- Can IBS Be Cured Permanently?
- Is There a Permanent Cure for IBS? A Clear Answer
- Why People Search “Can IBS Be Cured Permanently”
- What Is IBS? A Simple Medical Explanation
- Can IBS Be Cured Permanently According to Modern Medicine?
- Why IBS Symptoms Keep Coming Back
- Can IBS Be Cured Permanently Based on IBS Type?
- Conditions Commonly Misdiagnosed as IBS
- How Long Does It Take to Recover From IBS?
- What Does “Permanent Cure” Really Mean for IBS Patients?
- Can IBS Be Cured Permanently With Ayurveda?
- Ayurvedic Approach for Long-Term IBS Relief
- Why IBS Is More Persistent in Some Women
- Combining Modern Medicine and Ayurveda for IBS Recovery
- Is IBS a Lifelong Condition or Can It Go Away Completely?
- Frequently Asked Questions About IBS Cure
- Key Takeaways
- Reference
Can IBS Be Cured Permanently?
In modern medicine, irritable bowel syndrome is usually explained as a long term condition without a clear permanent cure. Doctors often tell patients that IBS can be controlled but not completely cured. The focus is mainly on reducing symptoms like abdominal pain, bloating, constipation, or diarrhoea through medicines, diet changes, and stress management [2]. This is because IBS is understood as a functional gut and brain disorder, where nerves, digestion, immunity, and gut bacteria do not work in proper coordination, even though scans and blood tests look normal [13]. For many patients, this leads to ongoing treatment without a clear end point.
Ayurveda looks at IBS very differently and does recognise the possibility of a cure. In Ayurvedic medicine, conditions similar to IBS are described as Grahani Roga. The root cause is believed to be weak digestion, accumulation of toxins, and imbalance in the body systems that control the gut. Instead of only calming symptoms, Ayurveda focuses on correcting digestion, strengthening the gut, and restoring balance between the gut and the nervous system. When digestion improves and the underlying imbalance is corrected, symptoms are expected to resolve in a stable and lasting way. Many patients are told that recovery is possible when treatment is personalised and followed correctly.
If you are someone living with IBS, this difference matters. From a modern medical point of view, you may hear that IBS has no permanent cure. From an Ayurvedic point of view, the condition is considered reversible when treated at the root. A detailed explanation of how Ayurveda diagnoses and treats IBS with the aim of long term recovery is explained here: https://panaceayur.com/ibs-ayurvedic-treatment-diagnosis-symptoms-cure/
This integrated understanding helps explain why some people continue to struggle with symptoms, while others experience meaningful and lasting improvement.
Is There a Permanent Cure for IBS? A Clear Answer
The clear answer depends on which medical system you are asking. In modern medicine, the answer is usually no. IBS is described as a chronic condition that can be managed but not permanently cured. Treatment focuses on controlling symptoms, avoiding triggers, and improving quality of life. Long term studies show that symptoms may improve, worsen, or return over time, which is why doctors often prepare patients for ongoing management rather than a final cure [2], [12].
Ayurveda gives a different answer. Yes, IBS can be cured when treated through Ayurveda. In this system, IBS is not seen as a lifelong disorder but as a reversible digestive imbalance. The focus is not on suppressing pain or bowel symptoms but on correcting weak digestion, restoring gut strength, and rebalancing the connection between the gut and the nervous system. When the root cause is corrected, symptoms are expected to resolve and remain stable.
This difference exists because modern medicine defines cure as eliminating a disease with a single treatment, while Ayurveda defines cure as restoring normal function and balance in the body. Long term medical research also supports that IBS does not follow a fixed lifelong pattern in all patients, and meaningful recovery is possible when underlying triggers and physiological imbalances are addressed [12], [13]. This is why many people who do not find lasting relief with symptom based treatment begin to look for root cause approaches that aim for true recovery rather than long term control.
Why People Search “Can IBS Be Cured Permanently”
People search this question because living with IBS is exhausting, unpredictable, and emotionally draining. Many individuals start their journey hoping the condition is temporary, but over time they realise symptoms often return despite diet changes, medications, or lifestyle adjustments. Long term follow up studies show that IBS does not follow a straight path. Symptoms may improve for a period, relapse again, or change in pattern, which creates ongoing uncertainty for patients [12]. This uncertainty leads people to keep searching for a final answer rather than another short term solution.
Another reason is the long duration of suffering. IBS often affects people for years during their most active working and family life. When symptoms interfere with daily routines, social life, travel, or professional responsibilities, frustration builds. Patients begin to question whether they will have to manage symptoms forever or whether true recovery is possible. This is why the word permanently appears so often in searches. People are not just looking for relief today. They want to know if there is an end point.
The global burden of IBS also plays a role. IBS affects millions of people worldwide and is one of the most common digestive disorders seen in clinics [17]. Despite its high prevalence, many patients feel unheard or inadequately helped because tests are normal and treatments feel limited. When repeated medical visits result in reassurance rather than resolution, people naturally turn to the internet looking for answers that go beyond symptom control.
What Is IBS? A Simple Medical Explanation
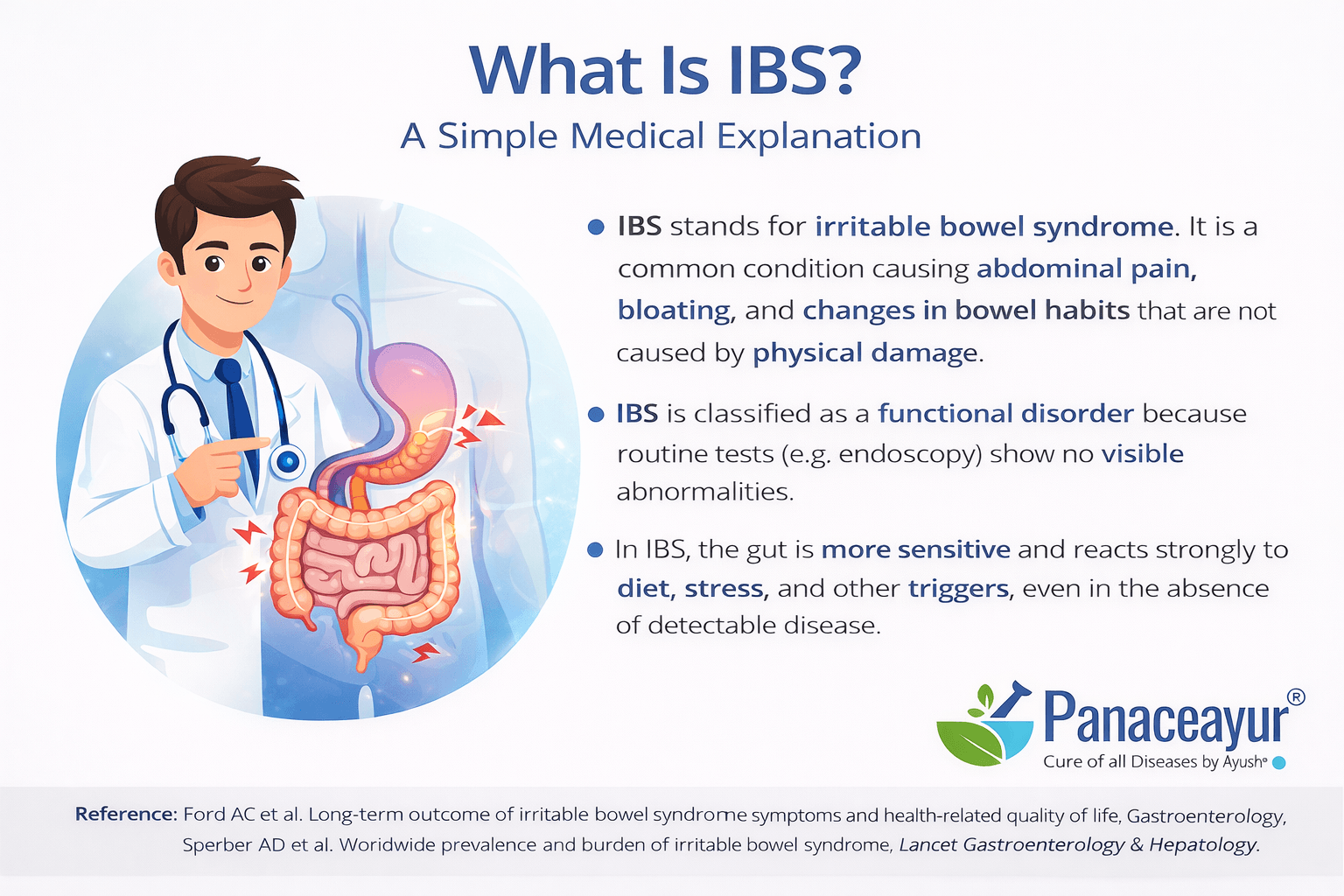
Irritable bowel syndrome, commonly called IBS, is a digestive condition that affects how the gut functions rather than how it looks. People with IBS experience symptoms such as abdominal pain, bloating, constipation, diarrhoea, or a mix of both, but standard medical tests usually do not show visible disease or damage [1]. This is why IBS often feels confusing and frustrating for patients. You may feel very real symptoms, yet scans, blood tests, and endoscopies come back normal.
From a medical point of view, IBS is understood as a disorder involving abnormal communication between the gut and the brain, increased gut sensitivity, altered bowel movement patterns, and changes in gut bacteria [2]. Because there is no single structural cause, IBS does not fit into the traditional disease model where a problem is seen and removed. This makes diagnosis and treatment very different from conditions like ulcers or inflammatory bowel disease.
How IBS Is Diagnosed in the UK and USA (Rome IV Criteria)
In both the UK and the USA, IBS is diagnosed using symptom based criteria known as the Rome IV criteria. Doctors look at your symptoms over time rather than relying on one specific test. According to these criteria, IBS is diagnosed when a person has recurring abdominal pain at least one day per week over the last three months, along with changes in bowel habits such as constipation, diarrhoea, or changes in stool form [1].
Before confirming IBS, doctors usually rule out serious conditions like infections, inflammatory bowel disease, or cancer through basic investigations. Once these are excluded and the symptom pattern matches Rome IV criteria, IBS is diagnosed. This explains why many patients are told they have IBS after being told that all tests are normal.
Why IBS Is Called a Functional Bowel Disorder
IBS is called a functional bowel disorder because the problem lies in how the bowel functions, not in visible damage or disease. The muscles of the gut may contract too fast or too slowly, the nerves may overreact to normal digestion, and the gut may respond abnormally to stress or food [1]. All of this can happen even when the intestine looks healthy on medical tests.
Research also shows that people with IBS often have heightened gut sensitivity and altered brain gut signalling, which explains why pain and discomfort feel intense even without structural disease [3]. This functional label does not mean the condition is psychological or imagined. It means that the disorder involves complex regulation problems between the gut, nervous system, and internal environment, making IBS real, chronic, and impactful on daily life.
Can IBS Be Cured Permanently According to Modern Medicine?
According to modern medicine, IBS is generally not described as a condition with a permanent cure. Medical guidelines explain IBS as a chronic functional disorder where symptoms can be reduced and managed, but the underlying tendency for the condition often remains [2]. This understanding is based on decades of research showing that IBS does not have a single identifiable cause that can be removed or corrected with one treatment. Instead, it involves ongoing interactions between the gut, nervous system, immune response, and gut bacteria [13].
Because of this complexity, modern medicine focuses on long term management rather than complete resolution. Patients are often advised to adjust diet, manage stress, and use medications as needed to control symptoms. While many people experience improvement, doctors usually avoid promising a permanent cure, as symptoms can return under stress, illness, or lifestyle changes [2], [13].
Why Doctors Say IBS Has No Cure
Doctors say IBS has no cure because there is no clear structural disease or single biological defect that can be corrected. Medical research shows that IBS symptoms arise from functional problems such as abnormal gut movement, increased nerve sensitivity, and altered gut brain communication rather than damage that can be surgically removed or medically reversed [2].
Another reason is the high variability of IBS. Symptoms differ from person to person and may change over time. Clinical studies also show strong placebo responses and fluctuating symptom patterns, which makes it difficult to define a clear end point for the disease [3]. Because symptoms can improve and return, doctors describe IBS as a condition that can be controlled but not definitively cured.
IBS Treatment vs IBS Cure: What’s the Difference?
In modern medicine, IBS treatment means reducing symptoms and improving daily functioning. This may include medications for pain, diarrhoea, or constipation, along with dietary advice and stress management. The goal is to help patients live more comfortably rather than to eliminate the condition entirely [2].
A cure, on the other hand, would mean restoring normal gut function in a stable and lasting way without ongoing treatment. Modern medical literature explains that this level of recovery cannot be consistently achieved with current therapies because IBS involves multiple systems working together in complex ways [13]. As a result, treatment and cure are not considered the same in conventional care.
Why Most IBS Treatments Focus on Symptom Control
Most IBS treatments focus on symptom control because symptoms are the most immediate problem affecting quality of life. Pain, bloating, bowel irregularity, and urgency interfere with daily activities, so medical care aims to reduce these effects as efficiently as possible [2].
Research also shows that IBS symptoms are influenced by stress, emotions, and the nervous system, which means symptoms can fluctuate even when treatment is ongoing [3]. Because of this unpredictability, doctors often adjust treatments over time rather than aiming for a single permanent solution. This approach helps patients manage symptoms but does not always address the deeper functional imbalance that contributes to recurrence.
Why IBS Symptoms Keep Coming Back
Many people with IBS notice a repeating pattern. Symptoms improve for some time and then return again. This cycle happens because IBS is not caused by a single problem. It involves ongoing disturbances in how the gut, nerves, and internal environment work together. When these deeper mechanisms are not fully corrected, symptoms may settle temporarily but often reappear under stress, illness, dietary changes, or emotional strain [4], [5], [6].
Gut Brain Axis Problems in IBS
The gut and the brain are closely connected through nerves, hormones, and immune signals. In IBS, this communication becomes dysregulated. Signals from the brain can overstimulate the gut, while signals from the gut can amplify stress and anxiety. Even after symptoms improve, this altered gut brain communication may remain unstable. As a result, emotional stress, fear of symptoms, or past negative experiences with food can easily trigger a relapse [4].
Nerve Sensitivity and Pain Memory in the Gut
People with IBS often develop increased sensitivity in the nerves of the intestine. Normal digestion that should not cause pain may be perceived as discomfort or cramping. Over time, the nervous system can develop a form of pain memory, where the gut reacts strongly even in the absence of active irritation. This explains why symptoms can return without an obvious trigger and why pain may persist even when digestion seems otherwise normal [5].
Gut Microbiome Imbalance and Incomplete Healing
Research shows that many IBS patients have altered gut bacteria compared to healthy individuals. When this imbalance is only partially corrected, digestion may improve temporarily but not fully stabilise. Changes in diet, antibiotics, infections, or stress can easily disrupt the microbiome again, leading to renewed symptoms [6]. Studies also show that IBS symptoms naturally fluctuate over time, which is why short term improvement does not always mean complete recovery [3]. Until the gut environment and its regulation fully normalise, symptoms may continue to come and go.
Can IBS Be Cured Permanently Based on IBS Type?
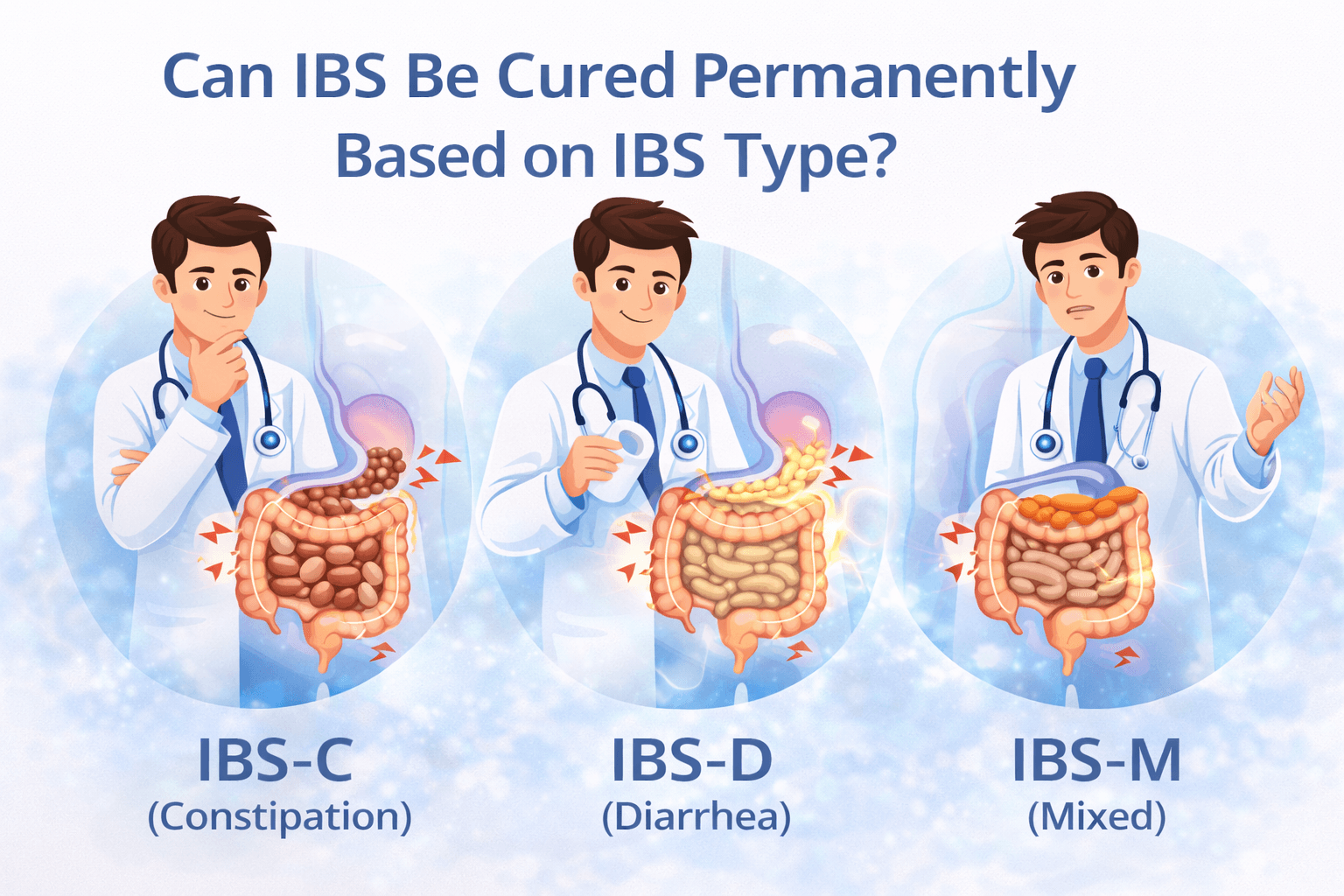
IBS does not present the same way in everyone, which is why outcomes differ from person to person. Medical research shows that IBS is divided into subtypes based on bowel patterns and triggers. Each type has a different dominant mechanism, and this strongly influences whether long term resolution is possible and how difficult it may be [8]. Understanding the type of IBS is an important step because treatment that helps one subtype may not work for another [7].
IBS-C (Constipation IBS): Can It Be Reversed Long Term?
In constipation predominant IBS, the main problems are slow bowel movement, poor gut motility, and increased sensitivity of the colon. Many patients experience bloating, incomplete evacuation, and abdominal discomfort. From a medical perspective, long term reversal is challenging because the underlying nerve and muscle coordination of the gut often remains impaired [8]. Medications can stimulate bowel movements, but they do not consistently restore normal gut function. Research also shows that constipation IBS often overlaps with nervous system dysregulation and stress sensitivity, which makes relapse possible when treatment stops [13].
IBS-D (Diarrhoea IBS): Why Symptoms Often Return
Diarrhoea predominant IBS is marked by frequent loose stools, urgency, and abdominal pain. Studies show that this subtype often involves abnormal gut motility, increased gut secretion, and in some cases bile acid imbalance [8]. Even when diarrhoea improves with medication or diet, symptoms may return if bile acid handling or gut sensitivity is not fully corrected [10]. This explains why IBS-D patients may experience cycles of improvement and relapse, especially during stress or dietary changes.
IBS-M (Mixed IBS): Why Alternating Symptoms Are Hard to Fix
Mixed type IBS involves alternating constipation and diarrhoea, making it one of the most difficult forms to manage. Medical research explains that this pattern reflects unstable gut regulation rather than a single dominant dysfunction [8]. Because bowel habits swing in both directions, treatments aimed at one symptom may worsen the other. This instability makes long term resolution more complex and requires careful, individualized management.
Post-Infectious IBS: Can the Gut Fully Heal?
Post infectious IBS develops after a bout of food poisoning or intestinal infection. Research confirms that inflammation, immune activation, and nerve damage can persist even after the infection clears [7]. Long term studies show that some patients gradually recover as the gut heals, while others continue to experience symptoms for many years [12]. Whether the gut fully heals depends on the severity of the initial infection, immune response, and how well gut function is restored over time.
Stress-Related IBS: When the Nervous System Is the Cause
In stress related IBS, symptoms are closely linked to emotional strain, anxiety, or past trauma. Research shows that the nervous system plays a central role in driving gut sensitivity and abnormal bowel responses [4]. Even when digestion appears normal, heightened nerve sensitivity can trigger pain, urgency, or bloating. Over time, the gut may develop pain memory, where symptoms recur even in the absence of active digestive disturbance [5]. In such cases, lasting improvement depends on calming and retraining the gut nervous system rather than focusing only on bowel symptoms.
Conditions Commonly Misdiagnosed as IBS
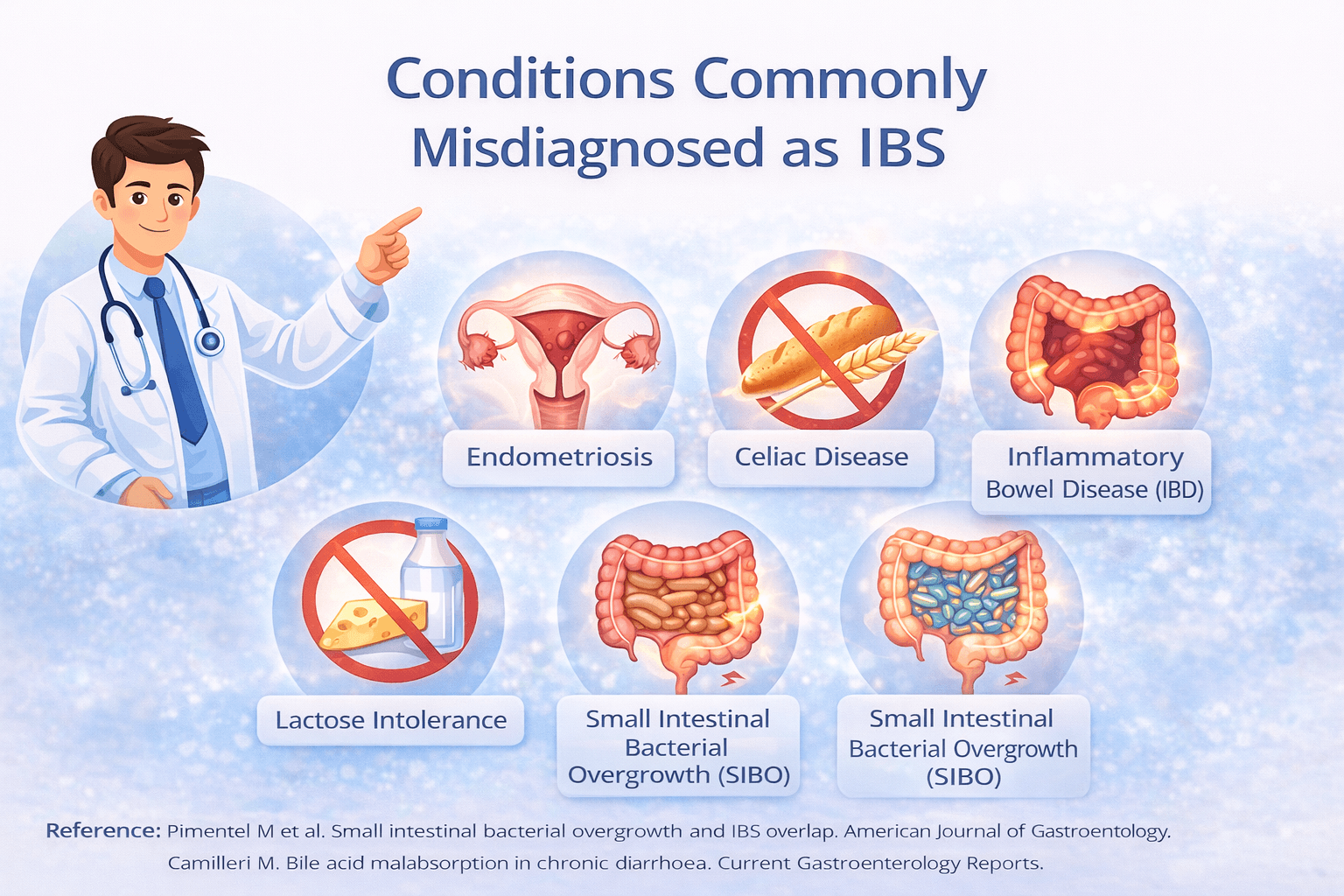
IBS is often diagnosed after routine investigations fail to show structural disease. However, medical research clearly shows that several distinct conditions can closely mimic IBS symptoms. When these are overlooked, patients may be told they have IBS even though a treatable underlying cause exists. This misdiagnosis is a major reason why symptoms persist despite repeated treatment attempts [9], [10].
SIBO and Small Intestinal Bacterial Overgrowth
Small intestinal bacterial overgrowth occurs when excessive bacteria colonise the small intestine, an area that normally contains relatively few microbes. These bacteria ferment food prematurely, producing gas and metabolic byproducts that cause bloating, abdominal distension, pain, diarrhoea, constipation, or alternating bowel habits. These symptoms overlap almost completely with IBS, which is why SIBO is frequently missed. Research shows that a significant proportion of patients diagnosed with IBS test positive for SIBO when properly evaluated [9]. If SIBO is not identified and treated, dietary restriction and symptom based medications often provide only partial or temporary relief, leading patients to believe their IBS is incurable when the true cause has not been addressed.
Food Intolerances Often Mistaken for IBS
Food intolerances such as lactose intolerance, fructose malabsorption, and sensitivity to fermentable carbohydrates can closely resemble IBS. In these conditions, symptoms occur because certain foods are poorly digested or absorbed, leading to gas production, bloating, pain, and altered bowel habits. When testing for food intolerances is not performed, symptoms may appear unpredictable and fluctuate over time, reinforcing an IBS label [9]. Research also shows that functional gut symptoms naturally vary, which further blurs the distinction between true IBS and food driven reactions [3]. Without identifying and addressing specific dietary triggers, patients may continue to experience symptoms despite following general IBS treatment advice.
Bile Acid Malabsorption and Chronic Diarrhoea
Bile acid malabsorption is an underdiagnosed condition in which excess bile acids enter the colon instead of being properly reabsorbed in the intestine. This leads to chronic watery diarrhoea, urgency, and abdominal discomfort, symptoms that are commonly labelled as diarrhoea predominant IBS. Studies show that a meaningful percentage of patients diagnosed with IBS-D actually have bile acid malabsorption [10]. Because this condition requires targeted treatment rather than standard IBS therapies, failure to recognise it often results in persistent symptoms and repeated treatment failure.
Hormonal Gut Disorders in Men and Women
Hormones play an important role in regulating gut movement, sensitivity, and fluid balance. In women, gastrointestinal symptoms often worsen during specific phases of the menstrual cycle, pregnancy, or hormonal transitions, while in men, hormonal imbalance can also influence bowel function. Research shows that gut symptoms frequently fluctuate in response to hormonal changes, which can mimic or worsen IBS patterns [11]. When hormonal influences are not considered, patients may be diagnosed with IBS without addressing an important underlying driver. In such cases, symptom control alone may offer only temporary relief unless hormonal factors are also taken into account.
How Long Does It Take to Recover From IBS?
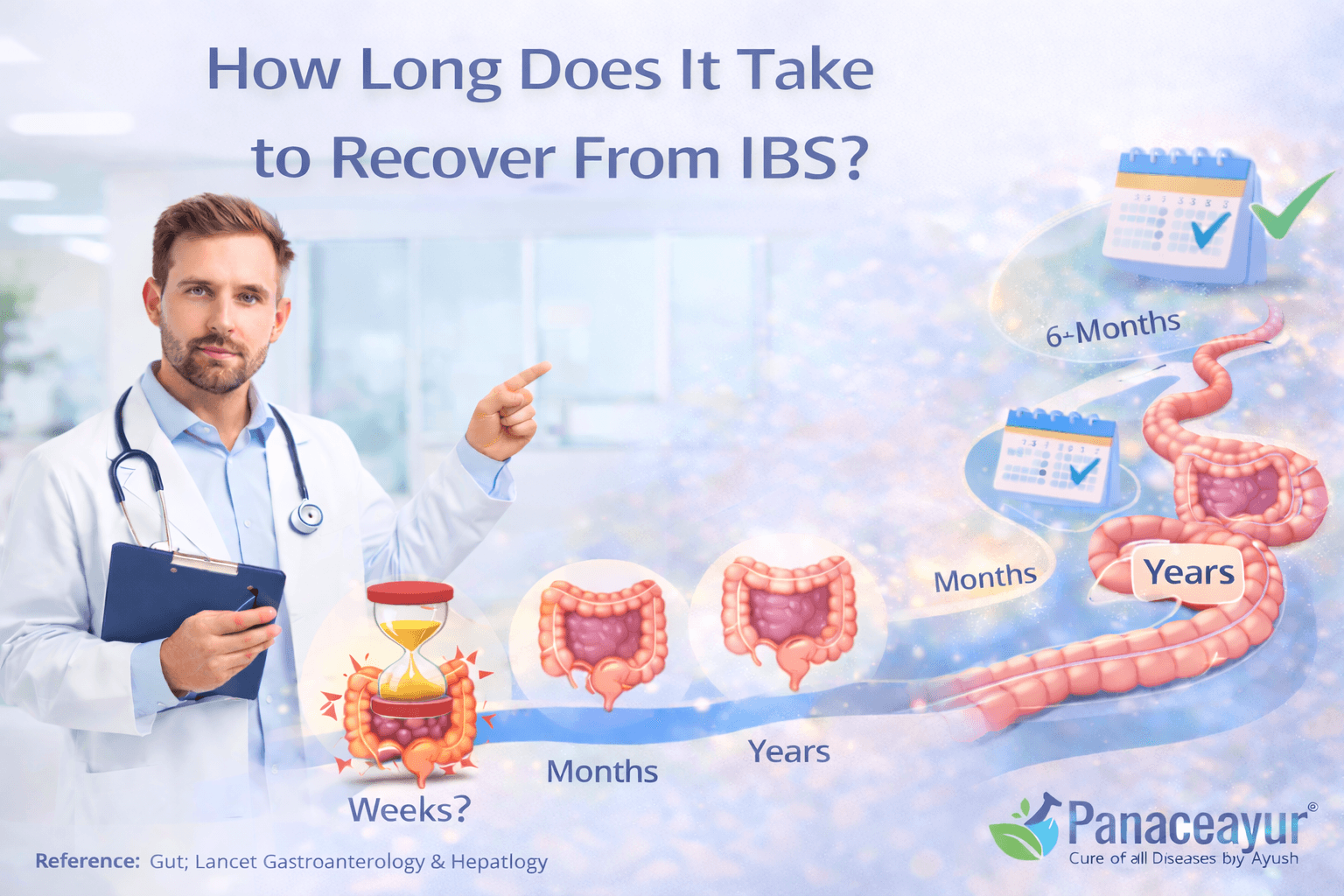
Recovery from IBS is not instant and it is not the same for everyone. IBS develops over time due to long standing disturbances in digestion, gut sensitivity, gut bacteria, and stress response. Because of this, recovery also happens in phases. Long term medical studies show that IBS symptoms often improve gradually, fluctuate, or relapse rather than disappear suddenly. Understanding these phases helps set realistic expectations and prevents frustration when progress feels slow [12], [17].
Short Term IBS Symptom Improvement Timeline
In the early phase of recovery, most patients experience symptom relief rather than true healing. This phase usually begins within a few weeks and may extend up to two or three months. During this time, abdominal pain may reduce, bloating may feel less intense, and bowel movements may become more predictable. These improvements often come from diet changes, stress reduction, medications, or supportive therapies. However, this phase mainly reflects symptom calming. The underlying gut sensitivity and regulation problems may still be present. This is why many people feel better initially but notice symptoms returning when stress increases, routines change, or treatment is stopped. Short term improvement should be seen as stabilisation, not complete recovery.
Medium Term Gut and Nervous System Recovery
The medium term phase focuses on deeper functional recovery and usually takes several months. During this stage, the gut begins to regain better coordination in movement, sensitivity, and digestion. At the same time, the nervous system gradually becomes less reactive to normal digestive processes. Gut bacteria also begin to stabilise, but this happens slowly and can be disrupted by infections, antibiotics, or stress. Many patients feel mostly well during this phase but still experience flare ups during emotional stress, travel, illness, or dietary changes. These flare ups indicate that healing is in progress but not yet complete. Consistency during this phase is important, as frequent changes in treatment can interrupt recovery.
Long Term IBS Remission and Relapse Prevention
Long term recovery is best described as remission rather than a sudden cure from a modern medical viewpoint. Remission means living for long periods with minimal or no symptoms and without the need for continuous medication. Long term studies show that some patients reach this stage and maintain stability for years, while others experience occasional symptoms under specific triggers. True stability depends on how well gut sensitivity, digestion, nervous system regulation, and immune balance are restored together. Relapse prevention becomes a key focus at this stage. This includes recognising early warning signs, maintaining dietary and lifestyle balance, managing stress, and avoiding repeated strain on the gut. When these factors are addressed consistently, many people are able to live a normal life with IBS no longer dominating daily decisions or quality of life.
What Does “Permanent Cure” Really Mean for IBS Patients?
For most people living with IBS, a permanent cure does not mean erasing a label or never having a digestive symptom again. It means getting life back to a place where IBS no longer controls daily choices, emotions, or confidence. In modern medicine, doctors are careful with the word cure because IBS symptoms can fluctuate and vary from person to person. Instead, recovery is often described as long term stability and restored gut function rather than a guaranteed lifelong absence of symptoms. From a patient’s point of view, a permanent cure is about freedom and predictability, not perfection.
Living Without Daily IBS Medication
For many IBS patients, daily life depends on medications. These may include laxatives, antidiarrhoeal drugs, pain relievers, or gut specific medicines taken regularly just to function normally. While these treatments can reduce symptoms, long term research shows they usually manage discomfort rather than change the underlying pattern of IBS. A meaningful sense of recovery begins when medication is no longer required every day. Patients often describe this stage as the point where they can stop planning their routine around pills and still feel stable. Being able to reduce or stop medication without symptoms immediately returning is a strong sign that gut regulation has improved.
Eating Normally Without Fear of Flare Ups
Food fear is one of the most emotionally exhausting aspects of IBS. Many people avoid eating outside, restrict their diet severely, or skip meals because they associate food with pain, bloating, or urgent bowel movements. Over time, this creates anxiety around eating itself. Long term improvement is reflected when a person can eat a wider range of foods without constant worry or predictable flare ups. This does not mean eating carelessly, but it does mean meals no longer trigger fear. Regaining confidence around food is often one of the clearest signs for patients that recovery is real and lasting.
No Stress Triggered IBS Symptoms
Stress related flare ups are extremely common in IBS. Even when digestion improves, emotional stress can quickly reactivate symptoms in many people. This happens because the gut and nervous system are closely linked. For patients, long term recovery means that everyday stress no longer immediately translates into gut pain, urgency, or bloating. Life stress still exists, but the gut response becomes calmer and more resilient. When stress no longer controls digestive symptoms, IBS stops feeling like a constant threat and becomes something that no longer dominates daily life or mental space.
Can IBS Be Cured Permanently With Ayurveda?
Yes, IBS can be cured permanently through Ayurveda when treatment is directed at correcting the root cause rather than suppressing symptoms. Classical Ayurvedic texts clearly describe IBS like conditions under Grahani Roga and explain that stable digestion is the foundation of lasting gut health. When digestion is restored and internal balance is re established, bowel symptoms resolve and do not continue to relapse. A detailed explanation of this curative Ayurvedic approach is available in the complete guide here: https://panaceayur.com/ibs-ayurvedic-treatment-diagnosis-symptoms-cure/
Ayurvedic Explanation of IBS Root Causes
Ayurveda explains that IBS develops due to progressive weakening of digestion, irregular food habits, mental stress, improper routines, and disturbance of the systems that regulate the gut. When digestion becomes weak, food is not properly transformed, leading to accumulation of Ama, which irritates the intestines and disrupts bowel rhythm. Over time, this results in chronic symptoms such as bloating, pain, constipation, diarrhoea, or alternating bowel habits.
Charaka Samhita clearly states that Grahani disorders arise when digestive strength is impaired and digestion becomes unstable:
“Mandagni eva sarvesham roganam karanam smritam”
Charaka Samhita, Chikitsa Sthana 15
This verse explains that weak digestive fire is the root cause of all digestive diseases. Ayurveda therefore treats IBS by correcting the underlying digestive dysfunction rather than repeatedly addressing individual symptoms.
Digestive Fire Agni and Gut Imbalance in IBS
Agni is the central regulator of digestion and metabolism in Ayurveda. When Agni is balanced, digestion is smooth and bowel movements are regular. When Agni becomes weak, irregular, or unstable, digestion becomes unpredictable. Food may be digested too slowly, too quickly, or incompletely, leading to gas, discomfort, and altered bowel habits. This instability also affects gut sensitivity and its response to stress.
Ashtanga Hridaya explains the role of Agni in Grahani disorders:
“Agni dushteshu grahani na sthira bhavati kvachit”
Ashtanga Hridaya, Nidana Sthana 8
This verse indicates that when digestive fire is disturbed, the intestines lose their stability and normal function. Ayurvedic treatment therefore focuses first on strengthening and stabilising Agni. Once digestion becomes consistent and efficient, the gut environment heals naturally, sensitivity reduces, and bowel function stabilises in a lasting way.
Why Ayurveda Aims for Restoration, Not Suppression
Ayurveda does not aim to stop diarrhoea abruptly, force bowel movements, or numb pain as a long term solution. Such approaches are considered suppressive and incomplete. Instead, Ayurveda focuses on restoring normal digestive intelligence and gut coordination. Treatment is personalised based on the individual’s constitution, digestive strength, symptom pattern, and mental state. Diet correction, daily routine alignment, and targeted herbal formulations are used to rebuild digestive capacity and balance the gut nervous system.
Charaka Samhita emphasises restoration over suppression in digestive disorders:
“Na hi roga prashamanam roga karana nivritim vina”
Charaka Samhita, Sutra Sthana
This principle explains that disease cannot be cured unless its cause is removed. From the Ayurvedic perspective, cure means restoring normal function so that symptoms no longer return. When digestion is restored and balance is maintained, IBS resolves at its root rather than remaining a lifelong condition.
Ayurvedic Approach for Long-Term IBS Relief
Ayurveda approaches long term IBS relief through a structured, step by step restoration of digestive strength, gut stability, and nervous system balance. Unlike symptom focused models, this approach is designed to correct the internal environment in which IBS develops. Classical Ayurvedic texts consistently explain that lasting relief is achieved only when digestion is stabilised, metabolic toxins are cleared, and daily habits are aligned with the body’s natural rhythms. This is why Ayurveda considers IBS a reversible condition when treated correctly and patiently.
Individualised IBS Diagnosis in Ayurveda
Ayurveda does not diagnose IBS as a single uniform disease. Instead, it evaluates the individual through a detailed assessment of digestive strength, bowel patterns, mental state, diet, lifestyle, and constitutional makeup. Two people with similar IBS symptoms may have completely different underlying imbalances. One person may suffer due to weak digestion and sluggish gut movement, while another may have hypersensitive digestion aggravated by stress and irregular routines.
Charaka Samhita clearly states that disease must always be understood in the context of the individual:
“Purusham purusham veekshya”
Charaka Samhita, Sutra Sthana
This principle means that treatment must be tailored to the person, not just the disease name. In IBS, this personalised diagnosis allows Ayurveda to target the exact mechanism responsible for symptoms rather than applying generic remedies that offer only temporary relief.
Improving Digestion and Gut Strength Naturally
Strengthening digestion is the cornerstone of Ayurvedic IBS treatment. Weak or unstable digestion leads to improper processing of food, gas formation, bowel irregularity, and gut irritation. Ayurveda focuses on gradually restoring digestive capacity so that food is digested completely and efficiently, without strain on the intestines.
Ashtanga Hridaya emphasises the central role of digestion in gut health:
“Rogah sarve api mande agnau”
Ashtanga Hridaya, Sutra Sthana
This verse explains that impaired digestion is at the root of all diseases. By improving digestive strength through diet correction, herbal support, and routine regulation, the gut regains stability. As digestion improves, bloating reduces, bowel movements normalise, and sensitivity decreases in a sustained way rather than fluctuating temporarily.
Detoxification and Gut Reset Therapies
In Ayurveda, long standing digestive imbalance leads to the accumulation of Ama, which refers to incompletely digested metabolic waste. Ama irritates the gut lining, disrupts bowel rhythm, and interferes with nutrient absorption. If this toxic load is not cleared, digestive therapies alone may not produce lasting results.
Charaka Samhita explains the importance of removing accumulated toxins before restoration
“Shodhanam shamanam chaiva”
Charaka Samhita, Sutra Sthana
This principle highlights the role of cleansing before strengthening. Gut reset therapies are selected carefully based on the individual’s strength and symptom pattern. The goal is not aggressive purging, but gentle removal of accumulated waste so that digestion can function normally again. When detoxification is done correctly, the gut becomes more receptive to healing and long term stability improves.
Diet and Lifestyle Changes for Permanent Balance
Ayurveda considers diet and lifestyle as daily medicine. Even the most effective treatments will fail if daily habits continue to weaken digestion. Long term IBS relief depends on eating in alignment with digestive capacity, maintaining regular meal timings, adequate rest, and managing mental stress.
Charaka Samhita highlights the role of proper daily habits in maintaining health:
“Ahara vihara samyogah svasthasya svastha rakshanam”
Charaka Samhita, Sutra Sthana
This verse explains that health is preserved through proper diet and lifestyle. In IBS, this means avoiding irregular eating, incompatible food combinations, excessive fasting, and chronic stress. When diet and lifestyle support digestion instead of challenging it, the gut maintains balance naturally and symptoms do not keep returning.
Why IBS Is More Persistent in Some Women
IBS is diagnosed more frequently in women, and many women also report more persistent or fluctuating symptoms over time. This is not simply due to differences in pain tolerance or reporting. Medical research shows that hormonal influences and heightened gut nervous system sensitivity play a major role in why IBS behaves differently in some women compared to men [11], [4]. These factors interact closely with digestion, stress response, and emotional regulation, making symptoms more likely to recur if not addressed at a deeper level.
Hormonal Changes and IBS Flare-Ups
Hormones significantly influence how the gut moves, senses pain, and responds to food. In women, fluctuations in oestrogen and progesterone during the menstrual cycle can directly affect bowel habits and gut sensitivity. Many women notice worsening bloating, pain, constipation, or diarrhoea in the days before menstruation or during periods. Research confirms that hormonal shifts can alter gut motility and pain perception, which explains cyclical IBS flare-ups [11].
Hormonal changes across different life stages also matter. Puberty, pregnancy, postpartum periods, and perimenopause can all influence IBS symptoms. During these transitions, the gut may become more reactive, and previously controlled symptoms may return. When hormonal influences are not recognised as part of the IBS picture, treatment may focus only on bowel symptoms while the underlying trigger continues to drive relapses.
Stress, Anxiety, and Gut Sensitivity
Women with IBS often show a stronger connection between emotional stress and gut symptoms. This is linked to increased sensitivity in the gut–brain communication pathways. Stress and anxiety can amplify normal digestive signals, turning them into pain, urgency, or discomfort. Research shows that the nervous system in IBS can remain in a heightened alert state, making the gut more reactive even to everyday stressors [4], [5].
Over time, repeated stress-related flare-ups can reinforce this sensitivity, creating a pattern where emotional strain quickly translates into physical symptoms. This does not mean IBS is psychological. It means the nervous system plays a central role in symptom persistence. For long-term improvement, both digestive balance and nervous system regulation need attention. When stress responses are calmed and gut sensitivity reduces, IBS symptoms become less frequent, less intense, and easier to control, especially in women who experience recurrent flare-ups.
Combining Modern Medicine and Ayurveda for IBS Recovery
For many people with IBS, lasting recovery does not come from choosing one system and rejecting the other. It comes from understanding where modern medicine and Ayurveda complement each other. Modern medicine excels at diagnosis, ruling out serious disease, and managing acute symptoms. Ayurveda excels at restoring digestion, strengthening gut resilience, and addressing long term functional imbalance. When used thoughtfully together, these approaches can support deeper and more stable recovery rather than repeated cycles of symptom control [17], [13].
Where Medical Science and Ayurveda Overlap
Although their language and frameworks differ, modern medicine and Ayurveda increasingly converge on key ideas about IBS. Medical research recognises the central role of the gut–brain axis, altered gut microbiota, immune activation, and nervous system sensitivity in IBS. Ayurveda has described these same processes for centuries using concepts of digestion strength, gut regulation, and mind–body interaction.
Both systems now acknowledge that IBS is not caused by visible damage but by disturbed regulation. Medical science explains this through altered gut motility, visceral hypersensitivity, and microbiome imbalance [4], [6]. Ayurveda explains the same pattern through impaired digestion, toxin accumulation, and imbalance in the systems governing gut and mental function. This overlap creates a natural bridge where dietary correction, stress regulation, gut microbiome support, and digestive strengthening can work together rather than in opposition [17].
Why Personalised Treatment Works Better for IBS
One of the strongest shared conclusions between modern research and Ayurveda is that IBS cannot be treated effectively with a one size fits all approach. Medical studies show wide variation in symptom patterns, triggers, stress sensitivity, and response to treatment among IBS patients [13], [17]. This explains why standardised protocols often fail to deliver lasting results.
Ayurveda has always emphasised individualised treatment, adjusting diet, lifestyle, and therapies based on the person rather than the diagnosis alone. When this personalised approach is combined with modern diagnostic clarity and safety monitoring, outcomes reminded improved. Patients benefit when treatment is adapted to their specific bowel pattern, stress profile, digestive strength, and life circumstances. Personalisation allows therapy to evolve as the gut heals, which reduces relapse risk and supports long term stability rather than temporary improvement.
Is IBS a Lifelong Condition or Can It Go Away Completely?
IBS is often described to patients as a lifelong condition, but this description is not entirely accurate. Long term medical studies show that IBS does not behave the same way in everyone. For some people, symptoms persist for many years with periods of improvement and relapse. For others, symptoms gradually reduce, change in pattern, or disappear altogether over time [12]. This variability is why IBS is better understood as a dynamic condition rather than a fixed lifelong diagnosis.
From a modern medical perspective, IBS is considered chronic because there is no single treatment that guarantees permanent symptom elimination in all patients [13]. Doctors therefore focus on long term management and caution patients that symptoms may return under stress, illness, or lifestyle changes. However, this does not mean recovery is impossible. It means that modern medicine lacks a universal curative intervention that works for every individual.
Clinical observations and follow up studies show that a meaningful proportion of patients experience long lasting remission, sometimes without ongoing medication [12]. In these cases, IBS effectively goes into the background and no longer interferes with daily life. Whether IBS goes away completely depends on how well underlying factors such as digestion, gut sensitivity, nervous system regulation, microbiome balance, and stress response are corrected [13].
In practical terms, IBS does not have to remain a defining feature of a person’s life. For some, it behaves as a chronic condition requiring ongoing care. For others, especially when root causes are addressed systematically, symptoms can fade to the point where IBS no longer feels present. The outcome depends less on the label and more on the depth and completeness of the approach used to restore gut balance.
Frequently Asked Questions About IBS Cure
Can IBS be cured permanently?
IBS can be cured permanently when the underlying causes are corrected rather than only controlling symptoms. Modern medicine usually focuses on long term management, but Ayurveda considers IBS a reversible digestive disorder. When digestion, gut sensitivity, and nervous system balance are restored, many patients experience stable and lasting relief instead of recurring flare ups.
Why do doctors say IBS has no cure?
Doctors say IBS has no cure because there is no single drug or procedure that eliminates IBS in every patient. IBS is classified as a functional disorder, meaning routine tests are normal and symptoms fluctuate. Because symptoms can return under stress or lifestyle changes, modern medicine avoids promising a permanent cure and focuses on symptom control.
Can IBS go away on its own?
In some people, IBS symptoms reduce or disappear over time, especially after lifestyle changes, stress reduction, or recovery from gut infections. Long term studies show that IBS may improve, relapse, or change pattern. However, relying on spontaneous improvement is unpredictable. Targeted treatment aimed at root causes improves the chances of lasting recovery.
How long does it take to recover from IBS?
Recovery time varies from person to person. Some people notice improvement within weeks, while deeper gut and nervous system recovery may take several months. Long term stability depends on correcting digestion, calming gut sensitivity, and preventing repeated triggers. IBS recovery is usually gradual rather than sudden.
Is IBS lifelong for everyone?
No. IBS is not lifelong for everyone. While some people experience symptoms for many years, others achieve long term remission where IBS no longer affects daily life. Whether IBS persists depends on factors such as stress, gut health, digestion, and how comprehensively treatment addresses the root causes.
Is Ayurveda effective for curing IBS?
Yes. Ayurveda focuses on restoring digestive strength, correcting gut imbalance, and stabilising the gut–brain connection. Unlike symptom based treatment, Ayurveda aims for functional recovery. Many patients turn to Ayurveda after repeated relapses with conventional treatment and experience long lasting improvement when therapy is personalised and followed consistently.
Key Takeaways
IBS is often presented as a lifelong condition in modern medicine, but long term research shows that its course is not fixed. Symptoms can improve, relapse, or even resolve over time depending on how deeply the underlying mechanisms are addressed. This explains why many people feel stuck when treatment focuses only on managing flare ups rather than correcting the root disturbance [2], [12].
A permanent solution to IBS does not mean the absence of all digestive sensations forever. It means reaching a stage where digestion is stable, symptoms no longer dominate daily life, and the gut does not overreact to food or stress. Modern medicine describes this as long term remission, while Ayurveda describes it as restoration of normal digestive function [13].
Ayurveda offers a fundamentally different framework by treating IBS as a reversible digestive disorder rather than a fixed diagnosis. By strengthening digestion, correcting gut imbalance, addressing stress sensitivity, and personalising treatment, Ayurveda aims for lasting recovery instead of repeated symptom suppression [14]. This approach explains why some people experience sustained improvement after years of unsuccessful symptom based treatment.
For anyone searching for a permanent IBS solution, the most important takeaway is this. IBS outcomes depend less on the label and more on the depth of the approach. When treatment addresses digestion, gut sensitivity, nervous system balance, and lifestyle together, long term stability becomes possible. The goal is not chasing quick relief, but rebuilding gut health in a way that allows normal life to resume without constant fear of relapse.
Reference
[1] Drossman, D. A., & Hasler, W. L. (2016). Rome IV—Functional gastrointestinal disorders: Disorders of gut–brain interaction. Gastroenterology, 150(6), 1257–1261. https://doi.org/10.1053/j.gastro.2016.03.035
This reference outlines the globally accepted criteria used to diagnose irritable bowel syndrome. It explains that IBS is a disorder of gut–brain interaction rather than a disease with visible damage, which is why routine scans and blood tests are often normal despite persistent symptoms.
[2] Ford, A. C., Lacy, B. E., & Talley, N. J. (2017). Irritable bowel syndrome. New England Journal of Medicine, 376(26), 2566–2578. https://www.nejm.org/doi/full/10.1056/NEJMra1607547
This paper explains why modern medicine considers IBS a chronic condition without a definitive drug-based cure and why current treatments focus mainly on symptom control rather than complete resolution.
[3] Enck, P., Azpiroz, F., & Boeckxstaens, G. (2016). Functional gastrointestinal disorders. Nature Reviews Disease Primers, 2, 16011. https://doi.org/10.1038/nrdp.2016.11
This study describes why IBS symptoms fluctuate over time, why placebo responses are common, and why symptom-focused treatment often does not lead to long-term relief.
[4] Mayer, E. A., Savidge, T., & Shulman, R. J. (2014). Brain–gut microbiome interactions. Gastroenterology, 146(6), 1500–1512. https://doi.org/10.1053/j.gastro.2014.02.009
This research explains the strong connection between the brain, nervous system, gut microbes, and digestion, showing why stress, anxiety, and emotional strain can worsen or prolong IBS symptoms.
[5] Zhou, Q., & Verne, G. N. (2011). New insights into visceral hypersensitivity. Gut, 60(6), 800–809. https://gut.bmj.com/content/60/6/800
This article explains why people with IBS experience heightened gut pain and discomfort even without visible disease, due to increased sensitivity of intestinal nerves.
[6] Jeffery, I. B., et al. (2012). An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota. Gut, 61(7), 997–1006. https://gut.bmj.com/content/61/7/997
This study shows that many IBS patients have altered gut bacteria, which can contribute to bloating, gas, irregular bowel movements, and ongoing digestive discomfort.
[7] Thabane, M., et al. (2007). Systematic review of post-infectious irritable bowel syndrome. American Journal of Gastroenterology, 102(9), 2119–2128. https://journals.lww.com/ajg/Fulltext/2007/09000/Systematic_Review_of_the_Incidence_and.26.aspx
This review confirms that IBS can develop after food poisoning or intestinal infections and may persist if the gut lining and nervous system do not fully recover.
[8] Mearin, F., et al. (2016). Bowel disorders. Gastroenterology, 150(6), 1393–1407. https://doi.org/10.1053/j.gastro.2016.02.031
This reference explains the different IBS subtypes such as constipation-predominant, diarrhea-predominant, and mixed IBS, and why each type behaves differently and requires individualized management.
[9] Pimentel, M., et al. (2020). Small intestinal bacterial overgrowth. American Journal of Gastroenterology, 115(2), 165–178.
https://journals.lww.com/ajg/Fulltext/2020/02000/Small_Intestinal_Bacterial_Overgrowth.8.aspx
This paper highlights how conditions like SIBO are frequently mistaken for IBS, which can explain why some patients fail to improve with standard IBS treatments.
[10] Camilleri, M. (2015). Bile acid diarrhea. Current Gastroenterology Reports, 17(4), 16. https://doi.org/10.1007/s11894-015-0436-6
This research describes bile acid imbalance as a common but underdiagnosed cause of chronic diarrhea that is often incorrectly labeled as IBS-D.
[11] Heitkemper, M., & Jarrett, M. (2008). Pattern of gastrointestinal symptoms across the menstrual cycle. American Journal of Gastroenterology, 103(2), 426–433. https://journals.lww.com/ajg/Fulltext/2008/02000/Pattern_of_Gastrointestinal_Symptoms_Across.16.aspx
This study explains why IBS symptoms often worsen in women during hormonal fluctuations, particularly around the menstrual cycle.
[12] Halder, S. L., et al. (2007). Natural history of irritable bowel syndrome over 12 years. American Journal of Gastroenterology, 102(6), 1223–1230.
https://journals.lww.com/ajg/Fulltext/2007/06000/Natural_History_of_Irritable_Bowel_Syndrome.9.aspx
This long-term study shows that IBS symptoms can improve, relapse, or resolve over time, helping patients understand realistic recovery patterns.
[13] Talley, N. J. (2020). What causes functional gastrointestinal disorders? The Lancet Gastroenterology & Hepatology, 5(1), 68–79. https://doi.org/10.1016/S2468-1253(19)30359-5
This article explains the complex interaction of nerves, digestion, immunity, and stress in IBS, clarifying why a single medication rarely provides a permanent solution.
[14] Charaka Samhita, Chikitsa Sthana, Chapter 15 (Grahani Chikitsa). Chaukhamba Orientalia, standard English edition.
This classical Ayurvedic text describes chronic digestive disorders comparable to IBS and emphasizes correcting digestion at its root rather than suppressing symptoms.
[15] Ashtanga Hridaya, Nidana Sthana, Chapter 8 (Grahani Nidana). Chaukhamba Orientalia, standard English edition.
This text explains how impaired digestive fire leads to chronic bowel disturbances and outlines principles for long-term digestive restoration.
[16] Kuttner, L., et al. (2006). Gut-directed hypnotherapy for irritable bowel syndrome. American Journal of Gastroenterology, 101(10), 2222–2228.
https://journals.lww.com/ajg/Fulltext/2006/10000/Gut_Directed_Hypnotherapy.16.aspx
This study demonstrates that calming the gut–brain axis through mind-based therapies can significantly reduce IBS symptoms and support long-term improvement.
[17] Black, C. J., & Ford, A. C. (2020). Global burden of irritable bowel syndrome. Gastroenterology, 158(1), 76–87.
https://doi.org/10.1053/j.gastro.2019.09.049
This research highlights how widespread IBS is globally and why personalized, long-term strategies are essential for meaningful and sustained recovery.