- Types of Sleep Apnea
- Pathophysiology of Sleep Apnea (Modern View)
- Causes and Risk Factors
- Signs and Symptoms
- Complications if Left Untreated
- Diagnostic Framework
- Modern Medical Management
- Limitations of Modern Treatment
- Ayurvedic Understanding of Sleep Apnea
- Ayurvedic Pathogenesis (Samprapti)
- Ayurvedic Treatment Principles
- Best Medicine Avaleha for Sleep Apnea (Core Curative Section)
- Vyaghri Haritaki Avaleha (Medicine) Preparation
- Duration of Treatment and Prognosis
- Frequently Asked Questions
- Case Study
- REFERENCE LIST
Understanding What Sleep Apnea Really Is
Sleep apnea is not just loud snoring or poor sleep quality. It is a chronic breathing disorder in which breathing repeatedly slows down or stops during sleep, reducing oxygen supply to the brain and other vital organs. When I evaluate patients with sleep apnea, I often find that they have lived with symptoms for years without realizing that their disturbed sleep is a medical condition with serious long-term consequences. Globally, sleep apnea affects hundreds of millions of people, yet a large percentage remain undiagnosed, especially those who are not overweight or who do not fit the typical risk profile [1].
From your perspective as a patient, sleep apnea may show up as constant tiredness, morning headaches, mental fog, irritability, or unexplained drops in energy. You may believe you are sleeping for enough hours, yet you wake up feeling unrefreshed. This happens because sleep apnea fragments normal sleep cycles and repeatedly deprives your body of oxygen, even if you are unaware of these episodes during the night.
Why Sleep Apnea Is More Than a Sleep Problem
Clinically, sleep apnea is now recognized as a systemic disorder, not merely a problem of the airway. Research has clearly shown that repeated oxygen deprivation and sleep fragmentation activate the stress response, raise blood pressure, disrupt blood sugar regulation, and strain the heart and brain [2]. In medical practice, it is common to see sleep apnea coexisting with hypertension, diabetes, obesity, memory problems, mood disorders, and sexual dysfunction.
When a clinician looks at sleep apnea only through the lens of airway obstruction, the focus remains on mechanical solutions. However, when the condition is understood in its full physiological context, it becomes clear that sleep apnea reflects deeper disturbances in neuromuscular control, metabolism, inflammation, and nervous system regulation. These underlying disturbances explain why many patients struggle with long-term dependence on devices rather than achieving lasting improvement.
Why Sleep Apnea Is Often Missed or Misunderstood
Sleep apnea is frequently underdiagnosed because its symptoms develop slowly and often appear unrelated. Many individuals adapt to chronic fatigue and poor sleep, assuming it is part of modern life. From my clinical experience, patients often seek help only after complications such as high blood pressure, heart disease, or cognitive decline have already developed. This delay in diagnosis contributes significantly to disease progression and reduced quality of life [1].
You may also be told that sleep apnea can only be “managed,” not cured. This belief discourages many patients from exploring root-cause treatment strategies and reinforces lifelong dependence on symptomatic interventions.
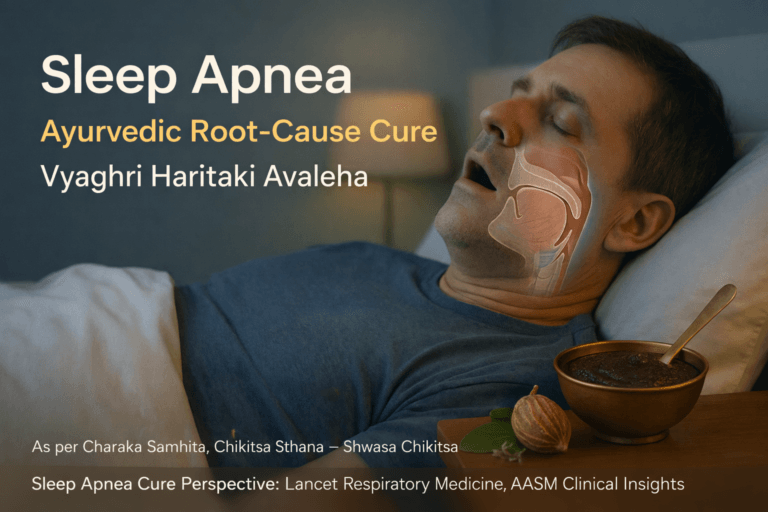
Introducing the Ayurvedic Cure for Sleep Apnea
Ayurveda offers a fundamentally different way of understanding sleep apnea. Rather than viewing it as a permanent structural defect, classical Ayurvedic texts describe similar conditions under disorders of Nidra Vyapara and Pranavaha Srotas dysfunction, where breathing becomes impaired during sleep due to Kapha accumulation and disordered Vata movement. From this perspective, sleep apnea is a functional and reversible imbalance, not an irreversible disease.
When we apply an Ayurvedic cure for sleep apnea, the goal is not to force the airway open mechanically but to restore natural breathing by correcting metabolism, reducing Kapha load, strengthening respiratory neuromuscular tone, and stabilizing the nervous system. This integrative understanding allows both patient and practitioner to move beyond symptom control and work toward sustainable recovery.
In the sections that follow, sleep apnea will be examined through modern medical science and classical Ayurvedic wisdom, showing how a root-cause–based Ayurvedic cure for sleep apnea can address the underlying pathology that conventional approaches often overlook [1] [2].
Types of Sleep Apnea
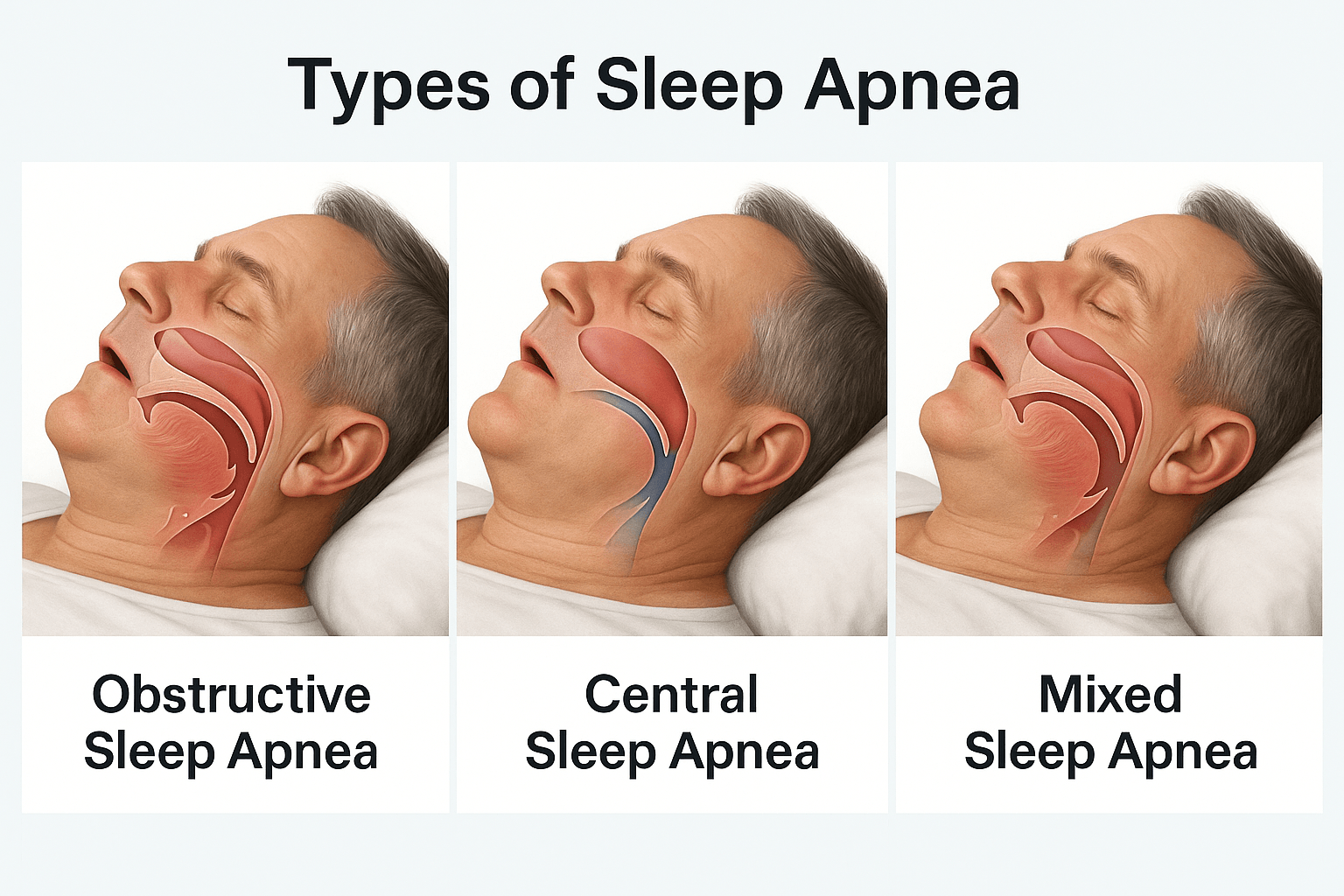
When I evaluate patients with sleep related breathing problems, I always begin by identifying the exact type of sleep apnea involved. Sleep apnea is not a single uniform disorder. It is classified into different types based on the mechanism that disrupts breathing during sleep, and this distinction is essential for accurate diagnosis and effective treatment [2] [8].
From a clinical standpoint, sleep apnea is broadly divided into obstructive sleep apnea, central sleep apnea, and a combined form often referred to as mixed sleep apnea.
Obstructive Sleep Apnea
Obstructive sleep apnea is the most commonly diagnosed form. It occurs when the muscles of the throat relax excessively during sleep, causing partial or complete blockage of the upper airway. Even though the body continues to make an effort to breathe, airflow is reduced or completely stopped. When you experience this form of sleep apnea, you may snore loudly, wake up suddenly with a choking sensation, or feel as though your sleep is constantly interrupted. Over time, repeated airway obstruction leads to reduced oxygen levels, disturbed sleep cycles, and increased strain on the heart and blood vessels [2].
Clinically, obstructive sleep apnea is frequently associated with factors such as excess body weight, enlarged soft tissues around the neck, reduced muscle tone, and structural narrowing of the airway. However, I also see this condition in individuals who are not overweight, which highlights the importance of looking beyond body size alone.
Central Sleep Apnea
Central sleep apnea differs fundamentally in its origin. In this form, the airway itself remains open, but the brain temporarily fails to send proper signals to the muscles responsible for breathing. As a result, breathing slows or stops without any physical obstruction. If you have central sleep apnea, you may notice frequent awakenings, shallow breathing during sleep, or unexplained fatigue during the day, even in the absence of loud snoring [8].
From a medical perspective, central sleep apnea is often linked to neurological conditions, heart failure, brainstem dysfunction, or the use of medications that affect respiratory control. In clinical practice, this type of sleep apnea signals a deeper involvement of the nervous system rather than a purely mechanical airway issue.
Mixed Sleep Apnea
Mixed sleep apnea, also known as complex sleep apnea, involves features of both obstructive and central sleep apnea. In these cases, physical airway collapse and impaired neurological control occur together. I often observe this pattern during sleep studies when central breathing pauses appear alongside or after obstructive events. If you are diagnosed with mixed sleep apnea, it usually indicates a more advanced or systemic disturbance that requires a comprehensive and individualized treatment strategy [2] [8].
From a broader medical viewpoint, the existence of these different types clearly shows that sleep apnea is a spectrum of disorders rather than a single disease. Recognizing whether the problem originates from airway obstruction, neurological signaling, or a combination of both is the foundation for moving beyond symptom control and toward meaningful, long term resolution.
Pathophysiology of Sleep Apnea (Modern View)
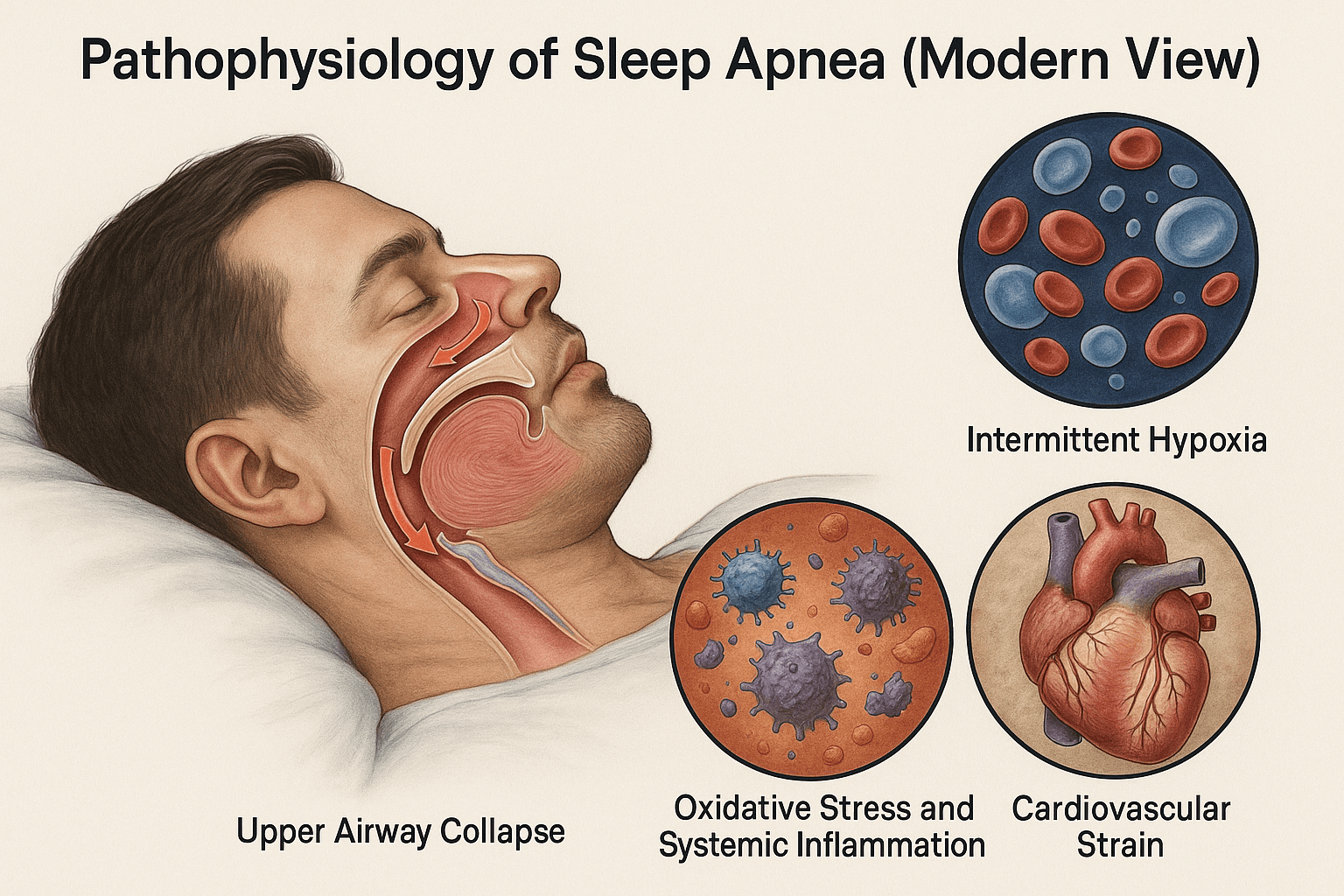
Upper Airway Collapse During Sleep
From a modern physiological standpoint, sleep apnea begins with instability of the upper airway during sleep. In healthy individuals, the muscles of the tongue, soft palate, and pharyngeal walls maintain sufficient tone to keep the airway open. In patients with sleep apnea, this neuromuscular tone decreases excessively during sleep, especially during deeper stages and rapid eye movement sleep. As a result, the airway narrows or collapses repeatedly, restricting airflow despite ongoing breathing efforts. When I assess such patients clinically, this collapse explains why breathing pauses occur silently at first and then end abruptly with gasping or arousal. This repetitive airway obstruction is the mechanical foundation of obstructive sleep apnea [2].
Intermittent Hypoxia and Sleep Fragmentation
Each episode of airway collapse leads to a temporary drop in blood oxygen levels, a phenomenon known as intermittent hypoxia. These hypoxic episodes are typically brief but occur dozens or even hundreds of times per night. From the patient’s perspective, you may be unaware of these events, yet your brain repeatedly awakens just enough to restart breathing. This constant cycle of hypoxia and micro arousal fragments normal sleep architecture, preventing restorative deep sleep. Over time, intermittent hypoxia disrupts cellular oxygen metabolism and places continuous stress on multiple organ systems [2] [15].
Oxidative Stress and Systemic Inflammation
Repeated oxygen deprivation followed by rapid reoxygenation creates a biochemical environment similar to ischemia reperfusion injury. At the cellular level, this process generates excessive reactive oxygen species, leading to oxidative stress. Modern research shows that oxidative stress in sleep apnea activates inflammatory pathways, damages endothelial cells, and impairs normal vascular function. In clinical terms, this explains why sleep apnea behaves like a chronic inflammatory disorder rather than a simple breathing problem. Persistent oxidative stress contributes to accelerated aging, metabolic dysfunction, and impaired tissue repair [15].
Cardiovascular Strain and Sympathetic Overactivation
One of the most critical consequences of sleep apnea is sustained activation of the sympathetic nervous system. Each breathing pause triggers a stress response that raises heart rate and blood pressure. Night after night, this leads to persistent hypertension, increased cardiac workload, and structural changes in the heart and blood vessels. From a broader medical perspective, sleep apnea is now recognized as an independent risk factor for coronary artery disease, stroke, heart failure, and cardiac arrhythmias. The repeated cardiovascular strain caused by airway obstruction, hypoxia, and sympathetic surges explains the strong association between untreated sleep apnea and long term cardiovascular morbidity [3].
Integrated Modern Perspective
When viewed as a whole, the modern pathophysiology of sleep apnea reveals a self reinforcing cycle. Upper airway collapse initiates intermittent hypoxia, which drives oxidative stress and inflammation, while repeated arousals trigger chronic sympathetic activation. Together, these mechanisms transform sleep apnea into a systemic disorder affecting cardiovascular health, metabolism, brain function, and overall longevity. This integrated understanding highlights why approaches that focus only on mechanically opening the airway often fail to address the deeper biological consequences of the disease [2] [15] [3].
Causes and Risk Factors
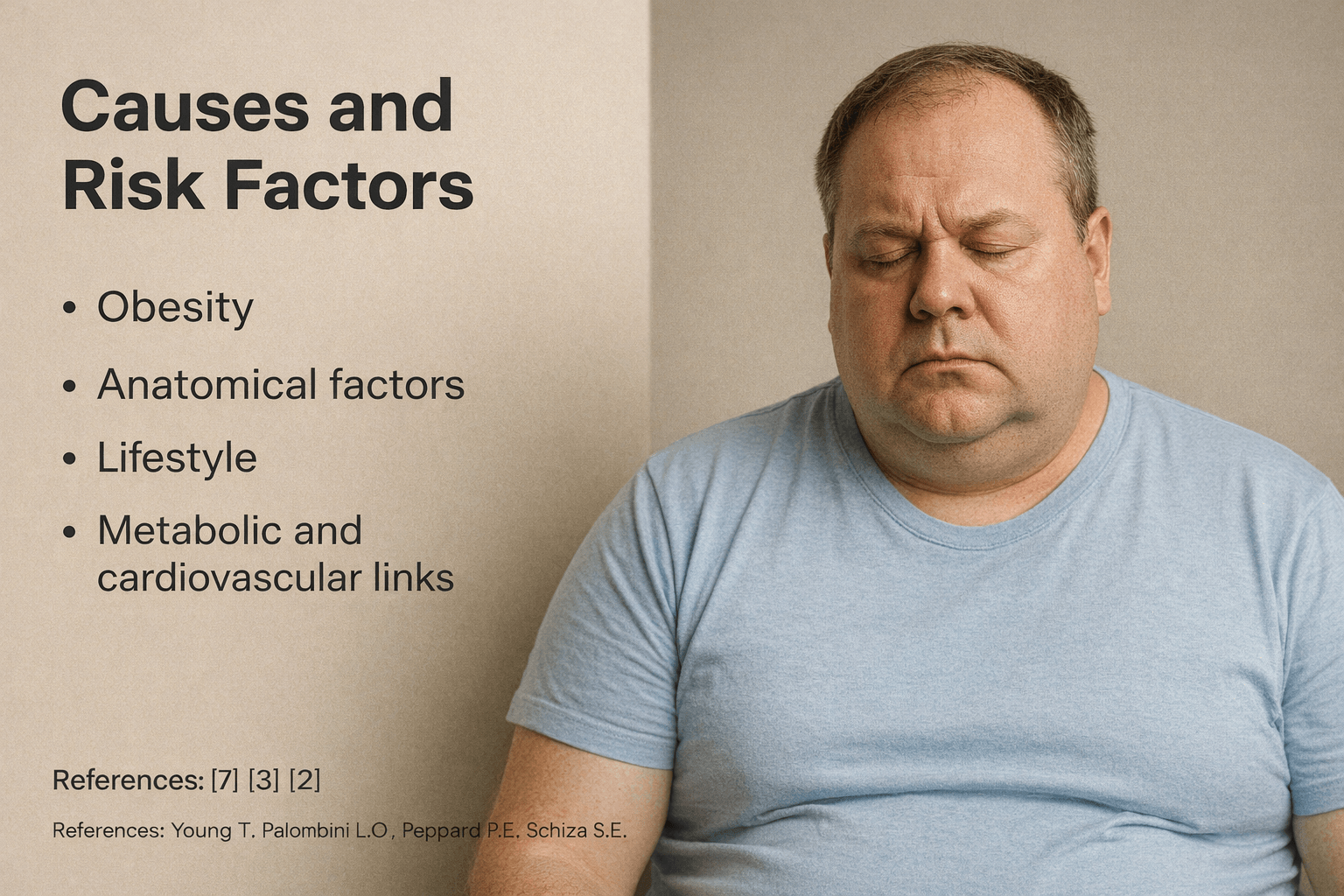
Sleep apnea develops from a combination of structural, metabolic, neurological, and lifestyle related factors rather than a single isolated cause. In clinical practice, I rarely see sleep apnea arising from one trigger alone. Instead, it reflects a convergence of risk factors that progressively destabilize breathing during sleep [7] [3] [2].
Obesity and Fat Distribution
Obesity is one of the strongest and most consistently identified risk factors for sleep apnea. Excess fat deposition around the neck, tongue, and upper airway increases external pressure on the pharyngeal structures, making airway collapse more likely during sleep. From a physiological perspective, increased abdominal and visceral fat also reduces lung volume, which further compromises airway stability. When you gain weight, especially centrally, the mechanical load on your respiratory system increases, and even small changes can significantly worsen nighttime breathing. Importantly, I also encounter patients with sleep apnea who are not obese, which confirms that obesity is a major but not exclusive contributor [7].
Anatomical and Structural Factors
Anatomical variations play a crucial role in sleep apnea risk. These include a narrow upper airway, enlarged tonsils, thickened soft palate, elongated uvula, recessed jaw, or nasal obstruction. Such structural features reduce airway diameter and make it more vulnerable to collapse when muscle tone decreases during sleep. From a clinical standpoint, these anatomical factors explain why some individuals develop sleep apnea at a younger age or at lower body weight. If you have chronic nasal congestion, sinus disease, or a history of facial or jaw abnormalities, your risk of sleep apnea increases even in the absence of obesity [2].
Lifestyle and Behavioral Contributors
Lifestyle habits significantly influence the severity and progression of sleep apnea. Alcohol consumption before bedtime relaxes airway muscles and suppresses arousal responses, increasing both the frequency and duration of breathing pauses. Sedative medications and smoking further impair airway stability and increase inflammation of the respiratory tract. From a practical perspective, I often observe that patients experience marked worsening of symptoms when sleep schedules are irregular or when late night meals and alcohol intake become routine. These modifiable behaviors play a substantial role in disease progression [2].
Metabolic and Cardiovascular Links
Sleep apnea is closely intertwined with metabolic and cardiovascular disorders. Conditions such as insulin resistance, type 2 diabetes, hypertension, and dyslipidemia both contribute to and are aggravated by sleep apnea. Chronic intermittent hypoxia promotes sympathetic overactivity, systemic inflammation, and endothelial dysfunction, which in turn worsen cardiovascular health. From a medical standpoint, this creates a bidirectional relationship where sleep apnea accelerates metabolic disease, and metabolic disease further destabilizes breathing during sleep. If you already have hypertension or heart disease, untreated sleep apnea significantly increases your risk of adverse cardiovascular outcomes [3].
Integrated Risk Perspective
When viewed together, these factors demonstrate that sleep apnea is not merely a consequence of excess weight or poor sleep habits. It is a multifactorial disorder shaped by anatomy, metabolism, nervous system regulation, and lifestyle choices. Recognizing these interconnected causes is essential for moving beyond symptomatic management and toward strategies that address the underlying drivers of the disease [7] [3] [2].
Signs and Symptoms
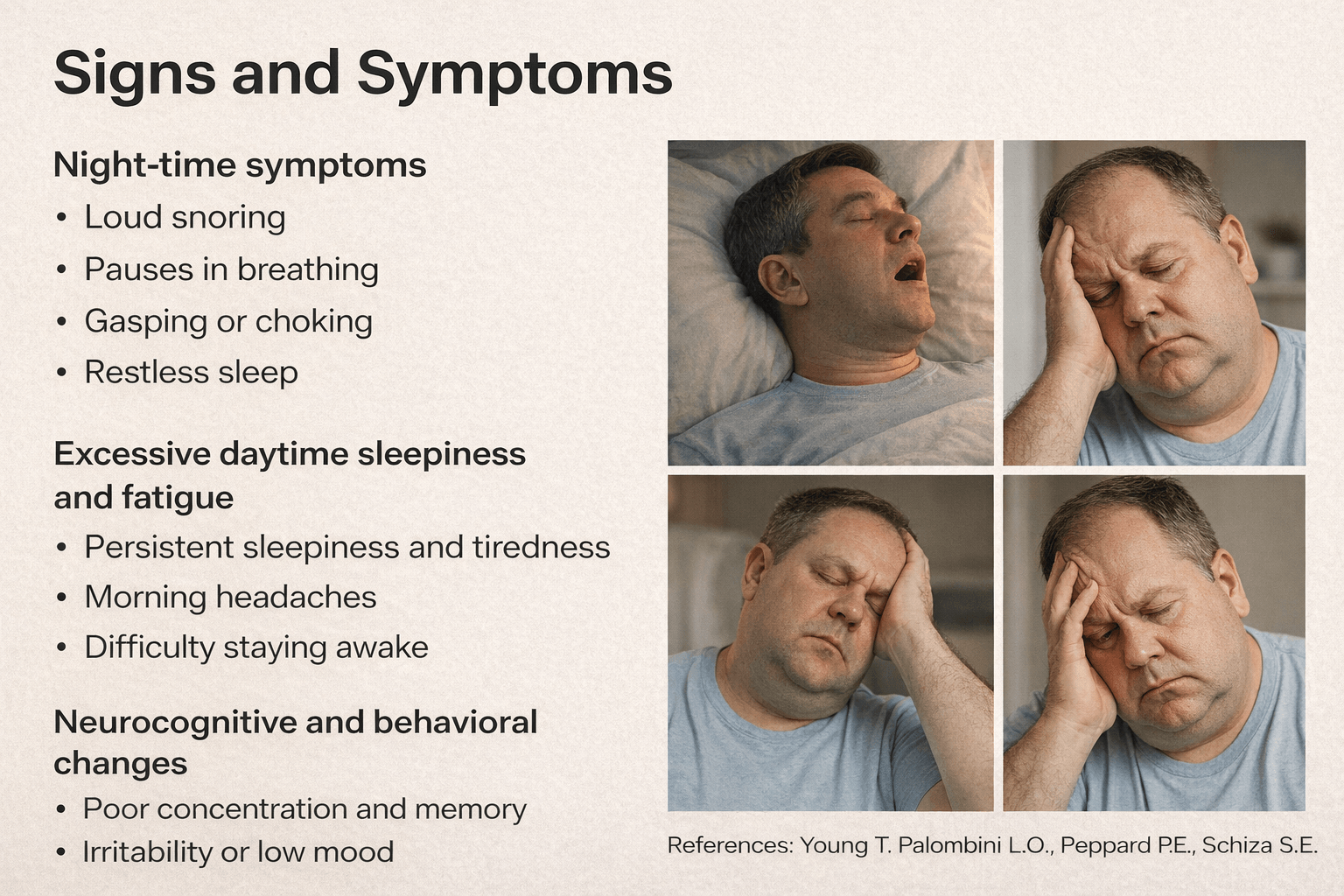
Sleep apnea presents with a wide range of symptoms that occur both during sleep and while awake. In clinical practice, I often observe that patients underestimate these symptoms because they develop gradually and are easily attributed to stress, aging, or poor lifestyle habits. However, when viewed together, these signs reflect significant disruption of normal breathing, sleep architecture, and brain function [2] [4].
Night-Time Symptoms
During sleep, the most characteristic signs of sleep apnea arise from repeated breathing interruptions and oxygen deprivation. Loud, chronic snoring is commonly reported, especially in obstructive sleep apnea, and is often accompanied by pauses in breathing witnessed by a bed partner. These pauses are frequently followed by choking, gasping, or sudden arousals as the body struggles to restore airflow. From the patient’s perspective, you may not remember these events clearly, but you might notice restless sleep, frequent awakenings, dry mouth on waking, or an urgent need to urinate at night. Clinically, these night-time disturbances indicate repeated airway collapse and fragmented sleep cycles [2].
Excessive Daytime Sleepiness and Fatigue
One of the most disabling consequences of sleep apnea is excessive daytime sleepiness. Because normal deep and rapid eye movement sleep are repeatedly interrupted, the brain never achieves restorative rest. If you are affected, you may feel persistently tired despite spending adequate hours in bed. Patients often describe an overwhelming urge to nap, reduced stamina, and difficulty staying alert during routine activities such as reading, driving, or working. From a medical standpoint, this chronic sleep deprivation significantly impairs reaction time and increases the risk of accidents and occupational errors [2].
Neurocognitive and Behavioral Changes
Beyond physical fatigue, sleep apnea has profound effects on brain function and behavior. Recurrent hypoxia and sleep fragmentation impair attention, memory, and executive functioning. In clinical settings, I frequently see patients reporting poor concentration, forgetfulness, slowed thinking, and reduced decision-making ability. Mood disturbances are also common, including irritability, anxiety, low motivation, and depressive symptoms. In some individuals, these changes may progress to more pronounced cognitive decline over time. From a neurological perspective, these symptoms reflect the vulnerability of the brain to repeated oxygen deprivation and disrupted sleep rhythms [4].
Integrated Symptom Perspective
When considered together, the signs and symptoms of sleep apnea extend far beyond disturbed sleep alone. Night-time breathing abnormalities directly translate into daytime fatigue, cognitive impairment, and behavioral changes that affect personal relationships, work performance, and overall quality of life. Recognizing this full symptom spectrum is essential, as early identification allows intervention before long-term neurological and systemic consequences become entrenched [2] [4].
Complications if Left Untreated
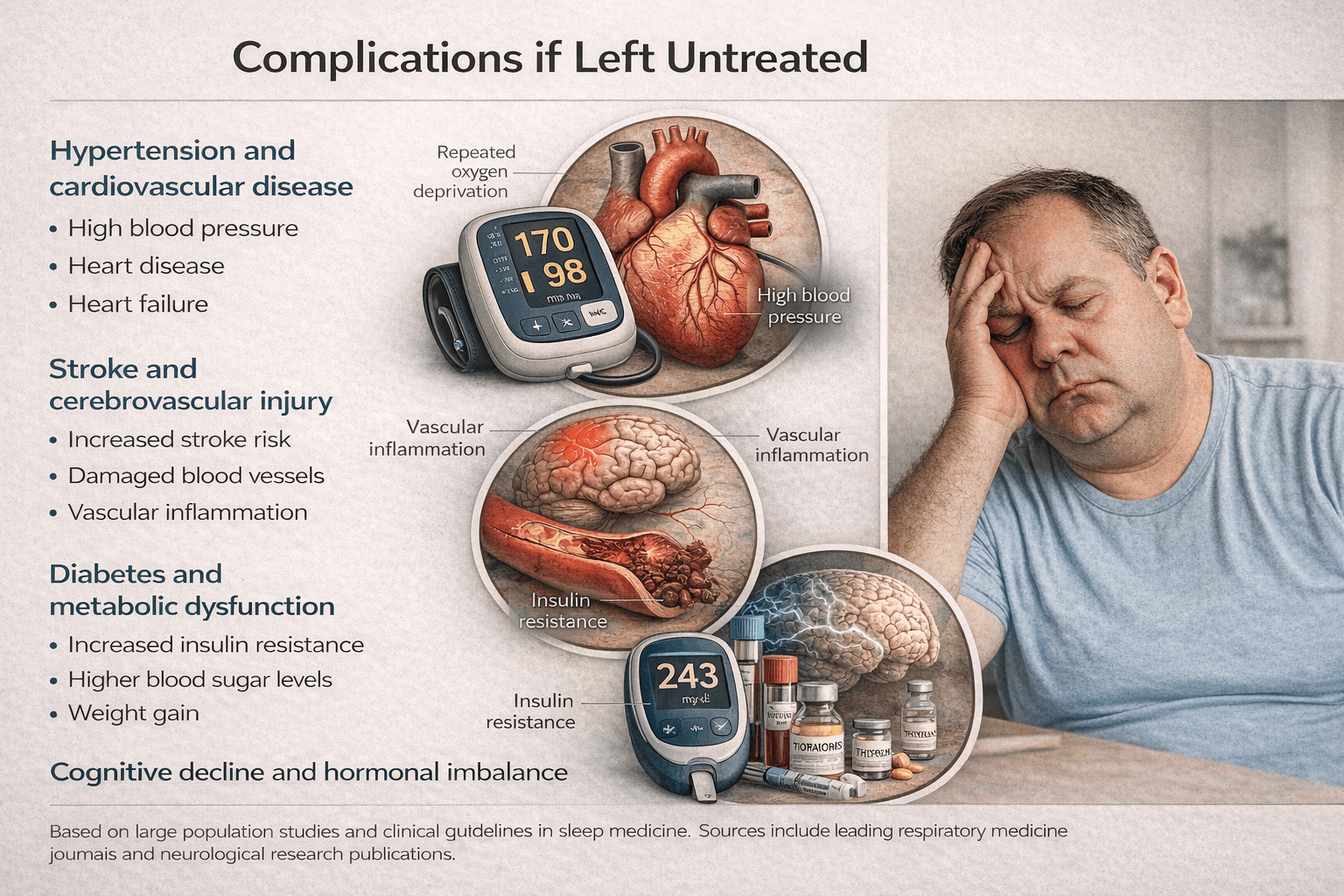
When sleep apnea is left untreated, it evolves from a nighttime breathing disorder into a progressive systemic disease. In clinical practice, I often see that patients initially seek help for fatigue or snoring, but the real danger lies in the silent complications that develop over years of repeated oxygen deprivation and sleep fragmentation. From a medical standpoint, untreated sleep apnea significantly increases long term morbidity and mortality through its effects on the cardiovascular system, metabolism, brain function, and hormonal balance [3] [4] [15].
Hypertension and Cardiovascular Disease
One of the earliest and most consistent complications of untreated sleep apnea is the development of hypertension. Repeated breathing pauses trigger surges in stress hormones that cause blood pressure to rise sharply during sleep. Over time, these nocturnal spikes persist into the daytime, leading to sustained high blood pressure. If you have untreated sleep apnea, your heart is forced to work harder every night, increasing the risk of coronary artery disease, heart failure, and abnormal heart rhythms. From a cardiology perspective, sleep apnea is now recognized as an independent risk factor for cardiovascular disease rather than a secondary association [3].
Stroke and Cerebrovascular Risk
Untreated sleep apnea also markedly increases the risk of stroke. Intermittent hypoxia, oxidative stress, and chronic inflammation damage blood vessels supplying the brain, while repeated blood pressure fluctuations impair cerebral blood flow regulation. In clinical settings, patients with moderate to severe sleep apnea are more likely to experience both ischemic and hemorrhagic strokes. If sleep apnea remains unaddressed, the cumulative vascular injury can lead to sudden neurological events with long lasting disability [3].
Diabetes and Metabolic Dysfunction
Sleep apnea has a strong bidirectional relationship with metabolic disorders, particularly type 2 diabetes. Recurrent oxygen deprivation and sleep disruption interfere with insulin signaling and glucose metabolism, promoting insulin resistance. When you live with untreated sleep apnea, your body remains in a constant stress state that favors fat accumulation, elevated blood sugar levels, and abnormal lipid profiles. Over time, this metabolic imbalance increases the risk of diabetes and worsens glycemic control in those already diagnosed [15].
Cognitive Decline and Neurobehavioral Effects
The brain is especially sensitive to repeated hypoxia and fragmented sleep. Untreated sleep apnea impairs attention, memory, executive function, and processing speed. In my clinical experience, patients often report worsening forgetfulness, reduced work performance, and difficulty making decisions. Long term studies have linked untreated sleep apnea to accelerated cognitive decline and an increased risk of dementia. These changes reflect cumulative neuronal injury caused by chronic oxygen deprivation and disrupted sleep cycles [4].
Hormonal and Sexual Dysfunction
Normal sleep plays a critical role in hormonal regulation. When sleep apnea disrupts deep and rapid eye movement sleep, hormone secretion patterns are altered. Untreated sleep apnea is associated with reduced testosterone levels in men, menstrual irregularities in women, thyroid dysfunction, and impaired stress hormone regulation. If left untreated, these hormonal imbalances can contribute to reduced libido, infertility, mood disturbances, and further metabolic deterioration, creating a self reinforcing cycle of disease [4] [15].
Integrated Complication Perspective
Taken together, these complications demonstrate that untreated sleep apnea is not a benign condition. It is a progressive disorder that quietly damages the cardiovascular system, brain, metabolism, and endocrine balance. Recognizing these risks underscores the importance of early diagnosis and comprehensive treatment aimed not only at improving sleep quality but also at preventing irreversible systemic consequences [3] [4] [15].
Diagnostic Framework
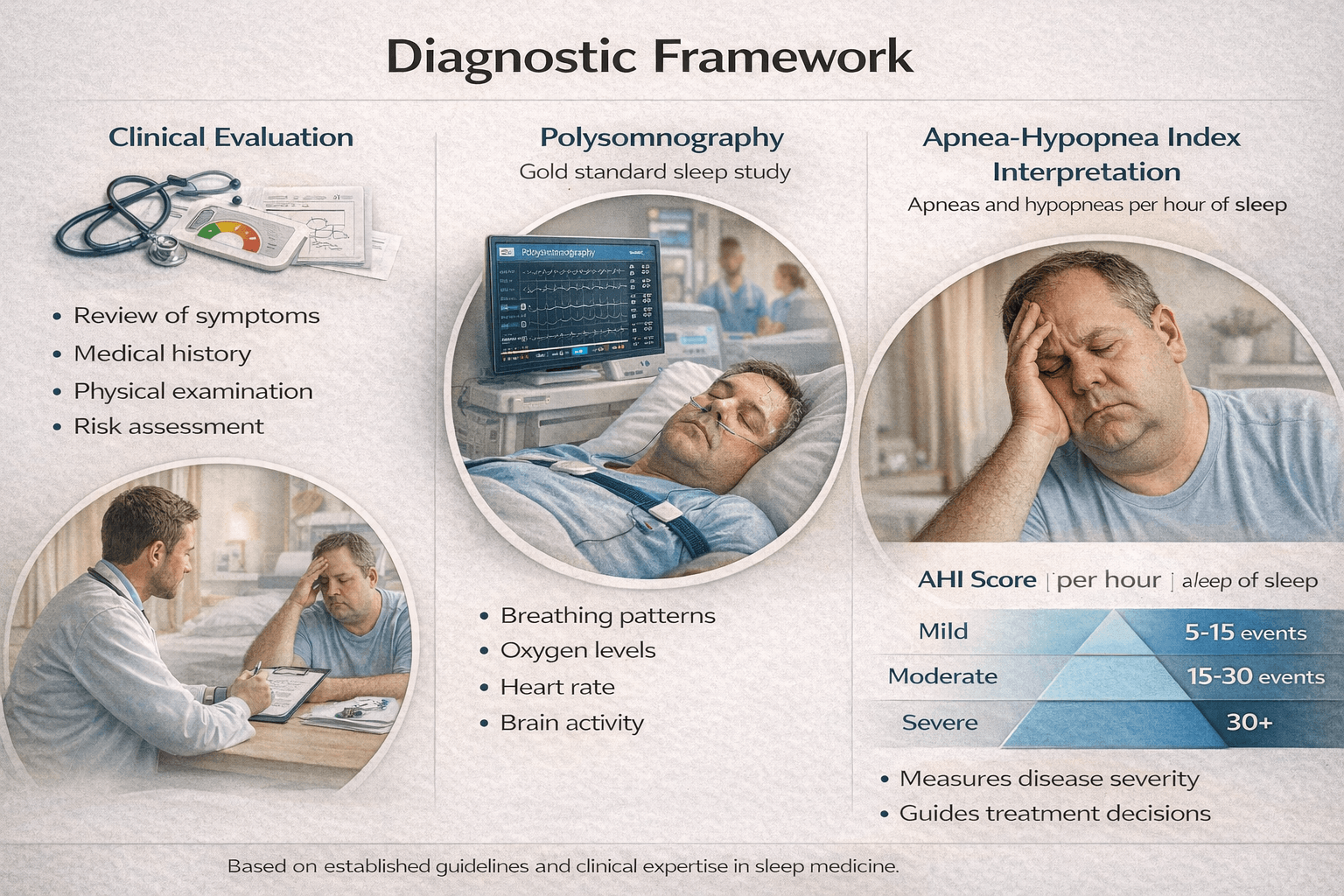
Accurate diagnosis is the foundation of effective sleep apnea management. In my clinical experience, many patients live with symptoms for years because proper diagnostic evaluation is delayed or incomplete. A structured diagnostic framework combines careful clinical assessment with objective sleep testing to confirm the presence, type, and severity of sleep apnea [5] [2].
Clinical Evaluation and Patient History
The diagnostic process begins with a detailed clinical evaluation. When I assess a patient for suspected sleep apnea, I focus on both night time and daytime symptoms, including snoring, witnessed breathing pauses, unrefreshing sleep, and excessive daytime sleepiness. From your perspective as a patient, this stage may feel conversational, but it is critical for identifying risk patterns that guide further testing.
Clinical evaluation also includes assessment of body weight, neck circumference, jaw structure, nasal airflow, and signs of cardiovascular or metabolic disease. Questionnaires such as sleepiness scales help quantify symptom severity, but they do not replace objective testing. From a medical standpoint, clinical evaluation identifies suspicion, but it cannot confirm the diagnosis on its own [2].
Polysomnography as the Gold Standard
Polysomnography is considered the gold standard diagnostic test for sleep apnea. This overnight sleep study records multiple physiological parameters simultaneously, including airflow, breathing effort, blood oxygen levels, heart rhythm, brain activity, eye movements, and muscle tone. When patients ask me why such detailed monitoring is necessary, I explain that sleep apnea is not just about breathing pauses but about how those pauses affect the entire body during sleep.
Polysomnography allows clinicians to differentiate between obstructive sleep apnea, central sleep apnea, and mixed patterns. It also reveals the frequency of breathing events, the degree of oxygen desaturation, and the extent of sleep fragmentation. From a diagnostic perspective, this comprehensive data provides clarity that cannot be achieved through symptoms alone [5].
Apnea Hypopnea Index Interpretation
A key outcome of polysomnography is the Apnea Hypopnea Index, commonly referred to as AHI. This index represents the average number of apneas and hypopneas occurring per hour of sleep. In practical terms, AHI helps quantify disease severity and guides treatment decisions.
If you are diagnosed with sleep apnea, your AHI value will typically be categorized as mild, moderate, or severe. However, from a clinical viewpoint, I do not rely solely on this number. The pattern of oxygen drops, duration of events, and associated symptoms often provide equally important information. Two patients with the same AHI may have very different clinical risks depending on their overall physiological response to sleep disruption [2].
Integrating Clinical and Objective Findings
A robust diagnostic framework integrates clinical evaluation with objective sleep study findings. Polysomnography confirms the diagnosis, AHI helps stratify severity, and clinical assessment provides context regarding symptoms, comorbidities, and functional impact. When these elements are interpreted together, they allow for a precise diagnosis rather than a generic label.
From a broader medical perspective, this integrated approach ensures that sleep apnea is recognized early and accurately, setting the stage for targeted treatment that addresses both symptoms and underlying physiological mechanisms [5] [2].
Modern Medical Management
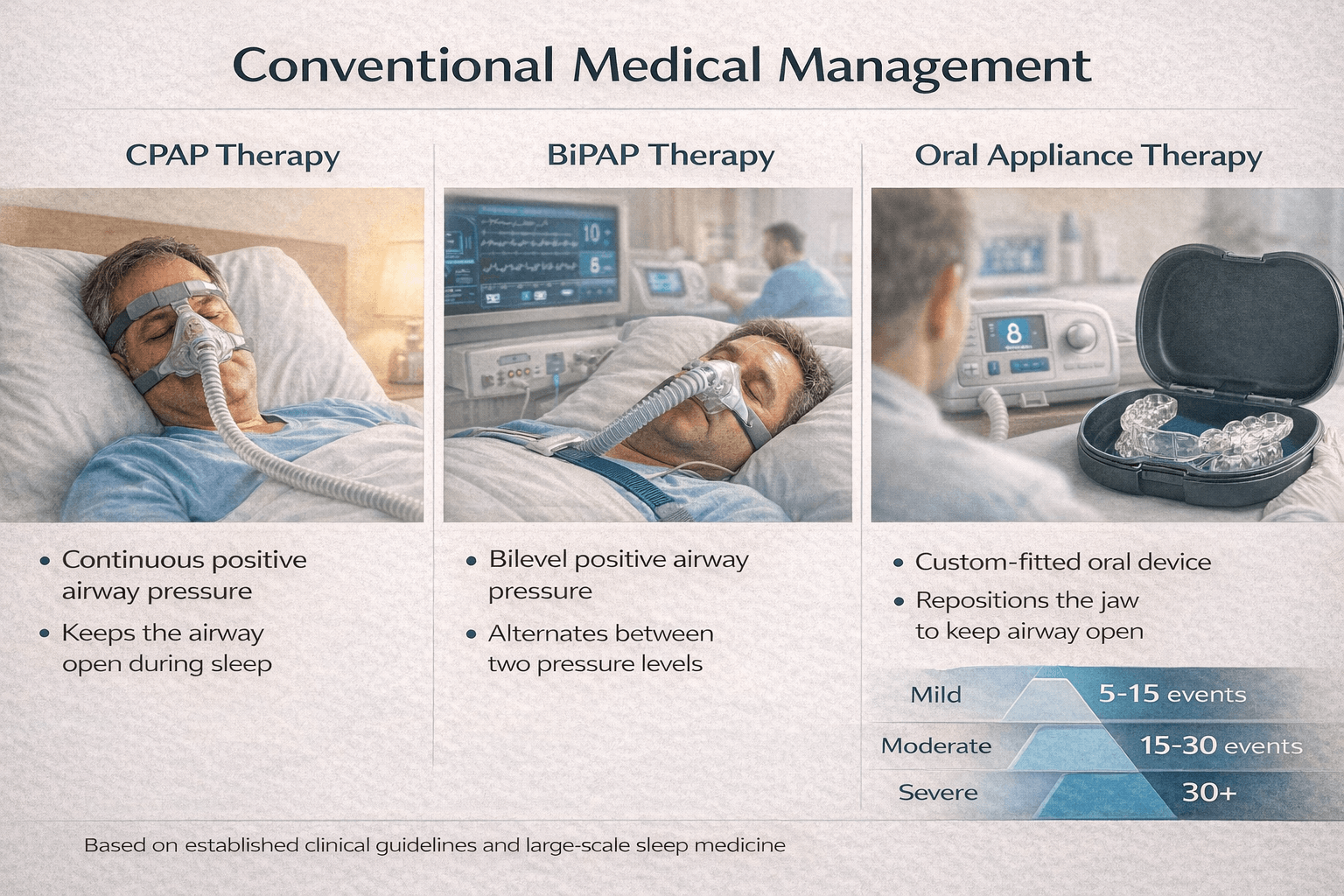
Conventional medical management of sleep apnea focuses primarily on mechanically preventing airway collapse during sleep rather than correcting the underlying biological drivers of the condition. In clinical practice, I often meet patients who have been advised that long term device based therapy is the standard and sometimes the only available option. While these approaches can reduce symptoms and improve short term outcomes, they are largely aimed at symptom control rather than disease reversal [6] [5].
Continuous Positive Airway Pressure Therapy
Continuous positive airway pressure, commonly known as CPAP, is considered the first line treatment for moderate to severe obstructive sleep apnea. This therapy delivers a constant stream of pressurized air through a mask worn during sleep, which acts as a pneumatic splint to keep the airway open. From a clinical standpoint, CPAP is effective in reducing apnea events, improving oxygen saturation, and lowering blood pressure when used consistently.
From the patient’s perspective, however, CPAP therapy can be challenging. Many individuals experience discomfort, nasal dryness, skin irritation, claustrophobia, or difficulty tolerating the mask throughout the night. In my clinical experience, long term adherence remains a significant limitation, and inconsistent use often reduces the overall effectiveness of the therapy [6].
BiLevel Positive Airway Pressure Therapy
BiLevel positive airway pressure, or BiPAP, is an alternative form of positive airway pressure therapy that provides two different pressure levels, one during inhalation and a lower pressure during exhalation. This approach is often prescribed for patients who have difficulty tolerating continuous pressure or who have coexisting conditions such as central sleep apnea or certain neuromuscular disorders.
BiPAP can improve comfort for some patients, particularly those requiring higher pressures. However, like CPAP, it does not address the root causes of sleep apnea and requires ongoing nightly use to maintain benefits. From a clinical perspective, discontinuation typically results in the return of symptoms [6].
Oral Appliance Therapy
Oral appliances are custom fitted devices designed to reposition the lower jaw and tongue forward during sleep, thereby increasing airway space and reducing collapse. These devices are commonly recommended for patients with mild to moderate obstructive sleep apnea or for those who cannot tolerate positive airway pressure therapy.
While oral appliances may reduce snoring and apnea frequency in selected individuals, their effectiveness varies depending on anatomical factors and disease severity. From a long term management perspective, they also require continued nightly use and regular dental follow up to monitor for jaw discomfort or bite changes [5].
Standard of Care and Clinical Limitations
From a broader medical standpoint, CPAP, BiPAP, and oral appliances represent the current standard of care in sleep medicine. These interventions are supported by clinical guidelines and are effective in reducing apnea events when used correctly. However, they do not correct metabolic dysfunction, neuromuscular instability, inflammation, or lifestyle factors that contribute to sleep apnea development.
As a result, conventional medical management often becomes a lifelong commitment to device use, with symptom recurrence occurring soon after discontinuation. This limitation highlights the gap between managing airway obstruction mechanically and achieving long term physiological correction of the disorder [6] [5].
Integrated Perspective
When viewed through an integrative lens, conventional therapies play an important role in immediate symptom relief and risk reduction, particularly in moderate to severe cases. However, their inability to reverse underlying pathology underscores the need for complementary strategies that address the root causes of sleep apnea rather than relying solely on mechanical support [6] [5].
Limitations of Modern Treatment

While conventional treatments such as CPAP, BiPAP, and oral appliances are widely accepted as standard care, they carry important limitations that affect long term outcomes. In clinical practice, I often see patients achieve temporary symptom relief yet continue to struggle with sustainability, comfort, and true disease resolution. These limitations explain why many individuals remain dependent on devices for years without experiencing meaningful reversal of sleep apnea [6] [2].
Compliance and Long Term Adherence Challenges
One of the most significant limitations of conventional therapy is poor long term adherence. Although CPAP and BiPAP devices are effective when used consistently, many patients find nightly use difficult. If you are prescribed a mask and machine, you may experience discomfort, nasal congestion, dryness, skin irritation, noise disturbance, or a sense of claustrophobia. From my clinical experience, even motivated patients often reduce usage over time, which directly diminishes therapeutic benefit.
Studies consistently show that a substantial proportion of patients do not use positive airway pressure devices for the recommended duration each night. As a result, the protective effects against cardiovascular and metabolic complications are only partially achieved [6].
Symptomatic Control Rather Than Root Correction
Conventional treatments primarily work by mechanically keeping the airway open during sleep. They do not correct the underlying factors that lead to airway collapse, such as reduced neuromuscular tone, metabolic dysfunction, chronic inflammation, or weight related changes. From a medical perspective, this means the disease process remains active beneath the surface even when symptoms appear controlled.
When I explain this to patients, I emphasize that these therapies function only while they are in use. They do not retrain the airway, restore physiological balance, or reverse the biological mechanisms driving sleep apnea. As a result, the condition is managed rather than healed [2].
Relapse After Discontinuation
Another critical limitation is the high likelihood of relapse once conventional treatment is stopped. If you discontinue CPAP, BiPAP, or oral appliance therapy, apnea events typically return quickly, often within days. This rapid relapse highlights the absence of lasting physiological correction.
From a broader clinical standpoint, this dependency creates a lifelong treatment model. Patients are frequently told that device use must continue indefinitely, which can lead to frustration, reduced motivation, and eventual noncompliance. This cycle reinforces the perception that sleep apnea is an irreversible condition rather than a modifiable disorder [6] [2].
Impact on Patient Experience and Quality of Life
Although conventional therapies reduce apnea frequency, they may negatively affect sleep comfort and intimacy. Some patients report disturbed sleep due to equipment noise or mask discomfort, while others struggle with travel or social situations that complicate device use. From the patient’s perspective, these practical burdens can significantly influence long term acceptance of treatment.
Integrated Perspective
Taken together, the limitations of conventional treatment highlight a fundamental gap between symptom suppression and true disease resolution. While these therapies play an important role in risk reduction and short term control, especially in moderate to severe cases, their dependence on continuous use and lack of root cause correction underscore the need for approaches that aim at long term physiological restoration rather than perpetual mechanical support [6] [2].
Ayurvedic Understanding of Sleep Apnea

From an Ayurvedic perspective, sleep apnea is not viewed as an isolated mechanical breathing disorder but as a functional disturbance involving respiration, sleep regulation, and systemic balance. When I interpret sleep apnea through classical Ayurvedic principles, it aligns closely with disorders of Pranavaha Srotas and Nidra Vyapara, where the natural rhythm of breathing and sleep becomes impaired due to doshic imbalance. This understanding allows sleep apnea to be approached as a reversible imbalance rather than a fixed structural disease [9] [12].
Pranavaha Srotas Dysfunction
Pranavaha Srotas refers to the channels responsible for respiration and the movement of Prana throughout the body. Classical texts describe that when these channels become obstructed or weakened, normal breathing patterns are disrupted, especially during sleep. In patients with sleep apnea, I commonly observe features that correspond to Pranavaha Srotas Dushti, such as irregular breathing, shallow respiration, heaviness in the chest, and disturbed sleep.
From this viewpoint, airway collapse during sleep is not merely a physical blockage but the result of impaired Prana flow. When Prana cannot move freely through its channels, breathing becomes unstable, particularly during states of reduced consciousness like sleep. This explains why breathing disturbances are most pronounced at night rather than during wakefulness [9].
Nidra Vyapara and Disturbed Sleep Physiology
Nidra Vyapara describes the physiological process governing sleep. Ayurveda emphasizes that healthy sleep depends on balanced Kapha, stable Vata, and unobstructed Prana. In sleep apnea, this balance is lost. Excess Kapha creates heaviness and obstruction in the upper airway, while aggravated Vata disrupts the rhythmic coordination of breathing muscles.
From the patient’s experience, you may feel that sleep is present in duration but absent in quality. This reflects disturbed Nidra Vyapara, where the body enters sleep but fails to achieve restorative depth. Classical descriptions link such disturbed sleep with respiratory obstruction, lethargy, and reduced vitality, all of which are common in sleep apnea [12].
Kapha and Vata Involvement
Ayurveda identifies sleep apnea as a Kapha Vata dominant disorder. Kapha contributes to structural heaviness, mucus accumulation, reduced muscle tone, and airway narrowing. This explains snoring, airway obstruction, and the feeling of heaviness on waking. Vata, when obstructed by Kapha, becomes erratic and loses its normal directional movement. This leads to irregular breathing patterns, sudden pauses in respiration, and abrupt awakenings.
In my clinical observation, when Kapha is reduced without stabilizing Vata, symptoms may fluctuate. Conversely, when Vata is pacified without clearing Kapha obstruction, breathing remains compromised. This interdependence highlights why Ayurvedic treatment must address both doshas simultaneously rather than focusing on a single factor [9] [12].
Integrated Ayurvedic Perspective
When Pranavaha Srotas obstruction, disturbed Nidra Vyapara, and Kapha Vata imbalance are viewed together, sleep apnea emerges as a disorder of functional regulation rather than irreversible anatomy. This integrated Ayurvedic understanding forms the foundation for curative strategies that aim to clear obstruction, stabilize respiratory rhythm, and restore natural sleep breathing cycles.
By correcting these underlying imbalances, Ayurveda offers a framework in which an Ayurvedic cure for sleep apnea becomes a rational therapeutic goal rather than an exception, addressing the root of the disorder instead of merely compensating for its symptoms [9] [12].
Ayurvedic Pathogenesis (Samprapti)
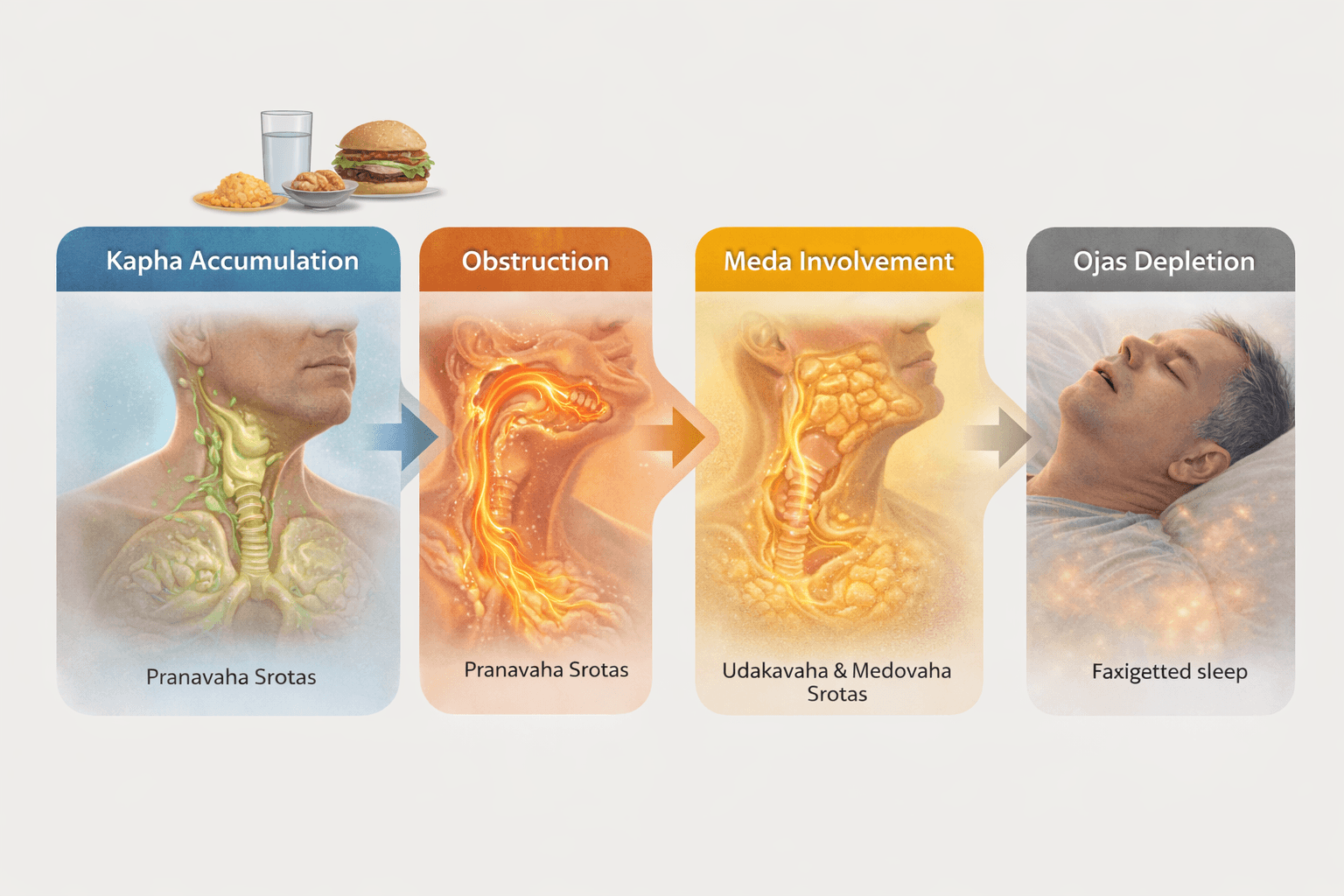
Ayurveda explains the development of sleep apnea through a stepwise pathological process known as Samprapti, which describes how doshic imbalance gradually manifests as disease. When I analyze sleep apnea from this perspective, it becomes clear that the condition does not arise suddenly. Instead, it evolves through progressive Kapha accumulation, channel obstruction, metabolic involvement, and eventual depletion of vital strength. This layered understanding is essential for identifying where and how intervention can reverse the disease process [9] [13].
Kapha Sanchaya and Prakopa
The pathogenesis begins with Kapha Sanchaya, the gradual accumulation of Kapha dosha due to factors such as sedentary lifestyle, excessive intake of heavy, oily, and sweet foods, irregular sleep habits, and weakened digestive fire. As Kapha continues to accumulate, it progresses to Kapha Prakopa, where its qualities of heaviness, coldness, and stickiness become dominant in the upper body.
In sleep apnea, this aggravated Kapha localizes in the region of the throat, chest, and head, leading to increased softness and laxity of tissues. From a clinical viewpoint, this stage corresponds to early snoring, heaviness on waking, and a feeling of unrefreshing sleep. At this point, symptoms may still be mild and intermittent, but the foundation of the disorder has already been laid [9].
Srotorodha in Pranavaha and Related Channels
As Kapha aggravation persists, it leads to Srotorodha, or obstruction of bodily channels. In sleep apnea, the primary channels affected are Pranavaha Srotas, which governs respiration, along with Udakavaha and Medovaha Srotas. This obstruction interferes with the smooth flow of Prana, especially during sleep when muscular tone naturally decreases.
From the patient’s experience, you may notice worsening snoring, frequent awakenings, choking sensations, or breath holding during sleep. Ayurvedically, these manifestations arise because Kapha blocks the normal pathway of Vata, forcing it into an abnormal, erratic movement. This phenomenon, known as Avarana of Vata by Kapha, is central to the development of breathing pauses during sleep [9] [13].
Meda Dhatu Involvement
With ongoing Srotorodha, Meda Dhatu becomes actively involved in the disease process. Disturbed metabolism leads to improper formation and deposition of Meda, particularly in the neck, chest, and upper airway regions. This excess or vitiated Meda further narrows respiratory passages and reduces tissue resilience.
From an Ayurvedic standpoint, Meda involvement explains the strong association between sleep apnea and obesity, insulin resistance, and metabolic sluggishness. However, I also observe that Meda Dushti can be present even in individuals who are not visibly overweight, manifesting instead as poor fat metabolism and localized tissue heaviness [13].
Progressive Ojas Depletion
As sleep apnea advances, repeated disturbance of sleep and impaired respiration begin to erode Ojas, the essence responsible for vitality, immunity, and mental stability. Inadequate oxygenation during sleep, combined with chronic stress on Prana and Vata, gradually weakens Ojas.
Clinically, this stage is reflected in persistent fatigue, reduced stamina, lowered immunity, mental dullness, mood changes, and accelerated aging. From an Ayurvedic perspective, Ojas depletion marks the transition of sleep apnea from a localized respiratory disorder into a systemic disease affecting overall health and longevity [9].
Integrated Samprapti Perspective
When viewed as a whole, the Samprapti of sleep apnea follows a clear and logical progression. Kapha accumulation initiates the disorder, Srotorodha disrupts respiratory flow, Meda involvement stabilizes the obstruction, and Ojas depletion amplifies systemic weakness. Understanding this sequence allows Ayurvedic treatment to be precisely targeted at reversing each stage of pathology rather than merely suppressing symptoms.
This classical framework explains why effective Ayurvedic management of sleep apnea must address digestion, metabolism, channel patency, and vitality simultaneously, restoring balance at every level of the disease process [9] [13].
Ayurvedic Treatment Principles
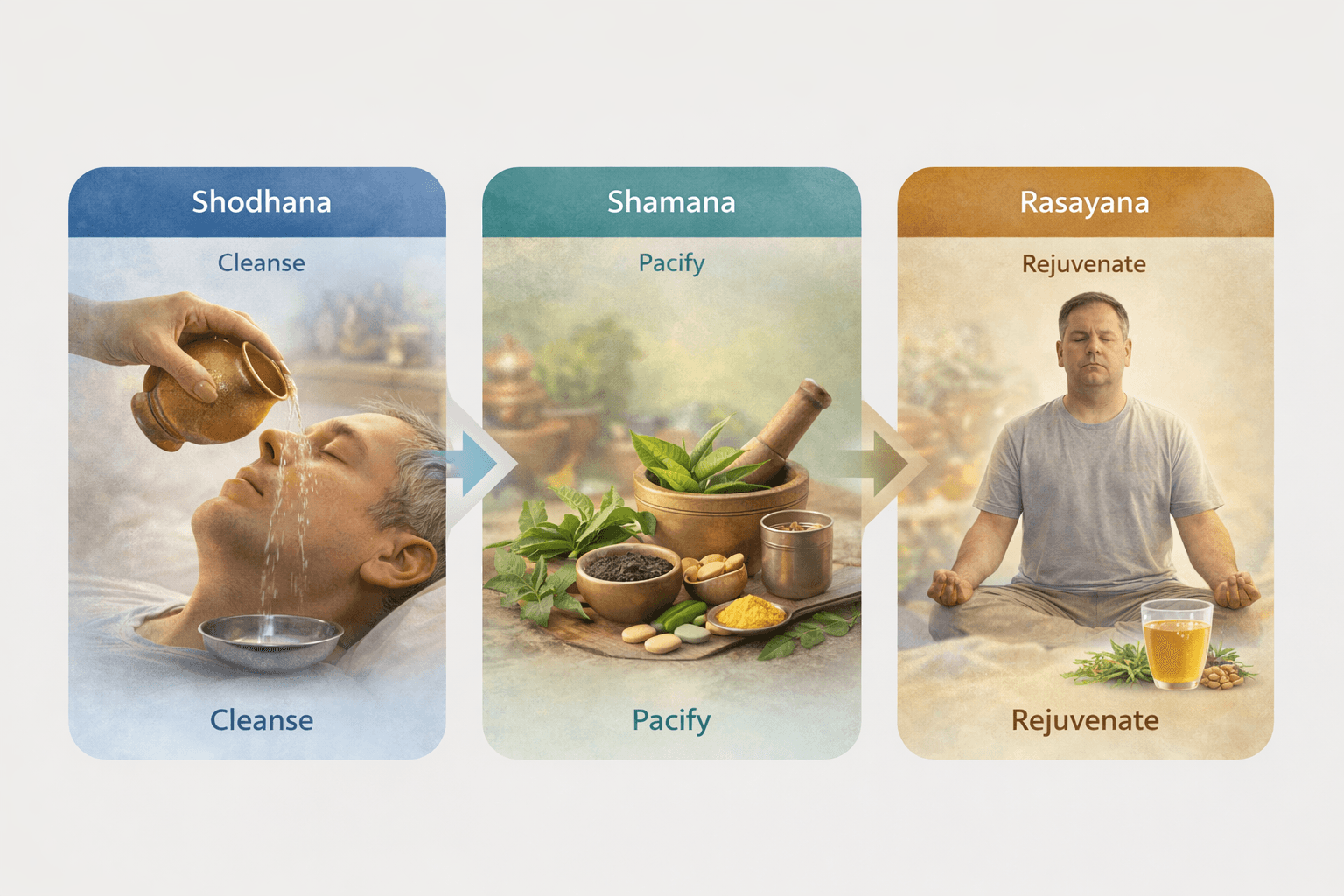
Ayurvedic management of sleep apnea is guided by a structured and time tested therapeutic framework that focuses on root cause correction rather than symptom suppression. When I apply Ayurvedic treatment principles in clinical practice, the goal is to restore natural breathing during sleep by correcting doshic imbalance, clearing obstructed channels, strengthening respiratory regulation, and rebuilding systemic vitality. This approach is classically organized into three interrelated pillars: Shodhana, Shamana, and Rasayana [9] [11].
Shodhana: Eliminating the Root Obstruction
Shodhana refers to bio purification therapies aimed at removing accumulated doshas and metabolic waste from the body. In sleep apnea, Shodhana is particularly important when Kapha accumulation and channel obstruction dominate the clinical picture. Excess Kapha lodged in the chest, throat, and head region weakens airway tone and interferes with the free movement of Prana.
From a therapeutic standpoint, Shodhana helps reduce the physical and functional load on Pranavaha Srotas. When appropriately indicated and carefully administered, purification therapies improve metabolic efficiency, reduce tissue heaviness, and restore responsiveness of the respiratory system. In my clinical experience, Shodhana prepares the body to respond more effectively to subsequent internal medications by removing the underlying barriers to healing [9].
It is important to emphasize that Shodhana is individualized and optional. Not every patient with sleep apnea requires purification therapy. The decision depends on constitution, strength, disease chronicity, and metabolic status.
Shamana: Pacifying Dosha Imbalance
Shamana therapy focuses on pacifying aggravated doshas and stabilizing physiological function through internal medicines, diet, and lifestyle correction. In sleep apnea, Shamana aims to balance Kapha and Vata simultaneously. Kapha reduction clears airway heaviness and mucus related obstruction, while Vata stabilization restores rhythmic breathing and neuromuscular coordination during sleep.
From the patient’s perspective, this phase often brings noticeable improvement in snoring intensity, sleep continuity, morning freshness, and daytime alertness. Shamana therapy addresses ongoing pathological processes without placing excessive stress on the body, making it suitable for long term use and for patients who are not candidates for purification therapies [9].
Classical formulations described for respiratory disorders are selected based on their ability to improve digestion, clear channels, regulate breathing, and stabilize sleep physiology. This phase forms the core therapeutic backbone in most cases of sleep apnea.
Rasayana: Restoring Strength and Preventing Relapse
Rasayana therapy represents the restorative and rejuvenative phase of Ayurvedic treatment. Once obstruction is reduced and doshic imbalance is controlled, Rasayana therapy is introduced to strengthen tissues, restore vitality, and prevent recurrence. In sleep apnea, Rasayana plays a crucial role because the condition often leads to long standing fatigue, reduced stamina, and gradual depletion of Ojas.
From an Ayurvedic standpoint, Rasayana enhances the quality of Dhatus, improves neuromuscular tone of the airway, stabilizes nervous system regulation, and supports deep restorative sleep. In my clinical observation, patients who receive appropriate Rasayana therapy show more stable long term outcomes and reduced dependency on external interventions [11].
Integrated Treatment Perspective
When applied together, Shodhana clears the terrain, Shamana corrects active imbalance, and Rasayana rebuilds strength and resilience. This sequential yet overlapping framework allows Ayurvedic treatment to address sleep apnea at every level, from metabolic and structural factors to nervous system regulation and vitality.
This integrated approach explains why Ayurveda views sleep apnea as a manageable and potentially reversible disorder when treatment is individualized, sustained, and aligned with classical therapeutic principles rather than limited to mechanical airway support [9] [11].
Best Medicine Avaleha for Sleep Apnea (Core Curative Section)
In classical Ayurveda, disorders marked by obstructed breathing, disturbed sleep, heaviness of the chest and throat, and Kapha dominated respiratory dysfunction are addressed with specific formulations described in the Shwasa Chikitsa chapters. When I evaluate sleep apnea through this lens, one formulation stands out consistently for its relevance, depth of action, and textual authority: Vyaghri Haritaki Avaleha. This Avaleha is not selected arbitrarily. It is rooted in classical indications, appropriate pharmacological design, and a delivery form uniquely suited to chronic respiratory and sleep related disorders [10] [11] [9].
Classical Indication of Vyaghri Haritaki Avaleha
Vyaghri Haritaki Avaleha is described in classical Ayurvedic texts for the management of Shwasa Roga and chronic Kapha dominant respiratory conditions. These descriptions closely mirror the clinical picture of sleep apnea, where breathing becomes impaired primarily during sleep due to obstruction, heaviness, and loss of rhythmic control.
From a textual standpoint, Vyaghri Haritaki Avaleha is indicated when Kapha obstructs the normal movement of Vata in the respiratory channels. This condition, known as Kapha Avarana of Vata, is central to the Ayurvedic explanation of breathing pauses and irregular respiration during sleep. When you experience snoring, choking, or breath holding at night, Ayurveda interprets this as Prana being unable to move freely due to Kapha obstruction, a state directly addressed by this formulation [10] [9].
Why Avaleha Form Is Therapeutically Superior
The Avaleha dosage form is not incidental. In Ayurveda, Avaleha is specifically chosen for chronic diseases involving the chest, throat, lungs, and upper channels. Its semi solid, unctuous nature allows for prolonged contact with tissues, deeper penetration into subtle channels, and sustained therapeutic action.
In my clinical experience, Avaleha formulations are particularly effective for night predominant conditions because they act gradually and continuously, supporting the body during sleep when symptoms are most pronounced. For sleep apnea, this is crucial. The Avaleha form nourishes while it clears, ensuring that Kapha is reduced without excessively aggravating Vata. This balance is difficult to achieve with lighter or sharply drying formulations alone [11].
Mechanism of Action in Sleep Apnea
Vyaghri Haritaki Avaleha works at multiple levels relevant to sleep apnea pathophysiology. At the channel level, it helps clear accumulated Kapha from Pranavaha Srotas, improving airway patency and reducing heaviness in the throat and chest. At the functional level, it supports proper Vata movement, restoring rhythmic breathing during sleep.
From the patient’s perspective, this often translates into reduced snoring intensity, fewer nocturnal awakenings, and a gradual return of more continuous, restorative sleep. Over time, improved oxygenation during sleep supports better daytime energy, mental clarity, and cardiovascular stability. Importantly, this improvement occurs not by forcing the airway open mechanically, but by restoring the body’s natural ability to maintain unobstructed breathing [9] [11].
Role in Long Term Correction Rather Than Temporary Relief
What distinguishes Vyaghri Haritaki Avaleha from symptomatic interventions is its role in long term correction. Classical texts emphasize that repeated use of properly indicated Avaleha formulations strengthens the respiratory system, improves tissue quality, and reduces disease recurrence. In sleep apnea, this is especially relevant because relapse is common when treatment does not address underlying Kapha accumulation and metabolic dysfunction.
When incorporated as part of a structured Ayurvedic treatment plan that includes dietary correction, lifestyle alignment, and, where appropriate, Rasayana support, Vyaghri Haritaki Avaleha serves as a core curative agent rather than a temporary measure [10] [11].
Integrated Classical Perspective
From an integrated Ayurvedic standpoint, Vyaghri Haritaki Avaleha aligns precisely with the Samprapti of sleep apnea. It addresses Kapha sanchaya, relieves srotorodha, supports balanced Vata movement, and gradually protects Ojas by restoring healthier sleep and respiration. This alignment between disease mechanism and formulation design is the reason classical texts continue to recommend this Avaleha for chronic respiratory disorders that resemble modern sleep apnea [10] [9].
When used judiciously and individualized to constitution and disease stage, Vyaghri Haritaki Avaleha represents the most appropriate Avaleha based intervention for the root cause management of sleep apnea as described in Ayurvedic medical literature [10] [11] [9].
Vyaghri Haritaki Avaleha (Medicine) Preparation
Preparation Method for 30-Day Batch
Dosage: 15 g twice daily
Total daily dose: 30 g
Total batch quantity: 900 g
Step 1. Raw Herbal Ingredients (Primary Kashaya Dravya)
These herbs form the core respiratory and Kapha-clearing base.
- Vyaghri (Solanum xanthocarpum) coarse powder – 150 g
- Haritaki (Terminalia chebula) coarse powder – 120 g
- Kantakari root and whole plant (additional support) – 80 g
- Vasa leaves (Adhatoda vasica) – 80 g
- Guduchi stem (Tinospora cordifolia) – 60 g
- Pushkarmool (Inula racemosa) – 50 g
Add all the above herbs to 8 liters of potable water.
Boil on mild fire and reduce to 1 liter of decoction.
Filter carefully through muslin cloth to obtain a clear Kashaya.
Step 2. Sweetening and Avaleha Base Formation
- Jaggery (Guda), purified – 400 g
Add jaggery to the filtered decoction.
Heat on mild flame with continuous stirring until a thread consistency begins to appear.
Ensure slow heating to avoid caramelization or burning.
Step 3. Fine Herbal Powders (Prakshepa Dravya)
Add the following powders gradually while stirring continuously:
- Pippali churna (Piper longum) – 25 g
- Shunthi churna (Zingiber officinale) – 20 g
- Maricha churna (Piper nigrum) – 15 g
- Bharangi churna (Clerodendrum serratum) – 20 g
- Musta churna (Cyperus rotundus) – 15 g
- Talisa patra churna (Abies webbiana) – 15 g
Cook until the mixture attains proper Avaleha paka lakshana
Thick, glossy, non-sticky, and aromatic.
Step 4. Medicated Ghee Addition
- Cow ghee (clarified butter) – 100 g
Add ghee at the final stage and mix thoroughly on low flame.
Ghee enhances tissue penetration, Vata balance, and night-time efficacy.
Step 5. Mineral and Bhasma Addition (After Cooling)
Once the Avaleha cools to lukewarm temperature, add the following micro-dosed, classical Bhasma, finely sieved and pre-triturated:
- Abhrak Bhasma (Shataputi) – 2 g
- Swarna Makshik Bhasma – 3 g
- Godanti Bhasma – 5 g
- Mukta Shukti Bhasma – 5 g
Mix thoroughly to ensure uniform dispersion.
These Bhasma support
respiratory tissue strength
neuromuscular coordination
metabolic correction
and Ojas preservation.
Step 6. Final Weight Adjustment
Adjust final consistency with minimal warm decoction if required.
Ensure total finished quantity is approximately 900 g.
Store in airtight, amber-colored glass containers.
Dosage and Administration
- Dose: 15 g twice daily
- Timing: Morning and evening
- Best taken with lukewarm water or lukewarm milk
- Duration: 30 days
Preferably taken 30–45 minutes before meals.
Precautions and Warning Factors
- This formulation should be taken only under the supervision of a qualified Ayurvedic physician, especially due to the inclusion of Bhasma.
- Not recommended during acute fever, active infection, or severe dehydration.
- Patients with advanced renal disease, uncontrolled hypertension, or known heavy-metal sensitivity require dose modification or exclusion of mineral components.
- Avoid concurrent use with alcohol or sedative drugs.
- Pregnant and lactating women should not use this formulation unless specifically prescribed.
- Overdosage may aggravate Pitta, causing gastric irritation or loose stools.
- Dietary regulation is essential. Heavy, cold, oily, and late-night meals reduce effectiveness.
Clinical Note
Vyaghri Haritaki Avaleha is not a general tonic or supplement. It is a therapeutic classical medicine designed to reverse Kapha-Vata driven respiratory obstruction when used with correct indication, dosage, and dietary discipline.
Duration of Treatment and Prognosis
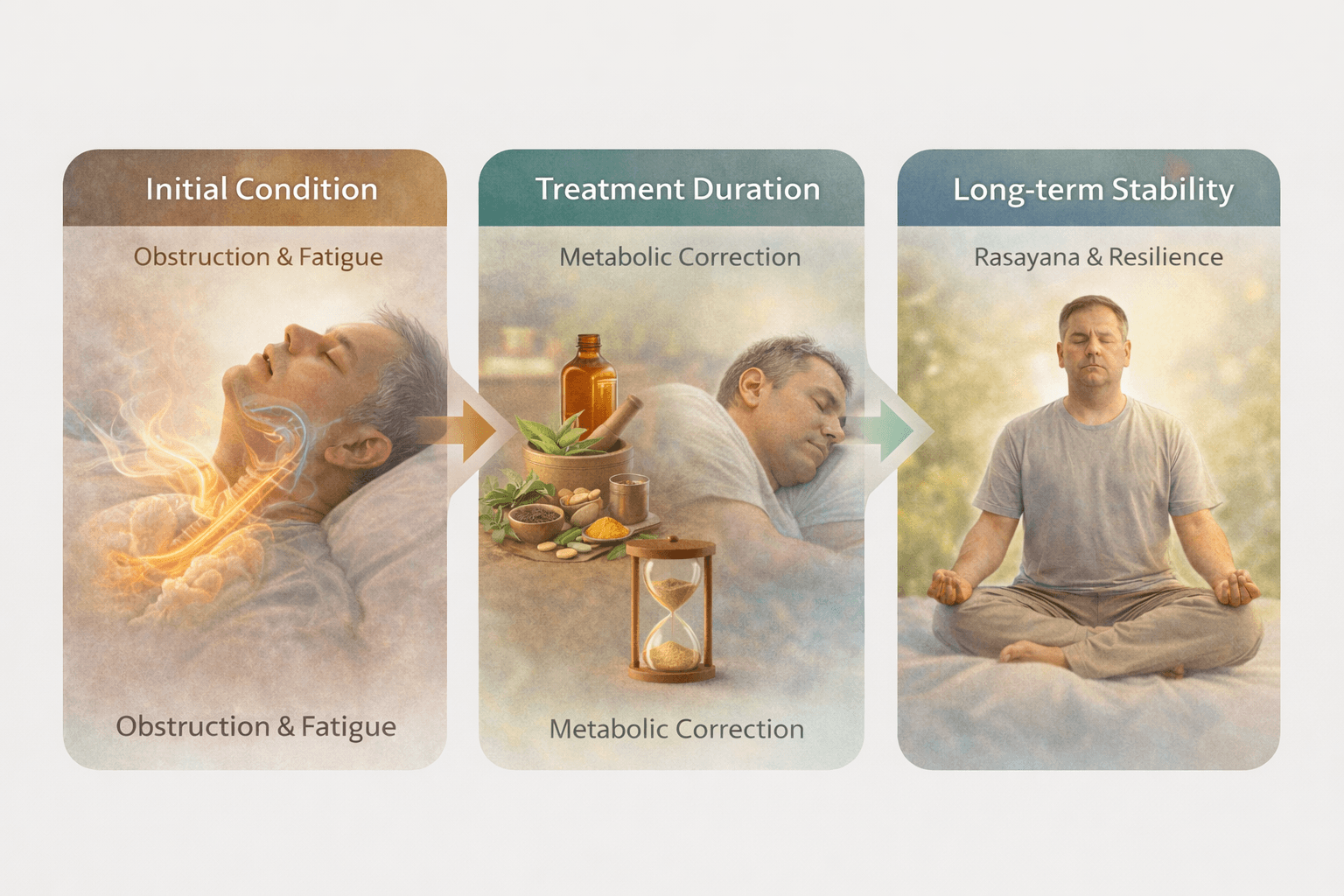
The duration of treatment for sleep apnea in an integrative Ayurvedic framework depends on multiple interacting factors rather than a fixed timeline. In my clinical experience, prognosis is not determined solely by the severity of breathing pauses but by how deeply the underlying metabolic, respiratory, and vitality related imbalances are corrected. When treatment addresses root pathology and is followed by appropriate Rasayana support, long term stability and sustained improvement are achievable [3] [11].
Factors Influencing Duration of Treatment
The time required for meaningful improvement varies from person to person. Key determinants include the chronicity of sleep apnea, degree of Kapha accumulation, involvement of Meda Dhatu, baseline metabolic efficiency, and the extent of Ojas depletion. Patients with recent onset symptoms, mild to moderate obstruction, and preserved metabolic strength often show noticeable improvement within a few weeks of structured therapy.
In contrast, individuals with long standing disease, obesity, metabolic syndrome, or cardiovascular involvement typically require a longer course of treatment. In such cases, therapy progresses in phases, beginning with obstruction reduction and metabolic correction, followed by stabilization and tissue strengthening. From a prognostic standpoint, patience and continuity are essential, as premature discontinuation often limits long term outcomes [3].
Role of Metabolic Correction in Prognosis
Metabolic correction is central to both treatment duration and prognosis. Sleep apnea is closely linked to impaired digestion, inefficient tissue metabolism, and abnormal fat deposition. If these factors are not corrected, symptomatic improvement remains fragile. When Agni is restored and Meda metabolism normalizes, the airway environment becomes more stable, and breathing during sleep improves naturally.
From a clinical perspective, patients who adhere to dietary regulation, lifestyle alignment, and metabolic supportive therapies experience faster and more sustained improvement. This metabolic reset reduces disease recurrence and enhances the effectiveness of respiratory focused interventions [3].
Rasayana and Long Term Outcome Stability
Rasayana therapy has a decisive influence on prognosis. While initial treatment phases address obstruction and imbalance, Rasayana determines whether the improvement endures. By strengthening Dhatus, stabilizing nervous system regulation, and restoring Ojas, Rasayana creates physiological resilience against relapse.
In my observation, patients who continue Rasayana support beyond the active treatment phase maintain better sleep quality, consistent breathing patterns, and improved daytime energy over the long term. Rasayana does not produce abrupt changes but gradually consolidates gains, making it a key determinant of long term success rather than short term relief [11].
Prognostic Outlook
When sleep apnea is approached as a reversible functional disorder rather than a permanent structural defect, the prognosis becomes favorable. Patients who engage in a comprehensive treatment plan that includes obstruction management, metabolic correction, and sustained Rasayana support often experience progressive reduction in symptoms and improved overall health.
From a broader medical perspective, correcting sleep apnea also reduces long term cardiovascular and metabolic risks, further improving prognosis and quality of life. This integrated outlook highlights that treatment duration should be viewed as an investment in long term stability rather than a race toward quick symptomatic control [3] [11].
Frequently Asked Questions
Can sleep apnea be cured or is it only manageable?
This is one of the most common and important questions I receive. From a conventional medical standpoint, sleep apnea is generally considered a chronic condition that is managed rather than cured, primarily through long term device based therapies such as CPAP [6]. However, from an Ayurvedic perspective, sleep apnea is viewed as a functional disorder arising from correctable imbalances involving Pranavaha Srotas, Kapha accumulation, Vata dysregulation, and metabolic dysfunction. When these root causes are systematically corrected through individualized treatment, sustained improvement and long term resolution are achievable [9] [10]. The key difference lies in addressing causation rather than compensating for symptoms.
How long do patients usually need to use CPAP?
In conventional care, CPAP is typically prescribed as a lifelong therapy. Patients are often advised to continue CPAP indefinitely because discontinuation usually leads to the rapid return of apnea events [6]. This is because CPAP does not alter the underlying pathology that causes airway collapse. In contrast, Ayurvedic management focuses on restoring natural airway stability and respiratory rhythm. As root imbalances improve, dependence on external mechanical support may reduce or become unnecessary in selected cases, provided treatment is consistent and appropriately guided [9].
Is it safe to stop CPAP if Ayurvedic treatment is started?
CPAP should never be discontinued abruptly without proper clinical assessment. In my practice, when patients are already using CPAP, Ayurvedic treatment is introduced in a phased manner. As symptoms, sleep quality, and objective indicators improve, CPAP use may be reassessed gradually. The transition must always be individualized and medically supervised. Ayurveda does not advocate unsafe discontinuation but aims to create conditions where the body can maintain airway patency naturally over time [6] [9].
How is Ayurvedic treatment different from conventional sleep apnea treatment?
The fundamental difference lies in treatment philosophy. Conventional medicine primarily relies on mechanical airway support and symptomatic control. Ayurveda, on the other hand, evaluates digestion, metabolism, tissue quality, nervous system regulation, and vitality alongside respiratory function. Treatment strategies include clearing obstruction, balancing doshas, strengthening neuromuscular control, and restoring Ojas. This comprehensive approach explains why Ayurveda targets long term stability rather than continuous dependence on devices [9] [10].
Who is an ideal candidate for Ayurvedic treatment of sleep apnea?
Patients with mild to moderate sleep apnea, metabolic imbalance, obesity related airway obstruction, chronic snoring, disturbed sleep, and poor daytime energy often respond well to Ayurvedic treatment. Even individuals with long standing disease may benefit, although treatment duration may be longer. Prognosis is best when patients are willing to follow dietary guidance, lifestyle correction, and sustained Rasayana therapy [1] [9].
Does Ayurvedic treatment work for central or mixed sleep apnea?
Ayurvedic treatment is particularly effective in conditions involving functional dysregulation rather than irreversible neurological damage. In central or mixed sleep apnea, outcomes depend on the underlying cause. When nervous system regulation, metabolic stress, or Vata imbalance is a contributing factor, Ayurvedic therapy may offer meaningful improvement. However, cases involving structural brain injury or advanced neurological disease require careful evaluation and integrative care [1] [10].
How long does it take to see improvement with Ayurvedic treatment?
Initial improvements such as reduced snoring, better sleep continuity, and improved morning freshness may be noticed within weeks in responsive cases. Deeper correction involving metabolic balance and airway stability takes longer and depends on disease chronicity, constitution, and adherence to therapy. Rasayana support plays a critical role in sustaining these improvements over time [9] [10].
Is Ayurvedic treatment safe for long term use?
When prescribed correctly by a qualified Ayurvedic physician, classical Ayurvedic medicines are designed for long term use and systemic restoration. Unlike symptomatic drugs, they aim to strengthen physiology rather than suppress function. However, individualized dosing, periodic reassessment, and proper selection of formulations are essential for safety and effectiveness [1] [9].
What makes Ayurvedic management more sustainable in the long run?
Ayurvedic management focuses on restoring the body’s inherent capacity to regulate breathing, sleep, and metabolism. By addressing Kapha accumulation, stabilizing Vata, improving tissue quality, and rebuilding Ojas, Ayurveda reduces the likelihood of relapse once improvement is achieved. This root oriented approach distinguishes it from models that rely solely on continuous external support [6] [9] [10].
These answers reflect the core philosophical and clinical differences between conventional and Ayurvedic approaches to sleep apnea, offering clarity to patients seeking long term solutions grounded in classical medical principles [1] [6] [9] [10].
Case Study
Case Study 1
Middle-Aged Male with Obstructive Sleep Apnea and Obesity
A 48-year-old male presented with loud snoring, witnessed breathing pauses during sleep, morning headaches, and excessive daytime sleepiness for over four years. He was overweight with central obesity and had been advised continuous CPAP therapy after polysomnography confirmed moderate obstructive sleep apnea. Although CPAP reduced symptoms initially, he reported poor compliance due to discomfort and fragmented sleep.
From an Ayurvedic assessment, the condition was diagnosed as Kapha-Vata dominant Pranavaha Srotas Dushti with significant Meda Dhatu involvement. Treatment focused on Kapha clearance, metabolic correction, and respiratory strengthening. Vyaghri Haritaki Avaleha was prescribed as the core formulation, supported by dietary regulation and Rasayana therapy.
Within eight weeks, the patient reported reduced snoring intensity, improved sleep continuity, and increased morning energy. Over four months, daytime sleepiness resolved significantly, body weight reduced modestly, and CPAP dependency decreased under supervision. Long-term Rasayana support helped maintain stable sleep and breathing patterns.
Case Study 2
Female Patient with Sleep Apnea and Metabolic Syndrome
A 42-year-old female reported chronic fatigue, non-refreshing sleep, difficulty concentrating, and mild snoring. She had insulin resistance, borderline hypertension, and disturbed sleep for nearly three years. Sleep study findings suggested mild to moderate sleep apnea.
Ayurvedic evaluation revealed Kapha accumulation with impaired Agni and early Ojas depletion. The patient was not advised CPAP initially due to mild disease severity. Treatment emphasized Shamana therapy using Vyaghri Haritaki Avaleha along with metabolic correction and gradual Rasayana introduction.
After six weeks, the patient experienced improved sleep quality, reduced fatigue, and better daytime alertness. At three months, metabolic markers showed improvement and snoring became occasional. Continued Rasayana therapy helped stabilize outcomes and prevent relapse, highlighting the role of metabolic correction in prognosis.
Case Study 3
Long-Standing Snoring and Sleep Fragmentation in a Lean Individual
A 36-year-old lean male presented with chronic snoring, frequent night awakenings, and poor sleep quality despite normal body weight. Polysomnography confirmed mild obstructive sleep apnea. There was no significant obesity, but the patient reported irregular eating habits, late nights, and chronic stress.
Ayurvedic assessment indicated Vata aggravation with Kapha Avarana in Pranavaha Srotas and early Majja Dhatu involvement. Treatment focused on stabilizing Vata, clearing subtle Kapha obstruction, and restoring neuromuscular coordination through Avaleha-based therapy and Rasayana support.
Within one month, sleep fragmentation reduced noticeably. Over three months, snoring diminished substantially and daytime cognitive clarity improved. This case demonstrated that sleep apnea is not solely weight dependent and can be effectively addressed by correcting functional imbalances.
Case Study 4
Patient with CPAP Intolerance and Recurrent Symptoms
A 55-year-old male with severe snoring, nocturnal choking, and daytime fatigue had been on CPAP therapy for over two years. He reported inconsistent use due to discomfort and travel-related difficulties. Symptoms returned quickly whenever CPAP was discontinued.
Ayurvedic evaluation identified long-standing Kapha accumulation, Meda Dushti, and significant Ojas depletion. A phased treatment approach was adopted, beginning with Shamana therapy using Vyaghri Haritaki Avaleha, followed by Rasayana therapy for tissue and vitality restoration.
Over five months, the patient reported improved sleep quality, reduced nocturnal awakenings, and better daytime stamina. CPAP usage was gradually reduced under supervision. While not immediately discontinued, dependence decreased, and overall quality of life improved, highlighting Ayurveda’s role in reducing device dependency.
Case Study 5
Sleep Apnea with Neurocognitive Complaints
A 50-year-old professional presented with memory issues, irritability, poor focus, and chronic sleep disruption. Snoring and breath holding during sleep were reported by the partner. Sleep apnea was confirmed through clinical evaluation.
Ayurvedic assessment revealed Pranavaha Srotas dysfunction with Majja Dhatu weakness and Ojas depletion due to prolonged sleep disturbance. Treatment emphasized airway clearance through Avaleha therapy combined with Rasayana aimed at nervous system support.
After two months, the patient noted improved mental clarity, reduced irritability, and more stable sleep. At six months, neurocognitive symptoms improved significantly, and sleep quality remained stable, reinforcing the link between respiratory stability, Ojas restoration, and cognitive health.
Clinical Insight
Across these cases, outcomes depended not on symptom suppression but on addressing Kapha obstruction, stabilizing Vata, correcting metabolism, and rebuilding Ojas. The consistency of improvement across varied patient profiles demonstrates why Ayurveda views sleep apnea as a modifiable functional disorder, not an irreversible condition.
REFERENCE LIST
Sleep Apnea (Modern Medicine + Ayurveda)
[1] Global definition, prevalence, and burden of sleep apnea
Supports sections: Introduction, Global burden, Complications, Underdiagnosis
Benjafield, A. V., Ayas, N. T., Eastwood, P. R., Heinzer, R., Ip, M. S. M., Morrell, M. J., … Malhotra, A. (2019). Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. The Lancet Respiratory Medicine, 7(8), 687–698.
https://doi.org/10.1016/S2213-2600(19)30198-5
[2] Pathophysiology of obstructive sleep apnea
Supports sections: Pathophysiology, Intermittent hypoxia, Sympathetic activation
Jordan, A. S., McSharry, D. G., & Malhotra, A. (2014). Adult obstructive sleep apnoea. The Lancet, 383(9918), 736–747.
https://doi.org/10.1016/S0140-6736(13)60734-5
[3] Cardiovascular and metabolic complications
Supports sections: Complications, Hypertension, Diabetes, Stroke
Somers, V. K., White, D. P., Amin, R., Abraham, W. T., Costa, F., Culebras, A., … Young, T. (2008). Sleep apnea and cardiovascular disease. Journal of the American College of Cardiology, 52(8), 686–717.
https://doi.org/10.1016/j.jacc.2008.05.002
[4] Neurocognitive and hormonal impact
Supports sections: Daytime symptoms, Cognitive decline, Sexual dysfunction
Beebe, D. W., & Gozal, D. (2002). Obstructive sleep apnea and the prefrontal cortex: Towards a comprehensive model linking nocturnal upper airway obstruction to daytime cognitive and behavioral deficits. Journal of Sleep Research, 11(1), 1–16.
https://doi.org/10.1046/j.1365-2869.2002.00289.x
[5] Diagnostic framework and polysomnography
Supports sections: Diagnosis, AHI interpretation, Sleep studies
American Academy of Sleep Medicine. (2014). International classification of sleep disorders (3rd ed.). Darien, IL: AASM.
https://aasm.org/clinical-resources/international-classification-of-sleep-disorders/
[6] CPAP mechanism and limitations
Supports sections: Conventional treatment, CPAP, Compliance issues
Weaver, T. E., & Grunstein, R. R. (2008). Adherence to continuous positive airway pressure therapy. Proceedings of the American Thoracic Society, 5(2), 173–178.
https://doi.org/10.1513/pats.200708-119MG
[7] Obesity, Kapha-like phenotype, and airway collapse
Supports sections: Causes, Risk factors, Obesity correlation
Schwartz, A. R., Patil, S. P., Laffan, A. M., Polotsky, V., Schneider, H., & Smith, P. L. (2008). Obesity and obstructive sleep apnea. Proceedings of the American Thoracic Society, 5(2), 185–192.
https://doi.org/10.1513/pats.200708-137MG
[8] Central sleep apnea and neurological regulation
Supports sections: CSA, Mixed apnea, Neural control
Eckert, D. J., & Malhotra, A. (2008). Central sleep apnea. Chest, 133(6), 1489–1500.
https://doi.org/10.1378/chest.07-2681
AYURVEDIC CLASSICAL REFERENCES
(Primary sources for Avaleha selection and pathogenesis)
[9] Shwasa Roga and Kapha-Vata obstruction
Supports sections: Ayurvedic correlation, Samprapti, Pathogenesis
Charaka Samhita, Chikitsa Sthana, Shwasa Chikitsa Adhyaya (Chapter 17).
English translation by R. K. Sharma & Bhagwan Dash. Chaukhambha Sanskrit Series Office, Varanasi.
(Reference to Kapha-avarana of Prana and Shwasa Roga)
[10] Vyaghri Haritaki Avaleha – primary indication
Supports sections: Best Avaleha, Core treatment
Charaka Samhita, Chikitsa Sthana, Chapter 17, verses describing Vyaghri Haritaki Avaleha.
Text: Charaka Samhita with Chakrapani commentary, Chaukhambha.
[11] Avaleha rationale and Rasayana action
Supports sections: Avaleha form benefits, Rasayana phase
Ashtanga Hridaya, Chikitsa Sthana, Shwasa-Hikka Chikitsa Adhyaya.
English translation by K. R. Srikantha Murthy. Chaukhambha Krishnadas Academy.
[12] Pranavaha Srotas and Nidra physiology
Supports sections: Pranavaha Srotas, Sleep disturbance, Ojas
Sushruta Samhita, Sharira Sthana, Srotas Vijnaniya Adhyaya.
English translation by Kaviraj Kunja Lal Bhishagratna.
[13] Kapha, Meda, and airway heaviness
Supports sections: Obesity, Kapha dominance, Relapse prevention
Bhavaprakasha, Purva Khanda, Medoroga and Shwasa Prakarana.
Edited by Pandit Sri Brahma Shankar Mishra. Chaukhambha Sanskrit Bhavan.
INTEGRATIVE & SUPPORTIVE MODERN RESEARCH
[14] Breathing retraining and autonomic balance
Supports sections: Pranayama, Yoga integration
Saoji, A. A., Raghavendra, B. R., & Manjunath, N. K. (2019). Effects of yogic breathing on autonomic nervous system. Journal of Ayurveda and Integrative Medicine, 10(4), 269–275.
https://doi.org/10.1016/j.jaim.2018.02.005
[15] Sleep, hypoxia, and oxidative stress
Supports sections: Ojas depletion, Tissue damage
Lavie, L. (2015). Oxidative stress in obstructive sleep apnea. Sleep Medicine Reviews, 20, 27–45.
https://doi.org/10.1016/j.smrv.2014.07.002