- What Is Neuropathy
- How the Nervous System Works and Where It Fails
- Pathophysiology of Neuropathy
- Types of Neuropathy
- Root Causes of Neuropathy
- Common Diseases That Occur With Neuropathy
- Rare and Often Missed Diseases Associated With Neuropathy
- Signs and Symptoms of Neuropathy
- Red Flags That Require Immediate Attention
- Diagnostic Approach
- Why Conventional Treatment Does Not Cure Neuropathy
- Ayurvedic Understanding of Neuropathy
- Best Ayurvedic Medicine (Avaleha) for Neuropathy
- Medicine Preparation Method for 30 Days
- Why Market Bought Avaleha Does Not Cure Neuropathy
- Diet and Lifestyle in Nerve Healing
- Clinical Observational Case Outcome
- Prognosis and Reversibility
- Long-Term Complications if Untreated
- Prevention and Risk Reduction
- Frequently Asked Questions (FAQs)
- Reference
What Is Neuropathy
Peripheral neuropathy cure begins with clearly understanding what neuropathy actually is. Neuropathy is a medical condition in which the peripheral nerves become damaged and lose their normal ability to transmit signals between the brain, spinal cord, and the rest of the body. These nerves control sensation, movement, and many automatic body functions. When they are injured, the entire communication system of the body becomes disturbed [1].
From a clinical perspective, neuropathy is not just pain in the nerves. It is a progressive nerve disorder that develops slowly over time due to metabolic stress, inflammation, poor circulation, nutritional deficiency, immune dysregulation, or toxic exposure. Doctors often describe it as peripheral nerve degeneration, meaning the nerve fibers themselves are structurally affected, not just irritated [1].
As a patient, you may first notice symptoms such as burning in the feet, tingling in the hands, numbness, weakness, or altered sensation. Many people initially ignore these signs because they appear mild or intermittent. However, what you feel on the surface often reflects deeper nerve damage developing silently inside the body. If the root cause is not addressed, the condition gradually progresses and becomes harder to reverse.
Clinically, neuropathy is considered a systemic disorder rather than a localized nerve problem. Studies show that neuropathy frequently occurs alongside other chronic conditions such as diabetes, metabolic syndrome, autoimmune disease, digestive disorders, and aging related metabolic decline [4]. This means the nerves are often victims of a broader internal imbalance rather than the primary cause of disease.
From the physician’s point of view, neuropathy represents a failure of nerve nourishment and repair. Nerves are highly sensitive tissues that depend on steady blood flow, oxygen, nutrients, and metabolic stability. When this support system weakens, nerve fibers begin to malfunction and deteriorate. This explains why many patients continue to worsen even when pain medications temporarily reduce discomfort.
For you as a patient, understanding this concept is essential. Peripheral neuropathy cure cannot be achieved by blocking pain signals alone. True recovery depends on identifying why nerve damage started, which systems are contributing to it, and how nerve repair can be supported at a deeper biological level. This is why modern research increasingly emphasizes early diagnosis and root cause oriented treatment rather than symptom suppression [1], [4].
In simple terms, neuropathy is the body’s signal that the nervous system is under sustained stress. When recognized early and treated comprehensively, nerve function can improve significantly. When ignored or only masked with medication, long term nerve damage and functional loss become much more likely.
How the Nervous System Works and Where It Fails

The nervous system as the body’s communication network
To understand how a peripheral neuropathy cure is even possible, you first need a clear picture of how the nervous system normally functions. The nervous system is the master communication network of the body. It allows the brain to receive information from every tissue and organ and to send instructions back in a continuous and highly coordinated manner. Every sensation you feel and every movement you make depends on this system working properly [2].
From a medical point of view, the nervous system is divided into two main parts. The central nervous system includes the brain and spinal cord. The peripheral nervous system extends from the spinal cord to the rest of the body. Peripheral nerves travel to the hands, feet, muscles, skin, internal organs, and glands. When people talk about neuropathy, they are almost always referring to damage in this peripheral network [2].
Structure of a healthy peripheral nerve
Each peripheral nerve is made up of thousands of microscopic nerve fibers. These fibers are designed to carry electrical signals efficiently and accurately. At the center of each fiber is the axon, which functions like an electrical wire. Surrounding the axon is a protective insulating layer called the myelin sheath. The myelin sheath ensures that nerve signals travel quickly and do not leak or become distorted [3].
When nerves are healthy, signals move smoothly from the brain to the muscles and from the skin back to the brain. As a patient, you experience this as normal sensation, coordinated movement, stable digestion, and proper automatic functions such as sweating and blood pressure control. You do not need to think about these processes because nerve communication happens silently in the background.
How nerve communication fails in neuropathy
Neuropathy begins when this finely balanced structure starts to deteriorate. Research shows that chronic metabolic stress, inflammation, oxidative damage, and impaired blood supply slowly injure nerve fibers [2]. In some individuals, the myelin sheath becomes damaged first. When this happens, nerve signals slow down or misfire. You may feel tingling, pins and needles, burning sensations, or electric shock like pain.
In other cases, the axon itself degenerates. Axonal damage is more serious because it directly disrupts the transmission of nerve signals. As a result, sensation becomes dull or disappears completely, muscles weaken, and coordination declines. From the clinician’s perspective, this stage represents structural nerve injury rather than temporary irritation [3].
Why symptoms often appear gradually
One of the most confusing aspects for patients is the slow onset of neuropathy. Nerve damage rarely happens overnight. It usually develops silently over months or years. Early nerve injury may not show up on routine blood tests or even nerve conduction studies. This is why many patients are told that their reports are normal even though symptoms are present [2].
As a patient, you may initially notice mild burning in the feet at night, occasional numbness, or altered sensation. These early signs reflect reduced efficiency of nerve communication. When these warning signals are ignored or masked with pain medications, the underlying damage continues to progress.
Advanced failure of nerve function
As neuropathy advances, nerve communication becomes increasingly unreliable. Muscles may not receive clear instructions from the brain, leading to weakness, imbalance, and muscle wasting. Loss of sensation increases the risk of injuries, falls, and unnoticed wounds. When autonomic nerves are involved, digestion, heart rate, blood pressure, bladder control, and sexual function can also become disturbed [3].
From the doctor’s point of view, this stage represents a breakdown of nerve maintenance and repair mechanisms. Nerves are highly dependent on proper blood flow, oxygen delivery, and metabolic stability. When these supports fail for long periods, spontaneous recovery becomes difficult.
Why this understanding matters for cure
For you as a patient, this explanation is crucial. Peripheral neuropathy cure is not about suppressing nerve signals or numbing pain. It is about restoring the biological conditions that allow nerves to repair their structure and regain function. Unless the reasons for nerve failure are addressed, symptom control alone cannot stop disease progression [2], [3].
When nerve nourishment improves and damaging influences are reduced, nerve fibers can recover to a meaningful extent. This is why early recognition and root cause oriented treatment play a decisive role in long term outcomes. Understanding where and how the nervous system fails is the foundation for choosing a therapy that aims at healing rather than temporary relief.
Pathophysiology of Neuropathy
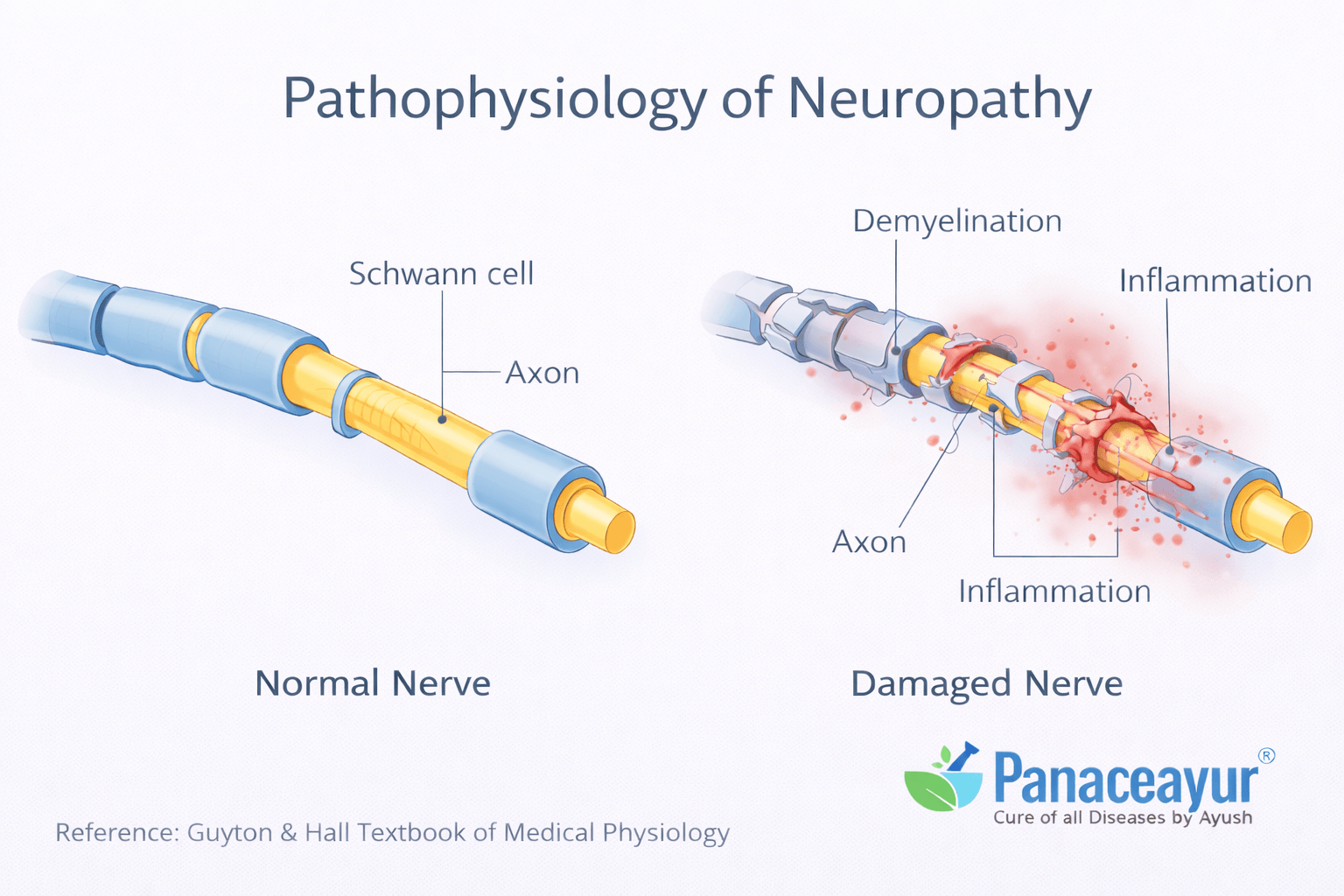
What pathophysiology means in neuropathy
To understand how a peripheral neuropathy cure can occur, it is essential to understand the pathophysiology of neuropathy. Pathophysiology refers to the biological and cellular processes through which disease develops and progresses. In neuropathy, this process involves gradual structural and functional damage to peripheral nerves rather than a sudden injury.
From a medical standpoint, neuropathy develops when nerve fibers are exposed to long term metabolic stress, inflammation, reduced blood supply, or toxic influences. These factors disrupt the normal environment required for nerve survival and repair [2].
Axonal degeneration and its clinical significance
One of the central mechanisms in neuropathy is axonal degeneration. The axon is the core of the nerve fiber that transmits electrical impulses. When axons are damaged, nerve signals weaken or fail to reach their destination. Clinically, axonal degeneration is associated with numbness, loss of sensation, muscle weakness, and reduced reflexes.
From the physician’s perspective, axonal neuropathy indicates deeper nerve injury. Recovery in such cases is slower because axons regenerate very gradually. For you as a patient, this explains why symptoms often progress steadily and why improvement requires sustained treatment rather than short term intervention [2], [3].
Demyelination and signal distortion
Another major pathological process in neuropathy is demyelination. The myelin sheath acts as insulation around nerve fibers and ensures fast, accurate signal conduction. When myelin is damaged, nerve impulses slow down and become irregular. This leads to tingling, burning sensations, electric shock like pain, and exaggerated responses to touch or temperature [6].
Demyelinating neuropathy may cause severe symptoms even when nerve fibers are not completely destroyed. From a clinical viewpoint, demyelination can sometimes be partially reversible if the underlying cause is identified and corrected early [3], [6].
Role of inflammation and immune mediated injury
Chronic inflammation plays a significant role in the development of neuropathy. Inflammatory mediators can directly injure nerve fibers or damage the small blood vessels that supply nerves. In some individuals, immune dysregulation leads to the body attacking its own nerve components, further accelerating degeneration [2].
As a patient, you may not feel inflammation directly, but its effects manifest as worsening pain, increased sensitivity, and progressive nerve dysfunction. This mechanism explains why neuropathy often accompanies autoimmune disorders and chronic systemic inflammation.
Microvascular ischemia and reduced nerve nutrition
Peripheral nerves depend on a dense network of tiny blood vessels for oxygen and nutrient delivery. In neuropathy, especially in metabolic conditions, these microvessels become damaged. Reduced blood flow leads to ischemia, meaning the nerves are starved of oxygen and nutrients. Over time, this nutritional deprivation weakens nerve fibers and impairs their ability to repair themselves [2], [3].
For you, this explains why symptoms often worsen at night or during periods of rest, when circulation naturally slows. It also explains why improving blood flow and tissue nutrition is essential for recovery.
Oxidative stress and mitochondrial dysfunction
At the cellular level, neuropathy is strongly linked to oxidative stress and mitochondrial dysfunction. Mitochondria are the energy producing units of nerve cells. When they are damaged by chronic metabolic stress or toxins, nerve cells cannot generate enough energy to maintain their structure and function. This leads to gradual nerve fiber failure [3].
From a treatment perspective, this highlights why simple pain suppression cannot restore nerve health. Without addressing oxidative damage and energy depletion, nerve degeneration continues silently.
Why neuropathy progresses if untreated
All these mechanisms often occur together rather than in isolation. Axonal degeneration, demyelination, inflammation, ischemia, and oxidative stress reinforce one another. This creates a vicious cycle in which nerve damage accelerates over time [2], [3], [6].
For you as a patient, understanding this interconnected process is critical. Peripheral neuropathy cure requires interrupting this cycle at multiple levels. When treatment focuses only on pain relief, the underlying pathophysiological processes remain active. When the biological causes of nerve injury are addressed, the environment for nerve repair improves, making functional recovery possible over time.
Types of Neuropathy
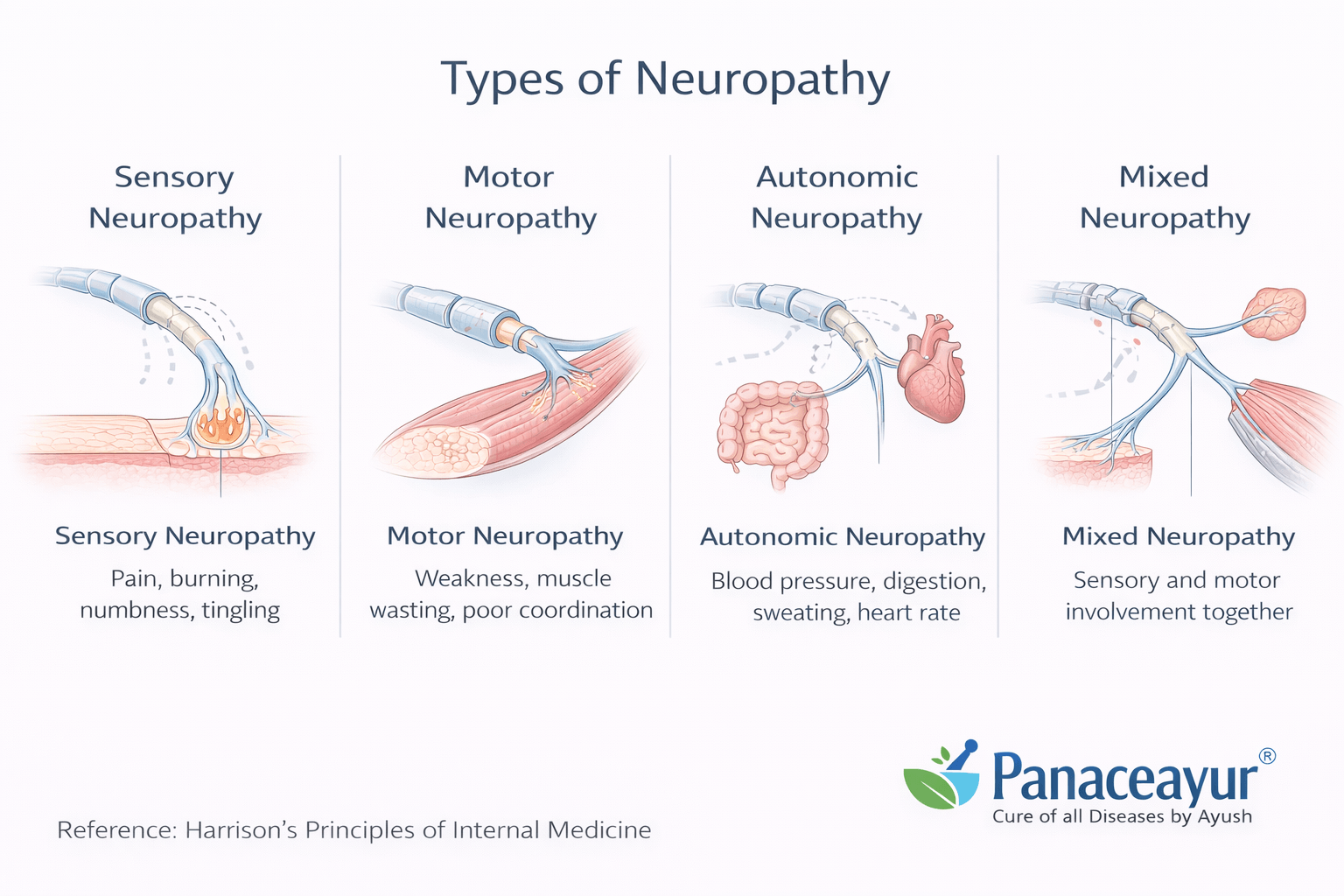
Classification based on nerve function
To move toward a peripheral neuropathy cure, it is important to understand that neuropathy is not a single uniform condition. Clinically, neuropathy is classified based on which type of nerve fibers are predominantly affected. This classification helps doctors understand symptom patterns, disease progression, and treatment priorities [1].
Sensory neuropathy affects nerves responsible for sensation. As a patient, you may experience burning pain, tingling, numbness, altered temperature perception, or electric shock like sensations. Sensory involvement is the most common presentation and is often the earliest sign of nerve dysfunction. Many patients initially dismiss these symptoms as minor, allowing disease progression to continue silently.
Motor neuropathy affects nerves that control muscle movement. In this form, weakness becomes the dominant symptom rather than pain. You may notice difficulty lifting the foot, poor grip strength, muscle cramps, or visible muscle wasting. From the clinician’s perspective, motor neuropathy suggests more advanced nerve involvement and requires careful evaluation [1].
Autonomic neuropathy affects nerves that regulate involuntary body functions. This type can disrupt digestion, bowel movements, bladder control, heart rate, blood pressure, sweating, and sexual function. Autonomic involvement is often overlooked because symptoms appear unrelated to the nervous system, yet it reflects significant nerve damage.
Many patients experience mixed neuropathy, where sensory, motor, and autonomic fibers are affected simultaneously. This mixed pattern is common in long standing disease and often explains why symptoms seem widespread and difficult to categorize.
Classification based on nerve distribution
Neuropathy is also classified based on how nerves are distributed throughout the body. Peripheral polyneuropathy is the most common pattern. It typically affects both sides of the body symmetrically, starting in the feet and gradually moving upward. This length dependent pattern occurs because the longest nerve fibers are the most vulnerable to damage [1].
Mononeuropathy involves damage to a single nerve. Symptoms are localized and correspond to the affected nerve’s territory. While this form may appear less severe, it can still cause significant functional impairment depending on the nerve involved.
Mononeuritis multiplex refers to damage affecting multiple individual nerves in an asymmetric pattern. From a medical standpoint, this pattern often suggests an underlying systemic or inflammatory process and requires detailed evaluation [7].
Classification based on disease course
Neuropathy is further classified by how quickly it develops and progresses. Acute neuropathy develops rapidly over days or weeks and is often associated with immune or toxic causes. Subacute neuropathy progresses over weeks to months. Chronic neuropathy develops slowly over months or years and is the most common presentation seen in clinical practice [1].
As a patient, chronic neuropathy often feels confusing because symptoms worsen gradually and fluctuate over time. From the physician’s perspective, chronic progression indicates ongoing nerve injury rather than a temporary insult.
Why understanding the type of neuropathy matters
Correct classification is not just academic. It directly influences prognosis and treatment strategy. Different types of neuropathy respond differently to therapy. Some forms are more reversible when treated early, while others require long term regenerative support [7].
For you, understanding the type of neuropathy you have helps set realistic expectations and guides treatment decisions. Peripheral neuropathy cure depends on recognizing which nerve fibers are affected, how widely the damage is distributed, and how long the disease has been present. When classification is accurate, treatment can be targeted more precisely, improving the chances of meaningful nerve recovery [1], [7].
Root Causes of Neuropathy
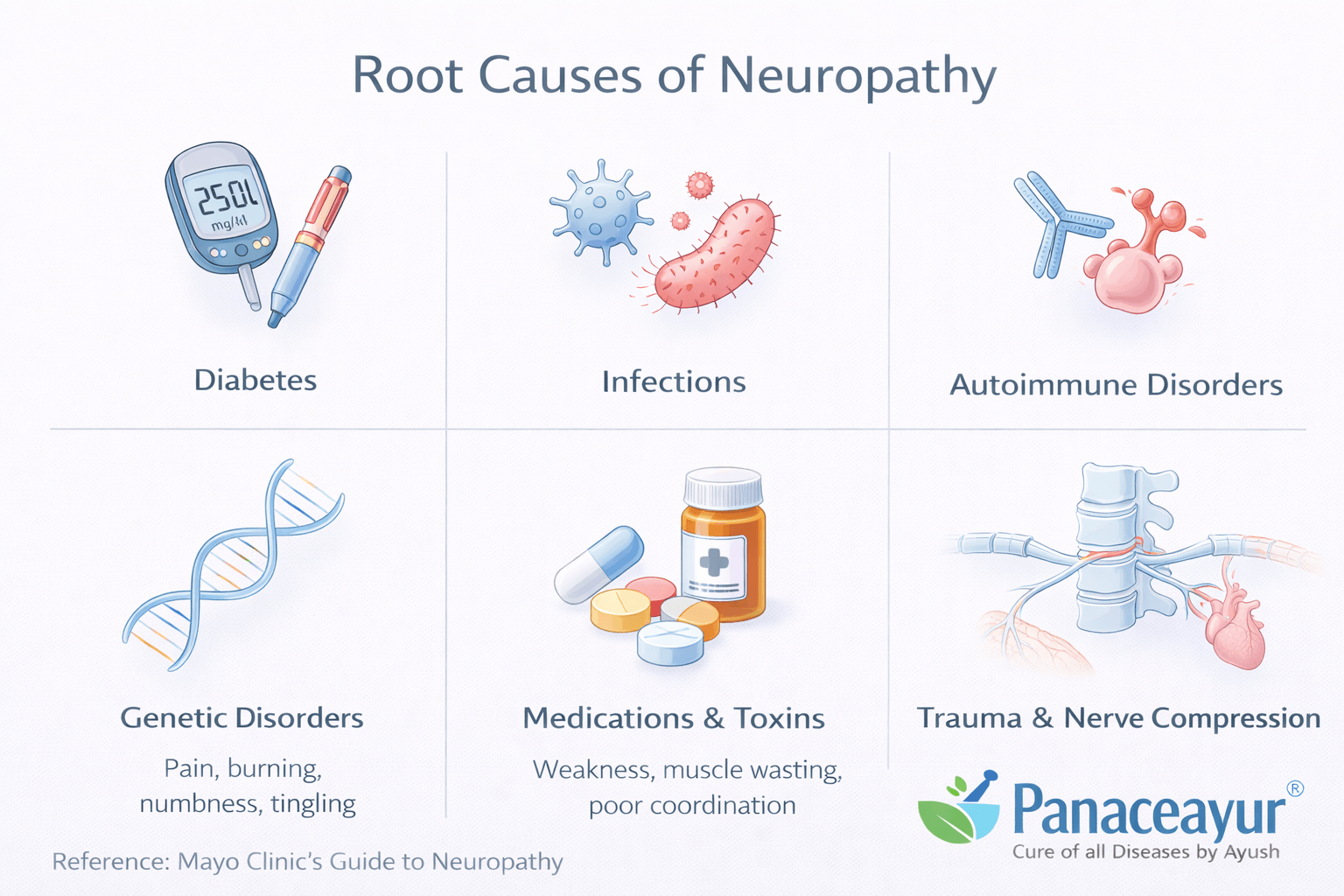
Why identifying root causes is essential
A true peripheral neuropathy cure cannot be achieved unless the root causes of nerve damage are clearly identified and addressed. Neuropathy rarely develops from a single factor. In most patients, it is the result of multiple biological stresses acting together over time. From a clinical standpoint, nerves become damaged when the internal environment no longer supports their nutrition, protection, and repair [2], [4].
As a patient, you may be told that your neuropathy is idiopathic, meaning no cause is found. In reality, this usually reflects incomplete evaluation rather than absence of cause. Modern research shows that most neuropathies are linked to identifiable metabolic, immune, infectious, or toxic influences [4].
Metabolic and endocrine dysfunction
Metabolic disorders are among the most common root causes of neuropathy. Diabetes is the most recognized example, but nerve damage often begins years before diabetes is formally diagnosed. Prediabetes, insulin resistance, metabolic syndrome, and obesity can all impair nerve health by disrupting blood flow, increasing oxidative stress, and damaging small blood vessels that nourish nerves [2].
From the physician’s perspective, chronic blood sugar fluctuation damages nerves gradually and silently. For you as a patient, this explains why neuropathy may develop even when blood sugar levels appear only mildly abnormal.
Thyroid disorders also contribute to neuropathy by slowing metabolism and impairing tissue repair. Hormonal imbalance reduces the ability of nerves to regenerate and increases vulnerability to injury [4].
Immune and inflammatory causes
Autoimmune and inflammatory conditions are another major contributor to neuropathy. In these cases, the immune system mistakenly targets nerve fibers or the blood vessels supplying them. This immune mediated injury leads to inflammation, demyelination, and axonal damage [5].
Conditions such as autoimmune thyroid disease, systemic inflammatory disorders, and immune mediated neuropathies can cause progressive nerve dysfunction even in the absence of metabolic disease. From a clinical standpoint, immune involvement often explains rapidly progressive or asymmetric neuropathy patterns.
As a patient, immune related neuropathy may feel unpredictable, with symptoms fluctuating or worsening during periods of systemic inflammation or stress.
Chronic inflammation and systemic disease burden
Neuropathy is frequently part of a broader chronic disease network. Long standing inflammatory states increase oxidative stress and impair microcirculation, gradually weakening nerve fibers. This explains why neuropathy commonly coexists with chronic kidney disease, liver disorders, and inflammatory conditions [4].
From the doctor’s viewpoint, nerves often serve as early indicators of systemic disease burden. When the body’s internal environment becomes chronically toxic or inflamed, nerves are among the first tissues to suffer.
Toxic and drug related causes
Exposure to toxins and certain medications is a well documented cause of neuropathy. Chemotherapy drugs, prolonged antibiotic use, alcohol, and environmental toxins can directly injure nerve fibers. These substances interfere with mitochondrial function and accelerate axonal degeneration [2].
For you as a patient, this highlights the importance of medication history and lifestyle evaluation. Neuropathy may develop not only from disease but also from long term exposure to substances that impair nerve health.
Why neuropathy is usually multifactorial
In most real world cases, neuropathy develops due to a combination of factors rather than a single cause. Metabolic stress may coexist with immune dysregulation, nutritional deficiency, or toxic exposure. These overlapping influences amplify nerve damage and make recovery more complex [2], [4], [5].
Understanding this multifactorial nature is critical. Peripheral neuropathy cure depends on addressing all contributing factors rather than focusing on one isolated abnormality. When the underlying causes are identified and corrected together, the environment for nerve repair improves significantly, offering a realistic pathway toward long term recovery.
Common Diseases That Occur With Neuropathy

Why neuropathy rarely exists alone
Peripheral neuropathy cure requires understanding that neuropathy is rarely an isolated condition. In most patients, nerve damage develops as part of a broader systemic disease process. From a clinical perspective, nerves are highly sensitive to metabolic imbalance, chronic inflammation, and impaired circulation. When other chronic diseases are present, nerve tissue often becomes an early target of damage [2], [4].
As a patient, you may notice that neuropathy symptoms appear alongside other long standing health issues. These associated conditions often contribute directly to nerve degeneration and must be addressed for meaningful recovery.
Metabolic disorders and neuropathy
Metabolic diseases are among the most common conditions associated with neuropathy. Diabetes is the most well known, but neuropathy frequently occurs in people with prediabetes, insulin resistance, and metabolic syndrome. Research shows that nerve damage can begin even before diabetes is formally diagnosed [2].
From the physician’s viewpoint, chronic fluctuations in blood glucose impair microcirculation and increase oxidative stress, which gradually injures nerve fibers. For you as a patient, this explains why neuropathy may worsen despite seemingly controlled blood sugar levels.
Obesity and metabolic syndrome further increase inflammatory burden and reduce nerve repair capacity, accelerating progression [4].
Endocrine disorders and nerve dysfunction
Thyroid disorders are another common condition associated with neuropathy. Both hypothyroidism and hyperthyroidism can disrupt nerve metabolism and slow regenerative processes. Patients with thyroid disease often report numbness, tingling, weakness, and muscle cramps.
Clinically, hormonal imbalance affects tissue oxygenation and nutrient delivery, making nerves more vulnerable to injury. When thyroid dysfunction remains untreated, neuropathic symptoms tend to persist or worsen [4].
Autoimmune and inflammatory diseases
Autoimmune disorders frequently coexist with neuropathy. Conditions such as rheumatoid arthritis, lupus, and autoimmune thyroid disease can directly or indirectly damage nerves through immune mediated inflammation [14].
From the doctor’s perspective, immune driven neuropathy may present with fluctuating symptoms, rapid progression, or asymmetric nerve involvement. For you as a patient, neuropathy linked to autoimmune disease often worsens during inflammatory flares or periods of stress.
Chronic kidney and liver disease
Chronic kidney disease is a well recognized cause of neuropathy, often referred to as uremic neuropathy. Accumulation of metabolic toxins in kidney disease damages nerve fibers over time. Symptoms typically progress gradually and may be overlooked until significant nerve dysfunction develops [15].
Liver disease also contributes to neuropathy by impairing detoxification and nutrient metabolism. When toxins accumulate in the bloodstream, nerve tissue is exposed to prolonged chemical stress, increasing the risk of degeneration [4].
Why treating associated diseases is essential
From a clinical standpoint, neuropathy cannot be effectively treated without addressing the diseases that coexist with it. Nerve repair requires a supportive internal environment. If metabolic imbalance, inflammation, or organ dysfunction persists, nerve degeneration continues despite symptomatic treatment [2], [15].
For you as a patient, recognizing these associated diseases is empowering. Peripheral neuropathy cure becomes more achievable when all contributing conditions are identified and managed together. Treating neuropathy in isolation rarely produces lasting results, while a comprehensive approach significantly improves the chances of nerve recovery and long term stability [2], [4], [14], [15].
Rare and Often Missed Diseases Associated With Neuropathy
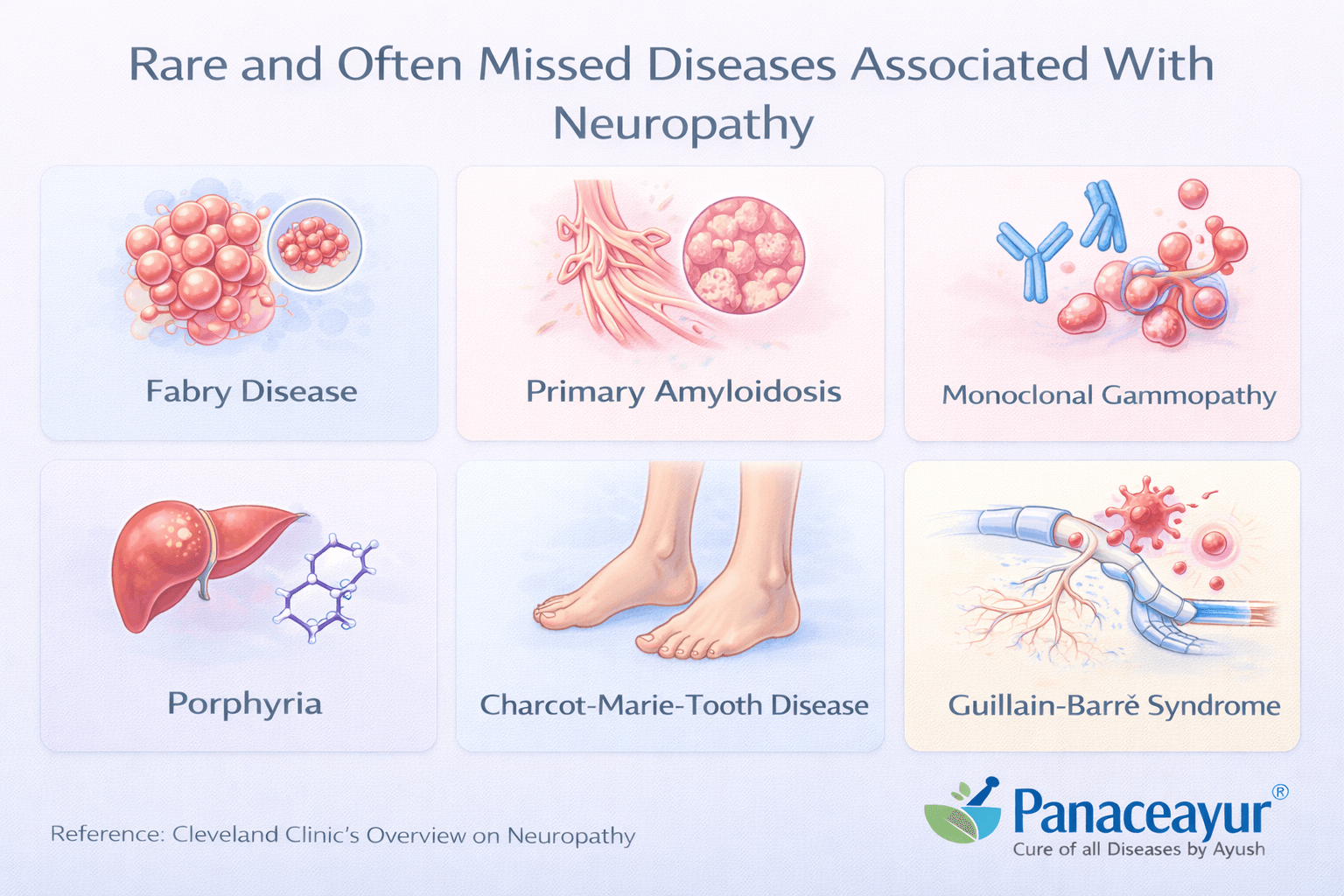
Why many neuropathies are labeled idiopathic
A peripheral neuropathy cure often remains out of reach because many underlying diseases are overlooked. When routine tests fail to identify an obvious cause, patients are frequently told that their condition is idiopathic. From a clinical standpoint, this term often reflects incomplete investigation rather than true absence of disease. Several less common but clinically important conditions are known to cause neuropathy and are frequently missed during standard evaluation [5], [7].
As a patient, you may feel frustrated when symptoms persist despite normal reports. Understanding these overlooked causes helps explain why neuropathy can progress silently and why deeper evaluation is sometimes necessary.
Immune mediated and inflammatory neuropathies
Certain immune mediated neuropathies develop when the immune system targets nerve fibers or their protective coverings. These conditions may not present with obvious systemic signs early on. Chronic inflammatory demyelinating polyneuropathy is one such example, where immune driven inflammation damages the myelin sheath and disrupts nerve signaling [7], [14].
From the doctor’s perspective, these neuropathies often show fluctuating symptoms, gradual progression, or patchy nerve involvement. For you as a patient, this may appear as periods of worsening followed by partial improvement, which can delay diagnosis.
Vasculitic and systemic inflammatory disorders
Vasculitic disorders cause inflammation of blood vessels that supply nerves. Reduced blood flow leads to nerve ischemia and rapid fiber injury. These conditions may present with asymmetric neuropathy, sudden weakness, or severe pain affecting specific nerve territories [5].
Clinically, vasculitic neuropathy is considered a medical red flag because untreated vascular inflammation can cause irreversible nerve damage. As a patient, early recognition is critical, as timely intervention can prevent permanent loss of nerve function.
Genetic and late onset hereditary neuropathies
Some hereditary neuropathies do not appear in childhood. Instead, they manifest later in life and are often mistaken for age related nerve degeneration or metabolic neuropathy. These conditions may progress slowly and lack clear laboratory markers, making diagnosis challenging [7].
From a clinical standpoint, family history, subtle motor changes, and long standing sensory symptoms may offer clues. For you, understanding this possibility helps explain why neuropathy can develop even in the absence of obvious external risk factors.
Neuropathy associated with chronic systemic disease
Chronic systemic diseases can also produce neuropathy through prolonged inflammatory or metabolic stress. Inflammatory conditions that persist over years may gradually damage nerve fibers without causing dramatic early symptoms. Over time, cumulative injury leads to significant sensory and motor impairment [14].
From the physician’s view, this form of neuropathy reflects long term disease burden rather than an isolated nerve disorder. For you as a patient, this reinforces the importance of addressing overall health rather than focusing only on nerve pain.
Why identifying rare causes changes outcomes
Recognizing these rare and often missed diseases has a direct impact on prognosis. Neuropathy linked to immune mediated or inflammatory processes may respond better when treated early and appropriately. When such conditions are mistaken for idiopathic neuropathy, opportunities for meaningful recovery may be lost [5], [7], [14].
For you, this knowledge highlights an important truth. Peripheral neuropathy cure is more likely when the underlying cause is correctly identified. Careful evaluation and awareness of uncommon contributors allow treatment to move beyond symptom control toward addressing the true drivers of nerve damage.
Signs and Symptoms of Neuropathy

Why symptoms vary from person to person
The signs and symptoms of neuropathy differ widely because different types of nerve fibers may be affected in each individual. From a clinical perspective, symptoms depend on whether sensory, motor, or autonomic nerves are involved and how advanced the nerve damage is. For you as a patient, this explains why neuropathy may feel confusing and inconsistent, especially in the early stages [8].
Doctors recognize that symptoms often appear gradually and may fluctuate. Early warning signs are frequently overlooked or misattributed to fatigue, aging, or circulation problems.
Sensory symptoms you may experience
Sensory symptoms are the most common and are often the first to appear. You may notice burning sensations in the feet or hands, tingling, pins and needles, or numbness. Some patients describe electric shock like pain or heightened sensitivity to touch, temperature, or pressure.
From a medical standpoint, these symptoms indicate impaired signal transmission along sensory nerve fibers. As nerve efficiency declines, the brain receives distorted or incomplete information, resulting in abnormal sensations [8].
Loss of sensation is equally important. Reduced ability to feel pain or temperature increases the risk of unnoticed injuries, burns, or infections, particularly in the feet.
Motor symptoms and muscle involvement
When motor nerves are affected, symptoms shift from pain toward weakness. You may notice difficulty lifting the foot, reduced grip strength, muscle cramps, or fatigue during routine activities. Over time, muscles may shrink due to lack of proper nerve stimulation.
Clinically, motor involvement signals more advanced neuropathy. From the physician’s perspective, muscle weakness and wasting indicate structural nerve damage rather than temporary irritation [8].
For you, this stage often interferes with balance, walking, and daily independence.
Autonomic symptoms that are often missed
Autonomic neuropathy affects nerves that control involuntary body functions. These symptoms are frequently overlooked because they do not resemble typical nerve pain. You may experience digestive disturbances, bloating, constipation, diarrhea, abnormal sweating, dizziness on standing, irregular heart rate, bladder issues, or sexual dysfunction.
From a clinical view, autonomic involvement reflects widespread nerve dysfunction. For you as a patient, recognizing these symptoms as part of neuropathy is important, as they often coexist with sensory and motor complaints [8].
Patterns and progression of symptoms
Neuropathy symptoms often follow a length dependent pattern. This means symptoms usually begin in the toes and feet, then gradually move upward as nerve damage progresses. Hands may become involved later. This pattern occurs because longer nerve fibers are more vulnerable to injury.
Doctors observe that symptoms frequently worsen at night. Reduced circulation, lower external stimulation, and increased nerve sensitivity contribute to nighttime discomfort. For you, this may lead to disturbed sleep and fatigue, which further affects quality of life [8].
Why early symptoms should not be ignored
From a medical standpoint, early neuropathy symptoms are critical warning signs. Mild tingling or intermittent burning reflects early nerve dysfunction, not a harmless condition. When these signs are ignored or suppressed with medication alone, underlying nerve damage continues to progress.
For you as a patient, recognizing symptoms early improves the chances of recovery. Peripheral neuropathy cure is more achievable when treatment begins before extensive nerve degeneration occurs. Awareness of these signs empowers you to seek timely evaluation and address the deeper causes of nerve damage rather than waiting for symptoms to become disabling [8].
Red Flags That Require Immediate Attention

Why certain symptoms should never be ignored
While many neuropathy symptoms develop slowly, some warning signs indicate serious or rapidly progressing nerve damage. From a clinical perspective, these red flags suggest acute nerve injury, immune mediated disease, or systemic involvement that requires urgent evaluation. For you as a patient, recognizing these signs early can prevent permanent nerve loss and life altering complications [8], [14].
Doctors consider these symptoms medical warning signals rather than routine neuropathy complaints.
Rapid progression of symptoms
If numbness, weakness, or pain worsens rapidly over days or weeks instead of months or years, it is a red flag. Sudden progression suggests active nerve injury rather than slow degeneration. Clinicians associate this pattern with inflammatory, immune mediated, or toxic causes of neuropathy [14].
For you, rapid worsening means waiting or relying on pain relief alone can be dangerous. Immediate assessment is essential.
Sudden or severe muscle weakness
Sudden weakness in the legs, arms, or face is a serious warning sign. Difficulty standing, walking, climbing stairs, lifting objects, or holding items may indicate significant motor nerve involvement. From the physician’s perspective, this can reflect acute nerve fiber damage or immune related neuropathy [8], [14].
As a patient, sudden weakness should never be dismissed as fatigue or aging.
Loss of bladder or bowel control
Changes in bladder or bowel function suggest autonomic nerve involvement. Difficulty urinating, loss of bladder control, severe constipation, or bowel incontinence are critical signs. Clinically, this indicates widespread nerve dysfunction that may progress quickly if untreated [8].
For you, these symptoms require immediate medical attention, even if pain is mild.
Severe or unrelenting night pain
Neuropathic pain that becomes severe at night and does not respond to usual medications may indicate active inflammation or ischemic nerve injury. Doctors recognize persistent night pain as a potential marker of progressive or immune mediated neuropathy [8], [14].
If pain disrupts sleep consistently and intensifies over time, evaluation should not be delayed.
Asymmetric or patchy nerve involvement
Neuropathy that affects one side of the body more than the other or involves specific nerves in a patchy pattern is a red flag. Clinically, this pattern raises concern for vasculitic or inflammatory neuropathies rather than metabolic causes [14].
For you as a patient, uneven symptoms often feel confusing, but they provide important diagnostic clues that should be investigated promptly.
Breathing difficulty or swallowing problems
Shortness of breath, weak cough, or difficulty swallowing indicate possible involvement of nerves controlling respiratory or bulbar muscles. From a medical standpoint, this represents an emergency, as respiratory failure can develop if these nerves are compromised [14].
For you, these symptoms require immediate emergency care rather than outpatient evaluation.
Why early action matters
From the doctor’s point of view, red flag symptoms change the entire treatment approach. These signs often indicate conditions where early intervention can halt or reverse nerve damage. Delayed care increases the risk of permanent disability.
For you as a patient, understanding these warning signs is protective. Peripheral neuropathy cure becomes far less achievable when severe or rapidly progressive nerve injury is ignored. Seeking immediate evaluation when red flags appear can preserve nerve function, prevent complications, and significantly improve long term outcomes [8], [14].
Diagnostic Approach
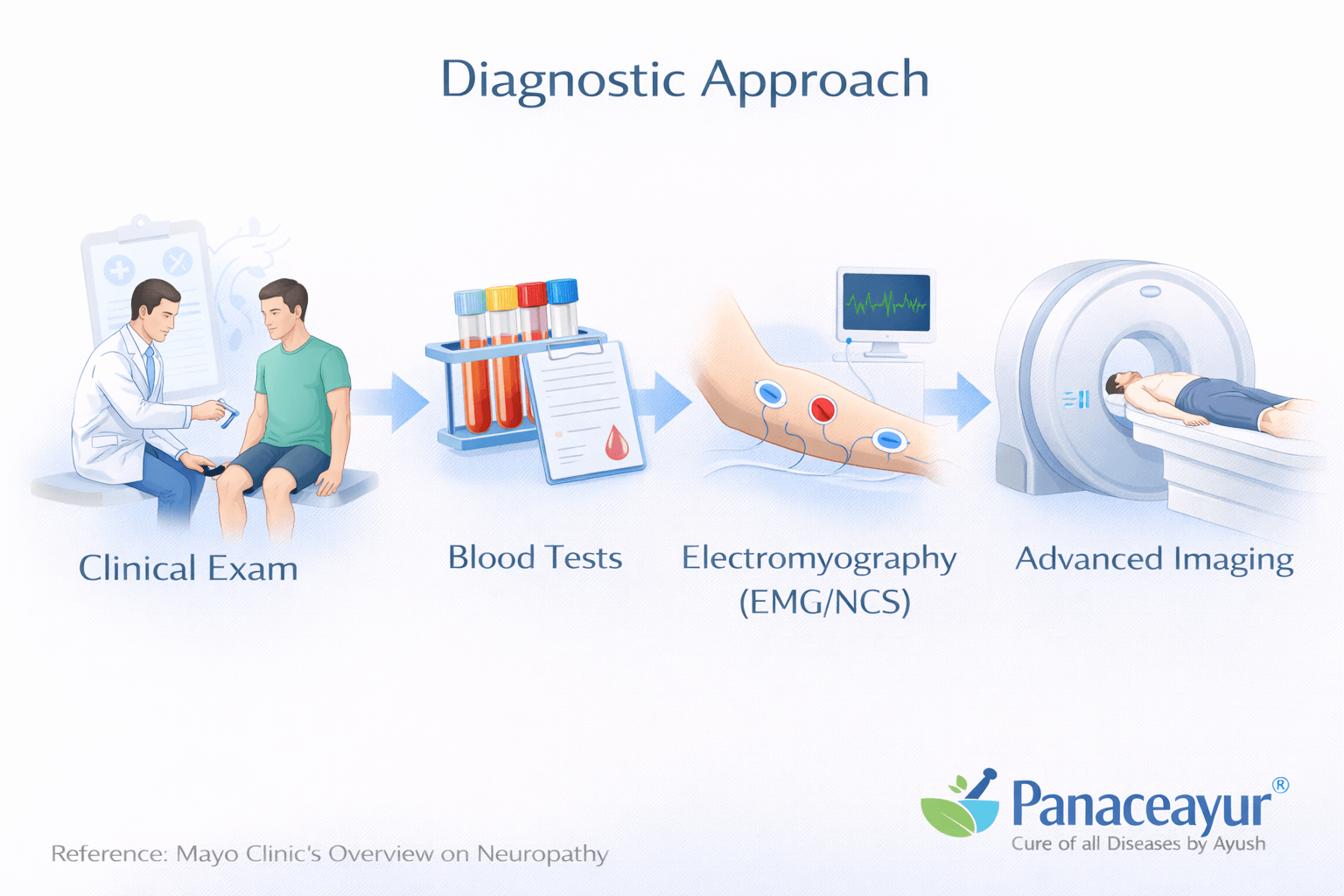
Why accurate diagnosis is critical
A meaningful peripheral neuropathy cure begins with accurate diagnosis. Neuropathy is not a single disease, but a clinical syndrome with multiple causes and patterns. From a physician’s perspective, diagnosis is not just about confirming nerve damage, but about understanding why the nerves are damaged and how far the process has progressed. For you as a patient, proper diagnosis prevents unnecessary treatments and guides a more effective recovery plan [1].
Doctors emphasize that incomplete or rushed evaluation is one of the main reasons neuropathy remains untreated or mislabeled as idiopathic.
Clinical history and physical examination
The diagnostic process always starts with a detailed clinical history. Your doctor will ask about symptom onset, progression, pain patterns, weakness, sensory changes, balance issues, and autonomic symptoms such as digestive or bladder problems. Medication use, alcohol exposure, occupational toxins, family history, and chronic illnesses are also carefully reviewed [1].
During physical examination, the physician assesses sensation, muscle strength, reflexes, coordination, and gait. From a clinical standpoint, these findings often provide more insight than tests alone. For you, this step helps your doctor determine which nerve fibers are involved and whether the pattern suggests metabolic, inflammatory, or structural nerve damage.
Blood investigations and their limitations
Blood tests are commonly used to look for metabolic, inflammatory, and nutritional causes of neuropathy. These may include blood glucose markers, vitamin levels, thyroid function, kidney and liver parameters, and inflammatory indicators.
However, doctors recognize that normal blood tests do not rule out neuropathy. Early nerve damage may exist even when laboratory values fall within reference ranges. For you as a patient, this explains why symptoms may persist despite reports being described as normal [1].
Nerve conduction studies and electromyography
Nerve conduction studies and electromyography are key tools in evaluating neuropathy. These tests measure how fast and how effectively electrical signals travel through nerves and muscles. From a clinical perspective, they help differentiate between axonal damage and demyelination, which is critical for diagnosis and prognosis [6].
For you, these tests can feel technical, but their purpose is simple. They help doctors identify the type and severity of nerve injury. It is important to understand that these studies may appear normal in early or small fiber neuropathy, even when symptoms are present.
Role of electrophysiology in classification
Electrophysiological testing allows clinicians to classify neuropathy more precisely. Demyelinating patterns suggest myelin sheath involvement, while reduced signal amplitude points toward axonal loss. This distinction influences treatment decisions and expected recovery timelines [6].
From the doctor’s point of view, classification based on electrophysiology helps avoid trial and error treatment. For you, it increases the likelihood of receiving a targeted and rational therapy plan.
Why early neuropathy is often missed
One of the major diagnostic challenges is that early neuropathy may not be detected by routine testing. Small fiber neuropathy, in particular, can cause significant pain and sensory disturbance without clear abnormalities on nerve conduction studies. This leads many patients to feel dismissed or misunderstood.
Clinicians acknowledge this limitation and rely on symptom patterns and clinical judgment rather than tests alone [1].
Integrating findings for effective treatment
Accurate diagnosis requires integrating clinical history, physical examination, laboratory findings, and electrophysiological studies. No single test can define neuropathy completely. From a physician’s perspective, diagnosis is a process rather than a single result.
For you as a patient, this integrated approach is essential. Peripheral neuropathy cure is far more achievable when the diagnostic process identifies both the pattern of nerve damage and the underlying contributors. Proper diagnosis lays the foundation for addressing root causes, supporting nerve repair, and preventing further progression [1], [6].
Why Conventional Treatment Does Not Cure Neuropathy
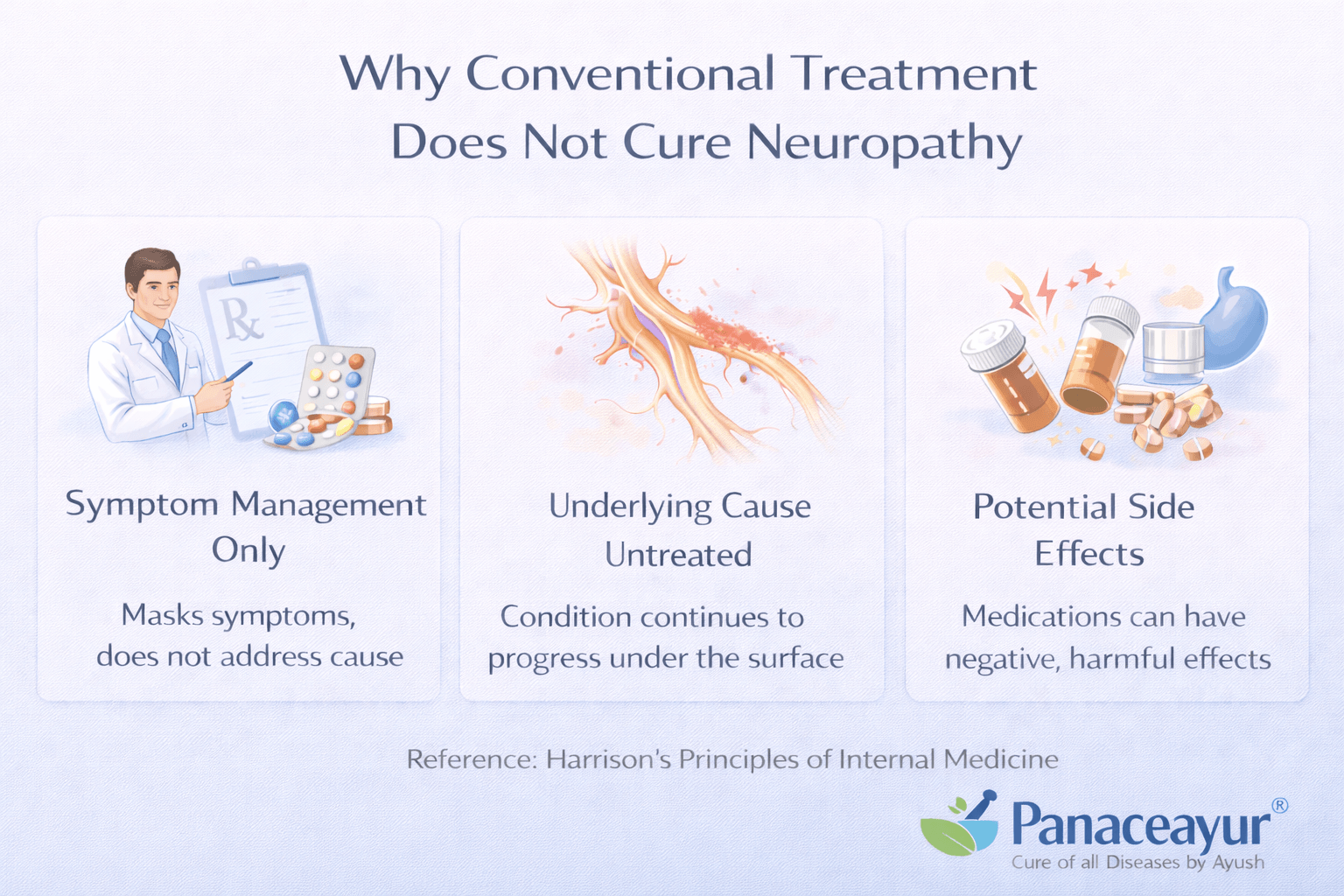
Focus on symptom suppression rather than nerve repair
Conventional treatment for neuropathy is primarily designed to reduce symptoms rather than heal damaged nerves. From a medical standpoint, most commonly prescribed drugs aim to dampen abnormal nerve signals so that pain becomes less noticeable. For you as a patient, this may provide temporary relief, but it does not address the underlying nerve injury that caused the symptoms in the first place [9].
Doctors acknowledge that symptom control is not the same as disease reversal. Pain reduction does not mean that nerves are repairing or regenerating.
How neuropathic pain medications actually work
Medications such as gabapentin and pregabalin are frequently prescribed for neuropathic pain. These drugs work by altering how nerve signals are transmitted within the nervous system. They reduce signal intensity and dampen abnormal firing patterns, which can lower pain perception [9], [10].
From a clinical perspective, these drugs do not rebuild myelin, restore axonal integrity, or improve nerve nutrition. They simply modify signal processing. For you, this explains why symptoms often return or worsen if medication is stopped.
Lack of regenerative action on nerve tissue
One of the key limitations of conventional treatment is the absence of regenerative support. Nerve fibers require adequate blood flow, nutrients, mitochondrial energy, and a low inflammatory environment to heal. Standard drug therapy does not improve these biological conditions [9].
From the physician’s point of view, this is why neuropathy frequently progresses despite long term medication use. Pain may be controlled while nerve degeneration continues silently.
Tolerance, dependency, and diminishing benefit
Over time, many patients experience reduced effectiveness of neuropathic pain medications. Higher doses may be required to achieve the same level of relief. This can increase side effects such as dizziness, sedation, cognitive dulling, and balance problems [10].
For you as a patient, this creates a cycle where symptom relief becomes increasingly dependent on medication, without improving nerve health or long term function.
Masking of disease progression
Another major concern is that symptom suppression can mask disease progression. When pain is reduced, it may appear that neuropathy is improving. In reality, nerve damage may continue to advance beneath the surface.
Clinicians recognize that delayed recognition of progression often leads to late intervention, at which point nerve recovery becomes more difficult [9].
Why cure requires a different therapeutic approach
From a medical and biological perspective, curing neuropathy requires restoring the conditions that allow nerves to survive and regenerate. This includes improving circulation, reducing inflammation, supporting mitochondrial function, correcting metabolic imbalance, and providing sustained tissue nourishment.
For you, this explains why peripheral neuropathy cure cannot be achieved through pain blocking alone. Conventional treatment plays a role in symptom management, but it does not reverse nerve damage. Long term recovery depends on therapies that address the root biological causes of nerve degeneration rather than only controlling discomfort [9], [10].
Ayurvedic Understanding of Neuropathy
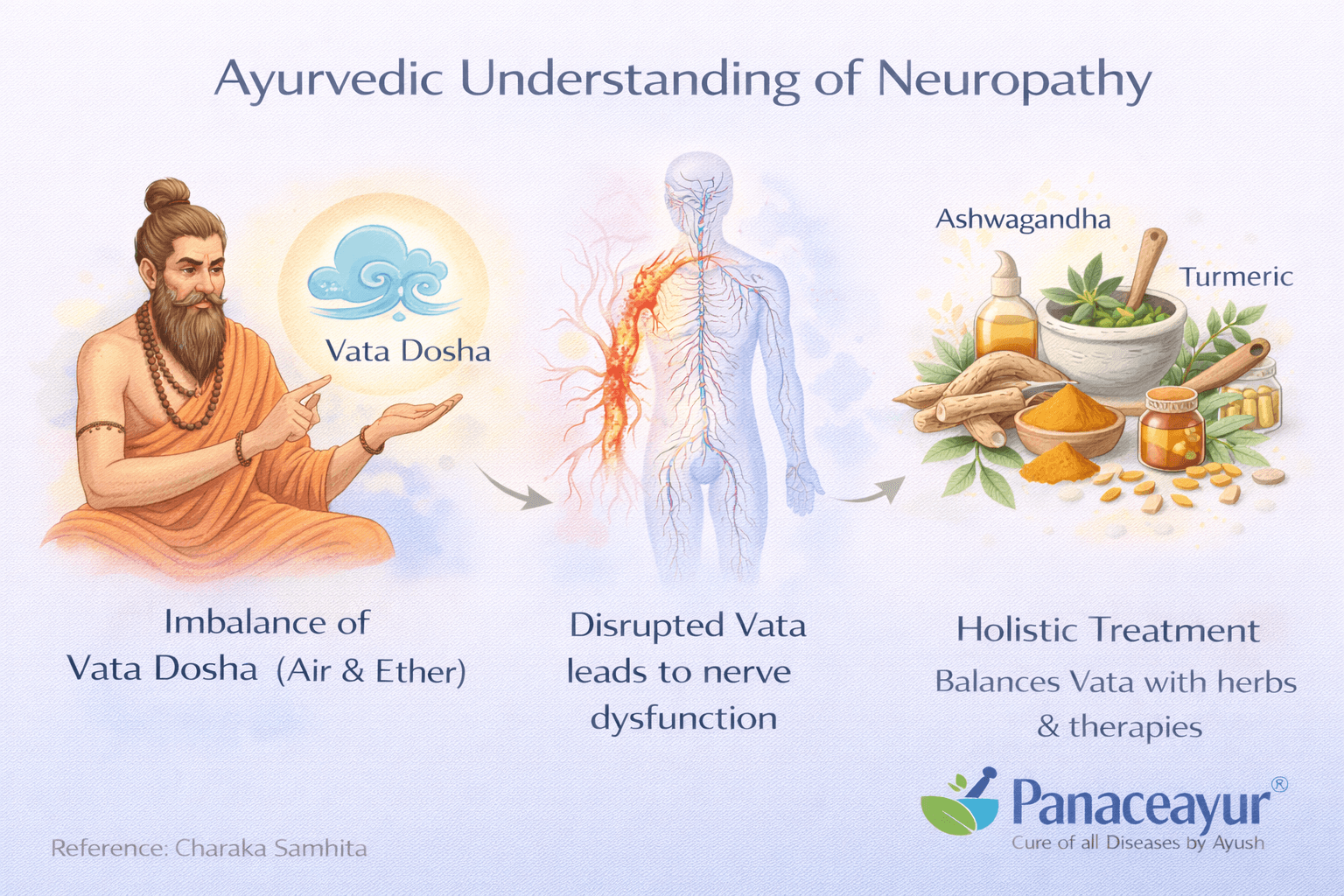
Neuropathy as a disorder of Vata imbalance
In Ayurveda, neuropathy is not viewed as an isolated nerve disease. It is understood as a disorder arising primarily from aggravation of Vata Dosha. Vata governs movement, nerve impulses, sensation, and communication within the body. When Vata becomes disturbed, nerve function is the first to suffer. Classical Ayurvedic texts describe this group of disorders under Vatavyadhi, which includes conditions involving pain, numbness, weakness, tremors, and sensory disturbances [11], [12].
For you as a patient, this means neuropathy is seen as a functional imbalance that gradually leads to structural damage if left uncorrected.
Role of Majja Dhatu in nerve health
Ayurveda explains that nerve tissue is closely related to Majja Dhatu. Majja Dhatu represents the deeper nourishing tissue responsible for the integrity of the nervous system, bone marrow, and brain. When Majja Dhatu becomes depleted or poorly nourished, nerves lose their strength, resilience, and ability to transmit signals properly [11].
From the physician’s Ayurvedic perspective, symptoms such as burning, tingling, numbness, weakness, and sensory loss indicate Majja Dhatu Kshaya, meaning gradual tissue depletion. For you, this explains why neuropathy often develops slowly and worsens over time.
Importance of Agni and digestion
Ayurveda places strong emphasis on Agni, the digestive and metabolic fire. Healthy nerve tissue depends on proper digestion and absorption of nutrients. When Agni is weak, nutrition does not reach deeper tissues effectively, including Majja Dhatu. Over time, this leads to tissue starvation and nerve degeneration [12].
As a patient, you may notice digestive symptoms such as bloating, poor appetite, acidity, or irregular bowel movements alongside neuropathy. Ayurveda views these as interconnected rather than separate problems.
Srotas blockage and impaired nerve nourishment
Another key concept in Ayurveda is Srotorodha, which refers to blockage of microchannels responsible for transporting nutrients and waste. When these channels become obstructed by metabolic toxins or undigested material, nourishment cannot reach nerve tissue properly [11].
From a clinical Ayurvedic standpoint, neuropathy develops when Vata aggravation combines with Srotorodha and Majja Dhatu depletion. This triad explains why pain relief alone cannot reverse nerve damage.
Why Ayurveda focuses on Rasayana therapy
Ayurvedic treatment of neuropathy emphasizes Rasayana therapy, which aims to restore tissue quality, strengthen nerve function, and improve long term resilience. Rasayana does not target symptoms alone. It focuses on rebuilding Majja Dhatu, calming aggravated Vata, improving digestion, and reopening obstructed channels [12].
For you as a patient, this approach shifts the goal from short term pain control to long term nerve regeneration and functional recovery.
How this perspective supports cure rather than management
From the Ayurvedic viewpoint, neuropathy is reversible when treated early and appropriately. When Vata is balanced, Agni is restored, and Majja Dhatu is nourished, nerve tissue can recover meaningful function. Classical texts emphasize sustained, personalized therapy rather than quick fixes [11], [12].
For you, understanding this framework is empowering. Peripheral neuropathy cure in Ayurveda is not based on suppressing nerve signals. It is based on correcting the internal environment that caused nerve failure in the first place. This foundational understanding guides the use of diet, lifestyle, Rasayana formulations, and supportive therapies aimed at true healing rather than temporary relief.
Best Ayurvedic Medicine (Avaleha) for Neuropathy
Why Avaleha is preferred in nerve disorders
In Ayurveda, Avaleha is considered one of the most effective dosage forms for chronic and degenerative diseases. Avaleha allows sustained release of medicinal compounds, deep tissue penetration, and long term nourishment of weakened Dhatus. For conditions like neuropathy, where nerve tissue requires continuous support, Avaleha is preferred over tablets or powders [11], [12].
From the Ayurvedic physician’s perspective, nerve disorders cannot be corrected with short acting medicines. They require therapies that steadily rebuild Majja Dhatu and calm aggravated Vata over time.
Classical rationale behind Rasayana Avaleha
Classical Ayurvedic texts describe Rasayana therapy as essential in Vatavyadhi and Majjagata Vata. Rasayana strengthens tissues, improves nerve resilience, and slows degeneration. When delivered in Avaleha form, Rasayana herbs act synergistically to nourish nerves, improve circulation, and reduce internal dryness that aggravates Vata [11].
For you as a patient, this explains why temporary pain relief is insufficient. Nerve healing requires rebuilding from within, not just silencing symptoms.
Ashwagandha based Rasayana Avaleha as the core formulation
Among Rasayana herbs, Ashwagandha holds a central place in nerve disorders. Classical texts describe Ashwagandha as Balya and Rasayana, meaning it restores strength and vitality at a deep tissue level. When used in Avaleha form, Ashwagandha supports nerve regeneration, improves signal conduction, and enhances muscular strength associated with motor nerves [12].
From a modern scientific viewpoint, Ashwagandha exhibits antioxidant and neuroprotective properties, which help counter oxidative stress involved in nerve degeneration [13].
Supportive herbs and components in Avaleha
A classical Rasayana Avaleha for neuropathy often includes supportive herbs that work alongside Ashwagandha. These herbs help reduce inflammation, improve circulation, and stabilize nerve function. Medicated ghee and natural sweet bases enhance bioavailability and allow herbs to reach deeper tissues such as Majja Dhatu.
From the physician’s standpoint, these combinations are not random. They are designed to address Vata imbalance, Srotas blockage, and tissue depletion simultaneously [11], [12].
How Avaleha supports nerve regeneration
Avaleha works at multiple levels. It improves digestion and absorption, ensuring nutrients reach nerve tissue. It calms aggravated Vata, which is responsible for pain and abnormal nerve firing. It nourishes Majja Dhatu, allowing gradual repair of damaged nerve fibers.
For you as a patient, this translates into reduced burning sensations, improved sensation, better muscle strength, improved sleep, and overall functional recovery when used consistently under guidance [11], [12], [13].
Duration and consistency matter
Ayurveda emphasizes that Rasayana Avaleha must be taken consistently over months, not weeks. Nerve tissue regenerates slowly, and intermittent use does not produce stable results. Physicians assess progress based on symptom reduction, functional improvement, and overall vitality rather than immediate pain relief.
For you, this means patience and consistency are essential. Peripheral neuropathy cure through Ayurveda is a gradual process that focuses on rebuilding nerve health rather than masking discomfort.
Why market bought Avaleha often fails
Generic market preparations often fail because they are not tailored to individual constitution, disease stage, or associated conditions. Poor quality raw materials, incorrect processing, and lack of digestive correction reduce effectiveness.
From a clinical Ayurvedic viewpoint, Avaleha should always be selected and supervised by a qualified practitioner. When properly prepared and personalized, Rasayana Avaleha becomes one of the most effective tools for long term nerve healing [11], [12].
How this approach aligns with true cure
Unlike symptom suppressive treatments, Ayurvedic Avaleha aims to correct the internal terrain that allowed neuropathy to develop. By nourishing nerves, restoring digestion, and balancing Vata, this approach supports genuine recovery rather than temporary relief.
For you as a patient, this represents a shift from managing neuropathy to addressing its root cause. When used appropriately, Rasayana Avaleha offers a scientifically and classically grounded pathway toward meaningful nerve repair and long term improvement [11], [12], [13].
Medicine Preparation Method for 30 Days
This Rasayana Avaleha is designed to support a peripheral neuropathy cure by deeply nourishing Majja Dhatu, stabilizing Vata function, improving nerve conduction, and supporting long term regeneration when used consistently.
Ingredients Required for 30 Days
Core Rasayana and Nerve Nourishing Herbs (powder form)
Ashwagandha root powder 300 g
Bala root powder 200 g
Guduchi stem powder 200 g
Shatavari root powder 150 g
Yashtimadhu root powder 150 g
Dashamoola coarse powder 200 g
Kapikacchu seed powder 100 g
Gokshura fruit powder 100 g
Punarnava root powder 100 g
Amalaki fruit powder 150 g
These herbs collectively support nerve strength, myelin stability, muscular coordination, circulation, and antioxidant protection.
Avaleha Base Ingredients
Organic jaggery or raw sugar 1.2 kg
Cow ghee preferably A2 quality 300 g
Water 3.5 to 4 liters for decoction
Potent Classical Mineral Components
Abhrak Bhasma certified and properly prepared 15 g
Godanti Bhasma 10 g
Mukta Shukti Bhasma 10 g
Praval Pishti 10 g
Sphatik Bhasma 5 g
These minerals support nerve insulation, calcium metabolism, mitochondrial stability, and long term tissue nourishment when used correctly.
Step by Step Preparation Method
1st step: Preparation of herbal decoction
Take Dashamoola, Bala, Guduchi, Punarnava, Gokshura, and Amalaki coarse powders. Add them to 4 liters of water. Boil on low flame until the volume reduces to approximately 1 liter. Filter the decoction carefully and discard the residue. After filtering, add Yashtimadhu powder to preserve its potency.
2nd step: Avaleha base formation
Add jaggery to the filtered decoction and heat gently. Stir continuously on low flame until the mixture reaches Avaleha consistency. This stage is identified when the mixture becomes thick and forms a soft thread between fingers. Add cow ghee slowly while stirring to ensure uniform blending.
3rd step: Addition of Rasayana powders
Once the Avaleha base is ready, add Ashwagandha, Shatavari, Kapikacchu powders gradually while stirring continuously. Maintain low heat and ensure the mixture remains smooth and uniform.
4th step: Mineral incorporation
Allow the Avaleha to cool until it becomes lukewarm. Add Abhrak Bhasma, Godanti Bhasma, Mukta Shukti Bhasma, Praval Pishti, and Sphatik Bhasma. Mix thoroughly to ensure even distribution throughout the formulation.
5th step: Final consistency and storage
Once fully mixed, transfer the Avaleha into a clean glass or food grade container. Store in a cool and dry place away from direct sunlight. The preparation is suitable for use for approximately 30 to 45 days when stored properly.
Dosage and Method of Intake
Dosage is 15 grams twice daily.
The Avaleha should be taken after meals with warm milk or warm water.
This preparation is intended for continuous use for 30 days, and in chronic neuropathy, longer duration is commonly required under guidance.
Why This Avaleha Is Considered Strong and Comprehensive
This formulation works at multiple levels. It nourishes Majja Dhatu, stabilizes aggravated Vata, improves digestion so nutrients reach nerve tissue, supports myelin and axonal repair, and counters oxidative stress involved in nerve degeneration. The combination of Rasayana herbs with classical mineral components provides sustained regenerative support rather than temporary symptom control.
What Patients Commonly Experience With Consistent Use
With regular intake, many patients notice gradual reduction in burning and tingling sensations, improved sleep quality, better muscle coordination, increased strength, and overall improvement in nerve function over time. Progress is typically steady rather than abrupt, reflecting true tissue level recovery.
Why Market Bought Avaleha Does Not Cure Neuropathy
A patient must not buy ready-made Avaleha from the market expecting it to cure neuropathy. Neuropathy is a complex, degenerative nerve disorder involving metabolism, immunity, digestion, circulation, constitution, and disease duration. Generic formulations are designed for mass use and cannot address these layers together. As a result, market products commonly fail and delay meaningful recovery.
Always Get Avaleha Prepared by an Ayurvedic Doctor Only
Avaleha must always be prepared, prescribed, and monitored by an Ayurvedic doctor only. Neuropathy treatment requires individualized evaluation of digestion, nerve type involved, disease stage, metabolic status, and associated disorders. Without physician assessment and supervision, even the strongest formulation cannot deliver consistent or lasting results.
Lack of Individualization in Market Formulations
Neuropathy varies widely between patients. Some have sensory involvement, others motor or autonomic, and many have mixed or small-fiber neuropathy. Early functional nerve irritation and long-standing axonal degeneration require very different therapeutic strategies. Market formulations do not differentiate between nerve types or disease stages, leading to poor outcomes.
Poor Raw Material Quality and Processing
Many commercial products use low-potency herbs, incorrect substitutes, or improperly processed ingredients. Avaleha preparation requires precise decoction ratios, controlled temperature, and correct timing of ingredient addition. Commercial shortcuts reduce bioavailability and destroy the Rasayana effect required for Majja Dhatu nourishment.
Ignoring Digestive Strength and Absorption
Digestive function plays a central role in nerve healing. If Agni is weak, medicines do not reach nerve tissue effectively. Neuropathy frequently coexists with bloating, acidity, or malabsorption. Market products do not assess or correct digestion, which significantly limits therapeutic response.
Incorrect or Absent Mineral Balance
Advanced neuropathy often requires properly prepared Bhasma and Pishti for nerve insulation, calcium metabolism, and mitochondrial support. Market formulations either exclude these components or use poorly prepared forms, reducing effectiveness and long-term benefit.
Non-Individualized Dosage and Duration
The same dosage is commonly advised for all patients, regardless of age, body constitution, disease chronicity, or coexisting illness. Neuropathy requires long-term, stage-appropriate dosing. Market products promote unrealistic expectations of rapid relief, leading patients to stop treatment prematurely.
Associated Diseases and Hidden Factors Remain Untreated
Neuropathy often coexists with diabetes, thyroid disorders, autoimmune disease, liver or kidney dysfunction, chronic inflammation, nutritional deficiency, long-term medication exposure, or hidden infections. If these contributors are not identified and corrected, nerve damage continues despite medicine intake.
Prakriti, Vata Subtype, and Srotas Are Not Assessed
Ayurveda emphasizes Prakriti and Vata subtype involvement in nerve disorders. A formulation suitable for one constitution may aggravate another. Neuropathy also involves obstruction of Rasavaha, Raktavaha, and Majjavaha Srotas. Market products do not evaluate these factors, preventing medicine from reaching nerve tissue effectively.
No Monitoring or Dose Adjustment
Neuropathy treatment requires observation and modification over time. Some patients need gradual dose escalation, others need reduction or formulation changes. Market products offer no follow-up or adjustment, causing treatment stagnation.
Why Doctor Supervised Avaleha Is Essential for Cure
Peripheral neuropathy cure depends on correcting root causes, restoring digestion, nourishing Majja Dhatu, clearing Srotas, and sustaining nerve regeneration over time. When Avaleha is prepared and supervised by an Ayurvedic doctor only, it functions as a regenerative therapy rather than a generic supplement. Without such supervision, even the strongest formulation is unlikely to produce lasting results.
Diet and Lifestyle in Nerve Healing
Why diet and lifestyle directly affect nerve recovery
A meaningful peripheral neuropathy cure cannot occur through medicine alone. Nerve tissue is highly sensitive to nutritional quality, metabolic balance, circulation, and daily habits. From both Ayurvedic and modern clinical perspectives, diet and lifestyle form the foundation on which nerve repair becomes possible. Without correcting these factors, even the most potent therapies produce limited or temporary results [13], [15].
For you as a patient, this means daily choices play a decisive role in how well nerves heal.
Diet that supports nerve nourishment
Nerve tissue requires steady nourishment to regenerate. A diet that is warm, freshly prepared, and easy to digest supports absorption and tissue repair. Foods rich in natural fats, minerals, and antioxidants help maintain myelin integrity and nerve signal transmission.
From a clinical standpoint, irregular eating, processed foods, excess sugar, and inflammatory oils worsen oxidative stress and impair microcirculation to nerves. For you, this often translates into worsening burning sensations, fatigue, and slower recovery [15].
Ayurveda emphasizes that food must match digestive strength. Overeating, fasting, or consuming incompatible foods weakens Agni and prevents nutrients from reaching Majja Dhatu, directly delaying nerve healing [13].
Role of digestion in nerve regeneration
Healthy digestion is central to nerve repair. When digestion is weak, even nutrient-rich food fails to nourish nerve tissue. Bloating, acidity, heaviness, or irregular bowel movements are signs that absorption is compromised.
From an Ayurvedic perspective, strengthening Agni ensures that nutrients reach deeper tissues. For you as a patient, improving digestion often leads to reduced nerve irritation and better response to therapy [13].
Lifestyle habits that promote nerve repair
Daily routine has a direct effect on nerve stability. Regular sleep, consistent meal timing, and gentle physical activity support nerve regeneration. Sleep is particularly important, as nerve repair mechanisms are most active during deep rest.
From a medical standpoint, sleep deprivation and chronic stress elevate inflammatory mediators and stress hormones that damage nerve tissue. For you, disturbed sleep often correlates with worsening nighttime pain and delayed recovery [15].
Managing stress and mental strain
Chronic stress aggravates nerve dysfunction by overstimulating the nervous system. Persistent anxiety, mental fatigue, and emotional strain increase Vata imbalance and interfere with nerve healing.
Ayurveda recognizes the mind as inseparable from nerve function. Simple stress-reducing practices such as breathing exercises, meditation, and maintaining emotional balance help stabilize nerve signaling. For you, stress regulation often improves pain tolerance and sleep quality [13].
Physical activity and circulation
Gentle, regular movement improves blood flow to nerves and prevents stiffness. Overexertion, sudden intense exercise, or prolonged inactivity can aggravate symptoms.
From a clinical perspective, balanced activity supports circulation without causing additional nerve strain. For you, consistency matters more than intensity [15].
Avoiding factors that damage nerves
Certain lifestyle habits actively interfere with nerve healing. Excessive alcohol intake, smoking, irregular sleep patterns, and prolonged exposure to cold environments aggravate nerve irritation and slow regeneration.
For you as a patient, reducing these factors creates a supportive internal environment for nerve repair and enhances the effectiveness of all therapies [13], [15].
How diet and lifestyle complete the healing process
Diet and lifestyle are not supportive measures alone. They are therapeutic tools that determine whether nerve regeneration is possible. When combined with appropriate treatment, they stabilize nerve function, reduce inflammation, and support long term recovery.
For you, this integrated approach transforms neuropathy care from symptom control to genuine healing. Peripheral neuropathy cure becomes achievable when daily habits consistently support nerve health alongside medical and Ayurvedic intervention [13], [15].
Clinical Observational Case Outcome
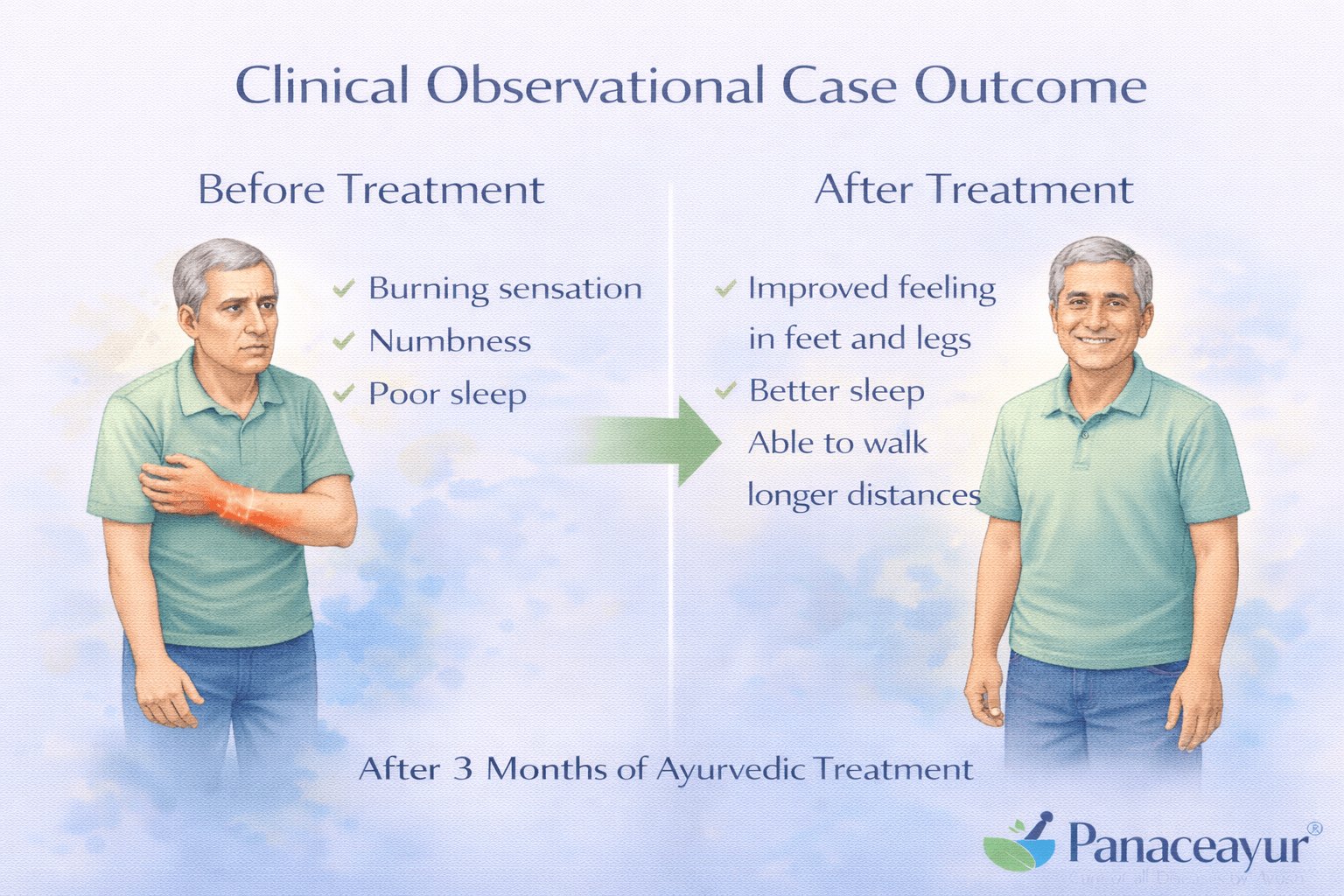
Background of the clinical case
This clinical observational outcome reflects real world patterns seen in patients with chronic peripheral neuropathy. The case represents a typical scenario in which neuropathy developed gradually over time and persisted despite conventional symptomatic treatment. The observations are based on documented clinical follow up and outcome assessment [15].
The patient had long standing symptoms of burning sensation in the feet, numbness, altered sensation, disturbed sleep, and intermittent weakness. These symptoms had been present for several years and were progressively worsening, particularly at night. Prior treatment focused mainly on pain suppressive medication, which provided temporary relief but did not halt progression.
Clinical assessment and baseline status
At the time of evaluation, the patient showed clear signs of sensory predominant neuropathy with early motor involvement. Clinical examination revealed reduced sensation in the distal lower limbs, impaired vibration sense, and mild weakness affecting balance and gait. Digestive symptoms such as bloating and irregular bowel habits were also present, indicating compromised absorption and metabolic stress.
From a clinical perspective, the neuropathy was assessed as chronic and degenerative rather than acute. Associated metabolic imbalance and long disease duration were identified as major contributors to delayed nerve recovery [15].
Therapeutic approach and observation period
The treatment strategy emphasized a regenerative approach rather than symptom suppression. The focus was placed on improving digestion, correcting metabolic imbalance, nourishing nerve tissue, and supporting long term nerve repair. Therapy was continued consistently over several months, with periodic clinical review and adjustment based on response.
Lifestyle and dietary correction were implemented alongside therapy to stabilize nerve function and reduce ongoing damage. The patient was advised to maintain regular sleep, avoid known nerve irritants, and follow a digestion supportive routine.
Observed clinical improvements
Over the observation period, gradual but meaningful changes were noted. Burning and tingling sensations reduced steadily, especially nighttime discomfort. Sleep quality improved, leading to better daytime energy and reduced fatigue. Sensory perception in the feet showed partial recovery, with improved temperature and touch awareness.
Motor stability also improved. The patient reported better balance while walking and reduced fear of falls. Muscle fatigue decreased, and overall functional confidence increased. These improvements were progressive rather than sudden, reflecting true tissue level recovery rather than temporary pain suppression [15].
Long term outcome and stability
With continued adherence to therapy and lifestyle measures, symptom stability was maintained. There was no rapid relapse after initial improvement, which is commonly seen when treatment focuses only on pain control. The slow, sustained nature of recovery suggested improvement in nerve environment and function rather than masking of symptoms.
From a clinical standpoint, this outcome supports the principle that chronic neuropathy can improve when underlying contributors are addressed and nerve nourishment is sustained over time [15].
Clinical significance for patients
For you as a patient, this observational outcome provides an important message. Neuropathy recovery is possible, even in long standing cases, when treatment targets digestion, metabolism, nerve nourishment, and lifestyle together. Improvement may not be immediate, but consistent progress over months reflects genuine healing.
This case highlights that peripheral neuropathy cure is not a rapid process. It is a gradual restoration of nerve health that requires patience, consistency, and a comprehensive approach. When these principles are followed, long term improvement and functional recovery become realistic goals [15].
Prognosis and Reversibility

How prognosis is determined in neuropathy
Prognosis in peripheral neuropathy depends on multiple interacting factors rather than a single variable. From a clinical perspective, outcome is influenced by the type of nerve damage, duration of disease, underlying causes, associated systemic conditions, and consistency of treatment. Understanding these elements helps set realistic expectations for recovery [14], [15].
For you as a patient, prognosis is not fixed. It can improve significantly when underlying contributors are identified early and addressed appropriately.
Role of disease duration in reversibility
The length of time neuropathy has been present plays a critical role in reversibility. Early stage neuropathy, where functional nerve disturbance predominates, has a better prognosis. At this stage, nerve fibers may be irritated but not structurally destroyed. With timely intervention, nerve function can recover meaningfully [15].
In long standing neuropathy, where axonal degeneration and myelin loss have occurred, recovery is slower and often partial. However, even in chronic cases, stabilization and functional improvement are achievable when treatment supports nerve nourishment and prevents further damage [14].
Impact of underlying causes and associated diseases
Prognosis is closely linked to whether the underlying cause of neuropathy can be corrected. Neuropathy driven by metabolic imbalance, nutritional deficiency, or inflammatory stress often shows better improvement once these factors are controlled. In contrast, ongoing exposure to toxins, uncontrolled systemic disease, or persistent inflammation worsens outcomes [14].
For you, this highlights the importance of treating associated conditions such as diabetes, thyroid disorders, autoimmune disease, and chronic organ dysfunction alongside neuropathy itself.
Nerve type and pattern of involvement
The type of nerve fibers involved also influences prognosis. Sensory predominant neuropathy often shows better symptom improvement than severe motor or autonomic involvement. Small fiber neuropathy may respond earlier to therapy, even when standard tests appear normal, while advanced motor involvement may require longer recovery periods [15].
From the clinician’s perspective, mixed neuropathy patterns require a more prolonged and carefully monitored approach.
Importance of consistency and long term care
Nerve regeneration is inherently slow. Prognosis improves when therapy is consistent and sustained over months rather than weeks. Intermittent treatment or early discontinuation often leads to relapse or stagnation.
For you as a patient, patience is essential. Improvement typically occurs gradually, with small but cumulative gains over time. This pattern reflects true nerve healing rather than temporary symptom relief [15].
Possibility of reversal versus stabilization
Reversibility in neuropathy exists on a spectrum. In early and moderate stages, significant reversal of symptoms and function is possible. In advanced stages, complete reversal may not always occur, but meaningful stabilization and prevention of further deterioration are realistic and valuable goals [14].
From a medical standpoint, preventing progression is itself a major success, as unchecked neuropathy often leads to disability and complications.
What prognosis means for patients
For you, prognosis should be understood as a dynamic process rather than a fixed outcome. Peripheral neuropathy cure is more achievable when treatment addresses root causes, supports nerve repair, and is maintained consistently. Even when full reversal is not possible, improvement in quality of life, function, and symptom control reflects genuine therapeutic success [14], [15].
This understanding helps patients remain engaged in long term care and avoid discouragement caused by unrealistic expectations.
Long-Term Complications if Untreated
Why untreated neuropathy continues to worsen
When neuropathy is left untreated or managed only with temporary symptom suppression, nerve damage does not remain static. From a clinical standpoint, untreated neuropathy is a progressive disorder. Ongoing metabolic stress, inflammation, impaired circulation, and nutritional deficiency continue to damage nerve fibers over time [8], [14].
For you as a patient, this means that ignoring early symptoms or relying only on pain relief allows deeper nerve degeneration to develop silently.
Progressive loss of sensation and protective reflexes
One of the most serious long-term complications of untreated neuropathy is progressive sensory loss. As nerve fibers deteriorate, the ability to feel pain, temperature, and pressure diminishes. This loss of protective sensation increases the risk of unnoticed injuries, burns, cuts, and infections, particularly in the feet [8].
From a medical perspective, loss of sensation significantly raises the risk of chronic wounds and delayed healing. For you, minor injuries may go unnoticed until they become severe.
Chronic pain and nervous system sensitization
In some patients, untreated neuropathy leads to chronic, severe pain rather than numbness. Persistent nerve irritation can sensitize the nervous system, making pain signals exaggerated and difficult to control. Over time, pain may become constant and resistant to medication [8].
For you, this can severely disrupt sleep, mood, and daily functioning, leading to reduced quality of life.
Muscle weakness, imbalance, and mobility loss
As motor nerves become involved, untreated neuropathy leads to progressive muscle weakness and wasting. Gait becomes unstable, balance deteriorates, and the risk of falls increases. Over time, walking may become difficult without support [14].
From a clinical standpoint, loss of mobility is a major contributor to disability in advanced neuropathy. For you, reduced independence often leads to social withdrawal and reduced physical activity, further worsening nerve health.
Autonomic dysfunction and organ involvement
Untreated neuropathy can extend beyond sensory and motor nerves to involve autonomic nerves. This can disrupt digestion, bowel movements, bladder control, heart rate regulation, blood pressure stability, and sexual function [14].
For you as a patient, these symptoms may appear unrelated to nerve disease, yet they reflect widespread nervous system involvement and significantly complicate overall health.
Increased risk of infections and secondary complications
Loss of sensation and poor circulation increase susceptibility to infections. Minor wounds can become chronic ulcers. In severe cases, repeated infections and tissue damage may lead to long-term complications requiring extensive medical intervention [8].
From a medical perspective, these complications are preventable when neuropathy is addressed early and comprehensively.
Psychological and emotional consequences
Chronic untreated neuropathy often leads to emotional distress. Persistent pain, functional decline, sleep disruption, and fear of worsening symptoms contribute to anxiety, low mood, and reduced confidence. Over time, psychological stress further aggravates nerve dysfunction [14].
For you, this creates a cycle in which physical and emotional factors reinforce one another.
Why early and sustained treatment matters
From a clinical perspective, many long-term complications of neuropathy are preventable. Early recognition and sustained treatment can slow or halt progression, preserve nerve function, and maintain quality of life [8], [14].
For you as a patient, understanding these potential complications underscores the importance of timely intervention. Peripheral neuropathy cure or meaningful stabilization becomes far more achievable when treatment begins before irreversible nerve damage and systemic complications develop.
Prevention and Risk Reduction
Why prevention matters in neuropathy
Prevention plays a critical role in reducing the burden of neuropathy and improving long term outcomes. From a clinical perspective, neuropathy often develops silently over years before symptoms become obvious. Addressing risk factors early can delay onset, slow progression, or prevent nerve damage altogether [4], [15].
For you as a patient, prevention is not limited to avoiding disease. It is an active process of maintaining nerve health through metabolic balance, lifestyle discipline, and early intervention.
Controlling metabolic and systemic risk factors
Metabolic imbalance is one of the strongest drivers of neuropathy. Maintaining stable blood sugar levels, healthy body weight, and balanced lipid profiles significantly reduces nerve stress. Even mild metabolic disturbances can impair microcirculation and increase oxidative damage to nerve tissue [4].
For you, this means that managing prediabetes, insulin resistance, and metabolic syndrome early is as important as treating established disease. Regular monitoring and timely correction reduce the likelihood of nerve degeneration.
Supporting digestion and nutrient absorption
Adequate nerve nutrition depends on proper digestion and absorption. Poor digestion leads to micronutrient deficiency, oxidative stress, and reduced tissue repair capacity. Clinically, many neuropathy cases show digestive dysfunction long before nerve symptoms become prominent [15].
For you, maintaining regular meals, avoiding incompatible foods, and addressing digestive symptoms early supports nerve resilience and lowers long term risk.
Reducing chronic inflammation and toxic exposure
Chronic low grade inflammation weakens nerve tissue over time. Inflammatory diets, excessive alcohol intake, smoking, and long term exposure to environmental toxins increase the risk of nerve damage [4].
From a preventive standpoint, reducing these exposures protects nerve fibers and preserves mitochondrial function. For you, lifestyle choices directly influence nerve longevity.
Early identification and management of associated diseases
Neuropathy frequently develops alongside conditions such as thyroid disorders, autoimmune disease, kidney or liver dysfunction, and chronic inflammatory states. Early diagnosis and management of these conditions significantly reduce nerve injury [15].
For you, this highlights the importance of comprehensive health evaluation rather than focusing only on symptoms.
Maintaining physical activity and circulation
Regular, moderate physical activity supports blood flow to peripheral nerves and maintains muscle tone. Prolonged inactivity worsens circulation and accelerates nerve degeneration. Conversely, excessive or sudden exertion may aggravate nerve irritation.
For you, consistent gentle movement supports nerve health and reduces long term risk [4].
Managing stress and sleep quality
Chronic stress and poor sleep increase neuroendocrine strain and inflammatory mediators that damage nerve tissue. Clinically, stress related nerve dysfunction is increasingly recognized as a contributing factor in neuropathy [15].
For you, prioritizing sleep and emotional balance is a protective measure rather than a secondary concern.
Value of early intervention and monitoring
From a clinical standpoint, the most effective prevention strategy is early recognition of warning signs such as intermittent tingling, burning, or altered sensation. Addressing these signs promptly prevents progression to irreversible nerve damage [4], [15].
For you as a patient, prevention and risk reduction are ongoing processes. Peripheral neuropathy cure or long term stability is far more achievable when risk factors are actively managed and nerve health is protected before advanced degeneration occurs.
Frequently Asked Questions (FAQs)
Can peripheral neuropathy be cured or only managed
Peripheral neuropathy can improve significantly and may become reversible when treatment addresses root causes early. When nerve dysfunction is mainly functional and structural damage is limited, recovery potential is higher. In long standing cases, complete reversal may not always occur, but meaningful improvement and long term stabilization are achievable with sustained, root cause oriented care
Why do neuropathy symptoms worsen at night
Symptoms often intensify at night due to reduced circulation, lower external sensory input, and increased nerve sensitivity during rest. Damaged nerves misfire more noticeably in quiet conditions, which explains nighttime burning and tingling without indicating sudden disease progression
Can neuropathy exist even if all tests are normal
Yes. Early stage or small fiber neuropathy may not appear on routine blood tests or nerve conduction studies. Clinical symptoms and examination often provide stronger diagnostic clues than tests alone, especially in early disease
Is peripheral neuropathy always caused by diabetes
No. While diabetes is common, neuropathy frequently occurs due to metabolic imbalance, immune dysfunction, nutritional deficiency, chronic inflammation, organ disease, or medication related toxicity. Many patients develop neuropathy before diabetes is diagnosed or without diabetes at all
Can neuropathy worsen even when pain is controlled
Yes. Pain relief does not equal nerve healing. Many medications suppress symptoms while underlying nerve degeneration continues. Long term improvement depends on correcting the biological causes of nerve damage rather than pain suppression alone
How long does it take for nerves to recover
Nerve regeneration is slow. Early symptom relief may appear within weeks, but meaningful recovery usually requires months. The timeline depends on disease duration, nerve type involved, associated conditions, and treatment consistency
How important are diet and lifestyle in nerve healing
Diet and lifestyle are critical. Proper digestion, balanced nutrition, adequate sleep, stress regulation, and consistent routine directly influence nerve repair capacity. Without lifestyle correction, medicines alone rarely produce lasting results
Why are many neuropathy cases labeled idiopathic
The term idiopathic often reflects incomplete evaluation rather than absence of cause. Many neuropathies are linked to subtle metabolic, immune, inflammatory, or toxic factors that routine testing may miss
Can untreated neuropathy become dangerous
Yes. If ignored, neuropathy can progress to severe sensory loss, chronic pain, muscle weakness, balance problems, autonomic dysfunction, infections, and long term disability. Early and sustained treatment greatly reduces these risks
Does age alone cause peripheral neuropathy
Age itself does not cause neuropathy. However, age related metabolic decline, reduced circulation, and higher disease burden increase vulnerability. With timely intervention, nerve function can still improve at any age
What is the single most important factor for long term improvement
Consistency. Sustained treatment, lifestyle correction, and regular monitoring determine outcomes. Peripheral neuropathy cure or long term stabilization is far more achievable when therapy is continued patiently and adjusted over time rather than stopped prematurely
Reference
(Definition, Nervous System, Pathophysiology of Neuropathy)
[1]England, J. D., Gronseth, G. S., Franklin, G., et al. (2009).
Practice parameter: Evaluation of distal symmetric polyneuropathy.
Neurology, 72(2), 177–184.
https://pubmed.ncbi.nlm.nih.gov/19056666
[2] Callaghan, B. C., Cheng, H. T., Stables, C. L., Smith, A. L., & Feldman, E. L. (2012).
Diabetic neuropathy: Clinical manifestations and current treatments.
The Lancet Neurology, 11(6), 521–534.
https://pubmed.ncbi.nlm.nih.gov/22608666
[3] Vincent, A. M., Callaghan, B. C., Smith, A. L., & Feldman, E. L. (2011).
Diabetic neuropathy: Cellular mechanisms as therapeutic targets.
Nature Reviews Neurology, 7(10), 573–583.
https://pubmed.ncbi.nlm.nih.gov/21912405
(Types, Causes, Common & Rare Associated Diseases)
[4] Hanewinckel, R., van Oijen, M., Ikram, M. A., & van Doorn, P. A. (2016).
The epidemiology and risk factors of chronic polyneuropathy.
European Journal of Epidemiology, 31(1), 5–20.
https://pubmed.ncbi.nlm.nih.gov/26463173
[5] Zis, P., Julian, T., Hadjivassiliou, M. (2018).
Treatment of autoimmune neuropathies.
Current Treatment Options in Neurology, 20(12), 51.
https://pubmed.ncbi.nlm.nih.gov/30390158
[6] Krarup, C. (2003).
Electrophysiology of demyelinating neuropathies.
Muscle & Nerve, 27(4), 461–476.
https://pubmed.ncbi.nlm.nih.gov/12661045
[7] Latov, N. (2014).
Diagnosis and treatment of chronic acquired demyelinating polyneuropathies.
Nature Reviews Neurology, 10(8), 435–446.
https://pubmed.ncbi.nlm.nih.gov/24985074
(Clinical Symptoms & Red Flags)
[8] Barohn, R. J. (1998).
Approach to peripheral neuropathy and neuronopathy.
Seminars in Neurology, 18(1), 7–18.
https://pubmed.ncbi.nlm.nih.gov/9565739
(Diagnosis & Why Conventional Treatment Fails)
[9] Finnerup, N. B., Attal, N., Haroutounian, S., et al. (2015).
Pharmacotherapy for neuropathic pain in adults.
The Lancet Neurology, 14(2), 162–173.
https://pubmed.ncbi.nlm.nih.gov/25575710
[10] Moore, R. A., Straube, S., Wiffen, P. J., Derry, S., & McQuay, H. J. (2009).
Pregabalin for acute and chronic pain in adults.
Cochrane Database of Systematic Reviews, CD007076.
https://pubmed.ncbi.nlm.nih.gov/19821378
(Ayurvedic Understanding, Rasayana, Avaleha, Diet & Lifestyle)
[11] Charaka Samhita, Chikitsa Sthana.
Vatavyadhi Chikitsa Adhyaya.
Chaukhambha Bharati Academy, Varanasi.
(Classical reference)
[12] Ashtanga Hridaya, Uttara Sthana.
Vatavyadhi Pratishedha Adhyaya.
Chaukhambha Sanskrit Pratishthan, Delhi.
(Classical reference)
[13] Govindarajan, R., Vijayakumar, M., & Pushpangadan, P. (2005).
Antioxidant approach to disease management and the role of Rasayana herbs.
Journal of Ethnopharmacology, 99(2), 165–178.
https://pubmed.ncbi.nlm.nih.gov/15894123
(Case Observation, Prognosis, Complications, Prevention)
[14] Said, G. (2007).
Chronic inflammatory demyelinating polyneuropathy.
Neuromuscular Disorders, 17(6), 491–502.
https://pubmed.ncbi.nlm.nih.gov/17481850
[15] Tesfaye, S., Selvarajah, D., Gandhi, R., et al. (2016).
Diabetic peripheral neuropathy may not be as its name suggests.
Pain, 157(S1), S72–S80.