- Ayurvedic Perspective
- Bridging Modern and Ayurvedic Understanding
- Anatomy and Physiology of Thyroid
- Risk Factors
- Pathology and Classification
- Symptoms
- Differentiated Thyroid Cancer
- Ayurvedic Correlation
- Medullary Thyroid Cancer
- Symptoms and Clinical Presentation
- Ayurvedic Correlation
- Anaplastic Thyroid Cancer
- Ayurvedic Correlation
- Diagnostic Approaches
- Modern Treatment
- Ayurvedic Care to Reverse Cancer
- Potent Herbal Interventions in Cancer Reversal
- Potent Mineral (Bhasmas and Rasoushadhis)
- FAQs on Ayurvedic Cancer Care
- References
Thyroid cancer represents the most common endocrine malignancy and has witnessed a striking global rise in incidence over the past several decades [1]. Current epidemiological data indicate that differentiated thyroid cancer (DTC), which includes papillary and follicular subtypes, accounts for nearly 85–90% of all cases worldwide. Among these, papillary thyroid carcinoma is the dominant variant, noted for its relatively indolent course and strong association with lymphatic spread [2]. Follicular carcinoma, while less common, demonstrates a hematogenous route of dissemination, frequently leading to distant metastases in the lungs and bones [3].
The global burden of thyroid cancer is unevenly distributed. Western countries such as the United States, Canada, and parts of Europe have recorded marked increases in incidence, partly attributed to enhanced diagnostic sensitivity, particularly through the widespread use of high-resolution ultrasound and fine-needle aspiration cytology (FNAC) [4]. However, this explanation alone does not account for the sharp rise, as parallel studies suggest genuine increases linked to radiation exposure, dietary imbalances in iodine, and endocrine-disrupting environmental toxins [5]. In South and East Asian populations, including India, China, and Japan, thyroid cancer exhibits distinct demographic and dietary correlations, with both iodine deficiency and excess acting as potential contributors to disease development [6].
From a demographic standpoint, thyroid cancer disproportionately affects women, with a female-to-male ratio of approximately 3:1. This striking gender bias has been associated with hormonal influences, particularly estrogen-mediated modulation of thyroid follicular cells [7]. The disease is most commonly diagnosed in individuals between the ages of 30 and 50, though differentiated cancers may present in children and young adults as well. In contrast, medullary thyroid carcinoma (MTC), which constitutes around 3–5% of cases, arises from parafollicular C cells and is often linked with germline RET mutations, making genetic counseling and family screening essential components of care [8]. Anaplastic thyroid carcinoma (ATC), although rare (accounting for less than 2% of cases), remains a critical clinical challenge. Its highly aggressive biology, rapid invasion of local structures, and resistance to conventional therapies result in median survival rates measured in months rather than years [9].
The public health implications of thyroid cancer are multifaceted. On one hand, the majority of differentiated cancers are associated with excellent long-term survival, exceeding 90% at 10 years with appropriate treatment. On the other hand, the aggressive subtypes (particularly ATC) represent a disproportionate share of thyroid cancer–related mortality. Furthermore, survivorship issues, including the lifelong use of levothyroxine following total thyroidectomy, metabolic adjustments, risk of recurrence, and psychosocial burdens, underscore the need for integrative and holistic models of care [10].
Ayurvedic Perspective
The ancient Ayurvedic classics provide remarkable insight into neck swellings resembling thyroid disorders, described primarily as Galaganda and Apachi. The Charaka Samhita (Nidana Sthana, Chapter 11) and Sushruta Samhita (Nidana Sthana, Chapter 11) mention Galaganda as a firm, localized swelling in the throat region, often associated with Kapha dosha aggravation and Meda Dhatu vitiation [11]. Clinically, this description parallels the indolent growth of differentiated thyroid cancers, where localized mass effects dominate the presentation.
Apachi, on the other hand, as detailed in the Bhavaprakasha (Madhyama Khanda), represents progressive glandular enlargements that may be multiple, painful, and associated with systemic manifestations such as cachexia and dyspnea [12]. This closely reflects the clinical aggressiveness of anaplastic carcinoma, which presents as a rapidly enlarging neck mass with systemic decline. Ayurveda interprets these pathologies through the lens of dosha imbalance:
- Kapha dominance manifests as slow, firm, non-painful growth (comparable to papillary/follicular cancers).
- Pitta involvement produces inflammatory changes, rapid progression, and destructive tissue changes (akin to anaplastic carcinoma).
- Vata association manifests in pain, hoarseness, and nerve-related symptoms, which often accompany advanced cancers infiltrating the recurrent laryngeal nerve.
From a causative perspective, Ayurvedic texts emphasize the role of Viruddha Ahara (incompatible diet), Mandagni (low digestive fire), and Ama (toxic metabolic residue) in creating a pathological terrain conducive to growths such as Galaganda and Apachi [13]. The conceptual overlap with modern oncology is profound: environmental carcinogens, hormonal dysregulation, and immune escape mechanisms align with the Ayurvedic view of disturbed internal balance.
Bridging Modern and Ayurvedic Understanding
By juxtaposing modern epidemiology with Ayurvedic nosology, a holistic picture emerges. Where modern oncology provides clarity on cellular mutations, signaling pathways, and systemic treatments, Ayurveda enriches the understanding with terrain-focused philosophy, where restoring Agni, balancing doshas, and supporting Ojas (vital immunity) are considered crucial not just for tumor control but also for long-term survival. This integrative lens offers a patient-centered model that acknowledges the strengths and limitations of both systems, laying the foundation for an expanded therapeutic approach.
Anatomy and Physiology of Thyroid
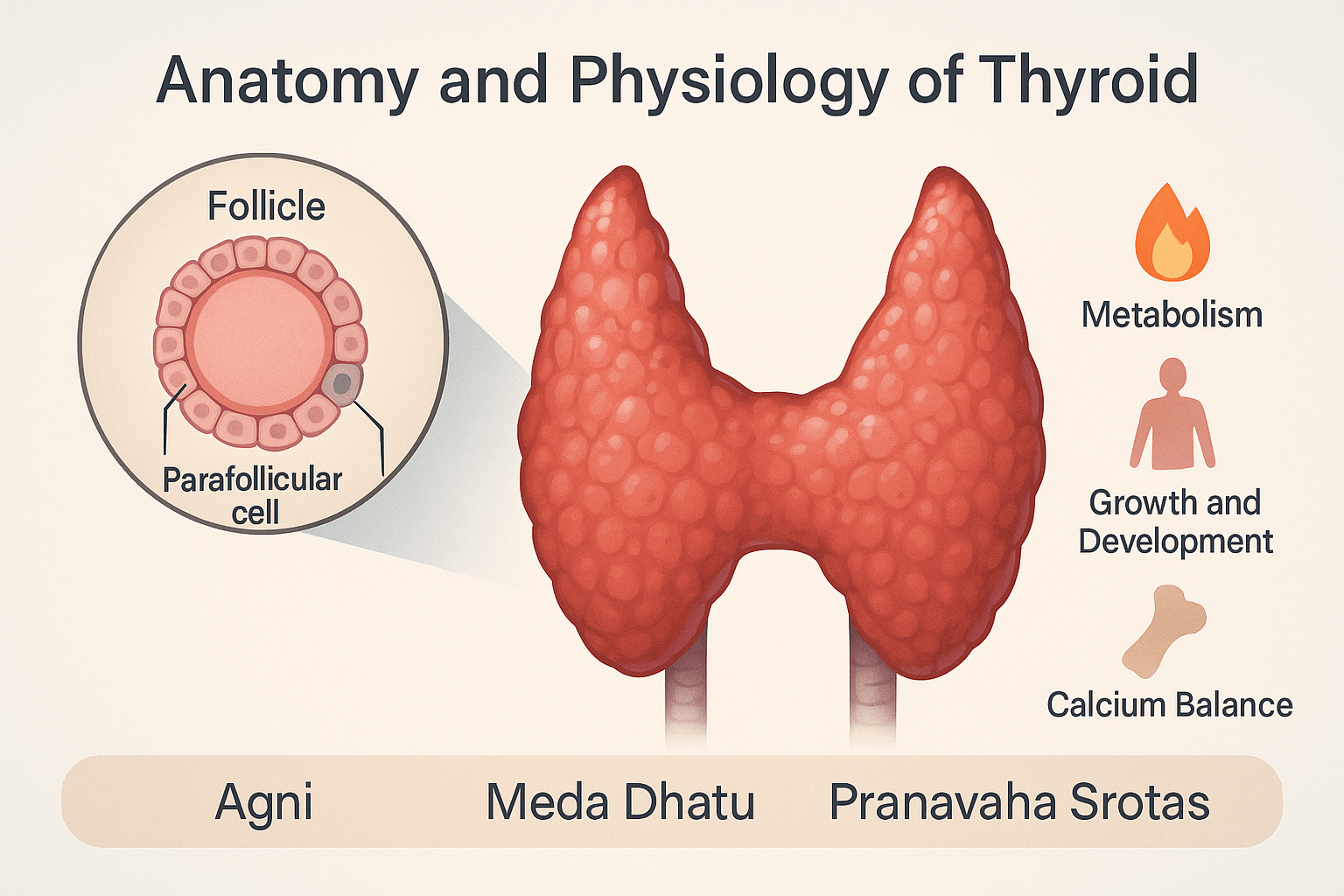
Structure of the Thyroid Gland
The thyroid gland is a butterfly-shaped endocrine organ located in the front of the neck, lying just below the larynx and straddling the trachea. It consists of two lateral lobes joined by a thin isthmus, giving it a distinctive H-shaped appearance. Each lobe is about 4–6 cm long, though size varies with age, sex, and body weight. The thyroid is highly vascular, receiving blood supply from the superior and inferior thyroid arteries, which ensures a constant hormonal output in response to metabolic demands [1]. On microscopic examination, the gland is composed of thyroid follicles—spherical units filled with colloid. The follicular cells that line these follicles are responsible for synthesizing thyroid hormones, while parafollicular cells, or C cells, located between the follicles, produce calcitonin [2]. This structural organization enables the thyroid to serve as both a hormone-producing and hormone-storing organ.
Hormones of the Thyroid
The thyroid produces three key hormones: thyroxine (T4), triiodothyronine (T3), and calcitonin. T3 and T4 are iodinated derivatives of the amino acid tyrosine and are crucial for controlling cellular metabolism. Their synthesis is stimulated by thyroid-stimulating hormone (TSH) released from the anterior pituitary, which itself is regulated by thyrotropin-releasing hormone (TRH) from the hypothalamus [3]. This hierarchical control mechanism is known as the hypothalamic–pituitary–thyroid (HPT) axis. Calcitonin, secreted by the C cells, plays a distinct role in calcium and bone metabolism, acting to lower serum calcium by inhibiting osteoclastic activity [4].
Functions of Thyroid Hormones
Thyroid hormones exert widespread effects on nearly every organ system. Their primary role is to regulate the basal metabolic rate, influencing oxygen consumption, thermogenesis, and energy utilization. In the cardiovascular system, T3 increases heart rate, cardiac output, and peripheral vasodilation, which explains why thyroid disorders often present with either palpitations in hyperthyroidism or bradycardia in hypothyroidism [5]. In the nervous system, thyroid hormones enhance synaptic activity and neuronal development, making them vital for normal cognitive and psychomotor growth in children. Growth and maturation of the skeleton are also dependent on adequate thyroid function, which is why hypothyroidism during childhood results in growth retardation. In addition, T3 and T4 regulate gastrointestinal motility, reproductive health, and lipid and carbohydrate metabolism, showing the gland’s central role in overall homeostasis [6].
Ayurvedic Mapping- Agni and Thyroid Function
In Ayurvedic science, the thyroid gland’s role in maintaining metabolism corresponds to the concept of Agni, the digestive and metabolic fire. Just as Agni governs digestion, transformation, and assimilation at the cellular and systemic levels, thyroid hormones drive similar functions in modern physiology. A sluggish thyroid parallels Mandagni, where digestion and metabolism slow down, leading to symptoms such as weight gain, lethargy, and constipation—features strikingly similar to hypothyroidism. Conversely, an overactive thyroid mirrors Tikshnagni, characterized by excessive metabolic activity, resulting in weight loss, irritability, palpitations, and diarrhea, akin to hyperthyroidism [7]. This conceptual overlap highlights how Ayurveda recognized the metabolic fire centuries before the endocrine role of the thyroid was discovered.
Meda Dhatu and Tissue Metabolism
The thyroid’s influence on fat metabolism can be mapped to Meda Dhatu, the adipose tissue described in Ayurveda. In hypothyroidism, there is increased accumulation of fat, sluggish metabolism, and swelling—all signs of Meda Vriddhi (increase of fat tissue). In hyperthyroidism, by contrast, rapid breakdown of stored fat leads to Meda Kshaya (depletion of fat tissue), resulting in emaciation and muscle wasting despite increased appetite [8]. This demonstrates that the balance of thyroid function is crucial for the maintenance of Meda Dhatu, and its derangement reflects as systemic disease both in modern pathology and Ayurvedic thought.
Pranavaha Srotas and Energy Utilization
Another important Ayurvedic correlation is with the Pranavaha Srotas, the channels responsible for respiration and energy distribution. Thyroid hormones facilitate oxygen utilization at the cellular level and drive mitochondrial energy production, which corresponds to the Ayurvedic view of Prana as the life force energizing body and mind. Disturbances in these functions lead to fatigue, shortness of breath, and lack of vitality—common presentations of thyroid disorders. In advanced thyroid cancers, compression of the trachea may even directly impair respiration, showing both structural and functional involvement of the Pranavaha Srotas [9].
Integrated Understanding
By aligning modern endocrinology with Ayurvedic principles, it becomes evident that the thyroid gland is more than an isolated endocrine organ. It is a regulator of Agni, a guardian of Meda Dhatu, and a vital participant in the Pranavaha Srotas. Both traditions, though separated by millennia, converge on the understanding that thyroid imbalance disturbs the entire systemic harmony. This integrative framework helps explain not only the anatomical and physiological basis of the gland but also the holistic terrain in which thyroid disorders and cancers manifest.
Risk Factors
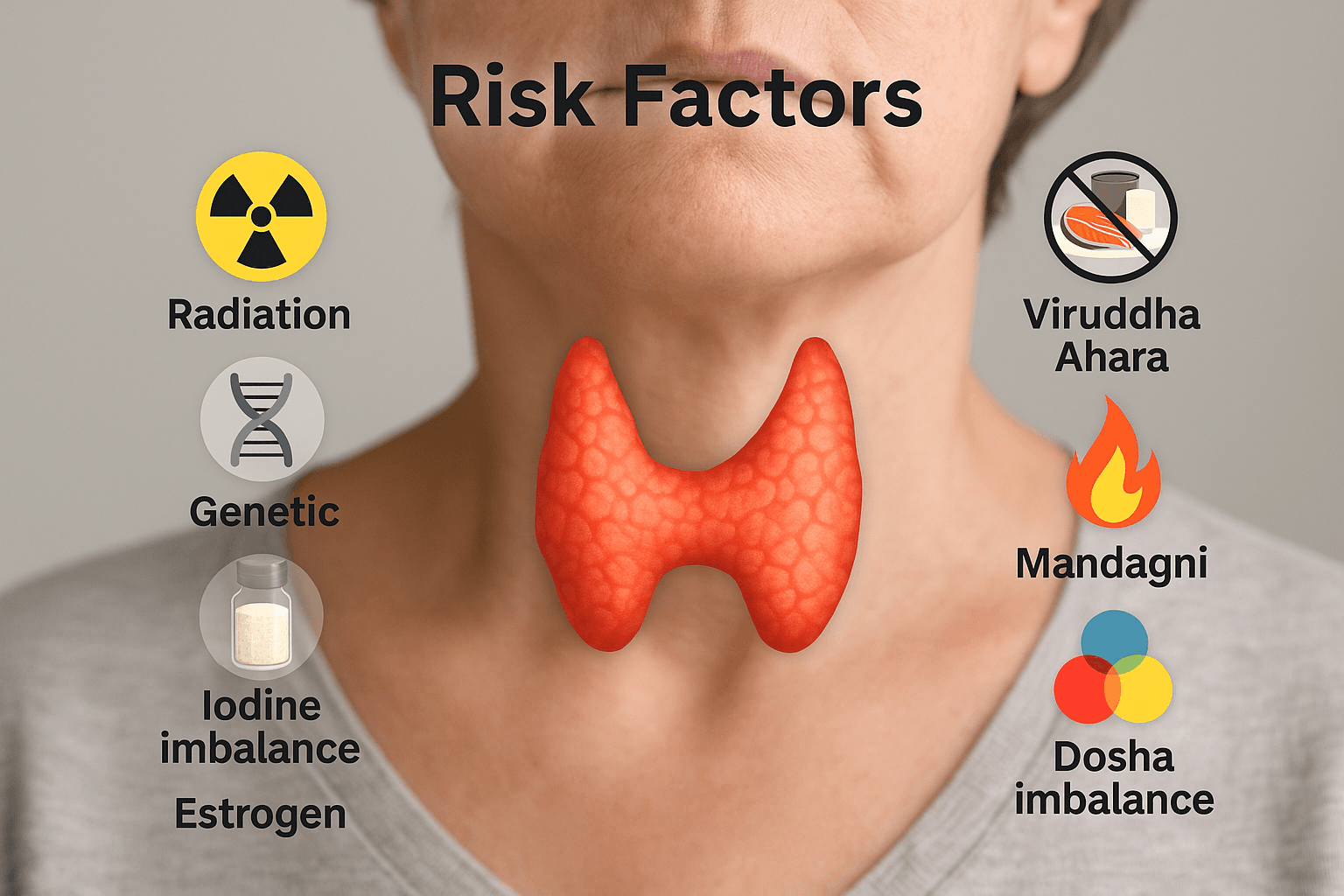
Genetic Factors
Genetic predisposition plays a significant role in the development of certain thyroid cancers. Medullary thyroid carcinoma is strongly linked to germline mutations in the RET proto-oncogene, particularly in familial syndromes such as Multiple Endocrine Neoplasia type 2 (MEN2A and MEN2B) [1]. These mutations not only increase cancer risk but also guide preventive strategies such as prophylactic thyroidectomy in high-risk individuals. Differentiated thyroid cancers, while mostly sporadic, have been associated with mutations in BRAF, RAS, and RET/PTC rearrangements, which drive abnormal cellular proliferation [2]. Anaplastic thyroid carcinoma, the most aggressive type, often arises from pre-existing differentiated cancers and involves mutations in TP53, TERT promoter, and PI3K/AKT pathways [3]. These genetic markers not only influence prognosis but are increasingly being targeted in precision oncology.
Environmental and Dietary Factors
Environmental exposures significantly contribute to thyroid cancer incidence. Radiation exposure—particularly during childhood—remains one of the strongest risk factors, as seen historically after nuclear accidents such as Chernobyl [4]. Iodine imbalance is another critical factor: deficiency can predispose to follicular carcinoma, whereas excess iodine intake may increase the risk of papillary carcinoma [5]. Industrial pollutants, endocrine-disrupting chemicals (such as bisphenol A and phthalates), and nitrate-contaminated water are emerging concerns in thyroid carcinogenesis [6]. Geographic variations in thyroid cancer incidence often reflect these environmental and dietary influences, underlining the interplay between external environment and internal susceptibility.
Lifestyle and Hormonal Influences
Lifestyle and hormonal status also shape thyroid cancer risk. Women are disproportionately affected, with a female-to-male ratio of about 3:1, suggesting the role of estrogen in thyroid cell proliferation [7]. Reproductive history, hormonal therapies, and obesity have all been linked with increased risk. Diets high in processed foods, refined sugars, and low in antioxidants contribute to oxidative stress and chronic inflammation, creating a pro-carcinogenic internal environment [8]. Conversely, diets rich in fruits, vegetables, selenium, and vitamin D may play a protective role. Sedentary lifestyle, stress, and metabolic syndrome further compound vulnerability by disturbing endocrine and immune function.
Ayurvedic Causative Factors
Ayurveda offers a complementary lens to understand thyroid cancer risk through the concepts of Ahara (diet), Vihara (lifestyle), and Dosha imbalance. One primary cause is Viruddha Ahara, or incompatible diet, which includes poor food combinations such as fish with milk, sour with dairy, or processed foods taken with natural foods. These combinations are believed to generate Ama (toxic metabolic residue), which blocks Srotas (channels) and creates a fertile ground for disease [9]. Another key factor is Mandagni, the weakened digestive and metabolic fire. When Agni is impaired, nutrients fail to be properly assimilated, leading to disturbances in Meda Dhatu (fat tissue) and abnormal growth processes that parallel tumor development. Dosha imbalance is central: Kapha aggravation encourages slow, firm swellings (similar to differentiated cancers), Pitta imbalance accelerates inflammatory and destructive processes (seen in aggressive cancers), while Vata involvement contributes to pain, voice changes, and rapid spread.
Integrative Perspective
By integrating modern and Ayurvedic insights, risk factors for thyroid cancer can be understood as both external exposures (radiation, toxins, diet) and internal vulnerabilities (genetic mutations, dosha imbalance, weak Agni). This dual perspective highlights not only the need for preventive measures such as genetic counseling, environmental regulation, and healthy diet, but also Ayurvedic strategies that strengthen Agni, balance doshas, and prevent Ama accumulation. Such holistic approaches may reduce susceptibility and improve resilience against thyroid pathologies.
Pathology and Classification
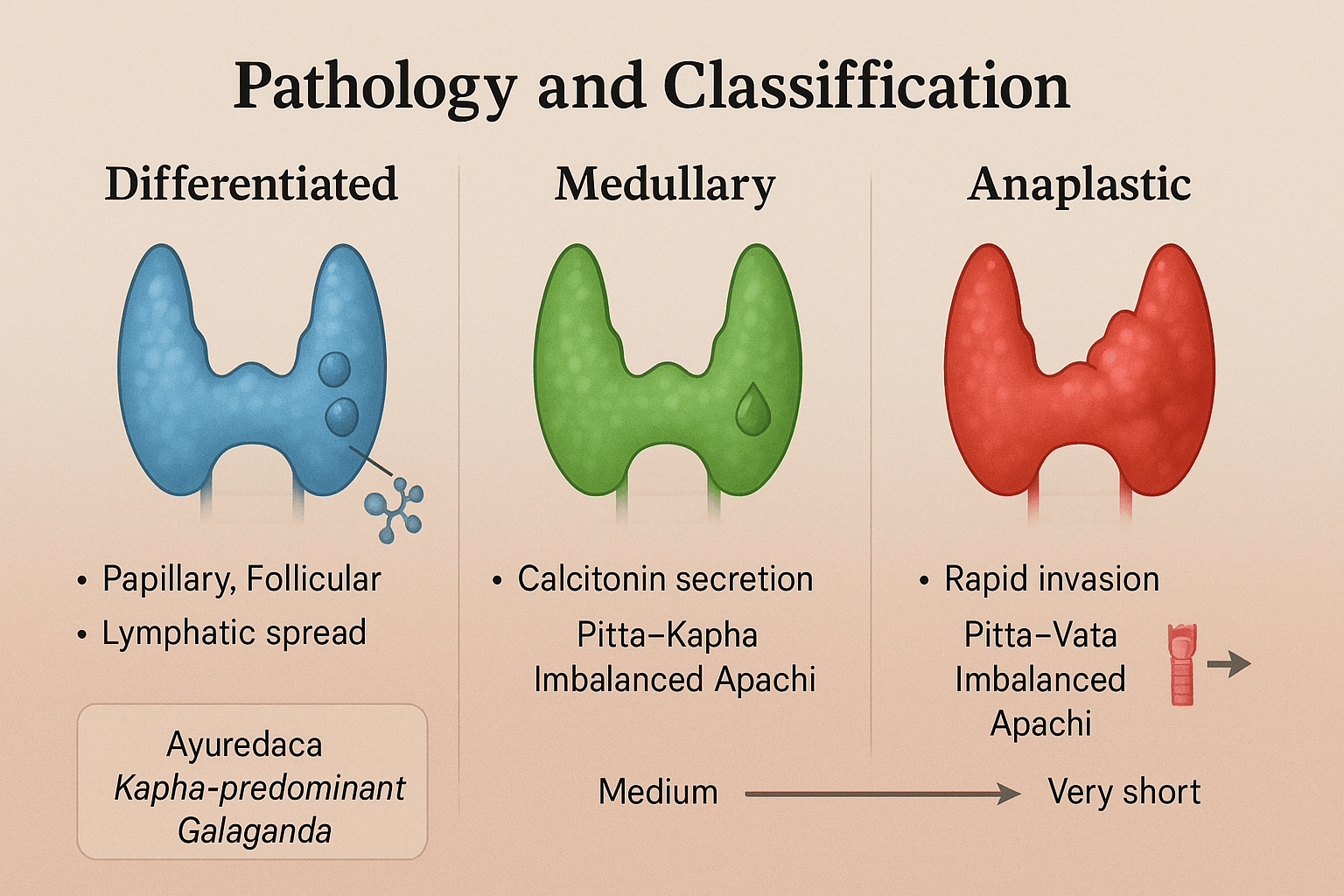
Thyroid cancers are classified based on their cell of origin, histological features, and biological behavior. The three principal categories are Differentiated thyroid cancer (papillary and follicular types), Medullary thyroid cancer, and Anaplastic thyroid cancer. Each type exhibits distinct morphology, progression, and prognosis, and their understanding is critical for both diagnosis and management. Ayurveda provides useful parallels, offering descriptions of neck swellings and systemic disturbances under the entities of Galaganda and Apachi, which can be conceptually aligned with these categories.
4.1 Differentiated Thyroid Cancer (Papillary and Follicular)
Papillary Thyroid Carcinoma (PTC):
Papillary thyroid carcinoma is the most common thyroid malignancy, accounting for nearly 70–80% of cases [1]. It arises from follicular epithelial cells and typically affects younger women. Histologically, it is characterized by papillary structures, nuclear clearing, grooves, and psammoma bodies. Clinically, PTC grows slowly and spreads primarily through the lymphatic system, often presenting with cervical lymph node involvement. Despite lymphatic spread, the overall prognosis is excellent, with a survival rate exceeding 90% when detected early [2].
Follicular Thyroid Carcinoma (FTC):
Follicular carcinoma comprises about 10–15% of thyroid cancers [3]. It also originates from follicular epithelial cells but tends to spread via the bloodstream rather than lymphatics, commonly metastasizing to lungs and bones. Histological hallmarks include follicular architecture with capsular and vascular invasion. FTC is more aggressive than PTC but still retains relatively favorable outcomes when treated promptly.
Ayurvedic Correlation:
Both papillary and follicular cancers can be related to Kapha-predominant Galaganda, where slow-growing, firm neck swellings occur without significant pain. The systemic spread seen in follicular carcinoma mirrors Meda Dhatu dushti (disorder of fat tissue) with involvement of deeper Dhatus such as Asthi (bone).
4.2 Medullary Thyroid Cancer (MTC)
Medullary thyroid carcinoma represents about 3–5% of thyroid cancers and arises from the parafollicular C cells, which produce calcitonin [4]. Clinically, patients often present with a thyroid nodule, diarrhea, or flushing due to hormone secretion. Biochemically, elevated calcitonin and carcinoembryonic antigen (CEA) serve as useful diagnostic markers.
Genetically, MTC is strongly associated with RET proto-oncogene mutations, and it may occur sporadically or as part of familial syndromes such as Multiple Endocrine Neoplasia type 2 (MEN2A and MEN2B). Prognosis varies: sporadic cases tend to have intermediate outcomes, while familial forms diagnosed early allow for preventive surgical approaches.
Ayurvedic Correlation:
MTC reflects a Pitta–Kapha imbalance, where glandular swelling is combined with systemic heat and toxin accumulation, leading to features such as diarrhea and metabolic disturbance. Ayurveda would recognize this as an aggravated Apachi with deeper Rakta and Meda Dhatu involvement, indicating systemic derangement.
4.3 Anaplastic Thyroid Cancer (ATC)
Anaplastic thyroid carcinoma is rare, accounting for less than 2% of thyroid cancers, but it is among the most lethal of all human malignancies [5]. It typically affects older adults and often arises from pre-existing differentiated thyroid cancers that have undergone genetic dedifferentiation.
Histologically, ATC is characterized by highly pleomorphic cells, giant cells, and spindle cells, with extensive necrosis and vascular invasion. Clinically, patients present with a rapidly enlarging neck mass, hoarseness, dysphagia, dyspnea, and pain due to local invasion of the trachea, esophagus, and recurrent laryngeal nerve. The disease course is fulminant, with median survival measured in months despite aggressive therapy.
Ayurvedic Correlation:
ATC resembles an extreme form of Pitta–Vata aggravated Apachi, where rapid tissue destruction, pain, hoarseness, and systemic decline occur. This aligns with Dhatupaka (destruction of tissues) and Srotorodha (blockage of channels), reflecting the aggressive and unstoppable nature of this malignancy.
Integrative Perspective
This classification illustrates a spectrum of thyroid cancers ranging from well-differentiated and indolent tumors (papillary, follicular) to intermediate forms (medullary) and finally to undifferentiated, highly aggressive anaplastic carcinoma. Ayurveda complements this understanding by contextualizing the disease within dosha imbalances and dhatu pathology, thereby offering insight into both prevention and supportive care.
Symptoms

General Symptoms of Thyroid Cancer
Thyroid cancers often remain silent in their early stages and may present as subtle changes that patients overlook until the disease progresses. The most common early manifestation is a neck lump or swelling, usually discovered by the patient during self-examination or incidentally during a clinical check-up. This swelling is typically firm, non-tender, and located in the anterior neck, sometimes accompanied by enlargement of cervical lymph nodes [1].
Another important symptom is hoarseness of voice, which occurs when the tumor compresses or infiltrates the recurrent laryngeal nerve. This leads to vocal cord paralysis and progressive alteration of voice quality. In some patients, this may be the first noticeable sign, particularly in aggressive forms of thyroid cancer [2].
Difficulty swallowing (dysphagia) is another frequent complaint, resulting from direct compression of the esophagus by the enlarging thyroid mass. Patients may describe a sensation of food sticking in the throat or discomfort when swallowing solid foods. As the tumor enlarges, this symptom may become more pronounced [3].
Breathing difficulties (dyspnea or stridor) are often observed when the tumor invades or compresses the trachea. Stridor, a harsh vibrating sound during breathing, indicates significant airway obstruction and usually signifies advanced disease requiring urgent intervention [4].
A persistent cough not related to infection is also a red flag. Unlike the cough associated with colds or bronchitis, this cough is chronic, dry, and unresponsive to standard treatments. It arises due to airway irritation from tumor invasion or enlarged lymph nodes pressing against respiratory passages [5].
From an Ayurvedic standpoint, these symptoms correspond to the classical features of Galaganda and Apachi. The Kapha predominance is reflected in neck swelling and heaviness, Vata disturbance manifests as hoarseness and difficulty in swallowing, while Pitta aggravation contributes to inflammation, pain, and rapid progression. Together, these signs provide an early clinical framework for recognizing thyroid malignancies in both modern and Ayurvedic paradigms [6].
Differentiated Thyroid Cancer
Symptoms and Clinical Presentation
1. Slow-Growing Nodule (Often Asymptomatic)
The hallmark of differentiated thyroid cancer is a slowly enlarging nodule in the anterior neck. Most patients initially do not notice it, as the growth is typically painless and subtle. In some cases, it may be discovered during a routine health check-up or incidentally on imaging done for unrelated reasons. As the nodule grows, patients may feel a localized fullness in the neck, or they may observe visible asymmetry when looking in the mirror. Unlike inflammatory swellings, the lump is usually firm, non-tender, and moves with deglutition, making it distinct from other cervical swellings [1].
2. Enlarged Cervical Lymph Nodes (Papillary Type)
In papillary thyroid carcinoma, lymphatic spread is very common, and patients may first present with enlarged lymph nodes in the neck before noticing any thyroid swelling. These nodes are often firm and fixed, occasionally causing cosmetic concern due to visible neck bulges. In advanced cases, metastatic lymph nodes may undergo cystic degeneration, giving rise to soft, fluctuant swellings. Compression of nearby structures by these enlarged nodes may result in hoarseness or difficulty swallowing [2].
3. Bone Pain and Skeletal Symptoms (Follicular Type)
Follicular thyroid carcinoma frequently spreads through the bloodstream, with a predilection for the skeletal system. Patients may complain of localized bone pain, tenderness, or even pathological fractures due to weakened bone integrity. Commonly affected sites include the ribs, pelvis, and vertebrae. Persistent, dull aching pain that does not respond to conventional pain relievers should raise suspicion of metastatic involvement. This presentation is often misinterpreted as arthritis or orthopedic problems until a proper workup is done [3].
4. Pulmonary Symptoms (Follicular Type)
When follicular carcinoma metastasizes to the lungs, patients may develop respiratory symptoms such as chronic cough, breathlessness on exertion, or chest discomfort. In advanced stages, hemoptysis (coughing up blood) may occur due to tumor invasion into the bronchi. These respiratory features may initially be attributed to infections like tuberculosis or asthma, leading to delays in cancer diagnosis. A high index of suspicion is crucial when such symptoms coexist with a thyroid nodule [4].
5. Hoarseness of Voice and Voice Fatigue
Although more common in aggressive thyroid cancers, differentiated cancers can occasionally cause voice changes if the tumor compresses the recurrent laryngeal nerve or if enlarged lymph nodes infiltrate nearby structures. Patients may notice progressive hoarseness, difficulty in projecting their voice, or unusual voice fatigue during speaking. These subtle changes may be ignored until they worsen, but they carry significant diagnostic value when paired with a thyroid swelling [5].
6. Difficulty Swallowing (Dysphagia)
A larger differentiated thyroid tumor may compress the esophagus, leading to dysphagia. Initially, this presents as a sensation of food “getting stuck” when swallowing solid foods, but in more advanced cases, even liquids may become difficult to swallow. This symptom reflects mechanical obstruction and is often accompanied by discomfort in the throat or upper chest during meals [6].
7. Pressure Sensation and Cosmetic Concerns
Patients sometimes describe a pressure or tightness in the neck, especially when lying down or wearing tight collars. Cosmetic concerns may also prompt medical consultation, as the swelling can alter the contour of the neck, particularly in slender individuals.
Ayurvedic Correlation
In Ayurveda, these symptoms align with Kapha-predominant Galaganda, where a firm, non-painful swelling develops in the anterior neck. The Kapha dominance explains the slow, painless progression, while Meda Dhatu involvement parallels the metastatic spread to bones and lungs in follicular carcinoma. Symptoms like dysphagia and hoarseness signify Vata aggravation, whereas any inflammatory changes (pain, warmth, redness) suggest Pitta involvement. This holistic mapping shows how symptomatology reflects the underlying dosha imbalance and dhatu pathology [7].
Medullary Thyroid Cancer
Symptoms and Clinical Presentation
1. Diarrhea and Flushing (Hormone Secretion Effects)
A distinctive feature of medullary thyroid carcinoma is its ability to secrete hormones and peptides, most notably calcitonin and carcinoembryonic antigen (CEA). In some cases, it also secretes vasoactive intestinal peptides (VIPs). These secretions cause persistent watery diarrhea, sometimes occurring more than 10–15 times per day, leading to severe dehydration, electrolyte imbalance, and weight loss [1]. In addition, patients may experience flushing episodes, characterized by sudden warmth, redness of the face and neck, and palpitations. These symptoms resemble carcinoid syndrome but are directly linked to medullary carcinoma’s neuroendocrine activity [2].
2. Neck Mass with Early Lymph Node Spread
The most common local presentation is a firm neck mass in the thyroid region. Unlike differentiated thyroid cancers, medullary carcinoma tends to spread to lymph nodes at an early stage. Patients may notice multiple enlarged cervical nodes or asymmetric neck swellings. On examination, these nodes are often firm and fixed, sometimes compressing adjacent structures, leading to hoarseness of voice, dysphagia, or a sensation of neck tightness [3].
3. Systemic Features in MEN Syndromes
Medullary thyroid carcinoma frequently occurs in association with Multiple Endocrine Neoplasia type 2 (MEN2A and MEN2B) syndromes. In these cases, symptoms may extend beyond the thyroid. Patients may present with pheochromocytoma, characterized by episodes of severe hypertension, sweating, palpitations, and headaches. Some may also develop hyperparathyroidism, leading to hypercalcemia, kidney stones, abdominal pain, and psychiatric disturbances [4]. These systemic features can complicate the clinical picture and often require genetic screening and family evaluation.
4. Other Associated Symptoms
Additional symptoms may include persistent cough, throat discomfort, and, in advanced disease, bone pain or liver involvement due to distant metastases. Fatigue, weakness, and unintended weight loss are often seen in later stages, reflecting both the tumor burden and the systemic metabolic disturbances caused by hormone secretion [5].
Ayurvedic Correlation
In Ayurveda, medullary thyroid cancer aligns with Pitta–Kapha dominant Apachi. The Pitta imbalance manifests as heat, flushing, and diarrhea (excessive metabolic fire disturbing water balance), while the Kapha component explains the firm neck mass and lymph node enlargement. The systemic spread in MEN syndromes can be viewed as Vyadhi Sankara (coexistence of multiple disorders), where one underlying imbalance triggers a cascade of diseases involving Rakta (blood), Meda (fat tissue), and Majja (nervous/endocrine system). Classical descriptions of Apachi include multiple glandular swellings and systemic disturbances, offering a close conceptual match to MTC [6].
Anaplastic Thyroid Cancer
Symptoms and Clinical Presentation
1. Rapidly Enlarging Painful Neck Mass
Anaplastic thyroid carcinoma often presents with a sudden, rapidly enlarging mass in the anterior neck, usually in older patients. Unlike the slow-growing nodules of differentiated thyroid cancers, this tumor expands aggressively over weeks rather than months. Patients frequently report pain, tenderness, and visible swelling that distorts the neck contour. The mass is often hard, irregular, and fixed to surrounding tissues, reflecting its invasive nature [1].
2. Hoarseness, Dysphagia, and Stridor
Because of its location and fast progression, ATC quickly compresses and infiltrates nearby structures. Hoarseness of voice arises from invasion of the recurrent laryngeal nerve, causing vocal cord paralysis. Dysphagia (difficulty swallowing) develops due to esophageal compression, while stridor (a harsh, high-pitched breathing sound) indicates significant airway narrowing. These symptoms often appear together, signaling advanced local disease. Patients may also complain of choking sensations, frequent coughing while eating, and progressive respiratory distress [2].
3. Local Invasion into Critical Structures
One of the most defining features of ATC is its relentless local invasion. The tumor infiltrates the trachea, causing obstruction and life-threatening respiratory compromise; the esophagus, resulting in severe swallowing difficulties; and the major blood vessels in the neck, leading to vascular encasement, hemorrhage, or venous obstruction. These aggressive behaviors distinguish ATC from other thyroid malignancies and explain its extremely poor prognosis [3].
4. Cachexia and Rapid Systemic Decline
Beyond local symptoms, patients with ATC experience cachexia—a wasting syndrome marked by unintentional weight loss, muscle wasting, profound fatigue, and anorexia. This reflects the tumor’s high metabolic demand, systemic inflammation, and release of catabolic factors. The general health decline is swift, and patients often transition from being relatively functional to severely debilitated within a short time frame [4].
5. Other Associated Features
Additional symptoms may include persistent cough, hemoptysis (coughing blood), or neck skin ulceration due to tumor infiltration. Unlike differentiated or medullary carcinomas, ATC rarely metastasizes at diagnosis because the local disease is already overwhelming, though distant spread to lungs and bones may occur late [5].
Ayurvedic Correlation
In Ayurveda, anaplastic carcinoma reflects an extreme form of Pitta–Vata aggravated Apachi. The Pitta dominance accounts for rapid tissue destruction, inflammation, and systemic wasting (Dhatupaka – burning and degeneration of body tissues), while Vata aggravation manifests as pain, hoarseness, difficulty in swallowing, and rapid systemic decline. The local invasion of trachea, esophagus, and vessels parallels the Ayurvedic concept of Srotorodha (blockage and destruction of vital channels), leading to collapse of essential life functions. The rapid deterioration and cachexia seen in ATC resonate with descriptions of Asadhya Vyadhi (incurable diseases) in the classical texts, where progression is quick and fatal if not addressed early [6].
Diagnostic Approaches
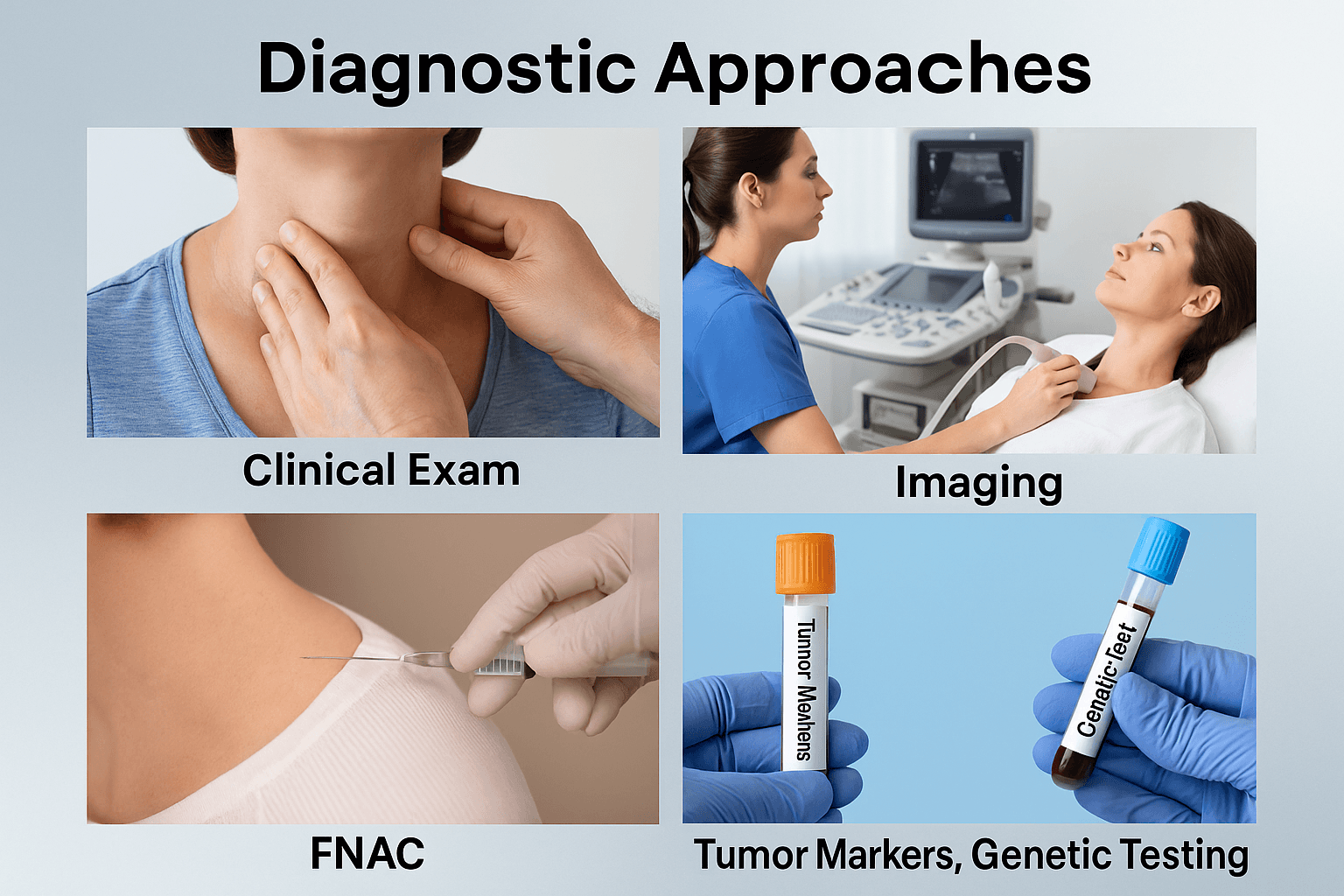
Clinical Examination
The first step in diagnosing thyroid cancer is a detailed clinical evaluation. A physician examines the neck for nodules, asymmetry, or swelling. Cancerous nodules are often firm, irregular, and fixed to surrounding tissues. Mobility during swallowing helps distinguish thyroid swellings from other cervical masses. Associated signs such as cervical lymphadenopathy, hoarseness of voice, dysphagia, or stridor further raise suspicion of malignancy [1].
Imaging Studies
Imaging plays a crucial role in characterizing thyroid nodules and planning treatment. Ultrasound of the thyroid is the gold standard for detecting suspicious nodules, assessing vascularity, margins, and microcalcifications. It also evaluates cervical lymph nodes for metastasis. In advanced disease, CT and MRI scans provide information on local invasion into the trachea, esophagus, or major vessels. PET scans may be used to detect distant metastases or evaluate aggressive variants such as anaplastic carcinoma [2].
Fine Needle Aspiration Cytology (FNAC)
FNAC remains the cornerstone of diagnosis for thyroid nodules. Under ultrasound guidance, a thin needle extracts cells from the suspicious lesion for cytological analysis. Papillary carcinoma often shows characteristic nuclear features, while follicular carcinoma requires evaluation of capsular or vascular invasion on surgical specimens. FNAC is minimally invasive and highly reliable, forming the basis of early detection and staging [3].
Tumor Markers
Certain biochemical markers support diagnosis and follow-up. Thyroglobulin is used to monitor differentiated thyroid cancers after thyroidectomy. Calcitonin and carcinoembryonic antigen (CEA) are elevated in medullary thyroid carcinoma and serve as sensitive markers for recurrence or residual disease. These markers are valuable for both staging and long-term surveillance [4].
Genetic Testing
Molecular diagnostics are increasingly important in thyroid oncology. RET proto-oncogene mutations are characteristic of medullary thyroid carcinoma, especially in familial cases associated with MEN2 syndromes. BRAF V600E and RAS mutations are common in papillary and follicular cancers, influencing both prognosis and treatment strategies. Genetic testing not only aids in confirming diagnosis but also helps guide targeted therapies and screening for at-risk family members [5].
Modern Treatment
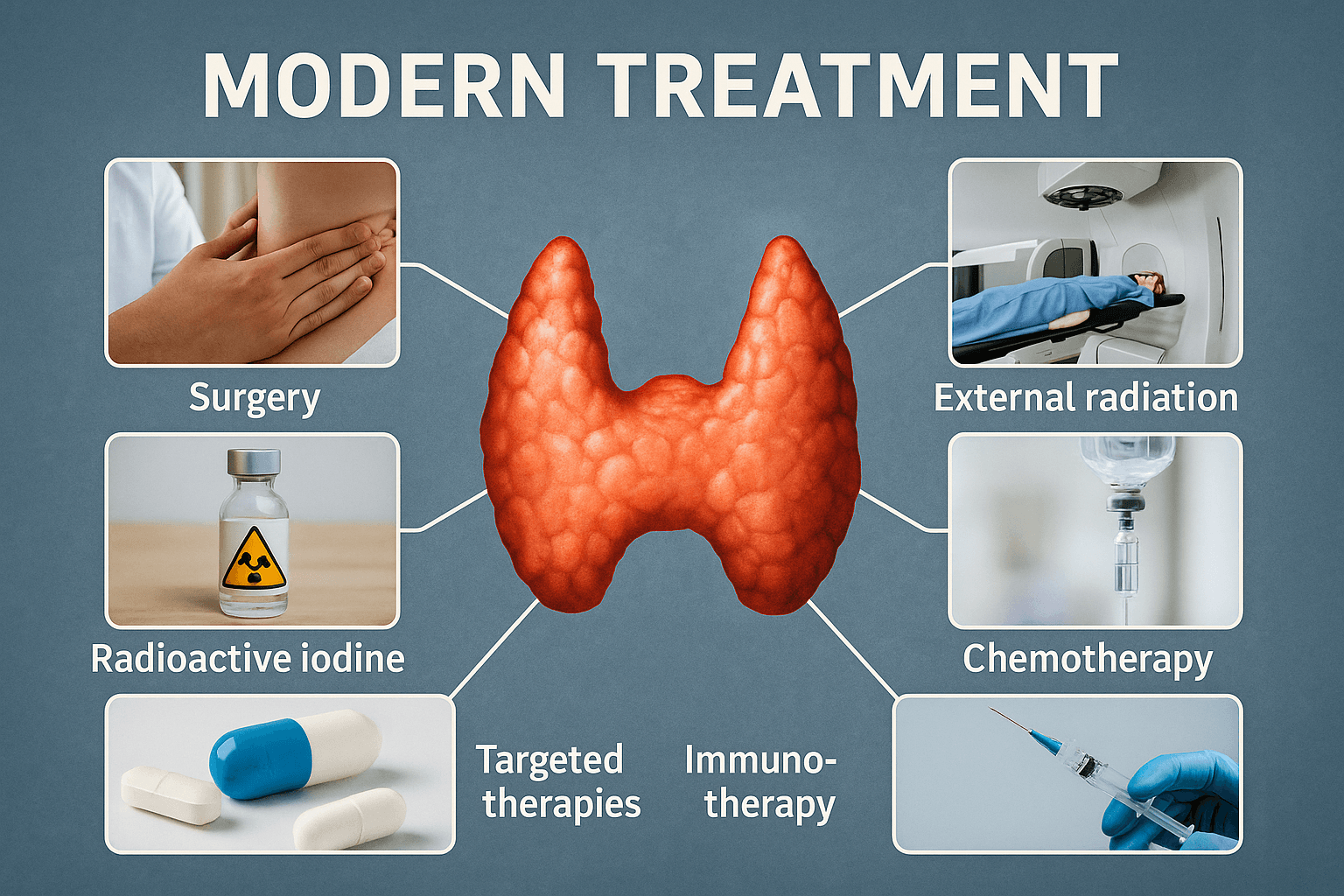
Surgery
Surgery remains the cornerstone of thyroid cancer management. For differentiated thyroid cancers, the standard procedure is total thyroidectomy, where the entire thyroid gland is removed. In cases with limited disease, a lobectomy may be performed, removing only the affected lobe. Surgery often includes lymph node dissection, particularly in papillary carcinoma where cervical lymph node spread is common. For medullary and anaplastic thyroid cancers, surgery may provide local control, although its role is limited in advanced or invasive cases [1].
Radioactive Iodine (RAI) Therapy
Following thyroidectomy, patients with differentiated thyroid cancers often undergo radioactive iodine ablation. Because thyroid follicular cells uniquely take up iodine, RAI selectively destroys residual thyroid tissue and microscopic metastatic deposits without harming most other tissues. This improves recurrence-free survival in intermediate- and high-risk patients. RAI is not effective in medullary or anaplastic cancers, since these do not arise from iodine-absorbing follicular cells [2].
External Beam Radiation Therapy (EBRT)
For patients with locally advanced disease not amenable to surgery or RAI, external beam radiation provides local control. It is particularly valuable in anaplastic carcinoma and in cases where surgical resection is incomplete. EBRT helps reduce tumor size, alleviate airway compression, and relieve symptoms such as pain or dysphagia [3].
Chemotherapy
Conventional chemotherapy has limited efficacy in thyroid cancer but is sometimes used in aggressive or refractory cases, especially anaplastic carcinoma. Agents such as doxorubicin and cisplatin may provide temporary disease control but are associated with significant side effects and poor long-term outcomes. In medullary carcinoma, chemotherapy plays only a supportive role when targeted therapies are unavailable [4].
Targeted Therapies
The advent of molecularly targeted drugs has transformed the landscape of thyroid cancer management.
- For differentiated cancers, tyrosine kinase inhibitors (TKIs) such as lenvatinib and sorafenib target vascular endothelial growth factor receptors (VEGFRs) and other kinases, showing significant benefits in progressive RAI-refractory disease.
- In medullary carcinoma, targeted therapies against RET mutations (e.g., selpercatinib, pralsetinib) have produced remarkable improvements in survival and disease control.
- In anaplastic carcinoma, drugs targeting BRAF V600E mutations (e.g., dabrafenib, trametinib combination) provide new hope for subsets of patients [5].
Immunotherapy
Immune checkpoint inhibitors, such as pembrolizumab (anti–PD-1 antibody), are under investigation for aggressive thyroid cancers, including anaplastic carcinoma. By reactivating the immune system to recognize tumor cells, these therapies offer potential for durable responses where traditional treatments fail. Although still emerging, immunotherapy represents a rapidly expanding frontier in thyroid oncology [6].
Ayurvedic Care to Reverse Cancer
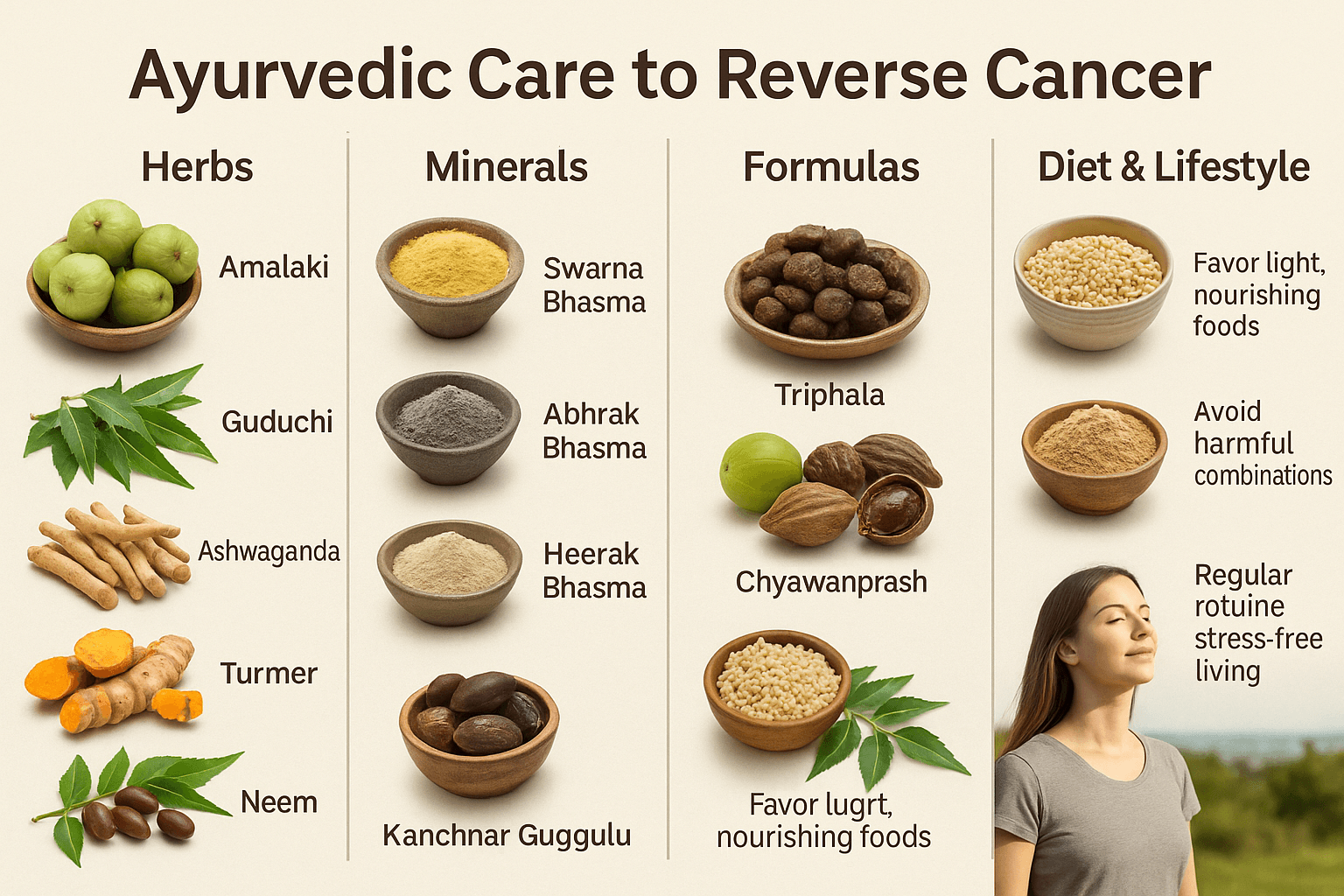
Understanding Cancer in Ayurveda
Ayurveda, the ancient science of life, looks at cancer in a very different way than modern medicine. Where modern oncology often sees cancer only as abnormal cells multiplying uncontrollably, Ayurveda goes deeper and asks: What created the ground for these cells to misbehave in the first place? This ground, or internal terrain, is just as important to heal as the tumor itself [1].
In classical Ayurvedic texts, conditions resembling cancer are described as Arbuda (tumor), Granthi (nodule), Apachi (glandular swelling), and Galaganda (neck swellings). These arise when the three doshas—Vata, Pitta, and Kapha—lose their harmony. Of the three, Kapha and Pitta usually dominate. Kapha provides the “substance” for a tumor to grow (thickening, heaviness, stagnation), while Pitta adds the “fire” that leads to inflammation, burning, and tissue destruction. Vata contributes later, bringing pain, rapid spread, and systemic weakness [2].
But Ayurveda does not stop at describing the problem. It provides a roadmap for healing. Ancient seers explained that when digestion and metabolism—called Agni (the metabolic fire)—become weak (Mandagni), food and experiences are not properly transformed. Instead, undigested toxins, known as Ama, accumulate in the tissues. This Ama blocks the natural channels of the body (Srotas) and disrupts normal tissue nutrition (Dhatu poshana). Over time, the tissues (dhatus) become distorted, leading to abnormal growths like Arbuda. In modern terms, we can compare this to chronic inflammation, oxidative stress, and immune dysfunction—all now recognized as drivers of cancer [3].
Ayurveda also points to wrong food and lifestyle choices (Viruddha Ahara and Viruddha Vihara) as causes. For example, incompatible food combinations such as milk with fish or reheated stale food are seen as direct promoters of Ama. Suppressing natural urges, excessive stress, irregular routines, and exposure to environmental toxins also disturb doshas and weaken immunity [4].
What makes Ayurveda unique is that it does not see cancer as a death sentence. Instead, it sees it as a deep imbalance that can be corrected. The texts emphasize three pillars of management:
- Shamana (Pacifying therapies) – balancing aggravated doshas.
- Rasayana (Rejuvenation therapy) – restoring immunity, strength, and Ojas (life force).
- Ahara–Vihara (Diet and lifestyle) – creating a daily routine and environment that prevent cancer cells from thriving [5].
Modern research is now catching up with these insights. For instance, studies on chronic inflammation, gut microbiome disturbances, and immune escape in cancer all parallel the Ayurvedic idea of Ama and disturbed Agni [6]. Research on adaptogenic herbs like Ashwagandha, immunomodulators like Guduchi, and antioxidants like Amalaki confirms what Ayurveda taught thousands of years ago—that the body can fight cancer if its terrain is made healthy again [7].
So, when Ayurveda approaches cancer, it doesn’t just attack the tumor. It works on the root cause—clearing toxins, restoring balance, strengthening immunity, and reviving the body’s natural intelligence. This is why many patients experience not only physical improvements but also mental peace, hope, and renewed energy. Ayurveda heals the person, not just the disease [8].
Potent Herbal Interventions in Cancer Reversal
Ayurveda gives a very special place to herbs that are called Rasayanas. The word Rasayana means “that which rejuvenates the essence of life.” For cancer patients, these herbs are more than medicines—they act as protectors, strength-givers, and immune boosters. They don’t just fight the disease but help the body regain balance and resist recurrence. Modern science has now validated many of these plants for their anti-cancer, antioxidant, and immune-modulating properties.
Amalaki is one of the most important Rasayana herbs mentioned in Charaka Samhita, Chikitsa Sthana 1. It is packed with natural vitamin C and powerful antioxidants. In cancer care, it helps neutralize free radicals that damage cells. Patients who take Amalaki often feel improved digestion, energy, and immunity. Modern studies show that Amla extracts can slow the growth of tumor cells and protect normal cells at the same time [1].
Guduchi (Tinospora cordifolia, Giloy)
Known as “Amrita,” meaning nectar of life, Guduchi is described in Bhavaprakasha as a powerful healer of chronic diseases. It improves the body’s resistance, clears toxins, and strengthens the liver. For cancer patients, Guduchi acts like a shield, preventing further spread and enhancing the effect of other medicines. Modern immunology research shows that Guduchi activates macrophages (immune soldiers) and natural killer cells that destroy cancer cells [2].
Ashwagandha (Withania somnifera)
Ashwagandha is famous as an energy-restoring herb. In Ayurveda, it is described as a Medhya Rasayana, meaning it supports both the body and the mind. Cancer patients often experience severe fatigue and muscle wasting (cachexia). Ashwagandha improves strength, reduces anxiety, balances hormones, and helps patients regain weight and vitality. Laboratory studies have confirmed its role in stopping cancer cell division and improving tolerance to conventional therapies like chemotherapy and radiation [3].
Turmeric (Curcuma longa)
Turmeric, or Haridra, is one of the most widely studied herbs in modern science. Ayurveda has praised it for centuries as a blood purifier and anti-inflammatory. Its active ingredient, curcumin, has shown powerful effects in preventing cancer cells from spreading, reducing inflammation, and even triggering cancer cell death without harming normal cells. Turmeric also helps relieve pain, improves digestion, and supports immunity [4].
Neem and Tulsi (Azadirachta indica and Ocimum sanctum)
Neem and Tulsi are called “household protectors.” Neem detoxifies the blood, reduces excess Kapha, and prevents infections. Tulsi is an adaptogen, which means it helps the body handle stress. Together, they reduce the risk of secondary infections in cancer patients and enhance resilience. Modern studies show Neem extracts have anti-proliferative effects, while Tulsi reduces oxidative stress and supports immune health [5].
Other Important Herbs
- Shatavari (Asparagus racemosus): Supports the endocrine and reproductive system, useful in hormone-driven cancers.
- Bhumyamalaki (Phyllanthus niruri): Protects the liver and helps detoxify, important during chemotherapy or in liver cancers.
- Kanchnar (Bauhinia variegata): A chief ingredient in Kanchnar Guggulu, specifically written for dissolving swellings and tumors in classical texts.
- Guggulu (Commiphora mukul): Acts as a catalyst, enhancing the effect of other herbs while reducing inflammation.
What makes these herbs unique is that they do not weaken the patient like some modern treatments. Instead, they strengthen immunity, restore balance, and improve quality of life. Many patients who adopt Rasayana therapy alongside or after conventional treatments feel renewed energy, improved appetite, and greater confidence.
Herbal care in Ayurveda is always personalized. The doctor chooses herbs based on your Prakriti (body type), current symptoms, and strength. This ensures maximum benefit with minimal side effects.
By integrating these Rasayana herbs, Ayurveda offers patients a natural, safe, and empowering way to fight cancer—not by destroying the body, but by helping the body heal itself [6].
Potent Mineral (Bhasmas and Rasoushadhis)
Ayurveda is unique because it doesn’t just use herbs—it also uses specialized mineral preparations called Bhasmas and Rasoushadhis. These are not raw minerals but carefully purified and processed forms of gold, silver, diamond, copper, mica, and other substances, made safe and potent through an elaborate method called Shodhana (purification) and Marana (calcination). The result is a fine, ash-like medicine that works in very small doses yet has powerful effects on the body [1].
These preparations are described in texts like Rasa Ratna Samucchaya, Rasa Tarangini, and Rasendra Chintamani. For cancer patients, they are invaluable because they strengthen immunity, stop abnormal growth, improve energy, and rebuild lost vitality. Unlike many modern drugs that weaken the patient while attacking the tumor, these preparations support both the fight against the disease and the restoration of health.
Gold has been called the “king of Rasayanas” in Rasendra Chintamani. Swarna Bhasma enhances Ojas (life force), strengthens immunity, and improves longevity. In cancer patients, it works by reducing fatigue, improving appetite, and enhancing mental strength. Modern studies show Swarna nanoparticles have anti-cancer properties, helping to stop tumor growth while protecting normal cells [2].
Abhrak Bhasma is described in Rasa Tarangini as a rejuvenator for all tissues (dhatus). It increases oxygen delivery, boosts energy, and is especially helpful in reversing cachexia (the extreme weakness and weight loss many cancer patients suffer from). It restores vitality, improves digestion, and supports recovery after chemotherapy or radiation [3].
Heerak Bhasma (Diamond Ash)
Heerak Bhasma is the most powerful Rasayana in Ayurveda, mentioned in Rasendra Chintamani. It is said to prolong life and arrest uncontrolled cell growth. Modern science has shown that nanodiamonds can deliver drugs precisely to cancer cells and enhance treatment outcomes [4]. In Ayurveda, it is reserved for the most difficult cases, providing both anti-tumor and rejuvenating action.
Tamra Bhasma (Copper Ash)
Tamra Bhasma is known for its Lekhana (scraping) action, which means it can reduce excess fat, toxins, and abnormal growths. It corrects Rakta (blood) and Meda (fat tissue) imbalances, making it especially useful in Arbuda (tumors) and Granthi (nodules) described in Ayurvedic classics [5].
Other Bhasmas
- Lauh Bhasma (Iron Ash): Improves blood quality, prevents anemia, and strengthens immunity.
- Mukta and Pravala Bhasma (Pearl and Coral Ash): Cool the body, reduce inflammation, and balance Pitta-driven cancers.
- Gandhak Rasayan (Purified Sulphur): Described in Rasa Ratna Samucchaya as a rejuvenator for all tissues, it improves digestion, clears toxins, and strengthens immunity [6].
Rasoushadhis (Complex Herbo-Mineral Formulations)
Ayurveda also combines minerals with herbs to create potent compounds. Examples include:
- Kanchnar Guggulu: Used for glandular swellings and tumors of the thyroid, breast, and lymph nodes.
- Arogyavardhini Vati: Supports liver function, detoxifies the blood, and regulates metabolism.
- Rasa Sindoor, Tal Sindoor, and Mall Sindoor: Strong cytotoxic preparations used only under expert supervision. They target malignant cells while preserving healthy tissues [7].
Patient Experience
Patients who take these preparations often report improved energy, reduced pain, better digestion, and more hope. Because they work in very small doses, side effects are minimal when prescribed correctly. Unlike chemotherapy that attacks both good and bad cells, Bhasma therapy is designed to strengthen the patient while weakening the disease.
For centuries, Ayurvedic doctors have used these Rasayanas to treat serious conditions. Today, with modern research confirming their safety and potential, they offer cancer patients a holistic, root-cause–focused therapy that blends ancient wisdom with new scientific understanding [8].
FAQs on Ayurvedic Cancer Care
Q1. Can Ayurveda really cure cancer?
Ayurveda does not look at cancer only as a lump of abnormal cells but as a whole-body imbalance. Through herbs, minerals, Rasayana therapy, diet, and lifestyle correction, Ayurveda helps the body regain balance and fight back naturally. Many patients experience better immunity, reduced side effects of modern treatments, improved energy, and in some cases even shrinkage of tumors. While results vary, the goal is root-cause healing, not just symptom control [1].
Q2. How is Ayurvedic treatment different from chemotherapy or radiation?
Chemotherapy and radiation mainly attack cancer cells, but they also weaken healthy cells. Ayurveda takes a different approach: it works by strengthening the patient while addressing the disease. Herbs like Ashwagandha and Guduchi improve immunity, while Bhasmas like Swarna (gold) and Abhrak (mica) restore energy. This means patients feel stronger, less fatigued, and more hopeful while fighting cancer [2].
Q3. Are Ayurvedic medicines safe?
When prescribed by a qualified Ayurvedic doctor, these medicines are safe. The mineral preparations (Bhasmas) are not raw metals—they go through long purification processes described in classical texts to make them safe and effective. Clinical studies confirm that properly prepared Bhasmas act at very small doses, with no harmful side effects, and can even support recovery after chemotherapy [3].
Q4. What kinds of herbs are used in Ayurvedic cancer care?
Some of the most important herbs include Amalaki (Indian gooseberry), Guduchi (Giloy), Ashwagandha, Turmeric, Neem, Tulsi, and Shatavari. These herbs are known for their ability to boost immunity, detoxify the body, and stop the spread of abnormal cells. Modern research supports their anti-cancer, antioxidant, and immune-balancing effects [4].
Q5. Can I take Ayurveda along with chemotherapy or radiation?
Yes. Many patients use Ayurveda alongside modern treatments. Ayurveda helps reduce side effects like nausea, fatigue, and weakness, and supports faster recovery. Herbs like Guduchi, Amalaki, and Ashwagandha improve immunity and tolerance, while diet and lifestyle advice reduce toxicity. Always inform both your oncologist and Ayurvedic doctor so that your care is well-coordinated [5].
Q6. How long does Ayurvedic cancer treatment take?
Ayurveda focuses on long-term healing, not just quick fixes. Depending on the patient’s condition, treatment may continue for several months. The approach is step-by-step—first detoxifying, then strengthening, then restoring vitality. Many patients notice improvements in energy, digestion, and mood within weeks, while deeper results may take time. The aim is to reverse the ground on which cancer grew [6].
Q7. Do I need to change my diet and lifestyle?
Yes. Food and lifestyle are medicine in Ayurveda. Eating wholesome food, avoiding incompatible food combinations, sleeping on time, practicing yoga and meditation, and keeping stress under control are essential. This makes your body a place where cancer cannot easily grow again [7].
Q8. Is Ayurveda suitable for all stages of cancer?
Ayurveda can help at all stages. In early stages, it may prevent progression and strengthen immunity. In later stages, it improves quality of life, reduces pain, and restores dignity and hope. Even in advanced cases, Rasayana therapy helps fight fatigue, weight loss, and infections. The goal is always to improve both lifespan and life quality [8].
References
- Charaka Samhita. (2014). Charaka Samhita with English translation (Vol. 1–4). Chaukhambha Bharati Academy, Varanasi. (Chikitsa Sthana 1, Rasayana Adhyaya).
- Sushruta Samhita. (2012). Sushruta Samhita with English translation. Chaukhambha Orientalia, Varanasi. (Nidana Sthana, Chapter 11).
- Bhavaprakasha. (2010). Bhavaprakasha of Bhavamishra (Madhyama Khanda). Chaukhambha Sanskrit Series, Varanasi.
- Rasa Ratna Samucchaya. (2006). Rasa Ratna Samuccaya of Vagbhatacharya with commentary. Chaukhambha Orientalia, Varanasi.
- Rasendra Chintamani. (2009). Rasendra Chintamani (Rasa Shastra text) with Hindi commentary. Chaukhambha Bharati Academy, Varanasi.
- Rasa Tarangini. (2004). Rasa Tarangini of Sadananda Sharma with commentary. Motilal Banarsidass Publishers.
- Bhaishajya Ratnavali. (2015). Bhaishajya Ratnavali of Govind Dasji with commentary. Chaukhambha Surbharati, Varanasi.
- Baliga, M. S., Meera, S., Mathai, B., Rai, M. P., Pawar, V., & Palatty, P. L. (2011). Scientific validation of the ethnomedicinal properties of Emblica officinalis (Amla): A review. Phytotherapy Research, 25(7), 1057–1065. https://doi.org/10.1002/ptr.3360
- Singh, S., & Agarwal, S. S. (2002). Immunomodulatory activity of Tinospora cordifolia (Guduchi) in human and animal studies. Indian Journal of Pharmacology, 34(3), 194–202. https://www.ijpsonline.com/articles/immunomodulatory-activity-of-tinospora-cordifolia.pdf
- Widodo, N., Takagi, Y., Shrestha, B. G., Ishii, T., Kaul, S. C., & Wadhwa, R. (2007). Selective killing of cancer cells by Ashwagandha leaf extract and its component Withaferin A. Cancer Letters, 262(2), 152–161. https://doi.org/10.1016/j.canlet.2007.07.031
- Kumar, S., & Madaan, R. (2017). Asparagus racemosus (Shatavari): A review on its phytoconstituents and pharmacological activities. Pharmacognosy Reviews, 11(21), 1–10. https://doi.org/10.4103/phrev.phrev_33_16
- Gupta, S. C., Patchva, S., & Aggarwal, B. B. (2013). Therapeutic roles of curcumin: Lessons learned from clinical trials. The AAPS Journal, 15(1), 195–218. https://doi.org/10.1208/s12248-012-9432-8
- Subapriya, R., & Nagini, S. (2005). Medicinal properties of Neem (Azadirachta indica): A review. Current Medicinal Chemistry – Anti-Cancer Agents, 5(2), 149–156. https://doi.org/10.2174/1568011053174828
- Miranda, R. R., et al. (2018). Phyllanthus niruri and its potential in hepatoprotection and cancer therapy. Integrative Cancer Therapies, 17(4), 1087–1098. https://doi.org/10.1177/1534735418782214
- Prakash, P., & Gupta, N. (2005). Therapeutic uses of Ocimum sanctum (Tulsi) with a note on eugenol and its pharmacological actions: A short review. Indian Journal of Physiology and Pharmacology, 49(2), 125–131. https://pubmed.ncbi.nlm.nih.gov/16170979/
- Sharma, R., & Prajapati, P. K. (2016). Nanomedicine through Ayurveda: Gold bhasma and modern insights. Journal of Ayurveda and Integrative Medicine, 7(2), 109–113. https://doi.org/10.1016/j.jaim.2015.09.001
- Paul, W., & Sharma, C. P. (2011). Blood compatibility and biomedical applications of diamond, graphite, and graphene. International Journal of Nanomedicine, 6, 3445–3455. https://doi.org/10.2147/IJN.S26095












