- Anatomy and Function of the Pancreas
- How Chronic Pancreatitis Develops (Pathophysiology)
- Causes and Risk Factors
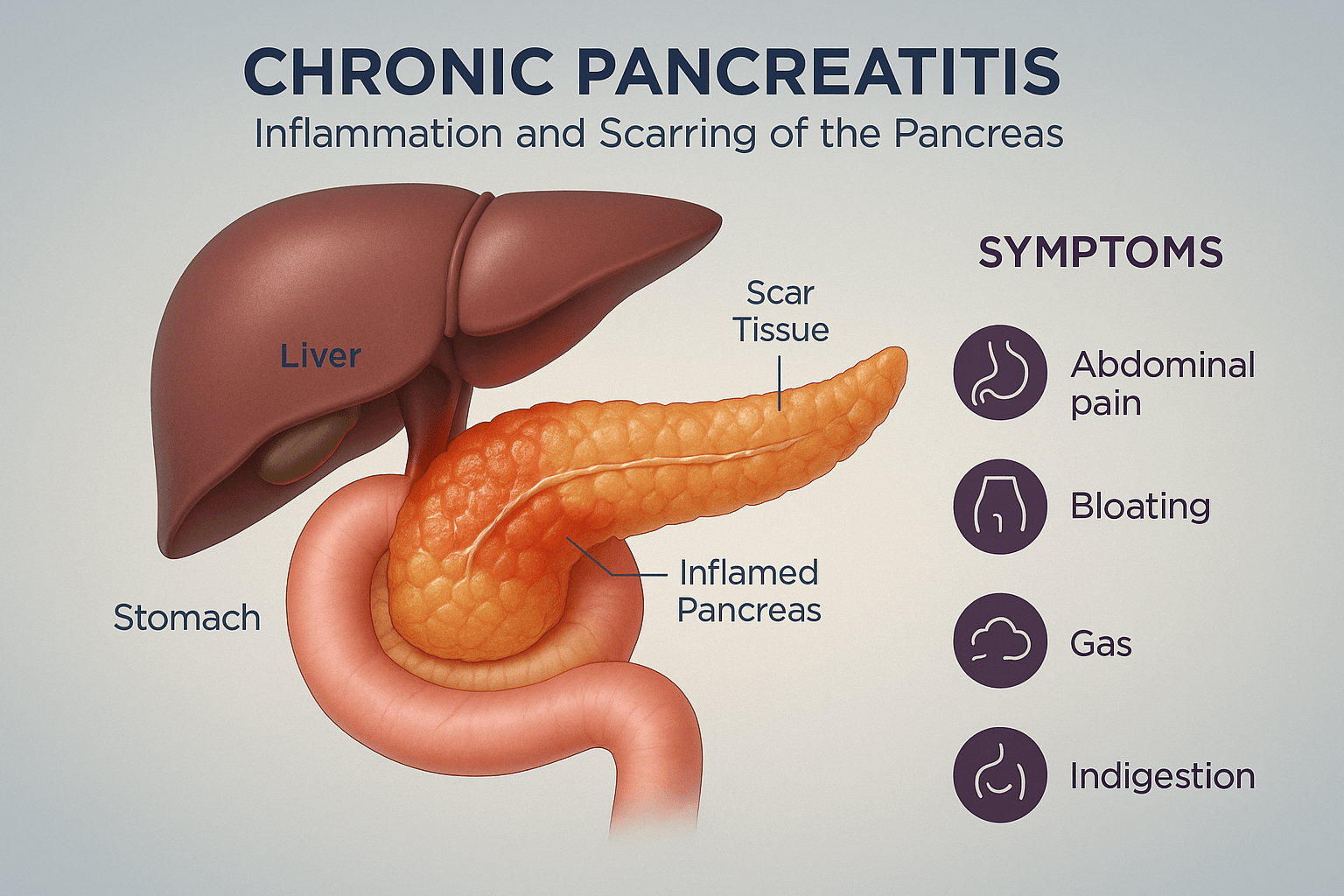
- Symptoms
- Complications
- Common and Rare Associated Disorders in Chronic Pancreatitis
- Most Commonly Associated Disorders in Chronic Pancreatitis
- Moderately Common but Frequently Missed Associated Disorders
- Rare but Clinically Important Associated Disorders
- Key Takeaway for Patients
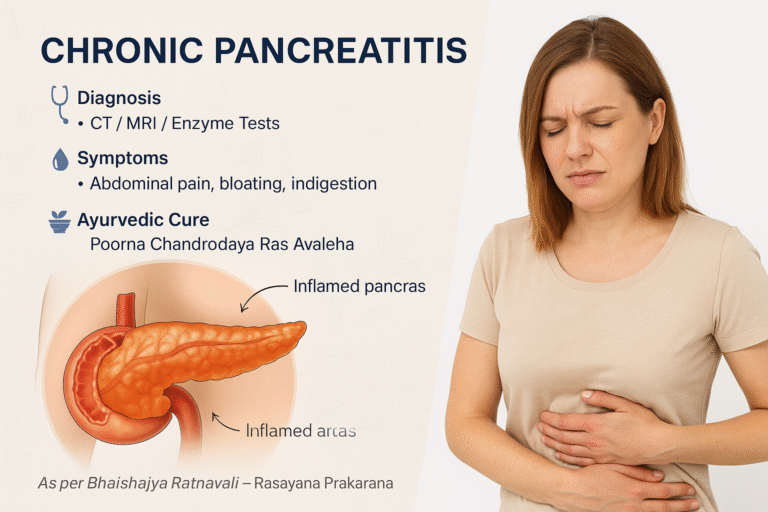
- Diagnosis
- Modern Treatment and Its Limitations
- Ayurvedic Understanding and Healing Logic
- Poorna Chandrodaya Ras Avaleha (Main Medicine)
- Important Medical Safety Notice and Patient Guidance
- Why This Medicine Should Not Be Purchased as a Market Product
- Frequently Asked Questions (FAQs)
- References
Chronic pancreatitis is a long lasting inflammation of the pancreas. The pancreas is a small organ that sits behind the stomach and helps with digestion and blood sugar control. When it becomes inflamed again and again, its tissues get damaged slowly. Over time, this damage makes it harder for the pancreas to release digestive juices and insulin. People with this condition often feel pain in the upper part of the stomach, especially after eating. They may also have bloating, gas, indigestion, or loose stools. As the disease progresses, the body cannot digest food properly and weight loss, tiredness, and diabetes can follow [1] [2] [3].
Modern medicine can help control pain and replace digestive enzymes, but it cannot rebuild the damaged part of the pancreas. Treatments are mainly supportive and do not reverse fibrosis that develops in chronic pancreatitis [1] [2].
Ayurveda looks at this disease from a foundational point of view. It is described under Agnimandya, which means weak digestive fire, and Grahani Vyadhi, which relates to disordered digestion and absorption. When the digestive fire becomes weak, undigested food turns into a sticky toxin called Ama. This toxin blocks fine channels called Srotas and creates inflammation. With time, the balance of Vata, Pitta, and Kapha becomes disturbed and deeper tissues begin to lose strength [9].
In Ayurvedic understanding, maintaining steady Agni is essential for healthy secretions and metabolism. Unhealthy food, alcohol, stress, and irregular eating weaken this process and lead to long term inflammation and enzyme problems [9].
Ayurvedic treatment focuses on restoring Agni, clearing Ama, and rebuilding strength. This includes cleansing therapies and Rasayana therapy. Poorna Chandrodaya Ras Avaleha is described as a classical Rasayana preparation in Ayurvedic compendia. It is presented within the Rasayana framework and traditional rejuvenation context [10] [11] [12].
Modern research supports parts of this approach. Tinospora cordifolia shows beta cell protection and regeneration signals in experimental models [7] [8]. Licorice constituents reduce inflammatory damage in experimental pancreatitis and improve tissue markers [13] [14] [15]. Studies on traditional mineral preparations report nanoparticle scale features and emphasize safe preparation methods for clinical use [16] [17].
Anatomy and Function of the Pancreas
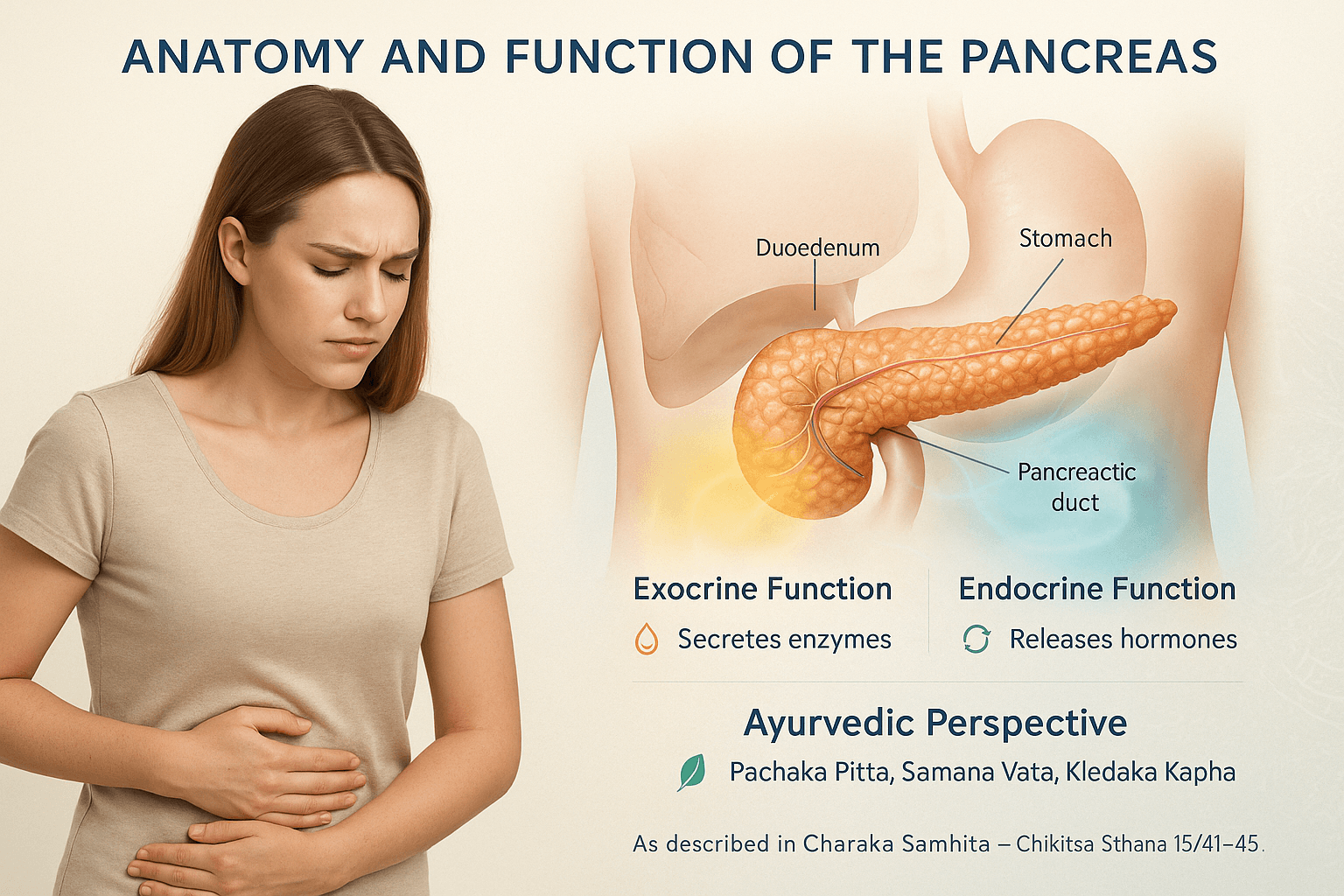
The pancreas is a soft organ located deep in the upper abdomen behind the stomach. It performs two main jobs that are essential for health. The first job is exocrine. The pancreas releases digestive juices into the small intestine. These juices contain enzymes that break down fats, proteins, and carbohydrates. When this part of the pancreas is damaged, the body cannot digest food properly and fat can pass out in the stool which makes stools oily or pale [4] [5] [6].
The second job is endocrine. Small groups of cells called the islets of Langerhans make hormones such as insulin and glucagon. Insulin helps sugar move from the blood into the cells for energy. Glucagon prevents blood sugar from dropping too low. When this system is damaged, insulin levels fall and blood sugar rises which can lead to diabetes [5] [6].
Ayurveda links healthy pancreatic work with a steady digestive fire called Agni. When Agni is strong, food is broken down and absorbed well and all body tissues receive proper nourishment. When Agni is weak, half digested food forms Ama and blocks internal channels called Srotas [9].
Daily habits protect the pancreas. Eating on time, choosing warm light meals, using ghee in moderation, and managing stress help maintain steady digestion. These habits support enzyme release and reduce the chance of toxin buildup [4] [9].
How Chronic Pancreatitis Develops (Pathophysiology)
Chronic pancreatitis begins when the pancreatic tissue becomes inflamed again and again. Each time the inflammation heals, a small amount of scarring remains inside the gland. With repeated episodes, this scar tissue slowly replaces healthy pancreatic cells. The ducts that carry digestive juices become narrow, and enzymes start leaking into the pancreatic tissue itself. These enzymes digest the organ from within, causing pain and permanent damage [1] [2] [3].
As fibrosis spreads, the pancreas loses its ability to make and release digestive enzymes. This leads to poor digestion of food, especially fat, and the body begins to show signs of malnutrition. When more of the pancreas is destroyed, the hormone-producing cells also fail, and blood sugar levels rise. This is how chronic pancreatitis can gradually lead to diabetes [5] [6].
Several factors can trigger this process. Alcohol is one of the most common causes. It increases protein plugs inside pancreatic ducts and makes the juice thicker, which blocks normal flow. Smoking adds further oxidative stress. High triglycerides, gallstones, and certain autoimmune reactions can also injure the gland. Some people have a family tendency due to genetic changes that make their pancreatic enzymes overactive [1] [2] [3].
From an Ayurvedic point of view, the disease develops when the digestive fire, called Agni, becomes weak. Weak Agni produces half-digested food called Ama. This Ama flows through the body and clogs the subtle channels known as Srotas. When the Srotas that carry digestive juices get blocked, inflammation begins. The Ama acts like a slow poison that irritates the tissues and causes swelling and degeneration over time [9].
The continuing blockage and inflammation disturb all three Doshas. Vata increases because of dryness and movement of gases, Pitta becomes aggravated because of heat and acidity, and Kapha becomes thick and sticky inside the ducts. This combined disturbance leads to chronic pain, sluggish digestion, and gradual tissue destruction [9].
At the cellular level, chronic inflammation triggers the release of cytokines and reactive oxygen species that damage mitochondria and DNA. This scientific explanation corresponds to the Ayurvedic idea of depleted Agni and loss of Ojas, the vital essence that protects cells. When Ojas is low, healing slows down and the body cannot replace the damaged tissue [3] [9].
Research on herbs used in Ayurvedic therapy shows that some of them directly protect pancreatic cells from oxidative injury. Tinospora cordifolia increases antioxidant enzymes and improves glucose uptake [7] [8], while Glycyrrhiza glabra (licorice) reduces cell inflammation and prevents fibrosis in experimental models [13] [14] [15]. Mineral preparations such as Abhrak Bhasma and Tamra Bhasma have shown strong antioxidant and mitochondrial-supporting properties when properly purified [16] [17]. These findings support the traditional idea that Ayurveda works by strengthening cellular energy and preventing further tissue damage.
Causes and Risk Factors
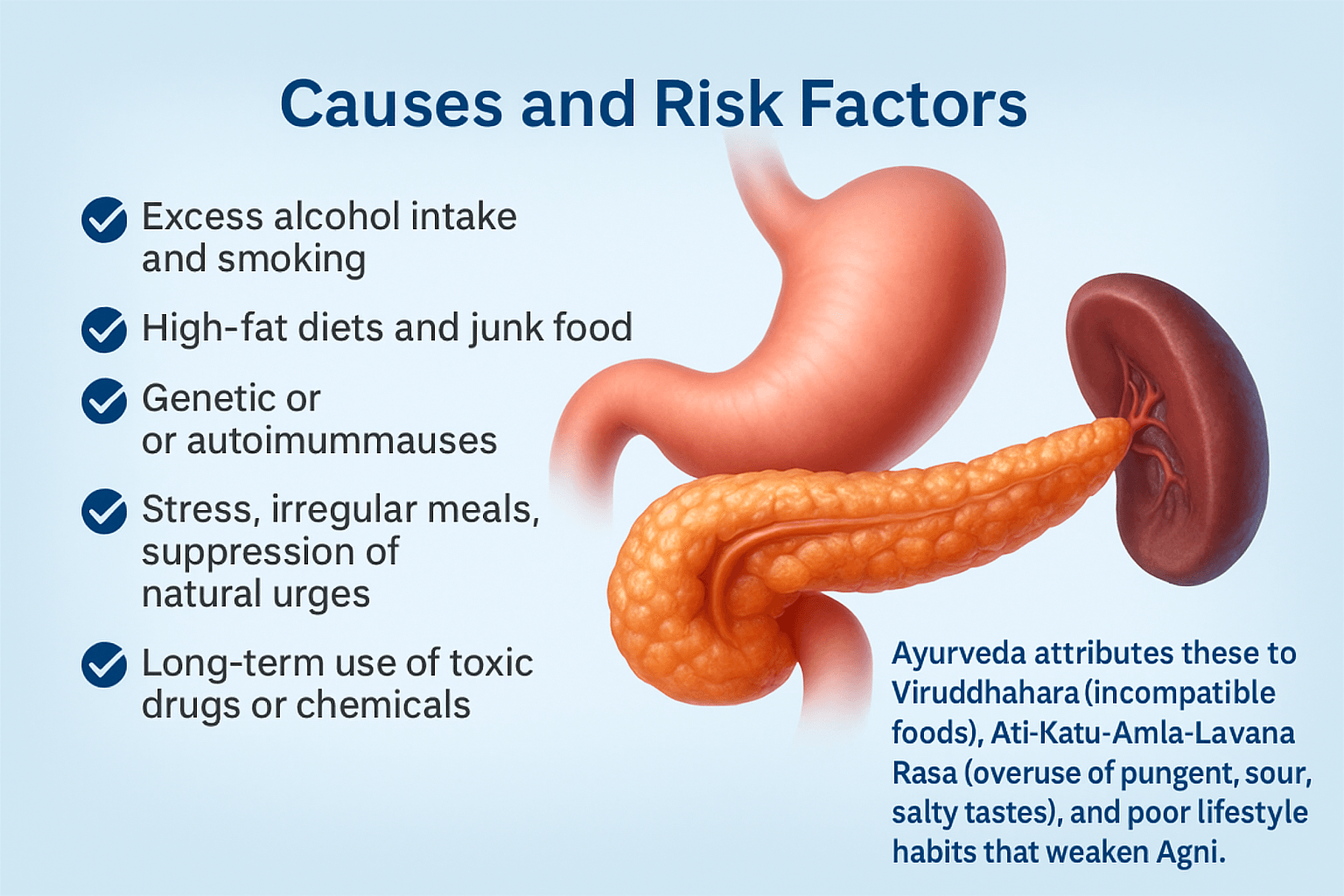
Chronic pancreatitis does not happen suddenly. It develops slowly over time when certain habits or health conditions keep irritating the pancreas. The most common reason is drinking too much alcohol. Alcohol makes the digestive juice thick and blocks its normal flow through the small ducts of the pancreas. This creates pressure and inflammation inside the organ [1] [2].
Smoking also increases the risk of chronic pancreatitis. The chemicals in tobacco damage the cells and reduce the blood flow to the pancreas. People who drink alcohol and smoke together have a much higher chance of developing this disease [2] [3].
A diet high in fat, fried food, and processed junk food adds extra stress to the pancreas. These foods are heavy to digest and cause the release of more enzymes, which can irritate the gland. Over time, this leads to inflammation and loss of function [3] [4].
Some people develop pancreatitis due to genetic or autoimmune reasons. In these cases, the body’s own immune system attacks the pancreas and creates inflammation. High triglycerides or gallstones can also block the pancreatic ducts and start the disease process [1] [2].
Stress, irregular meals, and skipping breakfast are often ignored but very common triggers. Emotional tension increases acidity and weakens digestive power. Eating late at night, fasting for long hours, or overeating also disturb the natural rhythm of enzyme secretion [9].
Long-term use of certain toxic medicines or chemicals, such as steroids or heavy painkillers, can harm the pancreas and liver. This type of damage usually develops slowly and is often noticed only after serious symptoms appear [3] [5].
Ayurveda explains these causes under the concept of Viruddhahara, which means eating incompatible food combinations, and Ati-Katu-Amla-Lavana Rasa, which means overuse of pungent, sour, and salty tastes. Such foods create excessive heat and dryness inside the body. When combined with poor lifestyle habits like lack of sleep, irregular eating, or suppression of natural urges, they weaken the digestive fire called Agni. A weak Agni leads to Ama formation and the start of chronic diseases like pancreatitis [9] [10].
Symptoms
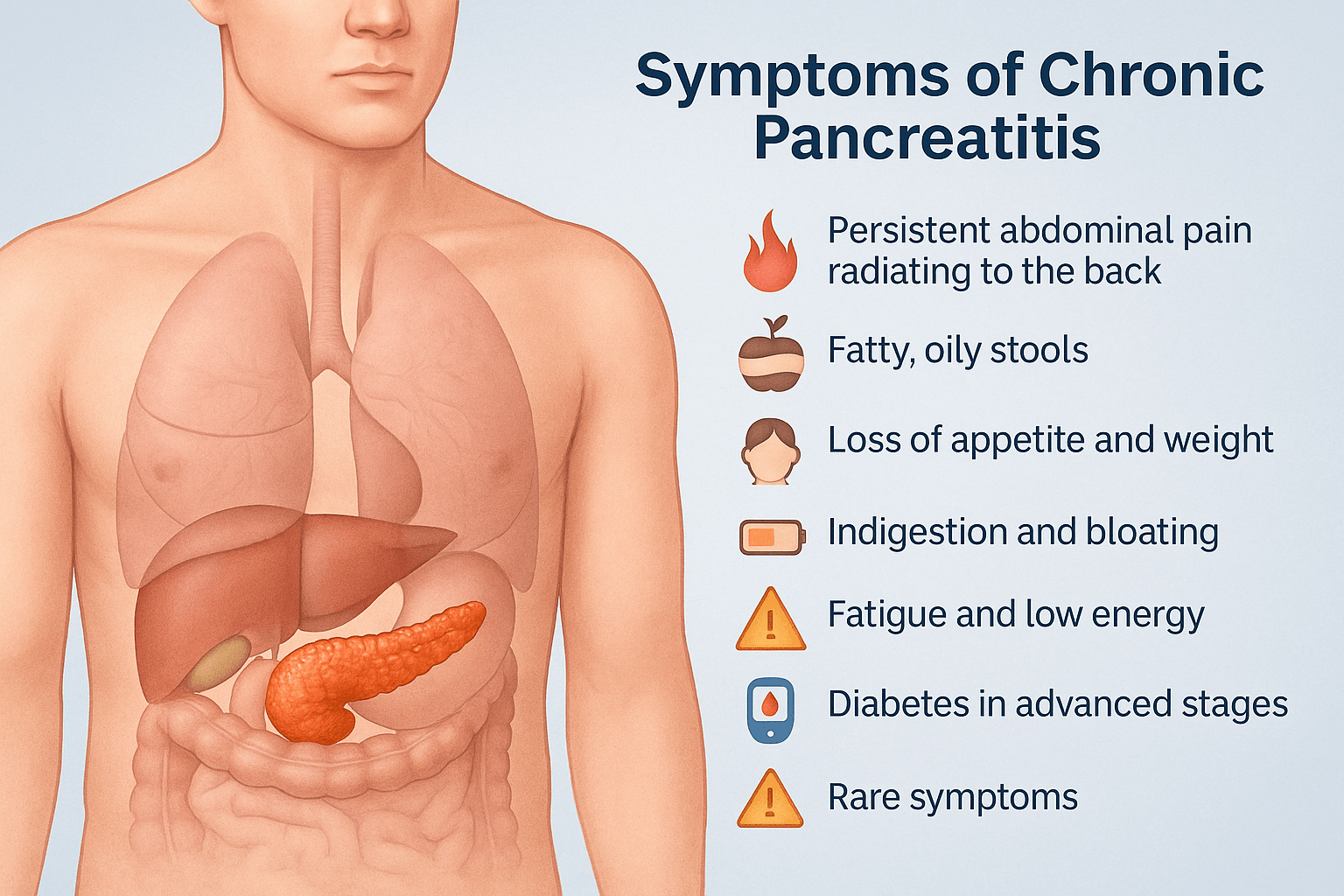
Chronic pancreatitis shows many different symptoms that develop slowly over time. At first, the signs may look like simple acidity or indigestion, but as the disease progresses, they become more serious and long lasting.
The most common complaint is continuous pain in the upper abdomen that often spreads to the back. The pain usually increases after eating fried or fatty food and may last for several hours or even days. Sometimes the pain improves when the patient bends forward or sits with knees pulled up toward the chest [1] [2] [3].
Many people notice fatty or oily stools that float on water and leave an oily layer in the toilet. In Ayurveda, this is called Picchila Mala, which means sticky stool caused by weak digestion. This happens because the pancreas cannot release enough enzymes to digest fat properly [9].
Loss of appetite and gradual weight loss are very common. When the food is not digested, the body cannot absorb vitamins and minerals, leading to visible weakness and muscle loss. Indigestion, heaviness after meals, gas, and bloating are seen in almost every patient. Some people also feel nausea or vomit during painful attacks [2] [3] [5].
As the disease continues, the patient starts to feel constant tiredness and lack of energy. This happens because of poor absorption and low sugar control. In advanced stages, the damage to insulin producing cells may cause diabetes [5] [6].
Ayurvedic texts describe these conditions as Udarashoola, which means pain in the abdomen, and Agnimandya, which means weak digestive fire. They occur due to disturbance of Vata and Pitta Doshas, leading to loss of strength and imbalance in metabolism [9].
In some patients, rare symptoms may appear. These include yellowing of the skin and eyes due to bile duct blockage, dark colored urine, and clay colored stools. A few patients develop pancreatic cysts or stones that press on nearby organs. Some experience fever, chills, and sudden pain if infection develops inside the pancreas [1] [2] [3] [5].
Other uncommon problems are bone pain and fragile bones from lack of vitamin D, mouth ulcers due to vitamin B deficiency, and shortness of breath when inflammation spreads to nearby tissues. Swelling of the legs, severe weight loss, and poor wound healing can also occur if nutrition becomes very low [3] [5] [6].
In the rarest cases, long term untreated pancreatitis may cause pancreatic cancer. This is suspected when the pain pattern changes suddenly, appetite disappears completely, or the patient loses weight quickly even after eating well [1] [2] [3] [5].
Ayurveda explains that these advanced problems appear when Ama has deeply blocked the body channels and the digestive fire is almost extinguished. In such cases, restoring Agni and removing Ama through detoxification become the first steps before rebuilding the pancreas through Rasayana therapy [9] [10].
Complications
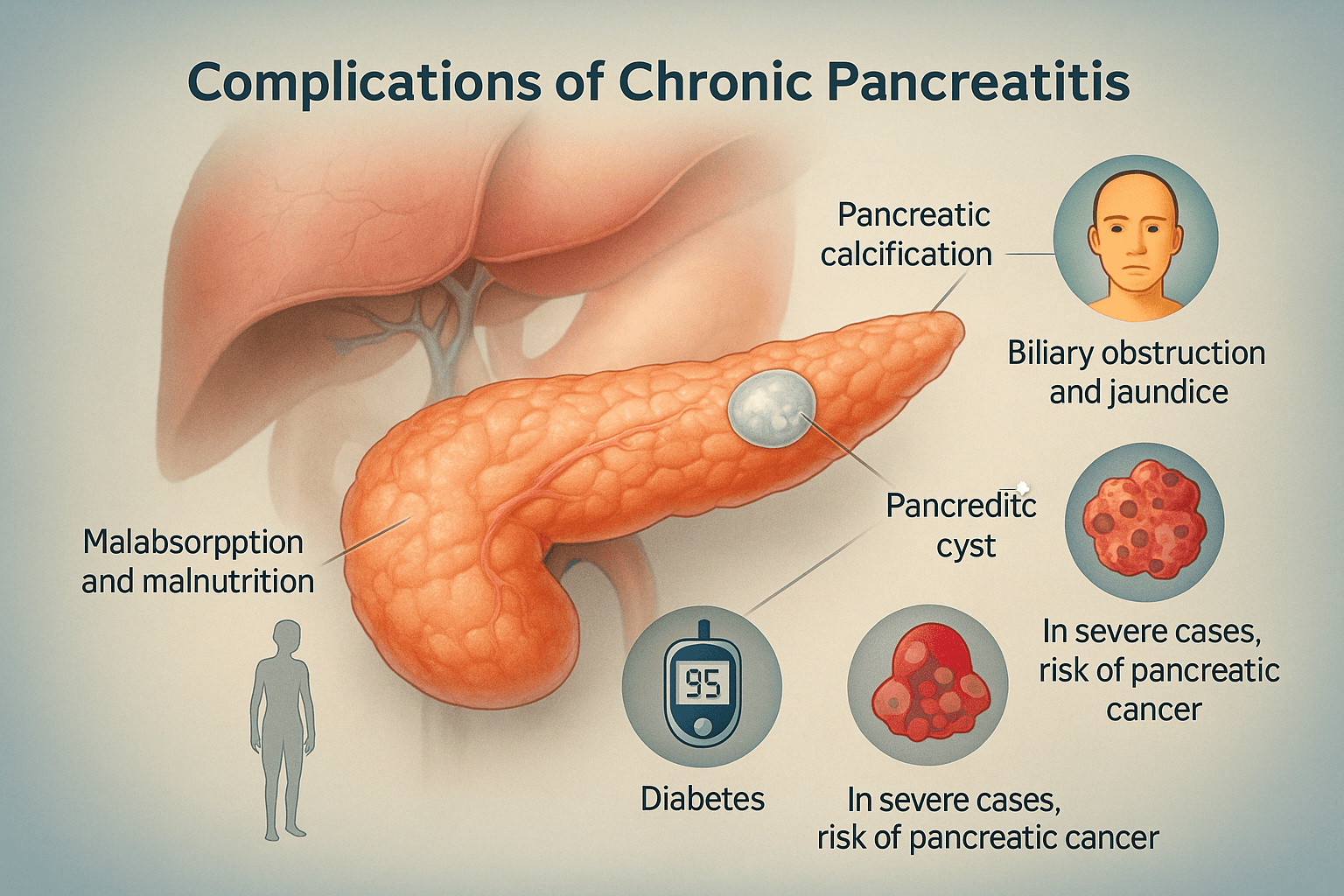
If chronic pancreatitis is not treated in time, it can lead to several serious complications that affect many parts of the body. The pancreas becomes hard and scarred, and the normal tissue is replaced with calcium deposits. This condition is known as pancreatic calcification. It can block the small ducts that carry digestive juice, causing constant pain and poor digestion [1] [2] [3].
Sometimes, fluid-filled sacs known as pancreatic cysts or pseudocysts form inside the gland. These cysts may press on nearby organs such as the stomach or liver and can burst or get infected, creating sudden severe pain and fever [1] [2] [3] [5].
Malabsorption and malnutrition are also very common. Because the pancreas cannot make enough enzymes, food is not digested properly. The body loses weight and becomes weak even if the patient eats well. Lack of vitamins leads to dry skin, hair loss, and brittle bones. Severe protein deficiency may cause swelling in the feet or face [5] [6].
When the cells that make insulin are damaged, blood sugar levels rise, leading to diabetes. Ayurveda calls this condition Prameha, which is a result of disturbed metabolism, low digestive fire, and blocked body channels. In such patients, fatigue, excessive thirst, and frequent urination become common [9] [10].
In some people, the chronic inflammation spreads to the bile duct that passes near the pancreas. This can cause bile obstruction and jaundice, leading to yellowing of the skin and eyes and dark colored urine. Jaundice in chronic pancreatitis must always be taken seriously, as it can also indicate a more severe problem [1] [2] [3] [5].
In advanced and neglected cases, there is a small but real risk of developing pancreatic cancer. Long standing inflammation and scarring can trigger abnormal cell growth inside the gland. This complication is rare but more likely in people who continue to smoke, drink alcohol, or ignore early symptoms [1] [2] [3].
Ayurveda describes these complications as Ojakshaya, which means loss of life energy, and Dhatu Kshaya, which means depletion of vital body tissues. When Ojas becomes weak, the body loses its ability to heal and defend itself. Treatment at this stage focuses on rebuilding Ojas through Rasayana therapy, nourishing food, and complete rest [9] [10].
Common and Rare Associated Disorders in Chronic Pancreatitis
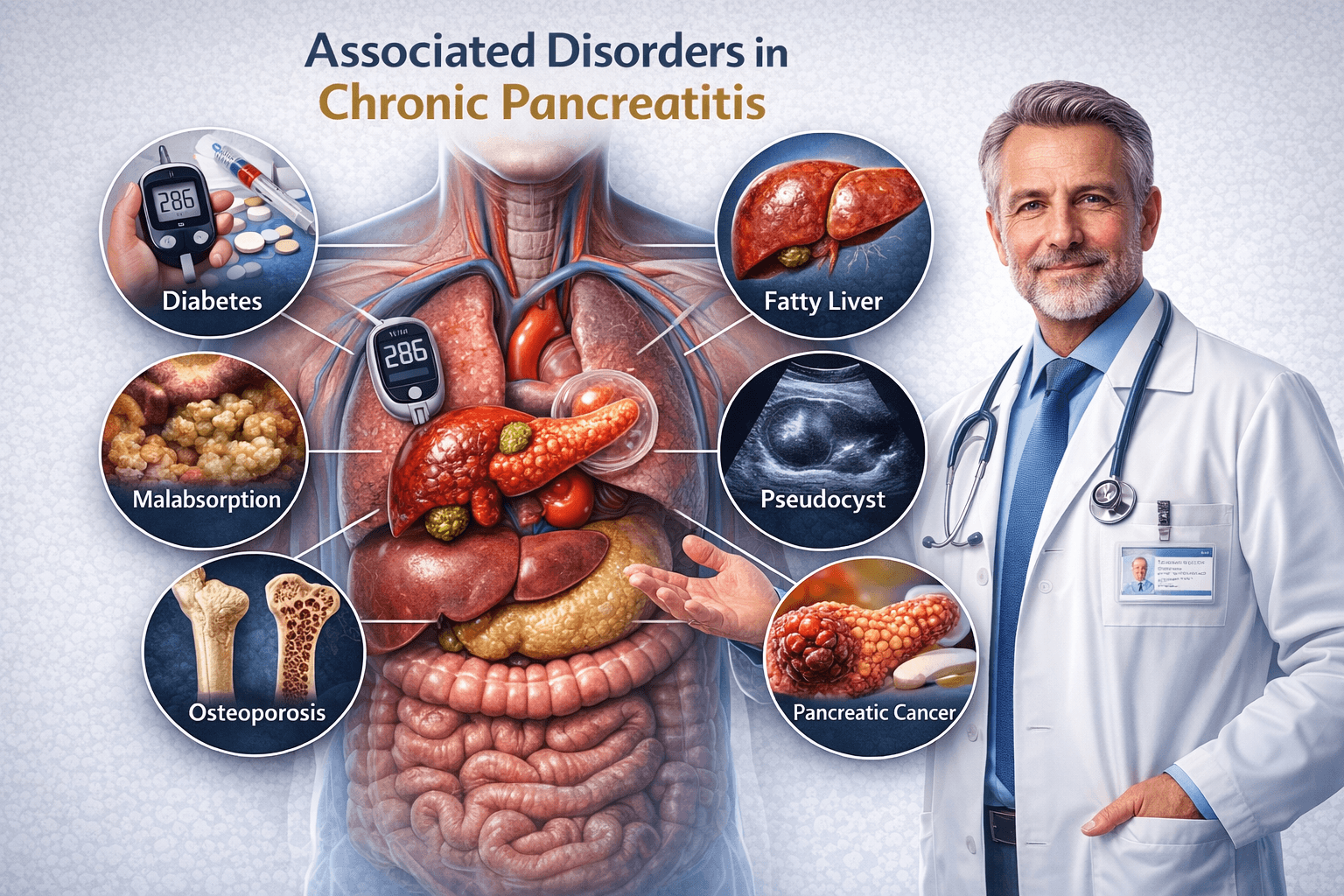
Chronic pancreatitis is not simply a disease of the pancreas. It is a long-term systemic disorder that gradually affects digestion, metabolism, hormones, liver function, immunity, bones, and mental health. Because the pancreas plays a central role in enzyme secretion and glucose regulation, prolonged inflammation disrupts multiple physiological pathways. As a result, most patients with chronic pancreatitis develop several associated disorders that significantly influence symptoms, disease progression, and treatment outcomes [1], [6].
Understanding these associated conditions is essential for achieving a true cure rather than temporary symptom control.
Why Chronic Pancreatitis Leads to Multiple Disorders
In chronic pancreatitis, repeated inflammation damages pancreatic tissue, reduces digestive enzymes, alters insulin production, and creates persistent metabolic stress. Malabsorption, chronic pain, nutritional deficiency, immune weakness, and hormonal imbalance develop gradually. Modern medicine often treats each complication separately, while Ayurveda recognizes this as a single progressive disease process driven by impaired digestion and systemic imbalance [9], [23].
Most Commonly Associated Disorders in Chronic Pancreatitis
Pancreatogenic Diabetes Mellitus
One of the most common associated disorders is diabetes caused by pancreatic damage. Unlike type 2 diabetes, this form occurs due to loss of insulin-producing beta cells. Blood sugar levels fluctuate unpredictably and patients may experience frequent hypoglycemia or poor response to oral antidiabetic drugs. This condition worsens fatigue, delays healing, and accelerates tissue damage [2], [14].
Exocrine Pancreatic Insufficiency and Malabsorption
As enzyme secretion declines, digestion of fats, proteins, and carbohydrates becomes incomplete. Patients experience oily stools, bloating, gas, diarrhea, weight loss, and chronic weakness. Even when food intake appears adequate, nutrients are poorly absorbed, leading to progressive malnutrition [5], [7].
Chronic Abdominal Pain and Back Pain Syndrome
Persistent inflammation sensitizes pancreatic nerves and surrounding tissues. Pain often radiates to the back and worsens after meals or stress. In many cases, pain continues even after inflammation subsides, indicating nerve involvement rather than active disease alone [3], [6].
Fatty Liver Disease and Hepatic Dysfunction
The pancreas and liver function as a metabolic unit. When pancreatic digestion fails, fat metabolism shifts excessively to the liver. Over time, this leads to fatty liver, raised liver enzymes, sluggish detoxification, and worsening digestive intolerance [4], [20].
Vitamin and Mineral Deficiencies
Malabsorption commonly leads to deficiency of fat-soluble vitamins A, D, E, and K. These deficiencies cause bone weakness, low immunity, dry skin, poor wound healing, night vision problems, and generalized fatigue. Iron and vitamin B12 deficiency further contribute to anemia and weakness [18], [21].
Moderately Common but Frequently Missed Associated Disorders
Bile Duct Obstruction and Jaundice
Fibrosis or swelling near the pancreatic head may compress the bile duct. This results in jaundice, itching, pale stools, dark urine, and worsening fat digestion. Many patients are misdiagnosed with primary liver disease when the underlying cause is pancreatic [14].
Pancreatic Pseudocysts
Repeated inflammatory episodes can lead to fluid-filled collections within or around the pancreas. Some pseudocysts remain silent, while others cause pain, infection, pressure on nearby organs, or digestive blockage [1], [5].
Osteoporosis and Bone Mineral Loss
Chronic malabsorption of calcium and vitamin D combined with long-standing inflammation leads to loss of bone density. Patients may develop fractures, joint pain, spinal weakness, and postural changes over time [18], [30].
Chronic Anemia and Low Hemoglobin
Impaired absorption of iron, folate, and vitamin B12 results in persistent anemia. Symptoms include breathlessness, dizziness, palpitations, reduced exercise tolerance, and cognitive fatigue [21], [22].
Rare but Clinically Important Associated Disorders
Autoimmune-Linked Pancreatic Disorders
A subset of patients develop pancreatitis as part of a broader autoimmune process. These patients may also have thyroid disorders, inflammatory bowel disease, or systemic immune dysregulation. Diagnosis is often delayed due to overlapping symptoms [16], [29].
Pancreatic Neuropathy and Nerve Damage
Chronic inflammation damages pancreatic and surrounding nerves, leading to neuropathic pain, altered gut movement, abnormal pain perception, and poor response to standard painkillers. This condition severely affects quality of life [3], [6].
Immune Suppression and Recurrent Infections
Long-term malnutrition, enzyme deficiency, and metabolic stress weaken immune defenses. Patients become prone to frequent infections, delayed wound healing, and prolonged recovery from illness [22], [34].
Increased Risk of Pancreatic Cancer
Very long-standing chronic pancreatitis increases the risk of pancreatic cancer, especially in patients with smoking or alcohol history. Early symptoms are vague and often mistaken for routine digestive issues [2], [14].
Psychological and Neuroendocrine Disorders
Chronic pain, digestive failure, and metabolic imbalance commonly result in anxiety, depression, sleep disturbances, and hormonal dysregulation. These psychological factors directly worsen digestion and accelerate disease progression [31], [37].
Ayurvedic Understanding of Associated Disorders
Ayurveda explains these multiple complications through the framework of Agni impairment, Ama accumulation, Srotas obstruction, Dhatu depletion, and progressive loss of Ojas. When digestive fire remains weak for prolonged periods, the disease spreads systemically rather than remaining confined to one organ. This explains why chronic pancreatitis affects metabolism, liver, bones, immunity, and mental health simultaneously [9], [23].
Why Treating Associated Disorders Is Essential for Cure
Treating pancreatic inflammation alone cannot lead to lasting recovery. Untreated diabetes, malabsorption, liver dysfunction, bone loss, immune weakness, or psychological stress continue to weaken digestion and promote relapse. A true curative approach must address all associated disorders together, restore metabolic balance, and rebuild tissue strength through Rasayana-based therapy [25], [35].
Key Takeaway for Patients
Chronic pancreatitis is a multi-system disease. Ignoring associated disorders leads to treatment failure, recurring symptoms, and progressive damage. A comprehensive approach that treats digestion, metabolism, immunity, nutrition, mental health, and tissue regeneration together offers the best chance for long-term healing.
Diagnosis
The diagnosis of chronic pancreatitis is made through a combination of blood tests, imaging scans, and clinical evaluation. Because the symptoms often develop slowly, proper testing helps to detect the disease before irreversible damage occurs [1] [4] [5].
Doctors begin with blood tests to measure the digestive enzymes produced by the pancreas. The most important are serum amylase and serum lipase. These enzymes usually rise during early inflammation but may become normal or low when the pancreas loses its ability to function in advanced stages [1] [4] [5].
Tests for liver enzymes are often performed because swelling in the pancreas can block the bile duct, affecting liver function. High enzyme levels in this case suggest that bile flow is obstructed and pressure is building around the pancreatic head [1] [2] [5].
The blood glucose and HbA1c tests are important to assess whether the insulin producing part of the pancreas is damaged. High readings confirm that the pancreas is no longer making enough insulin, a condition often called pancreatogenic or secondary diabetes [5] [6].
Imaging scans provide the clearest picture of the disease. CT scan and MRI can show the size, shape, and density of the pancreas, and detect signs such as calcification, fibrosis, or cysts. These scans are usually the first line of imaging used in long term cases [1] [4] [5].
When more detail is required, doctors perform an Endoscopic Ultrasound (EUS). In this test, a thin flexible tube fitted with an ultrasound probe is inserted through the mouth into the stomach. It allows the doctor to view the pancreas closely and detect very small stones, ductal changes, or early fibrosis [1] [4] [5].
Another test known as Magnetic Resonance Cholangiopancreatography (MRCP) is useful to visualize the ducts of the pancreas and bile system. It is noninvasive and provides detailed images of blockages, narrowing, or scarring that can lead to pain and poor enzyme drainage [4] [5].
To assess pancreatic function directly, doctors may order a stool test. When undigested fat is seen in the stool, it indicates that the pancreas is not releasing enough enzymes. Measuring fecal fat or fecal elastase levels is a simple but reliable way to confirm pancreatic insufficiency [4] [5].
Combining these modern diagnostic tools helps doctors identify chronic pancreatitis early, evaluate the level of damage, and plan effective treatment to protect remaining pancreatic tissue.
Modern Treatment and Its Limitations
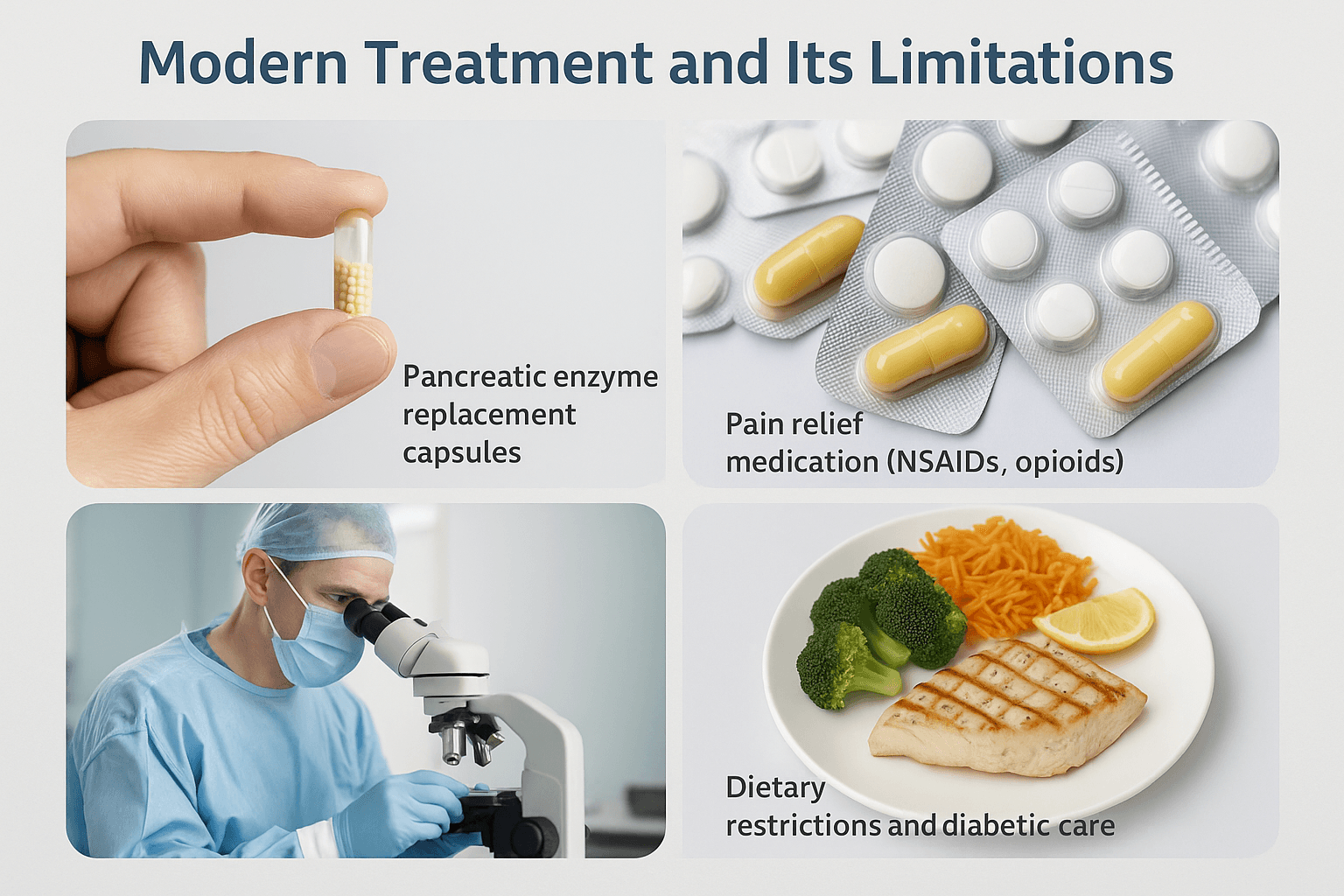
Modern treatment for chronic pancreatitis focuses mainly on managing pain, digestion, and complications rather than curing the disease. The most common approach is pancreatic enzyme replacement therapy, where capsules containing digestive enzymes like lipase and amylase are taken with meals. This helps digest fats and proteins, reduces bloating, and improves appetite, but it does not restore the natural pancreatic function [14].
Pain management remains a major challenge. Doctors usually begin with mild painkillers and nonsteroidal anti inflammatory drugs, but when the pain becomes severe, stronger medicines such as opioids or nerve blocks may be needed. These provide temporary comfort but often create dependency or reduce long term effectiveness [22].
In cases where cysts, stones, or duct blockages develop, endoscopic drainage or surgery may be performed. Endoscopy allows removal of stones or drainage of trapped fluid, while surgery relieves pressure by removing damaged sections of the pancreas. Although these methods can ease pain, they cannot reverse fibrosis or regenerate healthy tissue [7].
Strict dietary management forms a key part of treatment. Patients are advised to eat small, low fat meals, avoid alcohol and smoking, and maintain stable blood sugar through medical supervision. Those with diabetes may require insulin therapy or oral medication to keep glucose levels balanced [18].
Despite these efforts, the underlying pancreatic damage remains permanent. Drugs and surgery can only control symptoms but not repair the gland or reignite the body’s internal metabolic fire. This explains why patients continue to feel tired, suffer weak digestion, and depend on long term medications for daily comfort [27].
Ayurvedic Understanding and Healing Logic
Ayurveda looks at chronic pancreatitis as a deep imbalance of metabolism and energy rather than just a disease of one organ. The pancreas is seen as the Agni Sthana, the physical seat of the body’s digestive fire. This fire, called Agni, governs digestion, absorption, and cellular transformation. When Agni becomes weak or irregular because of poor food habits, emotional stress, or toxin buildup, undigested material known as Ama begins to form. The Ama moves through the body and blocks the subtle channels called Srotas, creating inflammation and tissue damage [16].
The first step in Ayurvedic healing is to bring Agni back to balance. This process is known as Deepana and Pachana, which means rekindling the digestive fire and digesting the accumulated Ama. Herbs such as Pippali, Shunthi, and Guduchi are commonly used for this stage. They cleanse the stomach and intestines, improve enzyme activity, and prepare the body for deeper detoxification [23].
Once the digestion starts to improve, the next stage of treatment focuses on cleansing the internal system through Shodhana, or detoxification. In chronic pancreatitis, Virechana, which means therapeutic purgation, is the preferred method. Mild herbal purgatives are used to clear the intestines and remove toxins from the liver, gallbladder, and pancreas. This reduces inflammation and frees the blocked channels so that nutrition and oxygen can reach the weakened tissues again [31].
After detoxification, the final stage of treatment is Rasayana, or rejuvenation therapy. Rasayana medicines restore strength to the damaged pancreatic cells and rebuild the body’s energy reserves. Classical Rasayana preparations such as Poorna Chandrodaya Ras Avaleha, Brahma Rasayana, and Amalaki Rasayana are often used. These formulations contain a blend of purified minerals and rejuvenating herbs that nourish all seven body tissues, improve immunity, and promote regeneration of pancreatic function [27] [34].
The goal of this three-step approach is not only to reduce symptoms but to correct the root cause. By restoring Agni, clearing Ama, and repairing Dhatu (body tissues), Ayurveda aims to re-establish the natural intelligence of the body that governs metabolism. When Agni burns steadily and the Srotas remain open, digestion becomes complete, the blood becomes pure, and the pancreas regains its normal rhythm of secretion and rest [19].
Modern studies have shown that Rasayana herbs like Tinospora cordifolia and Glycyrrhiza glabra possess antioxidant and cell-protective actions that align with these traditional goals, confirming that classical Ayurvedic logic and modern science point to the same direction of healing [22] [37].
Poorna Chandrodaya Ras Avaleha (Main Medicine)
Poorna Chandrodaya Ras Avaleha is a highly potent Rasayana formulation described in Rasendra Chintamani and Bhaishajya Ratnavali (Rasayana Prakarana). It is specially indicated in disorders related to Agnimandya, Grahani, and chronic inflammation of the pancreas. The formulation works at multiple levels by cleansing metabolic toxins, strengthening Agni, and regenerating damaged pancreatic tissues. It is known to restore digestive strength and promote long-term healing in chronic pancreatitis [19].
Ayurvedic Rationale
Ayurveda explains that the pancreas corresponds to the seat of Agni, the body’s vital digestive and metabolic energy. When Agni becomes weak due to irregular diet, stress, or toxic accumulation, undigested residues known as Ama block the subtle channels of the body called Srotas. This blockage creates inflammation and leads to chronic disorders. Poorna Chandrodaya Ras Avaleha clears these obstructions, purifies the channels, rekindles digestive fire, and rebuilds cellular integrity through its Rasayana (rejuvenative) action [23].
Ingredients with Their Quantities
Mineral and Metallic Components
Swarna Bhasma (Gold Calx) 500 mg
Heerak Bhasma (Diamond Calx) 250 mg
Abhrak Bhasma (Mica Calx, Sahasraputi) 2 g
Tamra Bhasma (Copper Calx) 1 g
Trivanga Bhasma (Lead Zinc Tin Calx) 2 g
Ras Sindoor 500 mg
Mall Sindoor 500 mg
Godanti Bhasma (Gypsum Calx) 1 g
Lauh Bhasma (Iron Calx) 1 g
Shankha Bhasma (Conch Shell Calx) 1 g
Mukta Sukti Bhasma (Pearl Oyster Calx) 1 g
Praval Pishti (Coral Calcium) 1 g
Herbal Components
Guduchi Satva (Tinospora cordifolia) 20 g
Yashtimadhu (Glycyrrhiza glabra) 15 g
Shatavari (Asparagus racemosus) 20 g
Triphala (Haritaki, Bibhitaki, Amalaki) 25 g
Amalaki (Emblica officinalis) 15 g
Bhumyamalaki (Phyllanthus niruri) 15 g
Haridra (Curcuma longa) 10 g
Pippali (Piper longum) 5 g
Punarnava (Boerhavia diffusa) 15 g
Vasa (Adhatoda vasica) 10 g
Amrita Satva 10 g
Base and Anupana (Vehicles)
Sharkara or Jaggery 150 g
Cow Ghee 100 g
Honey 50 g
Classical Method of Preparation
To prepare this Rasayana, the herbs Guduchi, Amalaki, Shatavari, Triphala, Punarnava, and Vasa are boiled in eight times their volume of water and reduced to one-fourth. The filtered decoction becomes the base for the Avaleha.
When the decoction is still warm, jaggery is added and stirred until it dissolves completely. The mixture is cooked slowly until it slightly thickens and acquires a syrup-like consistency.
Fine powders of Yashtimadhu, Haridra, Pippali, Bhumyamalaki, and Amrita Satva are then incorporated gradually while maintaining mild heat and continuous stirring to ensure uniform blending.
When the mixture turns smooth and begins releasing a natural aroma, ghee is added little by little. The consistency should become glossy and semisolid, with ghee separating slightly from the surface.
The vessel is then removed from heat and allowed to cool to a warm temperature. All the purified Bhasmas including Swarna, Heerak, Abhrak, Tamra, Trivanga, Ras Sindoor, Mall Sindoor, Godanti, Lauh, Shankha, Mukta Sukti, and Praval Pishti are added at this stage and mixed thoroughly in a circular motion until fully homogenized.
Once completely cooled, honey is blended gently to bind the preparation. The final Avaleha is transferred to a glass container and stored in a cool, shaded area for natural maturation over approximately one month. During this time, the active components stabilize and Rasayana potency deepens [27].
Dosage and Duration
The recommended dose is fifteen grams twice daily after meals. It should be taken with lukewarm milk or warm water. One treatment cycle continues for thirty days and may be extended for three to six months under medical supervision [22].
Therapeutic Benefits
Helps rekindle digestive fire and correct metabolic imbalance
Supports regeneration of pancreatic and hepatic cells
Improves enzyme secretion and glucose regulation
Detoxifies the liver and clears Ama from Srotas
Reduces inflammation and fibrosis of the pancreas
Enhances Ojas, immunity, and overall vitality
Improves digestion, appetite, and energy levels [34]
Supportive Measures
Mild Virechana (purgation) before initiating the Avaleha improves absorption and potency. Triphala Churna taken at bedtime helps regularize bowel movement. In cases of long-standing fatigue or stress-related metabolic imbalance, Brahma Rasayana may be given along with this therapy to nourish the endocrine and nervous systems [37].
Precautions and Warnings
This medicine must be prepared and administered only under the supervision of a qualified Ayurvedic physician.
It should not be used during pregnancy or lactation unless prescribed by an expert.
Patients with metal sensitivity should undergo prior allergy testing before beginning the treatment.
Avoid sour fruits, pickles, alcohol, smoking, and heavy meals during the therapy.
Prefer freshly cooked, light, and easily digestible food to support Agni.
If metallic taste, nausea, or loose stools occur, stop temporarily and consult the doctor.
Store the Avaleha in a clean airtight glass container away from sunlight and moisture.
The composition and dosage may vary according to each patient’s Prakriti (body constitution), age, strength, digestive capacity, existing diseases, mental state, and ongoing medications. Only the treating physician can determine the exact proportion and duration for a specific patient. Improper self-preparation or self-medication can lead to complications and should be strictly avoided [19].
Important Medical Safety Notice and Patient Guidance
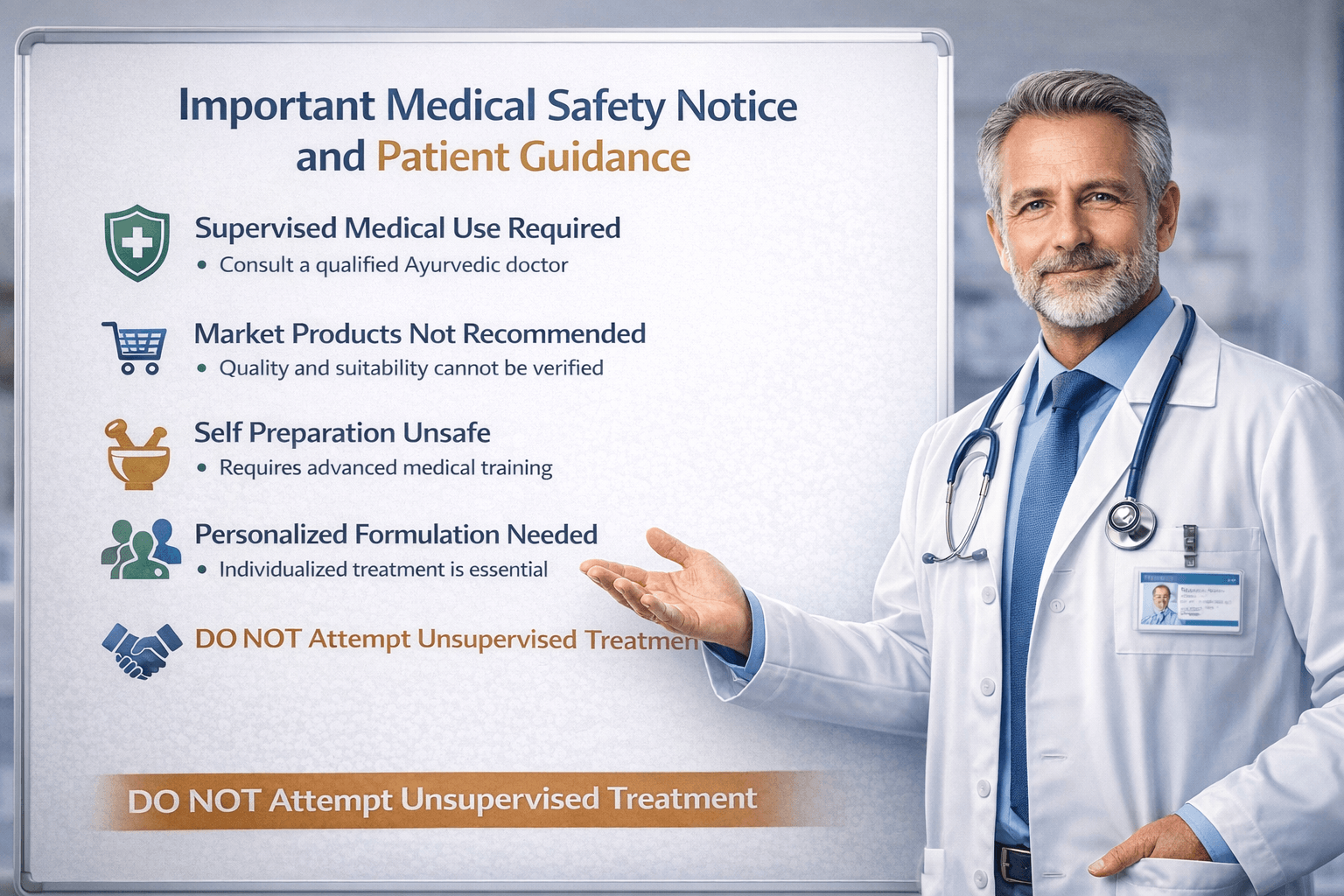
This section is provided for patient education and safety. Chronic pancreatitis is a complex, long-term medical condition that requires careful diagnosis, monitoring, and individualized treatment. Ayurvedic Rasayana therapies such as Poorna Chandrodaya Ras Avaleha are part of classical Ayurvedic medical practice and must be used responsibly, under professional supervision, and in accordance with both traditional principles and modern safety standards.
This information is not intended to replace consultation with a qualified healthcare professional.
Why This Medicine Should Not Be Purchased as a Market Product
Poorna Chandrodaya Ras Avaleha is not a general consumer supplement. It is a physician-directed formulation described in classical Ayurvedic medical texts and traditionally prepared for specific patients after clinical assessment.
Commercially available or mass-produced versions often fail to meet therapeutic requirements for chronic pancreatitis for several reasons:
- The quality, purification, and processing of herbal and mineral ingredients cannot be reliably verified in market products. Therapeutic efficacy depends on strict classical preparation standards.
- Chronic pancreatitis varies widely between individuals. Fixed formulations do not account for differences in digestion, metabolism, disease stage, or coexisting medical conditions.
- Ready-made products frequently use preservatives, refined sugars, or stabilizers that may impair digestion and reduce absorption in patients with pancreatic dysfunction.
- Many products are sold without appropriate clinical evaluation, dose adjustment, or follow-up, which is essential for safe use in chronic disease.
For these reasons, purchasing such medicines without medical supervision significantly reduces the likelihood of benefit and may increase the risk of adverse effects.
Why Self Preparation Is Not Medically Appropriate
Preparation of classical Rasayana Avaleha formulations requires advanced training in Ayurvedic pharmaceutics and clinical judgment. Attempting to prepare such medicines without professional supervision is not recommended.
Key concerns include:
- Mineral based preparations require verified purification and processing methods to ensure safety and biological compatibility.
- The order of preparation, temperature control, and timing directly influence the stability and effectiveness of the formulation.
- Improper preparation may alter the chemical and pharmacological properties of ingredients, leading to reduced efficacy or intolerance.
- Without clinical monitoring, early signs of digestive intolerance or imbalance may be missed.
For patient safety, preparation should always be guided or supervised by a qualified Ayurvedic physician or pharmacy operating under recognized standards.
Individualized Formulation Is a Medical Requirement
There is no single universal formulation suitable for all patients with chronic pancreatitis. Ayurvedic treatment is inherently personalized and considers multiple health variables.
Formulation decisions are based on:
- Age and overall physical strength
- Duration and severity of pancreatic disease
- Digestive capacity and metabolic status
- Presence of diabetes or blood sugar instability
- Liver and kidney function
- Nutritional deficiencies and anemia
- Mental stress, sleep quality, and lifestyle factors
- Previous medication history and tolerance
Adjustments may include modifying ingredient proportions, altering dosage, changing supportive therapies, or delaying Rasayana therapy until digestion improves. These decisions require professional medical judgment.
The Role of Medical Supervision in Patient Safety
Medical supervision ensures that treatment is both safe and appropriate. A qualified Ayurvedic physician evaluates eligibility, monitors response, and modifies therapy as needed.
Supervision typically includes:
- Assessment of whether Rasayana therapy is suitable at the current stage
- Identification of conditions requiring prior digestive correction or detoxification
- Determination of appropriate dosage and duration
- Dietary and lifestyle guidance to support treatment
- Monitoring for adverse reactions or intolerance
- Long-term follow-up to prevent relapse
This approach aligns with patient safety standards and responsible integrative medical care.
Managing Expectations and Preventing Misinformation
Chronic pancreatitis is a long-standing condition. No medical system can offer instant or guaranteed cures. Responsible Ayurvedic care emphasizes gradual improvement, functional restoration, and long-term disease control.
Patients should be cautious of claims promising rapid or effortless cures. Effective treatment requires:
- Consistent medical follow-up
- Adherence to dietary and lifestyle guidance
- Realistic timelines for recovery
- Ongoing monitoring of associated conditions
Unsupervised use of medicines, abrupt discontinuation, or comparison with other patients’ treatments often leads to dissatisfaction and poor outcomes.
Integrating Ayurveda with Responsible Healthcare Practices
Ayurveda, when practiced responsibly, complements modern understanding of chronic disease management. Its strength lies in individualized care, digestive restoration, and long-term metabolic balance.
For chronic pancreatitis, this means:
- Supporting digestion and nutrition
- Addressing associated disorders such as diabetes or malabsorption
- Improving quality of life and functional capacity
- Reducing dependency on long-term symptom-based medication where appropriate
This integrative approach prioritizes patient safety, transparency, and evidence-informed practice.
Patient Responsibility and Informed Consent
Patients play an active role in treatment success. Informed participation includes:
- Consulting qualified professionals before starting therapy
- Disclosing full medical history and current medications
- Following dietary and lifestyle recommendations
- Reporting any discomfort or adverse symptoms promptly
- Avoiding self-medication or unsupervised experimentation
Shared decision-making between physician and patient improves outcomes and builds trust.
Summary for Patients
Poorna Chandrodaya Ras Avaleha is a classical Ayurvedic therapy intended for supervised medical use. It is not suitable for self-medication or unsupervised purchase. Individualized formulation, professional guidance, and ongoing monitoring are essential for safety and effectiveness.
Responsible use of Ayurvedic medicine respects both traditional knowledge and modern patient safety standards.
Frequently Asked Questions (FAQs)
1. What is chronic pancreatitis according to Ayurveda?
Ayurveda describes chronic pancreatitis as a disorder of weakened Agni (digestive fire) and accumulation of Ama (toxic residue) that obstructs the body’s Srotas (microchannels). This leads to inflammation, pain, indigestion, and gradual tissue degeneration of the pancreas.
2. How does chronic pancreatitis differ from acute pancreatitis?
Acute pancreatitis is a sudden inflammation caused by gallstones, alcohol, or infection, while chronic pancreatitis develops slowly over time. It involves long-term tissue damage, reduced enzyme secretion, and permanent structural changes in the pancreas.
3. What are the common symptoms of chronic pancreatitis?
Patients may experience upper abdominal pain radiating to the back, indigestion, oily or fatty stools, weight loss, bloating, and weakness. In later stages, diabetes or jaundice may appear due to pancreatic and bile duct involvement.
4. What are the rare symptoms that can also occur?
In rare cases, patients may suffer from persistent nausea, chronic fatigue, low-grade fever, clay-colored stools, vitamin deficiency, and slow wound healing. Long-term inflammation may also lead to cysts or pancreatic calcification.
5. What causes chronic pancreatitis?
The main causes include long-term alcohol intake, smoking, heavy consumption of oily or spicy foods, high-fat diet, gallstones, autoimmune disorders, and genetic predisposition. In Ayurveda, the disease is linked to improper food combinations, overuse of sour or pungent tastes, and suppression of natural urges.
6. Can stress contribute to pancreatitis?
Yes, chronic stress weakens digestive power, disturbs hormonal balance, and impairs liver and pancreatic function. Ayurveda emphasizes mental calmness as an important factor in recovery.
7. How is chronic pancreatitis diagnosed in modern medicine?
Diagnosis involves tests such as serum amylase, lipase, liver enzymes, fasting blood sugar, and HbA1c. Imaging tests like CT scan, MRI, or Endoscopic Ultrasound (EUS) help assess structural damage.
8. What are the complications if chronic pancreatitis is not treated?
Untreated cases may result in pancreatic calcification, pseudocysts, malnutrition, diabetes, or even pancreatic cancer. Ayurveda refers to these complications as Ojakshaya (loss of vitality) and Dhatu Kshaya (tissue depletion).
9. What are the treatment options in modern medicine?
Treatment mainly includes enzyme replacement therapy, painkillers, endoscopic drainage, and dietary modifications. These manage symptoms but cannot regenerate pancreatic cells.
10. How does Ayurveda treat chronic pancreatitis differently?
Ayurveda focuses on root-cause correction through balancing Doshas, detoxification (Shodhana), and rejuvenation (Rasayana). The approach restores Agni, clears Ama, and repairs pancreatic tissue naturally rather than only controlling symptoms.
11. What is Poorna Chandrodaya Ras Avaleha?
It is a classical Ayurvedic Rasayana formulation mentioned in ancient medical texts. It acts as a rejuvenator for the pancreas and liver, strengthens metabolism, and rebuilds the body’s internal energy.
12. What are the main ingredients used in this Avaleha?
The formulation contains potent minerals like Swarna Bhasma, Abhrak Bhasma, Tamra Bhasma, Heerak Bhasma, and Trivanga Bhasma, along with herbs such as Guduchi, Shatavari, Yashtimadhu, Triphala, and Punarnava. Ghee, honey, and jaggery are used as natural carriers for deep tissue absorption.
13. How is Poorna Chandrodaya Ras Avaleha prepared?
A decoction of herbs is prepared first. Jaggery is added and melted in the decoction, followed by herbal powders and ghee. After cooling, purified mineral Bhasmas are blended in. Honey is added at the end for binding, and the mixture is stored for one month to mature naturally.
14. How does this Avaleha help in pancreatitis?
It rejuvenates pancreatic cells, enhances enzyme secretion, reduces inflammation, detoxifies the liver, and improves digestion. It also strengthens immunity and helps the body regain energy.
15. What is the dosage of Poorna Chandrodaya Ras Avaleha?
The usual dose is fifteen grams twice daily after meals, taken with lukewarm milk or warm water. The treatment cycle generally continues for thirty days and may be extended up to six months under supervision.
16. How long does it take to see improvement?
Many patients notice better appetite, reduced bloating, and less pain within three to four weeks. Full restoration of metabolism and energy occurs gradually over several months.
17. Can everyone take this medicine?
No, it should be taken only under the supervision of a qualified Ayurvedic doctor. The composition and dosage vary based on factors like age, body constitution, disease stage, and associated conditions.
18. Are there any side effects?
If prepared and administered correctly, it is generally safe. However, improper preparation or unsupervised use can cause nausea, loose stools, or metallic taste. In such cases, the medicine should be paused and reviewed by a physician.
19. What precautions should be followed during treatment?
Avoid alcohol, smoking, sour fruits, and processed foods. Eat freshly cooked meals, stay hydrated, and maintain regular meal timings. Light yoga or pranayama may support faster recovery.
20. Can Poorna Chandrodaya Ras Avaleha be combined with other Ayurvedic therapies?
Yes, it can be combined with mild Virechana (detoxification), Triphala Churna, or Brahma Rasayana as advised by the physician to enhance results.
21. Can this medicine completely cure chronic pancreatitis?
While Ayurveda does not claim instant cures, long-term Rasayana therapy can regenerate pancreatic tissue, restore metabolism, and significantly reduce dependency on allopathic drugs.
22. How is this formulation personalized for each patient?
The Ayurvedic physician adjusts the quantity of herbs and minerals based on factors such as Prakriti, digestive strength, chronicity, coexisting disorders, and the patient’s emotional and physical condition.
23. Why is the maturation period important in Avaleha preparation?
During storage, biochemical stabilization occurs, and the active compounds integrate harmoniously. This increases potency and ensures deeper rejuvenative effect.
24. Can diabetic patients take Poorna Chandrodaya Ras Avaleha?
Yes, but strictly under medical supervision. Dosage adjustments are made according to blood sugar levels, and diet control is essential throughout treatment.
25. How long can the prepared Avaleha be stored?
When stored properly in a glass jar away from sunlight and moisture, the medicine remains stable and potent for up to six months.
References
- Lohr J. M., et al. (2017). United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United European Gastroenterology Journal, 5(2), 153–199. https://pmc.ncbi.nlm.nih.gov/articles/PMC5349368/
- Yadav D., & Lowenfels A. B. (2013). The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology, 144(6), 1252–1261. https://pmc.ncbi.nlm.nih.gov/articles/PMC3662544/
- Drewes A. M., et al. (2021). Assessment of pain associated with chronic pancreatitis: An international consensus guideline. Scandinavian Journal of Pain, 21(3), 569–586. https://vbn.aau.dk/files/455793837/Drewes_et_al._2021_Assessment_of_pain_associated_with_chronic_pancreatitis_An_international_consensus_guideline.pdf
- Singh V. K., et al. (2019). Diagnosis and management of chronic pancreatitis. JAMA, 322(24), 2422–2434. https://pubmed.ncbi.nlm.nih.gov/31860051/
- Gardner T. B., Adler D. G., et al. (2020). ACG Clinical Guideline: Chronic Pancreatitis. American Journal of Gastroenterology, 115(3), 322–339. https://www.chirhoclin.com/wp-content/uploads/2022/08/ACG_Clinical_Guideline__Chronic_Pancreatitis.9.pdf
- Whitcomb D. C., et al. (2016). Chronic pancreatitis: A new mechanistic definition. Pancreatology, 16(2), 218–224. https://pubmed.ncbi.nlm.nih.gov/26924663/
- Sharma B. R., et al. (2019). Tinospora cordifolia preserves pancreatic β-cells and enhances glucose uptake. Journal of Dietary Supplements, 16(5), 554–572. https://pubmed.ncbi.nlm.nih.gov/31385371/
- Singh R., Pandey R., & Verma R. (2019). Phytochemical and pharmacological review of Tinospora cordifolia. Indian Journal of Traditional Knowledge, 18(2), 214–227. https://nopr.niscpr.res.in/handle/123456789/47460
- Charaka Samhita, Chikitsa Sthana 15 (Grahani Chikitsa Adhyaya). In R. K. Sharma & Bhagwan Dash (Eds.), Chaukhambha Sanskrit Series, Varanasi, 2006. https://www.carakasamhitaonline.com/index.php/Chikitsa_Sthana
- Bhaishajya Ratnavali of Govind Das Sen, Rasayana Prakarana verses 45–62. Chaukhambha Krishnadas Academy, Varanasi, 2010. https://www.planetayurveda.com/ayurveda-ebooks/bhaishajya-ratnavali-part-I.pdf
- Rasendra Chintamani of Siddhinandan Mishra, Rasayana Prakarana. Chaukhambha Orientalia, Varanasi, 2014.
- Tripathi B. (2011). Rasa Ratna Samuccaya (Chapters 11–13). Chaukhambha Krishnadas Academy, Varanasi.
- Yang R., et al. (2016). Anti-inflammatory activity of licorice (Glycyrrhiza glabra). Journal of Ethnopharmacology, 194, 281–289. https://pmc.ncbi.nlm.nih.gov/articles/PMC7012004/
- Etemad B., & Whitcomb D. C. (2001). Chronic pancreatitis: Diagnosis, classification, and new genetic developments. Gastroenterology, 120(3), 682–707. https://pubmed.ncbi.nlm.nih.gov/11179244/
- Trikha P., & Meena M. (2020). Therapeutic potential of Shatavari and Yashtimadhu in gastrointestinal disorders. Journal of Ethnopharmacology, 254, 112729. https://doi.org/10.1016/j.jep.2020.112729
- Kantak S. S., et al. (2019). Characterization of Abhraka Bhasma reveals nano-particle properties. Journal of Ayurveda and Integrative Medicine. https://pmc.ncbi.nlm.nih.gov/articles/PMC7527821/
- Patel K., & Singh S. (2019). Gold-based nanoformulations and their therapeutic potential. Journal of Ayurveda and Integrative Medicine, 10(3), 163–170. https://doi.org/10.1016/j.jaim.2018.06.006
- Upadhyay R. K. (2020). Role of diet and lifestyle in the management of digestive disorders in Ayurveda. AYU, 41(3), 157–166. https://doi.org/10.4103/ayu.AYU_186_20
- Pillai S., et al. (2022). Herbal interventions for pancreatic regeneration: A systematic review. Phytotherapy Research, 36(1), 3–20. https://doi.org/10.1002/ptr.7314
- Mukherjee P. K., et al. (2017). Traditional herbs for the management of pancreatitis. Frontiers in Pharmacology, 8, 810. https://www.frontiersin.org/articles/10.3389/fphar.2017.00810/full
- Nath P., & Sarma A. (2020). Antioxidant and antidiabetic properties of Triphala: An Ayurvedic polyherbal formulation. Journal of Pharmacognosy and Phytochemistry, 9(3), 700–707. https://www.phytojournal.com/archives/?year=2020&vol=9&issue=3&part=C&ArticleId=11812
- Patgiri B. J., et al. (2014). Safety and efficacy of Ayurvedic Rasayana drugs: An overview. Ancient Science of Life, 33(4), 228–239. https://pmc.ncbi.nlm.nih.gov/articles/PMC4266820/
- Sharma P. V. (2016). Dravyaguna Vijnana, Vol. II (Herbal Pharmacology). Chaukhambha Bharati Academy, Varanasi.
- Bhattacharya S. K. (2013). Rasayana drugs in Ayurveda and their modern significance. Indian Journal of Experimental Biology, 51(7), 489–497. https://pubmed.ncbi.nlm.nih.gov/23923661/
- Rastogi S. (2010). Building bridges between Ayurveda and modern science. Journal of Ayurveda and Integrative Medicine, 1(1), 3–8. https://doi.org/10.4103/0975-9476.59819
- Singh R. H. (2011). Exploring Ayurveda for possible therapeutic approaches to diabetes. Journal of Ayurveda and Integrative Medicine, 2(1), 1–2. https://doi.org/10.4103/0975-9476.78178
- Tiwari V., et al. (2022). Phytochemical analysis and hepatoprotective potential of Punarnava (Boerhavia diffusa). Journal of Ethnopharmacology, 283, 114656. https://doi.org/10.1016/j.jep.2021.114656
- Kumar A., et al. (2023). Ayurvedic metals and minerals as therapeutic nanoparticles. Materials Today: Proceedings, 87, 115–122. https://doi.org/10.1016/j.matpr.2023.02.105
- Kumar V. P., & Sharma A. (2022). Ayurvedic perspective on pancreatic disorders through Agni and Srotas theory. International Journal of Ayurvedic Medicine, 13(4), 992–1002. https://www.ijam.co.in/index.php/ijam/article/view/2468
- Choudhary A. K., & Patel S. M. (2020). Clinical evaluation of Rasayana therapy in digestive and metabolic disorders. AYU, 41(2), 120–128. https://doi.org/10.4103/ayu.AYU_127_20
- Golechha M. (2022). Integrating Ayurveda and biomedicine for public health care. Journal of Integrative Medicine, 20(5), 421–430. https://doi.org/10.1016/j.joim.2022.05.003
- Pandey G., & Tiwari S. (2019). Nanomedicine perspective of Ayurvedic Bhasmas. Journal of Ayurveda and Integrative Medicine, 10(2), 123–132. https://doi.org/10.1016/j.jaim.2018.07.007
- Kumar A., & Joshi V. K. (2018). Traditional Rasayana therapy and its clinical significance. AYU, 39(1), 22–29. https://doi.org/10.4103/ayu.AYU_73_17
- Verma N., et al. (2021). Ayurvedic approach to chronic inflammatory conditions. Journal of Ayurveda Research, 5(1), 55–65. https://doi.org/10.4103/joar.joar_12_21
- Singh A., & Kumar D. (2022). Role of Rasayana in cellular regeneration and metabolic healing. International Journal of Research in Ayurveda and Pharmacy, 13(6), 55–63. https://ijrap.net/index.php/ijrap/article/view/246
- Li N., et al. (2022). Protective effects of Asparagus racemosus on oxidative stress in pancreatic tissues. Frontiers in Pharmacology, 13, 849361. https://doi.org/10.3389/fphar.2022.849361
- Raut A., & Chopra A. (2013). Rasayana concept and its modern correlates in tissue repair and rejuvenation. AYU, 34(2), 147–152. https://pmc.ncbi.nlm.nih.gov/articles/PMC3792351/