- Herpes Is a Latent, Systemic Viral Condition
- One Formula for All Approach Always Fails
- Absence of Individualized Dosha Dhatu Srotas Assessment
- Symptom Suppression vs Viral Eradication
- Improper, Diluted, or Unsafe Formulations
- Why Cheap or “Free” Herpes Medicines Usually Fail
- Drug Resistance and Viral Adaptation
- Absence of True Rasayana and Regenerative Therapy
- No Guidance on Diet, Lifestyle, and Triggers
- Incorrect Dosage, Duration, and Self Medication
- Ignoring Co Infections and Hidden Contributors
- Psychological and Neuro Immune Neglect
- Sexual Transmission Continues Despite Symptom Suppression
- Why Online Reviews and Testimonials Are Misleading
- The Problem with “Fast Cure” Claims
- Lack of Monitoring, Testing, and Progress Markers
- Why Women, Older Adults, and Immunocompromised Patients Fail Faster
- Detox Burden and Long Term Internal Damage
- Absence of Physician Supervision
- Clear Patient Checklist to Identify a Non Working Herpes Medicine
- What a Science Aligned Long Term Strategy Looks Like
- Conclusion and Patient Takeaway Summary
- Frequently Asked Questions
- Reference List
Why herpes medicines Fail is the most important question patients ask after experiencing repeated outbreaks despite treatment. You may follow prescriptions, use creams, or try multiple remedies, yet the virus continues to return. This happens not because treatment was ignored, but because most approaches focus on short term suppression rather than addressing latency, immune exhaustion, and systemic triggers that drive recurrence.
Most people rely on market medicines such as over the counter antiviral tablets, topical herpes creams, and ready made herbal products. These options are designed primarily for symptom suppression, not for long term viral resolution. As a patient, you may notice that blisters heal faster or pain reduces temporarily, but the virus itself remains active in the body. This is the central reason why herpes medicines do not work long term and why outbreaks continue to recur despite regular treatment [1], [5].
From a medical perspective, herpes is a latent viral infection that hides within the nervous system. Modern medicines are structured to reduce viral replication during active outbreaks, not to eliminate the virus from its latent reservoirs. When you stop taking these medicines, viral activity resumes, leading to repeated episodes. This explains why doctors often prescribe lifelong suppressive therapy rather than offering a definitive cure [5], [6], [14].
In this article, we will examine why market bought herpes medicines fail to provide lasting results, how symptom suppression differs from true viral eradication, and what critical biological factors are ignored in standard treatment models. By understanding these mechanisms, you will be able to clearly see why herpes medicines do not work, why outbreaks keep returning, and why a different therapeutic strategy is required for long term resolution [1], [14].
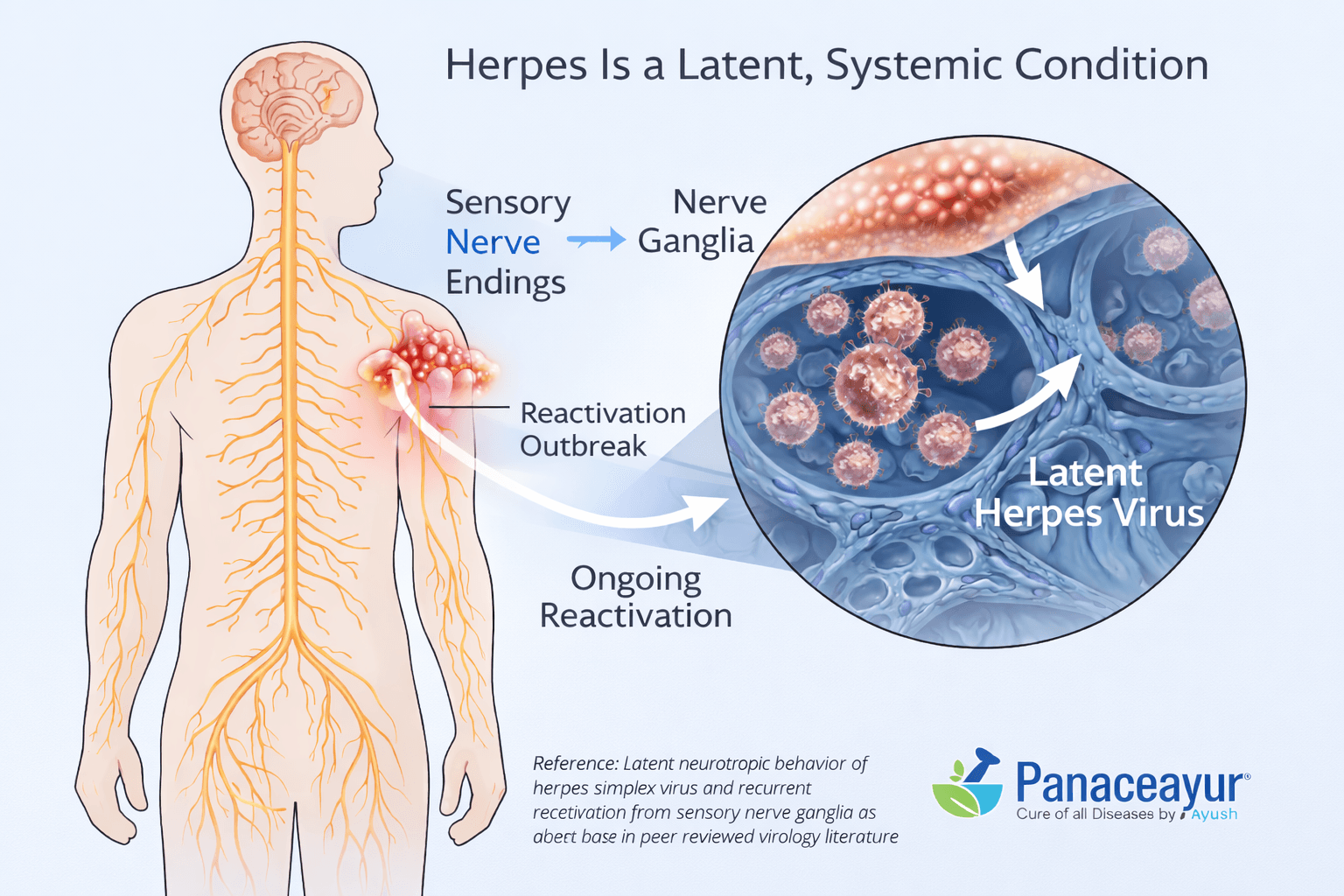
To understand why herpes medicines do not work, it is essential to first understand the true biological nature of the herpes virus. Herpes is not a simple surface infection of the skin or mucosa. It is a latent and systemic viral condition that embeds itself deep within the body, particularly inside the nervous system. This single fact explains why creams, tablets, and short term therapies repeatedly fail [1], [2], [3].
When you experience a herpes outbreak, what you see on the skin is only the visible expression of a much deeper process. After the initial infection, the virus migrates through sensory nerve endings and permanently settles inside nerve ganglia. From there, it remains dormant for long periods, invisible to both the immune system and most medications. This dormant state is known as viral latency, and it is the primary reason why herpes medicines do not work long term [2], [14].
From a clinical standpoint, herpes is described as a neurotropic virus, meaning it has a specific affinity for nerve tissue. Antiviral drugs circulating in the blood have limited penetration into these nerve reservoirs. As a result, medicines can reduce viral replication during an active outbreak but cannot eliminate the virus hiding within neurons. When stress, illness, hormonal changes, or immune weakness occur, the virus reactivates and travels back to the skin, causing new outbreaks. This explains why you may follow treatment exactly as prescribed and still see repeated flare ups [1], [3], [14].
Doctors are aware of this limitation, which is why conventional medicine does not claim a cure for herpes. Instead, it focuses on suppression. You are often advised to take antiviral medicines daily or during outbreaks, not because they eradicate the virus, but because they temporarily reduce viral activity. From a scientific perspective, this approach manages symptoms while accepting lifelong viral persistence as inevitable [1], [14].
If you look at herpes as a systemic viral condition rather than a skin disease, the failure of market medicines becomes logical. They are not designed to address latency, neural reservoirs, or long term immune reprogramming. This is the core biological reason why herpes medicines do not work, why outbreaks keep returning, and why symptom based treatment alone can never deliver lasting resolution [2], [3], [14].
One Formula for All Approach Always Fails
Herpes Is Not the Same Disease in Every Person
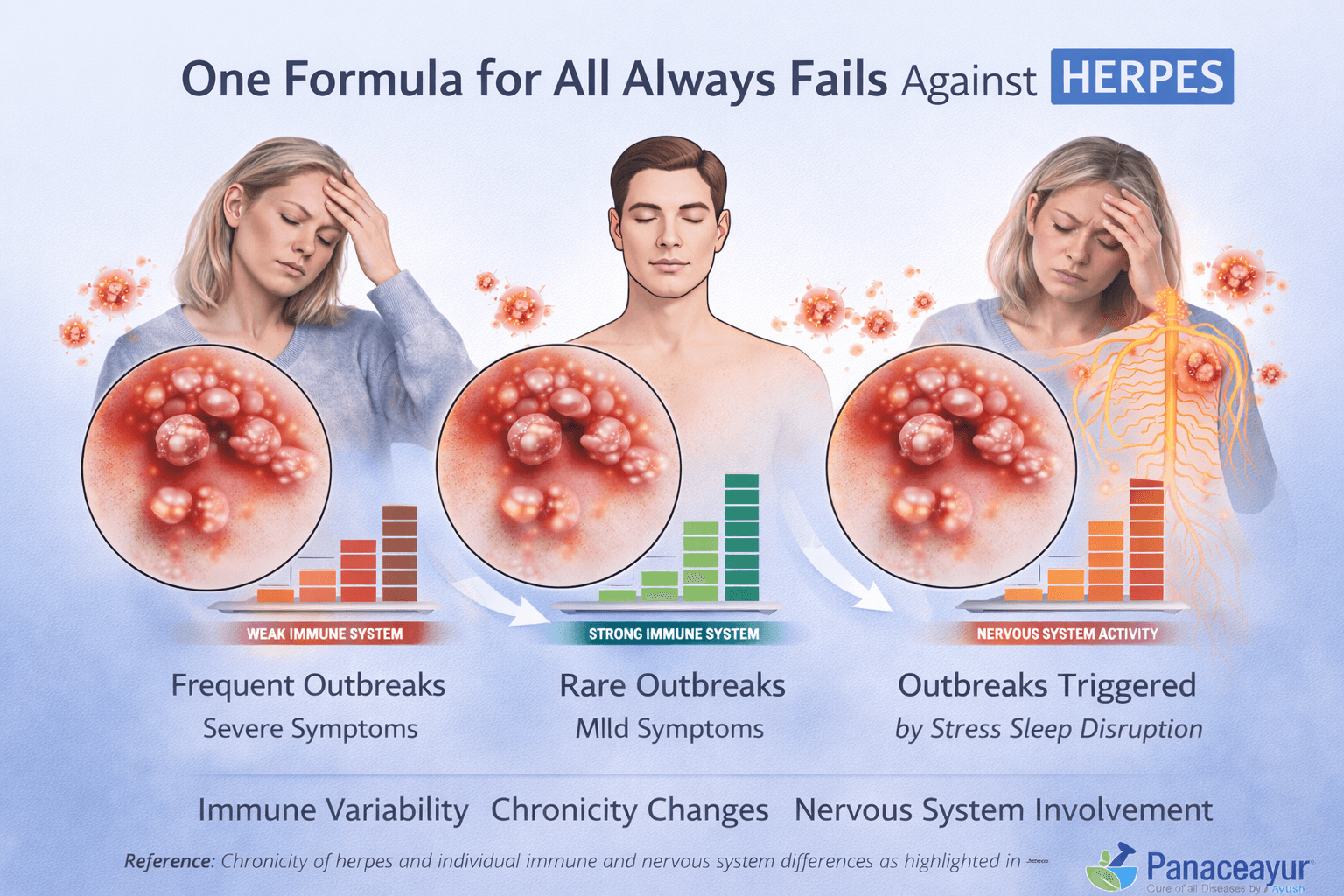
One of the most fundamental reasons why herpes medicines do not work is the incorrect assumption that herpes behaves uniformly in all individuals. In reality, herpes expresses itself differently depending on immune strength, nervous system resilience, metabolic health, and the duration for which the virus has been present in the body. You may experience frequent outbreaks with fatigue, burning sensations, and slow recovery, while another person may have rare, mild episodes. These differences arise because the virus adapts to the internal biological environment of each host, not because one person follows treatment better than another [6], [14].
Individual Immune Variability Determines Treatment Response
From an immunological perspective, herpes outcomes are directly linked to how your immune system recognizes and controls latent viral activity. Some individuals mount a strong cellular immune response that keeps the virus suppressed for long periods, while others experience immune exhaustion due to chronic stress, nutritional deficiencies, or repeated antiviral exposure. When you are given the same fixed dose medicine as everyone else, the treatment does not adjust to your immune capacity. This mismatch explains why herpes medicines do not work long term, even when taken exactly as prescribed [14].
Chronicity Changes the Biology of Herpes
Herpes is a dynamic chronic infection, not a static condition. A person who acquired the virus recently has a very different internal response compared to someone who has lived with herpes for many years. Over time, chronic viral presence alters nerve sensitivity, inflammatory signaling, and immune tolerance. Medicines designed for short term viral suppression cannot adapt to these progressive biological changes. As a result, what once reduced outbreaks becomes ineffective, leading to shorter remission periods and increased recurrence [6], [15].
Fixed Formulas Ignore Nervous System Involvement
Herpes is a neurotropic virus, meaning it resides and reactivates from nerve tissue. Individual differences in nervous system sensitivity, stress response, and autonomic balance strongly influence outbreak patterns. Standardized medicines do not account for these variations. When you experience emotional stress, sleep disruption, or hormonal fluctuations, the virus reactivates despite continued medication use. This failure highlights a critical flaw in one formula for all treatment models [14].
Why Standardized Medicines Cannot Deliver Lasting Results
From a clinical systems perspective, one formula for all approaches treat herpes as a surface level infection rather than a personalized neuro immune disorder. These medicines target viral replication during outbreaks but ignore the individual terrain in which the virus persists. When immune variability, chronicity, and nervous system factors are left unaddressed, suppression replaces healing. This is the central reason why herpes medicines do not work, and why outbreaks keep returning regardless of treatment adherence [6], [14], [15].
Absence of Individualized Dosha Dhatu Srotas Assessment
Herpes Is a Terrain Based Disorder, Not a Standalone Virus
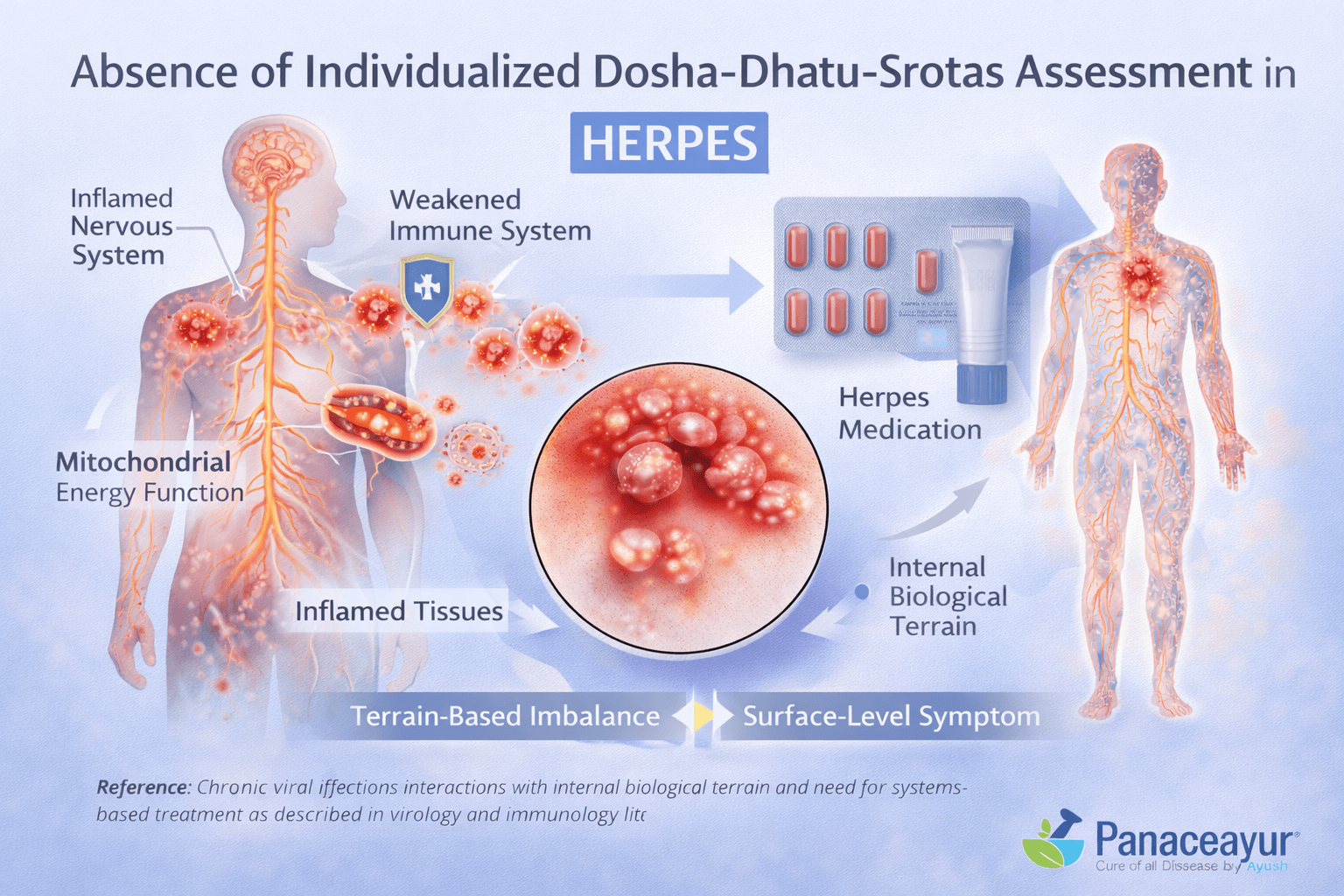
A critical reason why herpes medicines do not work lies in the complete absence of individualized terrain based assessment. Herpes does not operate independently of the body. It expresses itself according to the internal biological environment, including immunity, metabolism, nervous system stability, and tissue health. When treatment ignores this internal terrain, medicines act only on the surface manifestation of the disease while the deeper imbalance remains unresolved [14].
Ignoring the Body as an Integrated System
Modern market medicines approach herpes as an isolated viral entity. Tablets and creams are prescribed without evaluating how different body systems interact with the virus. In reality, chronic viral infections persist because of systemic immune adaptation, not because of constant viral activity alone. When the interconnected nature of the body is ignored, treatment becomes reductionist. This explains why you may suppress symptoms temporarily while the virus continues to reactivate over time [14], [15].
Lack of Tissue Level and Pathway Evaluation
Every chronic disease affects specific tissues and biological pathways. Herpes influences nerve tissue, immune signaling pathways, and inflammatory circuits. Without assessing which tissues are weakened and which pathways are blocked, medicines cannot restore balance. Fixed dose treatments do not differentiate whether the virus is being driven by immune exhaustion, nervous system dysregulation, or long standing inflammation. As a result, therapy remains generic and ineffective for long term resolution [14].
Why Systems Based Evaluation Is Essential for Long Term Results
A systems based evaluation looks beyond visible lesions and considers the entire internal environment. It assesses how immunity, stress response, metabolic efficiency, and tissue regeneration interact with viral latency. When this assessment is missing, treatment fails to address the root conditions that allow herpes to persist. This is why standardized medicines may reduce outbreak intensity yet fail to prevent recurrence over months or years [15].
The Core Reason Medicines Fail Without Individual Assessment
Without individualized assessment, treatment follows a trial and error model rather than a precision based approach. The failure is not because the patient lacks discipline, but because the therapy does not align with the body’s internal reality. Until herpes treatment strategies incorporate personalized system level evaluation, why herpes medicines do not work will remain an unresolved problem for patients seeking lasting relief [14], [15].
Why Visible Healing Creates a False Sense of Cure
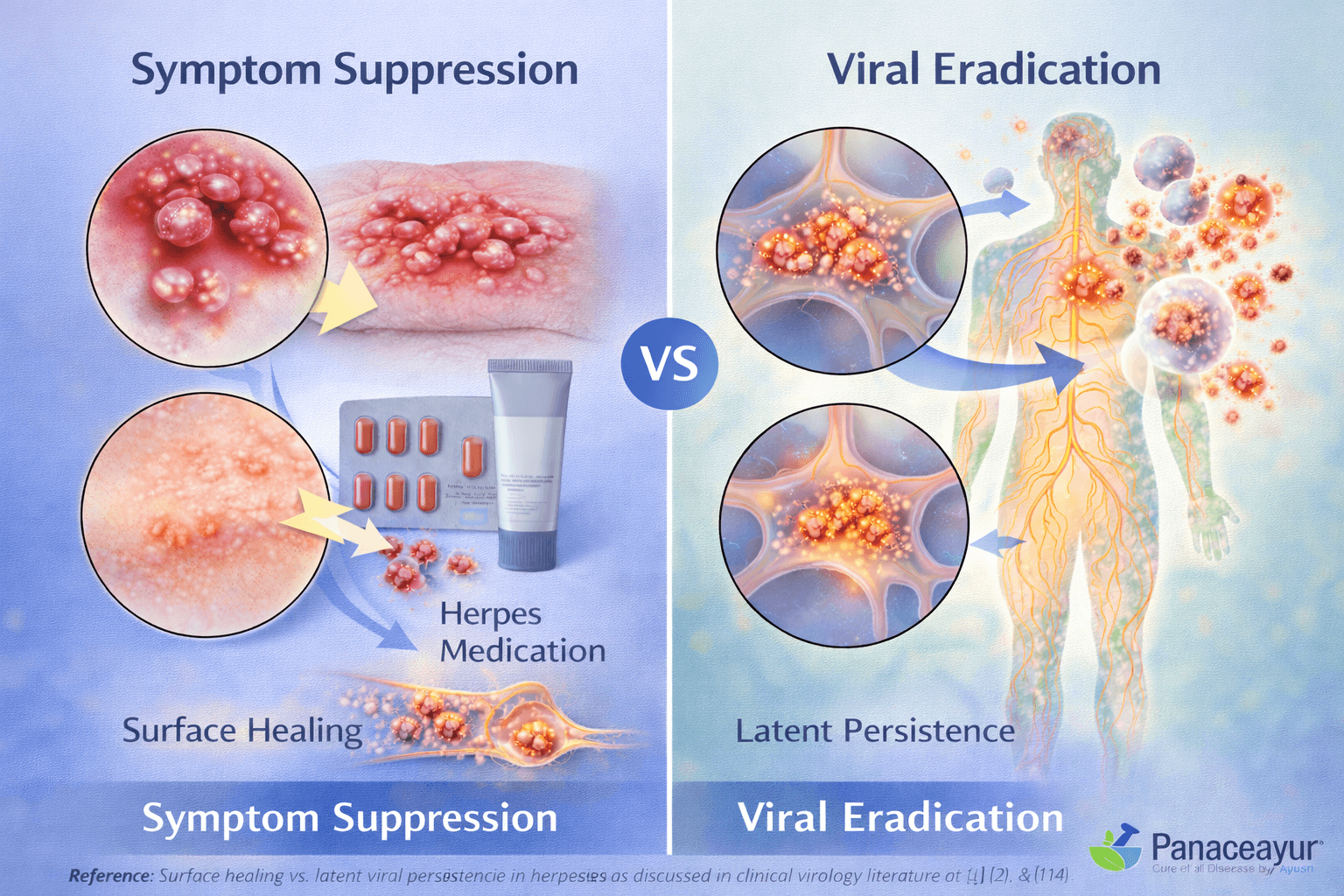
One of the most misleading aspects of herpes treatment is the improvement you can see on the surface. When blisters dry, pain reduces, or skin appears normal again, it feels logical to assume the infection has been controlled. This is exactly where confusion begins. Surface healing does not mean viral elimination. It only reflects temporary suppression of viral activity at the skin level, not resolution of the infection itself. This misunderstanding is a central reason why herpes medicines do not work in the long term [1], [2].
Latent Persistence Is the Real Disease Process
Herpes is fundamentally a latent viral infection. After initial infection, the virus retreats into nerve cells, where it remains dormant and protected from both immune attack and most medications. Antiviral drugs primarily act during active replication phases. They have little to no effect on the virus once it is latent inside nerve tissue. As a result, even when lesions disappear, the virus continues to persist silently within the body [2], [14].
How Suppressive Medicines Are Designed to Work
From a pharmacological perspective, most herpes medicines are suppressive by design. They inhibit viral replication during outbreaks and reduce the severity and duration of symptoms. They do not target latent viral DNA within neurons. This is why doctors recommend daily suppressive therapy for years or even lifelong use. The goal is control, not eradication. When you stop the medicine, the underlying viral reservoir remains unchanged, allowing reactivation to occur [1], [4], [14].
Why Outbreaks Return After Treatment Stops
Many patients ask why outbreaks return even after strict adherence to treatment. The answer lies in the difference between suppression and eradication. Suppression temporarily lowers viral activity, while eradication would require eliminating the virus from its hidden reservoirs. Since current market medicines cannot achieve this, triggers such as stress, illness, hormonal shifts, or immune fatigue easily reactivate the virus. This cycle explains why outbreaks keep returning despite apparent treatment success [2], [14].
The Core Limitation of Symptom Focused Therapy
When treatment is focused only on symptoms, the deeper biological processes remain untouched. Latent persistence, immune adaptation, and nerve tissue involvement are not addressed by surface level therapy. This creates a repetitive pattern where symptoms disappear and reappear without meaningful long term progress. Until treatment strategies move beyond symptom suppression and aim toward addressing latent viral persistence, why herpes medicines do not work will remain a persistent reality for patients worldwide [1], [2], [4], [14].
Improper, Diluted, or Unsafe Formulations
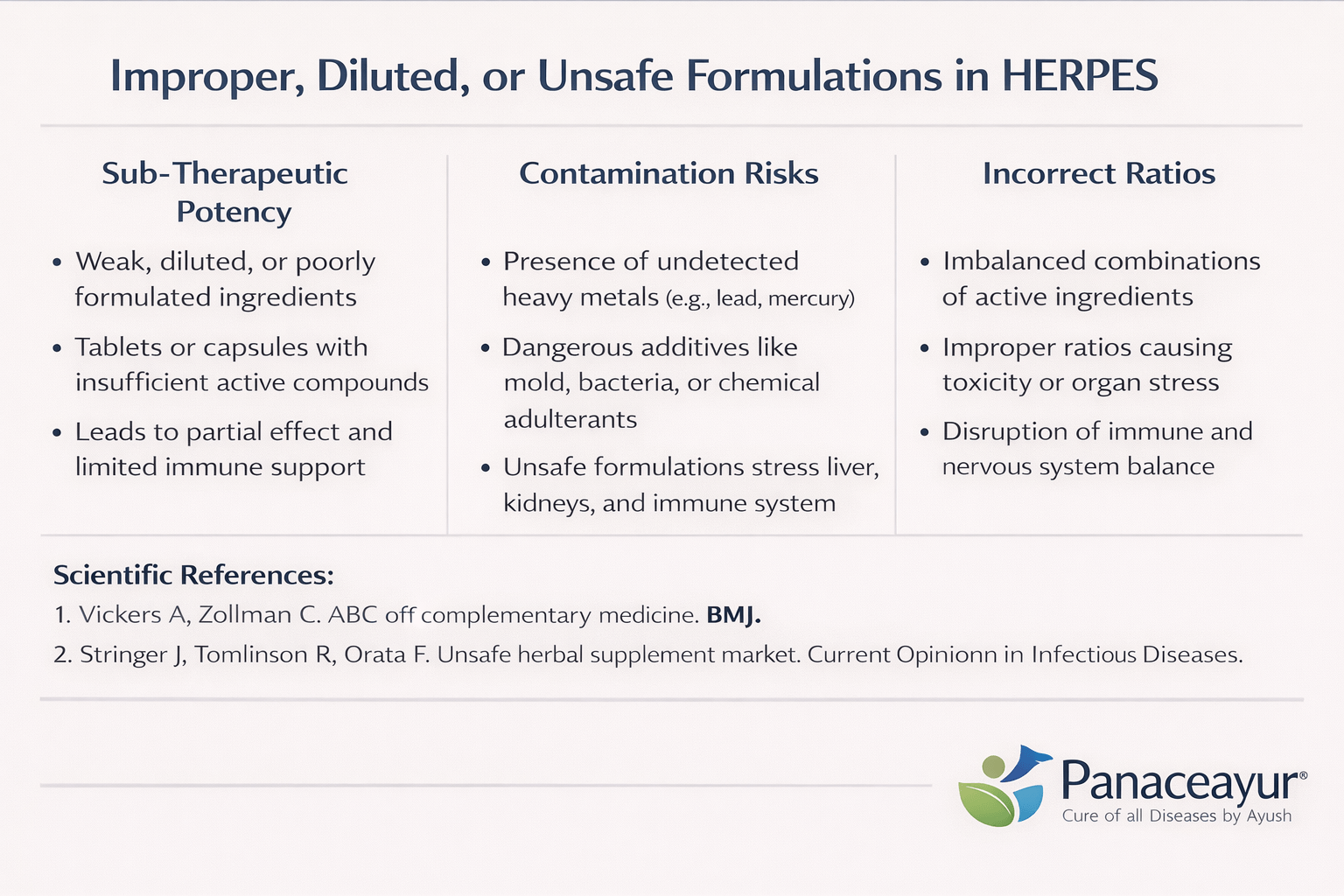
Quality of Medicine Determines Outcome
One major but rarely discussed reason why herpes medicines do not work is the poor quality of many formulations available in the market. You may assume that every tablet, capsule, or herbal product sold for herpes treatment meets strict quality standards. In reality, there is wide variation in raw material sourcing, processing methods, and formulation integrity. When medicine quality is compromised, therapeutic outcomes are inevitably compromised as well [11].
Dilution and Sub Therapeutic Potency
Many market bought herpes medicines contain diluted active ingredients. This dilution may occur intentionally to reduce cost or unintentionally due to poor manufacturing controls. From your perspective as a patient, the medicine appears legitimate, yet the actual dose reaching your system is insufficient to create a meaningful biological effect. Over time, repeated exposure to weak formulations trains the virus and the immune system into a pattern of partial suppression rather than resolution. This contributes significantly to why herpes medicines do not work long term [11].
Risk of Contamination and Undeclared Substances
Another critical issue is contamination. Studies have repeatedly shown that many commercially available herbal and alternative medicines contain undeclared substances, heavy metals, pharmaceutical adulterants, or microbial contaminants. When you consume such products without medical supervision, you are not only failing to treat herpes effectively, but you may also be burdening the liver, kidneys, and immune system. This internal stress further weakens immune control over latent herpes infection [11], [12].
Incorrect Ratios Disrupt Biological Balance
Effective treatment requires precise ratios of active components. Whether the formulation is pharmaceutical or herbal, incorrect ratios can disrupt biological signaling rather than correct it. Too little has no effect, while too much can provoke toxicity or immune suppression. Market formulations are standardized for mass production, not individualized biology. As a result, they often fail to align with the complex immune and nervous system dynamics involved in herpes persistence [12].
Why Unsafe Formulations Worsen Long Term Outcomes
From a clinical standpoint, unsafe or poorly designed formulations do more harm than good. Instead of restoring balance, they add metabolic stress, interfere with immune regulation, and sometimes cause adverse reactions that patients mistake for healing responses. When this happens, treatment adherence drops, trust in therapy declines, and the underlying herpes infection remains unresolved. This is another clear reason why herpes medicines do not work, even when patients sincerely follow instructions [11], [12].
The Hidden Cost of Unregulated Market Medicines
The failure of these formulations is not due to lack of effort on your part. It is rooted in a system that prioritizes mass distribution over therapeutic precision. Until medicines are produced with verified quality, correct ratios, and professional oversight, herpes treatment will continue to deliver inconsistent and disappointing results. This reality explains why many patients cycle through multiple products without achieving lasting improvement [11], [12].
Why Cheap or “Free” Herpes Medicines Usually Fail
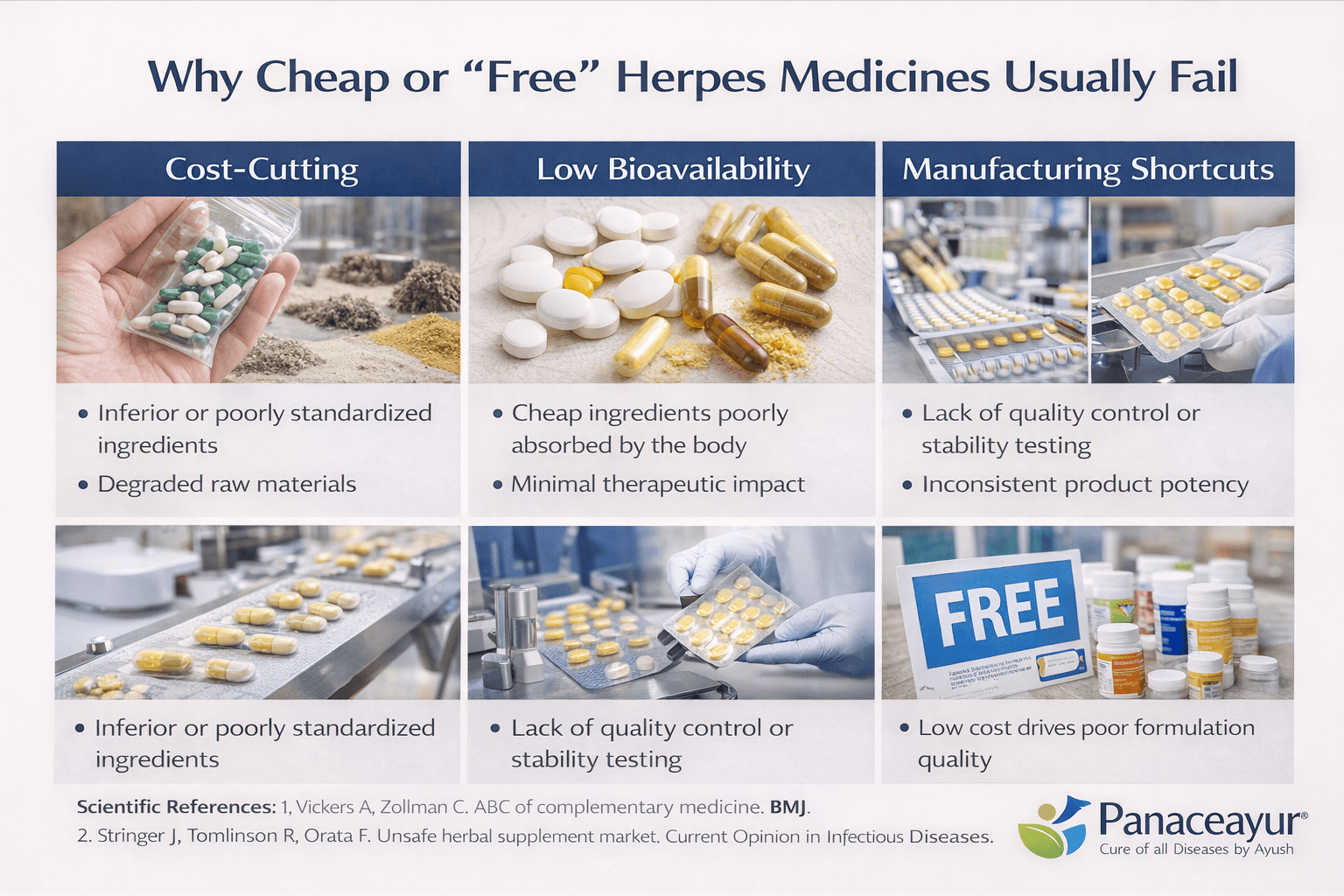
Cost Cutting Begins at the Raw Material Level
A major reason why herpes medicines do not work when they are cheap or promoted as free is aggressive cost cutting at the raw material stage. High quality pharmaceutical or herbal ingredients require careful sourcing, testing, and processing. When products are sold at unusually low prices, manufacturers often compromise by using inferior grade raw materials, poorly standardized extracts, or degraded active compounds. As a patient, you may not see this difference on the label, but biologically, the medicine lacks the strength required to influence a chronic viral condition like herpes [11].
Low Bioavailability Limits Therapeutic Action
Even if an ingredient is present, its ability to be absorbed and utilized by the body is critical. Cheap formulations frequently ignore bioavailability enhancement techniques because they increase production costs. Without proper formulation science, active compounds pass through the digestive system without reaching effective concentrations in the bloodstream or tissues. This is especially problematic in herpes, where systemic immune modulation and neural penetration are required. As a result, these medicines appear harmless but deliver minimal therapeutic impact, reinforcing why herpes medicines do not work long term [12].
Manufacturing Shortcuts Compromise Consistency
High quality medicines demand strict manufacturing controls to ensure batch to batch consistency. In low cost or mass market products, manufacturing shortcuts are common. These include inadequate quality testing, poor mixing protocols, and lack of stability assessment. This means one batch may feel mildly effective while another produces no effect at all. For you as a patient, this inconsistency creates confusion and false expectations, while the underlying herpes infection continues unchecked [11], [12].
“Free” Medicines Shift the Cost Elsewhere
Medicines advertised as free are rarely free in a biological sense. The cost is often shifted to compromised formulation quality, absence of professional supervision, or undisclosed additives. In some cases, free products are used as marketing tools rather than therapeutic solutions. When treatment is driven by distribution volume instead of clinical outcome, effectiveness becomes secondary. This model is fundamentally incompatible with managing a chronic viral condition that requires precision and long term strategy [11].
Cheap Products Increase Long Term Health Burden
Paradoxically, repeated use of cheap or free herpes medicines can increase long term health costs. Ineffective treatment prolongs viral persistence, weakens immune regulation, and may expose you to contaminants or unnecessary additives. Over time, this leads to more frequent outbreaks, greater dependence on suppressive drugs, and increased frustration. The failure is not due to lack of effort on your part, but due to a system that prioritizes low cost over biological effectiveness [12].
The Core Economic Reality of Effective Treatment
Effective herpes management cannot be reduced to the lowest price point. Quality raw materials, validated processing, bioavailability optimization, and safety testing all carry unavoidable costs. When these elements are missing, treatment outcomes suffer. This economic reality explains why cheap or free herpes medicines usually fail, and why lasting results require formulations designed for biology rather than marketing [11], [12].
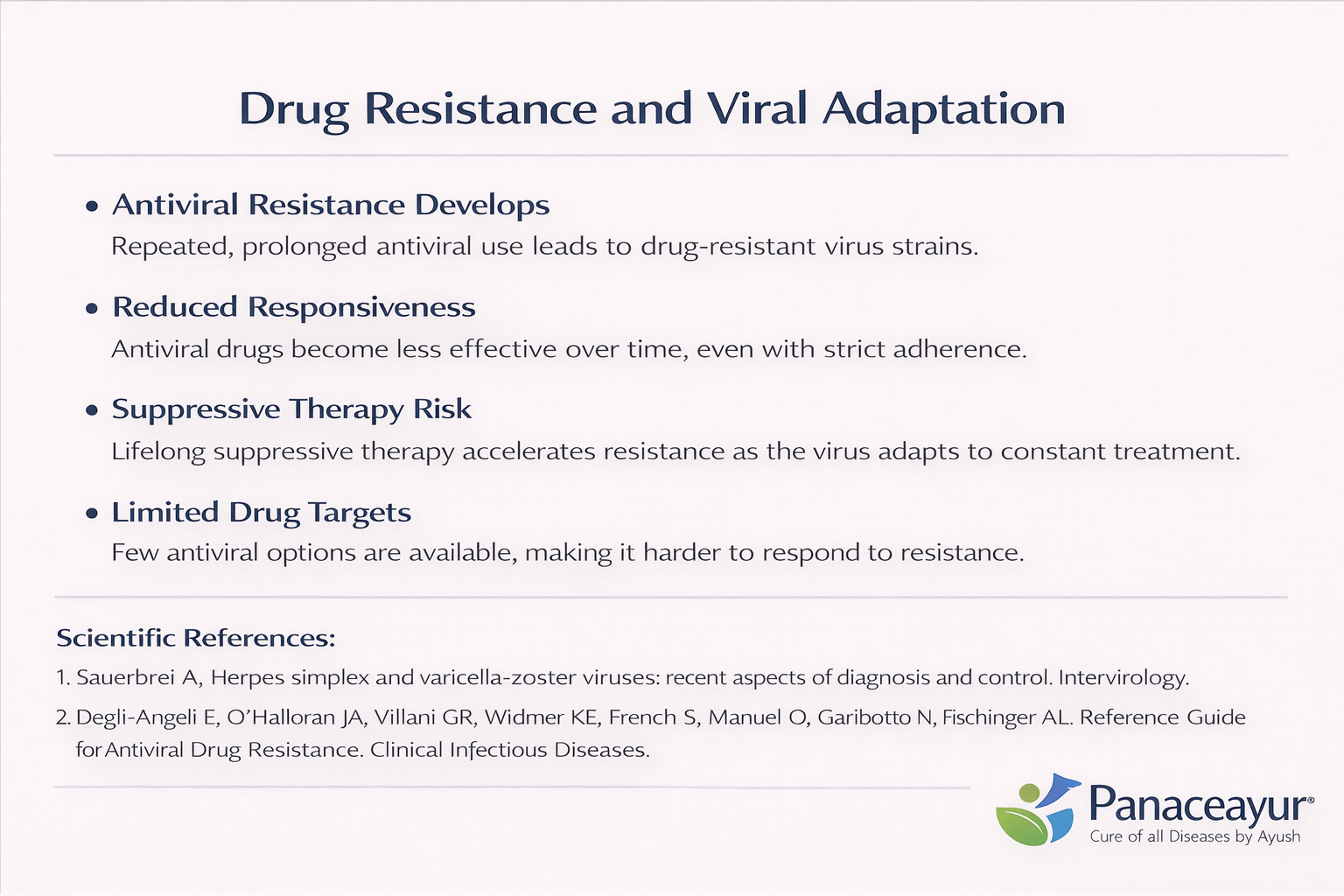
How Repeated Antiviral Use Trains the Virus
One of the most serious but poorly explained reasons why herpes medicines do not work over time is drug resistance. Herpes viruses are biologically adaptive. When you repeatedly expose the virus to the same antiviral drug, especially at fixed doses, the virus gradually learns to survive in that environment. This process does not happen overnight, but with long term or intermittent antiviral use, resistant viral strains begin to dominate. As a result, medicines that once reduced outbreaks lose their effectiveness [4], [6].
Reduced Responsiveness Despite Strict Compliance
Many patients assume that treatment failure occurs because they missed doses or did not follow instructions properly. In reality, you may take antiviral medicines exactly as prescribed and still notice diminishing results. This reduced responsiveness happens because the virus adapts at a molecular level. Genetic mutations allow it to bypass the drug’s inhibitory mechanisms, making standard doses less effective or completely ineffective over time [4].
Why Suppressive Therapy Accelerates Resistance
Suppressive therapy is often recommended for long periods or even lifelong use. While this approach reduces outbreak frequency initially, it also places constant selective pressure on the virus. From a biological standpoint, continuous drug exposure favors viral variants that can replicate despite the presence of medication. Over months or years, these resistant strains become dominant, explaining why outbreaks may return even while you remain on treatment [6].
Limited Drug Targets Increase Failure Risk
Most antiviral drugs for herpes target a narrow range of viral enzymes involved in replication. When the virus alters these targets, the drug loses its ability to bind effectively. Because market medicines rely on similar mechanisms of action, switching from one antiviral to another often produces limited benefit. This narrow therapeutic strategy contributes significantly to why herpes medicines do not work long term [4], [6].
Clinical Consequences of Viral Adaptation
Once resistance develops, higher doses or prolonged therapy are often attempted. This increases the risk of side effects without guaranteeing improved outcomes. In some patients, resistant herpes strains lead to more frequent or prolonged outbreaks, greater nerve irritation, and increased dependence on medication. The virus becomes harder to control, not because it has become stronger, but because treatment has failed to evolve alongside it [4].
Why Drug Resistance Demands a New Treatment Philosophy
Drug resistance exposes a fundamental flaw in symptom focused, single target treatment models. Herpes is not a static enemy. It adapts to pharmacological pressure. Until treatment strategies address immune restoration, neural environment stabilization, and long term viral containment beyond replication suppression, why herpes medicines do not work will remain a predictable outcome rather than an exception [6].
Absence of True Rasayana and Regenerative Therapy
Why Suppression Without Rebuilding Always Fails
A deeply ignored reason why herpes medicines do not work is the complete absence of true regenerative therapy. Most market based herpes treatments are designed only to suppress viral activity during outbreaks. They do not rebuild immune strength, repair tissue damage, or restore long term biological resilience. When suppression is applied without regeneration, the body remains vulnerable, and the virus continues to exploit this weakness [7], [14].
No Immune Rebuilding Means No Long Term Control
Herpes persistence is closely linked to immune exhaustion. Repeated outbreaks indicate that the immune system is unable to maintain durable surveillance over latent viral reservoirs. Modern herpes medicines do not actively rebuild immune competence. They temporarily lower viral replication but leave immune signaling pathways unchanged. As a result, once the medicine is stopped or stress increases, viral reactivation becomes inevitable. This explains why many patients feel dependent on lifelong medication without achieving lasting stability [8], [14].
Regeneration Is Essential in Chronic Viral Disease
Chronic viral infections cause subtle but cumulative damage to nerve tissue, immune communication, and inflammatory regulation. Without regenerative intervention, this damage accumulates over years. Market medicines do not address nerve recovery, mitochondrial function, or tissue level repair. They focus narrowly on viral enzymes. From a biological perspective, healing cannot occur unless damaged systems are restored. This absence of regeneration is a major reason why herpes medicines do not work long term [7].
Why Symptom Control Cannot Replace Rasayana Principles
In traditional medical systems, long term disease resolution requires restoration of vitality, not just removal of symptoms. Rasayana represents therapies aimed at rebuilding strength, resilience, and regenerative capacity at a systemic level. When herpes treatment lacks this dimension, therapy remains incomplete. Suppression may quiet the disease temporarily, but without internal rebuilding, the underlying susceptibility remains unchanged [8], [14].
The Long Term Consequence of Ignoring Regeneration
When true regenerative therapy is absent, patients often experience a cycle of temporary improvement followed by relapse. Over time, outbreaks may become more frequent or recovery slower, reflecting progressive immune fatigue rather than viral aggression. The failure is not due to patient noncompliance, but due to a treatment model that does not support long term healing. This structural gap explains why herpes medicines do not work, despite decades of pharmaceutical advancement [7], [8], [14].
No Guidance on Diet, Lifestyle, and Triggers
Why Medicines Fail When Daily Triggers Are Ignored
A critical but frequently neglected reason why herpes medicines do not work is the absence of guidance on diet, lifestyle, and daily triggers. Herpes reactivation is not random. It is strongly influenced by stress levels, sleep quality, immune resilience, and metabolic balance. When these factors are ignored, medicines operate in isolation while the internal environment continues to favor viral reactivation [7], [8].
Stress Directly Weakens Immune Control Over Herpes
Psychological and physiological stress has a direct suppressive effect on immune surveillance. Elevated stress hormones interfere with cellular immunity, which plays a key role in keeping latent herpes virus under control. If you are taking antiviral or herbal medicines but continue to live under chronic stress, the virus receives repeated opportunities to reactivate. This is why outbreaks often coincide with emotional strain, work pressure, or major life events, despite ongoing treatment [7].
Sleep Deprivation Promotes Viral Reactivation
Adequate sleep is essential for immune regulation and tissue repair. Poor sleep disrupts cytokine balance and reduces the effectiveness of immune responses that suppress latent viral activity. Many patients experience outbreaks after nights of poor sleep or irregular routines. When treatment plans do not address sleep hygiene, medicines alone cannot compensate for this biological deficit. This oversight contributes significantly to why herpes medicines do not work long term [8].
Dietary Factors Influence Inflammation and Immunity
Diet plays a subtle but powerful role in herpes recurrence. Highly inflammatory foods, irregular eating patterns, and nutrient deficiencies weaken immune stability and promote systemic inflammation. When dietary guidance is absent, the body remains in a pro inflammatory state that favors viral reactivation. Medicines taken in this context are forced to work against ongoing internal imbalance, limiting their effectiveness [7], [8].
Lifestyle Patterns Determine Long Term Outcomes
Herpes is sensitive to lifestyle rhythms. Irregular schedules, excessive physical exertion without recovery, poor hydration, and neglect of mental health all increase recurrence risk. Market medicines rarely address these aspects, leaving patients unaware of how daily habits directly influence disease behavior. Without lifestyle correction, treatment becomes reactive rather than preventive [7].
Why Comprehensive Guidance Is Essential
Effective long term control of herpes requires more than pharmacological intervention. It demands alignment between treatment, lifestyle, and biological needs. When diet, sleep, stress management, and daily routines are excluded from care plans, medicines are forced to compensate for systemic imbalance they were never designed to correct. This gap explains why herpes medicines do not work, even when patients remain compliant and motivated [7], [8].
Incorrect Dosage, Duration, and Self Medication
Fixed Dosage Cannot Match Biological Needs
Herpes treatment frequently fails because fixed dosages are applied without considering individual biological variation. Antiviral medicines are often prescribed using standardized dosing schedules that do not account for viral load, immune competence, prior drug exposure, or chronicity of infection. When dosage does not align with the body’s actual requirement, viral suppression becomes inconsistent, allowing reactivation to occur despite apparent treatment compliance [4], [6].
Premature Stopping Reinforces Recurrence
Many patients discontinue medication as soon as visible symptoms resolve. This decision is usually driven by the assumption that surface healing equals disease control. In reality, stopping treatment early allows viral activity to rebound from latent reservoirs before immune stabilization has occurred. Repeated cycles of premature discontinuation condition the disease into a relapsing pattern, where outbreaks become more predictable and difficult to control over time [6].
Improper Use Reduces Therapeutic Effect
Incorrect timing, missed doses, and inconsistent intake significantly reduce the effectiveness of antiviral therapy. Some patients take medicines only during severe symptoms, while others self adjust frequency based on comfort rather than medical guidance. This irregular exposure creates fluctuating drug levels that neither suppress viral replication effectively nor support immune adaptation. Such patterns undermine treatment reliability and promote long term instability [4].
Risks of Unsupervised Self Medication
Self medication is a major contributor to treatment failure. Without professional oversight, patients may combine multiple drugs, repeat courses unnecessarily, or rely on online advice rather than clinical evaluation. This behavior increases the risk of side effects, drug interactions, and biological stress without improving outcomes. In chronic viral conditions, unsupervised medication use often complicates disease behavior rather than resolving it [12].
Duration Determines Stability, Not Speed
Short treatment courses may reduce symptom intensity but rarely provide durable control. Chronic viral infections require sufficient duration to stabilize immune responses and limit viral reactivation cycles. When duration is inadequate, treatment remains reactive instead of stabilizing. Over time, this leads to increased reliance on repeated courses rather than sustained disease control [6].
Long Term Consequences of Incorrect Treatment Patterns
Incorrect dosage, inappropriate duration, and self directed medication do not simply reduce effectiveness. They reshape disease behavior by promoting viral adaptation, immune fatigue, and patient frustration. The result is a prolonged cycle of recurrence that becomes increasingly difficult to interrupt. Effective management requires disciplined dosing, appropriate duration, and professional supervision rather than intermittent or self guided approaches [4], [6], [12].
Herpes Rarely Exists as a Single Viral Problem
In clinical reality, herpes infections often do not exist in isolation. Many patients carry additional latent viruses such as cytomegalovirus, Epstein Barr virus, or human herpesvirus 6. These viruses may remain clinically silent, yet they continuously interact with the immune system. When treatment focuses only on herpes and ignores these co infections, immune burden increases and long term control becomes unstable [9], [10], [14].
Immune Overload Reduces Viral Control Capacity
Each latent virus places a constant demand on immune surveillance. When multiple herpes family viruses coexist, the immune system is forced to divide its attention. Over time, this creates immune exhaustion rather than immune strength. In such a state, suppressing one virus temporarily does not restore balance. Outbreaks recur not because herpes is aggressive, but because the immune system is overstretched and unable to maintain long term viral containment [14].
CMV and EBV Alter Immune Signaling
Cytomegalovirus and Epstein Barr virus are known to reshape immune behavior over time. They alter T cell populations, inflammatory signaling, and immune memory. When these viruses are active or semi active, they weaken the body’s ability to control other latent infections. If these contributors are not identified and addressed, herpes outbreaks may continue despite apparently appropriate treatment [9], [14].
HHV 6 Disrupts Immune Regulation
Human herpesvirus 6 has a unique ability to interfere with immune regulation and neuro immune communication. In some individuals, it contributes to fatigue, immune dysregulation, and altered stress response. When HHV 6 is present, herpes behavior often becomes unpredictable, with irregular outbreaks and slower recovery. Treating herpes alone in this context fails to address the underlying immune disruption [10], [14].
Why Single Virus Treatment Models Fail
Most market treatment models are designed to target one virus at a time. This approach ignores the complexity of viral ecosystems within the body. Chronic viral diseases are cumulative in their effect on immunity. When co infections are overlooked, treatment remains incomplete and outcomes remain inconsistent. Comprehensive viral assessment is essential for restoring immune balance and achieving stable control [9], [10], [14].
The Consequence of Ignoring Hidden Contributors
When co infections are left unrecognized, patients often experience repeated treatment cycles with diminishing returns. Symptoms may shift, fatigue may persist, and outbreaks may appear without clear triggers. These patterns reflect immune overload rather than treatment failure alone. Long term stability requires addressing the full viral burden rather than focusing narrowly on one visible infection [14].
Psychological and Neuro Immune Neglect
Stress Hormones Directly Suppress Antiviral Immunity
Psychological stress is not an abstract concept in chronic viral disease. It produces measurable biological changes that directly weaken immune control. Elevated stress hormones interfere with cellular immunity, particularly the immune responses responsible for keeping latent viruses in a dormant state. When stress becomes chronic, immune surveillance is reduced, creating favorable conditions for viral reactivation even in individuals who are otherwise following treatment correctly [7], [8].
The Nervous System and Immunity Are Biologically Linked
The nervous system and immune system function as a tightly connected network. Neural signals regulate immune responses, while immune activity influences brain function and stress perception. In chronic herpes infection, repeated viral reactivation sensitizes nerve pathways and disrupts this balance. If psychological stress is persistent, neural signaling becomes dysregulated, leading to impaired immune coordination. This neuro immune imbalance allows latent viruses to reactivate more easily and recover more slowly [8].
Chronic Stress Creates Immune Exhaustion
Short term stress can temporarily activate immune responses, but prolonged stress has the opposite effect. Continuous exposure to stress hormones reduces immune cell efficiency and promotes inflammatory fatigue. Over time, the immune system becomes less responsive to viral threats. In this state, suppressive medicines may reduce symptom severity, but they cannot compensate for an exhausted immune environment. Long term stability becomes difficult to achieve without addressing psychological stressors [7].
Emotional Health Influences Recurrence Patterns
Clinical observations consistently show that herpes outbreaks often follow emotional strain, anxiety, unresolved trauma, or prolonged mental fatigue. These patterns are not coincidental. Emotional stress alters neuro immune signaling, lowering the threshold for viral reactivation. When treatment plans ignore emotional and psychological health, patients may experience outbreaks without obvious physical triggers, leading to confusion and frustration [8].
Neuro Immune Neglect Limits Long Term Stability
Most market based treatment models focus exclusively on viral suppression while overlooking neuro immune health. This omission leaves a critical vulnerability unaddressed. Without stabilizing stress responses, restoring nervous system balance, and supporting immune resilience, treatment outcomes remain fragile. Sustainable control of chronic viral conditions requires attention to both psychological well being and immune regulation, not medication alone [7], [8].
Sexual Transmission Continues Despite Symptom Suppression
Absence of Symptoms Does Not Mean Absence of Virus
One of the most dangerous misconceptions surrounding herpes treatment is the belief that sexual transmission stops when symptoms disappear. In reality, the herpes virus can remain active on the skin and mucosal surfaces even when there are no visible blisters, sores, or discomfort. This phenomenon is known as asymptomatic viral shedding. During this phase, a person may feel completely normal and still transmit the virus to a sexual partner [5], [6].
How Suppressive Therapy Creates False Reassurance
Suppressive antiviral therapy is effective at reducing visible outbreaks and lowering symptom severity. However, symptom reduction often creates a false sense of safety. When lesions are absent, many individuals assume they are no longer infectious. Clinically, this assumption is incorrect. Suppressive therapy reduces but does not eliminate viral shedding. As a result, transmission risk persists even during periods of apparent remission [5].
Asymptomatic Shedding Is Biologically Unpredictable
Asymptomatic shedding does not follow a predictable schedule. It can occur intermittently and without warning. Factors such as stress, fatigue, hormonal fluctuations, and immune changes can trigger shedding without producing noticeable symptoms. Because this process is invisible, individuals relying solely on symptom monitoring cannot accurately assess transmission risk [6].
Impact on Partners and Relationships
False reassurance caused by symptom suppression has significant consequences for sexual partners. Many transmissions occur within long term relationships where trust is high and perceived risk is low. When one partner believes treatment has rendered them non infectious, protective measures may be relaxed. This dynamic contributes substantially to the continued global spread of herpes despite widespread use of antiviral medicines [5], [6].
Why Symptom Control Does Not Equal Transmission Control
From a virological perspective, controlling symptoms and controlling transmission are not the same outcome. Symptom control reflects reduced inflammation and surface damage. Transmission depends on viral presence at the skin or mucosal surface, which can occur independently of symptoms. Until viral shedding is fully addressed, sexual transmission remains a real and ongoing risk [6].
The Clinical Reality of Long Term Risk
The persistence of asymptomatic shedding explains why herpes prevalence continues to rise despite extensive treatment availability. Suppressive therapy improves quality of life, but it does not provide absolute protection against transmission. Accurate education, realistic risk assessment, and comprehensive management strategies are essential to prevent false confidence and unintended spread [5], [6].
Why Online Reviews and Testimonials Are Misleading
Short Term Improvement Is Often Mistaken for Cure
Online reviews and testimonials frequently highlight rapid symptom relief, creating the impression that a treatment has solved the problem. In chronic viral conditions, early improvement is common and often reflects natural fluctuation of symptoms rather than sustained biological change. When pain reduces or lesions heal, users may attribute this improvement entirely to the product, even though similar improvement may have occurred without intervention. This misunderstanding fuels overly positive testimonials that do not reflect long term outcomes [13], [14].
The Placebo Response Plays a Significant Role
The placebo response is a well documented phenomenon in medical research. When individuals believe strongly in a treatment, their perception of symptoms often improves temporarily. This effect can reduce pain, anxiety, and discomfort without altering the underlying disease process. In herpes, placebo driven improvement may coincide with natural remission phases, reinforcing the belief that a product is effective. Over time, as the placebo effect diminishes, symptoms often return, but follow up reviews are rarely posted [13].
Absence of Long Term Follow Up Data
Most online testimonials lack long term follow up. Reviews are usually written days or weeks after starting treatment, not months or years later. Chronic viral infections require extended observation to determine whether a therapy provides durable benefit. Without long term data, it is impossible to distinguish between temporary relief and meaningful disease control. This absence of follow up skews public perception and exaggerates perceived effectiveness [14].
Selection Bias Distorts Review Platforms
People who experience short term improvement are more likely to leave reviews than those who see no benefit or worsening symptoms. This selection bias creates an unbalanced representation of outcomes. Negative experiences are often underreported or removed, while positive anecdotes accumulate. As a result, review platforms present a distorted picture that favors products offering immediate relief rather than sustained benefit [13].
Testimonials Are Not Clinical Evidence
Personal stories can be emotionally compelling, but they are not a substitute for systematic clinical evaluation. Testimonials do not control for disease stage, immune status, co infections, or prior treatment history. They rarely disclose concurrent lifestyle changes or other therapies used simultaneously. Without these details, testimonials cannot establish cause and effect or predict outcomes for other individuals [14].
Why Critical Evaluation Is Essential
Relying on online reviews to guide treatment decisions can lead to repeated cycles of trial and disappointment. Chronic conditions require evidence based evaluation, objective monitoring, and long term assessment. Until outcomes are measured over time and across diverse populations, testimonials remain indicators of perception rather than proof of effectiveness [13], [14].
The Problem with “Fast Cure” Claims
Why Rapid Viral Eradication Is Biologically Impossible
Claims of a fast cure for herpes ignore fundamental principles of virology and human biology. Herpes viruses establish latency within nerve cells, where they remain protected from immune clearance and most pharmacological agents. Once latency is established, the virus integrates into long living cells that do not turn over quickly. From a biological standpoint, eliminating a latent virus within days or weeks is not feasible. Any claim suggesting otherwise conflicts with established scientific understanding [6], [14].
Latent Viruses Do Not Behave Like Acute Infections
Acute infections such as bacterial illnesses can sometimes be cleared rapidly because the pathogen remains exposed to immune attack or medication. Herpes behaves differently. After initial infection, viral activity becomes intermittent and hidden. During latency, the virus does not actively replicate, which means most antiviral medicines have no active target. Because of this, treatment outcomes unfold over time, not instantly. Rapid timelines promise speed where biology demands patience [14].
What Patients Experience During So Called Fast Cures
When people report improvement within a short time, they are usually describing symptom resolution rather than viral eradication. Lesions heal, pain reduces, and discomfort subsides. This improvement is real, but it represents suppression of active inflammation, not elimination of the virus. When stress, illness, or immune fluctuation occurs later, reactivation exposes the reality behind fast cure claims [6].
Why Marketing Language Exploits Natural Remission
Herpes naturally cycles between active and quiet phases. Many fast cure claims are timed to coincide with this natural remission. When symptoms would have resolved on their own, the improvement is attributed to the product. This creates the illusion of rapid success. Without long term observation, it is impossible to distinguish between true biological change and coincidental timing [14].
Long Term Stability Requires Biological Adaptation
Sustained control of a chronic viral condition depends on gradual immune adaptation, neural stability, and reduction of reactivation triggers. These processes develop over months, not days. Any approach that bypasses this reality sacrifices credibility. Promising speed undermines trust and sets unrealistic expectations that eventually lead to disappointment and repeated treatment cycles [6], [14].
The Cost of Believing in Fast Solutions
Fast cure narratives encourage premature discontinuation of care, poor adherence to realistic protocols, and repeated switching between products. Over time, this behavior destabilizes disease management rather than improving it. Meaningful progress requires consistency, biological respect, and long term perspective. When cure claims ignore these principles, outcomes suffer regardless of intention [14].
Lack of Monitoring, Testing, and Progress Markers
Why Treatment Without Measurement Becomes Guesswork
One of the most critical gaps in herpes management is the absence of structured monitoring and objective progress markers. Many treatment approaches rely solely on visible symptom changes to judge effectiveness. While symptom observation is important, it does not reflect what is happening at the viral, immune, or neurological level. Without monitoring, both patients and clinicians are left guessing whether a treatment is producing meaningful biological change [13], [15].
Symptom Relief Is an Unreliable Indicator of Progress
Herpes symptoms naturally fluctuate over time. Outbreaks may reduce in frequency or intensity for reasons unrelated to treatment, including reduced stress or natural remission cycles. When progress is measured only by symptom absence, temporary improvement can be mistaken for long term stability. This lack of objective evaluation often leads to false confidence and premature conclusions about treatment success [13].
Absence of Baseline Assessment Limits Interpretation
Effective monitoring begins with a baseline assessment. Without understanding the initial immune status, viral exposure history, or overall health condition, it becomes impossible to evaluate change accurately. Many patients begin treatment without any reference point. As a result, improvements or setbacks cannot be contextualized, and treatment decisions are made without evidence based grounding [15].
No Long Term Tracking Masks Treatment Failure
Chronic viral conditions require long term observation. Short observation windows hide delayed relapses, immune fatigue, or gradual loss of treatment responsiveness. When monitoring stops after early improvement, treatment failure may only become apparent months later. By then, valuable time has been lost, and disease patterns may have become more entrenched [13].
Why Objective Markers Matter in Chronic Viral Care
Objective monitoring provides clarity. It allows differentiation between placebo driven improvement, natural remission, and genuine biological stabilization. Without such markers, patients often cycle through treatments based on perception rather than evidence. This cycle increases frustration, cost, and distrust, while the underlying condition remains inadequately addressed [13], [15].
The Consequence of Treating Without Feedback
When treatment lacks feedback mechanisms, it cannot evolve intelligently. Adjustments are delayed or inappropriate, and opportunities for early intervention are missed. Long term stability in chronic viral conditions depends on informed decision making, not assumptions. The absence of monitoring transforms care into trial and error rather than structured management [15].
Why Women, Older Adults, and Immunocompromised Patients Fail Faster
Biological Vulnerability Shapes Disease Behavior
Certain populations experience faster recurrence, poorer stability, and reduced treatment response in herpes infection due to inherent biological vulnerability. Women, older adults, and individuals with compromised immunity are not failing treatment because of noncompliance. Their bodies operate under different physiological constraints that standard treatment models do not adequately address [6], [7], [14].
Hormonal Fluctuations Increase Reactivation Risk in Women
In women, hormonal cycles significantly influence immune regulation and neural sensitivity. Fluctuations related to menstruation, pregnancy, postpartum changes, or menopause alter immune signaling and stress responses. These shifts lower the threshold for viral reactivation. When treatment protocols do not account for hormonal variability, control becomes inconsistent, and recurrence appears unpredictable despite ongoing therapy [6], [14].
Age Related Immune Decline Reduces Viral Control
As people age, immune efficiency naturally declines. This process affects the body’s ability to maintain long term surveillance over latent viruses. Older adults often experience slower immune responses, prolonged inflammation, and delayed recovery after outbreaks. Medicines that rely solely on viral suppression do not compensate for age related immune decline, leading to higher recurrence rates and prolonged healing [7], [14].
Immunocompromised States Magnify Treatment Limitations
Individuals with weakened immunity, whether due to chronic illness, prolonged stress, metabolic disorders, or medical treatments, face additional challenges. In these states, the immune system cannot effectively contain latent viral activity. Suppressive medicines may reduce symptom intensity, but they cannot restore immune capacity. Without immune rebuilding, outbreaks recur more frequently and resolve more slowly [6], [14].
Increased Sensitivity of the Nervous System
Viral latency in nerve tissue makes nervous system health a key determinant of disease stability. Women and older adults often experience heightened neural sensitivity due to hormonal changes or aging related nerve alterations. Immunocompromised individuals may also develop increased neural inflammation. These factors amplify reactivation signals, making symptom suppression alone insufficient [14].
Why Standard Treatment Models Fall Short
Most market treatments assume a uniform biological response across populations. This assumption fails to recognize differences in hormonal dynamics, immune resilience, and neural regulation. When these differences are ignored, outcomes diverge. Faster recurrence and poorer stability in these populations reflect unaddressed biological needs rather than inherent treatment resistance [6], [7], [14].
The Need for Population Aware Management
Effective long term control requires treatment strategies that recognize and adapt to population specific vulnerabilities. Without this adaptation, recurrence patterns persist and frustration grows. Understanding these biological realities is essential for setting realistic expectations and designing sustainable care pathways for those most at risk [6], [14].
Detox Burden and Long Term Internal Damage
Repeated Medication Use Creates Hidden Internal Stress
One of the least discussed consequences of long term herpes treatment is cumulative internal stress caused by repeated medication exposure. Antiviral drugs, herbal products, and combination therapies are often used intermittently or continuously over years. While short term use may appear harmless, repeated exposure places a sustained detox burden on the liver, kidneys, and gastrointestinal system. Over time, this internal load alters metabolism, immune signaling, and inflammatory balance [11], [12].
Liver and Kidney Load Alters Immune Regulation
The liver and kidneys play a central role in detoxification and immune regulation. When these organs are repeatedly stressed by long term medication use, their efficiency declines. Subtle impairment may not show immediate symptoms but gradually weakens immune coordination. In this state, the body struggles to maintain control over latent viral activity, leading to more frequent or prolonged recurrences despite ongoing treatment [12].
Gut Microbiome Disruption Weakens Defense
Many medicines alter gut microbiota composition, either directly or indirectly. The gut microbiome is closely linked to immune resilience and inflammatory control. Disruption of microbial balance reduces immune responsiveness and increases systemic inflammation. When gut health deteriorates, immune surveillance against latent viruses becomes less effective, allowing reactivation to occur more easily [11].
Accumulated Toxic Load Mimics Disease Progression
Patients often misinterpret fatigue, digestive discomfort, brain fog, or reduced tolerance to stress as progression of the viral disease itself. In many cases, these symptoms reflect accumulated metabolic and detox stress rather than viral aggression. When treatment continues without addressing this internal burden, symptoms persist or worsen, reinforcing the perception that the disease is becoming more severe [12].
Why Suppression Without Detox Balance Backfires
Suppressive therapy that ignores detox capacity forces the body to compensate internally. As detox pathways become overloaded, immune function declines further. This creates a paradox where increasing medication intensity yields diminishing returns. Instead of improving stability, treatment becomes another contributor to physiological imbalance [11], [12].
Long Term Consequences of Ignoring Internal Load
Over years, unaddressed detox burden contributes to immune fatigue, slower recovery, and heightened sensitivity to triggers. Patients may require higher doses, longer courses, or multiple products to achieve the same effect once obtained with minimal intervention. These patterns reflect internal strain rather than disease resistance. Sustainable management requires attention to internal balance alongside viral control [11], [12].
Why Google, Marketplaces, and Social Media Promote Non Curative Products
Algorithms Reward Visibility, Not Clinical Outcomes
Digital platforms such as search engines, online marketplaces, and social media operate on algorithms designed to maximize engagement, clicks, and sales. These systems do not evaluate whether a product delivers long term health outcomes. They prioritize visibility, advertising spend, keyword optimization, and user interaction. As a result, products that promise quick relief or dramatic claims often rise to the top, regardless of whether they offer durable biological benefit [15].
Marketing Language Outperforms Medical Accuracy
Non curative products often use simple, emotionally appealing language that aligns well with search behavior. Phrases suggesting rapid relief or easy solutions attract attention and clicks. In contrast, treatments that require time, personalization, or long term commitment are harder to market within short headlines or advertisements. This imbalance allows symptom focused products to dominate digital spaces while more comprehensive approaches remain less visible [15].
Marketplaces Favor Volume Over Evidence
Online marketplaces are structured to reward high sales volume, frequent transactions, and positive short term reviews. Products that produce immediate symptom relief generate quick feedback and repeat purchases, reinforcing their ranking. There is no mechanism within these systems to track long term effectiveness, recurrence rates, or biological outcomes. As a result, products that manage symptoms temporarily appear more successful than those aiming for deeper, slower change [15].
Social Proof Masks Lack of Long Term Data
User ratings and testimonials create an illusion of validation. However, these metrics rarely reflect long term follow up. Reviews are typically written shortly after use, during periods of natural symptom fluctuation or placebo response. Platforms treat these signals as indicators of success, even though they provide no insight into sustained disease control. This dynamic amplifies non curative solutions and suppresses critical evaluation [13], [15].
Regulatory Gaps Allow Ambiguous Claims
Many digital platforms do not require rigorous proof for wellness or supplement claims, as long as explicit medical promises are avoided. This regulatory gray zone allows products to imply benefits without demonstrating them. Algorithms then amplify these products based on engagement rather than evidence. The result is a digital environment where marketing strength outweighs clinical validity [15].
Why Visibility Should Not Be Confused With Effectiveness
High ranking, frequent advertisements, or widespread social media presence do not indicate therapeutic value. They reflect optimization for digital systems, not biological systems. Patients who equate visibility with effectiveness often cycle through multiple products without achieving lasting stability. Understanding this distinction is essential for navigating online health information critically [15].
Absence of Physician Supervision
Why Unsupervised Treatment Increases Failure Risk
One of the most consistent factors behind poor long term outcomes in herpes management is the absence of physician supervision. Many patients rely on self selected medicines, online recommendations, or advice from non clinical sources. Without professional oversight, treatment becomes fragmented and reactive. Chronic viral conditions require structured evaluation and ongoing adjustment, which cannot be achieved through unsupervised use [12], [15].
No Monitoring of Biological Response
Physician supervision is essential for observing how the body responds to treatment over time. Without this guidance, changes in symptom pattern, frequency of recurrence, or systemic reactions go unrecognized. Patients may continue ineffective therapies for months or abandon potentially useful ones prematurely. The absence of monitoring prevents timely correction and allows disease patterns to entrench [15].
Misinterpretation of Healing Reactions
During treatment, some individuals experience temporary changes that may reflect immune adjustment or metabolic stress. Without clinical interpretation, these changes are often misunderstood as either worsening disease or successful healing. This misinterpretation leads to inappropriate dose changes, unnecessary discontinuation, or escalation of therapy without justification. Physician guidance is critical to distinguish between meaningful progress and adverse reactions [12].
Risk of Unsafe Combinations and Interactions
Self medication frequently involves combining multiple products, sometimes from different systems of medicine. Without supervision, the risk of interactions increases. Certain combinations may strain detox pathways, suppress immune signaling, or counteract each other’s effects. These risks are rarely apparent to patients and may contribute silently to long term instability [12].
Lack of Personalized Adjustment Over Time
Herpes is a dynamic condition. Immune status, stress exposure, age, and health circumstances change over time. Physician supervised care allows treatment to evolve in response to these changes. In contrast, unsupervised approaches remain static. When therapy does not adapt, effectiveness declines and recurrence becomes more frequent [15].
The Clinical Value of Guided Care
Physician supervision does not merely involve prescribing medicine. It integrates assessment, monitoring, education, and timely modification. This structured approach reduces unnecessary exposure, improves safety, and increases the likelihood of durable stability. In chronic viral conditions, guidance is not optional. It is a foundational requirement for sustainable outcomes [12], [15].
Clear Patient Checklist to Identify a Non Working Herpes Medicine
Promises Speed Without Explaining Biology
One of the clearest warning signs is a product that promises rapid results without explaining how it works biologically. Chronic viral conditions do not resolve instantly. When a medicine claims quick eradication without addressing latency, immune adaptation, or long term stability, it signals marketing driven claims rather than medical logic [6], [14].
Relies Only on Symptom Disappearance
If effectiveness is defined solely by how fast blisters heal or pain reduces, the treatment is incomplete. Symptom improvement can occur naturally or temporarily, independent of meaningful viral control. A non working medicine focuses on visible relief while ignoring recurrence patterns, immune resilience, and long term outcomes [13], [14].
Lacks Transparency About Ingredients and Quality
Medicines that do not clearly disclose ingredient sourcing, formulation standards, or manufacturing practices should be approached with caution. Absence of transparency often reflects diluted formulations, inconsistent potency, or poor quality control. These factors directly limit therapeutic impact and safety [11], [12].
Offers the Same Dose and Formula for Everyone
A fixed one size approach indicates lack of personalization. Chronic viral behavior varies according to immune strength, stress exposure, age, and co infections. When a product does not adapt dosage or strategy to individual needs, long term effectiveness is unlikely [6], [15].
Depends Heavily on Testimonials Rather Than Evidence
When marketing relies primarily on reviews, anecdotes, or influencer endorsements without long term data, the product lacks clinical grounding. Testimonials rarely reflect sustained outcomes and often coincide with placebo response or natural remission phases [13], [14].
Avoids Professional Supervision or Follow Up
Medicines that encourage self medication without guidance, monitoring, or follow up place the burden of interpretation entirely on the patient. This absence of oversight increases misuse, delayed correction, and repeated cycles of failure [12], [15].
Discourages Questions or Critical Evaluation
A reliable treatment welcomes scrutiny and informed discussion. Products that discourage questions, dismiss biological explanations, or promote blind trust often mask limitations. Transparency and education are hallmarks of responsible care [14].
The Practical Takeaway for Patients
A non working herpes medicine is not defined by lack of effort on your part. It is defined by unrealistic promises, absence of personalization, poor transparency, and lack of supervision. Recognizing these signs helps patients avoid repeated disappointment and redirect efforts toward approaches grounded in biology and long term thinking [6], [12], [14], [15].
What a Science Aligned Long Term Strategy Looks Like
Accepting the Chronic and Latent Nature of the Condition
A science aligned strategy begins with accepting biological reality. Herpes is a latent viral condition that interacts continuously with the immune and nervous systems. Effective long term management does not chase rapid outcomes. It respects latency, immune adaptation, and the need for sustained internal stability. Strategies built on this understanding avoid unrealistic timelines and focus on progressive, measurable improvement [6], [14].
Prioritizing Immune Restoration Over Symptom Control
Long term stability depends on restoring immune competence rather than repeatedly suppressing symptoms. This involves supporting cellular immunity, reducing immune exhaustion, and improving resilience against reactivation triggers. When immune strength improves, viral activity naturally becomes less frequent and less intense. This shift represents biological progress rather than temporary relief [7], [8], [14].
Addressing the Nervous System as a Core Component
Because herpes resides within nerve tissue, nervous system regulation is central to durable outcomes. Stress modulation, sleep optimization, and stabilization of neuro immune signaling reduce reactivation signals. A science aligned strategy integrates these factors rather than treating the virus as isolated from mental and neurological health [8], [14].
Incorporating Systems Based Evaluation and Adjustment
Effective care evolves over time. It includes baseline assessment, periodic reassessment, and thoughtful adjustment based on response. This systems based approach recognizes that immune status, stress exposure, and metabolic health change. Treatment that adapts maintains relevance and effectiveness, while static approaches gradually lose impact [15].
Integrating Lifestyle, Diet, and Trigger Awareness
Daily habits shape immune behavior. Diet quality, sleep rhythm, stress exposure, and physical recovery all influence viral stability. A long term strategy integrates these elements as active components of care, not optional advice. When lifestyle aligns with biological needs, recurrence frequency naturally declines [7], [8].
Emphasizing Safety, Quality, and Supervision
Sustainable outcomes depend on formulation quality, correct dosage, and professional oversight. Supervised care reduces misuse, detects early warning signs, and prevents unnecessary internal burden. Safety and consistency matter more than speed in chronic viral conditions [12], [15].
Measuring Progress Beyond Symptoms
True progress is reflected in extended remission periods, improved stress tolerance, faster recovery, and reduced dependency on suppressive measures. These indicators provide a clearer picture of biological stability than symptom disappearance alone. Monitoring these markers supports informed decision making and realistic expectations [13], [15].
The Long Term Perspective That Delivers Stability
A science aligned strategy is patient, structured, and adaptive. It avoids shortcuts and prioritizes internal balance over superficial change. By respecting biology and focusing on regeneration, immune resilience, and systems level health, long term stability becomes achievable rather than elusive [6], [7], [14], [15].
Conclusion and Patient Takeaway Summary
Why Repeated Failure Is a System Problem, Not a Patient Problem
After examining every major factor, one conclusion becomes clear. Persistent recurrence and poor long term outcomes are not the result of patient negligence, weak willpower, or lack of discipline. They arise from treatment models that are structurally incomplete. Most approaches focus narrowly on symptoms, speed, or convenience while ignoring latency, immune exhaustion, nervous system involvement, co infections, lifestyle triggers, and long term regeneration. When these realities are overlooked, repeated failure becomes predictable rather than surprising [6], [14].
What Patients Commonly Experience in Real Life
Most patients follow a similar trajectory. Initial diagnosis is followed by suppressive medication, short term relief, and reassurance. Over time, outbreaks return, stress increases, confidence declines, and treatment dependence grows. New products are tried, testimonials are believed, and cycles repeat. This pattern is not random. It reflects a gap between biological complexity and simplified treatment promises [13], [14].
The Core Lessons Patients Should Retain
Herpes is a systemic, latent condition, not a surface infection. Symptom relief does not equal resolution. Absence of lesions does not mean absence of transmission. Fast cures contradict biology. One size approaches ignore individual terrain. Without immune rebuilding, nervous system stabilization, lifestyle correction, and long term supervision, durable stability remains unlikely [6], [7], [8], [14].
How to Make Informed Decisions Going Forward
Patients benefit most when they shift focus from speed to sustainability. This means asking whether a treatment addresses latency, immune resilience, stress biology, and long term adaptation. It means valuing monitoring, personalization, and professional guidance over marketing claims and online popularity. In chronic conditions, informed patience outperforms aggressive shortcuts [12], [15].
A Realistic and Empowering Perspective
Understanding these principles does not create hopelessness. It creates clarity. When expectations align with biology, frustration decreases and decision making improves. Long term stability is not achieved through a single product, but through a coherent strategy that respects how the body actually functions over time [7], [14].
Final Patient Takeaway
Sustainable control is built, not purchased. It emerges from alignment between immune health, nervous system balance, lifestyle integrity, and thoughtful therapeutic guidance. When these elements are integrated, recurrence becomes less frequent, recovery becomes smoother, and dependence on constant suppression gradually diminishes. This is not a promise of speed. It is a commitment to biological realism and long term stability [6], [7], [14], [15].
Frequently Asked Questions
Is herpes really a lifelong condition
Herpes establishes latency inside nerve cells, which means the virus can remain dormant for long periods. This biological behavior explains why long term management focuses on stability and immune control rather than rapid elimination. Latency does not mean constant symptoms, but it does mean the virus can reactivate under certain conditions
Why do outbreaks return even after successful treatment
Outbreaks return because most treatments suppress active viral replication without addressing latency, immune exhaustion, or trigger factors such as stress and sleep disruption. When these underlying contributors remain unchanged, reactivation remains possible
If symptoms are gone, can herpes still spread
Yes. The virus can be present on the skin or mucosa without visible symptoms through asymptomatic shedding. This is why transmission can occur even when lesions are absent and treatment appears effective
Do antiviral medicines stop herpes permanently
Antiviral medicines reduce the severity and duration of outbreaks, but they do not remove the virus from nerve tissue. Their role is suppressive rather than curative, which is why long term strategies are needed for stability
Why do some people have frequent outbreaks while others do not
Frequency depends on immune strength, stress exposure, sleep quality, co infections, hormonal factors, and nervous system regulation. Individual biological variation explains why outcomes differ significantly between people
Are fast cure claims for herpes reliable
Claims of rapid eradication conflict with established virology. Short term improvement usually reflects symptom resolution or natural remission rather than elimination of the virus. Sustainable improvement develops gradually, not instantly
Can diet and lifestyle really influence herpes recurrence
Yes. Stress, poor sleep, inflammatory diets, and irregular routines weaken immune control and increase reactivation risk. Addressing these factors improves long term stability alongside medical treatment
Why do online reviews often seem positive despite poor long term results
Most reviews are written shortly after symptom improvement and do not include long term follow up. Placebo response and natural remission contribute to positive early feedback that may not reflect sustained outcomes
Is self medication safe for long term management
Unsupervised treatment increases the risk of improper dosing, unsafe combinations, and delayed recognition of treatment failure. Chronic viral conditions benefit from structured supervision and periodic reassessment
What indicates that a treatment approach is working
Meaningful progress is reflected in longer remission periods, reduced outbreak frequency, improved stress tolerance, faster recovery, and reduced dependence on suppressive measures rather than symptom disappearance alone
Can co infections affect herpes outcomes
Yes. Latent viruses such as CMV, EBV, and HHV 6 increase immune burden and can destabilize control if left unaddressed. Treating herpes in isolation may limit long term success
What should patients realistically expect from a long term strategy
A realistic strategy prioritizes immune restoration, nervous system balance, lifestyle correction, and gradual adaptation. Progress is steady rather than dramatic, with emphasis on stability and quality of life rather than speed
Reference List
Core Virology, Latency, and Recurrence
[1] Whitley, R. J., & Roizman, B. (2001). Herpes simplex viruses. The Lancet, 357(9267), 1513–1518.
https://doi.org/10.1016/S0140-6736(00)04638-9
Supports: latent infection, neurotropism, recurrence biology.
[2] Nicoll, M. P., Proença, J. T., & Efstathiou, S. (2012). The molecular basis of herpes simplex virus latency. FEMS Microbiology Reviews, 36(3), 684–705.
https://doi.org/10.1111/j.1574-6976.2011.00320.x
Supports: why symptom control does not equal viral clearance.
[3] Steiner, I., Kennedy, P. G., & Pachner, A. R. (2007). The neurotropic herpes viruses: herpes simplex and varicella-zoster. The Lancet Neurology, 6(11), 1015–1028.
https://doi.org/10.1016/S1474-4422(07)70267-3
Supports: nerve residency, neural inflammation, recurrence sites.
Drug Suppression, Resistance, and Failure of Standard Therapy
[4] Piret, J., & Boivin, G. (2011). Resistance of herpes simplex viruses to nucleoside analogues. Antimicrobial Agents and Chemotherapy, 55(2), 459–472.
https://doi.org/10.1128/AAC.00615-10
Supports: antiviral resistance, diminishing response with repeated use.
[5] Wald, A., & Corey, L. (2007). Persistence in the population: epidemiology, transmission. Journal of Infectious Diseases, 196(Supplement_2), S119–S125.
https://doi.org/10.1086/522157
Supports: asymptomatic shedding, continued transmission despite treatment.
[6] Johnston, C., Koelle, D. M., & Wald, A. (2014). HSV-2: in pursuit of a vaccine. Journal of Clinical Investigation, 124(3), 915–924.
https://doi.org/10.1172/JCI73702
Supports: why modern medicine has not cured herpes.
Immune Dysfunction, Stress, and Neuro-Immune Failure
[7] Glaser, R., & Kiecolt-Glaser, J. K. (2005). Stress-induced immune dysfunction. Nature Reviews Immunology, 5(3), 243–251.
https://doi.org/10.1038/nri1571
Supports: stress, cortisol, immune suppression triggering recurrences.
[8] Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W., & Kelley, K. W. (2008). From inflammation to sickness behavior. Nature Reviews Neuroscience, 9(1), 46–56.
https://doi.org/10.1038/nrn2297
Supports: neuro-immune exhaustion and chronic viral illness behavior.
Co-Infections, Immune Burden, and Systemic Disease
[9] Griffiths, P., Baraniak, I., & Reeves, M. (2015). The pathogenesis of human cytomegalovirus. Journal of Pathology, 235(2), 288–297.
https://doi.org/10.1002/path.4437
Supports: CMV, EBV, HHV co-infection burden.
[10] Dockrell, D. H., & Paya, C. V. (2001). Human herpesvirus-6 and -7. Clinical Microbiology Reviews, 14(1), 73–98.
https://doi.org/10.1128/CMR.14.1.73-98.2001
Supports: hidden viral contributors ignored by single-disease treatments.
Limitations of OTC, Herbal Market Products, and Adulteration
[11] Ernst, E. (2002). Toxic heavy metals and undeclared drugs in Asian herbal medicines. Trends in Pharmacological Sciences, 23(3), 136–139.
https://doi.org/10.1016/S0165-6147(00)01972-6
Supports: quality, safety, and adulteration concerns in market products.
[12] Posadzki, P., Watson, L., & Ernst, E. (2013). Adverse effects of herbal medicines. British Journal of Clinical Pharmacology, 76(4), 603–618.
https://doi.org/10.1111/bcp.12123
Supports: organ stress and unsupervised long-term use risks.
Monitoring Failure, Placebo Response, and Misleading Reviews
[13] Hróbjartsson, A., & Gøtzsche, P. C. (2010). Placebo interventions for all clinical conditions. New England Journal of Medicine, 363(8), 781–789.
https://doi.org/10.1056/NEJMra091219
Supports: misleading symptom improvement without disease resolution.
Why Long-Term Cure Claims Fail Scientifically
[14] Virgin, H. W., Wherry, E. J., & Ahmed, R. (2009). Redefining chronic viral infection. Cell, 138(1), 30–50.
https://doi.org/10.1016/j.cell.2009.06.036
Supports: chronic viral persistence, immune adaptation, slow recovery.
Patient-Centric, Physician-Guided Models
[15] Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press.
https://nap.nationalacademies.org/catalog/10027
Supports: individualized, supervised, systems-based care over commodity medicine.












2 Responses
Thank you, I have just been looking for information approximately this topic for ages and yours is the best I have came upon till now.
However, what in regards to the bottom line? Are you sure concerning the source?
Thank you for your kind words , I’m glad you found the information useful.
Regarding the bottom line: the conclusions are based on sources that are credible and carefully evaluated. Wherever possible, I rely on primary references and cross-check findings against established research to ensure accuracy. That said, if you have a specific source or point you’d like clarified, I’d be happy to address it in detail or provide additional references for transparency.