- Modern Perspective- A New Era in Breast Cancer Surgery
- Ayurvedic Perspective- The Shalya Tantra Foundation
- Holistic Aim-Sharira and Manas
- Principles of Oncoplastic Surgery and Ayurvedic Alignment
- Alignment of Modern and Ayurvedic Principles
- Classification of Oncoplastic Techniques
- Patient Selection and Evaluation
- Surgical Approaches with Ayurvedic Support
- Breast Reconstruction Options & Ayurvedic Perspectives
- Ayurvedic Perspectives- Supporting Flap Survival and Healing
- Psychosocial Recovery- Prasadhana and Self-Esteem
- Fat Grafting and Rasayana Synergy
- Oncoplastic in Special Situations
- Recent Advances and Ayurvedic Research Directions
- 3D planning in surgery ↔ Ayurvedic nanotechnology (Bhasma at nano-scale)
- FAQs
- References
Modern Perspective- A New Era in Breast Cancer Surgery
Breast cancer management has undergone a remarkable transformation over the last century. In the early twentieth century, radical mastectomy was considered the gold standard—a procedure designed to ensure oncological safety but often at the expense of body image and psychological health [1]. With the advent of breast-conserving surgery, supported by large randomized controlled trials, it became clear that lumpectomy with radiotherapy could achieve survival outcomes equivalent to mastectomy [2].
The rise of oncoplastic breast surgery further revolutionized this field. By integrating wide tumor excision with plastic surgical principles, it allows surgeons to balance oncological clearance with cosmetic outcomes [3]. This dual aim—cancer control and preservation of breast aesthetics—has been shown to improve quality of life, psychosocial well-being, and patient satisfaction [4].
Ayurvedic Perspective- The Shalya Tantra Foundation
Ayurveda, through the classical text Sushruta Samhita, described surgery (Shalya Tantra) not only as excision of diseased tissue but as part of a holistic continuum of care [5]. Sushruta outlined techniques such as chedana (excision), bhedana (incision), lekhana (scraping), and sandhana (suturing), always followed by shodhana (cleansing), ropana (healing), and systemic rejuvenation through Rasayana Chikitsa [6].
Breast tumors in Ayurveda were described under Granthi (benign swellings) and Arbuda (malignant growths). The therapeutic principles emphasized precise removal, detoxification of srotas (channels), balancing of doshas, and enhancement of Ojas (vital immunity) to prevent recurrence [7].
Holistic Aim-Sharira and Manas
Modern oncoplastic surgery primarily addresses the structural dimension: removing the cancer and reconstructing the breast mound. Ayurveda extends this aim by addressing terrain, immunity, and consciousness. It emphasizes complete restoration of both Sharira (body) and Manas (mind), ensuring that the patient emerges not only physically restored but also emotionally resilient and spiritually grounded [8].
Thus, the integration of oncoplastic surgery with Ayurvedic healing offers a synergistic paradigm:
- Surgery provides immediate oncological safety and physical reconstruction.
- Ayurveda ensures long-term immunity, wound healing, and psychosocial recovery through Rasayana, Panchakarma, and lifestyle-based care [9].
This combined approach transforms breast cancer care into a comprehensive model of survival, resilience, and renewal.
Principles of Oncoplastic Surgery and Ayurvedic Alignment
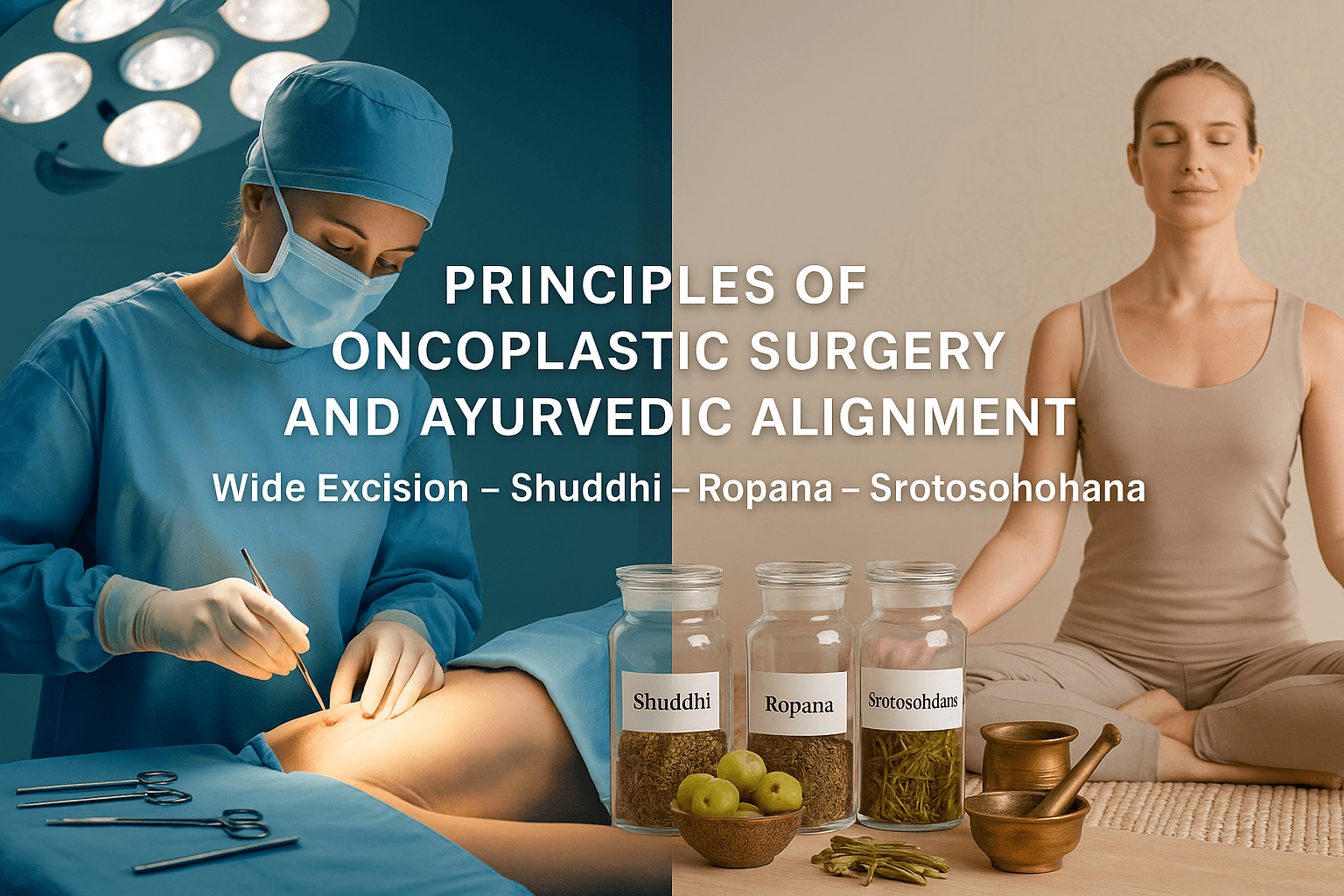
Modern Principles- Balancing Safety and Aesthetics
The cornerstone of oncoplastic breast surgery lies in its unwavering commitment to oncological safety. Malignant tissue must be excised with clear surgical margins to minimize the risk of local recurrence [1]. Historically, this principle guided radical procedures such as the Halsted mastectomy, which achieved control but left profound physical and psychological scars. Over time, landmark trials established that breast-conserving surgery with radiotherapy could yield equivalent survival outcomes when compared to mastectomy [2].
Building on this foundation, oncoplastic surgery has introduced a more patient-centered philosophy: tumor clearance should not compromise aesthetics. By merging wide local excision with plastic surgical techniques, surgeons can remove larger volumes of tissue while simultaneously reshaping the breast [3]. Procedures such as therapeutic mammoplasty, glandular rotation, local tissue advancement, and the use of volume replacement flaps are now standard approaches in early and locally advanced breast cancers [4].
Clinical data underscore the benefits. Women undergoing oncoplastic surgery consistently report higher satisfaction scores, improved psychosocial adjustment, and better sexual health compared to those undergoing traditional lumpectomy [5]. Importantly, oncological outcomes remain uncompromised, with recurrence rates comparable to standard breast-conserving surgery.
Thus, the modern principles of oncoplastic surgery can be distilled into three dimensions: (1) uncompromising margin-negative excision, (2) immediate breast reshaping for aesthetic restoration, and (3) enhancement of long-term quality of life. In this framework, the success of surgery is measured not solely in survival curves but in the preservation of dignity, identity, and emotional well-being.
Ayurvedic Principles-Shalya Chikitsa and Beyond
Ayurveda articulates principles of surgery that mirror and enrich modern oncoplastic standards. The discipline of Shalya Chikitsa, as detailed in the Sushruta Samhita, emphasizes Shuddhi, or the complete removal of diseased tissue, as the foundation of cure [6]. In many ways, this anticipates the modern principle of clear margins. Yet Ayurveda extends the process beyond excision, integrating Ropana (healing) and Rasayana (rejuvenation) into the continuum of surgical care [7].
According to Ayurvedic pathology, tumors (Arbuda) and swellings (Granthi) arise from dosha imbalance, srotorodha (obstruction of channels), and dhatu dushti (vitiation of tissues). Thus, after surgical removal, purification of the channels—Srotoshodhana—is essential to prevent recurrence [8]. This parallels modern oncology’s attention to microscopic disease, immune evasion, and the tumor microenvironment.
For wound care, classical texts prescribe medicated oils and ghritas such as Jatyadi Ghrita, which promotes cleansing, granulation, and tissue regeneration [9]. Herbal formulations containing Haridra (Curcuma longa) and Yashtimadhu (Glycyrrhiza glabra) are valued for antimicrobial and anti-inflammatory actions, validated by modern pharmacological studies [10]. Beyond physical healing, Rasayana therapies such as Amalaki (Emblica officinalis), Guduchi (Tinospora cordifolia), and Ashwagandha (Withania somnifera) restore depleted immunity and vitality, reinforcing systemic resilience [11].
Ayurveda also uniquely integrates Satvavajaya Chikitsa (psychological therapy), pranayama, and meditation for mental well-being. Here, the patient’s mind (manas) is given equal attention, acknowledging that healing must occur at both physical and psychological levels.
Thus, Ayurvedic surgical principles articulate a holistic paradigm: excision (Shuddhi), wound healing (Ropana), channel purification (Srotoshodhana), systemic rejuvenation (Rasayana), and psychological restoration (Satvavajaya). Together, they aim not only at eliminating disease but also at strengthening the host terrain to resist recurrence.
Alignment of Modern and Ayurvedic Principles
When juxtaposed, the principles of modern oncoplastic surgery and Ayurvedic Shalya Chikitsa reveal striking harmony. Both prioritize complete eradication of diseased tissue—modern surgery through clear margins, Ayurveda through Shuddhi [6]. Both insist on restoring form and function—modern approaches employ glandular reshaping and flaps, Ayurveda prescribes Ropana therapies with medicated oils and wound-healing herbs [9].
Where Ayurveda expands the paradigm is in addressing systemic balance and recurrence prevention. Modern oncology uses chemotherapy, endocrine therapy, and radiotherapy to minimize residual disease. Ayurveda employs Srotoshodhana to cleanse obstructed channels and Rasayana to enhance immunity (Ojas), thereby creating a hostile terrain for recurrence [8,11]. This terrain-focused approach resonates with emerging modern concepts such as tumor microenvironment modulation and immune checkpoint regulation [12].
Both traditions also converge on the recognition of psychosocial health. Oncoplastic surgery has demonstrated improvements in body image and quality of life, while Ayurveda has long emphasized mental stability through Satvavajaya Chikitsa, yoga, and meditation [13]. By addressing the patient’s emotional well-being, both traditions affirm that healing extends beyond the surgical scar.
In practice, this alignment enables a synergistic model:
- Oncoplastic surgery ensures oncological safety and aesthetic restoration.
- Ayurveda ensures wound healing, systemic purification, immune rejuvenation, and psychological harmony.
The result is not just a “cancer-free” breast but a woman restored to vitality, confidence, and wholeness. This integrative framework transforms the measure of success from mere survival into complete, dignified, and resilient recovery.
Classification of Oncoplastic Techniques
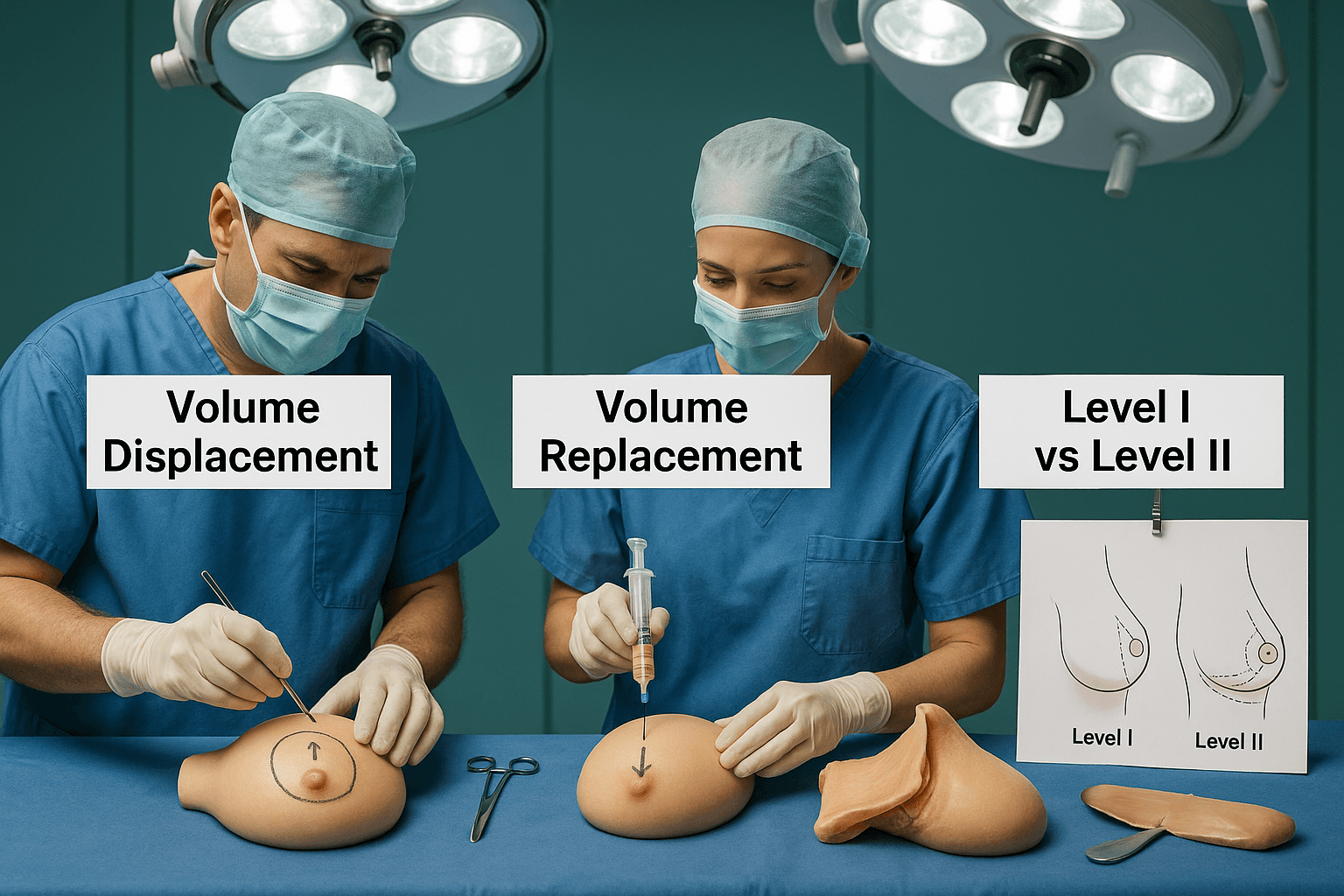
Volume Displacement Techniques
Volume displacement techniques are the most widely used oncoplastic strategies, particularly suited for women with medium to large breast sizes. The central principle is to rearrange the patient’s own breast tissue to fill the surgical defect created by wide excision [1]. Rather than introducing new material, the surgeon mobilizes existing parenchyma to achieve both oncological clearance and cosmetic balance.
Several methods are employed depending on tumor location. For upper pole lesions, crescent mastopexy and glandular advancement techniques provide good contour restoration. Central tumors may require round-block or batwing mammoplasty, which excise the tumor while simultaneously reshaping the breast mound [2]. For lower pole lesions, therapeutic reduction mammoplasty is particularly effective, combining cancer removal with contralateral reduction to achieve symmetry [3].
The advantages of displacement techniques are notable. They allow for wider excisions without deformity, improving oncological safety, while also enabling immediate aesthetic results. Furthermore, they avoid donor-site morbidity and additional scarring that may accompany more invasive reconstruction [4]. However, these methods are most effective when there is sufficient glandular volume; in women with small breasts or large tumors, volume replacement may be more appropriate.
In essence, displacement procedures embody the philosophy of “using what is already there.” By respecting the breast’s native tissue and vascular supply, they minimize complication risks while maximizing cosmetic outcomes. Their adaptability across quadrants and tumor sizes makes them a cornerstone of the oncoplastic approach.
Volume Replacement Techniques
Volume replacement techniques are indicated when excision leaves a defect too large to be corrected by glandular rearrangement alone. Instead of reshaping existing tissue, these methods involve filling the surgical cavity with autologous tissue or grafts to restore volume and contour [5].
Commonly used options include local and regional flaps. The latissimus dorsi mini-flap, harvested from the back and tunneled into the breast, is one of the most reliable methods for moderate defects [6]. Thoracoepigastric and lateral intercostal artery perforator flaps are alternatives for lateral quadrant defects. For central or upper quadrant lesions, perforator-based flaps provide tailored solutions with minimal donor-site morbidity [7].
Autologous fat grafting has gained popularity as a minimally invasive adjunct. By harvesting fat via liposuction and reinjecting it into the defect, surgeons can achieve subtle volume correction and contour smoothing. Although concerns exist about graft viability and interference with imaging, evidence suggests fat grafting is safe and effective when performed judiciously [8].
The strength of volume replacement techniques lies in their ability to preserve breast shape even in women with small breasts or those requiring larger excisions. They are especially valuable in cases of high tumor-to-breast volume ratio, where displacement alone would create deformity. However, these methods carry risks of donor-site morbidity, longer operative time, and, in some cases, more complex postoperative recovery [9].
Ultimately, volume replacement offers a critical solution in the oncoplastic toolbox, expanding the eligibility for breast-conserving therapy to women who would otherwise require mastectomy.
Level I vs. Level II Oncoplastic Procedures
Oncoplastic surgery is further classified into Level I and Level II techniques, a distinction based on the volume of tissue resected and the complexity of reconstruction [10].
Level I procedures are employed when less than 20% of breast volume is excised. These involve simple reshaping techniques such as glandular advancement, crescent mastopexy, or limited parenchymal rearrangement. They are relatively straightforward, preserve the breast’s natural contour, and do not usually require contralateral surgery for symmetry. Level I procedures are best suited for small to moderate tumors in patients with sufficient breast volume [11].
Level II procedures are indicated when 20–50% of breast tissue must be removed to achieve clear margins. These involve more extensive parenchymal reshaping, therapeutic reduction mammoplasty, and, at times, contralateral symmetrization surgery to achieve balance. Level II requires advanced surgical planning and often collaboration with plastic surgeons, as the procedures can significantly alter breast shape [12].
The distinction between levels is not merely academic; it carries clinical implications. Studies have shown that Level II procedures significantly reduce re-excision rates by enabling larger excisions while preserving cosmesis. However, they are associated with longer operative times and may carry slightly higher complication rates compared to Level I [13].
In practice, the choice between Level I and II depends on tumor size, breast volume, tumor-to-breast ratio, and patient expectations. By offering a graded approach, this classification ensures that surgical strategies are tailored to each patient’s unique anatomy and oncological requirements.
Patient Selection and Evaluation
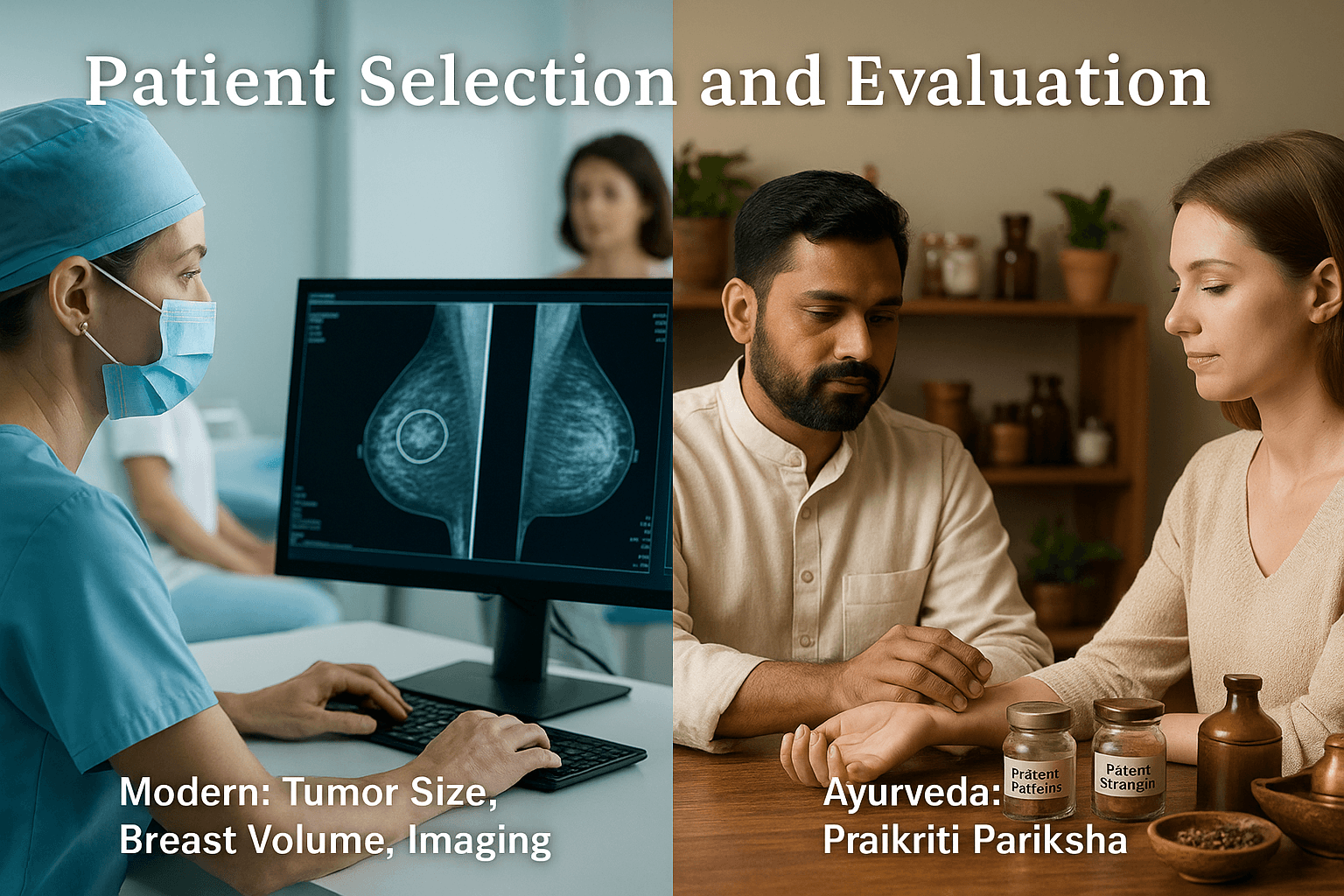
Modern Principles of Patient Selection
Patient selection for oncoplastic breast surgery is a critical determinant of surgical success. Surgeons must weigh both oncological and aesthetic factors to achieve optimal outcomes. Key considerations include tumor size, tumor-to-breast volume ratio, location, and imaging findings. Large tumors in small breasts, for example, pose a higher risk of deformity and may necessitate volume replacement techniques, whereas small tumors in larger breasts may be adequately treated with displacement approaches [1].
Breast volume is an especially important factor. Women with moderate to large breasts have more tissue available for rearrangement, making them better candidates for displacement-based procedures such as therapeutic mammoplasty. Conversely, in women with smaller breast volumes, larger resections can lead to contour irregularities, making replacement or flap-based approaches more suitable [2].
Preoperative imaging—mammography, ultrasound, and increasingly MRI—helps define tumor extent, multifocality, and relationship to cosmetic landmarks such as the nipple-areolar complex [3]. These insights allow surgeons to design excision patterns that maximize oncological safety while anticipating cosmetic outcomes.
Equally important is patient counseling. Women should be informed about the nature of the procedure, potential need for contralateral surgery, risks, complications, and expected recovery. Modern frameworks emphasize shared decision-making, aligning surgical strategies with patient priorities regarding aesthetics, body image, and long-term satisfaction [4].
Thus, the modern approach to patient selection integrates anatomical, pathological, and imaging data with psychosocial considerations to create a comprehensive surgical plan.
Ayurvedic Evaluation- Prakriti and Rogibala
Ayurveda provides a complementary framework for patient evaluation through Prakriti Pariksha (constitution assessment) and Rogibala Pariksha (evaluation of patient strength). Prakriti is determined by the predominance of Vata, Pitta, or Kapha doshas at birth and governs an individual’s physical, physiological, and psychological tendencies [5]. In surgical planning, understanding Prakriti allows for predicting wound-healing capacity, resilience, and response to therapies.
For instance, a Vata-dominant constitution may have thinner tissues, lower adiposity, and slower wound healing, requiring special emphasis on nourishing Rasayanas and Ghrita-based formulations postoperatively. Pitta-dominant individuals, with their strong metabolic fire, may heal faster but be prone to inflammation and scarring, thus benefiting from cooling, anti-inflammatory herbs like Yashtimadhu and Chandana. Kapha-dominant patients, with heavier body frames and slower metabolism, may exhibit robust healing but higher risks of sluggish circulation, edema, and fibrosis, requiring channel-cleansing herbs like Guggulu and Triphala [6].
Rogibala Pariksha assesses the patient’s vitality and capacity to withstand surgery, including factors like age, digestion (Agni), immunity (Ojas), mental stability, and previous disease history [7]. A patient with depleted Ojas, for example, may be more vulnerable to infection or delayed wound healing, and thus Rasayana preconditioning is recommended before surgery.
Through these lenses, Ayurveda emphasizes individualization: the same surgical intervention may demand entirely different postoperative regimens depending on the patient’s Prakriti and Rogibala. This ensures not only tissue healing but systemic balance and prevention of recurrence.
Integrative Evaluation- Aligning Modern and Ayurvedic Paradigms
The most powerful approach to patient selection arises from the integration of modern surgical evaluation with Ayurvedic assessment. Modern oncology provides objective data—tumor size, breast volume, radiologic extent—while Ayurveda personalizes care by aligning interventions with constitutional tendencies and systemic resilience.
For example, a patient with a small breast volume and Vata-dominant constitution may require a volume replacement flap combined with nourishing Rasayanas like Ashwagandha and Shatavari to counter tissue fragility. A Pitta-dominant woman with medium breast volume and inflammatory tendencies may undergo therapeutic reduction mammoplasty but benefit from postoperative use of Amalaki and Guduchi to reduce inflammation. Meanwhile, a Kapha-predominant patient undergoing large excision may be best supported with detoxifying measures such as mild Virechana (purgation) and Triphala to prevent sluggish wound metabolism [8].
This integrative strategy also addresses psychosocial dimensions. Modern frameworks emphasize patient counseling and expectation management, while Ayurveda stresses Satvavajaya Chikitsa (mental balance therapy), yoga, and meditation. Together, they support both body image recovery and mental resilience.
Finally, integrative evaluation offers insights into long-term outcomes. By combining precise surgical excision with constitutional strengthening, the risk of local recurrence, systemic vulnerability, and psychological distress is minimized. This is a step beyond “cancer-free survival”—it aspires to holistic survivorship: a state of restored Sharira (body), Manas (mind), and Ojas (vital force) alongside oncological safety [9].
Surgical Approaches with Ayurvedic Support

Post-Lumpectomy Wound Healing and Ayurvedic Enhancers
Lumpectomy remains a cornerstone of breast-conserving surgery, but postoperative wound healing is often challenged by risks of infection, delayed granulation, fibrosis, and scarring. Modern surgical principles focus on asepsis, suturing techniques, and antibiotics. Ayurveda complements these strategies by offering time-tested herbal wound-healing agents that accelerate tissue repair, reduce inflammation, and minimize scarring.
Haridra (Curcuma longa), revered for its krimighna (antimicrobial) and shothahara (anti-inflammatory) properties, has been shown to inhibit bacterial colonization and stimulate collagen deposition [1]. Yashtimadhu (Glycyrrhiza glabra), with its mucilaginous and cooling properties, supports epithelialization and reduces pain and burning sensation [2]. Lodhra (Symplocos racemosa), traditionally indicated for vrana ropana (wound healing), assists in controlling bleeding and supporting rapid granulation [3].
Modern studies corroborate these properties, with Haridra’s curcumin demonstrating antimicrobial and anti-fibrotic activity, while Yashtimadhu shows significant wound contraction and tensile strength improvement in experimental models [4]. Integrating such formulations—either as topical pastes, medicated ghritas, or decoction washes (kashaya dhavana)—can significantly improve outcomes in lumpectomy wounds.
Thus, combining precise surgical closure with Ayurvedic formulations ensures wounds heal not only structurally but also functionally, reducing complications like hypertrophic scarring or fibrosis.
Symmetrization Procedures and Ayurvedic Hormonal Support
Oncoplastic symmetrization procedures, including contralateral mastopexy or reduction, aim to restore balance between both breasts after tumor excision. While technically successful, these procedures interact with the endocrine system, as breast tissue is hormonally sensitive. Here, Ayurveda offers Stanya Shodhana (breast-cleansing) and Stanya Janana (lactogenic and hormonal-supporting) herbs to optimize recovery and balance [5].
Shatavari (Asparagus racemosus) is described as a potent galactagogue and hormonal regulator, supporting female reproductive tissues while stabilizing estrogenic activity [6]. Vidari Kand (Pueraria tuberosa), a nourishing Rasayana, enhances tissue strength and supports balanced hormonal secretions [7]. Together, they regulate stanya dhatu (lactational tissue) and restore post-surgical equilibrium.
Women undergoing symmetrization often experience transient hormonal imbalances, altered menstrual patterns, or menopausal symptoms if systemic therapies are involved. Ayurvedic support via Rasayana and endocrine-modulating herbs provides resilience against such fluctuations. In practice, this can be delivered as decoctions, ghritas, or powders, tailored to Prakriti and Rogibala.
By supporting hormonal balance, Ayurveda not only aids recovery but also reduces risk of cyclical mastalgia, cystic changes, or delayed healing linked with hormonal disruption.
Panchakarma as Adjunct Post-Surgery
Although not mandatory, Panchakarma therapies can serve as optional but valuable adjuncts in the postoperative recovery phase. They address both systemic detoxification and mental stabilization, domains often overlooked in conventional surgical recovery.
Basti (medicated enema) is particularly indicated for stabilizing Vata dosha, which is easily aggravated by surgical trauma, anesthesia, and psychological stress [8]. By delivering medicated oils or decoctions into the colon, Basti nourishes deeper tissues, enhances circulation, reduces postoperative constipation, and calms neurological imbalances.
Nasya (nasal therapy) plays a role in stress reduction and mental clarity. Using medicated oils like Anu Taila or Brahmi Ghrita, Nasya promotes relaxation, alleviates anxiety, and harmonizes Prana Vata, which governs mental resilience [9]. This can be particularly beneficial for women facing the emotional toll of breast surgery, body image shifts, and cancer-related anxiety.
While Panchakarma must be carefully timed (avoiding the immediate post-surgical period), once wounds have stabilized, it can serve as a rejuvenative adjunct to standard rehabilitation. Unlike chemotherapy or radiotherapy adjuncts, Panchakarma does not add toxicity but instead supports systemic recovery.
Thus, optional Panchakarma offers holistic enhancement: calming doshic imbalances, improving resilience, and ensuring mind-body alignment during the healing journey.
Breast Reconstruction Options & Ayurvedic Perspectives
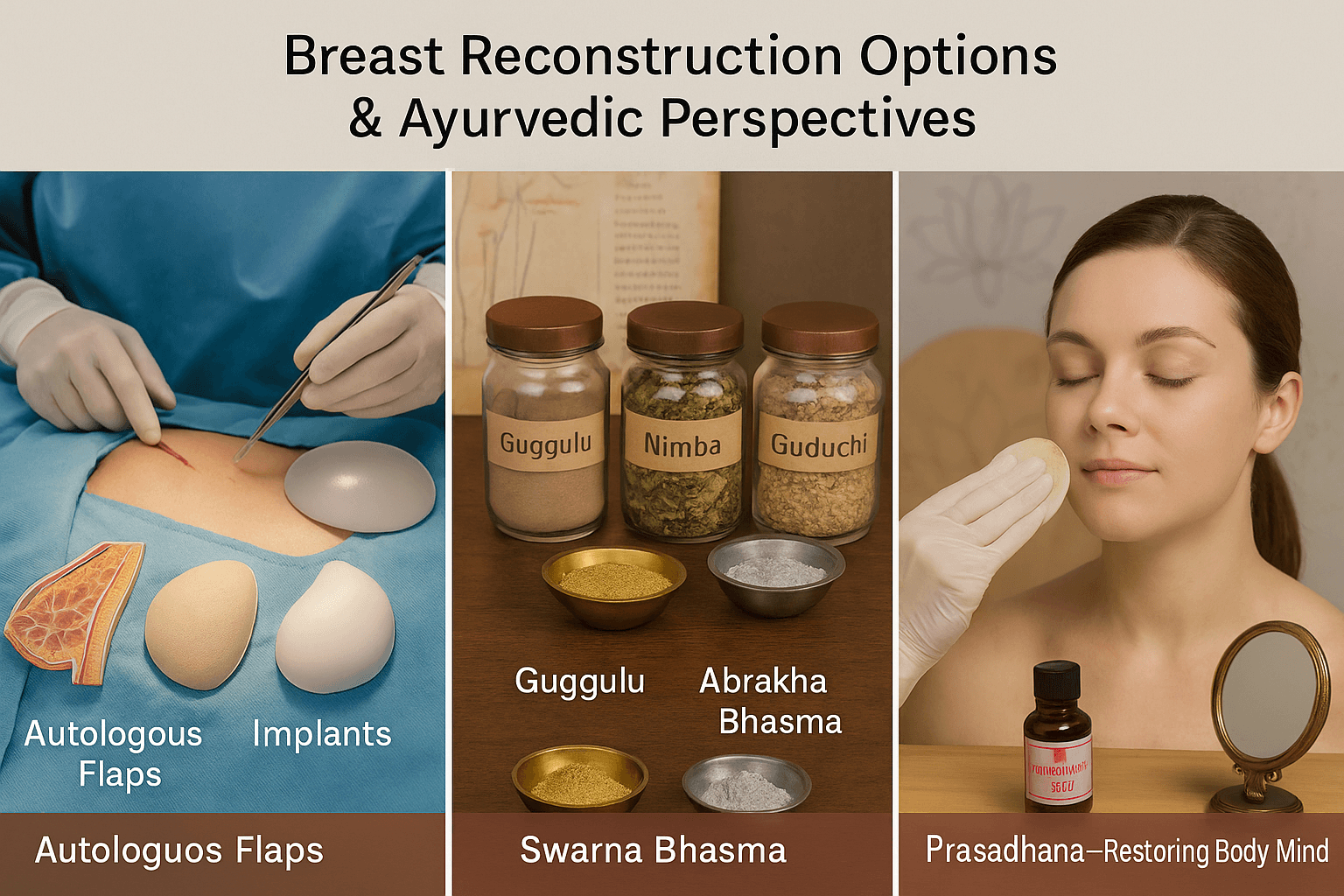
Modern Breast Reconstruction Approaches
Breast reconstruction is a cornerstone of comprehensive cancer care, restoring physical form and emotional well-being after oncological surgery. Modern reconstruction techniques can be broadly categorized into autologous tissue flaps, implant-based procedures, and fat grafting.
Autologous flaps use the patient’s own tissue to recreate the breast mound. The transverse rectus abdominis myocutaneous (TRAM) flap and deep inferior epigastric perforator (DIEP) flap are the most commonly used methods, offering natural contour and texture [1]. Latissimus dorsi flaps remain reliable alternatives, particularly for patients lacking abdominal tissue. Autologous flaps have the advantage of durability and better long-term aesthetic outcomes, though they involve longer operative times and donor-site morbidity [2].
Implant-based reconstruction remains popular for women seeking shorter surgeries and quicker recovery. This involves either a staged expander-to-implant approach or direct-to-implant placement. Recent advances such as prepectoral implant positioning and use of acellular dermal matrices have improved outcomes and reduced complications [3].
Fat grafting has gained significant attention as a minimally invasive option for volume correction and contour refinement. Liposuctioned fat is processed and reinjected into the breast to improve symmetry or correct defects after lumpectomy. While concerns persist about graft resorption and interference with imaging, current evidence supports its safety and efficacy when performed by experienced surgeons [4].
Thus, modern reconstructive surgery offers a spectrum of choices tailored to patient anatomy, preferences, and oncological requirements. Its ultimate goal is to combine oncological safety with restoration of body image and confidence.
Ayurvedic Perspectives- Supporting Flap Survival and Healing
Ayurveda offers complementary strategies to enhance the success of reconstructive procedures by improving circulation, reducing complications, and accelerating healing. Surgical flaps and grafts depend critically on vascular integrity and microcirculation. Ayurvedic herbs with proven srotoshodhana (channel-cleansing) and rasayana (rejuvenative) properties can optimize these parameters.
Guggulu (Commiphora mukul) improves circulation, reduces inflammation, and prevents fibrosis, acting as a vascular tonic for flap survival [5]. Nimba (Azadirachta indica) contributes antimicrobial and detoxifying actions, lowering infection risks in surgical wounds [6]. Arjuna (Terminalia arjuna), traditionally described as a cardio-tonic, enhances vascular tone and tissue oxygenation, indirectly supporting graft perfusion [7].
Beyond circulation, Rasayana therapy plays a pivotal role in systemic rejuvenation and tissue regeneration. Swarna Bhasma (incinerated gold) is renowned for its ability to promote cellular repair, boost immunity, and accelerate tissue integration [8]. Abhrak Bhasma (incinerated mica) supports microcirculation, nourishes deeper tissues (dhatus), and aids in wound healing [9]. Guduchi Satva (Tinospora cordifolia extract) provides potent immunomodulatory effects, reducing postoperative infections and strengthening overall resilience [10].
This combination of circulation-promoting herbs and Rasayana Bhasmas creates a supportive milieu for surgical outcomes. By enhancing blood flow, immunity, and tissue repair, Ayurveda offers a parallel healing channel that works synergistically with modern techniques.
Reconstruction is not only about restoring anatomy but also about reclaiming identity, confidence, and social presence. Modern literature underscores the psychological benefits of reconstruction, showing improvements in quality of life, body image, and sexual health [11]. Ayurveda expands this scope by integrating Prasadhana therapies—restorative and beautifying measures that go beyond physical repair.
Prasadhana encompasses external therapies, herbal applications, and lifestyle practices aimed at restoring both appearance and inner confidence. Medicated oils like Kumkumadi Taila and herbal lepas (cosmetic pastes) enhance skin tone and scar aesthetics, complementing surgical outcomes [12]. Ayurvedic facial and body therapies help women reconnect with their bodies, reestablishing positive self-perception after trauma.
Equally important is the restoration of manas shakti (mental strength). Postoperative distress, anxiety, or depression can hinder recovery. Ayurveda addresses this with Satvavajaya Chikitsa (mind-strengthening therapies), yoga, pranayama, and meditation. These practices not only reduce stress hormones but also foster acceptance, empowerment, and resilience [13].
Thus, the Ayurvedic concept of Prasadhana aligns seamlessly with modern psycho-oncology by focusing on body image, confidence, and holistic well-being. The integration of external therapies, Rasayana support, and mind-body practices ensures that reconstruction achieves more than anatomical replacement—it becomes a process of personal renewal and emotional healing.
Fat Grafting and Rasayana Synergy
Modern Perspective- Fat Grafting for Contour Correction
Fat grafting has become an increasingly popular adjunct in breast reconstruction, particularly for contour correction after lumpectomy, mastectomy, or implant-based procedures. The technique involves harvesting autologous fat through liposuction, processing it to remove impurities, and reinjecting it into the breast to improve shape, volume, and symmetry [1].
One of the greatest strengths of fat grafting is its minimally invasive nature. Unlike flap reconstruction, which requires major tissue transfer, fat grafting uses small-volume liposuction from donor sites such as the abdomen, thighs, or flanks. This makes it an attractive option for women seeking natural tissue-based refinement with reduced surgical morbidity [2].
Clinical evidence shows that fat grafting enhances not only cosmetic results but also patient satisfaction and quality of life. It is particularly effective for correcting contour irregularities, filling lumpectomy defects, and refining implant edges [3]. In addition, emerging data suggest that fat grafts may promote tissue regeneration through adipose-derived stem cells, improving skin quality and reducing radiation-induced fibrosis [4].
Despite its benefits, challenges exist. Variable fat resorption rates, risk of oil cysts, and the need for multiple sessions remain common concerns [5]. Long-term oncological safety has been studied extensively, with most evidence supporting that fat grafting does not increase recurrence risk when performed in properly selected patients [6].
Thus, fat grafting stands as a valuable tool in the reconstructive surgeon’s armamentarium, offering natural, minimally invasive, and biologically supportive correction of breast contours.
Ayurvedic Perspective- Medo Dhatu Rejuvenation
Ayurveda interprets fat tissue through the lens of Medo Dhatu, one of the seven fundamental body tissues (dhatus). Healthy Medo Dhatu contributes to structural support, energy storage, lubrication of joints, and protection of organs. When vitiated, it can result in imbalances such as obesity, sluggish metabolism, or conversely, tissue depletion [7].
In the context of breast reconstruction and fat grafting, Ayurvedic strategies emphasize rejuvenation and balancing of Medo Dhatu to ensure graft survival, harmonious fat distribution, and long-term systemic stability. Classical texts prescribe herbs and formulations that regulate fat metabolism while maintaining tissue vitality.
Guggulu (Commiphora mukul) is a prime medohara (fat-regulating) herb that improves circulation, reduces inflammation, and optimizes fat tissue function [8]. Triphala, a combination of Haritaki, Amalaki, and Bibhitaki, cleanses channels (srotas), prevents stagnation, and supports balanced fat metabolism [9]. Formulations like Medohara Rasayana specifically target pathological accumulation of fat while preserving the functional quality of Medo Dhatu [10].
These interventions ensure that fat grafts integrate effectively without excessive resorption or fibrosis. Additionally, they prevent systemic side effects such as sluggish digestion or impaired circulation that could undermine surgical outcomes.
By addressing fat as a dynamic and metabolic tissue rather than merely structural filler, Ayurveda provides a framework for ensuring sustainable results from modern fat grafting procedures.
Rasayana Synergy- Fat Metabolism and Long-Term Safety
The concept of Rasayana therapy adds an additional dimension to fat grafting by focusing on systemic rejuvenation, immune modulation, and metabolic balance. Unlike interventions that address only the surgical site, Rasayana therapies optimize the host terrain, which directly influences graft survival and long-term outcomes.
Herbs such as Guduchi (Tinospora cordifolia), Amalaki (Emblica officinalis), and Ashwagandha (Withania somnifera) serve as broad-spectrum Rasayanas that strengthen immunity, enhance microcirculation, and stabilize fat metabolism [11]. Their antioxidant and anti-inflammatory actions parallel modern findings that oxidative stress and inflammation impair graft survival [12].
Mineral Rasayanas like Abhrak Bhasma improve microvascular flow and tissue oxygenation, while Swarna Bhasma promotes cellular repair and integration of transplanted tissue [13]. Together, these Rasayanas create an internal environment conducive to long-term graft stability.
From a holistic standpoint, Ayurveda insists on lifestyle alignment to support Medo Dhatu balance. Balanced diet (ahara), moderate physical activity (vyayama), and purification therapies (srotoshodhana) ensure that fat grafts remain metabolically active, rather than becoming stagnant or pathologically altered.
Thus, the synergy of modern fat grafting with Rasayana therapy creates a two-layered approach: modern surgery restores external form, while Rasayana ensures systemic harmony and long-term safety. This integration reduces risks of fat necrosis, repeated procedures, and systemic imbalances, transforming reconstruction into a sustainable, whole-body healing process.
Oncoplastic in Special Situations

Genetic Carriers-Beejadosha and Garbhini Charya
Modern oncology recognizes that women carrying genetic mutations such as BRCA1 and BRCA2 face a significantly elevated lifetime risk of breast and ovarian cancers [1]. Surgical strategies for such patients often include prophylactic mastectomy with immediate or delayed reconstruction, alongside enhanced surveillance programs.
Ayurveda interprets these inherited vulnerabilities through the lens of Beejadosha—defects or imbalances in the reproductive seed (Beeja), which predispose future generations to specific conditions [2]. Classical texts highlight the importance of correcting these vulnerabilities not after disease manifestation but before conception, through a structured protocol called Garbhini Charya (pre-conception and prenatal regimen) [3].
Garbhini Charya includes purification therapies (shodhana), dietary regimens, and Rasayana formulations designed to strengthen reproductive tissue quality, purify genetic channels, and enhance immunity. Herbs such as Amalaki, Guduchi, and Shatavari are prescribed to restore balance at the seed level [4]. Mineral Rasayanas like Swarna Bhasma are described to promote superior progeny (supraja janana).
For women with hereditary risk undergoing oncoplastic surgery, Ayurvedic preconditioning through Rasayana can improve surgical resilience, reduce recurrence risk, and foster systemic vitality. This integrative strategy addresses both genetic predisposition and environmental triggers, aiming for comprehensive protection.
Post-Chemotherapy-Panchakarma Detoxification
Modern breast cancer management often employs chemotherapy before or after surgery to downstage tumors, eradicate micrometastases, and improve survival [5]. While effective, chemotherapy is associated with residual toxicity—manifesting as fatigue, neuropathy, impaired wound healing, and immune suppression. These after-effects can compromise recovery and reconstruction outcomes.
Ayurveda provides a structured response through Panchakarma, particularly Virechana (therapeutic purgation) and Basti (medicated enemas), to eliminate accumulated toxins (ama) and restore doshic balance [6]. Virechana, using formulations such as Trivrit Lehya or medicated castor oil, cleanses the gastrointestinal tract and liver, facilitating metabolic reset and improved tissue nutrition. Basti nourishes and stabilizes Vata dosha, which is often aggravated by chemotherapy-induced fatigue and neurological toxicity [7].
These therapies not only clear residual cytotoxic load but also prepare the body for Rasayana administration, which then restores Ojas (vital energy). Herbs like Ashwagandha, Amalaki, and Guduchi have demonstrated radioprotective and chemoprotective effects in modern studies, validating their inclusion in post-chemotherapy care [8].
For surgical candidates, Panchakarma thus ensures cleaner channels, improved circulation, and stronger immunity, enhancing both flap survival and postoperative recovery.
Inflammatory Cancers-Kshara Kalpa and Rakta Prasadana
Inflammatory breast cancer (IBC) is a rare but aggressive subtype characterized by diffuse erythema, edema, dermal lymphatic invasion, and rapid progression [9]. Management requires multimodal therapy, including neoadjuvant chemotherapy, mastectomy with reconstruction, and radiotherapy. Outcomes remain poor compared to non-inflammatory cancers.
Ayurveda parallels these features with conditions arising from Rakta Dushti (vitiation of blood) and aggravated Pitta and Kapha doshas [10]. Classical therapeutics include Kshara Kalpa (alkaline formulations) for resolving aggressive, infiltrative pathology, and Rakta Prasadana dravyas (blood-purifying herbs) to detoxify and stabilize circulation [11].
Kshara Kalpa, derived from alkaline extracts of plants like Apamarga (Achyranthes aspera), has caustic, tumor-reducing, and channel-cleansing properties [12]. These are used cautiously as adjuncts to debulk infiltrative processes. Simultaneously, Rakta Prasadana herbs such as Manjistha (Rubia cordifolia) and Sariva (Hemidesmus indicus) are prescribed for anti-inflammatory, detoxifying, and microcirculatory effects [13].
Modern pharmacological research supports Manjistha’s role in inhibiting angiogenesis and Sariva’s antioxidant and anti-inflammatory activity. Together, they provide systemic support, mitigating the aggressive biology of IBC while preparing the body for intensive treatment and reconstruction.
By combining modern multimodal treatment with Ayurvedic interventions, the goal is not only to manage the aggressive cancer but also to reduce systemic toxicity, enhance resilience, and support long-term healing.
Recent Advances and Ayurvedic Research Directions
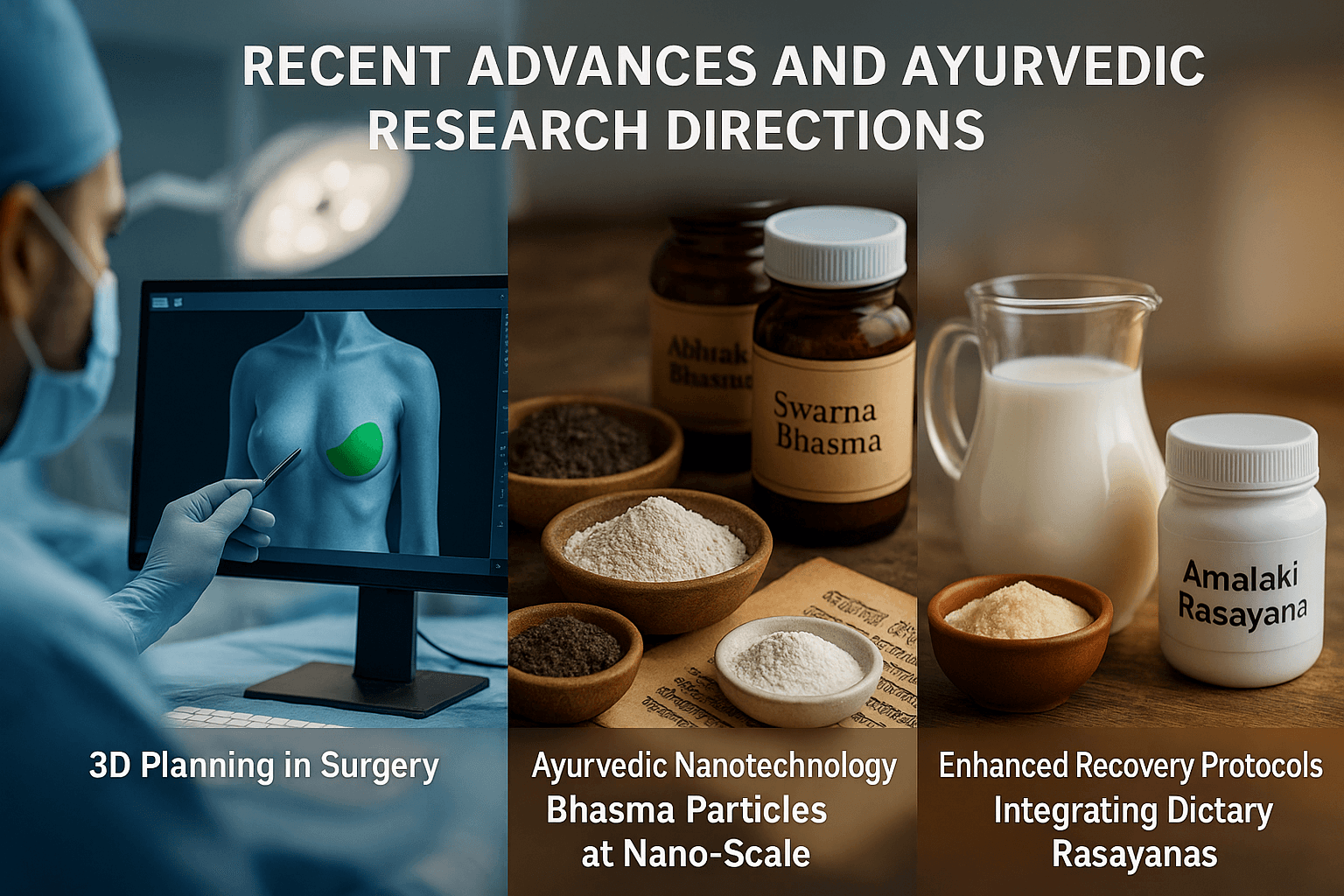
3D planning in surgery ↔ Ayurvedic nanotechnology (Bhasma at nano-scale)
Patient-specific 3D planning has become a powerful adjunct in oncoplastic and reconstructive breast surgery. Surgeons now use 3D surface imaging, CAD models, and 3D-printed guides to simulate resections, plan pedicles, and previsualize symmetry, which can shorten operative time and improve aesthetic predictability and patient satisfaction [1,2]. In parallel, microscale navigation templates and model-guided inset planning help anticipate volume displacement vs. replacement trade-offs before the first incision is made [1].
Ayurveda’s research frontier mirrors this precision trend through Ayurvedic nanomedicine: several characterization studies show that classical Bhasma preparations (e.g., Swarna Bhasma, Abhrak Bhasma) contain nano- to sub-micron particles when prepared with orthodox shodhana/marana protocols. Reported data include crystalline nanogold in Swarna Bhasma by XRD/FE-TEM and ~28–35 nm crystallites with favorable blood compatibility profiles; Abhrak Bhasma (mica) has likewise been characterized with modern analytical methods [7–9]. While clinical translation requires rigor and regulatory clarity, these findings suggest a plausible nano-scale basis for classical claims of targeted, low-dose, tissue-level effects—an intriguing parallel to modern personalization via 3D planning [7–9].
Microsurgical flap advances ↔ Rasayana to support microcirculation
Modern reconstruction increasingly leverages perforator-based flaps (e.g., DIEP), supermicrosurgery (lymphaticovenular anastomoses), and even robotic-assisted microsurgery, expanding options while reducing donor-site morbidity [3,4]. Contemporary protocols emphasize intraoperative perfusion assessment, meticulous venous outflow, and lymphedema mitigation—each hinging on microvascular integrity [3].
Ayurveda addresses the same physiologic bottleneck through Rasayana and srotas-oriented care: herbs and formulations that aim to optimize microcirculation, dampen inflammation, and strengthen tissue integration. Classical Rasayanas such as Amalaki Rasayana show antioxidant and immunomodulatory effects in experimental systems, while dietary ghṛta (ghee)—classically a Rasayana carrier—has emerging modern reviews discussing immunonutritive roles (used judiciously within balanced diets) [10,11]. These data support a plausible adjunctive role: Rasayana-guided nutrition and convalescence practices may help stabilize the flap milieu (microvascular tone, oxidative balance, host immunity) alongside standard antithrombotic, warming, and fluid strategies [3,10,11].
Enhanced Recovery After Surgery (ERAS) ↔ Dietary Rasayanas (milk, ghee, Amalaki Rasayana)
ERAS pathways for implant-based and autologous reconstruction consistently report less opioid use, shorter length of stay, faster mobilization, and equal or improved complication profiles when multimodal analgesia, early feeding, and standardized rehabilitation are used [5]. Recent overviews reinforce tailoring ERAS to reconstruction type (e.g., abdominal donor sites vs. prepectoral implants), perioperative nausea control, and thrombo-prophylaxis—without compromising oncologic timelines [5,6].
Ayurveda offers dietary Rasayana concepts that can be folded into ERAS-style nutrition: kṣhīra (milk) and ghṛta (ghee) as digestible, anabolic carriers for herbs, and Amalaki Rasayana for redox balance and immune tone—always individualized to prakriti and agni and mindful of modern lipid guidance [10,11]. Practically, this means (with clinical oversight): small, early, easily digestible feeds; measured use of ghṛta as a vehicle for Amalaki/Guduchi where appropriate; and graduated ambulation and yogic breathing to complement ERAS mobilization. The shared goal is faster functional recovery with fewer symptoms, by uniting perioperative standardization (ERAS) with personalized Rasayana-centric convalescence [5,6,10,11].
FAQs
1. What is oncoplastic breast surgery?
Oncoplastic breast surgery combines cancer removal with plastic surgical techniques. It ensures the tumor is excised safely while preserving or reconstructing breast shape for better physical and emotional recovery.
2. How does Ayurveda complement oncoplastic surgery?
Ayurveda supports surgery through Shalya Chikitsa principles: Shuddhi (complete excision of diseased tissue), Ropana (healing of wounds), and Rasayana (rejuvenation for long-term resilience). It also addresses the mental dimension (Manas) through yoga, meditation, and Satvavajaya Chikitsa.
3. Can Ayurvedic Rasayanas improve healing after surgery?
Yes. Herbs like Haridra (turmeric), Yashtimadhu (licorice), and Lodhra (Symplocos racemosa) promote wound healing, while Guduchi (Tinospora cordifolia), Amalaki (Emblica officinalis), and Ashwagandha (Withania somnifera) strengthen immunity and support microcirculation.
4. What are the benefits of integrating Ayurveda in reconstruction?
Ayurveda can:
- Improve wound healing and scar aesthetics.
- Reduce inflammation and infection risk.
- Support hormonal balance after symmetrization procedures.
- Enhance flap survival with circulation-promoting herbs like Guggulu and Arjuna.
- Rebuild self-confidence through Prasadhana (restorative therapies).
5. Is fat grafting safe when combined with Ayurveda?
Modern evidence shows fat grafting is safe for contour correction. Ayurveda strengthens Medo Dhatu (fat tissue) using Guggulu, Triphala, and Medohara Rasayana, which improve fat metabolism and reduce risks of fibrosis or fat resorption.
6. Can Ayurveda help women with genetic risk such as BRCA mutations?
Ayurveda explains hereditary vulnerabilities as Beejadosha. Preventive care is offered through Garbhini Charya (pre-conception Rasayanas) that enhance genetic resilience. For carriers undergoing surgery, Rasayana therapy may improve recovery and reduce systemic vulnerability.
7. How can Ayurveda assist after chemotherapy or radiation?
Detoxification through Panchakarma (Virechana, Basti, Nasya) eliminates residual toxins, stabilizes Vata dosha, and restores immunity. This prepares the body for reconstruction and reduces fatigue, neuropathy, and wound-healing delays.
8. Are there Ayurvedic options for aggressive cancers like inflammatory breast cancer?
Yes. Ayurveda recommends Kshara Kalpa (alkaline therapies) to target infiltrative processes and Rakta Prasadana herbs such as Manjistha and Sariva to cleanse and stabilize the blood, complementing modern multimodal therapy.
9. What role do dietary Rasayanas play in recovery?
Just as Enhanced Recovery After Surgery (ERAS) emphasizes early feeding, Ayurveda prescribes milk, ghee, and Amalaki Rasayana to nourish tissues, improve immunity, and speed rehabilitation.
10. Is this integration accepted by modern science?
Modern clinical studies confirm the safety and effectiveness of oncoplastic surgery. Ayurvedic therapies are increasingly being researched for wound healing, immune modulation, and nanomedicine applications of Bhasma. Together, they offer a promising path in integrative oncology.
References
- Albornoz, C. R., Bach, P. B., Mehrara, B. J., Disa, J. J., Pusic, A. L., McCarthy, C. M., & Cordeiro, P. G. (2014). A paradigm shift in U.S. breast reconstruction: Increasing implant rates. Plastic and Reconstructive Surgery, 131(1), 15–23. https://doi.org/10.1097/PRS.0b013e3182729cde
- Clough, K. B., Kaufman, G. J., Nos, C., Buccimazza, I., & Sarfati, I. M. (2010). Improving breast cancer surgery: A classification and quadrant per quadrant atlas for oncoplastic surgery. Annals of Surgical Oncology, 17(5), 1375–1391. https://doi.org/10.1245/s10434-009-0792-y
- Losken, A., Dugal, C. S., Styblo, T. M., & Carlson, G. W. (2014). A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Annals of Plastic Surgery, 72(2), 145–149. https://doi.org/10.1097/SAP.0b013e31825ea982
- Kronowitz, S. J., & Robb, G. L. (2009). Oncoplastic breast surgery: A review and systematic approach. Journal of Surgical Oncology, 99(2), 111–118. https://doi.org/10.1002/jso.21217
- Jeevan, R., Cromwell, D. A., Browne, J. P., Caddy, C. M., Pereira, J., Sheppard, C., … & Holcombe, C. (2014). Findings of a national comparative audit of oncoplastic breast conserving surgery in England. Breast, 23(6), 335–342. https://doi.org/10.1016/j.breast.2014.07.017
- Tamma, R., & Bonifacino, A. (2015). Clinical applications of fat grafting in breast surgery. Journal of Breast Cancer, 18(1), 9–15. https://doi.org/10.4048/jbc.2015.18.1.9
- Sushruta. (2007). Sushruta Samhita (English translation, Vol. 1–3). Chaukhambha Sanskrit Series Office. (See Chikitsa Sthana 1, 27–29 for Rasayana and wound healing).
- Charaka. (2001). Charaka Samhita (English translation by R. K. Sharma & Bhagwan Dash). Chowkhamba Sanskrit Series Office. (See Chikitsa Sthana 1, Rasayana Adhyaya).
- Sharma, R., Amin, H., Galib, R., Prajapati, P. K., & Ravishankar, B. (2014). Therapeutic potential of Suvarna Bhasma: A review. Ayu, 35(4), 335–339. https://doi.org/10.4103/0974-8520.158980
- Paul, W., & Sharma, C. P. (2011). Blood compatibility studies of Swarna Bhasma (Gold Bhasma). International Journal of Ayurveda Research, 1(4), 280–284. https://doi.org/10.4103/0974-7788.76791
- Rajani, J., Sumantran, V. N., & Bapat, R. D. (2012). Immunomodulatory activity of Amalaki Rasayana in laboratory models. Journal of Ayurveda and Integrative Medicine, 3(2), 112–118. https://doi.org/10.4103/0975-9476.96519
- Pandey, M. M., Rastogi, S., & Rawat, A. K. (2013). Indian traditional Ayurvedic system of medicine and nutritional supplementation. Evidence-Based Complementary and Alternative Medicine, 2013, 376327. https://doi.org/10.1155/2013/376327
- Biswas, S., Ghosh, A., & Chattopadhyay, P. (2021). Characterization and bioactivity of Suvarna Bhasma: A nanomedicine perspective. Nanobiomedicine, 8, 1–9. https://doi.org/10.1177/18495435211019044
- Kantak, S. S., et al. (2020). Analytical study of Abhraka Bhasma prepared by two different methods. Ayu, 41(1), 39–46. https://doi.org/10.4103/ayu.AYU_212_18
- Kataria, D., et al. (2024). Health benefits of ghee: A review of Ayurveda and modern evidence. Journal of Ayurveda and Integrative Medicine, 15(3), 100781. https://doi.org/10.1016/j.jaim.2024.100781