- Colorectal Cancer Risk Factors
- Early Warning Signs
- Diagnostic Pathway in Western Healthcare
- Standard Medical Treatment Options
- The Rising Interest in Integrative and Holistic Approaches
- Ayurvedic Interpretation of Colorectal Cancer
- Prevention Is Power
- Modern Research References
- Ayurvedic Textual References
Colorectal cancer is a malignancy that arises in the colon or rectum – two critical sections of the digestive system responsible for water absorption and waste elimination. Though often grouped together, colon and rectal cancers are distinguished based on their location. Colon cancer develops in the upper parts of the large intestine, while rectal cancer arises in the final 12 centimeters leading to the anus. Despite this anatomical distinction, both share similar risk factors, progression patterns, and treatment approaches.
Most colorectal cancers begin as noncancerous growths called polyps—specifically, adenomatous polyps. These benign lesions can silently exist for years before undergoing genetic mutations in key regulatory genes such as APC, KRAS, and p53. As these mutations accumulate, the polyp may transform into an invasive cancer capable of penetrating deeper layers of the colon wall and, eventually, spreading to other organs such as the liver or lungs. This well-documented progression is known as the adenoma–carcinoma sequence.
To determine the severity of the disease and guide treatment decisions, colorectal cancer is staged using the TNM classification system. This framework evaluates how deeply the tumor has invaded surrounding tissues (T), whether nearby lymph nodes are involved (N), and whether the cancer has metastasized to distant sites like the liver or lungs (M). These individual assessments are then grouped into stages ranging from 0 to IV. Stage 0 represents a carcinoma in situ, meaning the abnormal cells are confined to the inner lining of the colon. Stages I and II involve progressively deeper invasion without lymph node involvement. Stage III indicates regional lymph node spread, and Stage IV represents advanced disease with distant metastases.
Understanding this progression and staging is vital, not only for clinicians making treatment plans but also for patients seeking to comprehend the seriousness of their condition. With early detection, colorectal cancer is highly treatable. However, when diagnosed at an advanced stage, it becomes more challenging to manage and often requires multimodal therapy.
Colorectal Cancer Risk Factors
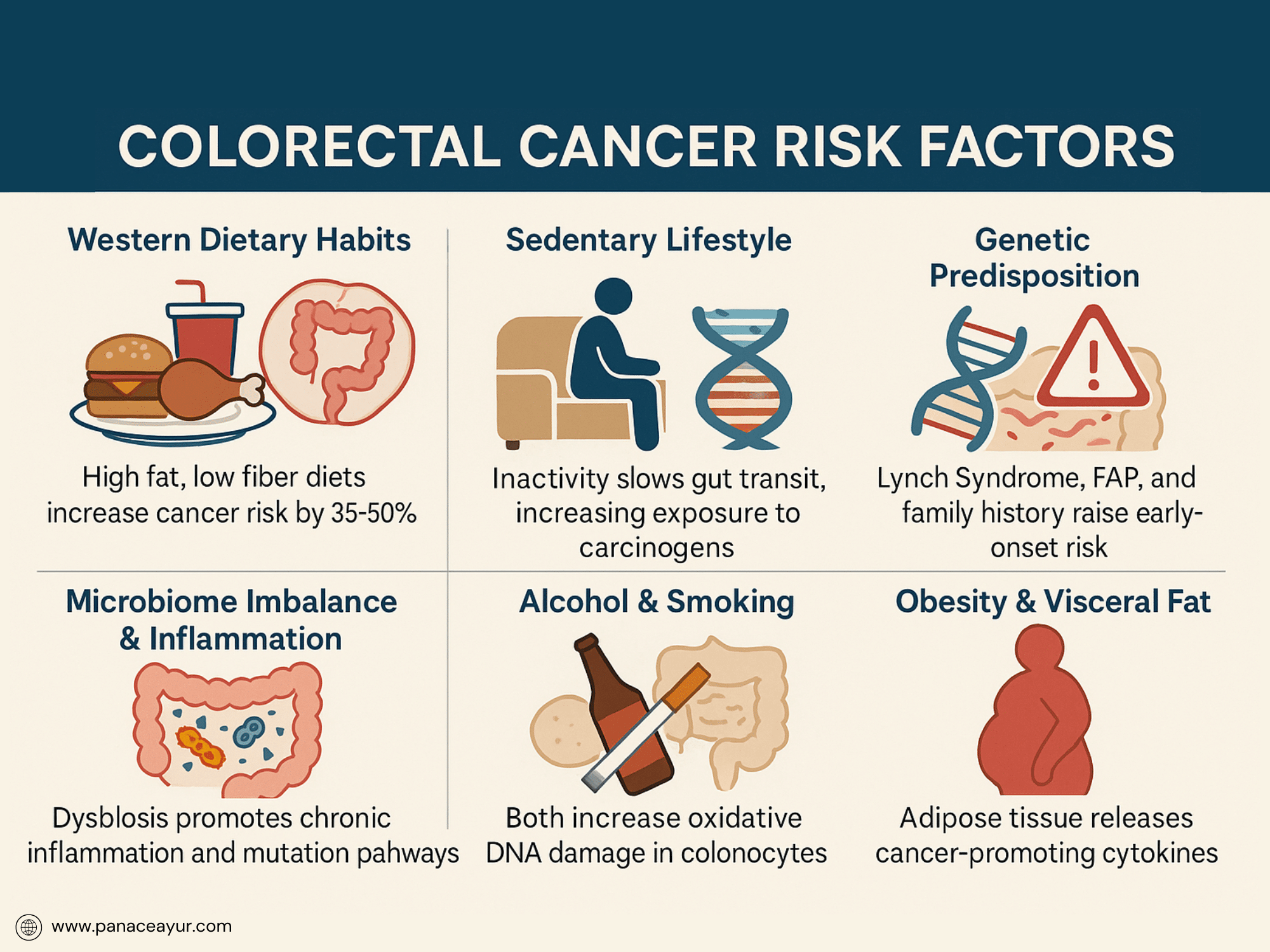
Colorectal cancer does not develop in isolation; it is the result of a complex interplay between genetic predispositions, environmental exposures, and lifestyle choices. In Western countries, one of the most significant contributors is diet. A typical Western diet—rich in red and processed meats, low in fiber, and high in refined carbohydrates—creates an inflammatory gut environment that promotes polyp formation and carcinogenic changes in the intestinal lining. Additionally, excessive alcohol consumption and long-term smoking have been directly associated with increased colorectal cancer risk, particularly when combined with a sedentary lifestyle and central obesity.
Obesity, especially visceral fat accumulation, is more than a cosmetic concern—it is a metabolic condition that drives chronic inflammation, insulin resistance, and hormonal imbalances, all of which are known to promote cancer development. Epidemiological studies consistently show that individuals with a high body mass index (BMI) face a significantly elevated risk of colorectal malignancies.
Genetics also plays a crucial role. Inherited syndromes such as Lynch Syndrome (also known as hereditary nonpolyposis colorectal cancer or HNPCC) and familial adenomatous polyposis (FAP) dramatically increase lifetime risk. Individuals with these conditions often develop cancer at a younger age, making early genetic screening and family history assessments essential.
Emerging research has also highlighted the role of the gut microbiome—a delicate ecosystem of trillions of microorganisms that reside in the colon. Disruption in the balance of beneficial and harmful bacteria, a condition known as dysbiosis, can produce carcinogenic metabolites, trigger inflammation, and compromise the gut barrier, setting the stage for tumorigenesis. Chronic diseases such as type 2 diabetes, inflammatory bowel disease (e.g., ulcerative colitis, Crohn’s disease), and a personal history of colorectal polyps or cancer further amplify the risk.
Understanding these risk factors allows patients and healthcare providers to adopt targeted prevention strategies. Lifestyle interventions—such as increasing physical activity, maintaining a healthy weight, adopting a plant-forward diet, and undergoing regular screening—can significantly reduce risk and are particularly effective when implemented early.
Early Warning Signs
Colorectal cancer often develops silently, without any symptoms in the early stages. This asymptomatic nature is one reason why many patients are diagnosed only when the disease has progressed significantly. However, as the tumor grows or begins to obstruct the bowel, a range of warning signs may emerge—signals that should never be dismissed as minor digestive discomfort.
One of the most common early indicators is the presence of blood in the stool. While this may appear as bright red streaks or darker, tar-like stools, it can also be microscopic and only detectable through a fecal occult blood test. Chronic blood loss from a tumor may lead to iron-deficiency anemia, especially in right-sided colon cancers. Patients often report unexplained fatigue, pale skin, and shortness of breath, which are not immediately linked to gastrointestinal issues but may be signs of a slow, internal bleed.
Another significant warning sign is a change in bowel habits. This includes persistent diarrhea, constipation, or a sudden change in stool consistency. A tumor that narrows the intestinal passage can also produce a sensation of incomplete evacuation, leading to frequent trips to the bathroom without relief. Some patients describe thin or ribbon-like stools as the cancer obstructs normal fecal passage.
Unexplained weight loss is another red flag. When cancer disrupts the body’s metabolic balance or spreads systemically, it can lead to rapid loss of muscle mass and appetite, even when the patient is not actively dieting or exercising. In more advanced cases, abdominal pain, rectal discomfort, bloating, or a persistent urge to pass stool (tenesmus) may occur, especially when the rectum is involved.
Because these symptoms can overlap with benign conditions like hemorrhoids, irritable bowel syndrome (IBS), or infections, they are often ignored or misdiagnosed. However, any persistent change—especially in individuals over age 45, or earlier in those with a family history—warrants immediate medical evaluation, including a stool test or colonoscopy. Early recognition of these signs dramatically improves treatment success and survival rates.
Diagnostic Pathway in Western Healthcare
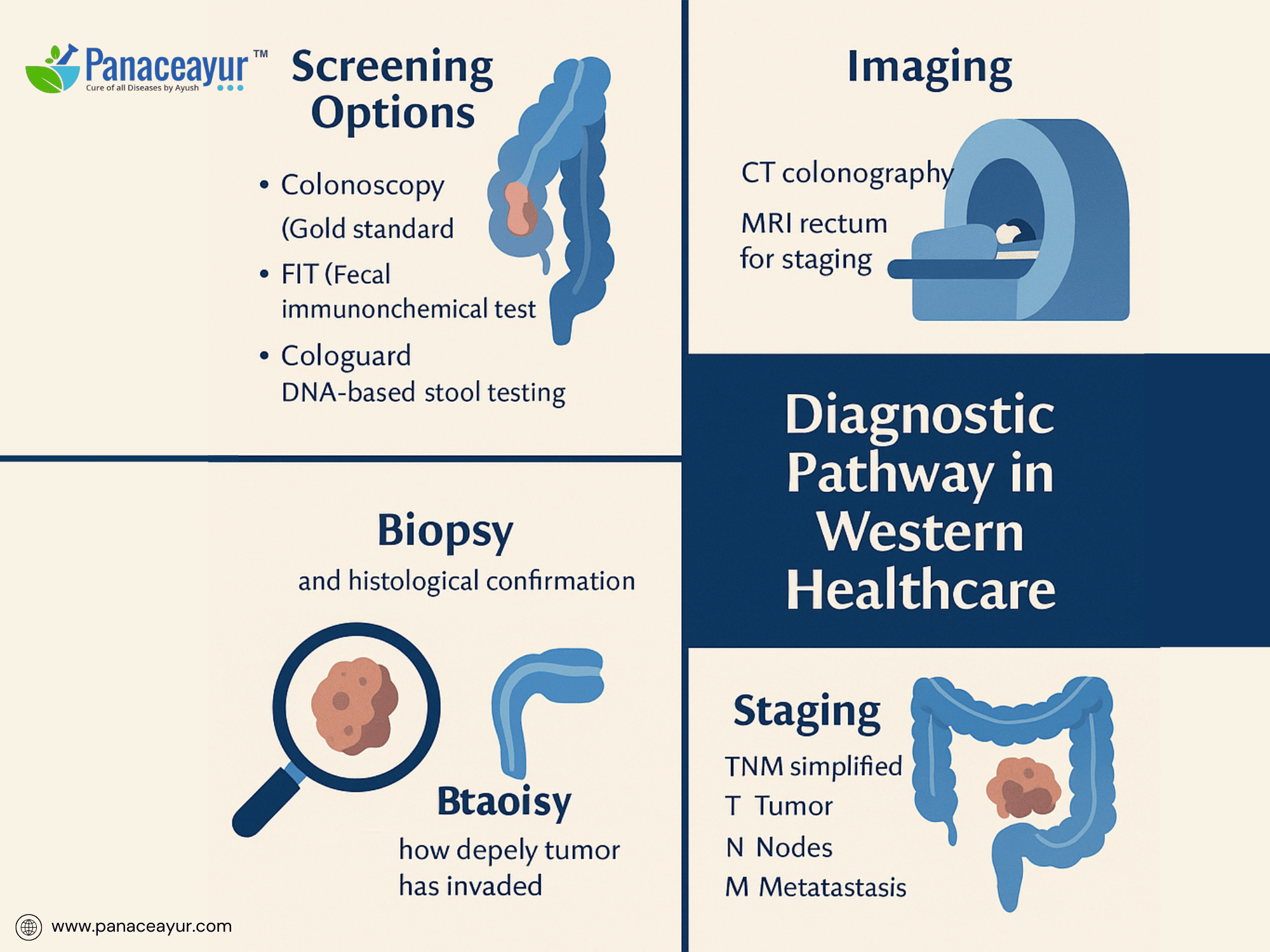
Detecting colorectal cancer early is one of the most powerful tools in preventing death and long-term complications. In Western medical systems, the diagnostic journey begins either with routine screening or the investigation of suspicious symptoms. Screening programs are especially vital because many patients are asymptomatic during the early, most treatable stages.
The most definitive and widely recommended screening method is colonoscopy, a procedure that uses a flexible tube with a camera to visually inspect the entire colon and rectum. If polyps or suspicious lesions are found during this examination, they can often be removed or biopsied immediately. Colonoscopy is typically recommended starting at age 45 for average-risk individuals and earlier for those with a family history or known genetic predispositions.
For patients seeking less invasive options, two primary stool-based tests are available. The Fecal Immunochemical Test (FIT) detects hidden blood in the stool—a possible sign of polyps or cancer. It is highly specific and does not require dietary restrictions. Another increasingly popular test is Cologuard, which analyzes both blood and abnormal DNA shed from cancerous or precancerous cells into the stool. While not a replacement for colonoscopy, it is a useful tool for those unwilling or unable to undergo more invasive procedures.
If abnormalities are detected through any of these initial screenings, the next steps involve tissue biopsy and histological analysis, typically obtained during colonoscopy. This allows pathologists to determine whether cancer is present, its grade (how aggressive the cells appear), and whether further imaging is needed.
Staging is then completed using imaging techniques such as CT scans of the abdomen and pelvis, MRI for rectal tumors, and sometimes PET scans to assess for distant metastasis. Blood tests, including carcinoembryonic antigen (CEA) levels, may be used to monitor tumor activity and track recurrence over time.
This structured diagnostic process—symptom recognition, screening, visual confirmation, biopsy, and staging—enables clinicians to accurately define the disease’s extent and plan a personalized treatment protocol. The emphasis on regular screening in Western healthcare has led to significant improvements in early detection rates, especially in countries where screening is integrated into national health policies.
Standard Medical Treatment Options
Once a diagnosis of colorectal cancer is confirmed and staged, treatment is guided by a combination of factors including tumor location, stage, genetic profile, and the patient’s overall health status. In Western medicine, a multidisciplinary approach is used, often combining surgery, chemotherapy, radiation, and newer targeted therapies. Each component is carefully selected to maximize tumor eradication while minimizing harm to healthy tissues.
Surgery remains the cornerstone of curative treatment, especially for localized cancers. Depending on the tumor’s location, different types of colectomy procedures may be performed—ranging from partial removal of the colon (hemicolectomy) to total colectomy in extensive cases. Minimally invasive techniques, such as laparoscopic and robotic-assisted surgeries, are increasingly favored in Western centers due to quicker recovery times and fewer complications. For rectal cancers, surgeons may also perform total mesorectal excision (TME) to ensure clean margins and reduce recurrence risk.
Chemotherapy plays a central role in both adjuvant (post-surgical) and neoadjuvant (pre-surgical) settings. Common drug regimens include FOLFOX (5-FU, leucovorin, and oxaliplatin) or CAPOX (capecitabine and oxaliplatin). These agents work by disrupting cancer cell DNA synthesis and replication. In stage III and some high-risk stage II cases, chemotherapy significantly improves survival outcomes by eradicating micrometastases that surgery alone cannot remove.
For advanced or metastatic cases, targeted therapies have expanded treatment options. Drugs like bevacizumab (an anti-VEGF monoclonal antibody) and cetuximab or panitumumab (EGFR inhibitors) are used based on the tumor’s molecular profile, particularly KRAS, NRAS, and BRAF mutation status. These precision medicines are administered alongside chemotherapy to halt tumor progression at the molecular level.
Immunotherapy has shown promise in a subset of colorectal cancers—particularly those classified as microsatellite instability-high (MSI-H) or mismatch repair-deficient (dMMR). In these cases, checkpoint inhibitors like pembrolizumab or nivolumab unleash the body’s immune system to recognize and destroy cancer cells.
Radiation therapy is primarily used for rectal cancer, either before surgery to shrink the tumor and increase operability, or afterward to reduce local recurrence. Advanced techniques such as intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) offer precise targeting of cancer cells while sparing surrounding tissues.
This layered, personalized approach to treatment reflects the sophistication of Western oncology. However, it also underscores the importance of genetic testing, tumor profiling, and coordinated care to optimize outcomes and reduce toxicity.
The Rising Interest in Integrative and Holistic Approaches
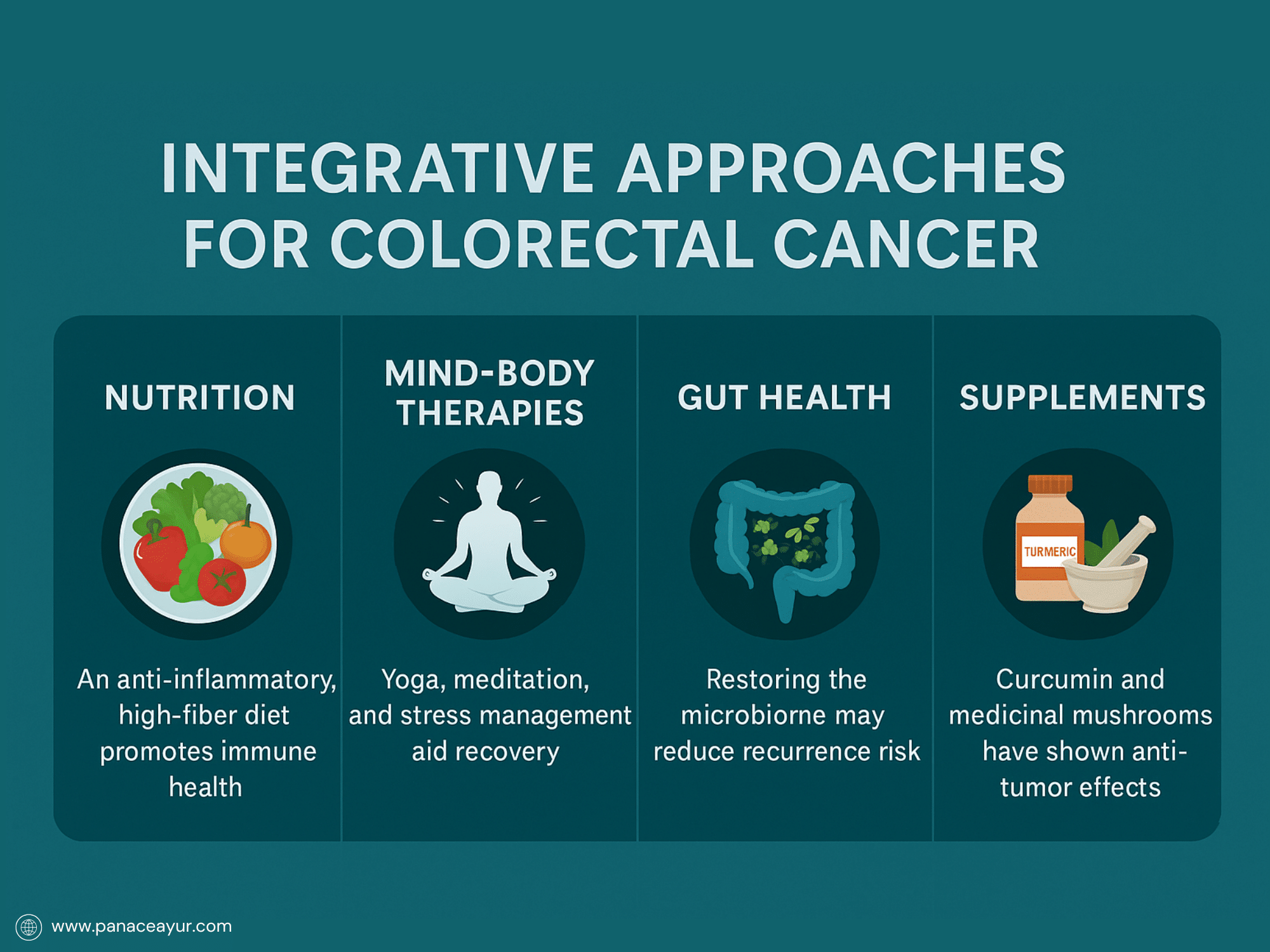
As survival rates improve and awareness spreads, a growing number of Western patients are seeking integrative strategies that go beyond conventional cancer treatments. While surgery, chemotherapy, and radiation remain the pillars of oncologic care, they often leave behind residual symptoms—fatigue, neuropathy, gut dysbiosis, or emotional trauma—that conventional medicine alone does not always address. This unmet need has driven an increased interest in holistic and complementary therapies that support the body’s resilience, restore internal balance, and enhance quality of life.
Functional medicine, a systems-based model gaining traction in the West, views cancer not only as a disease of uncontrolled cell growth but as a manifestation of metabolic, inflammatory, and immunological dysfunction. Practitioners in this field focus on restoring the terrain—particularly the gut microbiome, detoxification pathways, mitochondrial health, and chronic inflammation—as a way to improve recovery and reduce the chance of recurrence. This philosophy shares parallels with ancient healing systems such as Ayurveda, which emphasize balance, digestion, and detoxification as core pillars of health.
Dietary modification is a cornerstone of integrative care. Anti-inflammatory, high-fiber, plant-forward diets are encouraged to modulate insulin levels, reduce oxidative stress, and improve gut flora—all of which can influence cancer progression and immune function. Foods rich in polyphenols (e.g., berries, green tea, turmeric), cruciferous vegetables, and omega-3 fatty acids have been shown to possess cancer-protective properties. Nutrition plans are often personalized based on genetic markers, bloodwork, and metabolic needs.
Mind-body therapies such as yoga, mindfulness meditation, guided imagery, and breathwork are widely adopted in cancer centers across the U.S. and Europe. These practices not only help patients cope with treatment-related stress and anxiety but also improve immune modulation through measurable changes in cortisol and cytokine levels. Patients often report improved sleep, reduced pain perception, and enhanced emotional resilience.
Supplements and botanical therapies are also being integrated cautiously into care plans. Substances like curcumin (from turmeric), medicinal mushrooms (e.g., reishi, turkey tail), and vitamin D have demonstrated anti-tumor effects in preclinical or small-scale human studies. However, these should only be used under medical supervision to avoid interactions with chemotherapy or radiation.
The Western embrace of integrative oncology reflects a deeper shift in public consciousness: health is no longer viewed as merely the absence of disease, but as a dynamic state of physical, emotional, and spiritual harmony. This evolving model encourages patients to become active participants in their recovery, drawing from both science and tradition to create a personalized path toward healing.
Ayurvedic Interpretation of Colorectal Cancer
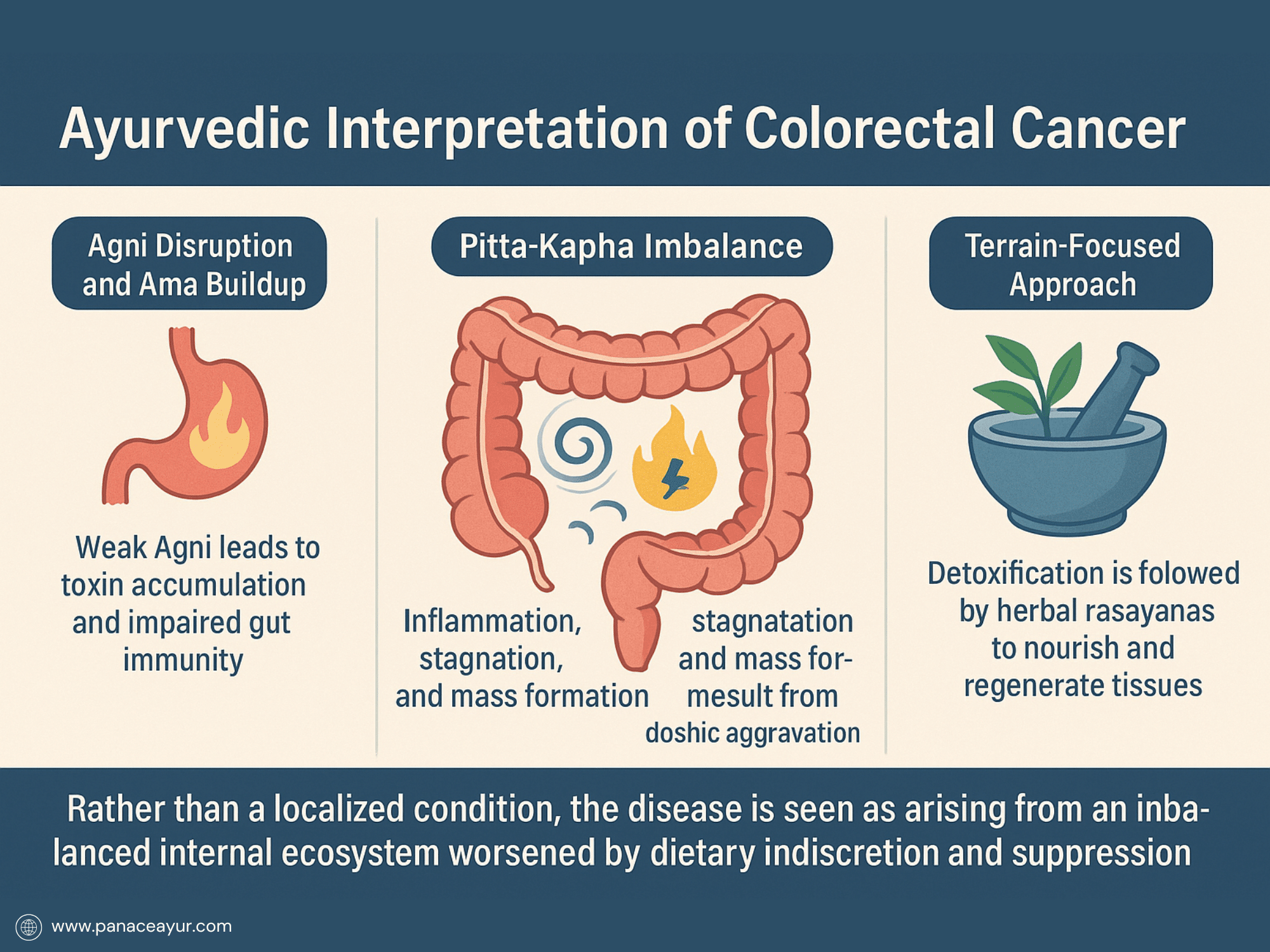
Ayurveda, the ancient Indian system of medicine, views colorectal cancer not merely as a tumor within the intestines but as the manifestation of deeper systemic imbalances. Rather than focusing solely on eradicating malignant cells, Ayurveda centers its attention on correcting the internal ecosystem—the terrain—in which the cancer developed. This terrain includes the Agni (digestive fire), the Srotas (microchannels of circulation), and the Dhatus (tissues) that collectively determine whether the body supports health or fosters disease. According to this perspective, colorectal cancer arises when digestion is weakened, toxins accumulate, cellular regeneration is impaired, and the body’s innate intelligence is disrupted.
In classical texts such as Charaka Samhita, Ashtanga Hridaya, and Bhavaprakasha, conditions that mirror the symptoms of colorectal cancer are described under categories like Grahani Roga (disorders of the small and large intestines), Arsha (abnormal growths or rectal masses), and Vidradhi (deep abscesses or tumors). These conditions are considered the result of Agnimandya—a chronic derangement of metabolic fire—and Ama—undigested metabolic waste that clogs the Srotas. Over time, the persistent presence of Ama within the gut leads to inflammation, stagnation, and tissue degeneration, setting the stage for neoplastic growths. This pathology is exacerbated by faulty lifestyle habits, such as suppressing natural urges (e.g., bowel movements, sleep), chronic emotional stress, incompatible food combinations (Viruddha Ahara), and irregular meal timings—all of which disrupt the harmony of the Doshas.
From a Dosha perspective, colorectal cancer is primarily driven by the vitiation of Pitta and Kapha, though advanced or metastatic forms often show Vata involvement. Pitta Dosha, when imbalanced, manifests as excess heat, inflammation, and ulceration of the intestinal lining. This fiery nature aggravates Rakta (blood tissue) and Mamsa (muscle tissue), creating conditions favorable for cellular mutation. Meanwhile, Kapha Dosha, characterized by heaviness, density, and stagnation, contributes to the formation of masses, mucosal overgrowth, and obstruction of channels. When Vata Dosha is also disturbed, especially in chronic and cachectic stages, it facilitates the spread of abnormal cells to distant sites through subtle energetic pathways.
To correct this imbalance, Ayurveda adopts a multi-phase, terrain-restorative approach. The first line of treatment begins with Deepana and Pachana, which involve rekindling the digestive fire and digesting Ama (toxic buildup) using pungent, bitter, and astringent herbs. Once digestion is stabilized, Shodhana (biological purification) is initiated—most notably Virechana (therapeutic purgation) to eliminate aggravated Pitta and Kapha from the gastrointestinal tract. In certain cases, Basti therapy (medicated enemas) is employed to cleanse the lower colon and restore Vata balance. These therapies are meticulously chosen based on the individual’s Prakriti (constitutional type) and Vikriti (current state of imbalance).
Following purification, the body enters the phase of Rasayana therapy, which aims to regenerate depleted tissues, strengthen Ojas (vital energy), and modulate the immune system. Herbs and formulations such as Ashwagandha (Withania somnifera), Guduchi (Tinospora cordifolia), Haritaki (Terminalia chebula), Kutaja (Holarrhena antidysenterica), and Triphala are extensively used to rejuvenate intestinal mucosa, reduce oxidative stress, and regulate gut immunity. Classical mineral preparations like Swarna Bhasma (gold ash), Abhrak Bhasma (mica ash), and Gandhak Rasayan (sulfur compound) are introduced with precision to detoxify at the cellular level and rebuild dhatus. These Rasayanas not only work on physical tissues but are also believed to restore the cellular intelligence or Prakriti Smriti—the memory of health encoded within the body.
Importantly, the Ayurvedic approach doesn’t exist in opposition to modern medicine—it complements it. Integrative practitioners often employ Ayurvedic therapies alongside chemotherapy or radiation to buffer side effects, support recovery, and enhance long-term wellness. For example, herbs like Curcuma longa (Turmeric) and Boswellia serrata (Shallaki) have been shown in modern research to inhibit inflammatory pathways (like COX-2 and NF-κB), reduce angiogenesis, and induce apoptosis in colon cancer cells. Additionally, Guduchi has demonstrated immunomodulatory activity, potentially supporting T-cell function during immunosuppression.
This integrative strategy also includes individualized dietary regimens, yoga therapy, pranic breathing, and spiritual cleansing. Diets focus on warm, cooked, digestible meals tailored to the patient’s constitution and disease stage. Yoga and meditation are used to calm the mind, support parasympathetic tone, and improve gut-brain harmony—an important factor in colorectal cancer, where stress and bowel irregularity are closely linked.
In essence, Ayurveda does not merely aim to kill the tumor; it seeks to transform the terrain so that cancer can no longer thrive. The terrain is likened to soil—if the soil is healthy, no weeds (cancer cells) can flourish. This philosophy echoes the terrain theory gaining traction in functional medicine and microbiome research in the West. By aligning modern pathology with ancient Ayurvedic insight, we uncover a deeply intelligent model of healing—one that respects the body’s wisdom, honors individuality, and restores balance at every level of existence.
Prevention Is Power
Colorectal cancer is one of the few major cancers that is both highly preventable and treatable—when caught early. Yet, despite the availability of effective screening tools, lifestyle awareness, and integrative strategies, tens of thousands of preventable cases continue to emerge each year, particularly in countries where sedentary habits, processed diets, and chronic stress dominate daily life.
Prevention begins with awareness, and awareness begins with education. Simple, consistent lifestyle changes can significantly reduce one’s lifetime risk. A fiber-rich diet that includes vegetables, legumes, whole grains, and healthy fats helps sweep carcinogens out of the colon and feeds beneficial gut bacteria. Limiting red and processed meats, sugary drinks, and alcohol directly lowers risk. Routine physical activity, even a 30-minute daily walk, boosts circulation, reduces inflammation, and supports healthy bowel motility.
Regular screenings are among the most powerful tools in modern medicine. Colonoscopy not only detects early cancers but removes pre-cancerous polyps before they have a chance to grow. For individuals of average risk, screening typically starts at age 45—but it may begin earlier for those with genetic predispositions or family history. Choosing to be screened is not just a medical decision—it’s a commitment to proactive self-care.
Stress management is another overlooked dimension of prevention. Chronic stress weakens immune surveillance, disrupts digestion, and alters the microbiome—each of which creates an internal environment favorable to disease. Practicing mindfulness, yoga, or breathwork, even briefly each day, helps reset the body’s healing response.
Ayurveda adds a profound preventive dimension by emphasizing daily rhythms (Dinacharya), seasonal cleansing (Ritucharya), and food-mind compatibility (Ahara-Vihara). By strengthening Agni, eliminating Ama, and aligning lifestyle with natural cycles, Ayurveda works to protect the body long before disease manifests. Its emphasis on self-awareness, proper digestion, and personalized care allows prevention to be tailored to an individual’s constitution rather than relying on generalized advice.
Ultimately, the message is clear: you have more control than you think. Colorectal cancer is not a random strike—it is often the outcome of years of internal imbalance. But just as imbalance accumulates, so too does healing. By investing daily in your gut health, emotional well-being, and metabolic vitality, you are not just preventing cancer—you are creating a foundation for a life of strength, clarity, and resilience.
Modern Research References
- National Cancer Institute. (2023). Possible Signs of Colorectal Cancer in Younger Adults. Retrieved from https://www.cancer.gov/news-events/cancer-currents-blog/2023/colorectal-cancer-young-people-warning-signs
- American Cancer Society. (2024). Colorectal Cancer Screening Tests. Retrieved from https://www.cancer.org/cancer/types/colon-rectal-cancer/detection-diagnosis-staging/screening-tests-used.html
- Mayo Clinic. (2022). Integrative Oncology: Lifestyle Medicine for People with Cancer. Retrieved from https://cancerblog.mayoclinic.org/2022/03/15/integrative-oncology-lifestyle-medicine-for-people-with-cancer/
- PubMed Central. (2023). Update on Targeted Therapy and Immunotherapy for Metastatic Colorectal Cancer. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10854977/
- National Center for Biotechnology Information. (2023). The Role of Diet and Lifestyle in Colorectal Cancer Incidence. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK585999/
- American Cancer Society. (2023). Colorectal Cancer Signs and Symptoms. Retrieved from https://www.cancer.org/cancer/types/colon-rectal-cancer/detection-diagnosis-staging/signs-and-symptoms.html
- PubMed Central. (2023). Integrative Treatment for Colorectal Cancer. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30247965/
- American Cancer Society. (2023). Colorectal Cancer: Screening. Retrieved from https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening
Ayurvedic Textual References
- Charaka Samhita. Sutrasthana, Chapter 28. Discusses the concept of Grahani Roga and its relation to digestive disorders.
- Sushruta Samhita. Nidanasthana, Chapter 2. Elaborates on Arsha (hemorrhoids) and its pathogenesis.
- Bhavaprakasha. Madhyamakhanda, Chapter 3. Details the properties and uses of Guduchi (Tinospora cordifolia) in digestive ailments.
- Rasa Tarangini. Chapter 24. Describes the preparation and therapeutic uses of Swarna Bhasma in chronic conditions.
- Ashtanga Hridaya. Chikitsasthana, Chapter 8. Provides insights into the management of Grahani and related disorders.
- Bhaishajya Ratnavali. Chapter 12. Lists formulations beneficial in treating digestive system ailments.
- Kashyapa Samhita. Khilasthana, Chapter 4. Discusses the importance of Agni (digestive fire) in maintaining health.
- Yogaratnakara. Chapter on Grahani Roga. Offers various herbal formulations for managing Grahani.