- Normal Menstrual Physiology
- How hormones guide your period
- The four phases of the cycle
- How Ayurveda explains the menstrual cycle
- Why this understanding is important
- Classification of Menstrual Disorders
- 2.Dysmenorrhea
- 3.Menorrhagia
- 4.Oligomenorrhea
- 5.Polymenorrhea
- 6.Metrorrhagia
- 7. Premenstrual Syndrome (PMS) and PMDD
- Symptoms and Clinical Features
- Diagnostic Approaches
- Complications if Untreated
- Frequently Asked Questions
- References
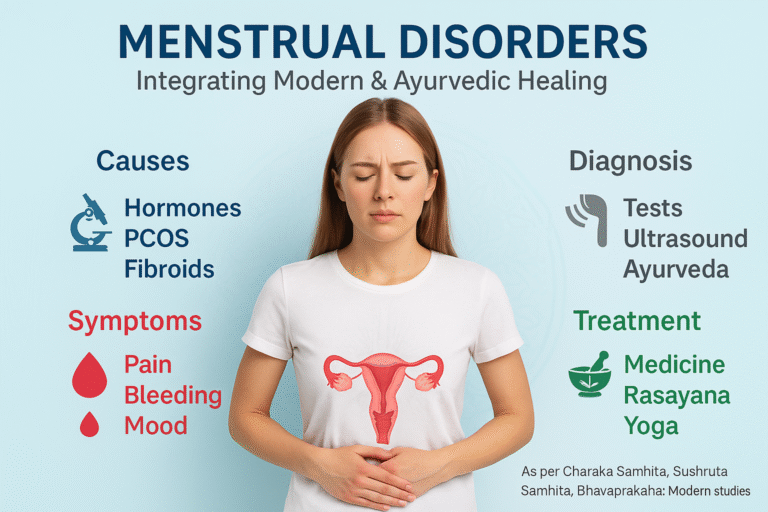
Menstrual disorders refer to a wide range of conditions that disturb the normal rhythm, flow, or symptoms associated with a woman’s monthly cycle. These may include irregular cycles, absence of menstruation, excessive bleeding, painful periods, or significant emotional and physical changes before menstruation. While occasional variations are common, persistent abnormalities often indicate underlying hormonal, structural, or systemic imbalances. In Ayurveda, such disturbances are linked to dysfunction of Artava (menstrual blood and ovum), impairment of Apana Vata (the downward-moving energy), and imbalance in Rasa and Rakta Dhatus (plasma and blood tissues).
Global prevalence and impact on women’s health
Menstrual disorders are among the most common gynecological complaints worldwide, affecting nearly 30–40% of women of reproductive age at some point in their lives. They contribute significantly to absenteeism from school and work, impaired productivity, emotional stress, and reduced quality of life. Heavy menstrual bleeding alone accounts for nearly one-third of gynecological referrals globally, while dysmenorrhea (painful periods) is reported by more than half of young women. Chronic cases may lead to anemia, infertility, or metabolic complications, further amplifying the disease burden.
Importance of integrative perspectives (modern gynecology + Ayurveda)
Modern gynecology offers valuable diagnostic tools, pharmacological therapies, and surgical interventions that address immediate symptoms and structural causes. However, many women continue to experience side effects or incomplete relief with conventional treatments. Ayurveda, on the other hand, emphasizes the root cause of imbalance, linking menstrual health to digestion, lifestyle, emotional state, and systemic harmony. By integrating modern precision diagnostics with time-tested Ayurvedic interventions such as Shamana (balancing therapies), Rasayana (rejuvenatives), and optional Shodhana (detox procedures), women can achieve not only symptom control but also long-term restoration of reproductive and overall health. This integrative framework is particularly relevant in an era where women seek both safety and sustainability in healthcare choices.
Normal Menstrual Physiology
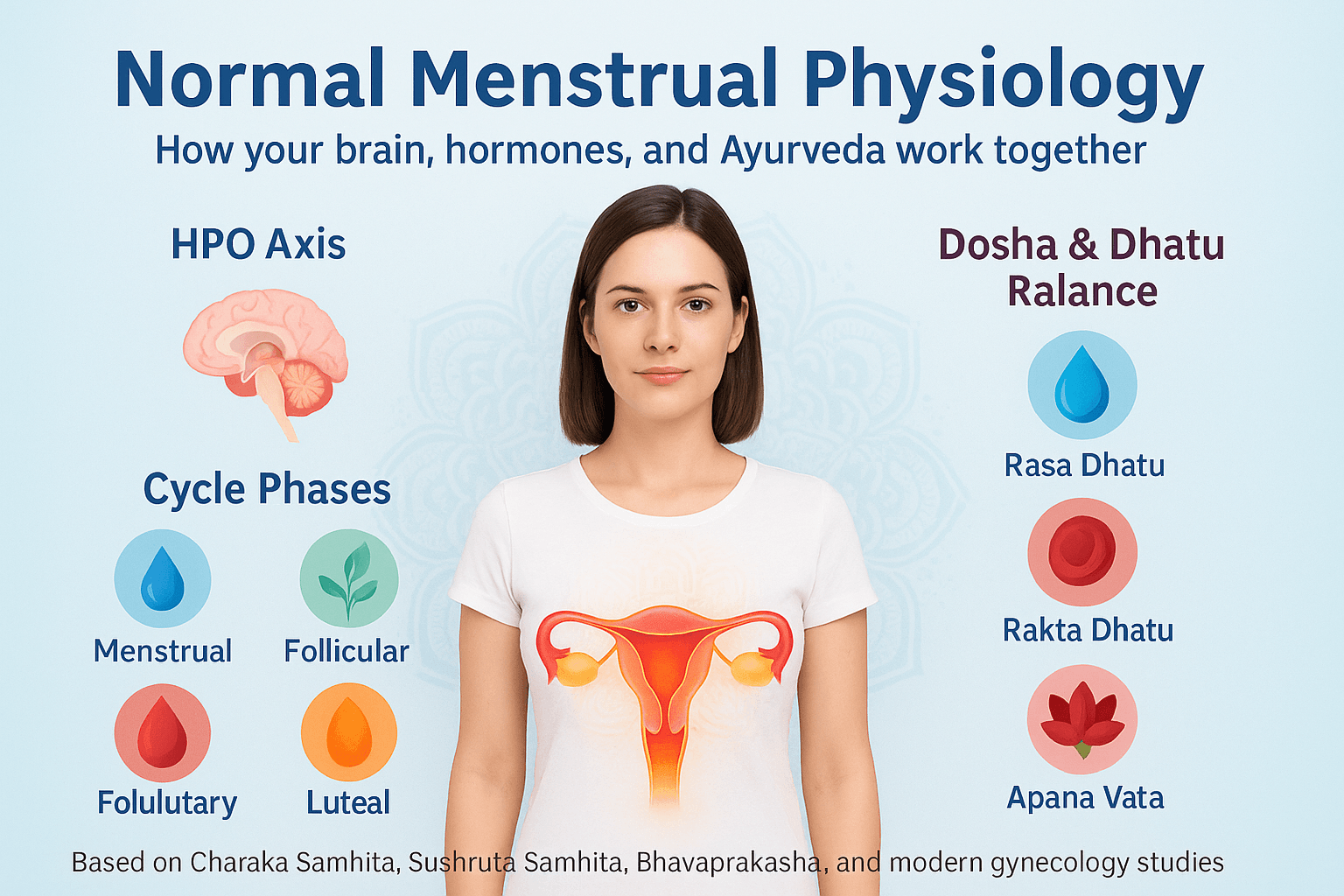
How hormones guide your period
Your menstrual cycle is controlled by a smart internal system called the hypothalamic–pituitary–ovarian (HPO) axis. You can imagine it as a chain of messages between your brain and your ovaries.
- The hypothalamus (a small part of your brain) sends out a signal that it is time to begin the cycle.
- The pituitary gland, which sits just below the brain, answers this signal by sending two important messengers: FSH (follicle-stimulating hormone) and LH (luteinizing hormone).
- These messengers travel in the blood to your ovaries, where they encourage the growth of eggs and stimulate the production of hormones—mainly estrogen and progesterone.
Estrogen helps the uterus lining to grow and prepare for a possible pregnancy, while progesterone supports this lining after the egg has been released. If the egg is not fertilized, the levels of estrogen and progesterone fall, and this drop tells the body to start shedding the lining of the uterus. This shedding is what we see as menstrual bleeding.
The four phases of the cycle
The average menstrual cycle lasts around 28 days, though anything between 21 and 35 days can be normal. It has four distinct phases, each with its own purpose:
- Menstrual phase (Day 1–5): This is when bleeding happens. The uterus clears away the old lining it had built up, which leaves the body as menstrual blood. Many women experience cramps at this time because the uterus is contracting to push the lining out.
- Follicular phase (Day 1–14, overlapping with menstruation at the start): The ovaries prepare a group of eggs, and one of them starts to mature under the influence of FSH. Estrogen levels begin to rise, encouraging the uterine lining to grow fresh and thick, ready to welcome a fertilized egg.
- Ovulatory phase (around Day 14 in a 28-day cycle): A sharp rise in LH triggers the release of a mature egg from the ovary. This is ovulation. At this point, a woman is most fertile. Some women may notice clear, stretchy vaginal discharge or mild abdominal twinges as signs of ovulation.
- Luteal phase (Day 15–28): After releasing the egg, the empty follicle in the ovary becomes the corpus luteum, which produces progesterone. This hormone stabilizes the uterine lining, making it ready for pregnancy. If pregnancy does not happen, the corpus luteum breaks down, progesterone levels fall, and the next period begins.
How Ayurveda explains the menstrual cycle
Ayurveda sees the menstrual cycle not just as a process of hormones but as a reflection of the balance of body energies and tissues.
- Rasa Dhatu (nourishing body fluids): This is the first body tissue created after digestion and is responsible for providing nutrition to the whole body. It plays a key role in keeping periods regular and healthy.
- Rakta Dhatu (blood tissue): Healthy Rakta means healthy blood and proper flow. Impurities or imbalance in Rakta Dhatu can lead to heavy, scanty, or painful periods.
- Artava (reproductive essence): This is the specific reproductive tissue in women that includes both menstrual blood and the ovum (egg). It is a direct sign of fertility and reproductive strength.
- Apana Vata (downward-moving energy of Vata dosha): This vital energy controls the movement of menstrual blood, the release of the ovum, and the timing of menstruation. When Apana Vata is disturbed, women may face irregular cycles, cramps, or even absent periods.
Why this understanding is important
Looking at menstruation from both modern and Ayurvedic perspectives shows that your period is not just about bleeding once a month. It is a mirror of your overall health. A smooth, pain-free, and regular cycle often means that hormones, organs, and body energies are all working in balance. On the other hand, irregular, painful, or very heavy periods may be a sign of deeper imbalance—whether hormonal, nutritional, or energetic.
By understanding how your cycle normally works, you can become more aware of your body’s signals, seek help when changes appear, and use both modern science and Ayurveda to restore balance.
Classification of Menstrual Disorders
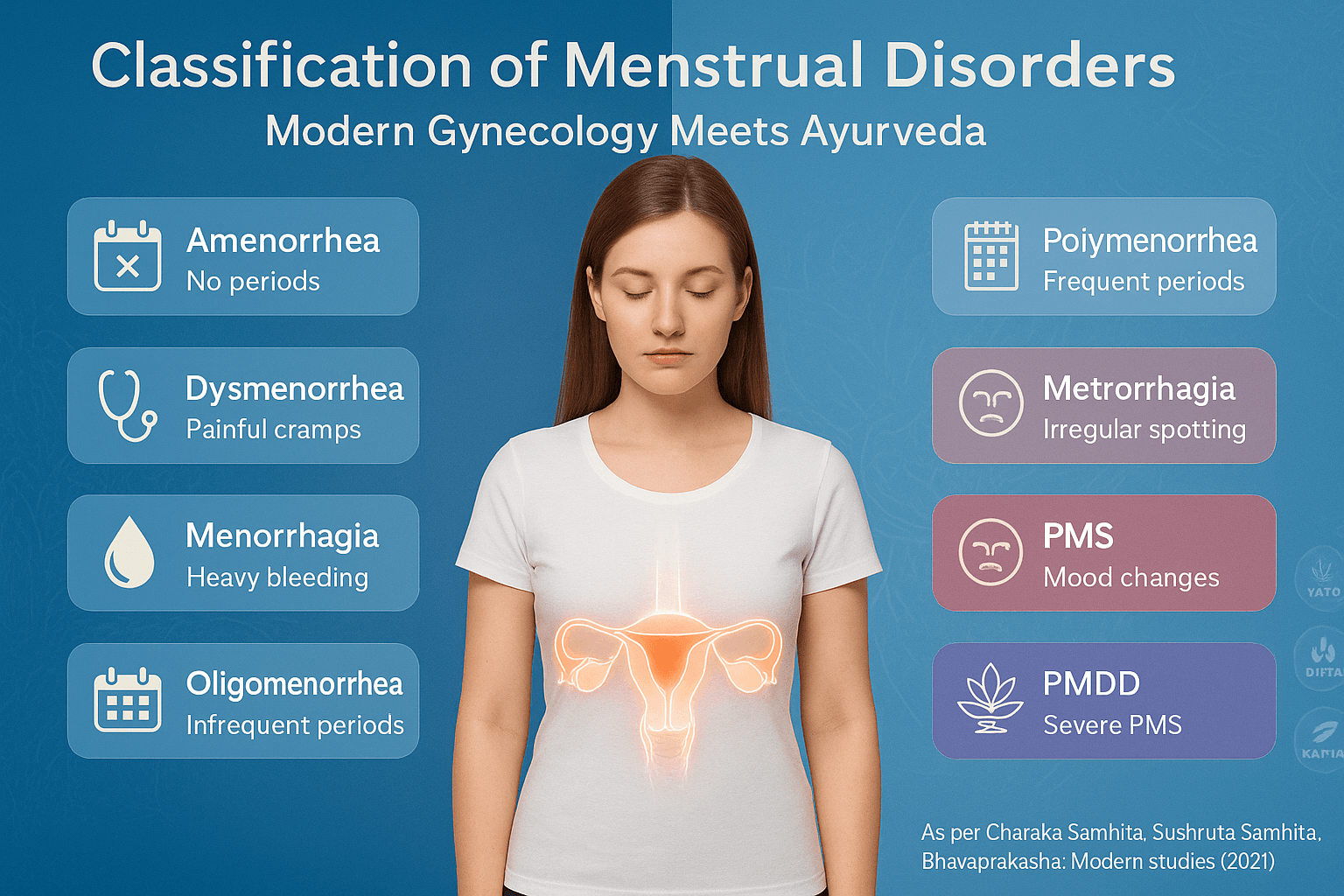
Menstrual disorders affect the timing, flow, and symptoms of the monthly cycle. They may range from missed periods to heavy bleeding or severe pain. Below are the main types.
- Amenorrhea
- Dysmenorrhea
- Menorrhagia
- Oligomenorrhea
- Polymenorrhea
- Metrorrhagia
- PMS/PMDD
1.Amenorrhea
Amenorrhea means the absence of menstruation.
- Primary amenorrhea happens when a girl does not start her periods by age 15–16, even though other signs of puberty are present. Causes may include genetic conditions, hormonal imbalance, or structural problems in the reproductive organs [1].
- Secondary amenorrhea occurs when a woman who previously had normal cycles stops menstruating for three months or longer. Common causes include pregnancy, PCOS, thyroid issues, high stress, or premature ovarian failure [2].
In Ayurveda, amenorrhea is linked to Apana Vata imbalance and poor nourishment of Artava Dhatu (the reproductive tissue) [3].
Amenorrhea refers to the absence of menstruation, which may be either primary or secondary depending on when it occurs.
Now let’s understand it more in detail
Primary Amenorrhea
Primary amenorrhea is diagnosed when a girl has not experienced her first menstrual period by the age of 15–16, despite showing other signs of puberty such as breast development and growth of pubic hair [1]. This condition may result from genetic abnormalities like Turner syndrome or androgen insensitivity syndrome, hormonal disruptions involving the hypothalamus, pituitary gland, or ovaries, and structural issues such as absence of the uterus or obstruction of the vaginal canal [2].
Secondary Amenorrhea
Secondary amenorrhea occurs when a woman who previously had regular menstrual cycles stops menstruating for three months or longer [3]. While pregnancy and breastfeeding are natural causes, other factors include polycystic ovary syndrome (PCOS), thyroid disorders, premature ovarian insufficiency, and lifestyle-related conditions such as extreme weight loss, over-exercise, or high stress. Certain medications, particularly chemotherapy drugs and hormonal contraceptives, can also lead to secondary amenorrhea [4].
Symptoms and Complications
The primary symptom of amenorrhea is the absence of menstruation, but women may also experience infertility, weight fluctuations, mood changes, or hot flashes depending on the underlying cause. If estrogen levels remain chronically low, complications such as osteoporosis and reduced bone density may occur over time [5].
Ayurvedic Perspective
In Ayurveda, amenorrhea is described as Nashta-Artava, which literally means the loss of menstrual flow. Classical texts explain it primarily as a disorder of Apana Vata, the downward-moving energy that governs menstruation, urination, and childbirth [6]. When Vata becomes aggravated, it can obstruct or dry the channels (Srotas), preventing normal flow. Deficiency of Rasa Dhatu (plasma tissue) and Rakta Dhatu (blood tissue) also weakens the generation of Artava (menstrual blood). In some cases, excess Kapha may block reproductive channels, while excess Pitta may cause damage or depletion of reproductive tissue. References in Charaka Samhita (Chikitsa Sthana 30) and Sushruta Samhita (Sharira Sthana 2) indicate that poor diet, excessive stress, or irregular lifestyle can disturb Apana Vata and result in absent menstruation.
Treatment Approaches
Modern treatment of amenorrhea focuses on correcting the underlying cause. This may include hormonal therapy for thyroid disorders or premature ovarian failure, treatment for PCOS, or lifestyle correction in cases of stress and malnutrition. In contrast, Ayurvedic management emphasizes restoring balance to Apana Vata and nourishing the reproductive tissues. Herbs such as Shatavari (Asparagus racemosus), Ashoka (Saraca indica), and Lodhra (Symplocos racemosa) are traditionally used to strengthen Artava and regulate cycles [7]. Rasayana therapy, yoga, pranayama, and diet modification are also recommended to restore balance and overall health.
Real-Life Example
For example, a 24-year-old woman working under chronic stress may suddenly stop menstruating. In modern medicine, this may be diagnosed as stress-induced hypothalamic amenorrhea. In Ayurveda, the condition would be explained as an imbalance of Apana Vata, aggravated by mental strain and irregular lifestyle. Treatment in such a case would involve stress reduction, a nourishing diet, and supportive Rasayana herbs to restore natural cycles.
2.Dysmenorrhea
Dysmenorrhea refers to painful periods.
- Primary dysmenorrhea is cramping pain that comes with menstruation but without an underlying disease. It is usually due to high levels of prostaglandins, which trigger uterine contractions [4].
- Secondary dysmenorrhea is pain caused by conditions like endometriosis, fibroids, or pelvic inflammatory disease [5].
Ayurveda sees painful periods as a result of Vata imbalance, especially in Apana Vata, which governs downward energy in the pelvic region [6].
Now let’s understand it more in detail
Dysmenorrhea
Dysmenorrhea refers to painful menstruation and is one of the most common gynecological problems among women of reproductive age. It is classified as primary or secondary, depending on whether it is associated with underlying disease.
Primary Dysmenorrhea
Primary dysmenorrhea is menstrual pain that occurs without any other medical condition. It typically begins during adolescence, usually within one to two years after menarche, and is strongly linked to the production of prostaglandins—hormone-like chemicals that cause uterine contractions [4]. These contractions reduce blood flow to the uterine lining, creating ischemia and resulting in cramping pain. Symptoms often include lower abdominal cramps, pain radiating to the back and thighs, nausea, fatigue, and sometimes headaches. The pain is most severe during the first one to two days of menstruation and may gradually decrease as women grow older or after childbirth.
Secondary Dysmenorrhea
Secondary dysmenorrhea is menstrual pain caused by an identifiable pelvic condition. Unlike primary dysmenorrhea, it often begins later in life and tends to worsen with time. Common causes include endometriosis, uterine fibroids, adenomyosis, pelvic inflammatory disease, and intrauterine devices (IUDs) [5]. Women with secondary dysmenorrhea usually experience longer-lasting pain, which may persist before, during, and after menstruation. The severity of symptoms depends on the underlying disorder, and additional symptoms like heavy bleeding, infertility, or pelvic tenderness may also be present.
Symptoms and Impact
Both types of dysmenorrhea cause significant discomfort, but secondary dysmenorrhea tends to be more disabling. Many women report missing school, work, or social activities due to pain. In some cases, the psychological impact, including anxiety and depression, can be as debilitating as the physical pain. Studies show that dysmenorrhea affects up to 50–90% of adolescents and young women worldwide, making it a leading cause of recurrent absenteeism [4].
Ayurvedic Perspective
In Ayurveda, dysmenorrhea is described as Kashtartava—a painful or difficult menstruation. It is primarily linked to aggravation of Vata dosha, particularly Apana Vata, which governs downward movement in the pelvic region [6]. When Apana Vata is imbalanced, it causes excessive uterine contractions, cramps, and obstruction of normal flow. If associated with Pitta aggravation, women may also experience burning sensations, irritability, or heavy bleeding. Kapha imbalance may cause associated heaviness, lethargy, and bloating. Ayurvedic texts emphasize that improper diet, irregular lifestyle, emotional stress, and suppression of natural urges can aggravate Vata, leading to painful cycles.
Treatment Approaches
Modern treatment often involves nonsteroidal anti-inflammatory drugs (NSAIDs) to block prostaglandin production, hormonal contraceptives to regulate cycles, and in severe cases, surgery for underlying causes such as fibroids or endometriosis. Complementary approaches include exercise, dietary changes, and heat therapy.
Ayurveda focuses on correcting Apana Vata imbalance and supporting reproductive health. Common formulations include Dashamoola Kwatha, Kumaryasava, Ashokarishta, and Hingvastaka Churna. Herbs like Shatavari (Asparagus racemosus) and Guduchi (Tinospora cordifolia) are used to reduce inflammation and restore balance. External therapies like abhyanga (oil massage) with warm medicated oils and basti (enema therapy) are also recommended in some cases.
Real-Life Example
A 19-year-old college student may experience severe cramps that force her to miss classes during every cycle. Modern diagnosis would identify this as primary dysmenorrhea due to prostaglandin-related uterine contractions. Ayurveda would describe it as Apana Vata disturbance, aggravated by stress, irregular meals, and late sleeping. Treatment could combine NSAIDs for short-term relief with Ayurvedic interventions such as a Vata-pacifying diet, herbal formulations, yoga, and pranayama for long-term balance.
3.Menorrhagia
Menorrhagia is unusually heavy or prolonged menstrual bleeding. Bleeding may last longer than seven days or involve large clots. Women often feel weak or develop anemia as a result. Fibroids, hormonal imbalance, clotting problems, and thyroid disorders are common causes [7].
Ayurveda connects heavy bleeding to Pitta aggravation in Rakta Dhatu (blood tissue), which produces excessive flow and burning sensations [8].
Detailed Explanation
Menorrhagia
Menorrhagia refers to abnormally heavy or prolonged menstrual bleeding. It is one of the most common menstrual disorders and significantly impacts a woman’s quality of life.
Definition and Clinical Features
Clinically, menorrhagia is defined as menstrual blood loss exceeding 80 milliliters per cycle or periods that last more than seven days [7]. Women may describe their bleeding as soaking through sanitary products every one to two hours, passing large clots, or needing double protection at night. Chronic menorrhagia can lead to anemia, fatigue, weakness, and reduced daily productivity.
Causes
Menorrhagia can arise from multiple underlying conditions. Structural causes include uterine fibroids, adenomyosis, endometrial polyps, and malignancies. Hormonal imbalances, such as those seen in thyroid disorders or anovulatory cycles, may also lead to excessive bleeding. Other contributors include clotting disorders, use of anticoagulant medications, pelvic infections, and intrauterine devices (IUDs) [7]. In adolescents, menorrhagia is often linked to immaturity of the hypothalamic–pituitary–ovarian axis, while in older women it may be associated with perimenopause or uterine pathology.
Symptoms and Complications
The hallmark symptom is excessive menstrual flow, but many women also experience pelvic pain, cramping, and passage of clots. If untreated, menorrhagia can cause iron-deficiency anemia, presenting with shortness of breath, dizziness, and chronic fatigue. Severe anemia may require hospitalization and blood transfusions [8]. Psychologically, the constant worry about bleeding and social embarrassment contributes to anxiety, low self-esteem, and reduced participation in normal activities.
Ayurvedic Perspective
In Ayurveda, menorrhagia is described as Asrigdara or Rakta Pradara—conditions of excessive uterine bleeding. The main pathology is attributed to Pitta dosha aggravation in Rakta Dhatu, leading to overheating, thinning, and excessive flow of blood [8]. Classical texts emphasize that excessive intake of hot, spicy, sour, or fermented foods, emotional stress, and exposure to heat can provoke Pitta and worsen bleeding. Additionally, weakness of uterine channels (Artavavaha Srotas) makes the tissue unable to hold blood properly, leading to continuous or heavy flow.
Treatment Approaches
Modern treatment depends on the severity and cause. Options include iron supplementation, antifibrinolytic agents (e.g., tranexamic acid), NSAIDs, and hormonal therapy with combined oral contraceptives or progesterone. In cases of fibroids or structural abnormalities, surgical treatments such as myomectomy, endometrial ablation, or hysterectomy may be considered [7].
Ayurveda, in contrast, emphasizes restoring balance to Pitta and strengthening Rakta Dhatu. Herbs such as Ashoka (Saraca indica), Lodhra (Symplocos racemosa), Shatavari (Asparagus racemosus), and Nagakesara (Mesua ferrea) are traditionally used to control heavy bleeding. Classical formulations like Ashokarishta, Lodhrasava, and Chandraprabha Vati are prescribed to stabilize the uterine lining and restore normal flow. Cooling measures such as intake of ghee, milk, and pitta-pacifying diets are also recommended, along with stress management and yoga for long-term regulation.
Real-Life Example
A 38-year-old woman may report soaking through pads every two hours and feeling exhausted from blood loss. Investigations may reveal uterine fibroids as the cause. A gynecologist may recommend hormonal therapy or surgery, while an Ayurvedic physician may diagnose Pitta-aggravated Asrigdara and advise Ashokarishta, Lodhra Churna, and dietary modifications to calm Pitta and strengthen the uterine channels. An integrative approach combining both methods can help manage symptoms while addressing the root imbalance.
4.Oligomenorrhea
Oligomenorrhea means infrequent periods, with cycles longer than 35 days. This often happens in PCOS, thyroid problems, or with extreme dieting and stress [9].
According to Ayurveda, oligomenorrhea is caused by Kapha-induced blockage and weak nourishment of Rasa and Rakta Dhatus [10].
Oligomenorrhea- Detailed Explanation
Oligomenorrhea refers to infrequent menstrual cycles, where the interval between periods is longer than 35 days. It is a common manifestation of hormonal imbalance and often indicates underlying reproductive or systemic disorders.
Definition and Clinical Features
Clinically, oligomenorrhea is defined as menstrual cycles that occur fewer than nine times a year, typically with gaps longer than 35 days [9]. Women may notice very delayed or unpredictable periods, sometimes accompanied by scanty bleeding. While occasional irregularity can be normal during adolescence or perimenopause, persistent oligomenorrhea requires medical evaluation.
Causes
The most common cause of oligomenorrhea is polycystic ovary syndrome (PCOS), where high levels of androgens disrupt regular ovulation. Other causes include thyroid dysfunction, hyperprolactinemia, uncontrolled diabetes, chronic stress, extreme weight loss, eating disorders, and excessive exercise [9]. Certain medications, particularly antipsychotics and chemotherapy agents, can also disturb menstrual cycles. During adolescence, cycles may remain irregular until the hypothalamic–pituitary–ovarian axis matures, while in perimenopausal women, irregular ovulation naturally contributes to oligomenorrhea.
Symptoms and Complications
The primary symptom is infrequent menstruation, but women may also experience infertility, weight fluctuations, acne, excessive hair growth (hirsutism), and mood disturbances, especially in PCOS-related cases. If cycles remain persistently irregular, there is a risk of endometrial hyperplasia and, in rare cases, progression to endometrial cancer due to unopposed estrogen exposure [10]. Emotional stress, anxiety, and social concerns about delayed periods further impact quality of life.
Ayurvedic Perspective
In Ayurveda, oligomenorrhea can be compared to Alpartava (scanty menstruation) or delayed Artava Pravritti (initiation of flow). The pathology is primarily linked to Kapha dosha aggravation, which causes obstruction of channels (Srotorodha), preventing normal and timely flow [10]. Deficiency in Rasa Dhatu (nutritive fluid) and Rakta Dhatu (blood tissue) also leads to insufficient nourishment of reproductive tissues, resulting in weak or delayed Artava (menstrual blood). Vata imbalance, particularly Apana Vata, may further complicate the cycle by causing irregular or painful flow. Ayurveda emphasizes that poor digestion (Agnimandya), excessive intake of heavy or oily foods, sedentary habits, and unresolved stress are key triggers of oligomenorrhea.
Treatment Approaches
Modern management of oligomenorrhea depends on the cause. In PCOS, lifestyle interventions such as weight loss, dietary regulation, and exercise are first-line treatments. Hormonal therapies, including oral contraceptives or progesterone, may help regulate cycles. In thyroid or prolactin disorders, specific medical correction is required.
Ayurvedic treatment focuses on clearing Kapha obstruction, improving Agni (digestive fire), and restoring balance to Vata. Herbs like Shatavari (Asparagus racemosus), Guduchi (Tinospora cordifolia), Trikatu (combination of ginger, black pepper, and long pepper), and Lodhra (Symplocos racemosa) are commonly prescribed to regulate cycles and strengthen reproductive tissues. Formulations such as Kumaryasava, Ashokarishta, and Rajah Pravartini Vati are also used to promote timely menstruation. Lifestyle changes including regular yoga, pranayama, and stress management form an important part of holistic care.
Real-Life Example
A 22-year-old woman with PCOS may experience only four periods in a year, along with acne and weight gain. Her gynecologist might prescribe oral contraceptives to regulate bleeding and insulin-sensitizing drugs to address hormonal imbalance. An Ayurvedic physician would view her condition as Kapha-dominant Srotorodha and recommend dietary changes, weight management, Kapha-reducing herbs, and Rasayana therapy to restore hormonal balance and improve cycle regularity.
5.Polymenorrhea
Polymenorrhea refers to very frequent cycles, where bleeding comes every 21 days or less. Causes include hormonal imbalance, stress, or uterine infections [11].
Ayurveda attributes this to Vata–Pitta imbalance, where Apana Vata forces early shedding of the uterine lining [12].
Polymenorrhea- More in Detail
Polymenorrhea refers to menstrual cycles that occur too frequently, usually with intervals of less than 21 days between periods. Although bleeding itself may be normal in volume, the shortened cycle causes significant physical and emotional strain.
Definition and Clinical Features
Clinically, polymenorrhea is defined as the recurrence of menstrual bleeding at intervals shorter than 21 days [11]. Women may feel that their next period begins before they have recovered from the previous one. The bleeding is often regular in pattern but abnormally frequent, leading to fatigue, weakness, and social discomfort.
Causes
Polymenorrhea is most commonly caused by hormonal imbalances, particularly those involving the luteal phase, where progesterone levels are inadequate to sustain a normal cycle length. Other causes include pelvic infections, thyroid dysfunction, endometrial hyperplasia, use of intrauterine devices (IUDs), and perimenopausal changes [11]. Chronic stress, undernutrition, and certain medications may also shorten cycles. In adolescents, immature hormonal regulation may cause frequent bleeding, while in older women, declining ovarian function is often responsible.
Symptoms and Complications
The main symptom is frequent menstrual cycles, often associated with weakness and irritability. Over time, polymenorrhea can lead to iron-deficiency anemia due to repeated blood loss. Women may also experience reduced fertility, as frequent cycles sometimes indicate disrupted ovulation. Psychologically, the unpredictability and strain of frequent menstruation can cause anxiety and reduce quality of life.
Ayurvedic Perspective
In Ayurveda, polymenorrhea is understood as Ati-Pravritti of Artava, meaning excessive or premature onset of menstruation. It is mainly linked to Vata–Pitta imbalance. An aggravated Apana Vata (downward-moving energy) pushes out Rakta Dhatu prematurely, while heightened Pitta increases bleeding tendency [12]. This combination causes cycles to come earlier than expected. Poor dietary habits, excessive heat, spicy foods, anger, stress, and lack of rest are noted triggers. Classical Ayurvedic texts also describe this condition under Asrigdara, highlighting repeated or untimely bleeding caused by doshic imbalance.
Treatment Approaches
Modern treatment focuses on correcting the underlying hormonal imbalance. Progesterone therapy may help lengthen cycles, while management of thyroid or infectious causes is essential. In perimenopausal women, hormone replacement therapy may be considered.
Ayurvedic management emphasizes pacifying both Vata and Pitta while strengthening Rakta Dhatu. Herbs like Ashoka (Saraca indica), Shatavari (Asparagus racemosus), Lodhra (Symplocos racemosa), and Nagakesara (Mesua ferrea) are commonly prescribed. Classical formulations include Ashokarishta, Lodhrasava, and Raktapitta-hara preparations to balance bleeding and restore cycle rhythm. Lifestyle adjustments such as a cooling, Pitta-pacifying diet, avoidance of late nights, and stress reduction through yoga and meditation are also recommended.
Real-Life Example
A 34-year-old woman may complain of periods every 18 days, leaving her exhausted and pale. Modern evaluation may reveal luteal phase deficiency, while Ayurveda would classify her condition as Vata–Pitta aggravated Asrigdara. She may be treated with hormonal therapy in conventional medicine, while an Ayurvedic approach would include Ashokarishta, Shatavari Kalpa, and Pitta-pacifying dietary changes to regulate her cycle.
6.Metrorrhagia
Metrorrhagia means irregular bleeding between periods. It may be caused by polyps, endometrial overgrowth, infections, or—rarely—cancers [13].
In Ayurveda, this irregular bleeding is linked to Rakta Dushti (impure blood) and weakness in Artavavaha Srotas (reproductive channels) [14].
Metrorrhagia-Explained in detailed
Metrorrhagia refers to bleeding that occurs at irregular times, outside the normal menstrual cycle. Unlike menorrhagia, which involves heavy but predictable periods, metrorrhagia is characterized by unexpected or intermenstrual bleeding that can range from spotting to heavier flow.
Definition and Clinical Features
Clinically, metrorrhagia is defined as uterine bleeding that occurs between regular menstrual periods [13]. Women may notice light spotting a few days after menstruation, prolonged low-level bleeding, or unpredictable heavy episodes. The irregularity often causes confusion and anxiety, since bleeding does not follow the expected cycle pattern.
Causes
Metrorrhagia can result from a wide range of causes. Structural abnormalities such as uterine polyps, fibroids, or endometrial hyperplasia are common culprits. Hormonal imbalances, particularly anovulatory cycles, are also frequent contributors. Other causes include pelvic infections, contraceptive use (IUDs, hormonal therapy), thyroid dysfunction, blood clotting disorders, and, in rare cases, endometrial or cervical cancers [13]. In adolescents, irregular bleeding is often due to immature hormonal control, while in older women it may reflect premenopausal changes.
Symptoms and Complications
The main feature of metrorrhagia is irregular bleeding outside the expected cycle. Some women may experience only mild spotting, while others have unpredictable heavy bleeding. Over time, persistent bleeding may cause anemia, weakness, and fatigue, similar to other menstrual disorders. Because metrorrhagia can sometimes indicate precancerous or cancerous conditions, it requires thorough medical evaluation. Psychologically, the unpredictability can cause significant stress, embarrassment, and disruption to daily activities.
Ayurvedic Perspective
In Ayurveda, metrorrhagia corresponds to Rakta Pradara or excessive/intermittent uterine bleeding. The pathology is primarily linked to Pitta aggravation in Rakta Dhatu (blood tissue), which leads to overheating and increased flow [14]. Weakness of the uterine channels (Artavavaha Srotas) also contributes to irregular bleeding. In some cases, Vata involvement may cause unpredictable timing, while Kapha aggravation may result in thick, mucus-like discharge alongside bleeding. Classical Ayurvedic texts emphasize dietary and lifestyle factors such as intake of spicy and sour foods, exposure to heat, stress, and suppression of natural urges as major triggers for Rakta Pradara.
Treatment Approaches
Modern management of metrorrhagia depends on identifying the cause. If related to fibroids or polyps, surgical removal may be required. Hormonal therapy can regulate cycles in women with anovulatory bleeding. In cases of infection, antibiotics are prescribed, while in older women, evaluation for malignancy is essential.
Ayurveda focuses on reducing Pitta aggravation and strengthening Rakta Dhatu. Herbs such as Ashoka (Saraca indica), Lodhra (Symplocos racemosa), Nagakesara (Mesua ferrea), and Amalaki (Emblica officinalis) are widely used. Classical formulations like Ashokarishta, Lodhrasava, and Pravala Pishti are prescribed to control bleeding and restore normal cycle rhythm. Lifestyle measures include cooling diets, avoidance of excessive physical strain, and stress-reducing practices like meditation and pranayama.
Real-Life Example
A 40-year-old woman may present with unpredictable spotting between her periods and occasional heavy bleeding. Modern investigations may reveal an endometrial polyp, requiring removal. From an Ayurvedic perspective, her condition would be considered Pitta-aggravated Rakta Pradara, managed with Ashokarishta, Lodhra Churna, and a Pitta-pacifying lifestyle. Combining surgical correction with Ayurvedic Rasayanas helps improve both physical recovery and long-term balance.
7. Premenstrual Syndrome (PMS) and PMDD
- PMS includes mood swings, bloating, fatigue, and breast tenderness before the period starts. These symptoms usually improve with menstruation [15].
- PMDD is a severe form of PMS, where symptoms like depression, anxiety, and irritability interfere with daily life [16].
Ayurveda explains PMS and PMDD as a combined Dosha imbalance: Vata contributes to anxiety, Pitta leads to irritability, and Kapha causes bloating and heaviness [17].
Premenstrual Syndrome (PMS) and Premenstrual Dysphoric Disorder (PMDD)
Premenstrual disorders represent a group of physical, emotional, and behavioral symptoms that occur during the luteal phase of the menstrual cycle and resolve once menstruation begins. While PMS is common and usually mild to moderate, PMDD is a severe form that can significantly impair quality of life.
PMS: Definition and Clinical Features
Premenstrual Syndrome (PMS) refers to a cluster of symptoms that appear 7–14 days before menstruation and disappear within a few days after bleeding starts. Common physical symptoms include bloating, breast tenderness, headaches, abdominal cramps, and fatigue. Emotional and behavioral symptoms include irritability, mood swings, anxiety, food cravings, and sleep disturbances [15]. PMS affects up to 75% of women of reproductive age to some degree, although only about 20–30% report symptoms severe enough to affect daily functioning.
PMDD: Definition and Severity
Premenstrual Dysphoric Disorder (PMDD) is a more severe form of PMS, affecting about 3–8% of women [16]. In PMDD, mood-related symptoms such as depression, intense irritability, anger, hopelessness, and social withdrawal dominate and can disrupt work, relationships, and overall mental well-being. Unlike PMS, PMDD is considered a psychiatric disorder in modern medicine and is classified under mood disorders in the DSM-5.
Causes and Pathophysiology
The exact cause of PMS and PMDD is not fully understood, but they are believed to result from abnormal sensitivity to normal hormonal changes, particularly fluctuations in estrogen and progesterone. These changes affect neurotransmitters like serotonin, leading to mood instability [16]. Other contributing factors include genetics, lifestyle, stress, and nutritional deficiencies such as low magnesium, calcium, and vitamin B6.
Ayurvedic Perspective
In Ayurveda, PMS and PMDD are not described as distinct conditions but are understood through the framework of Dosha imbalance. Symptoms vary depending on which Dosha is aggravated:
- Vata imbalance causes anxiety, insomnia, mood swings, and nervous tension.
- Pitta imbalance leads to irritability, anger, hot flashes, and headaches.
- Kapha imbalance results in bloating, lethargy, food cravings, and depression [17].
Classical texts also describe the influence of Apana Vata in regulating the menstrual cycle. When Apana is disturbed, emotional and physical symptoms appear before menstruation. Ayurveda emphasizes that poor diet, lack of rest, suppression of natural urges, and chronic stress can all provoke Dosha imbalance, making symptoms more intense.
Treatment Approaches
Modern treatment for PMS and PMDD depends on severity. For mild to moderate PMS, lifestyle interventions such as exercise, yoga, dietary regulation, and stress management are recommended. Nutritional supplementation with calcium, vitamin B6, or magnesium may provide relief. For PMDD, selective serotonin reuptake inhibitors (SSRIs) are the most effective treatment, alongside hormonal therapy in some cases [15].
Ayurvedic management focuses on pacifying aggravated Doshas and stabilizing Apana Vata. Herbs like Shatavari (Asparagus racemosus), Ashwagandha (Withania somnifera), Brahmi (Bacopa monnieri), and Guduchi (Tinospora cordifolia) are used to balance mood, reduce anxiety, and support reproductive health. Formulations such as Ashokarishta and Kumaryasava are also commonly prescribed. Yoga, pranayama, and meditation play an important role in calming the mind and reducing hormonal sensitivity.
Real-Life Example
A 29-year-old woman may experience irritability, breast tenderness, and bloating before every period, consistent with PMS. Lifestyle changes such as yoga and dietary correction may help her significantly. In contrast, another woman may report severe depression and anger before menstruation that interfere with work and relationships. This would be diagnosed as PMDD, requiring SSRIs in modern practice. An Ayurvedic physician might interpret her case as a combination of Vata–Pitta imbalance and recommend Shatavari, Ashwagandha, and stress-relieving therapies to restore harmony.
Symptoms and Clinical Features
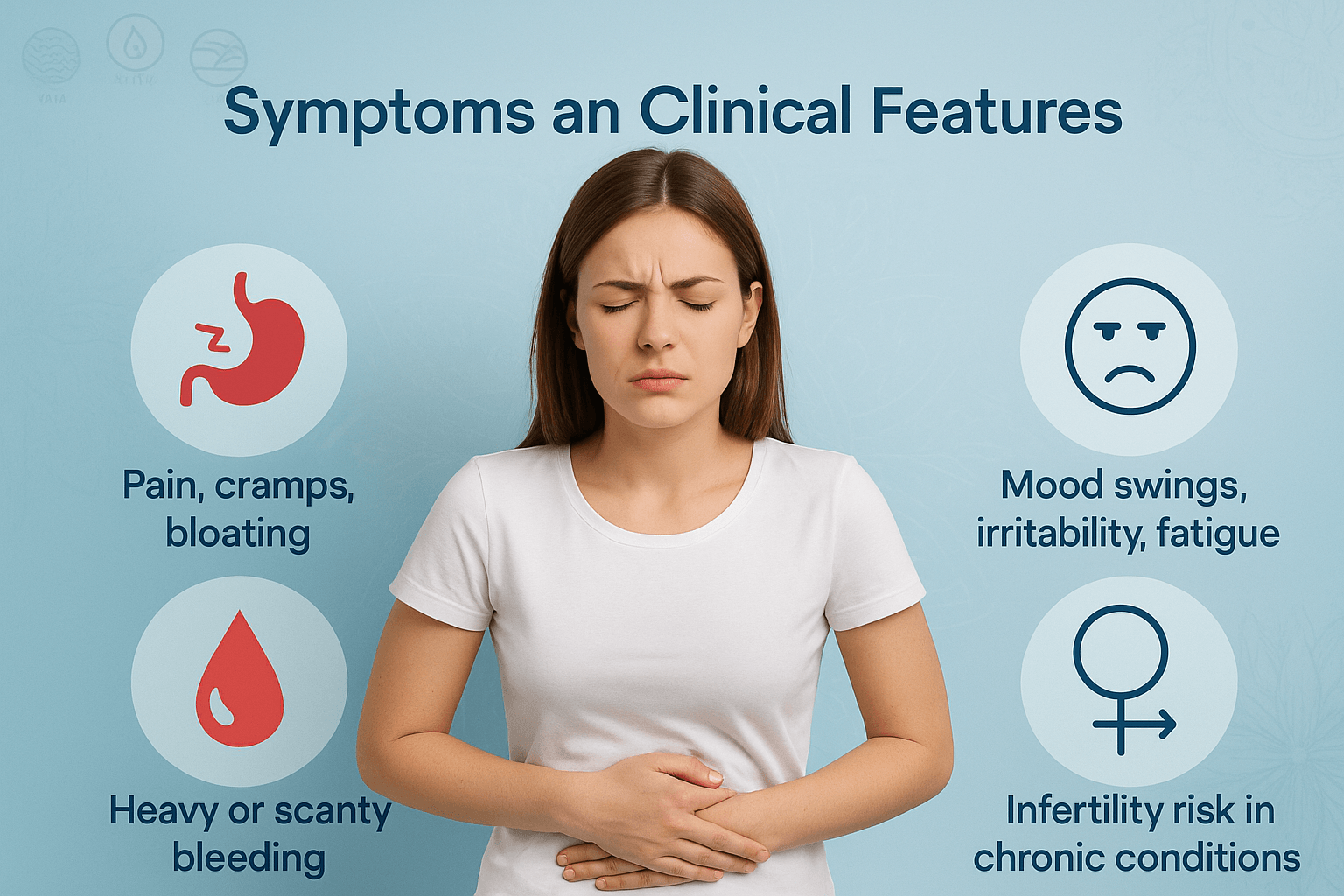
Pain, cramps, and bloating
One of the most common symptoms of menstrual disorders is abdominal pain. Many women experience cramping in the lower abdomen or back, caused by the uterus contracting to shed its lining. In some, the pain can be severe, radiating to the thighs and lower back, often accompanied by bloating or heaviness. Ayurveda explains this as a sign of Vata imbalance, especially Apana Vata, which governs downward movements in the body [1].
Heavy or scanty bleeding
Changes in the amount of bleeding are key indicators of menstrual disorders. Heavy bleeding (menorrhagia) can lead to weakness, dizziness, and anemia over time. Very scanty periods (hypomenorrhea) may indicate hormonal imbalance, poor nourishment, or blocked reproductive channels. Ayurveda links heavy bleeding to Pitta aggravation in Rakta Dhatu, while scanty flow is often associated with depleted Rasa Dhatu or obstruction by Kapha [2].
Mood swings, irritability, and fatigue
Emotional changes such as irritability, mood swings, anxiety, and fatigue are common in the days before and during menstruation. This cluster of symptoms is often grouped under premenstrual syndrome (PMS). In more severe cases (PMDD), symptoms may interfere with daily life. Ayurveda describes these as disturbances of Manovaha Srotas (mind channels) due to Dosha imbalance—Vata causing restlessness, Pitta causing anger, and Kapha causing lethargy [3].
Infertility risk in chronic conditions
Long-standing menstrual irregularities—such as missed periods, very infrequent cycles, or uncontrolled heavy bleeding—can interfere with ovulation and the ability to conceive. Conditions like PCOS, endometriosis, or chronic amenorrhea may increase infertility risk. Ayurveda emphasizes that disturbed Artava (reproductive essence) and weakened Ojas (vital energy) over time reduce natural fertility and overall reproductive health [4].
Diagnostic Approaches
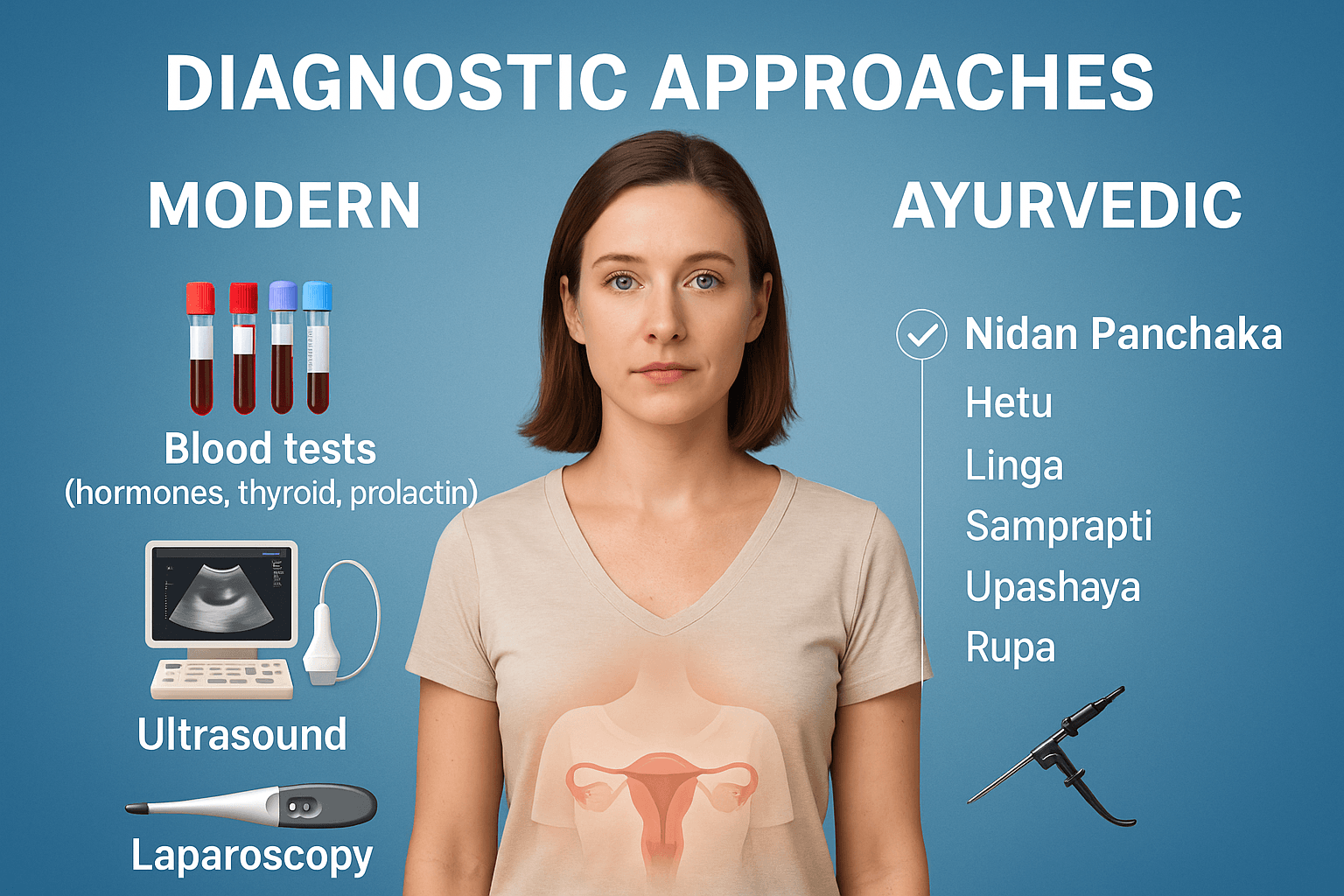
Modern medicine
Diagnosis of menstrual disorders begins with a detailed medical history and physical examination. Doctors ask about the age of first menstruation, cycle length, bleeding patterns, pain levels, lifestyle, and family history. Investigations then include:
- Blood tests: Hormone levels are checked to look for imbalances. This may include thyroid hormones (TSH, T3, T4), prolactin (linked to milk secretion and cycle irregularities), estrogen, progesterone, androgens, and FSH/LH levels. These tests help identify conditions like PCOS, thyroid dysfunction, or early ovarian failure [1].
- Ultrasound: Pelvic ultrasound gives a clear picture of the uterus and ovaries, showing fibroids, cysts, polyps, or structural abnormalities that may disturb menstruation [2].
- Laparoscopy: In some cases, doctors recommend a minor surgical procedure where a thin camera is inserted into the abdomen. This helps detect endometriosis, adhesions, or pelvic inflammatory disease that cannot always be diagnosed through imaging alone [3].
Modern diagnostics focus on structural and hormonal causes, providing a precise medical picture that can guide treatment.
Ayurvedic perspective
Ayurveda follows a structured diagnostic method called Nidan Panchaka, the five-fold framework for understanding disease:
- Hetu (causes): Identifying lifestyle, diet, stress, and environmental factors that may disturb the Doshas. For example, irregular eating, excessive cold food, or emotional strain may trigger Vata imbalance leading to irregular cycles [4].
- Linga (symptoms): Observing the patient’s symptoms—such as pain, heaviness, scanty flow, or mood swings—and connecting them to Dosha involvement.
- Samprapti (pathogenesis): Understanding how the disease has developed step by step inside the body, from initial Dosha imbalance to Dhatu (tissue) and Srotas (channel) involvement. For instance, aggravated Pitta in Rakta Dhatu leads to heavy bleeding, while Kapha in Artavavaha Srotas delays cycles.
- Upashaya (relieving factors): Assessing what brings relief or worsening. For example, warmth easing cramps suggests Vata dominance, while cooling herbs helping heavy bleeding points to Pitta aggravation.
- Rupa (signs and manifestations): The outward clinical picture observed during examination, such as pallor from anemia, acne from PCOS, or edema from Kapha imbalance.
This holistic approach looks beyond symptoms, seeking the root imbalance that disturbs the natural menstrual rhythm.
Integration of modern and Ayurvedic methods
By combining advanced medical tests with Ayurvedic diagnostic wisdom, practitioners can achieve both precision and depth. Blood tests and imaging pinpoint the structural and biochemical changes, while Nidan Panchaka uncovers the energetic and lifestyle roots. Together, they provide a complete map of menstrual health, enabling not just symptom management but true long-term healing.
Complications if Untreated
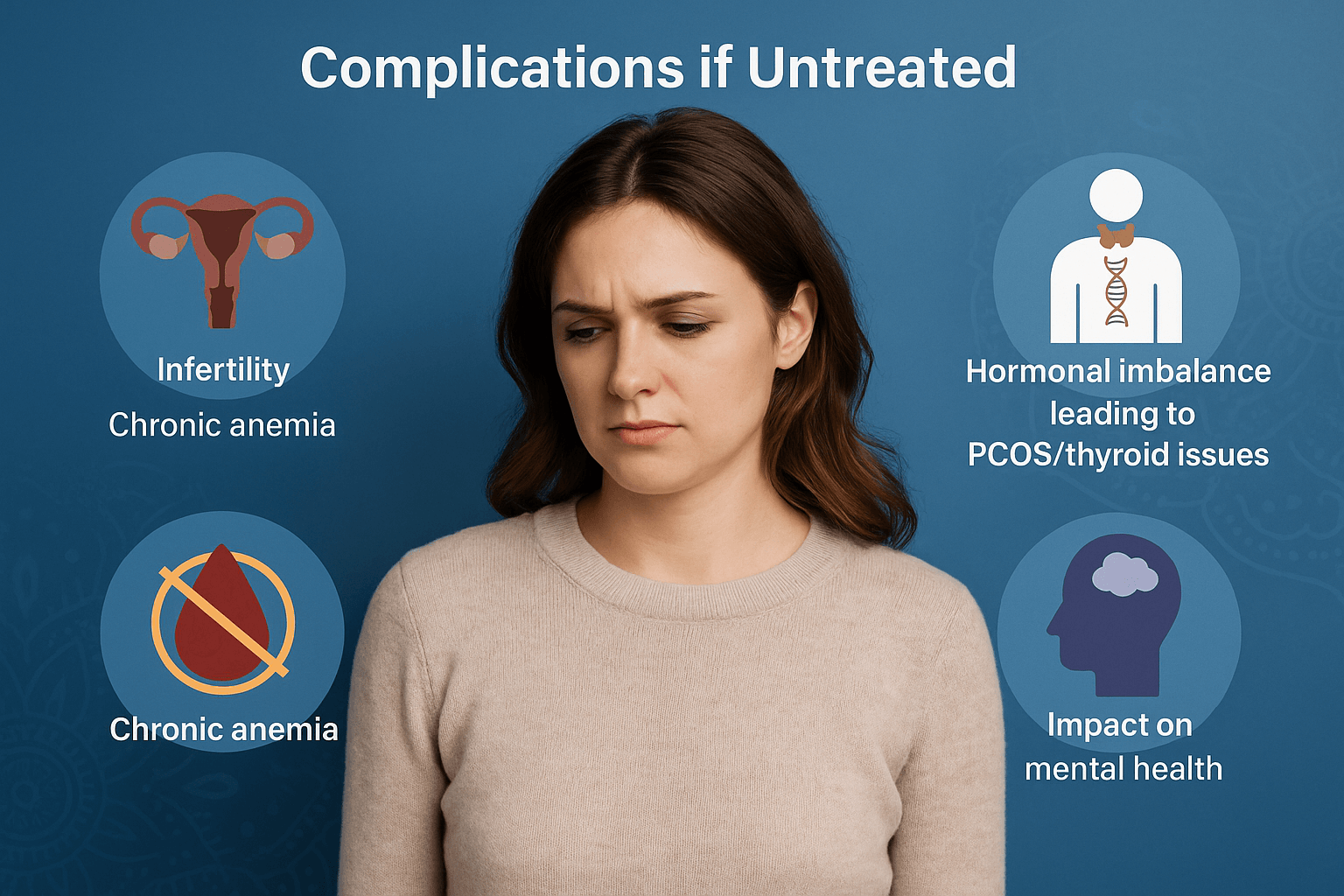
Infertility
When menstrual disorders are left untreated, one of the most serious long-term risks is difficulty conceiving. Irregular or absent ovulation, blocked reproductive channels, and damaged endometrial health can all make it harder to achieve pregnancy. Conditions such as PCOS, endometriosis, or chronic amenorrhea are common causes of infertility [1]. Ayurveda explains this as weakness or obstruction of Artava Dhatu (reproductive tissue) and depletion of Ojas (vital energy), both of which are essential for conception.
Chronic anemia
Heavy or prolonged menstrual bleeding (menorrhagia) can lead to iron-deficiency anemia. This means the blood cannot carry enough oxygen, causing constant fatigue, dizziness, pale skin, and weakness. Over time, untreated anemia may strain the heart and reduce overall immunity [2]. In Ayurveda, this is recognized as Pandu Roga, where loss of Rakta Dhatu (blood) weakens the whole system.
Hormonal imbalance leading to PCOS/thyroid issues
Persistent irregular cycles often signal underlying hormonal disturbances. If not corrected, these imbalances may progress to polycystic ovary syndrome (PCOS), thyroid dysfunction, or early ovarian failure [3]. Such conditions further disturb the menstrual cycle and can affect metabolism, weight, and fertility. Ayurveda describes this as Kapha–Vata involvement in Artavavaha Srotas, leading to stagnation, cyst formation, and metabolic disruption.
Impact on mental health
Menstrual disorders are not just physical. Ongoing pain, irregular cycles, and emotional swings can significantly affect mental well-being. Women often report depression, anxiety, irritability, and poor self-esteem when these problems remain untreated [4]. Ayurveda links this to disturbed Manovaha Srotas (channels of the mind) and Vata imbalance, which causes instability in both mood and energy.
Untreated menstrual disorders therefore carry risks beyond monthly discomfort—they can affect fertility, blood health, hormonal balance, and emotional stability. Early diagnosis and integrated care (modern + Ayurvedic) help prevent these complications and restore long-term reproductive and overall health.
Frequently Asked Questions
1. What are menstrual disorders?
Menstrual disorders are conditions that disturb the normal timing, flow, or symptoms of the menstrual cycle. They include irregular, absent, painful, or heavy periods, and may also involve mood changes or infertility [1].
2. What causes menstrual disorders?
They may be caused by hormonal imbalances (thyroid, PCOS, prolactin), structural issues (fibroids, polyps), lifestyle factors (stress, weight changes, excessive exercise), or chronic illnesses. Ayurveda adds that diet, emotional stress, and Dosha imbalance (Vata, Pitta, Kapha) also play a role [2].
3. When should I see a doctor?
Seek medical attention if your periods are extremely painful, last longer than 7 days, are very heavy or very light, come too often or not at all, or if you notice bleeding between cycles. These symptoms may point to conditions needing treatment [3].
4. Can menstrual disorders affect fertility?
Yes. Disorders such as PCOS, endometriosis, or chronic amenorrhea can prevent ovulation or damage the uterine lining, making it harder to conceive. In Ayurveda, long-standing disturbances of Artava Dhatu (reproductive essence) reduce fertility potential [4].
5. What tests are done for diagnosis?
Doctors may order blood tests for hormones, thyroid, and prolactin, along with ultrasounds or laparoscopy to look at the uterus and ovaries. Ayurveda uses Nidan Panchaka (Hetu, Linga, Samprapti, Upashaya, Rupa) to trace the root imbalance [5].
6. How are menstrual disorders treated in modern medicine?
Treatment may include NSAIDs for pain, hormonal therapy (like oral contraceptives, progesterone, or GnRH analogs), and surgery in severe cases such as fibroid removal, endometrial ablation, or hysterectomy [6].
7. How does Ayurveda manage menstrual disorders?
Ayurveda uses personalized therapies: balancing herbs (Ashoka, Shatavari, Lodhra), Rasayanas for tissue rejuvenation, optional Shodhana (detox therapies like Virechana, Basti), and diet-lifestyle adjustments. The focus is on correcting root imbalances in Doshas, Dhatus, and Srotas [7].
8. Can stress really affect my periods?
Yes. Stress alters the hypothalamic–pituitary–ovarian (HPO) axis, disturbing ovulation and hormone balance. Ayurveda also links excessive worry and emotional strain to Vata aggravation, leading to delayed or missed periods [8].
9. What happens if menstrual disorders are left untreated?
They may lead to infertility, chronic anemia, progression to PCOS or thyroid disease, and mental health problems such as depression or anxiety. Long-term untreated issues can severely affect quality of life [9].
10. Are menstrual disorders curable?
Many menstrual disorders can be managed or cured depending on the cause. For example, correcting thyroid function or PCOS with proper care often restores normal cycles. Ayurveda emphasizes complete restoration of balance, aiming not only to manage symptoms but to prevent recurrence [10].
References
1. Klein, J. R., & Poth, M. A. (2019). Amenorrhea: A systematic approach to diagnosis and management. American Family Physician, 100(1), 39–48. https://www.aafp.org/pubs/afp/issues/2019/0701/p39.html
2. Naz, T., Rizvi, S., & Ahmad, A. (2021). Etiological spectrum of secondary amenorrhea. Cureus, 13(9), e17906. https://doi.org/10.7759/cureus.17906
3. Charaka. Charaka Samhita, Chikitsa Sthana, Chapter 30 (Artava Dushti Chikitsa). Varanasi: Chaukhambha Orientalia; 2014.
4. Dawood, M. Y. (2006). Primary dysmenorrhea: Advances in pathogenesis and management. Obstetrics & Gynecology, 108(2), 428–441. https://doi.org/10.1097/01.AOG.0000223314.26638.0c
5. Osayande, A. S., & Mehulic, S. (2014). Diagnosis and initial management of dysmenorrhea. American Family Physician, 89(5), 341–346. https://www.aafp.org/pubs/afp/issues/2014/0301/p341.html
6. Sushruta. Sushruta Samhita, Sharira Sthana, Chapter 2 (Artava Vijnaneeya Adhyaya). Varanasi: Chaukhambha Sanskrit Series; 2015.
7. Munro, M. G., Critchley, H. O. D., Fraser, I. S., & FIGO Working Group. (2018). The FIGO classification system (PALM–COEIN) for causes of abnormal uterine bleeding. International Journal of Gynecology & Obstetrics, 143(3), 393–408. https://doi.org/10.1002/ijgo.12666
8. Sharma, P. V. Bhavaprakasha Nighantu, Chapter: Striroga Adhikara. Varanasi: Chaukhambha Bharati Academy; 2010.
9. Practice Committee of the American Society for Reproductive Medicine. (2022). Evaluation and treatment of oligomenorrhea and amenorrhea. Fertility and Sterility, 118(5), 923–934. https://doi.org/10.1016/j.fertnstert.2022.09.001
10. Singh, R. H. (2017). Foundations of Ayurveda: Menstrual disorders in classical texts. New Delhi: Chaukhambha Publications.
11. Berek, J. S. (2020). Berek & Novak’s Gynecology (16th ed.). Philadelphia: Wolters Kluwer.
12. National Institute for Health and Care Excellence (NICE). (2018). Heavy menstrual bleeding: Assessment and management (NG88). Retrieved from https://www.nice.org.uk/guidance/ng88
13. Johns Hopkins Medicine. (2021). Metrorrhagia. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/metrorrhagia
14. Vagbhata. Ashtanga Hridaya, Sharira Sthana, Chapter 1 (Artava Prashna). Varanasi: Chaukhambha Krishnadas Academy; 2016.
15. Hofmeister, S., & Bodden, S. (2016). Premenstrual syndrome and premenstrual dysphoric disorder. American Family Physician, 94(3), 236–240. https://www.aafp.org/pubs/afp/issues/2016/0801/p236.html
16. Yonkers, K. A., O’Brien, P. M. S., & Eriksson, E. (2008). Premenstrual syndrome. Lancet, 371(9619), 1200–1210. https://doi.org/10.1016/S0140-6736(08)60527-9
17. Tripathi, R. D. Ayurvedic Gynecology: A Commentary on Stri Roga. Varanasi: Chaukhambha Orientalia; 2012.











One Response
Good