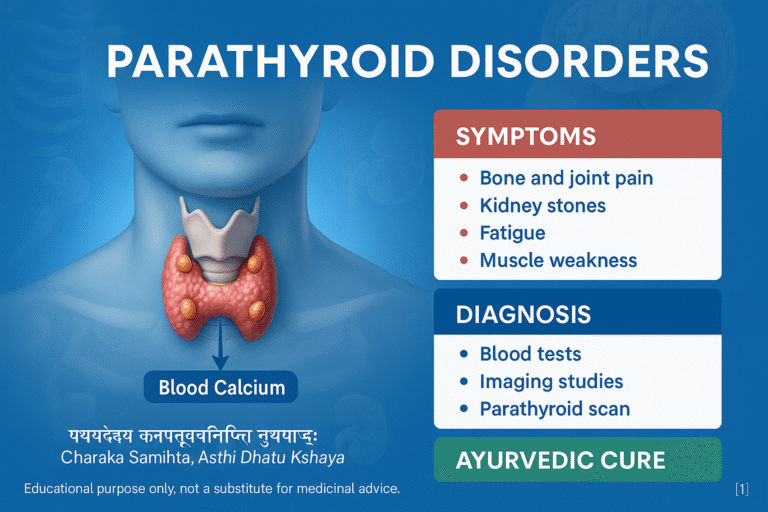
- Anatomy and Physiology
- Pathophysiology
- Disorders of the Parathyroid
- Hyperparathyroidism
- Hypoparathyroidism
- Parathyroid Carcinoma
- Diagnostic Approaches
- Diseases and Conditions Associated With Parathyroid Disorders
- Ayurvedic Perspective on Parathyroid Disorders
- Less Common and Rare Diseases Associated With Parathyroid Disorders
- Ayurvedic Interpretation of Less Common and Rare Parathyroid Related Diseases
- Modern Medical Management
- Ayurveda Avaleha (Medicine) for Cure
- Critical Warning About Market Purchased Avaleha and Self Preparation
- FAQs
- References
The parathyroid glands are four tiny endocrine structures located behind the thyroid gland, yet they play a crucial role in regulating calcium and phosphorus balance in the human body. Unlike the thyroid, which manages metabolism through thyroxine, the parathyroid glands secrete parathyroid hormone (PTH), a key regulator of bone strength, kidney function, and neuromuscular stability [1].
Disturbances in parathyroid function can lead to two opposite but equally dangerous conditions: hyperparathyroidism, where excess hormone causes calcium overload, kidney stones, and bone resorption, and hypoparathyroidism, where low hormone levels trigger tetany, seizures, and brittle bones [2]. Rarely, parathyroid cancer can arise, usually presenting with severe hypercalcemia and aggressive symptoms [3].
From an Ayurvedic perspective, parathyroid dysfunction may be correlated with Asthi Dhatu Kshaya (weakening of bone tissue), Majja Dhatu Dushti (marrow and nervous system imbalance), and Kapha-Pitta aggravation (stones, sluggish digestion, swelling) or Vata aggravation (tetany, cramps, dryness) [4]. Classical Ayurvedic texts emphasize maintaining calcium homeostasis through Rasayanas, mineral preparations like Praval Pishti, Mukta Sukti Bhasma, and Godanti Bhasma, and lifestyle measures such as sunlight exposure, diet, and stress regulation [5].
With rising cases of lifestyle disorders, thyroid–parathyroid surgeries, and chronic kidney disease, parathyroid disorders are becoming more prevalent worldwide. Modern medicine offers surgical and pharmacological interventions, while Ayurveda provides a holistic, root-cause–oriented approach that not only manages symptoms but also restores long-term balance [6].
Important Medical Safety Notice
Parathyroid disorders can lead to life-threatening complications if mismanaged. Symptoms such as confusion, seizures, severe muscle spasms, chest pain, extreme weakness, or dehydration require urgent medical attention. Ayurvedic support should never replace emergency care, surgery, or endocrinologist-guided treatment when clinically indicated.
Anatomy and Physiology
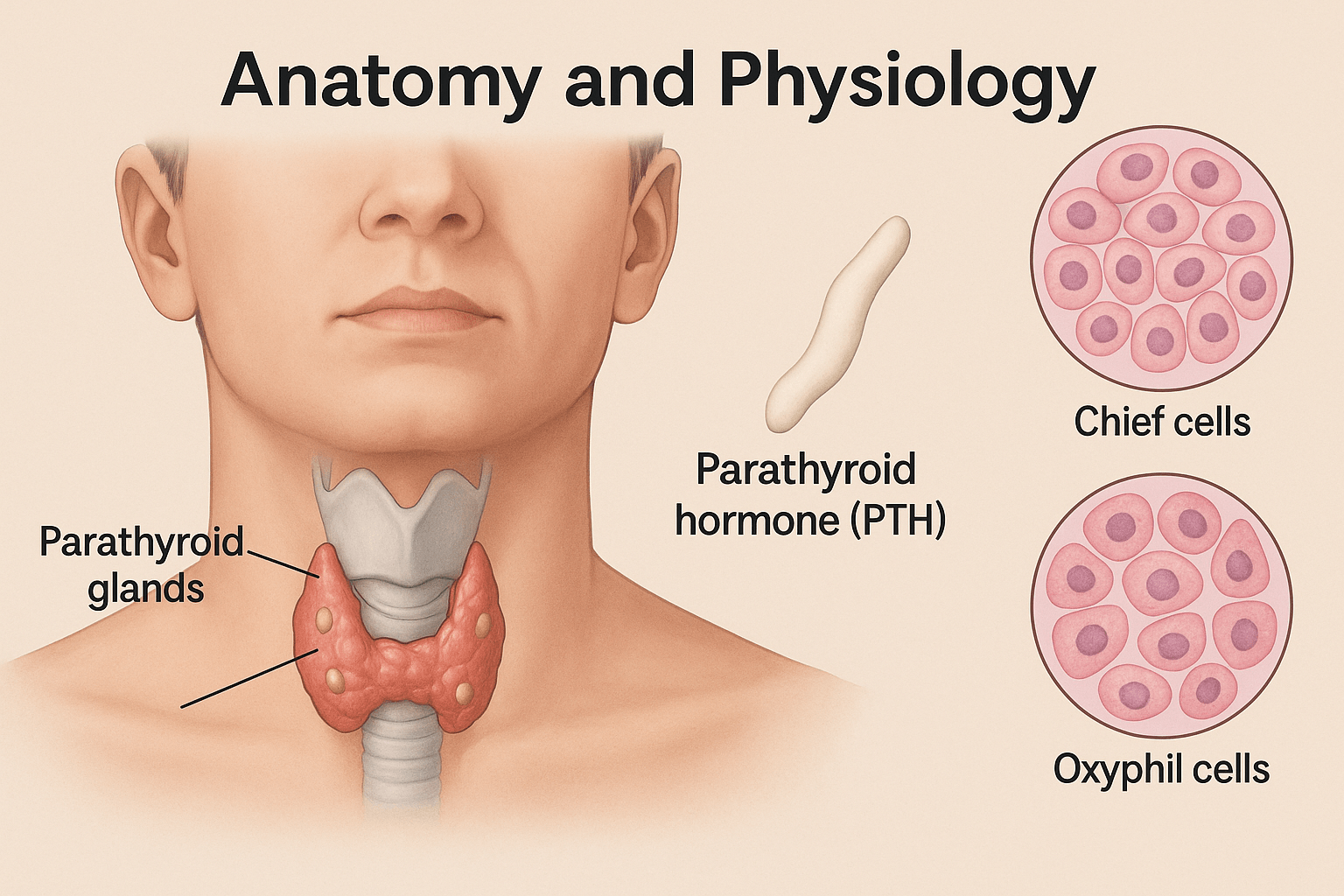
Structure of Parathyroid Glands
The parathyroid glands are typically four small, oval-shaped structures located on the posterior surface of the thyroid gland, though anatomical variations exist where individuals may have three or even five glands [1]. Each gland measures only a few millimeters in size yet carries immense importance for calcium balance. Unlike the thyroid, which is encapsulated and highly vascular, the parathyroid glands have a delicate capsule and are richly supplied with blood vessels to allow rapid hormone release into circulation [2].
Histology: Chief Cells and Oxyphil Cells
Microscopically, the parathyroid glands are composed primarily of two cell types. Chief cells are the most abundant and are responsible for the synthesis and secretion of parathyroid hormone (PTH). These cells contain numerous secretory granules, reflecting their endocrine function [3]. The second type, oxyphil cells, appear larger with an acidophilic cytoplasm rich in mitochondria. Their exact function remains less defined, though modern research suggests they may contribute to oxidative metabolism and possibly play a role in parathyroid hormone reserve [4].
Hormonal Function: Parathyroid Hormone (PTH)
The primary hormone secreted by the parathyroid glands is parathyroid hormone (PTH), a peptide consisting of 84 amino acids. PTH is a master regulator of serum calcium and phosphate levels, acting as a feedback mechanism when calcium levels drop in the bloodstream [5]. The release of PTH is tightly regulated by calcium-sensing receptors (CaSR) located on the parathyroid chief cells.
Role of PTH in Regulating Calcium, Phosphate, and Vitamin D
PTH increases serum calcium through three major mechanisms:
- Bone: Stimulates osteoclast activity indirectly via osteoblast signaling, leading to calcium release from bone matrix [6].
- Kidneys: Enhances calcium reabsorption in renal tubules while promoting phosphate excretion, preventing simultaneous hyperphosphatemia [7].
- Intestines: Indirectly increases calcium absorption by stimulating renal production of calcitriol (active vitamin D, 1,25-dihydroxycholecalciferol), which in turn promotes intestinal calcium uptake [8].
This finely tuned balance ensures adequate calcium availability for neuromuscular conduction, bone mineralization, and enzymatic functions. Disturbances in PTH secretion, therefore, have widespread systemic consequences.
From an Ayurvedic perspective, this regulation can be related to the dynamic interaction of Asthi Dhatu (bone tissue), Majja Dhatu (marrow and nervous system), and Shukra Ojas (vital essence). The parathyroid’s role in balancing calcium parallels the Ayurvedic concept of maintaining Dhatu Samya (tissue equilibrium), where disruption leads to conditions such as Asthi Kshaya (bone weakening) or Vata-related neuromuscular spasms [9].
Pathophysiology

Mechanism of Calcium Regulation
The parathyroid glands maintain calcium levels within a narrow physiological range (8.5–10.5 mg/dL). When serum calcium drops, calcium-sensing receptors (CaSR) on parathyroid chief cells are activated, stimulating the release of parathyroid hormone (PTH). PTH then works through bone, kidney, and intestines to restore calcium homeostasis [1]. Conversely, when calcium rises above normal, PTH secretion is suppressed, preventing hypercalcemia [2].
Interplay with Kidney, Bone, and Intestines
The action of PTH spans multiple organ systems:
- Bone: PTH stimulates osteoblasts to release RANKL, which activates osteoclasts, leading to the release of calcium and phosphate from bone into the blood. This ensures immediate calcium availability but contributes to bone resorption if prolonged [3].
- Kidneys: PTH promotes calcium reabsorption in the distal tubules, reduces phosphate reabsorption in the proximal tubules (preventing calcium-phosphate precipitation), and stimulates the conversion of 25-hydroxyvitamin D into active 1,25-dihydroxyvitamin D (calcitriol) [4].
- Intestines: The increase in calcitriol enhances calcium and phosphate absorption from the gut, supporting bone mineralization and systemic calcium balance [5].
Feedback Loop with Calcitonin and Vitamin D
Calcium regulation involves a delicate feedback loop. While PTH raises calcium, calcitonin—secreted by parafollicular cells (C-cells) of the thyroid—acts as a counter-regulatory hormone, lowering calcium by inhibiting osteoclast activity and increasing calcium deposition in bones [6]. In parallel, vitamin D plays a dual role: its active form, calcitriol, enhances intestinal calcium absorption but also provides negative feedback on the parathyroid gland to suppress excess PTH secretion [7].
This balance ensures that serum calcium remains stable, supporting neuromuscular conduction, cardiac rhythm, clotting mechanisms, and skeletal strength. Disturbances in any part of this axis—parathyroid glands, kidneys, bones, or vitamin D metabolism—result in clinical manifestations such as osteoporosis, kidney stones, or neuromuscular dysfunction [8].
From an Ayurvedic perspective, this dynamic interaction mirrors the Samyavastha (homeostasis) of Asthi Dhatu (bone tissue) and Majja Dhatu (nervous system and marrow). Disruption in this regulation can be correlated with Asthi Kshaya (bone weakening), Mutrashmari (urinary stones), and Vata-Pitta imbalance, where deranged fire (Agni) and obstructed channels (Srotas) disturb the equilibrium of mineral metabolism [9].
Disorders of the Parathyroid
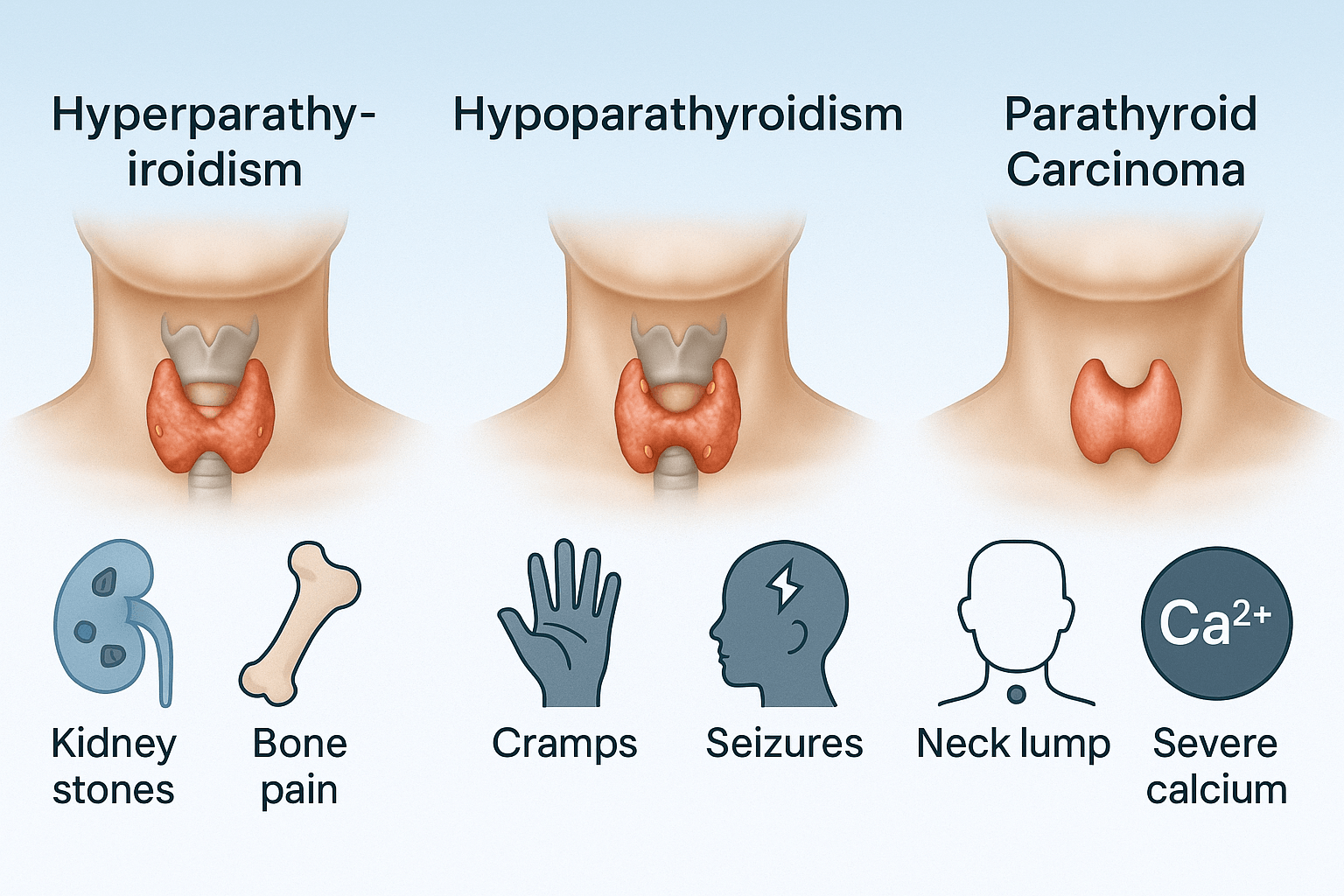
The parathyroid glands, despite their small size, are responsible for maintaining calcium-phosphate balance. Dysfunction of these glands leads to three major clinical entities: hyperparathyroidism, hypoparathyroidism, and parathyroid carcinoma. Each has distinctive causes and symptom clusters that can severely affect multiple organ systems.
Hyperparathyroidism
Hyperparathyroidism happens when the parathyroid glands make too much parathyroid hormone (PTH). This hormone normally helps regulate calcium and phosphorus levels, but when produced in excess, it disrupts the body’s mineral balance.
There are three main types:
- Primary hyperparathyroidism is most often caused by a benign growth (adenoma) on one of the parathyroid glands. Less commonly, all glands may be enlarged (hyperplasia).
- Secondary hyperparathyroidism develops as a result of another condition, most often chronic kidney disease (CKD). In CKD, the kidneys can’t properly regulate calcium and phosphate, which overstimulates the parathyroid glands.
- Tertiary hyperparathyroidism occurs when long-term secondary hyperparathyroidism becomes autonomous, with the glands continuing to release excess hormone even after the underlying problem is addressed.
Symptoms can vary widely, but the classic presentation is described as “stones, bones, groans, and psychic moans.”
- Stones: kidney stones, frequent urination, and calcium buildup in the kidneys.
- Bones: bone pain, fractures, and osteoporosis.
- Groans: abdominal discomfort, nausea, constipation, and sometimes pancreatitis.
- Psychic moans: depression, fatigue, and memory problems.
Other symptoms may include muscle weakness, hypertension, and generalized fatigue. If left untreated, complications such as severe bone loss, kidney damage, and cardiovascular problems can occur.
Hypoparathyroidism
Hypoparathyroidism is the opposite problem. It occurs when the parathyroid glands do not produce enough PTH. Without this hormone, calcium levels in the blood drop too low, while phosphate levels rise.
The most common cause is accidental damage or removal of the parathyroid glands during thyroid or neck surgery. Autoimmune conditions, genetic mutations, and certain metabolic disorders can also lead to hypoparathyroidism.
Symptoms are mainly related to low calcium (hypocalcemia) and include:
- Tingling or numbness in the lips, fingers, and toes.
- Muscle cramps, spasms, or painful contractions.
- Twitching of the facial muscles (Chvostek’s sign) or hand spasms when the arm is compressed (Trousseau’s sign).
- In more severe cases, seizures.
Over time, patients may also develop brittle nails, dry skin, coarse hair, and dental abnormalities. Psychological changes such as anxiety, irritability, and depression are also common. If untreated, hypoparathyroidism can cause chronic neuromuscular symptoms, calcification in soft tissues, and impaired quality of life.
Treatment usually involves calcium and vitamin D supplementation, and in some cases synthetic PTH therapy. Lifelong monitoring is typically required.
Parathyroid Carcinoma
Parathyroid carcinoma is a very rare but serious cancer of the parathyroid glands. It accounts for less than 1% of cases of primary hyperparathyroidism. Unlike benign adenomas, this tumor can invade nearby tissues and spread to other organs.
The exact cause is unknown, but certain inherited syndromes such as multiple endocrine neoplasia type 1 (MEN1) and mutations in the HRPT2 gene increase the risk.
Symptoms are usually more severe than in benign parathyroid disease because the tumor produces extremely high levels of PTH, leading to dangerous hypercalcemia. Common signs include:
- Persistent nausea, vomiting, dehydration, and confusion.
- A noticeable lump in the neck.
- Hoarseness or difficulty swallowing if the tumor presses on surrounding structures.
- Severe bone pain and fractures due to calcium loss.
Because symptoms often overlap with benign hyperparathyroidism, diagnosis can be challenging. Blood calcium and PTH levels are usually extremely elevated, and imaging may reveal a neck mass.
Treatment typically requires surgical removal of the cancerous gland along with surrounding tissue. Even with surgery, recurrence is common, and patients need close long-term monitoring.
Diagnostic Approaches
Diagnosing parathyroid disorders usually starts with simple blood work and then moves on to imaging and bone testing if needed. Doctors use these tools to confirm whether the glands are working properly and to check the effects of abnormal hormone levels.
Blood tests
The first step is usually blood testing. High or low calcium levels are a key sign of parathyroid problems. Other markers include phosphate, parathyroid hormone (PTH), and vitamin D. For example, high calcium and high PTH suggest hyperparathyroidism, while low calcium and low PTH point toward hypoparathyroidism.
Imaging
If a parathyroid tumor or enlarged gland is suspected, imaging can help locate the problem. Ultrasound of the neck is commonly used because it’s safe and non-invasive. A sestamibi scan is more specific, using a small radioactive tracer to highlight overactive parathyroid tissue. In difficult cases, advanced imaging such as MRI or CT scans may be used.
Bone mineral density testing
Because parathyroid disorders can weaken the bones, doctors often recommend a bone mineral density (DEXA) scan. This test measures bone strength and can reveal early osteoporosis or fracture risk, even before symptoms appear.
Diseases and Conditions Associated With Parathyroid Disorders
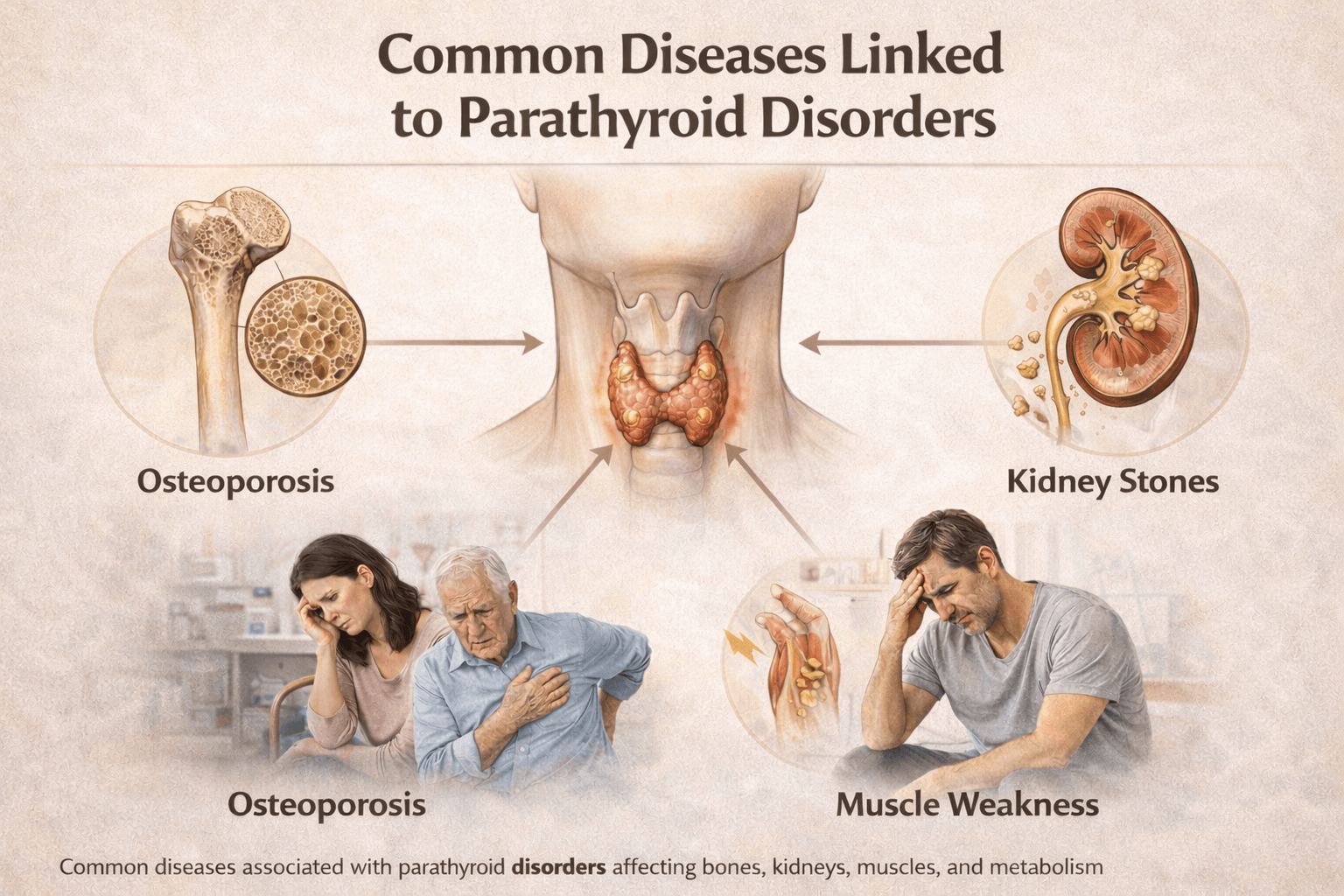
Parathyroid disorders influence far more than calcium values on a laboratory report. In my clinical experience, parathyroid hormone imbalance affects bones, kidneys, muscles, nerves, digestion, cardiovascular health, cognition, and long term metabolic stability. Many patients come with complaints such as bone pain, kidney stones, fatigue, anxiety, or seizures, while the underlying parathyroid disorder remains unrecognized. If you understand the full spectrum of associated diseases, you can identify patterns earlier and avoid years of misdirected treatment.
Bone and Skeletal Diseases
Excess parathyroid hormone accelerates bone resorption and weakens skeletal structure. Patients commonly develop osteopenia, osteoporosis, cortical bone loss, and fragility fractures. You may notice chronic back pain, height reduction, repeated fractures after minor trauma, or generalized bone discomfort. Clinicians often observe silent vertebral fractures even in patients who believe they are asymptomatic. In severe and prolonged disease, osteitis fibrosa cystica and brown tumor like lesions may appear, sometimes mimicking malignant bone disease on imaging. These skeletal manifestations represent advanced hormonal imbalance rather than isolated orthopedic problems.
Kidney and Urinary Tract Disorders
Renal involvement is one of the most frequent consequences of parathyroid dysfunction. Patients often experience recurrent kidney stones, flank pain, hematuria, or frequent urination. In many cases, nephrocalcinosis develops silently and is discovered incidentally. Over time, repeated calcium deposition and dehydration can reduce kidney function. If you have recurrent stones or unexplained decline in renal parameters, clinicians should consider parathyroid hormone excess as a contributing factor rather than treating stones as an isolated condition.
Neuromuscular and Neurological Conditions
Calcium imbalance directly alters nerve conduction and muscle excitability. In hypoparathyroidism, patients commonly experience tingling around the lips, fingers, and toes, muscle cramps, twitching, carpopedal spasm, and episodes of tetany. You may feel stiffness, restlessness, or involuntary contractions that worsen with stress. Severe hypocalcemia lowers the seizure threshold, and some patients are diagnosed with seizure disorders long before the metabolic cause is identified. Chronic cases may show basal ganglia calcification, movement disorders, or cognitive slowing, highlighting the deep neurological impact of untreated parathyroid disease.
Cardiac and Cardiovascular Associations
Parathyroid hormone and calcium balance play a critical role in cardiac conduction and vascular integrity. Patients may develop palpitations, prolonged QT interval, dizziness, syncope, or arrhythmias. Over the long term, mineral imbalance contributes to vascular calcification, arterial stiffness, hypertension, and increased cardiovascular risk. In patients with chronic kidney disease, these cardiovascular effects become more pronounced and contribute significantly to morbidity and mortality.
Gastrointestinal and Metabolic Disorders
Digestive symptoms are common but often overlooked. Patients frequently report constipation, abdominal discomfort, bloating, nausea, reduced appetite, and unexplained weight changes. Hypercalcemia can impair smooth muscle function and enzyme activity, leading to sluggish digestion. In some individuals, pancreatitis or peptic ulcer like symptoms develop in association with elevated calcium levels. If you have persistent gastrointestinal complaints along with fatigue, bone pain, or kidney stones, clinicians should evaluate parathyroid related causes.
Neuropsychiatric and Cognitive Conditions
Parathyroid disorders can significantly affect mental health and cognitive function. Patients often describe depression, anxiety, irritability, sleep disturbance, poor concentration, memory impairment, and a sense of mental clouding. I have seen patients treated for mood disorders for years without improvement until calcium and parathyroid hormone imbalance was corrected. These symptoms are biochemical in origin and not merely psychological, and they often improve when hormonal balance is restored.
Chronic Kidney Disease Related Parathyroid Disorders
In chronic kidney disease, secondary hyperparathyroidism develops due to phosphate retention and impaired vitamin D activation. Patients experience bone pain, muscle weakness, itching, fractures, and progressive vascular calcification. Over time, prolonged stimulation of the parathyroid glands can lead to tertiary hyperparathyroidism, where hormone secretion becomes autonomous and hypercalcemia persists even after kidney transplantation. If you or your patient has kidney disease, parathyroid monitoring becomes a long term necessity rather than an optional test.
Endocrine and Post Surgical Associations
Hypoparathyroidism is a well recognized complication after thyroid or neck surgery. Patients may develop early symptoms such as numbness, cramps, voice fatigue, or swallowing difficulty, followed by long term complications if calcium control remains unstable. Parathyroid disorders also coexist with other endocrine conditions such as diabetes and menopausal bone loss, where skeletal fragility and fatigue tend to be more severe. If you already have an endocrine disorder, parathyroid evaluation should not be overlooked.
Genetic and Familial Conditions
Some parathyroid disorders arise from inherited syndromes. Familial hyperparathyroidism, multiple endocrine neoplasia syndromes, familial hypocalciuric hypercalcemia, autoimmune polyglandular syndromes, pseudohypoparathyroidism, and congenital parathyroid absence are rare but clinically significant. These conditions often present earlier in life and may involve multiple organs. Recognizing them changes management not only for the patient but also for family members who may require screening.
Rare and Severe Complications
Parathyroid carcinoma is rare but aggressive and often presents with severe hypercalcemia, neck mass, hoarseness, dysphagia, profound bone disease, and rapid systemic decline. Calciphylaxis, particularly in patients with advanced kidney disease, represents a catastrophic form of vascular calcification associated with mineral imbalance. Chondrocalcinosis and crystal induced arthritis may occur due to altered calcium and phosphate metabolism, presenting as acute joint inflammation.
Ayurvedic Correlation of Associated Diseases
From an Ayurvedic perspective, these wide ranging disease patterns reflect Asthi Dhatu Kshaya, Majja Dhatu Dushti, Mutravaha Srotas imbalance, and Agni dysfunction. In practice, I observe that Vata aggravation aligns with degeneration, spasms, neurological instability, and weakness, while Kapha and Pitta involvement aligns with stone formation, calcification, inflammation, and metabolic overload. If you integrate this classical understanding with modern diagnostics and safety boundaries, Ayurveda can be applied responsibly to support long term correction rather than superficial symptom suppression.
Ayurvedic Perspective on Parathyroid Disorders
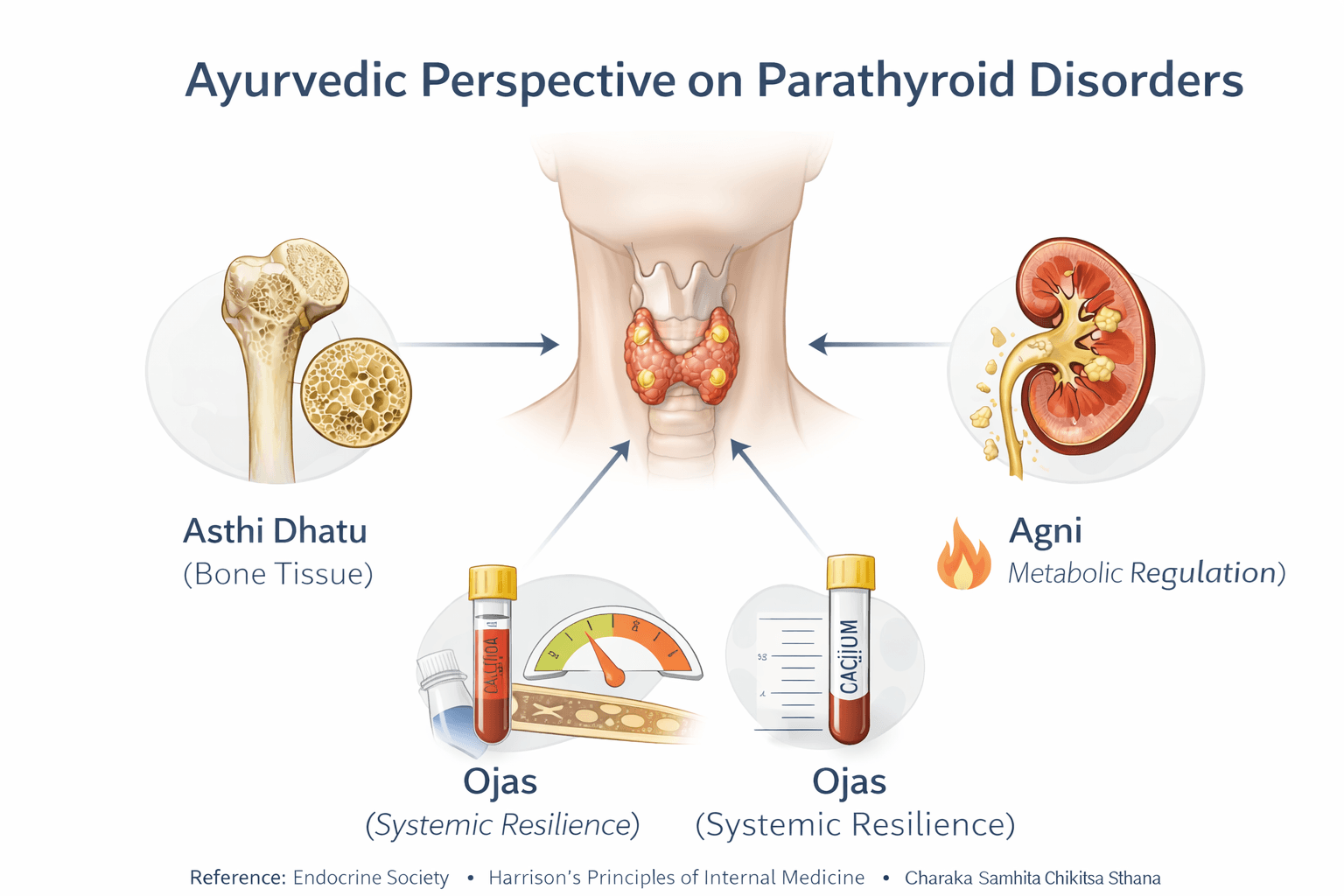
Ayurveda approaches parathyroid disorders not as isolated glandular diseases but as systemic disturbances rooted in Dhatu imbalance, Agni dysfunction, and Srotas obstruction. When I assess such patients, I do not look only at calcium levels. Ayurveda asks why the body has lost its ability to regulate minerals, nourish bone tissue, and maintain neuromuscular stability. If you understand this classical framework, the wide range of bone, kidney, neurological, and metabolic diseases associated with parathyroid disorders becomes logically connected rather than fragmented.
Asthi Dhatu Kshaya as the Foundation of Bone and Calcium Disorders
Asthi Dhatu governs bones, teeth, nails, and all mineralized structures. Classical Ayurveda clearly states that when Asthi Dhatu is depleted, degeneration, pain, and structural weakness follow.
Charaka Samhita Chikitsa Sthana Chapter 28 Asthi Pradoshaja Vikara states
“दन्तभेदः अस्थिभेदः केशरोमलोपः खलित्यम्”
Translation
Disorders arising from vitiation of bone tissue include pain in bones and teeth, loss of hair, and progressive degeneration of structural tissues.
In parathyroid disorders, especially hyperparathyroidism and chronic secondary hyperparathyroidism, excessive bone resorption mirrors this Asthi Dhatu Kshaya. Patients experience osteoporosis, fractures, and chronic bone pain. I consistently observe that calcium supplementation alone does not reverse these conditions unless Asthi Dhatu nourishment is addressed through Rasayana and Agni correction.
Majja Dhatu Dushti and Neuromuscular Instability
Majja Dhatu represents bone marrow and the nervous system. Hypocalcemia and hypoparathyroidism frequently present with spasms, tingling, seizures, anxiety, and cognitive disturbance. Ayurveda classifies these under Majja Dhatu Dushti combined with aggravated Vata Dosha.
Charaka Samhita Sutra Sthana Chapter 17 Dhatu Poshan Adhyaya explains
“मज्जा अस्थीनां पूरकः”
Translation
Majja Dhatu fills and nourishes the bones and supports neurological stability.
If Majja Dhatu is weakened, nerve conduction becomes unstable. You may see seizures or tremors treated symptomatically for years without improvement. In my clinical experience, strengthening Majja Dhatu through Vata pacifying Rasayana brings lasting neuromuscular stability rather than temporary biochemical correction.
Agni Mandya and Failure of Mineral Assimilation
Agni governs digestion, absorption, and tissue transformation. Ayurveda emphasizes that without proper Agni, nutrients cannot be utilized even if intake is sufficient.
Charaka Samhita Chikitsa Sthana Chapter 15 Grahani Chikitsa states
“अग्निमूलं बलं पुंसाम्”
Translation
Agni is the root of strength, health, and nourishment in the human body.
In parathyroid disorders, Agni Mandya leads to improper calcium absorption and erratic mineral metabolism. Patients often report adequate diet and supplements yet continue to show deficiency or imbalance. If you correct Agni, tissue uptake improves naturally and dependence on external supplementation reduces.
Mutravaha Srotas Dushti and Renal Stone Formation
Kidney stones and nephrocalcinosis are hallmark features of hyperparathyroidism. Ayurveda explains this through Mutravaha Srotas Dushti combined with Kapha and Pitta imbalance, leading to abnormal crystallization and obstruction.
Sushruta Samhita Nidana Sthana Chapter 3 Ashmari Nidana describes
“दोषाणां संमूर्छनात् अश्मरी जायते”
Translation
When Doshas accumulate and solidify, stone formation occurs.
In my practice, treating only hydration or stone removal without correcting Srotas pathology leads to recurrence. When Mutravaha Srotas are cleared and metabolism is corrected, recurrence reduces significantly.
Dosha Involvement in Parathyroid Disorders
Parathyroid disorders are rarely single Dosha diseases. Hypoparathyroidism shows dominant Vata aggravation with spasms, tremors, dryness, fear, and instability. Hyperparathyroidism shows Kapha involvement in calcification and stone formation and Pitta involvement in inflammation and tissue breakdown.
Ashtanga Hridaya Sutra Sthana Chapter 12 Dosha Bhediya explains
“वातः पित्तं कफश्चेति त्रयो दोषाः समासतः”
Translation
Vata, Pitta, and Kapha together govern all physiological and pathological processes.
If you treat only one Dosha, the disease shifts rather than resolves. Ayurveda demands individualized Dosha assessment for true cure.
Rasayana Therapy for Long Term Correction
Rasayana is central to curing parathyroid related disorders. It is not a tonic but a therapeutic discipline aimed at rebuilding Dhatus, stabilizing Agni, and restoring resilience.
Charaka Samhita Chikitsa Sthana Chapter 1 Rasayana Adhyaya states
“रसायनं नाम वयसः स्थापकं बलवर्णकरं”
Translation
Rasayana preserves vitality, strengthens tissues, and restores physiological balance.
In Asthi and Majja Dhatu disorders, Rasayana supports bone regeneration, neuromuscular stability, and metabolic correction. I emphasize to patients that Rasayana works gradually and requires discipline. It does not offer overnight biochemical correction but aims at permanent disease resolution.
Ayurvedic Mineral Preparations and Classical Safety Doctrine
Classical texts describe Praval Pishti, Mukta Sukti Bhasma, and Godanti Bhasma for bone and calcium disorders. These are processed medicines, not raw minerals.
Rasa Tarangini Chapter 13 Praval Varga describes proper purification and use of coral based formulations for Asthi related disorders.
Ayurveda strictly warns against unsupervised use. If you self medicate or ignore Agni and Dosha status, even classical medicines can aggravate disease. In my clinical approach, mineral formulations are used only after thorough assessment and always in limited duration.
Ayurvedic Definition of Cure in Parathyroid Disorders
Ayurveda defines cure as Samprapti Vighatana, the complete breakdown of disease causation.
Charaka Samhita Chikitsa Sthana Chapter 16 states
“सम्प्राप्तिविघटनमेव चिकित्सा”
Translation
True treatment is the reversal of disease pathogenesis.
From this standpoint, Ayurveda aims to cure parathyroid disorders by restoring Agni, correcting Doshas, rebuilding Dhatus, and preventing recurrence. When applied correctly and ethically, this approach seeks long term stability rather than lifelong dependency.
Less Common and Rare Diseases Associated With Parathyroid Disorders
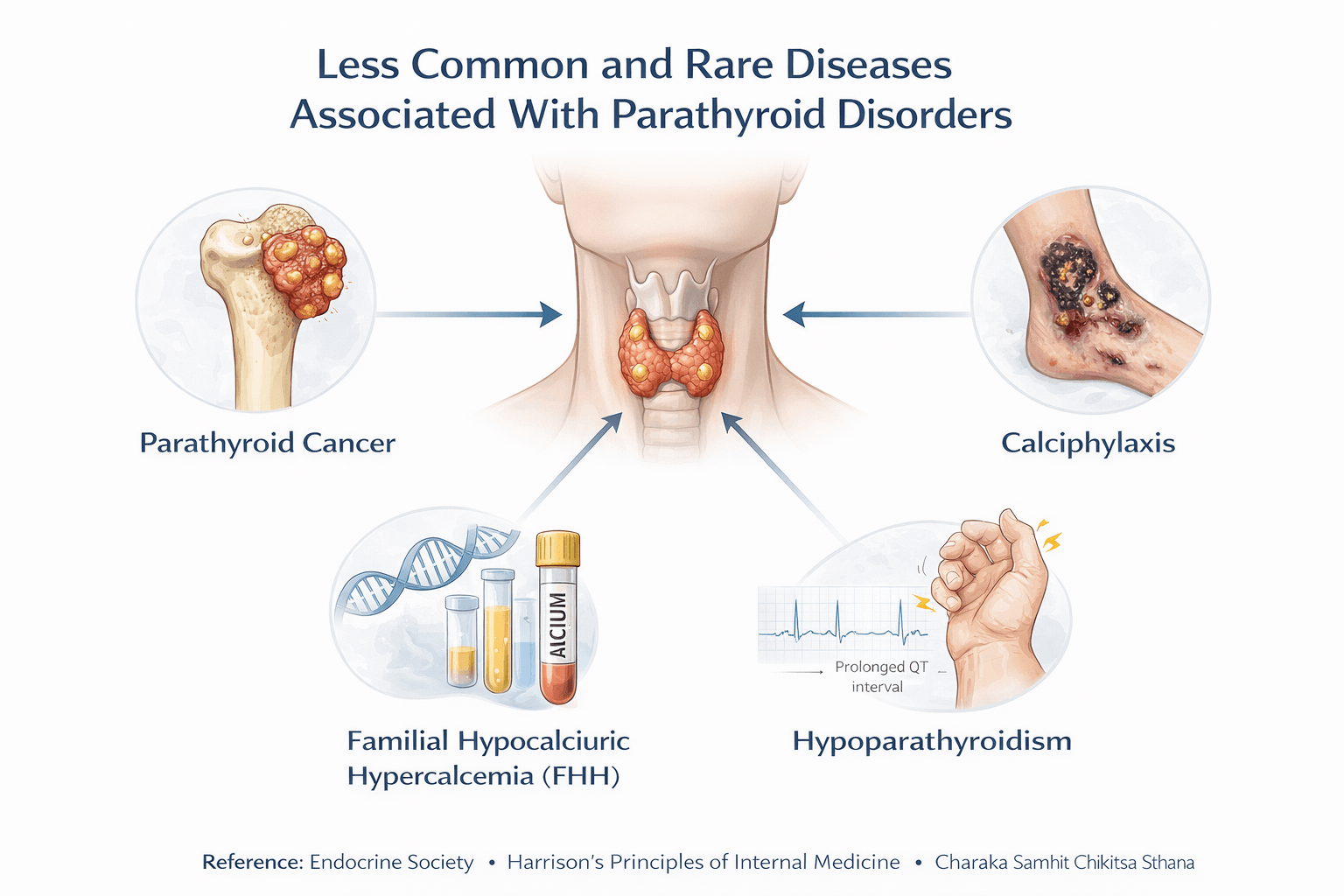
Parathyroid disorders can manifest through a wide range of less common and rare diseases that are frequently overlooked in routine clinical practice. In my experience, these conditions often appear after years of unrecognized hormonal imbalance and are mistakenly treated as isolated orthopedic, neurological, psychiatric, renal, or dermatological disorders. If you are aware of these associations, you can identify severe disease earlier and prevent irreversible damage. Clinicians also rely on these patterns to differentiate mild biochemical imbalance from advanced systemic pathology.
Advanced Skeletal Manifestations and Structural Bone Disease
In prolonged and severe hyperparathyroidism, bone disease progresses beyond osteoporosis into advanced structural damage. Patients may develop osteitis fibrosa cystica with extensive bone resorption, deformities, and pathological fractures. Radiological findings can include subperiosteal bone resorption, tapering of distal clavicles and phalanges, and a characteristic salt and pepper appearance of the skull. These changes can closely mimic malignant bone disease. I have seen patients undergo extensive cancer evaluation before parathyroid hormone excess was identified as the underlying cause. If you encounter destructive bone lesions with elevated calcium levels, parathyroid evaluation becomes mandatory.
Brown Tumors and Focal Bone Lesions
Brown tumors represent localized areas of excessive bone turnover and hemorrhage resulting from prolonged parathyroid hormone excess. They commonly affect the jaw, ribs, pelvis, spine, and long bones. Patients may present with swelling, localized pain, deformity, or fractures. These lesions are reactive rather than neoplastic, and they often regress when hormonal balance is restored. If you recognize them early, unnecessary surgical or oncologic interventions can be avoided.
Rare Neurological and Neuropsychiatric Presentations
Beyond common neuromuscular symptoms, parathyroid disorders can produce rare but severe neurological manifestations. Chronic hypoparathyroidism may lead to intracranial calcification, particularly in the basal ganglia. Patients can present with seizures, movement disorders, tremors, rigidity, gait disturbance, or progressive cognitive decline. Severe hypercalcemia in hyperparathyroidism can precipitate delirium, hallucinations, psychosis, or marked alteration in consciousness. If sudden psychiatric or neurological symptoms occur alongside calcium imbalance, they should never be considered primary psychiatric disease alone.
Raised Intracranial Pressure and Visual Complications
Chronic hypocalcemia can lead to increased intracranial pressure and papilledema. Patients may experience persistent headaches, blurred vision, visual field defects, or transient visual loss. These findings are uncommon and frequently misattributed to primary neurological conditions. If you or your patient has hypocalcemia with unexplained visual symptoms, this rare association should be actively investigated.
Cardiac and Electrical Conduction Abnormalities
Severe disturbances in calcium homeostasis can produce rare but dangerous cardiac complications. Patients may develop prolonged QT interval, ventricular arrhythmias, syncope, or sudden cardiac instability. These manifestations may occur without obvious cardiac disease and can be life threatening if unrecognized. In such cases, correcting calcium and parathyroid hormone imbalance becomes an urgent priority.
Renal and Vascular Calcification Disorders
Longstanding parathyroid dysfunction can lead to extensive soft tissue and vascular calcification. Calciphylaxis is a rare but catastrophic complication seen most often in advanced kidney disease with severe secondary hyperparathyroidism. It presents with painful skin lesions that progress to necrosis, infection, and systemic illness. Mortality remains high even with treatment. If painful skin lesions develop in a patient with kidney disease and mineral imbalance, this diagnosis requires immediate attention.
Genetic and Familial Disorders Affecting Parathyroid Function
Several rare genetic conditions alter parathyroid hormone regulation and calcium metabolism. Familial hypocalciuric hypercalcemia presents with lifelong mild hypercalcemia and low urinary calcium excretion. These patients are often misdiagnosed with primary hyperparathyroidism and may undergo unnecessary surgery. Multiple endocrine neoplasia syndromes involve parathyroid disease along with tumors of other endocrine glands. Pseudohypoparathyroidism represents hormone resistance rather than hormone deficiency and presents with hypocalcemia and characteristic skeletal features. If parathyroid disease appears at a young age or has a strong family history, genetic evaluation becomes essential.
Autoimmune and Congenital Parathyroid Disorders
Autoimmune hypoparathyroidism may occur as part of autoimmune polyendocrine syndromes. Patients can present with hypocalcemia alongside adrenal insufficiency, thyroid disease, chronic mucocutaneous candidiasis, or other immune mediated conditions. Congenital absence or underdevelopment of the parathyroid glands, as seen in DiGeorge syndrome, presents early in life with hypocalcemia, seizures, immune dysfunction, and cardiac anomalies. Early recognition is critical to prevent life threatening complications.
Dermatological, Dental, and Ocular Complications
Chronic hypocalcemia affects ectodermal tissues. Patients may develop dry scaly skin, brittle or deformed nails, hair texture changes, early onset cataracts, and dental enamel defects. These features often progress slowly and are rarely linked back to parathyroid dysfunction unless specifically evaluated. Dentists and ophthalmologists are sometimes the first to suspect an underlying metabolic disorder in such cases.
Rare Malignancy of the Parathyroid Glands
Parathyroid carcinoma is extremely rare but aggressive. It often presents with disproportionately severe hypercalcemia, profound weakness, bone destruction, kidney failure, neck mass, hoarseness, or difficulty swallowing. The severity of systemic manifestations is often greater than expected for benign disease. Early recognition and surgical management are critical for survival.
Clinical Importance of Recognizing Rare Associations
Less common and rare diseases associated with parathyroid disorders usually indicate advanced, long standing, genetic, or systemic disease. If you recognize these patterns early, you can prevent irreversible bone damage, neurological injury, cardiovascular events, and unnecessary procedures. From a clinical standpoint, these associations reinforce that parathyroid disorders are systemic diseases rather than isolated endocrine abnormalities.
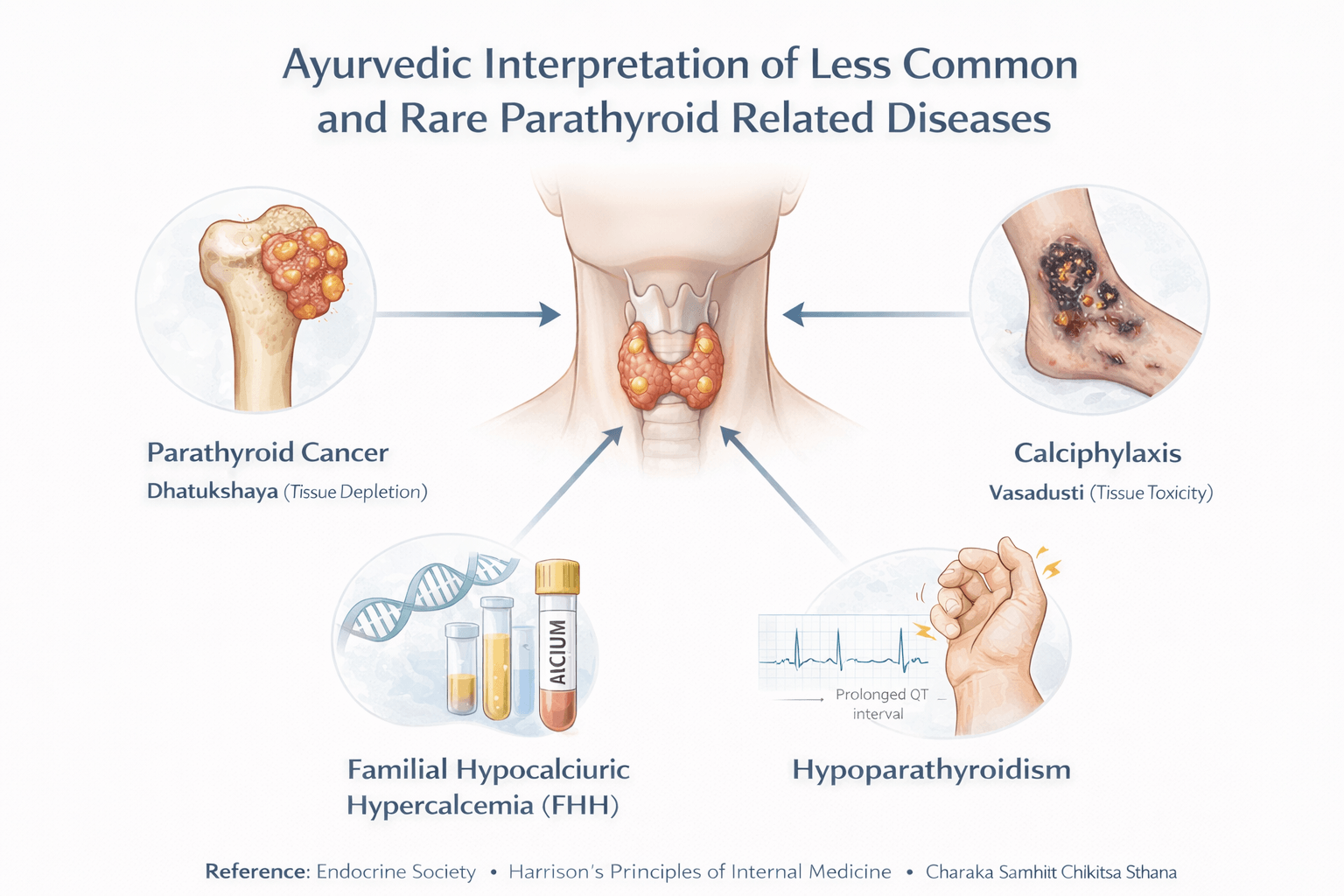
From an Ayurvedic standpoint, the appearance of rare and advanced diseases in parathyroid disorders indicates deep seated imbalance that has crossed beyond superficial metabolic disturbance. In my clinical experience, these manifestations arise when Dosha imbalance, Dhatu depletion, and Srotas obstruction remain uncorrected for prolonged periods. If you view these conditions through Ayurvedic principles, each rare complication reflects a predictable stage of systemic deterioration rather than an isolated event.
Advanced Bone Destruction and Osteitis Fibrosa Cystica
Severe bone destruction and deformities reflect profound Asthi Dhatu Kshaya combined with aggravated Vata Dosha. Ayurveda explains that when Asthi Dhatu loses nourishment, the body responds with excessive internal catabolism, leading to bone resorption, pain, deformity, and instability. Brown tumors and cystic bone changes represent localized failure of Asthi and Majja Dhatu integration. If this stage is reached, simple nourishment is insufficient. Rasayana aimed at Asthi and Majja Dhatu along with Vata pacification becomes essential for any chance of structural recovery.
Neurological Calcification and Movement Disorders
Basal ganglia calcification, seizures, tremors, and movement disorders are interpreted as Majja Dhatu Dushti with severe Vata aggravation. Ayurveda describes Majja as responsible for nerve conduction, mental stability, and motor control. When calcium metabolism fails, Majja Dhatu becomes depleted and unstable. You may see neurological symptoms that appear irreversible. In reality, Ayurvedic therapy focuses on stabilizing Vata, nourishing Majja, and restoring Agni to prevent further neurological decline.
Severe Psychiatric and Cognitive Manifestations
Delirium, hallucinations, psychosis, and profound cognitive impairment reflect combined Vata and Pitta disturbance affecting Manovaha Srotas. Ayurveda recognizes that the mind and nervous system are deeply influenced by metabolic heat and dryness. When mineral imbalance persists, mental symptoms emerge as systemic pathology rather than isolated psychiatric illness. If you treat only the mind, symptoms persist. When Dosha balance and Dhatu nourishment are restored, mental clarity often improves significantly.
Raised Intracranial Pressure and Visual Disturbance
Headache, papilledema, and visual impairment seen in chronic hypocalcemia represent obstruction of Majjavaha and Rasavaha Srotas. Ayurveda explains that improper fluid circulation combined with Vata instability leads to pressure phenomena within confined spaces such as the cranial cavity. If you ignore this stage, permanent visual damage may occur. Early correction of Agni and Srotas flow is crucial.
Cardiac Rhythm Disturbance and Sudden Instability
Arrhythmias and electrical instability of the heart reflect Prana Vata dysfunction combined with Rakta and Ojas depletion. Ayurveda considers the heart the seat of Prana and consciousness. When calcium regulation fails, Prana Vata becomes erratic, leading to rhythm disturbance. In such cases, Rasayana aimed at stabilizing Prana and strengthening Ojas is as important as biochemical correction.
Vascular Calcification and Calciphylaxis
Calciphylaxis and widespread vascular calcification indicate severe Kapha and Pitta involvement with Mutravaha and Raktavaha Srotas Dushti. Ayurveda describes this as pathological solidification where substances meant for nourishment instead obstruct circulation. Painful skin necrosis represents the final stage of tissue starvation. If you reach this stage, therapy must focus on clearing Srotas obstruction, cooling Pitta, and restoring metabolic discrimination.
Genetic and Hormone Resistance Disorders
Conditions such as pseudohypoparathyroidism and familial calcium regulation disorders reflect Beej Dushti meaning congenital or hereditary disturbance at the foundational level. Ayurveda acknowledges that such disorders require lifelong management rather than short term correction. If you identify Beej Dushti early, progression into severe Dhatu damage can be slowed through tailored Rasayana and lifestyle regulation.
Autoimmune and Congenital Gland Failure
Autoimmune hypoparathyroidism and congenital absence of parathyroid tissue reflect failure of Ojas and immune regulation. Ayurveda interprets this as deep seated Agni collapse affecting immune tolerance. Patients often show multi organ involvement. In such cases, Rasayana focused on immune balance and tissue resilience becomes the core strategy rather than symptom suppression.
Dermatological, Dental, and Ocular Manifestations
Dry skin, brittle nails, enamel defects, and early cataracts reflect Rasa and Asthi Dhatu malnourishment. Ayurveda teaches that when foundational Dhatus are weak, external tissues reveal early warning signs. If you observe these features, they should prompt evaluation of deeper metabolic imbalance rather than cosmetic treatment alone.
Rare Malignancy of the Parathyroid Glands
Parathyroid carcinoma represents uncontrolled Dhatu proliferation driven by deranged Pitta and Kapha under the influence of chronic Agni distortion. Ayurveda recognizes such growth as loss of cellular intelligence rather than random mutation. While modern surgery is mandatory, Ayurvedic intervention focuses on preventing recurrence by restoring metabolic order and tissue regulation.
Modern Medical Management
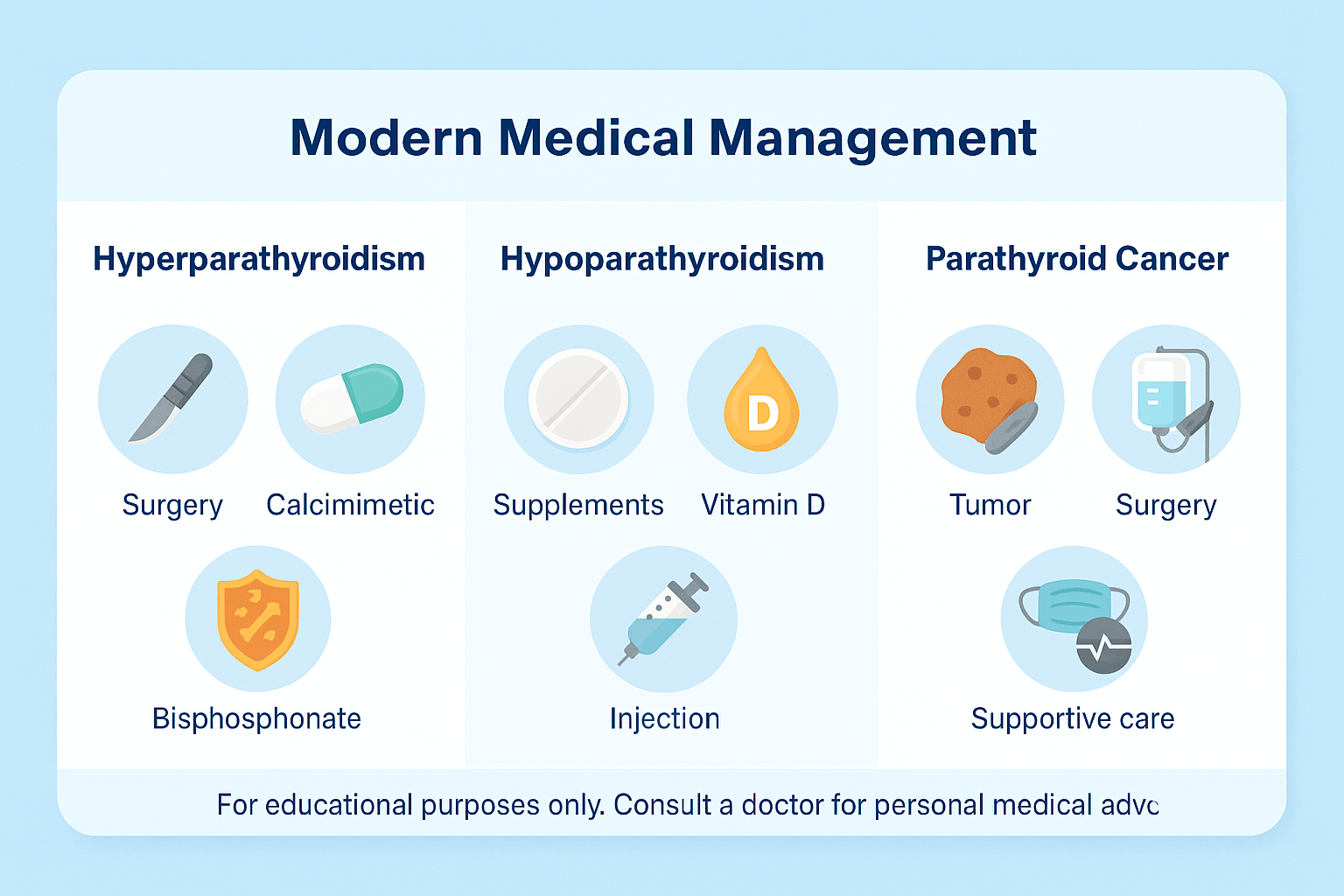
Treatment for parathyroid disorders depends on whether the glands are overactive, underactive, or affected by cancer. The main goal is to restore normal calcium balance while preventing long-term complications.
Hyperparathyroidism
The most effective treatment for primary hyperparathyroidism is surgery to remove the overactive gland. Parathyroidectomy is usually recommended if calcium levels are very high, if bone or kidney complications are present, or if the patient is young.
For people who cannot have surgery, medications may help. Calcimimetics, such as cinacalcet, reduce parathyroid hormone release and lower calcium levels. Bisphosphonates may be prescribed to protect bone strength by slowing down calcium loss from bones.
Hypoparathyroidism
Management focuses on raising calcium levels and keeping them stable. Most patients take lifelong calcium supplements along with active forms of vitamin D to improve calcium absorption. In some cases, recombinant parathyroid hormone (PTH) injections are used, particularly when standard supplements are not enough to control symptoms.
Parathyroid cancer
Treatment is more complex because the disease is rare and often aggressive. Surgery is the main option, with complete removal of the cancerous gland and sometimes surrounding tissue. After surgery, patients may still need supportive therapies to manage persistent high calcium levels, which can include hydration, bisphosphonates, or calcimimetics. Long-term monitoring is essential because the cancer often comes back.
Ayurveda Avaleha (Medicine) for Cure
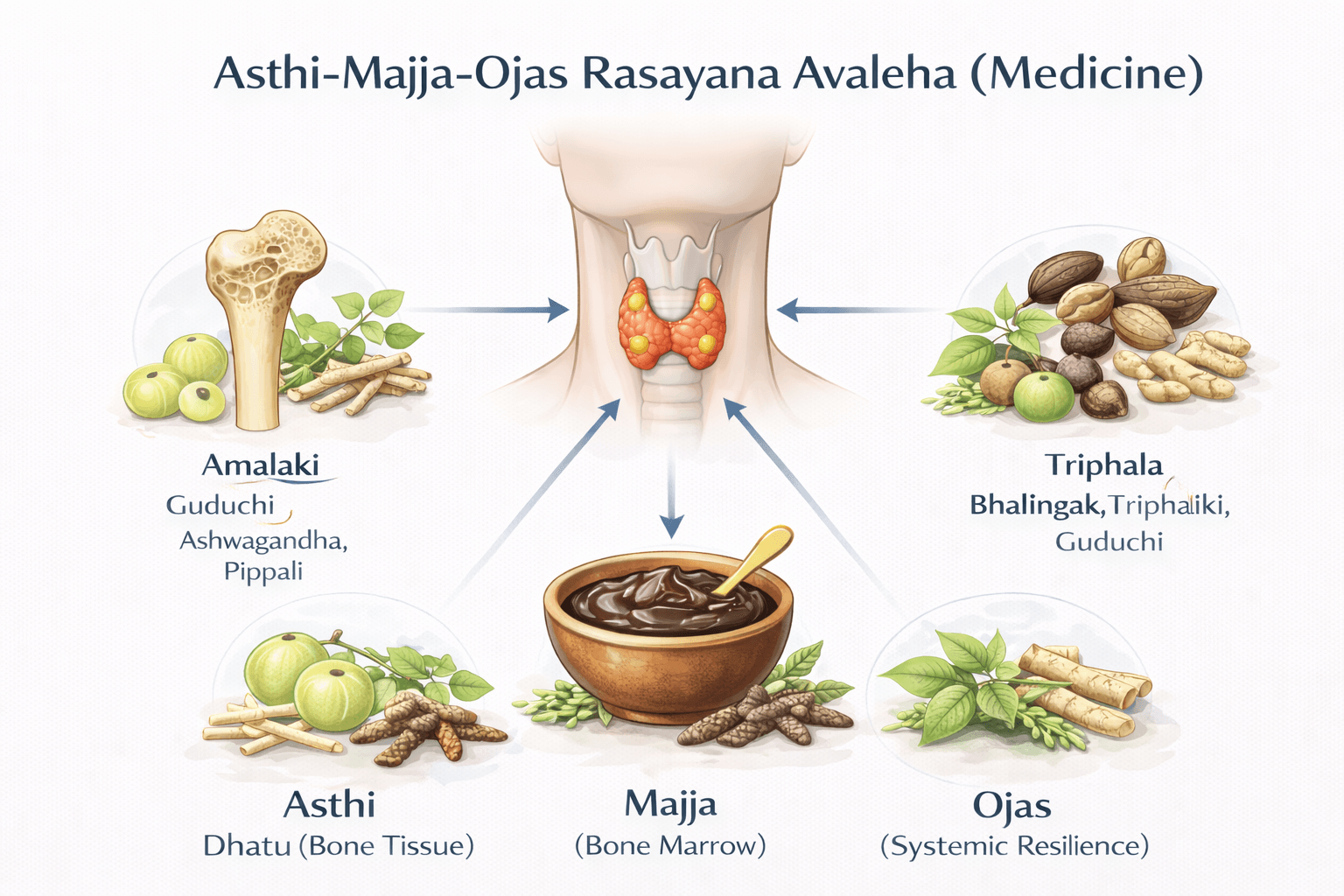
Name: Asthi-Majja-Ojas Rasayana Avaleha (Medicine)
Ingredients
Main Herbal Interventions
- Ashwagandha (Withania somnifera) – Vata pacifying, bone/muscle strength
- Arjuna (Terminalia arjuna) – Asthi support, cardiac protection
- Shatavari (Asparagus racemosus) – Pitta pacifying, nourishes dhatus
- Guduchi (Tinospora cordifolia) – Tridosha balancing, Rasayana, immunomodulator
- Amalaki (Emblica officinalis) – Potent Rasayana, antioxidant, calcium absorption enhancer
- Bala (Sida cordifolia) – Neuromuscular support, Vata pacifier
- Gokshura (Tribulus terrestris) – Supports urinary tract, prevents stones
- Varun (Crataeva nurvala) – Specific for Mutrashmari (urinary calculi)
- Punarnava (Boerhavia diffusa) – Diuretic, balances Kapha and Pitta
- Manjistha (Rubia cordifolia) – Rakta Shodhana (blood purifier)
- Sariva (Hemidesmus indicus) – Rakta Dushti correction, cooling, Pitta pacifier
Mineral Formulations (Shuddha and classical)
- Praval Pishti (Coral calcium) – Natural calcium source, bone strengthening
- Mukta Bhasma / Mukta Sukti Bhasma (Pearl/oyster shell calx) – Calcium rich, cooling
- Godanti Bhasma (Gypsum calx) – Pitta pacifier, calcium supply
- Abhrak Bhasma (Mica calx) – Majja Rasayana, improves nerve and marrow health
- Lauh Bhasma (Iron calx) – Rakta dhatu support, strengthens Ojas
- Swarnamakshik Bhasma (Chalcopyrite calx) – Supports metabolism and endocrine functions
- Rajata Bhasma (Silver calx) – Nervine tonic, cooling, Rakta protector
- Svarna Bhasma (Gold calx) – Rasayana, enhances immunity and Ojas
- Trivanga Bhasma (Lead, Tin, Zinc compound) – Corrects metabolic imbalances
- Sphatika Bhasma (Alum calx) – Cooling, Rakta Shodhana, stone prevention
Rasayana Supports
- Amalaki Rasayana – Base Rasayana
- Gandhak Rasayan (purified sulfur Rasayana) – Tissue rejuvenator
- Chyawanprash (optional) – Classic Avaleha base if desired
Base & Carriers
- Cow’s Ghee (Go Ghrita) – Enhances Rasayana effect, pacifies Vata
- Jaggery (Guda) or Sharkara (Sugar) – Sweet base, stabilizes formulation
- Honey (Madhu) – Yogavahi (catalyst), increases tissue penetration
Dietary Powders
- Sesame seed (Tila) powder – Rich in calcium and oil, supports Asthi dhatu
- Drumstick leaf (Moringa) powder – Calcium, vitamin D, and micronutrients
Preparation Method (Avaleh Kalpana as per Bhaishajya Ratnavali)
- Prepare a decoction (Kwatha) with Ashwagandha, Arjuna, Shatavari, Guduchi, Amalaki, Bala, Gokshura, Varun, Punarnava, Manjistha, Sariva (16 parts water, reduced to 1/4th).
- Add jaggery/sugar to the decoction and boil until Avaleha consistency forms.
- Incorporate cow’s ghee slowly while stirring.
- At the final stage, add all mineral formulations (Praval, Mukta Sukti, Godanti, Abhrak, Lauh, Swarnamakshik, Rajata, Svarna, Trivanga, Sphatika Bhasma) + Amalaki Rasayana and Gandhak Rasayan.
- Allow to cool slightly, then add honey.
- Mix in sesame seed powder and drumstick leaf powder.
- Store in an airtight glass container.
Dosage & Anupana
- Dose: 10–15 g twice daily
- Anupana (vehicle): Warm milk or lukewarm water
- Course: 3–6 months under supervision
Ayurvedic Action
- Rasayana – rejuvenates tissues, restores Ojas
- Asthi Dhatu Poshaka – nourishes bone tissue (Praval, Mukta, Godanti, Sesame)
- Majja Rasayana – supports marrow and nerves (Abhrak, Ashwagandha, Shatavari)
- Rakta Shodhana – blood purification, tumor prevention (Manjistha, Sariva, Sphatika)
- Mutravaha Srotas Shuddhi – prevents stones, protects kidneys (Gokshura, Varun, Punarnava)
- Ojasvardhaka – boosts immunity and vitality (Svarna, Rajata, Gandhak Rasayan)
Indications
- Hyperparathyroidism – prevents bone resorption, balances calcium, reduces stones
- Hypoparathyroidism – relieves spasms, tetany, neuromuscular irritability
- Parathyroid cancer – Rasayana and Rakta Shodhana for recurrence prevention, immune strengthening
Critical Warning About Market Purchased Avaleha and Self Preparation
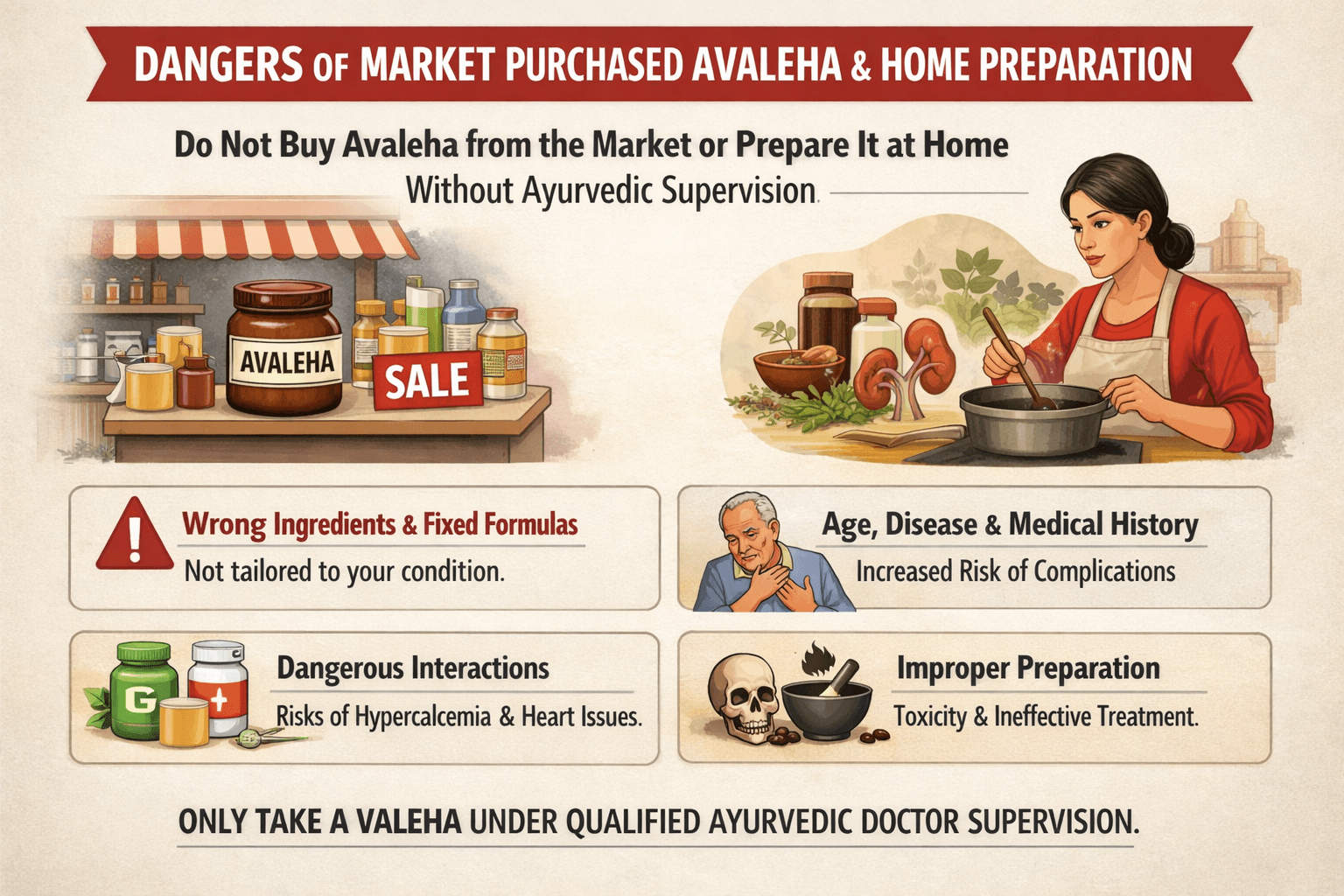
Ayurvedic Avaleha used in parathyroid related disorders is not a general health supplement and it is not meant for unsupervised use. In my clinical experience, patients who purchase Avaleha from the open market or attempt to prepare it themselves rarely achieve correction of the disease. In many cases, symptoms persist, progress slowly, or worsen due to improper formulation and lack of clinical oversight. If you are seeking cure through Ayurveda, it is essential to understand why this approach does not work.
Why Market Purchased Avaleha Fails in Parathyroid Disorders
Parathyroid disorders are endocrine conditions with significant variation between individuals. One patient may have primary hyperparathyroidism, another may have hypoparathyroidism following thyroid surgery, another may have secondary parathyroid involvement due to chronic kidney disease, while another may show parathyroid hormone elevation related to vitamin D deficiency. A fixed commercial Avaleha formula cannot address these different disease mechanisms and therefore cannot deliver cure.
Age and life stage play a decisive role. Calcium metabolism differs in children, adults, elderly individuals, and pregnant or breastfeeding women. Bone turnover, renal handling of minerals, and cardiovascular risk change with age. Market Avaleha products are not designed to adapt to these physiological differences, making them ineffective or unsafe in many situations.
Disease stage is equally important. Early stage imbalance may respond to metabolic correction and Rasayana support, whereas advanced disease with kidney stones, osteoporosis, fractures, seizures, cardiac rhythm disturbances, or vascular calcification requires staged therapy and close monitoring. Market products do not recognize disease progression and therefore fail to provide appropriate therapeutic sequencing.
Past surgical history changes endocrine stability. Patients who develop hypoparathyroidism after thyroid or neck surgery often have fragile calcium balance. In such cases, incorrect ingredients, dosing, or timing can precipitate muscle spasms, seizures, or cardiac instability. Commercial products do not account for post surgical physiology or long term risk.
Chronic medical conditions further complicate treatment response. Individuals with chronic kidney disease, recurrent kidney stones, diabetes, liver disorders, autoimmune diseases, chronic digestive disorders, osteoporosis, or long term steroid use require carefully modified formulations. Market Avaleha does not consider renal clearance, vascular calcification risk, or metabolic reserve, which leads to failure or harm.
Interactions with existing medicines are frequently overlooked. Many patients are already taking calcium supplements, vitamin D, calcitriol, thyroid hormone, diuretics, antiepileptic drugs, or dialysis related medications. Without supervision, combining these with market Avaleha can worsen hypercalcemia, trigger hypocalcemia fluctuations, or destabilize cardiac rhythm.
Individual constitution and Dosha dominance are fundamental in Ayurveda. Vata dominant individuals are prone to spasms, dryness, anxiety, and tissue depletion. Pitta dominant individuals are prone to inflammation and metabolic excess. Kapha dominant individuals are prone to sluggish metabolism and stone formation. Market Avaleha ignores these differences and often aggravates the wrong Dosha.
Digestive strength determines whether any medicine will work. Many patients have weak digestion, malabsorption, chronic constipation, or gut inflammation. Without correcting Agni and tissue metabolism, even high quality ingredients fail to act effectively. Market products do not assess or correct digestive capacity.
Quality and processing of ingredients vary widely in commercial preparations. Classical Avaleha requires precise heating stages, correct sequencing, and carefully selected raw materials. Industrial shortcuts, preservatives, excessive sweeteners, and long shelf storage reduce Rasayana potency and therapeutic depth.
Timing and Anupana are integral to treatment success. Avaleha must be taken at the correct time of day and with a specific carrier based on disease state and constitution. Market products do not provide individualized guidance, resulting in unpredictable absorption and inconsistent outcomes.
Ongoing monitoring is essential in endocrine disorders. Parathyroid related treatment requires periodic assessment of serum calcium, phosphate, vitamin D, kidney function, and sometimes urine calcium or bone density. Market use offers no follow up framework and delays detection of complications.
Why Buying Avaleha From the Market Can Be Harmful
In hyperparathyroidism, calcium levels may already be elevated. Inappropriate formulations can worsen hypercalcemia, dehydration, kidney stone formation, mental confusion, and cardiovascular risk. In hypoparathyroidism, unsupervised dosing can provoke tetany or seizures. In individuals with kidney disease, inappropriate mineral intake may accelerate vascular calcification and systemic complications.
Commercial products may not follow strict classical purification protocols, particularly when mineral ingredients are involved. Improper processing increases the risk of toxicity or therapeutic failure, creating false reassurance and delaying appropriate care.
Why Self Preparation of Avaleha Must Never Be Attempted
Patients must never attempt to prepare Avaleha at home. Avaleha preparation is a specialized pharmaceutical process that requires precise control of heat, correct identification of cooking stages, accurate sequencing of ingredients, and deep understanding of drug compatibility. Even small errors can destroy medicinal value or create harmful byproducts.
When mineral ingredients such as Bhasma or Pishti are involved, home preparation becomes dangerous. Proper purification and processing require specialized training. Without this expertise, risks include contamination, incorrect dosing, kidney strain, and worsening of calcium imbalance.
Self preparation also leads to inconsistent potency. Each batch differs in strength, making endocrine regulation unpredictable and unsafe.
Why Supervision by an Ayurvedic Physician Is Mandatory
Parathyroid disorders require individualized planning. A qualified Ayurvedic physician evaluates age, constitution, disease type, disease stage, laboratory values, kidney function, bone health, surgical history, chronic illnesses, current medications, digestive strength, and stress factors. Only then can the appropriate Avaleha composition, dosage, timing, Anupana, and duration be determined.
In clinical practice, formulations are adjusted based on response and follow up investigations. This dynamic correction is essential for safety and cure and cannot be achieved through market products or self preparation.
Final Advisory to Patients
If you are serious about curing parathyroid related disorders through Ayurveda, do not buy Avaleha from the market and do not attempt self preparation. These approaches do not work due to multiple individualized factors and may cause harm. Always follow a supervised Ayurvedic treatment plan under a qualified physician, supported by appropriate diagnostic monitoring and safety principles.
FAQs
What are the main symptoms of parathyroid disorders?
Parathyroid disorders present differently depending on hormone imbalance. Hyperparathyroidism often causes kidney stones, bone pain, fatigue, and digestive issues Hypoparathyroidism leads to muscle cramps, tetany, tingling around the mouth and extremities, and in severe cases, seizures.
How are parathyroid disorders diagnosed?
Diagnosis involves blood tests for calcium, phosphate, vitamin D, and PTH. Imaging such as ultrasound or sestamibi scans helps detect abnormal glands, while bone density scans reveal osteoporosis or bone weakening
Are parathyroid disorders common?
They are not as common as thyroid disorders but are increasingly seen due to lifestyle changes, rising cases of chronic kidney disease, and complications from thyroid surgeries affecting the parathyroid glands
What is the difference between hyperparathyroidism and hypoparathyroidism?
Hyperparathyroidism results from excess PTH, raising calcium levels in the blood. Hypoparathyroidism is due to insufficient PTH, causing low calcium and symptoms of neuromuscular irritability
Can Ayurveda help in parathyroid disorders?
Yes. Ayurveda provides holistic management by correcting dosha imbalances and nourishing dhatus. Remedies include Praval Pishti, Mukta Sukti Bhasma, Godanti Bhasma, and herbs like Ashwagandha, Guduchi, and Shatavari, which support calcium metabolism and bone strength
Is surgery always needed for parathyroid problems?
Surgery is the primary treatment for severe primary hyperparathyroidism or cancer. However, milder cases may be managed through monitoring, medication, dietary changes, and supportive Ayurvedic therapies
What diet is recommended for parathyroid disorders?
A calcium-rich diet is essential, including milk, sesame, leafy greens, and drumstick leaves. Sunlight exposure is vital for vitamin D. Ayurveda advises limiting sour and salty foods in hyperparathyroidism, while hypoparathyroidism patients benefit from warm, nourishing meals
Are Ayurvedic mineral formulations safe?
Classically prepared Bhasmas, when properly purified according to Rasashastra, are considered safe and effective. However, they must only be taken under the supervision of an Ayurvedic physician to avoid misuse or heavy metal toxicity
Can parathyroid disorders be prevented?
Complete prevention is not always possible, but lifestyle modification helps. Adequate calcium and vitamin D intake, regular sunlight exposure, and Ayurvedic Rasayana therapies strengthen bone and glandular function, reducing susceptibility
About the Doctor
Dr. Arjun Kumar is a qualified Ayurvedic physician with a focused clinical interest in chronic, metabolic, endocrine, and viral disorders. His work is grounded in the classical Ayurvedic principle that disease can be cured by identifying and correcting its root causes, rather than merely suppressing symptoms.
Dr. Kumar’s clinical approach is based on detailed assessment of Dosha imbalance, Dhatu involvement, Agni dysfunction, and Srotas pathology, with particular emphasis on Asthi Dhatu and Majja Dhatu disorders in endocrine conditions. He applies Rasayana therapy, personalized formulations, dietary regulation, and lifestyle correction as central tools aimed at long-term disease resolution and restoration of physiological balance, when applied appropriately and under medical supervision.
While firmly rooted in classical Ayurvedic medicine, Dr. Kumar recognizes the importance of modern diagnostics, laboratory monitoring, and emergency or surgical care where required. His practice follows an integrative yet Ayurveda-first philosophy, where modern medicine is used for diagnosis and stabilization, and Ayurveda is applied for curative, restorative, and preventive healing.
In addition to clinical practice, Dr. Kumar is actively involved in medical writing and research-based education. His work seeks to present Ayurveda as a complete, curative medical science, communicated responsibly and transparently for a global audience, without compromising patient safety or ethical standards.
Medical Disclaimer
This article is intended for educational and informational purposes only and is based on both modern medical literature and classical Ayurvedic medical texts. Parathyroid disorders are complex endocrine conditions, and medical evaluation, diagnosis, and monitoring by qualified healthcare professionals are essential.
Ayurveda, as a complete medical system, aims at curing disease by correcting root causes, restoring tissue balance (Dhatu Samya), regulating metabolism (Agni), and strengthening the body’s inherent healing capacity. When applied correctly, individually, and under proper medical supervision, Ayurvedic treatment is intended not merely for symptom control but for long-term resolution and disease reversal, wherever clinically feasible.
At the same time, this article recognizes that certain situations such as severe hypercalcemia, seizures, cardiac disturbances, or suspected malignancy require immediate modern medical or surgical intervention. In such cases, Ayurvedic treatment should be used integratively and sequentially, not as a replacement for emergency care.
Readers are strongly advised not to self-medicate, especially with mineral or herbomineral formulations. Ayurvedic medicines must be prescribed by a qualified Ayurvedic physician after proper assessment of diagnosis, disease stage, comorbidities, and individual constitution. Special caution is required in pregnancy, chronic kidney disease, history of kidney stones, or advanced systemic illness.
If symptoms such as confusion, seizures, severe muscle spasms, chest pain, or persistent vomiting occur, immediate medical attention is mandatory.
References
- Roumpou, A., & et al. (2025). Bone in Parathyroid Diseases Revisited. Endocrine Reviews, 46(4), 576-596. https://doi.org/10.1093/edrv/8104766
- Lee, M., & et al. (2019). Parathyroid hormone signaling in bone and kidney. Journal of Endocrinology, 241(2), R1-R14. https://doi.org/10.1530/JOE-18-0585
- Taniegra, E.D. (2004). Hyperparathyroidism. American Family Physician, 69(2), 333-339. https://www.aafp.org/pubs/afp/issues/2004/0115/p333.html
- Rejnmark, L., & et al. (2024). Treatment of hypoparathyroidism by re-establishing calcium homeostasis. Endocrinology and Metabolism, 39(1), 13-22. https://doi.org/10.3803/EnM.2024.1916
- Shankar, D., & Valiathan, M.S. (2007). Concepts and principles of Ayurveda. Ancient Science of Life, 26(3), 1-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3336313/
- Sharma, R.K., & Dash, B. (Eds.). (2005). Charaka Samhita (Vol. 2: Chikitsa Sthana, Asthi Dhatu Kshaya Adhyaya). Chowkhamba Sanskrit Series.
- Ureña-Torres, P., & et al. (2018). Report of The Parathyroid Day in Chronic Kidney Disease. Frontiers in Medicine, 5, 183. https://doi.org/10.3389/fmed.2018.00183
- Brandi, M.L., & et al. (2016). Management of hypoparathyroidism: summary statement and guidelines. Journal of Clinical Endocrinology & Metabolism, 101(6), 2273-2283. https://doi.org/10.1210/jc.2015-3907
- Fraser, W.D. (2009). Hyperparathyroidism. Lancet, 374(9684), 145-158. https://doi.org/10.1016/S0140-6736(09)60507-9
- Yeh, M.W., & et al. (2013). Surgery for primary hyperparathyroidism: a review. JAMA, 310(24), 2601-2610. https://doi.org/10.1001/jama.2013.282341
- Ketteler, M., & et al. (2025). Chronic kidney disease–mineral and bone disorder. Kidney International, 107(2), 192-208. https://doi.org/10.1016/j.kint.2024.11.018
- Indu, S., Kumar, P.A., Rao, S.K., & Jayaram, H. (2019). Ayurvedic perspective of calcium supplementation: A review. Vitamins & Minerals, 8, Article 185. https://www.researchgate.net/publication/341296797
- Khan, A.A., & et al. (2017). Standards of care for hypoparathyroidism in adults. Nature Reviews Endocrinology, 13, 550-561. https://doi.org/10.1038/nrendo.2017.56
- Bhadada, S.K., & et al. (2011). Dietary calcium intake and serum vitamin D in patients with primary hyperparathyroidism. Indian Journal of Endocrinology and Metabolism, 15(4), S141-S145. https://doi.org/10.4103/2230-8210.84863
- Joshi, N., & et al. (2015). Standardization and quality control parameters for Muktā (pearl) Bhasma/Pishti. Ancient Science of Life, 34(3), 138-143. https://doi.org/10.4103/0257-7941.157152
- Singh, A., Dubey, S.D., Patney, S., Kumar, V., & et al. (2010). Acute and subchronic toxicity study of calcium-based Ayurvedic Bhasmas and Pishti prepared from marine animals. Journal of Herbal Medicine & Toxicology, 4(1), 35-47. https://www.researchgate.net/publication/268432951
- Reddy, P.N., Lakshmana, M., & et al. (2003). Effect of Praval Bhasma (coral calx) in prevention of calcium and estrogen-deficient bone loss. Journal of Ethnopharmacology, 84(2-3), 259-264. https://doi.org/10.1016/S0378-8741(02)00327-2
- Kamble, S., Wanjari, A., Rathi, B., & Rajput, D. (2021). Pharmaceutico-analytical study of Muktashukti Pishti and Bhasma and comparative evaluation of oral bioavailability. Journal of Pharmaceutical Research International, 33(31B), 1-9. https://doi.org/10.9734/jpri/2021/v33i31B31680
- Patgiri, B., & Prajapati, P.K. (2015). Safety and efficacy of Ayurvedic mineral preparations. Ancient Science of Life, 34(1), 1-9. https://doi.org/10.4103/0257-7941.150771
- Valiathan, M.S. (2009). The Legacy of Charaka. Orient Blackswan.