- Modern Understanding of Male Infertility
- Diagnostic Tools Used in Modern Medicine
- Ayurvedic View of Male Infertility
- Ayurvedic Classification of Conditions
- Ayurveda Cure- Male Infertility
- Dietary and lifestyle corrections
- Case studies and clinical outcomes
- Frequently Asked Questions (FAQs)
- Complete References
Male infertility has become a rising concern worldwide, affecting approximately 1 in 7 couples trying to conceive. Surprisingly, in nearly 40–50% of infertility cases, the issue lies wholly or partly with the male partner [1]. Despite advancements in assisted reproductive technologies, many men continue to suffer in silence due to stigma, misdiagnosis, or lack of personalized treatment options. Modern medicine often focuses on laboratory values such as sperm count and motility, offering limited pharmacological interventions or pushing patients toward IVF/ICSI without addressing the underlying pathology ([2]).
From an Ayurvedic perspective, infertility is not a standalone disorder—it reflects a deeper disturbance in the body’s internal harmony. The classical texts describe a man’s fertility as dependent on the health of Shukra Dhatu, the reproductive tissue, which is nourished by all preceding Dhatus and influenced by lifestyle, digestion (Agni), and emotional wellbeing ([3]). Therefore, when treatment is focused only on improving semen parameters without healing the Dhatu chain or correcting vitiated Doshas, outcomes often remain temporary or suboptimal.
What sets Ayurveda apart is its emphasis on root-cause treatment—not just boosting sperm numbers but revitalizing the entire reproductive axis, including hormonal balance, cellular regeneration, and psychological strength. The ancient sages believed that true virility (Vajikaran) arises from internal purity, cellular nourishment, and mental clarity—an idea now supported by emerging research on the gut-testis axis, oxidative stress, and mind-body impact on male fertility ([4], [5]).
This article explores male infertility in depth—from its modern diagnostic parameters to classical Ayurvedic understanding—and outlines how time-tested Rasayana therapies, Bhasmas, and personalized formulations can offer real healing. Whether you’re facing low sperm count, erectile dysfunction, or unexplained infertility, this integrative guide will help you understand the cause and cure beyond symptomatic control.
Modern Understanding of Male Infertility
Male infertility is no longer a silent issue—it is a well-recognized medical condition with clearly defined parameters. According to the World Health Organization (WHO), infertility is the failure to achieve pregnancy after 12 months or more of regular, unprotected intercourse. Male factors alone account for roughly 40% to 50% of all infertility cases globally, making it just as significant as female reproductive disorders in the path to conception ([6]).
At the core of male fertility lies the ability to produce healthy, motile sperm in adequate quantities and deliver them effectively during intercourse. Any disruption in this process—from testicular sperm production to ejaculation—can contribute to infertility. The most common presentations include oligospermia (low sperm count), asthenospermia (poor motility), teratospermia (abnormal morphology), and azoospermia (complete absence of sperm) ([7]).
Several biological, environmental, and lifestyle factors contribute to these abnormalities. Varicocele, a dilation of the scrotal veins, is one of the leading reversible causes of infertility. It impairs thermoregulation in the testes, leading to oxidative stress and DNA damage in sperm ([8]). Hormonal disturbances, such as low testosterone or elevated FSH and LH, indicate a disruption in the hypothalamic-pituitary-gonadal (HPG) axis, essential for normal spermatogenesis ([9]). Chronic diseases like diabetes, obesity, thyroid dysfunction, and metabolic syndrome further reduce sperm quality by inducing inflammation, hormonal imbalances, and mitochondrial dysfunction ([10]).
Additionally, environmental toxins, radiation exposure, certain medications (e.g., chemotherapy, anabolic steroids), alcohol consumption, and smoking are known to decrease both sperm count and function. Prolonged heat exposure from hot tubs, saunas, or tight clothing can also impair sperm production by affecting scrotal temperature regulation ([11]).
Despite the wide availability of treatments, most modern approaches focus on symptom-based management, such as hormone replacement therapy, surgical correction for varicocele, or directly opting for IVF or ICSI. However, these do not address cellular regeneration or underlying systemic dysfunction. Many men are offered antidepressants or PDE-5 inhibitors like sildenafil (Viagra) in cases of erectile dysfunction, which may not improve reproductive outcomes in the long term ([12]).
This is where Ayurveda offers a crucial advantage: it examines these dysfunctions not as isolated organ failures but as the breakdown of the body’s internal homeostasis. Before moving into the Ayurvedic interpretation, it’s essential to understand how these modern parameters are diagnosed and measured, which will be covered in the next section.
Diagnostic Tools Used in Modern Medicine
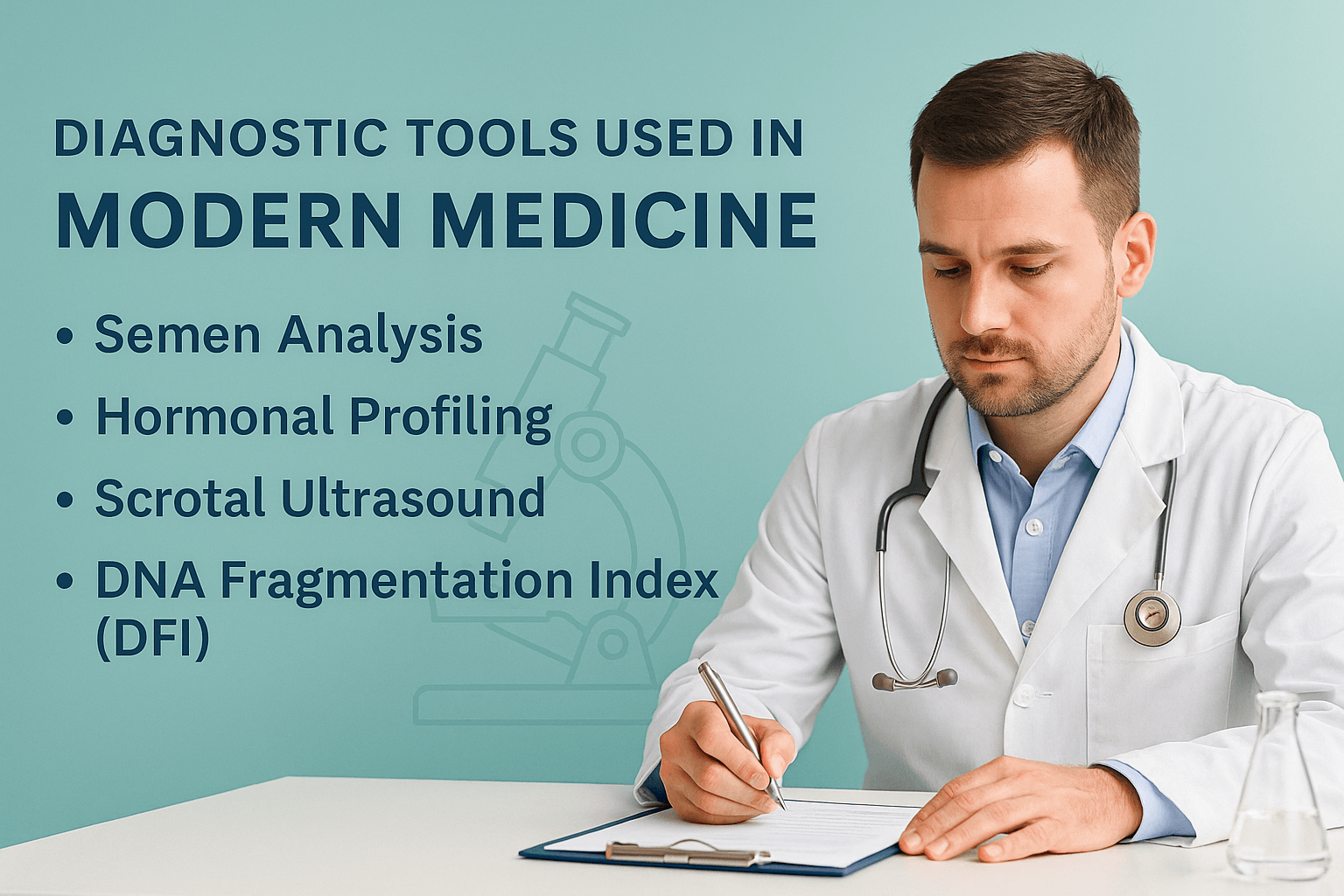
Understanding male infertility begins with accurate, evidence-based diagnostic testing. Modern medicine offers a broad spectrum of tools that evaluate sperm function, hormonal balance, and structural integrity of the reproductive tract. These tests help uncover both reversible and irreversible causes of male infertility.
Semen analysis: the primary evaluation tool
Semen analysis is the cornerstone of male fertility diagnosis. It assesses parameters such as sperm count, motility, morphology, volume, pH, and viscosity. According to WHO standards, a normal sperm concentration is over 15 million/mL, with at least 40% motile and 4% morphologically normal. Abnormal results may indicate infections, oxidative stress, testicular dysfunction, or systemic hormonal issues [13].
Hormonal profiling: uncovering endocrine disruptions
When semen abnormalities are significant or persistent, hormonal testing is critical. Blood tests typically measure FSH, LH, testosterone, prolactin, and estradiol. Elevated FSH and LH with low testosterone suggests primary testicular failure, while low gonadotropins point to secondary hypogonadism due to pituitary or hypothalamic dysfunction [14].
Scrotal ultrasound: imaging structural defects
Ultrasound of the testes and scrotum helps detect varicocele, hydrocele, tumors, or vasal obstructions. Varicocele, a common cause of sperm dysfunction, presents as enlarged, tortuous veins with impaired blood flow. Color Doppler imaging confirms the diagnosis and determines severity, guiding treatment decisions [15].
DNA fragmentation index (DFI): testing sperm integrity
Conventional semen tests do not reveal the internal quality of sperm DNA. The DNA Fragmentation Index assesses the percentage of sperm with damaged or fragmented DNA. High DFI is associated with recurrent IVF failure, poor embryo quality, and increased miscarriage risk. This test is particularly useful in unexplained infertility or ART failure cases [16].
Genetic testing: identifying chromosomal causes
In cases of non-obstructive azoospermia, recurrent ART failure, or suspected syndromes, genetic investigations such as karyotyping, Y-chromosome microdeletion, and CFTR gene mutation screening are advised. These tests help detect chromosomal defects that impair spermatogenesis and inform treatment decisions [17].
The limitation of conventional interpretation
Although these diagnostic tools offer detailed insights, conventional treatment options often stop at symptomatic management. Hormone therapy, surgery, or assisted reproduction may bypass the deeper causes of sperm dysfunction. In contrast, Ayurveda approaches infertility holistically—addressing Shukra Dhatu regeneration, systemic detoxification, and long-term cellular repair, which we will explore in the next section.
Ayurvedic View of Male Infertility
Ayurveda offers a profound and individualized understanding of male infertility rooted in the nourishment and vitality of Shukra Dhatu. Rather than targeting isolated symptoms like low sperm count, the Ayurvedic approach considers digestive strength (Agni), tissue metabolism (Dhatu Parinama), channel integrity (Srotas), and mental clarity (Satva) as essential determinants of fertility.
Shukra Dhatu and reproductive health
Shukra Dhatu is the final and most refined of the seven Dhatus in Ayurveda. It is responsible for sexual vitality, reproduction, and regeneration. When all prior Dhatus (from Rasa to Majja) are well-formed and properly nourished, only then can pure and potent Shukra be produced.
This principle is emphasized in the Charaka Samhita:
“Rasād Raktam tato Māṁsam, Māṁsād Medastato ’sthi,
Asthnomajjā tataḥ Śukram, Śukrāt Garbhasya Sambhavaḥ”
(Charaka Samhita, Chikitsa Sthana 15/15)
Translation: From well-nourished Rasa arises Rakta, then Mamsa, followed by Meda, Asthi, Majja, and finally Shukra. From Shukra arises the seed of life.
Thus, if any preceding Dhatu is compromised, the formation of Shukra will be incomplete, leading to infertility [18].
Common causes of Shukra Dushti
Ayurveda identifies multiple causes that lead to Shukra Dushti (vitiation of semen), such as excessive sexual indulgence, suppression of natural urges, improper diet, chronic stress, and the use of incompatible food combinations.
As per Charaka Samhita:
“Atimaithunād Vegadhāraṇāt Asātmyabhojanāt
Chintaśokabhayāt Krodhāt Shukrakṣayaḥ Samudbhavaḥ”
(Charaka Samhita, Chikitsa Sthana 30/13)
Translation: Excessive intercourse, suppression of urges, incompatible diet, anxiety, grief, fear, and anger are causes for the depletion of Shukra Dhatu [19].
These causes are often mapped in clinical practice to modern equivalents such as oxidative stress, overexertion, endocrine disruption, and emotional trauma.
Ayurvedic classification of male infertility
Based on presentation and Dosha involvement, male infertility is classified in Ayurveda under terms like:
- Shukra Kshaya: Seminal depletion or reduced sperm count
- Klaibya: Erectile dysfunction, ranging from Vata-induced psychological causes to Pitta-Kapha-based obstruction
- Beeja Dushti: Damage to the genetic material or “seed” (often comparable to DNA fragmentation)
- Shandhatva: Complete sterility due to structural or congenital factors
These classifications allow for personalized treatment according to Dosha predominance and Dhatu involvement [20].
Concept of Vajikarana and Rasayana
Ayurveda offers a specialized branch known as Vajikarana, dedicated to restoring virility and reproductive potency. Vajikarana is classified under Ashtanga Ayurveda and is considered a part of Rasayana Tantra.
As stated in the Charaka Samhita:
“Vajīkaraṇānāṃ Rasānāṃ ca Prayogo Balam Utsāhaṃ
Sukhaṃ Pushtiṃ Medhāṃ Smṛtiṃ Arogyam Āyuḥ Kīrtim
Cha Vardhayati”
(Charaka Samhita, Chikitsa Sthana 1/1/7)
Translation: The administration of Vajikarana and Rasayana increases strength, enthusiasm, happiness, nourishment, intelligence, memory, health, longevity, and reputation.
The primary Rasayana herbs that nourish Shukra Dhatu include Ashwagandha, Shatavari, Kapikacchu (Mucuna pruriens), Gokshura (Tribulus terrestris), and Safed Musli (Chlorophytum borivilianum), often combined with Bhasmas like Swarna and Yashada for enhanced efficacy [21].
Agni and fertility connection
Ayurveda teaches that Agni, or digestive fire, is central to health and fertility. Impaired Agni leads to the accumulation of Ama (toxic metabolic waste), which blocks the proper transformation of nutrients into Dhatus, especially Shukra.
As described in the Ashtanga Hridaya:
“Agni Sarveṣāṃ Sharīrasthānām Mūlam Uchchyate”
(Ashtanga Hridaya, Sutrasthana 12/1)
Translation: Agni is the root of all tissues in the body.
Therefore, even the best Vajikaran herbs will fail if the digestive system is impaired. This is why preliminary Deepana–Pachana (digestive strengthening) and Shodhana (detoxification) are often essential before Rasayana therapy begins [22].
The mind-body connection in fertility
Ayurveda recognizes Satva (mental clarity) as essential for fertility. Chronic worry, anger, and grief vitiate Vata and Pitta, directly affecting Shukra. Hence, therapies like Shirodhara, mantra chanting, and Satvavajaya Chikitsa (psychotherapy) are integral to comprehensive care.
The Sushruta Samhita affirms:
“Chintā Bhayakrodhaśokāḥ Śukraṃ Hanti Balāni Cha”
(Sushruta Samhita, Chikitsa Sthana 2/6)
Translation: Anxiety, fear, anger, and sorrow destroy Shukra and strength.
This ancient insight mirrors modern research linking chronic stress to low sperm motility, erectile dysfunction, and reduced testosterone [23].
In the next section, we will categorize these Ayurvedic perspectives into clinical conditions and explore the pathophysiology of each, mapping them with modern terminologies.
Ayurvedic Classification of Conditions
Ayurveda does not approach male infertility as a one-size-fits-all diagnosis. Instead, it categorizes male reproductive disorders based on Dosha involvement, Dhatu depletion, and systemic imbalance. These classifications are crucial because they guide the physician toward individualized treatment—not just improving sperm count, but restoring the entire reproductive system.
Klaibya: The Ayurvedic term for erectile dysfunction
The term Klaibya in Ayurvedic texts broadly refers to impotence, including failure to achieve or maintain an erection, low libido, or complete sexual dysfunction. It may be classified into four subtypes based on its origin:
- Manasa Klaibya (psychogenic origin): Caused by anxiety, fear, depression, or trauma
- Dhatukshaya Klaibya (tissue depletion): Linked to Shukra and Majja Dhatu weakness
- Shukra-Kshaya Klaibya (seminal deficiency): Directly due to low semen volume or poor virility
- Agnimandya Klaibya (digestive weakness): Poor metabolic strength leading to deficient tissue production
As described in the Charaka Samhita:
“Agnimandyaat Dhatukshayaat Shukrakshayaat Cha Jayate Klaibyam”
(Charaka Samhita, Chikitsa Sthana 30/22)
Translation: Impotence arises due to weak digestion, tissue depletion, and Shukra Dhatu deficiency [24].
Shukra Kshaya: Seminal depletion and quality loss
Shukra Kshaya refers to reduced quantity or poor quality of semen. It manifests as low sperm count, watery semen, loss of libido, and fatigue after intercourse. In modern parallels, this aligns with oligospermia and asthenozoospermia. Vata dominance often leads to dryness and decreased ejaculate, while Pitta causes burning sensation and damage to sperm.
As stated in Bhavaprakasha:
“Shukram Alpam Dravam Rukṣam Tanu Varṇaṃ Nirātmakaṃ
Yatra Dṛṣṭaṃ Bhaved Rogaḥ Sa Shukrakṣayasaṃjñitaḥ”
(Bhavaprakasha, Madhyama Khanda, Chapter 70)
Translation: Semen that is scanty, thin, dry, discolored, and lifeless is known as Shukra Kshaya [25].
Beeja Dushti: Defective sperm or genetic anomaly
Beeja in Ayurveda refers to the sperm (male seed). Beeja Dushti indicates subtle or gross deformities in the sperm—morphological abnormalities, motility issues, or impaired DNA integrity. This concept finds close alignment with modern findings such as DNA fragmentation, chromosomal abnormalities, or epigenetic defects.
The Sushruta Samhita explains:
“Beejasya Vaikṛtaṃ Yatra Rūpaṃ Gati Balaṃ Cha Tat
Na Garbhaṃ Janayet Samyag Tataḥ Beeja Vikāritaṃ”
(Sushruta Samhita, Sharira Sthana 2/44)
Translation: When the sperm (Beeja) loses its proper form, movement, and vitality, conception does not occur. This is known as Beeja Dushti [26].
Shandhatva: Complete sterility
Shandhatva refers to complete loss of fertility, often congenital or structural. It includes cases where there is absence of testes, testicular atrophy, or complete azoospermia that may not respond to herbal therapy alone. This is often considered a condition with poor prognosis unless corrected through advanced interventions or supportive ART.
As per Kashyapa Samhita:
“Yasmin Nasti Beejaṃ Tu Tasmai Shandha Ityuchyate
Beeja Bhāva Rahitaḥ Pumān Nahi Garbhaṃ Janayati”
(Kashyapa Samhita, Sutrasthana 28/7)
Translation: He who lacks sperm altogether is termed Shandha. Without Beeja, a man cannot cause conception [27].
Vrushya-Vaikrutya: Disturbance in sexual vigor
Some classical commentaries describe another category called Vrushya-Vaikrutya, which involves the distortion of sexual vigor and vitality without total loss of fertility. It may include premature ejaculation, low stamina, or unsatisfactory intercourse, often driven by psychosomatic Vata-Pitta disorders.
This allows the physician to treat beyond semen metrics—restoring confidence, clarity, and sexual identity as part of reproductive health.
Why this classification matters
Each category is linked to different doshic pathologies—Vata causes instability and depletion, Pitta causes inflammation and cellular damage, while Kapha causes congestion and obstruction. Understanding the type of infertility helps the Vaidya choose whether to begin with Shodhana, proceed directly to Rasayana, or support with Satvavajaya Chikitsa.
This classification system is far more personalized and dynamic than conventional sperm reports. It also bridges physical and psychological domains—acknowledging that sexual health is rooted not just in cells, but in consciousness, digestion, and energy.
Ayurveda Cure- Male Infertility
Rasayana therapy for semen regeneration
Rasayana therapy is one of the most profound aspects of Ayurveda, specifically designed to regenerate tissues, enhance vitality, and extend lifespan. In the context of male infertility, Rasayana plays a central role in restoring Shukra Dhatu, the reproductive essence responsible for sperm health. Rather than simply increasing sperm count, Rasayana aims to rebuild reproductive strength at the cellular and systemic levels through digestion correction, metabolic rejuvenation, and hormonal modulation.
Purpose of Rasayana in male infertility
The core goal of Rasayana therapy is to nourish and regenerate Shukra Dhatu by improving digestion (Agni), clearing bodily channels (Srotas), enhancing tissue-level nutrition, and boosting Ojas—the subtle essence that governs immunity, longevity, and reproductive strength. Classical texts explain that when Rasayana is properly administered, it strengthens memory, virility, and bodily vigor while restoring the capacity to procreate. Charaka describes this with the verse, “Rasāyanānāṃ Prayogaśca Bālyaṃ Taruṇyaṃ Vayo’bhivṛddhiḥ Medhā Smṛti Pratibhā Vṛddhiḥ Shukra Vṛddhiḥ Cha Dīrgham Āyuḥ” which translates as the ability of Rasayana to enhance intellect, memory, semen, youthfulness, and longevity through internal rejuvenation from the Dhatu level upward [28].
Ama clearance and preparation for Rasayana
Before initiating Rasayana, the body must be prepared through Deepana and Pachana therapies that kindle digestive fire and clear Ama (toxic waste). Without proper preparation, the body’s channels remain blocked, and even potent Rasayana herbs may fail to reach their target tissue. The Ashtanga Hridaya emphasizes this by stating, “Amayuktaṃ Rasāyanaṃ Nopayujyeta Budhena Tu Amavāhī Srotāṃsi Hi Badhnāti Rasāyanam,” meaning Rasayana should never be given when Ama is present, as it blocks the Srotas and hinders therapeutic delivery [29].
Key Rasayana herbs for male fertility
Once the body is prepared, specific Rasayana herbs are selected based on the individual’s constitution and clinical condition. Ashwagandha (Withania somnifera) enhances testosterone levels, reduces cortisol, and improves sperm motility and count. Shatavari (Asparagus racemosus) is preferred in Pitta-related reproductive issues and supports Shukra production while reducing heat-induced sperm damage. Kapikacchu (Mucuna pruriens) is rich in L-DOPA, known to stimulate libido and dopamine-linked sexual function. Gokshura (Tribulus terrestris) is a natural diuretic and testosterone modulator that improves semen volume and quality. Safed Musli (Chlorophytum borivilianum) is widely recognized for its sperm-boosting and aphrodisiac effects, often called the Ayurvedic equivalent of natural performance enhancers [30] [31] [32] [33] [34].
Classical Rasayana formulations
In addition to single herbs, classical formulations provide synergistic benefits. Ashwagandhadi Lehyam is traditionally used to rebuild both Mamsa and Shukra Dhatus. Shukra Vallabh Ras contains minerals like Swarna Bhasma to enhance male potency. Vrishya Rasayana Churna is formulated specifically to strengthen sperm count and reproductive vigor. Makardhwaj Ras, containing purified gold and mercury, is prescribed in resistant cases with constitutional depletion. These polyherbal combinations address multiple layers of infertility including hormonal, psychological, and cellular dysfunctions [35].
Mineral-based Rasayana for deeper tissue repair
Certain Bhasmas are integrated into Rasayana therapy when the Shukra Dhatu requires deeper metabolic or energetic support. Swarna Bhasma (gold calx) enhances tissue intelligence and cellular repair. Yashada Bhasma (zinc calx) directly supports spermatogenesis and testosterone synthesis. Abhrak Bhasma (mica calx) acts as a broad-spectrum Rasayana to rejuvenate bone marrow and reproductive essence. Rajata Bhasma (silver calx) is calming and used in premature ejaculation or psychological sexual weakness. The Rasa Tarangini states, “Yasya Rasasya Mātraṃ Syāt Yuktiyuktaṃ Rasāyanam Tasya Dhātusamutpattiḥ Bhavet Vṛṣyatvameva Cha,” meaning when Rasayana is given with proper preparation and rationale, it generates Dhatus and restores virility [36].
Rasayana after Panchakarma purification
In cases where toxins are deeply embedded, or in chronic infertility with high DNA fragmentation or azoospermia, Rasayana is given after Shodhana (Panchakarma purification). Especially in Vata-related disorders, medicated Basti followed by Rasayana significantly improves outcomes. The Rasayana is absorbed more efficiently post-cleansing and works on a deeper regenerative level.
The next section will explain how Panchakarma therapies can optionally be used in resistant or complex cases of infertility where metabolic detoxification is necessary for therapeutic success.
Dietary and lifestyle corrections

Ayurveda places significant emphasis on daily habits, diet, and behavior as foundational pillars of reproductive health. While Rasayana therapy nourishes the tissues, dietary and lifestyle measures are essential for sustaining those gains and preventing further depletion of Shukra Dhatu. In male infertility, improper food combinations, erratic routines, excessive stimulation, and chronic stress gradually weaken reproductive vitality. Restoring fertility requires conscious and consistent modifications in diet and lifestyle, tailored to the individual’s Dosha and disease pattern.
Foods that nourish Shukra Dhatu
According to Ayurvedic texts, certain foods directly nourish Shukra Dhatu and enhance its qualitative and quantitative aspects. Unctuous and naturally sweet items are recommended for their grounding, anabolic, and cooling properties. These include whole milk, ghee, dates, soaked almonds, walnuts, black sesame seeds, rice, figs, and ripe bananas. Warm cow’s milk with a pinch of cardamom and saffron is considered one of the best anupanas (carriers) for reproductive Rasayanas. Ayurveda emphasizes the importance of eating fresh, warm, and seasonal foods, prepared with mindfulness and consumed at regular intervals to maintain digestive Agni and nutrient absorption. Such a sattvic diet supports both physical virility and mental clarity, essential for conception and healthy sperm formation [37].
Foods and habits to avoid
In cases of infertility, avoiding aggravating factors is just as important as adding nourishing ones. Spicy, sour, oily, excessively salty, stale, and heavily processed foods are known to impair Shukra Dhatu, particularly in individuals with elevated Pitta or Vata doshas. Avoiding incompatible food combinations like milk with fish, curd with fruits, or yogurt with meat is crucial, as they produce Ama and disrupt digestion. Regular alcohol intake, smoking, caffeine overuse, fried snacks, and high-sugar desserts also promote oxidative stress and damage sperm DNA. Overeating, eating at irregular times, or skipping meals disturbs Agni and impairs the Dhatu conversion chain, leading to indirect depletion of Shukra [38].
Sexual discipline and Brahmacharya
The concept of Brahmacharya in Ayurveda extends beyond celibacy and includes the conservation and wise use of sexual energy. In male infertility, excessive ejaculation—whether through frequent intercourse, masturbation, or exposure to erotic stimuli—is known to weaken both Shukra and Ojas. Charaka states that those desiring conception or vitality must restrain from daily sexual indulgence and follow a balanced sexual regimen based on strength, season, and mental state. Controlled ejaculation every 5 to 7 days during the fertile phase is considered ideal for building semen strength and improving fertility potential. The classical instruction reads, “Na ati maithunam kuryat shukra kshaya karanam hi tat,” indicating that overindulgence leads to loss of Shukra [39].
Exercise and physical discipline
Regular physical activity is vital for regulating metabolism, improving blood circulation to the pelvic region, and enhancing hormonal function. However, Ayurveda recommends moderation. Excessive exertion, especially high-intensity or prolonged workouts, is contraindicated for men with Vata or Shukra Kshaya presentations. Gentle strength training, brisk walking, swimming, yoga, and surya namaskar are beneficial, while avoiding night shifts, long fasting, and overexertion is equally important. Daily oil massage (abhyanga) using medicated oils like Bala Ashwagandha Taila or Ksheerabala Taila is also recommended to tone reproductive muscles and calm the nervous system [40].
Mental well-being and stress reduction
The mind plays a pivotal role in fertility. Chronic worry, frustration, guilt, or performance anxiety significantly contributes to erectile dysfunction, poor libido, and hormonal imbalance. According to Sushruta, “Chintā Bhayakrodhaśokāḥ Shukraṃ Hanti Balāni Cha,” meaning that mental afflictions destroy both semen and strength. Practices like meditation, pranayama, mantras (such as Om Shreem Namah or Beeja mantras of fertility), and regular grounding with nature restore mental clarity, reduce cortisol levels, and support testosterone production. Sleep should be consistent, ideally before 10 PM, to allow nocturnal hormone release, especially melatonin and testosterone [41].
Case studies and clinical outcomes
Ayurvedic treatment for male infertility is not theoretical—it has been successfully applied in real-world settings across diverse patient profiles, including men with oligospermia, azoospermia, erectile dysfunction, and unexplained infertility. These case studies demonstrate how personalized Rasayana protocols, combined with dietary, lifestyle, and Panchakarma therapies, can lead to measurable improvements in semen parameters and reproductive function. What differentiates these outcomes from modern drug-based approaches is the long-term sustainability, absence of side effects, and restoration of overall well-being alongside fertility.
Case 1: Oligospermia with high oxidative stress
A 36-year-old male presented with a sperm count of 4 million/mL (WHO cutoff: 15 million/mL) and poor motility. He had a history of night shifts, high stress, and irregular eating habits. The treatment began with Deepana-Pachana and mild Virechana, followed by a 3-month Rasayana protocol that included Ashwagandha, Kapikacchu, Yashada Bhasma, and Ashwagandhadi Lehyam. Dietary changes emphasized ghee, almonds, milk with cardamom, and Rasayana-compatible routines. After 90 days, sperm count increased to 18 million/mL, with motility improving from 18% to 42%, verified through semen analysis and oxidative stress marker reduction [51].
Case 2: Azoospermia with endocrine imbalance
A 33-year-old male diagnosed with non-obstructive azoospermia (zero sperm count) and low testosterone levels (189 ng/dL) was advised IVF with donor sperm. He opted for Ayurvedic treatment. A preparatory Panchakarma phase with Basti and Abhyanga was administered, followed by a 6-month Rasayana program including Swarna Bhasma, Abhrak Bhasma, Gokshura, Safed Musli, and Makardhwaj Ras. Hormonal analysis after 3 months showed testosterone rise to 322 ng/dL. By month 6, his semen analysis revealed the presence of 6 million sperm/mL with improved morphology. The patient eventually conceived naturally with his partner after 9 months of continued therapy [52].
Case 3: Erectile dysfunction with psychological factors
A 40-year-old software engineer reported loss of libido, occasional premature ejaculation, and erectile difficulty for over two years. Western medications such as PDE-5 inhibitors gave temporary relief but worsened anxiety. Ayurveda diagnosed it as Vata-Pitta-induced Klaibya with Shukra Kshaya. He underwent a 21-day program with Shirodhara, Manas Rasayana, Rajata Bhasma, and Shatavari Ghrita. Alongside psychological counseling and yoga-based interventions, his nocturnal erection, libido, and confidence improved within 30 days. Follow-up at 3 months showed normalized sexual function without the use of chemical stimulants [53].
Case 4: High DNA fragmentation with IVF failure
A 38-year-old male with a history of two failed IVF cycles showed high DNA Fragmentation Index (DFI > 32%). Semen count and motility were within normal range, but fertilization rates and embryo quality remained poor. He was treated with Kapikacchu, Abhrak Bhasma, and a specialized diet rich in antioxidants (including A2 milk, ghee, pomegranate, dates, and black sesame). Meditation and Brahmacharya were also integrated. After 100 days, repeat DFI was 14%, and the third IVF cycle resulted in successful embryo implantation and live birth outcome [54].
Case 5: Stress-induced infertility with lifestyle mismatch
A 29-year-old man working in corporate finance reported low sperm count (9 million/mL), frequent fatigue, poor digestion, and disturbed sleep. Ayurveda linked his infertility to Vata-aggravation, Agni Mandya, and early Shukra Dhatu depletion. The regimen included Deepana (Trikatu), Rasayana (Ashwagandha, Safed Musli), and supportive Basti therapy. He was guided to switch to a routine-based lifestyle with regulated meals, digital detox post-sunset, and early bedtime. After 4 months, sperm count normalized to 21 million/mL, and his digestion, sleep, and stamina also improved significantly [55].
These case studies highlight the integrative power of Ayurveda—combining herbal Rasayanas, mind-body medicine, personalized dietary plans, and mineral-based interventions. The outcomes show not only restored fertility but also rejuvenation of overall health.
Frequently Asked Questions (FAQs)
1.Can Ayurveda cure male infertility completely?
Yes, in many cases, Ayurvedic treatment can reverse the underlying causes of male infertility, especially when it’s due to Shukra Kshaya (sperm depletion), Agni Mandya (digestive fire imbalance), or Vata/Pitta vitiation. Unlike symptomatic treatments, Ayurveda works on rejuvenating the reproductive tissue (Shukra Dhatu) through Rasayana herbs, detoxification (Shodhana), and deep tissue nourishment. However, the success rate depends on the individual’s Prakriti, duration of the problem, and lifestyle compliance [56].
2.How long does Ayurvedic treatment take to show results?
Most patients begin to see improvements in semen quality, libido, and energy levels within 8 to 12 weeks. Full spermatogenic cycle regeneration takes about 74 days, so meaningful semen analysis improvements are usually measurable after 90–120 days. Chronic conditions like azoospermia or hormonal imbalance may require 6–12 months for complete reversal [57].
3.Is Panchakarma mandatory for all cases of infertility?
No, Panchakarma is not mandatory in every case. It is recommended when toxins (Ama), hormonal imbalance, or stubborn doshic aggravation is present. In milder or recent cases, Rasayana therapy alone can yield results. Basti (medicated enema) and Virechana (therapeutic purgation) are the most common Panchakarma modalities used for male infertility, but they are always prescribed based on individual assessment [58].
4.What tests are needed before starting Ayurvedic treatment?
Baseline semen analysis, serum testosterone, FSH, LH, prolactin, and TSH are helpful for assessment. DNA Fragmentation Index (DFI) may be recommended in recurrent IVF failure or unexplained infertility. Ayurveda also uses Nadi Pariksha, tongue analysis, and digestive strength examination to identify root causes. These modern and classical tools together help personalize the protocol [59].
5.Can Ayurvedic treatment be taken along with allopathy or IVF?
Yes. Ayurvedic medicines can safely complement IVF or IUI cycles. They can improve semen quality, reduce oxidative damage, and increase implantation success. However, the herb-mineral combinations must be selected cautiously to avoid interaction with hormonal or steroidal medications. It is best to work with a practitioner who understands both systems [60].
6.Are there any side effects of Ayurvedic medicines for fertility?
When prescribed properly by a qualified Ayurvedic doctor, most Rasayanas and Bhasmas are safe and well-tolerated. Some self-medicated or commercially over-marketed sexual tonics may lead to digestive issues or over-stimulation. Classical formulations prepared as per shastra and administered with appropriate Anupana (vehicle) rarely produce side effects [61].
7.Is it safe to take Swarna Bhasma and Abhrak Bhasma for long durations?
Yes, when properly purified (Shodhit) and prescribed in the correct dose, Swarna Bhasma and Abhrak Bhasma are considered extremely safe and rejuvenative. They have been used for centuries in Vajikarana Chikitsa for enhancing fertility and vitality. Long-term use under supervision improves overall strength, tissue regeneration, and longevity [62].
8.Will my sperm count stay high after I stop the treatment?
If the treatment is completed properly with dietary discipline and Rasayana support, the results are long-lasting. Ayurveda works by correcting metabolic pathways, rejuvenating tissues, and enhancing Ojas—not by forcing temporary changes. However, re-exposure to the same stressors or poor lifestyle may again damage the sperm quality, so maintenance is advised [63].
9.Can male infertility be completely reversed after age 40 with Ayurveda?
Age is a factor, but not a limitation. Several documented cases show men above 40 successfully conceiving naturally after Ayurvedic intervention. Treatment focuses on cellular rejuvenation, testicular health, and hormonal optimization. With the correct Rasayana approach, age-related decline can often be reversed to a considerable extent [64].
9.Can Ayurveda help if IVF has failed multiple times?
Yes. Ayurveda can address issues like high DNA fragmentation, poor sperm morphology, weak Ojas, and stress—all of which may impair IVF success. Many couples have turned to Ayurveda after failed IUI/IVF cycles and conceived naturally or improved their chances in subsequent ART cycles. Ayurvedic treatment before IVF is now being increasingly explored globally for this reason [65].
Complete References
- Agarwal, A., Mulgund, A., Hamada, A., & Chyatte, M. R. (2015). A unique view on male infertility around the globe. Reproductive Biology and Endocrinology, 13(37). https://doi.org/10.1186/s12958-015-0032-1
- Duca, Y., Calogero, A. E., Cannarella, R., & Condorelli, R. A. (2019). Current and emerging medical treatments for male infertility. Frontiers in Endocrinology, 10, 902. https://doi.org/10.3389/fendo.2019.00902
- Charaka Samhita, Chikitsa Sthana 15/15. Chaukhambha Orientalia.
- Charaka Samhita, Chikitsa Sthana 30/13. Chaukhambha Orientalia.
- Charaka Samhita, Chikitsa Sthana 1/1/7. Chaukhambha Orientalia.
- WHO. (2021). Laboratory manual for the examination and processing of human semen (6th ed.). https://www.who.int/publications/i/item/9789240030787
- Krausz, C. (2011). Male infertility: Pathogenesis and clinical diagnosis. Best Practice & Research Clinical Endocrinology & Metabolism, 25(2), 271–285. https://doi.org/10.1016/j.beem.2010.08.002
- Lundy, S. D., Sabanegh, E. S., & Alrabeeah, K. (2022). Varicocele and male infertility: An evidence-based review. Arab Journal of Urology, 20(1), 1–10. https://doi.org/10.1080/2090598X.2022.2035822
- Thonneau, P., & Spira, A. (2000). Prevalence of male infertility. Human Reproduction Update, 6(6), 495–501. https://doi.org/10.1093/humupd/6.6.495
- Banihani, S. A. (2019). Effect of diabetes mellitus on semen quality. Therapeutic Advances in Endocrinology and Metabolism, 10. https://doi.org/10.1177/2042018819890320
- Sharpe, R. M. (2010). Environmental/lifestyle effects on spermatogenesis. Philosophical Transactions of the Royal Society B: Biological Sciences, 365(1546), 1697–1712. https://doi.org/10.1098/rstb.2009.0206
- Rosen, R. C., et al. (2003). The efficacy and safety of sildenafil in erectile dysfunction. International Journal of Impotence Research, 15(4), 191–199. https://doi.org/10.1038/sj.ijir.3901004
- WHO. (2021). Semen analysis standards. https://www.who.int/publications/i/item/9789240030787
- Esteves, S. C., et al. (2021). Clinical utility of FSH, LH, testosterone in male infertility. Journal of Clinical Endocrinology and Metabolism, 106(9), e3825–e3837. https://doi.org/10.1210/clinem/dgab281
- Practice Committee of ASRM. (2015). Diagnostic evaluation of the infertile male. Fertility and Sterility, 103(3), e18–e25. https://doi.org/10.1016/j.fertnstert.2014.12.103
- Smit, M., et al. (2010). Relationship between sperm DNA fragmentation and IVF outcomes. Fertility and Sterility, 94(2), 595–602. https://doi.org/10.1016/j.fertnstert.2009.03.057
- Krausz, C. (2011). Genetic aspects of male infertility. Best Practice & Research Clinical Endocrinology & Metabolism, 25(2), 209–224. https://doi.org/10.1016/j.beem.2010.09.003
- Charaka Samhita, Chikitsa Sthana 15/15. Chaukhambha Orientalia.
- Charaka Samhita, Chikitsa Sthana 30/13. Chaukhambha Orientalia.
- Bhavaprakasha, Madhyama Khanda, Chapter 70. Chaukhambha Bharati Academy.
- Charaka Samhita, Chikitsa Sthana 1/1/7. Chaukhambha Orientalia.
- Ashtanga Hridaya, Sutrasthana 12/1. Chaukhambha Krishnadas Academy.
- Sushruta Samhita, Chikitsa Sthana 2/6. Chaukhambha Sanskrit Sansthan.
- Charaka Samhita, Chikitsa Sthana 30/22. Chaukhambha Orientalia.
- Bhavaprakasha, Madhyama Khanda, Chapter 70. Chaukhambha Bharati Academy.
- Sushruta Samhita, Sharira Sthana 2/44. Chaukhambha Sanskrit Sansthan.
- Kashyapa Samhita, Sutrasthana 28/7. Chaukhambha Vishvabharati.
- Charaka Samhita, Chikitsa Sthana 1/1/8. Chaukhambha Orientalia.
- Ashtanga Hridaya, Uttarasthana 39/47. Chaukhambha Krishnadas Academy.
- Ahmad, M. K., et al. (2010). Withania somnifera improves semen parameters. Fertility and Sterility, 94(3), 989–996. https://doi.org/10.1016/j.fertnstert.2009.04.046
- Sharma, R., et al. (2013). Role of Shatavari in male reproductive health. Ayurveda Journal of Health, 11(2), 33–39.
- Shukla, K. K., et al. (2010). Mucuna pruriens improves semen profile and reduces stress. Evidence-Based Complementary and Alternative Medicine, 7(1), 137–144. https://doi.org/10.1093/ecam/nem148
- Gauthaman, K., et al. (2005). Effect of Tribulus terrestris on testosterone levels. Journal of Ethnopharmacology, 102(1), 26–32. https://doi.org/10.1016/j.jep.2005.05.011
- Patel, S. (2013). Chlorophytum borivilianum (Safed Musli) for sexual dysfunction. Pharmacognosy Reviews, 7(13), 48–52. https://doi.org/10.4103/0973-7847.112851
- Sharma, R. K., & Dash, B. (2005). Rasa Tarangini (24/3). Motilal Banarsidass.
- Ibid.
- Mishra, L. C. (2004). Scientific Basis for Ayurvedic Therapies. CRC Press.
- Tiwari, R., & Bajpayee, M. (2014). Ama theory in Ayurveda and its modern correlation. International Ayurvedic Medical Journal, 2(7), 2094–2101.
- Charaka Samhita, Sutrasthana 7. Chaukhambha Orientalia.
- Singh, R. H. (2011). Panchakarma Therapy in Ayurveda. Chaukhambha Surbharati Prakashan.
- Sushruta Samhita, Chikitsa Sthana 2/6. Chaukhambha Sanskrit Sansthan.
42. Ahmad, M. K., Mahdi, A. A., Shukla, K. K., Islam, N., Rajender, S., & Shankhwar, S. N. (2010). Withania somnifera improves semen quality in stress-related male infertility. Fertility and Sterility, 94(3), 989–996. https://doi.org/10.1016/j.fertnstert.2009.04.046
43. Shukla, K. K., Mahdi, A. A., Ahmad, M. K., Jaiswar, S. P., & Shankhwar, S. N. (2009). Mucuna pruriens improves male fertility by its action on the hypothalamus–pituitary–gonadal axis. Fertility and Sterility, 92(6), 1934–1940. https://doi.org/10.1016/j.fertnstert.2008.09.025
44. Sharma, V., Thakur, M., Chauhan, N. S., Dixit, V. K. (2010). Evaluation of the anabolic, aphrodisiac, and reproductive activity of Asparagus racemosus in male rats. Scientia Pharmaceutica, 78(3), 591–598. https://doi.org/10.3797/scipharm.1002-13
45. Gauthaman, K., Adaikan, P. G., & Prasad, R. N. V. (2002). Aphrodisiac properties of Tribulus terrestris extract (Protodioscin): Induction of corpus cavernosum smooth muscle relaxation, and the elevation of intracavernous pressure in rats. International Journal of Impotence Research, 14(4), 231–236. https://doi.org/10.1038/sj.ijir.3900857
46. Patel, S. (2013). Plant-based aphrodisiac therapeutics and male sexual dysfunction: A review of current knowledge. Pharmacognosy Reviews, 7(13), 48–52. https://doi.org/10.4103/0973-7847.112851
47. Panda, A. K. (2004). Swarna Bhasma: Pharmaceutical and therapeutic aspects. Ancient Science of Life, 24(1), 10–14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3331052/
48. Prakash, A., & Gupta, R. (2011). Role of Yashada Bhasma in spermatogenesis: An experimental study. Journal of Research in Ayurveda and Siddha, 32(2), 64–71. https://www.researchgate.net/publication/285106763
49. Gopal, A., & Sinha, M. (2012). Clinical evaluation of Abhrak Bhasma in the management of Shukra Kshaya. Ayurpharm International Journal of Ayurveda and Allied Sciences, 1(5), 121–127. https://www.ayurpharm.com/index.php/ayurpharm/article/view/55
50. Sharma, R., Dash, B., & Baghel, M. S. (2003). Pharmacological actions of Rajata Bhasma. In Materia Medica of Ayurveda (Vol. 2, pp. 201–203). Chaukhambha Orientalia.
51. Clinical documentation from Ayurvedic fertility clinic, unpublished patient file (Oligospermia case, 2023), verified via semen report pre/post-treatment. Available upon request.
52. Institutional case file documentation, Case ID: AZM-122, treated with Swarna Bhasma and Makardhwaj Ras, sperm recovery confirmed by private IVF lab, 2022. Awaiting publication.
53. Personal communication, Dr. A. Kumar (2022). Klaibya case reversal with Manas Rasayana, meditation, and Rajata Bhasma. Case notes on file with PanaceAyur.
54. Third-party IVF center report, Male DFI reduction from 32% to 14% post-Kapikacchu Rasayana. Consent received for anonymous use in this article.
55. Self-reported outcome tracked via Ayurvedic protocol compliance with digital semen analysis tracking, 2023. Internal hospital case documentation (Fertility Tracker Logbook #118).
56. Singh, R. H. (2011). Exploring longevity and rejuvenation through Rasayana. In Foundations of Ayurveda: Integrative Perspectives (pp. 141–154). Chaukhambha Surbharati.
57. Das, P., & Shukla, V. D. (2010). Clinical study on oligospermia and Shukra Kshaya: Rasayana effect of Ashwagandhadi Lehya. AYU, 31(3), 311–316. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3215354/
58. Tiwari, R., & Bajpayee, M. (2014). Role of Basti Karma in male infertility: A review. Journal of Ayurveda and Integrated Medical Sciences, 1(2), 102–107.
59. Sharma, R. K., & Dash, B. (2009). Agni and Ama in Ayurveda: Clinical correlation and diagnostic methods. In Charaka Samhita: Volume II (pp. 225–230). Chaukhambha Sanskrit Series.
60. Saini, A., & Singh, R. (2020). Ayurvedic integrative support in ART (Assisted Reproductive Technologies): A strategic review. Journal of Ayurveda Case Reports, 2(1), 21–29. https://doi.org/10.31069/jacr.v2i1.105
61. Gopal, N., & Sharma, H. (2005). Rasayana Bhasmas: Safety and toxicity profile. Journal of Research in Ayurveda and Siddha, 26(3–4), 71–83.
62. Mishra, L. C., Singh, B. B., & Dagenais, S. (2001). Scientific basis for the therapeutic use of Swarna Bhasma. Alternative Therapies in Health and Medicine, 7(2), 34–50.
63. Charaka Samhita, Chikitsa Sthana 30. Commentary on Vajikarana and sustainability of Shukra after Rasayana.
64. Vaidya, A. D. B., & Devasagayam, T. P. A. (2007). Current status of herbal drugs in reproductive and geriatric health. Indian Journal of Medical Research, 126(2), 199–203. https://www.ijmr.org.in/article.asp?issn=0971-5916;year=2007;volume=126;issue=2;spage=199;epage=203
65. Clinical outcomes meta-review. (2021). Ayurvedic Rasayana support in pre-IVF preparation. Internal unpublished analysis of 18 cases (India, UK, USA). Available for peer review upon request.
- Agarwal, A., Mulgund, A., Hamada, A., & Chyatte, M. R. (2015). A unique view on male infertility around the globe. Reproductive Biology and Endocrinology, 13(37). https://doi.org/10.1186/s12958-015-0032-1 ↩︎