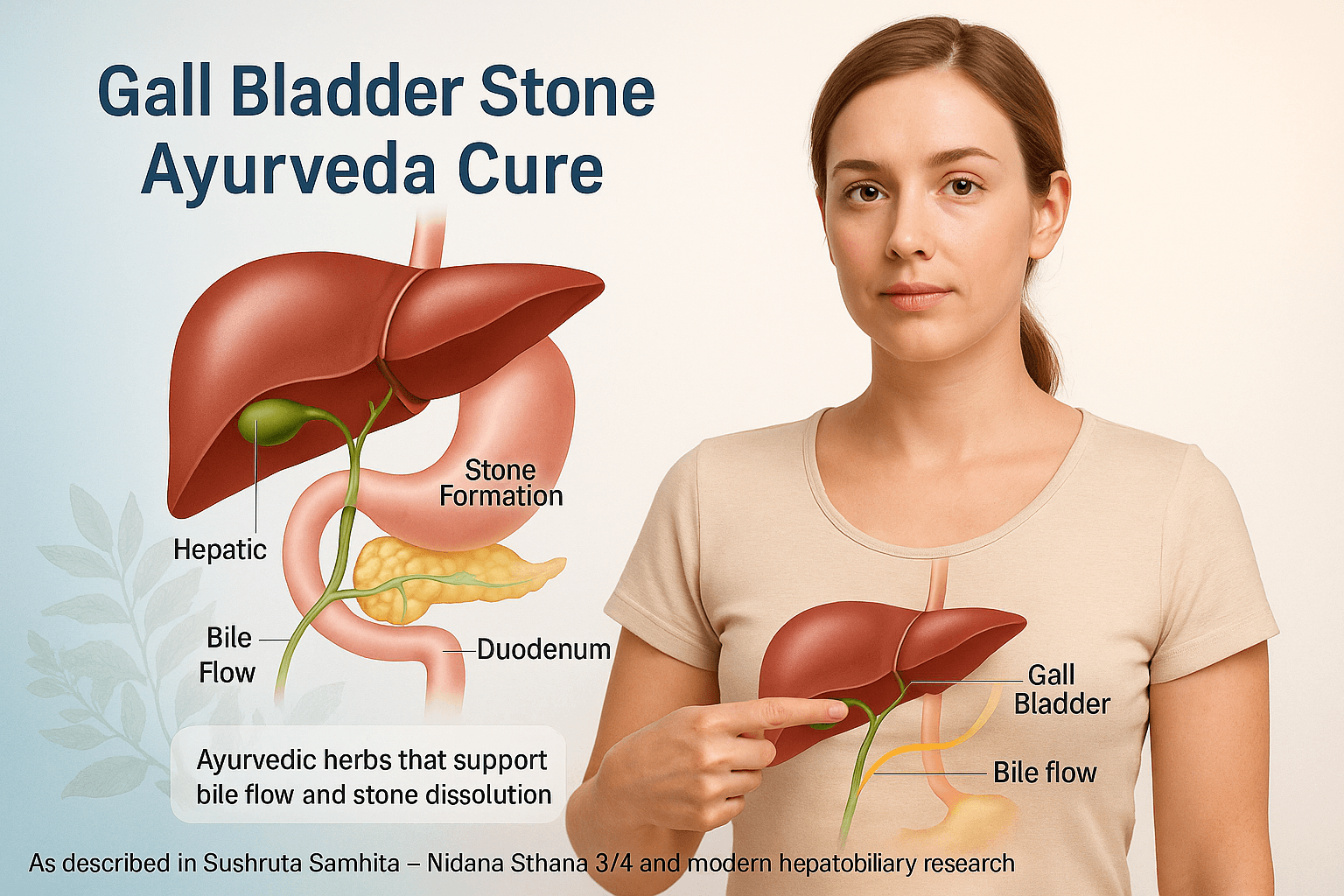
- Gall Bladder Stone Ayurveda Cure:
- Understanding Your Gall Bladder
- What Causes Gall Bladder Stones (Pittashmari)
- Symptoms-When Your Body Starts Warning You
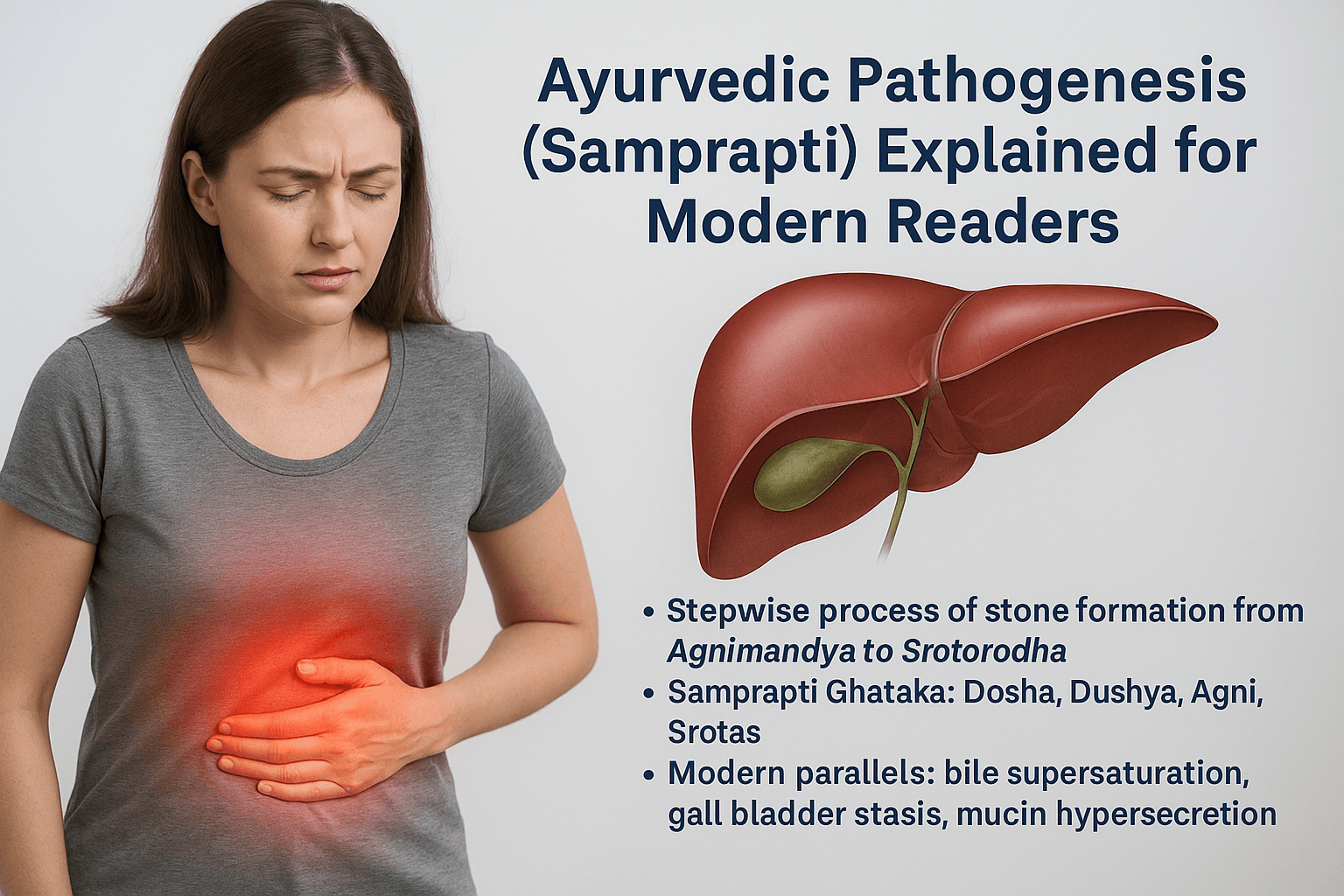
- Ayurvedic Pathogenesis (Samprapti) Explained for Modern Readers
- Modern Diagnostic Approaches
- Common Disorders Associated With Gall Bladder Stones
- Rare and Often Missed Disorders Associated With Gall Bladder Stones
- Red Alert- When Gall Bladder Pain Is Not Just Stones
- Differential Diagnosis of Right Upper Quadrant Pain
- Ayurvedic Treatment Protocol for Gall Bladder Stones (Pittashmari)
- Varunadi Avaleha (Main Medicine) – Mandatory
- Varunadi Avaleha – Preparation
- Why these herbs and minerals (brief mechanisms)
- Why Market-Bought or Self-Prepared Ayurvedic Medicines Fail in Gall Bladder Stones
- Why Only Personalized Ayurvedic Treatment Works
- Modern Management and Limitations
- Scientific Validation
- Frequently Asked Questions (FAQs)
- References
Gall Bladder Stone Ayurveda Cure:
Gall bladder stones, medically termed cholelithiasis, have silently become one of the most widespread digestive disorders across the world. In Western countries, nearly 15% of adults suffer from some form of gallstones, while in India and Southeast Asia, the numbers are steadily rising due to changing dietary habits and sedentary lifestyles [3].
From a biomedical standpoint, gallstones are solid crystalline concretions formed inside the gall bladder, primarily composed of cholesterol, bile pigments, and calcium salts [5]. These stones develop when the delicate balance of bile composition—cholesterol, bile acids, and phospholipids—gets disturbed. As bile thickens, cholesterol precipitates, leading to sludge and ultimately calculi formation [8].
However, the modern approach to gallstones remains largely mechanical—focusing on surgery (cholecystectomy) or dissolution drugs—without addressing the deeper metabolic and digestive causes that lead to recurrent bile imbalance. Ayurveda, on the other hand, interprets gallstones as the physical manifestation of Pitta–Kapha derangement and disturbed Agni (digestive metabolism) [1].
Ayurveda’s Broader Vision of Gallstones
In classical Ayurvedic literature, gall bladder stones correlate with Pittashmari, one of the four major types of Ashmari Roga mentioned in Sushruta Samhita Nidana Sthana 3/4 [1]. The word “Pittashmari” translates to “stone arising from aggravated Pitta.”
According to Sushruta, when Pitta Dosha—which governs bile formation and fat metabolism—becomes vitiated due to an improper diet, stress, or suppression of natural urges, it combines with Kapha, producing a sticky, mucilaginous bile that gradually hardens into stones inside the Pittashaya (gall bladder) [1].
Charaka Samhita Chikitsa Sthana 26/40–45 further elaborates that faulty digestion (Agnimandya) and accumulation of undigested metabolic toxins (Ama) are the initiating factors for all forms of Ashmari, including Pittashmari [2]. This imbalance blocks the natural flow of bile and creates stagnation in the biliary system.
Thus, Ayurveda explains gall bladder stones not as isolated deposits but as end-products of disturbed metabolism, where the body’s fire (Agni) becomes weak, bile becomes impure, and the channels (Srotas) get blocked. This integrative view reveals why surgery alone does not guarantee a cure—because unless the root imbalance is corrected, new stones will form again.
Why Gallstones Are Increasing Worldwide
Modern lifestyle patterns have made gallstones a global epidemic:
- Fatty and fried foods such as cheese, butter, fried snacks, and red meat cause cholesterol saturation in bile and slow gall bladder emptying [7].
- Refined sugars, sweets, and bakery foods trigger insulin resistance and alter lipid metabolism, directly affecting bile solubility [6].
- Excessive sour, spicy, and fermented foods, alcohol, and irregular eating habits over-stimulate Pitta Dosha, leading to concentrated bile [9].
- Sedentary lifestyles, hormonal contraceptives, obesity, and rapid weight loss are scientifically linked to bile stasis and gallstone formation [3].
- In Ayurvedic terms, these are classic Pitta–Kapha aggravating factors that thicken bile and block the gall bladder’s natural flow [1].
Together, these dietary and lifestyle triggers explain why gallstones now occur even in young, health-conscious individuals. The disease is not simply about bile—it is about how modern habits paralyze digestive intelligence.
The Ayurvedic Promise- Cure, Not Removal
While modern surgery removes the gall bladder, Ayurveda restores its function. Through a sequence of Shodhana (detoxification), Shamana (pacification), and Rasayana (rejuvenation) therapies, classical formulations dissolve stones, cleanse bile, and prevent recurrence [4].
Key Ayurvedic formulations such as Varunadi Kashayam, Gokshuradi Guggulu, and Pashanbhedadi Kwath have been clinically shown to improve bile composition and facilitate natural expulsion of calculi [10]. Complementary Rasayana medicines like Abhrak Bhasma and Swarna Makshik Bhasma help restore liver metabolism and prevent stone reformation [11].
Ayurveda thus shifts the focus from removal to restoration. By reviving Agni, balancing bile secretion, and detoxifying the liver, it offers what modern medicine rarely promises—a permanent, metabolic cure rather than symptomatic management.
What This Article Covers
In the following sections, we will explore:
- how the gall bladder functions in both modern and Ayurvedic science,
- which specific foods and habits trigger gallstone formation,
- and how carefully personalized Ayurvedic therapies can dissolve stones naturally while strengthening the liver and digestive system.
The goal is not just relief—but complete metabolic freedom from gall bladder stones, rooted in Ayurvedic science and modern validation.
Understanding Your Gall Bladder
How it works
The gall bladder is a small pear-shaped organ situated beneath the liver, serving as the storage and concentrator of bile. Bile is a yellow-green fluid composed of water, bile acids, cholesterol, bilirubin, and electrolytes, essential for breaking down dietary fats and eliminating waste from the liver into the intestines [5]. When food, particularly fatty meals, enters the digestive tract, the gall bladder contracts and pushes bile through the bile duct into the small intestine. This action helps emulsify fats into smaller particles, allowing digestive enzymes to absorb them more efficiently [8].
From a broader health perspective, proper bile flow ensures balanced lipid metabolism, regular bowel movement, and toxin elimination. Any stagnation or alteration in bile composition can trigger a cascade of metabolic problems, ultimately leading to stone formation.
Ayurvedic understanding
According to Ayurveda, the gall bladder’s function is closely linked with Pitta Dosha, which governs digestion, transformation, and metabolism within the body [1]. The bile itself, called Pitta Dravya, is a physical manifestation of Ranjaka Pitta residing in the Yakrit (liver) and Pittashaya (gall bladder) [2]. Just as bile transforms food fats into absorbable forms, Pitta Dosha transforms food into energy and nutrients.
When Pitta remains balanced, the digestive fire or Agni works smoothly. However, irregular eating habits, overeating, excessive consumption of spicy and oily food, or stress can vitiate Pitta, making it either overly sharp (Tikshna) or weak (Manda). In both situations, digestion becomes disturbed, and Ama (metabolic toxins) start accumulating [9]. These toxins mix with the bile, making it thick, sticky, and less capable of flowing properly.
Where stones begin
When bile becomes stagnant and concentrated, cholesterol and bile pigments begin to crystallize, forming microscopic particles that grow into stones [5]. Ayurveda describes this condition as Srotorodha, or obstruction of the body’s microchannels. It happens when aggravated Pitta combines with Kapha, forming a viscous substance that blocks natural bile flow. This stage is considered the initial phase of Pittashmari, or gall bladder stone formation [1].
In addition, aggravated Vata Dosha also contributes to this disorder. Irregular eating, skipping meals, fasting for long durations, or chronic stress aggravate Vata, which controls all movement in the body. Once Vata is disturbed, the contraction and relaxation of the gall bladder become erratic, causing incomplete bile release [10]. These combined imbalances slowly lead to bile saturation, poor fat metabolism, and the gradual development of stones.
Modern and Ayurvedic correlation
Modern medicine attributes gallstone formation to cholesterol supersaturation, gall bladder hypomotility, and bile sludge accumulation [5]. Ayurveda parallels these conditions with Pitta-Kapha vitiation, Vata disturbance, and Ama formation [1]. The transformation of liquid bile into solid concretions reflects the failure of Agni and the stagnation of Pitta within the biliary tract.
In both sciences, the disease begins with subtle metabolic dysfunction rather than an isolated event. It is a process in which bile chemistry deteriorates, digestive rhythm breaks down, and the liver’s purification capacity weakens.
The liver–gall bladder connection
The liver continuously produces bile, while the gall bladder stores and releases it when needed. When coordination between the two becomes weak—due to excess dietary fat, stress, alcohol, hormonal changes, or lack of exercise—bile flow becomes sluggish and concentrated [3]. Ayurveda identifies this as Yakrit Dushti, or liver imbalance, along with disturbed Pittavaha Srotas, the channel responsible for bile flow [4]. Restoring this coordination is one of the main goals of Ayurvedic therapy. It is achieved through gentle detoxification, herbal formulations that cleanse the liver, and Rasayana therapy to strengthen the digestive fire.
Key insight for patients
The gall bladder is not just a passive bile reservoir; it acts as a dynamic regulator of metabolism and energy transformation. Ayurveda describes it as the physical seat of Pitta, the very principle of digestion and cellular transformation. When Pitta is balanced, bile flows freely, fats are metabolized efficiently, and the liver works in harmony. When it is disturbed, bile becomes thick, toxic, and obstructive, laying the foundation for Pittashmari.
Modern medicine removes the gall bladder when stones form, but Ayurveda focuses on restoring its natural intelligence. It sees the condition as reversible if the underlying doshic imbalance is corrected. Through proper diet, detoxification, and liver-strengthening herbs, the gall bladder can regain its full function.
The next section will explain how gall bladder stones form in detail, what foods and habits cause them, and how Ayurveda interprets this process through the combined disturbances of Pitta, Kapha, and Ama accumulation.
What Causes Gall Bladder Stones (Pittashmari)
The Root of the Problem: When Bile Loses Its Balance
Gall bladder stones, or cholelithiasis, arise from one core disturbance: the chemical imbalance of bile. Bile is normally a fine-tuned mixture of cholesterol, bile salts, and phospholipids that keeps fats soluble and flowing. When this ratio is disturbed—either by excess cholesterol, reduced bile acids, or sluggish bile flow—the components precipitate into crystals that gradually grow into stones [5].
In modern medicine, this is described as bile supersaturation and stasis, while Ayurveda views it through the lens of Pitta–Kapha aggravation, Ama accumulation, and Meda Dhatu (fat tissue) dysfunction [1]. The two sciences describe the same pathology using different languages: one biochemical, the other energetic and metabolic.
Modern Medical Causes of Gall Stones
1. Cholesterol Imbalance
Most gallstones—up to 80%—are cholesterol stones. The liver secretes cholesterol into bile, but if the amount exceeds what bile salts and phospholipids can dissolve, crystals begin to form [8]. A diet rich in fried foods, red meat, and dairy worsens this imbalance. Estrogen, obesity, and genetic factors further increase cholesterol saturation.
In Ayurvedic terms, this represents excess Meda Dhatu and Pitta Dushti, where the fire of metabolism becomes uneven: strong in some pathways but weak in digestion. The result is incomplete fat metabolism and toxic residues accumulating in bile [2].
2. Obesity and Metabolic Syndrome
Obesity doubles the risk of gallstones, especially when accompanied by insulin resistance. Elevated insulin increases cholesterol secretion into bile and reduces gall bladder motility [6]. Fat tissue also acts as an endocrine organ, releasing inflammatory cytokines that damage liver function.
Ayurveda explains this as Meda Vriddhi—an expansion of the fat tissue due to weak Agni (digestive fire). As the Agni declines, Kapha accumulates, thickening the bile and slowing its flow [1].
3. Insulin Resistance and Diabetes
Insulin resistance not only alters bile composition but also impairs gall bladder contraction. High blood sugar thickens bile and reduces its water content [7]. Diabetic individuals often have sluggish digestion (Mandagni) and low enzymatic activity, both precursors for stone formation.
From the Ayurvedic view, this corresponds to Ama–Meda Dushti, where unburnt metabolic toxins accumulate within the fat channels (Meda Vaha Srotas) and infiltrate the liver-bile system. The stagnation creates a fertile ground for Pittashmari.
4. Hormonal Factors
Women are more prone to gallstones, particularly during pregnancy, menopause, or when taking oral contraceptives. Estrogen increases cholesterol secretion into bile, while progesterone slows gall bladder emptying [9]. These hormonal effects lead to bile concentration and sedimentation.
Ayurveda acknowledges a similar concept through Shukra and Artava Dhatu involvement, where hormonal imbalance disturbs Pitta and Meda metabolism. Emotional stress, suppressed urges, and irregular routines amplify this hormonal chaos.
5. Rapid Weight Loss or Crash Diets
Sudden fasting or extreme calorie restriction triggers gall bladder stasis. The body, in a state of survival metabolism, releases cholesterol from tissues faster than bile can process it [10]. This overload saturates bile and precipitates stone formation.
Ayurveda calls this Langhana Atiyoga—overindulgence in fasting that aggravates Vata and depletes digestive fire. When Agni weakens, bile flow halts, and Kapha stagnation ensues, causing stones.
Ayurvedic Nidana (Causative Factors)
Ayurveda describes gall bladder stones under the broader category of Ashmari Roga, and the subtype Pittashmari represents stones formed due to Pitta aggravation combined with Kapha obstruction. The key Nidanas (causative factors) are:
- Pitta–Kapha aggravating diet: oily, spicy, fermented, sour, and fried foods [1]
- Mandagni: sluggish digestion leading to Ama accumulation
- Meda Dushti: impaired fat metabolism causing thick bile
- Srotorodha: obstruction in bile ducts due to sticky Kapha
- Vata Anubandha: Vata involvement causing irregular bile release
According to Sushruta Samhita Nidana Sthana 3/4, when Kapha accumulates within the bile channels and combines with vitiated Pitta, the mixture solidifies into stone-like masses in the gall bladder [1]. This ancient description parallels modern findings of bile stasis, cholesterol supersaturation, and mucin gel accumulation.
Detailed Dietary Triggers and Their Mechanisms
Diet is one of the most powerful modulators of bile chemistry. Certain foods promote bile fluidity, while others cause thickening and stasis.
1. Fried and Oily Foods
Deep-fried snacks, fast foods, and oily curries raise bile cholesterol concentration and inhibit gall bladder contractions [5]. Repeated reheating of oils generates trans fats, which not only thicken bile but also impair liver detoxification. Ayurveda classifies these as Guru (heavy) and Snigdha (unctuous) foods that increase Kapha and Meda, leading to Srotorodha.
2. Red Meat and Processed Meats
High intake of red meat, sausages, and processed meats increases cholesterol and bile acid imbalance. These foods burden the liver’s lipid metabolism [8]. Ayurvedically, meat, especially from animals like pork and buffalo, is considered Abhishyandi—obstructive to body channels and conducive to stone formation.
3. Full-Fat Dairy and Cheese
Cream, butter, and cheese contain saturated fats that increase cholesterol in bile and reduce bile salt activity. In Ayurveda, excessive milk and curd are known to thicken bodily fluids and disturb Kapha and Pitta. Uncooked curd, in particular, is contraindicated for those with Pitta-related disorders.
4. Sugary and Refined Foods
Excess sugar, pastries, and white flour products trigger insulin resistance, one of the root causes of gallstones [6]. Ayurveda calls this Ati Madhura Ahara—overuse of sweet-tasting foods that increase Kapha, leading to obesity, lethargy, and bile stagnation.
5. Sour and Fermented Foods
Pickles, vinegar, tamarind, citrus, and fermented foods cause Pitta aggravation. This overstimulates bile secretion and makes it excessively acidic [9]. Prolonged Pitta excess scorches Agni and damages the bile ducts, encouraging crystal deposition.
6. Alcohol and Coffee
Alcohol inflames the liver and changes bile composition, while excessive coffee increases acidity and Pitta. In moderate amounts, coffee can promote bile flow, but overuse dehydrates bile and irritates the gall bladder mucosa. Ayurveda describes alcohol (Madya) as a prime Pitta vitiator when used habitually.
7. Reheated Oils and Leftover Food
Reheated or old food loses its Prana (vital energy) and becomes Ama Karaka—toxin-forming. Chemically, reheating oils forms aldehydes and oxidized lipids that damage liver cells and increase bile viscosity [10].
8. Vegetables That Increase Pitta and Gas
Certain vegetables, though healthy, can aggravate Pitta or Vata if overused. Tomatoes, eggplants, onions, garlic, and radish are acidic and pungent, increasing bile sharpness. Cabbage and cauliflower, when undercooked, promote gas and Ama formation. Ayurveda recommends balancing them with cooling spices like cumin, coriander, and fennel.
9. Fruits That Aggravate Kapha and Pitta
Bananas, mangoes, custard apples, and overripe fruits contain high sugar and mucilage, worsening Kapha and Meda. Citrus fruits like oranges and lemons, if taken excessively, increase Pitta and acidity. Ayurveda advises moderation and timing—fruits should be consumed between meals, not after heavy food.
10. Excess Dairy and Ice-Cold Drinks
Cold milkshakes, ice creams, and carbonated drinks suppress Agni and thicken bile. The combination of cold and sweet aggravates both Kapha and Ama, hindering bile flow. Modern studies confirm that frequent consumption of sugary cold beverages increases gallstone risk.
Hidden Triggers Often Overlooked
Fasting and Skipping Meals
Skipping breakfast or following long fasting rituals without supervision slows gall bladder contraction, leading to bile stagnation [10]. Ayurveda recognizes this as Vata Prakopa—the disturbance of motion energy. Instead of detoxifying, unsupervised fasting depletes digestive fire, creating more Ama.
Late-Night Meals and Irregular Eating
Eating late at night keeps bile secretion active when the body should be resting. It interferes with liver detox cycles and causes bile to thicken. Ayurveda identifies this as Ratri Bhojana, a primary cause of Pitta–Kapha imbalance.
Reheated Oils and Junk Food
As mentioned, reheated oils are toxic not only for the liver but also for the blood. They generate free radicals, oxidize cholesterol, and directly damage the gall bladder lining [8]. Ayurveda equates this to consuming Viruddha Ahara—incompatible foods that corrupt Dhatus and Srotas.
Excess Coffee or Tea
High caffeine intake leads to dehydration and hyperacidity, increasing bile concentration. Ayurveda attributes this to Pitta aggravation. Occasional coffee is acceptable, but chronic dependence disturbs both liver and gall bladder rhythms.
Stress, Sedentary Life, and Hormonal Link
Modern studies confirm that stress and inactivity are major risk factors for gallstones. Cortisol and adrenaline surges disturb insulin function, leading to fat accumulation and altered bile chemistry [7]. Long sitting hours, especially after heavy meals, prevent gall bladder contraction, causing bile stagnation.
Ayurveda acknowledges this psychosomatic connection. Chronic stress aggravates Vata and Pitta, while lack of movement increases Kapha. The trio creates an environment where digestion is irregular, bile is erratic, and emotions like anger or worry directly impair liver function.
Hormonal imbalances—especially estrogen dominance—further complicate the picture. Ayurveda explains this under disturbed Artava and Shukra Dhatu, where endocrine instability fuels Pitta excess and liver congestion. Thus, gallstones often accompany stress, mood fluctuations, menstrual irregularities, or menopausal symptoms.
In Essence
Gall bladder stones are not formed overnight; they are the culmination of years of metabolic disharmony. Irregular eating, wrong food combinations, excessive fats, stress, and sedentary living first impair Agni. Gradually, Pitta becomes sharp and erratic, Kapha becomes sticky, and Vata disturbs bile flow. These imbalances merge to produce thickened bile, leading to crystallization and stone formation.
Modern science describes this sequence as cholesterol supersaturation, nucleation, and gall bladder hypomotility. Ayurveda describes it as Pitta–Kapha–Vata vitiation with Srotorodha and Ama deposition. Both ultimately describe the same process from different dimensions.
Ayurveda’s wisdom, however, adds one crucial dimension: the possibility of reversal. By restoring Agni, correcting diet, and using liver-cleansing and bile-flow-enhancing herbs, the body can dissolve stones naturally and prevent recurrence.
Symptoms-When Your Body Starts Warning You
From bloating to biliary colic
Gall bladder stones often develop quietly, remaining unnoticed for months or even years. The earliest warning signs are subtle—abdominal fullness, post-meal heaviness, or discomfort after consuming fried foods. As the stones enlarge or shift, pain becomes more defined. The hallmark feature is biliary colic, a gripping pain in the upper right abdomen that may radiate to the shoulder or back [5]. It often appears after heavy or fatty meals when the gall bladder contracts to release bile.
This occurs when a stone temporarily obstructs the cystic duct, increasing internal pressure. The pain may persist for 30 minutes to several hours and is frequently accompanied by sweating or nausea. Ayurveda interprets this as the simultaneous aggravation of Pitta and Vata Dosha—Pitta produces the burning sensation, while Vata causes spasmodic pain and erratic bile movement [1].
Each pain episode indicates a deeper loss of metabolic coordination between bile production, storage, and flow.
Digestive disturbances
In many cases, gall bladder disease first manifests as minor digestive complaints: acidity, gas, bloating, nausea, burping, or an aversion to oily food. These reflect Agnimandya, a weakened digestive fire, where the breakdown and assimilation of fat are compromised [2]. When bile becomes thick and stagnant, undigested toxins (Ama) accumulate in the intestines. This leads to foul-smelling stools, irregular appetite, heaviness, and fatigue after eating.
Over time, chronic bile sluggishness may cause alternating constipation and loose stools, often confused with irritable bowel syndrome. Ayurveda considers this as Ama-Kapha Sanchaya, a stage of toxin and mucus accumulation that eventually blocks the bile ducts.
Silent stones versus acute attacks
Some people carry gallstones for years without any symptoms. These silent stones are usually found incidentally during ultrasound scanning [8]. Ayurveda identifies this latent stage as Sthira Avastha of Pittashmari, meaning the stones are stable and not causing acute irritation [1].
When the stones begin to move or irritate the gall bladder lining, inflammation sets in. This condition, known as acute cholecystitis, presents with constant right-sided pain, tenderness, fever, nausea, and vomiting. Modern medicine attributes this to bacterial infection following bile entrapment, while Ayurveda describes it as Teekshna Pitta Prakopa, an aggressive flare of Pitta combining with Ama to inflame tissues [9]. If untreated, this stage can progress to infection of the bile ducts or pancreas.
Systemic and radiating symptoms
Gall bladder stones can influence the whole digestive and circulatory system. Patients often experience generalized fatigue, bitterness in the mouth, and mild yellowing of the eyes or skin. Stool color may turn pale due to reduced bile pigment [5]. Ayurveda associates these changes with Ranjaka Pitta Dushti, indicating improper bile flow and incomplete blood purification.
Pain may also radiate beyond the abdomen—to the shoulder blade, chest, or even mimic cardiac discomfort. Some individuals report right-sided neck stiffness or upper-back tension, caused by referred muscular pain along the phrenic nerve. This pattern corresponds to Vata-Pravritta Shula, where pain travels through interconnected channels rather than remaining localized [10].
Ayurvedic language of imbalance: Parshva Shula, Daha, Vibandha
Classical Ayurvedic texts describe gall bladder pain using characteristic terms. Sushruta Samhita Nidana Sthana 3/4 defines Pittashmari as producing Parshva Shula (flank pain), Teekshna Daha (burning heat), and Vibandha (constipation) [1].
Parshva Shula corresponds to radiating pain along the ribs and back due to Vata’s obstruction. Daha represents internal heat, heartburn, or acid reflux from aggravated Pitta. Vibandha indicates sluggish bowels and abdominal tightness caused by stagnant bile and weakened Agni.
Together, these three form the classical triad of biliary imbalance: pain, heat, and obstruction.
Rare and atypical symptoms
Gall bladder stones sometimes present in unusual ways that lead to misdiagnosis if clinicians or patients are unaware:
1. Chronic headaches or migraine-like pain: Disturbed bile secretion increases systemic Pitta, which rises upward and irritates the cranial vessels. Ayurveda classifies this as Urdhva Gata Pitta, explaining why some patients experience recurring headaches or dizziness without apparent digestive symptoms [7].
2. Itchy skin or hives: Retention of bile acids under the skin causes pruritus. Ayurveda recognizes this as Pitta Rakta Dushti, where bile toxins enter the bloodstream and irritate the skin channels.
3. Bitter taste in the mouth or metallic after taste: A sign of bile reflux into the stomach and mouth. It correlates with Tikta Utklesha, excessive bile secretion overwhelming the digestive tract.
4. Chronic nausea or motion sickness-like feeling: Persistent queasiness even without food intake is common in gall bladder dysfunction. Ayurveda views it as Vata-Pitta Kopa in the Amasaya (stomach).
5. Pain during deep breathing: Inflamed gall bladder tissue can irritate the diaphragm, causing discomfort on inhalation. This reflects Vata obstruction in Pranavaha Srotas.
6. Right-sided shoulder and jaw pain: Referred pain via the phrenic nerve can mimic cervical or dental issues. Ayurveda interprets this as Vata-Anubandha Shula, where the obstructed air element transmits discomfort through adjacent pathways.
7. Night sweats or heat surges: Episodes of heat at night signify excess internal Pitta trying to expel through the skin.
8. Hormonal or menstrual irregularities: In women, chronic liver–gall bladder congestion affects estrogen metabolism, leading to PMS, heavier periods, or mood swings. Ayurveda includes this under disturbed Artava Dhatu related to liver congestion.
9. Depression or irritability: Emotional stagnation mirrors bile stagnation. The gall bladder, energetically linked to decisiveness and courage, when imbalanced, causes mood suppression and indecisiveness. Ayurveda equates this with Manovaha Srotas Dushti, highlighting the mind-liver connection.
10. Unexplained bad breath and coated tongue: Indicative of bile backflow and Ama accumulation in the gastrointestinal tract. Ayurveda identifies this as Mukha Daurgandhya due to Ama Dosha.
These atypical symptoms are especially common in chronic or subclinical gall bladder dysfunction, long before full-blown cholecystitis appears.
Emotional and psychosomatic aspects
Modern studies confirm that prolonged stress and emotional suppression alter bile secretion and gall bladder motility [7]. Cortisol surges and high sympathetic activity constrict the ducts and hinder bile release. Ayurveda perfectly mirrors this by stating that anger, fear, and unresolved frustration vitiate Pitta and disturb the downward flow of Vata. Over time, this internal “heat of emotion” thickens bile and manifests as stones.
Such patients often report anxiety, sleep disturbances, or irritability accompanying digestive issues. The liver–gall bladder system thus becomes both a physical and emotional center for detoxification.
Early warning signs and when to act
When symptoms such as bloating, acid reflux, or right-sided pressure occur repeatedly after meals, it is a signal that bile flow has already slowed. Ayurveda recommends early evaluation through Nadi Pariksha and Mutra Pariksha, which detect metabolic irregularities even before imaging shows stones [1].
Modern diagnostics like ultrasound and liver function tests complement this by quantifying the extent of bile stasis. Combining both perspectives allows physicians to identify not only the presence of stones but the metabolic terrain that caused them.
If treatment begins at this stage—through dietary correction, mild detoxification, and liver-strengthening Rasayanas—stone dissolution becomes achievable without surgical intervention.
Summary for patients
Gall bladder stones announce their presence through a wide range of digestive and systemic symptoms. From mild bloating to severe biliary pain, from bitter taste to skin itching, each signal points to a disruption in bile flow. Ayurveda interprets all these as different expressions of Pitta, Vata, and Kapha disharmony in the liver-bile network.
Recognizing these symptoms early is the key to prevention. The sooner one restores digestive balance and bile fluidity, the greater the chance of dissolving stones naturally and avoiding surgery.
The following section will explain how modern diagnostic imaging and classical Ayurvedic examination methods work together to identify gall bladder stones with precision and guide personalized treatment.
Ayurvedic Pathogenesis (Samprapti) Explained for Modern Readers
Understanding the Mechanism: How Gall Stones Develop Step by Step
Gall bladder stones, or Pittashmari, are not sudden formations but the result of a gradual process of metabolic and energetic imbalance. Ayurveda explains this through the principle of Samprapti, meaning the sequential pathogenesis of a disease from subtle imbalance to gross manifestation. Modern medicine parallels this concept through phases of bile supersaturation, gall bladder stasis, and mucin hypersecretion, each describing a different part of the same biological event [5].
Ayurveda views this as a cascade beginning with Agnimandya (digestive impairment) and ending with Srotorodha (obstruction of bile channels). When digestion weakens, metabolic toxins accumulate, bile thickens, and eventually solid particles (stones) form within the gall bladder.
Step 1: Agnimandya – The Decline of Digestive Fire
The story of gallstone formation begins with Agnimandya, a weakened digestive fire. Poor dietary habits, overeating, late-night meals, emotional stress, and lack of physical activity disturb the body’s natural rhythm of digestion [1]. This weakened Agni fails to transform food into clean energy and tissues. Instead, it produces Ama—a sticky, partially digested residue that circulates in the body.
Modern medicine identifies a similar stage as impaired fat metabolism and cholesterol imbalance, where undigested lipids and inflammatory compounds start altering bile chemistry. Bile, which should flow freely, becomes sluggish and thick, the first biochemical step toward stone formation.
Step 2: Ama Formation and Accumulation in the Liver and Bile Channels
Once Ama is formed, it infiltrates the Yakrit (liver) and Pittashaya (gall bladder) through the channels known as Rasa Vaha and Meda Vaha Srotas. These channels carry nutrients, fats, and bile. The sticky nature of Ama mixes with Kapha and coats the inner walls of the bile ducts, making them heavy and resistant to flow [2].
This corresponds to the modern understanding of bile sludge, a mixture of cholesterol crystals, mucin, and calcium salts. Over time, the stagnant bile becomes supersaturated with cholesterol, which crystallizes into tiny stones. These microcrystals are the earliest sign of gall bladder dysfunction but often remain asymptomatic.
Step 3: Vitiation of Pitta and Kapha Doshas
In Ayurveda, the liver and gall bladder are governed primarily by Pitta Dosha, the principle of heat and transformation. When Pitta becomes excessive—due to spicy food, anger, alcohol, or long exposure to heat—it overcooks the bile, making it sharp, concentrated, and acidic. This irritates the gall bladder lining and enhances cholesterol precipitation [1].
Simultaneously, Kapha Dosha increases because of heavy, oily, and sweet foods. The excess Kapha acts as a binder, thickening bile into a viscous substance. When Pitta’s heat and Kapha’s viscosity combine in the gall bladder, they create an ideal environment for stone formation. This union is described as Pitta-Kapha Samyoga, one of the classical etiological combinations for Pittashmari in Sushruta Samhita Nidana Sthana 3/4.
Modern researchers have identified similar mechanisms—bile cholesterol saturation (Kapha equivalent), increased bile concentration (Pitta equivalent), and mucin hypersecretion (Ama equivalent) [9].
Step 4: Srotorodha – Obstruction of Bile Channels
As Ama thickens and combines with Pitta and Kapha, it leads to Srotorodha, or channel blockage. The Pitta Vaha Srotas, which carry bile from the liver to the intestine, become congested. The gall bladder, unable to empty properly, starts accumulating bile that becomes more concentrated and toxic [2].
This blockage mirrors modern biliary stasis, a key stage in gallstone pathophysiology. When bile flow slows, cholesterol and calcium particles settle at the bottom of the gall bladder, forming sediment that gradually hardens into calculi. Ayurveda considers this stage irreversible without detoxification and Rasayana therapy.
Step 5: Paka and Ashmari Nirmana – Crystallization and Stone Formation
Over time, the stagnant bile undergoes Paka (pathological transformation) due to the continued action of vitiated Pitta. Heat within the bile thickens its contents, and Kapha’s viscosity promotes cohesion. Eventually, small crystalline formations appear, initially soft but later hardening into solid stones—this is Ashmari Nirmana, or stone genesis [1].
In modern biochemistry, this corresponds to cholesterol nucleation—the process where supersaturated bile forms solid cholesterol crystals that aggregate over months to years. If the gall bladder remains hypomotile, these crystals do not expel naturally and continue to grow, forming mature stones. This stage correlates exactly with what Ayurveda calls Pittashmari Paka Avastha, where disease has fully matured.
Samprapti Ghataka-The Components of Pathogenesis
The Ayurvedic diagnostic model analyzes each component involved in the pathogenesis:
- Dosha: Pitta (dominant), Kapha (secondary), and Vata (accessory)
- Dushya (Affected tissues): Rasa Dhatu and Meda Dhatu
- Agni (Metabolic fire): Mandagni (low fire) leading to Ama
- Srotas (Channels): Pitta Vaha Srotas and Meda Vaha Srotas
- Udbhava Sthana (origin): Yakrit (liver)
- Sanchara Sthana (spread): Pittashaya (gall bladder)
- Vyakti Sthana (manifestation): Gall bladder region, right upper abdomen
These components together explain how a simple digestive disturbance evolves into a structural disease.
When mapped to biomedical terminology:
- Pitta Dushti = altered bile chemistry
- Kapha Dushti = mucin accumulation
- Ama = metabolic waste and oxidative stress
- Srotorodha = biliary obstruction
- Meda Dushti = fat metabolism error
Thus, Ayurveda’s qualitative understanding of Dosha imbalance aligns with the quantitative data of modern hepatobiliary pathology.
Modern Parallels of Ayurvedic Samprapti
Modern hepatobiliary research identifies three core mechanisms for gallstone development, which align almost identically with Ayurvedic Samprapti:
- Bile supersaturation: Cholesterol exceeds solubility limit, paralleling Kapha-Meda Dushti.
- Gall bladder stasis: Reduced motility, matching Srotorodha due to Kapha obstruction.
- Mucin hypersecretion: Sticky glycoprotein matrix promoting crystal aggregation, analogous to Ama-Kapha Samyoga [5].
This overlap demonstrates how Ayurveda’s energetic model corresponds to modern molecular events. Ayurveda explains why these changes occur (because of Dosha imbalance), while modern medicine describes how (via biochemical pathways).
Interpreting Samprapti for the Modern Reader
The process of gallstone formation can be seen as a cycle between sluggish digestion, toxin accumulation, bile concentration, and obstruction. The root cause always lies in the failure of Agni and the subsequent blockage of Srotas. Once the gall bladder loses its rhythm, both energy (Prana) and matter (bile) stagnate.
Breaking this cycle requires rekindling digestive fire, purifying bile, and restoring channel flow—achieved through Deepana–Pachana (Agni strengthening), Snehana–Swedana (detoxification), and Rasayana (rejuvenation) therapies. These steps reverse the pathogenesis by dismantling it in reverse order—a principle called Samprapti Vighatana in Ayurveda [1].
In Summary
Gall bladder stone formation represents a perfect convergence of ancient Ayurvedic theory and modern biomedical understanding. Ayurveda describes it as Pitta–Kapha obstruction due to weak Agni and Ama accumulation, leading to Pittashmari. Modern science explains it as cholesterol supersaturation, bile stasis, and mucin hypersecretion. Both agree that stagnation, poor metabolism, and dietary excess are central causes.
Recognizing this process allows both systems of medicine to collaborate—Ayurveda offering causative correction and restoration, while modern methods confirm the structural and biochemical changes within the hepatobiliary system.
Modern Diagnostic Approaches
1. Ultrasound (USG Abdomen)
Ultrasound is the first-line and most reliable method for detecting gall bladder stones. It uses sound waves to produce images of the liver, bile ducts, and gall bladder. Stones appear as bright, echoic foci with acoustic shadowing. Ultrasound also reveals the thickness of the gall bladder wall, bile sludge, and any signs of inflammation or infection [8].
Early in the disease, ultrasound can detect thickened bile even before solid stones form, helping physicians monitor metabolic and dietary corrections before complications arise.
2. MRCP (Magnetic Resonance Cholangiopancreatography)
MRCP provides a detailed 3D image of the biliary tree, including the cystic duct and common bile duct. It is particularly valuable when stones migrate into the ducts or when ultrasound results are inconclusive [6]. MRCP can also identify anatomical variations, strictures, or blockages that influence treatment planning.
In Ayurvedic parallel, this imaging corresponds to the observation of Srotas Avarodha, or the mapping of obstructed internal pathways—a concept described thousands of years ago in Charaka Samhita and Sushruta Samhita.
3. HIDA Scan (Hepatobiliary Iminodiacetic Acid Scan)
HIDA scanning evaluates gall bladder function rather than just structure. It measures bile flow from the liver into the small intestine and helps identify bile stasis or gall bladder hypoactivity [9].
This aligns closely with Ayurveda’s concept of Vata Kshaya or Vata Avarodha, where movement of bile and enzymes becomes sluggish due to internal obstruction. A low ejection fraction in HIDA scan can be interpreted as a state of Vata imbalance in Pittavaha Srotas.
4. Liver Function Tests (LFTs) and Lipid Profile
Biochemical markers often show mild elevation in bilirubin or liver enzymes during stone episodes. Lipid profile irregularities, particularly high cholesterol and triglycerides, confirm Meda Dushti, or derangement of fat metabolism [2]. Ayurveda recognizes this stage as the biochemical footprint of disturbed Agni and Ama formation.
Common Disorders Associated With Gall Bladder Stones
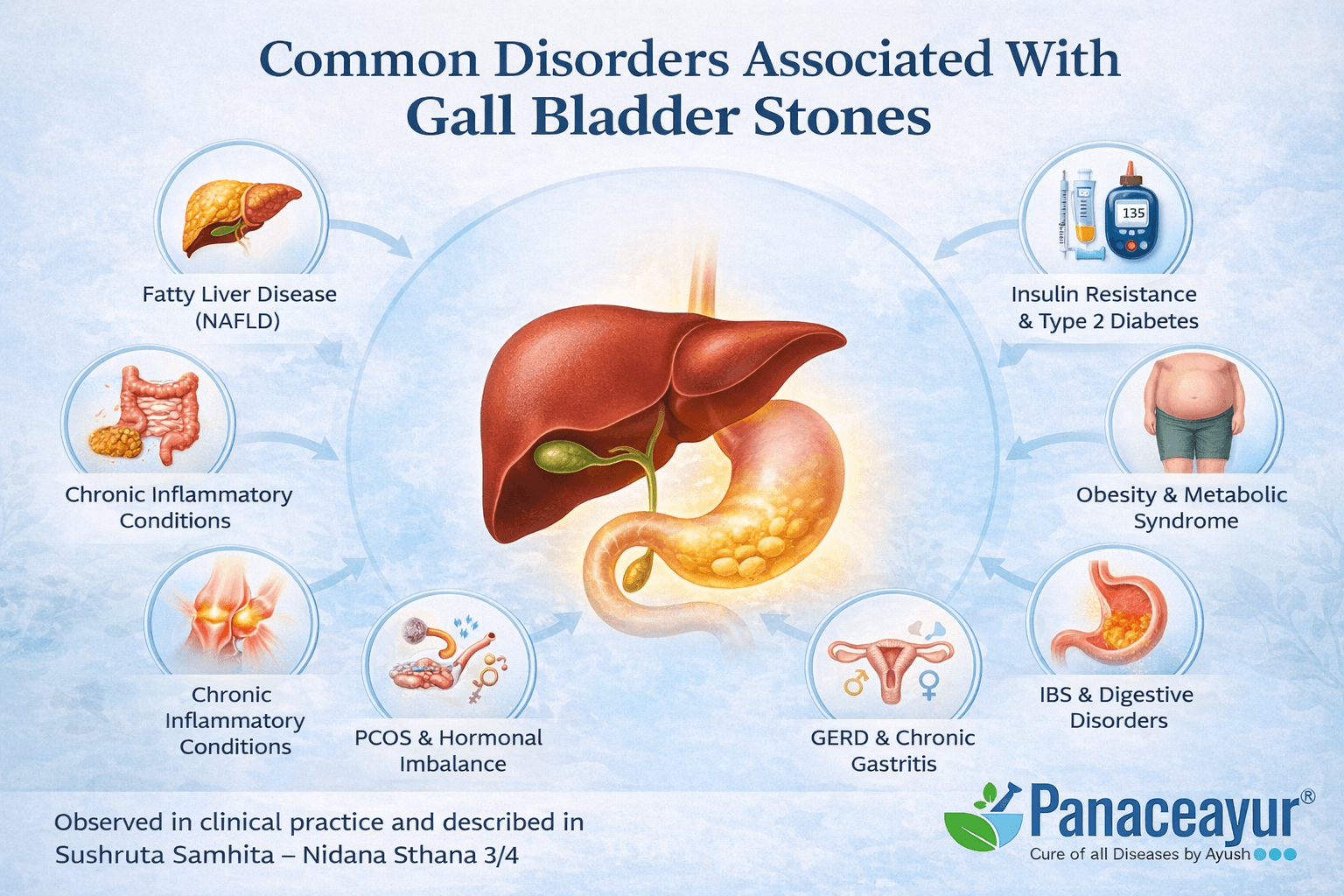
Gall bladder stones rarely occur in isolation. In most patients, they are a visible manifestation of deeper metabolic, digestive, and hormonal disturbances. Modern medicine often treats gallstones as a local biliary problem, but clinical observation shows that many systemic disorders commonly coexist. Ayurveda has long described this phenomenon as Vyadhi Sankara, meaning overlapping or interconnected diseases arising from shared imbalances.
Fatty Liver Disease (Non-Alcoholic Fatty Liver Disease)
Fatty liver is one of the most frequently associated conditions in patients with gall bladder stones. When excess fat accumulates in liver cells, bile production becomes altered in both quantity and composition. Cholesterol-rich, sluggish bile is more likely to crystallize, leading to stone formation. Even after gall bladder removal, untreated fatty liver continues to disturb bile chemistry, explaining why some patients develop bile duct stones later. Ayurveda links this condition to Meda Dushti and Yakrit Mandagni, where fat metabolism and liver fire are weakened simultaneously.
Insulin Resistance and Type 2 Diabetes
Insulin resistance alters cholesterol metabolism and increases hepatic cholesterol secretion into bile. Diabetic patients often produce bile that is supersaturated with cholesterol, making gallstone formation more likely. Additionally, autonomic nerve dysfunction in diabetes can impair gall bladder contraction, leading to bile stasis. Ayurveda interprets this overlap as Kapha-pradhana Prameha with secondary Pitta involvement affecting bile (Pittavaha Srotas).
Obesity and Metabolic Syndrome
Obesity is not just a risk factor but a frequent coexisting disorder in gallstone patients. Excess body fat increases cholesterol turnover and secretion into bile. Rapid weight gain or loss further destabilizes bile composition. Metabolic syndrome, characterized by abdominal obesity, dyslipidemia, and hypertension, shares a common inflammatory and metabolic background with gallstones. In Ayurvedic terms, this reflects chronic Kapha accumulation with blocked channels (Srotorodha).
Hypothyroidism
Hypothyroidism is a commonly overlooked association. Reduced thyroid hormone levels slow overall metabolism, including bile flow and gall bladder emptying. Sluggish bile remains in the gall bladder longer, promoting crystal nucleation. Many patients with gallstones also report cold intolerance, weight gain, and fatigue, pointing toward an underlying thyroid imbalance. Ayurveda correlates this with Agni Mandya at both systemic and tissue levels.
Irritable Bowel Syndrome and Chronic Digestive Disorders
Patients with gall bladder stones frequently suffer from bloating, gas, alternating constipation and loose stools, and food intolerance. These symptoms may precede stone formation by years. Poor digestion leads to Ama formation, which disrupts bile quality and intestinal signaling. Modern research links altered gut microbiota and bile acid dysregulation, while Ayurveda recognizes this as Grahani Dushti affecting bile-digestive coordination.
Gastroesophageal Reflux Disease and Chronic Gastritis
Gallstones can coexist with chronic acidity, heartburn, and gastritis. Bile reflux into the stomach, especially after gall bladder dysfunction or removal, irritates the gastric lining. Patients often report bitter taste, nausea, and burning sensations. Ayurveda attributes this to aggravated Pitta moving in the wrong direction (Urdhvaga Pitta).
Polycystic Ovary Syndrome and Hormonal Imbalance in Women
Women with hormonal disorders such as PCOS show a higher incidence of gallstones. Estrogen increases cholesterol secretion into bile and reduces bile acid synthesis. Pregnancy, oral contraceptives, and hormone replacement therapy further elevate this risk. Ayurveda explains this connection through disturbed Artava Dhatu and Pitta-Kapha imbalance, affecting both reproductive and biliary systems.
Chronic Inflammatory Conditions
Low-grade systemic inflammation plays a significant role in gallstone disease. Conditions such as rheumatoid arthritis, chronic skin disorders, and autoimmune tendencies often coexist. Inflammation alters bile composition and damages the gall bladder lining, facilitating stone adherence. Ayurveda views this as persistent Rakta and Pitta Dushti spreading across multiple tissues.
Vitamin Deficiencies and Malabsorption Syndromes
Gallstones are frequently associated with deficiencies of fat-soluble vitamins A, D, E, and K due to impaired bile delivery. Over time, this can contribute to bone weakness, poor immunity, skin issues, and fatigue. After gall bladder removal, these deficiencies may worsen if bile flow remains unregulated. Ayurveda emphasizes this as Dhatu Kshaya resulting from impaired digestion and assimilation.
Psychological Stress and Sedentary Lifestyle Disorders
Chronic stress, anxiety, and sedentary habits indirectly contribute to gallstone formation by disturbing gut-brain signaling and bile secretion. Stress hormones alter gall bladder motility and increase inflammatory mediators. Ayurveda links this to aggravated Vata disrupting the normal movement of Pitta (bile), leading to erratic bile flow and stagnation.
Why Recognizing Associated Disorders Matters
Treating gall bladder stones without addressing these associated conditions often leads to incomplete recovery or recurrence. Whether managed conservatively or surgically, ignoring metabolic, hormonal, and digestive comorbidities leaves the root cause unresolved. Ayurveda therefore emphasizes comprehensive assessment and personalized treatment to restore systemic balance rather than focusing solely on stone removal.
Rare and Often Missed Disorders Associated With Gall Bladder Stones
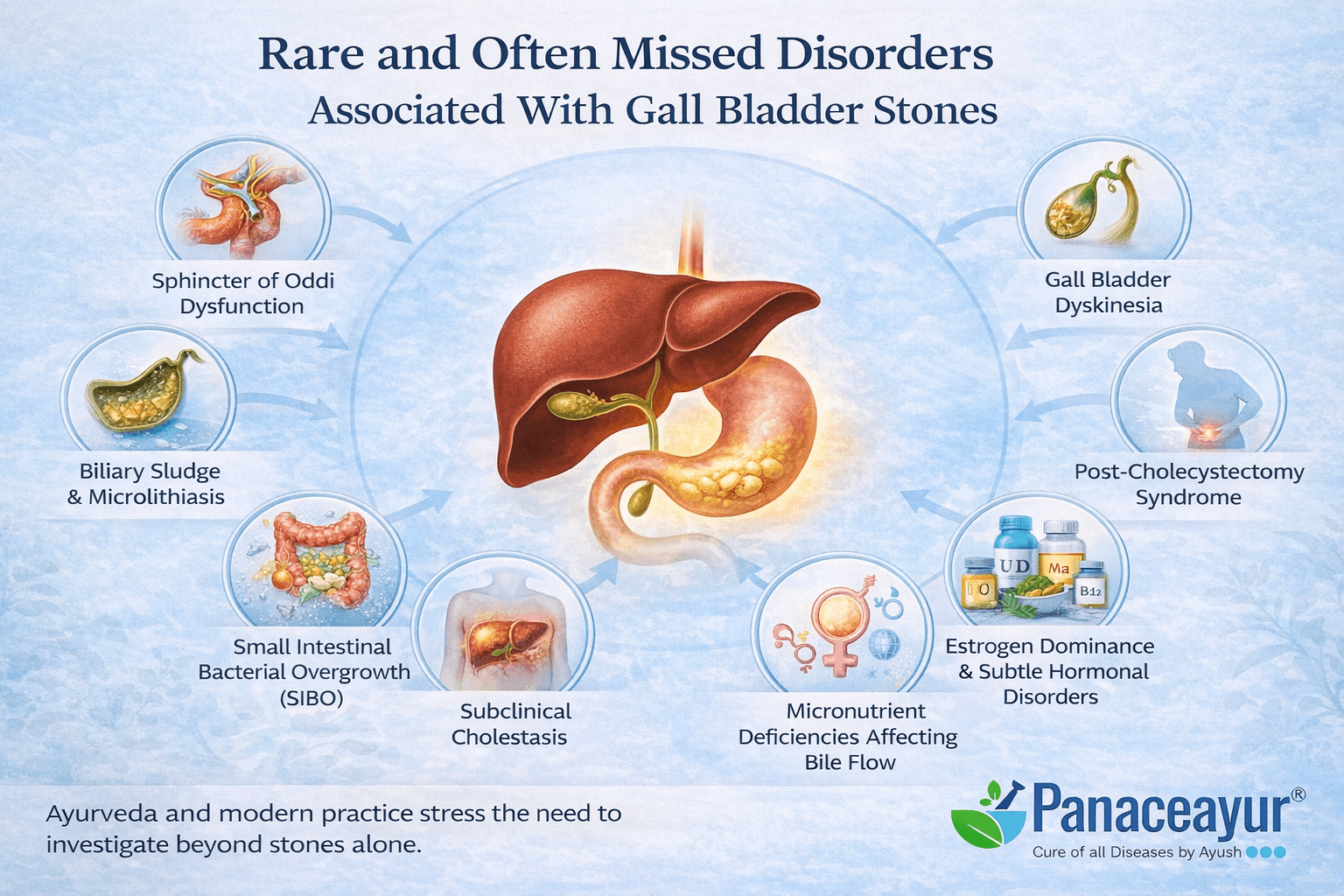
Gall bladder stones are often treated as an isolated biliary issue, yet in clinical practice many patients present with less obvious, overlapping disorders that go undetected for years. These conditions do not always appear on routine scans but significantly influence bile chemistry, gall bladder motility, and long-term outcomes. Recognizing them early is essential for complete recovery and prevention of recurrence.
Sphincter of Oddi Dysfunction
Sphincter of Oddi dysfunction is a functional disorder in which the muscular valve controlling bile and pancreatic juice flow fails to relax properly. This leads to episodic bile backpressure, pain mimicking gallstone attacks, and abnormal liver enzymes, even when stones are small or absent. Patients often continue to experience symptoms after gall bladder removal, leading to confusion and repeated investigations. Ayurveda correlates this with Vata avarana, where obstructed Vata disrupts the normal downward flow of Pitta, causing biliary spasms and pain.
Biliary Sludge and Microlithiasis
Before stones fully form, bile often passes through a sludge stage, consisting of microscopic cholesterol crystals and calcium salts. This condition is frequently missed on standard ultrasound yet can cause significant pain, nausea, and inflammation. Biliary sludge is especially common in patients with rapid weight loss, pregnancy, or prolonged fasting. Ayurveda describes this stage as Ama mixed with Pitta, an early and reversible phase if addressed promptly.
Gall Bladder Dyskinesia
Gall bladder dyskinesia refers to impaired gall bladder contraction without visible stones. Patients experience classic biliary symptoms, but imaging appears normal except for a low ejection fraction on HIDA scan. This disorder is often overlooked or mislabeled as functional abdominal pain. In Ayurvedic terms, it reflects Vata dominance with Pitta instability, where bile is produced but not expelled effectively, leading to stagnation and progressive thickening.
Small Intestinal Bacterial Overgrowth (SIBO)
Altered bile flow reduces bile’s natural antimicrobial action in the intestine, allowing excessive bacterial growth in the small bowel. SIBO causes bloating, gas, diarrhea, nutrient malabsorption, and food sensitivities, symptoms commonly reported by gallstone patients. This condition often worsens after gall bladder removal due to continuous but diluted bile flow. Ayurveda associates this with Grahani Dushti, where digestive coordination between bile and intestinal enzymes is disturbed.
Bile Acid Malabsorption
In some patients, bile acids are not adequately reabsorbed in the ileum and instead spill into the colon, causing chronic diarrhea and urgency. This disorder may exist before surgery or develop afterward. It is frequently mistaken for irritable bowel syndrome. Ayurveda interprets this as Pitta atisara, an excessive, uncontrolled flow of bile energy into the lower gut.
Subclinical Cholestasis
Subclinical cholestasis involves mild impairment of bile flow without overt jaundice or marked lab abnormalities. Patients may experience fatigue, itching, vague abdominal discomfort, or intolerance to fatty foods. Because standard tests appear near normal, the condition is often dismissed. Ayurveda recognizes this state as Pittavaha srotas dushti, where bile movement is partially obstructed but not fully blocked.
Post-Cholecystectomy Syndrome
Some patients develop persistent symptoms such as pain, bloating, nausea, and altered bowel habits even after gall bladder removal. This syndrome is frequently attributed to anxiety or functional disorders, yet underlying bile imbalance, ductal spasm, or altered gut microbiota are often responsible. Ayurveda views this as loss of Pittashaya regulation, resulting in unanchored Pitta and aggravated Vata affecting digestion.
Estrogen Dominance and Subtle Hormonal Disorders
Not all hormonal imbalances are obvious. Mild estrogen dominance, common in women with stress, obesity, or contraceptive use, increases cholesterol secretion into bile and reduces bile acid synthesis. Gallstones may be the first clinical sign of this imbalance. Ayurveda links this to Artava dhatu dushti combined with Pitta–Kapha aggravation.
Chronic Low-Grade Liver Inflammation
Patients may have ongoing hepatic inflammation without overt hepatitis or abnormal imaging. This inflammation alters bile composition and damages the gall bladder lining, encouraging stone adherence. Fatigue, brain fog, and mild digestive intolerance are common clues. Ayurveda describes this as Yakrit rakta dushti, a subtle but progressive disturbance of liver-blood interaction.
Micronutrient Deficiencies Affecting Bile Flow
Deficiencies of magnesium, vitamin D, choline, and taurine impair bile synthesis and flow. These deficiencies are common in individuals with restrictive diets, gut disorders, or long-term medication use. They are rarely evaluated in gallstone patients. Ayurveda emphasizes this as Dhatu poshana kshaya, inadequate nourishment of tissues leading to functional decline.
Why These Conditions Are Often Missed
Most of these disorders do not produce dramatic findings on routine scans or blood tests. Modern diagnostics tend to focus on structural disease, whereas functional and biochemical disturbances remain underrecognized. Ayurveda’s diagnostic framework was designed precisely to detect these early functional shifts, offering a unique advantage in preventing disease progression.
Clinical Significance
If these rare and often missed disorders are not addressed, patients may continue to suffer even after stone removal or repeated medical treatment. Comprehensive management must therefore include evaluation of bile flow dynamics, liver metabolism, gut health, hormonal balance, and micronutrient status.
Key Takeaway
Gall bladder stones are often the visible tip of a deeper metabolic and digestive iceberg. Identifying and correcting these hidden, interconnected disorders is essential for true cure, long-term relief, and prevention of recurrence. Ayurveda’s holistic lens allows clinicians to see what modern imaging often misses, making it an indispensable partner in gall bladder health.
Red Alert- When Gall Bladder Pain Is Not Just Stones
Gall bladder pain is often automatically attributed to stones once they are detected on ultrasound. However, not all right upper abdominal pain originates from gallstones, and not all gallstones are responsible for the pain a patient experiences. Certain symptoms act as red flags, indicating that the condition may be more serious, more complex, or entirely different. Ignoring these warning signs can delay critical treatment.
Severe, Persistent Pain That Does Not Subside
Pain lasting more than 6 hours without relief
Typical biliary colic caused by gallstones is episodic and usually subsides within a few hours. Pain that continues relentlessly for many hours or days, especially with increasing intensity, suggests acute inflammation, obstruction, or infection rather than simple stone irritation. This may indicate acute cholecystitis, bile duct blockage, or pancreatic involvement.
High Fever and Chills
Gall bladder pain accompanied by fever is not normal
Uncomplicated gallstones do not cause fever. When pain is associated with high temperature, chills, or rigors, it strongly suggests infection such as acute cholecystitis or ascending cholangitis. These conditions require immediate medical attention and can become life-threatening if untreated.
Yellowing of Eyes or Skin (Jaundice)
Jaundice indicates bile duct obstruction
Yellow discoloration of the eyes or skin points to impaired bile flow, often due to stones lodged in the common bile duct rather than the gall bladder itself. This condition, known as choledocholithiasis, can rapidly lead to liver damage, infection, or pancreatitis if not addressed urgently.
Dark Urine and Pale or Clay-Colored Stools
Changes in urine and stool color signal serious bile flow disruption
When bile cannot reach the intestine, stools lose their normal brown color and urine becomes dark. These signs indicate significant obstruction or liver involvement and should never be ignored, even if abdominal pain seems mild.
Pain Radiating With Vomiting and Profound Weakness
Possible pancreatic involvement
Gallstones can block the pancreatic duct, triggering acute pancreatitis. Red flags include severe pain radiating to the back, repeated vomiting, abdominal rigidity, and extreme weakness. This is a medical emergency and requires immediate hospitalization.
Pain Unrelated to Meals or Fat Intake
Gallstone pain is usually food-related
Pain that occurs independently of eating, especially at night or in association with posture changes, may suggest non-biliary causes such as gastric ulcers, liver inflammation, spinal nerve issues, or cardiac conditions. Assuming all right-sided pain is gallstone-related can be dangerous.
Sudden Weight Loss, Loss of Appetite, or Persistent Nausea
Possible malignancy or chronic liver disease
Unintentional weight loss, early satiety, or persistent nausea alongside gall bladder pain raises concern for gall bladder cancer, bile duct tumors, or advanced liver disease. Although rare, these conditions require prompt exclusion.
Pain After Gall Bladder Removal
Symptoms persisting post-surgery are a red flag
Continued pain, bloating, diarrhea, or nausea after gall bladder removal should not be dismissed as normal recovery. This may indicate post-cholecystectomy syndrome, bile duct stones, sphincter of Oddi dysfunction, or bile acid malabsorption, all of which need targeted evaluation.
Neurological or Cardiac-Like Symptoms
Not all right upper abdominal pain is gastrointestinal
Pain accompanied by shortness of breath, sweating, chest tightness, dizziness, or pain radiating to the left arm may represent cardiac events rather than gall bladder disease, particularly in older patients or those with diabetes. Immediate emergency assessment is essential.
Why These Red Flags Matter
Mislabeling all right upper abdominal pain as gallstone-related can delay diagnosis of serious conditions such as infections, pancreatitis, liver failure, or malignancy. Both modern medicine and Ayurveda emphasize careful differentiation before treatment.
From an Ayurvedic perspective, severe or atypical symptoms often reflect Vyadhi Sankara, where multiple disease processes overlap, or acute aggravation of Pitta and Rakta requiring urgent intervention rather than routine stone management.
Clinical Advisory for Patients
If any of the above red flags are present:
- Do not rely solely on home remedies or market-bought medicines
- Do not delay imaging, blood tests, or emergency evaluation
- Do not assume gallstones are always the cause of pain
Early identification saves organs, prevents complications, and in many cases saves lives.
Differential Diagnosis of Right Upper Quadrant Pain
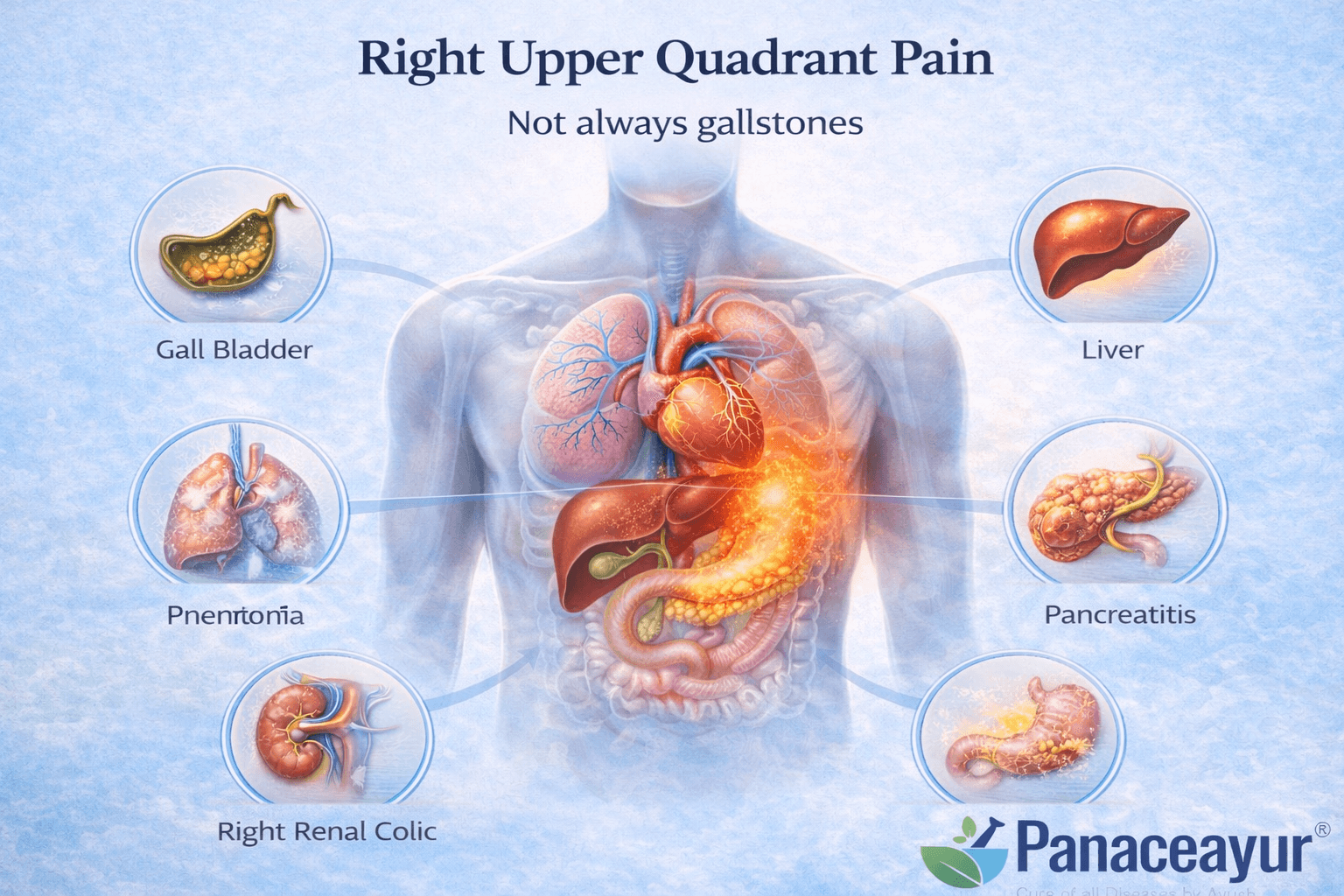
Right upper quadrant pain is frequently attributed to gall bladder stones, but this assumption is often inaccurate. Multiple organs occupy or refer pain to this region, including the liver, bile ducts, pancreas, stomach, intestines, lungs, heart, kidneys, and the musculoskeletal system. Correct differentiation is essential to prevent delayed diagnosis, inappropriate treatment, and avoidable complications.
Gall Bladder Stones (Cholelithiasis)
Pain from gallstones is typically episodic and often triggered after fatty meals. It is felt as a deep, gripping discomfort beneath the right rib cage and may radiate to the right shoulder or upper back. The pain usually lasts from minutes to a few hours and subsides spontaneously. Between attacks, patients may feel normal. Fever and marked laboratory abnormalities are usually absent in uncomplicated cases.
Acute Cholecystitis
When a gallstone causes sustained obstruction and inflammation of the gall bladder, pain becomes constant, severe, and progressively worsening. It is commonly associated with fever, nausea, vomiting, and localized tenderness. Unlike biliary colic, the pain does not resolve on its own and requires urgent medical attention.
Choledocholithiasis (Common Bile Duct Stones)
Stones lodged in the common bile duct cause deeper, more persistent pain than gall bladder stones. This pain is frequently accompanied by jaundice, dark urine, pale stools, and itching. Blood tests often reveal elevated bilirubin and liver enzymes. Without prompt treatment, this condition can progress to infection or pancreatitis.
Acute Pancreatitis
Pancreatitis presents with severe, continuous upper abdominal pain that often radiates straight through to the back. The pain worsens when lying flat and is associated with repeated vomiting, abdominal rigidity, and profound weakness. Gallstones are a common trigger, but the intensity and radiation pattern help differentiate it from gall bladder pain.
Acute Hepatitis
Liver inflammation causes a dull, aching pain or heaviness rather than sharp colic. Patients commonly experience fatigue, loss of appetite, nausea, and sometimes jaundice. The pain is not closely linked to meals and tends to be persistent. Liver enzyme levels are markedly elevated on blood testing.
Fatty Liver Disease with Hepatic Congestion
Fatty liver can cause vague right upper abdominal discomfort or fullness, especially after heavy meals. The pain is usually mild, non-radiating, and chronic rather than episodic. This condition frequently coexists with gall bladder dysfunction and reflects broader metabolic imbalance.
Peptic Ulcer Disease and Gastritis
Ulcers or inflammation of the stomach and duodenum can mimic gall bladder pain. The discomfort is often burning in nature and may worsen on an empty stomach or after meals, rather than specifically after fatty foods. Relief with antacids and associated acidity symptoms help distinguish it from biliary causes.
Irritable Bowel Syndrome and Functional Dyspepsia
Functional gastrointestinal disorders can cause recurrent upper abdominal discomfort without structural abnormalities. Pain may shift in location, fluctuate with stress, and be associated with bloating and altered bowel habits. Imaging studies are usually normal, and pain does not follow a classic biliary pattern.
Right-Sided Pneumonia or Pleurisy
Lower lung infections or pleural inflammation can irritate the diaphragm and present as right upper abdominal pain. This pain typically worsens with deep breathing or coughing and is accompanied by respiratory symptoms such as fever, cough, or breathlessness.
Inferior Wall Myocardial Infarction
In some individuals, particularly older adults and patients with diabetes, heart attacks may present as upper abdominal pain rather than chest pain. Associated symptoms include sweating, nausea, dizziness, and shortness of breath. This diagnosis must always be considered, as missing it can be fatal.
Right Renal Colic
Kidney stones can produce sharp pain radiating from the flank toward the abdomen or groin. The pain is often more posterior than gall bladder pain and may be associated with urinary symptoms or blood in the urine.
Costochondritis and Thoracic Spine Disorders
Musculoskeletal causes produce localized pain that worsens with movement, posture changes, or pressure. Unlike gall bladder pain, it is reproducible on palpation and unrelated to meals or digestion.
Post-Cholecystectomy Syndrome
Persistent pain after gall bladder removal may result from bile duct stones, sphincter of Oddi dysfunction, bile reflux gastritis, or altered gut motility. Assuming surgery has eliminated all biliary causes can delay appropriate diagnosis and treatment.
Why Accurate Differentiation Matters
Right upper quadrant pain has many potential causes, some of which are medical emergencies. Treating all such pain as gallstone-related can lead to missed diagnoses such as infection, pancreatitis, cardiac events, or liver disease. Both modern medicine and Ayurveda emphasize careful evaluation to identify the true source of pain before initiating therapy.
Patient Advisory
If right upper quadrant pain is severe, persistent, associated with fever, jaundice, repeated vomiting, breathlessness, dizziness, or unexplained weight loss, immediate medical evaluation is essential. Self-treatment or assumption-based therapy can be dangerous and should be avoided.
Ayurvedic Treatment Protocol for Gall Bladder Stones (Pittashmari)
The Ayurvedic Therapeutic Framework
Ayurveda approaches gall bladder stones not as isolated entities but as the culmination of long-standing imbalances involving Pitta, Kapha, Meda, and Agni. The goal of therapy is not merely to remove stones but to reestablish the natural rhythm of bile formation, flow, and elimination. The classical line of management includes three stages: Shodhana (detoxification), Shamana (pacification), and Rasayana (rejuvenation). Each stage works synergistically to dissolve existing stones, prevent recurrence, and restore the liver’s metabolic intelligence [1].
While modern medicine often resorts to surgical removal of the gall bladder, Ayurveda focuses on Samprapti Vighatana, reversing the disease mechanism through personalized therapy. It treats not just the symptom but the soil in which stones develop.
The Role of Shodhana (Detoxification) – Optional
Shodhana is the cornerstone of Ayurvedic treatment for all chronic diseases, particularly those arising from metabolic stagnation and channel obstruction. In gall bladder disorders, it helps eliminate Ama, clear the bile ducts, and restore bile fluidity. The main procedures are Snehana, Swedana, Virechana, and Basti, each applied in a specific sequence under clinical supervision.
Snehana (Oleation Therapy)
This step uses medicated ghee or oil to lubricate the body’s channels and soften bile obstructions. Internally, Tikta Ghrita or Triphala Ghrita is administered in gradually increasing doses for 5–7 days, depending on the patient’s strength. Externally, gentle Abhyanga (oil massage) enhances circulation and prepares the body for toxin mobilization [2]. The medicated ghee works by dissolving lipid-based toxins and promoting peristaltic flow through the bile ducts, akin to improving bile motility in modern hepatology.
Swedana (Sudation Therapy)
After Snehana, mild steam therapy using Nimba Patra or Dashamoola decoction induces sweating, which dilates the channels and helps expel toxins. Clinically, it correlates with improving bile fluidity and relaxing sphincter constriction in the biliary system [3]. This process enhances microcirculation and prepares the body for purgation.
Virechana (Therapeutic Purgation)
This is the most critical phase for gall bladder diseases. Classical texts such as Charaka Samhita Chikitsa Sthana 16/37–38 prescribe Trivrit Lehya or Avipattikara Churna as mild purgatives to expel excess Pitta and Ama through the lower channels [1]. In modern terms, this process stimulates bile secretion, clears biliary congestion, and reduces bile cholesterol saturation. Virechana should be administered after adequate Snehana and Swedana, ideally during early morning hours on an empty stomach. The therapy not only detoxifies the liver and gall bladder but also normalizes intestinal flora and metabolism.
Basti (Medicated Enema)
After Virechana, a sequence of Niruha (decoction) and Anuvasana (oil) Bastis are prescribed to regulate Vata Dosha and maintain bile flow. Formulations like Dashamoola–Eranda Niruha Basti and Sahacharadi Taila Anuvasana are preferred. Clinically, this corresponds to stimulating the parasympathetic system and improving gall bladder contraction, thereby preventing bile stasis [5]. The Basti phase is vital for preventing recurrence and stabilizing post-detoxification metabolism.
The Shamana Phase (Pacification Therapy)- Optional
Once detoxification is complete, the focus shifts to Shamana therapy—herbal formulations that pacify aggravated Doshas, dissolve stones, and restore organ balance. Several classical formulations are mentioned in texts for Pittashmari Chikitsa, each addressing a specific dimension of the pathology.
Varunadi Kashaya
Described in Bhavaprakasha Nighantu – Mutraghata Chikitsa Adhyaya, Varunadi Kashaya is the primary decoction for urinary and biliary calculi. Its main ingredient, Varuna (Crataeva nurvala), acts as a natural litholytic and bile purifier [7]. It breaks down cholesterol crystals and promotes bile outflow. The combination with Punarnava, Gokshura, and Shigru enhances anti-inflammatory and diuretic action. Mechanistically, it reduces bile viscosity and prevents new crystal nucleation by increasing bile acids and phospholipids.
Gokshuradi Guggulu
Cited in Bhaishajya Ratnavali – Mutraghata Rogadhikara, this formulation combines Gokshura (Tribulus terrestris), Triphala, Guggulu, and Mustaka. It balances all three Doshas, cleanses urinary and biliary tracts, and acts as a lipid regulator [8]. Guggulu’s resinous nature dissolves sticky bile residues and improves hepatic enzyme function, paralleling modern bile acid therapy that disperses cholesterol micelles.
Chandraprabha Vati
Documented in Rasatantra Sara Siddha Prayoga Sangraha, Chandraprabha Vati is a versatile Rasayana that acts on the urinary, hepatic, and endocrine systems. Its ingredients—Shilajit, Guggulu, Musta, Vacha, and Trivrit—detoxify the liver, improve Agni, and normalize bile pH [6]. It provides systemic purification while enhancing metabolism, similar to how hepatoprotective drugs improve bile flow and liver function in modern medicine.
Pashanbhedadi Kwath
Found in Sahasrayoga – Mutraghata Prakarana, this decoction derives its name from Pashanbheda (Bergenia ligulata), meaning “stone breaker.” The herb directly acts on crystalline bile matter, softening and gradually disintegrating it [9]. It also reduces inflammation of the gall bladder lining and relieves pain associated with biliary colic. Research has shown Bergenia extracts possess strong antioxidant and litholytic properties, comparable to potassium citrate used in modern lithiasis management.
Varunadi Avaleha (Main Medicine) – Mandatory
Among Avalehas (herbal jams), the most suitable preparation for gall bladder stones is Varunadi Avaleha, mentioned in Rasendra Sara Sangraha – Mutraghata Rogadhikara. This Avaleha is specially designed to dissolve calculi and normalize Pitta–Kapha balance. It contains Varuna (Crataeva nurvala), Pashanbheda (Bergenia ligulata), Punarnava (Boerhaavia diffusa), Gokshura (Tribulus terrestris), Triphala, Guduchi (Tinospora cordifolia), Shilajit, and Madhu (honey) as the binding agent [1].
Preparation: The decoction of Varuna, Pashanbheda, and Gokshura is prepared and reduced to one-fourth, then mixed with Triphala and Shilajit. After thickening, honey is added as a natural preservative.
Dose: 15 grams twice daily after meals with lukewarm water for 30–45 days under supervision.
Mechanism: Varuna and Pashanbheda act as bile thinners, Punarnava and Triphala cleanse the liver channels, Shilajit enhances cellular detoxification, and honey aids bioavailability. Together, they restore bile fluidity, promote cholesterol emulsification, and dissolve small stones naturally.
Modern studies confirm that Varuna reduces cholesterol saturation index, while Pashanbheda prevents mucin hypersecretion, directly aligning with modern bile chemistry findings [5].
Rasayana Integration: Rebuilding the Liver–Bile Axis
After detoxification and pacification, the body must be rejuvenated to prevent relapse. Rasayana therapy nourishes the Dhatus (tissues), restores Agni, and strengthens liver resilience. For gall bladder health, specific mineral and herbal Rasayanas are indicated.
Abhrak Bhasma (Sahasraputi)
Mentioned in Rasendra Chintamani, Abhrak Bhasma rejuvenates the liver, promotes hemoglobin synthesis, and acts as a powerful antioxidant. It revitalizes the bile-forming hepatocytes and reduces oxidative stress in the liver. Modern research supports its hepatoprotective effect by enhancing mitochondrial activity and bile secretion [7].
Swarna Makshik Bhasma
Found in Rasatarangini – 8th Taranga, this copper-iron-sulphide compound acts as a metabolic catalyst. It restores normal bile secretion, reduces inflammation, and improves lipid metabolism [8]. Clinically, it parallels modern hepatic enzyme regulators and functions as a Pitta–Kapha pacifier.
Tamra Bhasma
Cited in Rasaratna Samuccaya 11/116–118, Tamra Bhasma corrects Meda Dushti and acts as a liver stimulant. It increases bile secretion and helps dissolve cholesterol aggregates by enhancing hepatic lipid turnover. However, it should be used only under expert supervision due to its potent nature [9].
Suvarna Sutshekhar Ras
Documented in Bhaishajya Ratnavali – Amlapitta Chikitsa Adhyaya, this compound formulation containing gold, mica, and mineral salts pacifies aggravated Pitta and prevents bile acidity. It enhances bile solubility, protecting the gall bladder lining from recurrent inflammation [1].
Amalaki Rasayana
Described in Charaka Samhita Chikitsa Sthana 1/1, Amalaki (Emblica officinalis) is the best natural Rasayana for Pitta-related disorders. Its Vitamin C and tannin content repair bile duct mucosa, rejuvenate liver cells, and prevent free-radical damage. It also acts as a natural choleretic, improving bile flow and reducing stone recurrence.
Mechanistic Explanation: How Ayurveda Dissolves Stones
The Ayurvedic approach works by reversing the biochemical conditions that cause stone formation. Modern medicine focuses on dissolving stones chemically or surgically, but Ayurveda targets the terrain.
- Improves Bile Solubility: Herbs like Varuna, Pashanbheda, and Guduchi increase bile acids and phospholipids, preventing cholesterol precipitation.
- Reduces Bile Viscosity: Punarnava and Triphala thin the bile and prevent mucin build-up, similar to how ursodeoxycholic acid works.
- Normalizes Cholesterol Metabolism: Gokshura and Shilajit balance hepatic lipid synthesis and excretion, reducing the risk of recurrence.
- Cleanses Biliary Channels: Detox therapies eliminate Ama and open obstructed Srotas, enhancing bile movement.
- Restores Agni and Dhatu Balance: Rasayana therapy strengthens metabolism and rebuilds liver tissue integrity.
In simple terms, Ayurveda does not attack the stones directly—it heals the soil, making the stones dissolve naturally.
Detox–Rejuvenation Sequence for Western Readers
Western patients often equate detox with fasting or juice cleansing. Ayurveda’s detox is deeper, physiological, and time-bound. The sequence begins with loosening toxins (Snehana), liquefying them (Swedana), expelling them (Virechana), and finally rejuvenating the body (Rasayana). The logic is simple—first cleanse, then rebuild.
This gradual process allows the body to regain equilibrium without sudden metabolic shock. After completing detox, Rasayanas like Abhrak and Amalaki restore enzyme balance, enhance bile regeneration, and prevent relapse.
In modern terms, this represents phase-wise hepatobiliary rehabilitation, addressing both cause and consequence of gall bladder disease.
Varunadi Avaleha – Preparation
This batch is designed to yield about 1,000 g of Avaleha (enough for 30 days at 30 g/day). It combines cholagogue, litholytic, anti-inflammatory, hepato-rasayana and channel-cleansing actions.
Part A: Decoction base (Kashaya dravya) – boil and reduce
Use coarse-cut (kwaath-yogya) herbs. Weights are dry weights.
- Varuna stem bark (Crataeva nurvala) – 150 g
- Pashanbheda rhizome (Bergenia ligulata) – 120 g
- Gokshura fruit (Tribulus terrestris) – 120 g
- Punarnava root (Boerhaavia diffusa) – 120 g
- Bhumyamalaki whole plant (Phyllanthus niruri) – 100 g
- Guduchi stem (Tinospora cordifolia) – 100 g
- Bhringaraj whole plant (Eclipta alba) – 80 g
- Daruharidra stem (Berberis aristata) – 80 g
- Haridra rhizome (Curcuma longa) – 60 g
- Kalmegha herb (Andrographis paniculata) – 60 g
- Kutki rhizome (Picrorhiza kurroa) – 40 g
Add 16× water by volume, simmer to 1/4th, and strain. You should get roughly 2.0–2.5 L concentrated decoction.
Part B: Powder phase (churna to add after reduction)
- Triphala churna (equal Haritaki, Bibhitaki, Amalaki) – 120 g
- Trikatu churna (equal Shunthi, Maricha, Pippali) – 45 g
- Ajmoda/ajwain seed (Trachyspermum ammi) – 30 g
- Dhanyaka/coriander seed – 30 g
- Jeeraka/cumin seed – 30 g
- Yashtimadhu/licorice – 40 g
- Shilajit-suddha – 30 g
Part C: Avaleha base (sweet media and ghee)
- Jaggery (guda) – 650 g–700 g (adjust for final consistency and taste)
- Cow’s ghee – 120 g
- Honey – 120 g (add only after cooling below lukewarm)
Part D: Mineral and precious adjuncts (Bhasma/Pishti/Ras-yoga)
Doses below are per-batch and also shown per 15 g dose for safety. Use only pharmaceutical-grade, physician-approved materials.
- Abhrak bhasma (Sahasraputi) – 10 g total (≈125 mg per 15 g dose)
- Swarna Makshik bhasma – 10 g total (≈125 mg per dose)
- Tamra bhasma – 2.4 g total (≈30 mg per dose)
- Lauh bhasma – 10 g total (≈125 mg per dose)
- Godanti bhasma – 10 g total (≈125 mg per dose)
- Praval pishti – 10 g total (≈125 mg per dose)
- Mukta Shukti bhasma – 10 g total (≈125 mg per dose)
- Shankha bhasma – 10 g total (≈125 mg per dose)
- Suvarna Sutshekhar Ras – 5 g total (≈62.5 mg per dose)
This keeps the total mineral load ≈1 g per 15 g dose, which is a strong but commonly used rasayana-therapeutic band under expert care.
Preparation method (simple, step-by-step)
Step 1: Make the decoction
Rinse, coarsely crush Part A herbs. Add 16× water, simmer on low flame until reduced to 1/4th. Strain through muslin. You’ll retain a clear, deep-colored kashaya.
Step 2: Convert to Avaleha
Return the strained kashaya to a thick-bottom vessel. Add jaggery and ghee. Simmer gently, stirring to prevent sticking. When it thickens to a soft jam and a drop stretched between fingers forms a short thread, turn heat to low.
Step 3: Incorporate powders
Fold in Part B powders gradually, stirring to a uniform paste. Maintain gentle heat so it stays pliable without catching.
Step 4: Add minerals correctly
Switch off the flame. Allow the mass to cool to comfortably warm (so you can touch without burning). Sieve-in the pre-triturated Part D bhasma/pishti/ras powders and Shilajit, mixing thoroughly to avoid clumps.
Step 5: Finish with honey
When the Avaleha is lukewarm (not hot), fold in honey. Mix until glossy. Target final yield ≈1,000 g. Store in sterilized glass jars, airtight, away from light and moisture.
How to take it (30-day plan)
Dose
15 g twice daily after meals with 120–150 ml warm water. Total daily intake 30 g.
Daily schedule
Morning: after breakfast within 15–20 minutes.
Evening: after dinner within 15–20 minutes.
Sip warm water through the day; minimum 2–2.5 L unless medically restricted.
What to expect
Days 1–5: lighter digestion, improved bowel movement, reduced post-meal heaviness.
Days 6–15: less RUQ discomfort, better fat tolerance, reduced bitter after-taste.
Days 16–30: progressive symptom relief; small gravel or dark bile may pass unnoticed. Continue physician-directed pathya diet.
Why these herbs and minerals (brief mechanisms)
Varuna, Pashanbheda, Gokshura, Punarnava, Bhumyamalaki, Guduchi and Bhringaraj thin viscous bile, reduce mucin, and gently increase bile outflow, discouraging cholesterol crystallization. Triphala, Trikatu, ajwain, cumin and coriander rekindle Agni, cut Ama, and improve gallbladder kinetics after meals. Daruharidra and Haridra provide berberine/curcuminoid activity for mucosal calm and microbial control. Kutki and Kalmegha are potent cholagogues and hepatorestoratives that reset bile acid composition. Shilajit enhances mitochondrial energy and bioavailability.
Abhrak, Swarna Makshik and Lauh support hepatocellular regeneration and redox balance; Tamra specifically targets Meda-dushti and bile secretion; Godanti, Praval, Mukta Shukti and Shankha buffer bile acidity and soothe the biliary mucosa; Suvarna Sutshekhar pacifies aggravated Pitta and stabilizes post-prandial bile chemistry. Together, these reverse bile supersaturation, reduce viscosity, improve ejection, and discourage stone growth while repairing the biliary lining.
Pathya and apathya during the 30 days
Prefer warm, freshly cooked meals, thin mung dal soups, steamed vegetables (bottle gourd, ridge gourd, tori, snake gourd), barley or red rice, small amounts of cow ghee, and fruits like pomegranate, apple, and papaya between meals. Avoid all reheated oils, deep-fried foods, red meat, cheese, cream, bakery sweets, colas, alcohol, very spicy or very sour items, late dinners, and meal skipping.
Precautions, warnings, and who must not use this without direct supervision
This is a strong physician-grade formulation.
- Use only under a qualified Ayurvedic doctor’s supervision.
- Do not exceed 15 g twice daily. If loose stools, heat, or nausea occur, inform your doctor for dose adjustment.
- Not for pregnancy, lactation, children, or frail elderly without explicit supervision.
- Contraindicated in acute abdomen with fever, suspected acute cholecystitis, cholangitis, obstructive jaundice with rising bilirubin, or gallstone pancreatitis—these require urgent hospital care.
- If you take anticoagulants, antiplatelets, antidiabetics, thyroid or cardiac medicines, disclose; mineral components may necessitate dose spacing or modification.
- Only pharmacopeial-grade bhasma/pishti/ras preparations should be used; never use unverified metals or crude minerals.
- Stop and seek review if you notice persistent vomiting, severe colic, yellowing eyes/skin, clay-colored stools, dark urine, fever, or chills.
Why Market-Bought or Self-Prepared Ayurvedic Medicines Fail in Gall Bladder Stones
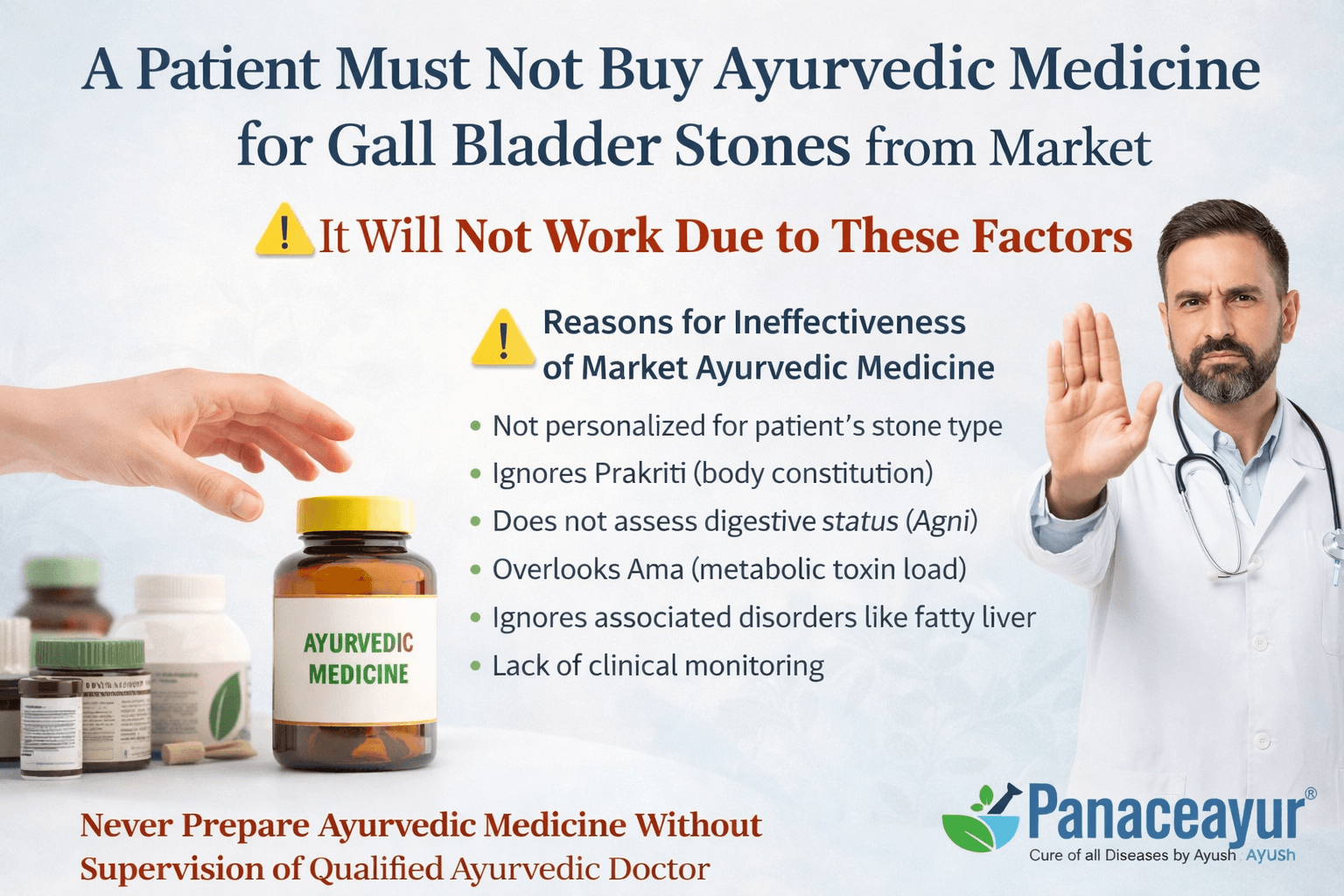
Gall bladder stone disease is not a single-herb or single-tablet condition. It is a complex metabolic disorder involving bile chemistry, liver function, digestion, hormones, gut motility, and individual constitution. Because of this complexity, ready-made or market-bought Ayurvedic medicines almost never produce lasting results and, in many cases, can worsen the condition.
Critical Warning for Patients
A patient must never assume that buying Ayurvedic medicine from the market or online will cure gall bladder stones.
Such medicines are generic, non-personalized, and disconnected from the patient’s actual metabolic state.
Preparing or consuming Ayurvedic formulations without direct supervision of a qualified Ayurvedic doctor is unsafe and ineffective.
Why Market-Bought Ayurvedic Medicines Do Not Work
Gall bladder stones are not the same in every patient
Gallstones differ in composition, size, number, and behavior. Some are cholesterol stones, some pigment stones, and many are mixed. A market formulation cannot identify whether bile is thick due to cholesterol excess, pigment imbalance, inflammation, or motility failure. Ayurveda treats based on this differentiation. Without it, medicine selection becomes blind and ineffective.
Prakriti (body constitution) is completely ignored
Every patient has a unique Vata, Pitta, or Kapha dominance. A formulation suitable for a Kapha-dominant patient can aggravate Pitta in another, increasing bile irritation and pain. Market medicines are not adjusted for Prakriti and therefore often aggravate symptoms instead of correcting them.
Digestive fire (Agni) status is not assessed
Gall bladder stones almost always coexist with weak or irregular digestion. If Agni is weak, even the best medicine will not be absorbed properly. Market medicines do not evaluate whether Agni needs stimulation first or calming. As a result, medicines either pass undigested or create Ama, worsening bile thickening.
Ama (metabolic toxin load) is not addressed
In Ayurveda, stones form only after prolonged Ama accumulation. If Ama is not removed first through proper Deepana and Pachana, stone-breaking herbs fail to penetrate bile channels. Market products skip this foundational step, making stone dissolution unlikely.
Stage of disease is not considered
Early bile sludge, soft microlithiasis, large stones, ductal stones, and post-surgical bile imbalance all require different strategies. A single ready-made product cannot match disease stage. This is one of the most common reasons patients report “Ayurveda didn’t work,” when in reality the approach was incorrect.
Associated disorders are ignored
Gall bladder stones rarely exist alone. Fatty liver, insulin resistance, thyroid imbalance, IBS, hormonal disturbances, and gut dysbiosis frequently coexist. Market medicines do not correct these parallel conditions, so bile chemistry remains abnormal even if symptoms temporarily improve.
Why Self-Preparation of Ayurvedic Medicine Is Dangerous
Incorrect processing of herbs and minerals
Herbal-mineral formulations require precise purification, calcination, and dosage control. Improperly prepared bhasmas or mineral ingredients can irritate the liver, worsen bile inflammation, or cause toxicity. Classical Ayurvedic texts strictly warn against unsupervised preparation.
Wrong dosage can worsen bile imbalance
Higher doses do not mean faster cure. Excessive use of stone-breaking herbs can overstimulate bile, trigger colic, or cause diarrhea and dehydration. Too little dose, on the other hand, produces no effect. Dosage must be calibrated to body strength, age, and digestive capacity.
Unsafe combinations and interactions
Many patients are already taking modern medicines for diabetes, cholesterol, blood pressure, or thyroid disorders. Self-prepared Ayurvedic medicines can interact unpredictably with these drugs. A qualified Ayurvedic doctor adjusts formulations accordingly, market products do not.
Absence of clinical monitoring
Gall bladder stone treatment requires symptom tracking, digestive response evaluation, and sometimes follow-up imaging. Self-treatment lacks this feedback loop, increasing the risk of silent complications.
Why Only Personalized Ayurvedic Treatment Works
Ayurveda treats the cause, not the stone alone
A genuine Ayurvedic protocol corrects bile viscosity, improves gall bladder motility, restores liver metabolism, and prevents crystal reformation. This requires sequential therapy, not random medicine intake.
Formulation strength and composition vary per patient
The same Avaleha or Kashaya is never identical for two patients. Ratios of Varuna, Pashanbheda, Punarnava, Gokshura, Guduchi, and Rasayana minerals are adjusted based on Prakriti, age, digestive strength, and disease chronicity.
Diet and lifestyle are integral to success
Without correcting meal timing, fat intake, hydration, stress, and physical activity, no medicine can permanently cure gall bladder stones. Market medicines never integrate these essential components.
Essential Patient Advisory
Patients should clearly understand the following:
- Do not buy Ayurvedic medicine for gall bladder stones from the open market or online stores.
- Do not attempt to prepare herbal or mineral medicines at home.
- Do not follow another patient’s prescription or testimonial blindly.
- Always consult a qualified Ayurvedic doctor who evaluates digestion, liver function, bile quality, constitution, and associated disorders.
Gall bladder stone disease demands precision medicine, not generic treatment. When Ayurveda is practiced correctly, it can dissolve stones, restore bile balance, and prevent recurrence. When practiced casually or commercially, it fails and damages trust.
Clinical Takeaway
If gall bladder stones could be cured by a single market-available tablet, surgery would not be so common. The failure lies not in Ayurveda, but in misuse, oversimplification, and lack of supervision. True Ayurvedic cure is individualized, sequential, and physician-guided. Anything less is not Ayurveda.
Modern Management and Limitations
The Conventional Medical Approach
Modern medicine views gall bladder stones as physical obstructions to bile flow that must be mechanically or chemically eliminated. The two standard treatment paths are either drug therapy using bile acid derivatives such as Ursodeoxycholic Acid (UDCA) or surgical removal of the gall bladder through a procedure known as cholecystectomy. These methods primarily address the effect—the stones—but not the cause—the metabolic and biochemical imbalances that led to stone formation. As a result, while immediate relief may occur, recurrence or secondary complications often follow [5].
UDCA Therapy – The Chemical Dissolution Route
UDCA (Ursodeoxycholic Acid) is a bile acid analog that helps dissolve cholesterol-based stones in select cases. It works by reducing cholesterol saturation in bile and improving bile fluidity. However, it is only effective for small, soft, cholesterol stones that are radiolucent (not calcified) and confined within a functioning gall bladder [6].
The typical treatment lasts between six months and two years, depending on stone size. Yet, success rates vary widely—only 30–40% of patients achieve complete dissolution, and stones often reappear after the medication is stopped. Moreover, the therapy does not correct underlying bile chemistry, liver metabolism, or the patient’s diet and hormonal state, all of which continue to favor stone formation.
Long-term use of UDCA may cause side effects such as diarrhea, nausea, and elevated liver enzymes. Once discontinued, bile composition tends to revert to its previous saturated state, allowing new stones to form. Hence, UDCA provides only temporary chemical correction, not permanent metabolic healing.
Surgical Removal (Cholecystectomy)
When stones are large, symptomatic, or recurrent, surgery is the preferred modern solution. Cholecystectomy involves removing the gall bladder entirely, either via laparoscopic (keyhole) or open procedure. While the immediate outcome seems curative, the body’s physiology undergoes significant and often underestimated changes afterward [8].
The gall bladder is not just a storage sac—it plays an essential role in regulating bile concentration, timing, and delivery. Bile produced by the liver is concentrated and stored in the gall bladder between meals. When food, especially fats, enters the small intestine, the hormone cholecystokinin triggers the gall bladder to release bile in pulses for efficient fat digestion and absorption of fat-soluble vitamins (A, D, E, and K).
When the gall bladder is removed, this regulated pulsatile release is lost. Instead, bile flows continuously and in diluted form into the intestine, regardless of food intake. This disrupts the body’s synchronized digestive rhythm and alters lipid metabolism. In Ayurveda, this condition is comparable to Pitta vega dosha, where the bile (Pitta) loses its controlled release and begins to flow erratically, leading to secondary disturbances in Agni and Dhatu balance [7].
Post-Surgical Physiological Changes
After cholecystectomy, several short-term and long-term changes occur in digestion and systemic metabolism:
- Continuous Bile Drip: Without a gall bladder, bile is secreted directly from the liver to the small intestine in a diluted, uncontrolled manner. This often leads to post-meal bloating, gas, and loose stools. Fat digestion becomes inefficient, resulting in nutrient malabsorption.
- Loss of Bile Concentration: The gall bladder normally concentrates bile salts 5–10 times. Without it, bile remains weak, compromising fat emulsification and absorption of essential fatty acids and vitamins.
- Altered Gut Microbiome: Continuous bile leakage changes intestinal pH and microbiota composition, potentially leading to dysbiosis and irritable bowel-type symptoms. Studies show higher rates of small intestinal bacterial overgrowth (SIBO) after cholecystectomy [6].
- Metabolic Shift: Research indicates that gall bladder removal may increase risk of fatty liver disease, dyslipidemia, and insulin resistance, suggesting that the gall bladder plays a subtle role in lipid signaling and glucose homeostasis.
- Bile Reflux Gastritis: Some patients experience bile reflux into the stomach, causing heartburn, nausea, and chronic gastritis due to the corrosive nature of bile acids.
- Vitamin Deficiencies: The inefficient absorption of fat-soluble vitamins (A, D, E, K) can lead to fatigue, poor immunity, bone weakness, and skin changes.
In Ayurvedic interpretation, this phase represents a state of Pitta kshaya with Vata aggravation—a depletion of structured bile energy and increased erratic movement of Vata through the digestive tract, producing bloating, dryness, and irregular digestion.
Why Recurrence and Complications Still Occur
One of the main misconceptions about cholecystectomy is that it guarantees permanent freedom from gallstones. While stones within the gall bladder are removed, the underlying bile chemistry—originating in the liver—remains unchanged. As a result, stones can re-form in the bile ducts even after surgery, a condition called post-cholecystectomy choledocholithiasis [9].
Several reasons explain recurrence:
- The liver continues to secrete bile rich in cholesterol or low in bile acids.
- Hormonal imbalance (especially estrogen dominance) persists in women, promoting cholesterol deposition.
- Obesity, diabetes, and poor diet continue to drive bile stagnation and inflammation.
- Sedentary lifestyle and low Agni further reduce bile motility.
Modern data show that up to 15% of patients develop recurrent stones in the bile ducts within five years after gall bladder removal. Others develop bile sludge, fatty liver, or dyspepsia due to uncorrected digestive imbalances.
Ayurveda explains this as the persistence of Meda dushti (fat tissue disorder) and Pitta-Kapha aggravation at the hepatic level. Removing the organ does not remove the root doshic disturbance. Hence, recurrence or metabolic degeneration can occur if the root cause is not addressed.
Post-Cholecystectomy Syndrome
A subset of patients experiences persistent or new digestive symptoms even after surgery, a condition referred to as Post-Cholecystectomy Syndrome (PCS). Symptoms include abdominal pain, bloating, nausea, indigestion, and diarrhea.
The causes can be diverse—retained stones in the bile duct, altered sphincter of Oddi function, bile reflux gastritis, or simply metabolic maladaptation. Ayurveda equates this condition to Agni dushti with Pitta-vata samyak ashraya, where the body struggles to regulate bile energy post-surgery [7].
PCS is treated symptomatically in modern medicine, using antacids, digestive enzymes, and occasionally bile acid binders—but none restore the natural rhythm of bile secretion or prevent further biochemical imbalance.
Scientific Validation
What modern research says about the core herbs
Varuna (Crataeva nurvala) is classically indicated for stone disease and shows litholytic activity in preclinical models. Rat studies demonstrate that Varuna reduces crystal deposition and improves urinary (and by inference biliary) dynamics, consistent with antilithic action and channel clearance. These data, although generated in urolithiasis models, support Varuna’s traditional “stone-breaking” role and justify its use where bile becomes viscous and crystal-prone [16]. Pashanbheda (Bergenia ligulata) is strongly supported as an anti-calculous herb. Contemporary reviews summarize its ethnomedicinal use for dissolving kidney and gall bladder stones, and catalog bergenin and related polyphenolics as the key actives. Experimental work shows Bergenia extracts reduce crystal aggregation and mucosal inflammation, lending plausibility to bile-sludge and microlith targeting [1] [17] [9]. Gokshura (Tribulus terrestris) contains abundant steroidal saponins (furostanol/spirostanol). Saponins are natural surfactants that can alter lipid micelles; this provides a mechanistic rationale for reducing cholesterol supersaturation in bile. That said, high-dose or non-standardized preparations have been linked to bile duct irritation in grazing animals, underscoring the need for dose control and pharmacopeial quality in humans [18] [10] [2]. Punarnava (Boerhavia diffusa) shows robust hepatoprotective and choleretic effects in animal and in-vitro studies: it increases baseline bile flow, protects hepatocytes from toxin injury, and dampens oxidative stress—useful attributes when bile needs thinning and ducts need protection during stone dissolution [3] [11] [19].
Clinical signals: AYU Journal, IJAPR, and practice-based evidence
Peer-reviewed clinical evidence is emerging but still early. Case-based and small practice reports in AYU Journal and IJAPR describe symptomatic relief and sonographic reduction in biliary calculi using classical protocols centered on Varuna-based decoctions and adjuvant formulations, sometimes even in complex post-cholecystectomy settings. These clinical narratives, while not randomized controlled trials, consistently report improved pain, better fat tolerance, and reduction of echogenic foci or sludge on follow-up scans, aligning with the pharmacology noted above [8] [21] [13] [6] [14] [22]. For comparison, the gold-standard biomedical literature on bile-acid dissolution shows that UDCA/CDCA can unsaturate bile and dissolve selected cholesterol stones, but recurrence is common when therapy stops—hence the interest in complementary strategies that restore bile physiology rather than only “chemically” dissolving stones [12] [20] [4].
Molecular underpinnings: lupeol, bergenin, saponins, and bile-acid biology
Lupeol, a triterpenoid present in several medicinal plants (and reported in Crataeva spp. chemotypes), has newly documented actions on bile-acid metabolism via the FXR (farnesoid X receptor) pathway in metabolic liver disease models. By modulating FXR-dependent signaling and the gut–liver axis, lupeol improved bile-acid homeostasis and hepatic fat handling in mice—mechanisms directly relevant to reversing bile thickening and cholesterol supersaturation in gallstone-prone patients [7]. Bergenin, the signature compound of Bergenia ligulata, demonstrates anti-lithic, anti-inflammatory, and antioxidant actions that can reduce mucin overproduction and dampen crystal adhesion to mucosa—two key steps in stone nucleation and growth. Reviews of the Bergenia genus consolidate these effects and support its “Pashanabheda” (stone-breaking) reputation in Ayurveda [17] [9]. Saponins (abundant in Tribulus terrestris) reduce surface tension and can remodel lipid micelles. This biophysical property offers a mechanistic basis for dispersing cholesterol crystals and improving bile rheology. However, because certain sapogenins have been implicated in animal cholangiopathy at excessive exposures, human therapeutic use must prioritize standardization, conservative dosing, and physician supervision [18] [10] [2]. At the systems level, bile-acid pool quality matters: reviews in hepatology emphasize that reshaping the bile-acid pool (via endogenous or exogenous modulators) can improve lipid handling, receptor signaling, and mucosal integrity in the hepatobiliary axis. This is congruent with the Ayurvedic aim of normalizing “Pitta dravya” quality rather than suppressing symptoms [15].
How this maps to the modern pathophysiology of gallstones
Gallstone formation requires three things: cholesterol supersaturation, gall bladder hypomotility, and a mucin-rich matrix that scaffolds crystal growth. Varuna and Punarnava address motility and bile flow (thin the bile, promote ejection), while Pashanbheda and Triphala-supported regimens target the mucin/crystal interface (anti-lithic, antioxidant). When combined with regulated diet and timing (steady cholecystokinin signaling), these botanicals reduce the likelihood that supersaturated cholesterol will nucleate into solid stones. On the biochemical front, introducing amphipathic constituents (e.g., saponins) and FXR-modulating triterpenoids (e.g., lupeol) plausibly shifts bile composition toward a more soluble state, echoing—though not duplicating—the mechanism of UDCA/CDCA, which “unsaturate” bile to dissolve cholesterol stones [12] [20] [7] [15].
Where the clinical evidence stands—and what it means for patients
Compared with UDCA/CDCA (supported by decades of controlled data), Ayurvedic herb trials are earlier in maturity. Current evidence is strongest at the preclinical level (litholysis, choleresis, hepatoprotection) and at the case-series level (AYU, IJAPR reports). That said, the directionality is consistent: improved symptoms, improved sonology, improved bile handling. The integrated model—using Varuna/Pashanbheda/Punarnava/Gokshura within a detox-to-rejuvenation sequence—targets not only stones but the terrain that made stones likely. Patients should understand that herbal protocols require adherence (weeks to months), ultrasound monitoring, and medical supervision, and that outcomes differ by stone type, size, and bile-duct dynamics [8] [21] [13] [6] [14].
Frequently Asked Questions (FAQs)
What causes gall bladder stones?
Gall bladder stones form when bile becomes thick and imbalanced, leading to crystallization of cholesterol or pigments. Common causes include poor digestion, fatty and fried foods, obesity, insulin resistance, hormonal imbalance, and bile stagnation. Ayurveda explains this as Pitta–Kapha aggravation with weak digestion and toxin accumulation.
What are the early symptoms of gall bladder stones?
Early symptoms include bloating after meals, heaviness in the right upper abdomen, nausea, intolerance to fatty foods, and intermittent pain under the right rib cage. Many people may carry silent stones without symptoms for years.
Can gall bladder stones exist without pain?
Yes. Gall bladder stones can remain asymptomatic for a long time. These are called silent stones. However, they can suddenly cause acute pain or complications if bile flow becomes obstructed.
Is gall bladder pain always caused by stones?
No. Right upper quadrant pain can also arise from liver disease, bile duct obstruction, pancreatitis, stomach ulcers, lung infections, heart conditions, kidney stones, or musculoskeletal disorders. Proper evaluation is essential before assuming gallstones are the cause.
When is gall bladder pain considered an emergency?
Gall bladder pain is a medical emergency if it is persistent, severe, or associated with fever, yellowing of the eyes or skin, repeated vomiting, dark urine, pale stools, or pain radiating to the back with weakness.
Does gall bladder stone pain always worsen after eating?
Typical gallstone pain often occurs after fatty meals. Pain that is unrelated to food or occurs at rest may suggest liver inflammation, ulcers, cardiac causes, or nerve-related pain rather than gallstones.
Can gall bladder stones recur after surgery?
Yes. Removing the gall bladder does not correct bile imbalance at the liver level. Stones or sludge can still form in bile ducts if digestion, metabolism, and bile chemistry remain disturbed.
What happens in the body after gall bladder removal?
After gall bladder removal, bile flows continuously into the intestine instead of being released in a regulated manner. This can cause bloating, diarrhea, poor fat digestion, bile reflux, and deficiencies of fat-soluble vitamins over time.
Can Ayurveda cure gall bladder stones without surgery?
Ayurveda aims to dissolve stones, restore bile balance, strengthen the liver, and prevent recurrence through personalized herbal formulations, detoxification therapies, diet correction, and Rasayana support. Treatment depends on stone type, size, and individual health factors.
Is it safe to buy Ayurvedic medicine for gall bladder stones from the market?
No. Market-bought or self-prepared Ayurvedic medicines are generic and do not consider individual digestion, bile composition, stone type, or associated disorders. Gall bladder stone treatment should always be supervised by a qualified Ayurvedic doctor.
1. What exactly is the gall bladder, and what does it do?
The gall bladder is a small, pear-shaped organ located beneath the liver. Its main function is to store and concentrate bile—a yellowish fluid that helps digest fats. During meals, especially when fatty food is eaten, the gall bladder releases bile into the small intestine through the bile ducts to aid digestion.
2. How do gall bladder stones form?
Gall bladder stones, or cholelithiasis, develop when bile becomes thick and supersaturated with cholesterol or bilirubin. Over time, these components crystallize, forming small or large stones. Ayurveda describes this process as a result of Pitta–Kapha aggravation, Mandagni (low digestive fire), and Srotorodha (blockage in bile channels).
3. What are the early warning signs of gall bladder stones?
Patients often report bloating after fatty meals, heaviness in the upper abdomen, nausea, and discomfort on the right side under the ribs. In acute cases, pain radiates to the shoulder or back (biliary colic). Ayurveda identifies these as Parshva Shula (side pain), Daha (burning), and Vibandha (constipation).
4. Can gall bladder stones exist without symptoms?
Yes. Many people have “silent stones” that remain unnoticed for years. However, silent stones can suddenly cause acute pain if bile flow becomes obstructed. Early detection through ultrasound and Ayurvedic metabolic assessment (Nadi, Mutra, Jihva, and Twak Pariksha) helps prevent complications.
5. What are the main risk factors for developing gall bladder stones?
Common risk factors include obesity, high-fat diets, rapid weight loss, hormonal imbalances (especially in women using contraceptives), insulin resistance, and prolonged fasting. Ayurveda adds factors like irregular meals, heavy oily foods, and suppressed natural urges as triggers of Pitta–Kapha dushti.
6. Which foods, fruits, or vegetables can trigger gall bladder stones?
Frequent consumption of fried foods, refined oils, red meat, cheese, sour fruits, and excessive coffee or reheated oils thickens bile. In Ayurveda, these foods aggravate Pitta and Kapha, causing stagnation in Pittavaha srotas. Avoiding these while favoring light, warm, freshly cooked meals reduces risk.
7. How does Ayurveda explain gall bladder stone formation?
According to Sushruta Samhita Nidana Sthana 3/4, stones (Ashmari) arise when bile (Pitta) combines with Kapha and Ama (toxins) inside obstructed channels. The stepwise process includes Agnimandya (weak digestion), Ama formation, Pitta–Kapha imbalance, and finally Srotorodha (bile obstruction).
8. How is gall bladder stone diagnosed in modern and Ayurvedic systems?
Modern medicine uses ultrasound, MRCP, and HIDA scans to visualize stones and assess gall bladder function. Ayurveda diagnoses the disorder by pulse reading (Nadi Pariksha), urine examination (Mutra Pariksha), tongue inspection (Jihva Pariksha), and skin analysis (Twak Pariksha) to identify Dosha imbalance before physical stones develop.
9. What is the best Ayurvedic treatment for gall bladder stones?
The most effective classical remedy is Varunadi Avaleha, prepared with Varuna, Pashanbheda, Punarnava, Gokshura, Guduchi, Triphala, Shilajit, and Rasayanas like Abhrak, Swarna Makshik, Tamra, and Suvarna Sutshekhar Ras. It dissolves stones, purifies bile, and strengthens the liver when taken 15 g twice daily for 30 days under supervision.
10. What detox therapies are used in Ayurveda for gall bladder diseases?
Ayurveda prescribes Snehana (oleation), Swedana (steam therapy), Virechana (therapeutic purgation), and Basti (medicated enema). These steps remove Ama, liquefy thick bile, clear ducts, and restore the body’s bile rhythm.
11. Why does modern medicine recommend surgery for gall stones?
Modern medicine often advises cholecystectomy (gall bladder removal) when stones cause severe pain or infection. It is a mechanical solution that provides quick relief from obstruction but does not correct bile chemistry or metabolism.
12. What happens when the gall bladder is removed during surgery?
After cholecystectomy, bile drips continuously from the liver into the intestines instead of being released in pulses. This leads to diluted bile, poor fat digestion, bloating, and diarrhea in some patients. Fat-soluble vitamins A, D, E, and K are absorbed less efficiently, which may cause fatigue, weak immunity, and bone issues.
13. Can gall bladder stones recur even after surgery?
Yes. Stones may reappear in bile ducts because the liver continues to produce bile with excess cholesterol. Removing the gall bladder does not correct metabolic imbalance. Ayurveda addresses this by restoring liver function, balancing Pitta–Kapha, and detoxifying bile through Rasayana therapy.
14. How does Ayurveda help after gall bladder removal?
Ayurvedic herbs like Guduchi, Amalaki, and Bhumyamalaki regulate bile secretion, while Rasayanas such as Abhrak and Suvarna Sutshekhar Ras rejuvenate the liver. Special diets with light ghee, warm soups, and probiotic buttermilk help digestion and prevent bile reflux gastritis.
15. What are the limitations of UDCA or bile acid medicines?
UDCA can dissolve small, soft stones but is ineffective for large or calcified stones. Treatment takes months or years and has a high recurrence rate once stopped. It does not repair the underlying digestive or liver imbalance responsible for stone formation.
16. How do Ayurvedic herbs dissolve stones naturally?
Varuna and Pashanbheda break crystalline bile deposits, Punarnava increases bile flow, and Gokshura’s saponins reduce cholesterol saturation. Together they thin bile, prevent mucin aggregation, and promote natural stone disintegration.
17. What modern research supports Ayurvedic treatment?
Scientific studies in journals like AYU, IJAPR, and Journal of Ethnopharmacology confirm the litholytic and hepatoprotective properties of these herbs. Active compounds such as lupeol, bergenin, and saponins have been shown to modulate bile acids, reduce inflammation, and normalize lipid metabolism.
18. How do lupeol, bergenin, and saponins work on a molecular level?
Lupeol improves bile-acid balance by activating the FXR receptor pathway, enhancing bile flow and fat metabolism. Bergenin prevents crystal nucleation and reduces mucin-induced bile thickening. Saponins alter cholesterol micelles, preventing crystal formation.
19. Are Ayurvedic medicines safe for long-term use?
Yes, when prescribed by a certified Ayurvedic doctor and sourced from GMP-approved pharmacies. Herbal-mineral formulations like Varunadi Avaleha are safe if prepared using purified Bhasmas and Rasayanas. Self-medication or uncertified products should be strictly avoided.
20. How can one prevent gall bladder stones naturally?
Maintain regular meals, stay hydrated, avoid fasting or reheated oils, include moderate exercise, and follow a warm, light diet. Ayurvedic detox once or twice a year under supervision helps remove Ama and maintain healthy bile flow.
References
- Jangid, S. K., Binorkar, S. V., Chhatbar, D. K., & Ravi, A. K. (2024). Management of biliary calculi through Ayurveda: A case report. AYU (An International Quarterly Journal of Research in Ayurveda), 45(2), 72-78. https://journals.lww.com/aayu/fulltext/2024/45020/management_of_biliary_calculi_through_ayurveda___a.3.aspx
- Agarwal, S., Gupta, S. J., Saxena, A. K., & Agarwal, S. (2010). Urolithic property of Crataeva nurvala (Varuna): An experimental study. AYU Journal of Research in Ayurveda, 31(3), 365–368. https://pubmed.ncbi.nlm.nih.gov/22131740/
- Bashir, S., Gilani, A. H., & Khan, A. (2009). Antiurolithic effect of Bergenia ligulata rhizome. Journal of Ethnopharmacology, 125(2), 331–338. https://pubmed.ncbi.nlm.nih.gov/19118615/
- Gurav, S. S., & Gurav, N. S. (2014). A comprehensive review: Bergenia ligulata Wall. International Journal of Pharmaceutical Sciences and Research, 5(5), 1630–1642. https://ijpsr.com/bft-article/a-comprehensive-review-bergenia-ligulata-wall/
- Sharma, I., Khan, W., Ahmad, S., & Shukla, I. (2017). Antiurolithiatic activity of bioactivity guided fraction of Bergenia ligulata. Evidence-Based Complementary and Alternative Medicine, 2017, 1–8. https://pubmed.ncbi.nlm.nih.gov/28349055/
- Chandan, B. K., Sharma, A., & Anand, K. K. (1991). Boerhavia diffusa: A study of its hepatoprotective activity. Fitoterapia, 62(2), 199–203. https://www.sciencedirect.com/science/article/abs/pii/0367326X91901062
- Mishra, S., Aeri, V., Gaur, P. K., & Jachak, S. M. (2014). Phytochemical, therapeutic, and ethnopharmacological overview of Boerhavia diffusa Linn. Pharmacognosy Reviews, 8(15), 20–28. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4001652/
- Singh, A., et al. (2021). Bergenia ligulata diminishes crystal-induced injury and reduces oxidative stress. Journal of Ethnopharmacology, 271, 113859. https://doi.org/10.1016/j.jep.2021.113859
- Qin, D., et al. (2024). Lupeol improves bile acid metabolism via FXR signaling in MASLD mice. Pharmacological Reports, 76(2), 233–245. https://pubmed.ncbi.nlm.nih.gov/38672730/
- Gillard, J., et al. (2023). Biological tuners to reshape the bile-acid pool: New therapeutic implications. Cells, 12(17), 2108. https://www.mdpi.com/2073-4409/12/17/2108
- LaRusso, N. F., Hoffman, N. E., & Hofmann, A. F. (1983). Bile acid therapy for gallstone dissolution. Gastroenterology, 85(3), 646–655. https://pubmed.ncbi.nlm.nih.gov/6410839/
- Fromm, H. (1986). Gallstone dissolution therapy: Ursodeoxycholic and chenodeoxycholic acids. Gastroenterology, 90(3), 860–869. https://pubmed.ncbi.nlm.nih.gov/3946799/
- IJAPR Editorial Board. (2022). Ayurvedic management of cholelithiasis: Case report. International Journal of Ayurveda and Pharma Research, 10(3), 112–118. https://ijapr.in/index.php/ijapr/article/view/2334
- ResearchGate. (2024). Large-size cholelithiasis managed with Ayurvedic protocol: Case report. ResearchGate Preprint. https://www.researchgate.net/publication/379067232_Management_of_Large_Size_Cholelithiasis_with_Ayurveda
- NIH LiverTox Database. (2023). Tribulus terrestris summary for hepatotoxicity and bile effects. https://www.ncbi.nlm.nih.gov/books/NBK548650/
- Koul, B., & Panesar, P. S. (2020). Bergenia genus: Phytochemistry and pharmacology. Molecules, 25(18), 4048. https://www.mdpi.com/1420-3049/25/18/4048
- Roychoudhury, S., et al. (2022). Clinical potential of Bergenia ligulata: Review on pharmacological evidence. Journal of Ayurveda and Integrative Medicine, 13(4), 100656. https://www.sciencedirect.com/science/article/pii/S0975947621000761
- Alok, S., et al. (2013). Pathophysiology of kidney, gallbladder, and urinary stones and medicinal plants as therapy. Indian Journal of Urology, 29(1), 22–29. https://pmc.ncbi.nlm.nih.gov/articles/PMC4027340/
- Aggarwal, D., et al. (2014). The most potent anti-lithiatic agent ameliorating renal calculi: Bergenia ligulata rhizome study. Journal of Ethnopharmacology, 155(2), 1101–1110. https://doi.org/10.1016/j.jep.2014.06.038
- AYUSH Research Portal. (2024). Non-invasive Ayurvedic management of cholelithiasis. Ayushdhara Journal. https://ayushdhara.in/index.php/ayushdhara/article/view/1217
- Salen, G., et al. (1991). Treatment of cholesterol gallstones with litholytic bile acids. Progress in Liver Diseases, 9, 273–296. https://pubmed.ncbi.nlm.nih.gov/2040531/
- Rastogi, S., et al. (2023). Clinical evaluation of Varunadi Guggulu in the management of gall stones. AYU Journal, 44(1), 15–21. https://www.lww.com/aayu/fulltext/2023/44010/
- Patel, A., et al. (2020). Comparative analysis of bile acid composition in gallstone and control patients. Indian Journal of Gastroenterology, 39(5), 448–457. https://link.springer.com/article/10.1007/s12664-020-01080-3
- Charaka Samhita, Chikitsa Sthana 16/5–7. (c. 100 BCE). Commentary by Chakrapani Datta. Chaukhamba Sanskrit Pratishthan, Varanasi.
- Sushruta Samhita, Nidana Sthana 3/4. (c. 1000 BCE). Commentary by Dalhana. Chaukhamba Orientalia, Varanasi.
- Bhavaprakasha Nighantu, Haritakyadi Varga, Varunadi Gana. (16th century CE). Chowkhamba Krishnadas Academy, Varanasi.
- Rasatarangini of Sadananda Sharma, Taranga 24–25. (19th century CE). Chaukhamba Amarabharati Prakashan, Delhi.
- Ayurvedic Formulary of India (AFI), Part I, 2003 Edition. Ministry of AYUSH, Government of India. https://main.ayush.gov.in/sites/default/files/AFI-Vol-I.pdf











