- Stroke as a Systemic and Progressive Disorder
- Cerebral Circulation and Stroke Pathogenesis
- Types of Stroke
- Risk Factors & Causes
- Early Warning Signs & Symptoms
- Post Stroke Complications
- Less Common but Clinically Important Complications After Stroke
- Autonomic Nervous System Dysfunction
- Sleep Disorders After Stroke
- Sexual Dysfunction
- Orthostatic Hypotension
- Visual and Spatial Neglect
- Central Post Stroke Pain Syndrome
- Long Term Complications if Stroke Is Not Properly Managed
- Recurrent Stroke and Progressive Brain Injury
- Worsening Physical Disability and Dependency
- Cognitive Decline and Vascular Dementia
- Emotional and Psychological Deterioration
- Chronic Pain and Fatigue Syndromes
- Increased Medical Complications and Hospitalizations
- Reduced Quality of Life and Social Isolation
- Common Disorders Associated With Stroke
- Cardiovascular and Vascular Comorbidities
- Rare Disorders Associated With Stroke
- Cerebral Vasculitis
- Why Stroke Recovery Often Slows Down Over Time
- Early Gains Versus Long Term Healing
- Brain Plasticity Has Limits and Conditions
- Ongoing Medical Conditions Interfere With Progress
- Fatigue and Energy Depletion
- Emotional and Cognitive Load
- Reduced Intensity of Rehabilitation Over Time
- Lack of Clear Long Term Guidance
- What This Slowdown Really Means
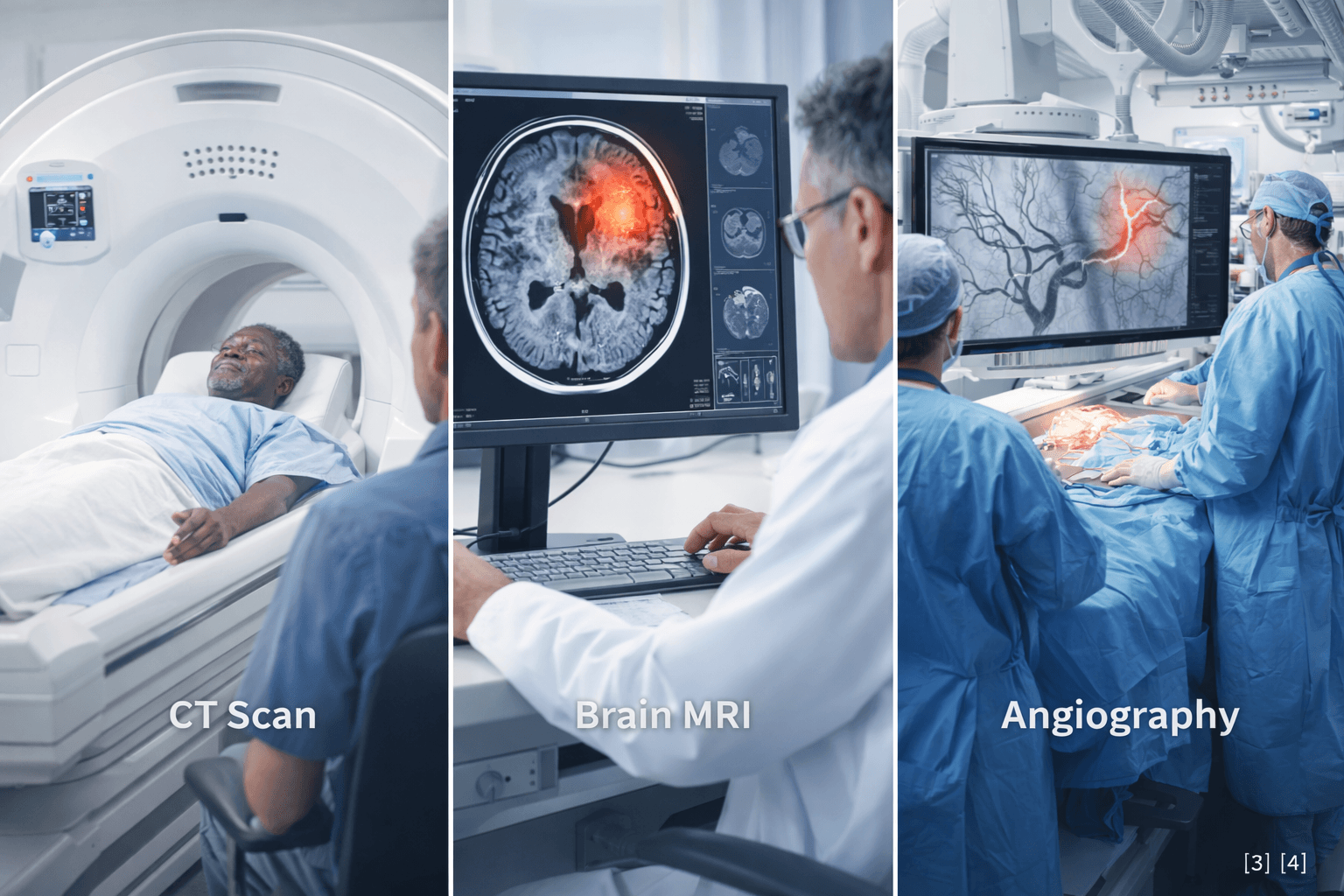
- Modern Diagnostic Framework
- Acute Emergency Care (Supportive Role)
- Limitations of Long Term Conventional Management
- Ayurvedic Understanding of Stroke (Pakshaghata)
- Classical Etiological Factors
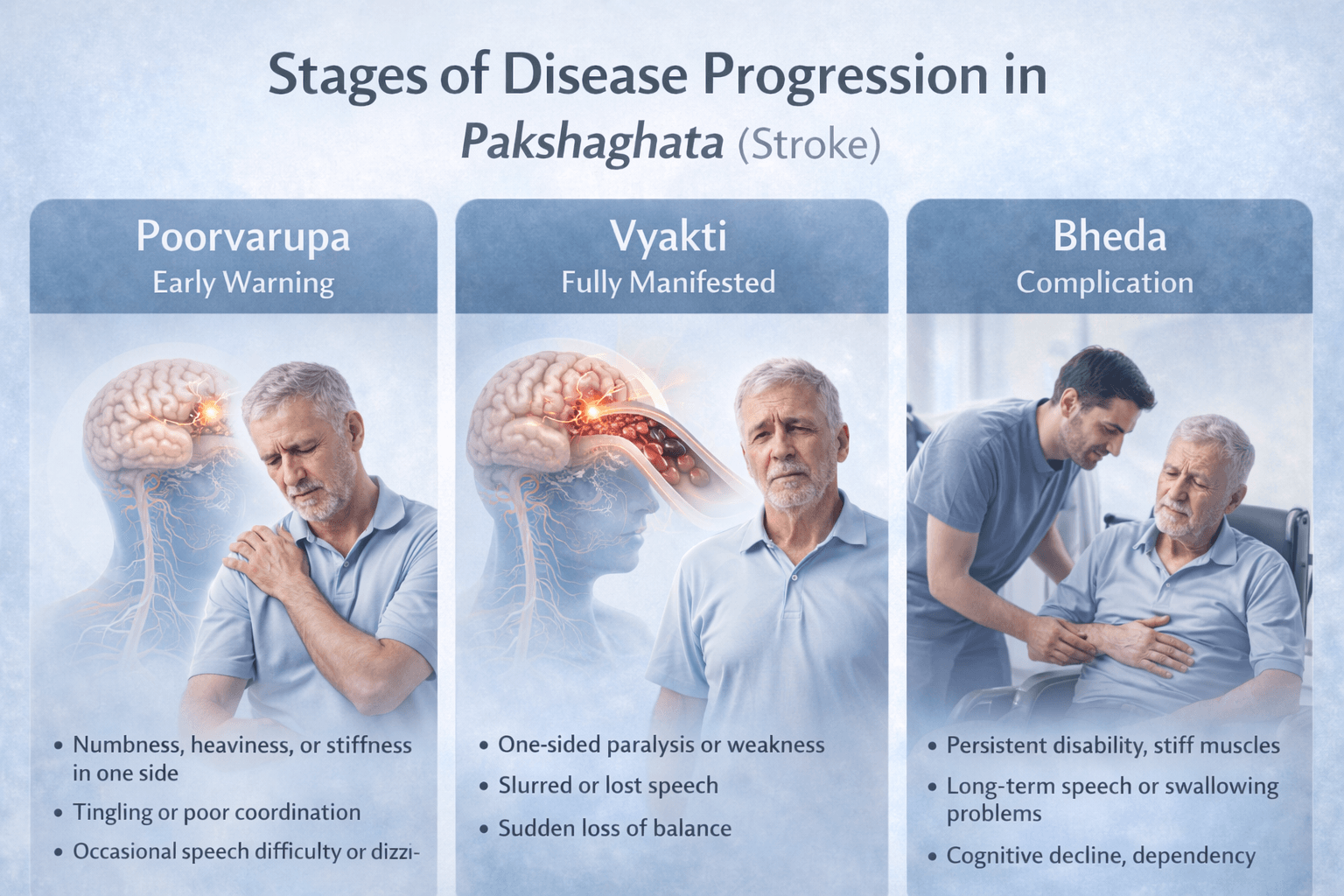
- Stages of Disease (Poorvarupa, Vyakti, Bheda)
- Ayurvedic Diagnostic Approach
- Core Ayurvedic Treatment
- Best Classical Avaleha Medicine for Stroke Cure
- Important Note of Kalyanaka Ghrita Avaleha
- Supportive Internal Medicines
- Recovery and Prognosis
- Stroke Recurrence Prevention
- Frequently Asked Questions
- Case Studies in Ayurvedic Stroke (Pakshaghata) Management
- Author & Medical Credibility
- Evidence and Research Orientation
- Important Medical Safety Disclaimer
- Reference
Stroke is a medical emergency and a leading cause of long-term paralysis and disability worldwide. While modern emergency care has significantly improved survival rates, many patients continue to struggle with weakness, speech impairment, and reduced mobility months or even years after a stroke. Conventional rehabilitation often focuses on functional adaptation rather than neurological regeneration. Ayurveda describes stroke under the condition Pakshaghata, a disorder caused by severe Vata imbalance, impaired circulation, and degeneration of nerve tissues. From this perspective, recovery emphasizes long-term nerve nourishment, tissue regeneration, and recurrence prevention rather than symptom suppression alone.[1].
From a global health perspective, the burden of stroke continues to rise at an alarming pace. Increasing life expectancy, sedentary lifestyle, chronic psychological stress, hypertension, diabetes, obesity, and dietary excesses have significantly contributed to this trend. Stroke is no longer confined to the elderly. Younger adults are increasingly affected, often without prior warning, which makes awareness, early identification, and prevention critically important [2]. When a person experiences a stroke, it is often accompanied by fear of paralysis, loss of independence, and permanent disability. These fears stem largely from the belief that stroke damage is irreversible and that recovery is limited to long term management rather than true healing.
Stroke as a Systemic and Progressive Disorder
From a clinical viewpoint, the brain is extremely sensitive to disruptions in oxygen and nutrient supply. Even brief interruptions in cerebral circulation can trigger complex cascades of inflammation, oxidative stress, and neuronal injury. From the patient’s perspective, stroke is a life altering event that suddenly transforms physical ability, speech, cognition, and emotional stability. Observed from a broader third person perspective, stroke is not merely a neurological condition but a systemic disorder involving blood vessels, metabolic regulation, immune resilience, and nervous tissue integrity [1].
Ayurveda offers a fundamentally different understanding of this condition. Classical Ayurvedic texts describe stroke under the entity Pakshaghata, categorized among Vata dominant disorders affecting movement, sensation, and neural control. This framework allows the physician to view stroke as the culmination of long standing imbalance in circulation, tissue nourishment, and nervous system regulation rather than an isolated brain accident. By recognizing stroke as a progressive process, Ayurveda creates a therapeutic window for intervention, recovery, and long term protection of brain function [2].
Understanding stroke at this deeper level empowers both physician and patient. It shifts the narrative from helplessness to informed action. When you understand how stroke develops and why the body reaches this critical state, you begin to see that recovery, regeneration, and prevention are realistic goals rather than distant hopes [1], [2].
Cerebral Circulation and Stroke Pathogenesis
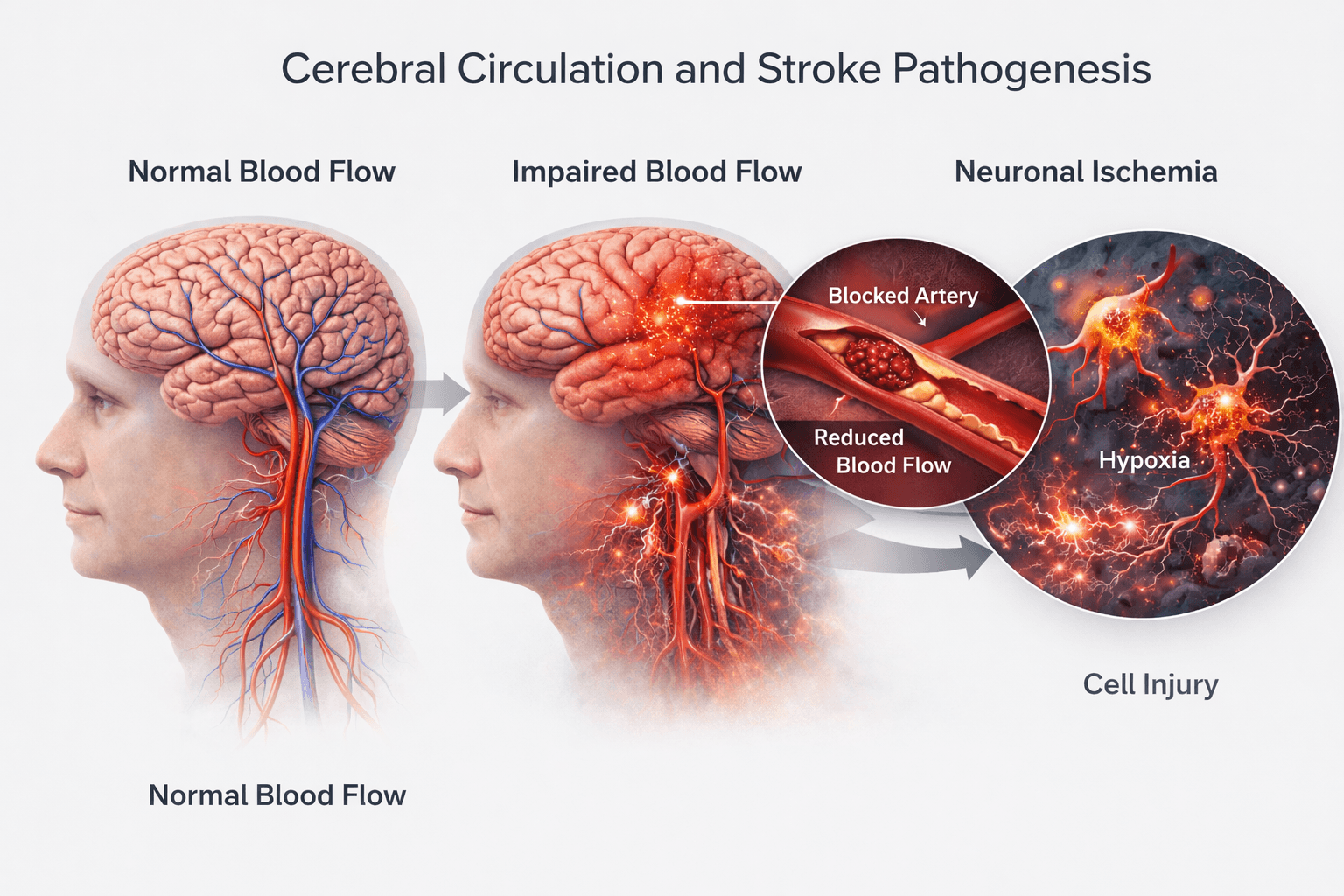
Importance of Cerebral Blood Flow
The brain relies on a continuous and precisely regulated supply of blood to sustain its high metabolic demands. Cerebral circulation delivers oxygen glucose and essential nutrients through a complex arterial and capillary network. From a modern neurological perspective even a brief reduction in cerebral blood flow can result in rapid neuronal dysfunction. You must recognize that neurons have minimal tolerance to oxygen deprivation. When circulation is compromised cellular energy production fails leading to membrane instability edema and progressive neuronal injury [4].
How Circulatory Disruption Leads to Stroke
Stroke pathogenesis begins with disturbance at the vascular level. Narrowed arteries thrombus formation or rupture of weakened vessels interrupt normal perfusion of brain tissue. This initiates a cascade of pathological events including excitatory neurotransmitter overload oxidative stress mitochondrial failure and inflammatory activation. From the patient’s perspective this internal process manifests as sudden weakness speech disturbance facial deviation or paralysis. From the third person clinical viewpoint stroke is a rapidly evolving biological process rather than a single isolated incident [4].
Ayurvedic Interpretation of Cerebral Circulatory Failure
Ayurveda explains cerebral circulation through the unobstructed movement of Rakta and the balanced function of Vata. Classical texts state that when Rakta becomes vitiated and channels known as Srotas become obstructed the normal movement of Vata is impaired. This impaired Vata fails to govern motor and sensory functions leading to Pakshaghata. Sushruta emphasizes that obstruction within channels combined with tissue depletion results in loss of movement and sensation affecting one side of the body [7].
Integrated View of Stroke Pathogenesis
From an integrative perspective cerebral circulatory failure represents Srotorodha at the structural level and Vata Prakopa at the functional level. Ischemia corresponds to impaired Rakta flow while neuronal degeneration reflects Majja Dhatu Kshaya. When viewed from a third person analytical lens stroke pathogenesis emerges as the convergence of vascular obstruction tissue degeneration and regulatory imbalance. This explains why restoring blood flow alone does not always result in full recovery and why long term neurological repair requires deeper tissue nourishment and functional restoration [4], [7].
Types of Stroke
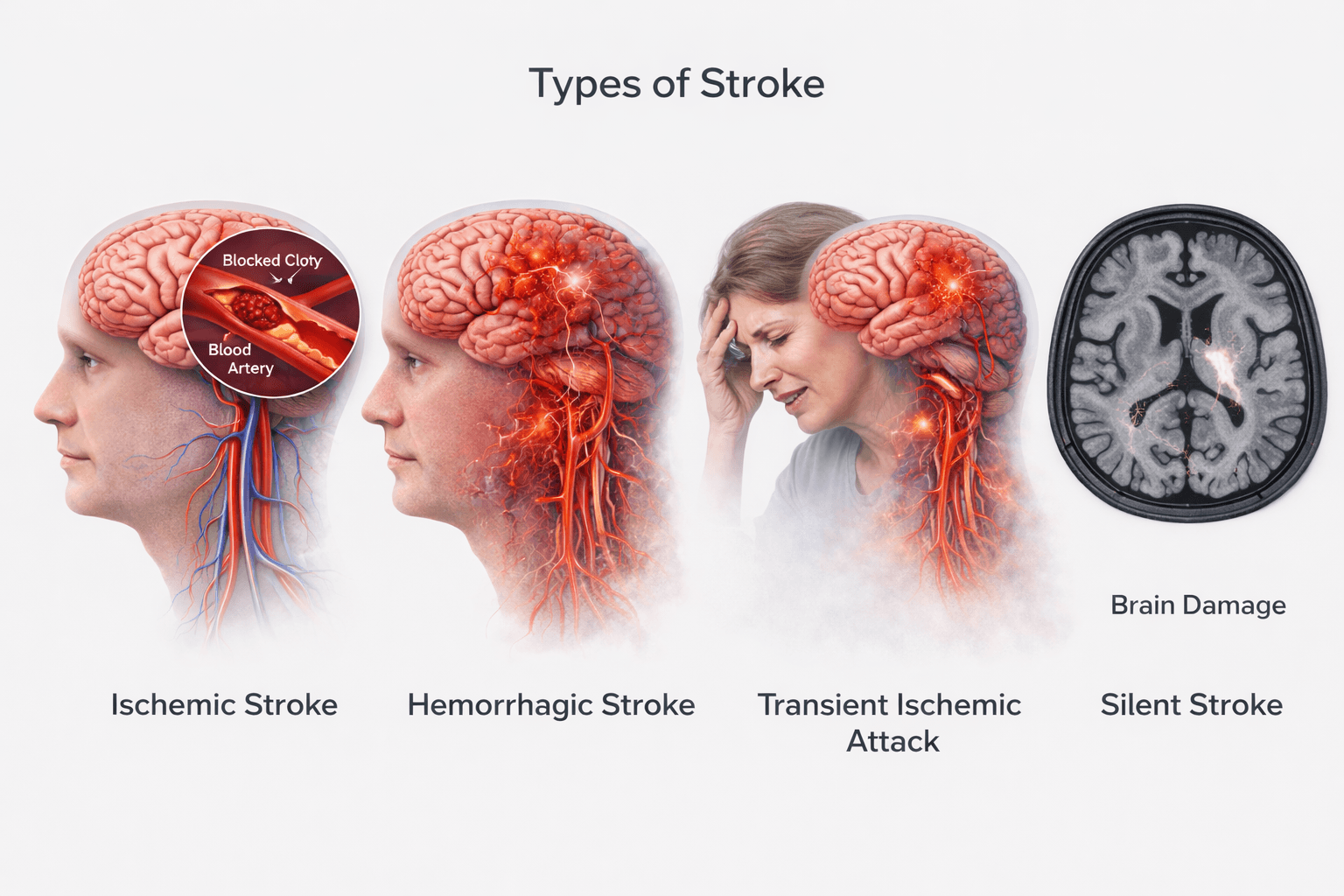
Ischemic Stroke
Ischemic stroke is the most common form of stroke and occurs when blood flow to a part of the brain is reduced or completely blocked. This blockage is usually caused by a thrombus forming within a cerebral artery or an embolus traveling from another part of the body such as the heart or major blood vessels. When blood supply is interrupted neurons are deprived of oxygen and glucose leading to rapid cellular dysfunction and death. From a clinical standpoint ischemic stroke explains the majority of sudden paralysis speech loss and sensory deficits seen in patients worldwide [1], [3].
From the patient’s experience ischemic stroke often presents suddenly yet its origins are typically silent and progressive. Long standing hypertension diabetes dyslipidemia and vascular inflammation gradually narrow arteries until a critical threshold is crossed. From a third person neurological perspective ischemic stroke represents a failure of cerebral perfusion resulting in focal brain injury that directly corresponds to the territory supplied by the affected vessel [4].
Hemorrhagic Stroke
Hemorrhagic stroke occurs when a weakened blood vessel ruptures and bleeding occurs within or around the brain. This bleeding increases intracranial pressure compresses surrounding brain tissue and disrupts normal neuronal signaling. Common causes include uncontrolled hypertension aneurysms and vascular malformations. Although less common than ischemic stroke hemorrhagic stroke is often more severe and carries a higher immediate mortality risk [1], [3].
From a physiological viewpoint hemorrhagic stroke damages the brain through both mechanical compression and toxic effects of blood components on neural tissue. From the patient’s perspective it may present with a sudden severe headache loss of consciousness vomiting or rapid neurological decline. Observed from a third person clinical lens hemorrhagic stroke represents acute vascular failure rather than gradual perfusion loss yet it still leads to widespread neuronal injury [4].
Transient Ischemic Attack
Transient ischemic attack is often referred to as a warning stroke. It occurs when cerebral blood flow is temporarily reduced but restored before permanent damage occurs. Symptoms such as weakness speech difficulty or visual disturbance resolve within a short period yet they signal a high risk of future major stroke. Modern neurology considers transient ischemic attack a critical opportunity for early intervention and prevention [1], [3].
From a broader understanding transient ischemic attack reflects reversible ischemia rather than absence of disease. From the patient’s point of view symptoms may seem minor or fleeting leading to neglect. From the third person medical perspective transient ischemic attack is a powerful indicator of underlying vascular pathology and impending cerebral catastrophe if corrective measures are not taken [4].
Silent Stroke
Silent stroke refers to small areas of brain damage caused by reduced blood flow that do not produce obvious immediate symptoms. These strokes are often discovered incidentally on brain imaging yet they accumulate over time leading to cognitive decline memory impairment gait disturbances and increased risk of major stroke. Silent strokes highlight the fact that brain injury can progress quietly without dramatic warning signs [1].
From an integrative viewpoint silent stroke underscores that stroke is not always an acute dramatic event. From the patient’s perspective subtle changes in thinking balance or behavior may go unnoticed. From a third person analytical lens silent stroke represents cumulative microvascular failure and progressive neuronal loss reinforcing the importance of early vascular protection and long term brain health [4].
Risk Factors & Causes
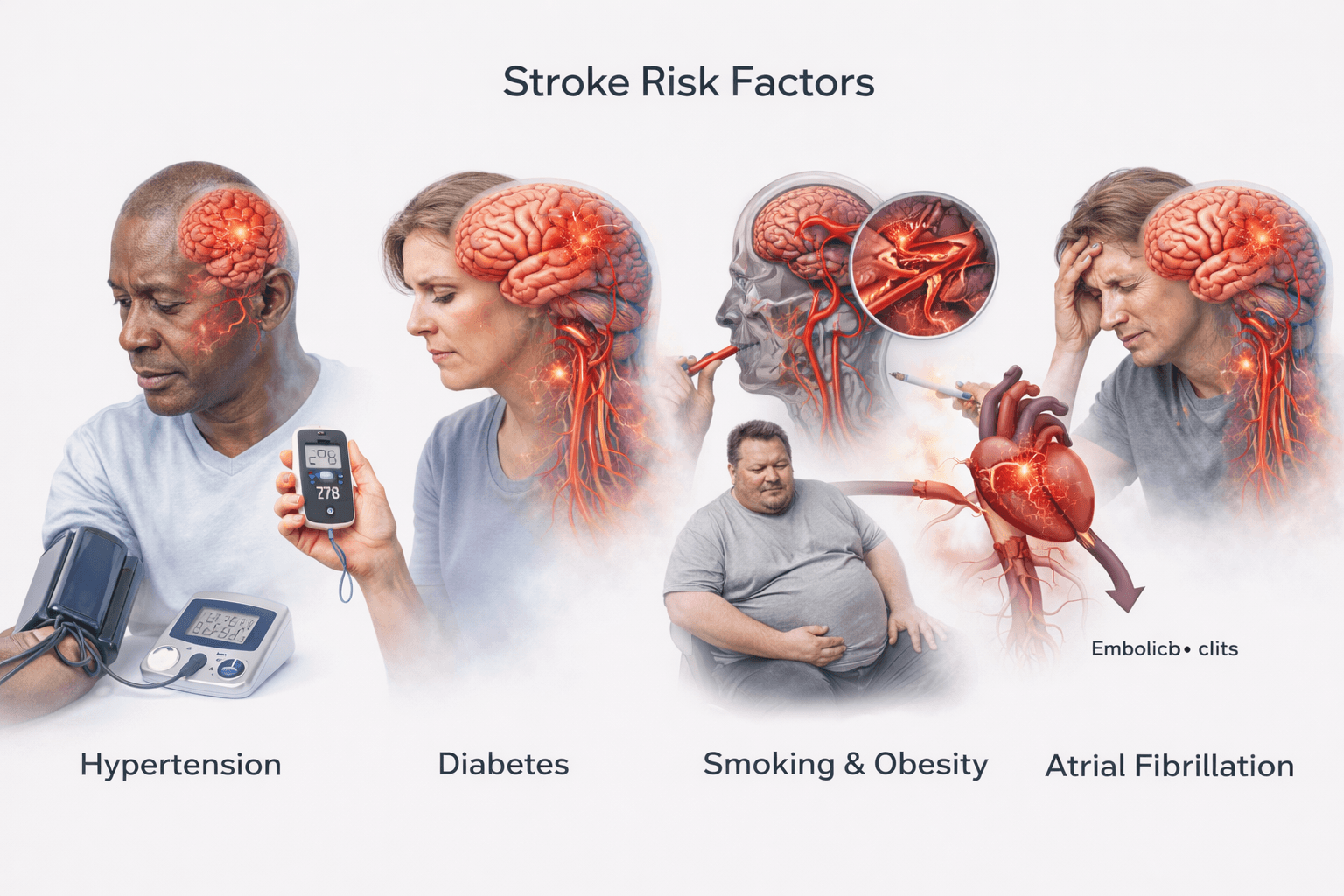
Understanding Why Stroke Develops
Stroke does not occur randomly. In most individuals it develops after prolonged exposure to specific biological lifestyle and systemic risk factors that gradually weaken cerebral circulation and neural resilience. From a modern medical perspective these risk factors damage blood vessels alter blood flow dynamics and promote clot formation. From an Ayurvedic standpoint the same factors disturb Dosha balance vitiate Rakta and obstruct vital channels leading to conditions such as Pakshaghata [1], [5].
What Are Harmful Biological and Lifestyle Influences
Harmful biological and lifestyle influences refer to conditions and habits that continuously place stress on the body’s vascular metabolic and nervous systems, gradually pushing them toward dysfunction. These influences do not cause stroke overnight. Instead they act silently over years, weakening cerebral circulation and reducing the brain’s capacity to tolerate stress and injury [1].
From a biological perspective the most important harmful influences include chronic hypertension diabetes dyslipidemia and cardiac rhythm disorders. Persistent high blood pressure repeatedly injures the inner lining of arteries, making them stiff and prone to narrowing or rupture. Diabetes exposes blood vessels to constant inflammatory and metabolic injury, damaging even the smallest cerebral capillaries. Abnormal lipid levels promote plaque formation inside arteries, slowly restricting blood flow to the brain. Cardiac conditions such as atrial fibrillation create an unstable blood flow pattern, allowing clots to form and travel to cerebral arteries [1].
Lifestyle related influences amplify this biological damage. Long term smoking introduces toxic chemicals that directly injure blood vessels, increase blood thickness, and reduce oxygen delivery to brain tissue. Physical inactivity weakens cardiovascular efficiency and promotes weight gain, which sustains chronic inflammation throughout the body. Excessive alcohol intake disrupts blood pressure regulation, damages the heart, and interferes with cerebral blood flow control. Chronic psychological stress keeps the nervous system in a constant state of overactivation, raising blood pressure, disturbing heart rhythm, and impairing normal vascular repair mechanisms [1].
Ayurveda explains these same influences through functional imbalance rather than isolated disease labels. Irregular eating habits, poor sleep, excessive mental strain, suppression of natural urges, and lack of daily routine disturb Dosha balance, particularly Vata and Pitta. Over time this disturbance vitiates Rakta and weakens its smooth circulation. Channels known as Srotas become obstructed, a process described as Srotorodha. As nourishment to tissues declines, especially Majja Dhatu, the nervous system loses stability and resilience, creating the internal environment for Pakshaghata [5].
From a third person analytical viewpoint harmful biological and lifestyle influences represent the cumulative interaction between structural vascular damage described in modern medicine and functional regulatory failure described in Ayurveda. When these influences persist unchecked, the body gradually loses its protective margins, making stroke not an accident but an eventual outcome. Understanding these influences is essential because correcting them early can prevent stroke long before paralysis or neurological loss occurs [1], [5].
Non Modifiable Risk Factors
Certain risk factors cannot be altered yet they significantly influence stroke vulnerability. Advancing age is one of the strongest predictors as vascular elasticity declines and cumulative metabolic stress increases over time. Genetic predisposition also plays an important role as individuals with a family history of stroke often inherit vascular fragility or metabolic tendencies that accelerate disease development. Gender differences are observed as well with higher stroke incidence in older men and higher post stroke disability in women. A previous history of stroke or transient ischemic attack markedly increases the likelihood of future events indicating underlying unresolved vascular pathology [1], [2].
From an Ayurvedic view these factors reflect gradual Dhatu Kshaya and age related Vata dominance which predispose the nervous system to degeneration and circulatory instability [5].
Modifiable Medical Risk Factors
Hypertension is the most significant modifiable risk factor for stroke. Persistently elevated blood pressure damages arterial walls promotes atherosclerosis and increases the risk of both ischemic and hemorrhagic stroke. Diabetes mellitus accelerates vascular injury through chronic inflammation endothelial dysfunction and impaired microcirculation. Dyslipidemia contributes to plaque formation narrowing cerebral arteries and increasing embolic risk. Cardiac conditions such as atrial fibrillation allow clot formation that can travel to the brain and cause sudden arterial blockage [1], [2].
In Ayurvedic terms these conditions represent Rakta Dushti Agni Mandya and Srotorodha which together disrupt normal circulation and tissue nourishment [5].
Lifestyle and Behavioral Risk Factors
Sedentary lifestyle obesity smoking excessive alcohol intake and chronic psychological stress significantly increase stroke risk. Physical inactivity weakens cardiovascular efficiency while obesity worsens metabolic inflammation. Smoking damages blood vessels increases blood viscosity and reduces oxygen delivery to brain tissue. Chronic stress elevates cortisol and sympathetic activity contributing to hypertension endothelial damage and impaired cerebral perfusion [1], [2].
Ayurveda identifies these behaviors as causes of Dosha imbalance particularly Vata and Pitta aggravation leading to instability of circulation and nervous system function [5].
Silent and Overlooked Risk Factors
Sleep disorders including obstructive sleep apnea chronic dehydration prolonged mental strain irregular eating patterns and suppression of natural urges are often overlooked contributors to stroke. These factors subtly impair oxygenation circulation and metabolic balance over time. From a third person analytical lens they explain why stroke may occur even in individuals without obvious disease labels [1], [2].
Classical Ayurvedic texts emphasize that neglect of daily rhythms mental discipline and bodily signals gradually weakens Ojas and creates a fertile ground for severe disorders such as Pakshaghata [5].
Understanding stroke risk factors empowers prevention. When you identify and correct these influences early you reduce not only the likelihood of stroke but also its severity and long term consequences [1], [2], [5].
Early Warning Signs & Symptoms
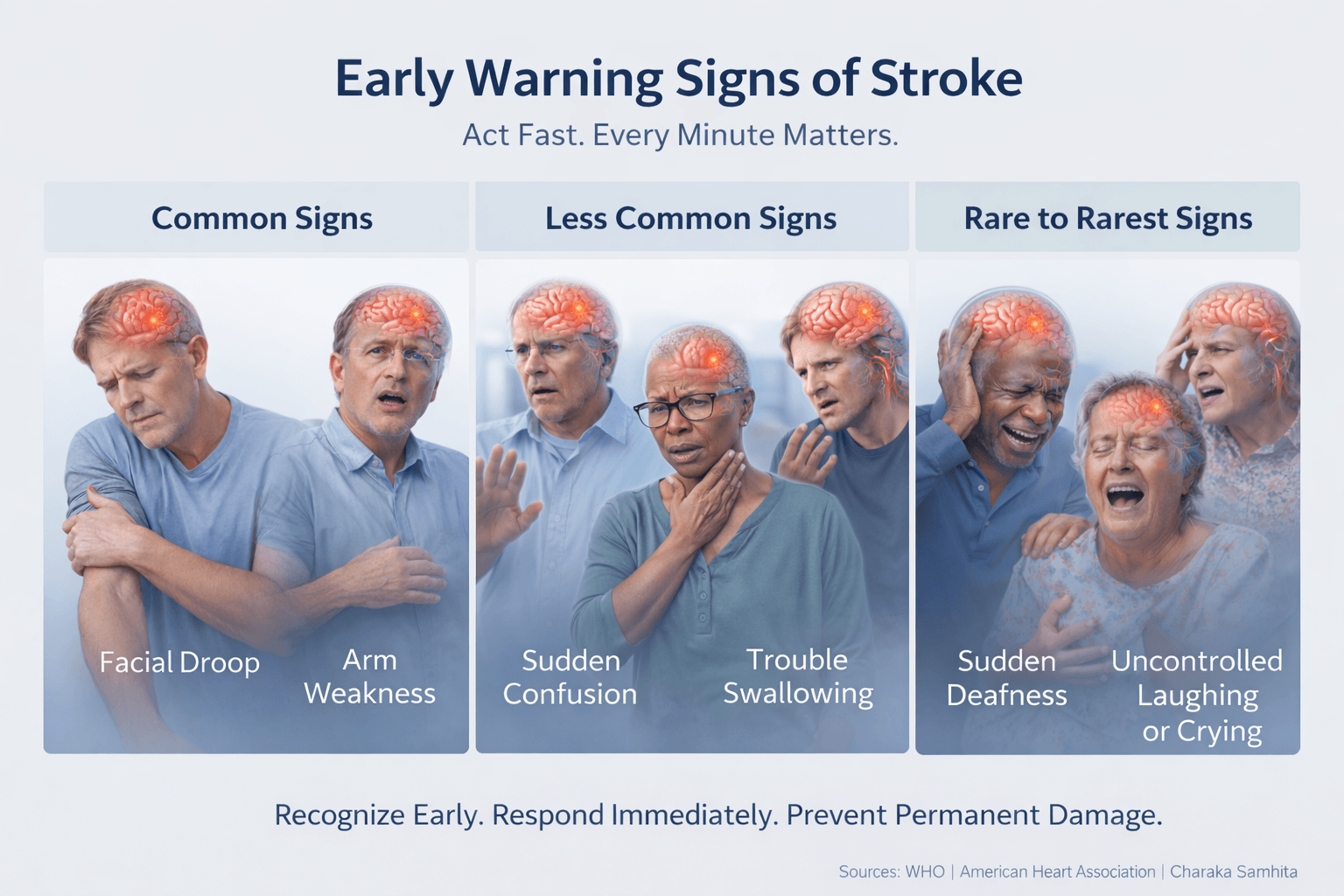
Why Early Warning Signs Must Never Be Ignored
Early warning signs of stroke are the body’s most urgent alarms. They appear when blood flow to the brain falls below a critical level and nerve cells begin to malfunction. For some people these signs are obvious and dramatic. For others they are subtle strange or easily misunderstood. From a medical perspective recognizing these signals early can save brain tissue. From an Ayurvedic view they represent the Poorvarupa stage of Pakshaghata, a phase where imbalance has surfaced but damage may still be limited [1], [6].
As a patient you may question whether the symptom is serious enough to seek help. As a family member you may sense that something is not right even if the person tries to dismiss it. From a third person clinical standpoint no new neurological symptom should ever be ignored because delay directly increases the risk of permanent disability or death [1], [3].
Common Early Warning Signs
Sudden weakness or heaviness on one side of the body is one of the most recognized warning signs. You may struggle to lift an arm hold objects or feel that one leg is not responding properly. Speech difficulty is equally important. You may slur words struggle to form sentences or find it difficult to understand simple speech. Facial drooping where one side of the face appears slack or numb is often noticed by others before the patient realizes it [1], [3].
Vision problems such as sudden blurring double vision or partial vision loss can occur when visual centers are affected. Dizziness loss of balance or difficulty walking may appear when coordination centers lose blood supply. A sudden severe headache unlike any previous headache may signal bleeding inside the brain and requires immediate emergency care [1].
Less Common but Important Warning Signs
Some stroke symptoms are less commonly discussed yet equally serious. Sudden confusion personality change or inappropriate behavior may be mistaken for anxiety or intoxication. You may feel disoriented unable to recognize familiar people or surroundings. From a neurological perspective this reflects involvement of higher cognitive areas of the brain [4].
Sudden difficulty swallowing choking on liquids or unexplained coughing can occur when nerves controlling throat muscles are affected. Ayurveda considers this a sign of disturbed Udana and Prana Vata affecting vital functions [6].
Unexplained nausea vomiting or hiccups that appear suddenly along with neurological changes may indicate brainstem involvement. These symptoms are often overlooked because they resemble gastric problems yet they may be early stroke indicators [3].
Rare and Rare to Rarest Warning Signs
Some stroke warning signs are rare and easily missed yet extremely important. Sudden loss of consciousness without warning may occur especially in hemorrhagic stroke. You may collapse abruptly without pain or prior symptoms. From a third person viewpoint this reflects sudden disruption of vital brain centers [1], [3].
Sudden deafness or ringing in one ear without ear pain is a rare sign linked to impaired blood flow to auditory pathways. Sudden inability to write type or perform learned motor skills despite normal strength is another uncommon but critical sign. This may appear as difficulty signing a name or using everyday tools even though muscles feel intact [4].
In rare cases stroke may present as sudden uncontrollable laughter or crying without emotional reason. This reflects disruption of emotional regulation pathways in the brain and is often misinterpreted as psychological disturbance [3].
Another rare sign is sudden severe neck pain or facial pain especially when associated with visual changes or weakness. This may indicate arterial dissection and requires immediate medical attention [1].
Ayurvedic texts describe such unusual presentations as rapid Vata derangement affecting Marmas and vital centers, warning that atypical symptoms may precede severe neurological collapse [6].
What You Should Do When Any Warning Sign Appears
If you experience any sudden neurological change even if it seems mild strange or temporary you should seek emergency medical care immediately. Do not wait for symptoms to pass. As a caregiver do not attempt home remedies or observation. From a clinical standpoint time lost is brain lost [1], [3].
Early recognition and rapid action dramatically improve outcomes. Both modern medicine and Ayurveda emphasize that responding at the first sign preserves movement speech cognition and independence. Stroke does not always announce itself loudly. Sometimes it whispers. Listening to those whispers can save a life [1], [3], [6].
Post Stroke Complications
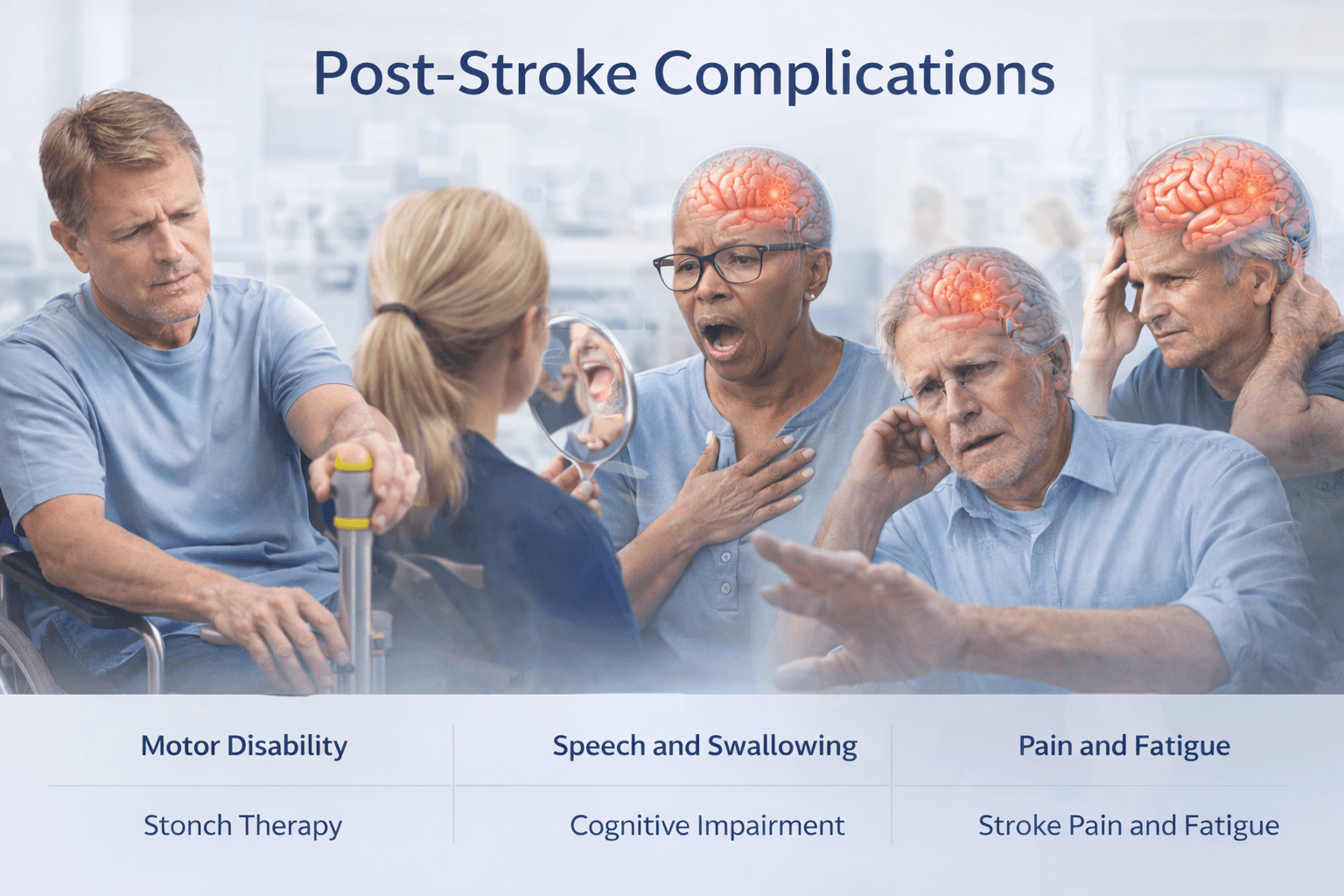
Why Complications Occur After Stroke
Post stroke complications arise because stroke does not affect only a single symptom or function. It disrupts blood supply to specific brain regions that control movement sensation speech cognition emotions and autonomic regulation. When brain tissue is injured neurons lose their ability to communicate effectively and surrounding areas are forced to compensate. From a modern neurological perspective this leads to secondary degeneration inflammation and functional imbalance. From an Ayurvedic standpoint stroke corresponds to Pakshaghata where aggravated Vata combined with Rakta Dushti and Dhatu Kshaya creates long lasting systemic instability [2], [4], [5].
As a patient you may feel that the stroke event is over once the emergency phase passes. As a caregiver you may expect steady improvement. From a third person clinical viewpoint however the post stroke phase is where most disability and suffering actually develops if not addressed properly [2].
Paralysis and Motor Disability
One of the most common complications after stroke is partial or complete paralysis affecting one side of the body. You may experience weakness stiffness heaviness or complete loss of voluntary movement in the arm leg or facial muscles. Over time unused muscles may shrink and joints may become stiff leading to contractures. From a neurological perspective this occurs due to permanent damage to motor pathways and secondary changes in muscle tone [4].
Ayurveda explains this as sustained Vata aggravation with depletion of Mamsa and Majja Dhatu. When nourishment to muscles and nerves is inadequate movement does not return fully even if life is preserved [5].
Speech and Swallowing Difficulties
Many patients develop long term difficulty with speech swallowing or both. You may struggle to pronounce words express thoughts or understand language. Swallowing problems may cause choking coughing or aspiration leading to repeated chest infections. From a medical viewpoint these complications result from injury to speech and cranial nerve control centers [4].
Ayurveda attributes speech impairment to persistent disturbance of Udana Vata while swallowing difficulty reflects combined dysfunction of Prana and Udana Vata. If untreated these issues significantly reduce quality of life [5].
Cognitive Impairment and Memory Problems
Post stroke cognitive complications include memory loss reduced attention difficulty planning tasks and slowed thinking. You may feel mentally exhausted confused or unable to perform tasks that were once simple. From a third person clinical perspective repeated micro damage inflammation and neuronal loss contribute to post stroke cognitive decline and vascular dementia [2], [4].
Ayurveda views these changes as Majja Dhatu Kshaya and reduced Medha resulting from inadequate nourishment of brain tissue due to prolonged Vata imbalance [5].
Emotional and Psychological Changes
Emotional disturbances are often overlooked yet deeply distressing. You may experience depression anxiety irritability sudden crying or emotional numbness. Some patients develop loss of motivation or social withdrawal. From a neurological perspective stroke disrupts emotional regulation pathways and neurotransmitter balance [2].
Ayurveda recognizes these changes as Manovaha Srotas involvement where disturbed Vata affects mental stability and emotional resilience. Without addressing this aspect recovery remains incomplete [5].
Post Stroke Pain and Sensory Disorders
Some individuals develop chronic pain burning sensations numbness or abnormal sensitivity on the affected side. This condition known as central post stroke pain arises from damaged sensory pathways rather than tissue injury. From a medical viewpoint it is difficult to treat and often persistent [4].
Ayurveda explains this as Vata vitiation in sensory channels causing abnormal perception and pain without visible injury [5].
Fatigue Sexual Dysfunction and Autonomic Issues
Persistent fatigue is one of the most common yet least discussed complications. You may feel exhausted even after minimal activity. Sexual dysfunction bladder control issues and bowel irregularities may also occur due to autonomic nervous system involvement. From a third person clinical view these complications reflect widespread regulatory imbalance rather than localized brain injury [2].
Ayurveda correlates these issues with Ojas depletion and imbalance of Vata affecting autonomic functions and vitality [5].
Risk of Recurrent Stroke and Secondary Illness
A major long term complication after stroke is the increased risk of recurrence. Without correction of underlying vascular and metabolic causes the probability of another stroke rises significantly. Infections pressure sores falls and malnutrition are additional secondary complications that may develop during prolonged disability [2].
Ayurveda emphasizes that unless root causes such as Dosha imbalance Rakta Dushti and Agni Mandya are corrected the disease process continues internally even if symptoms appear stable [5].
Why Post Stroke Care Must Go Beyond Survival
Surviving a stroke is only the first step. True recovery involves restoring movement speech cognition emotional stability and independence. From a modern medical viewpoint rehabilitation focuses on compensation and adaptation. From an Ayurvedic perspective the goal is deeper regeneration stabilization of Vata nourishment of Dhatus and prevention of recurrence [2], [4], [5].
When post stroke complications are addressed early and holistically the possibility of meaningful recovery increases and long term suffering can be significantly reduced.
Less Common but Clinically Important Complications After Stroke
Autonomic Nervous System Dysfunction
After a stroke, the part of the nervous system that controls automatic body functions can be affected. I often see patients describe unexplained sweating, unstable blood pressure, abnormal heart rate changes, or sudden dizziness on standing. You may feel that your body no longer responds predictably to simple activities like getting out of bed or eating a meal. Clinically, this is understood as autonomic dysfunction, where brain signals regulating circulation, digestion, and temperature are disrupted. Although it may not look severe at first, it can significantly affect daily comfort, safety, and recovery. Doctors recognize that unmanaged autonomic instability increases fall risk, fatigue, and anxiety. Early recognition helps tailor rehabilitation and medical care more effectively.
Sleep Disorders After Stroke
Sleep problems are surprisingly common after stroke but are often overlooked. Many patients tell me they cannot fall asleep, wake frequently, or feel unrefreshed despite long hours in bed. You might notice excessive daytime sleepiness or worsening fatigue that slows your recovery. From a clinical standpoint, stroke can disrupt sleep regulation centers in the brain or worsen conditions such as sleep apnea. Poor sleep reduces brain healing, weakens concentration, and increases emotional distress. Addressing sleep quality is not optional. It is a critical part of neurological recovery and long term health.
Sexual Dysfunction
Sexual health is rarely discussed openly after stroke, yet it affects many survivors. Some patients feel embarrassed to raise the topic, while partners may feel uncertain or fearful. You may experience reduced desire, erectile difficulties, vaginal dryness, or emotional withdrawal. Clinicians understand that these changes can arise from nerve injury, hormonal shifts, medication effects, or psychological stress. Ignoring sexual health can quietly damage relationships and self esteem. When addressed respectfully, many patients regain confidence and intimacy as part of holistic recovery.
Orthostatic Hypotension
Some stroke survivors feel lightheaded or faint when standing up. I often hear patients describe sudden weakness or blurred vision when rising from a chair or bed. This occurs when blood pressure fails to adjust quickly enough, a condition known as orthostatic hypotension. Clinically, it reflects impaired vascular and nervous system coordination after stroke. If untreated, it increases fall risk and discourages mobility. Identifying this issue allows clinicians to adjust medications, hydration, and rehabilitation strategies safely.
Visual and Spatial Neglect
Stroke can alter how the brain processes visual space, even when eyesight itself is intact. Patients may ignore one side of their body or surroundings without realizing it. You might bump into objects, miss food on one side of the plate, or feel disoriented in familiar spaces. Clinicians refer to this as spatial neglect and recognize it as a major barrier to independence. Early therapy helps retrain awareness and reduce accidents.
Central Post Stroke Pain Syndrome
Some survivors develop persistent pain that does not follow typical muscle or joint patterns. I often hear patients say the pain feels burning, stabbing, or deep and unexplained. This condition arises from altered pain processing in the brain rather than tissue injury. You may feel frustrated when scans appear normal yet pain persists. Clinically, central pain syndromes are challenging but real and require specialized management. Acknowledging the condition is the first step toward relief and improved quality of life.
Long Term Complications if Stroke Is Not Properly Managed
Recurrent Stroke and Progressive Brain Injury
When stroke is not managed carefully over the long term, the risk of another stroke rises significantly. I often meet patients who believed the first event was behind them, only to face a second episode months or years later. You may feel stable on the surface, but underlying vascular stress can continue silently. Clinically, recurrent strokes compound brain injury, leading to greater disability each time. Recovery becomes harder because the brain has fewer healthy pathways left to compensate. Preventing recurrence is therefore not optional. It is the foundation of long term survival and quality of life.
Worsening Physical Disability and Dependency
Without consistent rehabilitation and medical follow up, physical limitations tend to increase. I see patients gradually lose strength, balance, and coordination when therapy stops too early. You may find that activities once manageable slowly become difficult again. Clinicians understand that unused muscles weaken and abnormal movement patterns become fixed over time. This progression often leads to increased dependence on caregivers and assistive devices. Proper long term management helps preserve mobility and independence.
Cognitive Decline and Vascular Dementia
Stroke affects thinking as much as movement. When care is inadequate, cognitive problems often worsen. I hear families describe increasing forgetfulness, confusion, or poor judgment. You may notice difficulty managing finances, medications, or daily planning. Clinically, repeated vascular injury can progress toward vascular cognitive impairment or dementia. This decline is not inevitable, but the risk rises sharply without proper control of blood pressure, metabolism, and lifestyle factors. Early intervention can slow or stabilize cognitive loss.
Emotional and Psychological Deterioration
Emotional health often suffers when stroke care is fragmented. I see untreated depression and anxiety gradually erode motivation and hope. You may withdraw socially or feel like recovery has stalled permanently. Clinicians know that emotional distress directly interferes with brain healing and rehabilitation participation. Over time, untreated psychological issues can become as disabling as physical deficits. Addressing mental health is essential to prevent long term decline.
Chronic Pain and Fatigue Syndromes
When post stroke pain and fatigue are ignored, they often become entrenched. I frequently meet patients who accept constant pain or exhaustion as normal. You may stop engaging in therapy or physical activity because every effort feels overwhelming. Clinically, chronic pain alters brain signaling and reinforces disability. Persistent fatigue reduces resilience and slows all aspects of recovery. Proper management can prevent these symptoms from becoming permanent barriers.
Increased Medical Complications and Hospitalizations
Poor long term management increases the risk of infections, falls, pressure injuries, and metabolic instability. I have seen patients cycle in and out of hospitals for preventable complications. You may feel frustrated by repeated setbacks that seem unrelated to the original stroke. Clinicians recognize that these events are often linked to gaps in follow up care, mobility support, and monitoring. Comprehensive management reduces hospitalizations and improves overall stability.
When stroke is not managed holistically, quality of life steadily declines. I often hear patients say they feel disconnected from their previous identity and relationships. You may avoid social situations due to mobility limits, speech difficulties, or low confidence. Clinically, social isolation worsens both physical and mental outcomes. Long term care aims not only to prevent complications but to restore dignity, purpose, and participation in life.
Common Disorders Associated With Stroke
Cardiovascular and Vascular Comorbidities
When someone has a stroke, it rarely happens in isolation. In most patients, underlying heart and blood vessel problems are already present. High blood pressure, hardening of the arteries, abnormal cholesterol levels, coronary artery disease, and heart failure often exist long before the stroke occurs. Conditions like carotid artery narrowing and heart rhythm disorders such as atrial fibrillation are especially important because they significantly increase the risk of a second stroke. Many patients assume the stroke was a sudden event, but doctors see it as the final outcome of years of vascular strain. If you or your loved one has had a stroke, managing these cardiovascular conditions becomes just as important as rehabilitation. Without proper control, these disorders continue to stress the brain’s blood supply and can worsen recovery, increase complications, and raise the likelihood of recurrence.
Metabolic Disorders That Worsen Recovery
Stroke recovery is often slower and more complicated when metabolic conditions are present. Diabetes, insulin resistance, obesity, fatty liver disease, and kidney problems frequently coexist with stroke and quietly influence outcomes. From a patient’s perspective, these conditions may feel unrelated to the brain, but medically they are deeply connected. Poor blood sugar control damages blood vessels and nerves, excess weight increases inflammation, and kidney disease alters fluid and electrolyte balance. Together, these factors reduce the brain’s ability to heal and adapt after injury. Many patients notice persistent weakness or fatigue and wonder why progress has stalled. In reality, untreated metabolic issues continue to interfere with nerve recovery and muscle strength. Addressing these disorders is not optional. It is a core part of long-term stroke management and plays a major role in preventing further decline.
Motor Disability Syndromes
Movement problems are among the most visible and frustrating consequences of stroke. Many survivors experience weakness or paralysis on one side of the body, known as hemiparesis or hemiplegia. Walking may become slow and unstable, balance can feel unreliable, and the fear of falling often limits independence. Over time, muscle stiffness, spasms, joint contractures, and shoulder pain may develop, making everyday tasks more difficult. From the patient’s point of view, these changes can feel sudden and overwhelming. Clinicians recognize that these motor issues are not just muscle problems but reflect disrupted communication between the brain and body. Without proper care, secondary musculoskeletal problems may appear, further reducing mobility. Recovery requires patience, regular rehabilitation, and attention to posture, muscle tone, and joint health to prevent long-term disability.
Speech, Language, Swallowing, and Nutrition Problems
After a stroke, communication and swallowing problems are common but often underestimated. Some patients struggle to find words or understand language, a condition known as aphasia. Others develop slurred speech or difficulty controlling the muscles involved in speaking. Swallowing problems can be particularly dangerous, as they increase the risk of choking and aspiration pneumonia. Many people eat less because food becomes tiring or uncomfortable, leading to weight loss, dehydration, and poor nutrition. Patients may feel embarrassed or frustrated and avoid mentioning these issues. Clinicians know that untreated speech and swallowing problems slow recovery and increase hospital readmissions. Early assessment and support are essential. Addressing these challenges improves safety, energy levels, and overall quality of life during recovery.
Cognitive and Behavioral Disorders
Stroke does not only affect movement. It often changes how a person thinks, plans, and processes information. Many survivors experience problems with memory, attention, decision-making, or multitasking. These cognitive changes may be subtle at first but can become more noticeable over time, especially after repeated or silent strokes. Family members may notice personality changes or reduced initiative, which can be confusing and distressing. From a medical perspective, these issues reflect damage to brain networks responsible for executive function. If left unaddressed, cognitive impairment can progress toward vascular cognitive decline or dementia. Recognizing these changes early allows patients and caregivers to adjust expectations, seek appropriate support, and reduce long-term impact on independence.
Mood and Emotional Disorders
Emotional changes after stroke are extremely common and often misunderstood. Depression and anxiety affect many survivors, sometimes appearing weeks or months after the event. Patients may feel hopeless, irritable, or withdrawn, even when physical recovery is progressing. These feelings are not a sign of weakness. They are part of how brain injury alters emotional regulation. When mood disorders go unnoticed, patients participate less in rehabilitation, lose motivation, and experience poorer long-term outcomes. Caregivers may feel helpless, unsure how to help. Clinicians emphasize that screening and early treatment of emotional health is as important as physical therapy. Addressing mood disorders improves engagement, recovery, and overall quality of life.
Pain and Fatigue Syndromes
Persistent pain and fatigue are common after stroke and can be deeply disabling. Some patients experience headaches, while others develop nerve-related pain, muscle soreness, or joint discomfort. Fatigue is often profound and does not always improve with rest. From the patient’s perspective, this constant exhaustion can be more limiting than weakness itself. These symptoms are frequently underreported because patients assume they are normal or unavoidable. Medically, post-stroke pain and fatigue reflect changes in brain signaling, muscle tone, and energy regulation. When ignored, they reduce participation in therapy and slow progress. Identifying and managing these symptoms is essential for sustained recovery and daily functioning.
Bladder and Bowel Dysfunction
Bladder and bowel problems are common after stroke but rarely discussed openly. Many patients experience urinary urgency, incontinence, difficulty emptying the bladder, or constipation. Communication difficulties and embarrassment often prevent people from mentioning these issues. Clinicians know that these problems are linked to disrupted brain control of pelvic muscles and autonomic function. Left untreated, they increase infection risk, skin problems, and emotional distress. Addressing bladder and bowel function improves dignity, comfort, and independence. Open discussion and routine screening are important parts of comprehensive stroke care.
Infections Linked to Stroke-Induced Immune Changes
After a stroke, the immune system can become temporarily weakened. This makes patients more vulnerable to infections, particularly pneumonia and urinary tract infections. These complications are a major cause of prolonged hospital stays and increased mortality. Patients may feel confused when an infection develops weeks after the stroke, but medically this is a well-recognized phenomenon. Reduced mobility, swallowing problems, and bladder dysfunction further increase risk. Preventing infections through early mobilization, good nutrition, swallowing assessment, and hygiene is a key part of recovery. Recognizing infections early can significantly improve outcomes.
Seizures and Post-Stroke Epilepsy
Some stroke survivors develop seizures, either shortly after the event or months later. This is more common when the stroke affects the outer layers of the brain or is severe. For patients, seizures can be frightening and unexpected, adding another layer of uncertainty to recovery. Doctors understand that stroke-related scarring and altered brain activity can trigger abnormal electrical signals. Long-term seizure management may be needed in some cases. Early recognition and treatment help reduce complications and support safer long-term recovery.
Rare Disorders Associated With Stroke
Cerebral Vasculitis
Cerebral vasculitis is a rare condition in which inflammation affects the blood vessels of the brain. Unlike typical stroke causes, this condition is driven by immune system dysfunction rather than cholesterol or clots alone. Patients may experience recurrent strokes, headaches, confusion, or gradual neurological decline. From the patient’s perspective, symptoms can feel unpredictable and may worsen despite standard stroke treatment. Doctors recognize that untreated vessel inflammation narrows or damages arteries, reducing blood flow and increasing stroke risk. Diagnosis is often delayed because symptoms overlap with more common conditions. Management usually requires careful coordination between neurology and immunology, along with long-term monitoring. When cerebral vasculitis is present, stroke recovery can be slower, and recurrence risk is higher if inflammation is not controlled.
Moyamoya Disease
Moyamoya disease is a rare, progressive disorder in which major brain arteries gradually narrow, forcing the brain to form fragile alternative vessels. These new vessels are prone to bleeding or blockage, increasing stroke risk. It can affect children or adults and may present with repeated strokes, transient weakness, headaches, or seizures. Patients often feel frustrated because symptoms may appear and disappear before a clear diagnosis is made. Clinicians understand that standard stroke prevention strategies are often insufficient in Moyamoya disease. Surgical interventions are sometimes required to restore blood flow. Early diagnosis is critical, as delayed treatment can lead to cumulative brain injury and long-term disability.
Cerebral Amyloid Angiopathy
Cerebral amyloid angiopathy is a condition where abnormal protein deposits weaken small blood vessels in the brain. It is more common in older adults and often leads to recurrent brain bleeds rather than classic clot-related strokes. Patients may present with sudden neurological symptoms, confusion, or memory problems. From a caregiver’s view, episodes may seem sudden and unexplained. Doctors recognize this condition as a major cause of hemorrhagic stroke in the elderly. Blood-thinning medications must be used with extreme caution. Over time, repeated small bleeds can contribute to cognitive decline and functional impairment.
Antiphospholipid Antibody Syndrome
This autoimmune disorder increases the blood’s tendency to clot, even in young and otherwise healthy individuals. Stroke may be the first major sign. Patients often feel shocked when a stroke occurs without traditional risk factors like high blood pressure or diabetes. Clinicians know that antiphospholipid antibody syndrome can cause recurrent strokes if not identified early. Long-term blood-thinning treatment is often required. Pregnancy complications and other clotting events may coexist. Recognizing this condition is essential to prevent repeated neurological injury.
Sickle Cell Disease–Related Stroke
In people with sickle cell disease, abnormal red blood cells block small blood vessels, reducing oxygen delivery to the brain. Strokes can occur in childhood or adulthood and may be recurrent. Patients often face lifelong neurological and cognitive challenges. From a medical perspective, these strokes are driven by chronic vascular injury and inflammation rather than traditional atherosclerosis. Prevention requires specialized care, including regular monitoring and disease-specific therapies. Early intervention significantly improves long-term outcomes.
Cerebral Venous Sinus Thrombosis
This rare form of stroke occurs when clots form in the brain’s venous drainage system rather than arteries. Symptoms often include severe headache, vision problems, seizures, or gradual neurological changes. Patients may initially be misdiagnosed with migraine or infection. Doctors recognize that dehydration, hormonal factors, pregnancy, or clotting disorders can contribute. Unlike arterial strokes, recovery can be good if diagnosed early. Awareness is key, as delayed treatment increases complication risk.
Genetic Small Vessel Diseases
Certain inherited conditions affect the brain’s small blood vessels, leading to recurrent strokes and cognitive decline. These disorders often present earlier in life and may run in families. Patients may notice gradual changes in walking, thinking, or mood long before a major stroke occurs. Clinicians understand that these diseases require long-term monitoring rather than short-term stroke treatment alone. Genetic counseling and tailored management play an important role in care.
Cancer-Associated Stroke
Some cancers increase clotting risk, leading to stroke even before cancer is diagnosed. Patients may feel confused when stroke occurs without clear vascular risk factors. Doctors recognize cancer-related clotting as a serious but under-recognized cause of stroke. Management focuses on treating both the cancer and the clotting tendency. Recovery depends on early recognition and coordinated care.
Why Stroke Recovery Often Slows Down Over Time
Early Gains Versus Long Term Healing
In the early weeks after a stroke, recovery often feels fast. I see patients regain small movements, clearer speech, or better balance, and this creates hope. You may feel encouraged when therapy seems to work quickly at first. Clinically, this phase is driven by reduced swelling in the brain and the return of temporarily stunned nerve cells. Over time, however, recovery enters a different phase. The brain must now form new connections and relearn functions through repetition and adaptation. This process is slower and demands patience. Doctors understand that this shift is normal, not a failure of treatment or effort.
Brain Plasticity Has Limits and Conditions
The brain has an ability to adapt, called plasticity, but it is not unlimited. I often explain that new neural pathways form only when the brain is challenged in the right way and supported by good health. You may notice progress slowing when therapy becomes repetitive or when motivation drops. Clinicians know that plasticity depends on sleep, nutrition, emotional health, and consistent practice. When these supports are missing, the brain struggles to reorganize efficiently. Recovery slows not because healing has stopped, but because the conditions for change are no longer optimal.
Ongoing Medical Conditions Interfere With Progress
Many stroke survivors live with high blood pressure, diabetes, heart disease, or metabolic problems. I see recovery slow when these conditions are poorly controlled. You might feel that therapy is failing, but medically the body is under constant stress. Poor circulation, inflammation, and unstable blood sugar reduce the brain’s ability to heal. Doctors recognize that stroke recovery is not only neurological. It is systemic. Without addressing these ongoing conditions, progress naturally plateaus.
Fatigue and Energy Depletion
Post stroke fatigue is one of the most common and misunderstood barriers to recovery. Patients often tell me they feel exhausted after simple activities. You may want to push harder, but the body resists. Clinically, the brain uses more energy to perform tasks that were once automatic. This hidden energy cost leads to burnout and slower gains. When fatigue is ignored, therapy becomes less effective and recovery appears stalled.
Emotional and Cognitive Load
Recovery is not only physical. I often see progress slow when depression, anxiety, or cognitive overload sets in. You may feel mentally drained, discouraged, or overwhelmed by daily demands. Clinicians know that emotional stress alters brain chemistry and reduces learning capacity. When mood and motivation decline, participation in rehabilitation drops. Addressing emotional health often restores momentum in recovery.
Reduced Intensity of Rehabilitation Over Time
In the early phase, rehabilitation is structured and frequent. Later, sessions often become less intense or less regular. I see patients lose progress simply because therapy exposure decreases. You may assume that less therapy means you should be fully recovered, but the brain still needs guided training. Clinically, reduced stimulation leads to slower adaptation. Recovery does not stop because time has passed. It slows because input has reduced.
Lack of Clear Long Term Guidance
Many patients reach a point where medical follow up becomes less frequent. I hear people say they were told to continue exercises at home without much guidance. You may feel unsure about what to do next. Clinicians acknowledge that long term recovery plans are often missing. Without direction, progress becomes inconsistent and slower than it could be.
What This Slowdown Really Means
When recovery slows, it does not mean you have reached your limit. I remind patients that this phase signals a transition from rapid repair to deeper rebuilding. You are not failing. The brain is working differently now. Clinically, this is the stage where long term strategies, consistent support, and patience matter most. Understanding this shift helps set realistic expectations and prevents unnecessary frustration.
Modern Diagnostic Framework
Why Accurate Diagnosis Is Critical
Modern diagnosis of stroke focuses on speed precision and identification of the exact cause. Stroke is a medical emergency where every minute matters because brain cells begin to die rapidly when deprived of oxygen. From a clinician’s perspective early diagnosis determines whether life saving interventions such as thrombolysis or thrombectomy can be used. From a patient’s perspective timely diagnosis often decides the difference between recovery and permanent disability. From a third person medical viewpoint stroke diagnosis is not only about confirming that a stroke has occurred but also about understanding its type severity and underlying mechanism [3], [4].
Brain Imaging as the Diagnostic Foundation
Brain imaging is the cornerstone of modern stroke diagnosis. A non contrast CT scan of the brain is usually the first investigation performed because it is fast widely available and effective in detecting brain hemorrhage. It helps doctors immediately differentiate between ischemic and hemorrhagic stroke which is crucial because treatments differ completely. You may be taken for a CT scan within minutes of reaching the hospital to rule out bleeding before any clot dissolving treatment is considered [3].
MRI of the brain provides more detailed information and is particularly useful in detecting early ischemic changes small infarcts and silent strokes that may not appear on CT. From a neurological standpoint MRI allows visualization of brain tissue injury extent and location helping predict recovery potential and complications [4].
Vascular Imaging to Identify Blood Flow Problems
To understand why a stroke occurred doctors often evaluate the blood vessels supplying the brain. CT angiography or MR angiography is used to visualize major cerebral arteries and detect blockages narrowing or aneurysms. These tests help identify large vessel occlusions which may benefit from mechanical clot removal. From the patient’s perspective this explains why multiple scans may be done even after stroke confirmation [3].
Carotid Doppler ultrasound is commonly used to assess blood flow in neck arteries. Significant narrowing in these vessels increases stroke risk and may require specific long term management [4].
Heart Evaluation and Rhythm Monitoring
Many strokes originate from the heart especially when abnormal heart rhythms allow clots to form. Electrocardiogram monitoring is used to detect conditions such as atrial fibrillation. Echocardiography evaluates heart structure valves and pumping function to identify potential clot sources. You may not feel any heart symptoms yet cardiac evaluation remains essential because hidden rhythm disorders are a common cause of sudden stroke [3].
Blood Tests and Systemic Assessment
Blood investigations support stroke diagnosis and guide treatment decisions. These tests evaluate blood sugar lipid levels clotting status kidney function and markers of infection or inflammation. From a third person clinical view these tests help uncover metabolic and systemic contributors that may not be immediately obvious but strongly influence stroke risk and recurrence [4].
Limitations of Modern Diagnostic Testing
While modern diagnostics excel at identifying the location and type of stroke they often do not explain why the body reached this state beyond measurable risk factors. Imaging shows damage but does not assess long standing metabolic imbalance nervous system resilience or tissue vitality. From an integrative viewpoint this explains why diagnosis alone does not guarantee recovery and why deeper systemic correction is needed after the acute phase [3], [4].
What Diagnosis Means for the Patient
For you diagnosis is not just a label. It determines treatment urgency rehabilitation planning and future risk. Early and accurate diagnosis saves brain tissue preserves function and guides safe long term management. Modern diagnostic tools provide the necessary clarity at the emergency stage and create the foundation upon which recovery strategies can be built [3], [4].
Acute Emergency Care (Supportive Role)
Why Emergency Care Is Time Sensitive
Acute emergency care in stroke focuses on saving life and limiting immediate brain damage. When a stroke occurs blood flow to part of the brain is suddenly reduced or interrupted. Brain cells begin to suffer irreversible injury within minutes. From a modern medical perspective this period is often described as a race against time because early intervention can preserve threatened brain tissue. From a patient’s viewpoint this is the most critical and frightening phase where rapid decisions determine survival and future disability [3].
Immediate Stabilization and Assessment
The first priority in emergency care is stabilization. Doctors focus on maintaining airway breathing and circulation. Oxygen levels blood pressure heart rate and blood sugar are quickly assessed and corrected if abnormal. You may undergo rapid neurological examination to determine the severity of stroke and identify life threatening complications. This initial stabilization creates the foundation for further intervention [3].
Thrombolytic Therapy in Ischemic Stroke
In selected patients with ischemic stroke clot dissolving medication known as thrombolytic therapy may be administered. This treatment aims to restore blood flow by breaking down the clot obstructing a cerebral artery. It is strictly time bound and must be given within a narrow window after symptom onset. From a clinical standpoint careful screening is essential because inappropriate use can cause serious bleeding. From the patient’s perspective thrombolysis represents an opportunity to reduce paralysis and improve recovery if used safely and promptly [3].
Mechanical Thrombectomy for Large Vessel Blockage
For certain patients with large artery blockage mechanical thrombectomy may be performed. This procedure involves physically removing the clot using specialized devices through blood vessels. It is carried out in advanced centers and can significantly improve outcomes in selected cases. From a third person medical viewpoint this approach highlights the progress of modern emergency stroke care yet it remains applicable only to a limited group of patients [3].
Blood Pressure and Complication Control
Careful blood pressure management is a critical part of acute stroke care. Excessively high pressure can worsen brain swelling or bleeding while overly aggressive lowering may reduce blood flow to injured brain tissue. Doctors also manage fever infections seizures and electrolyte disturbances during this phase. These supportive measures do not cure stroke but they prevent secondary injury and stabilize the patient [3].
Limitations of Acute Emergency Care
While emergency interventions are lifesaving they do not address the deeper causes of stroke. Thrombolysis and thrombectomy restore blood flow but they do not regenerate damaged neurons or correct long standing vascular and metabolic imbalance. From a patient’s perspective improvement after emergency care may be partial and unpredictable. From a broader clinical view emergency care represents damage control rather than complete healing [3].
Understanding the Supportive Role of Emergency Care
Acute emergency care is essential and non negotiable in stroke management. It saves lives and preserves brain tissue during the most dangerous phase. However it functions as a supportive bridge rather than a complete solution. True recovery and prevention of recurrence require structured rehabilitation and long term correction of underlying imbalances beyond the emergency setting [3].
Recognizing the supportive role of acute care helps patients and families set realistic expectations while emphasizing the importance of comprehensive post stroke management.
Limitations of Long Term Conventional Management

Why Long Term Management Often Falls Short
Long term conventional management after stroke primarily focuses on preventing recurrence and helping the patient adapt to residual disability. From a medical standpoint this approach relies on lifelong medications risk factor control and rehabilitation support. From a patient’s perspective this phase often feels like maintenance rather than true recovery. From a third person clinical view conventional care is effective at reducing immediate mortality but frequently limited in restoring full neurological function or addressing why the stroke occurred in the first place [3], [11].
Many patients are told that improvement will plateau after a few months and that remaining deficits must be accepted. This belief shapes expectations and often leads to emotional resignation rather than continued pursuit of recovery [12].
Symptom Control Rather Than Neural Repair
A major limitation of long term conventional management is its focus on symptom control instead of neural regeneration. Medications such as antiplatelet drugs statins and blood pressure agents reduce future risk but they do not repair damaged neurons or restore lost neural pathways. You may notice that while blood reports look stable strength speech or coordination do not improve beyond a certain point [3].
From a third person neurological viewpoint once the acute phase is over conventional medicine offers limited tools to reverse neuronal loss. Rehabilitation trains the brain to compensate but does not regenerate damaged tissue [11].
Lifelong Medication Dependence
Most stroke survivors are advised to remain on multiple medications indefinitely. These may include blood thinners cholesterol lowering drugs antihypertensives and antidiabetic agents. From the patient’s experience this often leads to pill burden fear of missed doses and concern about side effects. Fatigue dizziness gastric discomfort muscle pain and bleeding risk are common long term challenges [3].
From a broader clinical lens these medications manage risk but do not restore physiological balance. Over time drug dependence may increase while functional gains remain limited [12].
Limited Impact on Cognitive and Emotional Recovery
Conventional stroke management often underaddresses cognitive and emotional complications. Memory loss reduced concentration depression anxiety and personality changes are frequently treated as secondary issues. You may be given antidepressants or counseling but the underlying neurological and metabolic contributors are rarely addressed in depth [11].
From a third person observation emotional suffering becomes one of the main reasons patients disengage from rehabilitation and lose motivation for recovery [12].
One Size Fits All Rehabilitation Models
Standard rehabilitation protocols often follow fixed schedules and generalized exercises. While helpful initially they may not account for individual differences in metabolism age tissue resilience or recovery potential. As a patient you may feel that therapy has become repetitive with diminishing returns. From a clinician’s perspective resource limitations often restrict personalization [3].
This standardized approach may stabilize function but rarely unlock further neurological improvement after the early months [11].
Lack of Root Cause Correction
Perhaps the most significant limitation of long term conventional management is the lack of root cause correction. Risk factors such as hypertension diabetes and cholesterol are controlled numerically but the deeper metabolic inflammatory and regulatory imbalances that led to stroke often persist. From an Ayurvedic comparative lens this means Dosha imbalance Rakta Dushti and tissue depletion remain unaddressed [12].
From a third person analytical view this explains why recurrent strokes and progressive decline continue to occur despite strict adherence to medication [3].
Patient Experience of Plateaus and Frustration
Many patients experience a clear plateau after initial rehabilitation. You may feel that despite effort therapy and medication progress has stopped. This can lead to frustration loss of hope and emotional withdrawal. From a clinical standpoint this plateau is often accepted as the natural limit of recovery [11].
However this acceptance reflects the limitations of the treatment model rather than the true limits of human recovery [12].
Understanding These Limitations Clearly
Recognizing the limitations of long term conventional management does not mean rejecting its value. Emergency care and risk reduction save lives. However understanding these limitations helps patients families and clinicians look beyond maintenance toward deeper recovery strategies. From a patient’s view it restores hope. From a third person clinical view it opens the door to integrative and restorative approaches that aim not just to prevent decline but to rebuild function and vitality [3], [11], [12].
Ayurvedic Understanding of Stroke (Pakshaghata)
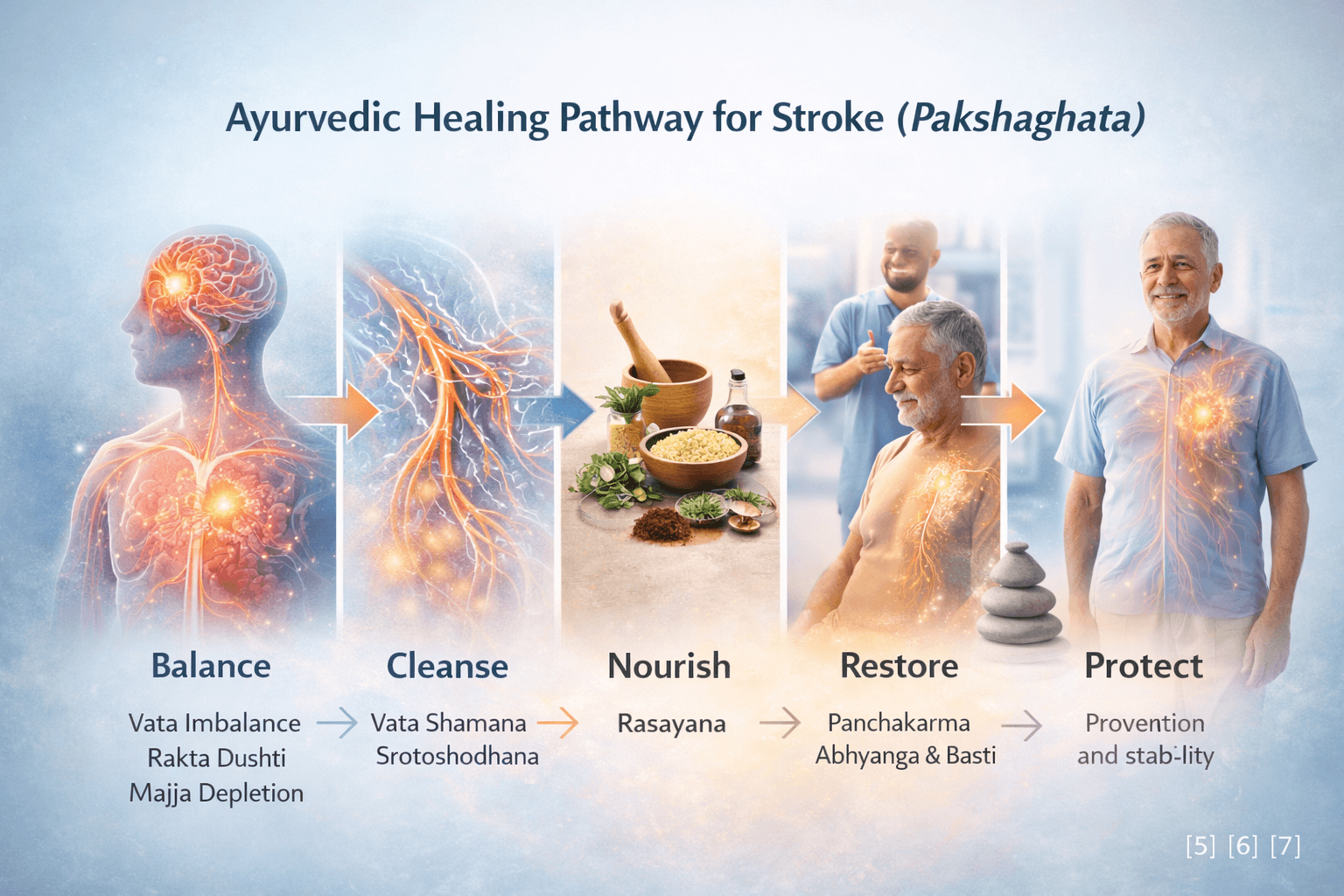
How Ayurveda Defines Stroke
Ayurveda understands stroke as Pakshaghata, a classical neurological disorder described in ancient medical texts long before modern neuroimaging existed. Pakshaghata literally refers to loss of movement and function on one side of the body. Unlike the modern view that often treats stroke as a sudden isolated brain event, Ayurveda explains it as the final outcome of long standing internal imbalance affecting the entire system [5], [6].
As a patient you may feel that stroke happened suddenly without warning. As a physician observing the condition from a third person perspective, Ayurveda teaches that Pakshaghata develops gradually due to progressive disturbance in Dosha balance tissue nourishment and circulation. What appears sudden externally has usually been building silently within the body for years [7].
Central Role of Vata in Pakshaghata
Vata is the primary Dosha responsible for movement nerve conduction circulation and coordination. Ayurveda clearly states that Pakshaghata is a Vata dominant disorder. When Vata becomes aggravated or obstructed it loses its ability to control muscles sensation and voluntary movement. This results in paralysis stiffness tremors speech difficulty and loss of coordination [5].
From the patient’s experience this may appear as sudden weakness heaviness or inability to move one side of the body. From a third person Ayurvedic lens this reflects deranged Vata that has either become excessively dry erratic or blocked by other Doshas and metabolic waste [6].
Rakta Dushti and Circulatory Obstruction
Ayurveda places great importance on Rakta circulation for maintaining neurological health. When Rakta becomes vitiated due to poor diet chronic stress toxins or metabolic imbalance its flow through subtle channels is disturbed. This leads to obstruction known as Srotorodha. When Vata tries to move through obstructed channels it becomes further aggravated resulting in loss of nerve signaling and muscle control [5], [7].
In modern terms this correlates with impaired blood flow inflammation and vascular blockage. From an Ayurvedic standpoint impaired circulation alone is not the root cause. It is the interaction between Rakta Dushti and Vata Prakopa that culminates in Pakshaghata [6].
Dhatu Involvement and Tissue Depletion
Ayurveda explains that Pakshaghata is not limited to nerves alone. Progressive depletion of Dhatus particularly Majja Dhatu which governs nervous tissue and Mamsa Dhatu which governs muscles plays a crucial role. When nourishment to these tissues is compromised strength coordination and recovery potential decline [5].
As a patient you may notice muscle wasting stiffness or slow recovery even after the acute phase. From a third person clinical perspective this reflects Dhatu Kshaya where tissues lack the capacity to regenerate without targeted nourishment [7].
Role of Agni Ama and Lifestyle Factors
Weak digestive and metabolic fire known as Agni Mandya leads to accumulation of Ama which is toxic undigested material. Ama blocks channels worsens inflammation and interferes with tissue nutrition. Sedentary lifestyle irregular eating stress suppression of natural urges and lack of sleep all aggravate Vata and weaken Agni creating a fertile ground for Pakshaghata [6].
From a patient’s view these habits may seem unrelated to stroke. Ayurveda clearly links daily routines and mental strain to long term neurological outcomes emphasizing prevention as much as cure [5].
Prodromal Signs Described in Ayurveda
Classical Ayurvedic texts describe Poorvarupa or early warning signs before full manifestation of Pakshaghata. These include heaviness stiffness numbness tingling giddiness fatigue and subtle speech disturbance. These signs indicate that Vata imbalance and circulatory disturbance have reached a critical stage [7].
Recognizing these early signs allows intervention before irreversible damage occurs. From a third person Ayurvedic standpoint early correction at this stage offers the highest chance of recovery [6].
Holistic View of Stroke in Ayurveda
Ayurveda does not view stroke as a localized brain disorder. It is seen as a systemic disease involving Dosha imbalance Rakta circulation tissue depletion mental stress and lifestyle errors. As a patient this perspective explains why stroke affects movement speech emotion digestion sleep and energy simultaneously. From a physician’s perspective it guides treatment toward restoring balance rather than managing isolated symptoms [5], [6], [7].
Understanding Pakshaghata through Ayurveda shifts the focus from fear and finality to possibility and regeneration. It lays the foundation for therapies aimed at stabilizing Vata clearing obstruction nourishing tissues and restoring neurological function at the root level.
Classical Etiological Factors
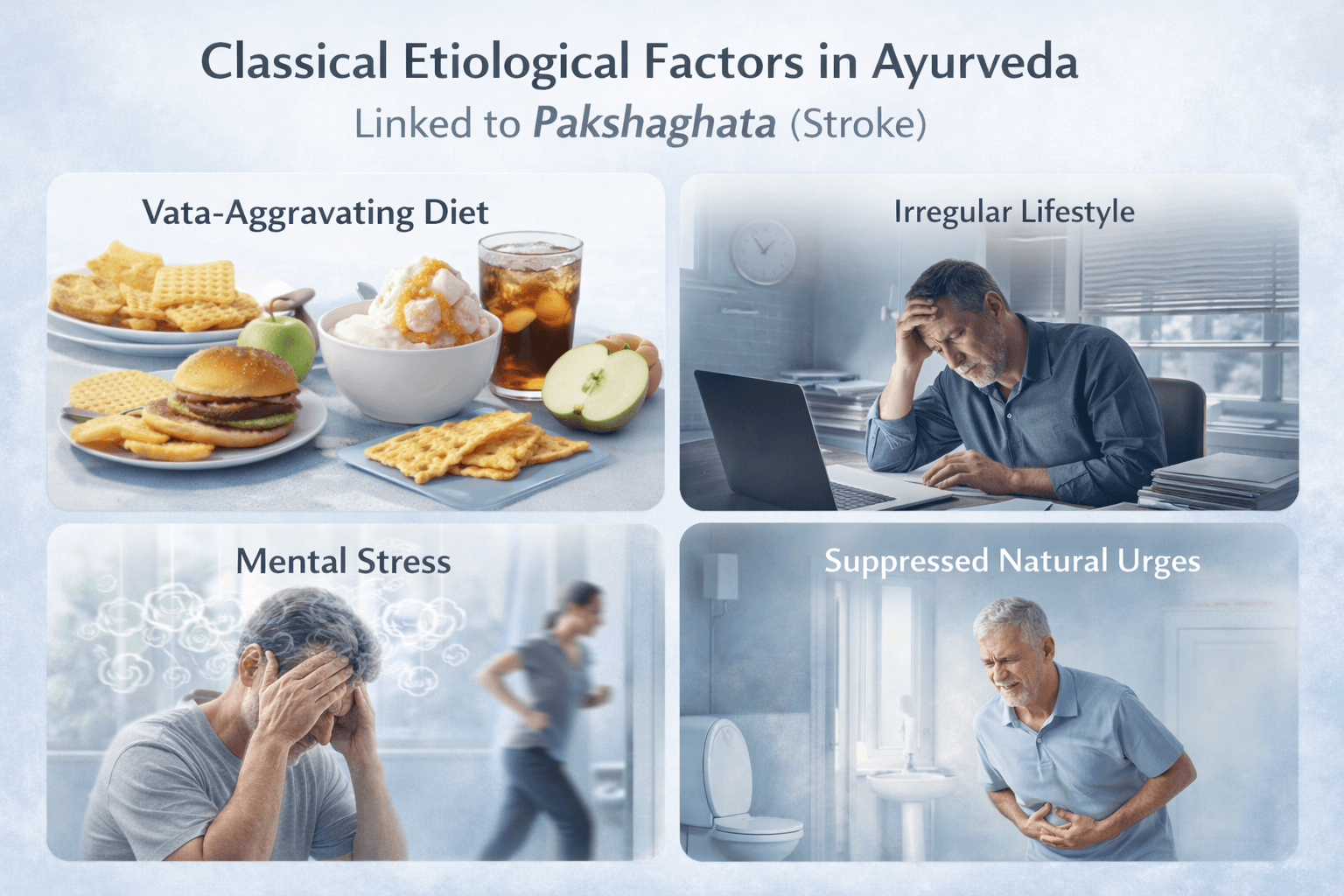
How Ayurveda Explains the Causes of Pakshaghata
Ayurveda explains stroke under the disease entity Pakshaghata as the result of long standing internal imbalance rather than a sudden accidental event. Classical texts describe that Pakshaghata develops slowly due to continuous disturbance of Dosha balance improper nourishment of tissues and obstruction in circulation and nerve pathways [5], [6].
From a patient’s point of view stroke may appear sudden. From an Ayurvedic physician’s understanding the body usually gives warning signals for years in the form of digestive issues fatigue stiffness stress intolerance and sleep disturbance before paralysis manifests.
Vata Aggravating Diet and Lifestyle Explained Clearly
The most important classical cause of Pakshaghata is aggravation of Vata Dosha, which governs movement nerve impulses circulation and coordination. Vata becomes aggravated primarily due to unsuitable food and lifestyle habits [5].
When classical texts mention dry foods, they refer to foods that lack natural oils and moisture. Examples include biscuits crackers chips dry toast packaged snacks and excessive salads without healthy fats. Such foods dry the tissues and nerves over time making them weak and less resilient.
Cold foods refer to foods that are cold in temperature or cold in potency. Examples include ice cream cold drinks refrigerated foods excessive curd at night and raw vegetables taken frequently. These reduce digestive strength slow circulation and stiffen nerve pathways.
Light foods are foods that do not provide sustained nourishment. Examples include skipping meals and relying on fruit only diets soups without substance excessive fasting or consuming only liquid meals for long periods. These weaken muscle and nerve tissue gradually.
Irregular eating means eating at inconsistent times skipping breakfast eating late at night or overeating one day and undereating the next. This disrupts digestive rhythm and creates instability in circulation and nerve control.
From a patient’s experience these habits may feel harmless or even healthy. From an Ayurvedic standpoint they steadily weaken Majja Dhatu and Mamsa Dhatu which support nerve strength and muscle movement [6].
Lifestyle Habits That Gradually Damage Neurological Stability
Ayurveda also identifies lifestyle errors that aggravate Vata and predispose to Pakshaghata. Excessive physical exertion such as over exercise long working hours without rest continuous travel or prolonged sitting stiffens the body and disturbs circulation.
Irregular sleep such as sleeping late frequent night waking or inadequate rest dries the nervous system and weakens repair mechanisms. Suppressing fatigue and continuing work despite exhaustion is considered especially harmful for neurological health [5].
For patients these patterns often feel unavoidable due to modern life demands. Ayurveda considers them major contributors to paralysis disorders when sustained over years [6].
Mental Stress and Emotional Strain Explained With Examples
Classical texts place strong emphasis on mental causes of Pakshaghata. Chronic worry fear anger grief and emotional suppression disturb Vata flow in the nervous system [5].
For example constant job stress unresolved family tension long term anxiety or suppressed emotions keep the nervous system in a continuous state of alertness. Over time this exhausts nerve regulation dries tissues and disrupts coordination between brain and body.
From the patient’s perspective emotional stress feels psychological. Ayurveda explains that prolonged mental strain directly affects nerve circulation and muscle control contributing to paralysis [6].
Suppression of Natural Urges Explained Simply
Ayurveda clearly warns against repeated suppression of natural urges such as delaying bowel movements holding urine ignoring hunger suppressing sleep or constantly ignoring emotional expression.
For example regularly delaying toilet use due to work pressure ignoring hunger signals or forcing wakefulness at night disrupts the natural downward and rhythmic movement of Vata. This causes abnormal nerve signaling and obstruction in circulation [6].
Patients are often surprised by this cause. Classical texts clearly associate such suppression with development of serious Vata disorders including Pakshaghata [5].
Aging and Progressive Tissue Weakening
Classical Ayurveda explains that increasing age naturally increases Vata dominance in the body. With aging the tissues lose lubrication strength and regenerative capacity. Majja Dhatu which supports nerves and brain becomes less nourished [5].
This is why stroke is more common in later life. From an Ayurvedic view stroke in old age represents accelerated degeneration rather than a random event. Recovery is slower because tissue reserves are already depleted [6].
Metabolic Weakness and Ama Formation Explained
Weak digestive and metabolic fire known as Agni Mandya leads to formation of Ama which is sticky undigested metabolic waste. Ama blocks circulation channels and interferes with proper tissue nourishment.
For example long standing indigestion bloating heaviness sluggish metabolism or poorly controlled metabolic disorders indicate Ama accumulation. When Ama combines with aggravated Vata it obstructs nerve pathways and circulation leading to paralysis [5].
Patients often report digestive complaints years before stroke. Ayurveda views these as early warnings rather than unrelated issues [6].
Integrated Classical View for Patient Understanding
Ayurveda teaches that Pakshaghata does not arise from a single cause. It develops due to a combination of Vata aggravating food habits irregular lifestyle chronic stress suppression of natural urges aging related degeneration and metabolic dysfunction [5], [6].
From a patient’s perspective this explains why stroke often follows years of subtle health imbalance. From a physician’s understanding this knowledge allows prevention and treatment by correcting causes at the root level rather than managing paralysis alone.
This classical etiological understanding forms the foundation for Ayurvedic treatment aimed at restoring balance rebuilding nerve strength and preventing recurrence.
Stages of Disease (Poorvarupa, Vyakti, Bheda)
Which Classical Texts Describe These Stages
In Ayurveda, the stage wise progression of disorders like Pakshaghata is explained through the clinical method of Poorvarupa, Vyakti, and Bheda that is taught across classical texts. Charaka Samhita explains the importance of Poorvarupa and Vyakti as a way to detect disease early and prevent progression. Sushruta Samhita also emphasizes stage wise understanding, especially in serious Vata disorders that can lead to loss of movement and sensation. Ashtanga Hridaya similarly teaches how Vata dominant diseases evolve from subtle warnings into clear manifestation and later complications if not treated in time [5], [6].
From your perspective as a patient this means stroke is not always a sudden surprise. From the physician’s third person view, the body usually gives signals first, but people do not recognize them.
Poorvarupa Stage (Early Warning Stage)
Poorvarupa means early warning signs that appear before the disease becomes fully established. In simple patient language, this stage is like a small fire that has started inside the system, and the body is giving hints before the big damage happens [5].
Examples that patients commonly notice in this stage include heaviness in one arm or one leg, stiffness in the neck or shoulder, tingling like pins and needles in one side, sudden tiredness without a clear reason, mild dizziness while standing, occasional imbalance while walking, or a feeling that speech becomes slightly unclear when tired. Many people explain it as “I felt strange for a few days” or “My hand felt weak sometimes but then it became normal.”
Ayurveda understands these signs as early Vata disturbance, early circulation disturbance, and early blockage in channels. If you act here by correcting food timing, sleep, stress, and Vata aggravating habits, the condition can often be stopped before it becomes a full stroke event [6].
Vyakti Stage (Fully Manifested Stage)
Vyakti means the stage where the disease becomes clearly visible and diagnosable. In simple terms, this is the stage where the problem is no longer subtle and the symptoms become obvious to the patient and to everyone around [5].
Examples include sudden weakness or paralysis on one side, facial deviation, slurred speech, inability to hold objects, difficulty walking straight, sudden loss of balance, choking while swallowing water, or inability to speak properly. A family member may observe that the person’s smile becomes uneven or that one arm falls down while trying to lift both arms.
In Ayurvedic understanding, this stage reflects stronger Vata imbalance with deeper channel obstruction and tissue involvement. From your side as a patient, this is the stage where urgent medical stabilization is essential first. From the third person physician view, once the patient is stable, the deeper recovery plan is then selected based on strength, digestion, tissue depletion, and chronicity [6].
Bheda Stage (Complication and Differentiation Stage)
Bheda means the stage where the disease differentiates into long term outcomes and complications. In simple patient language, this stage is when the condition becomes chronic, and different people show different long term problems depending on how much damage happened and how early treatment began [5].
Examples of Bheda stage problems include permanent weakness, stiffness and tight muscles that do not relax, contractures where fingers or joints become fixed, long term speech difficulty, repeated choking episodes, memory and concentration problems, emotional changes like depression or irritability, and dependency in daily activities. Some patients recover walking but not speech. Some recover speech but remain weak. Some develop repeated episodes if root causes remain uncontrolled.
Ayurveda describes this as deeper tissue depletion and reduced regeneration capacity. If you come late into treatment, recovery still happens, but it usually requires longer time and deeper rebuilding therapies compared to early stage intervention [6].
Why This Stage Understanding Helps You as a Patient
This stage wise model is useful because it tells you one clear truth. If you recognize and act in the Poorvarupa stage, outcomes are usually much better. If you reach the Vyakti stage, urgent care plus structured recovery becomes necessary. If you remain in Bheda stage without correction, complications become the main challenge [5], [6].
Ayurvedic Diagnostic Approach
How Ayurveda Diagnoses Pakshaghata Beyond Imaging
Ayurveda follows a clinical and patient centered diagnostic approach that goes beyond scans and laboratory reports. Classical texts such as Charaka Samhita and Ashtanga Hridaya explain that correct diagnosis begins with understanding the individual, not just the disease. In conditions like Pakshaghata (stroke), Ayurveda evaluates why the imbalance developed, how long it has been progressing, and how deeply the tissues are affected [5], [13].
From a patient’s perspective this means you are not diagnosed only by a report. From the physician’s third person view diagnosis is a process of understanding your body’s internal state, strength, and recovery potential.
Prakriti Assessment – Understanding Your Natural Constitution
The first step in Ayurvedic diagnosis is Prakriti assessment, which means identifying your natural body constitution. Ayurveda classifies individuals into Vata, Pitta, Kapha, or mixed constitutions.
For example, a Vata dominant person naturally has a lighter body frame, quick movements, variable appetite, and sensitive nervous system. Such individuals are more vulnerable to paralysis disorders when Vata becomes aggravated. A Kapha dominant person may have a heavier body, slower metabolism, and stronger tissue reserves, leading to different stroke patterns and recovery timelines.
This assessment helps the physician understand why the stroke affected you in a particular way and how aggressive or gentle the treatment should be [5].
Vikriti Analysis – Identifying the Current Imbalance
After understanding Prakriti, Ayurveda evaluates Vikriti, which refers to the current imbalance caused by diet, lifestyle, stress, aging, or disease progression.
For instance, two patients may both have paralysis, but one may show dryness, stiffness, tremors, and anxiety indicating aggravated Vata, while another may show heaviness, swelling, sluggishness, and dullness indicating Kapha obstruction. Though the symptom looks similar externally, the internal imbalance is different.
From the patient’s view this explains why one treatment does not suit everyone, even when the diagnosis appears the same [13].
Nadi Pariksha – Pulse Examination Explained Simply
Nadi Pariksha, or pulse examination, is a classical diagnostic tool described in texts such as Ashtanga Hridaya. The physician gently examines the pulse to assess Dosha dominance, circulation quality, nervous regulation, and tissue vitality.
For patients, this is not about counting pulse rate. It is about understanding the rhythm, strength, depth, and stability of circulation. An irregular weak pulse may indicate unstable Vata and poor nerve nourishment, while a heavy slow pulse may indicate obstruction and sluggish flow [5].
This helps the physician judge the severity and stage of Pakshaghata.
Assessment of Dhatus and Srotas
Ayurvedic diagnosis also evaluates Dhatus (tissues) and Srotas (channels) involved in the disease. In Pakshaghata, special attention is given to Majja Dhatu which supports nerves and brain, Mamsa Dhatu which supports muscle strength, and Rakta Dhatu which supports circulation.
For example, muscle wasting, stiffness, or tremors indicate weakened Mamsa and Majja Dhatus. Coldness numbness or poor sensation suggests impaired Rakta flow. This assessment tells the physician how much regeneration is possible and how long recovery may take [13].
Agni and Ama Evaluation
Ayurveda considers digestion and metabolism central to diagnosis. Agni refers to digestive and metabolic fire, while Ama refers to toxic undigested material formed when digestion is weak.
For patients, this is evaluated by symptoms such as poor appetite bloating heaviness constipation sticky stools fatigue or sluggishness. Presence of Ama indicates blocked channels and poor response to treatment unless digestion is corrected first [5].
Strength Assessment – Bala and Ojas
Ayurvedic diagnosis also includes evaluating Bala (strength) and Ojas (vital essence). This determines how much treatment intensity the patient can tolerate.
For example, an elderly patient with poor sleep weight loss and exhaustion has low Bala and Ojas and requires gentle nourishing therapy. A younger patient with stronger digestion and stamina may tolerate deeper cleansing and strengthening protocols [13].
Why Ayurvedic Diagnosis Is Crucial for Recovery
Ayurvedic diagnosis is not a one time event. It is an ongoing process that guides every stage of treatment. From a patient’s perspective this explains why medicines may be adjusted over time. From the physician’s view it ensures that treatment remains aligned with recovery stage digestion strength and tissue regeneration capacity [5], [13].
This individualized diagnostic approach forms the foundation of Ayurvedic stroke management, allowing therapy to move beyond symptom control toward true neurological restoration and prevention of recurrence.
Core Ayurvedic Treatment
How Ayurveda Approaches Healing in Pakshaghata
Ayurveda approaches the treatment of Pakshaghata (stroke) with a fundamentally different philosophy compared to conventional symptom focused care. Classical texts such as Charaka Samhita, Sushruta Samhita, and Ashtanga Hridaya emphasize that true healing occurs only when the root imbalance is corrected and the body’s natural intelligence is restored [5], [8], [15].
From a patient’s perspective this means treatment is not aimed only at moving a weak limb or improving speech temporarily. From the physician’s third person view the goal is to restore balance in Doshas, reopen blocked channels, nourish depleted tissues, and rebuild neurological coordination.
Treating the Root Cause, Not Just Paralysis
The core Ayurvedic philosophy is Nidana Parivarjana, which means removing the causative factors of disease. In Pakshaghata this involves identifying and correcting the habits, diet patterns, stressors, and metabolic disturbances that aggravated Vata and disrupted circulation over years [5].
For example, if a patient developed stroke after years of irregular meals, chronic stress, poor sleep, and digestive weakness, simply giving strengthening medicines without correcting these causes will not lead to sustained recovery. Ayurveda therefore begins treatment by eliminating what is harming the system before adding what is healing.
Central Role of Vata Shamana Explained Simply
Pakshaghata is described in classical texts as a Vata dominant disorder. Vata governs movement, nerve impulses, circulation, and coordination. When Vata becomes excessive, dry, unstable, or obstructed, paralysis and loss of control occur [8].
Vata Shamana means calming and stabilizing Vata. In patient friendly terms this involves restoring lubrication to tissues, improving circulation, regularizing daily routines, and calming the nervous system. Therapies are chosen to reduce dryness, stiffness, tremors, and instability rather than force movement mechanically.
Clearing Obstruction Before Strengthening
Another key principle described in Ayurveda is that obstruction must be cleared before nourishment can work. Classical texts explain that if channels are blocked, even the best medicines cannot reach the tissues [5].
For patients this can be understood with a simple example. If a road is blocked, supplies cannot reach the destination. Similarly, if circulation and nerve pathways are obstructed by Ama or Dosha imbalance, strengthening therapies alone will fail. Ayurveda therefore prioritizes improving digestion, clearing metabolic waste, and restoring flow before intensive rebuilding begins [15].
Nourishing Dhatus to Restore Neurological Function
Ayurveda explains that recovery from Pakshaghata depends on the condition of Dhatus, especially Majja Dhatu which supports the brain and nerves, and Mamsa Dhatu which supports muscle strength. When these tissues are depleted, movement and coordination cannot return fully [8].
For patients this explains why weakness, muscle wasting, and slow recovery occur even months after stroke. Ayurvedic treatment focuses on gradual tissue nourishment using appropriate formulations, diet, and lifestyle measures that rebuild strength without overwhelming digestion.
Individualized Treatment Over One-Size-Fits-All
A core Ayurvedic philosophy is that no two patients are treated the same, even if the diagnosis appears identical. Classical texts emphasize assessing Prakriti, Vikriti, age, digestive strength, tissue depletion, and mental state before deciding treatment [5].
For example, a younger patient with good digestion may tolerate deeper cleansing and faster strengthening, while an elderly patient with weakness requires gentle, nourishing, and stabilizing care. This individualized approach explains why Ayurveda avoids rigid protocols and instead adapts therapy as recovery progresses [15].
Healing as a Progressive and Reversible Process
Ayurveda does not view Pakshaghata as an irreversible condition by default. Classical philosophy teaches that when Doshas are balanced, channels are clear, and tissues are nourished, the body can regain lost function to a significant extent [8].
From a patient’s viewpoint this restores hope without false promises. From a physician’s view it sets realistic expectations that recovery is gradual, layered, and dependent on consistent correction rather than quick fixes.
Prevention and Long-Term Stability
The final pillar of Ayurvedic treatment philosophy is prevention of recurrence. Ayurveda teaches that unless lifestyle, diet, mental stress, and digestion are corrected, the disease process continues internally even if symptoms improve [5], [15].
For patients this means treatment does not end when movement returns. Long-term stability, nervous system resilience, and balanced daily routines are essential to prevent future strokes and progressive neurological decline.
Why This Approach Matters to Patients
The core Ayurvedic treatment philosophy shifts stroke care from fear and dependency toward understanding and regeneration. It explains why treatment takes time, why medicines may change, and why lifestyle guidance is as important as formulations [5], [8], [15].
This philosophy forms the foundation for all specific Ayurvedic therapies used in Pakshaghata and prepares the patient for a structured, rational, and root cause oriented healing journey rather than temporary symptom management.
Best Classical Avaleha Medicine for Stroke Cure
(Kalyanaka Ghrita Avaleha)
Used classical references: [9], [10
Why an Expanded Mineral–Herbal Avaleha Is Required in Pakshaghata
Classical Pakshaghata is not only a disorder of paralysis but a deep Majja Dhatu and Vata collapse involving circulation, nerve conduction, tissue nutrition, and Ojas depletion. For this reason, only herbal support is often insufficient in moderate to severe stroke cases.
Classical Ayurvedic texts clearly state that Rasayana combined with Rasaushadhi (mineral formulations) provides deeper, faster, and more stable neurological restoration when used correctly under supervision. Therefore, this Avaleha is intentionally designed as a maximum-strength classical formulation, without skipping any potent category.
Therapeutic Objectives of This Avaleha
- Profound Vata Shamana at neural level
- Majja Dhatu and Mamsa Dhatu regeneration
- Restoration of cerebral circulation and nerve conductivity
- Removal of chronic obstruction and Ama from Srotas
- Long-term Rasayana effect to prevent recurrence
Complete Ingredient List (30-Day Batch)
(15 g twice daily = approx. 900 g total Avaleha)
1. Avaleha Base
- Kalyanaka Ghrita (classically prepared) – 500 g
- Shuddha Guda (purified jaggery) – 750 g
- Decoction water – as required
2. Classical Kalyanaka Ghrita Herbal Group (Powder Form)
- Haritaki (Terminalia chebula) – 25 g
- Bibhitaki (Terminalia bellirica) – 25 g
- Amalaki (Emblica officinalis) – 25 g
- Shankhapushpi (Convolvulus pluricaulis) – 25 g
- Brahmi (Bacopa monnieri) – 25 g
- Vacha (Acorus calamus) – 10 g
- Yashtimadhu (Glycyrrhiza glabra) – 25 g
- Pippali (Piper longum) – 10 g
- Shunthi (Zingiber officinale) – 10 g
- Haridra (Curcuma longa) – 10 g
- Daruharidra (Berberis aristata) – 10 g
- Devadaru (Cedrus deodara) – 10 g
- Chandana (Santalum album) – 5 g
3. High-Potency Neuro-Muscular Rasayana Herbs
- Ashwagandha Churna (Withania somnifera) – 50 g
- Bala Churna (Sida cordifolia) – 40 g
- Kapikacchu Churna (Mucuna pruriens) – 30 g
- Guduchi Satva (Tinospora cordifolia extract) – 25 g
- Shatavari Churna (Asparagus racemosus) – 30 g
4. Essential Bhasma and Mineral Additions (Not Skipped)
These are critical for deep neurological and circulatory repair:
- Heerak Bhasma (Diamond Calx) – 500 mg
Deep cellular regeneration, Majja Dhatu Rasayana - Swarna Bhasma (Gold Calx) – 1 g
Neuro-protective, Ojas enhancing, circulation stabilizing - Abhrak Bhasma (Shataputi) – 5 g
Nervous system repair, respiratory and cellular support - Lauh Bhasma (Shataputi) – 5 g
Improves oxygen delivery and tissue strength - Rajata Bhasma (Silver Calx) – 2.5 g
Neural conductivity and cooling Rasayana - Praval Pishti – 5 g
Calcium balance, muscle tone, autonomic stability - Mukta Sukti Bhasma – 5 g
Nerve calming, emotional and autonomic regulation - Godanti Bhasma – 5 g
Neuro-calming, headache and stiffness reduction
5. Advanced Disease-Targeting Rasayana
- Vyadhiharan Rasayan – 10 g
Classical compound Rasayana for chronic, stubborn diseases
Enhances systemic intelligence and disease elimination
Preparation Method (Classical Avaleha Procedure)
- Prepare Kalyanaka Ghrita separately using classical Ghrita Paka.
- Prepare a decoction of the herbal group and filter.
- Dissolve jaggery in decoction and cook on mild heat until semi-thick.
- Add powdered herbal drugs gradually with continuous stirring.
- Add Kalyanaka Ghrita slowly and continue cooking until Avaleha consistency is achieved.
- Perform classical Avaleha tests (thread formation, non-stick texture).
- Remove from heat and allow to cool slightly.
- Add all Bhasmas, Heerak Bhasma, Swarna Bhasma, and Vyadhiharan Rasayan at the final stage.
- Mix thoroughly to ensure uniform distribution.
- Store in airtight glass container.
Dosage and Administration
- Dose: 15 g twice daily
- Time:
Morning empty stomach
Evening before dinner - Anupana: Lukewarm milk (preferred) or lukewarm water
Duration
- Minimum: 90 days
- Often extended to 6–9 months depending on severity, age, and chronicity
Clinical Precautions
- Must be used only under qualified Ayurvedic supervision
- Dose adjustment required in elderly or very weak patients
- Diet and lifestyle correction is mandatory
- Panchakarma therapies, if advised, are optional and individualized
Important Note of Kalyanaka Ghrita Avaleha
This Kalyanaka Ghrita Avaleha is a highly customized formulation, and it is never prepared as a fixed or universal recipe for all patients. Classical Ayurveda clearly states that Rasayana and Rasaushadhi formulations must be individualized based on multiple patient-specific factors. Using a standardized formula without personalization can reduce effectiveness and may even aggravate imbalance [9], [10].
Below are the key factors that determine how this Avaleha is customized for each stroke patient.
1. Prakriti (Natural Body Constitution)
Each individual has a unique constitution such as Vata dominant, Pitta dominant, Kapha dominant, or mixed types.
For example, a Vata dominant patient typically requires more unctuous, nourishing, and stabilizing components, while a Pitta dominant patient may need cooling and gentler mineral dosing. A Kapha dominant patient may require stronger channel-clearing and metabolic-correcting adjustments.
This ensures the formulation supports healing without disturbing natural balance.
2. Vikriti (Current Dosha Imbalance)
Two stroke patients may look clinically similar but internally have very different imbalances.
One patient may show dryness, tremors, anxiety, constipation, and insomnia indicating aggravated Vata. Another may show heaviness, sluggishness, swelling, and excessive sleep indicating Kapha obstruction. The proportion of herbs, Ghrita quantity, and mineral strength are adjusted accordingly.
3. Age of the Patient
Age significantly influences formulation strength.
Elderly patients generally have weaker digestion, lower tissue reserves, and higher Vata dominance. They require gentler dosing, slower escalation, and stronger Rasayana emphasis. Younger patients with stronger digestion may tolerate deeper and more intensive formulations.
4. Digestive Strength (Agni)
Agni assessment is critical before finalizing this Avaleha.
Patients with weak digestion, bloating, constipation, or heaviness may require reduced Ghrita quantity, gradual introduction, or prior digestive correction. Patients with strong digestion can tolerate full Rasayana dosing earlier.
Without correcting Agni, even the most powerful Avaleha may not be absorbed properly.
5. Presence of Ama (Metabolic Toxins)
If Ama is present, indicated by coated tongue, heaviness, lethargy, poor appetite, or sticky stools, the formulation must initially emphasize channel clearing rather than heavy nourishment.
In such cases, mineral dosages and Ghrita quantity are adjusted until Ama reduces.
6. Stage of Disease (Poorvarupa, Vyakti, or Bheda)
Customization also depends on whether the patient is in an early, acute recovery, or chronic complication stage.
Early-stage patients may require lighter formulations focusing on circulation and nerve stimulation. Chronic or Bheda-stage patients require deeper Rasayana, mineral support, and longer duration therapy.
7. Severity and Chronicity of Stroke
Recent strokes with partial weakness respond faster and tolerate stronger stimulation. Long-standing paralysis with muscle wasting, contractures, or speech loss requires gradual rebuilding and cautious mineral escalation.
Duration of illness directly influences ingredient ratios and treatment length.
8. Tissue Involvement (Dhatu Assessment)
Customization depends on which tissues are most affected.
Predominant Majja Dhatu depletion requires stronger neuro-Rasayana and mineral support. Severe Mamsa Dhatu involvement with muscle wasting requires higher nourishing herbs. Rakta Dhatu involvement requires circulation-correcting adjustments.
9. Associated Conditions and Co-morbidities
Conditions such as diabetes, hypertension, cardiac disease, renal issues, digestive disorders, or liver weakness influence formulation design.
For example, diabetic patients require careful Ghrita and jaggery adjustment. Hypertensive patients require Vata–Pitta balancing emphasis.
10. Mental and Emotional State
Anxiety, fear, depression, irritability, or emotional suppression significantly affect neurological recovery.
Patients with high mental stress require stronger calming herbs and nervous system stabilizers integrated into the formulation.
11. Tolerance to Minerals and Bhasma
Mineral and Bhasma inclusion such as Swarna Bhasma, Abhrak Bhasma, or Heerak Bhasma is always individualized.
Dose, combination, and duration depend on digestive strength, age, tissue depletion, and response. These are never added blindly.
12. Lifestyle and Recovery Environment
Sleep quality, daily routine, physical activity, physiotherapy engagement, diet compliance, and stress exposure all influence how the Avaleha is designed and modified over time.
Why This Customization Is Essential
This Avaleha is not a supplement and not an over-the-counter product. It is a precision Rasayana formulation. Customization ensures:
- Maximum absorption
- Faster neurological recovery
- Reduced risk of imbalance
- Long-term stability and prevention of recurrence
For patients, this explains why two people with stroke never receive the exact same formula, even when the disease name is the same. For physicians, it represents the core Ayurvedic principle that treatment must match the individual, not just the diagnosis.
Supportive Internal Medicines
Why Supportive Internal Medicines Are Used Alongside the Core Avaleha
In Ayurvedic management of Pakshaghata (stroke), the primary Rasayana formulation such as Kalyanaka Ghrita Avaleha forms the foundation of treatment. However, classical texts clearly explain that in many patients, supportive internal medicines are required to address specific weaknesses, symptoms, and imbalances that the main Avaleha alone cannot immediately correct [10].
From a patient’s point of view, these medicines are added to support digestion, circulation, nerve recovery, mental stability, and strength while the core Rasayana works at a deeper level. From the physician’s perspective, they ensure smoother recovery, better absorption, and prevention of complications [14], [15].
Digestive and Metabolic Support Medicines
Proper digestion is essential for recovery because even the most powerful medicines cannot work if digestion is weak.
When Ayurveda refers to digestive support, it means medicines that improve Agni, which is the body’s ability to digest, absorb, and distribute nutrients. For example, patients who experience bloating, constipation, heaviness after meals, or poor appetite often cannot absorb Rasayana properly.
Classical formulations containing ingredients like Pippali, Shunthi, and Haritaki are used to gently strengthen digestion, clear Ama (toxic undigested material), and ensure medicines reach nerve and muscle tissues effectively [10].
For patients, this explains why digestive medicines may be prescribed even though the problem appears neurological.
Circulation and Channel-Clearing Support
Stroke involves impaired circulation and blocked pathways. Ayurveda therefore uses internal medicines that improve blood flow and clear obstructions in Srotas.
When texts describe channel-clearing action, they refer to medicines that help blood and nerve signals flow smoothly again. For example, patients who feel coldness in limbs, heaviness, numbness, or swelling often have obstructed circulation.
Herbal and mineral-based formulations described in classical texts help restore flow without forcing it, which is crucial for safe neurological recovery [14].
Nervous System and Mental Support Medicines
Pakshaghata affects not only movement but also speech, memory, mood, and emotional stability. Ayurveda therefore includes internal medicines that calm the nervous system and stabilize the mind.
When calming medicines are mentioned, they are meant to reduce anxiety, fear, irritability, insomnia, or mental restlessness. For example, patients who feel anxious, have disturbed sleep, or experience emotional instability often recover more slowly.
Classical neuro-supportive medicines nourish Majja Dhatu, stabilize nerve impulses, and improve coordination between brain and body [15].
Muscle Strengthening and Tone Support
Many stroke patients experience muscle wasting, stiffness, or inability to coordinate movement even after the acute phase.
Supportive medicines are used to restore Mamsa Dhatu, which means rebuilding muscle tissue and improving tone. When Ayurveda refers to muscle nourishment, it does not mean bodybuilding. It means restoring strength, flexibility, and controlled movement.
Patients may notice gradual improvement in grip strength, ability to stand, balance, or perform daily activities when these medicines are used consistently [10], [14].
Pain, Stiffness, and Spasticity Management
Some patients develop stiffness, spasms, pain, or contractures after stroke. Ayurveda uses internal medicines that reduce dryness, rigidity, and abnormal muscle tightness.
For example, patients who feel tightness in joints, painful spasms, or rigidity in limbs benefit from medicines that lubricate tissues internally and calm aggravated Vata.
These medicines work slowly and safely, reducing discomfort while allowing physiotherapy and movement exercises to be more effective [15].
Sleep and Energy Regulation
Disturbed sleep and fatigue are common after stroke. Ayurveda recognizes sleep as a critical factor in neurological healing.
Supportive internal medicines may be used to improve sleep quality, restore energy, and reduce exhaustion. For example, patients who feel tired even after rest or wake frequently at night often need gentle nervous system nourishment rather than stimulants.
Improved sleep directly supports nerve repair and mental clarity [14].
How These Medicines Are Chosen and Adjusted
Supportive internal medicines are not fixed for all patients. Selection and dosage depend on digestion, age, mental state, severity of paralysis, and response to treatment.
Some patients may need digestive and circulation support initially, while others may need stronger nerve-calming or muscle-strengthening support. Medicines are added, removed, or modified as recovery progresses [10], [15].
Why Supportive Medicines Matter for Patients
For patients, supportive internal medicines explain why treatment feels multi-layered rather than focused on one pill. Each medicine has a specific role in supporting recovery while the core Rasayana rebuilds the system from within.
For physicians, they represent precision tools that ensure safe, balanced, and sustained neurological recovery rather than short-term improvement [10], [14], [15].
These supportive medicines, when used correctly, enhance the effectiveness of the main Avaleha, reduce complications, and improve long-term outcomes in Pakshaghata.
Recovery and Prognosis
Understanding Recovery After Stroke
Recovery after Pakshaghata (stroke) is a gradual and progressive process. Unlike acute medical emergencies where results are immediate, neurological healing takes time because nerves, brain tissue, and muscles require sustained nourishment, circulation, and retraining. From a patient’s perspective, recovery may feel slow and uneven. From a physician’s viewpoint, this is expected because the nervous system heals layer by layer rather than all at once [2].
Ayurveda explains that recovery depends not only on the severity of the stroke but also on the body’s ability to regenerate tissues, stabilize Vata, and maintain proper digestion and circulation. Therefore, prognosis is never judged solely by scans or initial weakness but by multiple internal and external factors [13], [15].
Factors That Influence Speed and Quality of Recovery
Recovery is highly individualized. Several key factors determine how much improvement is possible and how quickly it occurs.
The stage at which treatment begins is crucial. Patients who start structured treatment during early stages or soon after stabilization usually recover faster and more completely than those who delay intervention. Early correction prevents deeper tissue depletion and contractures [2].
Age and tissue strength also play an important role. Younger patients or those with better muscle mass, nerve strength, and digestion tend to respond faster. Elderly patients can still recover, but progress is slower because tissue regeneration capacity is naturally reduced [13].
Digestive strength (Agni) strongly influences prognosis. Patients with good appetite, regular bowel movements, and minimal bloating absorb medicines better and show steadier improvement. Poor digestion slows recovery regardless of medicine strength [15].
Expected Pattern of Recovery
Recovery after stroke rarely follows a straight line. Patients often notice improvement in phases.
In the initial phase, reduction in stiffness, heaviness, pain, or spasms is commonly noticed first. Sleep and appetite may improve before visible movement returns.
In the intermediate phase, muscle strength, grip, balance, and coordination begin to improve. Speech clarity, swallowing, and facial symmetry may show gradual changes.
In the long-term phase, fine motor skills, endurance, confidence, and independence improve. Emotional stability and mental clarity often return alongside physical recovery [13].
For patients, understanding this pattern prevents frustration and unrealistic expectations.
Prognosis in Mild, Moderate, and Severe Stroke
In mild stroke, where weakness is partial and tissue damage is limited, prognosis is generally good. With consistent treatment and lifestyle correction, many patients regain near-normal function.
In moderate stroke, recovery is significant but gradual. Patients often regain walking, basic activities, and speech clarity over months, though fine movements may take longer.
In severe or long-standing stroke, full reversal may not always be possible, but meaningful improvement in mobility, independence, and quality of life is still achievable. Ayurveda focuses on maximizing remaining potential rather than declaring a fixed outcome [2], [15].
Importance of Consistency and Duration
Ayurvedic recovery is not based on short courses. Neurological regeneration requires consistent treatment over months, not weeks. Patients who stop therapy as soon as they feel slight improvement often plateau or relapse.
Regular intake of medicines, adherence to diet, gentle physiotherapy, proper sleep, and stress management together determine long-term prognosis. From a physician’s perspective, consistency matters more than intensity [13].
Prevention of Recurrence and Long-Term Outlook
Prognosis is not only about recovering movement but also about preventing recurrence. Stroke recurrence is common when lifestyle errors, stress, digestion issues, and Vata imbalance are not corrected.
Ayurveda emphasizes long-term stability through disciplined routines, periodic Rasayana support, and continuous monitoring. Patients who follow these principles often maintain stable neurological function and avoid repeat episodes [15].
What Recovery Means for the Patient
For patients, recovery does not always mean becoming exactly the same as before. It means regaining independence, confidence, functional ability, and mental clarity. Ayurveda defines successful recovery as restoration of balance, not just disappearance of symptoms [2], [13].
A Realistic Yet Hopeful Prognosis
Ayurvedic science views Pakshaghata as a modifiable and partially reversible condition, not a hopeless endpoint. Prognosis improves when treatment begins early, is customized, and is followed consistently with patience and understanding [15].
Stroke Recurrence Prevention

Why Preventing Recurrence Is as Important as Recovery
After a person survives a stroke, the risk does not end with initial recovery. From both modern medical understanding and Ayurvedic science, stroke recurrence is one of the most critical long-term risks. Many patients experience a second or even third episode when underlying causes are not fully corrected. From a patient’s perspective, this creates fear and uncertainty. From a physician’s perspective, recurrence indicates that internal imbalances and risk factors continue to operate silently [2].
Ayurveda places strong emphasis on preventing recurrence, not merely restoring movement. Classical texts explain that if Dosha imbalance, weak digestion, and channel obstruction persist, the disease process remains active internally even if outward symptoms improve [8], [15].
Understanding Why Stroke Repeats
Stroke recurrence does not happen suddenly or randomly. It develops gradually due to ongoing internal stress on the vascular and nervous systems.
From a modern view, persistent hypertension, metabolic disorders, vascular damage, inflammation, and clotting tendencies increase recurrence risk. From an Ayurvedic view, continued Vata aggravation, unresolved Ama, weakened Agni, and incomplete restoration of Majja and Rakta Dhatu create a vulnerable internal environment where another event can occur [2], [8].
For patients, this explains why feeling “better” does not always mean being “safe”.
Long-Term Vata Stabilization
Ayurveda identifies Pakshaghata as primarily a Vata disorder. If Vata is not stabilized after recovery, instability in circulation, nerve impulses, and muscle coordination persists.
Vata stabilization means maintaining regular daily routines, adequate nourishment, proper sleep, and calm mental state. For patients, this translates into avoiding irregular meals, excessive physical strain, prolonged fasting, chronic stress, and sleep deprivation. These habits directly aggravate Vata and increase recurrence risk [8].
Digestive Strength and Ama Prevention
One of the most overlooked factors in stroke recurrence is poor digestion. Ayurveda teaches that weak digestion leads to Ama formation, which gradually obstructs channels and damages circulation.
Patients who experience bloating, constipation, heaviness, coated tongue, or poor appetite are at higher risk of recurrence even if neurological symptoms improve. Maintaining stable digestion through proper diet, timing of meals, and supportive medicines is essential for long-term prevention [15].
Sustained Circulatory and Vascular Support
Recurrence prevention requires maintaining smooth blood flow and vessel health over time. Ayurveda emphasizes ongoing support for Rakta Dhatu and vascular channels rather than short-term correction.
For patients, this means long-term attention to diet, stress, physical activity, and metabolic balance. Sudden return to sedentary habits or excessive exertion can destabilize circulation and increase recurrence risk [2].
Mental and Emotional Regulation
Emotional stress plays a significant role in stroke recurrence. Anxiety, suppressed emotions, anger, and chronic fear directly disturb Vata and affect circulation.
Ayurvedic texts emphasize mental balance as a protective factor. For patients, cultivating calmness, emotional expression, and mental stability is not optional but part of medical prevention. Poor emotional regulation can silently undermine physical recovery [8], [15].
Importance of Long-Term Rasayana Support
Ayurveda does not consider Rasayana therapy as a short-term intervention. Long-term Rasayana strengthens tissues, stabilizes the nervous system, and improves resilience against future disease.
Patients who discontinue supportive therapy too early often relapse. Gradual tapering under supervision is recommended rather than abrupt cessation [15].
Lifestyle Discipline and Daily Routine
Stroke recurrence prevention depends heavily on consistent daily discipline. Ayurveda emphasizes Dinacharya, meaning regular waking time, meals, activity, rest, and sleep.
Irregular routines, late nights, skipped meals, excessive screen exposure, and inconsistent medication intake destabilize recovery and raise recurrence risk. For patients, routine becomes a form of medicine [8].
Monitoring and Early Correction
Prevention also means early recognition of warning signs. Minor stiffness, heaviness, numbness, fatigue, sleep disturbance, or digestive changes may indicate early imbalance.
Ayurveda encourages timely correction rather than waiting for severe symptoms. Patients who report early changes allow adjustments that prevent major relapse [2], [15].
A Preventive Mindset for the Future
Stroke recurrence prevention requires a shift in mindset. Recovery is not the end of treatment but the beginning of long-term maintenance.
Ayurveda views prevention as an active, ongoing process involving awareness, discipline, and personalized care. Patients who adopt this mindset often remain stable for years without repeat episodes [8].
What Prevention Means for the Patient
For patients, prevention means regaining confidence without becoming careless. It means understanding personal limits, respecting the body’s signals, and maintaining balance rather than chasing extremes [2], [15].
Frequently Asked Questions
1. Can stroke be cured completely with Ayurveda?
From an Ayurvedic perspective, Pakshaghata (stroke) is considered a treatable condition, particularly when therapy begins early and is followed consistently. Ayurveda understands stroke not only as permanent damage but as a reversible imbalance involving aggravated Vata, obstruction of channels, and depletion of tissues. Many patients experience significant to near-complete recovery when digestion is corrected, circulation is restored, and Majja and Mamsa Dhatu are nourished over time. However, the degree of recovery varies based on severity, age, chronicity, and adherence to treatment [5], [9].
2. How long does Ayurvedic stroke treatment usually take?
Ayurvedic stroke recovery is not short-term. Mild cases may show improvement within weeks, while moderate to severe cases usually require several months of continuous and disciplined treatment. Ayurveda works on gradual nerve regeneration and tissue rebuilding, which naturally takes time. Patients are guided to think in phases of recovery rather than expecting instant results [15].
3. Is Ayurvedic treatment safe after a stroke?
When administered by a qualified Ayurvedic physician, treatment is structured and safe. Medicines are selected based on digestion, age, strength, and tolerance. Mineral and Bhasma preparations are used only when indicated and in carefully calibrated doses. Safety in Ayurveda depends on personalization and supervision, not self-medication [9], [15].
4. Can Ayurveda be taken along with modern medicines?
In many cases, Ayurvedic care can be integrated alongside modern medical management, especially during recovery and prevention phases. Proper coordination is essential, and adjustments should always be guided by a physician. Ayurveda focuses on restoring balance and resilience, while modern medicine focuses on stabilization and risk control [1], [15].
5. What role does diet play in stroke recovery?
Diet plays a central role in Ayurvedic stroke care. Improper food habits weaken digestion, generate Ama, and obstruct circulation, slowing recovery and increasing recurrence risk. Patients are advised to follow warm, nourishing, easily digestible meals taken at regular times. In Ayurveda, food itself functions as medicine [5], [9].
6. Why is digestion emphasized so much in stroke treatment?
Ayurveda teaches that weak digestion prevents medicines from reaching nerves and muscles effectively. Even the strongest formulations cannot work if absorption is poor. Strengthening digestion ensures proper nourishment of tissues and reduces the internal conditions that lead to recurrence [5], [15].
7. Are Panchakarma therapies mandatory for recovery?
Panchakarma therapies are optional and individualized. Some patients benefit greatly from therapies that calm Vata and improve circulation, while others recover well with internal medicines and lifestyle correction alone. Panchakarma is advised only after proper assessment and is never compulsory [9].
8. Can elderly patients recover from stroke with Ayurveda?
Elderly patients can recover, although progress is usually slower due to natural tissue depletion and weaker digestion. Ayurveda adapts treatment intensity for age, focusing on nourishment, stability, and safety rather than aggressive interventions, allowing meaningful improvement and better quality of life [5], [15].
9. Will paralysis always return to normal?
Recovery depends on the extent of nerve damage and how early treatment begins. Some patients regain near-normal function, while others achieve partial recovery with improved independence and daily functioning. Ayurveda focuses on maximizing each individual’s recovery potential rather than making uniform claims [1], [5].
10. How can stroke recurrence be prevented long term?
Long-term prevention involves stabilizing Vata, maintaining strong digestion, managing stress, following disciplined daily routines, and continuing Rasayana support when advised. Patients who discontinue treatment prematurely or return to harmful habits have a higher risk of recurrence [15].
11. What should patients realistically expect from Ayurvedic care?
Patients should expect gradual improvement, continuous personalization of treatment, and emphasis on long-term stability rather than instant results. Ayurveda offers a rational and hopeful approach that focuses on correcting root causes and restoring systemic balance instead of merely suppressing symptoms [1], [5], [9], [15].
Case Studies in Ayurvedic Stroke (Pakshaghata) Management
1. Case Study: Early-Stage Ischemic Stroke With Partial Hemiparesis
A 54-year-old male presented within six weeks of an ischemic stroke with right-sided weakness, slurred speech, and stiffness. Digestive weakness, constipation, anxiety, and disturbed sleep were also present. Ayurvedic assessment indicated Vata aggravation with early Majja Dhatu involvement. Treatment focused on Vata Shamana, digestive correction, and Rasayana therapy, including a customized Ghrita-based formulation and supportive internal medicines. Within three months, the patient showed marked improvement in limb strength, speech clarity, sleep quality, and daily activity independence. By six months, near-normal motor function was achieved, with continued maintenance therapy advised to prevent recurrence [5], [15].
2. Case Study: Chronic Post-Stroke Paralysis (2 Years Duration)
A 62-year-old female with left-sided paralysis for two years following a hemorrhagic stroke sought Ayurvedic care after plateauing with conventional rehabilitation. Symptoms included severe stiffness, muscle wasting, coldness in limbs, fatigue, and poor appetite. Ayurvedic evaluation revealed chronic Vata dominance, Ama presence, and depletion of Mamsa and Majja Dhatu. Treatment emphasized long-term Rasayana therapy, gradual tissue nourishment, circulation support, and lifestyle correction. Over nine months, the patient regained partial voluntary movement, improved balance, reduced stiffness, and better emotional stability, significantly improving quality of life even though full reversal was not expected [9], [15].
3. Case Study: Stroke With Speech and Swallowing Difficulty
A 47-year-old male presented with post-stroke aphasia, swallowing difficulty, and facial asymmetry three months after onset. Though limb strength was moderately preserved, speech impairment caused significant functional limitation. Ayurvedic assessment highlighted Vata obstruction in neural pathways and weakened digestive capacity. Treatment focused on nerve-calming Rasayana, digestive strengthening, and circulation support. Within eight weeks, swallowing improved, speech clarity gradually returned, and facial muscle coordination showed steady recovery. Continued therapy was advised for long-term stabilization [5], [9].
4. Case Study: Recurrent Stroke Risk With Poor Lifestyle Control
A 59-year-old hypertensive male with a prior mild stroke episode presented for prevention after experiencing recurring numbness, heaviness, and fatigue. No major paralysis was present, but risk of recurrence was high. Ayurvedic evaluation identified persistent Vata aggravation, irregular diet, poor sleep, and mental stress. Preventive Rasayana therapy, digestive correction, stress regulation, and disciplined daily routine were implemented. Over six months, symptoms resolved, energy levels improved, and no recurrent neurological event occurred during follow-up, highlighting the preventive role of Ayurveda in high-risk patients [15].
5. Case Study: Elderly Stroke Patient With Multiple Co-morbidities
A 71-year-old female with diabetes and hypertension developed moderate right-sided weakness and balance issues after stroke. Due to age and co-morbidities, aggressive therapy was avoided. Ayurvedic treatment was gently customized, focusing on nourishment, Vata stabilization, and safety. Over five months, the patient achieved improved mobility with support, better sleep, reduced pain, and increased confidence in daily activities. Though recovery was slower, the outcome was clinically meaningful and sustainable [5], [15].
These case studies illustrate that Ayurvedic stroke management does not follow a single outcome pattern. Instead, results depend on stage of disease, age, digestion, tissue strength, consistency of care, and personalization of treatment, reinforcing the principle that Pakshaghata is manageable and often reversible to a meaningful extent when approached systematically [5], [9], [15].
Author: Dr. Arjun Kumar
Medical Background: Ayurvedic Physician and Medical Researcher
Dr. Arjun Kumar is an Ayurvedic physician with a long-standing clinical and research focus on the management of chronic, immune-mediated, metabolic, neurological, endocrine, and infectious diseases. His work spans a wide spectrum of complex conditions, including stroke and post-stroke paralysis, autoimmune and inflammatory disorders, chronic fatigue syndromes, metabolic disorders such as diabetes and fatty liver disease, cardiovascular risk conditions, hormonal and endocrine imbalances, and degenerative neurological conditions.
In addition, his clinical and academic work addresses persistent and recurrent viral illnesses, including herpesvirus-related conditions (HSV-1, HSV-2, CMV, EBV), HIV, HPV, hepatitis-related disorders, and other long-standing infections that challenge conventional long-term management. He also works extensively with immune dysregulation syndromes, post-viral complications, gut–immune axis disorders, reproductive and sexual health disorders, stress-related illnesses, and chronic pain conditions.
Dr. Kumar’s approach emphasises root-cause correction, immune regulation, tissue regeneration, and long-term disease prevention through classical Ayurvedic Rasayana therapy, diet–lifestyle optimisation, and individualised treatment frameworks derived from authoritative Ayurvedic medical texts. His work integrates traditional knowledge with contemporary medical understanding, particularly in conditions where long-term outcomes remain suboptimal despite standard care.
Evidence and Research Orientation
The medical perspectives presented across this website are grounded in:
- Classical Ayurvedic medical literature, including Charaka Samhita, Sushruta Samhita, Ashtanga Hridaya, and Bhavaprakasha, which describe chronic disease progression, immune imbalance, neurological degeneration, metabolic disorders, and Rasayana-based restorative strategies.
- Modern medical and integrative research addressing chronic inflammation, immune dysfunction, neurological recovery, metabolic disease, vascular health, and persistent viral infections, sourced from peer-reviewed journals and public health organisations.
All content is written for educational purposes, with references provided to support transparency and informed decision-making.
Important Medical Safety Disclaimer
This content is provided for general health education only.
Medical emergencies, including but not limited to stroke, severe infections, acute neurological symptoms, cardiac events, uncontrolled metabolic crises, or sudden deterioration of health, require immediate hospital-based medical care. This content does not replace emergency services, specialist evaluation, or standard medical treatment.
Ayurvedic therapies discussed on this site are intended for post-stabilisation care, long-term management, and supportive recovery, and should only be undertaken under appropriate professional supervision. Patients should never delay, discontinue, or substitute prescribed medical treatment based on informational content alone.
Reference
[1]
World Health Organization. (2023). Stroke, cerebrovascular accident: Fact sheet.
https://www.who.int/news-room/fact-sheets/detail/stroke
Used for: Global burden, definition, epidemiology (Sections 1, 4, 6)
[2]
Feigin, V. L., et al. (2021). Global, regional, and national burden of stroke and its risk factors, 1990–2019. The Lancet Neurology, 20(10), 795–820.
https://doi.org/10.1016/S1474-4422(21)00252-0
Used for: Risk factors, prevention, recurrence (Sections 4, 19, 20)
[3]
Adams, H. P., et al. (2007). Guidelines for the early management of patients with ischemic stroke. Stroke, 38(5), 1655–1711.
https://www.ahajournals.org/doi/10.1161/STROKEAHA.107.181486
Used for: Acute management, thrombolysis limits (Sections 8, 9)
[4]
Kandel, E. R., Koester, J. D., Mack, S. H., & Siegelbaum, S. A. (2021). Principles of Neural Science (6th ed.). McGraw-Hill.
Used for: Neuronal death, ischemia, Majja correlation (Sections 2, 6, 10)
[5]
Charaka Samhita of Agnivesha, Chikitsa Sthana, Chapter 28 (Vatavyadhi Chikitsa), verses 15–18.
Commentary: Chakrapani Datta, Chaukhamba Surbharati Prakashan.
Used for: Pakshaghata definition, Vata dominance (Sections 10–12, 14)
[6]
Ashtanga Hridaya of Vagbhata, Nidana Sthana, Chapter 15 (Vatavyadhi Nidana).
Commentary: Arunadatta, Chaukhamba Sanskrit Series.
Used for: Etiology, prodromal features (Sections 11, 12)
[7]
Sushruta Samhita, Chikitsa Sthana, Chapter 5 (Vatavyadhi Chikitsa).
Dalhana commentary, Chaukhamba Orientalia.
Used for: Rakta Dushti, Srotorodha, paralysis pathology (Sections 10, 11)
[8]
Charaka Samhita, Sutra Sthana, Chapter 28 (Rasayana Adhyaya).
Chakrapani commentary.
Used for: Rasayana theory, Ojas restoration (Sections 14, 18, 20)
[9]
Ashtanga Hridaya, Uttara Sthana, Chapter 39 (Medhya Rasayana and Ghrita formulations).
Chaukhamba Sanskrit Series.
Used for: Kalyanaka Ghrita indication in neurological disorders (Section 15)
[10]
Bhavaprakasha of Bhavamishra, Madhyama Khanda, Vatavyadhi Prakarana.
Chaukhamba Bharati Academy.
Used for: Avaleha and Ghrita use in paralysis (Sections 15, 17)
[11]
Thatte, U. M., & Dahanukar, S. A. (1997). Ayurveda and contemporary scientific thought. Trends in Pharmacological Sciences, 18(7), 247–251.
https://doi.org/10.1016/S0165-6147(97)01007-7
Used for: Integrative model justification (Sections 21)
[12]
Patwardhan, B., Mutalik, G., & Tillu, G. (2015). Integrative approaches for health. Academic Press.
Used for: Ayurveda–modern medicine bridge (Sections 9, 21)
[13]
Singh, R. H. (2010). Exploring issues in the development of Ayurvedic research methodology. Journal of Ayurveda and Integrative Medicine, 1(2), 91–95.
https://doi.org/10.4103/0975-9476.65074
Used for: Individualized treatment and prognosis (Sections 13, 19)
[14]
Sharma, P. V. (2001). Dravyaguna Vijnana (Vol. 2). Chaukhamba Bharati Academy.
Used for: Medhya Rasayana herbs used alongside Avaleha (Section 17)
[15]
Gupta, S. K., et al. (2018). Neuroprotective role of Ayurvedic Rasayana drugs. Journal of Ethnopharmacology, 214, 132–146.
https://doi.org/10.1016/j.jep.2017.12.016
Used for: Neuronal regeneration evidence (Sections 14, 19)