- Anatomy and Physiology
- Psychosexual Framework
- Male Sexual Disorders
- Female Sexual Disorders
- Sexually Transmitted Infections (STIs)
- Infertility
- Hormonal Imbalance
- Ayurvedic Sexual Medicine (Vajikarana)
- Therapeutic Formulations
- Diagnostic Protocol
- Therapeutic Approach
- Special Topics
- Research and Case Studies
- Frequently Asked Questions (FAQs)
- Reference
Sexual health for men and women is more than intimacy. It is emotional connection, physical comfort, personal confidence, hormonal balance, and relationship harmony. Many people do not talk about sexual concerns openly, yet these issues silently affect quality of life, body image, and even marital or romantic satisfaction.
When I began studying sexual medicine, I realised how common these problems are, even among seemingly healthy individuals. You may relate to this. You may have questions that feel difficult to ask. You may wonder why your desire has changed or why intimacy no longer feels effortless. You are not alone.
Why Sexual Health Matters
The World Health Organization describes sexual health as complete physical, emotional, mental, and social well being in relation to sexuality, not merely the absence of dysfunction [2]. This means sexual health for men and women is a real medical subject. It is not a taboo matter and not something to feel shy about.
A man struggling with erections may think it is age or stress. A woman experiencing low lubrication may believe it is normal. A couple may feel distance and think it is fate. In reality, most sexual problems are treatable with proper evaluation. Everybody has the right to understand their body and seek recovery confidently.
How Sexual Medicine Helps
Sexual medicine brings together reproductive biology, hormones, brain chemistry, psychology, lifestyle science, and relationship behaviour to understand intimacy [1]. It looks at human experience from all angles because sexual function is influenced by more than the genital organs. Hormonal shifts, emotional stress, sleep, pelvic circulation, chronic illness, self image, and partner communication play important roles.
Sexual health for men and women therefore involves the whole person. It belongs to every patient. It belongs to couples who want deeper connection. It belongs to those who feel something has changed. It belongs to anyone who is searching for answers and healing.
If You Are Reading This
You may want to improve performance. You may want to regain desire. You may wish to solve erection difficulty or premature ejaculation. You may want support for female sexual pain, low libido, or recovery after childbirth or menopause. Whatever brings you here, this guide is for you. You will learn the science of sexual function and how solutions exist for both men and women.
This is the beginning of your journey. A journey of awareness and healing. A journey from silence to understanding. A journey where sexual health for men and women becomes clear, respectful, and supported by real medical evidence.
Anatomy and Physiology
When we speak about sexual health, we first try to understand how the body is built and how each part works. I realise that for many people the sexual system feels like a private subject, but once you look at it from a scientific and human perspective, everything becomes easier to understand. You as a reader will be able to visualise what happens inside the body in a simple and clear way, and any person who studies human sexuality can appreciate how beautifully this system functions.
Understanding the Male Body and Function
A man has sexual organs which include the penis, testes, epididymis, vas deferens, prostate gland and seminal vesicles. Inside the penis we find erectile tissue called corpora cavernosa and corpus spongiosum. During sexual stimulation the brain sends a message through the nerves, I would call it a signal of excitement. Nitric oxide gets released which relaxes the smooth muscles and allows blood to fill the penis. This is what causes a firm erection [3] [5].
The testes create sperm and testosterone. A man usually feels desire, confidence and sexual strength when testosterone stays within a healthy range [3] [5].
Understanding the Female Body and Function
A woman has her own unique sexual anatomy which includes the clitoris, vagina, cervix, uterus, ovaries and breasts. The clitoris contains a very high concentration of nerves which is why even a gentle touch can produce intense pleasure. When a woman feels safe, comfortable and emotionally connected, blood flow naturally increases in the genital area and the body creates lubrication. Female desire is strongly influenced by hormones like estrogen, progesterone and oxytocin. These hormones help her feel loved, connected, emotionally fulfilled and ready for sexual intimacy [4].
How Body and Mind Work Together
In simple terms, sexual response is not just physical. The brain produces desire, the nerves carry messages, the hormones refine the feeling and the blood vessels complete the physical response we call arousal [3] [4] [5]. If any one part struggles, the entire experience changes. For example stress, anxiety, diabetes, hormonal imbalance, lack of sleep and even relationship tension can affect erection, desire, pleasure or orgasm. When we view the body this way, we understand that sexual difficulty is not a weakness. It is a signal that some part of the system needs attention and healing.
This understanding forms the foundation for recovery. When you know how your body works, you will no longer feel confused or helpless. You can look at your own sexual health with confidence, knowledge and clarity.
Psychosexual Framework

When we look deeper into sexual health, we realise that it is not only about organs and hormones. I often explain to patients that sexuality lives in both the mind and the body. You feel desire not only because the body is ready, but also because the mind allows it. Every person carries emotions, memories and thoughts that shape the sexual experience. When you understand this, you can view sexual challenges with compassion instead of blame.
Understanding the Role of the Mind
During sexual activity, the brain becomes the first switch. If the mind is relaxed, confident and emotionally open, the body responds smoothly. When a person feels pressured, insecure or stressed, the nervous system pulls back. You may have noticed this yourself. A worrying thought, a moment of self judgement or fear of performance can interrupt arousal. This is why many men struggle with erection during anxiety and many women lose desire when they feel unheard or emotionally distant [6].
Emotions, Relationships and Past Experiences
Sexuality is powerful because it connects both emotion and physical sensation. A happy relationship, gentle touch and feeling loved increase the sexual response. On the other hand, relationship conflict, shame, guilt, trauma or negative experiences can create invisible blocks in the mind. These blocks are rarely spoken about, but they are real for many couples. When a couple learns to communicate openly, intimacy grows naturally and the body follows [6] [7].
Porn Exposure and Sensory Conditioning
Modern research shows that regular pornography alters expectation and sensitivity. When the mind becomes used to high intensity stimulation on screen, real intimacy may feel less exciting. A person may become dependent on visual content to achieve arousal and this can interfere with natural sexual connection. When we understand this pattern, we can guide the patient step by step to retrain the brain toward real life intimacy again [7].
Why Psychosexual Understanding Matters
Sexual dysfunction often begins in the mind before the body shows symptoms. When we address stress, relationship dynamics, lifestyle, confidence and beliefs about sex, recovery becomes faster and more complete. I remind patients that their mind is not their enemy. It is a guide that needs support and reassurance. You have the ability to heal sexual concerns by nurturing both emotional and physical well being together.
Male Sexual Disorders
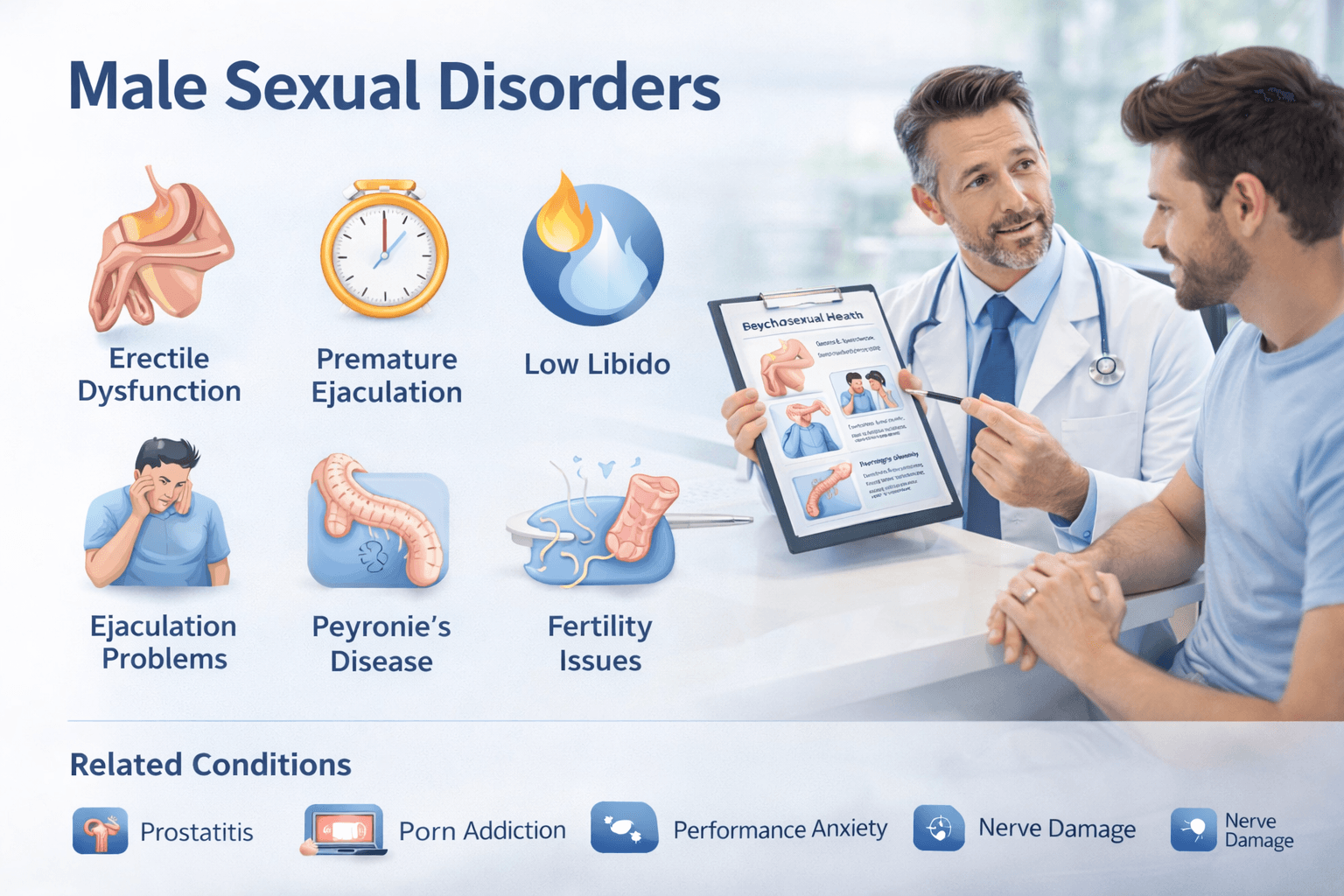
A man’s sexual life is shaped by biology, emotion and self identity, therefore when a problem appears in this area the entire confidence system of a person is affected. I often meet men who look strong on the outside, but inside they carry silent fear. You might also recognise this feeling. Sexual disorders are not signs of weakness. They are clinical conditions that can be understood, diagnosed and treated step by step. When we understand how they arise, we can heal with clarity instead of shame.
Erectile Dysfunction
Erectile dysfunction means the penis does not become firm enough or does not stay firm long enough for satisfying intercourse. Many men tell me that they feel desire mentally yet the body does not respond. You may have noticed morning erections decreasing or erections becoming inconsistent. This can be linked to blood vessel stiffness, nitric oxide shortage, diabetes, stress, alcohol use, smoking, pornography conditioning, pelvic floor weakness or vascular ageing [3] [5] [8].
Recovery becomes possible when we restore circulation, reduce fear of failure, strengthen pelvic nerves and address lifestyle factors scientifically.
Premature Ejaculation
In premature ejaculation, sexual climax occurs earlier than the man or partner wishes. Sometimes even before penetration begins. This makes a person feel a loss of control. A man may worry that his partner is unsatisfied which further increases anxiety. The condition is often a combination of sensitive ejaculation reflex, anxiety, overstimulation, past habits and mental tension [9].
With breathing training, stimulation timing control and specific exercises, control gradually returns.
Delayed Ejaculation and Anejaculation
Delayed ejaculation means ejaculation takes a very long time and requires intense effort. Some men can have penetration but cannot reach climax inside the partner. Anejaculation means zero release despite stimulation.
In my experience, this happens when dopamine reward pathways become blunted due to overstimulation by pornography or masturbation patterns, or when there is reduced nerve sensitivity, depression, medication side effects and sometimes post surgical nerve compromise [5] [8].
You may still feel pleasure but struggle to finish. Treatment focuses on retraining nerves, reducing dependency on intense stimulation and rebuilding arousal rhythm.
Low Libido and Loss of Sexual Desire
Low libido means a reduced inner drive for sexual activity. Many men are surprised to learn that libido is not only sexual energy but also emotional energy. I tell my patients that desire is like a flame that burns when the mind is peaceful. Stress, poor sleep, hormonal decline, low testosterone, exhaustion, nutritional deficiency and relationship stress reduce this flame [3] [5] [8].
With proper nourishment, couple bonding, exercise, sleep restoration and emotional healing, desire returns naturally.
Peyronie Disease and Penile Curvature
Some men notice the penis bending during erection which causes pain and difficulty during penetration. This is Peyronie disease, usually caused by plaque formation in penile tissue after micro trauma. A man may feel embarrassed or try to hide it from his partner. Curvature can increase over time if untreated. Treatment focuses on fibrosis softening, tissue healing and restoring flexibility [8].
Anorgasmia (Inability to Orgasm)
A man may be able to get an erection and maintain penetration but may not reach climax. This often appears when mental distraction, anxiety, fear of performance or guilt blocks the pleasure response. Neurological conditions, antidepressants and uncontrolled diabetes also contribute. Many men believe they are alone in this, but many others experience the same condition silently.
Sperm and Male Fertility Disorders
Infertility affects emotional identity deeply. When sperm count, motility or morphology becomes weak, conception may fail. Some men feel guilt even when they are not responsible. Semen analysis, hormone tests and lifestyle review help identify the cause. With improvement in diet, stress management, micronutrients and therapy guided treatment, sperm quality increases in many cases [9].
Testicular Pain, Varicocele and Hormonal Decline
Varicocele causes heavy or dragging pain in the scrotum and reduces sperm quality. Age related testosterone decline may cause fatigue, muscle loss, erectile weakness and emotional dullness. You may feel like your vitality is slipping. This is reversible when treatment addresses the cause instead of the symptom alone.
Prostatitis and Prostate Enlargement Impact
Chronic prostatitis creates pelvic pain, burning, ejaculatory discomfort and reduced sexual pleasure. Benign prostate enlargement can reduce erection quality and cause incomplete ejaculation. Many men only treat urine symptoms and forget that sexual life is also affected.
Pornography Induced Dysfunction
With constant artificial stimulation online, the brain becomes less responsive to real intimacy. A man might get a strong response to a screen but not to a real partner. This is a growing problem worldwide. When we slowly reverse stimulus dependency and rebuild natural arousal sensitivity, pleasure returns.
Priapism (Persistent Painful Erection)
Priapism is a rare emergency condition where erection continues for long hours without sexual desire and becomes painful. This requires immediate medical care to prevent tissue damage [5] [8].
Understanding the Emotional Side of Male Sexual Disorders
Every disorder above is not only physical. It is emotional, relational and psychological. You may fear judgement or you may feel less masculine. A partner may feel unloved or confused. A doctor, on the other hand, views it clinically without criticism. When you approach treatment with openness, healing begins. When a couple supports each other, results improve even faster.
A man is not defined by sexual performance alone. He is a complete human being, deserving care and healing.
Female Sexual Disorders
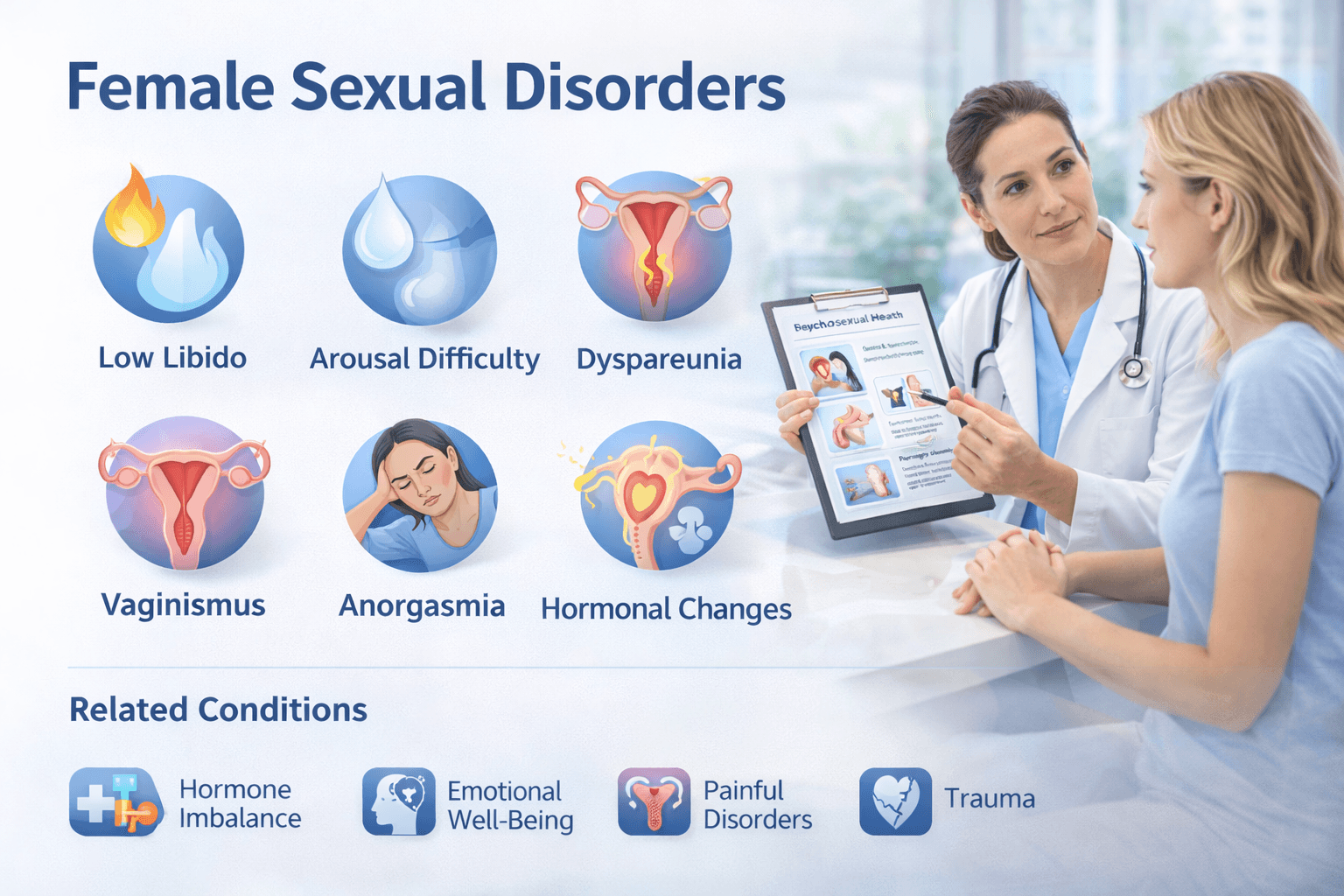
Female sexuality is complex and layered. It is shaped by the body, the brain, the heart, and even the hidden emotional world. When a woman faces sexual difficulty, she often carries that pain quietly. Many women tell me that they do not speak up because they do not want to disappoint their partner. You may have seen women normalise pain during intercourse, dismiss loss of desire as stress, or believe that pleasure is not important for them. In truth, female sexual disorders are real clinical conditions that deserve understanding, care, and treatment. When we look at them deeply, we see that healing is possible when the mind and body work together.
Low Libido or Reduced Sexual Desire
Low libido means a reduced inner desire for intimacy. Many women feel love emotionally but do not feel sexual spark in the body. A woman may think that something is wrong with her, but this condition is extremely common. Desire in women does not switch on instantly like a light switch. It behaves more like a flame that grows slowly with emotional closeness, safety, and stimulation.
Low libido can appear due to exhaustion, work stress, childbirth recovery, childcare responsibility overload, body image insecurity, poor sleep, hormonal imbalance, anemia, thyroid disorder, depression, side effects of antidepressants or contraceptive pills, and relationship dissatisfaction [10] [11].
I often remind women that desire is not forced, it is nurtured. When she feels relaxed, loved, supported, respected, and emotionally connected, the brain releases dopamine and oxytocin which open the pathways of intimacy. When understanding, gentle touch, and communication increase, desire begins to return naturally.
Arousal Difficulty and Lack of Lubrication
A woman may mentally want intimacy, yet her body may not respond with lubrication or sensitivity. This can be confusing and emotionally painful. Vaginal dryness is a major reason for arousal difficulty. It becomes more common during menopause, postpartum period, breastfeeding, post hysterectomy state, after radiation or chemotherapy, and during persistent stress [10].
Estrogen plays an important role in lubrication and tissue softness. When estrogen declines, the vaginal walls may feel dry or tight. A woman may start to avoid intercourse simply because her body associates it with discomfort instead of pleasure. This does not mean she is not attracted to her partner. It only means her body needs hormonal support, arousal time, and relaxation.
Slow foreplay, longer time to warm up, deep breathing, pelvic floor relaxation, warm oil based lubrication, and emotional reassurance help the tissues respond again. When the woman is allowed to take her time, arousal grows gradually.
Dyspareunia (Painful Intercourse)
Pain during intercourse is one of the most silently endured conditions in women. Many women believe that pain is normal or that they must tolerate it. Pain can appear at the vaginal entrance or deeper inside during thrusting. Causes include pelvic floor tension, vaginal dryness, recurrent fungal or urinary infections, vulvodynia, endometriosis, post childbirth scar sensitivity, thin vaginal tissue, trauma memories, or fear of pain itself [10] [12].
Pain creates anticipation of more pain. The body tightens as protection. You may notice how the mind wants intimacy but the body withdraws. The solution is gentle care. Relaxation therapy, pelvic muscle training, lubricants, Ayurvedic oil application, progressive desensitisation, partner patience, and trauma informed counseling bring relief over time.
Vaginismus
Vaginismus occurs when vaginal muscles contract involuntarily whenever penetration is attempted. This is not a woman’s fault. Her body reacts like it is protecting her. It is a subconscious reflex often rooted in fear, negative sexual conditioning, strict cultural upbringing, past trauma, or early painful experience [11].
Women describe it as the body closing by itself. Even inserting a finger or tampon becomes difficult. The solution is not force. It is gradual trust building. Under guided therapy, the woman learns to breathe through fear, use dilators slowly, practice relaxation, and introduce penetration step by step. When the mind feels safe, the body allows entry without fight.
Anorgasmia (Difficulty to Orgasm)
Some women can enjoy intimacy but cannot reach climax. This may cause self doubt or frustration. Many never discuss it because they fear judgement. Orgasm is a brain body event. The brain evaluates safety, desire, stimulation type, and emotional bonding. When thoughts interrupt the process, climax gets blocked.
Causes include anxiety, overthinking, guilt, religious shame conditioning, lack of clitoral stimulation, insufficient foreplay, hormonal imbalance, antidepressant medicines, peripheral neuropathy, or trauma [11] [12].
Orgasm improves when the woman learns her body, explores what she enjoys, communicates openly, and receives stimulation that matches her sensitivity. Patience and self awareness are key.
Female Sexual Arousal Disorder
In this disorder the woman feels desire emotionally, but the body does not show lubricated arousal. She may want closeness but her physical response remains weak. This disconnect often appears during menopause when estrogen falls and blood flow reduces [12].
This reminds us that sex in women is energy plus emotion. When blood circulation, hormones, and confidence are restored, arousal returns.
Hormonal and Reproductive Factors
Hormonal shifts throughout life affect sexual function. During childbirth recovery, breastfeeding, and menopause, estrogen drops. This can cause dryness, mood change, low libido, and painful sex. Thyroid disorders disrupt energy levels and anxiety threshold. Polycystic ovarian condition, anemia, vitamin D deficiency, obesity, chronic illness, and post surgery states also influence sexual wellness.
A woman’s sexual health is delicate because her endocrine system and emotional system speak to each other constantly.
Psychological and Emotional Blocks
For many women, sexual response begins in the mind. If she feels misunderstood or emotionally distant, desire fades. Fear of pregnancy, body shame, self consciousness, unresolved trauma, pressure to perform, hurried intercourse, betrayal, and lack of affection create emotional walls.
Trust, conversation, slow pace, and emotional intimacy melt these walls gently. When she feels valued and not demanded, her body responds.
Social Conditioning and Cultural Silence
Society often teaches women to be shy about desire. Many were raised hearing that sex is duty, not pleasure. Some women never explore their body, so pleasure remains unknown. Education changes this. When a woman understands her anatomy, her right to pleasure, and her emotional needs, sexuality becomes uplifting instead of stressful.
How Healing Happens
A woman is not defined by pain, dryness, low desire, or orgasm difficulty. She is a whole person. Sexual healing happens slowly but surely when body comfort, mind relaxation, relationship understanding, hormonal balance, nutrition, and confidence come together.
When a woman receives patience instead of pressure, love instead of fear, and knowledge instead of silence, she grows again. Intimacy becomes gentle, connected, and meaningful.
Sexually Transmitted Infections (STIs)
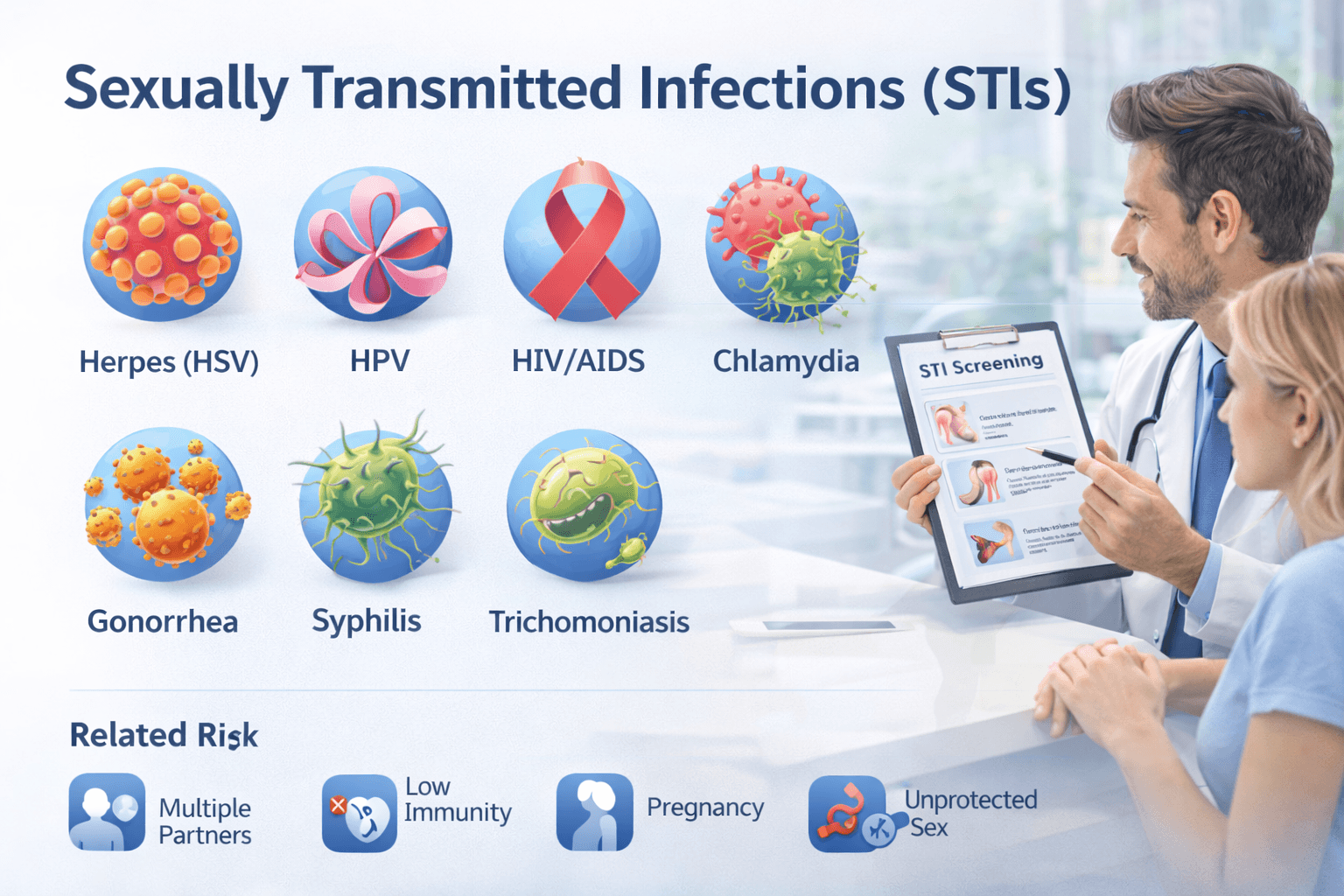
Sexually transmitted infections are infections that spread from one person to another mainly through sexual contact. This includes oral sex, vaginal sex, anal sex and even skin to skin genital contact in many cases. When we speak about STIs, most people think only of obvious symptoms. But in practice, a large portion of infected individuals look healthy, feel normal and carry the infection silently for months or even years. You may meet someone who shows no signs of illness and still transmits the virus unknowingly. This is why regular screening is not only important but necessary when a person is sexually active.
Many patients feel fear or shame when they hear the word infection. If you feel the same, you are not alone. I always tell them that infection is not a reflection of morality. It is a biological event, something that can be detected, treated and managed with correct medical support. When we replace fear with clarity, the body and mind both begin to heal.
How STIs Behave Inside the Body
Once an infection enters, some organisms multiply in the genital tract, some enter the bloodstream and some remain dormant inside nerves. Viral infections like HSV can sleep inside nerve ganglia and reactivate later. HPV can remain inside cervical cells without symptoms. HIV destroys immune cells slowly over time. Bacterial infections like chlamydia and gonorrhea may silently inflame reproductive organs and later present as infertility.
You may not feel anything at first, but inside the body small changes begin. Inflammation, mucosal damage, immune stress or hormonal imbalance appear gradually. When these signs are ignored, advanced disease results.
Herpes Simplex Virus (HSV 1 and HSV 2)
Herpes presents as painful blisters around the genitals or mouth. The first outbreak may cause fever, body pain, swollen glands and emotional shock. After this, the virus hides inside nerve cells and waits. During emotional stress, menstrual cycle fluctuation, weak immunity, poor sleep or illness, it can return and cause sores again.
A person may ask me whether herpes is permanent. The virus stays in the body, yes, but you can control outbreaks. Immunity, lifestyle stability, antiviral support and stress reduction reduce recurrence [14]. Many individuals live long comfortable lives with proper management.
Human Papillomavirus (HPV)
HPV is widespread globally. Most infections clear naturally as the immune system removes the virus within two years. Some strains produce warts, others increase the risk of cervical cancer. Smoking, weak immunity, poor vaginal microbiome and multiple partners increase persistence [15].
Women must undergo regular Pap smear and HPV testing especially after becoming sexually active. HPV also spreads through oral contact, so throat and mouth can become infected.
Human Immunodeficiency Virus (HIV)
HIV weakens the immune system by reducing CD4 cells. In early stages, there may be mild fever, fatigue or no symptom at all. Over months or years without treatment, immunity falls. The person becomes vulnerable to infections like tuberculosis and fungal disease [16].
Modern therapy helps people live normal long lives. Early diagnosis and treatment keep viral load low. Regular testing and condom use give strong protection.
Chlamydia
Chlamydia spreads silently. Women may notice unusual discharge, pelvic pain or spotting after intercourse. Men may feel burning while urinating or light discharge from the penis. Untreated chlamydia travels into the fallopian tubes and can cause infertility in women. Early treatment prevents long term damage [13].
Gonorrhea
Gonorrhea presents with yellow discharge, urethral burning and pelvic discomfort. In women, it may be missed easily since internal infection is less visible. If ignored, it leads to pelvic inflammatory disease and infertility. Reinfection is common if both partners are not treated together.
Syphilis
Syphilis begins with a painless sore. The sore heals but the infection continues deeper inside the body. Later it causes rash, fever and swollen glands. In advanced stages it affects the heart, nerves and brain. Screening is necessary for sexually active individuals [13].
Trichomoniasis
This is a parasitic infection. Women may notice frothy discharge and itching. Men often stay asymptomatic and spread it unknowingly. Treatment is simple but reinfection happens if one partner is untreated.
Additional STIs that Affect Sexual Wellbeing
• Hepatitis B and C transmitted sexually or through blood exposure
• Mycoplasma genitalium increasing infertility risk
• Bacterial vaginosis altering vaginal microbiome
• Candidiasis recurrent due to sugar diet and antibiotics
• Pubic lice and scabies causing genital itching
• Zika and CMV impact pregnancy and fetal health
Each infection has a unique behavior, so evaluation must be personalized.
Factors that Increase STI Risk
A woman or man is more vulnerable when:
• multiple partners are involved
• condoms are not used regularly
• alcohol or drugs reduce judgement
• stress weakens immunity
• vaginal dryness increases micro tears
• oral sex is practiced without protection
• menstrual phase lowers cervical immunity
• nutrient deficiency lowers defense
• pornography leads to unprotected encounters
• low self esteem leads to unsafe decisions
The body is not weak. It is unprotected at certain moments. Education empowers decision.
STIs in Pregnancy
Some infections cross from mother to baby during birth. HSV can cause newborn complications. Syphilis passes through placenta. HIV can be transmitted during pregnancy or breastfeeding if not controlled. Screening in pregnancy protects both mother and child.
Mental and Emotional Burden of STIs
The physical symptoms heal faster than the emotional impact. A person may feel guilt, betrayal or fear of rejection. Some break relationships due to stigma. I tell them that infection is temporary, but emotional scars remain if we do not heal them. When partners communicate honestly, trust rebuilds. When education replaces shame, sexual confidence returns.
Path to Healing
Testing, treatment, immunity building, partner treatment and safe practices create recovery. With awareness, antiviral or antibiotic support where required, lifestyle correction, and emotional acceptance, a person lives fully again.
Silence feeds infection. Knowledge cures.
Infertility
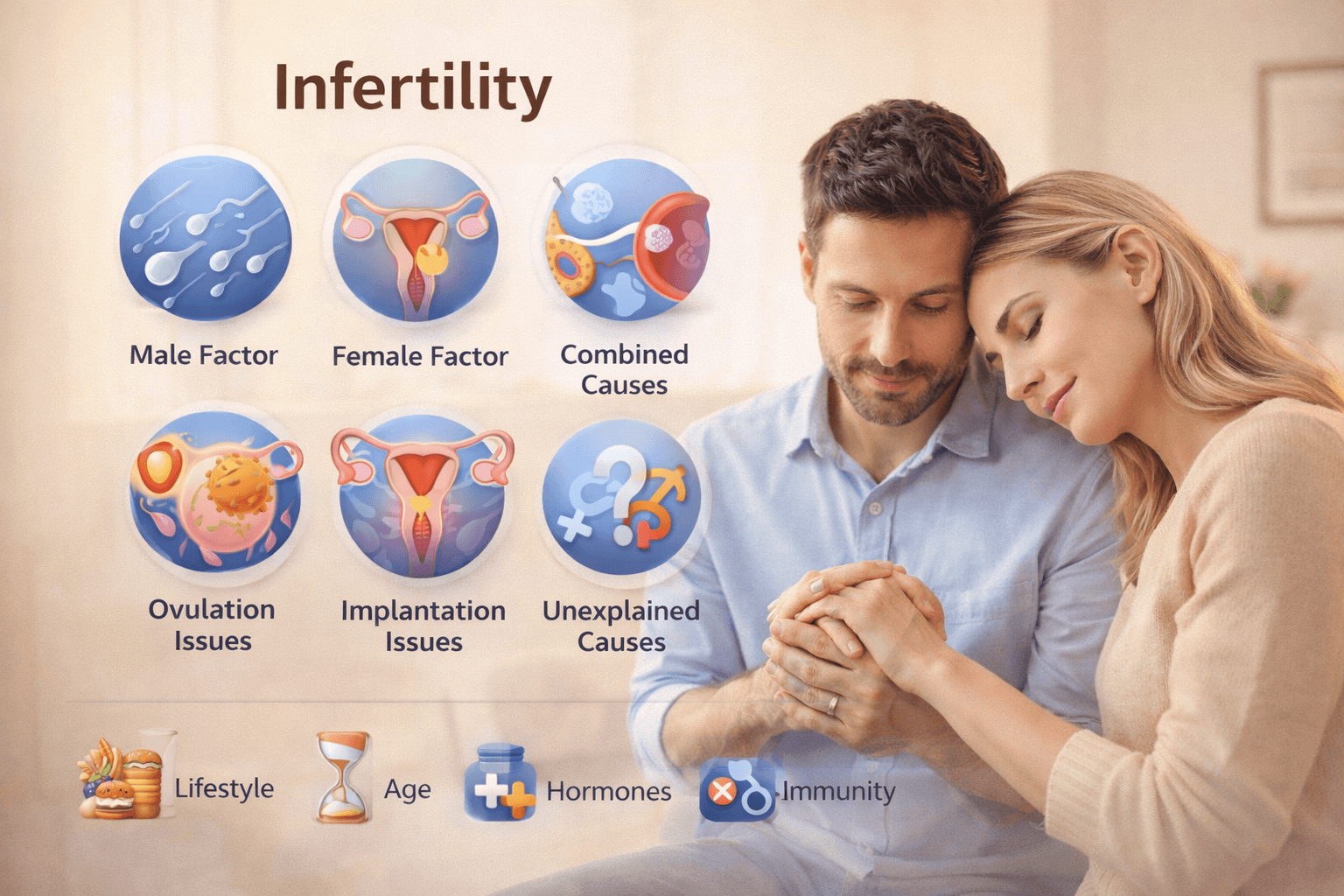
Infertility is a condition where a couple is unable to achieve conception despite regular and unprotected sexual intercourse for a significant period of time. What makes infertility unique is that it affects not only the reproductive system but also the emotional world of individuals. I have met women who feel a silent grief every month when menstruation arrives instead of pregnancy. Men often hide their disappointment behind a strong face. You may have witnessed how infertility slowly turns joy into anxiety, and hope into pressure. It is important to understand that infertility is a medical state, not a reflection of worth or identity.
Pregnancy is a biological miracle. For conception to occur, sperm must be healthy, an egg must mature and release, fallopian tubes must allow passage, the embryo must form and the uterus must accept and nourish new life. If even one link in this chain is disturbed, conception becomes difficult. Once we locate the weak link, treatment becomes clear.
Male Factor Infertility
Male infertility contributes to a large portion of infertility cases. Sometimes a man looks healthy, exercises well, eats normally, yet the semen analysis shows low count or slow motility. Semen quality depends on hormones, nutrition, testicular function, heat exposure, blood circulation, and stress. Environmental chemicals, smoking, alcohol, long sitting hours, mobile phones kept in pockets, excessive cycling, high fever, chronic illness and even frequent late night work weaken sperm production [17] [18].
When I speak to a man with low sperm report, I remind him that this is a biological imbalance, not a measure of masculinity. The body can recover when supported with antioxidants, minerals, better circulation, proper sleep and emotional calm. Many men improve beautifully when lifestyle and treatment go hand in hand. The WHO semen manual guides improvement evaluation [20].
Female Factor Infertility
Female infertility is often linked to ovulation issues, poor egg quality, fallopian tube blockage, hormonal imbalance, uterine conditions or endometrial receptivity. A woman’s body is sensitive to monthly hormonal rhythm. Stress, weight changes, thyroid imbalance or PCOS can disrupt ovulation. When the egg does not mature or release, conception becomes uncertain [19].
Endometriosis creates inflammation inside the pelvis. Fibroids, polyps or thin endometrium make implantation difficult. Previous infections like chlamydia may block tubes silently. Age also influences fertility. Egg reserve and genetic quality reduce gradually as time passes, especially after mid thirties. Age is not a barrier but a biological rhythm that needs awareness.
Combined and Unexplained Infertility
In many couples, both partners contribute small factors. Alone they may not cause infertility, but together conception becomes slow.
The most emotionally confusing situation is unexplained infertility where all reports look normal yet pregnancy does not happen. When this happens, couples feel helpless. They ask why everything appears fine yet nothing moves. Here we look deeper into hidden reasons like embryo quality, sperm DNA fragmentation, endometrial immunity, subtle hormone imbalance, chronic inflammation, stress chemistry, sleep cycle and even emotional energy between partners [17] [18].
The body is not refusing pregnancy. It is protecting balance. We must listen to what it needs.
How Ovulation Works and Why It Fails
Ovulation requires harmonious interaction between the brain, pituitary gland and ovaries. Stress, over dieting, intense exercise, low fat diet, trauma, shock or grief can pause ovulation. Many women are surprised when they learn that emotional burden can stop the egg from releasing. The body waits for safety first and pregnancy later.
Egg quality depends on mitochondrial strength, which declines with age, poor diet, oxidative stress, environmental toxins and lack of sleep. Antioxidants, healthy fat, protein, sunlight, micronutrients and deep rest nourish eggs.
Uterus and Endometrium
Even when sperm meets egg, implantation is the real doorway to pregnancy. A receptive uterus is essential. A thin endometrium, poor blood flow, inflammation, fibroids or adhesions may prevent implantation. Women with repeated early miscarriages often have endometrial issues that go unnoticed.
The goal is not only to fertilize an egg but to create a womb that welcomes and protects new life.
Lifestyle, Metabolism and Immunity in Fertility
Fertility reflects overall health. Modern lifestyle weakens reproductive capacity through:
• Sugar rich diet
• Junk food consumption
• Caffeine excess
• Smoking and alcohol
• Sedentary routine
• Late sleep pattern
• Vitamin D deficiency
• Screen addiction
• Stress hormones like cortisol
• Plastics and endocrine disruptors
These factors reduce sperm count and damage egg mitochondria. Immunological imbalance may also attack sperm or embryo, preventing implantation. When we heal metabolism, improve diet, reduce toxins and nourish the gut, fertility improves naturally.
Emotional Layer of Infertility
Infertility is heavier emotionally than medically. A woman may cry silently after every negative test. A man may feel helpless even if he never speaks it aloud. Partners may start blaming themselves or each other. Sexual intimacy becomes pressured, mechanical and joyless. I often encourage couples to return to love, not just reproduction. When intimacy becomes affectionate again, the body feels safe.
The womb opens when the heart opens.
Diagnostic Approach
Evaluation begins with semen analysis for men and ovulation tracking for women. Hormone tests measure thyroid, prolactin, FSH, LH and AMH levels. Follicular ultrasound monitors egg growth. HSG identifies blocked tubes. Advanced assessment includes sperm DNA fragmentation and endometrial receptivity mapping [20].
Information prevents confusion. Diagnosis brings direction.
Hope
Infertility is not a dead end. Many couples conceive naturally through lifestyle correction, ovulation regulation, pelvic healing, emotional support and targeted treatment. Others conceive through IVF or ICSI when needed. The journey requires patience but outcomes are often beautiful.
Your body is not broken. It is waiting for balance.
Hormonal Imbalance
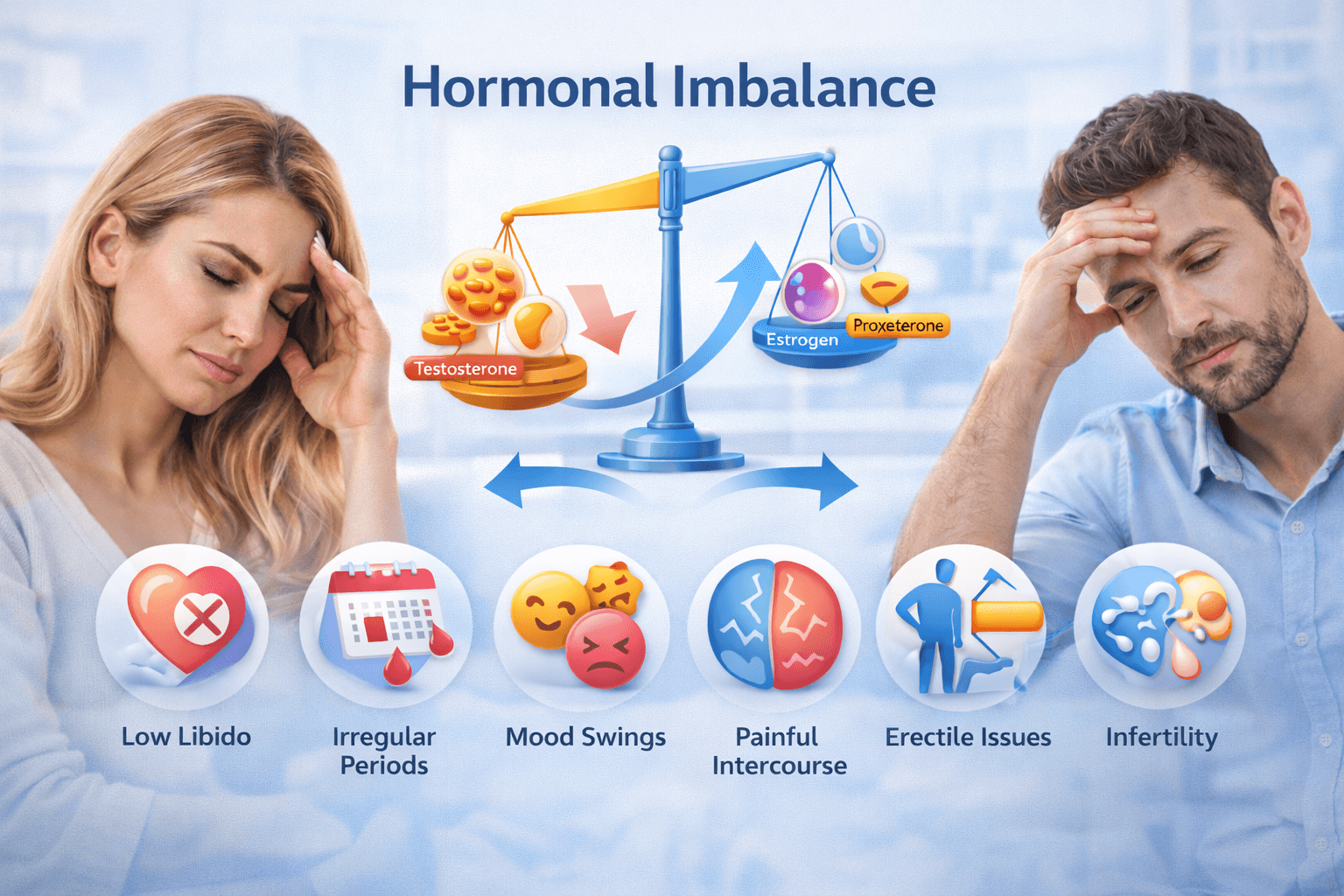
Hormones are the invisible messengers of the body. They move through blood, speak to organs, regulate mood, control energy, govern fertility and influence sexual desire. When hormones flow in harmony, the body feels light, thoughts stay calm and intimacy becomes natural. When the balance shifts, even slightly, the entire internal rhythm changes. A person may feel tired, irritable or emotionally fragile without understanding why. Hormonal imbalance is not visible externally, yet it silently affects sexual health, reproductive capacity and overall wellbeing.
I have met patients who tell me, “I love my partner but I do not feel the urge for sex anymore.” Another patient may say, “My mood switches without reason and I feel disconnected from my body.” These feelings are not weakness. They are signals from within. Hormones are speaking.
How Hormones Influence Sexual Function
Sexual function is not only about organs. It begins in the brain. Dopamine sparks desire, oxytocin builds bonding, testosterone strengthens libido, estrogen maintains lubrication and progesterone provides emotional calm for intimacy. When even one messenger drops or rises unusually, desire may fade or become irregular.
A man with low testosterone may experience reduced drive, fatigue and weaker erections. A woman with low estrogen may face dryness, pain during intercourse or reduced arousal. Hormonal imbalance is not only physical. It touches emotion, self confidence and relationship connection.
Female Hormonal Disturbance
Women experience continuous hormonal fluctuations throughout the month. If estrogen and progesterone do not rise and fall naturally, menstruation, ovulation and sexual desire are disturbed. PCOS, thyroid dysfunction, high prolactin, stress, poor sleep, nutritional deficiency and sedentary lifestyle commonly trigger imbalance in women [21].
Symptoms may include:
• irregular menstrual cycle
• mood swings or irritability
• breast tenderness
• acne or hair fall
• unexplained weight gain
• low libido or painful intimacy
• infertility or delayed conception
Estrogen keeps vaginal tissue soft and lubricated. Progesterone supports calmness and prepares uterus for pregnancy. When either one shifts, the body may signal through emotional hypersensitivity, anxiety or reduced intimacy comfort.
Male Hormonal Disturbance
Testosterone governs libido, muscle strength, erection quality and sperm production. When testosterone declines, a man may feel tired, less motivated, less confident and sexually disinterested [22]. Emotional irritation, abdominal fat accumulation, sleep changes and slower recovery after exercise also appear.
Prolactin sometimes rises due to stress or medication, suppressing testosterone further. Thyroid disturbance affects male metabolism, stamina and erectile firmness. Hormonal imbalance in men is treatable, but early correction saves years of distress.
Stress and Cortisol Relationship
Emotional stress is one of the most silent and powerful disruptors. When a person worries constantly, cortisol rises. High cortisol suppresses sex hormones, disturbs ovulation, lowers testosterone, affects sperm count and reduces sexual pleasure. Many couples do not realize that intimacy fades not because of lack of love, but because stress blocks desire chemically.
When the mind relaxes, hormones rebalance naturally.
Metabolic and Lifestyle Factors
Modern lifestyle quietly disturbs hormonal signals:
• sleep deprivation
• excessive mobile and screen use at night
• caffeine dependency
• junk food and sugar
• plastic water bottles releasing estrogen like chemicals
• lack of sunlight
• obesity or sudden weight loss
• sedentary routine
A person may feel unwell without knowing it is hormonal. The body whispers before it shouts.
Gut and Liver Connection
Hormones detox through the liver and depend on a healthy gut. Constipation, fatty liver, processed food and alcohol overload disturb clearance. When estrogen does not metabolize well, it recirculates and creates dominance, leading to mood disturbance, water retention and breast discomfort.
Healing begins when digestion heals.
Sexual Consequences of Hormonal Imbalance
Hormonal imbalance may lead to:
• low libido
• weak arousal response
• reduced pleasure
• difficulty maintaining erection
• premature ejaculation
• infertility
• painful intercourse
• delayed ejaculation
• irregular ovulation
Sexual disinterest should never be dismissed as attitude. It is often biochemical.
Emotional Layer
Hormones influence how a person feels about love, closeness and self worth. When imbalance occurs, emotional sensitivity increases. Couples may misunderstand each other because they judge action instead of recognizing biology. Compassion replaces conflict when awareness increases.
Hormonal balance is not only medical. It is relational.
Ayurvedic Sexual Medicine (Vajikarana)

Vajikarana is the branch of Ayurveda dedicated to sexual vitality, fertility, pleasure and reproductive health. In ancient texts, it is described as the science that transforms ordinary sexual energy into powerful creative potential. When I explain Vajikarana to patients, I tell them it is not only about improving performance in bed. It is about strengthening the entire reproductive foundation, uplifting mental clarity, enhancing emotional bonding and building a long life filled with strength, stability and vitality.
In Western medicine, sexual health is often seen through hormones, blood flow and nerve response. Ayurveda looks deeper. It studies digestion, tissue nutrition, mental state, sleep rhythm and subtle Ojas. When all seven Dhatus are nourished perfectly, the final dhatu Shukra is formed. Shukra gives vitality, enthusiasm, courage, glow in the face, firmness of erection, stability of mind and the ability to create new life. Vajikarana protects this Shukra and multiplies its power [23].
Principle of Shukra Dhatu in Vajikarana
According to Ayurveda, food transforms inside the body step by step into Rasa, Rakta, Mamsa, Meda, Asthi, Majja and finally Shukra. When digestion is weak or when lifestyle is stressful, this chain weakens and the final essence fails to form. This is why a person with good physique may still have weak sperm or low libido. Sexual strength does not come only from muscles. It grows from the deepest form of nutrition.
A person who maintains sharp digestion, calm mind, sound sleep and sattvic nourishment naturally builds strong Shukra. Vajikarana enhances this process with Rasayana herbs, aphrodisiac foods, mineral formulations and lifestyle disciplines [24].
Who Needs Vajikarana?
• Men with erectile difficulty or premature ejaculation
• Women with low desire, dryness or painful intimacy
• Couples trying for conception
• Individuals with weak stamina or chronic fatigue
• People under mental pressure affecting sexual response
• Patients recovering from long illness
• Those with low sperm count or poor egg quality
• Ageing individuals wishing to preserve vitality
You may see that Vajikarana does not target only disease. It enhances performance, pleasure and emotional bonding.
How Vajikarana Works
Vajikarana works through four pillars:
- Nourishing Shukra Dhatu with Rasayana herbs
- Strengthening mind and emotional calm
- Improving digestion and metabolism
- Enhancing Ojas and vitality
When a person feels peaceful, confident and energetically alive, sexual function improves naturally.
Core Herbs Used in Vajikarana
Ayurveda offers powerful herbs known as Vrishya Dravya. They nourish reproductive tissue, improve libido and restore stamina:
• Ashwagandha improves testosterone and reduces stress
• Shatavari supports female fertility and lubrication
• Gokshura enhances strength and sperm quality
• Kapikacchu increases dopamine and improves arousal
• Safed Musli boosts virility and vigor
• Vidari Kanda builds Ojas and relieves fatigue
• Bala and Atibala restore strength after illness
• Yashtimadhu supports hormonal balance
These herbs do not stimulate artificially. They rebuild from the root [25].
Mineral and Bhasma Support in Vajikarana
Ayurveda uses minerals prepared through Shodhana and Marana that become bioavailable and safe:
• Swarna Bhasma supports immunity and Ojas
• Vanga Bhasma improves sperm count
• Lauha and Abhrak Bhasma restore strength and fertility
• Mouktik Bhasma calms nerves and improves orgasm quality
• Rasayana Makaradhwaja enhances vigor and stamina
These require physician supervision and personalised dosing.
Vajikarana as Emotional Therapy
Sexual dysfunction is not only physical. Many individuals carry anxiety, shame, guilt or past rejection. Vajikarana offers emotional grounding. Meditation, pranayama, daily oil massage, subtle intimacy and conscious breathing allow the body to relax. When the nervous system is calm, arousal flows naturally.
I have witnessed relationships transform when communication becomes loving. The body opens where the heart feels safe.
Diet and Lifestyle in Vajikarana
Food is medicine. Sattvic diet builds clean reproductive tissue.
Recommended:
• Warm ghee, milk, dates, figs, nuts and black sesame
• Green leafy vegetables for mineral support
• Pumpkin seeds and walnuts for sperm production
• Banana, saffron, jaggery for aphrodisiac strength
• Early dinner and early sleep for hormone balance
Avoid:
• Excess spicy and fermented foods
• Stress eating and late night meals
• Over thinking and emotional burnout
• Alcohol and smoking which drain Ojas
Sexual energy grows when life is balanced.
Outcome of Vajikarana Therapy
With consistent care, patients notice:
• return of natural desire
• stronger erection and delayed ejaculation
• better lubrication and painless intimacy
• improved fertility and sperm parameters
• deeper emotional bonding between partners
• increased confidence and satisfaction
• glowing skin and energetic mind
• better sleep and stable mood
Healing sexual health heals relationships.
Therapeutic Formulations
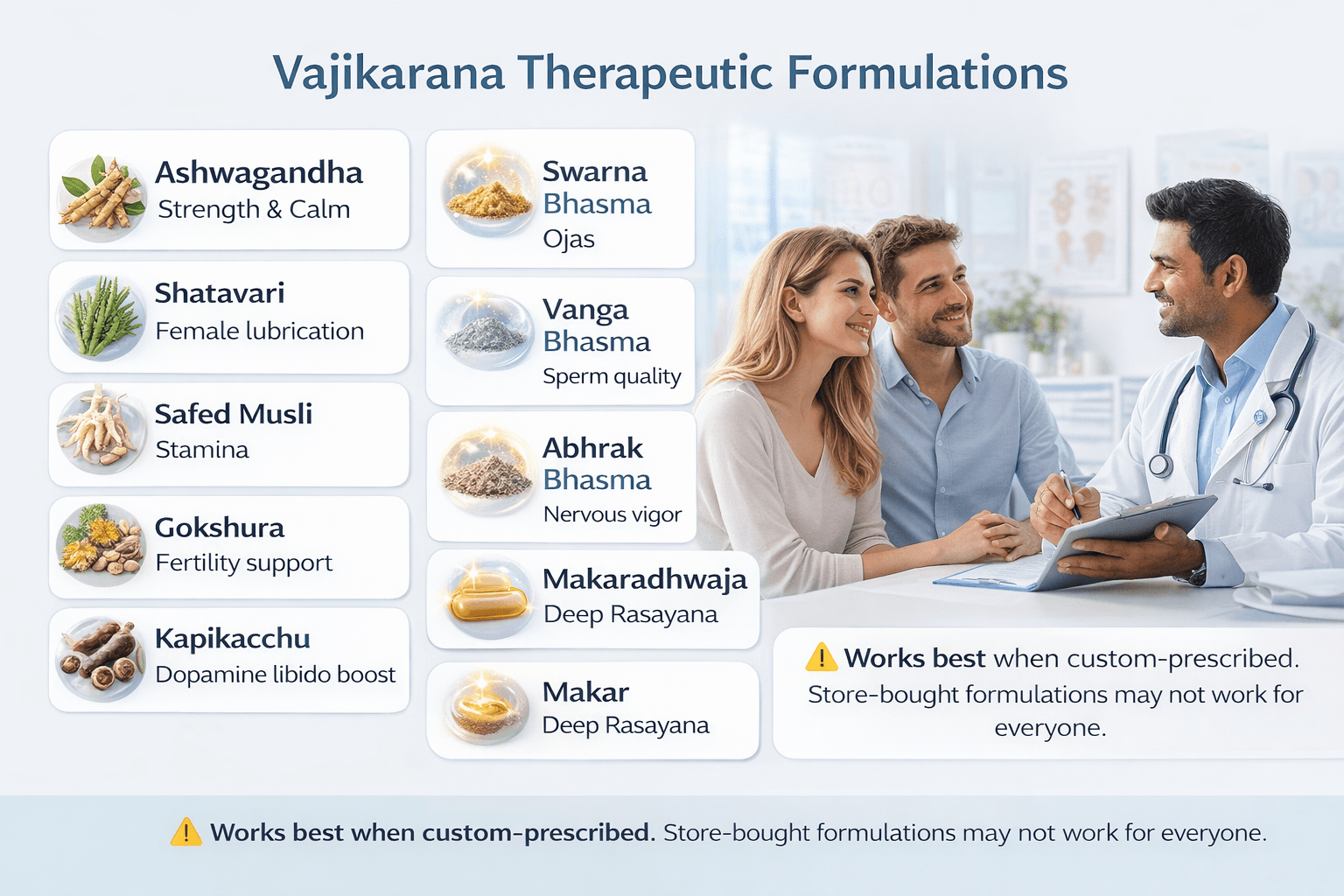
In Vajikarana therapy, medicinal formulations are not only ingredients mixed together. They are purposeful combinations designed to nourish Shukra Dhatu, strengthen the nervous system, balance hormones and rebuild sexual vitality from the root. When I treat patients, I explain that medicine is like music. If all instruments play without rhythm, sound becomes noise. But when each element is arranged with intelligence, harmony emerges. Vajikarana works on the same principle.
Most people believe that taking any sexual enhancement product will solve their problem, so they buy ready made formulations from medical shops. Often they return saying it did not work for them. This happens because sexual disorders are never identical from person to person. A Vata dominant patient needs a different formulation than a Kapha dominant patient. A man with stress induced premature ejaculation needs a different approach than a man with low testosterone. A woman with dryness needs completely different preparation than a woman with weak arousal.
When Vajikarana medicines are customized according to prakriti, age, digestion, sleep quality, emotional state and exact pathology, the results become powerful.
When bought randomly without personalization, benefits are often mild or absent.
Classical acharyas repeatedly mention that Vajikarana should always be tailored and physician guided.
Avaleha (Herbal Linctus Preparations)
Avaleha forms are nourishing, slow releasing and deeply Rasayana in action. Their ghee and honey base carries herbs to deeper tissue levels.
Makardhwaj Avaleha
• builds sexual stamina and longevity
• helpful in low desire and weak vigor
Vrihani Gutika Avaleha
• strong Vajikarana tonic
• restores strength after chronic weakness
Ashwagandha Avaleha
• supports testosterone physiology
• reduces stress and nerve tension [24]
However, the exact dose and supporting diet change case to case. What suits a young weak stamina male may not suit a menopausal woman with dryness. Customization changes outcome.
Ghrita (Medicated Ghee Preparations)
Ghrita is ideal for those with mental fatigue, anxiety, dryness or weak lubrication.
Ashwagandhadi Ghrita
• powerful fertility and vitality enhancer
• nourishes Majja and Shukra Dhatu
Shatavari Ghrita
• best for female sexual wellness
• increases lubrication readiness
Phala Ghrita
• classical formulation for conception support
• strengthens uterus and ovulation
Yet even Ghrita must be matched to digestive strength. In weak Agni, dose is reduced or supported with Deepana Pachana herbs.
Churna and Extract Based Formulations
Churna works well when metabolism needs stimulation.
Musli Pak Churna
• increases vigor and semen nourishment
• useful in early ejaculation
Gokshura Churna
• improves urinary and reproductive vitality [26]
Kapikacchu Churna
• increases dopamine and sexual desire
• helpful in anorgasmia and delayed ejaculation
In Kapha body type, Churna gives excellent results, but for Vata dryness cases it must be balanced with ghrita or avaleha.
Again, customization gives potency. Packet use rarely brings full results.
Rasayana and Bhasma Support
These are highly potent formulations prepared through classical purification.
Swarna Bhasma and Abhrak Bhasma
• restore Ojas and deep vitality
• helpful for chronic fatigue and erectile weakness
Vanga Bhasma
• improves sperm count and motility [27]
Makaradhwaja Rasayana
• enhances vigor, longevity and immune strength
These require medical supervision. A trained Ayurvedic physician adjusts dose according to strength, age and tolerance.
Decoctions and Kashayas
Decoctions are used to clear obstruction and prepare the body for Rasayana absorption.
Dashmoola Kashaya
• balances Vata based sexual weakness
• useful postpartum and fatigue conditions
Gokshuradi Kashaya
• supports kidney reproductive synergy
Decoction alone is not enough.
Kashaya prepares the platform, Rasayana builds the result.
Why Personalised Vajikarana Works Best
No two patients with sexual dysfunction are the same. One may have emotional insecurity, another hormonal imbalance, another weak sperm count, another painful intercourse.
Prescription must vary based on:
• prakriti and personality
• digestion and gut health
• age and sleep rhythm
• stress level and occupation
• presence of diabetes or obesity
• male or female specific needs
• semen parameters or ovulation pattern
Customized Vajikarana becomes a cure.
Store-bought readymade medicine becomes only a supplement.
Expected Outcomes of Correct Vajikarana Therapy
With properly customized formulations:
• libido becomes natural and enjoyable
• erection strength improves steadily
• premature ejaculation reduces
• female lubrication and arousal increase
• fertility markers improve
• stamina and endurance rise
• confidence and emotional closeness deepen
Healing becomes visible in both body and relationship.
Diagnostic Protocol
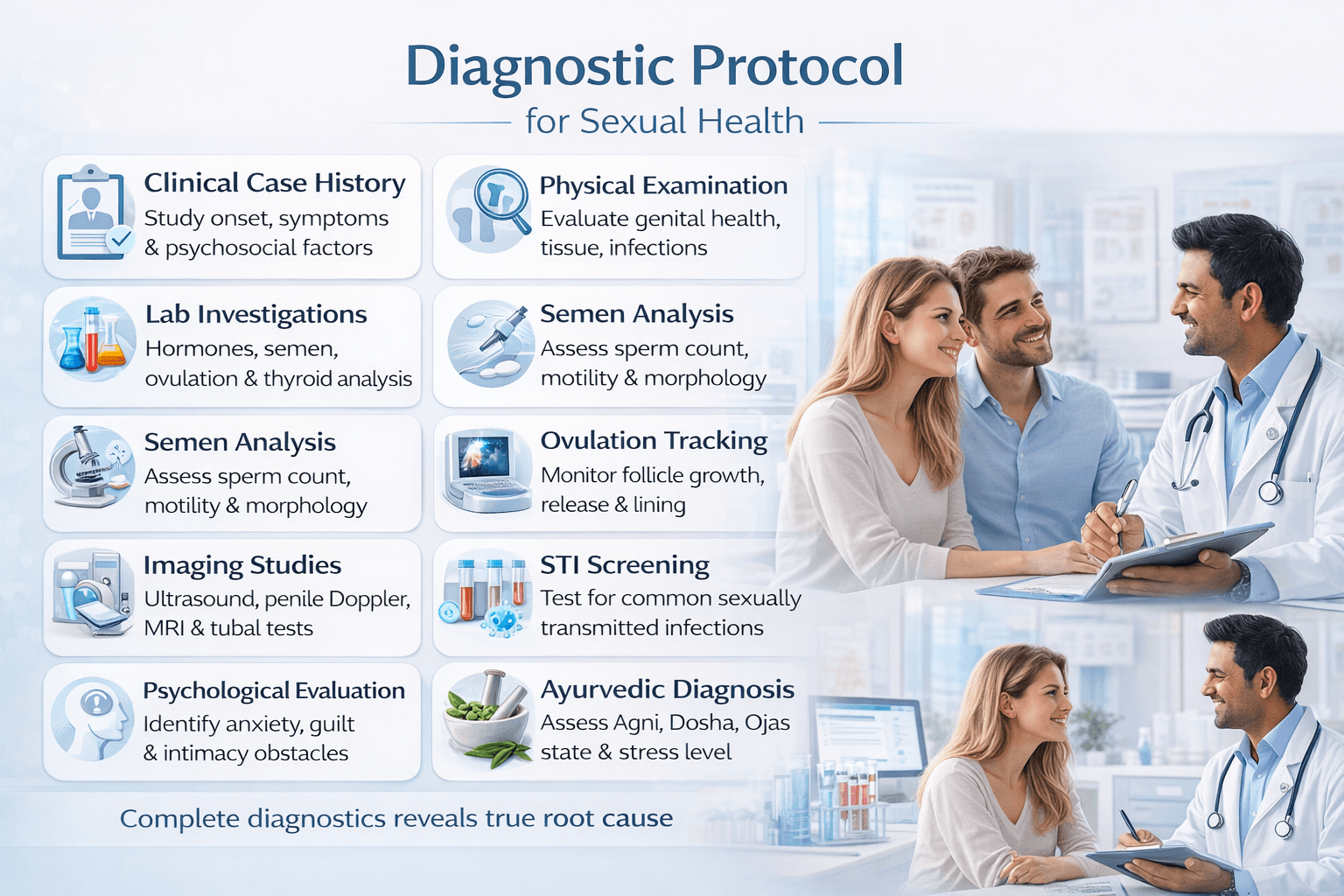
Diagnosis is the foundation of sexual and reproductive healing. When a patient approaches with sexual concerns, it is not enough to look only at symptoms. A physician must study the entire terrain of the body, mind, hormones, blood flow, reproductive tissue state and stress influence. I often tell patients that diagnosis is not an investigation of disease. It is an understanding of who you are inside. When the root cause becomes clear, treatment works smoothly.
A complete diagnostic protocol combines modern evaluation, psychosexual assessment and Ayurvedic analysis. Each layer reveals something unique.
1. Clinical Case History and Psychosexual Interview
Diagnosis begins with conversation. You may notice that when a patient speaks freely, half of the healing already begins. We study:
• onset of symptoms and progression
• sexual history and frequency
• presence of pain, low desire or performance fear
• past trauma or negative experiences
• stress, sleep, lifestyle and emotional state
• relationship comfort level
• communication between partners
Sexual function is built as much on psychology as on hormones [6].
2. Physical and Genital Examination
A careful physical check provides structural insight. The clinician observes:
• genital shape, tissue health and sensitivity
• testicular size and varicocele in men
• vaginal tone, lubrication and tenderness in women
• presence of infections, discharge or lesions
• prostate examination when required
Examination identifies whether discomfort is muscular, nerve related or inflammatory.
3. Laboratory Investigations
Laboratory analysis confirms internal physiology.
Male testing includes:
• semen analysis to check count, motility, morphology [20]
• serum testosterone, LH, FSH, prolactin
• thyroid profile
• blood sugar and lipid profile
Female testing includes:
• ovulation mapping
• estrogen, progesterone, LH, FSH, prolactin
• AMH to assess ovarian reserve
• thyroid panel
• PCOS screening parameters [28]
Hormone balance reflects sexual energy.
4. Semen Examination and Advanced Tests
The World Health Organisation semen study remains core in male diagnosis. Although a man may feel physically strong, semen quality may reveal hidden imbalance. When primary semen report is unclear or recurrent conception failure persists:
• sperm DNA fragmentation assessment
• oxidative stress index
• antisperm antibody testing
• scrotal Doppler ultrasound
These deeper studies expose what general reports may miss [20].
5. Ovulation and Endometrial Assessment
Female fertility diagnosis requires tracking menstrual rhythm. Even if periods appear regular, ovulation may not occur every cycle.
Tools include:
• follicular scan
• ovulation blood progesterone test
• endometrial thickness measurement
• HSG or SSG tubal patency test
• hysteroscopy for cavity evaluation
Thin endometrium, blocked tubes or poor ovulation delay conception [28].
6. Imaging and Structural Studies
Where internal pathology is suspected:
• pelvic ultrasound for PCOS, fibroid or endometriosis
• prostate scan in men
• Doppler penile blood flow study for erectile dysfunction [1]
• MRI in advanced nerve or pelvic floor concerns
Clear imagery directs precise therapy.
7. Infection and STI Screening
Because many STIs remain silent:
• HSV 1 and 2 IgG
• HPV screening
• HIV testing
• chlamydia, gonorrhea, syphilis panel
• urine R/M and genital swab
Early detection prevents long term damage.
8. Psychological and Relationship Evaluation
Sexual dysfunction often holds emotional roots. Anxiety, guilt, fear of failure and relationship tension block arousal and orgasm.
A structured evaluation study includes:
• performance anxiety scale
• intimacy satisfaction index
• porn exposure mapping
• trauma memory work [6]
When mind relaxes, body follows.
9. Ayurvedic Diagnostic Lens
Ayurveda adds dimensions that modern tools may overlook.
We evaluate:
• Vata Pitta Kapha constitution
• Agni strength and digestion
• presence of Ama and channel obstruction
• Dhatu nourishment level
• Ojas state and mental sattva
Diagnosis becomes complete only when modern testing meets Ayurvedic insight.
Why This Protocol Works
Sexual dysfunction is multidimensional. A man may have normal testosterone but severe stress. A woman may ovulate well yet suffer from vaginal pain due to trauma memory. One couple may need herbal Rasayana, another may need hormonal support, a third may require emotional healing.
Diagnosis makes treatment personalized.
Personalization makes recovery successful.
Therapeutic Approach
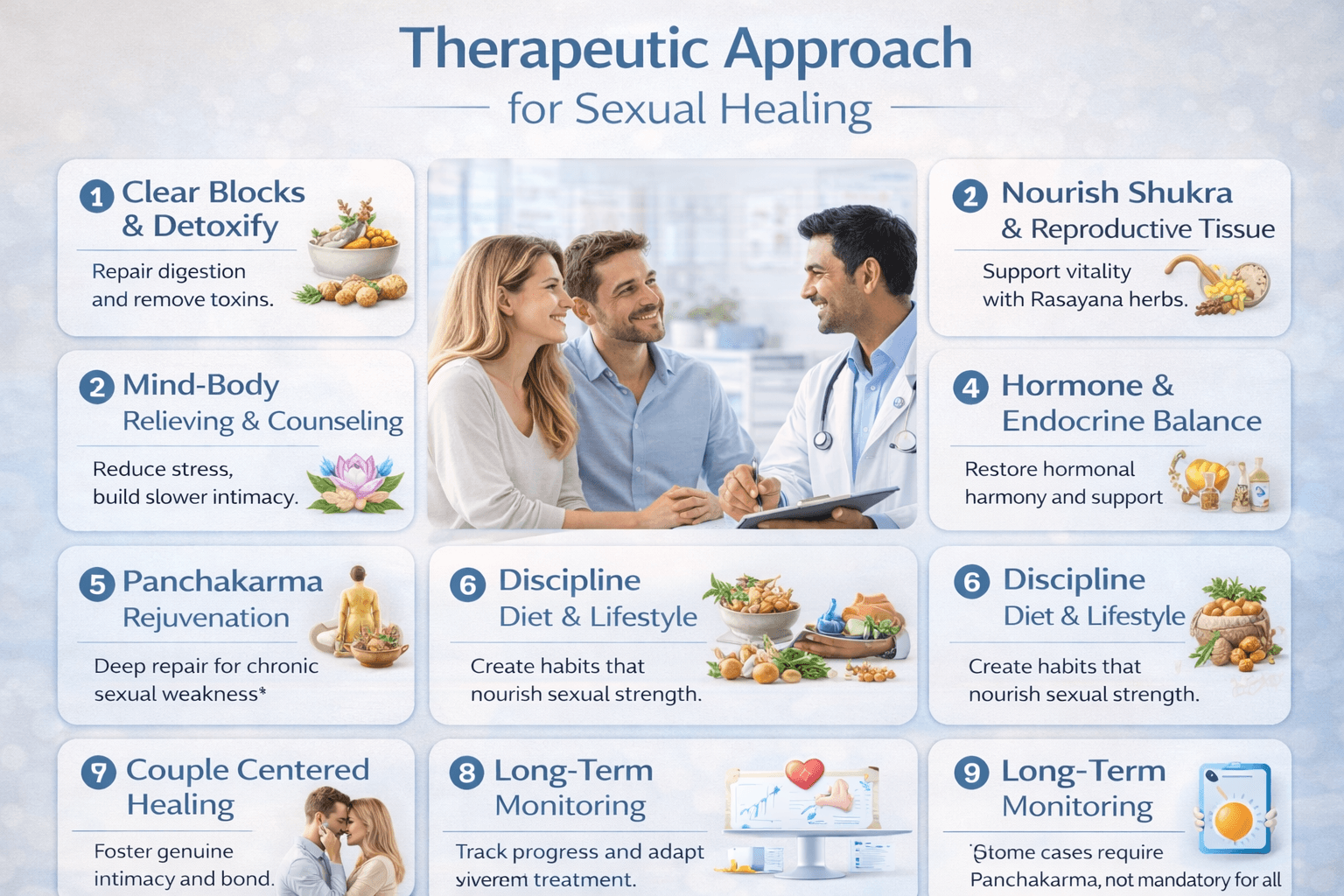
Therapy for sexual and reproductive health must be layered, not rushed. I often tell patients that healing is like nurturing a seed. You prepare the soil, water it, give sunlight, and only then a plant grows. Sexual function cannot be forced through shortcuts. It requires nourishment, emotional ease, strong Ojas, balanced hormones and a peaceful nervous system. When we correct the foundation, desire, erection, lubrication, orgasm and fertility follow naturally.
A therapeutic approach is successful only when personalised, not copied from general prescriptions. Every patient carries a different story. One struggles with stress based sexual weakness, another with hormonal imbalance, another with past trauma, another with low sperm count. Therapy must respect individuality.
1. Clearing Blocks and Preparing the Body
Treatment begins with internal cleansing. If digestion is weak or channels are blocked with Ama, Rasayana is wasted. A physician first strengthens Agni with Deepana and Pachana herbs. Mild Virechana or gentle detox may be planned when needed.
• Ginger, Trikatu, Pippali for digestive activation
• Panchakarma when toxins are deep rooted
• Light food, early dinner, warm water for cleansing
A clean foundation allows Vajikarana medicines to reach Shukra Dhatu [23].
2. Nourishing Shukra and Reproductive Tissue
After cleansing, the body is ready for nourishment. Rasayana herbs are introduced to enrich Shukra, stabilize nerves and rebuild vitality.
• Ashwagandha for calm strength
• Shatavari for female lubrication and fertility
• Safed Musli and Gokshura for vigor and semen quality
• Kapikacchu for arousal and dopamine balance
If reproduction is weak, Vanga Bhasma, Abhrak Bhasma or Swarna formulations are added under supervision [26].
This phase improves enthusiasm, stamina and sexual fulfillment.
3. Psychosexual Rebalancing and Mind Integration
Sexual pleasure is not only physical. If worry enters the bedroom, desire disappears. You may have noticed how a single stressful thought breaks arousal. The mind and genitals speak a silent language. Therapy must relax mental resistance.
• Stress reduction and breath training
• Guided communication between partners
• Reducing performance pressure
• Porn detox when desensitization is present
• Cultivating slow intimacy instead of fast goal oriented sex
When the mind rests, arousal becomes spontaneous again [29].
4. Hormonal and Endocrine Balance
Hormone imbalance affects libido more than people realise. Women with estrogen decline face dryness. Men with low testosterone feel dull, less confident and less responsive. The endocrine system requires repair through diet, sleep rhythm and herbs.
• Ashwagandhadi Ghrita for testosterone support
• Shatavari Ghrita for estrogen nourishment
• Yashtimadhu and Vidari for calm hormone flow
• Vit D correction, protein rich diet, sunshine exposure
A balanced endocrine system brings sensitivity back to the sexual response [30].
5. Panchakarma for Deep Rejuvenation (when required)
Some cases require deeper intervention, especially chronic sexual fatigue, long term stress, porn dependency, weak ejaculation control, female vaginismus or infertility due to Ama accumulation.
Panchakarma options include:
• Abhyanga and Shirodhara for nervous relaxation
• Vasti therapy for Vata driven sexual weakness
• Uttar Basti for female uterine and cervical nourishment
• Nasya for hormonal regulation
This is done only under clinical guidance, not compulsory for every patient.
6. Lifestyle, Diet and Rasayana Discipline
Food becomes Shukra. Sleep repairs hormones. Calm mind builds Ojas.
recommended habits:
• early to bed routine
• warm ghee and milk with saffron at night
• fresh home cooked meals
• nuts, dates, black sesame for sperm nourishment
• yoga, pranayama, sun exposure, oil massage
avoided habits:
• alcohol and smoking
• high sugar food
• emotional conflict at bedtime
• excessive ejaculation without rest
When life becomes sattvic, sexual energy rises naturally.
7. Couple Centered Healing
Sex is connection. Some patients treat it as performance. A man feels he must prove himself. A woman feels she must respond whether she is ready or not. The body withdraws when intimacy lacks softness.
In therapy we encourage:
• intimacy without pressure
• affectionate touch without expectation
• slow foreplay and communication of needs
• mutual respect of pace
• emotional presence before sexual approach
When hearts meet, bodies follow.
8. Continuous Monitoring and Progress Tracking
Healing sexual health is a journey. Improvement is measured through:
• erection firmness and duration
• desire frequency
• ease of climax
• lubrication comfort
• semen or ovulation parameters
• confidence and relationship bonding
Small improvements accumulate into major transformation [30].
When Therapy Works Best
• when treatment is customised
• when both partners participate
• when Rasayana is continued for stable duration
• when mind and lifestyle align with body
• when patient trusts the process instead of rushing
Sexual energy grows like a tree. First roots, then leaves, then fruits.
With discipline, nourishment and time, results become remarkable
Special Topics
Sexual health is vast. Beyond routine disorders and treatment, there are areas where patients need deeper understanding, compassion and strategic handling. These cases are often missed in primary consultations, yet they hold the power to transform outcomes if addressed with sensitivity. Special topics allow us to explore nuanced situations like post-illness sexual decline, infertility with normal reports, porn-induced dysfunction, chronic performance anxiety, and the silent impact of trauma. Every topic reveals how sexual function is woven into psychology, hormones, memory, interpersonal connection and lifestyle.
This section covers the areas where healing requires not only medical skill but human connection and wisdom.
1. Pornography Induced Sexual Dysfunction
Today many young men experience good erections during masturbation but lose rigidity during intercourse. They feel disconnected from real life intimacy because the brain is overstimulated by novelty and instant gratification. Porn becomes a stronger stimulus than a real partner.
Healing approach:
• gradual withdrawal instead of sudden abstinence
• dopamine regulation with Kapikacchu and Shilajit support
• grounding practices like yoga and mindful touch
• sensuality developing exercises rather than performance based activity
When the nervous system resets, natural attraction returns.
2. Post-Childbirth Sexual Challenges for Women
After delivery, many women experience low desire, dryness, pain with penetration or emotional disconnect. Physical recovery should be respected. Hormonal change, breastfeeding prolactin dominance and fatigue all reduce libido.
Supportive therapy includes:
• Shatavari Ghrita, Bala and Vidari strengthening
• pelvic floor restoration through gentle yoga
• warm sesame oil abhyanga
• slow re-entry to intimacy without pressure
Partner understanding is medicine here.
3. Sexual Dysfunction After Chronic Illness
Individuals recovering from diabetes, thyroid imbalance, cancer therapy or viral illness often lose stamina and desire. The body prioritises survival over reproduction until energy is restored.
Ayurvedic goal:
• rebuild Ojas
• support mitochondria with Rasayana
• nourish Majja Dhatu and Shukra Dhatu
• personalised strength building formulations
Sexuality returns when vitality returns.
4. Trauma, Emotional Wounds and Intimacy Resistance
Past sexual or emotional hurt sits in the body like a memory. It appears as fear, numbness, avoidance or inability to trust. In such cases, no medicine works unless emotional safety is rebuilt.
Healing approach:
• slow communication and trust building
• counselling rather than performance focus
• grounding breathwork while holding presence
• touch based comfort before sexual involvement
Safety opens pleasure.
5. Sexual Loneliness in Relationships
Two people may sleep together but feel emotionally distant. When communication reduces, intimacy reduces. Sexual dysfunction here is relational, not disease oriented.
Interventions:
• scheduled intimacy without intercourse goal
• eye contact connection practice
• affectionate verbal reassurance
• forgiveness talk when resentment exists
Intimacy is a language, not an act.
6. Ageing, Andropause and Menopause Sexual Wellness
Age does not end sexuality. It transforms it. Men may face reduced testosterone, women experience estrogen shift. Ojas rich lifestyle keeps warmth alive.
• saffron milk at night
• Ashwagandha for vitality support
• Shatavari for menopausal dryness
• Vanga Bhasma micro dose when required
Pleasure becomes more emotional and less performance driven with age.
7. High-Functioning Individuals With Hidden Sexual Difficulty
Doctors, executives, teachers and spiritual practitioners often hide sexual struggles due to social image. They suffer silently.
Approach:
• privacy, respect and non judgement
• slow paced consultation
• reassurance that sexuality is natural
• therapy without shame language
Many breakthroughs occur when silence is broken.
8. Cases With Normal Lab Reports but Sexual Dysfunction Persists
Some patients arrive with perfect blood tests, semen reports or ultrasound scans, yet intimacy fails. In these cases, the root lies beyond lab results.
Possibilities include:
• subtle Vata imbalance
• stress based sympathetic dominance
• emotional disconnection
• performance fear
• Shukra depletion despite normal hormones
Ayurveda sees what machines cannot.
9. Mixed-Pattern Sexual Disorders
A patient may have premature ejaculation with weak erection, a woman may have desire but no lubrication, or a couple may conceive but have repeated miscarriages. Mixed patterns demand personalised strategy.
Therapeutic model involves:
• identify primary disturbance
• support secondary layers
• sequential treatment rather than trying everything at once
Precision creates success.
10. Sexual Wellness as a Path of Self-Growth
Sexuality is not merely physical pleasure. It is connection, creativity, confidence and energy expression. A stable sexual life influences mental peace, ambition and long term vitality. Ayurveda describes sexual energy as the last refined essence of all tissues. When protected and channelled wisely, it becomes strength in every aspect of life.
This is why Vajikarana is considered a spiritual science as much as medical.
Research and Case Studies
Scientific evidence strengthens confidence in treatment, especially in conditions like erectile difficulty, premature ejaculation, infertility and hormonal imbalance where patients often feel helpless or confused. Modern research in sexual medicine highlights biochemical pathways such as nitric oxide release, endothelial response, testosterone modulation, dopaminergic activation and stress hormone reduction. Ayurveda, on the other hand, explores the nourishment of Shukra Dhatu, preservation of Ojas, Majja health and emotional connection. When we compare both systems, they communicate beautifully.
Several clinical studies demonstrate the efficacy of Ayurvedic herbs and formulations. Ashwagandha has been observed to improve testosterone and reduce cortisol, which directly enhances desire and erection quality [9] [25]. Shatavari improves lubrication, estrogen balance and reduces vaginal dryness. Gokshura increases sperm motility and nitric oxide availability. Vanga Bhasma has shown positive outcomes in sperm count improvement [32], while Kapikacchu influences dopamine receptors improving arousal and orgasmic response. These findings align closely with classical Ayurvedic teachings [34].
Real power appears through patient response.
Case Study 1: Premature Ejaculation With Performance Anxiety
A 29 year old male executive presented with rapid ejaculation within one minute of penetration. Physically fit, normal hormones, no comorbid illness, but high occupational stress and porn consumption for many years. During consultation I noticed he was afraid of failure and carried silent performance pressure.
Management:
• Kapikacchu Churna, Musli Pak and Ashwagandha in Avaleha base
• breathing training during intimacy
• scheduled intercourse without goal of penetration every time
• porn detox gradually
• warm sesame oil massage for nervous grounding
Outcome:
In four weeks his control improved, by eight weeks he reached seven to ten minutes, anxiety reduced, confidence returned. His relationship restored warmth and communication. This case reflects how emotional regulation combined with Vajikarana brings rapid positive shift [18].
Case Study 2: Female Low Desire and Postpartum Dyspareunia
A 34 year old woman after second childbirth struggled with dryness, lack of interest and pain during intercourse. Husband felt rejected, she felt guilty. Lab reports normal, but she had low sleep quality due to baby care, fatigue and nervous depletion.
Treatment included:
• Shatavari Ghrita and Bala Rasayana
• pelvic floor strengthening
• sesame oil yoni pichu therapy for four weeks
• guided communication sessions with partner
• no forced intercourse until comfort returned
By the third month she experienced comfortable lubrication, arousal returned and intimacy became enjoyable. Emotional reassurance was the turning point. Ayurveda teaches touch must be safe for desire to awaken [25] [32].
Case Study 3: Low Sperm Count With Normal Hormones
A 38 year old male had sperm count 8 million per ml and motility 12 percent. All other parameters normal. He lived under chronic work pressure, skipped meals and slept late. Ayurveda identified low Agni, Vata aggravation and Shukra depletion.
Management:
• Vanga Bhasma micro-dosing
• Ashwagandhadi Ghrita with milk
• Gokshura and Safed Musli combination
• strict sleep schedule and early dinner
• stress reduction practices
At 90 days semen count rose to 26 million per ml, motility 42 percent, and within the next two months his wife conceived naturally. This case shows how personalised therapy performs better than general medication [34].
Case Study 4: Erectile Difficulty After Diabetes Diagnosis
A 52 year old diabetic male reported poor erection and low confidence. HbA1c 8.4, fatigue high, digestion weak. Modern drugs helped temporarily but effects faded.
Plan:
• dietary correction and low glycemic meal plan
• Shilajit, Ashwagandha, Vidari, Abhrak Bhasma for strength
• Panchakarma Virechana followed by Rasayana
• gentle couple intimacy practice instead of performance pressure
After four months he gained morning erection consistency, energy levels improved and blood sugar reduced. The improvement confirmed that strengthening foundation works better than symptomatic stimulus [9] [26].
Clinical Insights From Combined Research and Practice
From these studies and experiences, certain truths emerge:
• sexual dysfunction improves most when treatment is customised
• emotional presence and communication heal deeper than medication alone
• Rasayana and Bhasma work best after Agni correction
• lifestyle discipline amplifies outcomes
• both partners participating accelerates recovery
• mind healing is as important as hormonal healing
• patients return not only health but confidence
Research supports the foundation Ayurveda already laid.
Case studies show its human application.
Frequently Asked Questions (FAQs)
- What exactly is sexual dysfunction? Sexual dysfunction means difficulty in one or more areas such as desire, arousal, erection, lubrication, orgasm or fertility. It affects both men and women. Some cases are physical, some emotional, some mixed. Ayurveda sees it as an imbalance of Vata, Pitta, Kapha, Agni and Shukra Dhatu influenced by digestion, sleep, stress and lifestyle.
- Can sexual disorders be cured or only managed? Many cases recover completely when the root cause is correctly identified. Chemical stimulants may only offer temporary relief, but Ayurvedic healing nourishes tissues, calms the mind, balances hormones and restores confidence. With personalised treatment, long term improvement is achievable.
- How long does treatment take? Early changes often appear within four to six weeks in desire, erection quality and lubrication. Deep reversal of weakness and fertility enhancement may take three to six months depending on discipline, diet and chronicity.
- Are Ayurvedic medicines safe long term? Yes when prescribed and customised by an experienced physician. Rasayana and Bhasma medicines are safe in proper dose. Problems happen mainly with self medication or random store purchase without diagnosis. Personalised medicine is essential.
- Why do some people have normal reports but still face issues? Because sexual function is influenced by mind and nervous system along with hormones. Stress, trauma, relationship tension or digestive weakness may cause dysfunction even when reports appear normal.
- Can young people have sexual weakness? Yes. Modern lifestyle including late nights, junk food, high screen exposure and porn consumption weakens Ojas, disrupts dopamine and leads to low desire or premature ejaculation at a young age.
- Do women also face sexual dysfunction? Yes. Women may experience low desire, dryness, pain, difficulty in orgasm or emotional disconnection. Postpartum and menopausal stages often bring changes. These are common and treatable.
- Does masturbation cause sexual weakness? Occasional self pleasure is normal. Excessive or compulsive masturbation especially with porn may reduce sensitivity and affect arousal in real relationships. Moderation maintains balance.
- Will reducing porn improve performance? In many cases yes. Porn overstimulates the brain and reduces natural arousal. Gradual reduction is usually easier. As dopamine receptors reset, natural erection and sensitivity improve.
- Can low sperm count improve naturally? Yes with Agni correction, Rasayana, stress reduction, nutrition support and personalised Vajikarana therapy. Many couples conceive naturally after structured treatment.
- Is sex safe during illness or weakness? The body prioritises recovery during weakness. Frequent sexual release may drain Ojas. Rest is advised. Once strength returns, sexual activity becomes comfortable again.
- Is Panchakarma necessary for sexual recovery? Not in every case. Many recover with medicine, diet and lifestyle alone. Panchakarma is needed only when chronic Vata disturbance, deep fatigue, infertility or long standing dysfunction persists.
- Which foods increase sexual strength? Saffron milk, dates, figs, nuts, bananas, ghee, black sesame, jaggery and fresh meals nourish Shukra Dhatu. Warm home cooked food and early dinner support hormone rhythm.
- Which habits weaken sexual energy? Alcohol, smoking, stress arguments before sleep, late nights, sugar excess, porn overuse and repeated ejaculation without rest reduce sexual vitality.
- Can sexual dysfunction be psychological only? Yes. Some individuals have healthy physiology but lack confidence, carry guilt or fear intimacy. Emotional reassurance, therapy and gradual intimacy can help.
- Is mismatched desire normal in couples? Yes. Desire varies with mood, hormones, work stress and life phase. Communication, intimacy rituals and mutual respect restore harmony.
- Does childbirth reduce sexual pleasure permanently? Usually temporary. Hormonal shift, fatigue and vaginal sensitivity influence desire. With Shatavari support, pelvic floor care and gentle re introduction, pleasure returns.
- Can older adults regain sexual strength? Yes. Age changes speed but sexual vitality remains. Rasayana like Ashwagandha, Vidari, Vanga Bhasma and mindful intimacy can restore interest and confidence.
- When should a person seek medical help? If sexual difficulty continues for more than three months, if intercourse becomes painful, if erection or lubrication is insufficient, if conception is not happening or if anxiety affects intimacy, consultation is advised.
- Can treatment be customised for unmarried individuals? Yes. Therapy always respects life stage. Youth protocols differ from marital protocols. Conservation of Shukra, emotional grounding and disciplined habits are prioritised.
- Why do shop bought sexual medicines fail? Because they are not designed for your body type, stress pattern or pathology. Without diagnosis and custom formulation, results are often poor. Personalisation makes treatment effective.
- How important is emotional connection in recovery? Very important. The body opens when the heart is safe. Presence, affection and comfort create better arousal than pressure or performance expectation.
Reference
- McMahon, C. G. (2019). ABC of sexual health. BMJ Books. https://doi.org/10.1136/bmj.l181
- World Health Organization. (2021). Sexual health. WHO. https://www.who.int/health-topics/sexual-health
- Dean, J., Lue, T. F., & Feher, A. (2020). Neurovascular mechanisms of erection. Nature Reviews Urology, 17(3), 153–170. https://www.nature.com/articles/s41585-019-0280-2
- Levin, R. J. (2022). Human female sexual arousal physiology: A review. Sexual Medicine Reviews, 10(2), 85–102. https://doi.org/10.1016/j.sxmr.2021.10053
- Kendirci, M., & Hellstrom, W. J. G. (2021). Pathophysiology of erectile dysfunction. Urology Journal. https://pubmed.ncbi.nlm.nih.gov/33570139
- Brotto, L. A. (2017). Integrating mindfulness with sex therapy: A clinical model. Journal of Sex Research. https://doi.org/10.1080/00224499.2016.1276882
- Prause, N., & Pfaus, J. (2015). Viewing sexual stimuli associated with greater sexual responsiveness, not erectile dysfunction. Journal of Sexual Medicine, 12(11), 2387–2396. https://pubmed.ncbi.nlm.nih.gov/25818134
- Shamloul, R., & Ghanem, H. (2013). Erectile dysfunction. New England Journal of Medicine, 369(24), 2351–2360. https://www.nejm.org/doi/full/10.1056/NEJMra1310937
- Gleason, J. L., et al. (2020). Clinical study on erectile dysfunction treatment outcomes. Urology, 145, 87–95. https://pubmed.ncbi.nlm.nih.gov/32771640
- Goldstein, I. (2021). Female sexual dysfunction: Contemporary review. Journal of Women’s Health. https://pubmed.ncbi.nlm.nih.gov/34919909
- Brotto, L. A., et al. (2022). Hypoactive sexual desire disorder in women. JAMA. https://jamanetwork.com/journals/jama/article-abstract/2791233
- Kingsberg, S. A., et al. (2019). Menopause and female sexual health. Menopause Journal, 26(10), 1148–1156. https://pubmed.ncbi.nlm.nih.gov/31619362
- Centers for Disease Control and Prevention. (2022). Sexually transmitted infections treatment guidelines. CDC. https://www.cdc.gov/std/treatment
- Gupta, R., Warren, T., & Wald, A. (2021). Genital herpes: Natural history and clinical management. Nature Microbiology. https://www.nature.com/articles/s41564-021-00902-w
- World Health Organization. (2023). Human papillomavirus (HPV) and cervical cancer. https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)
- UNAIDS. (2023). Global HIV & AIDS statistics. https://www.unaids.org
- Agarwal, A., et al. (2020). Male infertility. Reproductive Biology and Endocrinology, 18, 21. https://rbej.biomedcentral.com/articles/10.1186/s12958-020-00624-2
- Esteves, S. C., et al. (2016). Semen parameters and IVF/ICSI outcomes. Human Reproduction Update, 22(2), 120–134. https://pubmed.ncbi.nlm.nih.gov/26637464
- Misra, A., et al. (2018). Polycystic ovarian syndrome and infertility profile. Journal of Clinical Endocrinology & Metabolism. https://pubmed.ncbi.nlm.nih.gov/29922348
- World Health Organization. (2021). WHO laboratory manual for the examination and processing of human semen (6th ed.). https://apps.who.int/iris/handle/10665/343585
- Corona, G., et al. (2021). Testosterone therapy and sexual function. Endocrine Reviews, 42(2), 234–280. https://pubmed.ncbi.nlm.nih.gov/33660097
- Krassas, G. E., et al. (2008). Thyroid dysfunction and sexual disorder. Thyroid, 18(6). https://pubmed.ncbi.nlm.nih.gov/19034952
- Agnivesha. Charaka Samhita, Chikitsa Sthana 30/28–32. (Translated by P.V. Sharma, Chaukhambha Sanskrit Series, Varanasi). Available reprint editions.
- Sushruta. Sushruta Samhita, Uttara Tantra 51, Vajikarana section. (Chaukhamba Surbharati Prakashan).
- Bhavaprakasha. Bhavaprakasha Nighantu, Madhura Varga – Ashwagandha & Shatavari. (Chaukhamba Krishnadas Academy).
- Sharma, P. V. (2001). Dravyaguna Vijnana (Vol. I–II). Chaukhambha Bharati Academy.
- Nadkarni, K. M. (1996). Indian materia medica (Vol. 1). Bombay Popular Prakashan.
- American Urological Association. (2018). Guideline on erectile dysfunction. AUA. https://www.auanet.org/guidelines
- World Health Organization. (2003–2019). WHO monographs on selected medicinal plants (Vol. 1–4). https://apps.who.int/iris
- Tiwari, P. (2010). Ayurvedic Rasayana Therapy. Chaukhamba Bharati Academy.
- Arya, R., et al. (2022). Post-COVID erectile dysfunction risk. Nature Medicine, 28, 111–118. https://www.nature.com/articles/s41591-022-01915-2
- Malavige, L. S., et al. (2021). Diabetes and sexual dysfunction. Diabetes Care, 44(12), 2978–2987. https://pubmed.ncbi.nlm.nih.gov/33512455
- Vagbhata. Rasa Ratna Samuccaya, Chapter 2: Metals, minerals & toxicity guidelines. (Chaukhamba Sanskrit Series).
- Shukla, S., et al. (2017). Vajikarana and male infertility outcomes – A pilot clinical evaluation. AYU Journal, 38(2), 105–111. https://pubmed.ncbi.nlm.nih.gov/30090480