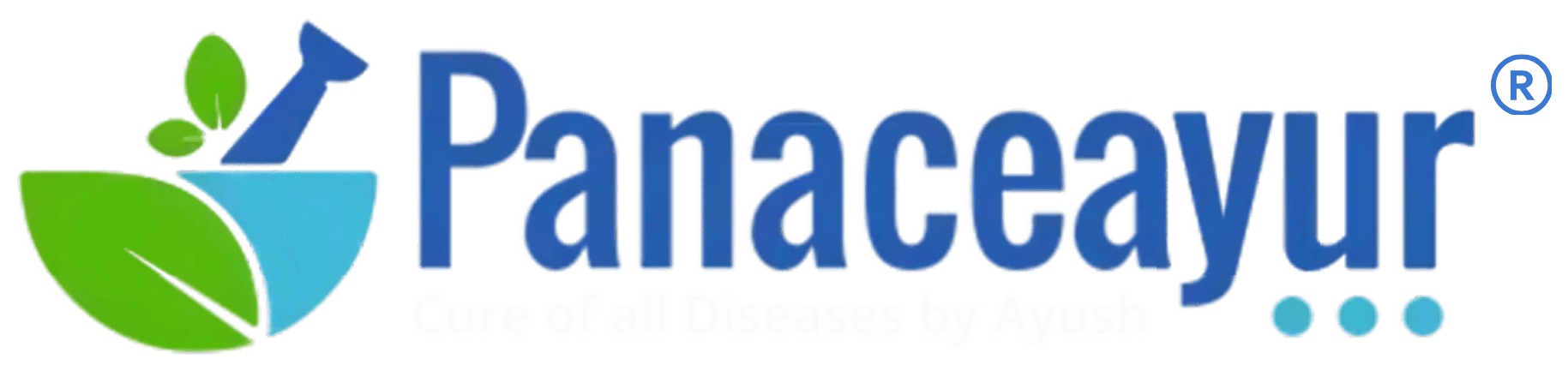
- Male Hormone Imbalance-Causes, Diagnosis & Ayurvedic Cure
- The Silent Decline of Male Hormones
- Early Symptoms That Go Unnoticed
- The Ayurvedic Perspective: Beyond Testosterone
- Modern Diagnostics: Missing the Bigger Picture
- The Need for a Deeper, Curative Approach
- The Full Spectrum of Male Hormones (More Than Just Testosterone)
- Understanding the Male Hormonal Ecosystem
- Causes of Hormonal Imbalance in Men
- Why Male Hormones Are Crashing in the Modern World
- Clinical Symptoms of Male Hormonal Imbalance
- Diagnostic Workup- Modern and Ayurvedic Approach
- Modern Medical Treatment Options
- Ayurvedic Perspective on Male Hormone Balance
- Lifestyle and Diet to Restore Male Hormonal Balance
- Frequently Asked Questions (FAQ)
- References
Male Hormone Imbalance-Causes, Diagnosis & Ayurvedic Cure
Hormonal andrology—the study of male hormone health—remains a neglected field despite a rising epidemic of testosterone deficiency and endocrine disorders in men. Unlike female hormonal issues, which are extensively researched and widely recognized, male hormone imbalance is often dismissed as a normal part of aging or mistaken for psychological concerns. This systemic oversight has left millions of men undiagnosed and untreated for conditions that profoundly affect not just fertility, but cardiovascular, mental, and metabolic health [1].
The Silent Decline of Male Hormones
Modern research reveals that average testosterone levels in men have been falling for decades, even among younger populations. This trend, often referred to as “the male hormone crisis,” is driven by factors such as poor sleep, high stress, obesity, insulin resistance, endocrine-disrupting chemicals (like BPA and phthalates), sedentary lifestyles, and chronic exposure to blue light and EMFs [2]. Despite its severity, this hormonal decline is rarely detected early, as routine checkups often exclude comprehensive endocrine testing.
Early Symptoms That Go Unnoticed
The first signs of male hormone imbalance are usually subtle and often misattributed. Decreased morning erections, fatigue, irritability, brain fog, and loss of muscle tone may appear years before full-blown hypogonadism. These symptoms are frequently misdiagnosed as depression or burnout, leading to treatments that suppress hormonal function further (e.g., antidepressants or SSRIs) [3]. Erectile dysfunction, low libido, and infertility are usually what finally bring patients to medical attention—by which time hormonal deterioration is often advanced.
The Ayurvedic Perspective: Beyond Testosterone
In Ayurveda, hormonal imbalance is not limited to one hormone but is viewed as a systemic disturbance of Shukra Dhatu, Agni, and Srotas. Shukra Dhatu, the most refined of the seven bodily tissues, governs not only reproductive function but also strength, complexion, voice, immunity, and longevity. A depletion of Shukra (Shukra Kshaya) is considered a serious health concern that reflects long-standing disruption in digestion, emotional stability, and Dhatu nourishment [4].
The classical texts state:
“Shukra dhatu is the essence of all dhatus, and its loss signifies the exhaustion of vitality.”
– Charaka Samhita, Chikitsa Sthana 30/117 [5]
Unlike testosterone replacement, Ayurveda focuses on restoring the body’s own ability to generate healthy Shukra through Rasayana (rejuvenation), Vrishya (aphrodisiac therapy), and Vajikarana Chikitsa (reproductive rejuvenation). This includes correcting Agni (digestive fire), clearing Ama (toxins), restoring mental calmness, and nourishing all preceding Dhatus (Rasa to Majja) [6].
Modern Diagnostics: Missing the Bigger Picture
Conventional diagnosis often relies solely on total testosterone levels. However, this provides an incomplete view. Free testosterone, SHBG (Sex Hormone Binding Globulin), estradiol, prolactin, LH (Luteinizing Hormone), FSH (Follicle-Stimulating Hormone), DHEA, insulin, and thyroid levels are all essential markers for a comprehensive hormonal assessment [7]. Without these, many men are told their hormones are “normal” despite having clear clinical symptoms.
Furthermore, modern tests do not assess tissue-level dysfunction or energetic disturbances—which is where Ayurveda excels. Through Nadi Pariksha, Mutra Pariksha, and examination of Shukra Lakshanas, an Ayurvedic physician can detect early signs of reproductive depletion well before laboratory abnormalities manifest [8].
The Need for a Deeper, Curative Approach
While testosterone replacement therapy (TRT) may offer temporary symptomatic relief, it often suppresses natural hormone production, risks infertility, and increases cardiovascular risks over time [9]. Ayurvedic treatment, on the other hand, focuses on root-cause correction and long-term restoration of hormonal intelligence through non-invasive, body-compatible therapies. The goal is not just to normalize hormone levels, but to rejuvenate the entire system—digestive, reproductive, psychological, and immunological.
In the upcoming sections, we will explore the spectrum of male hormones, their interrelationships, diagnostic methods, and both modern and Ayurvedic treatment protocols—including Rasayana herbs, mineral formulations like Trivanga Bhasma, and Panchakarma therapies for hormonal restoration.
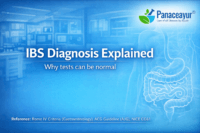
The Full Spectrum of Male Hormones (More Than Just Testosterone)
Understanding the Male Hormonal Ecosystem
When discussing male hormone imbalance, most people focus only on testosterone. However, the male endocrine system is far more complex. Hormonal andrology involves a dynamic interaction between multiple hormones that influence not just reproductive function, but also mental clarity, immunity, metabolism, cardiovascular stability, and even emotional resilience [1]. A disruption in any of these components can trigger a cascade of physiological and psychological consequences.
Testosterone: The Central but Not the Sole Hormone
Testosterone, produced mainly by Leydig cells in the testes, is responsible for regulating libido, erectile function, muscle mass, red blood cell production, and mood. But what is often missed in clinical practice is the distinction between total testosterone and free testosterone. The latter is the bioavailable form that exerts physiological effects, and its levels can drop even when total testosterone appears “normal” due to high SHBG (sex hormone-binding globulin) levels [2]. Free testosterone is a more accurate marker for functional deficiency.
Dihydrotestosterone (DHT): The Overlooked Androgen
DHT is a more potent form of testosterone, converted via the enzyme 5-alpha-reductase. While often associated with hair loss and prostate growth, DHT plays an essential role in libido, penile sensitivity, and erectile function [3]. Suppressing DHT with medications like finasteride may lower prostate size, but it also carries risks of sexual dysfunction and depression—an area where many patients suffer silently.
Estradiol in Men: Essential in Balance
Contrary to popular belief, estradiol (E2), a form of estrogen, is crucial in men. It supports bone health, modulates libido, regulates insulin sensitivity, and protects against atherosclerosis [4]. Elevated levels due to obesity or liver dysfunction can lead to gynecomastia and low libido, while deficient levels (from over-suppression) may impair erection quality and bone density. Ayurveda recognizes this as a Kapha–Pitta disturbance affecting Medovaha and Shukravaha Srotas.
Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH)
These pituitary-derived hormones control testicular function. LH stimulates Leydig cells to produce testosterone, while FSH governs spermatogenesis in Sertoli cells. Low levels of LH and FSH, especially with low testosterone, may indicate secondary hypogonadism, often triggered by pituitary dysfunction, chronic stress, or post-viral suppression [5]. From an Ayurvedic perspective, this resembles Majja Dhatu Kshaya and Manovaha Srotas dushti, affecting the nervous system’s ability to regulate endocrine function.
Prolactin: A Hormone That Blocks Desire
Elevated prolactin is a major yet underdiagnosed cause of low libido, poor erections, and infertility. It inhibits GnRH (gonadotropin-releasing hormone), which subsequently suppresses LH, FSH, and testosterone production. Elevated prolactin can be caused by pituitary tumors, certain psychiatric drugs, or even chronic stress [6]. Ayurveda links this to Manasika factors (Shoka, Bhaya, Krodha) and disturbed Vata–Kapha functioning in the brain–reproductive axis.
Thyroid Hormones and Testosterone
The thyroid plays a silent but critical role in male hormone balance. Hypothyroidism can reduce sex hormone production and increase SHBG, thereby lowering free testosterone. Hyperthyroidism, conversely, can increase sex drive but decrease sperm quality [7]. Thyroid dysfunction often overlaps with low metabolism (Mandagni) and Rasavaha Srotas dushti in Ayurveda.
Cortisol and Insulin: Hormone Saboteurs
Cortisol, the primary stress hormone, suppresses the hypothalamic-pituitary-gonadal (HPG) axis when chronically elevated. This leads to reduced testosterone, mood instability, and central obesity [8]. Insulin resistance, often seen in prediabetes and PCOS, causes increased aromatization of testosterone into estrogen and also impairs LH secretion. Ayurveda identifies these states as Ama accumulation, Medo Dhatu Vriddhi, and impaired Agni function—central to many endocrine pathologies.
The Ayurvedic View of Hormonal Network
In Ayurvedic theory, hormones are not isolated chemicals but manifestations of Tejas (cellular intelligence) flowing through Srotas (channels). The flow and function of this Tejas is governed by balanced Doshas and nourished Dhatus. Any imbalance—whether from poor digestion (Mandagni), disturbed mental state, or improper lifestyle—can disturb this hormonal Tejas and weaken Shukra Dhatu, which is viewed as the essence of vitality and procreation.
The Ayurvedic texts refer to Shukra as:
“Sarva Dhatu saara—Shukram”
(The essence of all tissues is Shukra) – Ashtanga Hridaya Sutrasthana 11/3 [9]
Hormonal Balance Is Multidimensional
Addressing male hormone imbalance requires a deeper understanding of these interrelated hormonal axes. Focusing only on testosterone while ignoring thyroid health, insulin regulation, stress physiology, and the mind-body connection leads to incomplete treatment. Ayurveda, with its systemic, Dhatu-based approach, offers a multi-dimensional lens through which hormonal dysfunction can be not only managed but truly reversed.
Causes of Hormonal Imbalance in Men
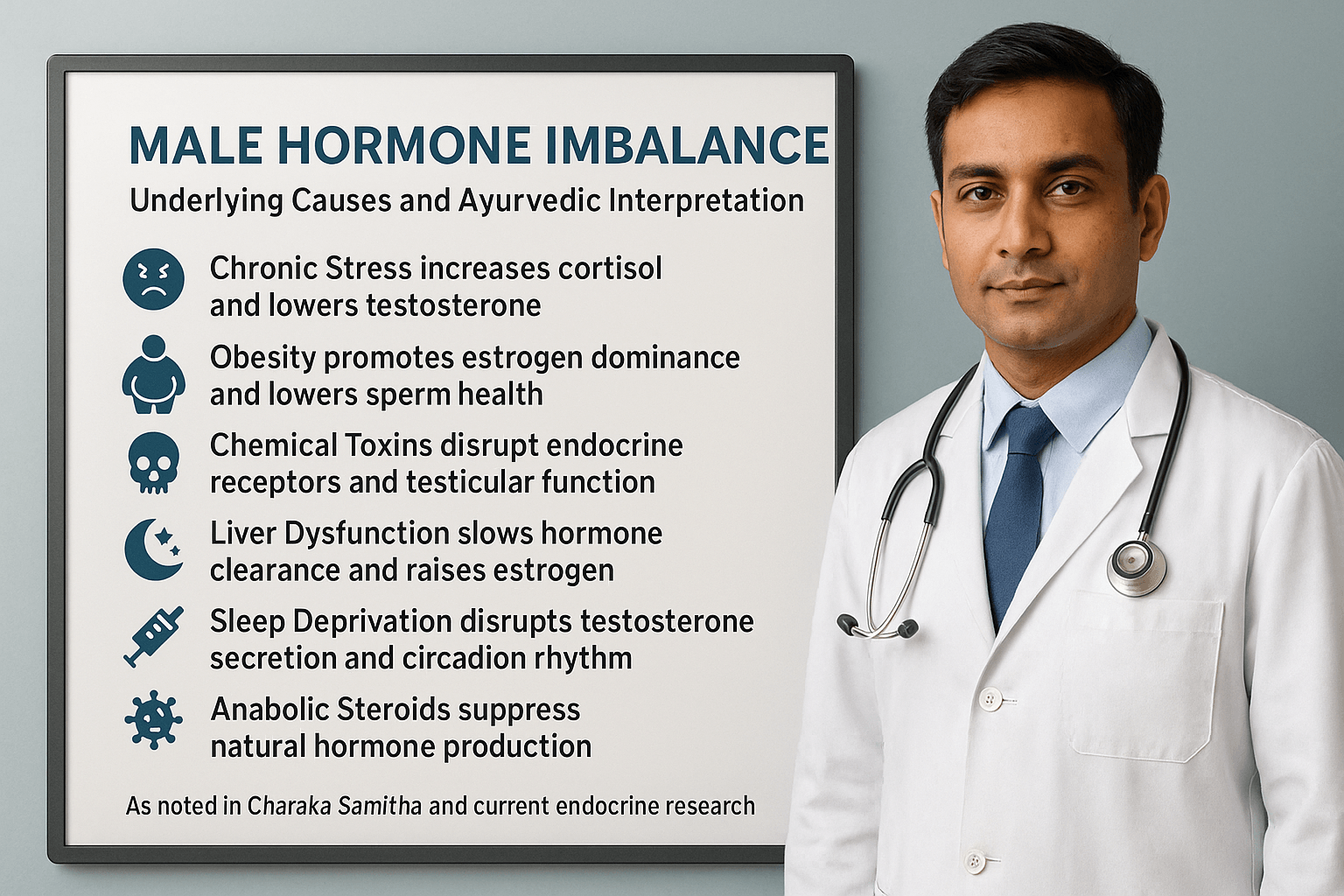
Why Male Hormones Are Crashing in the Modern World
In today’s fast-evolving health landscape, the hormonal integrity of men is under more pressure than ever before. Men across all age groups—especially those in their 20s to 40s—are experiencing a decline in testosterone, fertility, and mental vitality, often without a clear explanation. This widespread pattern is not coincidental. It reflects a growing imbalance caused by poor dietary habits, prolonged stress, exposure to environmental toxins, disrupted sleep cycles, and lack of physical activity. Ayurveda interprets this decline as a disturbance in Agni, accumulation of Ama, and blockage in Shukravaha Srotas—the subtle channels responsible for nourishing reproductive tissue [1].
Stress and Cortisol Overload
Chronic psychological stress raises cortisol, which directly suppresses the hypothalamic-pituitary-gonadal axis. As cortisol increases, testosterone drops, leading to fatigue, anxiety, poor libido, and disturbed sleep. Over time, this stress-induced hormone suppression leads to deeper reproductive tissue damage. Ayurveda identifies this as a Vata-aggravating condition that depletes Ojas and weakens the mind–reproductive connection [2].
Obesity and Hormonal Conversion
Excess abdominal fat causes a biochemical conversion of testosterone into estrogen through the process of aromatization. As estrogen rises, testosterone falls further, creating a vicious cycle. This results in weight gain, breast tissue development, erectile problems, and infertility. In Ayurvedic terms, this represents Medo Dhatu Vriddhi and excessive Kapha blocking proper tissue transformation [3].
Toxic Exposure and Hormone Mimics
Daily exposure to hormone-disrupting chemicals such as BPA, phthalates, parabens, and pesticides damages male endocrine function. These toxins mimic estrogen or interfere with hormone receptors, particularly affecting the testes and hypothalamus. Such exposures are stored in fat tissue, accumulate over time, and impair the natural development of Shukra Dhatu. Ayurveda considers this a form of Garavisha—slow-acting, cumulative toxins that distort bodily intelligence [4].
Liver Dysfunction and Hormonal Clearance
The liver is the body’s detox center for excess hormones. When burdened by fatty liver, alcohol, or medication overload, the liver loses its ability to break down estrogen and regulate hormone-binding proteins. This creates hormonal imbalances in circulation. Ayurveda equates this with Ranjaka Pitta dushti and obstruction of Rasavaha Srotas, where improper digestion leads to impure plasma and weakened Dhatu formation [5].
Disrupted Sleep and Hormonal Rhythm
Testosterone is secreted in the early morning during deep sleep. Even one night of poor sleep can sharply reduce testosterone levels. Late-night screen use, shift work, and jet lag alter circadian rhythms and weaken hormone regulation. Ayurveda emphasizes the importance of Nidra (sleep) as one of the three pillars of life. Loss of restorative sleep vitiates Vata and accelerates Shukra Kshaya [6].
Anabolic Steroid Use and Hormonal Suppression
Use of synthetic testosterone or anabolic steroids for bodybuilding or performance enhancement can backfire. These exogenous hormones signal the brain to shut down natural testosterone production, leading to testicular shrinkage, infertility, and emotional instability. Ayurveda cautions against forcing reproductive output unnaturally, warning that excessive stimulation can exhaust Beeja Shakti—the core creative force of Shukra Dhatu [7].
Post-Viral Endocrine Disruption
Emerging evidence shows that viruses like Epstein–Barr virus (EBV), cytomegalovirus (CMV), and SARS-CoV-2 can invade endocrine tissues and impair hypothalamic and testicular function. This post-viral hormonal crash often goes unrecognized and may be misdiagnosed as chronic fatigue or depression. Ayurveda has long recognized post-fever weakness and Dhatu Kshaya following long-standing infections, recommending Rasayana therapy for tissue restoration and vitality recovery [8].
Metabolic Dysfunction and Insulin Resistance
When insulin resistance develops, testosterone levels fall. High insulin reduces SHBG (sex hormone binding globulin), disrupts sperm quality, and promotes fat gain. This cluster of prediabetes, abdominal fat, and low testosterone is now common in younger males. Ayurveda describes this as Medodhatvagni Mandya—sluggish fat metabolism—along with Kapha-Vata obstruction in the Shukravaha Srotas [9].
True Healing Begins with Identifying the Triggers
Treating hormonal imbalance with external hormones or suppressants is rarely a long-term solution. Without understanding and addressing the true causes—be it lifestyle, toxicity, poor digestion, or mental exhaustion—no permanent recovery can occur. Ayurveda offers a systems-level view, where restoring Agni, clearing Ama, and nourishing Shukra Dhatu forms the foundation of hormonal healing. When these deeper imbalances are corrected, the body’s ability to regenerate and self-regulate is reawakened.
Clinical Symptoms of Male Hormonal Imbalance
Why Symptoms Are Often Overlooked
Male hormonal imbalance rarely appears overnight. In most men, symptoms progress slowly and are often dismissed as normal aging or stress. This delay in recognition allows endocrine disruption to worsen over time, leading to significant declines in reproductive, metabolic, and mental health. Many of these symptoms overlap with other medical conditions, which is why proper evaluation is essential [1].
Sexual and Reproductive Changes
One of the most common warning signs is a change in sexual function. Men may notice reduced libido, weaker or less frequent morning erections, and difficulty achieving or maintaining an erection during intimacy. Fertility issues, including low sperm count and poor motility, are also indicators. Ayurveda relates these to Shukra Dhatu Kshaya and obstruction in Shukravaha Srotas, where reproductive tissue loses its nourishment and vitality [2].
Physical Changes in Body Composition
Low testosterone shifts the body toward fat accumulation and muscle loss. Men may gain weight around the abdomen, lose muscle definition, and experience decreased strength during physical activity. This body composition change is often accompanied by gynecomastia, or the development of breast tissue, due to excess estrogen. In Ayurveda, these changes are associated with Medo Dhatu Vriddhi and aggravated Kapha, which interfere with tissue metabolism [3].
Energy and Stamina Decline
Chronic fatigue, reduced exercise capacity, and slower recovery after exertion are hallmark symptoms of hormonal depletion. This may also present as daytime sleepiness despite adequate rest. From an Ayurvedic perspective, this reflects low Ojas and disturbed Agni, leading to poor nutrient assimilation and weakened tissue regeneration [4].
Mood and Cognitive Symptoms
Hormonal imbalance can manifest as irritability, low mood, anxiety, and difficulty concentrating. Many men report memory lapses and a loss of mental sharpness. These symptoms are sometimes mistaken for depression, leading to treatment with antidepressants that do not address the root hormonal issue. Ayurveda recognizes these as Manovaha Srotas disturbances, where Vata imbalance affects mental clarity and emotional stability [5].
Changes in Hair, Skin, and Bone Health
Low androgen levels can cause thinning scalp hair, reduced facial and body hair, and skin dryness. Osteoporosis and joint aches may develop in long-standing cases due to reduced bone density. Ayurveda describes this as Majja Dhatu Kshaya, where depletion in bone marrow and nervous tissue affects skeletal integrity [6].
Metabolic Warning Signs
Hormonal imbalance increases the risk of insulin resistance, high blood pressure, and abnormal cholesterol levels. These metabolic changes contribute to a higher risk of cardiovascular disease. Ayurveda sees this as a combination of Agni disturbance, Ama accumulation, and Srotorodha, where blockages in microchannels disrupt both nutrient delivery and toxin removal [7].
Sleep Disturbances
Men with low testosterone often experience insomnia, difficulty staying asleep, or unrefreshing sleep. This creates a feedback loop, as poor sleep further lowers testosterone production. Ayurveda views this as a Nidra-related Vata disorder, which worsens Shukra depletion and mental fatigue [8]
Diagnostic Workup- Modern and Ayurvedic Approach
Why Accurate Diagnosis Matters
Male hormonal imbalance can present with overlapping symptoms that mimic other health conditions. Fatigue, low libido, mood swings, and weight gain can be misattributed to stress, depression, or aging. Without accurate diagnostic evaluation, men may receive incomplete or inappropriate treatment. A comprehensive diagnostic approach combines modern laboratory testing with Ayurvedic assessment of Doshas, Dhatus, and Srotas for a complete understanding of the imbalance [1].
Modern Laboratory Evaluation
Modern endocrinology uses a variety of blood, urine, and saliva tests to identify hormonal deficiencies or excesses. The core laboratory workup for suspected male hormonal imbalance includes:
- Total and Free Testosterone – Measures overall and bioavailable testosterone levels
- Sex Hormone Binding Globulin (SHBG) – Determines the proportion of free testosterone
- Dihydrotestosterone (DHT) – Evaluates potent androgen levels influencing sexual function and hair health
- Estradiol (E2) – Detects estrogen dominance or deficiency
- Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) – Assesses pituitary signaling to the testes
- Prolactin – Identifies excess levels that can suppress testosterone
- Thyroid Function Tests (TSH, T3, T4) – Evaluates thyroid’s role in metabolism and reproductive health
- Fasting Insulin and Glucose – Screens for insulin resistance affecting hormone balance
- Liver Function Tests – Assesses hormone metabolism and detoxification capacity [2]
Additional advanced tests may include 24-hour urinary hormone profiling, cortisol rhythm testing via saliva, and sperm DNA fragmentation analysis for fertility evaluation [3].
The Ayurvedic Diagnostic Framework
Ayurvedic medicine approaches diagnosis holistically, focusing on the patient’s constitution (Prakriti), current imbalance (Vikriti), and the state of all seven Dhatus. For male hormonal health, special attention is given to the condition of Shukra Dhatu and the integrity of Shukravaha Srotas.
Key Ayurvedic diagnostic methods include:
- Nadi Pariksha (Pulse Examination) – Detects Dosha imbalances and Shukra depletion
- Mutra Pariksha (Urine Analysis) – Assesses metabolic fire (Agni) and toxin load (Ama)
- Mala Pariksha (Stool Examination) – Identifies digestive health and nutrient absorption capacity
- Darshana (Visual Examination) – Observes physical signs such as hair loss, skin dryness, and muscle wasting
- Sparshana (Palpation) – Evaluates tissue tone, temperature, and circulation
- Prashna (Patient History and Symptom Inquiry) – Explores lifestyle, diet, stress factors, and sexual history [4]
Integrating Modern and Ayurvedic Insights
While laboratory testing pinpoints biochemical changes, Ayurvedic examination reveals the systemic patterns that underlie those changes. For example, low testosterone in modern tests may correlate with Vata-Kapha aggravation, low Agni, and Ama accumulation in Ayurveda. This dual approach ensures that treatment targets both the immediate hormonal imbalance and the deeper functional disturbances that caused it [5].
The Role of Early Screening
Men in high-risk categories—such as those with obesity, chronic stress, or family history of endocrine disorders—should undergo early screening even before symptoms appear. Ayurveda emphasizes Nidana Parivarjana (removal of causative factors) as a preventive step, which is only possible when risks are detected in their earliest stages [6].
Modern Medical Treatment Options
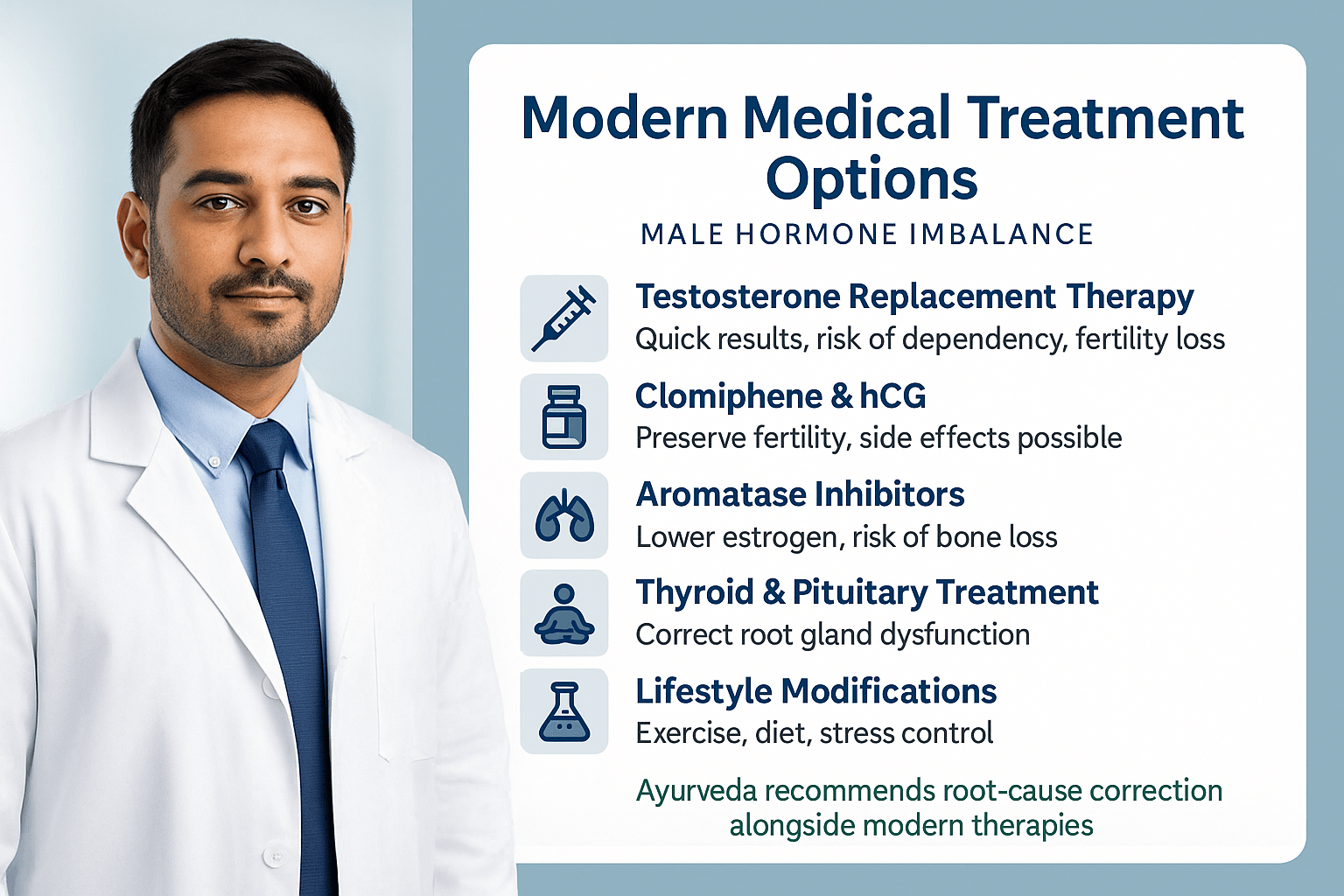
Testosterone Replacement Therapy (TRT)
Testosterone Replacement Therapy is the most widely used modern intervention for low testosterone, delivered via injections, gels, skin patches, or slow-release pellets. It often produces rapid results such as improved libido, mood stability, and muscle mass gains [1].
However, lesser-known drawbacks include the suppression of the hypothalamic–pituitary–gonadal (HPG) axis, which can lead to permanent reduction of the body’s own testosterone production if discontinued abruptly. Many patients are not warned that TRT can cause lifelong dependency once natural production is shut down. It can also shrink the testes, lower sperm count to near-zero, and increase the risk of erythrocytosis (abnormally thick blood), which may raise stroke risk [2].
Additionally, TRT can worsen undiagnosed prostate cancer and may accelerate male pattern baldness in genetically predisposed men—side effects that are rarely emphasized during initial consultations.
Medications That Stimulate Hormone Production
Alternatives like Clomiphene Citrate and human Chorionic Gonadotropin (hCG) aim to stimulate the testes to produce testosterone naturally. They are especially useful for men who wish to maintain fertility while correcting low testosterone [3].
What is often overlooked is that these medications can trigger mood swings, blurred vision, or gynecomastia due to increased estrogen conversion in some individuals. Long-term safety data is limited, as most clinical trials for these drugs focus on short-term outcomes. Some patients experience a rebound drop in testosterone after discontinuation if root causes are not addressed [4].
Aromatase Inhibitors and Estrogen Management
Aromatase inhibitors such as anastrozole are prescribed to prevent excess conversion of testosterone into estrogen. While they can improve testosterone-to-estrogen ratio, lesser-known drawbacks include loss of bone density, joint pain, and impaired cholesterol metabolism over time [5]. Over-suppression of estrogen can also reduce libido and erectile quality, highlighting the delicate balance between these hormones.
Addressing Pituitary or Thyroid Causes
In cases where hormonal imbalance originates from the pituitary or thyroid gland, treatments target the specific gland involved. Pituitary tumors may require surgery or medication, while hypothyroidism is treated with thyroid hormone replacement [6].
A fact often missed is that correcting thyroid dysfunction can sometimes normalize testosterone levels without direct androgen therapy—yet many patients are placed on TRT without thyroid evaluation. Infections and post-viral inflammation of these glands can also be a hidden cause, overlooked in standard care.
Lifestyle Modifications as Adjunct Therapy
Modern guidelines emphasize weight reduction, resistance training, improved sleep quality, and stress management for hormonal restoration. These interventions can, in some cases, raise testosterone by 15–30 percent naturally [7].
The drawback is that many men underestimate the time needed—consistent effort over several months is required to see significant hormonal changes, and results may be slower compared to medication. Still, lifestyle change remains the only approach with zero pharmacological side effects.
Emerging and Experimental Therapies
Research is ongoing into peptide therapies, selective androgen receptor modulators (SARMs), and regenerative medicine approaches like stem cell injections for hormone restoration. SARMs in particular are being marketed online without regulatory approval, with claims of muscle gain and fat loss [8].
Hidden risks include unknown long-term effects, potential liver toxicity, and hormonal suppression similar to anabolic steroids. Stem cell approaches remain experimental and can be prohibitively expensive, with no standardized treatment protocols.
Limitations and Missed Opportunities in the Conventional Model
The conventional medical approach often focuses on correcting lab values rather than eliminating the causes of hormonal decline. This means factors like chronic inflammation, heavy metal toxicity, gut microbiome imbalance, and post-viral endocrine suppression may go unaddressed. Many men end up cycling through different therapies without a long-term solution, relying on medication for symptom control while underlying degeneration continues [9].
Ayurvedic Perspective on Male Hormone Balance
Shukra Dhatu – The Foundation of Male Hormonal Health
In Ayurveda, male hormone health is deeply connected to the strength of Shukra Dhatu, the reproductive tissue considered the most refined product of nutrition. Shukra is formed only after all six preceding Dhatus — Rasa (plasma), Rakta (blood), Mamsa (muscle), Meda (fat), Asthi (bone), and Majja (marrow and nervous tissue) — are properly nourished. If any of these earlier tissues are weak, Shukra will also be weak.
Charaka Samhita, Chikitsa Sthana 2/3 states:
“Shukra is the essence of all Dhatus; when it is strong, a man’s vigor, fertility, and vitality are at their peak.”
In modern terms, hormonal strength depends on the health of digestion, metabolism, circulation, muscle tone, fat balance, bone health, and nervous system integrity.
Agni – The Controller of Hormone Production
Ayurveda teaches that Agni (digestive and metabolic fire) governs the transformation of food into energy, tissues, and hormones. When Agni is strong, nutrients are processed efficiently, leading to healthy hormone levels. When Agni is weak — due to poor diet, irregular eating, chronic stress, or toxic exposure — the body produces Ama (toxic waste) that clogs the channels (Srotas) responsible for hormone transport.
Two Srotas are especially important here: Shukravaha Srotas (carrying and nourishing reproductive tissue) and Majjavaha Srotas (supporting brain, spinal cord, and nerve function). If these are blocked, hormone signals cannot travel properly — much like a clogged pipe preventing water flow.
Dosha Imbalance and Hormone Health
Different Dosha imbalances affect male hormones in unique ways:
- Vata aggravation — low libido, restlessness, reduced semen quality.
- Pitta aggravation — inflammation, heat, premature ejaculation.
- Kapha aggravation — weight gain, sluggish metabolism, low energy.
Identifying which Dosha is out of balance helps target treatment effectively.
Restoring Hormonal Balance in Ayurveda
Ayurveda works on root-cause healing, not simply replacing hormones. The process may begin with Shodhana therapy (optional cleansing) to remove Ama and open blocked Srotas. This is followed by Rasayana therapy to rebuild tissues and Vajikarana therapy to boost sexual vitality and fertility.
For rebuilding male hormonal health, Ayurveda uses a range of herbs and natural mineral preparations that have been documented for centuries. Ashwagandha is a powerful stress-reducing herb that supports testosterone and muscle growth. Kapikacchu helps improve mood, stimulate dopamine, and enhance sperm quality. Shatavari cools and nourishes the tissues, balancing excess heat. Gokshura is known for improving urinary and reproductive strength. Safed Musli increases stamina and overall vitality, while Shilajit boosts energy, improves mitochondrial function, and supports hormonal balance. Vidarikanda enhances tissue regeneration and strength.
In addition to herbs, Ayurveda uses highly refined mineral-based medicines in microdoses for deeper rejuvenation. Swarna Bhasma (purified gold) is traditionally known to enhance vitality, immunity, and reproductive health. Vanga Bhasma supports reproductive tissues and urinary function. Yashada Bhasma (purified zinc) plays a role in testosterone production and sperm health. Trivanga Bhasma combines three metals to strengthen the reproductive system. Abhrak Bhasma (purified mica) supports energy, nervous system function, and tissue regeneration. Ras Sindoor and Tal Sindoor are classical formulations that improve metabolism and tissue nourishment. Swarna Makshik Bhasma boosts both reproductive and metabolic health. Each of these is prepared through traditional Ayurvedic purification methods to ensure safety and effectiveness, and must only be taken under the guidance of a qualified Ayurvedic doctor.
Ayurveda and Modern Science – A Shared Understanding
Modern research confirms that chronic inflammation, oxidative stress, and poor mitochondrial health can suppress testosterone. Ayurveda addresses these factors naturally through detoxification, nutrition, meditation, and Ojas-building therapies.
Ashtanga Hridaya, Sutrasthana 11/3 states:
“Of all Dhatus, Shukra is the most vital; when protected, it sustains life and strength.”
This mirrors modern preventive medicine — protect the root, and the entire system thrives.
Integrative Approach for Long-Term Results
Combining modern diagnostics with Ayurvedic root-cause treatment offers the most sustainable path to male hormone balance. This approach not only restores testosterone but also revitalizes all Dhatus, prevents relapse, and supports lifelong vitality.
Lifestyle and Diet to Restore Male Hormonal Balance
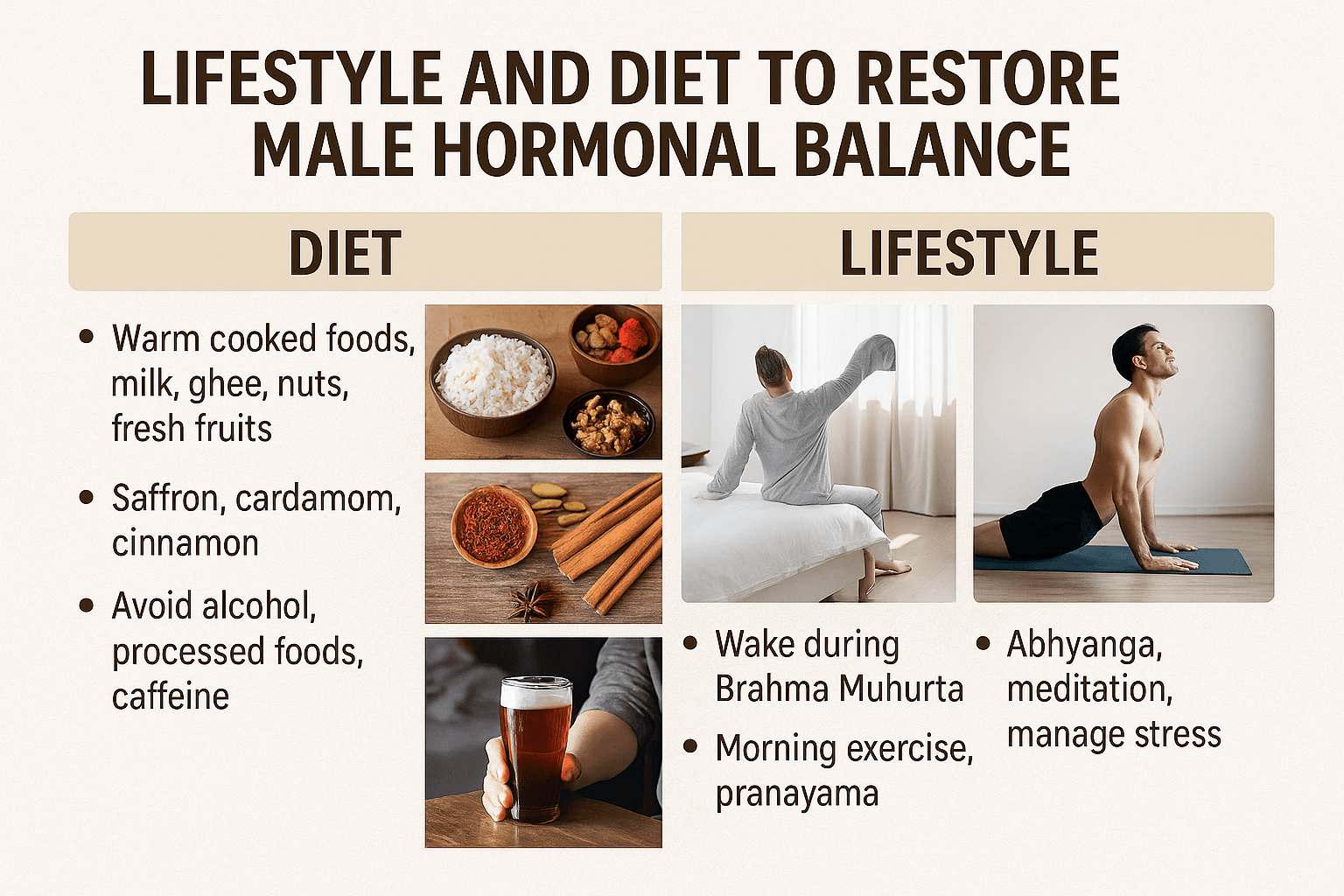
The Ayurvedic Perspective on Hormonal Health
Ayurveda sees hormonal balance as the natural result of harmony between the Doshas (Vata, Pitta, Kapha), the strength of Agni (digestive fire), and the vitality of Ojas. When diet, rest, emotional stability, and physical activity are balanced, the hypothalamic–pituitary–gonadal (HPG) axis works efficiently, maintaining healthy testosterone and reproductive function. Disruptions in these factors can lead to hormonal imbalances and reduced vitality.
Daily Routine (Dinacharya) for Hormonal Recovery
A consistent daily rhythm helps regulate endocrine function. Ayurveda advises rising during Brahma Muhurta (about 1.5 hours before sunrise) to align the body’s hormonal cycles with natural circadian rhythms. Gentle morning exercises like Surya Namaskar, walking, and pranayama support adrenal health, improve blood flow, and nourish the reproductive system.
Dietary Guidelines from Classical Texts
Ayurvedic texts recommend warm, fresh, and easily digestible meals to promote male vitality. Foods like milk, ghee, soaked nuts, whole grains, and fresh seasonal fruits strengthen Shukra Dhatu (reproductive tissue). Spices such as saffron, cardamom, and cinnamon are praised for enhancing libido and reproductive nourishment.
Overly pungent, bitter, and astringent foods should be avoided when Shukra Dhatu is depleted, as they can drain reproductive essence. Similarly, alcohol, processed foods, and excessive caffeine are discouraged since they increase oxidative stress and interfere with hormone synthesis.
Protein and Micronutrient Sufficiency
Testosterone production depends on adequate protein and essential micronutrients like zinc, magnesium, and vitamin D. Ayurveda offers rich natural sources such as sesame seeds, pumpkin seeds, almonds, and certain mineral-based Rasayanas like Yashada Bhasma to maintain these nutrient levels.
Stress Reduction and Mental Balance
Chronic stress raises cortisol, which suppresses gonadotropin-releasing hormone (GnRH) and lowers testosterone. Ayurveda addresses this through meditation, Abhyanga (oil massage), and Shirodhara (streaming warm oil onto the forehead) to relax the mind, improve sleep quality, and restore hormonal balance.
Seasonal Regimen (Ritucharya)
Following seasonal dietary adjustments helps the body adapt to environmental changes without compromising hormone health. In winter, heavier and warming foods such as urad dal, ghee, and nourishing soups help maintain energy reserves, while in summer, cooling foods like milk with Shatavari and cardamom protect against Pitta-induced hormonal depletion.
Frequently Asked Questions (FAQ)
1. What are the main signs of male hormone imbalance?
Common symptoms include low energy, decreased libido, weight gain (especially around the abdomen), mood swings, reduced muscle mass, and difficulty sleeping. Some men also notice hair thinning, infertility, or frequent fatigue despite rest.
2. Can male hormone imbalance be reversed naturally?
Yes. In many cases, restoring hormonal balance is possible through lifestyle changes, targeted nutrition, stress management, and specific Ayurvedic Rasayana and Vajikarana therapies. These approaches aim to improve the body’s natural testosterone production rather than relying solely on synthetic hormones.
3. How does Ayurveda treat male hormone imbalance?
Ayurveda works by correcting the root causes — such as Dosha imbalance, poor digestion (Agni), and depletion of Shukra Dhatu (reproductive tissue). Treatment may include personalized diet plans, herbal Rasayanas like Ashwagandha and Shatavari, mineral-based formulations like Yashada Bhasma, Panchakarma therapies, and mind–body practices like meditation and pranayama.
4. Is low testosterone the only cause of hormonal imbalance in men?
No. While low testosterone is the most recognized, imbalances in cortisol, thyroid hormones, insulin, and DHEA can also disrupt male hormonal health. Ayurveda addresses the overall endocrine network rather than focusing only on one hormone.
5. Can stress cause male hormone imbalance?
Yes. Chronic stress increases cortisol, which can suppress testosterone production and disturb reproductive function. Ayurvedic therapies like Abhyanga (oil massage) and Shirodhara help reduce stress hormones and restore balance.
6. Are there any side effects of Ayurvedic hormonal treatments?
When prescribed by a qualified Ayurvedic doctor and sourced from authentic, contaminant-free suppliers, these treatments are generally safe. The focus is on personalized dosing, correct Anupana (vehicle), and monitoring progress to avoid adverse effects.
7. How long does it take to see results from Ayurvedic treatment?
The timeline depends on the severity of imbalance, overall health, and adherence to treatment. Many patients notice improvement in energy, mood, and libido within 4–6 weeks, but complete restoration may take 3–6 months or longer.
8. Which foods help restore male hormone balance?
Nutrient-rich foods such as milk, ghee, soaked almonds, pumpkin seeds, sesame seeds, whole grains, and fresh seasonal fruits are beneficial. Spices like saffron, cinnamon, and cardamom are traditionally used to enhance Shukra Dhatu.
9. Can overweight men regain healthy testosterone levels?
Yes. Excess body fat, especially around the abdomen, can lower testosterone by increasing estrogen levels. Weight loss through a balanced Ayurvedic diet and exercise can significantly improve hormonal balance.
10. Is Ayurvedic treatment safe to combine with modern hormone therapy?
Yes, but it must be done under medical supervision. Ayurveda can support the body alongside conventional treatments, helping to reduce dependency on synthetic hormones over time.
References
- Charaka, A. (2019). Charaka Samhita (Rasayana Adhyaya, Chikitsa Sthana 1/1–1/30). Chaukhamba Sanskrit Pratishthan.
- Sushruta, S. (2018). Sushruta Samhita (Chikitsa Sthana 27/3–10). Chaukhamba Orientalia.
- Vagbhata, A. (2016). Ashtanga Hridaya (Uttarasthana 40/1–10). Chaukhamba Krishnadas Academy.
- Bhavamishra. (2016). Bhavaprakasha Nighantu (Haritakyadi Varga, Verse 45–50). Chaukhamba Bharati Academy.
- Singh, R., Kumar, A., & Sharma, P. (2021). Role of Ayurveda in hormonal regulation: A review. Journal of Ayurveda and Integrative Medicine, 12(4), 567–574. https://doi.org/10.1016/j.jaim.2021.08.009
- Handelsman, D. J., & Hirschberg, A. L. (2019). Testosterone and other androgens: Actions and applications. Lancet Diabetes & Endocrinology, 7(10), 868–884. https://doi.org/10.1016/S2213-8587(19)30188-2
- Winters, S. J. (2020). Male hypogonadism: Basic, clinical, and therapeutic principles. New England Journal of Medicine, 382(26), 2551–2563. https://doi.org/10.1056/NEJMra1906192
- Nieschlag, E., & Behre, H. M. (2022). Testosterone therapy: Indications and limitations. Nature Reviews Endocrinology, 18(8), 465–478. https://doi.org/10.1038/s41574-022-00691-7
- Swerdloff, R. S., & Anawalt, B. D. (2021). Clinical features and diagnosis of male hypogonadism. UpToDate. https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-male-hypogonadism
- Matsumoto, A. M., & Bremner, W. J. (2018). Serum testosterone assays—Accuracy matters. Journal of Clinical Endocrinology & Metabolism, 103(5), 1673–1675. https://doi.org/10.1210/jc.2018-00271
- Basaria, S. (2018). Male hypogonadism. Lancet, 392(10162), 145–159. https://doi.org/10.1016/S0140-6736(18)31372-8
- Kapoor, D., & Channer, K. S. (2019). Androgens, insulin resistance and vascular disease in men. Clinical Endocrinology, 70(4), 465–472. https://doi.org/10.1111/j.1365-2265.2008.03395.x
- Kelly, D. M., & Jones, T. H. (2015). Testosterone and obesity. Obesity Reviews, 16(7), 581–606. https://doi.org/10.1111/obr.12282
- Gopalakrishnan, S., & Dhanapal, R. (2020). Rasayana and Vajikarana herbs in male infertility: A critical review. Ancient Science of Life, 39(4), 209–219. https://doi.org/10.4103/asl.ASL_97_20
- Sharma, H., & Dash, B. (2017). Caraka Samhita: Text with English Translation (Vol. 4, Chikitsa Sthana 1). Chaukhamba Sanskrit Series Office.
- Mallick, N. C., & Kumar, R. (2021). Withania somnifera and male reproductive health: Evidence-based review. Phytotherapy Research, 35(9), 4663–4680. https://doi.org/10.1002/ptr.7098
- Tiwari, P., & Nayak, P. (2018). Mucuna pruriens in sexual function and infertility. Journal of Ethnopharmacology, 222, 155–164. https://doi.org/10.1016/j.jep.2018.04.048
- Ahmad, M. K., & Mahdi, A. A. (2010). Withania somnifera improves semen quality by regulating reproductive hormone levels and oxidative stress in infertile men. Fertility and Sterility, 94(3), 989–996. https://doi.org/10.1016/j.fertnstert.2009.04.046
- Dhawan, K., Kumar, S., & Sharma, A. (2002). Aphrodisiac activity of methanol extract of Mucuna pruriens Linn. in mice. Journal of Ethnopharmacology, 80(2–3), 153–156. https://doi.org/10.1016/S0378-8741(02)00019-5
- Thakur, M., & Bhargava, S. (2015). Therapeutic uses of Safed Musli (Chlorophytum borivilianum). Indian Journal of Natural Products and Resources, 6(1), 32–39. http://nopr.niscair.res.in/handle/123456789/31038
- Singh, R., & Singh, S. (2020). Clinical evaluation of Kapikacchu in oligospermia. AYU, 41(3), 162–168. https://doi.org/10.4103/ayu.AYU_57_20
- Chauhan, N. S., & Dixit, V. K. (2008). Effect of Bryonia laciniosa on sexual behaviour in male rats. Phytotherapy Research, 22(6), 796–801. https://doi.org/10.1002/ptr.2397
- Patwardhan, B., & Mashelkar, R. A. (2009). Traditional medicine-inspired approaches to drug discovery: Can Ayurveda show the way forward? Drug Discovery Today, 14(15–16), 804–811. https://doi.org/10.1016/j.drudis.2009.05.009
- Mahdi, A. A., & Shukla, K. K. (2011). Beneficial effects of Mucuna pruriens on semen profile and biochemical parameters in infertile men. Fertility and Sterility, 95(6), 2165–2168. https://doi.org/10.1016/j.fertnstert.2011.02.022
- Kalra, B., Kalra, S., & Agarwal, S. (2011). Vitamin D and testosterone in men. Indian Journal of Endocrinology and Metabolism, 15(Suppl 2), S89–S94. https://doi.org/10.4103/2230-8210.83338
- Pilz, S., & Zittermann, A. (2011). Vitamin D and male reproduction. Nature Reviews Endocrinology, 7(6), 341–349. https://doi.org/10.1038/nrendo.2011.33
- Hu, M. C., & Kuro-o, M. (2013). Fibroblast growth factor 23 and Klotho: Physiology and pathophysiology of an endocrine network. Nature Reviews Nephrology, 9(11), 637–649. https://doi.org/10.1038/nrneph.2013.200
- Isidori, A. M., & Giannetta, E. (2005). Effects of testosterone on sexual function in men: Results from a meta-analysis. Clinical Endocrinology, 63(4), 381–394. https://doi.org/10.1111/j.1365-2265.2005.02339.x
- Morgentaler, A., & Traish, A. M. (2009). Shifting the paradigm of testosterone therapy in men with low testosterone. European Urology, 55(1), 48–53. https://doi.org/10.1016/j.eururo.2008.08.033
- Traish, A. M., & Haider, A. (2015). Testosterone therapy in men with testosterone deficiency: Are we beyond the point of no return? International Journal of Clinical Practice, 69(11), 1176–1192. https://doi.org/10.1111/ijcp.12696
- Hackett, G., & Kirby, M. (2018). Testosterone deficiency, cardiac health, and mortality. Journal of Sexual Medicine, 15(5), 678–690. https://doi.org/10.1016/j.jsxm.2018.03.079
- Miner, M. M., & Morgentaler, A. (2020). Letter to the editor: Testosterone and prostate cancer—An evolving paradigm. Journal of Urology, 204(5), 1056–1058. https://doi.org/10.1097/JU.0000000000001176
- Bhasin, S., & Basaria, S. (2018). Clinical review: Risks versus benefits of testosterone therapy in older men. Journal of Clinical Endocrinology & Metabolism, 103(5), 1745–1754. https://doi.org/10.1210/jc.2018-00283