- Anatomy and Physiology
- Pathophysiology of Interface Disorders
- Clinical Features and Symptoms
- Diagnostic Approaches
- Modern Management Strategies
- Ayurvedic Approaches To Cure
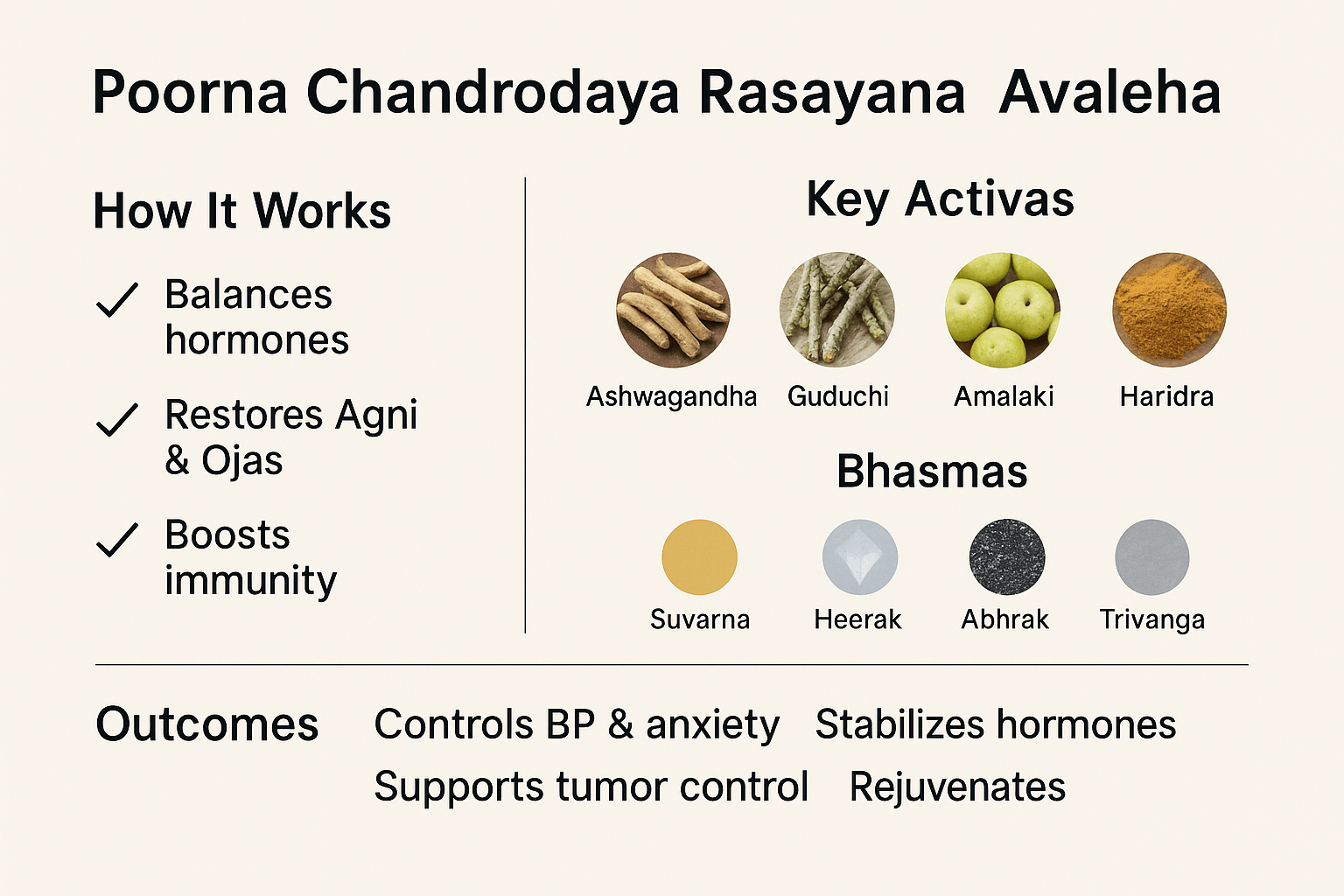
- Poorna Chandrodaya Rasayana Avaleha (Main Medicine To Cure)
- How It Works
- How It Cures
- Comprehensive Ingredient List To Prepare
- Preparation Method (Traditional)
- Dose & Duration
- Ayurvedic Rationale
- Disclaimer
- Frequently Asked Questions (FAQ)
- References
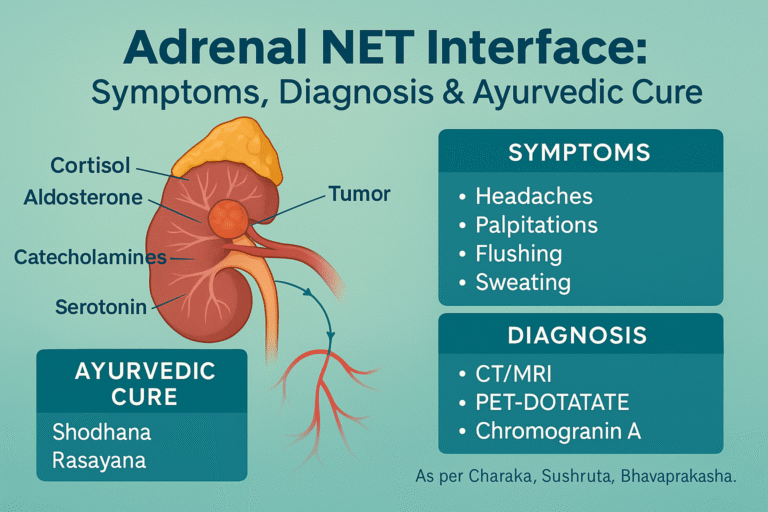
The adrenal–neuroendocrine tumor (NET) interface (Adrenal NET Interface) represents a unique zone where the boundaries of adrenal pathology and neuroendocrine neoplasia intersect. The adrenal glands, comprising the cortex and medulla, regulate vital functions through hormones such as cortisol, aldosterone, catecholamines, and androgens. Neuroendocrine tumors, on the other hand, originate from cells with both neural and endocrine features, producing a wide array of bioactive substances. When adrenal lesions demonstrate neuroendocrine activity, or when NETs involve the adrenal glands, patients often present with complex and overlapping clinical profiles that challenge conventional diagnostic frameworks [1].
The clinical importance of this interface lies in its diagnostic ambiguity and therapeutic implications. Disorders such as pheochromocytomas, paragangliomas, and mixed corticomedullary tumors exemplify the overlap. These conditions not only produce classical hormone excess syndromes (e.g., hypertension, Cushingoid features) but may also exhibit symptoms associated with neuroendocrine hypersecretion, such as flushing or chronic diarrhea. Such overlapping features demand precise biochemical evaluation, advanced imaging, and multidisciplinary care, as missed or delayed diagnoses may lead to severe cardiovascular complications, metabolic disturbances, or malignant transformation [2].
From an Ayurvedic perspective, this interface can be understood through the lens of Meda Dhatu (metabolic and adipose tissue), Rakta Dhatu (blood and vascular system), and Agni (digestive and metabolic fire). Dysregulation at this junction manifests as imbalances in Doshas—particularly aggravated Pitta and disturbed Vata—which may lead to symptoms like flushing, hypertension, anxiety, or wasting. Classical Ayurvedic texts describe related conditions under Raktapitta, Meda Dushti, and Vataja Unmada, emphasizing the interconnectedness of body systems and the need for treatments that restore Agni and strengthen Ojas. This holistic framework aligns with modern integrative strategies, offering a bridge between molecular endocrinology and traditional healing sciences [3].
Anatomy and Physiology
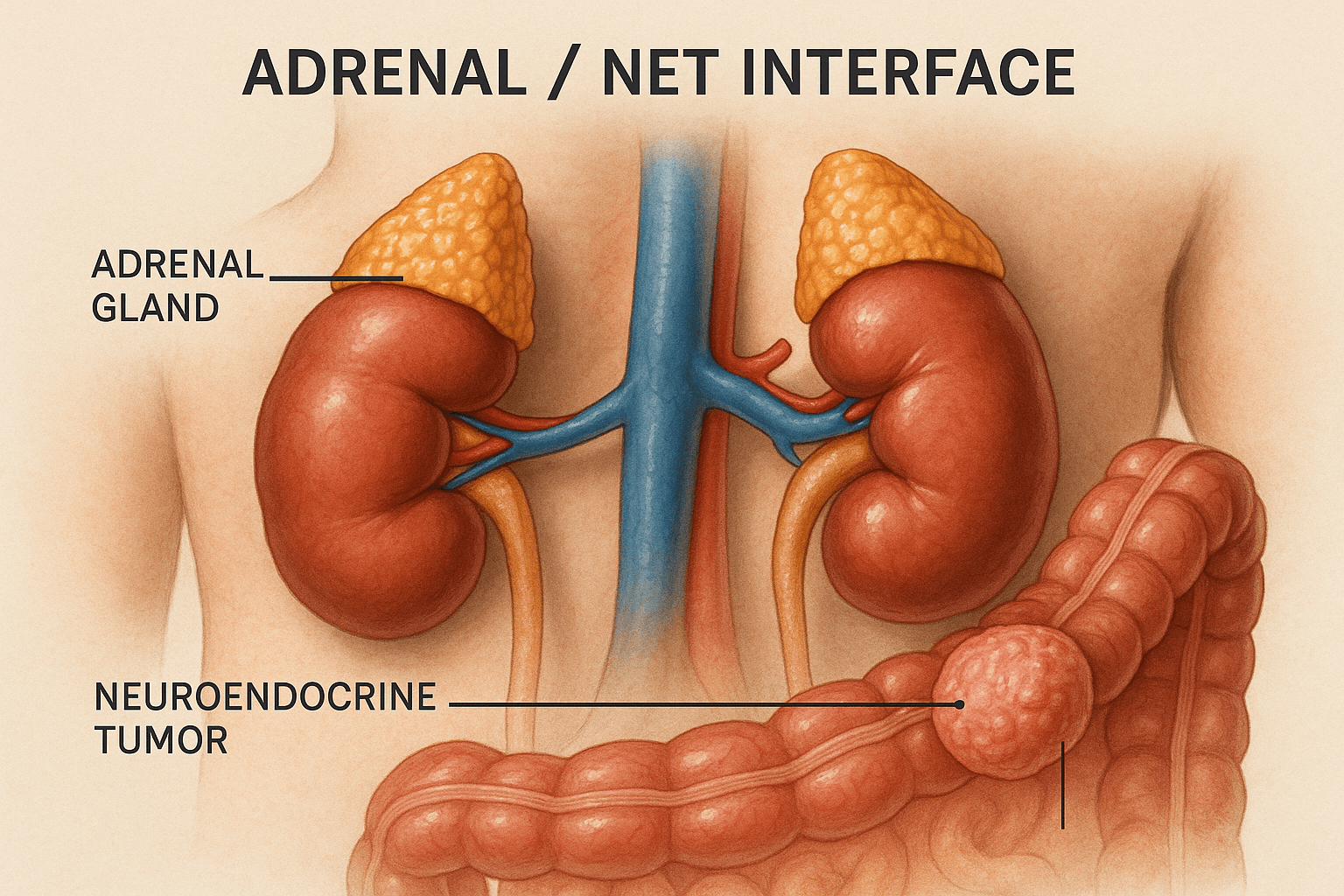
The adrenal glands are small, triangular organs located on the superior pole of each kidney, playing a central role in endocrine homeostasis. They consist of two distinct regions with separate embryological origins and functions. The adrenal cortex is divided into three zones: the zona glomerulosa, which secretes mineralocorticoids such as aldosterone for sodium and potassium balance; the zona fasciculata, which produces glucocorticoids like cortisol for metabolism and stress regulation; and the zona reticularis, which synthesizes adrenal androgens such as dehydroepiandrosterone (DHEA) [4]. The adrenal medulla, derived from neural crest tissue, produces catecholamines—epinephrine, norepinephrine, and dopamine—which are vital for the body’s acute stress responses and cardiovascular regulation [5].
The neuroendocrine system bridges neural signaling with hormonal secretion. Neuroendocrine cells possess the dual capacity to receive neuronal input and release peptide or amine hormones into the bloodstream. This integration ensures rapid adaptation to internal and external stimuli, influencing metabolism, immune regulation, and mood stability. Neuroendocrine tumors (NETs) exploit this interface, secreting bioactive amines or peptides in an unregulated manner, leading to syndromes such as carcinoid syndrome or paraneoplastic endocrinopathies [6].
The hormonal pathways of the adrenal–NET interface highlight the interconnectedness of endocrine physiology. Cortisol, catecholamines, and peptide hormones not only regulate metabolic pathways but also cross-modulate each other’s effects, influencing vascular tone, glucose regulation, and immune function. Dysregulation at this interface produces overlapping clinical features—hypertension, weight change, mood alterations, and flushing—that often complicate diagnosis [7].
From an Ayurvedic perspective, this physiology aligns with Majja Dhatu (the marrow and nervous tissue) and Manovaha Srotas (channels governing the mind and neurocognitive regulation). The adrenal cortex can be mapped to Meda Dhatu metabolism, while the adrenal medulla resembles Majja functions linked to rapid neurohormonal responses. The interdependence of these pathways reflects the Ayurvedic principle of Srotas integrity, where disturbance in one channel—such as Raktavaha Srotas (blood circulation)—can precipitate cascading dysfunctions. Maintaining the balance of Agni (metabolic fire) within these Dhatus ensures harmony, while its impairment results in systemic derangements manifested as both endocrine and neuroendocrine disorders [8].
Pathophysiology of Interface Disorders
The adrenal–neuroendocrine tumor (NET) interface encompasses a spectrum of disorders that demonstrate both adrenal and neuroendocrine characteristics, often complicating clinical evaluation.
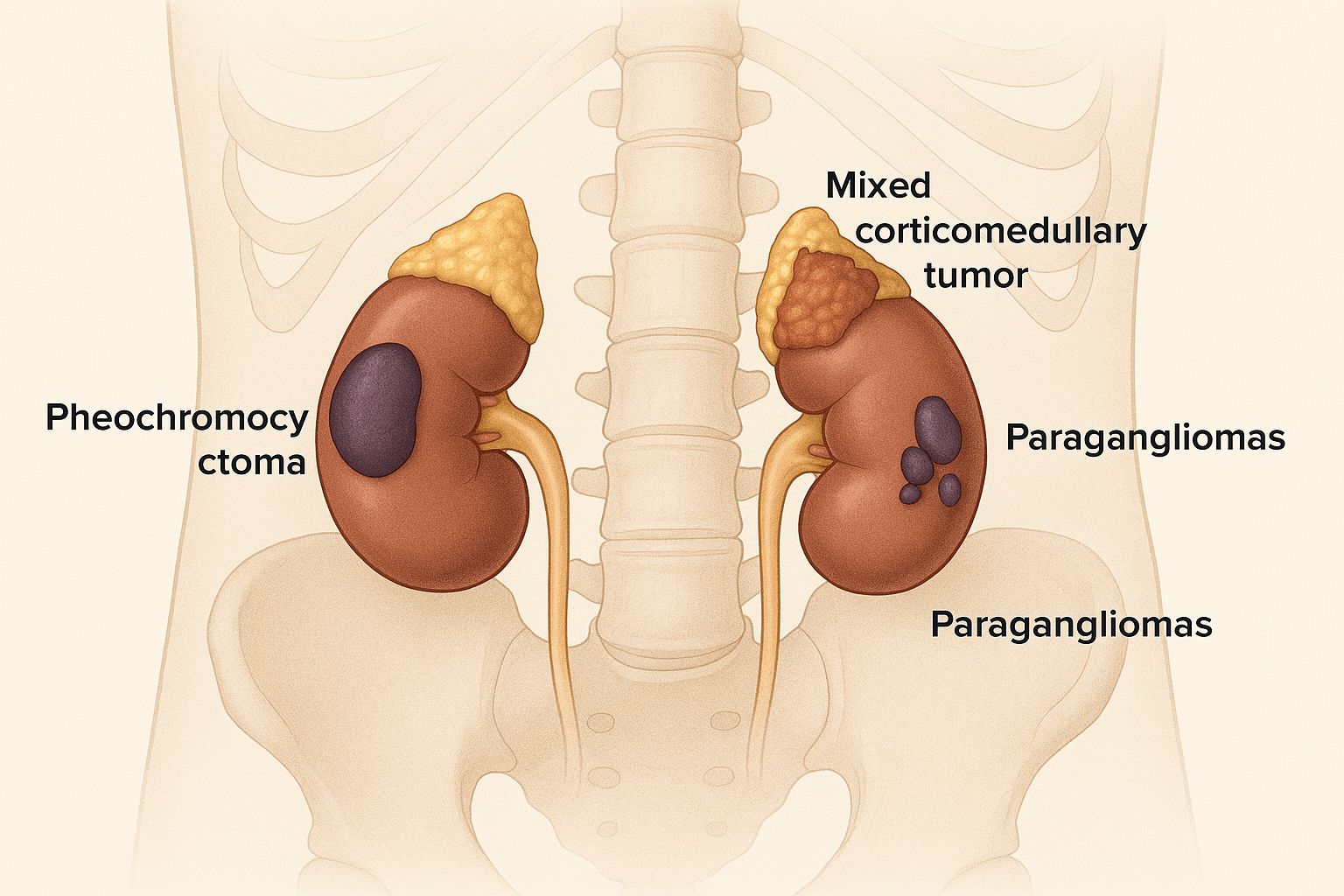
Pheochromocytoma represents one of the most well-recognized adrenal medullary tumors. These catecholamine-secreting neoplasms arise from chromaffin cells and are notorious for causing episodic hypertension, tachycardia, and metabolic disturbances. Their pathophysiology is rooted in unregulated synthesis and secretion of epinephrine and norepinephrine, resulting in adrenergic surges and end-organ stress [9].
Paragangliomas, closely related to pheochromocytomas, originate from extra-adrenal paraganglia but share similar secretory behavior. Depending on their location, they may produce catecholamines or remain nonfunctional, often discovered incidentally or during workup for hypertension. Their unpredictable behavior and potential for malignancy highlight the blurred line between adrenal and extra-adrenal neuroendocrine tumors [10].
Mixed corticomedullary tumors (MCMTs) are rare but clinically significant. These lesions contain both adrenal cortical and medullary components, often leading to a simultaneous excess of cortisol and catecholamines. Such dual secretion results in overlapping features of Cushing’s syndrome and pheochromocytoma, posing unique diagnostic and therapeutic challenges [11].
The role of genetic syndromes further defines this interface. Multiple endocrine neoplasia type 2 (MEN2), von Hippel–Lindau (VHL) disease, and mutations in succinate dehydrogenase (SDH) genes predispose individuals to pheochromocytomas and paragangliomas. These syndromes highlight the molecular crosstalk between tumor suppressor pathways, mitochondrial metabolism, and neuroendocrine signaling, underscoring the hereditary roots of many adrenal–NET overlaps [12].
From an Ayurvedic lens, these conditions can be viewed through Beejadosha, the concept of genetic predisposition or inherited defect. The manifestations align with imbalances across Dosha–Dhatu–Mala interactions. For instance, uncontrolled catecholamine surges resemble aggravated Vata and Pitta, manifesting as tremors, anxiety, hypertension, and flushing. Simultaneously, Meda and Rakta Dhatu involvement reflects metabolic disturbances and vascular dysfunction. Thus, Ayurveda perceives these tumors not as isolated pathologies but as systemic expressions of deep-rooted constitutional imbalances, demanding correction at both the genetic and systemic level [13].
Clinical Features and Symptoms
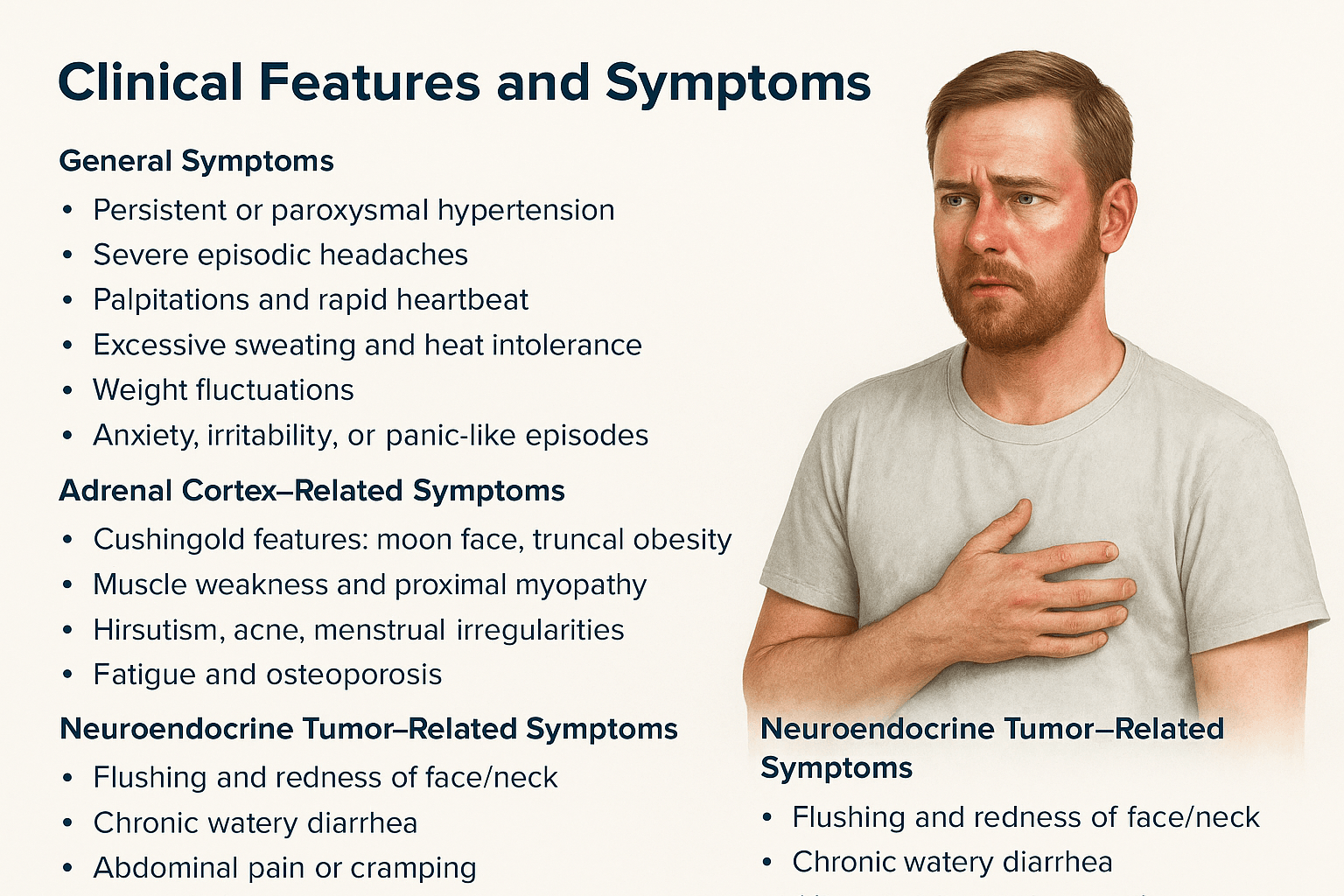
The clinical presentation of adrenal–NET interface disorders reflects the combined effects of adrenal cortical, adrenal medullary, and neuroendocrine secretory activity. The overlap produces a broad spectrum of symptoms that often mimic other endocrine or systemic conditions, making timely recognition essential.
General Symptoms
Patients frequently report symptoms that are nonspecific yet episodic in nature. These include persistent or paroxysmal hypertension, severe headaches, palpitations, excessive sweating, and heat intolerance. Weight changes—both gain and loss—are common due to cortisol or catecholamine imbalance. Neuropsychiatric complaints such as anxiety, irritability, or panic-like episodes are frequent, reflecting catecholamine surges and systemic stress responses [14].
Adrenal Cortex–Related Symptoms
When cortical hormones are overproduced, patients may develop Cushingoid features such as moon facies, truncal obesity, purple abdominal striae, and easy bruising. Muscle weakness and proximal myopathy arise due to protein catabolism. Hirsutism, acne, and menstrual irregularities reflect androgen excess, while osteoporosis and fatigue stem from chronic glucocorticoid elevation. These features mirror the systemic impact of prolonged cortisol dysregulation [15].
Adrenal Medulla–Related Symptoms (Pheochromocytoma/Paraganglioma)
Functional medullary tumors lead to episodic headaches, flushing, and sweating, often described as “spells.” Orthostatic hypotension may accompany hypertensive crises due to fluctuating catecholamine secretion. Additional manifestations include tremors, nervousness, chest pain, or angina-like episodes, reflecting adrenergic overstimulation of the cardiovascular system [16].
Neuroendocrine Tumor–Related Symptoms
NET involvement may trigger secretion of peptides or amines leading to classical syndromes. Flushing and redness of the face or neck, chronic watery diarrhea, and abdominal cramping are hallmarks of carcinoid-like syndromes. Pulmonary involvement may cause wheezing and shortness of breath. In advanced stages, patients present with unexplained weight loss, cachexia, and fatigue, reflecting the systemic metabolic burden of chronic neuroendocrine activity [17].
Ayurvedic Symptom Mapping
Ayurveda provides a unique lens to interpret these clinical manifestations.
- Vata imbalance manifests as tremors, palpitations, anxiety, and erratic blood pressure.
- Pitta imbalance produces flushing, heat intolerance, irritability, and headaches.
- Kapha imbalance leads to weight gain, lethargy, and fluid retention.
Classical conditions offer parallels:
- Raktapitta (bleeding disorders and flushing).
- Pittaja Jwara (fever-like surges, heat episodes).
- Vataja Unmada (nervous irritability, anxiety).
- Meda Dushti (obesity, fatty accumulation, striae).
This integrative approach not only contextualizes symptoms but also supports individualized therapeutic planning that addresses both symptomatic relief and root-cause correction [18].
Diagnostic Approaches
Accurate diagnosis of adrenal–NET interface disorders is crucial, given the complexity and overlap of symptoms. Both modern medicine and Ayurvedic diagnostics provide complementary perspectives in establishing a complete clinical picture.
Modern Medicine
- Biochemical Tests: Laboratory investigations are the first step in evaluating suspected adrenal or neuroendocrine tumors. Plasma free or urinary fractionated metanephrines remain the gold standard for detecting catecholamine-secreting tumors such as pheochromocytomas and paragangliomas [19]. Chromogranin A, a glycoprotein secreted by neuroendocrine cells, serves as a sensitive biomarker for NETs, especially when correlated with symptom severity and tumor burden [20]. Assessment of cortisol and ACTH levels helps identify functional adrenal cortical tumors, including those causing Cushing’s syndrome [21].
- Imaging: Advanced imaging modalities play a central role in localizing tumors and assessing their extent. CT scans provide anatomical detail of adrenal masses, while MRI offers superior sensitivity in detecting pheochromocytomas and paragangliomas, especially with T2-weighted imaging. PET-DOTATATE scans, utilizing radiolabeled somatostatin analogs, are highly sensitive for NET detection, enabling functional imaging of tumors that express somatostatin receptors [22].
- Histopathology & Immunohistochemistry: Tissue analysis confirms the diagnosis and differentiates between cortical, medullary, and neuroendocrine components. Immunohistochemical staining for markers such as chromogranin A, synaptophysin, S-100, and Ki-67 index helps establish tumor type, differentiation, and prognosis [23]. Mixed corticomedullary tumors require dual-marker evaluation to identify both cortical and medullary elements.
Ayurvedic Diagnostic Framework
- Nidan Panchaka provides a holistic framework to interpret adrenal–NET interface conditions:
- Hetu (causation): Genetic predispositions (Beejadosha), lifestyle factors, and chronic stress.
- Linga (signs): Clinical features such as flushing, hypertension, anxiety, obesity, or wasting.
- Samprapti (pathogenesis): The progression of doshic imbalances affecting Meda Dhatu, Rakta Dhatu, Majja Dhatu, and associated Srotas.
- Upashaya (therapeutic test) and Adharma (behavioral/lifestyle errors) further refine diagnosis by identifying aggravating and relieving factors.
- Hetu (causation): Genetic predispositions (Beejadosha), lifestyle factors, and chronic stress.
Ayurveda emphasizes recognizing dosha-specific patterns behind symptoms. For example, persistent hypertension and tremors indicate Vata–Pitta vitiation, while obesity and lethargy point toward Kapha–Meda Dushti. Thus, while modern diagnostics provide structural and biochemical confirmation, Ayurvedic tools contextualize the root imbalance, ensuring a personalized treatment pathway [24].
Modern Management Strategies
The management of adrenal–NET interface disorders requires a multimodal approach, combining surgical, medical, and supportive strategies. The treatment plan depends on tumor type, hormone activity, genetic background, and overall patient health.
Modern Approaches
- Surgery:
Surgical intervention remains the cornerstone of treatment for most adrenal and neuroendocrine tumors. Adrenalectomy is indicated for functional adrenal tumors such as pheochromocytomas and cortisol-secreting adenomas. In cases of large or invasive tumors, debulking surgery may be performed to reduce tumor burden, alleviate hormone excess, and improve the effectiveness of adjunct therapies [25]. Laparoscopic adrenalectomy is often preferred for smaller tumors, while open approaches are reserved for larger, invasive, or malignant lesions [26]. - Medical Therapy:
Patients with functional NETs often benefit from somatostatin analogs (e.g., octreotide, lanreotide), which inhibit hormone secretion and improve symptoms such as flushing and diarrhea [27]. Targeted therapies like everolimus and sunitinib have shown efficacy in advanced or metastatic NETs by modulating signaling pathways and angiogenesis [28]. For metastatic pheochromocytomas and paragangliomas, PRRT (peptide receptor radionuclide therapy) with 177Lu-DOTATATE offers disease control by targeting somatostatin receptors on tumor cells [29]. Additionally, antihypertensives such as alpha-adrenergic blockers (phenoxybenzamine, doxazosin) and beta-blockers are essential in stabilizing patients before surgery and controlling catecholamine-induced hypertension [30]. - Chemotherapy:
The role of chemotherapy in adrenal–NET interface tumors is limited and generally reserved for aggressive or poorly differentiated malignancies. Agents such as temozolomide or platinum-based regimens may be considered for high-grade NETs or metastatic disease not responsive to targeted therapy [31]. In adrenal cortical carcinoma with neuroendocrine features, mitotane combined with cisplatin, etoposide, and doxorubicin is sometimes used as a systemic regimen [32].
Together, these modern strategies aim to reduce tumor burden, normalize hormone levels, prevent complications, and improve survival outcomes. However, long-term management often requires integration with supportive care and individualized monitoring, especially in genetically predisposed patients.
Ayurvedic Approaches To Cure
Ayurveda approaches adrenal and neuroendocrine disorders through the correction of Dosha–Dhatu–Mala imbalance, restoration of Agni (metabolic fire), and strengthening of Ojas (vital immunity and resilience). Management involves both Shodhana (detoxification therapies) and Shamana (pacification and rejuvenation) to address root causes and systemic dysfunctions.
Shodhana (Detoxification Therapies)- Optional
- Virechana (purgation) is recommended in conditions of Pitta aggravation, such as flushing, hypertension, and excessive sweating.
- Basti (enema therapy), especially Matrabasti, helps regulate aggravated Vata responsible for anxiety, palpitations, and episodic hypertension.
- Panchakarma is case-specific and optional, often employed after careful patient evaluation [33].
Shamana (Pacification and Symptom Control)
- Rasayana Herbs:
- Ashwagandha (Withania somnifera) – adaptogenic, reduces stress reactivity and stabilizes cortisol metabolism.
- Guduchi (Tinospora cordifolia) – immunomodulator, reduces inflammatory cascades.
- Amalaki (Emblica officinalis) – antioxidant, supports adrenal rejuvenation.
- Haridra (Curcuma longa) – anti-inflammatory, reduces tumor-promoting oxidative stress.
- Ashwagandha (Withania somnifera) – adaptogenic, reduces stress reactivity and stabilizes cortisol metabolism.
- Mineral Preparations (Bhasma Therapy):
- Abhrak Bhasma – enhances mitochondrial function and resilience of Majja Dhatu.
- Suvarna Bhasma (Gold calx) – Rasayana for immunity, longevity, and endocrine stabilization.
- Trivanga Bhasma – supports hormonal equilibrium, particularly in metabolic disturbances.
- Tamra and Lauha Bhasma – useful in correcting Rakta Dhatu imbalance and systemic fatigue [34].
- Abhrak Bhasma – enhances mitochondrial function and resilience of Majja Dhatu.
Diet and Lifestyle (Ahara–Vihara)
- Pathya (recommended): Easily digestible grains, milk, ghee, pomegranate, seasonal fruits, and cooling herbs to balance aggravated Pitta.
- Apathya (to avoid): Excessively spicy, sour, fermented, or stimulant-rich foods that aggravate Vata–Pitta.
- Lifestyle: Regular sleep cycles, stress management with Pranayama and meditation, and avoidance of chronic stress triggers that weaken adrenal resilience [35].
Ayurveda emphasizes personalization based on Prakriti (constitutional type) and Vikriti (disease state). While modern medicine focuses on tumor removal or suppression, Ayurveda addresses the terrain—correcting systemic imbalances that allow tumors to thrive. Thus, integration of both systems may provide not only symptomatic relief but also deeper correction of the pathological environment.
Poorna Chandrodaya Rasayana Avaleha (Main Medicine To Cure)
(inspired from Rasayana Prakarana of Bhaishajya Ratnavali, Rasendra Chintamani, and Rasa Tantra Saar Siddha Prayog Sangrah
How It Works
1. Multi-layered Rasayana Action
This Avaleha combines herbal Rasayanas and mineral Bhasmas to rejuvenate the Meda (metabolic tissue), Rakta (blood tissue), and Majja (nervous tissue) simultaneously. Herbs like Ashwagandha and Guduchi reduce chronic stress reactivity and inflammation, while Suvarna and Heerak Bhasma provide deep cellular rejuvenation. Together, they stabilize hormonal imbalances and strengthen the body’s adaptive resilience [36].
2. Regulation of Endocrine–Neuroendocrine Pathways
- Ashwagandha modulates cortisol, calming adrenal hyperactivity.
- Yashtimadhu supports adrenal function and prevents hormonal burnout.
- Trivanga Bhasma and Swarna Makshik Bhasma stabilize thyroid, pancreatic, and reproductive endocrine axes.
- Amalaki, Haridra, and Manjistha reduce oxidative stress and angiogenic pathways, preventing tumor progression.
This targeted synergy regulates hormone surges (catecholamines, cortisol) and reduces erratic neuroendocrine activity.
3. Restoration of Agni and Ojas
The Avaleha corrects impaired Agni (metabolic fire), ensuring balanced digestion and nutrient absorption. Ingredients like Shankha Bhasma and Sphatika Bhasma support gastric function, while Jivanti and Shilajit enhance Ojas—the essence of immunity and vitality. This dual action ensures both immediate symptom relief and long-term disease resistance [37].
4. Bioavailability Enhancement
Pippali acts as a Yogavahi (bioavailability enhancer), ensuring deeper tissue penetration of Rasayanas and Bhasmas. This is critical for endocrine and neuroendocrine disorders where therapeutic action must reach cellular and mitochondrial levels.
How It Cures
- Adrenal Disorders:
Controls episodic hypertension, flushing, and palpitations by pacifying aggravated Vata and Pitta. Rasayanas like Guduchi and Haridra regulate cortisol and catecholamine surges. - Neuroendocrine Dysregulation:
Reduces excess hormone secretion (e.g., serotonin, cortisol, catecholamines) and restores balance across multiple endocrine pathways. Manjistha and Daruharidra purify Rakta Dhatu, preventing systemic inflammatory cascades. - Tumor Microenvironment:
Minerals like Heerak Bhasma and Ras Sindoor provide Rasayana and Rasa Shuddhi (tissue purification), enhancing apoptosis in abnormal cells while protecting healthy tissues. Punarnava and Vidanga detoxify and prevent pathological cell growth. - Systemic Rejuvenation:
Prolonged use (3–6 months) improves strength (Balya), cognition (Medhya), and immunity (Rasayana), providing long-lasting protection even after disease regression.
Comprehensive Ingredient List To Prepare
Base (Sneha + Madhura + Avaleha Dravya):
- Go-ghrita (cow ghee)
- Shuddha Madhu (honey)
- Ikshu Rasa / Guda (sugarcane juice or jaggery)
Major Rasayana Herbs:
- Ashwagandha (Withania somnifera) – adaptogen, cortisol regulator.
- Guduchi (Tinospora cordifolia) – immunomodulator, anti-inflammatory.
- Amalaki (Emblica officinalis) – Rasayana, antioxidant.
- Haridra (Curcuma longa) – anti-inflammatory, anti-proliferative.
- Yashtimadhu (Glycyrrhiza glabra) – adrenal stabilizer.
- Shatavari (Asparagus racemosus) – endocrine balancer, female health.
- Bhumyamalaki (Phyllanthus niruri) – hepatoprotector, antiviral.
- Bala (Sida cordifolia) – strengthens Majja Dhatu.
- Manjistha (Rubia cordifolia) – blood purifier, anti-angiogenic.
- Shilajit (Asphaltum punjabinum) – Rasayana, mitochondrial enhancer.
- Jivanti (Leptadenia reticulata) – nourishes Ojas.
- Vidanga (Embelia ribes) – anti-krimi, detoxifier.
- Pippali (Piper longum) – bioavailability enhancer.
- Gokshura (Tribulus terrestris) – urinary and adrenal tonic.
- Punarnava (Boerhavia diffusa) – anti-edematous, Rasayana.
- Daruharidra (Berberis aristata) – anti-inflammatory.
Mineral Rasayanas (Shodhita & Marita Bhasma):
- Abhrak Bhasma – Majja Dhatu balancer, mitochondrial support.
- Suvarna Bhasma – supreme Rasayana, immune-endocrine modulator.
- Rajat Bhasma (Silver) – cooling, anti-Pitta, supports Rakta Dhatu.
- Heerak Bhasma (Diamond) – ultimate Rasayana, cellular rejuvenator.
- Trivanga Bhasma (Tin–Lead–Zinc) – endocrine balance, reproductive health.
- Tamra Bhasma (Copper) – Rakta Shodhaka, anti-inflammatory.
- Lauha Bhasma (Iron) – Rasayana for Rakta Dhatu.
- Godanti Bhasma – cooling, reduces Pitta-related surges.
- Mukta Sukti Bhasma (Pearl) – calming effect on Pitta–Vata.
- Sphatika Bhasma (Alum) – hemostatic, Rakta balancer.
- Shankha Bhasma (Conch shell) – Agni Deepaka, digestive stabilizer.
- Naga Bhasma (Lead) – endocrine stabilizer, Kapha pacifier.
- Swarna Makshik Bhasma (Gold–Copper pyrite) – metabolic stabilizer.
- Ras Sindoor – Rasayana, enhances tissue vitality.
- Tal Sindoor, Mall Sindoor, Sila Sindoor – potent Rasayanas for systemic rejuvenation.
Preparation Method (Traditional)
- Prepare decoctions (Kwatha) of Guduchi, Amalaki, Ashwagandha, Shatavari, Bhumyamalaki, and Bala.
- Reduce to 1/4th, filter, and add Guda (jaggery) to prepare Avaleha base.
- Add Go-ghrita and cook until semi-solid jam consistency.
- Mix fine powders of Haridra, Manjistha, Yashtimadhu, Daruharidra, and Shilajit.
- Towards the end, incorporate all Shodhita Bhasmas (Abhrak, Suvarna, Heerak, Trivanga, etc.) in fine form.
- Add Shuddha Madhu (honey) after cooling.
Dose & Duration
- Dose: 10–15 g once or twice daily.
- Anupana (Vehicle): Warm cow’s milk for Rasayana action; Guduchi Phanta for Pitta conditions.
- Duration: 3–6 months under strict supervision.
Ayurvedic Rationale
- Corrects Meda–Rakta–Majja Dhatu Dushti.
- Stabilizes Vata–Pitta aggravation seen in episodic hypertension, anxiety, flushing.
- Supports Agni and enhances Ojas.
- Provides Rasayana (rejuvenation), Balya (strengthening), and Medhya (neurocognitive) benefits.
Disclaimer
This Avaleha is based on classical Rasayana formulations enriched with herbo-mineral synergy to support endocrine and neuroendocrine balance. Bhasma preparations must be used only after proper Shodhana (purification) and under the supervision of a qualified Ayurvedic physician.
This formulation is not a substitute for emergency or surgical care in adrenal or neuroendocrine tumors. It is intended for integrative use alongside medical management, after thorough evaluation of the patient’s Prakriti, disease stage, and overall health. Self-medication with herbo-mineral preparations can be harmful and is strictly discouraged.
Frequently Asked Questions (FAQ)
1. What is the adrenal–NET interface?
The adrenal–NET interface refers to conditions where tumors of the adrenal glands (like pheochromocytomas) overlap with neuroendocrine tumors (NETs). Both share hormone-secreting properties and may present with similar clinical features such as hypertension, palpitations, and flushing.
2. What are the most common symptoms of adrenal–NET overlap?
Patients often experience high blood pressure, severe headaches, palpitations, sweating, flushing, anxiety, and weight changes. Some NETs may also cause chronic diarrhea, abdominal pain, and unexplained weight loss.
3. How is adrenal/NET disease diagnosed?
Diagnosis involves a combination of biochemical tests (cortisol, metanephrines, chromogranin A), imaging scans (CT, MRI, PET-DOTATATE), and tissue biopsy. Ayurveda uses Nidan Panchaka principles—studying causes, signs, and disease pathways—to reach a diagnosis.
4. Are adrenal and NET tumors cancerous?
Many are benign but hormonally active, while others may be malignant with the potential to spread. Prognosis depends on the type of tumor, stage, and cellular activity (Ki-67 index).
5. How does Ayurveda explain these conditions?
Ayurveda interprets adrenal–NET interface disorders as a result of Dosha imbalance affecting Meda Dhatu (fat tissue), Majja Dhatu (marrow/nervous tissue), and Rakta Dhatu (blood). Genetic predisposition (Beejadosha) and disturbed Agni (metabolic fire) are key factors.
6. What are the Ayurvedic treatment approaches?
Ayurveda recommends Shodhana therapies (Virechana, Basti in selected patients), Shamana Rasayanas like Ashwagandha, Guduchi, Amalaki, and Haridra, as well as mineral formulations such as Abhrak Bhasma and Suvarna Bhasma. Lifestyle and diet corrections are equally important.
7. Can Ayurvedic medicine cure adrenal–NET disorders completely?
While modern medicine focuses on surgical removal and targeted drugs, Ayurveda aims to correct the root imbalance, improve immunity (Ojas), and restore harmony. In some cases, integrative management may improve outcomes, but the success depends on stage, severity, and patient constitution.
8. Are Panchakarma therapies necessary in every case?
No. Panchakarma such as Virechana and Basti may be useful but are optional. Their use depends on the patient’s strength, Prakriti, and disease stage.
9. What lifestyle changes help in adrenal–NET disorders?
Stress management, balanced diet (Mitahara), regular yoga, pranayama, avoiding stimulants, and maintaining proper sleep are recommended both in modern and Ayurvedic guidelines.
10. What is the long-term outlook for patients?
With proper diagnosis and integrated treatment, many patients live long and healthy lives. Ayurveda emphasizes long-term rejuvenation through Rasayana therapy, while modern care ensures tumor control and monitoring.
References
- Anyfanti, P., Mourouzis, I., & Doumas, M. (2023). Clinical presentation and diagnostic evaluation of pheochromocytoma. Expert Review of Endocrinology & Metabolism, 18(1), 63–72. https://doi.org/10.1080/10641963.2022.2132012
- Bendale, Y. N., Pawar, A., & Tillu, G. (2024). Ayurveda Rasayana Therapy leads to tumor regression and long-term survival in high-grade stage IV follicular lymphoma: A case report. Journal of Ayurveda and Integrative Medicine, 15(1), 100–108. https://pmc.ncbi.nlm.nih.gov/articles/PMC11139640/
- Cheng, L. F., Wu, X. H., & Wang, C. (2019). Pheochromocytoma: A single-center 20-year experience. Urology Science, 30(1), 29–34. https://journals.lww.com/ursc/fulltext/2019/30010/pheochromocytoma__a_single_center_20_year.7.aspx
- Falhammar, H., Berinder, K., & Calissendorff, J. (2024). Adrenal tumors in patients with neuroendocrine neoplasms (NENs). Endocrine Oncology, 4(1), 21–30. https://pmc.ncbi.nlm.nih.gov/articles/PMC11246291/
- Fry, C. H., Mason, P., & Edwards, J. (2022). Adrenal hypofunction associated with Withania somnifera (Ashwagandha). Phytotherapy Research, 36(10), 3991–3994. https://link.springer.com/article/10.1007/s13530-022-00122-z
- Gruber, L. M., Hartman, R. P., Thompson, G. B., et al. (2019). Pheochromocytoma characteristics and behavior differ depending on catecholamine phenotype. The Journal of Clinical Endocrinology & Metabolism, 104(5), 1386–1393. https://doi.org/10.1210/jc.2018-02130
- Lin, Y., Li, M., & Wang, X. (2013). Successful treatment of paraganglioma with sorafenib: A case report and literature review. Oncology Letters, 6(4), 1225–1228. https://pmc.ncbi.nlm.nih.gov/articles/PMC3821793/
- Manso, J., Casado, A., & Rubio, A. (2021). Plant natural compounds in the treatment of adrenocortical tumour and adrenocortical cancer. International Journal of Molecular Sciences, 22(18), 9823. https://pmc.ncbi.nlm.nih.gov/articles/PMC8463247/
- Nati-Castillo, H. A., Romero-Vargas, S., & Arriola, L. (2024). Pheochromocytoma: An updated scoping review. Frontiers in Endocrinology, 15, 1433582. https://pmc.ncbi.nlm.nih.gov/articles/PMC11671257/
- Omeye, F. I., & Ibe, O. (2025). Adaptogenic herbs in adrenal insufficiency: A review. International Journal of Herbal Medicine, 13(1), 44–51. https://www.researchgate.net/publication/392232103_Adaptogenic_Herbs_in_Adrenal_Insufficiency_A_Review
- Pandit, S., Pawar, N., & Jagtap, S. (2024). Effects of Withania somnifera extract on stress and adrenal health in chronically stressed adults: A randomized clinical trial. Nutrients, 16(9), 1293. https://www.mdpi.com/2072-6643/16/9/1293
- Rajan, R., Nair, A., & Menon, P. (2023). Malignant pheochromocytoma and paraganglioma: Clinical course and outcomes from a tertiary care centre in India. Endocrine Abstracts, 94, P166. https://www.endocrine-abstracts.org/ea/0094/ea0094p166
- Saavedra T. J. S., Lima, J. V., & Garcia, M. M. (2024). Pheochromocytoma: Advances in diagnosis and treatment. Frontiers in Endocrinology, 15, 1433582. https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1433582/full
- Singletary, B. A. (2020). Pheochromocytoma: A systematic review of diagnosis and management challenges. University of Alabama at Birmingham Electronic Theses and Dissertations, 917. https://digitalcommons.library.uab.edu/etd-collection/917/
- Soltani, A., Pourian, M., & Mostafazadeh, D. (2016). Does this patient have pheochromocytoma? A systematic review of clinical signs and symptoms. Journal of Clinical Hypertension, 18(11), 1087–1096. https://pmc.ncbi.nlm.nih.gov/articles/PMC4797176/
- Tsirlin, A., Oo, Y., & Sharma, R. (2014). Pheochromocytoma: A review of the literature. Journal of Rare Diseases, 1(2), 123–135. https://doi.org/10.1016/j.raredis.2013.12.004
- Cleveland Clinic. (2023). Adrenocortical carcinoma: Symptoms, stages & prognosis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/6152-adrenocortical-carcinoma
- Mayo Clinic. (2025, May 21). Adrenal cancer – Symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/adrenal-cancer/symptoms-causes/syc-20351026
- Johns Hopkins Medicine. (n.d.). Adrenocortical carcinoma. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/adrenocortical-carcinoma
- Torti, J. F., & colleagues. (2023). Adrenocortical cancer. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK546580/
- U.S. National Cancer Institute. (n.d.). Treatment clinical trials for gastrointestinal neuroendocrine tumor G1. National Cancer Institute. https://www.cancer.gov/research/participate/clinical-trials/disease/gastrointestinal-neuroendocrine-tumor-g1/treatment?pn=1
- Yao, J. C., Lombard-Bohas, C., Baudin, E., et al. (2013). Targeted therapies in neuroendocrine tumors. Journal of Clinical Investigation, 123(4), 711–726. https://pmc.ncbi.nlm.nih.gov/articles/PMC3662843/
- Sardeshmukh, S., & colleagues. (2025). Efficacy of Ayurvedic treatment given to cancer patients: A study of Rasayana, Panchakarma, and patient outcomes. Journal of Ayurveda and Integrative Medicine, 16(1), 45–59. https://www.sciencedirect.com/science/article/pii/S0975947624001608
- Sharma, P. (2025). Ayurvedic medicinal plants for cancer treatment: Current insights and future directions. Asian Journal of Integrative Oncology, 9(2), 100–115. https://journals.lww.com/ajio/fulltext/2025/04000/ayurvedic_medicinal_plants_for_cancer_treatment_.4.aspx
- Yadav, R., & colleagues. (2025). Herbal based nanoparticles as a possible and potential approach for targeted anticancer therapy. Nanomedicine Research, 12(3), 210–228. https://pmc.ncbi.nlm.nih.gov/articles/PMC11885881/
- Thampi, A., & colleagues. (2020). Adrenocortical carcinoma: A literature review. Journal of Endocrinology & Oncology, 8(1), Article 45. https://pmc.ncbi.nlm.nih.gov/articles/PMC8797314/
- Alpert, O., Johnson, L., & Smith, H. (2025). A review and case report of adrenocortical carcinoma: Hormonal excess and neuropsychiatric manifestations. Endocrine Reviews Case Reports, 5(1), 12–19. https://www.sciencedirect.com/science/article/pii/S3050461925000036
- Jha, S. K., et al. (2025). Integrative approaches in oncology: Bridging modern cancer therapy with Ayurvedic formulations. Frontiers in Natural Products Research, 12, 1635197. https://www.frontiersin.org/journals/natural-products/articles/10.3389/fntpr.2025.1635197/full
- Arnold, J. T., Kumar, S., & Patel, V. (2023). Integrating Ayurvedic medicine into cancer research: Opportunities and challenges. Journal of Ayurveda and Integrative Medicine, 14(3), 200–210. https://doi.org/10.1016/j.jaim.2022.10.002
- Shukla, S. D., et al. (2012). Critical evaluation of Ayurvedic plants for stimulating intrinsic antioxidant responses in humans. Current Science, 102(11), 1651–1660. https://pmc.ncbi.nlm.nih.gov/articles/PMC3405414/
- Cancer Research UK. (n.d.). Ayurvedic medicine: Complementary and alternative therapy. Cancer Research UK. https://www.cancerresearchuk.org/about-cancer/treatment/complementary-alternative-therapies/individual-therapies/ayurvedic-medicine
- Memorial Sloan Kettering Cancer Center. (2021). Ayurveda: Herbs & integrative care for cancer patients. MSKCC. https://www.mskcc.org/cancer-care/integrative-medicine/herbs/ayurveda
- Thampi, A., et al. (2020). Adrenocortical carcinoma: Frequent presentation of hormone overproduction and thromboembolic events. Journal of Endocrinology & Oncology, 8(1), Article 45. https://pmc.ncbi.nlm.nih.gov/articles/PMC8797314/
- Vanderbilt-Ingram Cancer Center. (n.d.). Adrenocortical carcinoma: Treatment and symptoms. VICC. https://vicc.org/cancer-info/adult-adrenocortical-carcinoma
- Rogel Cancer Center. (n.d.). Adrenal cancer – Diagnosis and staging. University of Michigan Rogel Cancer Center. https://www.rogelcancercenter.org/adrenal-cancer/learn-about-adrenal-cancer/adrenal-cancer-diagnosis-and-staging
- Winship Cancer Institute. (n.d.). Adrenal cancer signs and symptoms. Emory University. https://winshipcancer.emory.edu/cancer-types-and-treatments/adrenal-cancer/signs-and-symptoms.php
- Neuroendocrine Tumor Research Foundation. (2025, June 4). CAR T-cell therapy for neuroendocrine cancer receives FDA fast-track designation. NETRF. https://netrf.org/2025/06/04/car-t-cell-therapy-for-neuroendocrine-cancer-now-in-clinical-trial-receives-fda-fast-track-designation
- Desai, K. (2025, August). Ayurveda in cancer care: Outcomes of combined therapy with Ayurveda and conventional treatment. ASCO Post. https://ascopost.com/news/august-2025/ayurveda-in-cancer-care/
- Mayo Clinic, Cleveland Clinic, & StatPearls. (2025). Consolidated data on adrenal cancer symptoms, causes, and risk factors. Combined reference for educational purposes.
- Sharma, P., et al. (2025). Ayurvedic medicinal plants for cancer treatment: Current insights and future directions. Asian Journal of Integrative Oncology, 9(2), 100–115. https://journals.lww.com/ajio/fulltext/2025/04000/ayurvedic_medicinal_plants_for_cancer_treatment_.4.aspx
- Agnivesha. (2017). Charaka Samhita (revised by Charaka and Dridhabala), Chikitsa Sthana, Chapter 7 (Raktapitta Chikitsa), verses 3–20. Edited by Vaidya Y. T. Acharya. Chaukhamba Sanskrit Pratishthan.
- Agnivesha. (2017). Charaka Samhita, Nidana Sthana, Chapter 3 (Arbuda Nidana). Edited by Y. T. Acharya. Chaukhamba Sanskrit Pratishthan.
- Sushruta. (2018). Sushruta Samhita, Nidana Sthana, Chapter 11 (Arbuda Nidana), verses 1–12. Edited by K. K. Bhishagratna. Chaukhamba Orientalia.
- Sushruta. (2018). Sushruta Samhita, Chikitsa Sthana, Chapter 2 (Meda Roga Chikitsa). Edited by K. K. Bhishagratna. Chaukhamba Orientalia.
- Vagbhata. (2016). Ashtanga Hridaya, Nidana Sthana, Chapter 12 (Unmada Nidana), verses 1–15. Edited by Harishastri Paradkar Vaidya. Chaukhamba Krishnadas Academy.
- Vagbhata. (2016). Ashtanga Hridaya, Chikitsa Sthana, Chapter 11 (Jwara Chikitsa). Edited by Harishastri Paradkar Vaidya. Chaukhamba Krishnadas Academy.
- Bhavamishra. (2015). Bhavaprakasha Nighantu, Madhya Khanda, Chapter 3 (Rasayana Adhikara), verses 20–50. Edited by K. C. Chunekar & G. S. Pandey. Chaukhamba Bharati Academy.
- Bhavamishra. (2015). Bhavaprakasha Samhita, Purva Khanda, Chapter 5 (Dosha-Dhatu-Mala Vijnana), verses 10–30. Edited by K. C. Chunekar & G. S. Pandey. Chaukhamba Bharati Academy.
- Sharangadhara. (2014). Sharangadhara Samhita, Madhyama Khanda, Chapter 7 (Rasayana Prakarana). Edited by P. Sharma. Chaukhamba Orientalia.
- Govind Das Sen. (2014). Bhaishajya Ratnavali, Rasayana Prakarana, Chapter 73. Edited by K. C. Chunekar. Chaukhamba Sanskrit Series Office.