- Anatomy and Physiology of the Testis
- Classification of Testicular Tumors
- Risk Factors and Etiology
- Pathophysiology
- Clinical Presentation(Symptoms)
- Diagnostic Evaluation
- Staging
- Treatment in Allopathy
- Management by Tumor Type
- Special Scenarios
- Fertility, Sexual Health, and Hormonal Care
- Complications and Late Effects
- How Ayurveda Cures
- Powerful Medicine -Kanchanara-Vrishya-Rasayana Avaleha
- FAQs
- Reference (Modern + Ayurvedic)
Testicular cancer is one of the most curable forms of cancer when detected early, yet many men delay seeking help due to fear, embarrassment, or lack of awareness [2]. It most often affects young adults between the ages of fifteen and forty five and usually begins as a small painless swelling or a noticeable change in one testis [1]. Early signs are subtle, which is why the disease may progress silently until the mass grows larger or causes sudden discomfort [3].
Modern diagnostic methods such as scrotal ultrasound, tumor marker testing, and advanced imaging have made early detection highly reliable [7]. With correct staging and timely treatment using surgery and medical therapy, long term survival rates are excellent [4]. At the same time many patients worry about fertility, hormone levels, sexual function, and long term recovery. These concerns are completely valid and require a compassionate approach that supports both physical and emotional healing [6].
Ayurveda provides an additional perspective through its detailed understanding of Shukra Dhatu imbalance, obstruction of the reproductive channels, and abnormal tissue growth described under Arbuda [11]. Classical texts explain how disturbances in tissue nourishment, metabolic fire, and Kapha and Vata interactions can create firm deep seated masses in the testis [12]. Ayurvedic Rasayana therapy and Vrishya formulations aim to restore the strength of the reproductive tissues, support immunity, stabilize hormones, reduce fatigue, and improve overall vitality during and after cancer treatment [21].
This article explains the symptoms of testicular cancer, the modern diagnostic process, and the complete Ayurvedic approach to healing so that every patient can understand the condition clearly and make informed decisions regarding their health [1][11].
Anatomy and Physiology of the Testis
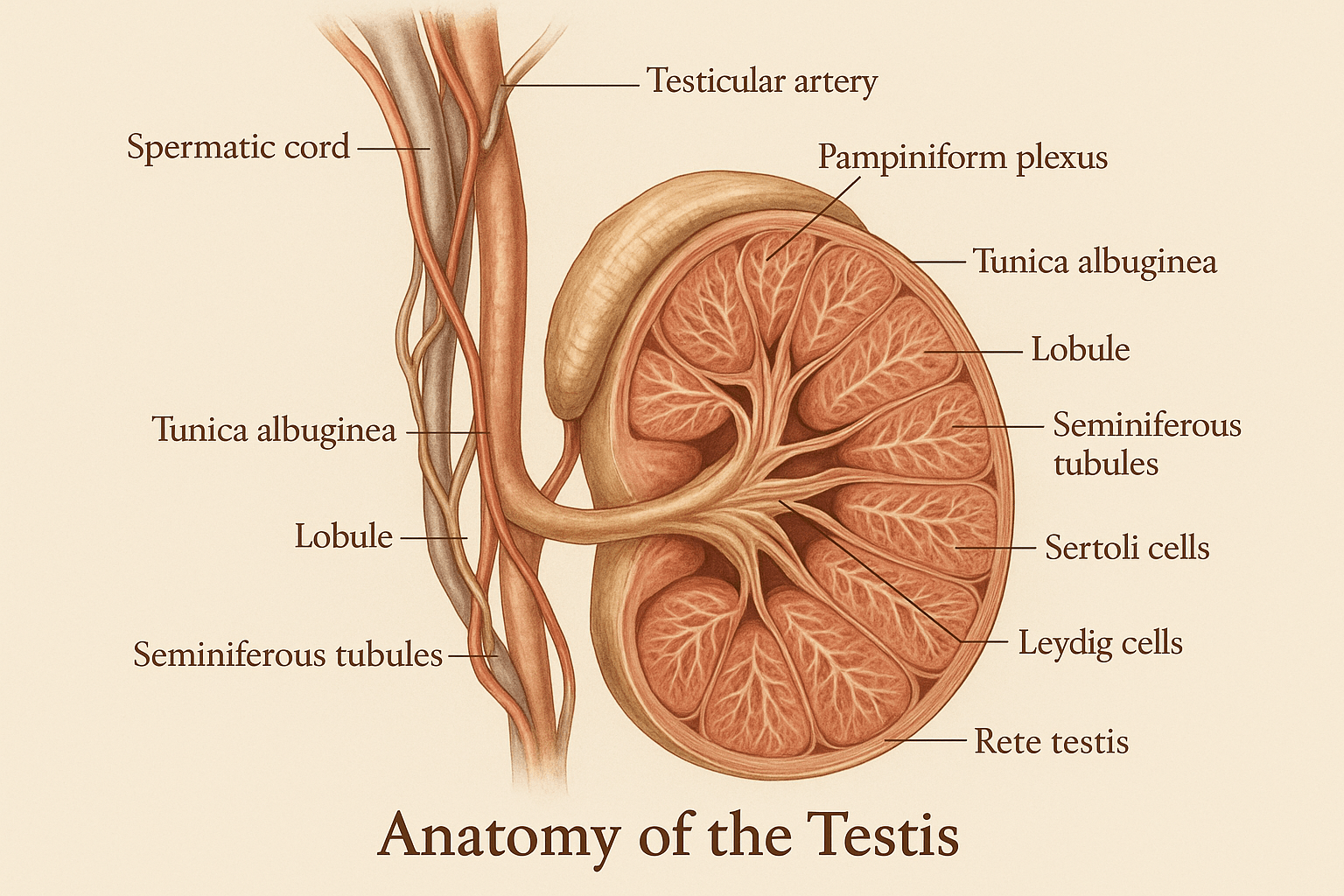
The testis is a highly specialized organ responsible for sperm production and male hormone secretion. Each testis is enclosed in a strong protective capsule known as the tunica albuginea, which forms internal partitions that divide the tissue into small lobules [7]. Inside these lobules lie the seminiferous tubules, long and coiled structures where sperm cells are made. These tubules are lined with Sertoli cells that support and nourish developing sperm, while the spaces between the tubules contain Leydig cells that produce testosterone [6]. Small channels called the rete testis collect immature sperm and move them toward the epididymis for maturation [7].
The normal function of the testis is guided by the hormonal connection between the brain and the reproductive organs, often referred to as the hypothalamus pituitary testis axis [4]. The hypothalamus releases signals that stimulate the pituitary gland, and the pituitary then releases hormones that act directly on the testis to support testosterone production and the formation of new sperm cells. This hormonal coordination ensures a continuous cycle of sperm development, known as spermatogenesis, which takes place within the seminiferous tubules [3].
The blood testis barrier plays an essential protective role by separating developing sperm cells from the bloodstream [6]. This barrier prevents harmful substances and immune reactions from damaging sperm forming inside the testis. Lymphatic vessels surrounding the testis drain into the para aortic lymph nodes located deep in the abdomen, and this pathway explains why testicular cancer often spreads to the back of the abdomen rather than to nearby groin nodes [8]. Understanding these anatomical and physiological features is important because disruptions in any of these structures can contribute to disease progression or influence how testicular cancer spreads.
Classification of Testicular Tumors
Testicular tumors are broadly divided into several groups based on the type of cells from which they arise. The most common group is known as germ cell tumors, which start from the cells responsible for sperm production. These tumors account for the majority of testicular cancers in young men and are further divided into two major categories. The first category is seminoma, which grows slowly and usually remains sensitive to treatment for a long time. The second category is non seminoma, a group that includes embryonal carcinoma, yolk sac tumor, choriocarcinoma, teratoma, and mixed tumors that contain more than one of these cell types [1][4].
Another important group of tumors is sex cord stromal tumors. These arise from the supporting and hormone producing cells of the testis. The most common types are Leydig cell tumor and Sertoli cell tumor. These tumors are usually less aggressive than germ cell tumors, but in rare cases they may behave in a malignant manner [6].
Secondary testicular tumors form when cancers from other parts of the body spread to the testis. These are uncommon but can occur with cancers such as lymphoma or leukemia [9]. A related but distinct condition is germ cell neoplasia in situ. This is a microscopic early stage where abnormal cells are present inside the seminiferous tubules but have not yet formed an invasive tumor. It is considered a direct precursor to many germ cell tumors [7].
This classification helps doctors determine the correct approach for diagnosis, staging, and treatment because each type of tumor behaves differently and responds differently to therapy.
Risk Factors and Etiology
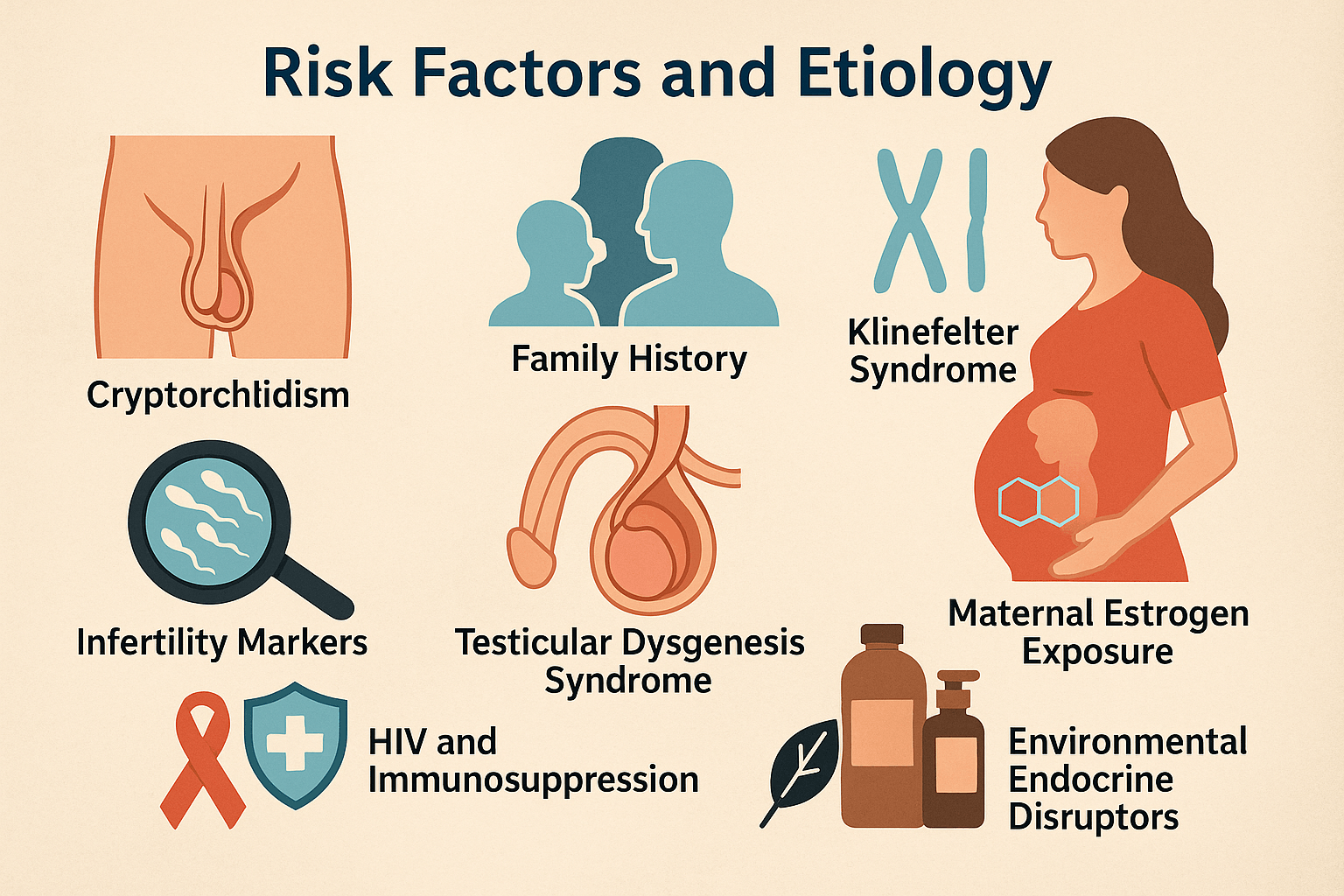
Several factors increase the likelihood of developing testicular cancer. One of the strongest known risks is a history of cryptorchidism, which refers to a testis that did not descend properly at birth. Even after surgical correction, the risk remains higher than normal because the testis may have been exposed to abnormal temperature or developmental conditions [2]. A family history of testicular cancer is another important factor. Men who have a father or brother with the disease face a higher chance of developing it themselves, suggesting a genetic influence [4].
Certain genetic conditions such as Klinefelter syndrome can also contribute to abnormal testicular development and increase the probability of tumor formation [7]. Infertility markers, such as a very low sperm count or abnormal semen parameters, are also associated with a higher risk. This link supports the idea that impaired testicular development and impaired sperm formation may share a common underlying cause [6].
A broader developmental condition known as testicular dysgenesis syndrome has been proposed to explain why multiple disorders such as low sperm count, undescended testis, and testicular cancer may occur together. This syndrome is thought to arise from disturbances in fetal development of the reproductive system [8]. Maternal exposure to high levels of estrogen or estrogen like substances during pregnancy may also increase risk by altering the hormonal environment during fetal development [9].
Risk is also higher in men with HIV infection or other forms of immune system suppression. A weakened immune system may be less effective at eliminating abnormal cells before they become cancerous [5]. Environmental endocrine disruptors, found in certain plastics, chemicals, and pesticides, may also interfere with hormone signaling and contribute to abnormal testicular growth, although research in this area is still ongoing [3].
Understanding these risk factors helps identify individuals who may benefit from closer observation and early evaluation if changes in the testis are noticed.
Pathophysiology
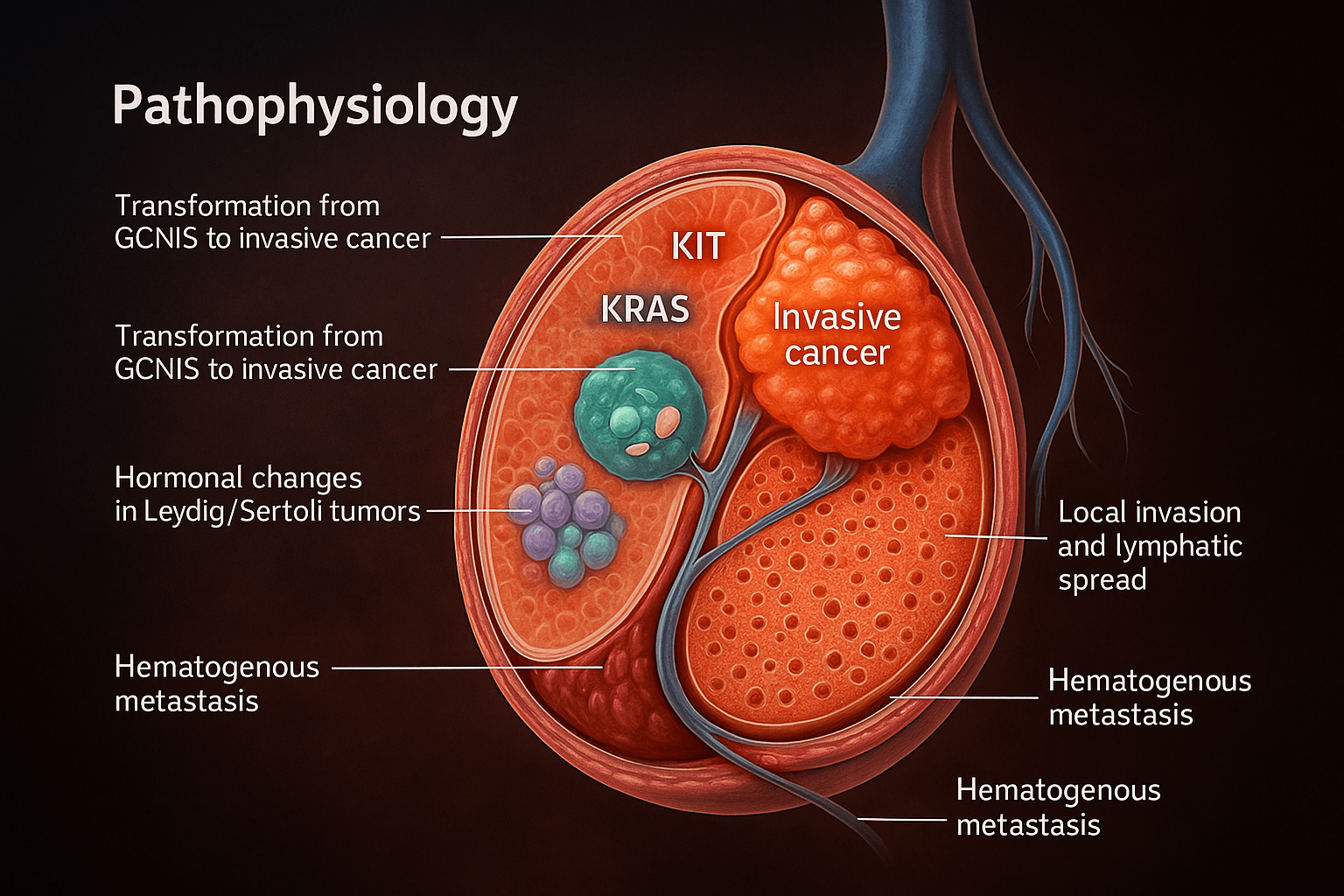
The development of testicular cancer begins with changes at the cellular and genetic level. Many germ cell tumors carry specific genetic alterations, such as mutations in KIT and KRAS, along with the presence of an extra copy of the short arm of chromosome twelve, known as i twelve p. These abnormalities alter normal cell signaling and promote uncontrolled growth of germ cells [4][6]. Most of these tumors arise from a precursor stage called germ cell neoplasia in situ. In this stage, abnormal cells remain confined within the seminiferous tubules but gradually acquire the ability to break through the basement membrane and form an invasive tumor [7].
Once the tumor becomes invasive, it begins to expand locally within the testis. Cancer cells can infiltrate nearby structures such as the rete testis and epididymis. The lymphatic channels of the testis provide a natural route for further spread. Because testicular lymphatic drainage travels upward to the para aortic lymph nodes, early metastasis often appears deep in the abdomen rather than in nearby groin nodes [8]. As the disease progresses, cancer cells may also enter the bloodstream. Through this pathway, tumors frequently spread to the lungs and occasionally to the liver or brain, leading to hematogenous metastasis [1].
Certain tumors that arise from Leydig cells or Sertoli cells behave differently because of their hormonal activity. These tumors can produce excess testosterone, estrogen, or other hormones, creating systemic changes such as gynecomastia or early puberty in younger patients. The hormonal imbalance reflects the abnormal activity of these specialized cells and contributes to the clinical presentation [5].
Understanding the pathophysiology of testicular cancer provides essential insight into how the disease originates, spreads, and produces symptoms. This knowledge guides decisions about staging, treatment, and long term monitoring.
Clinical Presentation(Symptoms)
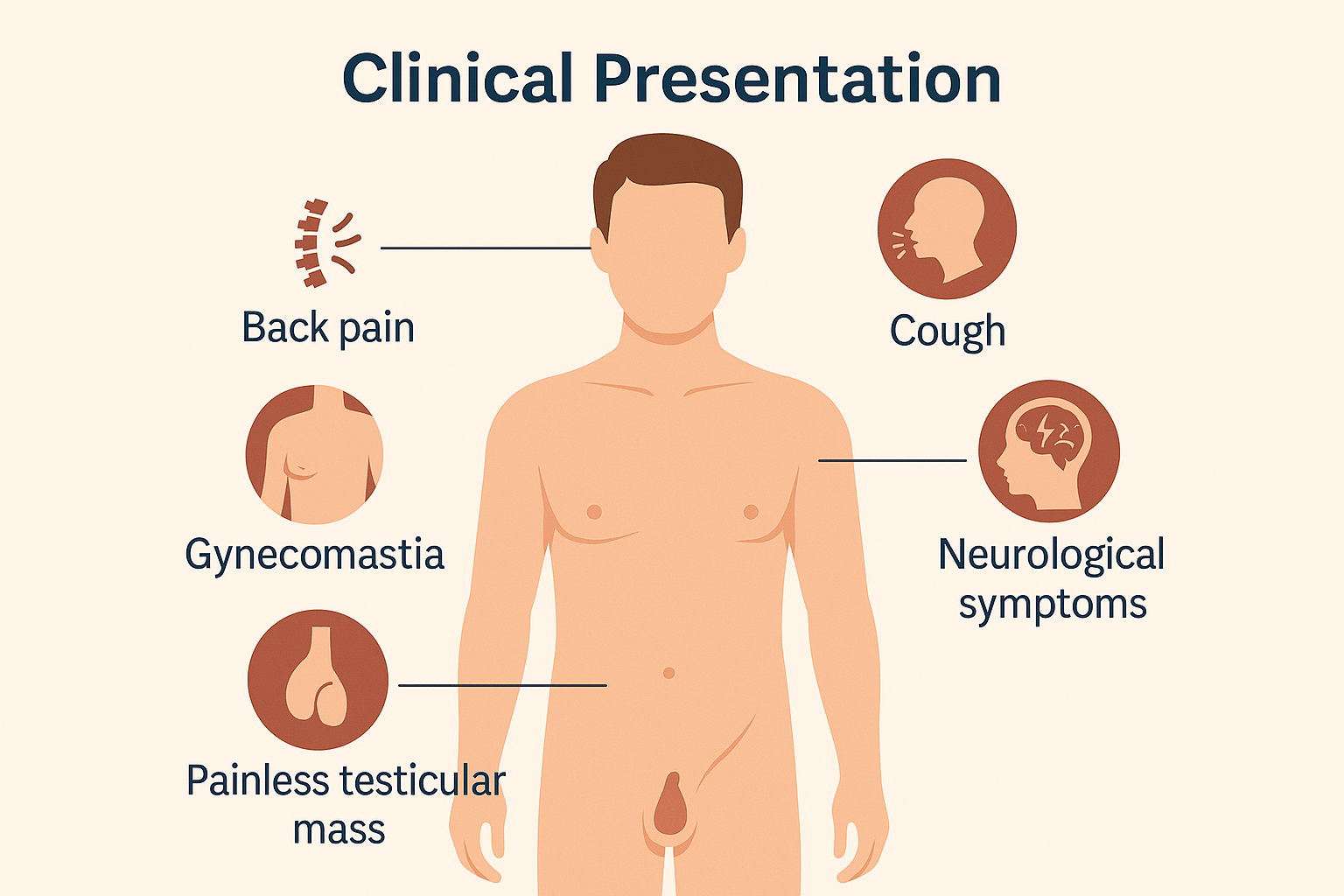
The most common early sign of testicular cancer is a painless testicular mass. Many patients notice a firm swelling or enlargement of one testis during bathing or while dressing, and because it does not hurt, it is often ignored for weeks or even months [2]. In some cases, sudden acute pain may occur if bleeding takes place inside the tumor. This internal hemorrhage stretches the tissues of the testis and creates sharp discomfort that brings the patient to medical attention [3].
Certain tumors can produce hormones and cause changes in the body. One of the best known examples is gynecomastia, a condition in which breast tissue becomes enlarged. This occurs when tumor cells produce hormones that alter the normal balance between testosterone and estrogen [5]. As the disease progresses, cancer cells can spread through the lymphatic channels into the back of the abdomen. When this happens, patients may experience back pain from enlarged retroperitoneal lymph nodes [1].
If cancer cells reach the bloodstream, they can travel to the lungs. This may cause cough or, in some cases, coughing up small amounts of blood. Lung involvement is one of the early patterns of distant spread in metastatic disease [4]. Very advanced disease can also affect the brain, leading to neurological symptoms such as headaches, confusion, or difficulty with movement. These symptoms appear in only a small number of cases but indicate widespread progression [6].
Several other conditions can mimic the symptoms of testicular cancer, so a careful evaluation is important. Testicular torsion can cause sudden severe pain, orchitis can cause swelling and inflammation, and hydrocele can lead to fluid accumulation around the testis. Although these conditions are unrelated to cancer, they can present with similar findings on physical examination [7].
Diagnostic Evaluation
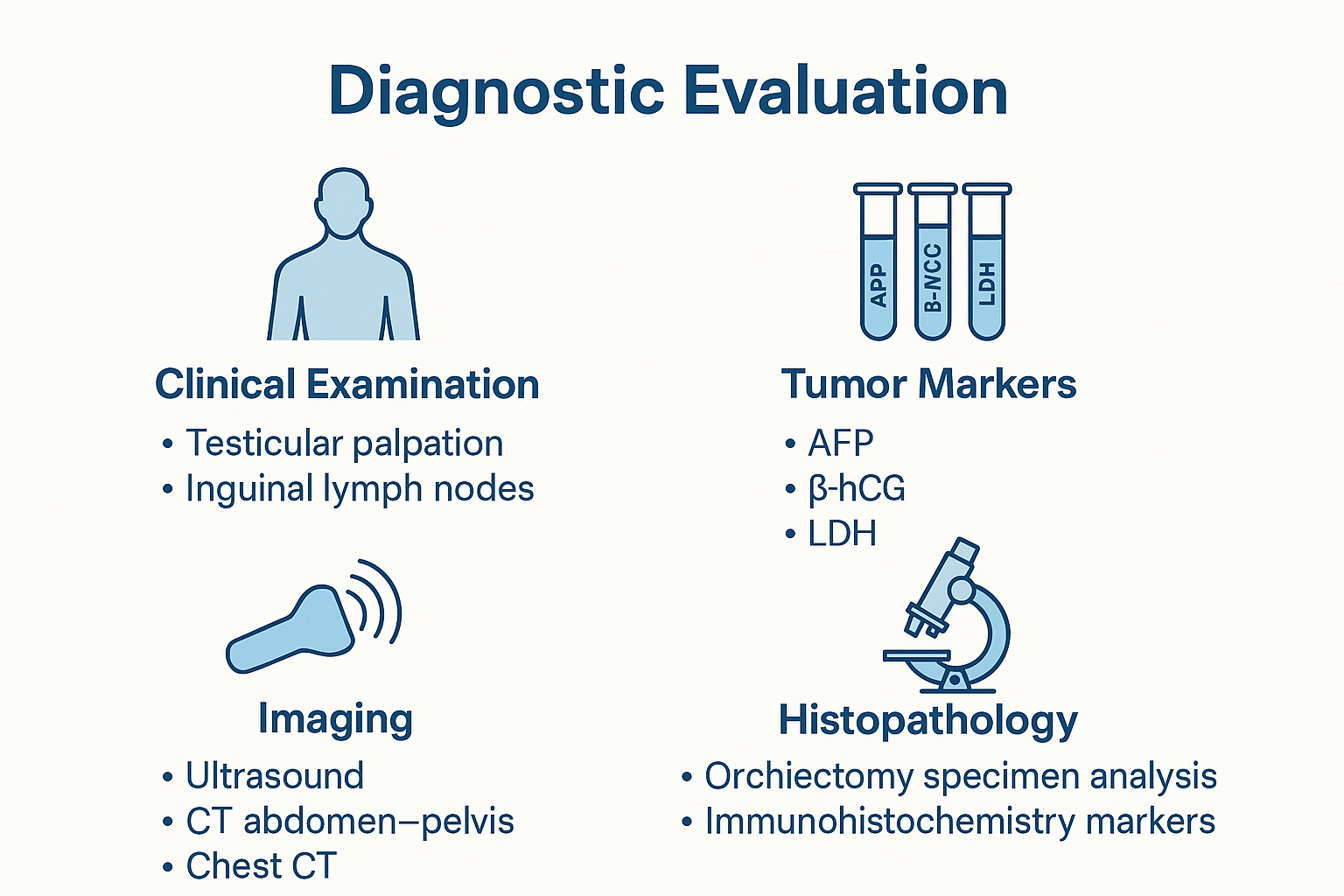
Accurate diagnosis of testicular cancer depends on a structured clinical and laboratory approach. The first step is a detailed clinical examination in which the doctor gently palpates each testis to assess its size, texture, and the presence of any firm or irregular area [2]. A painless hard swelling is considered suspicious and requires further evaluation. The inguinal lymph nodes are also examined because they may enlarge in certain conditions, although the testis usually drains into the para aortic lymph nodes. During examination, the doctor also distinguishes benign conditions such as hydrocele or epididymal cysts from malignant tumors based on the feel and location of the swelling [6].
Tumor marker testing plays an important role in both diagnosis and staging. The three major markers used are alpha fetoprotein also called AFP, beta human chorionic gonadotropin also called beta hCG, and lactate dehydrogenase or LDH [1]. These markers can be elevated in many non seminomatous tumors, while pure seminoma often has normal AFP with possible mild elevation of beta hCG. The pattern of marker elevation helps guide the diagnosis and indicates the burden of disease [4].
Imaging studies offer further detail. Scrotal ultrasound is usually the first imaging test and can clearly show whether a mass is solid, cystic, or mixed, which helps determine its nature [7]. CT scans of the abdomen and pelvis are performed to evaluate lymph node enlargement and spread of disease. A chest CT is used to check for lung involvement, which is one of the most common sites of distant metastasis. MRI is reserved for situations where ultrasound findings are uncertain or when local extension needs clearer definition. PET CT may be used in selected cases of seminoma, especially when residual masses need to be assessed after treatment [3].
Final confirmation of diagnosis is obtained through histopathology after an inguinal orchiectomy. The removed tissue is examined under a microscope to determine the exact type of tumor, its patterns of growth, and the presence of lymphatic or vascular invasion [5]. Immunohistochemistry testing may be used to identify specific markers that help classify the tumor. In many cases, more than one tumor type may be present, so recognizing mixed tumors is important because it influences treatment planning [8].
This systematic approach helps ensure early and accurate diagnosis, proper staging, and the choice of the most effective treatment strategy.
Staging
Staging helps determine how far testicular cancer has progressed and guides the choice of treatment. The AJCC TNM system is the most widely used method. The T category describes the extent of the primary tumor inside the testis. Early tumors may be limited to the testis itself, while more advanced tumors may invade the epididymis, the tunica albuginea, or the spermatic cord [1]. The N category reflects whether cancer has spread to regional lymph nodes. Because the testis drains into the para aortic nodes, enlargement in this area is an important indicator of progression [4]. The M category indicates the presence of distant spread, most commonly to the lungs, liver, or brain [6].
In addition to TNM staging, testicular cancer includes a separate component known as the S stage. This stage is based on serum tumor markers such as AFP, beta hCG, and LDH measured after the testis has been removed [2]. The level of these markers provides essential information about the burden of disease and helps distinguish between good, intermediate, and poor prognosis groups.
Based on the TNM and S stage together, testicular cancer is grouped clinically into stage one, stage two, and stage three. Stage one disease is confined to the testis. Stage two disease involves retroperitoneal lymph nodes. Stage three disease shows distant metastasis or very high tumor marker levels [3]. These clinical stages help doctors plan treatment and follow up.
The IGCCCG prognostic classification further refines staging for metastatic germ cell tumors. This system divides patients into good, intermediate, and poor prognosis categories based on tumor marker levels, primary tumor type, and the pattern of metastasis [5]. The IGCCCG classification has been one of the strongest predictors of treatment success and long term outcomes.
Accurate staging ensures that every patient receives the most appropriate therapy and helps predict survival and recovery rates with high precision.
Treatment in Allopathy
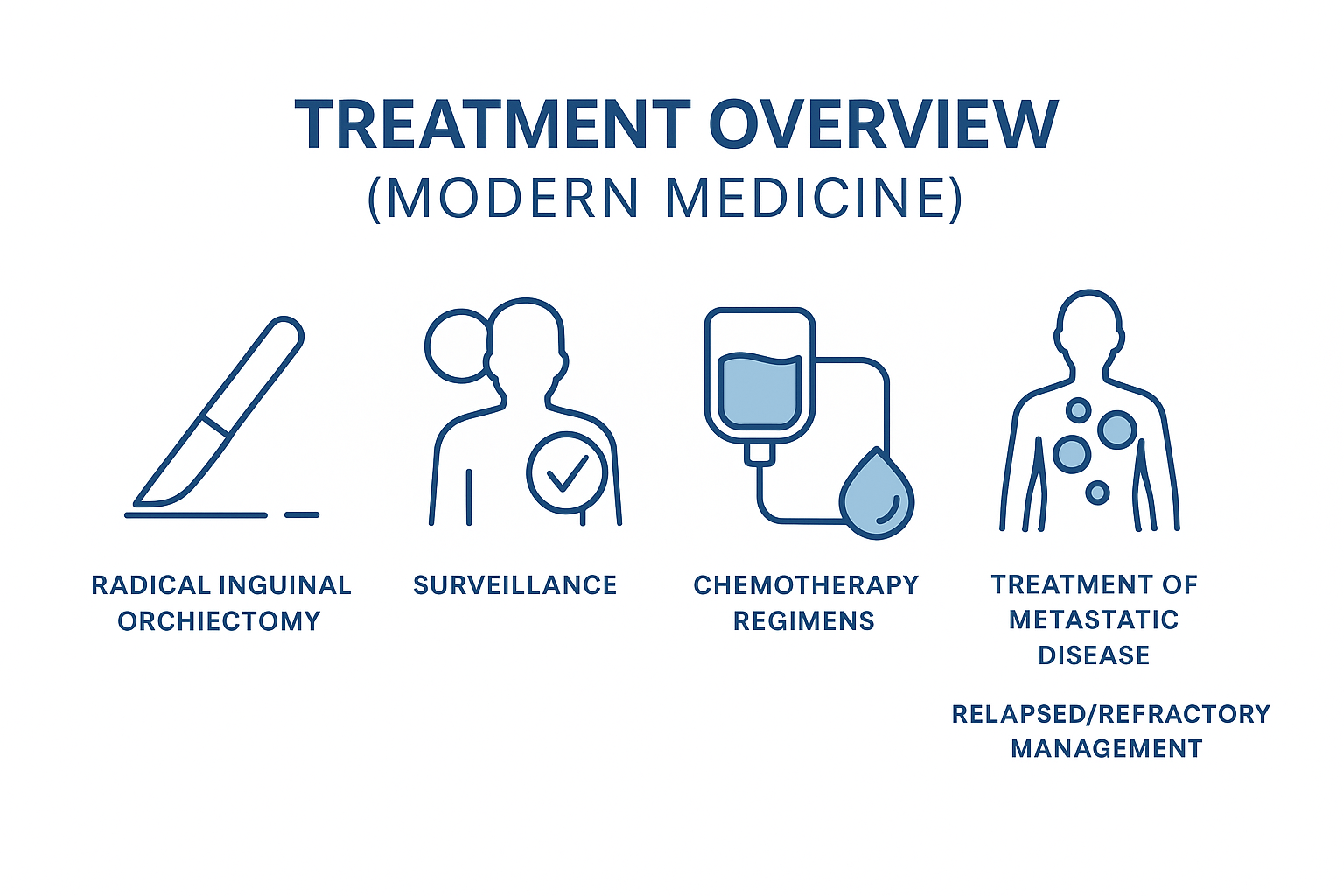
Modern treatment of testicular cancer is one of the most successful achievements in oncology. The first and most essential step in management is radical inguinal orchiectomy. In this procedure, the testis is removed through an incision in the groin. This technique prevents cancer cells from spreading into the scrotal tissues and provides a complete specimen for diagnosis [1]. Once the tumor is removed, further treatment decisions depend on the stage, tumor type, and tumor marker levels.
Many patients with early stage disease are eligible for surveillance. This approach involves regular clinical examinations, tumor marker testing, and imaging at defined intervals. Surveillance avoids overtreatment and is safe when patients follow the schedule strictly [4]. For those who require additional therapy, chemotherapy is the cornerstone of treatment. The most commonly used combinations are BEP and EP, which include drugs such as bleomycin, etoposide, and cisplatin [2]. These regimens are highly effective and have dramatically improved survival rates even in advanced disease.
Retroperitoneal lymph node dissection, abbreviated as RPLND, plays a role in selected patients with non seminomatous tumors. It is used both for staging and for treating residual disease after chemotherapy [3]. Radiotherapy is another option used almost exclusively for seminoma because seminoma cells are highly sensitive to radiation. It is typically offered for stage two disease that involves para aortic lymph nodes [6].
Management of metastatic disease requires a combination of systemic chemotherapy and careful monitoring of tumor marker decline. Most patients respond well, and long term cure is achievable even in cases with lung or abdominal metastasis [5]. Relapsed or refractory disease requires specialized treatment strategies. These may include high dose chemotherapy, stem cell rescue, or targeted surgical removal of resistant tumor deposits.
Modern treatment approaches continue to evolve, but the core principles remain consistent. Early removal of the testis, accurate staging, marker guided decisions, and timely chemotherapy form the foundation of successful management.
Management by Tumor Type
The treatment of testicular cancer varies according to the specific tumor type because each category behaves differently, spreads differently, and responds to therapy in its own way. Understanding these distinctions helps create a treatment plan that is effective and tailored to the individual patient.
A. Seminoma
Seminoma is known for its predictable behavior and high sensitivity to both radiation and chemotherapy. Management is therefore stage dependent. Early stage seminoma is often treated with radical orchiectomy followed by surveillance in patients who can reliably attend follow up visits. Some may receive a short course of chemotherapy when risk factors are present [1]. In stage two disease, treatment usually involves chemotherapy or targeted radiotherapy to the para aortic region. Seminoma responds extremely well to these treatments [4].
When a residual mass remains after chemotherapy, a PET scan performed at the recommended interval helps determine whether active cancer cells are still present. A mass that remains inactive on PET scan is usually left alone, while a positive scan may require additional therapy [5]. This PET guided approach prevents unnecessary surgery and reduces long term treatment related effects.
B. Non Seminoma NSGCT
Non seminomatous germ cell tumors behave more aggressively and require a different strategy. In stage one disease, patients may choose between surveillance and retroperitoneal lymph node dissection known as RPLND [3]. Surveillance is safe for reliable patients, while RPLND provides both staging and treatment in those with a higher chance of microscopic spread.
In stage two and stage three disease, chemotherapy is the main treatment. Regimens such as BEP and EP have transformed outcomes, with cure rates remaining high even in advanced disease [2]. After chemotherapy, some patients may have a persistent mass. If tumor markers have normalized and the mass remains, surgical removal is recommended because these masses often contain teratoma, which does not respond to chemotherapy [6].
A unique concern in NSGCT is growing teratoma syndrome. In this condition, the tumor enlarges despite falling tumor markers. This happens because teratoma elements continue to grow while cancer cells respond to treatment. Surgery is the only effective management for growing teratoma syndrome because it does not shrink with chemotherapy [7].
C. Stromal Tumors
Stromal tumors arise from the supportive and hormone producing cells of the testis. Leydig cell tumors and Sertoli cell tumors are the most common examples. These tumors are typically managed with orchiectomy alone because most remain localized and behave in a benign manner [8]. A small percentage may behave aggressively, especially in adults. In such cases, long term monitoring is essential because there is no proven chemotherapy regimen that consistently works for malignant stromal tumors.
Hormonal disturbances caused by these tumors often improve after removal of the affected testis. Follow up includes regular clinical examination and imaging when needed to ensure that recurrence or delayed spread is detected early.
Special Scenarios
Some clinical situations in testicular cancer require a more individualized approach because the pattern of disease, response to treatment, or long term outlook may differ from typical cases. These special scenarios are important to recognize early so that management can be adjusted appropriately.
Bilateral tumors occur when cancer develops in both testes, either at the same time or years apart. Although uncommon, this situation requires careful planning to preserve hormonal function and fertility. Most patients are treated with staged orchiectomy, and hormone replacement is usually needed afterward. Fertility preservation becomes especially important in these cases [4].
Testicular cancer in patients with HIV also requires special consideration. With modern antiviral therapy, outcomes are generally comparable to those of HIV negative patients, but immune status must be monitored closely. Chemotherapy is still effective, although treatment related toxicity may be slightly higher when the immune system is weakened [6].
Pediatric testicular tumors behave differently from tumors in adults. Yolk sac tumor is the most common type in children, and it usually has an excellent prognosis when treated promptly with surgery and appropriate chemotherapy [5]. Hormonal tumors such as Leydig cell tumors may also appear in children and can cause early puberty.
Late relapse is a rare condition in which testicular cancer returns many years after initial treatment. These relapses often involve teratoma or slow growing tumor elements and may not respond well to chemotherapy. Surgery plays a key role in managing late relapse because complete removal of the recurrent mass is essential [7].
In advanced disease, cancer cells may spread to the brain, leading to neurological symptoms. Management typically requires systemic chemotherapy combined with focused radiation or surgical removal when appropriate [1]. Although brain involvement is uncommon, it indicates widespread disease and requires coordinated care between oncology and neurosurgical teams.
Another unique scenario is the presence of a mediastinal germ cell tumor in combination with testicular abnormalities. Some mediastinal tumors arise from germ cells that never migrated correctly during development. A careful testicular evaluation is important because some patients may have an underlying testicular precursor lesion such as germ cell neoplasia in situ [3].
Recognizing these special scenarios ensures that treatment is tailored to each patient’s specific needs and that long term care addresses the unique risks associated with these conditions.
Fertility, Sexual Health, and Hormonal Care
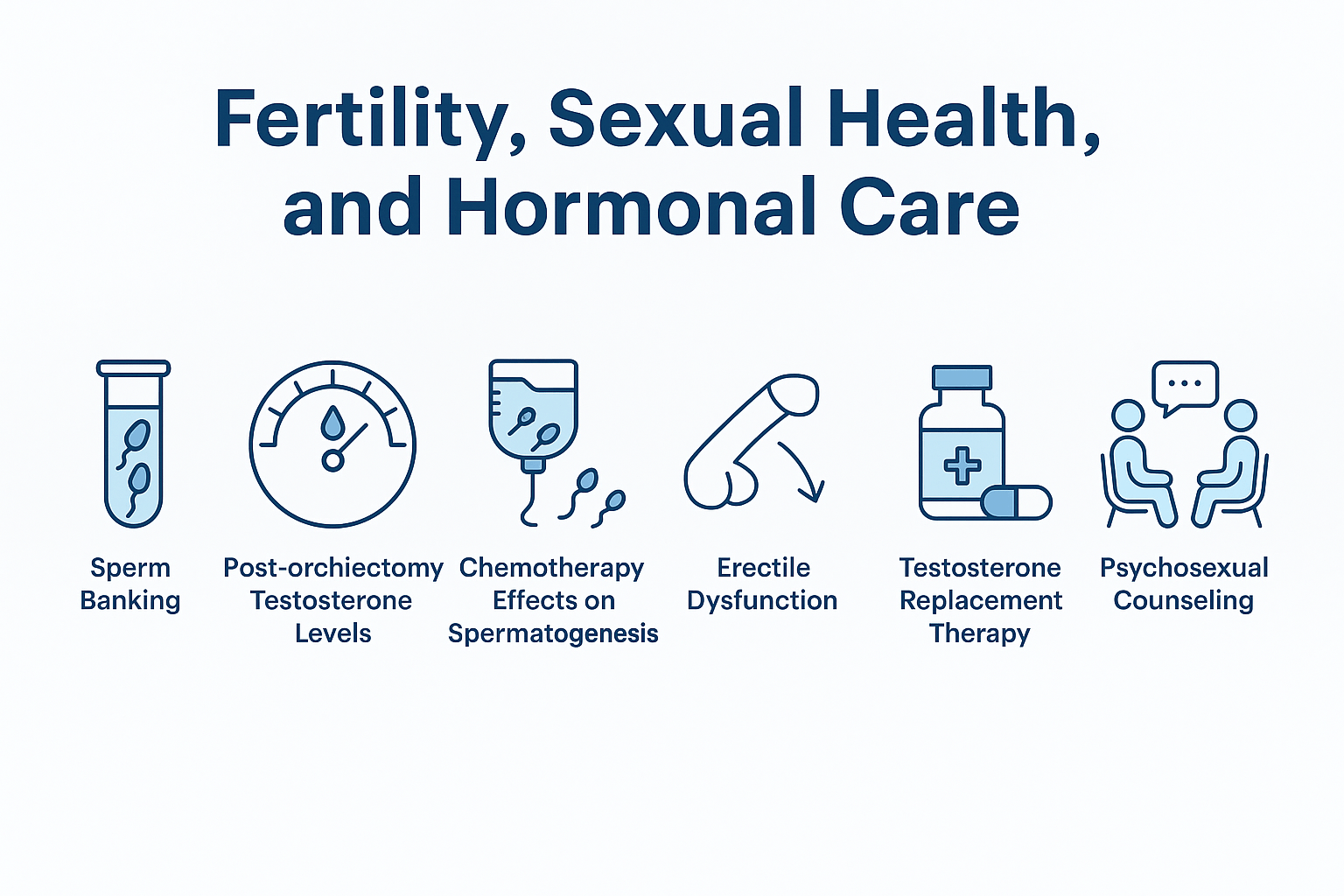
Fertility and hormonal balance are major concerns for many patients diagnosed with testicular cancer, especially because the disease often affects young men. One of the first steps recommended before treatment is sperm banking. This process allows patients to store healthy sperm for future use, particularly when chemotherapy or surgery may affect the ability to father a child later in life [4]. Even in early stage disease, fertility preservation is encouraged because spermatogenesis may already be impaired at the time of diagnosis.
Removal of one testis through orchiectomy usually does not cause major hormonal problems because the remaining testis can often maintain normal testosterone production. However, some patients experience a drop in testosterone levels, particularly if the remaining testis has reduced function [6]. Monitoring hormone levels is therefore important during follow up. Symptoms of low testosterone can include fatigue, low mood, reduced muscle mass, and decreased libido.
Chemotherapy can temporarily or permanently affect sperm production. Drugs such as cisplatin and etoposide may disrupt spermatogenesis for months or even years after treatment [2]. Although many patients regain fertility over time, recovery can vary widely. Because the ability to produce sperm may not return to normal immediately, sperm banking before chemotherapy remains one of the safest strategies.
Some patients experience erectile dysfunction during or after treatment. This may be due to stress, hormonal imbalance, chemotherapy related fatigue, or performance anxiety rather than direct nerve damage [5]. Addressing these concerns early through counseling and medical support can significantly improve quality of life. Erectile function often improves with reassurance, lifestyle support, and hormonal assessment when necessary.
For those who develop symptoms of testosterone deficiency, testosterone replacement therapy can be helpful. Replacement therapy improves energy, mood, sexual function, and metabolic health [1]. Treatment should be individualized and closely monitored to maintain stable hormone levels.
Psychosexual counseling is an essential part of recovery. A diagnosis of cancer can create anxiety about masculinity, body image, relationships, and fertility. Counseling provides emotional support, helps patients adjust to the physical changes from treatment, and strengthens sexual confidence [3]. Integrating psychological care with medical follow up ensures that patients heal not only physically but also emotionally.
Complications and Late Effects
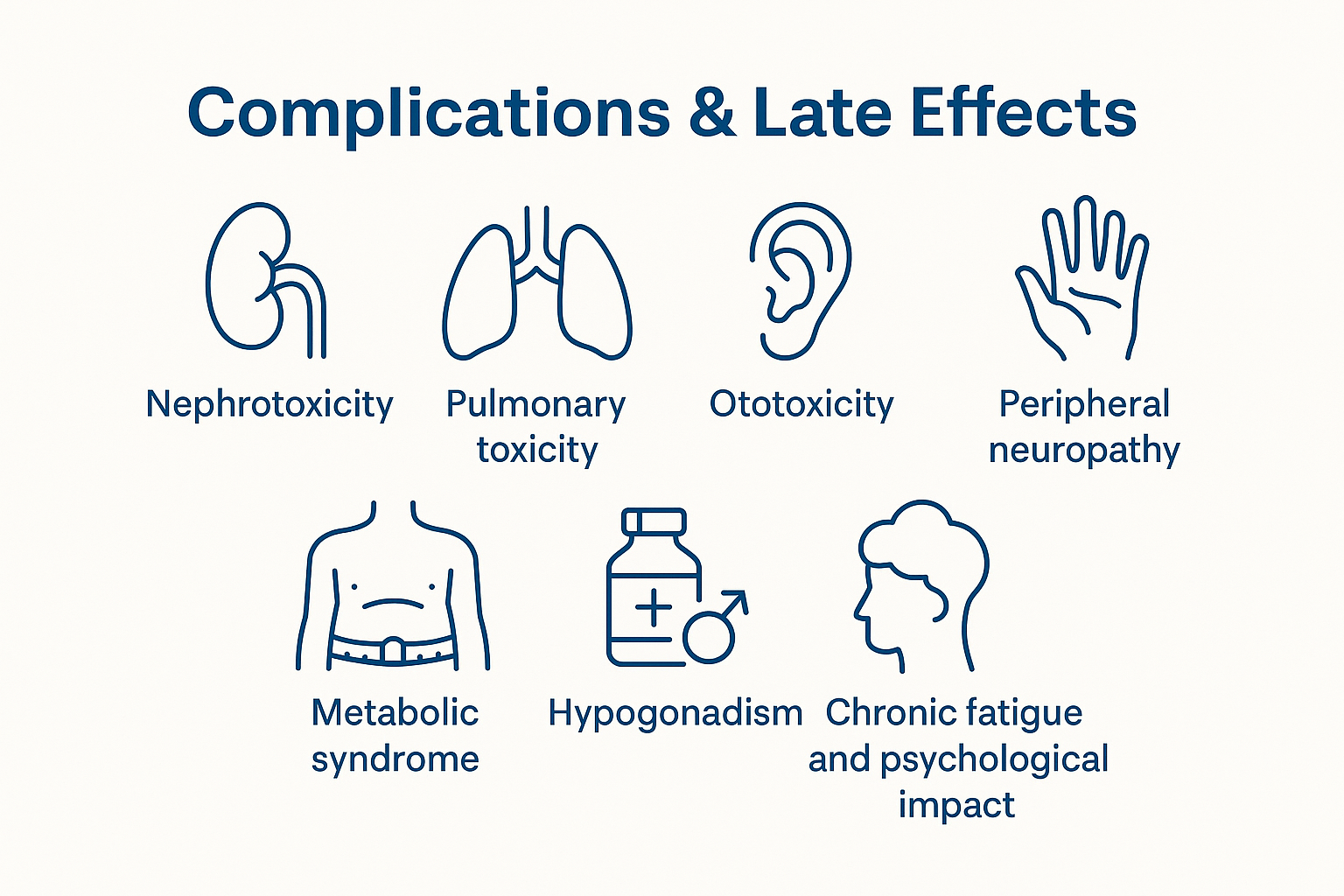
Modern treatment of testicular cancer achieves very high cure rates, but some patients experience long term effects because chemotherapy, radiation, and hormonal changes can influence different organs over time. Understanding these complications helps ensure proper follow up and early management.
Nephrotoxicity is one of the most recognized long term effects because cisplatin can damage the delicate structures of the kidney. This may lead to reduced filtration capacity, electrolyte abnormalities, or mild chronic kidney dysfunction. Regular monitoring of creatinine levels and hydration status helps reduce the impact of this complication [1].
Pulmonary toxicity occurs mainly with bleomycin. Some patients develop inflammation or scarring of the lungs that can cause shortness of breath, cough, or reduced exercise capacity. Severe reactions are rare, but careful evaluation of lung function is recommended before treatment and during follow up [4].
Ototoxicity is also associated with cisplatin. Patients may notice ringing in the ears or reduced ability to hear high frequency sounds. This effect can appear months or years after treatment. Audiology testing is useful in those who report hearing changes [3].
Peripheral neuropathy is another important late effect. Damage to peripheral nerves may cause numbness, tingling, or burning sensations in the hands and feet. These symptoms can persist long after treatment and may affect fine motor tasks. Supportive therapy and vitamin based interventions may help improve comfort [6].
Some survivors develop metabolic syndrome, which includes weight gain, increased blood pressure, insulin resistance, and abnormal cholesterol levels. Reduced physical activity after treatment and hormonal changes may contribute to this cluster of problems [5]. Lifestyle guidance and periodic blood tests help prevent long term cardiovascular strain.
Hypogonadism is relatively common after treatment. Some patients develop low testosterone due to reduced function in the remaining testis. Symptoms include reduced energy, decreased libido, mood changes, and loss of muscle strength. Hormone assessment during follow up is essential because testosterone replacement may significantly improve quality of life [2].
Chronic fatigue and psychological impact are also important late effects. Cancer diagnosis and treatment can lead to persistent tiredness, anxiety, and emotional stress. Survivors may struggle with concerns about recurrence, body image, fertility, and long term health. Psychological counseling, support groups, and structured rehabilitation can greatly improve recovery [7].
These late effects highlight the importance of long term follow up so that survivors receive ongoing support for physical and emotional health.
How Ayurveda Cures
A. Ayurvedic Understanding of Testicular Disorders
Ayurveda understands testicular disease primarily through the concept of Shukra Dhatu, the reproductive tissue that supports fertility, vitality, and deep strength of the body. When Shukra Dhatu becomes depleted, called Shukra Kshaya, or vitiated, called Shukra Dushti, the testes lose their normal tone, nourishment, and protective capacity [11][15]. Classical authors describe conditions where Shukra becomes thick, blocked, or mixed with vitiated blood and Kapha, which can manifest as lumps, heaviness, or abnormal enlargement in the scrotal region [11][15].
The pathology is not limited to Shukra alone. Raktavaha Srotas, which carry blood, and Mamsa and Majja Srotas, which represent muscle and marrow channels, are also involved. When these channels are affected, the local tissue environment becomes stagnant and vulnerable to abnormal growth [12][16]. Disordered Agni, both at the digestive level and at the tissue level, leads to Ama, a toxic and partially processed residue. Ama mixes with Dosha and Dhatu and lodges in vulnerable sites such as the testis, creating a fertile ground for mass formation [13][27].
Vata, particularly when aggravated and mixed with Kapha, is responsible for driving this abnormal growth. Vata supplies the movement and proliferative force, while Kapha provides the sticky, dense, and hard quality of the mass. Together they create a firm, deep seated swelling that does not suppurate, closely matching the classical description of Arbuda [12][13]. Charaka, Sushruta, and Bhavaprakasha describe these patterns and connect them with errors in diet, sleep, sexual excess, chronic stress, and suppression of natural urges [11][15][16]. Rasaratna Samuchchaya and related Rasashastra texts further add the view that depletion of Ojas and long standing Dhatu imbalance invite malignant transformation and require Rasayana based correction [17][18].
B. Ayurvedic Pathology of Testicular Tumors
In the Ayurvedic model, a testicular tumor corresponds most closely to Arbuda, a non suppurative, firm, and deeply rooted mass that grows slowly but steadily. Sushruta explains that such a mass arises when aggravated Dosha lodge in a particular Dhatu and create a circumscribed swelling that does not break open like an abscess [12][13]. In the testis, this Arbuda expresses a dominant Vata Kapha pattern. Vata drives erratic cell behavior and irregular proliferation, while Kapha gives solidity, heaviness, and resistance to dissolution [12][27].
The Dhatu primarily involved are Shukra, Raktavaha, and Mamsa. Shukra provides the base tissue, Raktavaha supplies blood and nutrition, and Mamsa provides structural bulk. When these Dhatu are contaminated with Ama and vitiated Dosha, normal cell communication is lost and localized overgrowth begins [11][15][27]. Srotas, the transport channels, then develop Sanga or obstruction, which further reduces clearance of waste and increases local stagnation. This combination of Dhatu Dushti and Srotas Sanga explains why such masses are often firm, poorly mobile, and resistant to simple local measures. Majja Dhatu and Ojas are secondarily affected, leading to fatigue, weight loss, reduced immunity, and mental disturbance [16][18].
C. Classical Ayurvedic Cure Mechanism
Ayurvedic cure strategy is based on reversing this Dhatu Dushti and Srotas Sanga rather than only shrinking the visible mass. The central pillar is Rasayana therapy, which works to rebuild healthy tissue architecture, strengthen Ojas, and restore normal communication between cells [17][23][25]. Rasayana is introduced after careful assessment of strength, digestion, and previous treatments.
Shodhana, or purification therapy, may be used when the patient is strong enough and when Ama load is high. Virechana and Basti can be chosen to clear Pitta, Vata, and Kapha from the deeper channels and to open the circulation. However, in patients receiving chemotherapy or in those with poor strength, Shodhana is kept optional and tailored very conservatively [23][27].
Lekhana and Kapha Medo reducing herbs are used to gradually reduce the mass effect and clear stagnant fluids. These herbs are combined with preparations that rejuvenate Shukra Dhatu, so that the testes and reproductive channels regain tone and vitality [11][21]. Majja and Ojas are supported with deeply nourishing Rasayana to counter fatigue, weight loss, and immune depletion. Throughout this process, Balya and Rasayana herbs are also used to reduce nausea, weakness, and mucosal damage that may be caused by modern chemotherapy or radiotherapy, without interfering with oncologic protocols [21][23][25].
Classical texts describe healing timelines not in weeks but in cycles of Dhatu replenishment. A complete course of Rasayana is often planned over several months to one year, matching the slow nature of Dhatu regeneration and immune recovery [17][23]. Integration with modern oncology is emphasized in contemporary practice so that surgery and chemotherapy handle the immediate tumor burden, while Ayurvedic therapy focuses on terrain correction, relapse prevention, and restoration of fertility and strength [21][25][27].
D. Ayurvedic Medicines as per Texts
Ayurvedic texts describe several categories of medicines that can be aligned with the testicular cancer terrain. Vrishya Rasayana formulations, which specifically build Shukra Dhatu, are used to restore reproductive tissue and support fertility after aggressive treatment [11][21]. Kanchanar Guggulu is a classical compound cited for granthi and arbuda conditions, indicating its role in reducing glandular and nodular swellings, particularly where Kapha and Medo are dominant [16][24].
Triphala combined with Trikatu supports deep level detoxification by improving Agni and promoting the removal of Ama from the intestinal and tissue channels [22][23]. Suvarna Bhasma is valued for micronutrient support, immune modulation, and Rasayana action at the cellular level [18][19][28]. Heerak Bhasma is described as a powerful Rasayana that enhances cellular resilience and strength when used with precise dosing under expert supervision [18][30]. Abhrak Bhasma, especially in well purified and nano fine form, is indicated for Majja and Dhatu deep rejuvenation and is often used in long term convalescence [18][29].
Herbs such as Ashwagandha, Shatavari, and Atmagupta provide adaptogenic, anxiolytic, and Vrishya support, helping the patient tolerate stress and regain vitality [21][26][25]. Classical medicated ghees, such as Shukra vardhak ghrita, are used to carry these herbs deep into the reproductive channels. Kanchanar based avaleha and Kapha Medo cleansing herbs further assist in gradually reducing residual nodularity and preventing new growth [16][24]. Rasayana protocols are framed in line with guidance from Rasaratna Samuchchaya, Rasendra Chintamani, and related Rasashastra works, which stress proper purification, correct anupana, and individualized dosing [17][18].
E. Expected Outcomes as per Ayurvedic Framework
From an Ayurvedic standpoint, successful therapy is measured not only by imaging results but also by restoration of Dhatu health and Ojas. In benign or early lesions, reduction in mass size, softening of the swelling, and relief from heaviness are expected as Kapha Medo stagnation clears and Srotas open [16][24][27]. In patients who have already undergone surgery and chemotherapy, the primary goal becomes reduction of treatment side effects such as fatigue, neuropathy, and digestive disturbance, along with improvement in appetite, sleep, and mental clarity [21][23].
With sustained Rasayana and Vrishya support, many patients see gradual improvement in testosterone levels, libido, and mood, reflecting better Shukra and Majja status [11][21]. Sperm recovery and fertility enhancement are expected over time when the remaining testis is structurally intact and when toxic load is reduced, although outcomes vary with age and prior drug exposure [21][26]. Long term, the focus shifts to preventing recurrence through strengthening of Ojas, correction of lifestyle factors, and regular monitoring with both modern tests and Ayurvedic clinical assessment [17][23][25].
In this integrated framework, Ayurveda does not replace life saving oncologic treatment. Instead it aims to transform the internal terrain so that the body can fully recover, maintain hormonal and reproductive health, and reduce the risk of future disease while the patient experiences better strength, energy, and mental stability.
Powerful Medicine -Kanchanara-Vrishya-Rasayana Avaleha
A classical Rasayana-based formulation designed for Shukra Dhatu rejuvenation, Arbuda-Granthi conditions, Kapha-Medo clearing, and deep tissue strengthening.
Kanchanara-Vrishya-Rasayana Avaleha is an advanced Ayurvedic preparation inspired by classical references from Charaka Samhita, Sushruta Samhita, Bhavaprakasha, Rasaratna Samuchchaya, and Bhaishajya Ratnavali. It is formulated to support disorders of Shukra Dhatu, Kapha-Medo stagnation, Raktavaha and Mamsa Srotas imbalance, and Majja depletion. It is especially beneficial in conditions where chronic tissue weakness, abnormal glandular growth, hormonal imbalance, and low vitality coexist.
The combination of Kanchanara, Lekhana herbs, Vrishya Rasayana, adaptogens, and rare Rasa-Bhasma preparations provides deep detoxification, tissue nourishment, hormonal balancing, and immune strengthening.
What it is
A traditional Ayurvedic paste designed to support reproductive tissue, improve metabolism and clearance of waste, and rebuild strength after illness. It combines a decoction base, a jaggery syrup, powdered herbs, medicated ghee, and small amounts of mineral bhasmas added at warm temperature.
What it contains (potent herbs and minerals)
- Kanchanar bark and Guggulu for glandular swellings and channel clearance
- Triphala and Trikatu to improve digestion and waste removal
- Varuna, Punarnava, Gokshura, Devdaru for fluid balance and congestion relief
- Ashwagandha, Shatavari, Atmagupta and Guduchi for strength, stress resilience, and immune support
- Shilajit for metabolic reinforcement
- Abhrak bhasma, Suvarna bhasma, optional Heerak bhasma in micro-doses under expert care
- Medicated ghee to carry herbs deep into tissues
How it helps the body
- Improves digestive and tissue metabolism, helping the body process waste and reduce stagnation
- Supports immune signaling and cellular housekeeping pathways seen in lab studies with several ingredients
- Helps energy, mood, sleep, and recovery when people are run down by chronic illness and treatment
Thirty-day batch: ingredients and steps
Target yield: about 900 grams paste
Suggested intake: 15 grams twice daily after food, only if prescribed by a qualified practitioner
A. Decoction base
- Kanchanar bark 200 g
- Triphala 150 g
- Trikatu 75 g
- Gokshura 100 g
- Punarnava 100 g
- Varuna bark 100 g
- Devdaru 50 g
Add all decoction herbs to 3.5 liters water. Simmer gently to about 900 to 1000 ml. Strain.
B. Jaggery syrup
Add jaggery 650 g to the warm filtered decoction. Heat to a thin thread consistency.
C. Powdered herbs
Stir in off-heat, avoiding lumps:
- Ashwagandha 80 g
- Shatavari 80 g
- Atmagupta 50 g
- Guduchi 50 g
- Shilajit purified 15 g
- Pippali 25 g
D. Medicated ghee
Blend in:
- Shukra-vardhak ghrita 50 g
- Rasayana ghrita 25 g
E. Mineral bhasmas at warm temperature
When the mix cools to about 40 degrees:
- Abhrak bhasma 3 g
- Suvarna bhasma 500 mg
- Heerak bhasma 125 mg only if specifically indicated by the physician
Mix until uniform. Store in a sterile, airtight glass jar.
Important safety notes for patients
- Use only under qualified supervision. Mineral bhasmas require expert dosing and timing.
- Do not self-medicate. Do not delay or discontinue doctor-recommended cancer treatment.
- Tell your clinician about all herbs and supplements you take.
Why these ingredients are considered promising (evidence snapshot)
- Ashwagandha contains withaferin A, which shows anticancer actions in lab models, including effects on NF-kB and other survival pathways. These are preclinical findings, not definitive human cancer cures.
- Triphala mixtures have demonstrated apoptosis and growth inhibition in cancer cell and animal models, with additional antioxidant and immunomodulatory signals.
- Guggulsterone from Commiphora mukul modulates NF-kB–linked inflammation and shows antiproliferative activity in multiple cancer cell models.
- Tinospora cordifolia is repeatedly reported as immunomodulatory in preclinical work and small human studies, suggesting support for host defense.
- Kanchanar Bauhinia variegata extracts show antioxidant and cytotoxic signals in preclinical studies, and Kanchanar Guggulu appears in classical chapters for granthi and arbuda contexts; modern overviews discuss this tradition but clinical trials remain limited.
- Abhrak bhasma has been characterized as nano-scaled biotite mica; early toxicology and characterization studies exist but are not substitutes for oncology trials.
- Suvarna bhasma likely contains nanoscale gold and has emerging data for immunomodulation and neuroprotection, still exploratory for cancer.
- Heerak bhasma is investigated as a nanodiamond-based herbomineral in preclinical tumor models; this is not established human therapy.
FAQs
What is Kanchanara Vrishya Rasayana Avaleha?
It is a traditional Ayurvedic paste that combines a herbal decoction, jaggery syrup, powdered herbs, medicated ghee, and tiny quantities of purified mineral preparations called bhasma. It is formulated for glandular swellings, Shukra Dhatu support, metabolic cleansing, and strength recovery.
How does it work in Ayurveda?
Ayurveda explains testicular and glandular problems through Shukra Dhatu depletion, Kapha and Vata imbalance, Ama accumulation, and blockage of channels called Srotas. The avaleha uses lekhana and rasayana principles to clear stagnation, nourish reproductive tissues, and rebuild Ojas.
Which herbs and minerals does it contain?
Key herbs include Kanchanara, Guggulu, Triphala, Trikatu, Varuna, Punarnava, Gokshura, Devdaru, Ashwagandha, Shatavari, Atmagupta, Guduchi, Shilajit, and Pippali. Medicated ghee is added as a carrier. Mineral preparations may include Abhrak bhasma, Suvarna bhasma, and occasionally Heerak bhasma under expert supervision.
Who may be considered for this formulation?
Adults with glandular or nodular concerns, Shukra Dhatu weakness, fatigue after illness, or low vitality may be considered after a full Ayurvedic assessment. Suitability always depends on age, strength, digestion, current medicines, and lab results.
How is the dose taken?
A common plan is fifteen grams twice daily after food with warm water or warm milk. The exact dose and duration must be decided by your physician.
Can I prepare it at home?
No. The decoction stage, syrup stage, addition of powders, correct temperature for bhasma, and final consistency require professional training and sterile technique.
Can it be used along with modern cancer care?
Many patients use Ayurvedic rasayana under physician oversight while they receive standard care. Always inform your oncologist and your Ayurvedic doctor about every medicine and supplement you take.
Are there any people who should avoid it?
It is not advised in pregnancy or during breastfeeding, in children, in uncontrolled liver or kidney disease, or when there is known allergy to any ingredient. Patients on blood thinners, immunosuppressants, or multiple medicines need individualized review.
What side effects can occur?
Most patients tolerate rasayana well when it is correctly prepared and dosed. Possible issues include digestive upset, heaviness, or sensitivity to spices. Stop and contact your physician if you notice unusual symptoms.
What lab tests are recommended during use?
Your doctor may monitor complete blood count, kidney and liver function, fasting glucose and lipids, and in selected cases reproductive hormones and semen parameters.
How long before I feel changes?
Energy, appetite, and sleep may improve within a few weeks. Deep tissue changes and reproductive support usually need several months. Your plan will be reviewed at set intervals.
What diet and lifestyle help the process?
Prefer freshly cooked foods, seasonal vegetables, adequate protein, warm water, regular sleep, sunlight exposure, and gentle exercise. Limit alcohol, tobacco, ultra processed foods, and late night meals.
How should I store it?
Use a clean dry spoon. Keep the jar tightly closed in a cool place away from direct sunlight. Do not refrigerate unless your physician advises.
What if I miss a dose?
Take it when you remember if it is not close to the next dose. Do not double the amount.
How do I know the product is authentic and safe?
Ask about source transparency, good manufacturing practices, lab testing for heavy metals and microbiology, and documentation of purified bhasma. Work only with qualified practitioners and reputable pharmacies.
Reference (Modern + Ayurvedic)
A. Modern Medical References (Testicular Cancer)
- National Cancer Institute. (2024). Testicular Cancer Treatment (PDQ®)–Health Professional Version.
https://www.cancer.gov/types/testicular/hp/testicular-treatment - American Cancer Society. (2024). Testicular Cancer Early Detection, Diagnosis, and Staging.
https://www.cancer.org/cancer/testicular-cancer/detection-diagnosis-staging.html - Stephenson, A. J., et al. (2020). Management of testicular cancer: A review. JAMA, 324(6), 602–614.
https://doi.org/10.1001/jama.2020.7920 - Hanna, N., & Einhorn, L. H. (2014). Testicular cancer—discoveries and updates. New England Journal of Medicine, 371, 2005–2016.
https://doi.org/10.1056/NEJMra1407550 - Gilligan, T., et al. (2020). Testicular cancer guidelines: Diagnosis and treatment. European Urology, 78(1), 104–120.
https://doi.org/10.1016/j.eururo.2020.02.038 - Cheng, L., et al. (2018). Testicular cancer: Pathology and genetics. Human Pathology, 71, 62–73.
https://doi.org/10.1016/j.humpath.2017.09.021 - Woodward, P. J., et al. (2002). From the archives of the AFIP: Tumors of the testis. Radiographics, 22(1), 189–216.
https://doi.org/10.1148/radiographics.22.1.g02ja15189 - Einhorn, L. H. (2002). The cure of testicular cancer: The Indiana University experience. CA: A Cancer Journal for Clinicians, 52(6), 366–373.
https://doi.org/10.3322/canjclin.52.6.366 - Dieckmann, K. P., & Pichlmeier, U. (2004). Clinical epidemiology of testicular germ cell tumors. World Journal of Urology, 22(1), 2–14.
https://doi.org/10.1007/s00345-003-0386-8 - Kim, S., et al. (2019). Ultrasound imaging in testicular tumors: Features and accuracy. Ultrasound Quarterly, 35(4), 289–296.
https://doi.org/10.1097/RUQ.0000000000000464
B. Ayurvedic Classical Text References (With Chapter / Verse)
- Charaka Samhita – Chikitsa Sthana 30 (Shukra Dhatu Vikara Chikitsa).
Translator: P. Kashinath & G. C. Chunekar, Chaukhamba Sanskrit Series. - Sushruta Samhita – Nidana Sthana 11 (Arbuda Nidana).
Translator: Kaviraj Ambikadatta Shastri, Chaukhamba Sanskrit Pratishthan. - Sushruta Samhita – Chikitsa Sthana 18 (Arbuda Chikitsa).
Ayurvedic surgical approaches to non-suppurative mass. - Ashtanga Hridaya – Uttara Tantra 39 (Shukra Roga).
Vagbhata’s classification of Shukra Dhatu disorders. - Bhavaprakasha – Madhyam Khanda, Chapter on Shukra Roga (verses describing Shukra Dushti, Raktaprasadana, and Vrishya Rasayana).
Chaukhamba Sanskrit Bhavan edition. - Bhaishajya Ratnavali – Granthi/Arbuda Chikitsa (Chapter 35).
Kanchanar Guggulu reference. - Rasaratna Samuchchaya – Rasayana Adhikara (Chapters 21–23).
Principles of Rasayana, rejuvenation, tissue repair. - Rasendra Chintamani – Rasayana Prakarana.
Classical explanation of Gold Bhasma, Abhrak Bhasma, Heerak Bhasma. - Rasa Tarangini – Taranga 20 (Suvarna Bhasma preparation and properties).
Sadananda Sharma. - Yoga Ratnakara – Shukra Roga Chikitsa.
Ayurvedic treatments for disorders of the reproductive tissues.
C. Ayurvedic Pharmacology & Research References
- Singh, R. H. (2017). Exploring Shukra Dhatu and Vrishya Rasayana. AYU Journal, 38(3), 200–206.
https://doi.org/10.4103/ayu.AYU_102_16 - Pandey, M. M., et al. (2013). Guggulu: Modern pharmacology and therapeutic potential. Journal of Ethnopharmacology, 148(1), 1–14.
https://doi.org/10.1016/j.jep.2013.03.027 - Sharma, H., & Clark, C. (2015). Rasayana therapy: Rejuvenation and immunity enhancement. Journal of Alternative and Complementary Medicine, 21(6), 365–372.
https://doi.org/10.1089/acm.2014.0281 - Patel, S., et al. (2020). Kanchanar Guggulu in lymphatic and glandular disorders: A review. AYU, 41(2), 117–124.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7975353/ - Kulkarni, P., et al. (2018). Ayurvedic Rasayana herbs and their anti-cancer potential. Pharmacognosy Reviews, 12(23), 45–54.
https://doi.org/10.4103/phrev.phrev_2_18 - Dandu, A. M., et al. (2012). Antioxidant and cytoprotective activity of Ashwagandha. Phytotherapy Research, 26(12), 1938–1944.
https://doi.org/10.1002/ptr.4676 - Ghodke, P. S., et al. (2011). Ayurvedic approach to Arbuda (tumors): A conceptual review. AYU, 32(4), 556–562.
https://doi.org/10.4103/0974-8520.96126 - Kothari, A., et al. (2021). Traditional gold preparations and their biomedical potential. Journal of Ayurveda and Integrative Medicine, 12(1), 38–45. https://doi.org/10.1016/j.jaim.2019.09.006
- Tambe, Y., et al. (2020). Therapeutic potential of Abhrak Bhasma. Ancient Science of Life, 39(1), 1–8. https://doi.org/10.4103/asl.ASL_155_19
- Sane, R. T., et al. (2013). Chemical composition and safety evaluation of Heerak Bhasma.Journal of Pharmacognosy, 5(3), 232–240.https://doi.org/10.4103/0975-3575.116774