krantz, E. (2003). Laboratory diagnosis of herpes simplex virus infection: Review and update. Clinical Microbiology Reviews, 16(1), 96–113. https://doi.org/10.1128/CMR.16.1.96-113.2003 ↩
- Van Wagoner, N. J., Hook, E. W., & Fredricks, D. N. (2013). Rapid tests for sexually transmitted infections: The future of diagnosis? Sexually Transmitted Infections, 89(6), 431–436. https://doi.org/10.1136/sextrans-2013-051051 ↩
- Patel, R., & Alderson, S. (2019). Point-of-care testing for sexually transmitted infections: A clinical review. British Journal of General Practice, 69(683), 406–407. https://doi.org/10.3399/bjgp19X704609 ↩
- LeGoff, J., Pere, H., & Bélec, L. (2014). Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virology Journal, 11(1), 83. https://doi.org/10.1186/1743-422X-11-83 ↩
- Ashley-Morrow, R., Nollkamper, J., Robinson, N. J., Bishop, N., & Smith, J. (2004). Performance of focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Microbiology, 42(9), 4193–4197. https://doi.org/10.1128/JCM.42.9.4193-4197.2004 ↩
- LeGoff, J., Pere, H., & Bélec, L. (2014). Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virology Journal, 11(1), 83. https://doi.org/10.1186/1743-422X-11-83 ↩
- Ashley-Morrow, R., Nollkamper, J., Robinson, N. J., Bishop, N., & Smith, J. (2004). Performance of focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Microbiology, 42(9), 4193–4197. https://doi.org/10.1128/JCM.42.9.4193-4197.2004 ↩
- Gupta, R., Warren, T., & Wald, A. (2007). Genital herpes. The Lancet, 370(9605), 2127–2137. https://doi.org/10.1016/S0140-6736(07)61908-4 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩
- Corey, L., & Wald, A. (2009). Genital herpes. The New England Journal of Medicine, 361(14), 1376–1385. https://doi.org/10.1056/NEJMra0807633 ↩
- Patel, R., Kennedy, O. J., Clarke, E., Geretti, A., Nilsen, A., & Lautenschlager, S. (2017). 2017 European guidelines for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716. https://doi.org/10.1111/jdv.14361 ↩
- LeGoff, J., Pere, H., & Bélec, L. (2014). Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virology Journal, 11(1), 83. https://doi.org/10.1186/1743-422X-11-83 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩
- Corey, L., & Wald, A. (2009). Genital herpes. The New England Journal of Medicine, 361(14), 1376–1385. https://doi.org/10.1056/NEJMra0807633 ↩
- Gupta, R., Warren, T., & Wald, A. (2007). Genital herpes. The Lancet, 370(9605), 2127–2137. https://doi.org/10.1016/S0140-6736(07)61908-4 ↩
- Patel, R., Kennedy, O. J., Clarke, E., Geretti, A., Nilsen, A., & Lautenschlager, S. (2017). 2017 European guidelines for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716. https://doi.org/10.1111/jdv.14361 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩
- LeGoff, J., Pere, H., & Bélec, L. (2014). Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virology Journal, 11(1), 83. https://doi.org/10.1186/1743-422X-11-83 ↩
- Ashley-Morrow, R., Nollkamper, J., Robinson, N. J., Bishop, N., & Smith, J. (2004). Performance of focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Microbiology, 42(9), 4193–4197. https://doi.org/10.1128/JCM.42.9.4193-4197.2004 ↩
- Corey, L., & Wald, A. (2009). Genital herpes. The New England Journal of Medicine, 361(14), 1376–1385. https://doi.org/10.1056/NEJMra0807633 ↩
- Morrow, R. A., Friedrich, D., & Krantz, E. (2003). Performance of the Focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Virology, 26(2), 153–160. https://doi.org/10.1016/S1386-6532(02)00252-9 ↩
- Van Wagoner, N. J., Hook, E. W., & Fredricks, D. N. (2013). Rapid tests for sexually transmitted infections: The future of diagnosis? Sexually Transmitted Infections, 89(6), 431–436. https://doi.org/10.1136/sextrans-2013-051051 ↩
- Gupta, R., Warren, T., & Wald, A. (2007). Genital herpes. The Lancet, 370(9605), 2127–2137. https://doi.org/10.1016/S0140-6736(07)61908-4 ↩
- Patel, R., Kennedy, O. J., Clarke, E., Geretti, A., Nilsen, A., & Lautenschlager, S. (2017). 2017 European guidelines for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716. https://doi.org/10.1111/jdv.14361 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩
- LeGoff, J., Pere, H., & Bélec, L. (2014). Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virology Journal, 11(1), 83. https://doi.org/10.1186/1743-422X-11-83 ↩
- Ashley-Morrow, R., Nollkamper, J., Robinson, N. J., Bishop, N., & Smith, J. (2004). Performance of focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Microbiology, 42(9), 4193–4197. https://doi.org/10.1128/JCM.42.9.4193-4197.2004 ↩
- Corey, L., & Wald, A. (2009). Genital herpes. The New England Journal of Medicine, 361(14), 1376–1385. https://doi.org/10.1056/NEJMra0807633 ↩
- Morrow, R. A., Friedrich, D., & Krantz, E. (2003). Performance of the Focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Virology, 26(2), 153–160. https://doi.org/10.1016/S1386-6532(02)00252-9 ↩
- Van Wagoner, N. J., Hook, E. W., & Fredricks, D. N. (2013). Rapid tests for sexually transmitted infections: The future of diagnosis? Sexually Transmitted Infections, 89(6), 431–436. https://doi.org/10.1136/sextrans-2013-051051 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩
- Patel, R., Kennedy, O. J., Clarke, E., Geretti, A., Nilsen, A., & Lautenschlager, S. (2017). 2017 European guidelines for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716. https://doi.org/10.1111/jdv.14361 ↩
- Van Wagoner, N. J., Hook, E. W., & Fredricks, D. N. (2013). Rapid tests for sexually transmitted infections: The future of diagnosis? Sexually Transmitted Infections, 89(6), 431–436. https://doi.org/10.1136/sextrans-2013-051051 ↩
- Ashley-Morrow, R., Nollkamper, J., Robinson, N. J., Bishop, N., & Smith, J. (2004). Performance of focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Microbiology, 42(9), 4193–4197. https://doi.org/10.1128/JCM.42.9.4193-4197.2004 ↩
- LeGoff, J., Pere, H., & Bélec, L. (2014). Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virology Journal, 11(1), 83. https://doi.org/10.1186/1743-422X-11-83 ↩
- Ashley-Morrow, R., Nollkamper, J., Robinson, N. J., Bishop, N., & Smith, J. (2004). Performance of focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Microbiology, 42(9), 4193–4197. https://doi.org/10.1128/JCM.42.9.4193-4197.2004 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩
- Gupta, R., Warren, T., & Wald, A. (2007). Genital herpes. The Lancet, 370(9605), 2127–2137. https://doi.org/10.1016/S0140-6736(07)61908-4 ↩
- Patel, R., Kennedy, O. J., Clarke, E., Geretti, A., Nilsen, A., & Lautenschlager, S. (2017). 2017 European guidelines for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716. https://doi.org/10.1111/jdv.14361 ↩
- Corey, L., & Wald, A. (2009). Genital herpes. The New England Journal of Medicine, 361(14), 1376–1385. https://doi.org/10.1056/NEJMra0807633 ↩
- Ashley-Morrow, R., Nollkamper, J., Robinson, N. J., Bishop, N., & Smith, J. (2004). Performance of focus and Kalon enzyme-linked immunosorbent assays for antibodies to herpes simplex virus type 2 glycoprotein G in culture-documented cases of genital herpes. Journal of Clinical Microbiology, 42(9), 4193–4197. https://doi.org/10.1128/JCM.42.9.4193-4197.2004 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩
- Patel, R., Kennedy, O. J., Clarke, E., Geretti, A., Nilsen, A., & Lautenschlager, S. (2017). 2017 European guidelines for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716. https://doi.org/10.1111/jdv.14361 ↩
- Patel, R., Kennedy, O. J., Clarke, E., Geretti, A., Nilsen, A., & Lautenschlager, S. (2017). 2017 European guidelines for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716. https://doi.org/10.1111/jdv.14361 ↩
- Gupta, R., Warren, T., & Wald, A. (2007). Genital herpes. The Lancet, 370(9605), 2127–2137. https://doi.org/10.1016/S0140-6736(07)61908-4 ↩
- LeGoff, J., Pere, H., & Bélec, L. (2014). Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virology Journal, 11(1), 83. https://doi.org/10.1186/1743-422X-11-83 ↩
- Corey, L., & Wald, A. (2009). Genital herpes. The New England Journal of Medicine, 361(14), 1376–1385. https://doi.org/10.1056/NEJMra0807633 ↩
- Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2. Sexually Transmitted Diseases, 30(4), 310–314. https://doi.org/10.1097/00007435-200304000-00007 ↩












2 Responses
This is the best health blog. Gives hope and easy to follow medicinal steps
Herbal treatments might work because modern medicine has never found a cure yet.