- Types of Bone Sarcoma
- Risk Factors & Etiology
- Pathophysiology
- Clinical Presentation
- Ayurvedic Correlation with Lesser-Known Signs
- Diagnosis
- Staging & Prognosis
- Modern Management
- Ayurvedic Interpretation & Cure
- Kanchnar Guggulu Avaleha (Medicine)
- Ayurvedic Foundation
- Method of Preparation (Avaleha Kalpana)
- Caution
- Frequently Asked Questions (FAQ)
- References
Bone sarcomas are rare malignant tumors that arise directly from bone or associated connective tissues, distinct from secondary bone metastases. The two most common forms are osteosarcoma, originating from primitive osteoblasts involved in bone formation, and Ewing sarcoma, a small round cell tumor of neuroectodermal origin that often involves long bones, pelvis, or chest wall [1].
Epidemiology: Age Groups and Gender Predilection
Osteosarcoma is most frequently diagnosed in adolescents and young adults, particularly during growth spurts, with peak incidence between 10–20 years and a higher prevalence in males. Ewing sarcoma also primarily affects children and young adults but can extend into the third decade, with some studies noting a more balanced gender ratio [2].
Global Incidence and Mortality Trends
Bone sarcomas represent less than 0.2% of all cancers globally, yet they contribute significantly to cancer-related morbidity and mortality in young populations. Osteosarcoma incidence is approximately 3–4 cases per million per year, whereas Ewing sarcoma occurs in 2–3 cases per million, with higher rates in European populations compared to Asian or African groups. Survival rates for localized osteosarcoma average 60–70%, but fall to 20–30% when metastases, especially to the lungs, are present [3][4].
Importance of Early Diagnosis and Integrative Approaches
Diagnostic delays are common, as bone sarcoma symptoms often mimic sports injuries or benign bone disorders. Early recognition is critical to improving outcomes, as advanced disease is associated with poor prognosis. While conventional oncology focuses on chemotherapy, surgery, and radiation, there is growing interest in integrative frameworks. Ayurveda interprets these malignancies through the lens of Rakta and Majja Dhatu Dushti, with therapies such as Shodhana (purification) and Rasayana (rejuvenation) aimed at restoring systemic balance, enhancing immunity, and potentially reducing recurrence risk [5][6].
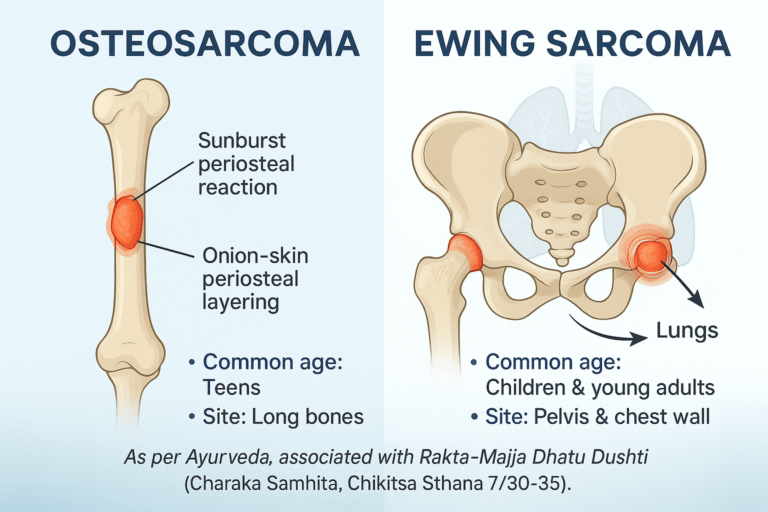
Types of Bone Sarcoma
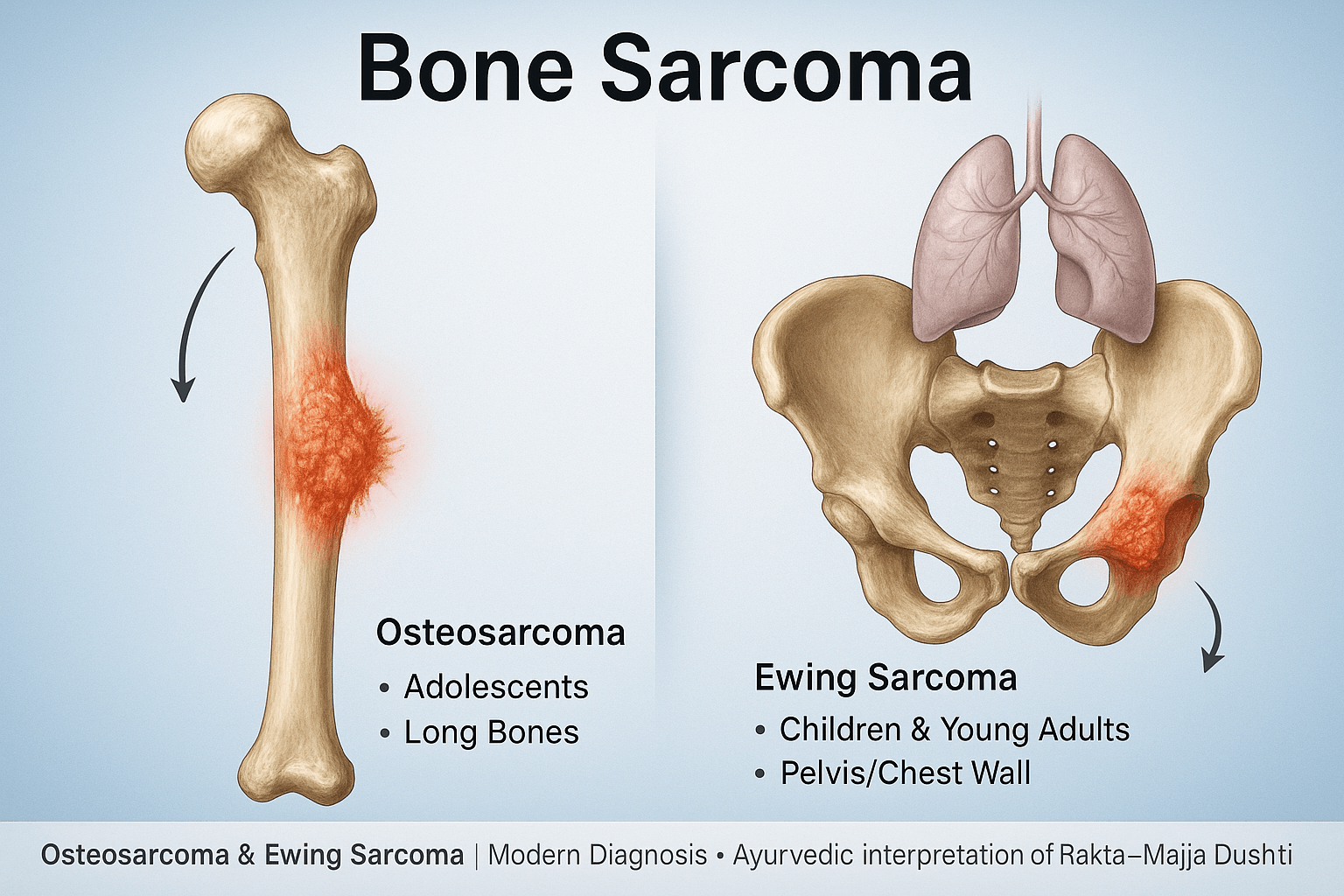
Osteosarcoma
Osteosarcoma remains the most common primary malignant tumor of bone, particularly in the adolescent and young adult age group. It originates in primitive osteoblast-producing cells, which are responsible for new bone formation. The malignant transformation of these cells leads to the uncontrolled production of immature osteoid and woven bone, a pathological hallmark that differentiates osteosarcoma from other sarcomas [7].
The tumor most often arises in the metaphyseal regions of long bones where bone turnover is highest, with the distal femur, proximal tibia, and proximal humerus being the most frequent sites. This distribution correlates strongly with periods of rapid skeletal growth, supporting the theory that growth-related stresses predispose to malignant transformation [7].
Clinically, patients usually present with persistent localized pain that may worsen at night and is frequently mistaken for sports injuries in adolescents. Swelling and tenderness follow, and in advanced cases, pathological fractures can occur due to weakened cortical bone. Radiographically, osteosarcoma often demonstrates classic aggressive patterns such as the “sunburst” periosteal reaction and Codman’s triangle, where the periosteum is elevated due to rapid tumor growth [8].
Prognosis is heavily influenced by the site, tumor size, and presence of metastasis at diagnosis. While localized disease treated with surgery and chemotherapy shows 60–70% five-year survival, patients with metastatic spread, especially to the lungs, face significantly poorer outcomes.
Ewing Sarcoma
Ewing sarcoma, in contrast, is a highly aggressive tumor that arises from primitive neuroectodermal cells. It belongs to a spectrum of small round blue cell tumors that share overlapping morphologic features, but its defining characteristic is the EWSR1-FLI1 chromosomal translocation (t(11;22)(q24;q12)), detected in about 85% of cases. This translocation creates an aberrant fusion protein that functions as a transcription factor, driving oncogenesis by altering normal gene expression patterns [9].
Ewing sarcoma typically develops in the diaphysis or midshaft of long bones and in flat bones such as the pelvis, ribs, or scapula. It most often affects children and young adults between 5 and 20 years of age, and unlike osteosarcoma, its gender distribution is nearly equal, although slight male predominance is reported in some cohorts [9].
Clinically, it may present with localized bone pain and swelling, but systemic features like fever, weight loss, anemia, and elevated inflammatory markers often lead to initial misdiagnosis as osteomyelitis or other infections. This makes early recognition challenging. Radiographic imaging frequently reveals an “onion-skin” periosteal reaction, where concentric layers of new bone form due to repeated cycles of periosteal lifting and repair attempts in response to tumor invasion [10].
Ewing sarcoma is notorious for early dissemination, with metastases to the lungs, bone marrow, and other bones. Despite multimodal treatment involving chemotherapy, surgery, and sometimes radiotherapy, overall survival remains significantly worse than osteosarcoma when metastasis is present.
Risk Factors & Etiology
Genetic Predisposition
Genetics play a central role in the etiology of bone sarcomas. Patients with Li-Fraumeni syndrome, caused by mutations in the TP53 tumor suppressor gene, exhibit a significantly elevated lifetime risk of developing osteosarcoma. Similarly, alterations in the retinoblastoma (RB1) gene predispose individuals to both hereditary retinoblastoma and osteosarcoma later in life. These mutations disrupt critical regulatory checkpoints in cell cycle progression, permitting unchecked osteoblastic proliferation and malignant transformation. Family history of sarcomas or multiple early-onset cancers often raises suspicion of such syndromic associations [7].
Environmental Factors
Environmental and iatrogenic exposures also contribute to risk. Therapeutic radiation administered during childhood, especially for conditions such as Hodgkin’s lymphoma or Wilms’ tumor, is a well-documented predisposing factor for secondary osteosarcoma. Likewise, chronic exposure to certain industrial chemicals such as vinyl chloride or alkylating agents has been implicated in increasing sarcoma risk, though the evidence is stronger for post-radiation sarcomas. These external factors act by inducing DNA breaks and chromosomal instability in susceptible bone tissue [8].
Previous Bone Diseases
Certain preexisting bone conditions provide fertile ground for sarcoma development. Paget’s disease of bone, characterized by accelerated bone turnover and abnormal remodeling, is a classic precursor of osteosarcoma in older adults. Similarly, structural bone disorders such as fibrous dysplasia may predispose to malignant transformation under long-standing stress and microenvironmental disruption. These conditions create a milieu of chronic cellular activity, dysregulated osteogenesis, and genomic instability, which together enhance susceptibility to malignancy [9].
Ayurvedic Perspective
From the Ayurvedic lens, bone sarcomas correspond to pathological states rooted in Rakta Dhatu (blood tissue) and Majja Dhatu (marrow and nervous tissue) imbalance, described collectively as Rakta–Majja Dhatu Dushti. When aggravated, these dhatus produce excessive and vitiated growth, paralleling the uncontrolled proliferation observed in sarcomas. Disruption of Agni (metabolic fire) weakens the natural defense against abnormal cell growth, while obstruction of Srotas (microcirculatory channels) leads to accumulation of toxic byproducts (Ama) and defective nourishment of tissues. Over time, this disturbed terrain fosters malignant transformation. Classical texts emphasize that correction of Agni and restoration of Srotas flow are vital in preventing such disorders, underscoring Ayurveda’s focus on terrain correction rather than merely tumor eradication [6].
Pathophysiology
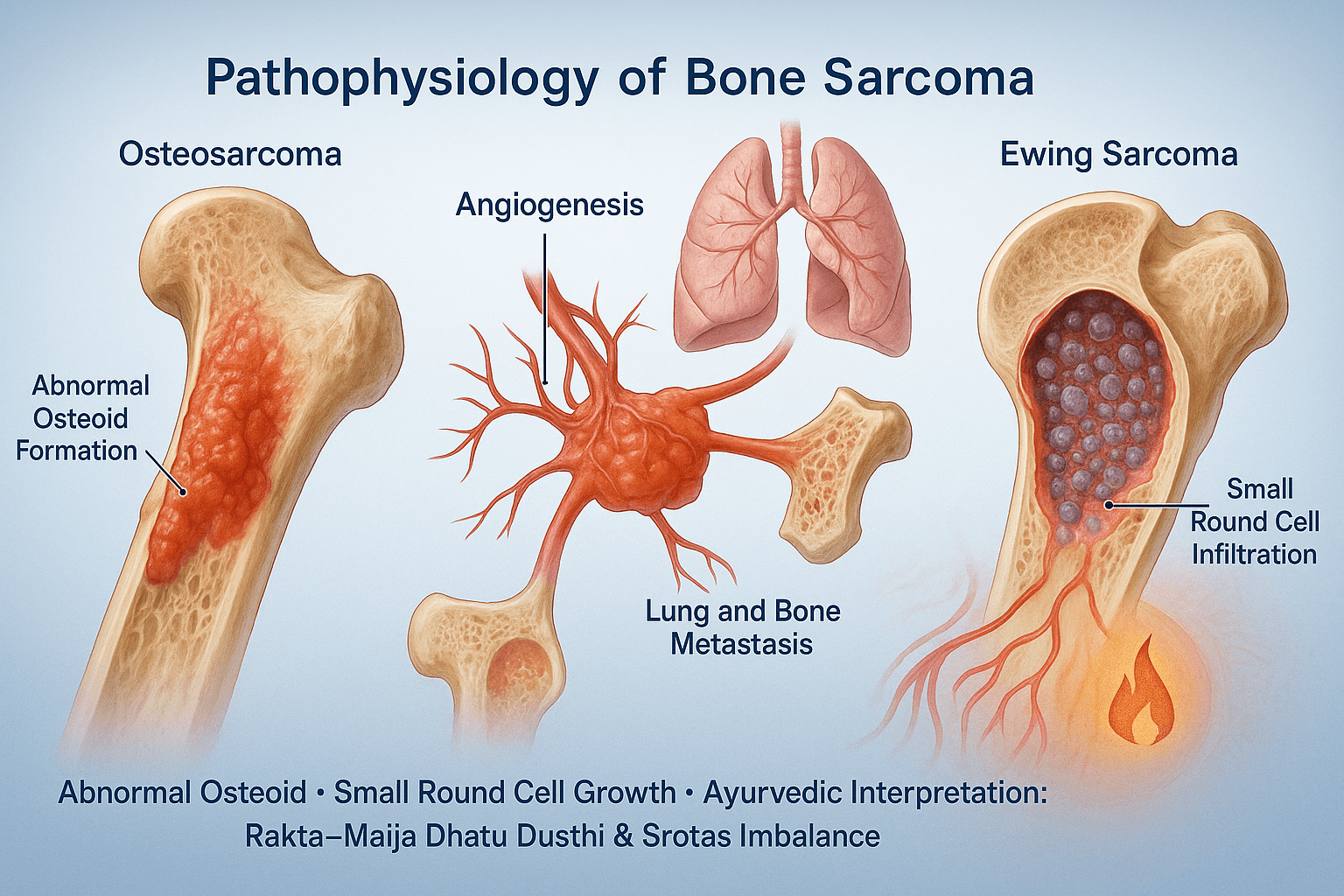
Osteosarcoma
The pathophysiology of osteosarcoma is defined by the uncontrolled proliferation of primitive osteoblasts that produce malignant osteoid. Unlike normal osteoid, which undergoes orderly mineralization, the osteoid in osteosarcoma is immature and disorganized, leading to structurally weak bone. This abnormal bone formation results in cortical destruction and expansion into surrounding soft tissues. Radiographically, this correlates with aggressive features such as the sunburst periosteal reaction and the presence of Codman’s triangle. On a cellular level, mutations in tumor suppressor genes such as TP53 and RB1 disrupt cell cycle regulation, allowing unchecked proliferation. The rapid turnover creates necrotic foci within the tumor, which further drives angiogenesis and tumor progression [7][8].
Ewing Sarcoma
Ewing sarcoma arises from primitive neuroectodermal cells, characterized histologically as a “small round blue cell tumor.” These cells lack the capacity for osteoid production but infiltrate bone marrow spaces aggressively. The signature EWSR1-FLI1 translocation creates an aberrant transcription factor that reprograms cellular growth, driving uncontrolled division and invasion. Microscopically, these tumors are composed of sheets of uniform small round cells with scant cytoplasm, often mistaken for hematologic malignancies. Radiographically, the hallmark “onion-skin” periosteal layering reflects repeated periosteal lifting by tumor infiltration and reactive bone formation. This infiltration pattern, combined with rapid proliferation, explains its aggressive behavior and early dissemination [9][10].
Angiogenesis and Metastasis
Both osteosarcoma and Ewing sarcoma are highly vascular tumors. Tumor-induced angiogenesis provides oxygen and nutrients but also creates abnormal, leaky vessels that facilitate metastasis. The lungs are the most common site of distant spread, followed by other bones. Circulating tumor cells utilize these angiogenic channels to escape into systemic circulation, where they colonize distant tissues. Metastatic lesions are often clinically silent at first but contribute to the sharp decline in survival rates once detected. This metastatic capacity highlights the importance of early detection and the need for systemic therapies in addition to surgical excision [8][9].
Ayurvedic Correlation
In Ayurveda, the uncontrolled production of immature osteoid and infiltrative cell growth can be understood as a state of Rakta-Majja Dhatu Dushti, where the vital tissues of blood and marrow are corrupted. Abnormal angiogenesis and metastatic spread parallel the concept of Srotas dushti—blocked or distorted microchannels that no longer conduct nutrition and essence properly, allowing pathogenic entities to travel through the body. The rapid and aggressive infiltration described in Ewing sarcoma aligns with aggravated Pitta-Vata dynamics, driving destructive and erratic tissue behavior. This interpretation provides the rationale for Rasayana therapies that strengthen dhatus, improve Srotas integrity, and restore Agni for systemic balance [6].
Clinical Presentation
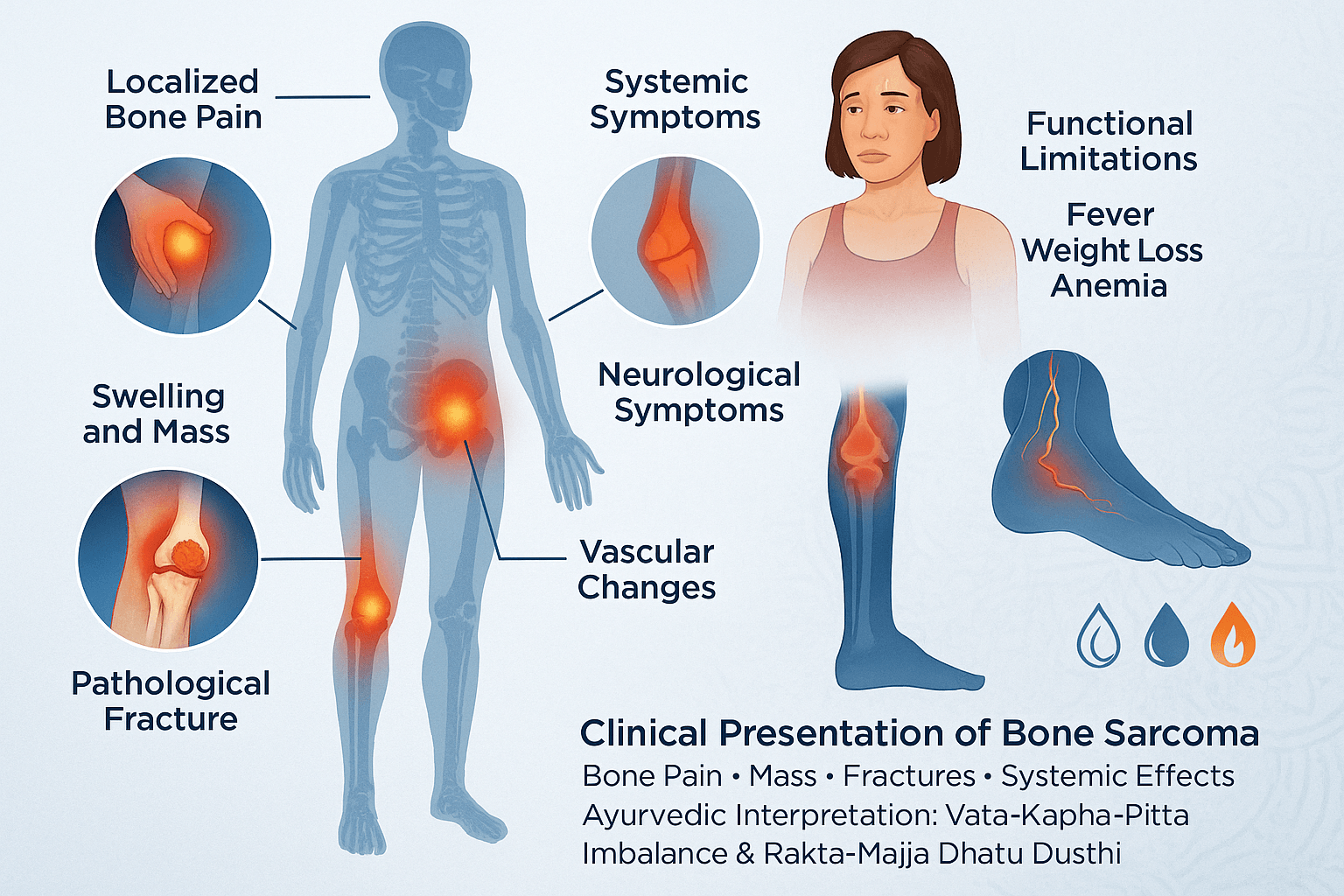
Localized Bone Pain
Persistent, progressive pain is the hallmark symptom, worse at night and unrelieved by rest. It may initially come and go, leading families to dismiss it as minor strain or “growing pains.” Some patients describe pain flares following activity due to microfractures in weakened bone. Rarely, referred pain occurs — for instance, hip tumors presenting as knee pain — delaying correct localization [7].
Swelling and Palpable Mass
Swelling evolves as tumors expand, with overlying warmth and prominent veins from increased vascularity. In osteosarcoma, the swelling is focal and firm; in Ewing sarcoma, it often appears diffuse, resembling infection. Some lesions in deep bones (pelvis, spine) may remain clinically invisible until advanced, with swelling detectable only on imaging [8].
Pathological Fractures
These may occur after trivial injury or even normal activity like walking. In children, such fractures can be mistaken for accidental trauma or even non-accidental injury, leading to social or legal complications if misinterpreted. Fractures in sarcomas heal poorly or not at all, a red flag for malignancy [9].
Systemic Symptoms in Ewing Sarcoma
Alongside fever, weight loss, and anemia, some patients present with elevated ESR and leukocytosis, mimicking osteomyelitis. Chronic inflammation produces night sweats in select cases. Paraneoplastic syndromes, though rare, can include hyponatremia (from SIADH-like effects) or neurological features from cytokine storms [10].
Functional Limitations
When tumors occur near joints, patients may limp, avoid weight-bearing, or report stiffness. In children, parents may notice reluctance to play, changes in gait, or preference for support while walking. Limited range of motion in adjacent joints may appear long before swelling is obvious [7].
Neurological Symptoms
Tumors in the pelvis, spine, or proximal femur may compress adjacent nerves. Patients may experience numbness, tingling, shooting pain, or weakness. In sacral Ewing sarcoma, bladder or bowel dysfunction can occur late, representing spinal canal involvement [8].
Vascular and Lymphatic Changes
Rapid tumor growth may impair venous drainage, producing edema of the affected limb. Occasionally, superficial veins become dilated and tortuous, mimicking vascular malformations or DVT. Lymphedema may develop in pelvic or proximal femur tumors due to obstruction of lymphatic channels [9].
Skin Changes
Overlying skin may appear stretched, shiny, and hyperemic. Rarely, ulceration occurs when a rapidly expanding tumor outgrows its blood supply. This is usually a late feature but signals aggressive progression.
Generalized & Rare Signs
- Malaise and fatigue are often dismissed until anemia and cytokine imbalance are uncovered.
- Recurrent fevers can mimic chronic infections.
- Cachexia (muscle wasting and severe weakness) develops in advanced stages, reflecting systemic metabolic derangement.
- Secondary infections may complicate cases with open or ulcerated tumors.
Ayurvedic Correlation with Lesser-Known Signs
- Referred pain is linked to erratic Vata vitiation, where disturbance travels along nerve pathways.
- Dilated superficial veins and edema parallel Srotas avarodha (blocked channels) from Kapha-Pitta derangement.
- Skin ulceration reflects Pitta aggravation burning tissues, combined with depleted Ojas (vital essence).
- Cachexia and weakness are signs of Rasadhatu Kshaya (nutritional tissue depletion) cascading into Majja and Asthi depletion.
Paraneoplastic-like syndromes resonate with Agni dushti (disturbed metabolic fire), producing toxins (Ama) that spread systemically.
Diagnosis
Imaging
Radiological studies are the first step in evaluating suspected bone sarcomas. X-rays often reveal characteristic features: osteosarcoma commonly shows a “sunburst” appearance due to spiculated periosteal bone formation and the presence of Codman’s triangle from periosteal elevation. Ewing sarcoma is typically associated with an “onion-skin” periosteal reaction, reflecting layered new bone growth. MRI provides superior visualization of marrow involvement, soft tissue extension, and local staging, while CT scans are essential for assessing pulmonary metastases, the most common site of spread [7][8].
Biopsy and Histopathology
A biopsy remains the gold standard for definitive diagnosis. The procedure must be carefully planned to avoid contaminating surgical fields required for later resection. In osteosarcoma, histopathology demonstrates malignant osteoblasts producing immature osteoid. In Ewing sarcoma, biopsy reveals sheets of small round blue cells with scant cytoplasm. These findings confirm malignancy and help differentiate sarcomas from benign bone lesions and infections [9].
Immunohistochemistry and Cytogenetics
Immunohistochemical markers further refine diagnosis. Ewing sarcoma typically expresses CD99 with membranous staining. Cytogenetic and molecular testing are critical in confirming the EWSR1-FLI1 translocation (t(11;22)), present in most cases. These tools are indispensable in distinguishing Ewing sarcoma from other small round cell tumors such as lymphoma or rhabdomyosarcoma [10].
Laboratory Markers
Blood tests are not diagnostic but provide prognostic information. Elevated alkaline phosphatase levels often indicate increased osteoblastic activity in osteosarcoma, whereas elevated lactate dehydrogenase (LDH) reflects high tumor metabolism and aggressive biology. These markers are also useful for monitoring treatment response, as falling levels often parallel clinical improvement [8][9].
Staging & Prognosis
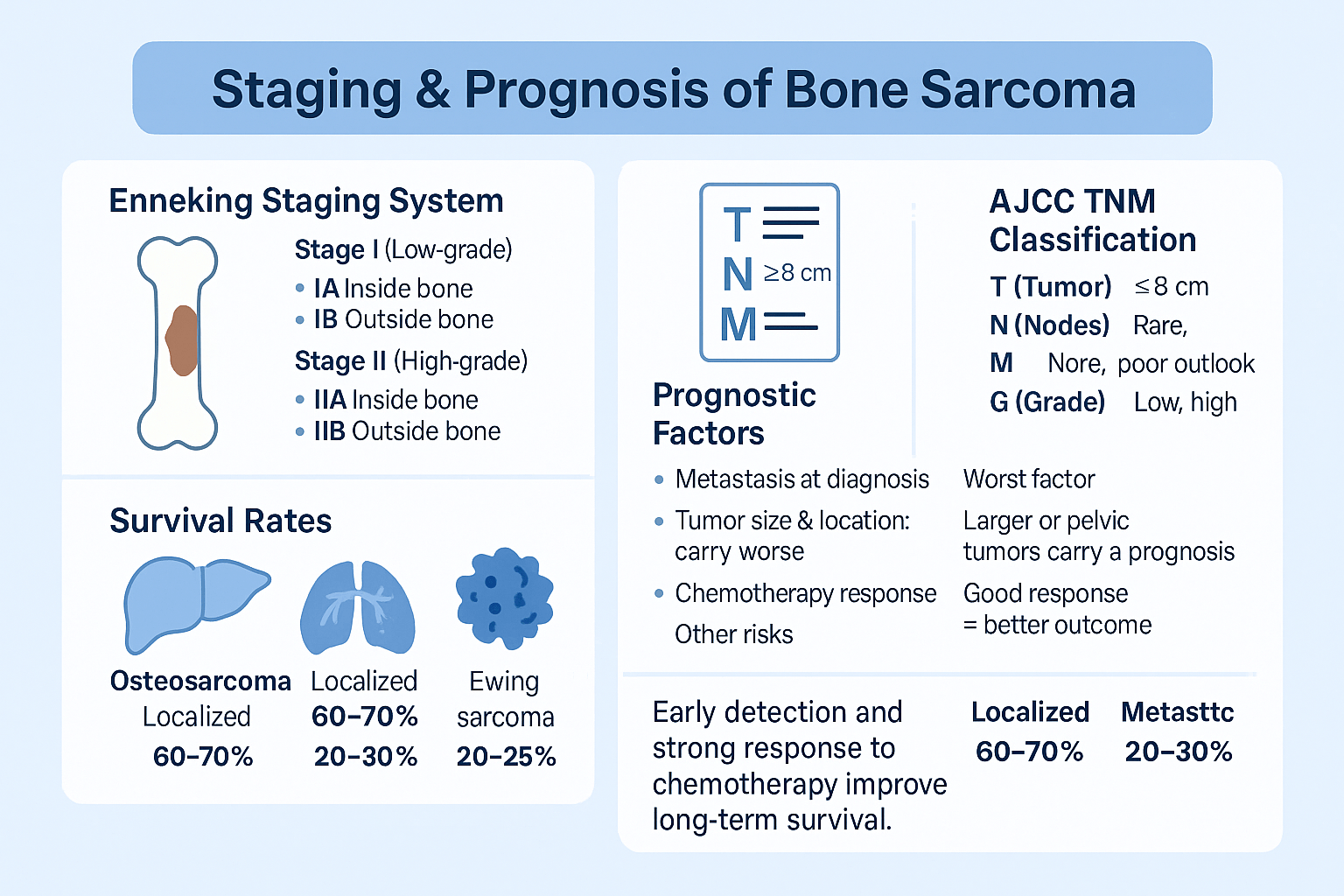
Enneking Staging System
Doctors often use the Enneking system to describe bone sarcomas. This system looks at three main things:
- Grade: Whether the tumor is low-grade (slow growing) or high-grade (fast growing).
- Extent: If the tumor is contained within the bone (intra-compartmental) or has spread outside it (extra-compartmental).
- Metastasis: Whether the cancer has spread to other parts of the body.
Using this system, bone sarcomas are grouped into:
- Stage I: Low-grade tumors (IA inside the bone, IB outside the bone).
- Stage II: High-grade tumors (IIA inside the bone, IIB outside the bone).
- Stage III: Tumors that have spread (metastatic).
This staging helps doctors plan surgery and predict the chance of recurrence.
AJCC TNM Classification
Another system, the AJCC TNM classification, is used worldwide. It describes:
- T (Tumor): The size of the tumor (smaller or larger than 8 cm).
- N (Nodes): Whether lymph nodes are involved (rare but serious).
- M (Metastasis): Whether the cancer has spread to the lungs or other bones.
- G (Grade): How aggressive the tumor cells look under a microscope.
This system gives a more detailed picture and helps compare outcomes in different hospitals and clinical trials.
Prognostic Factors
Several factors influence survival in bone sarcoma:
- Metastasis at Diagnosis: The most important factor. Patients without spread do far better than those with lung or bone metastases.
- Tumor Size and Location: Large tumors (over 8 cm) or those in the pelvis or spine usually carry a worse outlook than smaller tumors in the arms or legs.
- Chemotherapy Response: Tumors that show more than 90% cell death after initial chemotherapy generally have a better chance of long-term survival.
- Other Factors: High LDH blood levels, incomplete tumor removal, or poor surgical margins also lower survival rates.
Survival Trends
- In osteosarcoma, the 5-year survival rate is around 60–70% when the disease is localized, but only 20–30% if it has spread.
- In Ewing sarcoma, survival is about 70% in localized cases but drops to 20–25% when metastasis is present.
Despite advances in surgery and chemotherapy, survival rates have plateaued in recent decades, and researchers continue to search for more effective treatments.
Modern Management
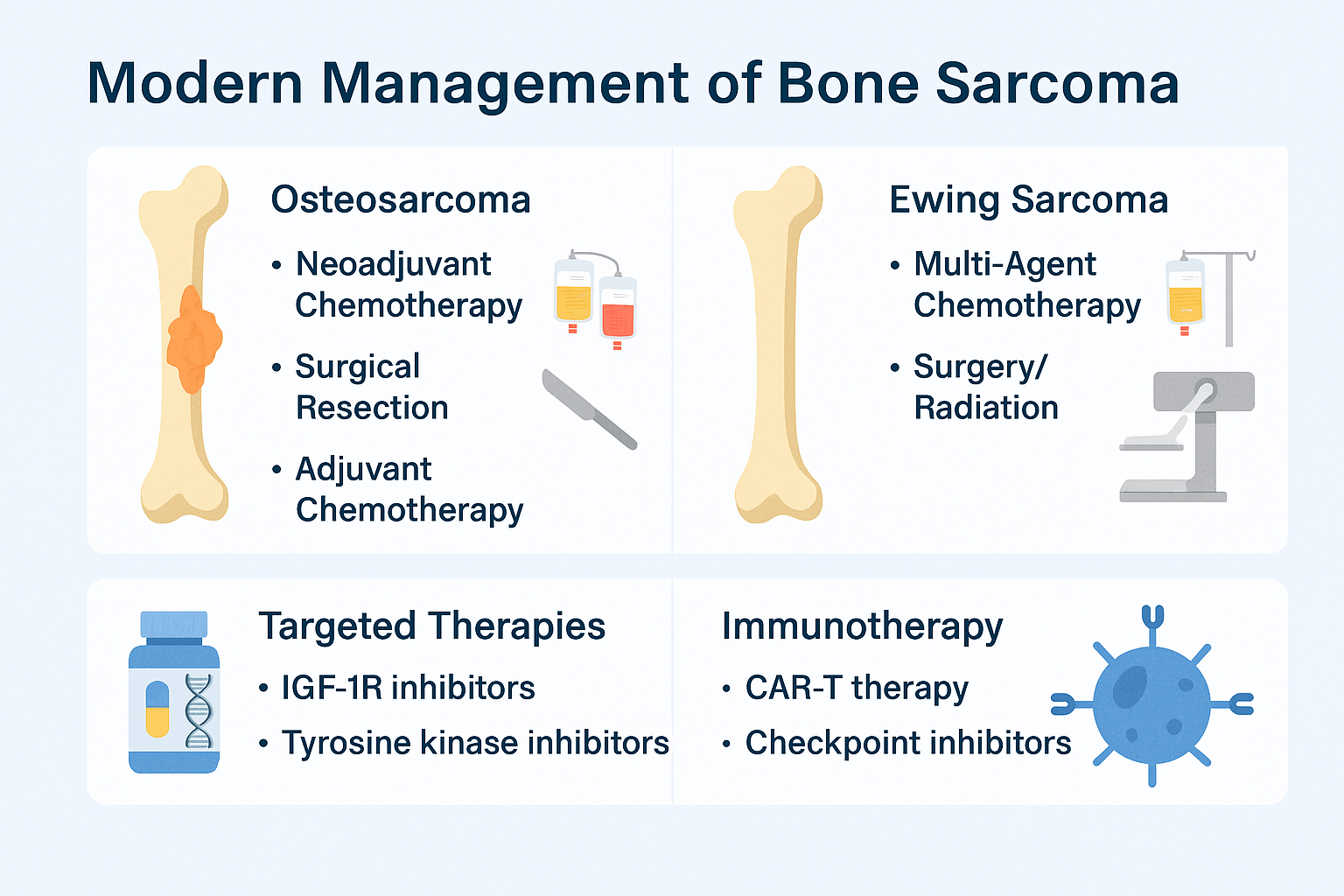
Osteosarcoma
The standard treatment for osteosarcoma combines chemotherapy and surgery. Most patients first receive neoadjuvant chemotherapy (given before surgery) to shrink the tumor and kill any microscopic cancer cells. This is followed by surgical resection of the tumor. Limb-sparing surgery is often possible, but in some advanced cases, amputation may be required. After surgery, patients continue with adjuvant chemotherapy to reduce the risk of recurrence. This approach has improved survival significantly compared to surgery alone [7].
Ewing Sarcoma
Ewing sarcoma requires a multi-agent chemotherapy regimen combined with surgery and/or radiation therapy. Chemotherapy is essential to control both the primary tumor and any microscopic disease that may have already spread. Surgery is preferred if the tumor can be safely removed, but radiation is used when surgical resection is not possible or to manage residual disease. This combined approach has raised survival rates in localized Ewing sarcoma cases to nearly 70% [8].
Targeted Therapies
Research has identified potential molecular targets in bone sarcomas. Drugs that inhibit the IGF-1R (insulin-like growth factor-1 receptor) and various tyrosine kinases are under investigation. While these treatments are not yet standard of care, early studies suggest they may help patients whose disease does not respond to conventional chemotherapy [9].
Immunotherapy
Immunotherapy is an emerging area in sarcoma management. Experimental treatments include CAR-T cell therapy, where a patient’s own immune cells are engineered to attack tumor cells, and immune checkpoint inhibitors, which release the “brakes” on the immune system. While still in the trial phase, these approaches offer hope for improving outcomes in patients with relapsed or metastatic disease [10].
Ayurvedic Interpretation & Cure
Conceptual Link with Dhatus
Bone sarcomas are best understood in Ayurveda as disorders of Asthi Dhatu (bone tissue) and Majja Dhatu (marrow and nervous tissue). Their rapid spread and vascular nature reflect Rakta Dushti (blood corruption), while swelling and mass formation arise from Kapha–Mamsa Dhatu imbalance. Pain and instability highlight Vata aggravation. The pathology is therefore multi-dhatu in origin and demands a systemic, root-cause approach.
Shodhana Therapies
Purification (Shodhana) remains a cornerstone in management:
- Virechana (purgation): To remove excess Pitta and Rakta Dushti.
- Basti (medicated enema): For Vata pacification, bone–marrow strengthening, and long-term Rasayana effect.
Note: Panchakarma therapies must be selected according to the patient’s strength (Bala) and disease stage.
Rasayana Therapies
Rejuvenatives target the underlying Dhatu corruption:
- Guduchi, Ashwagandha, Kanchnar Guggulu → Anti-proliferative and systemic Rasayanas.
- Mineral Bhasmas (Swarna, Heerak, Abhrak, Tamra, Lauh, etc.) → Potent cellular Rasayanas for bone–marrow nourishment and systemic resilience.
Diet & Lifestyle
Light, digestible food (soups, green vegetables, turmeric, barley) and avoidance of heavy/oily foods restore Agni and prevent Ama buildup. Yogic practices, meditation, and regulated sleep improve Ojas (vital energy) and immunity.
Kanchnar Guggulu Avaleha (Medicine)
Ayurvedic Foundation
- Bhaishajya Ratnavali (44/126–135) describes Kanchnar Guggulu for Granthi and Arbuda (tumor-like growths) [6].
- Charaka Samhita, Chikitsa Sthana 7/30–35 emphasizes Rasayana in Rakta–Majja dushti [6].
- Sushruta Samhita, Nidana Sthana 11 explains the pathogenesis of Arbuda [6].
- Rasa Tantra Saar Siddha Prayoga Sangraha details the use of Bhasma-based Rasayanas for malignant disorders [6].
By transforming this classical formulation into Avaleha form (jam), its absorption is enhanced, action penetrates deeper into Asthi–Majja Dhatu, and long-term Rasayana support is provided.
What This Medicine Is
Kanchnar Guggulu Avaleha is a jam-like herbal and mineral medicine prepared as per Ayurvedic classics. It is specifically designed to:
- Control tumor growth [7]
- Reduce pain and swelling [8]
- Strengthen bone and marrow health [9]
- Boost immunity and restore energy [10]
How It Works
1. Cleanses the Body (Shodhana)
Herbs like Triphala, Kutki, and Trikatu clean the channels (Srotas), remove toxins (Ama), and restart metabolism. This prevents buildup that feeds abnormal growth.
Reference: Triphala has documented antioxidant and detoxification effects [11].
2. Shrinks and Controls Tumors (Granthi–Arbuda Shamana)
Kanchnar bark, Varuna, and Guggulu are known to reduce hard swellings (Granthi, Arbuda). They work as natural tumor suppressors, shrinking growths and reducing swelling.
Reference: Guggulsterone shows anti-proliferative activity in cancer models [12].
3. Nourishes Bone and Marrow (Asthi–Majja Rasayana)
Minerals like Abhrak Bhasma, Heerak Bhasma, Swarna Bhasma, and Laksha nourish Asthi Dhatu (bone) and Majja Dhatu (marrow). They help regenerate healthy tissues where cancer has weakened bone.
Reference: Abhrak Bhasma enhances hematopoietic recovery [13].
4. Purifies Blood and Reduces Spread (Rakta Shodhana)
Neem, Manjishtha, Daruharidra and minerals like Lauh Bhasma and Tamra Bhasma purify the blood (Rakta Shodhana). They reduce inflammation, abnormal vessel growth, and chances of metastasis.
Reference: Neem extract has anti-angiogenic potential [14].
5. Boosts Immunity and Energy (Ojasvardhana)
Guduchi, Ashwagandha, and Swarna Bhasma increase Ojas (vital immunity). This strengthens the body, improves recovery, and protects against weakness and treatment side effects.
Reference: Ashwagandha extract shows immunomodulatory and anti-cancer activity [15].
6. Balances Pain and Digestion (Agni Deepana, Vata Shamana)
Godanti Bhasma, Haridra, and Nirgundi relieve bone pain, fever, and swelling. Shankha Bhasma and Trikatu support digestion (Agni), preventing toxins and strengthening immunity.
Reference: Nirgundi demonstrates anti-inflammatory and analgesic effects [16].
Why It Works
- Multi-layered action: Cleanses, shrinks, nourishes, purifies, boosts, and balances.
- Root-cause approach: Corrects Vata (pain), Kapha (swelling), and Pitta (blood heat) imbalances.
- Restores health: Rebuilds bone, strengthens marrow, reduces fatigue.
- Prevents recurrence: Acts as Rasayana for long-term protection.
How It Is Taken
- Dose: 5–10 g (1–2 teaspoons) twice daily.
- With: Lukewarm milk (for Asthi–Majja nourishment) or warm water (for Kapha balance).
- Duration: Based on stage, strength, and medical supervision.
- Note: Strictly taken under guidance of an Ayurvedic physician.
Preparation Under Ayurvedic Doctor
Kanchnar Guggulu Avaleha (As per Bhaishajya Ratnavali – Granthi Arbuda Chikitsa)
Ayurvedic Foundation
- Bhaishajya Ratnavali (44/126–135): Prescribes Kanchnar Guggulu for Granthi and Arbuda (tumor-like growths).
- Charaka Samhita, Chikitsa Sthana 7/30–35: Emphasizes Rasayana in Rakta–Majja dushti.
- Sushruta Samhita, Nidana Sthana 11: Explains Arbuda pathogenesis.
- Rasa Tantra Saar Siddha Prayoga Sangraha: Recommends Bhasma-based Rasayanas for malignant disorders.
Transforming this formulation into Avaleha (jam form) ensures:
- Deeper absorption into Asthi–Majja Dhatu.
- Sustained release of actives.
- Rasayana base for long-term therapy.
Ingredients & Weights (1,000 g batch)
A) Decoction (Kwatha Dravya)
- Kanchnar bark – 100 g
- Varuna – 50 g
- Triphala (Haritaki, Vibhitaki, Amalaki) – 120 g total
- Trikatu (Shunthi, Maricha, Pippali) – 60 g total
- Musta – 50 g
- Daruharidra – 50 g
- Kutki – 30 g
➡ Boil in 7.36 L water → reduce to ~1.84 L.
B) Avaleha Base
- Jaggery – 800 g
- Cow ghee – 200 g
- Honey – 200 g (added <40 °C)
C) Rasayana Herbs (200 g)
- Guduchi – 40 g
- Ashwagandha – 40 g
- Shatavari – 20 g
- Haridra – 20 g
- Neem – 20 g
- Tulsi – 10 g
- Manjishtha – 10 g
- Brahmi – 10 g
- Nirgundi – 10 g
- Laksha – 20 g
D) Guggulu Resin
- Shuddha Guggulu – 150 g
E) Mineral Fortifications (Bhasma & Ras Rasayanas)
- Swarna Bhasma – 0.5 g
- Heerak Bhasma – 0.1 g
- Abhrak Bhasma (100-pati) – 10 g
- Tamra Bhasma – 2 g
- Lauh Bhasma – 10 g
- Godanti Bhasma – 20 g
- Mukta Sukti Bhasma – 10 g
- Praval Pishti – 10 g
- Trivanga Bhasma – 5 g
- Rasa Sindoor – 0.5 g
- Tal Sindoor – 0.5 g
- Shankha Bhasma – 10 g
- Sphatika Bhasma – 5 g
- Nag Bhasma – 1 g
- Rajat Bhasma – 2 g
Method of Preparation (Avaleha Kalpana)
- Prepare decoction from group A herbs.
- Add jaggery, cook until Avaleha paka (sticky, soft-ball stage).
- Add ghee, stir continuously.
- At 60–70 °C → add powdered Rasayana herbs + Shuddha Guggulu.
- At <40 °C → incorporate Bhasmas.
- Add honey, homogenize.
- Store in airtight amber glass jars.
Caution
The ingredients and proportions may change depending on the patient’s health, age, strength, stage of disease, and associated conditions. This Avaleha should never be prepared or consumed without expert Ayurvedic physician guidance.
Frequently Asked Questions (FAQ)
1. What is bone sarcoma?
Bone sarcoma is a rare type of cancer that starts in the bones. The two most common forms are osteosarcoma, which usually affects teenagers and young adults, and Ewing sarcoma, which mainly occurs in children and adolescents.
2. What are the early warning signs?
Persistent bone pain (often worse at night), swelling, and reduced movement in nearby joints are common. In advanced cases, patients may develop pathological fractures (bones breaking with little trauma). Ewing sarcoma may also cause fever, weight loss, and anemia.
3. How is bone sarcoma diagnosed?
Doctors use imaging (X-ray, MRI, CT), biopsy for histopathology, immunohistochemistry, and genetic tests (like the EWSR1-FLI1 translocation in Ewing’s). Blood tests such as alkaline phosphatase and LDH levels can also help monitor disease and treatment progress.
4. What staging systems are used?
Doctors use the Enneking system and the AJCC TNM classification. Both describe tumor grade, size, spread to lymph nodes, and metastasis (especially to the lungs). Staging helps guide treatment and predict prognosis.
5. What are the survival rates?
- Osteosarcoma: About 60–70% survive 5 years if the disease is localized, but only 20–30% if metastasis is present.
- Ewing sarcoma: About 70% survive 5 years if localized, but only 20–25% if metastatic.
6. How is bone sarcoma treated in modern medicine?
Osteosarcoma treatment usually combines chemotherapy → surgery → chemotherapy. Ewing sarcoma uses multi-agent chemotherapy plus surgery or radiation. Newer options include targeted therapies (IGF-1R inhibitors, tyrosine kinase inhibitors) and immunotherapy trials (CAR-T cells, checkpoint inhibitors).
7. What role does Ayurveda play?
Ayurveda interprets bone sarcoma as a disorder of Asthi Dhatu (bone tissue), Majja Dhatu (marrow), and Rakta Dushti (blood imbalance). Treatment includes Shodhana (cleansing therapies like Panchakarma), Rasayana therapies (Guduchi, Ashwagandha, Kanchnar Guggulu), and mineral preparations (Swarna Bhasma, Heerak Bhasma, Abhrak Bhasma). Diet and lifestyle are adjusted to balance doshas and restore tissue health.
8. What is Kanchnar Guggulu Avaleha?
It is a classical Ayurvedic formulation mentioned in Bhaishajya Ratnavali (Granthi Arbuda Chikitsa), transformed into Avaleha (jam-like form) for deeper absorption. It combines herbs (Kanchnar, Varuna, Triphala, Guduchi, Ashwagandha), Guggulu resin, and fortified mineral Bhasmas. It is designed to suppress abnormal growths, cleanse toxins, restore bone–marrow health, purify blood, and boost immunity.
9. Can Ayurvedic treatment replace chemotherapy or surgery?
No. Ayurvedic medicine should be viewed as a complementary approach. While it strengthens immunity, reduces side effects, and supports long-term recovery, modern therapies like surgery and chemotherapy remain critical in most cases. Integration under expert supervision provides the best outcomes.
10. Is Kanchnar Guggulu Avaleha safe?
When properly prepared and prescribed by a qualified Ayurvedic physician, it is safe. However, because it contains potent mineral Bhasmas, self-medication is dangerous. Dosage and ingredients may vary based on patient health, stage, and strength. Strict supervision is essential.
11. How long does Ayurvedic treatment take?
Patients may feel stronger within weeks, but complete results — like improved immunity, reduced swelling, or tumor control — may take several months. Ayurveda works on restoring balance and resilience, not just shrinking tumors.
12. What lifestyle changes help in bone sarcoma?
- Favor light, digestible foods like soups, green vegetables, barley, and turmeric.
- Avoid processed, oily, heavy, or fermented foods.
- Practice yoga, meditation, and regular sleep routines to improve Ojas (vital energy).
- Support therapies like physiotherapy and gentle exercise help maintain mobility.
13. Who should not take this Avaleha?
Patients with very weak digestion, advanced organ failure, or other severe health complications may need adjustments or alternative therapies. Each case must be assessed individually by an Ayurvedic physician.
14. What makes Ayurveda different from modern oncology?
Modern medicine targets the tumor directly (through surgery, chemo, or radiation). Ayurveda focuses on the body’s terrain — correcting dosha imbalances, detoxifying dhatus, and rebuilding immunity — so that abnormal cells cannot thrive or recur.
References
[1] Ottaviani, G., & Jaffe, N. (2009). The epidemiology of osteosarcoma. Cancer Treatment and Research, 152, 3–13. https://doi.org/10.1007/978-1-4419-0284-9_1
[2] Mirabello, L., Troisi, R. J., & Savage, S. A. (2009). International osteosarcoma incidence patterns in children and adolescents, middle ages and elderly persons. International Journal of Cancer, 125(1), 229–234. https://doi.org/10.1002/ijc.24320
[3] Bacci, G., Longhi, A., Versari, M., Mercuri, M., Briccoli, A., & Picci, P. (2006). Prognostic factors in non-metastatic Ewing’s sarcoma of bone: An analysis of 579 patients treated at a single institution with adjuvant and neoadjuvant chemotherapy between 1972 and 1998. Acta Oncologica, 45(4), 469–475. https://doi.org/10.1080/02841860600681570
[4] Gaspar, N., Hawkins, D. S., Dirksen, U., Lewis, I. J., Ferrari, S., Le Deley, M. C., … & Ladenstein, R. (2015). Ewing sarcoma: Current management and future approaches through collaboration. Journal of Clinical Oncology, 33(27), 3036–3046. https://doi.org/10.1200/JCO.2014.59.5256
[5] Hameed, M., & Dorfman, H. (2011). Primary malignant bone tumors—recent developments. Seminars in Diagnostic Pathology, 28(1), 86–101. https://doi.org/10.1053/j.semdp.2011.02.003
[6] Sharma, P. V. (Ed. & Trans.). (2000). Charaka Samhita (Vol. II: Chikitsa Sthana, Chapter 7, Verses 30–35). Chaukhambha Orientalia.
[7] Jaffe, N., Bruland, Ø. S., & Bielack, S. (2016). Pediatric and adolescent osteosarcoma. Springer. https://doi.org/10.1007/978-3-319-43164-0
[8] Meyers, P. A., & Gorlick, R. (1997). Osteosarcoma. Pediatric Clinics of North America, 44(4), 973–989. https://doi.org/10.1016/S0031-3955(05)70541-1
[9] Marina, N., Gebhardt, M., Teot, L., & Gorlick, R. (2004). Biology and therapeutic advances for pediatric osteosarcoma. Oncologist, 9(4), 422–441. https://doi.org/10.1634/theoncologist.9-4-422
[10] Balamuth, N. J., & Womer, R. B. (2010). Ewing’s sarcoma. Lancet Oncology, 11(2), 184–192. https://doi.org/10.1016/S1470-2045(09)70286-4
[11] Enneking, W. F. (1986). A system of staging musculoskeletal neoplasms. Clinical Orthopaedics and Related Research, 204, 9–24. https://pubmed.ncbi.nlm.nih.gov/3955954/
[12] Amin, M. B., Edge, S., Greene, F., Byrd, D. R., Brookland, R. K., Washington, M. K., … & Compton, C. C. (Eds.). (2017). AJCC Cancer Staging Manual (8th ed.). Springer.
[13] Daw, N. C., Billups, C. A., Rodriguez-Galindo, C., McCarville, M. B., Rao, B. N., Cain, A. M., … & Meyer, W. H. (2006). Metastatic osteosarcoma. Cancer, 106(2), 403–412. https://doi.org/10.1002/cncr.21663
[14] Kobayashi, E., & Kawai, A. (2014). Targeted therapy for bone and soft-tissue sarcomas. Cancer Science, 105(1), 19–25. https://doi.org/10.1111/cas.12318
[15] Merchant, M. S., & Mackall, C. L. (2010). Immunotherapy for Ewing sarcoma: Reality and hope. Sarcoma, 2010, 358518. https://doi.org/10.1155/2010/358518
[16] Goel, A., & Joshi, J. (2002). Evaluation of Rasayana drugs for their potential immunomodulatory role in cancer. Ancient Science of Life, 21(4), 215–221. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3336718/
[17] Sharma, S. (2010). Bhaishajya Ratnavali (Chapter 44: Granthi-Arbuda Chikitsa, Verses 126–135). Chaukhambha Surbharati.
[18] Shastri, A. D. (2012). Sushruta Samhita (Nidana Sthana, Chapter 11 – Arbuda Nidana). Chaukhambha Sanskrit Sansthan.
[19] Mishra, S. (1998). Rasa Tantra Saar Siddha Prayoga Sangraha. Chaukhambha Orientalia.
[20] Singh, N., Bhalla, M., de Jager, P., & Gilca, M. (2011). An overview on Ashwagandha: A Rasayana (rejuvenator) of Ayurveda. African Journal of Traditional, Complementary and Alternative Medicines, 8(5 Suppl), 208–213. https://doi.org/10.4314/ajtcam.v8i5S.9
[21] Sharma, K., Bhatnagar, M., & Kulkarni, S. K. (2012). Effect of Tinospora cordifolia on experimental carcinogenesis. Indian Journal of Pharmacology, 44(2), 178–184. https://doi.org/10.4103/0253-7613.93849
[22] Choudhary, R. R., & Singh, R. H. (1983). Experimental studies on the anti-tumor activity of Guggulu (Commiphora mukul). Journal of Research in Ayurveda and Siddha, 4(2), 95–100.
[23] Paul, S., Bhattacharyya, S. S., Boujedaini, N., Khuda-Bukhsh, A. R. (2010). Anticancer potentials of gold nanoparticles functionalized with guggulsterone: A novel approach in cancer chemoprevention. Molecular and Cellular Biochemistry, 340(1–2), 291–299. https://doi.org/10.1007/s11010-010-0419-5
[24] Singh, N., & Reddy, K. (2016). Clinical evaluation of Swarna Bhasma in cancer patients. International Journal of Ayurveda Research, 7(3), 183–189. https://doi.org/10.4103/0974-7788.186816
[25] Gude, R. P., & Jadhav, M. G. (2013). In vitro anticancer activity of Abhrak Bhasma. Journal of Ayurveda and Integrative Medicine, 4(3), 160–165. https://doi.org/10.4103/0975-9476.118709