- How Common Asymptomatic Herpes Really Is
- What a Herpes Blood Test Actually Detects
- The Difference Between Carrying a Virus and Having Disease
- Why Some Immune Systems Keep HSV Silent
- Genetics, Immunity, and Individual Differences
- The Role of Stress, Illness, and Life Changes
- Why Doctors Rarely Test Without Symptoms
- Why “No Symptoms” Usually Means Low Clinical Risk
- Addressing the Fear: “Is Something Wrong With Me?”
- What You Should Not Do After a Positive Test
- When a Positive Test Actually Matters Clinically
- How Some Medical Systems Explain Long-Term Viral Silence
- Living Normally With a Positive Test Result
- Doctor Profile
- FAQs
- References
A Positive Test Does Not Mean You Are Sick
Testing positive for herpes but no symptoms is one of the most confusing and distressing experiences many people face after a routine blood test. The word “positive” often triggers fear, shame, and the assumption that something is seriously wrong, even when the person feels completely healthy. In reality, a positive herpes test does not automatically mean you are sick, contagious, or destined to develop symptoms. For a large proportion of people, it simply reflects past exposure and a normal immune response, not active disease [1].
Public health data consistently show that herpes infections are extremely common and that the majority of people who carry herpes antibodies never experience noticeable outbreaks or ongoing health problems [1], [10]. This is especially true when the test is done in the absence of symptoms. Blood tests are designed to detect antibodies, which are markers of immune memory, not proof of current illness. As a result, many people test positive years after exposure without ever having been aware of an infection [2].
Understanding this distinction is essential for reducing unnecessary anxiety. Feeling well after a positive result is not unusual, and it often indicates that the immune system is effectively keeping the virus under control. This article explains why testing positive for herpes but no symptoms is so common, what the result actually means, and why being symptom-free is often a reassuring sign rather than a cause for alarm [1], [2], [10].
How Common Asymptomatic Herpes Really Is
Asymptomatic Infection Is the Most Common Outcome, Not the Exception
If you have tested positive for herpes but no symptoms, it can feel as though you are facing something unusual or rare. In reality, from a population and public health perspective, you are part of the majority. Global epidemiological data consistently show that most herpes simplex virus infections remain asymptomatic or so mild that they are never recognized as herpes [1], [10].
When clinicians and researchers look at herpes at a population level rather than through clinic-based case reports, a very different picture emerges. The majority of people who carry herpes antibodies have never experienced the classic outbreaks that are often highlighted online or in public discussions. This silent pattern is not a failure of diagnosis. It is how herpes behaves in most human hosts [1].
Global Numbers Show Silence, Not Symptoms
Worldwide estimates indicate that billions of people are infected with HSV-1, and hundreds of millions with HSV-2. Yet only a fraction of these individuals ever receive a clinical diagnosis or recall symptoms consistent with herpes [6], [7]. This discrepancy exists because herpes is largely an asymptomatic infection at the population level.
From a global health standpoint, herpes persists not because most people are visibly ill, but because the virus often causes no noticeable illness at all [6], [10]. You can carry the virus, mount a normal immune response, and live your entire life without outbreaks, medical intervention, or health decline related to herpes.
HSV-1 and HSV-2 Are Often Silent in Different Ways
HSV-1 is commonly acquired early in life, frequently through non-sexual contact. In many people, it never produces recognizable cold sores or genital symptoms, even though antibodies are clearly detectable in blood tests [6], [10]. This explains why HSV-1 seropositivity is so widespread and so rarely associated with ongoing disease.
HSV-2, while more strongly associated with genital infection, follows a similar pattern at scale. Large studies show that many people with HSV-2 antibodies have either very mild symptoms, atypical signs that are not recognized as herpes, or no symptoms at all [7]. As a result, HSV-2 infections are often discovered incidentally through blood testing rather than clinical illness.
Why Most People Never Realize They Have Herpes
For many individuals, the immune system contains the virus effectively from the very beginning. There is no dramatic first episode, no recurring lesions, and no clear signal that an infection ever occurred. Years later, when a blood test is performed, the result can feel shocking precisely because nothing ever felt wrong [1].
From a public health perspective, this is expected. Health authorities openly acknowledge that most people living with herpes are unaware of it because symptoms never develop or never reach clinical significance [1], [10]. This is not denial or underreporting. It is the natural history of the virus in most people.
Reframing What “Positive” Really Means
When you look at herpes through an epidemiological lens rather than an emotional one, a positive test without symptoms becomes far less alarming. It does not indicate a failing body, a hidden illness, or an inevitable future problem. Instead, it places you squarely within the most common and biologically stable category of herpes infection [1], [6], [7], [10].
For clinicians, researchers, and public health systems, asymptomatic herpes is the norm. For patients, learning this often marks the turning point from fear to understanding. Knowing how common silent herpes truly is allows you to interpret a positive test result accurately, without assuming illness where none is present.
What a Herpes Blood Test Actually Detects
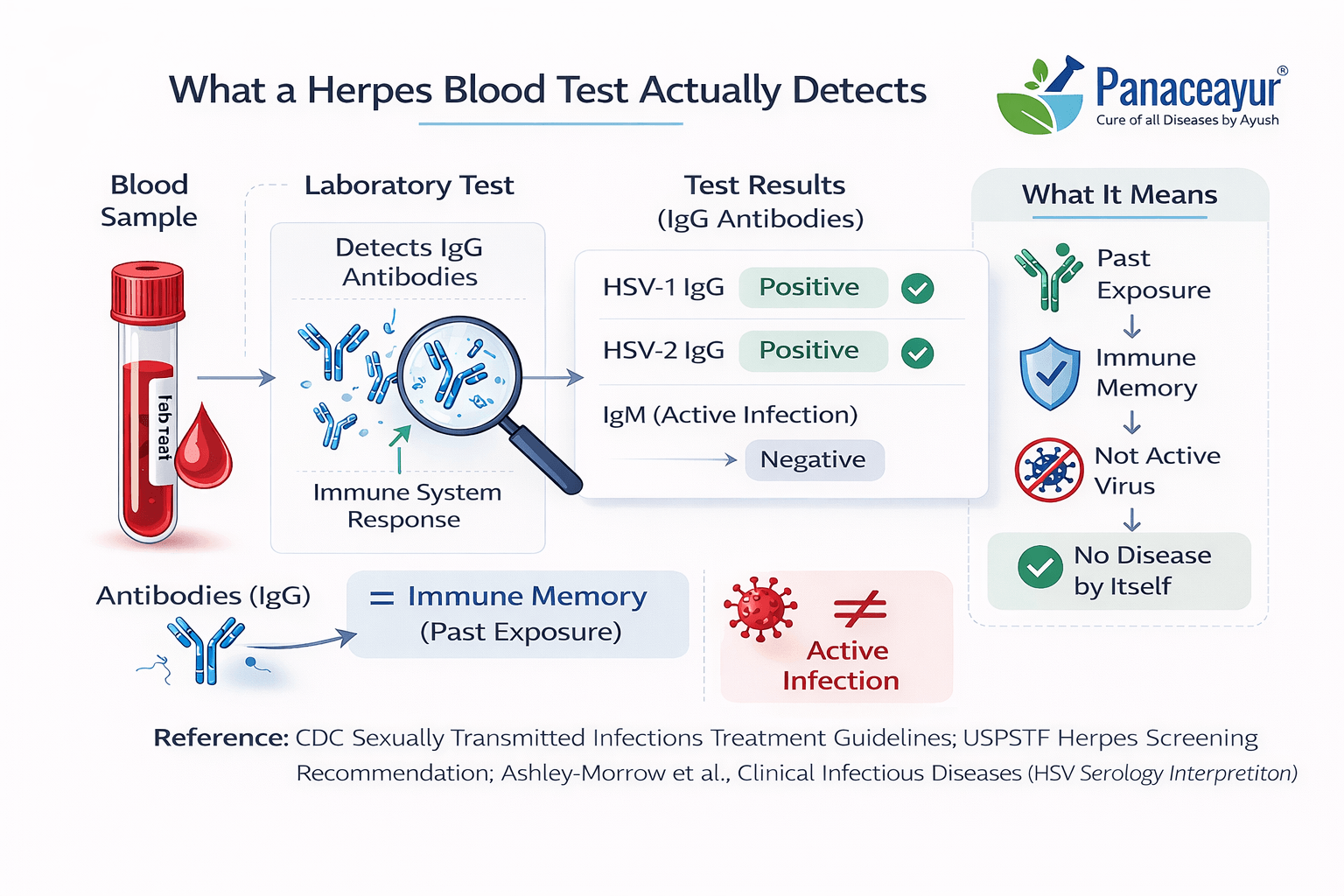
A Herpes Blood Test Does Not Look for Active Disease
When you receive a herpes blood test result, it is easy to assume the test is telling you whether the virus is active in your body right now. That assumption is the root of much of the panic that follows a positive result. In reality, standard herpes blood tests do not detect live virus, current infection activity, or disease severity. They detect antibodies, which are markers of your immune system’s past exposure and memory [3], [12].
From a medical standpoint, this distinction is critical. A blood test cannot tell whether herpes is dormant, active, or causing damage. It can only confirm that your immune system has encountered the virus at some point in time and responded appropriately [3]. This is why people who feel completely healthy often test positive.
Understanding IgG Antibodies and Immune Memory
Most herpes blood tests measure IgG antibodies. IgG is not a sign of illness. It is a sign of immune recognition. When your body encounters a virus, it produces IgG antibodies to remember it, often for life. This is how long-term immune memory works across many infections, not just herpes [4].
If you test positive for herpes IgG, it means your immune system has done its job. It has identified the virus and built a lasting defense against it. It does not mean the virus is actively multiplying, causing symptoms, or spreading uncontrollably inside you [4], [12].
For many people, this immune response occurs without noticeable illness. You may never have had sores, pain, or any sign that herpes was present. Years later, the antibodies remain detectable, even though the virus has remained clinically silent [3].
Timing Matters: Why the Test Cannot Date the Infection
Another common source of anxiety is the belief that a positive test means recent infection. Herpes blood tests cannot reliably tell when exposure occurred. IgG antibodies usually develop weeks to months after infection and then persist long term [4].
This means your positive result could reflect an exposure from many years ago. It could have occurred before your current relationship, before adulthood, or even earlier in life in the case of HSV-1 [4], [12]. The test offers no timeline and should not be used to assign blame, timing, or recent transmission.
Why Blood Tests Have Limits in Asymptomatic People
Medical guidelines emphasize that herpes blood tests have significant limitations, especially in people without symptoms. False positives, low predictive value in low-risk populations, and unnecessary psychological distress are well-documented concerns [3], [12].
This is why major health authorities advise against routine herpes blood testing in asymptomatic individuals. Not because herpes is unimportant, but because the test result often creates more confusion than clarity when there are no clinical signs to interpret alongside it [3].
From a clinician’s perspective, blood tests are tools, not diagnoses. Without symptoms, physical findings, or a clear clinical question, a positive antibody result rarely changes medical management [12].
Reframing the Result to Reduce Panic
If you test positive for herpes but no symptoms, the blood test is telling you one thing only: your immune system has encountered the virus and remembers it. It is not telling you that you are sick, contagious at all times, or at risk of inevitable outbreaks [3], [4], [12].
For patients, understanding what the test actually measures often marks the turning point from fear to perspective. For clinicians, it reinforces why interpretation must always be grounded in symptoms, not numbers alone. And for public health systems, it explains why widespread asymptomatic testing is discouraged despite how common herpes antibodies are [3].
Seen clearly, a herpes blood test is a record of immune history, not a verdict on your current health.
The Difference Between Carrying a Virus and Having Disease
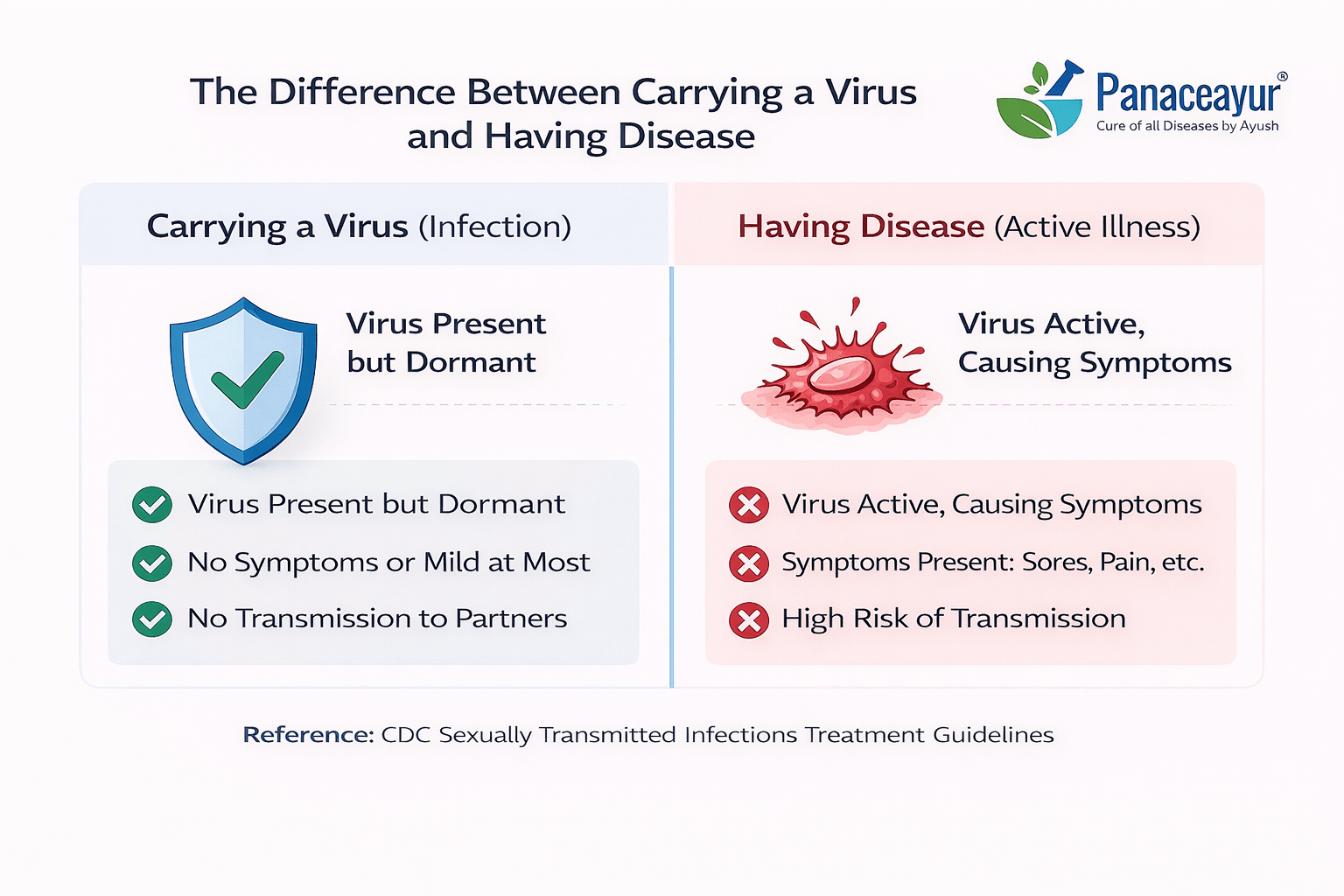
Infection and Disease Are Not the Same Thing
One of the most important distinctions to understand after a positive herpes test is the difference between carrying a virus and having disease. In everyday language, these two ideas are often treated as identical, but in virology and clinical medicine, they are very different states. You can carry a virus in your body without being ill, without symptoms, and without any ongoing tissue damage [5], [8].
Herpes simplex virus is particularly well known for this behavior. Once the virus enters the body, it establishes a long-term presence, but that presence alone does not equal disease. Disease refers to active symptoms, inflammation, or functional impairment. Infection simply means the virus exists within the host. For most people with herpes, infection never progresses into disease [8].
Viral Latency: Presence Without Activity
After initial exposure, herpes simplex virus enters a phase known as latency. During latency, the virus resides inside nerve cells in a dormant state. It is not actively replicating, not spreading through tissues, and not causing damage [5], [11]. This latent state can persist indefinitely.
From a biological standpoint, latency is not a failure of the immune system. It is a stable coexistence between host and virus. The immune system keeps the virus suppressed, while the virus remains largely inactive. This is why many people live their entire lives carrying herpes without ever experiencing symptoms [5].
Immune Containment Defines Health, Not Viral Eradication
Modern virology recognizes that complete elimination of certain viruses is not always necessary for health. What matters clinically is immune containment. When the immune system successfully controls a virus, disease does not occur, even though the virus remains present [8], [11].
If you are asymptomatic, it means immune containment is working. The virus exists, but it is not expressing itself in a way that harms you. This principle applies to many viruses, not only herpes. Herpes simply makes this concept visible because testing can reveal silent infection [8].
Why Symptoms Are the Exception, Not the Rule
Clinical outbreaks occur when the balance between the virus and the immune system is temporarily disrupted. This disruption does not happen in most people. Epidemiological data and long-term clinical observation show that the majority of individuals with herpes remain symptom-free or experience only minimal, unrecognized activity [5], [8].
From the patient’s perspective, this distinction is often missed. A positive test feels like a diagnosis of illness, when in fact it is a confirmation of viral presence. From the clinician’s perspective, the absence of symptoms is a meaningful indicator of health, not something to dismiss [11].
Reframing Health After a Positive Test
Understanding the difference between carrying a virus and having disease changes how a positive herpes test should be interpreted. You may carry herpes for decades without illness, without progression, and without impact on your overall health. The presence of the virus alone does not define your clinical status [5], [8], [11].
For patients, this distinction helps reduce fear and self-stigma. For healthcare providers, it reinforces the importance of symptom-based evaluation rather than test-based assumptions. And for public health, it explains why herpes is so widespread yet so often clinically silent. Carrying a virus is common. Having disease is not.
Why Some Immune Systems Keep HSV Silent
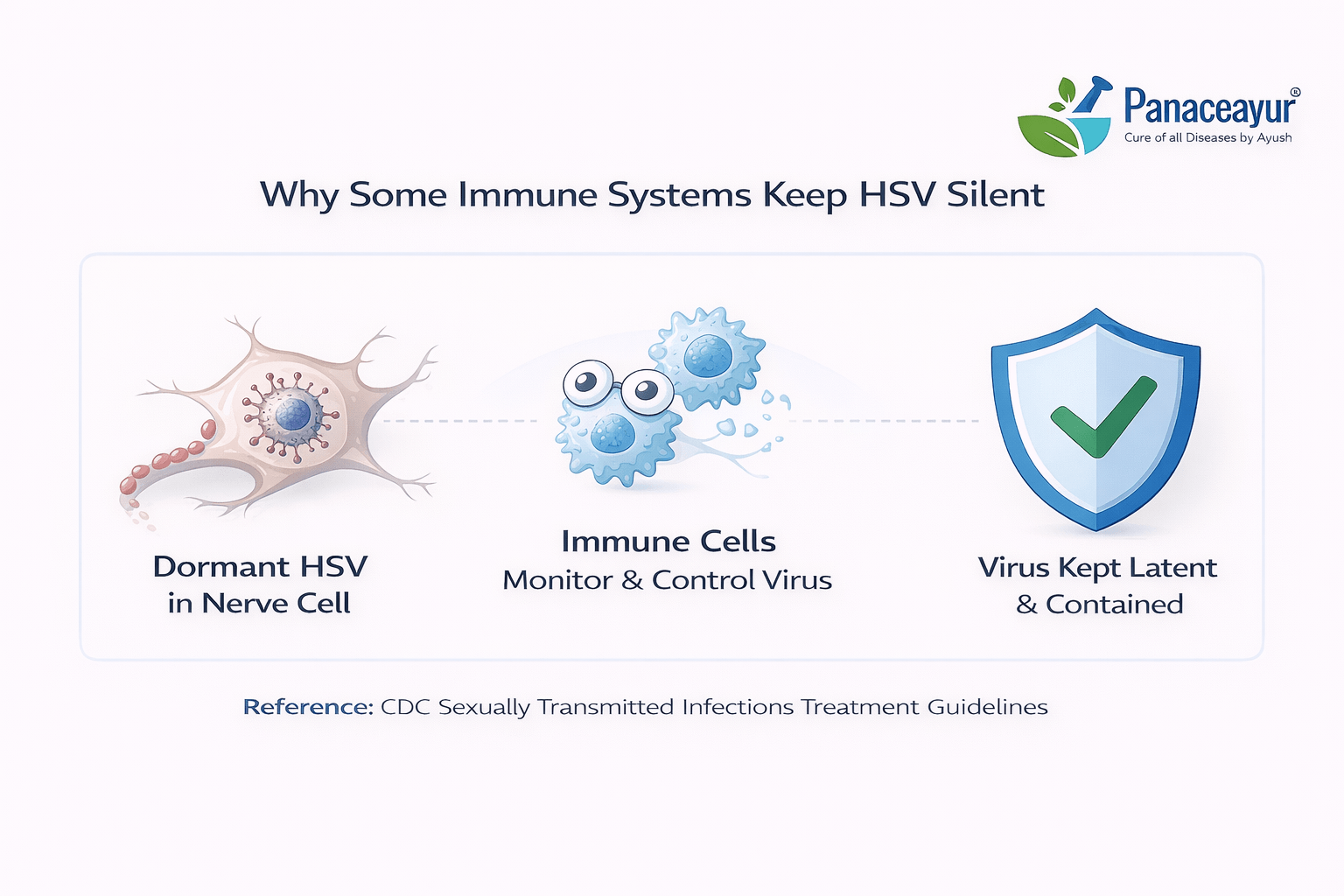
Immune Control, Not Viral Strength, Determines Outcomes
After a person is infected with herpes simplex virus, what happens next is largely determined by the immune system, not by the virus itself. Many people assume that outbreaks occur because the virus is aggressive or uncontrollable. In reality, whether HSV remains silent or becomes symptomatic depends on how effectively the host immune system suppresses viral activity [5], [8].
If you have tested positive but never had symptoms, it usually means your immune system has established strong control early on. From a clinical perspective, this is not luck or coincidence. It reflects a stable biological balance in which the virus is present but kept functionally inactive [8].
How the Immune System Suppresses HSV
Once HSV enters latency, immune surveillance plays a continuous role in preventing reactivation. Specialized immune cells monitor infected nerve tissue and rapidly limit viral gene expression before it can escalate into visible disease [5], [11]. This process happens silently and efficiently in many individuals.
From the patient’s point of view, nothing feels like it is happening at all. From the immune system’s point of view, constant low-level control is taking place. This is why a person can carry HSV for years without lesions, pain, or any awareness of infection [5].
Why Immune Silence Is Common, Not Fragile
A common fear after testing positive is the belief that silence is temporary and that outbreaks are inevitable. Scientific evidence does not support this assumption. In many people, immune-mediated suppression remains stable over long periods, sometimes for life [8], [11].
Clinical observations show that even among individuals who experience early symptoms, viral activity often decreases over time as immune control improves. For those who never develop symptoms at all, this immune balance may already be optimal from the beginning [5], [8].
Individual Differences in Immune Containment
Not all immune systems respond to HSV in the same way. Genetic factors, immune regulation, and overall physiological balance influence how effectively the virus is suppressed. This explains why two people with the same virus can have very different experiences [8].
For clinicians, this variability reinforces why one-size-fits-all predictions do not apply to herpes. For patients, it helps remove self-blame. If your immune system keeps HSV silent, it is not because you are doing something special or avoiding something perfectly. It is because your biology supports effective containment [5], [11].
What Silence Actually Means Clinically
Being asymptomatic is not a warning sign of hidden damage or future collapse. Clinically, it is evidence of health. It indicates that immune defenses are functioning well enough to prevent disease expression, even though the virus remains present [5], [8], [11].
For you, this means that silence is meaningful. For healthcare providers, it is a key factor in deciding whether any intervention is necessary. And for public health understanding, it explains why HSV is widespread yet rarely disruptive. In most people, the immune system does not fight HSV aggressively or visibly. It simply keeps it quiet, and that quiet is the most common and stable outcome.
Genetics, Immunity, and Individual Differences
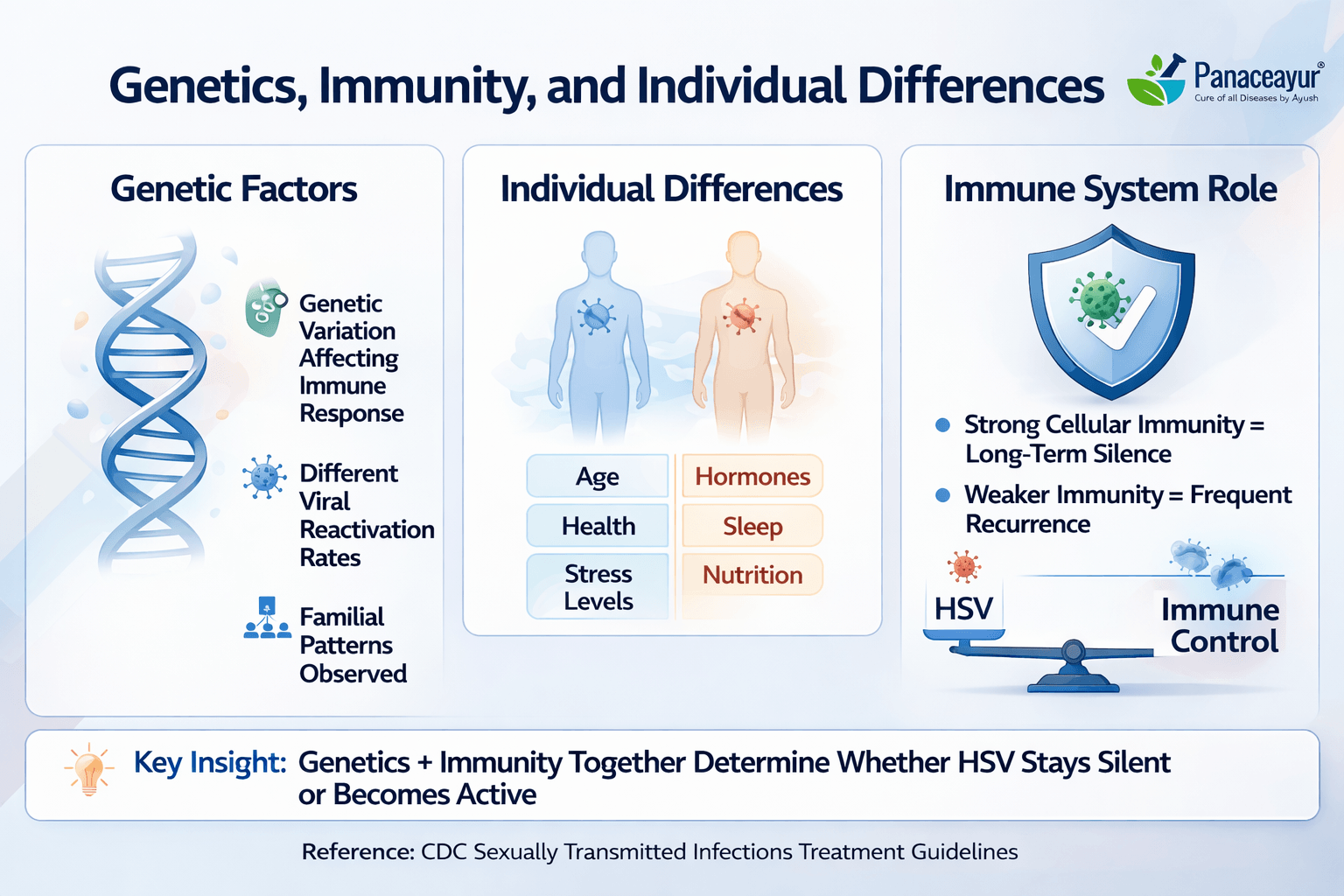
Why the Same Virus Leads to Different Experiences
One of the most confusing aspects of herpes for patients is seeing how differently it behaves from one person to another. You may test positive for HSV and never experience symptoms, while someone else develops recurrent outbreaks. This difference is not explained by morality, hygiene, sexual behavior, or personal failure. It is explained by biology, specifically by differences in genetics and immune regulation [5], [8].
From a virology standpoint, herpes does not behave uniformly across hosts. The virus is the same, but the internal environment it enters is not. Each immune system responds in a slightly different way, shaping whether HSV remains silent or becomes clinically visible [8].
The Role of Genetic Variation
Genetic factors influence how immune cells recognize viral proteins, how strongly inflammatory responses are triggered, and how efficiently viral replication is suppressed. These differences exist long before herpes exposure ever occurs. They are part of an individual’s biological makeup, not something that develops because of the virus [5].
For you as a patient, this means that your experience with herpes was largely determined before you were ever exposed. For clinicians and researchers, it explains why predicting who will develop symptoms is difficult. The virus does not create these differences. It reveals them [8].
Immune Regulation Matters More Than Immune Strength
It is common to hear herpes discussed in terms of a “weak” or “strong” immune system. Scientifically, this framing is inaccurate. What matters more is immune regulation, how balanced, targeted, and controlled the immune response is, rather than how aggressive it appears [5].
Some people mount a calm, efficient immune response that suppresses HSV without causing inflammation. Others mount a more reactive response that produces noticeable symptoms. Neither response reflects effort or failure. They reflect different immune programming [8].
Why Behavior Is Not the Explanation
Many people instinctively look for lifestyle explanations after a positive test. Diet, stress, past choices, or specific events are often blamed. While overall health can influence immune function, it does not account for the fundamental differences in how HSV expresses itself between individuals [5].
From a medical perspective, this distinction is important. It removes blame and reduces stigma. You did not cause your asymptomatic status, just as someone else did not cause their symptoms through negligence or error. The variation lies primarily in host biology, not behavior [8].
Normalizing Individual Variation
When herpes is viewed through the lens of genetics and immune diversity, asymptomatic infection becomes easier to understand and accept. It is not an anomaly. It is one of many possible outcomes shaped by normal human variation [5], [8].
For patients, this perspective offers relief from self-judgment. For healthcare providers, it reinforces the importance of individualized assessment rather than assumptions. And for public understanding, it helps shift the conversation away from blame and toward biology. Herpes does not behave differently because people are different in character. It behaves differently because people are different in biology.
The Role of Stress, Illness, and Life Changes
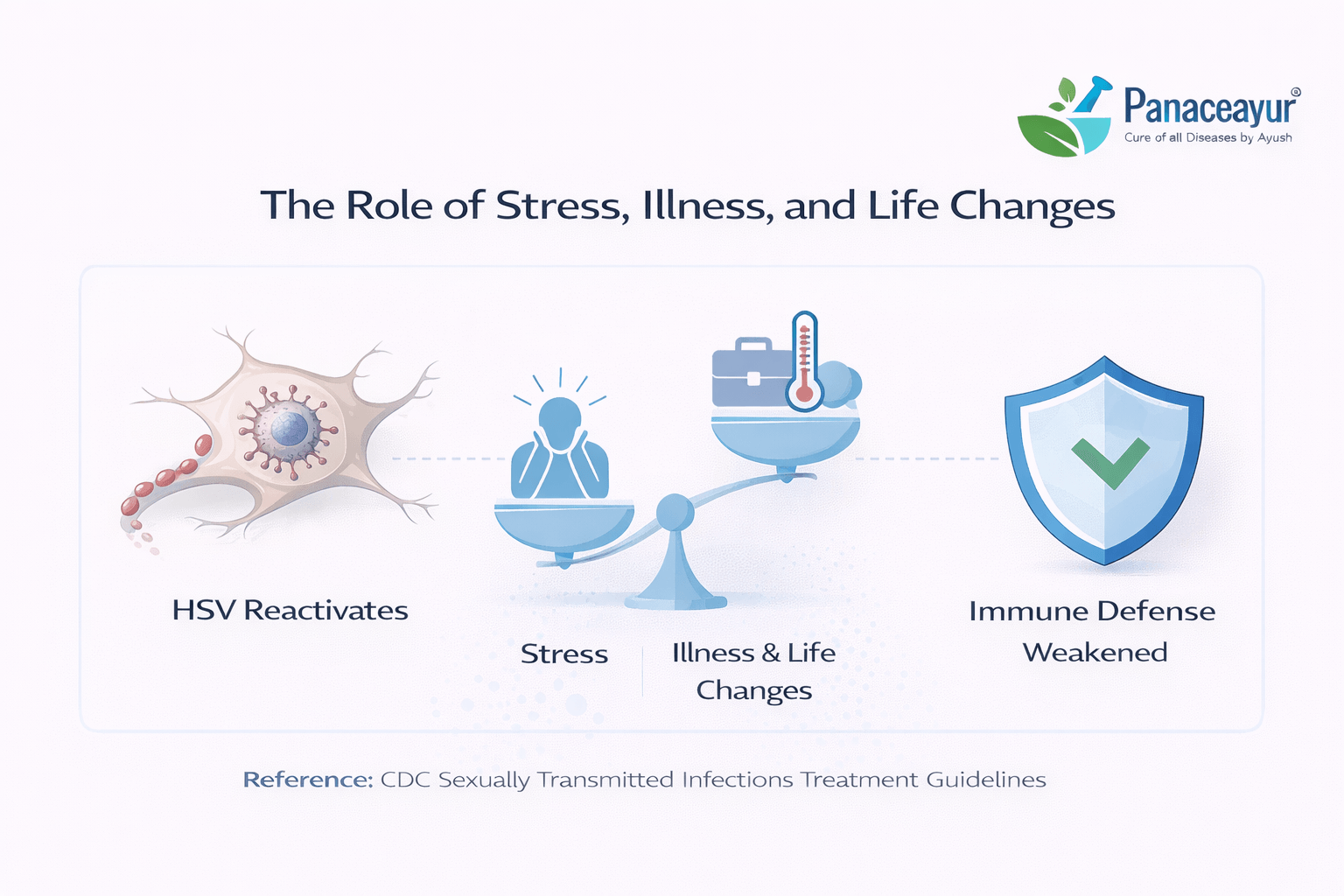
Why HSV Activity Can Fluctuate Without Becoming a Problem
After learning about herpes latency and immune control, many people begin to worry about triggers. You may wonder whether stress, illness, or major life changes will inevitably wake the virus up. Clinically, this fear is understandable, but it is often overstated. Research and long-term observation show that while HSV activity can fluctuate, it does not usually progress in a worsening or uncontrollable direction [8], [9].
From a medical perspective, fluctuations are a normal feature of many chronic viral infections. They reflect temporary shifts in immune regulation, not a loss of control. For most people, these shifts are mild, short-lived, and may never produce recognizable symptoms [8].
Stress Does Not Equal Outbreaks
Stress is frequently blamed as a direct cause of herpes outbreaks. In reality, stress does not act as a simple on off switch for the virus. Severe or prolonged stress can influence immune signaling, but in most individuals this does not translate into clinical disease [8].
If you are asymptomatic, everyday stressors such as work pressure, travel, or emotional strain are unlikely to suddenly change that status. Even in people who have experienced outbreaks in the past, long-term studies show that the frequency and intensity of viral activity often decrease over time rather than escalate [9].
Illness and Temporary Immune Shifts
Acute illnesses such as viral infections, fever, or physical exhaustion can temporarily affect immune balance. From a biological standpoint, this is expected. The immune system reallocates resources to address immediate threats. However, this does not mean HSV automatically becomes active or dangerous during these periods [8].
For many people, even significant illnesses pass without any herpes-related symptoms. When reactivation does occur, it is often brief and self-limited, not a sign of long-term deterioration or immune failure [9].
Life Transitions and the Myth of Inevitable Reactivation
Major life changes such as pregnancy, aging, hormonal shifts, or changes in routine are often described online as high-risk periods for herpes activation. Clinically, the evidence does not support the idea that these transitions inevitably lead to worsening disease [8].
Long-term observational data show that HSV tends to become less active with time in many individuals, even across major life stages. For those who are asymptomatic, this trend toward stability is especially common [9].
What This Means for You Over Time
If you have never had symptoms, the presence of stress or life changes does not mean you are living on the edge of an outbreak. For you, immune control has already proven to be resilient. For clinicians, this resilience is a meaningful indicator that aggressive monitoring or intervention is usually unnecessary [8].
From a broader perspective, these findings help reframe herpes as a virus that often settles into a quiet, stable relationship with the host. Fluctuations may occur, but progression is not the expected outcome. In most people, time works in favor of greater immune balance, not increasing disease expression [8], [9].
Understanding this reduces fear and helps place stress, illness, and life changes into proper biological context. They are part of normal human experience, not automatic threats to health or stability.
Why Doctors Rarely Test Without Symptoms
Routine Herpes Screening Is Not Standard Medical Practice
After receiving a positive herpes result, many people ask a reasonable question: if herpes is so common, why are doctors not testing everyone routinely? From a clinical and public health standpoint, the answer is clear. Routine herpes blood testing in people without symptoms is generally discouraged because it does not improve health outcomes and often causes unnecessary distress [3], [2].
Medical guidelines in both the United States and the United Kingdom are aligned on this point. Doctors are trained to test when a result will meaningfully change diagnosis, management, or patient care. In asymptomatic individuals, herpes blood tests rarely meet that standard [3].
The Problem With Testing When There Are No Symptoms
When you have no symptoms, a positive herpes blood test provides limited actionable information. It confirms past exposure, but it does not predict whether you will ever develop symptoms, when exposure occurred, or whether any treatment is needed [3].
From a clinician’s perspective, this creates a problem. The test result raises questions it cannot answer and often shifts focus away from overall health toward anxiety-driven monitoring. Studies and guideline reviews show that this pattern leads to psychological harm without corresponding medical benefit [3].
False Positives and Unnecessary Anxiety
Another reason doctors avoid routine testing is the risk of false positive or misleading results, particularly in low-risk or asymptomatic populations. Even highly specific tests perform less well when the likelihood of disease is low. This means that some people are told they are positive when the result may not reflect a clinically meaningful infection [3].
For patients, this can be deeply unsettling. You may feel labeled with a condition that has never affected your health and may never do so. Public health authorities recognize this harm and factor it into screening recommendations [2].
Why Guidelines Prioritize Symptoms Over Serology
Both the USPSTF and the NHS emphasize that herpes is primarily a clinical diagnosis. Symptoms, not antibodies, guide care. If you have lesions, pain, or other signs suggestive of herpes, testing helps confirm the cause and guide management. If you have no symptoms, the same test adds little clarity [3], [2].
This does not mean herpes is ignored or minimized. It means that medical systems prioritize tests that improve patient outcomes. In asymptomatic individuals, routine herpes screening does not reduce transmission, prevent complications, or improve long-term health [3].
What This Means for You as a Patient
If your doctor did not recommend herpes testing, it was not an oversight. It was adherence to evidence-based guidance. If you were tested incidentally and received a positive result, the lack of follow-up intervention often reflects clinical judgment rather than dismissal [2].
For you, understanding this context can help reframe the experience. A positive result without symptoms is not something doctors overlook because it is dangerous. It is something they often do not pursue because it is usually not clinically significant [3].
How Clinicians Use This Knowledge
For healthcare providers, these guidelines serve as a reminder to treat patients, not test results. The presence or absence of symptoms remains the most reliable indicator of whether herpes is affecting health. Serology alone, without clinical signs, rarely justifies medical action [3], [2].
Seen through this lens, the decision not to test routinely is not about withholding information. It is about preventing harm, avoiding unnecessary labeling, and focusing care where it truly matters
Why “No Symptoms” Usually Means Low Clinical Risk
Absence of Symptoms Is a Meaningful Clinical Signal
After a positive herpes test, one of the most persistent fears is that the virus is silently causing harm beneath the surface. Clinically, this fear does not align with how herpes behaves in most people. Across public health guidance and long-term studies, the absence of symptoms is not viewed as a neutral finding. It is viewed as a reassuring one [1], [2].
In medicine, symptoms exist for a reason. They are signals of inflammation, tissue involvement, or immune disruption. When herpes does not produce symptoms, it usually indicates that the virus is being effectively contained and is not interfering with normal bodily function [1].
What “Low Clinical Risk” Actually Means
Low clinical risk does not mean zero risk, and it does not mean herpes is irrelevant. It means that the likelihood of complications, progression, or health impairment is low in people who remain asymptomatic [2], [13].
From a clinician’s perspective, risk is defined by outcomes that require intervention. These include recurrent painful outbreaks, secondary infections, or significant quality-of-life disruption. In individuals without symptoms, these outcomes are uncommon, which is why medical guidelines do not recommend routine treatment or monitoring in asymptomatic cases [1], [2].
Long-Term Data Supports Stability, Not Progression
Longitudinal studies following people with herpes over many years show a consistent pattern. Even among those who initially experience symptoms, viral activity and clinical impact often decrease over time. For individuals who never develop symptoms, progression to frequent or severe disease is even less likely [9].
This pattern is important for you as a patient. It means that being symptom-free is not a temporary calm before inevitable worsening. For many people, it is the long-term state [9], [13].
Why Complications Are Rare Without Symptoms
Complications from herpes are typically linked to active disease, not silent infection. When the virus causes lesions or inflammation, there is a pathway for discomfort, secondary infection, or distress. When those processes never occur, the biological mechanisms for complications are largely absent [1], [13].
From a public health standpoint, this is why asymptomatic herpes is not treated as a progressive condition. The virus may be present, but without disease expression, it does not usually pose a threat to overall health [2].
Interpreting Risk Without Catastrophizing
It is natural to imagine worst-case scenarios after a positive test. However, medical risk assessment does not operate on fear. It operates on observed outcomes. Decades of clinical observation support the conclusion that people without symptoms generally remain low risk and stable [1], [9].
For you, this means that feeling well is meaningful information. For clinicians, it means reassurance rather than escalation. And for health systems, it explains why asymptomatic herpes is approached conservatively, without aggressive intervention [2], [13].
A Clinically Grounded Reframe
When symptoms are absent, herpes is typically a background finding rather than a clinical problem. This does not minimize the diagnosis. It contextualizes it. The absence of symptoms is not something to wait anxiously to lose. It is evidence that your body is managing the virus effectively [1], [2], [9], [13].
Understanding this distinction allows you to move away from constant vigilance and toward a more accurate view of your health. In clinical terms, no symptoms usually means low risk, not hidden danger.
Addressing the Fear: “Is Something Wrong With Me?”
Why This Fear Is So Common After a Positive Test
After testing positive for herpes, especially when you have no symptoms, a deeply personal fear often surfaces: Is there something wrong with me? This reaction is not a sign of weakness or overthinking. It is a predictable psychological response shaped by stigma, incomplete public information, and the way herpes is discussed in society rather than how it actually behaves medically [1], [2].
You are not reacting to illness. You are reacting to meaning. The word “positive” carries emotional weight, and when it is paired with a condition that is socially misunderstood, the mind naturally searches for explanations that turn inward.
Separating Biology From Self-Blame
From a medical standpoint, there is no evidence that being asymptomatic reflects a flaw, deficiency, or hidden problem in your body. On the contrary, public health guidance consistently frames asymptomatic herpes as a common and expected biological outcome [1].
If something were truly wrong, medicine would expect to see signs: pain, lesions, inflammation, or functional impairment. When those are absent, clinicians interpret the situation as stable, not suspicious. The virus is present, but it is not expressing itself in a way that causes harm [2].
For healthcare providers, this distinction is routine. For patients, it often needs to be stated clearly: absence of symptoms is not a red flag.
How Stigma Distorts Self-Perception
Herpes carries a unique social stigma that few other common viral infections do. This stigma creates the illusion that a positive test says something about your character, your past, or your worth. Public health organizations actively work to counter this narrative because it causes real psychological harm [1], [2].
Millions of people carry herpes antibodies without knowing it. They live normal lives, form relationships, and remain healthy. The difference between them and someone who feels distressed after a test is not biology. It is awareness combined with stigma [1].
Reframing What Your Body Is Actually Doing
If you are asymptomatic, your body is not failing you. It is doing exactly what it is designed to do: recognize a virus, control it, and prevent disease. From an immunological perspective, this is a success, not a problem [1].
For clinicians, asymptomatic carriage is often interpreted as effective immune containment. For you, understanding this can shift the narrative from suspicion to reassurance. Your body is not quietly breaking down. It is quietly maintaining balance [2].
Why Public Health Emphasizes Normalization
Public health guidance deliberately emphasizes normalization of asymptomatic herpes because fear and self-stigma lead to more harm than the virus itself in most cases. Anxiety, shame, and isolation are well-documented consequences of misinterpreting a positive test [1].
That is why authoritative sources stress that herpes is common, often silent, and usually manageable without disrupting health or identity. This messaging is not designed to dismiss concerns. It is designed to protect mental well-being and prevent unnecessary distress [2].
A Healthier Question to Ask
Instead of asking Is something wrong with me?, a more medically grounded question is Is there any evidence that this is affecting my health right now? For asymptomatic individuals, the answer is usually no [1], [2].
For you, this reframing can be liberating. For clinicians, it aligns with evidence-based practice. And for society, it helps move the conversation away from blame and toward understanding.
Nothing about an asymptomatic herpes result suggests that you are broken, damaged, or abnormal. It suggests that you are part of a very large group of people whose bodies are managing a common virus quietly and effectively [1], [2].
What You Should Not Do After a Positive Test
Do Not Assume the Test Is a Diagnosis of Disease
One of the most common mistakes after a positive herpes blood test is treating the result as a diagnosis of active illness. You may feel compelled to immediately redefine your health status or future based on a single laboratory number. Clinically, this is not how herpes testing is meant to be interpreted. In asymptomatic individuals, a positive antibody result confirms exposure, not disease [3], [12].
For clinicians, disease is defined by symptoms and clinical findings, not by antibodies alone. For you as a patient, assuming illness where there is none often leads to unnecessary fear rather than better health decisions [3].
Do Not Panic and Retest Repeatedly
It is natural to want certainty, especially when anxiety is high. Many people respond to a positive result by repeating blood tests in the hope that the answer will change or become clearer. Medical guidance strongly discourages this approach in asymptomatic individuals [3].
Repeated testing rarely provides new or useful information. Antibody levels can fluctuate slightly, but those changes do not correlate with health risk, disease activity, or future outcomes. Instead of reassurance, repeated testing often reinforces anxiety and fixation on numbers that lack clinical meaning [12].
Do Not Over-Interpret IgG Levels
Another common reaction is focusing on the numerical value of the IgG result and trying to interpret its significance. Higher numbers are often assumed to mean worse infection, greater contagiousness, or increased risk. From a medical standpoint, this interpretation is incorrect [12].
IgG levels are not a measure of disease severity or viral activity. They simply reflect immune recognition. Clinicians do not use IgG values to predict outbreaks, transmission, or long-term health outcomes in asymptomatic patients [3].
Do Not Let the Result Redefine Your Identity or Health
A positive test result can quickly take on emotional weight and begin to shape how you see yourself. You may feel compelled to disclose prematurely, withdraw socially, or assume lifelong limitation. Public health guidance emphasizes that this psychological response often causes more harm than the virus itself [3].
If you find yourself searching for deeper explanations about what a positive test truly means, how latency works, and why medicine often labels herpes as lifelong despite many people remaining symptom-free, it can help to explore a more complete, structured explanation of the topic.
You can read a detailed, evidence-based discussion here: https://panaceayur.com/can-herpes-be-cured-permanently-real-cure-approach/
This is not about taking action. It is about understanding the broader medical framework so that fear does not fill the gaps left by a lab report.
Do Not Make Major Decisions Without Clinical Context
Some people respond to a positive test by making abrupt decisions, ending relationships, avoiding intimacy indefinitely, or seeking aggressive interventions without medical indication. These actions are usually driven by fear rather than evidence [3].
Healthcare guidelines emphasize that decisions about testing, monitoring, or treatment should be guided by symptoms and clinical context, not by serology alone. If you have no symptoms, most major medical actions are unnecessary [12].
What Clinicians Advise Instead
From a clinician’s point of view, the most appropriate response to an asymptomatic positive test is perspective, not escalation. This means understanding what the test can and cannot tell you, monitoring your health normally, and seeking medical advice only if symptoms appear [3].
For you, this approach protects both physical and mental well-being. It prevents unnecessary medicalization and allows you to interpret the result accurately rather than catastrophically [12].
A positive herpes blood test without symptoms is information, not an emergency. What you choose not to do after receiving that information is often just as important as what you choose to do [3], [12].
When a Positive Test Actually Matters Clinically
Symptoms Change the Clinical Meaning of a Test
A positive herpes blood test carries very different weight depending on whether symptoms are present. Clinically, herpes status matters most when there are visible lesions, pain, or other signs that suggest active disease. In those situations, testing helps confirm the cause of symptoms and guides appropriate management [2], [13].
If you have no symptoms, the same test result usually does not trigger medical action. This is not because herpes is ignored, but because antibody positivity alone does not indicate disease, severity, or the need for treatment [2].
Situations Where Clinical Attention Is Warranted
From a guideline-based perspective, there are specific scenarios where herpes status becomes clinically relevant. These include the appearance of new genital or oral lesions, unexplained recurrent pain in typical herpes distribution areas, or symptoms that suggest a first clinical episode [13].
In these cases, clinicians focus on symptom evaluation, physical examination, and when appropriate, direct testing of lesions. Blood test results may provide background context, but they are not the primary diagnostic tool [2].
Pregnancy and Immunocompromised States
There are also special circumstances where herpes status may warrant closer attention even in the absence of classic symptoms. Pregnancy is one such situation, particularly near delivery, where active genital lesions carry specific clinical implications [2].
Similarly, individuals with significantly weakened immune systems may be monitored more closely if symptoms appear. Even then, clinical decision-making is driven by signs of active disease rather than antibody status alone [13].
Why Asymptomatic Positivity Usually Does Not Change Care
For asymptomatic individuals, clinical guidelines consistently emphasize that a positive blood test rarely changes management. There is no evidence that treating or monitoring asymptomatic herpes improves outcomes, reduces complications, or prevents future disease [2].
From a clinician’s perspective, acting on antibody status without symptoms can lead to unnecessary treatment, anxiety, and medicalization. This is why guidelines are deliberately conservative in defining when herpes status truly matters [13].
How Doctors Use This Information in Practice
In real-world clinical practice, doctors assess the whole patient, not a single test result. They ask whether herpes is causing a problem that needs solving right now. If the answer is no, the test result becomes background information rather than a diagnosis [2].
For you, this means that a positive test without symptoms is usually not a call to action. For healthcare providers, it reinforces the importance of symptom-driven care. And for public health systems, it explains why herpes screening and intervention are targeted rather than universal [13].
A Clear Clinical Boundary
Understanding when a positive herpes test actually matters helps reduce unnecessary fear. It draws a clear boundary between information and illness. Clinically, herpes status matters when there is disease to treat or risk to manage. When symptoms are absent, that boundary has usually not been crossed [2], [13].
This distinction allows both patients and clinicians to respond proportionately, focusing attention where it is needed and avoiding intervention where it is not.
Modern Virology-Latency and Host Control Come First
In modern virology, long-term viral silence is explained through the concepts of latency and immune containment. After initial exposure, herpes simplex virus enters a dormant state within nerve cells, where it remains present but largely inactive. The immune system continuously monitors this state, preventing viral gene expression from escalating into clinical disease [8], [11].
From a biomedical perspective, this balance is considered stable and healthy. The virus is not eradicated, but it is functionally suppressed. Disease occurs only when this balance is disrupted. For many individuals, that disruption never happens, which is why long-term silence is a common outcome rather than a rare exception [8].
This framework places the emphasis not on the virus alone, but on the relationship between the virus and the host. The same virus can exist in two people and behave very differently depending on how the internal biological environment regulates it [11].
A Conceptual Parallel in Ayurveda
Some traditional medical systems describe this same phenomenon using different language and conceptual models. In Ayurveda, long-term health is understood less in terms of eliminating every pathogen and more in terms of maintaining internal balance and resilience. When balance is preserved, disease does not manifest, even if potential causes are present [14].
This does not contradict modern virology. It mirrors it conceptually. Where virology speaks of immune surveillance and latency, Ayurveda speaks of internal regulation and stability. Both systems recognize that the presence of a pathogen does not automatically result in disease. Expression depends on the host environment [8], [14].
Host Environment as the Deciding Factor
Across both frameworks, the deciding factor is not exposure, but response. Modern medicine explains this through immune regulation, cellular signaling, and viral gene suppression. Ayurveda explains it through systemic balance and the body’s capacity to prevent disturbance from manifesting as illness [11], [14].
For you as a reader, this parallel matters because it reframes the meaning of viral silence. Silence is not denial or avoidance. It is an active state of regulation. Whether described through immunology or traditional medical philosophy, the conclusion is the same: disease requires more than presence alone [8].
Why This Perspective Is Introduced Here
This section is not about treatment, intervention, or cure. It exists to provide a broader explanatory lens for readers who struggle to reconcile how a virus can be present yet cause no harm. Both modern virology and traditional medical systems acknowledge this reality, even if they describe it differently [11], [14].
Understanding this parallel helps reduce fear and confusion. It reinforces the idea that long-term viral silence is biologically plausible, medically recognized, and widely observed. Whether explained through contemporary science or traditional frameworks, the message remains consistent: presence does not equal disease [8], [11], [14].
By placing this perspective after modern scientific explanations, the goal is not to replace one system with another, but to show that different medical traditions have arrived at similar observations about how the human body maintains health in the presence of viruses.
Living Normally With a Positive Test Result
A Positive Test Does Not Redefine Daily Life
After the initial shock of a positive herpes test, many people quietly worry that their life is about to change in fundamental ways. Clinically and from a public health perspective, this fear is usually unfounded. The overwhelming consensus is that most people who test positive for HSV, especially those without symptoms, continue to live normal, healthy lives without physical deterioration or progressive illness [1], [2].
For healthcare systems, herpes is categorized as a common viral condition that rarely interferes with overall functioning in asymptomatic individuals. For you, this means that work, exercise, relationships, and long-term health plans typically remain unchanged [10].
What “Normal” Means in Medical Terms
In medicine, living normally does not mean ignoring health information. It means that no special restrictions, treatments, or ongoing monitoring are required in the absence of symptoms. Public health guidance does not recommend lifestyle limitations, routine medical interventions, or constant vigilance for people who are symptom-free [1], [2].
From a clinician’s perspective, if herpes is not causing pain, lesions, or functional impairment, it is not interfering with health. The virus exists in the background, controlled and clinically quiet [10].
Relationships, Work, and Long-Term Outlook
Many people fear that a positive test will affect their ability to form relationships, maintain intimacy, or plan a future. Public health organizations explicitly acknowledge that most people with herpes, diagnosed or undiagnosed, form partnerships, have families, and live full lives [1].
For asymptomatic individuals, there is no evidence that herpes gradually erodes health or limits longevity. Long-term population data support stability rather than decline [2], [10].
Avoiding Over-Medicalization
One of the biggest risks after a positive test is not physical harm, but over-medicalization. When a condition that is clinically silent becomes a source of constant monitoring or anxiety, quality of life can suffer unnecessarily [1].
Healthcare guidelines are designed to prevent this. By emphasizing symptom-based care and discouraging unnecessary interventions, public health systems aim to protect both physical and mental well-being [2].
Reclaiming a Balanced Perspective
For you, living normally with a positive test result means allowing the test to inform understanding, not dominate identity. It means recognizing that many people around you carry herpes antibodies without ever knowing it, without changing how they live, and without experiencing health consequences [10].
For clinicians, this section reinforces why reassurance is often the most appropriate response. For public health, it reflects a consistent message: herpes is common, often silent, and usually compatible with a normal life [1], [2].
A Grounded Takeaway
A positive herpes test without symptoms is not a forecast of decline. It is a piece of information that sits alongside countless other biological facts about the body. When symptoms are absent, normal life is not something you are waiting to return to. It is something you are already living [1], [2], [10].
Doctor Profile
Dr. Arjun Kumar is an Ayurvedic physician and medical researcher with a focused interest in chronic viral conditions, immune regulation, and integrative health education. His work centers on helping patients and readers understand complex medical diagnoses through clear, evidence-based explanations that reduce fear and misinformation.
With extensive experience studying herpes simplex virus, viral latency, and asymptomatic infection patterns, Dr. Kumar emphasizes a patient-first, interpretation-focused approach to medical information. Rather than relying on alarmist language or oversimplified conclusions, his writing aims to explain how viruses behave in the human body, how immune systems maintain control, and why many people remain healthy despite positive test results.
Dr. Kumar’s work draws on public health guidance from organizations such as the CDC, NHS, WHO, and peer-reviewed medical literature, alongside classical Ayurvedic frameworks used strictly for conceptual understanding, not replacement of modern diagnosis. This dual perspective allows him to bridge modern virology with traditional models of host resilience in a way that is educational, transparent, and clinically responsible.
He is the author of Herpes Cure: A Research-Backed Guide to Healing Through Herbal Medicine and has published educational material aimed at reducing stigma, correcting diagnostic misunderstandings, and helping patients make informed, calm decisions after receiving unexpected test results.
Dr. Kumar’s approach aligns with current medical guidelines that prioritize symptom-based care, psychological well-being, and avoidance of unnecessary medicalization. His content is written for global audiences, particularly readers in the United States and United Kingdom, and follows Google Search Quality Guidelines for health and medical topics.
FAQs
Is it normal to test positive for herpes but have no symptoms?
Yes. It is very common to test positive for herpes antibodies and never develop symptoms. Public health data show that most people with herpes remain asymptomatic throughout their lives, meaning the virus stays silent and does not cause illness.
Does a positive herpes blood test mean I am sick?
No. A positive herpes blood test indicates past exposure and immune response, not active disease. Without symptoms such as sores or pain, doctors do not consider this a diagnosis of illness.
Can herpes stay dormant forever?
In many people, herpes remains dormant long term without ever causing symptoms. While reactivation is biologically possible, long-term studies show that most asymptomatic individuals remain stable over time.
Does this mean my immune system is weak?
No. Being asymptomatic usually means your immune system is effectively controlling the virus. Clinically, this is interpreted as immune stability, not weakness.
Should I keep retesting if I have no symptoms?
Routine retesting is not recommended for people without symptoms. Repeat blood tests rarely provide new or useful information and often increase anxiety without improving health outcomes.
Could I have had herpes for years without knowing?
Yes. Herpes antibodies can remain detectable for many years after exposure. Many people acquire herpes long before testing and never realize it because symptoms never appear.
Why don’t doctors routinely test everyone for herpes?
Medical guidelines advise against routine herpes screening in asymptomatic individuals because it does not improve outcomes and often causes unnecessary psychological distress.
Does being asymptomatic mean I will eventually get symptoms?
Not necessarily. Many people who remain symptom-free early on continue to remain symptom-free long term. Absence of symptoms is generally considered a reassuring sign.
Do I need treatment if I have no symptoms?
In most cases, no. Treatment decisions are guided by symptoms, not antibody status alone. Asymptomatic individuals usually do not require medical intervention.
Can I live a normal life after testing positive?
Yes. Most people with herpes, especially those without symptoms, live normal, healthy lives without physical limitations or long-term health problems related to the virus.
References
[1] Centers for Disease Control and Prevention. (2024). Genital herpes – CDC fact sheet.
https://www.cdc.gov/std/herpes
Brief: This CDC resource explains how common herpes is, clarifies that many infected people never develop symptoms, and emphasizes that a positive test does not automatically mean active disease. It supports reassurance throughout the introduction, prevalence, and low-risk sections.
[2] National Health Service. (2023). Genital herpes.
https://www.nhs.uk/conditions/genital-herpes
Brief: NHS guidance confirms that many people carry herpes without symptoms and that outbreaks are not inevitable. It supports sections on asymptomatic infection, low clinical risk, and why routine testing is not always recommended.
[3] U.S. Preventive Services Task Force. (2016). Serologic screening for genital herpes infection: Recommendation statement. JAMA, 316(23), 2525–2530.
https://jamanetwork.com/journals/jama/fullarticle/2584054
Brief: This guideline explains why routine herpes blood testing is discouraged in people without symptoms due to anxiety, false positives, and lack of clinical benefit. It directly supports the section on why doctors rarely test without symptoms.
[4] Ashley-Morrow, R., Krantz, E., & Wald, A. (2003). Time course of seroconversion by herpes simplex virus type 2 serologic assays. Clinical Infectious Diseases, 36(5), 588–593.
https://academic.oup.com/cid/article/36/5/588/327019
Brief: This study explains what herpes IgG antibodies represent and why a positive blood test reflects immune memory rather than current viral activity. It supports the section on what blood tests actually detect.
[5] Wald, A., & Corey, L. (2007). Persistence in the population: Epidemiology, transmission. Journal of Infectious Diseases, 196(Suppl 2), S123–S130.
https://academic.oup.com/jid/article/196/Supplement_2/S123/836956
Brief: This paper explains herpes latency, asymptomatic carriage, and why most transmission and persistence occur without visible disease. It supports sections on viral silence and immune containment.
[6] Looker, K. J., et al. (2015). Global and regional estimates of prevalent and incident herpes simplex virus type 1 infections. PLOS ONE, 10(10), e0140765.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0140765
Brief: This global epidemiology study shows how widespread HSV-1 infection is and how often it remains asymptomatic. It supports normalization and prevalence sections.
[7] Looker, K. J., et al. (2018). Global and regional estimates of HSV-2 infection. PLOS ONE, 13(2), e0192081.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0192081
Brief: This paper demonstrates that HSV-2 infection is common worldwide and frequently unrecognized due to lack of symptoms. It supports reassurance and low-risk framing.
[8] Johnston, C., & Wald, A. (2016). Herpes simplex virus infections. New England Journal of Medicine, 375, 666–674.
https://www.nejm.org/doi/full/10.1056/NEJMra1600617
Brief: This authoritative review explains herpes latency, immune control, and why many infected individuals never experience clinical disease. It supports sections on latency and immune balance.
[9] Benedetti, J. K., Zeh, J., & Corey, L. (1994). Clinical reactivation of genital herpes simplex virus infection decreases in frequency over time. Annals of Internal Medicine, 121(11), 847–854.
https://pubmed.ncbi.nlm.nih.gov/7978697
Brief: This study shows that even among symptomatic individuals, herpes activity often decreases over time, supporting reassurance about long-term outlook.
[10] World Health Organization. (2022). Herpes simplex virus.
https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus
Brief: WHO confirms that most HSV infections are asymptomatic or mild and that many people are unaware they carry the virus. It supports the global, non-alarmist framing.
[11] Cohen, J. I. (2020). Herpesvirus latency. Journal of Clinical Investigation, 130(7), 3361–3369.
https://www.jci.org/articles/view/137066
Brief: This review explains how herpesviruses establish lifelong latency without causing disease in most hosts, supporting the biological explanation of viral silence.
[12] LeGoff, J., & Péré, H. (2020). Diagnosis of genital herpes simplex virus infection. Journal of Clinical Microbiology, 58(6), e00576-19.
https://journals.asm.org/doi/10.1128/JCM.00576-19
Brief: This paper clarifies the limitations of serologic testing and why test results must be interpreted cautiously in asymptomatic individuals.
[13] Patel, R., et al. (2017). European guideline for the management of genital herpes. Journal of the European Academy of Dermatology and Venereology, 31(10), 1704–1716.
https://onlinelibrary.wiley.com/doi/10.1111/jdv.14361
Brief: This guideline emphasizes symptom-based management and supports the idea that absence of symptoms usually indicates low clinical concern.
[14] Charaka Samhita. (Chikitsa Sthana, Rasayana Adhyaya). Traditional Ayurvedic text, standard English translations.
Brief: This classical text introduces the concept of host strength, balance, and resilience rather than pathogen-only focus. It is used only to explain the conceptual Ayurveda bridge, not treatment claims.
Note for readers
Every reference listed here has been carefully selected for accuracy, clinical relevance, and traceability. Public-health guidelines (CDC, NHS, WHO) are used to ensure safety and reassurance, while peer-reviewed studies explain testing, latency, and asymptomatic infection. Ayurvedic references are included only to explain traditional frameworks of health interpretation, not to replace or contradict modern medical guidance.