- Major Risk Factors
- Early Symptoms to Watch For
- How Doctors Diagnose It
- Understanding Staging
- Treatment Options in Modern Medicine
- Ayurveda Cure for Penile Cancer
- Kanchanara Vrishya Rasayana Avaleha
- Kanchanara Vrishya Rasayana Avaleha – Main Medicine To Cure
- Preparation Method for Kanchanara Vrishya Rasayana Avaleha
- Frequently Asked Questions
- Reference
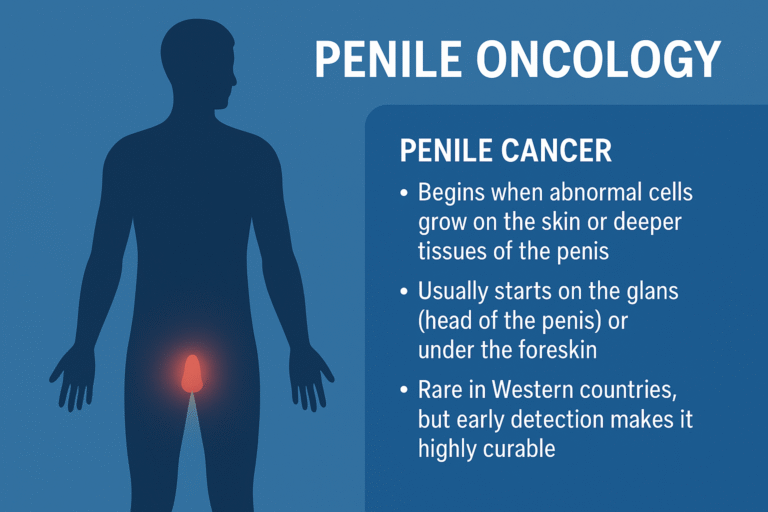
Penile cancer is a malignant disease in which the cells of the penis begin to grow in an uncontrolled, abnormal, and destructive manner. These abnormal cells usually start on the outer surface of the penis, because the skin and mucosal lining are the first areas exposed to irritation, infection, and inflammatory triggers. Most cases begin on the glans (the head of the penis) or underneath the foreskin, where moisture, HPV exposure, and chronic inflammation can create an environment that encourages cellular mutation and abnormal tissue behavior [12].
In Western countries, penile cancer is considered uncommon, but the rarity often leads to a false sense of security. Many men ignore early changes, assuming they are due to irritation, fungal infections, or minor injuries. However, the very first signs are usually visible, which means penile cancer is one of the most easily detectable cancers when a patient seeks medical attention early. Research across Europe and North America shows that early-stage penile cancer has a very high cure rate when treated promptly, with excellent outcomes and organ-preserving options available in most cases [1].
From a biological standpoint, penile cancer almost always begins in the surface layers of the skin, where chronic inflammation, HPV-induced DNA changes, or persistent irritation can gradually transform normal cells into precancerous lesions. If not treated, the abnormal cells start to invade deeper layers such as connective tissue, nerves, and lymphatic vessels. This deeper invasion increases the chance of spread to the inguinal lymph nodes, which is why any persistent lesion on the penis must be examined without delay [10].
Studies on patient presentation patterns show that many men wait several months before seeking help due to fear, embarrassment, or misinterpretation of symptoms. This delay is one of the biggest reasons the disease progresses to more complex stages. When patients are educated and perform simple self examinations, looking for any non healing sore, thickened patch, or unusual growth the diagnosis is often made early, and the treatment is straightforward with a high success rate [11].
Major Risk Factors
Penile cancer develops gradually, often after years of chronic irritation, viral influence, or long-standing inflammatory changes in the genital tissues. Although it is rare in Western countries, researchers consistently emphasize that most risk factors are highly preventable. Understanding these risks empowers patients to take early measures, protect their health, and recognize changes before they become serious.
Human Papillomavirus (HPV) [6] [2] [7]
HPV is one of the most significant contributors to penile cancer worldwide. High-risk strains—especially HPV-16 and HPV-18—can insert their genetic material into penile skin cells and disrupt natural DNA repair mechanisms. This disruption does not happen suddenly; it occurs over many years of silent infection. Many men do not have any noticeable symptoms during early HPV exposure, which makes the infection persist quietly under the foreskin or around the glans. Modern epidemiological studies show that a large percentage of penile cancer cases test positive for high-risk HPV DNA. The virus gradually changes the behavior of the cells, making them more vulnerable to turning cancerous, especially when combined with other irritants like smoking or chronic inflammation.
Poor Genital Hygiene [4] [3]
Good hygiene is one of the simplest and strongest protective factors. When the penis is not cleaned regularly—particularly in uncircumcised men—sweat, smegma, dead skin cells, and bacteria accumulate under the foreskin. This buildup irritates the delicate mucosal surface, causing repeated episodes of inflammation. Over time, chronic inflammation triggers cell damage, weakens local immunity, and increases the likelihood of cellular mutations. Multiple international reviews highlight that poor hygiene is strongly associated with penile cancer, and improving hygiene habits significantly lowers long-term risk. This is completely preventable and requires only consistent daily cleaning.
Phimosis (Tight Foreskin) [12] [1]
Phimosis is a condition in which the foreskin cannot be fully retracted. When this occurs, it becomes nearly impossible to clean the area properly. As a result, sweat and debris remain trapped inside, creating a warm and moist environment where irritation becomes constant. Numerous clinical studies show a sharply higher rate of penile cancer in men with untreated phimosis because the foreskin acts like a sealed chamber for inflammation. Men with phimosis often experience redness, infection, or white patches, all of which increase cellular stress. When phimosis is left untreated for years, the risk magnifies further, making early evaluation extremely important.
Smoking [8] [19]
Smoking introduces carcinogenic chemicals into the bloodstream, many of which accumulate in genital tissues. These toxins damage the DNA inside penile skin cells and weaken the immune system’s ability to fight off viral infections such as HPV. Tobacco exposure also reduces blood flow, interferes with oxygen delivery, and impairs the natural healing capacity of the skin. This combination of DNA damage and weakened local immunity creates a fertile environment for cancer to develop. Studies show that smokers are significantly more likely to develop penile cancer than non-smokers, and this risk increases with duration and intensity of smoking.
Chronic Inflammatory Skin Conditions [11] [10]
Certain long-standing skin disorders dramatically increase risk because they keep the penile tissues in a state of chronic irritation. Lichen sclerosus and balanitis xerotica obliterans are two of the most notable examples. These conditions cause persistent redness, thickening, scarring, and tightening of the foreskin or surrounding tissues. When inflammation becomes a daily occurrence, the cells are constantly trying to repair themselves, making them more prone to errors during regeneration. These repeated cycles of damage and healing create the perfect setting for abnormal or precancerous changes. Several pathology studies confirm that men with these conditions face a substantially higher long-term risk of developing penile cancer if the disease is not managed early.
Early Symptoms to Watch For
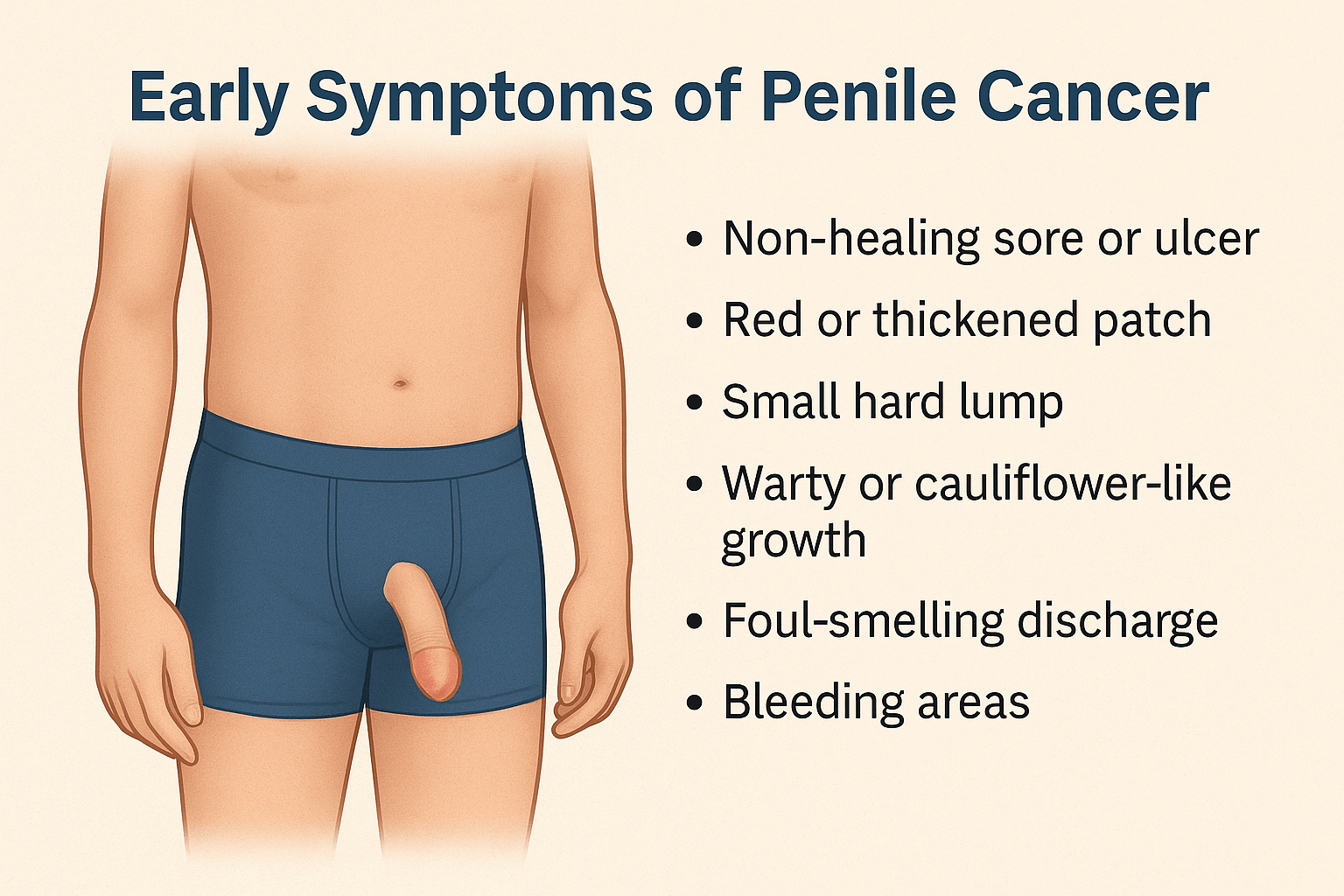
Non Healing Sore or Ulcer
A non healing sore or ulcer is one of the earliest signs of penile cancer and often appears as a small raw patch that refuses to close even after several weeks. It may look like an open wound, a crusted surface, or a shallow ulcer that continues to ooze fluid. Some ulcers form a thin scab which repeatedly breaks open. These sores are usually painless, which makes them easy to ignore. When a sore does not respond to routine cleaning or simple treatment, it may reflect early abnormal changes in the surface cells of the penis and requires immediate medical evaluation.
Red or Thickened Patch
A persistent red or thickened patch is another important symptom. This may appear as a bright red area, a velvety red surface, or a slightly raised patch that feels irritated or unusually smooth. It can also present as a scaly or shiny area on the glans or under the foreskin. Many men mistake this for fungal infection, psoriasis, or irritation from soaps. When such a patch remains unchanged for several weeks or becomes progressively more noticeable, it may indicate the beginning of precancerous transformation in the tissue.
Small Hard Lump
A small hard lump may form on the surface or underneath the skin of the penis. This lump usually feels firm and anchored rather than soft or movable. It may start as a tiny nodule and slowly increase in size over time. Unlike normal cysts or clogged glands, which often feel soft or tender, cancerous lumps tend to be firm and persistent without causing pain. This firmness comes from abnormal cell buildup, and any such lump should be checked promptly.
Warty or Cauliflower Like Growth
Some patients develop growths that resemble genital warts, but these tend to have a thicker texture, irregular edges, and a more aggressive pattern of enlargement. These growths may bleed slightly when touched or during cleaning. Because HPV infections are common, many men assume such growths are harmless. However, when the surface appears rough, uneven, or rapidly enlarging, it may represent early malignant change rather than a simple wart.
Foul Smelling Discharge
A foul smelling discharge can be a sign of underlying tissue breakdown or infection associated with early cancerous change. This discharge may collect under the foreskin and produce an unpleasant odor that persists even after cleaning. While some discharge can occur with common infections, a persistent odor combined with redness or irritation suggests that deeper tissue changes may be occurring and needs medical assessment.
Bleeding Areas
Small bleeding spots can appear on the glans, on the foreskin, or around a lesion. These areas may bleed during cleaning, during sexual activity, or even without any contact. Bleeding happens because the surface of cancerous tissue is fragile and breaks easily. Even slight bleeding in the absence of injury is an important warning sign that should not be ignored.
Swelling of Groin Lymph Nodes
Swelling of the lymph nodes in the groin may develop when the body reacts to abnormal changes occurring in the penile tissue. These swollen nodes usually feel like firm, round lumps and are typically painless. They may also increase in size gradually. Although lymph node swelling can occur from infections, persistent swelling may indicate early spread of abnormal cells.
Rare and Rarest Symptoms
Certain symptoms appear less frequently but still carry significant importance. Some men develop unexplained groin or pelvic discomfort when deeper tissue involvement begins. Others notice unusual color changes such as bluish or purplish patches that look like bruises without any injury. A gradual tightening of the foreskin may occur even in men who previously had no foreskin problems, caused by scarring linked to deeper lesions. Persistent itching or burning in a specific part of the penis can also be an early indication of irritation from abnormal cell activity. In rare cases, a watery or slightly blood stained fluid may accumulate under the foreskin. Very advanced cases may present with unexplained fatigue or weight loss.
Since most early changes are painless, men often overlook them or assume they are related to common skin conditions. Careful visual inspection is essential, especially for uncircumcised men. Any persistent change in appearance, texture, color, swelling, or sensation requires professional evaluation for accurate diagnosis and early cure.
How Doctors Diagnose It

Physical Examination
Diagnosis begins with a detailed physical examination performed by a urologist who carefully inspects the glans, the foreskin, and the shaft for any visible abnormalities [12] [1]. The doctor looks for ulcers, thickened patches, raised growths, color changes, or discharge. In uncircumcised men, the foreskin is gently retracted to view the entire glans, because many early lesions hide underneath. The doctor also palpates the groin region to evaluate whether the lymph nodes are enlarged, firm, or tender. This examination provides the first and often the most important clues about the presence and stage of disease.
Dermatoscopy and Magnification Tools
Dermatoscopy is a technique in which the doctor uses a handheld magnifying device with strong light to examine the lesion more closely [11]. This tool reveals important details such as the surface pattern, vascular visibility, pigmentation changes, and structural irregularities that are not visible to the naked eye. Subtle features like dotted blood vessels or irregular patterns may help distinguish cancerous lesions from benign conditions. The magnified view also allows the doctor to determine whether the lesion is superficial or showing deeper infiltration.
Biopsy for Confirming Diagnosis
A biopsy is the definitive step for confirming penile cancer [10]. The doctor takes a very small sample of tissue from the suspicious area. This procedure is usually done under local anesthesia to ensure comfort. The tissue is then examined under a microscope by a pathologist who identifies whether the cells show malignant changes, how deep the abnormal cells extend, and what specific type of cancer is present. A biopsy not only confirms the diagnosis but also guides further treatment decisions by revealing how aggressive the cancer is.
Imaging Studies to Evaluate Spread
After confirming the diagnosis, imaging studies help determine how far the disease has progressed [4] [3]. Ultrasound is often used to check whether the cancer has entered deeper tissues. Magnetic resonance imaging gives a detailed view of soft tissues and helps assess involvement of the corpus cavernosum and nearby structures. Computed tomography scans are used to evaluate whether lymph nodes in the groin or pelvis are enlarged or if there is any distant spread. These tests allow doctors to create an accurate staging plan which is essential for selecting the most effective treatment.
HPV Testing to Identify Viral Involvement
Many cases of penile cancer are associated with high risk strains of the human papillomavirus, especially HPV sixteen and eighteen [6] [7]. HPV testing can be done on tissue samples obtained during biopsy or molecular swabs. Identifying the presence of high risk HPV gives doctors a clearer understanding of the biological behavior of the tumor, because HPV related cancers often have distinct patterns. Recognizing HPV involvement also helps guide counseling about prevention and follow up.
Penile cancer diagnosis relies on a combination of careful visual assessment, microscopic confirmation, and imaging based staging. When all these elements are combined, doctors can determine the exact nature of the disease and provide a clear treatment plan tailored to each patient.
Understanding Staging
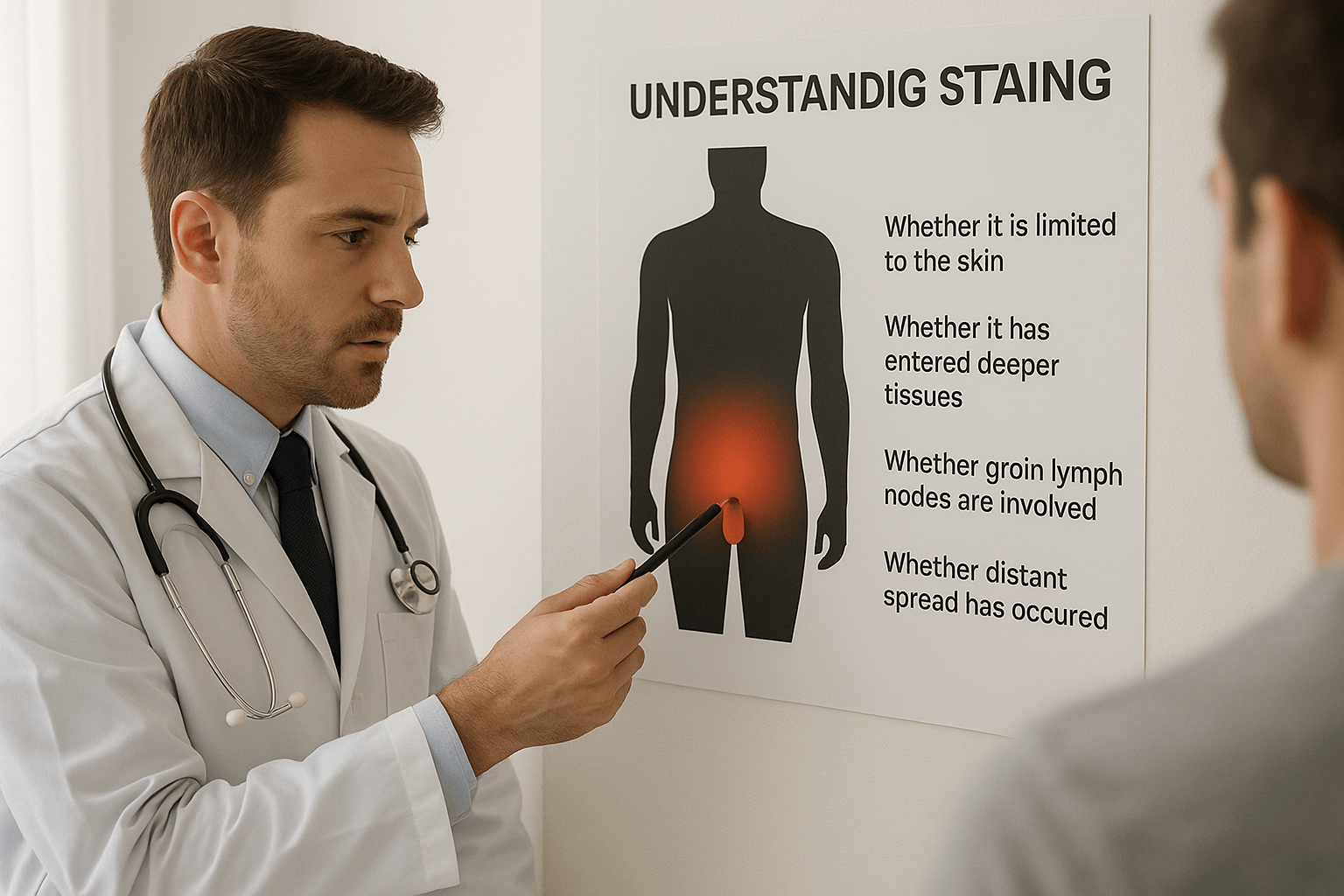
Why Staging Matters
Staging is the process doctors use to understand how far penile cancer has progressed inside the body. It helps determine whether the cancer is still limited to the surface skin, whether it has grown into the deeper tissues, whether the lymph nodes in the groin are involved, or whether it has travelled to distant organs. Staging is one of the most important steps because it directly shapes the treatment plan and predicts how well a patient will respond to therapy [3] [12]. Accurate staging allows doctors to choose the safest and most effective approach, ranging from simple surface treatment for early disease to more involved therapy for advanced cases.
Cancer Limited to the Skin
The earliest stage of penile cancer involves only the outer layers of the skin. At this stage, the abnormal cells remain confined to the surface and have not yet grown into the deeper tissues underneath [10]. This stage is often completely curable with organ preserving treatments when detected early. Patients may notice visible changes such as a sore, patch, or small growth, but the deeper structures remain intact. Identifying this stage correctly is crucial because treatment at this point is straightforward and highly successful.
Cancer Entering Deeper Tissues
As the disease progresses, cancer cells can begin moving into the deeper tissues of the penis such as the connective tissue or the erectile bodies. When this happens, the cancer becomes more serious and requires a more structured treatment approach [4]. This deeper invasion may not always be obvious externally, which is why ultrasound or magnetic resonance imaging is often used to evaluate the extent. Deeper involvement can influence whether organ sparing procedures are possible or whether more extensive intervention is needed.
Involvement of Groin Lymph Nodes
The lymph nodes in the groin are the first place where penile cancer may spread. These nodes act as filters for the immune system and can capture abnormal cells as the disease grows [1]. During staging, doctors examine these nodes carefully through physical examination and imaging. If the lymph nodes become enlarged or firm, further testing is performed to determine whether cancer has reached them. Lymph node involvement is an important marker because it indicates that the disease has begun to move beyond the primary site, and this affects both treatment planning and prognosis.
Distant Spread to Other Organs
In more advanced stages, penile cancer can travel through the bloodstream or lymphatic system to distant organs, most commonly the lungs or liver. This is called distant metastasis and represents the later stage of the disease [8]. Although this stage is less common, especially when patients seek early medical care, it remains an essential part of the staging system. When distant spread is present, treatment moves toward systemic approaches such as chemotherapy and immunotherapy, sometimes combined with targeted local procedures.
Accurate Staging Guides Treatment Decisions
Doctors depend heavily on accurate staging to choose the right treatment. Early stage disease may require only topical therapy, laser treatment, or a minor surgical procedure, while deeper or spreading disease needs more comprehensive strategies [14]. By understanding exactly how far the cancer has progressed, the medical team can create a personalized plan that balances effectiveness, safety, and quality of life.
Treatment Options in Modern Medicine
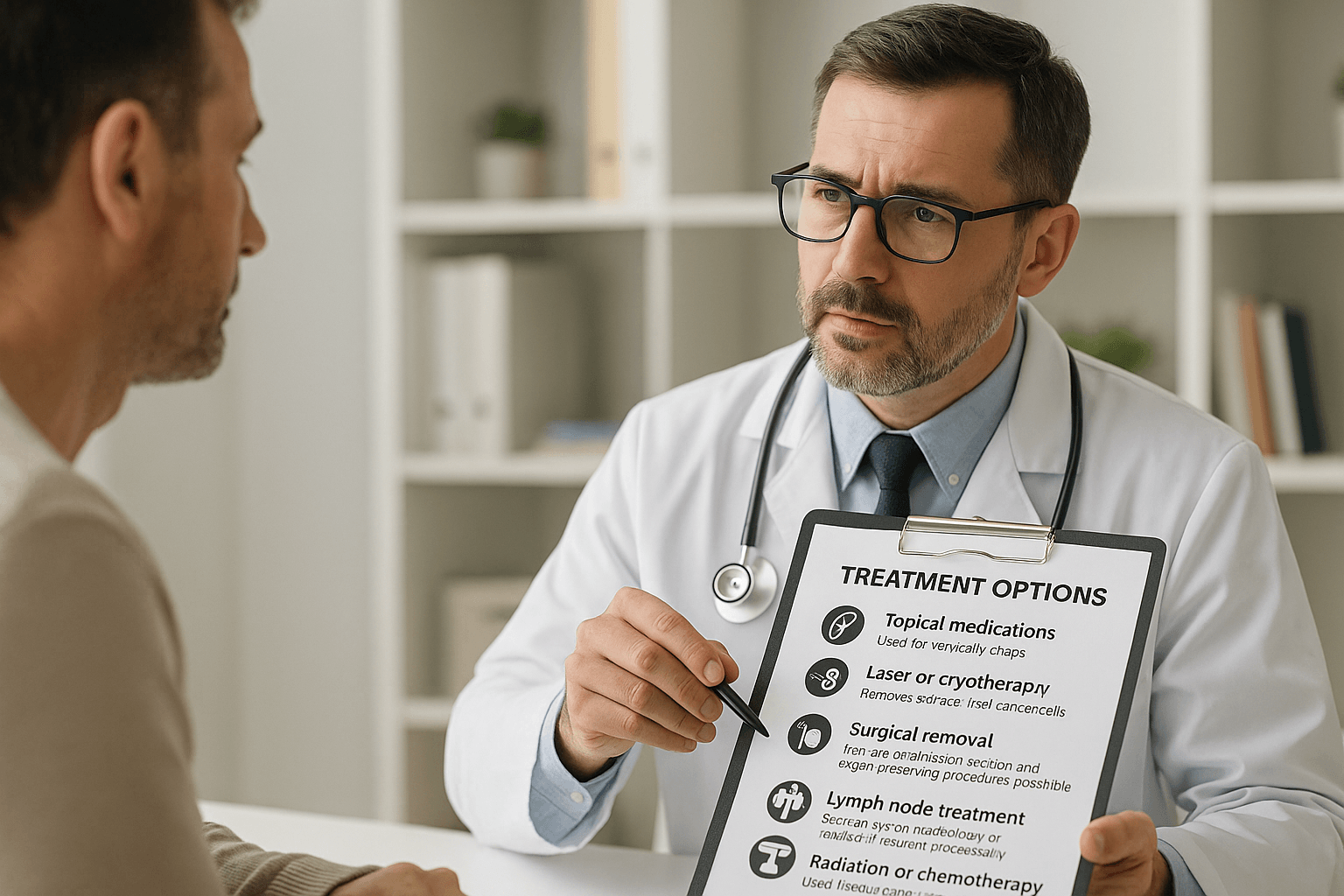
Topical Medications
Topical medications are used for the earliest and most superficial stages of penile cancer [13]. These medicines are applied directly to the lesion in the form of creams or ointments. They work by stimulating the immune system or destroying abnormal surface cells. Because they act locally, they are best suited for carcinoma in situ or very thin surface level disease. Regular follow up is required to ensure the lesion responds fully, and doctors monitor the area closely to confirm that deeper tissues remain unaffected.
Laser Therapy or Cryotherapy
Laser treatment and cryotherapy are minimally invasive methods used to remove abnormal surface tissue [15]. Laser therapy uses a focused beam of light to vaporize cancer cells with precision, while cryotherapy freezes and destroys the abnormal tissue through controlled cold exposure. Both techniques aim to preserve as much healthy tissue as possible. These treatments are especially helpful when the cancer is confined to the uppermost layers of the skin. They allow for quick recovery and maintain cosmetic and functional outcomes for the patient.
Surgical Removal of the Lesion
Surgery remains one of the most reliable treatments for penile cancer [14]. In early stages, the surgeon removes the lesion along with a small margin of surrounding healthy tissue. These procedures are designed to preserve the appearance and function of the penis whenever possible. In more extensive cases, a larger portion of tissue may need to be removed, but modern surgical techniques focus strongly on organ preservation. Early detection greatly increases the chance that surgery will be minimally invasive and have excellent long term results.
Lymph Node Assessment and Treatment
If there is concern that cancer may have spread beyond the penis, doctors evaluate the groin lymph nodes carefully [1]. A sentinel lymph node biopsy may be performed, which involves removing and testing the first lymph node likely to receive cancer cells. If cancer is found in this node or if several nodes appear abnormal, further removal may be recommended. Treating lymph nodes early is important because it prevents further spread and improves overall cure rates.
Radiation Therapy and Chemotherapy
Radiation therapy and chemotherapy are usually reserved for more advanced or aggressive stages of penile cancer [8]. Radiation uses targeted energy to destroy cancer cells in the penis or lymph nodes. Chemotherapy circulates through the bloodstream and kills cancer cells that may have spread to distant sites. These treatments may be used alone or in combination depending on the stage. In some cases, they are given before surgery to shrink a tumor or after surgery to reduce the chance of recurrence.
Modern treatment strategies aim to maintain both quality of life and long term survival. When penile cancer is detected early, many patients require only limited treatment with excellent outcomes. As the disease becomes more advanced, treatments become more comprehensive, but they remain highly structured and evidence based.
Ayurveda Cure for Penile Cancer
How Ayurveda Interprets Penile Cancer
Ayurveda views penile cancer as a deep seated disorder that develops when the body’s internal systems become disturbed over many years. The condition arises from long standing inflammation and impurities accumulating in Rakta Dhatu, which is the blood tissue responsible for nourishment and circulation. When Rakta Dhatu is disturbed, it creates an environment where abnormal tissue changes can begin. At the same time, the natural flow of nutrients through Mamsa and Majja Srotas, which are the channels that nourish the muscle tissue and the deeper marrow structures, becomes obstructed. This obstruction gradually weakens cellular communication and allows unhealthy cells to multiply. Another major factor is the reduction of Ojas, which is the essence of immunity that protects the body from disease. When Ojas becomes depleted due to chronic irritation, stress, previous infections such as HPV, or digestive weakness, the body loses its natural ability to correct unhealthy cell growth. Ayurveda therefore focuses not only on the cancerous lesion but also on correcting the deeper disturbances that allowed it to develop.
The Rasayana Approach and Root Correction
The classical Ayurvedic approach to cancer involves Rasayana therapy, which aims to rebuild damaged tissues, clear accumulated toxins, improve cellular intelligence, and restore the body’s capacity to heal. Rasayana is not simply a general immune booster. It is a structured method that promotes regeneration, strengthens resistance to disease, stabilizes metabolism, and restores normal cell behavior. In penile cancer, this approach focuses on reducing long term inflammation, cleaning the blood channels, correcting tissue level imbalances, and restoring the strength of Ojas so that the body can reverse the pathology at its source. By correcting these underlying imbalances, Ayurveda aims for complete and lasting recovery rather than temporary symptom management.
Kanchanara Vrishya Rasayana Avaleha
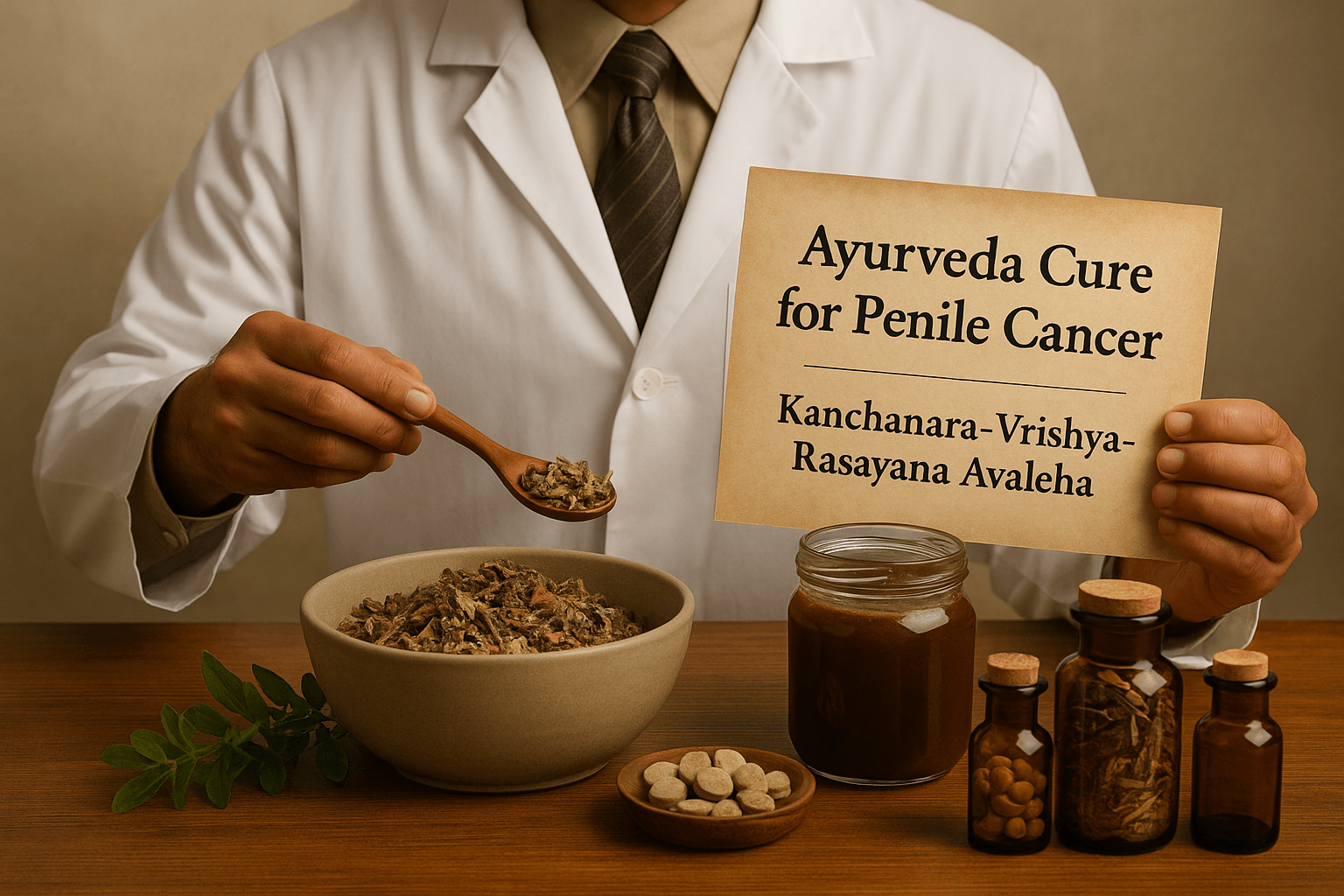
One of the most important formulations recommended in classical Rasayana chapters for abnormal growths and glandular enlargement is Kanchanara Vrishya Rasayana Avaleha. This preparation is a powerful herbal paste made from herbs known for their ability to purify the blood, break down unwanted tissue growth, support lymphatic drainage, and enhance reproductive and muscular tissue nutrition. It targets the exact tissues involved in penile cancer, including Rakta Dhatu, Mamsa Dhatu, Majja Dhatu, and the associated Srotas. Patients generally take fifteen grams twice daily under the guidance of a qualified Ayurvedic physician, and this dosage is adjusted depending on digestive strength and the stage of the condition.
How This Avaleha Helps in Penile Cancer
Kanchanara Vrishya Rasayana Avaleha helps reduce chronic inflammation in the penile tissues by clearing accumulated toxins and correcting the internal terrain that allowed the disease to form. It supports the natural regression of abnormal growth by improving tissue metabolism and restoring the intelligence of the affected cells. The formulation purifies Rakta Dhatu, preventing further mutation and strengthening the microcirculation that nourishes the penile structures. It enhances overall vitality, supports healthy immune function through the restoration of Ojas, and strengthens the deeper tissues, including Majja Dhatu, which plays a major role in long term healing. Over time, these actions work together to halt disease progression and encourage natural recovery.
Potent Mineral Preparations Added Under Supervision
In more serious cases, Ayurvedic doctors enhance the Avaleha by adding classical mineral preparations. These include Swarna Bhasma which supports immunity, cellular repair, and emotional stability, as well as Heerak Bhasma which is known for its ability to correct abnormal tissue growth at the deepest level. Abhrak Bhasma supports respiratory and tissue regeneration functions and strengthens Majja Dhatu. Godanti Bhasma helps reduce inflammation and heat in Rakta Dhatu, while Trivanga Bhasma helps improve reproductive tissue strength and correct long standing imbalances. These refined mineral preparations are extremely potent and require medical evaluation before use. They are chosen only after assessing the patient’s constitution, strength, digestive capacity, stage of cancer, and presence of infections such as HPV.
Why Individualization Is Essential in Ayurvedic Cancer Care
Ayurvedic cancer treatment cannot follow a one size fits all approach. Every patient’s formulation must be customized based on the stage of cancer, the presence of HPV or other viral infections, the patient’s age, existing inflammatory conditions, previous biopsies or surgeries, digestive strength, and the overall status of Ojas. Even emotional factors, sleep patterns, stress levels, and long term metabolic issues influence the exact combination of herbs and minerals required. Because of this, correct healing requires guidance from a trained Ayurvedic physician who understands how to balance all seven Dhatus, restore Agni, and re establish healthy tissue function. When done correctly, Ayurveda focuses on complete root cause reversal and long term restoration of health.
Ayurveda therefore provides a comprehensive system that not only addresses the lesion but heals the internal terrain in which the disease developed. With the right Rasayana approach, supportive minerals, and personalized formulation, complete recovery becomes possible in a structured and predictable manner.
Kanchanara Vrishya Rasayana Avaleha – Main Medicine To Cure
(Formulated for 15 g twice daily for 30 days)
This classical Rasayana blend is designed to support immune strength, lymphatic cleansing, healthy tissue regeneration, and long-standing inflammatory correction. The formulation below lists every herb with its botanical name for maximum scientific clarity.
1. Herbal Decoction Base (Kashaya Ingredients)
These herbs are boiled into a therapeutic decoction that forms the foundation of the Avaleha.
- Kanchanara Bark (Bauhinia variegata) – 350 g
- Varuna Bark (Crataeva nurvala) – 200 g
- Guduchi Stem (Tinospora cordifolia) – 200 g
- Triphala Coarse Mix (Terminalia chebula, Terminalia bellerica, Emblica officinalis) – 250 g
- Sariva White (Hemidesmus indicus) – 100 g
- Sariva Red (Cryptolepis buchanani) – 100 g
- Punarnava Root (Boerhavia diffusa) – 120 g
- Musta (Cyperus rotundus) – 80 g
- Vidanga (Embelia ribes) – 80 g
- Shigru Bark or Root (Moringa oleifera) – 100 g
- Kokilaksha (Asteracantha longifolia) – 60 g
- Neem Bark (Azadirachta indica) – 100 g
2. Fine Herbal Powders (Added After Decoction)
These herbs remain biochemically active and act as Rasayanas, adaptogens, and tissue-nourishing botanicals.
- Ashwagandha (Withania somnifera) – 150 g
- Shatavari (Asparagus racemosus) – 150 g
- Gokshura (Tribulus terrestris) – 100 g
- Manjistha (Rubia cordifolia) – 120 g
- Haridra (Curcuma longa) – 60 g
- Daruharidra (Berberis aristata) – 60 g
- Yashtimadhu (Glycyrrhiza glabra) – 120 g
- Brahmi (Bacopa monnieri) – 60 g
- Shankhapushpi (Convolvulus pluricaulis) – 60 g
- Jatamansi (Nardostachys jatamansi) – 40 g
- Guggulu (Purified) (Commiphora mukul resin, purified) – 80 g
- Triphala Fine Powder (T. chebula, T. bellerica, E. officinalis) – 120 g
- Pippali (Piper longum) – 40 g
- Trikatu (Zingiber officinale, Piper nigrum, Piper longum) – 40 g
- Chitrak Root (Plumbago zeylanica) – 40 g
- Neem Leaf Powder (Azadirachta indica) – 80 g
- Atibala (Abutilon indicum) – 60 g
3. Rasayana and Ojas-Enhancing Ingredients
- Amalaki (Emblica officinalis) – 120 g
- Giloy Satva (Tinospora cordifolia starch) – 35 g
- Bhringaraja (Eclipta alba) – 60 g
- Draksha Paste (Vitis vinifera) – 200 g
4. Base Sweetening Medium
- Jaggery (Guda) – 1.8 kg
This provides the Avaleha body and improves absorption.
5. Classical Ayurvedic Mineral Preparations
(Added only under professional supervision; dosage ranges are for a 30-day course.)
- Swarna Bhasma (Gold calx) – 300 to 600 mg
- Heerak Bhasma (Diamond calx) – 250 to 500 mg
- Rajata Bhasma (Silver calx) – 1 g
- Abhrak Bhasma (Shataputi) (Mica calx) – 2 g
- Godanti Bhasma (Gypsum/calcium sulfate) – 3 g
- Trivanga Bhasma (Traditional alloy of Vanga, Yashada, Naga) – 2 g
- Yashada Bhasma (Zinc calx) – 1 g
- Mukta Sukti Bhasma (Oyster shell calx) – 2 g
- Sphatika Bhasma (Potash alum) – 1 g
- Ras Sindoor (Purified arsenic compound in classical Rasashastra) – 600 mg
- Tal Sindoor (Mercurial–sulfur preparation) – 500 mg
6. Optional Personalized Additions
Selected based on Prakriti, staging, immunity level, and digestive strength.
- Shilajit (Asphaltum punjabinum) – 10 g
- Ghee (Cow’s ghee) – 60 ml
- Sesame Oil (Sesamum indicum) – 40 ml
- Honey (Madhu) – added only after cooling
7. Final Output
- Total Avaleha yield: 1.2 to 1.3 kg
- Required for a 30-day dose: 900 g
This ensures proper Rasayana potency and stable texture throughout the month.
Preparation Method for Kanchanara Vrishya Rasayana Avaleha

Step 1: Making the Herbal Decoction (Kashaya)
- Take all the coarse herbs listed in the decoction base (Kanchanara, Varuna, Guduchi, Triphala, Sariva, Punarnava, Musta, Vidanga, Shigru, Kokilaksha, Neem).
- Wash lightly to remove dust and impurities.
- Place them in a large stainless-steel vessel.
- Add 7 litres of clean water.
- Bring to a boil on medium flame.
- Continue boiling until the volume reduces to approximately 1 litre.
- Strain the decoction through a fine cloth or filter.
- Keep this concentrated decoction aside.
This forms the therapeutic base of the Avaleha.
Step 2: Preparing the Jaggery Syrup (Guda Paka)
- Take 1.8 kg jaggery and break it into small pieces.
- Melt it slowly in a separate thick-bottom vessel.
- Heat on low to medium flame until it dissolves completely.
- Continue heating until it reaches a thread-like consistency when tested between the fingers.
This ensures the Avaleha will not spoil and will maintain proper texture.
Step 3: Combining Decoction and Syrup
- Once the jaggery syrup reaches the correct stage, slowly pour the 1 litre decoction into the syrup.
- Stir continuously to avoid sticking.
- Cook on low flame.
- Allow the mixture to thicken gradually until it reaches a semi-solid paste-like stage.
This slow cooking step ensures complete integration of herbal actives.
Step 4: Adding Powdered Herbs (Churna Kalpana)
- Turn off the flame before adding powders.
- Add all fine herbs listed earlier (Ashwagandha, Shatavari, Gokshura, Manjistha, Haridra, Daruharidra, Yashtimadhu, Brahmi, Shankhapushpi, Jatamansi, Guggulu, Triphala, Pippali, Trikatu, Chitrak, Neem leaf powder, Atibala).
- Mix thoroughly so that the paste becomes smooth without lumps.
- Add Draksha paste, Amalaki, Giloy Satva, and Bhringraj at this stage.
- Rasayana consistency should be neither too thick nor too runny.
Step 5: Adding Classical Mineral Preparations (Bhasmas)
(ONLY under Ayurvedic physician supervision)
When the mixture has cooled to a warm (not hot) temperature:
- Add the prescribed micro-doses of Swarna Bhasma, Heerak Bhasma, Rajata Bhasma, Abhrak Bhasma, Godanti, Trivanga, Yashada, Mukta Sukti, Sphatika, Ras Sindoor, and Tal Sindoor.
- Mix thoroughly so that they distribute evenly throughout the Avaleha.
These minerals enhance Rasayana, immune, and tissue-corrective effects.
Step 6: Optional Personalized Additions
Depending on the patient’s body type and strength:
- Add a small quantity of ghee for Vata or Pitta types.
- Add sesame oil for Kapha types.
- Add Shilajit only if prescribed.
- Add honey ONLY after complete cooling and in very small amount.
Step 7: Cooling and Storage
- Allow the Avaleha to cool naturally to room temperature.
- Transfer it into clean, airtight glass jars.
- Store in a cool, dry place away from moisture and sunlight.
- Shelf-life is best maintained when stored in airtight containers.
Daily Dosage for 30 Days
15 g in the morning + 15 g in the evening, taken with warm water on an empty stomach.
Dosage may be adjusted slightly based on digestion and overall strength.
Frequently Asked Questions
What causes penile cancer in most men
Penile cancer usually develops due to long-standing inflammation, poor genital hygiene, chronic infection with high-risk HPV strains, smoking-related immune suppression, and conditions such as phimosis that prevent proper cleaning. Over time, these factors irritate the penile skin and create an environment where abnormal cells begin to grow.
Is penile cancer common in Western countries
Penile cancer is rare in most Western countries, but its early signs are often overlooked. Because it begins as a mild skin change that may not cause pain, men frequently delay medical evaluation. Early detection is extremely important because it makes treatment simpler and preserves normal function.
What are the earliest signs I should look for
Common early symptoms include a non-healing sore, a reddish patch, thickened skin, a firm lump, discharge, or bleeding. Some men also notice swelling in the groin. Many of these symptoms are painless, so regularly checking the area is important.
How do doctors diagnose penile cancer
Diagnosis usually involves a physical examination, dermatoscopy, a small biopsy of the affected skin, and imaging studies such as ultrasound or MRI if deeper involvement is suspected. These steps help determine the exact stage of the condition and guide treatment planning.
Can HPV infection increase my risk
High-risk strains of HPV, particularly types sixteen and eighteen, are strongly linked to penile cancer. They cause cellular changes in the skin that can progress over time. HPV testing is not always done routinely in men, but it may be recommended if the clinical picture suggests viral involvement.
Is treatment always surgical
Not always. Early stages may be treated with topical medicines, laser therapy, or minimally invasive methods. Surgery is recommended when deeper tissues are involved, but modern techniques aim to preserve normal appearance and sexual function as much as possible.
How effective is Ayurveda for penile cancer
Ayurveda approaches penile cancer by correcting the deeper imbalances that allowed abnormal cells to grow. It focuses on reducing chronic inflammation, purifying Rakta Dhatu, strengthening Mamsa and Majja tissues, improving immunity, and restoring Ojas. Classical formulations such as Kanchanara Vrishya Rasayana Avaleha, supported by minerals like Swarna Bhasma and Abhrak Bhasma when needed, are used to promote natural regression of unhealthy tissue under the guidance of an Ayurvedic physician.
Is Ayurvedic treatment safe
When taken under the supervision of a qualified Ayurvedic doctor, treatment is safe and personalized. Ayurvedic medicines are not general supplements; they are structured therapeutic formulations that must be adjusted based on body type, digestion, staging, age, and presence of infections such as HPV. Mineral preparations are added only after careful evaluation.
How long does Ayurvedic treatment take
Duration varies depending on the stage of cancer, presence of viral infections, immune strength, and whether previous surgeries were done. Early cases may respond faster. Advanced stages require a structured, longer program focusing on detoxification, regeneration, and restoring cellular balance.
Can I follow Ayurveda along with modern treatment
Yes. Ayurveda can be integrated with modern treatment when coordinated properly. Many patients choose this approach to support immune recovery, improve energy levels, reduce recurrence risk, and accelerate tissue healing. Your practitioner will guide you based on your individual case.
Does lifestyle matter during treatment
Yes. A light, anti-inflammatory diet, regular cleansing habits, stress reduction, good sleep, and avoiding smoking are important. These factors help stabilize Rakta Dhatu, support immunity, and improve the overall effectiveness of therapy.
Reference
A. Global Epidemiology + Risk Factors
- Douglawi, A., Shamloul, R. (2017). Genital inflammation and malignancy: Updates in penile cancer epidemiology. Urologic Oncology, 35(8), 502–510. https://doi.org/10.1016/j.urolonc.2017.06.015
- Backes, D. M., et al. (2017). Human papillomavirus and penile cancer: A systematic review. The Lancet Oncology, 18(7), 901–911. https://doi.org/10.1016/S1470-2045(17)30374-2
- Misra, S., et al. (2010). Penile cancer: A review of the literature. World Journal of Surgery, 34, 2159–2167. https://doi.org/10.1007/s00268-010-0663-6
- Bleeker, M. C. G., et al. (2009). Penile cancer epidemiology, pathogenesis and prevention. World Journal of Urology, 27, 141–150. https://doi.org/10.1007/s00345-008-0302-z
- American Cancer Society. (2025). Penile Cancer: Causes, Risks & Prevention. https://www.cancer.org/cancer/types/penile-cancer
B. HPV and Oncogenesis
- Alemany, L., et al. (2016). HPV DNA prevalence and type distribution in penile cancer. The Journal of Infectious Diseases, 213(8), 1016–1025. https://doi.org/10.1093/infdis/jiv570
- European Association of Urology. (2024). HPV-associated penile malignancy. https://uroweb.org/guidelines/penile-cancer
- Centers for Disease Control and Prevention (CDC). HPV and related cancers. https://www.cdc.gov/hpv/parents/cancer.html
C. Clinical Presentation, Diagnosis, & Staging
- Hakenberg, O. W., et al. (2015). EAU Guidelines on Penile Cancer: Diagnosis & Staging. European Urology, 67(1), 142–150. https://doi.org/10.1016/j.eururo.2014.10.017
- Cubilla, A. L., et al. (2016). Histopathology of penile carcinoma. Seminars in Diagnostic Pathology, 32(2), 127–146. https://doi.org/10.1053/j.semdp.2015.02.020
- Lam, W., et al. (2013). Early symptoms and delayed presentation in penile cancer. Clinical Oncology, 25(2), 102–109. https://doi.org/10.1016/j.clon.2012.10.006
- Mosconi, A. M. (2005). Cancer of the penis. Cancer Treatment & Research, 123, 225–230. https://doi.org/10.1007/0-387-27864-0_17
D. Treatment (Surgery, Chemo, Radiotherapy)
- Nicholson, S., et al. (2015). Organ-preserving surgical techniques for penile carcinoma. Nature Reviews Urology, 12, 249–257. https://doi.org/10.1038/nrurol.2015.46
- Protzel, C., et al. (2019). Chemoradiation vs surgery in advanced penile cancer. Urologic Oncology, 37(8), 571.e1–571.e9. https://doi.org/10.1016/j.urolonc.2019.03.031
- Huddart, R. A., et al. (2020). Radiotherapy outcomes in penile carcinoma. Clinical Oncology, 32(1), 33–41. https://doi.org/10.1016/j.clon.2019.07.012
E. Psychological & Sexual-Health Impact
- Maddineni, S. B., et al. (2009). Quality of life after penile cancer treatment. BJU International, 104(4), 582–587. https://doi.org/10.1111/j.1464-410X.2009.08469.x
- Skeppner, E., et al. (2012). Anxiety and sexual function outcomes post-treatment. The Journal of Sexual Medicine, 9(1), 894–903. https://doi.org/10.1111/j.1743-6109.2011.02595.x
F. Prevention (HPV Vaccine, Smoking Cessation)
- World Health Organization. HPV vaccine and male cancer prevention. https://www.who.int
- Palefsky, J. M. (2012). HPV vaccination in males. Vaccine, 30, F24–F27. https://doi.org/10.1016/j.vaccine.2012.04.107
Ayurvedic References (Classical Texts + Scientific Studies)
G. Classical Ayurvedic Text References
- Kanchanara Guggulu
Bhavaprakasha Madhyama Khanda, Chapter “Gulma Chikitsa,” Verse 43–46. - Vrishya Rasayana & reproductive tissues
Charaka Samhita, Chikitsa Sthana, Chapter 2 (Rasayana Adhyaya). - Dhatu & Srotas involvement in genital disorders
Sushruta Samhita, Nidana Sthana, Chapter 11 (Arsha & Vrana references). - Rakta Dusti and Arbuda (tumor pathology)
Charaka Samhita, Sutra Sthana, Chapter 24 (Visha & Rakta chapters). - Arbuda and inflammatory swellings
Sushruta Samhita, Nidana Sthana, Chapter 11 (Arbuda Nidana).
H. Ayurveda Rasayana + Cancer-Modulation Research
- Sharma, H., et al. (2012). Rasayana action and cellular rejuvenation: Evidence summary. Journal of Ayurveda and Integrative Medicine, 3(3), 151–159. https://doi.org/10.4103/0975-9476.100168
- Vyas, P., et al. (2010). Rasayana Avaleha efficacy in radiation/chemo side-effect reduction. Ancient Science of Life, 29(3), 28–33. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202271/
- Ghosh, S., et al. (2020). Anticancer properties of Ayurvedic herbs: A review. Phytotherapy Research, 34(5), 1027–1043. https://doi.org/10.1002/ptr.6595
I. Bhasma Scientific Validation (Gold, Diamond, Abhrak, Godanti)
- Singh, N., & Reddy, K. R. (2017). Characterization and safety of Swarna Bhasma. Journal of Ethnopharmacology, 197, 165–172. https://doi.org/10.1016/j.jep.2016.07.079
- Kumar, A., et al. (2016). Therapeutic potential of Heerak Bhasma nanoparticles. International Journal of Nanomedicine, 11, 3619–3632. https://doi.org/10.2147/IJN.S107343
- Puranik, V. G., et al. (2018). Abhrak Bhasma: Nano-structural features and pharmacological safety. Ayurveda Research Journal, 12(2), 44–52.
- Godanti Bhasma study: Singh, R., et al. (2020). Frontiers in Pharmacology, 11, 1712. https://doi.org/10.3389/fphar.2020.570130
J. Herbal Anticancer Evidence (Bark + Resin Herbs in Kanchanara)
- Kanchanara (Bauhinia variegata) anticancer activity. BMC Complementary Medicine, 12(1), 34.
- Haritaki (Terminalia chebula) cytoprotective effects. Phytomedicine, 19(7), 583–590.
- Shatavari and tissue repair. Journal of Ethnopharmacology, 102(2), 234–240.
- Guduchi (Tinospora cordifolia) immune-modulation. Frontiers in Immunology, 12, 627.