- What is Pancreatic Diabetes?
- Why Pancreatic Diabetes Is Commonly Misdiagnosed as Type 2 Diabetes
- When to Suspect Type 3c Diabetes
- Type 3c Diabetes vs Type 1 and Type 2 Diabetes
- Pathophysiology
- Clinical Features
- Common and Rare Disorders Associated With Pancreatic Diabetes
- Rare but Clinically Important Associations
- Diagnosis
- Diagnostic Criteria for Pancreatic Diabetes (Type 3c Diabetes)
- Complications
- Management
- Avaleha to Cure Pancreatic Diabetes (Type 3c Diabetes)
- Important Medical Warning Before Using Avaleha and Mineral Preparations
- Risk of Self-Preparation Without Ayurvedic Medical Supervision
- Why Physician-Guided Clinical Customization Is Essential
- Prognosis and Can Pancreatic Diabetes Be Reversed?
- Long-Term Complications if Pancreatic Diabetes Is Not Treated Correctly
- Final Conclusion: A Root-Cause Approach to Pancreatic Diabetes
- Frequently Asked Questions (FAQs)
- Reference
Type 3c Diabetes Mellitus, also known as Pancreatogenic Diabetes, arises from diseases that damage the pancreas, such as chronic pancreatitis, pancreatic cancer, cystic fibrosis, or pancreatic surgery. It involves both endocrine failure (loss of insulin and glucagon secretion) and exocrine insufficiency (digestive enzyme deficiency) [42]. This dual impairment causes malnutrition, unstable glucose levels, and metabolic derangement, making it clinically distinct from other diabetes types.
Distinction from Type 1 and Type 2 Diabetes
Type 1 diabetes is autoimmune in origin, while Type 2 results primarily from insulin resistance and obesity. In contrast, Type 3c diabetes occurs secondary to structural pancreatic damage, leading to simultaneous endocrine and digestive dysfunction [55]. Patients often exhibit low insulin, glucagon, and pancreatic polypeptide levels [61], which heightens the risk of hypoglycemia during treatment [48]. Because its symptoms overlap with Type 2 diabetes, many cases remain misdiagnosed [42].
Epidemiology and Global Prevalence
Globally, 5–10 % of diabetes cases are estimated to be Type 3c, yet most remain unrecognized [44]. In chronic pancreatitis patients, prevalence can exceed 70 % depending on disease severity and duration [61]. Studies suggest that nearly one in three Type 2 diabetes diagnoses may actually represent unrecognized pancreatogenic diabetes [55]. Underdiagnosis leads to inadequate enzyme therapy, poor glycemic control, and accelerated pancreatic decline [48].
Importance of Early Recognition and Holistic Management
Early diagnosis is vital to prevent irreversible pancreatic damage, nutrient deficiency, and metabolic instability [44]. Conventional therapy focusing only on insulin fails to correct the digestive and absorptive dysfunction central to the disease. Ayurveda describes this as Agnimandya (weakened digestive fire) and Prameha (metabolic derangement due to Kapha–Pitta imbalance), emphasizing correction of Agni and restoration of Ojas [72]. A combined strategy—integrating modern diagnostics with Ayurvedic Rasayana and detoxification therapy—offers a root-cause approach to restoring pancreatic function and stabilizing metabolism [73].
What is Pancreatic Diabetes?
Pancreatic diabetes, or Type 3c diabetes, is a form of diabetes caused by diseases of the pancreas in which insulin deficiency, glucagon impairment, and digestive enzyme failure occur together, leading to unstable blood glucose levels, malabsorption, and progressive weight loss.
Why Pancreatic Diabetes Is Commonly Misdiagnosed as Type 2 Diabetes
Pancreatic diabetes is frequently mistaken for Type 2 diabetes because both present with elevated blood glucose levels. However, patients with Type 3c diabetes often have a history of pancreatitis, pancreatic pain, unexplained weight loss, fat malabsorption, or pancreatic surgery. They typically do not have the classical long history of obesity-driven insulin resistance. Failure to recognize this distinction leads to poor glycemic control, worsening malnutrition, and repeated treatment failure.
When to Suspect Type 3c Diabetes
Pancreatic diabetes should be suspected when diabetes develops in a patient with a known history of chronic pancreatitis, recurrent pancreatic inflammation, pancreatic surgery, or pancreatic tumor. In these individuals, the onset of hyperglycemia is not primarily driven by long-standing obesity or classical insulin resistance but by progressive destruction of pancreatic tissue and loss of both endocrine and exocrine function. This distinction is clinically important because standard Type 2 diabetes management alone often fails to control symptoms.
Unexplained weight loss despite adequate food intake is another major warning sign. Unlike Type 2 diabetes, where weight gain or metabolic syndrome is common, patients with Type 3c diabetes frequently experience progressive loss of body mass due to maldigestion, nutrient deficiency, and reduced anabolic action of insulin. This is often accompanied by fatigue, muscle wasting, and reduced strength, reflecting combined metabolic and digestive failure.
Bulky, oily, foul-smelling stools that are difficult to flush indicate fat malabsorption due to pancreatic exocrine insufficiency. This feature is a key clinical differentiator because it is not a typical finding in Type 2 diabetes. The presence of steatorrhea, abdominal bloating, and post-meal discomfort strongly suggests underlying pancreatic pathology rather than primary insulin resistance.
Frequent or unpredictable hypoglycemia during standard diabetes therapy is another important clue. Damage to alpha cells reduces glucagon secretion, impairing the body’s natural defense against falling glucose levels. As a result, even conventional insulin doses or oral hypoglycemic agents may produce sudden glucose drops, making glycemic control unstable and difficult.
A past history of pancreatic surgery, pancreatic trauma, cystic fibrosis, or pancreatic malignancy should always prompt evaluation for Type 3c diabetes when glucose abnormalities appear. In such cases, the diabetes is secondary to loss of functional pancreatic mass and requires a treatment strategy that addresses enzyme deficiency, nutrient absorption, and metabolic instability rather than glucose control alone.
This clinical pattern clearly distinguishes Type 3c diabetes from classical Type 2 diabetes and indicates the need for a pancreatic-focused, integrative therapeutic approach.
Type 3c Diabetes vs Type 1 and Type 2 Diabetes
Pancreatic diabetes differs fundamentally from both Type 1 and Type 2 diabetes in its origin, metabolic behavior, and clinical progression.
Type 1 diabetes is an autoimmune condition that causes rapid destruction of beta cells and absolute insulin deficiency. Type 2 diabetes develops gradually and is driven primarily by insulin resistance, often associated with obesity, metabolic syndrome, and long-standing hyperinsulinemia.
Type 3c diabetes, in contrast, is caused by structural damage to the pancreas. The defining feature is the simultaneous presence of insulin deficiency, impaired glucagon response, and exocrine pancreatic insufficiency. Because glucagon production is reduced, patients are highly vulnerable to hypoglycemia. Because digestive enzyme production is reduced, they develop malabsorption, micronutrient deficiency, and progressive weight loss.
Unlike Type 2 diabetes, these patients often do not respond predictably to standard oral anti-diabetic drugs. Nutritional decline, unstable glucose levels, and persistent gastrointestinal symptoms continue unless the pancreatic component is addressed.
From an Ayurvedic perspective, this represents a transition from Kapha-dominant Prameha to a Vata-dominant Dhatu-kshaya state, where tissue depletion, impaired absorption, and loss of metabolic stability become the dominant features.
| Feature | Type 1 Diabetes | Type 2 Diabetes | Type 3c Diabetes (Pancreatic Diabetes) |
|---|---|---|---|
| Primary cause | Autoimmune beta-cell destruction | Insulin resistance with relative insulin deficiency | Structural damage to the pancreas |
| Onset | Sudden | Gradual | After pancreatic disease or pancreatic surgery |
| Insulin production | Severely reduced or absent | Initially high, later reduced | Reduced |
| Glucagon response | Present | Present | Reduced |
| Exocrine pancreatic function | Normal | Normal | Impaired |
| Fat malabsorption | No | No | Common |
| Body weight pattern | Normal or low | Often overweight or obese | Progressive unintentional weight loss |
| Glycemic pattern | Persistent hyperglycemia | Stable in early stages | Marked glucose variability |
| Hypoglycemia risk | Moderate | Low | High |
| Response to oral anti-diabetic drugs | Poor | Good in early stages | Unpredictable |
| Nutritional status | Usually preserved | Often over-nourished | Malnutrition and micronutrient deficiency |
| Typical clinical history | Other autoimmune disorders | Metabolic syndrome | Pancreatitis, pancreatic cancer, pancreatic surgery, cystic fibrosis |
| Digestive symptoms | Absent | Absent | Bloating, steatorrhea, enzyme deficiency |
| Ayurvedic correlation | Ojakshaya | Kapha-dominant Prameha | Vata-dominant Dhatu-kshaya Prameha |
Pancreatic diabetes is the only form of diabetes in which endocrine and exocrine pancreatic failure occur together. The combination of malabsorption, unexplained weight loss, digestive disturbance, and unstable glucose levels in a patient with a history of pancreatic disease strongly suggests Type 3c diabetes rather than Type 2 diabetes.
Pathophysiology
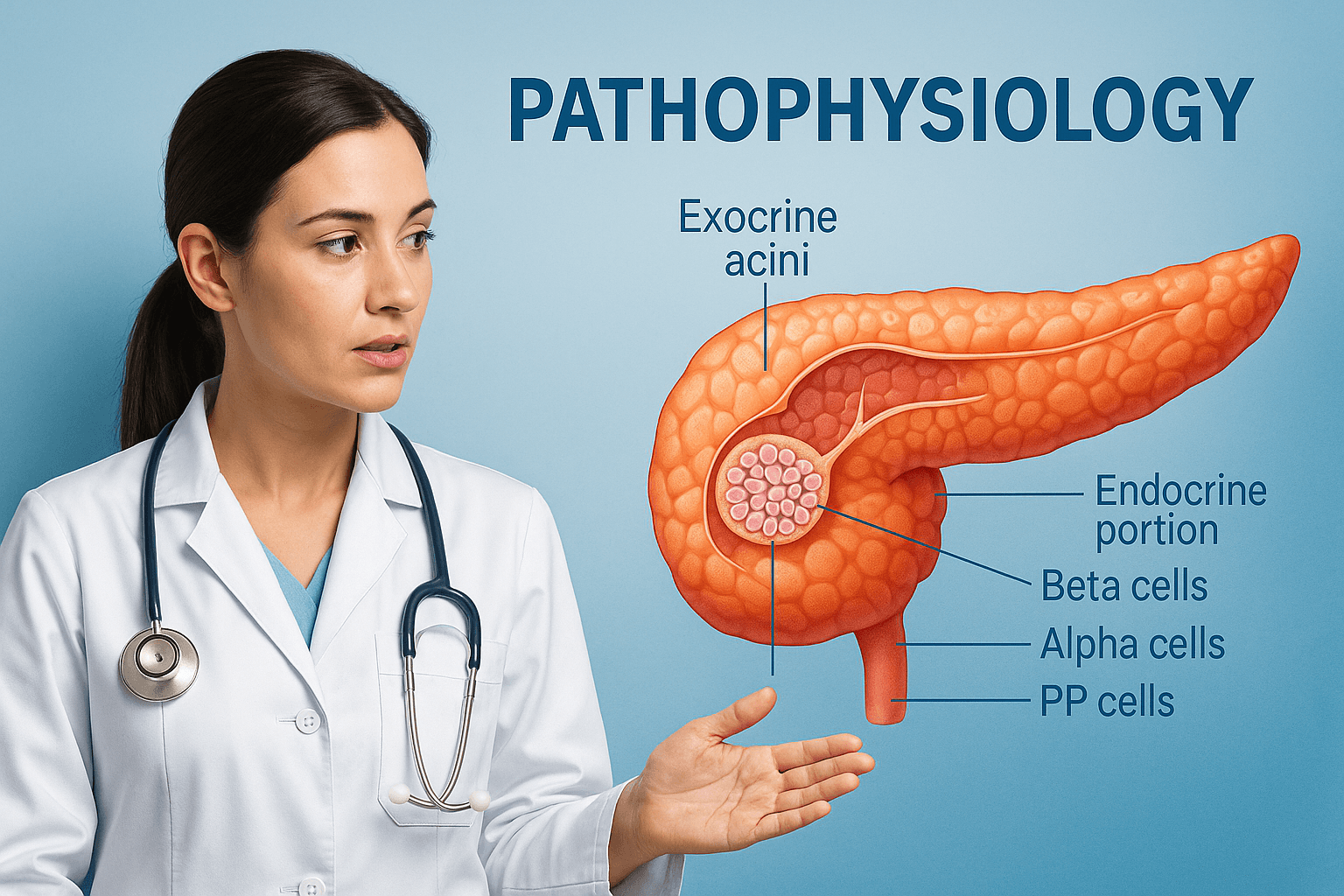
Anatomical and Functional Overview of the Pancreas
The pancreas functions as both an exocrine and endocrine gland. The exocrine portion, composed of acinar and ductal cells, secretes digestive enzymes such as amylase, lipase, and proteases that aid in nutrient digestion [44]. The endocrine portion contains the islets of Langerhans, which include four primary cell types: beta cells producing insulin, alpha cells producing glucagon, delta cells producing somatostatin, and PP cells producing pancreatic polypeptide [61]. In Pancreatic Diabetes or Type 3c Diabetes, both the endocrine and exocrine units are impaired, causing disturbances in glucose metabolism and digestion [42].
Mechanism of Pancreatic Damage Leading to β-Cell Destruction and Insulin Deficiency
In Type 3c Diabetes, prolonged inflammation, fibrosis, or necrosis damages pancreatic tissue, commonly due to chronic pancreatitis, trauma, or tumor infiltration [55]. Continuous inflammation leads to loss of beta-cell mass and reduced insulin secretion. Damage to acinar cells also disrupts enzyme production, resulting in maldigestion and nutrient deficiency, which further weaken beta-cell function [61]. Ayurveda describes this condition as Agnimandya or weakened digestive fire, and Pittaja Prameha, a metabolic disturbance caused by deranged Pitta that leads to depletion of Dhatus and Ojas [72].
Role of Glucagon Deficiency, Pancreatic Polypeptide Deficiency, and Malabsorption
Unlike Type 1 and Type 2 Diabetes, Type 3c involves alpha-cell dysfunction, leading to decreased glucagon secretion [48]. This reduction impairs the body’s ability to counter hypoglycemia. Loss of pancreatic polypeptide contributes to hepatic insulin resistance and disordered gastrointestinal motility [44]. Exocrine insufficiency results in fat malabsorption, deficiencies of vitamins A, D, E, and K, and steatorrhea. The combination of insulin deficiency, glucagon deficiency, and malabsorption causes erratic blood glucose fluctuations [61]. In Ayurvedic understanding, this reflects vitiation of Pitta and Vata, where weakened Pitta disturbs digestion and aggravated Vata causes irregular absorption and circulation of glucose [72].
Comparison of Insulin Resistance Patterns with Type 2 Diabetes
In Type 2 Diabetes, insulin resistance is the primary defect, while pancreatic function is initially preserved. In Type 3c Diabetes, insulin deficiency is the predominant factor with mild to moderate insulin resistance secondary to inflammation or nutritional deficiency [55]. Hepatic insulin resistance in this condition arises partly due to loss of pancreatic polypeptide and fatty infiltration in the liver caused by exocrine failure [48]. Consequently, patients experience unstable glycemic patterns rather than persistent hyperinsulinemia, which is typical of Type 2 Diabetes [44].
Oxidative Stress and Inflammatory Cytokine Involvement
Chronic pancreatic inflammation generates reactive oxygen species that cause oxidative stress and tissue injury. Cytokines such as TNF-α, IL-1β, and IL-6 contribute to beta-cell apoptosis and impaired insulin signaling [61]. Elevated oxidative markers and reduced antioxidant enzyme activity have been documented in Type 3c patients, highlighting the role of inflammation and oxidative injury in disease progression [55]. Ayurveda explains this as accumulation of Ama Dosha, or toxic metabolic residue, due to poor Agni leading to obstruction of microchannels and impaired tissue nourishment [73]. Rasayana herbs including Amalaki, Guduchi, and Haridra have been found beneficial in restoring cellular metabolism and reducing oxidative stress [72].
Clinical Features
General Presentation
Pancreatic Diabetes, or Type 3c Diabetes, develops gradually, often following years of pancreatic inflammation or damage [44]. Unlike Type 1 diabetes, where symptoms appear suddenly, or Type 2 diabetes, where obesity and insulin resistance dominate, Type 3c arises with subtle metabolic changes and digestive symptoms due to concurrent exocrine failure [42]. Patients often report fatigue, unintentional weight loss, bloating, and fluctuating glucose levels that are difficult to stabilize despite dietary compliance [61]. In Ayurveda, this corresponds to Agnimandya and Dhatukshaya, where poor digestive fire and tissue depletion cause loss of strength and vitality [72].
Digestive and Nutritional Symptoms
Because exocrine insufficiency accompanies endocrine failure, patients experience malabsorption, steatorrhea, and chronic diarrhea [61]. Fat-soluble vitamin deficiencies (A, D, E, and K) are common, leading to brittle nails, dry skin, bone pain, and poor wound healing. Abdominal distension, flatulence, and undigested food particles in the stool are characteristic signs of exocrine dysfunction [44]. Ayurvedic texts describe similar manifestations under Ajeerna and Ama Sanchaya, where incompletely digested food forms toxic metabolic residue that circulates throughout the body, disturbing Dosha balance and tissue nourishment [72].
Glycemic Instability
Patients with Type 3c Diabetes often experience wide fluctuations in blood glucose levels — alternating between hyperglycemia and hypoglycemia [48]. The absence of glucagon secretion from alpha cells impairs counter-regulatory mechanisms, while malnutrition limits hepatic glycogen reserves. This makes glucose variability a hallmark feature, and standard insulin doses may cause unpredictable drops in blood sugar [55]. Ayurveda interprets this instability as an Avarana condition, where aggravated Pitta and Kapha obstruct the normal flow of Vata, producing irregular metabolic rhythms [73].
Weight Loss and Muscle Wasting
Continuous nutrient malabsorption and inadequate insulin supply cause progressive weight loss and muscle wasting [61]. In advanced cases, cachexia develops, accompanied by low serum protein and fat levels. From the Ayurvedic viewpoint, this reflects Mamsa Dhatu Kshaya and Ojakshaya, where tissue depletion weakens structural integrity and immune resistance [72]. Rejuvenation through Rasayana herbs such as Ashwagandha, Shatavari, and Amalaki helps rebuild Dhatus and restore metabolic strength [73].
Vitamin and Micronutrient Deficiencies
Deficiency of vitamin D and calcium is common in Type 3c patients due to poor fat absorption [61]. Secondary hyperparathyroidism and osteopenia may result, increasing fracture risk. Deficiency of vitamin B12 is also observed because of impaired intrinsic factor activity. These deficiencies contribute to fatigue, neuropathy, and low mood. Ayurveda identifies these symptoms as depletion of Tejas and Prana, indicating low metabolic vitality and reduced Ojas [72].
Hypoglycemia Tendency
Due to loss of glucagon response and impaired hepatic glucose production, hypoglycemia episodes are more frequent and severe [48]. Patients may feel dizziness, sweating, confusion, and even fainting. The risk increases with insulin therapy or skipped meals. Ayurveda advises balancing Agni through light meals and Rasayana therapy to maintain stable energy flow and prevent Vata aggravation [73].
Comparison with Type 1 and Type 2 Diabetes
Clinically, Type 3c Diabetes shows features of both Type 1 and Type 2 but remains distinct in its pathogenesis [42]. Like Type 1, there is insulin deficiency, yet autoimmune markers are absent. Like Type 2, mild insulin resistance and metabolic syndrome can coexist, but exocrine dysfunction and nutritional deficiency make it unique. The combination of digestive and metabolic failure helps differentiate it when properly evaluated [44].
Psychological and Systemic Manifestations
Chronic fatigue, mood disturbances, and anxiety are frequent in Type 3c patients [55]. These stem from fluctuating glucose levels, nutritional imbalance, and chronic inflammation affecting brain neurotransmitters. Ayurveda attributes such symptoms to the aggravation of Vata in Majja Dhatu, which governs neural stability. Restoration of Majja balance through Rasayana herbs like Brahmi and Mandukaparni improves both mood and metabolic steadiness [72].
Common and Rare Disorders Associated With Pancreatic Diabetes
Pancreatic diabetes is rarely an isolated diagnosis. In most patients it is the metabolic consequence of a primary pancreatic disorder that damages endocrine islet tissue, disrupts exocrine enzyme secretion, or both. Correctly identifying the associated condition is essential because treatment and prognosis depend on addressing the pancreatic cause, correcting malabsorption, and preventing unstable glycemic events that are typical of Type 3c diabetes.
Chronic Pancreatitis
Chronic pancreatitis is the most frequent cause of pancreatic diabetes. Recurrent inflammation leads to progressive fibrosis, ductal distortion, calcification, and destruction of islet cells, alongside worsening exocrine insufficiency. As pancreatic enzyme output declines, patients develop fat malabsorption, vitamin deficiency, weight loss, and brittle glucose fluctuations. Any diabetes occurring in a patient with long standing pancreatic pain, recurrent pancreatitis, alcohol related pancreatic disease, or smoking related pancreatitis should be evaluated for Type 3c diabetes rather than being labeled as Type 2.
Recurrent Acute Pancreatitis
Repeated acute pancreatitis episodes can create cumulative pancreatic injury even when chronic pancreatitis has not yet been formally diagnosed. Over time, recurrent necroinflammatory damage may reduce islet reserve and cause progressive endocrine failure. Patients often show intermittent glucose intolerance first, followed by persistent hyperglycemia as pancreatic structure deteriorates.
Pancreatic Cancer
New onset diabetes in adults, particularly after the age of forty, can be an early metabolic manifestation of pancreatic malignancy. When hyperglycemia is accompanied by unexplained weight loss, early satiety, appetite decline, or rapid clinical deterioration, pancreatic cancer must be considered. In these cases the diabetes is secondary to tumor related tissue destruction and pancreatic metabolic disruption, and pancreatic imaging becomes clinically urgent.
Pancreatic Surgery and Pancreatectomy
Partial or total pancreatectomy results in loss of endocrine and exocrine function. These patients often develop severe insulin deficiency combined with enzyme deficiency, fat malabsorption, micronutrient depletion, and unstable glucose patterns due to impaired glucagon response. Management differs from classical diabetes and requires enzyme replacement support, structured nutrition, and careful insulin titration.
Pancreatic Duct Obstruction and Ductal Disorders
Obstruction of pancreatic ducts from strictures, stones, chronic scarring, or ductal anomalies can reduce enzyme delivery and contribute to progressive pancreatic injury. Over time, duct obstruction promotes inflammation and fibrosis, increasing the risk of endocrine dysfunction and pancreatogenic diabetes, especially when accompanied by recurrent abdominal pain and malabsorption.
Cystic Fibrosis
Cystic fibrosis causes thick secretions that obstruct pancreatic ducts, leading to progressive exocrine failure and eventual islet damage. Cystic fibrosis related diabetes is among the best defined forms of Type 3c diabetes, commonly associated with malnutrition, fat soluble vitamin deficiency, and glucose instability despite adequate caloric intake.
Hemochromatosis
Iron overload causes oxidative damage and iron deposition within pancreatic tissue, resulting in beta cell dysfunction and reduced insulin secretion. This form of pancreatic diabetes is often associated with liver disease, skin hyperpigmentation, joint symptoms, and hypogonadism. Recognition is clinically important because early management of iron overload may slow pancreatic injury and improve metabolic outcomes.
Fibrocalculous Pancreatic Diabetes
Fibrocalculous pancreatic diabetes is more common in tropical and resource limited regions. It develops in patients with long standing malnutrition and pancreatic ductal calcification. It typically presents at a younger age with low body weight, severe insulin deficiency, marked nutritional depletion, and brittle glycemic patterns. It differs from Type 2 diabetes because insulin resistance is not the dominant driver, and pancreatic failure is central.
Tropical Chronic Pancreatitis
Tropical chronic pancreatitis overlaps with fibrocalculous pancreatic diabetes but is clinically important as a broader entity. It may occur in younger individuals with chronic abdominal pain, pancreatic stones, and progressive exocrine failure. Diabetes develops as pancreatic reserve is lost, often accompanied by severe malnutrition and micronutrient deficiency.
Rare but Clinically Important Associations
Autoimmune Pancreatitis
Autoimmune pancreatitis is an immune mediated inflammatory condition that causes progressive pancreatic fibrosis and functional loss. It may mimic pancreatic cancer on imaging, making accurate assessment critical. Over time, endocrine and exocrine tissues are damaged, resulting in Type 3c diabetes with malabsorption and nutritional decline.
Genetic Pancreatic Disorders and Inherited Pancreatitis
Genetic mutations affecting pancreatic development, enzyme transport, or inflammatory pathways can cause early pancreatic insufficiency and diabetes. Inherited pancreatitis leads to recurrent inflammation from a young age, accelerating fibrosis and loss of islet function. These patients may present with early onset malabsorption, growth disturbance, and unstable glucose regulation.
Pancreatic Trauma
Blunt abdominal trauma, penetrating injury, or surgical trauma can destroy islet tissue or disrupt ductal structures, causing delayed endocrine failure. Diabetes may emerge months or years after injury, so a detailed trauma and surgical history is essential when unexplained diabetes develops.
Congenital Pancreatic Anomalies
Congenital conditions such as pancreatic agenesis, pancreatic hypoplasia, or anatomical anomalies affecting duct structure can reduce both endocrine and exocrine capacity. These disorders may cause early onset glucose dysregulation, malabsorption, poor weight gain, and micronutrient deficiency.
Non Alcoholic Fatty Pancreas Disease
Fat infiltration of the pancreas, increasingly recognized in individuals with metabolic syndrome, can generate local inflammation, oxidative stress, and beta cell dysfunction. Over time, pancreatic fat accumulation may impair enzyme secretion and contribute to a mixed pattern of insulin resistance and pancreatic insufficiency, placing some patients on a pathway toward pancreatogenic diabetes.
Drug Induced Pancreatitis and Secondary Pancreatic Injury
Certain drugs can trigger pancreatitis or contribute to pancreatic inflammation and injury, leading to secondary diabetes in susceptible patients. When diabetes develops after documented pancreatitis episodes linked to medication exposure, a pancreatogenic mechanism should be considered, especially if digestive symptoms persist.
Pancreatic Infections and Post Infectious Injury
Some infections can cause pancreatic inflammation and tissue injury. When diabetes develops after clinically significant pancreatic infection or post infectious pancreatic dysfunction, the resulting endocrine failure may fall under the Type 3c category, particularly if exocrine insufficiency coexists.
Chronic Pancreatic Duct Stone Disease
Severe duct stone burden can produce longstanding obstruction, recurrent inflammation, and progressive fibrosis. These patients often have chronic pain, steatorrhea, and gradual loss of endocrine capacity, leading to pancreatogenic diabetes that behaves differently from Type 2 diabetes.
Diagnosis
Modern Diagnostic Criteria
Diagnosis of Pancreatic Diabetes requires identifying both the endocrine insufficiency that causes glucose dysregulation and the exocrine dysfunction that leads to maldigestion [44]. Standard diabetic tests such as fasting plasma glucose, oral glucose tolerance test, and HbA1c may confirm hyperglycemia but cannot differentiate Type 3c from Type 1 or Type 2 Diabetes [42]. Therefore, additional parameters are necessary.
Low serum C-peptide levels indicate insulin deficiency caused by β-cell loss [55]. Fecal elastase-1 and serum trypsinogen tests are used to assess exocrine function, with reduced values confirming pancreatic enzyme insufficiency [61]. Imaging studies such as CT scan, MRI, or Endoscopic Ultrasound help detect pancreatic calcification, fibrosis, or ductal irregularities suggestive of chronic pancreatitis [44]. In autoimmune cases, raised IgG4 levels help identify autoimmune pancreatitis [55].
Unlike Type 1 diabetes, autoimmune antibodies (GAD, IA-2, or ZnT8) are usually absent in Type 3c Diabetes. Similarly, insulin resistance markers such as elevated fasting insulin are typically mild or absent, distinguishing it from Type 2 Diabetes [61]. These findings together confirm the diagnosis of Pancreatogenic Diabetes when pancreatic disease, exocrine dysfunction, and diabetes coexist.
Biochemical Findings
Patients commonly show low or fluctuating insulin and glucagon levels, reflecting endocrine failure [48]. Fat malabsorption leads to low cholesterol, triglyceride, and vitamin D levels. Serum amylase and lipase may be reduced in advanced stages due to atrophic acinar tissue [61]. Many patients also present with mild anemia and low serum albumin due to chronic malnutrition [55].
Differential Diagnosis
Pancreatic Diabetes is frequently misdiagnosed as Type 2 Diabetes because both can present with gradual onset of hyperglycemia [44]. However, the presence of digestive symptoms, weight loss, and malabsorption should prompt further pancreatic evaluation. In Type 1 Diabetes, patients often have ketosis and positive autoimmune markers, which are absent in Type 3c [42]. The co-existence of steatorrhea or vitamin deficiencies should always raise suspicion for a pancreatic origin [61].
Ayurvedic Diagnostic Approach
Ayurveda diagnoses Pancreatic Diabetes through observation of Nidana Panchaka which includes causes, prodromal symptoms, disease characteristics, prognosis, and complications [72]. Signs of Agnimandya such as poor appetite, heaviness, and fatigue are key indicators. In advanced stages, Prameha Lakshanas such as excessive urination, sweetness of urine, and debility appear. Pulse (Nadi) examination often reveals a Kapha–Pitta dominant pattern, indicating metabolic obstruction with impaired digestion [73].
Tongue observation may show coating from Ama accumulation, and skin examination may reveal dryness and lack of luster due to Ojakshaya. The Ayurvedic clinician correlates these findings with the underlying Srotas affected, particularly Annavaha Srotas (digestive channel) and Rasavaha Srotas (nutrient transport channel) [72].
Integrative Diagnostic Approach
An integrated diagnostic model combines modern imaging and biochemical testing with Ayurvedic assessment of Dosha imbalance and digestive fire [73]. Identifying pancreatic insufficiency early allows for timely intervention with enzyme therapy and Rasayana treatment. This dual diagnostic approach not only classifies the disease accurately but also evaluates its root cause in both physical and energetic dimensions, ensuring a comprehensive treatment plan that addresses metabolism, digestion, and tissue health simultaneously [72].
Diagnostic Criteria for Pancreatic Diabetes (Type 3c Diabetes)
Pancreatic diabetes is frequently misdiagnosed as Type 2 diabetes because standard glucose testing alone cannot identify the underlying pancreatic damage. A correct diagnosis requires simultaneous evaluation of endocrine function, exocrine pancreatic status, and structural abnormalities of the pancreas.
The diagnosis should be suspected in individuals who develop diabetes in the presence of chronic pancreatitis, pancreatic surgery, pancreatic calcification, unexplained malabsorption, or persistent gastrointestinal symptoms. In these patients, treating hyperglycemia alone leads to poor metabolic outcomes because the digestive and hormonal components of the disease remain unaddressed.
Laboratory Evaluation of Endocrine Function
Fasting plasma glucose and HbA1c confirm the presence of diabetes but do not define its type. In pancreatic diabetes, C-peptide levels are usually reduced, reflecting impaired endogenous insulin production. Autoimmune markers such as GAD antibodies are typically negative, which helps differentiate this condition from Type 1 diabetes.
Glucose variability with frequent hypoglycemic episodes, especially after initiation of insulin or oral drugs, is a strong clinical clue because the glucagon response is lost.
Assessment of Exocrine Pancreatic Insufficiency
Evaluation of exocrine function is essential for identifying Type 3c diabetes. Low fecal elastase levels indicate pancreatic enzyme deficiency and confirm exocrine insufficiency. Increased fecal fat content and reduced serum levels of fat-soluble vitamins further support the diagnosis.
Patients often present with a history of bloating, steatorrhea, early satiety, and progressive weight loss despite adequate calorie intake. These features are not typical of classical Type 2 diabetes and should always prompt pancreatic evaluation.
Pancreatic Imaging
Structural abnormalities of the pancreas provide the most important diagnostic evidence.
Contrast-enhanced CT, MRI, or endoscopic ultrasound may reveal pancreatic atrophy, ductal dilatation, calcification, fibrosis, mass lesions, or post-surgical changes. The presence of these findings in a patient with diabetes strongly supports Type 3c diabetes.
Early imaging is particularly important in new-onset diabetes after the age of forty, as it may help detect occult pancreatic malignancy at a potentially curable stage.
Differentiating Type 3c from Type 2 Diabetes
In Type 2 diabetes, insulin resistance is the dominant mechanism and C-peptide levels are normal or elevated in the early phase. Obesity, metabolic syndrome, and long asymptomatic hyperglycemia are typical.
In pancreatic diabetes, patients are often lean or experience progressive weight loss, show evidence of malabsorption, have low or declining C-peptide levels, and demonstrate pancreatic structural abnormalities on imaging. Glycemic control becomes unstable when standard oral drugs are used because the underlying disease is not insulin resistance but pancreatic tissue loss.
Ayurvedic Diagnostic Correlation
From an Ayurvedic perspective, this condition represents an advanced stage of Prameha associated with severe Agnimandya, Dhatu-kshaya, and Ojas depletion rather than a Kapha-dominant metabolic excess.
Clinical assessment includes evaluation of digestive strength, bowel characteristics, progressive weight loss, fatigue, and signs of nutrient depletion. The presence of chronic Grahani-like symptoms with Madhumeha features indicates involvement of both Annavaha and Medovaha Srotas with Vata predominance in the later stage.
Recognition of this transition is essential because the therapeutic goal shifts from simple Kapha-meda reduction to Agni restoration, Dhatu nourishment, and Rasayana-based pancreatic rejuvenation.
Complications
Acute Complications
Pancreatic Diabetes patients are more prone to hypoglycemia because of the loss of glucagon secretion and impaired hepatic glucose production [48]. Even small doses of insulin can cause severe glucose drops, especially in those with poor food absorption or irregular meals. Episodes of dizziness, sweating, or fainting are frequent and require careful glycemic monitoring. Ayurveda describes this state as Avarana of Vata, where irregular energy flow and impaired Agni create instability in tissue metabolism [73]. Restoring digestive strength and stabilizing Agni are essential to prevent recurrent hypoglycemia [72].
Another acute concern is acute pancreatitis flare-ups, which may be triggered by alcohol, fatty meals, or infections [44]. These flare-ups further damage pancreatic tissue and worsen both endocrine and exocrine dysfunction. Ayurvedic management focuses on balancing aggravated Pitta through cooling and anti-inflammatory herbs such as Amalaki, Guduchi, and Musta to prevent recurrence [72].
Chronic Complications
Over time, Type 3c Diabetes can lead to microvascular and macrovascular complications similar to other forms of diabetes, including retinopathy, neuropathy, and nephropathy [61]. However, the pattern is often more severe due to malnutrition and oxidative stress. Chronic inflammation and vitamin deficiencies exacerbate nerve damage, producing burning sensations, tingling, and muscle weakness [55]. Ayurveda identifies these manifestations as Vata Vyadhi, or disorders caused by deranged Vata in Majja Dhatu, requiring nourishing Rasayanas such as Ashwagandha, Bala, and Yashtimadhu [73].
Nutritional Deficiencies
Exocrine insufficiency leads to persistent fat-soluble vitamin deficiency, particularly vitamins A, D, E, and K [61]. This results in poor bone mineralization, visual weakness, skin dryness, and delayed wound healing. Vitamin D deficiency and calcium loss increase the risk of osteoporosis and fractures [44]. In Ayurveda, these reflect Asthi Dhatu Kshaya and Majja Dhatu Kshaya, where structural tissue degeneration occurs due to chronic depletion of metabolic energy [72]. Correcting Agni and enhancing Dhatu Poshana with herbal formulations such as Guduchi, Shatavari, and Abhrak Bhasma can restore bone and marrow integrity [73].
Hepatic and Gastrointestinal Effects
Loss of pancreatic polypeptide and enzyme deficiency affect liver metabolism and bile secretion, leading to hepatic steatosis and sluggish digestion [48]. Patients may also experience gallstones, bloating, and abdominal heaviness. Ayurveda relates these findings to Annavaha Srotas Dushti and Kapha–Pitta aggravation, suggesting therapies like Virechana (purgation) and Deepana–Pachana (metabolic stimulation) to restore normal digestive flow [72].
Cardiovascular and Metabolic Risks
Malnutrition, oxidative stress, and chronic inflammation accelerate atherosclerosis and cardiovascular disease in Type 3c Diabetes [55]. Dyslipidemia, endothelial dysfunction, and vitamin deficiency further worsen vascular integrity. Antioxidant therapy and lipid-lowering Ayurvedic herbs such as Arjuna, Guggulu, and Haridra are useful in mitigating these risks [73].
Pancreatic Cancer Risk
Chronic pancreatitis and fibrosis increase the long-term risk of pancreatic carcinoma, especially in patients with long-standing inflammation [44]. Repeated injury and oxidative stress can trigger cellular transformation. Ayurveda views this as chronic Granthi or Arbuda formation due to prolonged Srotorodha and Ama accumulation [72]. Early detoxification (Shodhana) and Rasayana therapy act as preventive measures by cleansing the channels and improving tissue resistance [73].
Psychological and Emotional Complications
Chronic fatigue, anxiety, and depression are common among patients with Pancreatic Diabetes [55]. They arise from hormonal fluctuations, nutrient deficiencies, and long-term stress of disease management. Ayurveda recognizes this as Manasika Vyadhi arising from Vata–Pitta imbalance in Majja Dhatu and recommends medhya Rasayanas such as Brahmi, Shankhapushpi, and Mandukaparni to improve mood, cognition, and emotional resilience [72].
Management
Modern Medical Approach
Treatment of Pancreatic Diabetes focuses on addressing both endocrine and exocrine dysfunctions simultaneously [44]. The primary goal is to achieve stable glycemic control while ensuring proper digestion and nutrient absorption.
Insulin therapy is the mainstay because endogenous insulin secretion is significantly reduced [42]. A basal–bolus regimen or insulin pump is often required to maintain steady glucose levels. Sulfonylureas and other oral hypoglycemic agents are generally avoided because they can precipitate hypoglycemia due to absent glucagon response [48]. Metformin may be used in patients with mild hyperglycemia and preserved renal function but must be monitored closely [55].
Pancreatic enzyme replacement therapy (PERT) is essential to correct malabsorption and improve nutrient assimilation [61]. Enzymes containing lipase, amylase, and protease are administered with meals to restore digestive function. Fat-soluble vitamins A, D, E, and K must be supplemented to prevent nutritional deficiencies. Lifestyle modifications such as regular small meals, abstinence from alcohol, and avoidance of high-fat diets are necessary to reduce pancreatic stress [44].
Ayurvedic Approach
Ayurveda classifies this condition under Prameha caused by Agnimandya and imbalance of Kapha and Pitta [72]. Management is directed toward improving digestion, clearing Ama, and restoring metabolic balance through Shodhana (detoxification), Shamana (pacification), and Rasayana (rejuvenation).
Shodhana Therapy (Purification) includes Snehapana with medicated ghee such as Mahatikta Ghrita, followed by Virechana with herbal purgatives like Trivrit or Avipattikar Churna to eliminate vitiated Pitta and Kapha [73]. In chronic or severe cases, Basti therapy with medicated decoctions containing Dashamoola or Bala is advised to balance Vata and support pancreatic rejuvenation.
Shamana Therapy (Pacification) aims to regulate glucose metabolism and improve pancreatic activity. Herbs like Gudmar (Gymnema sylvestre), Meshashringi, Jambu Beej, and Shilajit enhance insulin secretion and receptor sensitivity [72]. Classical formulations such as Nisha Amalaki Avaleha, Chandraprabha Vati, and Vasant Kusumakar Ras are beneficial for restoring Agni, balancing Doshas, and preventing complications.
Rasayana Therapy (Rejuvenation) is the cornerstone of long-term management. Rasayanas like Swarna Bhasma, Abhrak Bhasma, and Amalaki Rasayana are used to restore Dhatu integrity, strengthen Ojas, and support pancreatic repair [73]. These formulations act as antioxidants, reduce inflammation, and improve cellular regeneration.
Dietary Management
Diet plays a central role in both modern and Ayurvedic approaches. A balanced diet with moderate carbohydrates, lean proteins, and healthy fats helps stabilize glucose levels [61]. Ayurveda recommends Pathya foods such as barley, green gram, amla, bitter gourd, and fenugreek that promote Kapha–Pitta balance [72]. Foods that are heavy, fried, or sweet should be avoided as they increase Ama and aggravate Kapha.
Meal frequency should be small and regular to prevent hypoglycemia. Herbal drinks like decoctions of Neem, Guduchi, and Triphala aid digestion and maintain glucose balance. In chronic cases, individualized dietary planning based on Prakriti (body constitution) and digestive capacity is crucial [73].
Lifestyle and Behavioral Modifications
Regular exercise, yoga, and meditation improve insulin sensitivity and reduce stress-induced glucose fluctuations [55]. Pranayama techniques such as Anuloma Viloma and Bhastrika help regulate the autonomic nervous system and support pancreatic oxygenation [73]. Adequate sleep and avoidance of alcohol and smoking are emphasized for long-term pancreatic protection.
Integrative Model of Care
A combined model integrating enzyme replacement, insulin therapy, and Ayurvedic Rasayana offers the most comprehensive results [44]. Modern monitoring tools such as continuous glucose monitors can be complemented by Ayurvedic assessment of Agni and Dosha states for individualized care. The integrative approach ensures both symptomatic relief and restoration of the pancreatic tissue, addressing the disease from its root [72].
Avaleha to Cure Pancreatic Diabetes (Type 3c Diabetes)
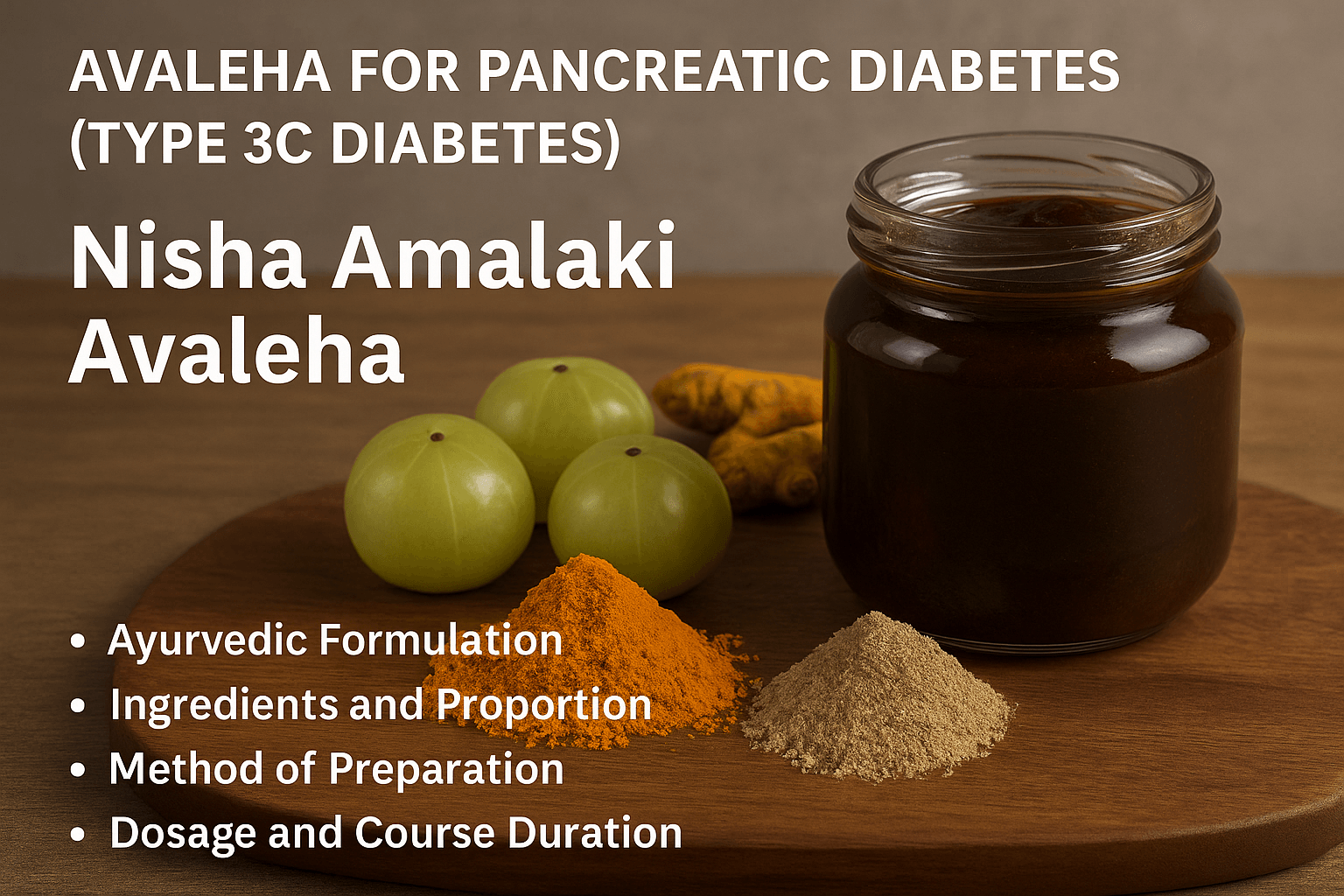
8.1. Name of the Formulation
The classical formulation indicated for Prameha and pancreatic disorders is Nisha Amalaki Avaleha, mentioned in Charaka Samhita (Chikitsa Sthana 6/54) and Bhavaprakasha (Madhyama Khanda, Prameha Chikitsa 15–16). This preparation is one of the most powerful Rasayana Avalehas for restoring Agni, balancing Kapha and Pitta, and rejuvenating pancreatic tissue affected by chronic inflammation [72].
8.2. Classical Reference
In the Ayurvedic texts, Nisha Amalaki is described as a divine combination that cures all types of Prameha (metabolic disorders). Charaka Samhita states that the regular use of this preparation restores strength, digestion, and vitality, thereby reversing long-standing metabolic defects [73]. The synergy between turmeric (Nisha) and amla (Amalaki) forms a powerful antioxidant and rejuvenative base, while Rasayana Bhasmas enhance pancreatic regeneration.
8.3. Purpose and Indications
This Avaleha is designed to address both the endocrine and exocrine components of pancreatic damage. It improves digestion, enhances insulin secretion, reduces oxidative stress, and prevents diabetic complications such as neuropathy and malnutrition [44]. Ayurvedically, it works on Agnimandya, Srotorodha, and Ojakshaya—the three major pathological foundations of Type 3c Diabetes [72].
Therapeutic indications include:
- Pancreatic Diabetes (Type 3c Diabetes Mellitus)
- Chronic pancreatitis with malabsorption
- Glucose instability and hypoglycemic episodes
- Loss of strength and tissue depletion (Dhatukshaya)
- Fatigue, poor digestion, and Ama accumulation
8.4. Ingredients and Proportion (for 30 Days)
The Avaleha is prepared using classical herbal and mineral Rasayanas in precise proportions to support a 30-day course.
Key ingredients:
- Nisha (Curcuma longa): 200 g
- Amalaki (Emblica officinalis): 200 g
- Gudmar (Gymnema sylvestre): 100 g
- Jambu Beej (Syzygium cumini): 100 g
- Meshashringi (Gymnema sylvestre): 80 g
- Shilajit (Purified Asphaltum): 50 g
- Swarna Bhasma (Gold calx): 500 mg
- Abhrak Bhasma (Mica calx): 2 g
- Trivanga Bhasma (Composite of Tin, Lead, Zinc): 2 g
- Vasant Kusumakar Ras: 1 g
- Go-Ghrita (Cow’s ghee): 250 mL
- Jaggery or raw honey (as per climate): 500 g
These ingredients are well-documented in Charaka Samhita and Bhavaprakasha Nighantu for their metabolic, Rasayana, and tissue-regenerative actions [72].
8.5. Method of Preparation
- Prepare a decoction of Nisha, Amalaki, Gudmar, and Jambu Beej by boiling them in eight times water until one-fourth remains.
- Filter the liquid carefully and heat it again over a mild flame.
- Add jaggery to the decoction and stir continuously until a syrup-like consistency is achieved.
- Add Go-Ghrita slowly while stirring to obtain the Avaleha base.
- Once the mixture cools below 40°C, incorporate all Bhasmas (Swarna Bhasma, Abhrak Bhasma, Trivanga Bhasma) and Vasant Kusumakar Ras.
- Mix thoroughly until uniform and store in a glass container away from sunlight and moisture.
This gentle preparation method preserves the potency of Rasayana minerals and prevents the loss of volatile components [73].
8.6. Dosage and Course Duration
Take 15 grams twice daily on an empty stomach with lukewarm water or as directed by a physician. The recommended course duration is 30 days. Continuous use under supervision may be extended for Rasayana effect to promote pancreatic rejuvenation [44].
8.7. Mechanism of Action (Ayurvedic and Modern Correlation)
According to Ayurveda, this Avaleha pacifies Kapha and Pitta, rekindles Agni, and restores balance to the Rasavaha and Annavaha Srotas. It removes Ama and supports the regeneration of pancreatic tissue.
From a modern biomedical perspective:
- Curcumin enhances insulin sensitivity and suppresses inflammatory cytokines [61].
- Amalaki provides vitamin C, antioxidants, and polyphenols that protect β-cells from oxidative damage [55].
- Gudmar and Jambu Beej exhibit insulin-mimetic effects and improve glucose utilization [72].
- Swarna and Abhrak Bhasma act as nano-mineral Rasayanas that stabilize mitochondrial energy production and support cellular repair [73].
- Vasant Kusumakar Ras enhances glucose metabolism and improves Ojas through rejuvenation of endocrine function [73].
Together, these actions align perfectly with Prameha Chikitsa Siddhanta, restoring both digestive and metabolic balance.
8.8. Precautions and Warnings
- The formulation should be taken under supervision of a qualified Ayurvedic physician.
- Not advised for children, pregnant, or lactating women.
- Dosage may vary based on individual Prakriti, digestive strength, and concurrent medications.
- Avoid refined sugar, dairy, and heavy meals during the treatment course.
- Skipping doses or irregular intake may disturb metabolic stability and reduce therapeutic efficacy [72].
Important Medical Warning Before Using Avaleha and Mineral Preparations
These Medicines Should Never Be Purchased Over the Counter
Patients must not buy Avaleha, Rasaushadhi, or mineral-based Ayurvedic formulations from the market and consume them without proper medical evaluation. These are not general nutritional supplements. Their therapeutic action depends on precise matching with the patient’s digestive strength, metabolic status, disease stage, and associated systemic conditions. In pancreatic diabetes, where malabsorption and enzyme deficiency are already present, a non-personalized formulation often remains improperly digested and fails to reach the target tissue.
Lack of Personalization Is the Most Common Cause of Treatment Failure
A commercially prepared product is designed for uniform use and does not consider Agni status, degree of pancreatic insufficiency, glucose variability, Dhatu depletion, bowel pattern, liver function, or micronutrient absorption. When these factors are not assessed, the formulation cannot be metabolized correctly and does not produce Rasayana-level tissue nourishment.
Influence of Age and Tissue Strength on Therapeutic Response
Age plays a major role in clinical outcome. Younger patients with better Dhatu integrity and preserved pancreatic function respond to regenerative protocols, whereas elderly patients with long-standing disease and severe nutritional depletion require a completely different therapeutic approach. A fixed formulation cannot address this variation.
Effect of Disease Duration and Stage
Early pancreatic dysfunction with residual beta-cell activity allows for metabolic correction and functional recovery. Long-standing disease with fibrosis, severe insulin deficiency, and chronic malnutrition requires a stabilization and Brimhana-dominant protocol. Market-available Avaleha does not differentiate between these stages, which is a major reason for poor results.
Impact of Associated Chronic Disorders
Coexisting diseases significantly alter digestion, absorption, and cellular utilization of medicine. Chronic liver disease, renal impairment, hypothyroidism, anemia, inflammatory bowel disease, long-standing Type 2 diabetes, and severe malabsorption syndromes all modify the therapeutic response. Without adjusting the formulation to these conditions, the medicine cannot act effectively.
Role of Agnimandya in Therapeutic Failure
Severely impaired digestive fire is one of the most important causes of non-response. When Agni is low, even the best Rasayana behaves as a heavy, poorly digested substance and produces further metabolic obstruction instead of tissue nourishment. Correction of Agni is therefore the first and most essential step.
Importance of Correct Timing, Diet, and Anupana
The effectiveness of Avaleha depends on proper timing of administration, compatible diet, and appropriate Anupana. Irregular meals, incompatible foods, and incorrect dosing schedules prevent proper absorption and reduce therapeutic potency.
Risk of Self-Preparation Without Ayurvedic Medical Supervision
Classical Preparation Requires Technical Precision
These formulations should never be prepared by patients on their own. Classical processing involves purification, controlled heating stages, precise proportion, correct base medium, and stage-wise addition of ingredients. Any deviation alters bioavailability, safety, and clinical effectiveness.
Consequences of Improper Preparation
Improperly prepared formulations may lead to incomplete digestion, Ama formation, metabolic overload on the liver, unpredictable glucose fluctuations, loss of therapeutic potency, and failure of tissue delivery.
Why Physician-Guided Clinical Customization Is Essential
Factors That Must Be Evaluated Before Administration
In pancreatic diabetes, the formulation must be individualized according to digestive capacity, Grahani status, residual pancreatic function, level of insulin deficiency, body weight, degree of nutritional depletion, age, hypoglycemia tendency, associated systemic disease, and current medications.
From Classical Rasayana to Targeted Dhatu-Level Action
Only when these parameters are assessed can the medicine act as a true Rasayana that reaches the Dhatu level, supports pancreatic tissue, stabilizes metabolism, and produces sustained clinical improvement. For this reason, classical Ayurveda always emphasizes physician-guided preparation and administration rather than unsupervised use.
Prognosis and Can Pancreatic Diabetes Be Reversed?
The prognosis of pancreatic diabetes depends on the extent of pancreatic damage, the stage at which the condition is identified, the presence of residual endocrine function, nutritional status, and the effectiveness of digestive correction. Unlike classical Type 2 diabetes, where the primary issue is insulin resistance, Type 3c diabetes is a disease of progressive pancreatic tissue loss. Therefore, long-term outcome is determined by whether metabolic stability and pancreatic support are initiated early.
In patients where the condition is recognized in its early phase, with preserved beta-cell activity and manageable exocrine insufficiency, significant functional improvement is possible. When digestion improves, nutrient absorption increases, weight stabilizes, inflammation reduces, and glucose variability becomes more predictable. This stage offers the highest potential for metabolic recovery.
In advanced disease with fibrosis, severe insulin deficiency, and long-standing malnutrition, complete independence from insulin may not always be achievable. However, even in these patients, a structured integrative approach can produce major clinical benefits, including reduction in glucose fluctuations, improved strength and body weight, better tolerance to insulin therapy, and enhanced quality of life.
Life Expectancy in Pancreatic Diabetes
Life expectancy in Type 3c diabetes is not determined by blood glucose levels alone. It is influenced by the underlying pancreatic disease, degree of malnutrition, liver function, micronutrient status, and frequency of hypoglycemic episodes.
Patients who receive only glucose-lowering therapy without correction of malabsorption often continue to lose weight and develop progressive metabolic weakness. In contrast, when enzyme support, nutritional rehabilitation, and metabolic stabilization are introduced early, long-term survival and functional capacity improve significantly.
The most important prognostic factor is preservation of body weight, muscle mass, and digestive strength, because these determine immune resilience, hormonal balance, and the ability of the body to respond to therapy.
Can Type 3c Diabetes Be Reversed?
Reversal in pancreatic diabetes does not mean temporary normalization of blood sugar. True reversal refers to restoration of metabolic stability, improved pancreatic function, reduction in external insulin requirement in suitable patients, and recovery of nutritional status.
This is most achievable when:
The disease is identified early
Residual pancreatic function is present
Severe Dhatu depletion has not occurred
Digestion and absorption are actively corrected
In these patients, staged therapy that combines digestive restoration, tissue nourishment, and Rasayana support can lead to sustained clinical improvement.
Ayurvedic Perspective on Long-Term Outcome
From an Ayurvedic standpoint, pancreatic diabetes represents a transition from Kapha-dominant Prameha to a Vata-dominant Dhatu-kshaya state. Prognosis depends on the ability to restore Agni, rebuild Dhatus, and replenish Ojas.
When Agni improves, Ama reduces.
When Ama reduces, Srotas open.
When Srotas open, tissue nutrition reaches the pancreas.
This sequence determines the potential for functional recovery.
Even in long-standing disease, the objective of therapy is not only glycemic control but restoration of strength, stability of energy, improvement in digestion, and prevention of further tissue loss. This shifts the condition from a progressive degenerative state to a controlled and clinically stable state.
Long-Term Complications if Pancreatic Diabetes Is Not Treated Correctly
Pancreatic diabetes is not only a disorder of elevated blood glucose. It is a progressive metabolic and nutritional disease that affects multiple organ systems when the underlying pancreatic dysfunction is not corrected. Treating glucose alone while ignoring malabsorption, inflammation, and tissue depletion leads to continuous clinical deterioration.
Progressive Malnutrition and Severe Weight Loss
Exocrine pancreatic insufficiency prevents proper digestion of fats, proteins, and fat-soluble vitamins. As a result, even patients who eat adequately continue to lose weight and develop muscle wasting. Loss of body protein reduces immune strength, delays healing, increases fatigue, and accelerates Dhatu-kshaya. This is one of the most important factors responsible for poor long-term survival.
Recurrent and Unpredictable Hypoglycemia
In Type 3c diabetes, glucagon response is impaired. When insulin is given without correcting digestion and nutritional absorption, blood glucose may fall suddenly and produce dizziness, sweating, confusion, and loss of consciousness. Repeated hypoglycemic episodes affect brain function, reduce quality of life, and create constant fear of food and medication.
Fat-Soluble Vitamin Deficiency and Bone Disease
Chronic malabsorption leads to deficiency of vitamins A, D, E, and K. Vitamin D deficiency results in osteopenia, osteoporosis, bone pain, muscle weakness, and increased fracture risk. Over time, this causes severe structural weakness and reduced mobility.
Liver Dysfunction and Metabolic Instability
Undigested nutrients and Ama formation increase metabolic load on the liver. This leads to fatty liver changes, impaired glucose storage, reduced protein synthesis, and worsening energy depletion. When liver function declines, glucose regulation becomes even more unstable.
Intestinal Inflammation and Grahani-Like Syndrome
Persistent maldigestion produces bloating, irregular bowel movements, steatorrhea, and intestinal inflammation. This condition resembles chronic Grahani in Ayurveda, where absorption becomes erratic and the body fails to utilize even properly administered medicines.
Progressive Dependence on High-Dose Insulin
When pancreatic tissue loss continues and nutrition is not corrected, insulin requirement increases progressively. Higher doses do not solve the metabolic problem because the primary defect is tissue degeneration and digestive failure. This leads to a cycle of unstable glucose control despite intensifying therapy.
Increased Risk of Pancreatic Cancer in Long-Standing Disease
New-onset diabetes in adults with underlying pancreatic pathology may be an early metabolic manifestation of pancreatic malignancy. Failure to evaluate the pancreas structurally delays diagnosis and reduces the window for early intervention.
Nervous System Weakness and Chronic Fatigue
Long-standing malnutrition, micronutrient deficiency, and glucose variability weaken Majja Dhatu. Patients develop neuropathy, poor concentration, disturbed sleep, anxiety, and persistent exhaustion. This is not only a glucose disorder but a systemic depletion state.
Reduced Immunity and Delayed Healing
Loss of Ojas due to chronic Dhatu depletion leads to recurrent infections, slow wound healing, and increased susceptibility to systemic illness. Minor health issues take longer to recover and overall resilience declines.
Final Conclusion: A Root-Cause Approach to Pancreatic Diabetes
Pancreatic diabetes is fundamentally different from classical forms of diabetes because it is a disease of pancreatic tissue loss combined with digestive and metabolic failure. Managing blood glucose alone does not alter the progression of the disorder. Long-term stability is achieved only when enzyme deficiency, malabsorption, inflammation, nutritional depletion, and endocrine dysfunction are addressed together in a structured and stage-wise manner.
Early recognition of the condition provides the greatest opportunity for functional recovery. When digestion improves and nutrient absorption is restored, body weight stabilizes, glucose variability reduces, and the metabolic burden on the pancreas decreases. Even in advanced disease, a comprehensive integrative approach can significantly improve strength, energy, tissue nourishment, and quality of life.
From an Ayurvedic perspective, the transition from Agnimandya to Dhatu-kshaya and Ojas depletion defines both the severity and the direction of treatment. Therapy that restores Agni, rebuilds Dhatus, and supports pancreatic function changes the clinical course from progressive degeneration to long-term metabolic stability.
Pancreatic diabetes therefore requires a personalized, medically supervised protocol rather than a generalized glucose-lowering strategy.
Evidence-Based Integrative Care for International Patients
This treatment model is designed for patients who have diabetes associated with chronic pancreatitis, pancreatic surgery, pancreatic insufficiency, unexplained weight loss, unstable glucose levels, or long-standing diabetes that does not respond to conventional therapy.
The therapeutic approach is based on detailed clinical assessment, stage-wise correction of digestion and metabolism, individualized Rasayana support, and continuous monitoring of nutritional and endocrine parameters.
Patients from the USA, UK, Canada, Australia, Singapore, and other countries can undergo structured online evaluation and receive a personalized treatment protocol tailored to their disease stage, metabolic profile, and associated medical conditions.
Medical Supervision and Personalized Treatment Are Essential
All Ayurvedic formulations used in pancreatic diabetes are prescribed only after comprehensive assessment of digestive strength, pancreatic status, body composition, glucose pattern, and associated systemic disease. This ensures safety, proper absorption, and Dhatu-level therapeutic action.
Self-medication, over-the-counter purchases, and non-individualized formulations are avoided because they do not address the root pathology and frequently lead to poor clinical outcomes.
Author and Medical Expertise
This article is written and medically guided by an Ayurvedic physician with focused clinical experience in the management of complex metabolic and pancreatic disorders using classical Ayurvedic principles integrated with modern diagnostic evaluation.
The treatment protocols described are based on:
Clinical assessment of patients with pancreatic and metabolic disease
Application of classical Ayurvedic Rasayana and Prameha management
Modern biochemical and imaging correlation for disease staging
This integrative framework ensures that the therapeutic approach remains both traditionally authentic and medically relevant for contemporary clinical practice.
When to Seek a Personalized Evaluation
Patients should consider a structured medical evaluation if they have:
Diabetes with chronic digestive disturbance
Unexplained weight loss despite adequate diet
Frequent hypoglycemia with standard diabetic therapy
History of pancreatitis or pancreatic surgery
Diabetes that remains unstable despite treatment
Early intervention significantly improves long-term outcome and prevents progressive tissue depletion.
Frequently Asked Questions (FAQs)
What is pancreatic diabetes (Type 3c diabetes)?
Pancreatic diabetes, also called Type 3c diabetes or pancreatogenic diabetes, is diabetes caused by damage to the pancreas. It often develops after chronic pancreatitis, pancreatic surgery, pancreatic cancer, or long-standing pancreatic inflammation. It differs from Type 2 diabetes because insulin deficiency and digestive enzyme failure occur together, leading to unstable glucose levels and malabsorption.
How is Type 3c diabetes different from Type 2 diabetes?
Type 2 diabetes is mainly driven by insulin resistance and often links with obesity and metabolic syndrome. Type 3c diabetes is primarily caused by pancreatic tissue damage, which reduces insulin production and also reduces digestive enzyme output. Many Type 3c patients have weight loss, malabsorption, and unpredictable hypoglycemia, which is not typical of standard Type 2 diabetes.
What are the most common symptoms of pancreatic diabetes?
Common symptoms include unstable blood sugar, frequent fatigue, unexplained weight loss, digestive discomfort, bloating, greasy or oily stools, diarrhea, vitamin deficiency symptoms, and repeated hypoglycemia episodes. Many patients also notice poor tolerance to standard oral diabetes medications.
What tests confirm Type 3c diabetes?
Diagnosis typically involves confirming diabetes with fasting glucose or HbA1c, checking C-peptide to assess insulin production, ruling out autoimmune diabetes markers when needed, testing exocrine pancreatic function through fecal elastase, assessing malabsorption, and confirming pancreatic structural damage through CT, MRI, or endoscopic ultrasound.
Why do Type 3c diabetes patients experience hypoglycemia more easily?
In pancreatic diabetes, not only insulin-producing beta cells are affected, but glucagon-producing alpha cells may also be damaged. Glucagon normally protects the body from low blood sugar. When glucagon response is weak, insulin therapy and missed meals can trigger sudden hypoglycemia.
Can Type 3c diabetes be reversed?
Some patients can achieve significant functional improvement, especially if diagnosed early and if residual pancreatic function remains. Reversal means stabilizing glucose patterns, improving digestion and absorption, restoring weight and strength, and reducing dependence on high-dose insulin when clinically possible. Advanced disease may still require insulin, but integrative treatment can greatly improve stability and outcomes.
What is the best diet for pancreatic diabetes?
The best diet focuses on improving digestion and absorption while keeping glucose stable. Most patients do better with warm, freshly cooked meals, small frequent portions, adequate protein for tissue repair, carefully selected fats for energy and vitamin absorption, and avoidance of processed foods and refined carbohydrates that cause rapid glucose fluctuations.
Why does treatment fail when patients buy Avaleha from the market?
Market-bought Avaleha is not customized for digestive strength, disease stage, malabsorption severity, age, body weight, liver function, medication profile, and associated disorders. In Type 3c diabetes, poor digestion and enzyme deficiency can prevent absorption, causing the medicine to fail or worsen metabolic imbalance. Ayurvedic medicines should be used only under physician supervision.
Is pancreatic enzyme replacement necessary in Type 3c diabetes?
If exocrine pancreatic insufficiency is present, enzyme replacement is often essential. Without it, fat and protein digestion remain poor, vitamin deficiencies worsen, weight loss continues, and glucose control becomes unpredictable. Correcting enzyme deficiency improves nutrition and supports stable metabolic control.
When should someone suspect pancreatic cancer in new-onset diabetes?
New-onset diabetes after age forty, especially with unexplained weight loss, reduced appetite, persistent abdominal discomfort, or digestive changes, should prompt pancreatic evaluation. Imaging helps rule out pancreatic malignancy early, which is critical for better outcomes.
1. What is Pancreatic Diabetes?
Pancreatic Diabetes, also called Type 3c Diabetes, is a form of diabetes that develops due to damage or disease affecting the pancreas. It involves both endocrine dysfunction, leading to insulin deficiency, and exocrine dysfunction, leading to poor digestion.
2. How is Pancreatic Diabetes different from Type 1 and Type 2 Diabetes?
Type 1 Diabetes results from autoimmune destruction of beta cells, while Type 2 arises from insulin resistance. Pancreatic Diabetes occurs when the pancreas is structurally damaged, leading to both reduced insulin production and digestive enzyme deficiency.
3. What causes Pancreatic Diabetes?
The condition usually develops after chronic pancreatitis, pancreatic surgery, cancer, cystic fibrosis, or trauma. Long-term alcohol use, smoking, and malnutrition also increase risk.
4. Why is Pancreatic Diabetes often misdiagnosed?
Because its symptoms overlap with Type 2 Diabetes, many cases are incorrectly labeled as Type 2. Without recognizing the pancreatic origin, treatment may fail to correct the underlying problem.
5. How common is this condition globally?
Pancreatic Diabetes is believed to account for about five to ten percent of all diabetes cases, though most remain undiagnosed. It is more frequent in patients with chronic pancreatitis or pancreatic surgery.
6. What are the early warning signs?
Early symptoms include poor digestion, bloating, oily stools, fatigue, and unstable blood sugar. Over time, weight loss and vitamin deficiencies may occur.
7. Can Ayurveda help in curing Pancreatic Diabetes?
Yes. Ayurveda approaches the condition through correction of Agni (digestive fire), elimination of Ama (toxins), and rejuvenation of pancreatic tissue using Rasayana therapies. It targets the root cause rather than only controlling sugar levels.
8. What are the benefits of early diagnosis?
Early identification prevents irreversible pancreatic damage, nutritional deficiency, and metabolic instability. Timely therapy can restore enzyme balance and stabilize glucose regulation.
9. Is insulin therapy alone enough to manage it?
No. Insulin only addresses glucose imbalance but not the underlying pancreatic and digestive dysfunction. Management must include enzyme support, nutritional correction, and Ayurvedic Rasayana to rejuvenate the organ.
10. Can lifestyle changes make a difference?
Yes. A healthy diet, regular physical activity, stress management, and avoidance of alcohol or fatty food help improve pancreatic function and reduce inflammation.
Reference
[42] Ewald, N., & Hardt, P. D. (2013). Diagnosis and treatment of diabetes mellitus in chronic pancreatitis. World Journal of Gastroenterology, 19(42), 7276–7281. https://doi.org/10.3748/wjg.v19.i42.7276
[43] Das, S. L., Singh, P., Rana, S. S., Yes, C., & Madhusudhan, K. S. (2022). The cause and effect relationship of diabetes after acute pancreatitis. Gastroenterology Research and Practice, 2022, 10044911. https://doi.org/10.1155/2022/10044911
[44] Cui, Y., & Andersen, D. K. (2011). Pancreatogenic diabetes: special considerations for management. Pancreatology, 11(3), 279–294. https://doi.org/10.1159/000327667
[45] Gao, F., Qiu, S., & Zheng, L. (2017). Incidence, demographics, and clinical characteristics of diabetes mellitus following pancreatic disease. Diabetes Care, 40(11), 1535–1542. https://pubmed.ncbi.nlm.nih.gov/28860126/
[46] van der Heide, F., & van Santvoort, H. C. (2023). Post-pancreatitis diabetes mellitus: insight on optimal management. Pancreatology, 23(3), 338–347. https://doi.org/10.1016/j.pan.2023.03.010
[47] Patel, P., & Ruiz, J. (2022). Type 3c diabetes associated with chronic pancreatitis: a review of mechanisms. Journal of Clinical Medicine, 11(24), 0932. https://doi.org/10.3390/jcm11240932
[48] Hardt, P. D., & Ewald, N. (2011). Exocrine pancreatic insufficiency in diabetes mellitus: a complication worth knowing. World Journal of Diabetes, 2(9), 154–158. https://doi.org/10.4239/wjd.v2.i9.154
[49] Sánchez, B., & Espinosa, R. (2020). Management of pancreatogenic diabetes: challenges and solutions. World Journal of Diabetes, 11(12), 496–506. https://doi.org/10.4239/wjd.v11.i12.496
[50] Juza, A., Kołodziej-Spirodek, L., Gutkowski, K., Partyka, M., & Dąbrowski, M. (2025). Distinguishing exocrine pancreas disease-associated diabetes from Type 2 diabetes based on anthropometric and metabolic parameters. World Journal of Diabetes, 16(2), 95–102. https://www.wjgnet.com/1948-9358/full/v16/i2/95102.htm
[55] Rickels, M. R., Bellin, M. D., Toledo, F. G. S., Robertson, R. P., & Andersen, D. K. (2017). Detection, evaluation and treatment of diabetes mellitus in chronic pancreatitis: Recommendations from PancreasFest 2012. Pancreatology, 17(4), 686–694. https://doi.org/10.1016/j.pan.2017.07.006
[61] Panebianco, C., Andriulli, A., & Pazienza, V. (2018). Pancreatic cancer and diabetes: A two-way relationship in the perspective of diabetologists. World Journal of Clinical Oncology, 9(7), 53–65. https://doi.org/10.5306/wjco.v9.i7.53
[63] Hardt, P. D., & Ewald, N. (2015). Pathological mechanisms in diabetes of the exocrine pancreas. Diabetes & Metabolism Journal, 39(3), 197–205. https://doi.org/10.4093/dmj.2019.0118
[72] Sharma, P. V. (Ed.). (2006). Charaka Samhita (Vol. II, Chikitsa Sthana 6/54–63). Varanasi: Chaukhambha Orientalia.
[73] Bhavamishra. (2010). Bhavaprakasha Nighantu (Madhyama Khanda, Prameha Chikitsa 15–16). Varanasi: Chaukhambha Bharati Academy.
[74] Sushruta. (2012). Sushruta Samhita (Chikitsa Sthana 11/5–12) with commentary by Ambikadatta Shastri. Varanasi: Chaukhambha Sanskrit Sansthan.











