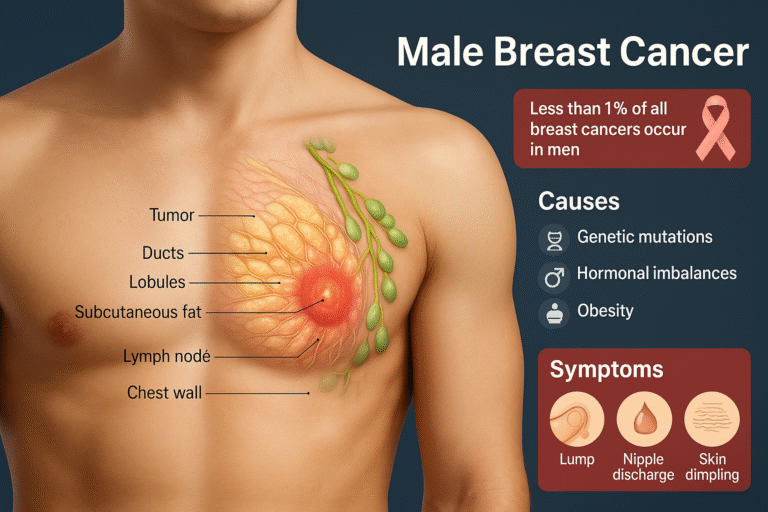
- Causes
- Genetic Mutations
- Chromosomal Disorders
- Environmental and Lifestyle Factors
- Ayurvedic Perspective
- Risk Factors
- Symptoms
- Painless Lump Beneath the Nipple or Areola
- Diagnosis
- Staging and Classification
- Invasive Ductal Carcinoma (Most Common in Men)
- Ductal Carcinoma In Situ (DCIS)
- Treatment
- Immunotherapy-Checkpoint Inhibitors
- Ayurvedic Integration in Male Breast Cancer Treatment
- Prevention & Awareness
- Frequently Asked Questions (FAQs)
- References
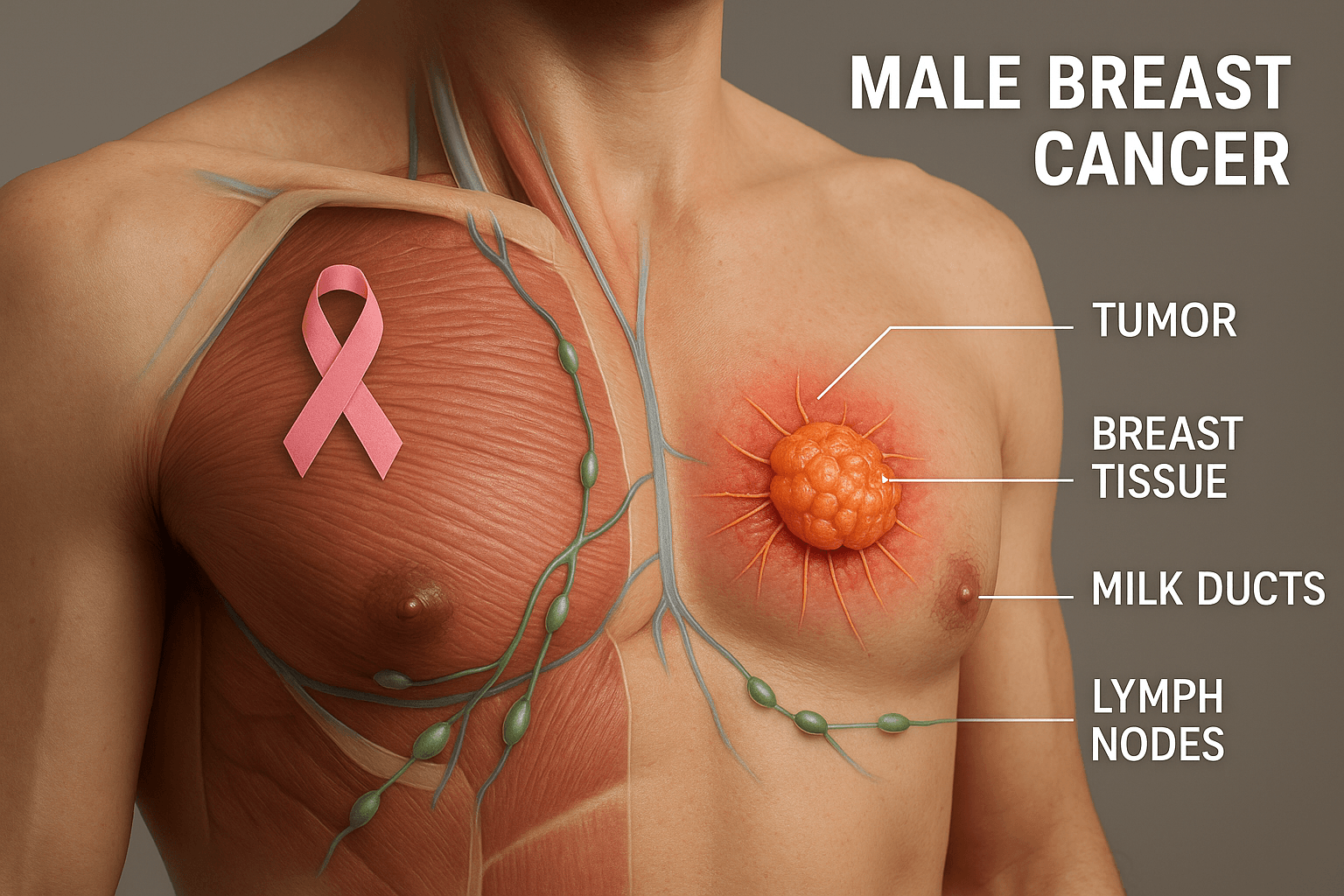
Male breast cancer is a rare but serious condition in which malignant cells develop in the breast tissue of men [1]. Although men have a much smaller amount of breast tissue compared to women, they still possess ducts, lobules, and fatty tissue where cancer can arise [2]. Because of its rarity and the lack of widespread awareness, male breast cancer is often diagnosed at a more advanced stage than female breast cancer [3].
In comparison, breast cancer in women is far more common, making up the majority of global cases, while male breast cancer accounts for less than 1% of all breast cancers worldwide [4]. Despite this small percentage, the biological behavior, treatment strategies, and potential outcomes in men are largely similar to those in women [5]. However, unique challenges exist, such as delayed diagnosis due to social stigma, limited screening programs for men, and lack of awareness among both patients and healthcare professionals [6].
The global incidence of male breast cancer has shown a slight increase in recent years, attributed to better diagnostic capabilities and increased reporting [7]. This emphasizes the importance of awareness, early detection, and timely intervention. Recognizing the symptoms early—such as a painless lump near the nipple, changes in skin texture, or nipple discharge—can drastically improve prognosis and survival rates [8].
Awareness not only reduces stigma but also encourages men at risk, especially those with family history or genetic mutations, to seek medical evaluation sooner [9]. By educating the public about this condition, healthcare providers and integrative systems such as Ayurveda can play a significant role in promoting early diagnosis, timely treatment, and holistic survivorship strategies [10].
Causes
The development of male breast cancer is not the result of a single trigger but arises from multiple interacting causes. These can be broadly understood under genetics, hormonal factors, chromosomal disorders, environmental and lifestyle influences, and traditional Ayurvedic perspectives. Expanding each of these helps patients, caregivers, and practitioners see the bigger picture of why this condition occurs and how awareness can reduce risk.
Genetic Mutations
One of the strongest predictors of male breast cancer is the presence of inherited genetic mutations [11]. Among these, BRCA1 and BRCA2 mutations are the most well-established. Men carrying these faulty genes have a dramatically higher lifetime risk compared to the general male population. BRCA2, in particular, has a closer association with male breast cancer than BRCA1, but both disrupt the DNA repair process, allowing harmful mutations to accumulate. In addition to BRCA mutations, other tumor suppressor genes such as p53 and PTEN play important roles. When these genes are damaged, they fail to regulate cell division and apoptosis, leading to uncontrolled proliferation of breast tissue cells.
Importantly, genetic mutations not only predispose an individual to breast cancer but may also influence how aggressive the disease becomes and how well it responds to treatment. For instance, men with BRCA2 mutations often present with hormone receptor–positive cancers, making hormone therapy an effective option, but they may also face increased risks of other cancers, such as prostate and pancreatic cancer. Genetic counseling and testing have therefore become crucial tools for identifying high-risk men, allowing for early surveillance and informed lifestyle changes.
From a preventive standpoint, knowledge of inherited mutations empowers families to undergo regular checkups, avoid modifiable risk factors, and adopt integrative measures, including Ayurveda’s emphasis on balancing metabolism and strengthening immunity, which can complement modern surveillance strategies [12].
Hormonal Imbalance
Hormonal imbalance is another critical factor in the development of male breast cancer [13]. Unlike women, men produce only small amounts of estrogen, while testosterone remains the dominant hormone. However, when this natural balance shifts—either due to increased estrogen or decreased androgen—the risk of breast tissue changes increases. Conditions such as obesity, liver disease, and chronic alcohol use are known to elevate estrogen levels in men, creating a hormonal environment that fosters malignant transformation.
Estrogen stimulates the growth of breast ducts and lobules, and prolonged exposure can trigger DNA damage and abnormal cell growth. Meanwhile, reduced testosterone levels fail to counteract this effect, leaving breast tissue more vulnerable. Certain medications, such as hormone treatments for prostate cancer, can also increase circulating estrogen, further enhancing the risk.
Clinically, men with high estrogen levels may notice physical changes such as gynecomastia (enlarged breast tissue), infertility, or decreased libido long before cancer develops. These symptoms act as red flags, signaling the need for medical evaluation. Early intervention can help detect abnormalities before they progress into cancer.
Ayurveda interprets hormonal imbalance as Agni Mandya, or impaired metabolic fire. When digestion and metabolism are weak, toxins (Ama) accumulate and disturb the equilibrium of Doshas, particularly leading to Meda Dhatu Dushti (disorders of fat tissue). This not only predisposes individuals to obesity but also affects hormonal stability, echoing modern observations of increased estrogen in overweight men. Thus, both modern medicine and Ayurveda point to the importance of balanced metabolism, detoxification, and lifestyle regulation in reducing hormonal risks for male breast cancer [14].
Chromosomal Disorders
Among the rare but significant causes of male breast cancer, chromosomal disorders play an important role. The most well-documented example is Klinefelter syndrome, a condition where men are born with an extra X chromosome (47,XXY instead of the typical 46,XY) [15]. This genetic variation results in reduced testosterone production and elevated estrogen levels, creating a hormonal imbalance that resembles the female hormonal profile more closely than the male one.
Men with Klinefelter syndrome often present with small testes, infertility, gynecomastia, and tall stature. These features not only affect reproductive health but also increase the risk of breast malignancies. Studies suggest that men with Klinefelter syndrome have a 20- to 50-fold higher risk of developing breast cancer compared to men without the condition.
The reason lies in the prolonged exposure of breast tissue to estrogen coupled with reduced androgen protection. Additionally, immune dysregulation and metabolic abnormalities commonly associated with Klinefelter syndrome may further promote cancer development. Unfortunately, awareness of this risk remains low, and many men with the condition are not routinely screened for breast changes.
From an Ayurvedic lens, chromosomal abnormalities can be understood under the concept of Beejadosha, or defects in the reproductive seed. Classical texts describe how imbalances in parental health, exposure to toxins, or improper regimen before conception can lead to structural or functional abnormalities in offspring. While Ayurveda did not describe chromosomes in the modern sense, its principle of inherited vulnerabilities aligns closely with modern genetic science. For men with Klinefelter syndrome, Ayurvedic interventions may emphasize preconception health, strengthening of reproductive tissues, and long-term Rasayana therapy to improve vitality and immunity [16].
Environmental and Lifestyle Factors
Beyond genes and chromosomes, everyday choices and exposures play a major role in male breast cancer. Lifestyle factors such as obesity, alcohol consumption, and tobacco use are linked to higher risk [17]. Obesity, in particular, is strongly correlated with elevated estrogen levels, since fat tissue actively converts androgens into estrogens through a process called aromatization. This means that overweight and obese men live in a state of continuous estrogen stimulation, predisposing breast tissue to abnormal growth.
Alcohol adds another layer of risk. Chronic intake impairs liver function, reducing the liver’s ability to metabolize estrogen, which further raises circulating levels. Radiation exposure, whether from prior chest treatments for conditions like lymphoma or accidental exposure, is another established cause of male breast cancer. Radiation damages DNA directly, creating mutations that, over time, may turn into cancer.
Unhealthy dietary habits, sedentary lifestyle, and chronic stress indirectly contribute by weakening immunity and metabolism. Ayurveda would call this Agni Mandya combined with Meda Dhatu Dushti—a disruption of digestive fire and fat tissue metabolism. Over time, this creates an internal environment conducive to Ama (toxic by-products), which accumulates in vulnerable tissues such as the breast and blood (Rakta Dushti).
The positive side of lifestyle causes is that they are modifiable. Weight control, balanced nutrition, physical activity, and reduced alcohol intake significantly lower the risk of male breast cancer. From an Ayurvedic perspective, adopting a Satvic diet, practicing regular yoga and pranayama, and seasonal detox therapies (Shodhana) strengthen the immune system and keep Doshas balanced. This holistic prevention strategy aligns modern science with traditional wisdom, highlighting that proactive choices can reduce risk even in genetically predisposed individuals [18].
Ayurvedic Perspective
Ayurveda provides a unique lens through which the causes of male breast cancer can be interpreted. The classical concept of Beejadosha refers to defects in the reproductive seed (sperm or ovum), which corresponds to inherited genetic mutations in modern terms [19]. Such defects can predispose individuals to serious illnesses, including cancer.
Another relevant concept is Agni Mandya, or impaired metabolic fire. When digestion and metabolism are weak, toxins (Ama) accumulate in the body and disturb the equilibrium of the Doshas. Over time, this leads to systemic vulnerability and opens the door for malignant changes. In modern parallels, poor metabolism manifests as obesity, diabetes, and hormonal disturbances, all of which are established risk factors for male breast cancer.
Meda Dhatu Dushti refers to imbalances in the fat tissue. Excessive or deficient fat metabolism creates vulnerability in tissues, echoing the role of obesity and estrogen dominance. Rakta Dushti, or vitiation of blood, points to systemic toxicity and poor circulation, which in modern science is comparable to chronic inflammation, free radical damage, and carcinogenic exposures.
Ayurveda not only explains the root causes but also emphasizes preventive and corrective strategies. Shodhana therapies (detoxification), Rasayana herbs like Amalaki and Guduchi, and mineral formulations such as Swarna Bhasma aim to purify, rejuvenate, and strengthen the system. Lifestyle guidance—including a Satvic diet, stress reduction, yoga, and meditation—forms the foundation for preventing disease progression.
In this way, Ayurveda complements modern oncology by offering root-cause correction, while modern science contributes diagnostic precision and targeted therapies. Together, they form an integrative framework for understanding and addressing the causes of male breast cancer [20].
Risk Factors
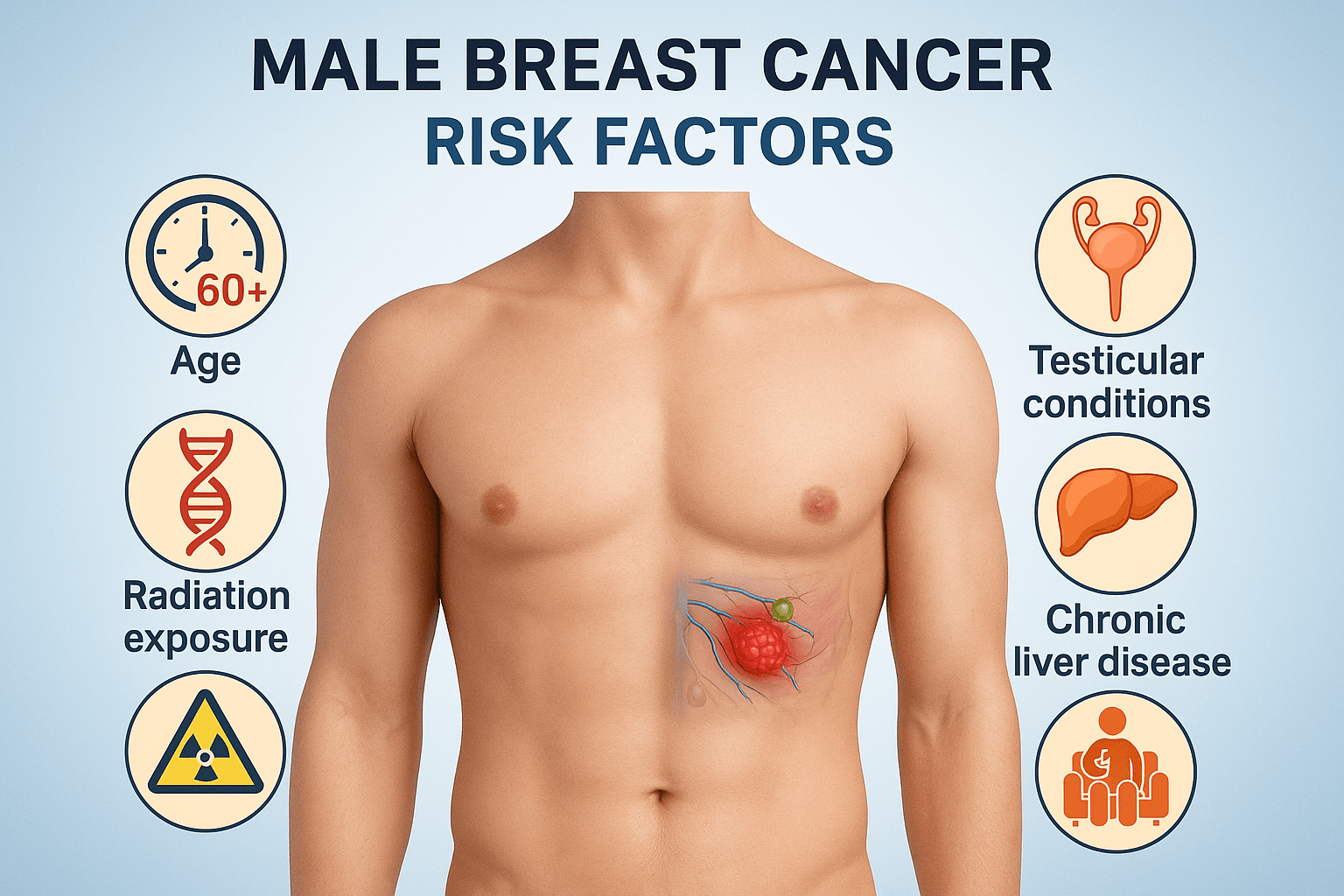
While the exact cause of male breast cancer may differ from patient to patient, several risk factors are well established. These risk factors do not guarantee the development of the disease, but they significantly increase the likelihood. Understanding them is crucial for awareness, prevention, and early detection.
Age (commonly after 60 years)
Age is one of the most important risk factors for male breast cancer [21]. The majority of cases are diagnosed in men between the ages of 60 and 70. As men age, breast tissue, although minimal, undergoes cellular wear and tear. The DNA repair mechanisms become less efficient, leading to an accumulation of genetic errors that can trigger cancerous changes.
Hormonal balance also shifts with age. Testosterone production declines, while estrogen, though low, may remain stable or slightly rise due to reduced metabolism and increased aromatization of fat tissue. This prolonged estrogenic influence on breast cells increases the risk of malignant transformation. Moreover, the immune system becomes less efficient at recognizing and eliminating abnormal cells, allowing cancers to develop more easily.
Ayurveda interprets the role of age in disease susceptibility through the lens of Vaya (life stage) and Dhatu Kshaya (tissue depletion). With advancing years, there is natural decline in Ojas (vitality) and the predominance of Vata Dosha, which creates instability in tissue structures. This internal environment is more vulnerable to cancer development. Hence, both Ayurveda and modern science emphasize age as a non-modifiable but important factor in male breast cancer [22].
Family History of Breast/Ovarian Cancer
Family history plays a powerful role in the risk of male breast cancer [23]. Men who have close relatives—especially mothers, sisters, or daughters—diagnosed with breast or ovarian cancer are at significantly higher risk. This connection is most commonly linked to hereditary genetic mutations such as BRCA1 and BRCA2. These faulty genes can be inherited and passed down generations, explaining why clusters of breast and ovarian cancers are often found in the same family.
In addition, men from families with multiple cases of cancer may carry other inherited mutations in DNA repair genes, which predispose them to malignancies. Even without confirmed genetic mutations, a strong family history is a red flag that calls for genetic counseling, early screening, and heightened awareness of symptoms.
Ayurveda frames family history under Beejadosha (genetic seed defects). The texts describe how the health and balance of parental Doshas and Dhatus during conception strongly influence the child’s constitution and disease vulnerability. This ancient wisdom aligns closely with modern genetic science. Men from high-risk families are advised to practice preventive care, maintain optimal metabolism, and adopt Rasayana therapy to strengthen resistance against malignancies [24].
Radiation Exposure in Chest Area
Radiation exposure is a recognized risk factor for male breast cancer [25]. Men who have received therapeutic chest radiation—for example, during treatment for Hodgkin’s lymphoma or other cancers—are at increased risk later in life. Radiation damages DNA, and even though the effects may not be immediate, the risk persists for decades.
The breast tissue, although less developed in men, is still sensitive to radiation-induced changes. Prolonged or high-dose exposure, whether medical or environmental, increases the likelihood of cellular mutations that can progress into malignancy. Awareness of this risk is critical because men with prior radiation exposure may dismiss early symptoms like lumps or nipple changes, attributing them to scarring or benign effects.
In Ayurveda, external damaging influences like radiation can be compared to Agantuja Nidana (external causative factors). These create disturbances in Rakta Dhatu (blood) and Meda Dhatu (fat), both of which are central to the pathology of breast cancer. Preventive strategies involve Rasayana herbs like Amalaki and Guduchi, which have demonstrated radioprotective and DNA-repair properties in modern research. This integrative approach may help reduce the long-term effects of radiation [26].
Testicular Conditions (Orchitis, Undescended Testes)
Testicular health is closely linked to the risk of male breast cancer [27]. Conditions such as orchitis (inflammation of the testes), undescended testes (cryptorchidism), or surgical removal of testes reduce testosterone production. With diminished testosterone, the protective androgenic influence over breast tissue is lost, while estrogen activity becomes relatively stronger. This imbalance fosters conditions for abnormal breast cell growth.
Men with orchitis due to infections like mumps may experience permanent testicular damage. Similarly, undescended testes, if not corrected in childhood, may result in lifelong hormonal disturbances. Even surgical castration, historically performed for certain conditions, increases vulnerability to male breast cancer.
From an Ayurvedic standpoint, the testes correspond to Shukra Dhatu, responsible for reproductive strength and hormonal balance. Disturbances in Shukra Dhatu lead not only to infertility but also systemic vulnerabilities, including cancers. Classical texts also describe how retained impurities and improper development of reproductive tissues can predispose individuals to disease. This offers a parallel explanation for the link between testicular conditions and male breast cancer [28].
Chronic Liver Disease Leading to Estrogen Dominance
The liver plays a vital role in metabolizing hormones, including estrogen. Chronic liver diseases such as cirrhosis, hepatitis, or fatty liver impair this function, leading to excess estrogen circulating in the blood. This condition, known as estrogen dominance, is a significant risk factor for male breast cancer [29].
Men with liver disease often exhibit feminizing features such as gynecomastia, reduced body hair, and decreased libido. These clinical signs highlight the altered hormonal environment, which places breast tissue at risk. Alcohol-induced liver disease is especially concerning, as both alcohol and impaired liver function combine to amplify risk.
Ayurveda associates liver dysfunction with Yakrit Vikara (liver disorders) and links them to Rakta Dushti (vitiated blood) and Pitta aggravation. When the liver’s detoxifying capacity is weakened, Ama (toxins) accumulate, disturbing the endocrine system and metabolism. Herbs like Kutki (Picrorhiza kurroa) and Bhumyamalaki (Phyllanthus niruri) are traditionally used to strengthen liver function, which aligns with modern understanding of supporting hormone balance and reducing cancer risks [30].
Sedentary Lifestyle and Poor Diet
A sedentary lifestyle coupled with poor dietary habits is one of the most preventable risk factors for male breast cancer [31]. Lack of physical activity leads to obesity, insulin resistance, and hormonal imbalance—all of which raise cancer risk. Diets high in processed foods, red meat, and alcohol further add to the toxic load, while inadequate intake of fruits, vegetables, and fiber reduces the body’s natural defense mechanisms.
Regular physical activity improves metabolism, balances hormones, and strengthens the immune system. Studies show that even moderate exercise significantly reduces estrogen levels in overweight men, thereby lowering breast cancer risk. Balanced nutrition with antioxidants, vitamins, and phytochemicals also provides protective effects against DNA damage and abnormal cell growth.
Ayurveda emphasizes Dinacharya (daily routines) and Ahara (dietary discipline) for maintaining balance. Sedentary lifestyle is seen as Kapha aggravating, leading to obesity and Meda Dhatu Dushti (fat tissue disorder). Poor dietary practices result in Ama accumulation, which clogs Srotas (channels) and weakens tissue health. Preventive care thus involves regular exercise, a Satvic diet, seasonal detox therapies, and Rasayana formulations to sustain vitality and immunity. These holistic measures align with modern lifestyle medicine and offer powerful protection against male breast cancer [32].
Symptoms
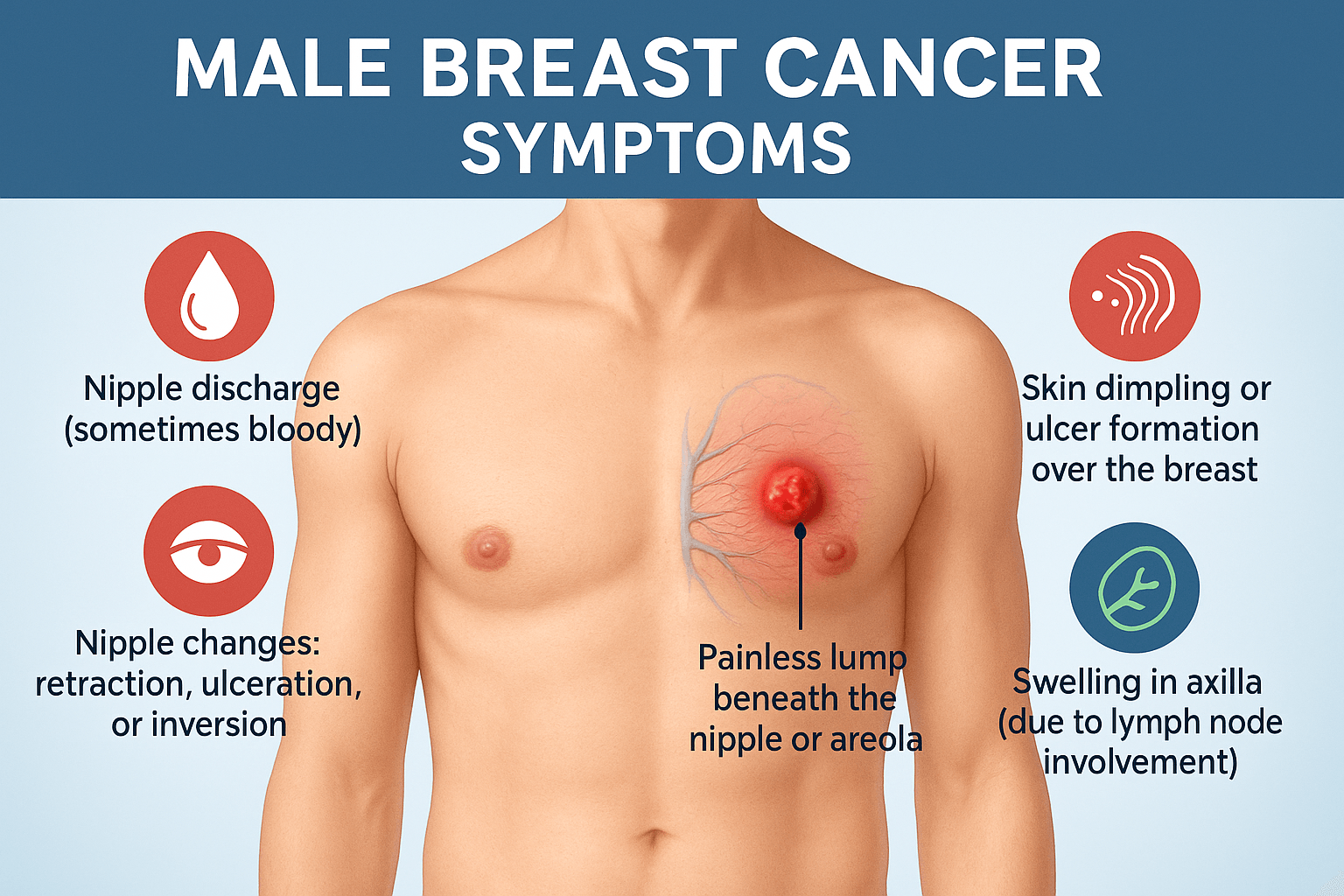
The symptoms of male breast cancer can often be subtle and easily overlooked. Because men generally do not expect to develop breast cancer, they may delay seeking medical care. This results in later diagnoses compared to women, often at more advanced stages. Recognizing symptoms early is essential for improving survival and treatment outcomes.
Painless Lump Beneath the Nipple or Areola
The most common presenting symptom of male breast cancer is a painless lump located directly beneath the nipple or areola [33]. Unlike women, men have less breast tissue, and tumors tend to arise close to the nipple, making them easier to detect with palpation. These lumps are usually firm, irregular, and non-tender.
Because the mass is painless, many men dismiss it as harmless or confuse it with benign conditions such as gynecomastia. However, any lump in the male breast warrants immediate evaluation. Delay in diagnosis allows the tumor to grow and invade nearby tissues, leading to worse outcomes.
From an Ayurvedic standpoint, such localized swellings are described as Granthi (tumor-like growths) or Shotha (swelling). These are considered to arise from vitiation of Doshas, particularly Kapha and Rakta, leading to abnormal proliferation of tissue. In both systems of medicine, the key message is that early identification of a lump is the most critical step toward effective treatment [34].
Nipple Changes- Retraction, Ulceration, or Inversion
Another important sign of male breast cancer is alteration of the nipple’s normal appearance [35]. Nipple retraction, where the nipple turns inward, often occurs when tumors pull on the ducts. Ulceration or breakdown of the nipple skin is also common in more advanced stages, as the tumor invades superficial layers. Nipple inversion can be mistaken for congenital variation, but when it develops later in life, it is a red flag for malignancy.
Clinically, such changes should always raise suspicion, especially when associated with hardness beneath the areola. Unfortunately, many men hesitate to report nipple changes due to stigma or lack of awareness.
Ayurveda parallels this with the concept of Vrana (ulceration), which can form when vitiated Rakta (blood) and Pitta (fire element) damage delicate tissues. Vrana is described as painful, non-healing, and prone to spreading, closely resembling modern descriptions of malignant ulcerations. Thus, nipple changes are not cosmetic concerns but warning signs of male breast cancer [36].
Nipple Discharge (Sometimes Bloody)
Nipple discharge in men is abnormal and should always be investigated. In cases of male breast cancer, the discharge may be clear, milky, or blood-stained [37]. Bloody discharge is particularly concerning, as it often indicates ductal carcinoma or invasive disease.
This symptom arises when tumors erode or infiltrate ducts, releasing cellular debris and blood into the nipple opening. Even small amounts of discharge should prompt a physician’s evaluation, as it may be an early indicator of malignancy.
In Ayurveda, discharges are categorized under Dushta Srava (vitiated secretions), which result from imbalance in Rakta and Pitta. Such secretions are considered signs of deeper pathology within tissues, demanding immediate attention. Modern oncology and Ayurveda both stress that nipple discharge in men is never normal and should be taken seriously [38].
Skin Dimpling or Ulcer Formation Over the Breast
Skin changes overlying the breast are another hallmark of male breast cancer [39]. Dimpling or puckering of the skin occurs when tumors tether to the overlying dermis, creating an orange-peel appearance (peau d’orange). As the disease progresses, ulcers may develop due to invasion of cancer cells through the skin.
Such lesions may be mistaken for infections, eczema, or trauma-related scars. However, persistence of dimpling or ulceration without obvious cause should alert clinicians to possible malignancy. These changes often signify advanced disease with lymphatic involvement.
Ayurveda equates this to Vrana (ulcer) and Shotha (swelling with deformity), reflecting the combined effects of Dosha imbalance and tissue degeneration. Skin manifestations are considered external indicators of deep systemic pathology, emphasizing the need for holistic evaluation and treatment [40].
Swelling in Axilla (Due to Lymph Node Involvement)
Swelling in the armpit is often the first sign of regional spread of male breast cancer [41]. The axilla contains lymph nodes that serve as drainage pathways for the breast. When cancer spreads beyond the primary tumor, these nodes enlarge and become firm or fixed.
Patients may feel discomfort, heaviness, or a palpable mass under the arm. Axillary involvement has important prognostic implications—it often signals more advanced disease and influences surgical and therapeutic strategies.
In Ayurvedic understanding, axillary swellings are described under Shotha (enlargement due to Dosha vitiation) and sometimes Apachi (lymphatic swellings). They indicate that Rakta and Kapha Doshas are severely imbalanced, with toxins spreading through Srotas (channels). Clinically and traditionally, axillary swelling is recognized as a warning of systemic spread, highlighting the urgency of treatment [42].
Ayurvedic Perspective- Shotha, Vrana, and Rakta Dushti
Ayurveda views the symptoms of male breast cancer as expressions of deeper systemic imbalance. Shotha (swelling) explains the painless lumps and axillary enlargements. Vrana (ulcer) accounts for nipple ulceration and skin breakdown. Rakta Dushti (blood vitiation) explains abnormal discharges, discoloration, and the aggressiveness of lesions [43].
By correlating these ancient terms with modern symptoms, Ayurveda provides a framework for both understanding disease progression and guiding holistic treatment strategies. Rasayana therapy, purification (Shodhana), and blood-cleansing herbs (Rakta Prasadana) are emphasized to address these manifestations at the root level, not just symptomatically.
Diagnosis
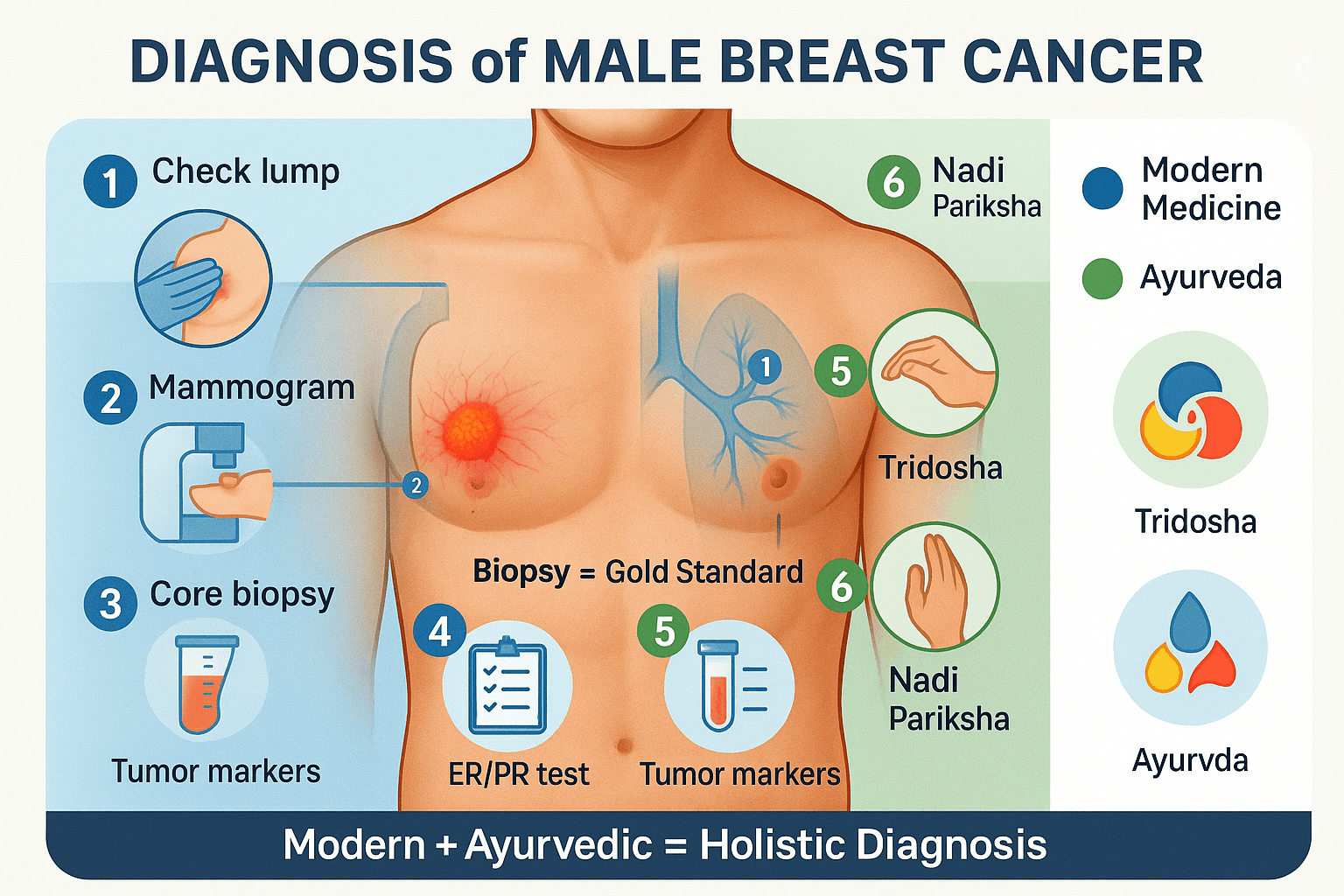
Timely and accurate diagnosis of male breast cancer is crucial because most men are diagnosed at later stages due to lack of awareness. Diagnosis involves a combination of clinical examination, imaging, histopathology, molecular testing, and supportive blood work. Ayurveda also provides unique diagnostic approaches, offering a holistic perspective.
Clinical Examination- Palpation of Breast and Lymph Nodes
The first step in diagnosing male breast cancer is a thorough clinical examination [44]. Physicians palpate the breast to detect lumps, irregularities, or skin changes. Unlike women, where tumors may be masked by abundant breast tissue, male breast tumors are often located directly beneath the nipple and areola, making them more easily palpable.
A physician also examines nearby lymph nodes, particularly in the axilla (underarm). Enlarged, firm, or immobile lymph nodes often indicate spread beyond the primary tumor. In some cases, supraclavicular or cervical lymph nodes may also be affected, pointing to advanced disease.
The clinical examination is simple yet powerful. However, because many men ignore early signs or mistake them for benign conditions like gynecomastia, the cancer is often advanced by the time medical help is sought.
Ayurveda parallels this approach with Sparsha Pariksha (tactile examination) and Darshana Pariksha (visual inspection). These methods aim to detect swelling (Shotha), ulcers (Vrana), or abnormalities of Rakta and Meda Dhatu. Thus, both modern and Ayurvedic practices emphasize the value of touch and observation as first-line diagnostic tools [45].
Imaging- Mammography, Ultrasound, MRI
Imaging plays a critical role in confirming clinical findings and guiding biopsy. Mammography remains the gold standard for breast cancer imaging, even in men [46]. It can detect calcifications, masses, and architectural distortions that may not be palpable. However, due to smaller male breast size, mammography can sometimes be technically challenging.
Ultrasound is frequently used alongside mammography. It provides detailed visualization of solid versus cystic lesions and can assess axillary lymph nodes. It is especially useful for guiding needle biopsies.
Magnetic Resonance Imaging (MRI) offers superior sensitivity and is used for complex or ambiguous cases. MRI can provide information on tumor extent, chest wall involvement, and multifocal disease. For men with genetic mutations (BRCA1/2), MRI may also serve as a screening tool in high-risk populations.
From an Ayurvedic standpoint, imaging reflects the concept of Antar Pariksha (internal examination). While Ayurveda traditionally used observation, inference, and pulse reading, the integration of modern imaging aligns with its spirit of exploring hidden disease processes within the body [47].
Biopsy- Core Needle Biopsy, Excisional Biopsy for Histology
Definitive diagnosis of male breast cancer requires tissue sampling [48]. A core needle biopsy is the most common method, in which a hollow needle extracts tissue samples from the suspicious lump. This minimally invasive procedure is performed under ultrasound or mammographic guidance.
If the lesion is too small or inconclusive, an excisional biopsy may be performed, where the entire lump is surgically removed and sent for histopathological analysis. The pathologist then examines cellular architecture to confirm malignancy and subtype (e.g., invasive ductal carcinoma, lobular carcinoma).
Histology also provides insights into tumor grade, mitotic activity, and presence of necrosis—all of which influence prognosis and treatment planning.
Ayurveda would classify this under Nidana Pariksha (causal investigation), where identifying the root pathology (Beejadosha, Rakta Dushti, or Meda Dushti) is essential for designing personalized treatment. Although Ayurveda does not employ biopsies, its philosophy aligns with the principle of finding the underlying cause [49].
Immunohistochemistry- Hormone and HER2 Testing
Once tissue is obtained, immunohistochemistry (IHC) is performed to identify molecular markers [50]. These tests evaluate whether the tumor expresses estrogen receptors (ER), progesterone receptors (PR), or HER2/neu proteins.
The results guide therapy:
- ER/PR positive tumors respond well to hormone therapy such as Tamoxifen.
- HER2 positive tumors benefit from targeted therapy like Trastuzumab.
- Triple-negative tumors lack these markers and may require aggressive chemotherapy.
IHC provides personalized treatment planning, moving beyond a “one-size-fits-all” approach. In Ayurveda, this mirrors the concept of Prakriti-based diagnosis, where therapies are customized according to an individual’s constitution and disease pattern. Just as IHC identifies biological targets, Ayurvedic analysis identifies constitutional vulnerabilities to personalize treatment [51].
Blood Tests- Tumor Markers (CEA, CA 15-3 – Limited Role)
Blood tests play a supportive role in diagnosing and monitoring male breast cancer [52]. Tumor markers such as Carcinoembryonic Antigen (CEA) and CA 15-3 may be elevated, but they are not specific or sensitive enough for early detection. Their main utility lies in tracking treatment response or disease recurrence.
Other blood work, including liver function tests, kidney function tests, and complete blood counts, are essential for assessing baseline health and readiness for chemotherapy or surgery.
Ayurveda emphasizes the evaluation of blood quality through Rakta Pariksha, noting changes in color, consistency, and circulation. Rakta Dushti (vitiated blood) is often considered a precursor to cancerous processes, aligning conceptually with the use of tumor markers and blood studies in modern oncology [53].
Ayurvedic Diagnosis- Nadi Pariksha, Tridosha Assessment, Dhatu and Srotas Mapping
Ayurveda employs a holistic diagnostic approach that goes beyond identifying localized tumors. Nadi Pariksha (pulse diagnosis) is used to detect imbalances in Vata, Pitta, and Kapha Doshas, which underlie the disease process [54].
A detailed Tridosha assessment evaluates how each Dosha contributes to pathology. In male breast cancer, Kapha is often involved in the abnormal growth, Pitta in inflammatory changes, and Vata in the spread and metastasis.
Ayurveda also emphasizes Dhatu and Srotas mapping. Cancer is often linked to Meda Dhatu Dushti (fat tissue pathology), Rakta Dushti (blood vitiation), and impairment of Rasa and Majja Dhatus (plasma and marrow). Srotas (channels) such as Rasavaha (circulatory) and Medovaha (fat transport) are considered obstructed or corrupted, allowing malignancy to manifest.
This comprehensive framework enables personalized care, integrating physical, mental, and systemic health for both diagnosis and treatment planning [55].
Staging and Classification
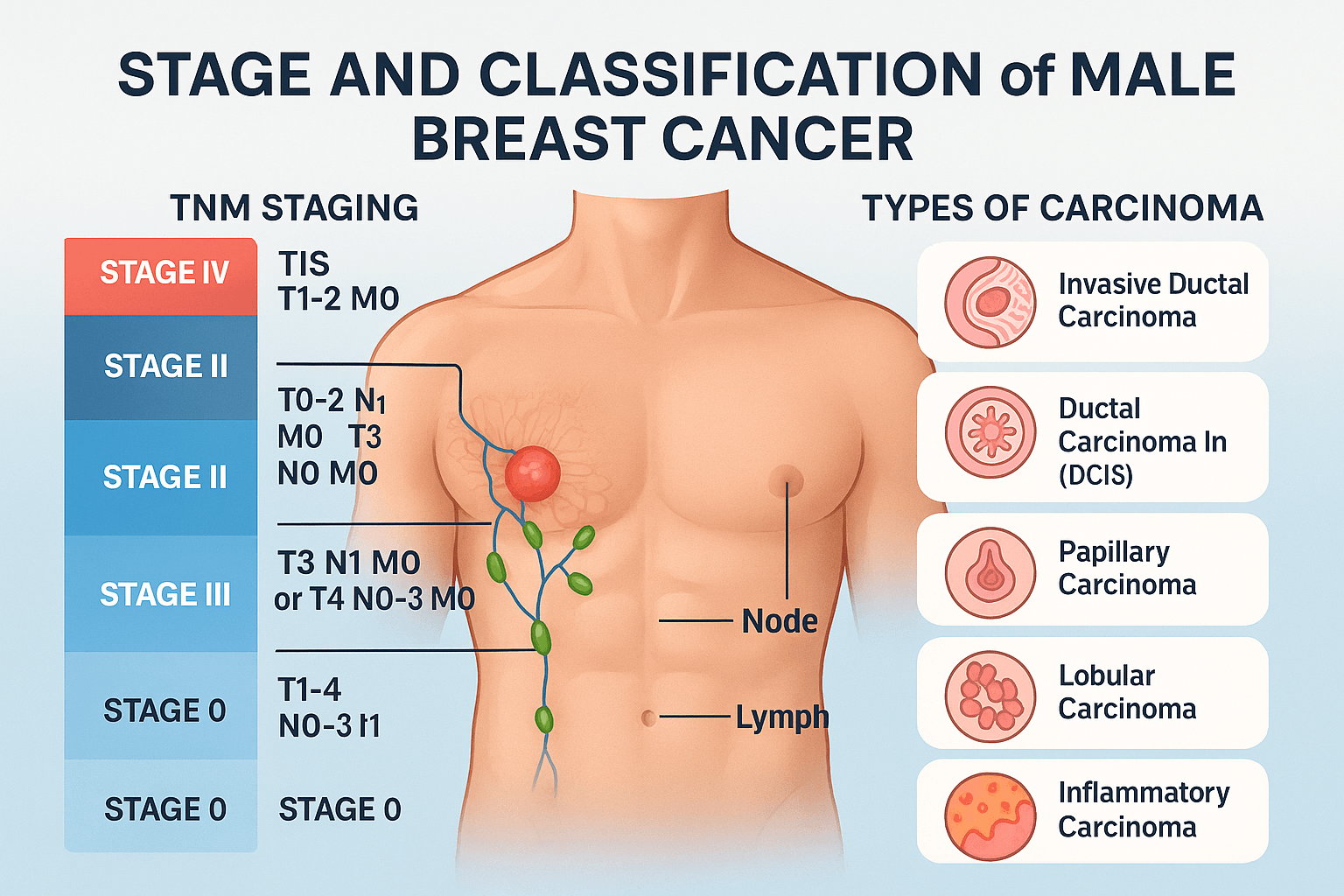
Correct staging and classification of male breast cancer are essential for determining prognosis and guiding treatment. Staging defines how far the cancer has progressed, while classification describes the type of tumor under the microscope. Together, they provide a roadmap for physicians and help patients understand the seriousness of their condition.
TNM Staging System (Tumor size, Node involvement, Metastasis)
The TNM staging system is the most widely used method for describing the extent of male breast cancer [56]. It considers three major components:
- T (Tumor size): Ranges from Tis (carcinoma in situ) to T4 (large tumors invading chest wall or skin). Small tumors confined to the breast (T1) have the best prognosis, while larger tumors (T3–T4) often signal more advanced disease.
- N (Node involvement): Refers to whether the cancer has spread to nearby lymph nodes. N0 means no lymph node spread, while N1–N3 indicates increasing involvement, particularly in axillary and supraclavicular nodes.
- M (Metastasis): Indicates whether the cancer has spread to distant organs such as bones, lungs, liver, or brain. M0 means no metastasis; M1 means the disease has spread.
Staging ranges from Stage 0 (non-invasive carcinoma in situ) to Stage IV (metastatic disease). Each stage has unique survival rates and treatment approaches. Ayurveda parallels staging with the progression of Dosha imbalance and spread of disease through Srotas (channels). Early stages reflect localized Dosha vitiation, while advanced stages correspond to systemic spread of toxins and Dhatu Dushti (tissue damage) [57].
Invasive Ductal Carcinoma (Most Common in Men)
The vast majority of male breast cancers are invasive ductal carcinomas (IDC) [58]. This type of cancer originates in the ducts that carry milk (though underdeveloped in men) and invades the surrounding breast tissue. IDC often presents as a firm, painless lump beneath the nipple or areola, frequently associated with nipple retraction or skin changes.
IDC is usually hormone receptor positive (ER and PR positive), which means that hormone therapy, particularly Tamoxifen, is highly effective. However, men with HER2-positive IDC may require targeted therapy such as Trastuzumab.
Pathologically, IDC shows irregular nests and cords of malignant epithelial cells invading fibrous stroma. Its aggressiveness varies depending on grade, hormone receptor status, and presence of lymph node involvement.
In Ayurveda, IDC aligns with Granthi (tumor formation) progressing into Arbuda (malignant growth) when unchecked. Kapha Dosha contributes to tissue proliferation, Pitta drives inflammation and ulceration, and Vata promotes spread. This multi-dosha imbalance makes IDC the archetype of male breast cancer in both modern and Ayurvedic frameworks [59].
Ductal Carcinoma In Situ (DCIS)
Ductal carcinoma in situ (DCIS) is a non-invasive form of male breast cancer where malignant cells are confined within the ducts and have not invaded surrounding tissues [60]. Though rare in men, DCIS is important because it represents Stage 0 disease, the earliest form of breast cancer.
DCIS usually appears as microcalcifications on mammography. It often does not produce a palpable lump but may occasionally present with nipple discharge. Left untreated, DCIS can progress to invasive ductal carcinoma, which is why early detection and surgical removal (often via mastectomy in men) are strongly recommended.
Ayurvedically, DCIS resembles an early-stage Granthi—a localized tumor without systemic involvement. The pathology is confined, Dosha imbalance is minimal, and Rakta Dushti is in its earliest phase. This makes early detection critical, as interventions at this stage—whether modern surgical excision or Ayurvedic detoxification and Rasayana therapy—can halt progression toward invasive disease [61].
Rare Subtypes- Papillary, Lobular, Inflammatory Carcinoma
Although rare, men can develop unusual subtypes of male breast cancer, each with unique characteristics [62].
- Papillary carcinoma is characterized by finger-like projections of malignant cells. It tends to have a better prognosis and occurs more often in older men.
- Lobular carcinoma is extremely rare in men because lobules (milk-producing glands) are usually absent or underdeveloped. When it does occur, it behaves similarly to lobular carcinoma in women, spreading in a single-file pattern.
- Inflammatory carcinoma is one of the most aggressive forms. It presents with redness, swelling, and peau d’orange (skin dimpling resembling orange peel). Although uncommon in men, when it occurs, it signals advanced disease with poor prognosis.
Ayurveda would interpret these rare variants under the spectrum of Arbuda types, distinguished by Dosha predominance. Papillary carcinoma aligns with milder Kapha dominance (slow-growing), lobular with hidden Meda Dushti (fat tissue imbalance), and inflammatory carcinoma with severe Pitta aggravation and Rakta Dushti, explaining its redness, heat, and aggressive spread [63].
Treatment
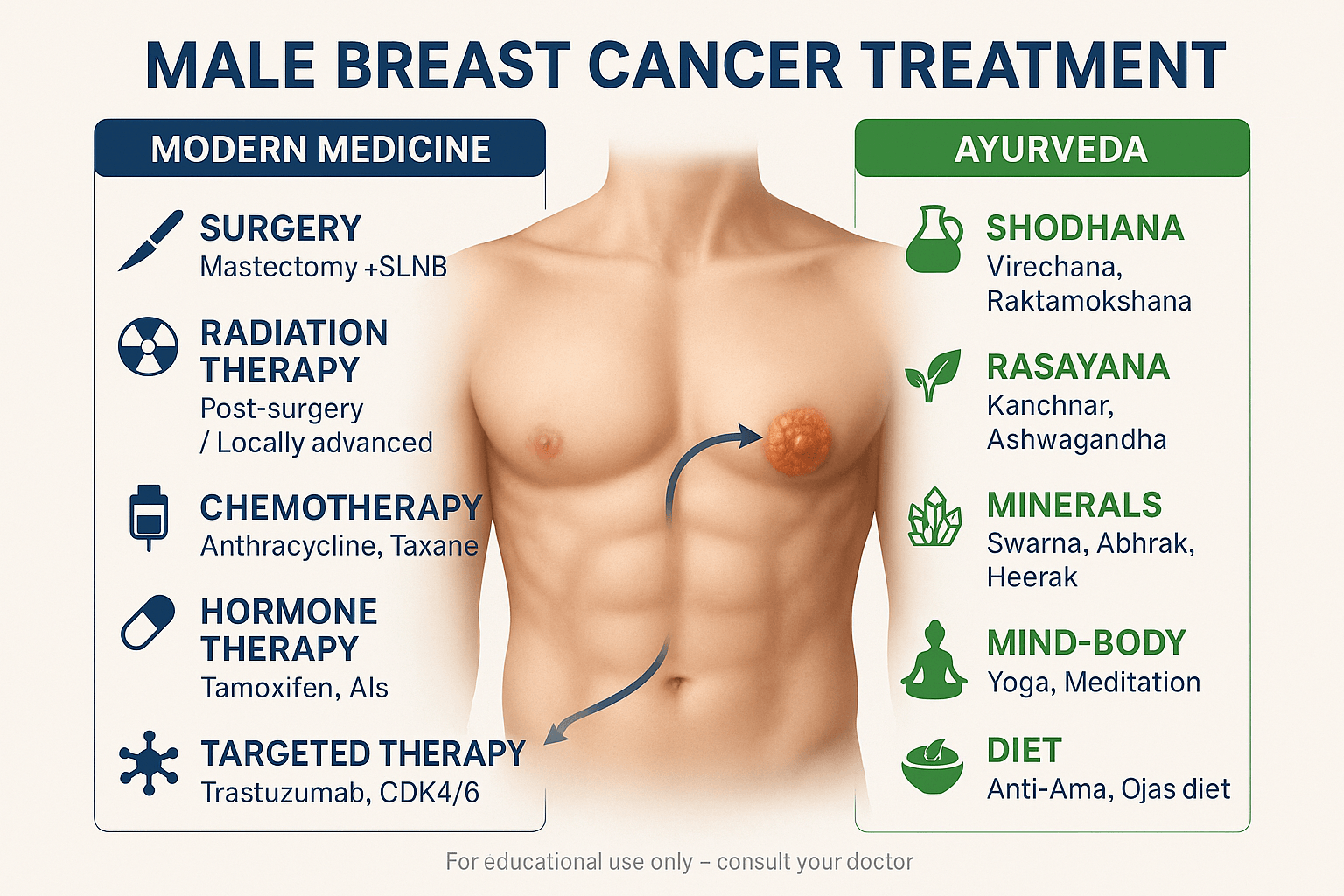
Management of male breast cancer requires a multidisciplinary approach that combines surgery, systemic therapies, radiation, and supportive care. While modern medicine offers targeted and evidence-based protocols, Ayurveda contributes through detoxification, Rasayana therapy, and holistic lifestyle interventions. Integrating both ensures not just tumor control but also improved quality of life and systemic healing.
Surgery-Modified Radical Mastectomy, Sentinel Lymph Node Biopsy
Surgery remains the cornerstone of treatment for male breast cancer [64]. The most common operation is a modified radical mastectomy, which involves removal of the entire breast tissue along with axillary lymph nodes, while preserving the pectoral muscles. Because men have limited breast tissue, lumpectomy is rarely an option.
To reduce surgical morbidity, a sentinel lymph node biopsy (SLNB) is often performed. This technique identifies the first draining lymph node from the tumor. If the sentinel node is free of cancer, further axillary dissection can be avoided, reducing complications like lymphedema and shoulder dysfunction.
From an Ayurvedic perspective, surgical removal of a localized tumor is comparable to Shastra Karma (surgical intervention), which is advocated for certain types of Arbuda (malignant growths). Sushruta Samhita specifically recommends excision of abnormal masses when feasible, followed by wound healing and Rasayana therapy to restore balance [65].
Radiation Therapy- Post-Surgery or Locally Advanced Cases
Radiation therapy is recommended for men with locally advanced male breast cancer, close surgical margins, or extensive lymph node involvement [66]. It uses high-energy X-rays to destroy residual cancer cells, reducing recurrence rates.
Modern protocols may involve external beam radiation directed at the chest wall and axilla. Side effects include skin irritation, fatigue, and rare long-term risks like rib fractures or secondary malignancies. Despite these risks, radiation remains a critical adjunct for comprehensive care.
Ayurveda conceptualizes radiation injury as Agantuja (external trauma) causing Rakta Dushti (blood vitiation). Radioprotective herbs such as Guduchi (Tinospora cordifolia) and Amalaki (Emblica officinalis) have shown potential in reducing oxidative stress and enhancing tissue repair. Thus, Ayurveda may help mitigate radiation side effects while supporting systemic resilience [67].
Chemotherapy-Anthracycline- and Taxane-Based Regimens
Chemotherapy is used in high-risk, recurrent, or metastatic male breast cancer [68]. Standard regimens include anthracyclines (doxorubicin, epirubicin) and taxanes (paclitaxel, docetaxel). These drugs attack rapidly dividing cells, shrinking tumors and reducing systemic spread.
Adjuvant chemotherapy is often administered after surgery, while neoadjuvant chemotherapy may be given before surgery to shrink large tumors. Side effects include nausea, vomiting, hair loss, neutropenia, and cardiotoxicity. Supportive care is essential to improve tolerance.
In Ayurveda, chemotherapy parallels Shodhana (cleansing therapy), which eliminates diseased tissues but also weakens healthy Dhatus (tissues). Rasayana therapy is recommended alongside to restore Ojas (vitality) and immunity. Herbs like Ashwagandha and Shatavari may help reduce fatigue and enhance recovery during chemotherapy [69].
Hormone Therapy-Tamoxifen, Aromatase Inhibitors
Most male breast cancers are hormone receptor positive, making hormone therapy the mainstay of systemic treatment [70]. Tamoxifen, a selective estrogen receptor modulator, is the first-line therapy, significantly reducing recurrence and improving survival.
In some cases, aromatase inhibitors (AIs) such as letrozole or anastrozole may be used, particularly in combination with gonadal suppression. However, Tamoxifen remains superior for men due to differences in hormonal physiology compared to women.
Ayurveda explains hormone imbalance in terms of Agni Mandya (impaired metabolism) and Meda Dushti (fat tissue pathology). Correcting these imbalances with anti-estrogenic and detoxifying herbs like Turmeric and Kanchnar Guggulu may support hormone therapy outcomes, making integrative strategies highly valuable [71].
Targeted Therapy-Trastuzumab, CDK4/6 Inhibitors
Targeted therapies have revolutionized the treatment of HER2-positive male breast cancer [72]. Trastuzumab (Herceptin) specifically binds to HER2 receptors, blocking signaling pathways that drive tumor growth. When combined with chemotherapy, it significantly improves survival.
For hormone receptor–positive tumors, CDK4/6 inhibitors (palbociclib, ribociclib) are being increasingly studied in men. These agents disrupt the cancer cell cycle, slowing or halting proliferation. Targeted therapies are generally better tolerated than chemotherapy, though they carry risks like cardiotoxicity or neutropenia.
In Ayurveda, targeted therapy resonates with the idea of Vyadhiharan Rasayana, or disease-specific rejuvenation, where herbs and minerals are chosen for precision action against particular disease pathways. This concept reinforces the importance of personalized treatment [73].
Immunotherapy-Checkpoint Inhibitors
Immunotherapy is an evolving field for male breast cancer management [74]. Drugs called checkpoint inhibitors (e.g., pembrolizumab, atezolizumab) unleash the immune system to recognize and destroy cancer cells. While currently used mainly in triple-negative breast cancer, ongoing clinical trials are exploring their role in men.
Although not yet standard of care, immunotherapy represents hope for advanced, treatment-resistant cancers. Common side effects include autoimmune-like reactions, fatigue, and skin rashes.
Ayurveda emphasizes strengthening immunity through Ojas restoration. Rasayana therapies such as Swarna Bhasma and Guduchi are considered immunomodulators, enhancing the body’s ability to fight disease naturally. The synergy between modern immunotherapy and Ayurvedic Ojas-building principles opens exciting integrative possibilities [75].
Ayurvedic Integration in Male Breast Cancer Treatment
Ayurveda views male breast cancer not as an isolated disease of the breast but as a manifestation of deeper systemic imbalances involving the Doshas (Vata, Pitta, Kapha), Dhatus (body tissues), and Agni (metabolic fire). While modern medicine targets the tumor directly, Ayurveda aims to correct the underlying terrain that allows malignancy to develop and spread. This complementary approach can enhance overall treatment effectiveness, minimize side effects, and support long-term healing.
Shodhana Therapies-Detoxification and Channel Purification
In Ayurveda, Shodhana (purification therapies) are central to cancer management. The principle is that accumulated Ama (toxins) and Dosha imbalances clog the Srotas (body channels), impairing tissue health and immunity. Clearing these obstructions allows the body to respond better to treatment.
- Virechana (Therapeutic Purgation): Especially useful when Pitta Dosha is aggravated, as seen in inflammatory cancers. Virechana eliminates excess heat and toxins through controlled purgation using herbal formulations like Trivrit (Operculina turpethum) or Avipattikar Churna. For male breast cancer, it helps control inflammatory processes and improves liver function, crucial for metabolizing hormones and drugs [78].
- Raktamokshana (Bloodletting): In selective cases of Rakta Dushti (vitiated blood), small-scale controlled bloodletting may be considered. Traditionally, this reduces congestion, removes toxins, and improves microcirculation. In modern interpretation, it parallels detox strategies that improve systemic balance. While not universally applied, it demonstrates Ayurveda’s emphasis on cleansing the terrain in which cancer thrives [79].
- Basti (Medicated Enema): Considered the prime therapy for Vata imbalance, Basti nourishes tissues and clears channels. In advanced male breast cancer, where Vata contributes to metastasis, Basti may help slow systemic spread and improve quality of life.
Shodhana therapies are ideally done under strict specialist supervision and are often combined with Rasayana therapies to rebuild strength after detoxification.
Rasayana Therapy- Rejuvenation and Immune Restoration
Rasayana is one of Ayurveda’s most powerful tools in cancer management. It refers to therapies that rejuvenate the body, enhance immunity, and restore Ojas (vital essence). In male breast cancer, Rasayana plays three critical roles: slowing tumor progression, improving tolerance to modern therapies, and supporting long-term survivorship.
- Kanchnar Guggulu: A classical formulation specifically indicated for Granthi (benign/malignant tumors). It reduces abnormal growths, clears Kapha congestion, and supports lymphatic health. Modern studies have shown its anti-tumor and anti-inflammatory potential [80].
- Ashwagandha (Withania somnifera): A potent adaptogen that reduces stress, improves stamina, and modulates immunity. It is particularly beneficial for men undergoing chemotherapy, reducing fatigue, improving muscle mass, and supporting hormonal balance. Experimental research shows anti-cancer activity through apoptosis induction and angiogenesis inhibition [81].
- Guduchi (Tinospora cordifolia): Known as “Amrita,” Guduchi enhances immune surveillance and helps the body resist infections and therapy-related toxicities. It also reduces oxidative stress and inflammation, making it a valuable Rasayana in cancer care [82].
- Amalaki (Emblica officinalis): Rich in Vitamin C and antioxidants, Amalaki supports detoxification, enhances digestion, and acts as a Rasayana for Rasa Dhatu (plasma) and Rakta Dhatu (blood). It strengthens tissues and prevents oxidative DNA damage, reducing recurrence risk [83].
- Turmeric (Curcuma longa): Curcumin, its active compound, has been studied extensively for anti-cancer properties. It modulates signaling pathways, reduces inflammation, and improves chemotherapy sensitivity. Ayurveda prescribes Haridra (Turmeric) both internally and externally in Granthi and Arbuda conditions [84].
These Rasayanas are not used as isolated herbs but are integrated into holistic regimens tailored to the patient’s Prakriti (constitution), stage of disease, and tolerance.
Mineral Preparations- Precision and Deep-Acting Therapies
Ayurvedic Rasashastra (alchemy) introduced mineral and metallic preparations that act at a profound cellular level. In male breast cancer, these formulations are used cautiously, only under specialist supervision, but they are considered powerful tools for halting disease progression and restoring vitality.
- Swarna Bhasma (Gold Ash): Revered for its Rasayana and immune-strengthening properties. In modern research, gold nanoparticles derived from Swarna Bhasma exhibit targeted anti-tumor effects, including apoptosis induction and inhibition of angiogenesis. In Ayurveda, it is also credited with rejuvenating Shukra Dhatu (reproductive tissue), supporting hormonal balance [85].
- Abhrak Bhasma (Purified Mica Ash): A potent rejuvenator used in long-standing chronic conditions. It enhances tissue regeneration, improves stamina, and corrects imbalances in Majja Dhatu (marrow), making it valuable for patients weakened by prolonged therapies.
- Heerak Bhasma (Diamond Ash): Rare and precious, Heerak Bhasma is traditionally described as the most powerful Rasayana, capable of halting Arbuda (malignancy). Modern studies on diamond nanoparticles suggest anti-proliferative properties, aligning with classical claims [86].
These formulations are prescribed in microdoses, combined with herbal decoctions or Rasayanas to maximize absorption and minimize toxicity. Their role is often complementary, supporting systemic immunity and resilience during aggressive modern treatments.
Satvavajaya Chikitsa-Mind–Body Healing
Cancer is not only a physical disease but also a profound psychological challenge. Male breast cancer patients often experience stigma, anxiety, and depression, given the perception that breast cancer is a “female disease.” This psychosocial burden can weaken immunity and negatively impact treatment outcomes.
Ayurveda addresses the mind through Satvavajaya Chikitsa (psychotherapy and mind control techniques). This includes:
- Meditation and mindfulness practices: Reduce stress hormones like cortisol, improve immune resilience, and enhance emotional stability.
- Yoga and Pranayama: Improve circulation, oxygenation, and relaxation, helping patients tolerate surgery, radiation, and chemotherapy better.
- Counseling and supportive therapies: Provide reassurance, reduce fear, and foster optimism. Ancient texts emphasized that a strong Satva (mind) empowers the body to resist disease and enhances treatment outcomes.
Modern psycho-oncology has reached similar conclusions, showing that integrative mind–body practices improve survival and quality of life in cancer patients [87].
Diet and Lifestyle- Correcting Terrain, Building Ojas
Ayurveda emphasizes that food and daily regimen are as important as medicine. In male breast cancer, dietary and lifestyle correction supports metabolism, reduces toxin load, and enhances immunity.
- Anti-Ama Diet: Patients are advised to avoid heavy, processed, oily, and excessively sweet foods that create Ama (metabolic toxins). Instead, light, easily digestible meals with whole grains, legumes, seasonal vegetables, and herbal teas are recommended.
- Ojas-Enhancing Foods: Milk, ghee, almonds, Amalaki Rasayana, and Chyawanprash are prescribed to strengthen immunity and vitality.
- Spices for Balance: Turmeric, black pepper, cumin, and coriander enhance Agni (digestive fire) and reduce Kapha accumulation.
- Lifestyle Practices: Regular physical activity tailored to strength, adequate rest, and daily routines (Dinacharya) to balance Doshas.
- Seasonal Detox (Ritucharya): Gentle Panchakarma cleansing in specific seasons helps maintain Dosha balance and prevents recurrence.
These lifestyle measures not only aid recovery but also serve as preventive strategies for those at high risk of male breast cancer.
The Integrative Vision
When modern oncology and Ayurveda are combined, the treatment of male breast cancer becomes truly holistic. Surgery, radiation, chemotherapy, and targeted therapy directly eliminate cancer cells, while Ayurvedic Shodhana, Rasayana, and mind–body practices restore systemic balance, immunity, and resilience. Together, they reduce side effects, improve survival, and enhance quality of life, addressing not just the tumor but the entire person.
Prevention & Awareness
While male breast cancer cannot always be prevented, awareness of risk factors and proactive measures can significantly reduce its impact. Prevention involves a combination of genetic counseling, lifestyle changes, Ayurvedic Rasayana therapies, and public health campaigns to overcome stigma.
Genetic Counseling for High-Risk Individuals
Genetic predisposition is one of the strongest contributors to male breast cancer [78]. Men with a family history of breast or ovarian cancer, especially those with BRCA1 or BRCA2 mutations, should undergo genetic counseling. This process involves a detailed review of family history, assessment of individual risk, and discussion of genetic testing options.
Genetic counseling provides clarity about whether a man carries mutations that significantly increase cancer risk. If mutations are found, regular screening, earlier imaging, or prophylactic interventions may be considered. In addition, family members may also benefit from testing, which can help identify risk across generations.
Ayurveda explains such inherited risks under the principle of Beejadosha (genetic seed defects). Preventive measures include strengthening reproductive health before conception and using Rasayana herbs to minimize vulnerabilities. By combining modern genetic counseling with Ayurvedic preventive strategies, high-risk men can take informed steps to safeguard their health [79].
Lifestyle Modifications: Balanced Diet, Exercise, Avoiding Alcohol/Tobacco
Lifestyle choices play a major role in reducing the risk of male breast cancer [80]. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports healthy metabolism and reduces obesity, a known risk factor. Regular physical exercise lowers estrogen levels in overweight men, improves immune function, and enhances overall well-being.
Avoiding alcohol and tobacco is equally important. Alcohol impairs liver function, leading to higher estrogen levels, while tobacco contains carcinogens that directly damage DNA. Even moderate alcohol consumption increases the risk of breast cancer, making abstinence the safest preventive approach.
Ayurveda describes these principles in Dinacharya (daily regimen) and Swasthavritta (science of health maintenance). A Satvic diet, regular yoga, pranayama, and seasonal detox therapies are recommended to maintain balance, reduce Ama (toxic buildup), and keep Doshas aligned. Thus, both modern and Ayurvedic frameworks emphasize lifestyle discipline as a cornerstone of prevention [81].
Ayurvedic Preventive Rasayanas
Ayurveda emphasizes preventive care through Rasayana therapy, which rejuvenates tissues, enhances immunity, and restores Ojas (vital energy) [82]. For male breast cancer, preventive Rasayanas include:
- Amalaki (Emblica officinalis): Rich in vitamin C and antioxidants, supports detoxification and DNA repair.
- Guduchi (Tinospora cordifolia): Immunomodulator, reduces oxidative stress.
- Ashwagandha (Withania somnifera): Adaptogen that restores balance under stress and improves overall vitality.
- Kanchnar Guggulu: Traditionally used for dissolving abnormal growths, balancing Kapha Dosha.
These formulations not only strengthen natural defenses but also reduce the risk of metabolic imbalances that contribute to cancer development.
In modern terms, Rasayana therapy aligns with chemoprevention strategies, where natural compounds are used to reduce cancer risk in high-risk individuals. Preventive Rasayanas, when integrated with regular screening, create a holistic shield against male breast cancer [83].
Public Education to Overcome Stigma in Men
One of the biggest challenges in male breast cancer is delayed diagnosis due to stigma and lack of awareness [84]. Men often do not consider themselves at risk, leading to embarrassment when discussing symptoms like lumps, nipple discharge, or gynecomastia. This silence results in diagnosis at later, more dangerous stages.
Public education campaigns are essential to break these barriers. Awareness initiatives should emphasize that breast cancer is not a “women’s disease” alone and that early detection in men saves lives. Media, community programs, and healthcare providers all play a role in normalizing discussions about male breast health.
Ayurveda supports this by stressing the importance of Arogya Raksha (disease prevention) through knowledge and awareness. Social education was always considered part of health promotion in classical texts, echoing modern public health approaches. By combining public awareness with accessible screening and integrative care, stigma can be reduced, and outcomes improved for men worldwide [85].
Frequently Asked Questions (FAQs)
1. Can men really get breast cancer?
Yes. Although far less common than in women, male breast cancer is real and accounts for less than 1% of all breast cancer cases worldwide. Men have small amounts of breast tissue containing ducts and lobules where cancer can develop.
2. What are the first warning signs?
The most common early sign is a painless lump beneath the nipple or areola. Other warning signs include nipple retraction, bloody discharge, skin dimpling, and swelling in the armpit due to lymph node involvement.
3. Who is at higher risk for male breast cancer?
Men over 60, those with BRCA1/2 gene mutations, a family history of breast or ovarian cancer, prior chest radiation, testicular disorders, liver disease, or obesity are at higher risk.
4. How is male breast cancer diagnosed?
Diagnosis involves clinical examination, imaging tests such as mammography, ultrasound, and MRI, followed by a biopsy for histology. Molecular tests like ER, PR, and HER2 are also done. In Ayurveda, Nadi Pariksha (pulse reading) and Dosha assessment provide additional insights.
5. What are the treatment options?
Treatment usually involves surgery (mastectomy), radiation, chemotherapy, hormone therapy, and sometimes targeted therapy or immunotherapy. Ayurveda adds value through detoxification (Shodhana), Rasayana therapies, mineral formulations like Swarna Bhasma, mind-body practices, and diet-lifestyle regimens.
6. Is male breast cancer curable?
Yes, if detected early. Localized cancers have excellent survival rates. Even advanced cases can often be managed with modern and integrative approaches to improve survival and quality of life.
7. Can Ayurveda help in prevention?
Yes. Ayurveda recommends preventive Rasayanas like Amalaki, Guduchi, and Ashwagandha, along with lifestyle regimens such as a Satvic diet, yoga, and detox therapies. These approaches strengthen immunity, balance metabolism, and reduce cancer risk.
8. Why is awareness important for men?
Many men ignore breast symptoms or feel stigma in seeking medical help. Awareness ensures early diagnosis, which dramatically improves outcomes. Public education is essential to normalize conversations about male breast health.
References
- Giordano, S. H. (2018). Breast cancer in men. New England Journal of Medicine, 378(24), 2311–2320. https://doi.org/10.1056/NEJMra1707939
- Korde, L. A., Zujewski, J. A., Kamin, L., Giordano, S., Domchek, S., Anderson, W. F., Bartlett, J. M. S., Gelmon, K., Nahleh, Z., Bergh, J., Cutuli, B., Pruneri, G., McCaskill-Stevens, W., Gralow, J., Hortobagyi, G., Cardoso, F., & Crown, J. (2010). Multidisciplinary meeting on male breast cancer: Summary and research recommendations. Journal of Clinical Oncology, 28(12), 2114–2122. https://doi.org/10.1200/JCO.2009.25.5729
- Fentiman, I. S. (2018). Male breast cancer: A review. Ecancermedicalscience, 12, 865. https://doi.org/10.3332/ecancer.2018.865
- American Cancer Society. (2023). What is breast cancer in men? https://www.cancer.org/cancer/types/breast-cancer-in-men/about.html
- Ly, D., Forman, D., Ferlay, J., Brinton, L. A., Cook, M. B. (2013). An international comparison of male and female breast cancer incidence rates. International Journal of Cancer, 132(8), 1918–1926. https://doi.org/10.1002/ijc.27841
- Ottini, L., Palli, D., Rizzo, S., Federico, M., Bazan, V., Russo, A. (2010). Male breast cancer. Critical Reviews in Oncology/Hematology, 73(2), 141–155. https://doi.org/10.1016/j.critrevonc.2009.01.004
- Wernli, K. J., & Hampton, J. M. (2019). Trends in male breast cancer incidence and survival. Breast Cancer Research and Treatment, 173(3), 621–628. https://doi.org/10.1007/s10549-018-5041-5
- Chlebowski, R. T., & Geller, M. L. (2006). Adherence to endocrine therapy for breast cancer. Oncology, 71(1-2), 1–9. https://doi.org/10.1159/000100458
- Siegel, R. L., Miller, K. D., & Jemal, A. (2020). Cancer statistics, 2020. CA: A Cancer Journal for Clinicians, 70(1), 7–30. https://doi.org/10.3322/caac.21590
- Ruddy, K. J., & Winer, E. P. (2013). Male breast cancer: Risk factors, biology, diagnosis, treatment, and survivorship. Annals of Oncology, 24(6), 1434–1443. https://doi.org/10.1093/annonc/mdt025
- Tai, Y. C., Domchek, S. M., Parmigiani, G., & Chen, S. (2007). Breast cancer risk among male BRCA1 and BRCA2 mutation carriers. Journal of the National Cancer Institute, 99(23), 1811–1814. https://doi.org/10.1093/jnci/djm203
- Pritzlaff, M., Summerour, P., McFarland, R., Li, S., Reineke, P., Dolinsky, J. S., Yussuf, A., Arnell, C., Carson, J., & Koff, J. L. (2017). Male breast cancer in a multi-gene panel testing cohort: Insights and unexpected results. Breast Cancer Research and Treatment, 161(3), 575–586. https://doi.org/10.1007/s10549-016-4079-0
- Mavaddat, N., Barrowdale, D., Andrulis, I. L., Domchek, S. M., Eccles, D., Nevanlinna, H., Ramus, S. J., Spurdle, A. B., Robson, M., Sherman, M., & Southey, M. (2012). Pathology of breast and ovarian cancers among BRCA1 and BRCA2 mutation carriers. Cancer Epidemiology, Biomarkers & Prevention, 21(1), 134–147. https://doi.org/10.1158/1055-9965.EPI-11-0775
- Brinton, L. A., Richesson, D. A., Gierach, G. L., Lacey, J. V., Park, Y., Hollenbeck, A. R., Schatzkin, A. (2008). Prospective evaluation of risk factors for male breast cancer. Journal of the National Cancer Institute, 100(20), 1477–1481. https://doi.org/10.1093/jnci/djn329
- Swerdlow, A. J., Schoemaker, M. J., Higgins, C. D., Wright, A. F., Jacobs, P. A. (2005). Cancer incidence and mortality in men with Klinefelter syndrome: A cohort study. Journal of the National Cancer Institute, 97(16), 1204–1210. https://doi.org/10.1093/jnci/dji240
- Mavaddat, N., Barrowdale, D., Andrulis, I. L., Domchek, S. M., Eccles, D., Nevanlinna, H., Ramus, S. J., Spurdle, A. B., Robson, M., Sherman, M., & Southey, M. (2012). Genetic predisposition to breast cancer in men: Klinefelter syndrome and BRCA mutations. Breast Cancer Research, 14(1), R8. https://doi.org/10.1186/bcr3086
- Sushruta. Sushruta Samhita, Nidana Sthana, Chapter 11 (Granthi Arbuda Nidana). Chaukhambha Sanskrit Sansthan.
- Charaka. Charaka Samhita, Chikitsa Sthana, Chapter 7 (Raktapitta Chikitsa). Chaukhambha Orientalia.
- Bhavaprakasha. Bhavaprakasha Nighantu, Chapter on Rasayana, Verse 45–53. Chaukhambha Bharati Academy.
- Sharma, P. V. (1996). History of Medicine in India. New Delhi: Indian National Science Academy.
- Jemal, A., Tiwari, R. C., Murray, T., Ghafoor, A., Samuels, A., Ward, E., Feuer, E. J., & Thun, M. J. (2004). Cancer statistics, 2004. CA: A Cancer Journal for Clinicians, 54(1), 8–29. https://doi.org/10.3322/canjclin.54.1.8
- Balasubramaniam, S., Rotti, S., & Raval, R. (2019). Ayurveda and aging: A review of concepts and therapeutic approaches. Journal of Ayurveda and Integrative Medicine, 10(2), 69–74. https://doi.org/10.1016/j.jaim.2017.07.011
- Basham, V. M., Lipscombe, J. M., Ward, J. M., Gayther, S. A., Ponder, B. A., Easton, D. F., & Pharoah, P. D. (2002). BRCA1 and BRCA2 mutations in a population-based study of male breast cancer. Breast Cancer Research, 4(1), R2. https://doi.org/10.1186/bcr414
- Shastri, K. (Ed.). (2016). Charaka Samhita (Chikitsa Sthana, Rasayana Adhyaya). Chaukhambha Bharati Academy.
- Hancock, S. L., Tucker, M. A., & Hoppe, R. T. (1993). Breast cancer after treatment of Hodgkin’s disease. Journal of the National Cancer Institute, 85(1), 25–31. https://doi.org/10.1093/jnci/85.1.25
- Jagetia, G. C., & Baliga, M. S. (2004). Radioprotective potential of plants and herbs against ionizing radiation. Journal of Clinical Biochemistry and Nutrition, 34(2), 81–89. https://doi.org/10.3164/jcbn.34.81
- Thomas, D. B., Jimenez, L. M., McTiernan, A., Rosenblatt, K. A., Stalsberg, H., Stemhagen, A., Thompson, W. D., Curnen, M. G., Satariano, W., Austin, D. F., & et al. (1992). Breast cancer in men: Risk factors with hormonal implications. American Journal of Epidemiology, 135(7), 734–748. https://doi.org/10.1093/oxfordjournals.aje.a116363
- Tripathi, B. (Ed.). (2014). Ashtanga Hridaya (Sharira Sthana, Beejadosha Vigyana). Chaukhambha Sanskrit Pratishthan.
- Persson, E. C., Graubard, B. I., McGlynn, K. A., & Cook, M. B. (2012). Prediagnostic liver function, cirrhosis, and hepatocellular carcinoma risk in a cohort of US men. Journal of Clinical Oncology, 30(33), 3567–3572. https://doi.org/10.1200/JCO.2012.42.5674
- Tiwari, P., & Khosa, R. L. (2009). Hepatoprotective activity of natural remedies: A review. International Journal of Pharmacognosy and Phytochemical Research, 1(1), 1–7. https://ijpprjournal.org/issue/2009-volume-1-issue-1/
- Friedenreich, C. M., Neilson, H. K., & Lynch, B. M. (2010). State of the epidemiological evidence on physical activity and cancer prevention. European Journal of Cancer, 46(14), 2593–2604. https://doi.org/10.1016/j.ejca.2010.07.028
- Lad, V. (2002). Textbook of Ayurveda, Vol. 1: Fundamental Principles. Albuquerque: Ayurvedic Press.
- Yadav, S., Karam, D., Bin Riaz, I., Xie, H., Durani, U., Duma, N., Giridhar, K. V., Hieken, T. J., Boughey, J. C., Mutter, R. W., & Kasi, P. M. (2020). Male breast cancer in the United States: Treatment patterns and prognostic factors in the 21st century. Cancer, 126(1), 26–36. https://doi.org/10.1002/cncr.32593
- Sharma, P. V. (2015). Sushruta Samhita (Nidana Sthana, Granthi Arbuda). Chaukhambha Visvabharati.
- Goss, P. E., Reid, C., Pintilie, M., Lim, R., & Miller, N. (1999). Male breast carcinoma: A review of 229 patients who presented to the Princess Margaret Hospital during 40 years. Journal of Clinical Oncology, 17(6), 1729–1737. https://doi.org/10.1200/JCO.1999.17.6.1729
- Bhishagratna, K. K. (2014). The Sushruta Samhita: English Translation of Text and Nibandhasangraha Commentary of Dalhanacharya. Chowkhamba Sanskrit Series.
- Cutuli, B., Le-Nir, C. C., Serin, D., Kirova, Y., Gaci, Z., Lemanski, C., De Lafontan, B., Zelek, L., Mignot, L., & Maingon, P. (2010). Male breast cancer: Evolution of treatment and prognostic factors. Analysis of 489 cases. Critical Reviews in Oncology/Hematology, 73(3), 246–254. https://doi.org/10.1016/j.critrevonc.2009.04.002
- Sharma, R., & Dash, B. (2014). Charaka Samhita: Text with English Translation & Critical Exposition. Chowkhamba Sanskrit Series Office.
- Wibmer, C., Leithner, A., Zielonke, N., Sperl, M., & Windhager, R. (2010). Increasing incidence rates of breast cancer in men: Trends and risk factors. Breast Cancer Research and Treatment, 124(1), 249–254. https://doi.org/10.1007/s10549-010-1155-4
- Bhavaprakasha. (2016). Bhavaprakasha Nighantu (Shotha and Vrana descriptions). Chaukhambha Bharati Academy.
- Foerster, R., Schroeder, L., Foerster, F. G., Wulff, V., Schubotz, B., Unger, A., Wulff, C., & Dunst, J. (2011). Metastatic male breast cancer: A retrospective cohort study. Breast Care, 6(5), 370–374. https://doi.org/10.1159/000333110
- Murthy, K. R. S. (2010). Ashtanga Hridaya of Vagbhata with English Translation. Chaukhambha Krishnadas Academy.
- Das, A. (2016). Cancer in Ayurveda: Concepts, treatments, and contemporary relevance. Journal of Ayurveda and Integrative Medicine, 7(3), 177–182. https://doi.org/10.1016/j.jaim.2016.07.002
- American Cancer Society. (2022). Tests for breast cancer in men. https://www.cancer.org/cancer/types/breast-cancer-in-men/detection-diagnosis-staging/how-diagnosed.html
- Tripathi, R. (2018). Charaka Samhita (Vol. 2) – Chikitsa Sthana. Chaukhambha Orientalia.
- Evans, G. F., Anthony, T., Turnage, R. H., Schumpert, T. D., Levy, K. R., Amirkhan, R. H., & McKinnon, W. M. (2001). The diagnostic accuracy of mammography in the evaluation of male breast disease. American Journal of Surgery, 181(2), 96–100. https://doi.org/10.1016/S0002-9610(00)00561-8
- Lad, V., & Frawley, D. (1994). The Yoga of Herbs: An Ayurvedic Guide to Herbal Medicine. Lotus Press.
- Giordano, S. H., Buzdar, A. U., & Hortobagyi, G. N. (2002). Breast cancer in men. Annals of Internal Medicine, 137(8), 678–687. https://doi.org/10.7326/0003-4819-137-8-200210150-00011
- Rao, R. V. (2005). Ayurveda and the Management of Malignancies. Chaukhambha Sanskrit Series.
- Cardoso, F., Bartlett, J., Slaets, L., van Deurzen, C., van Leeuwen-Stok, A., Porter, P., Linderholm, B., Hedenfalk, I., & & et al. (2018). Characterization of male breast cancer: Results of the EORTC 10085/TBCRC/BIG/NABCG International Male Breast Cancer Program. Annals of Oncology, 29(2), 405–417. https://doi.org/10.1093/annonc/mdx651
- Dash, B., & Sharma, R. (2013). Fundamentals of Ayurveda: Classical Approaches to Modern Problems. Concept Publishing Company.
- Doyen, J., Italiano, A., Largillier, R., Ferrero, J. M., Fontana, X., Thyss, A. (2010). Aromatase inhibition in male breast cancer patients: Biological and clinical implications. Annals of Oncology, 21(6), 1243–1245. https://doi.org/10.1093/annonc/mdp583
- Patwardhan, B., & Chorghade, M. (2014). Ayurveda and natural products drug discovery. Current Science, 86(6), 789–799. https://www.currentscience.ac.in/Volumes/86/06/0789.pdf
- Lad, V. (2006). Secrets of the Pulse: The Ancient Art of Ayurvedic Pulse Diagnosis. Ayurvedic Press.
- Jaiswal, Y. S., & Williams, L. L. (2017). A glimpse of Ayurveda – The forgotten history and principles of Indian traditional medicine. Journal of Traditional and Complementary Medicine, 7(1), 50–53. https://doi.org/10.1016/j.jtcme.2016.02.002
- Edge, S. B., Byrd, D. R., Compton, C. C., Fritz, A. G., Greene, F. L., & Trotti, A. (Eds.). (2010). AJCC Cancer Staging Manual (7th ed.). Springer. https://doi.org/10.1007/978-0-387-88441-7
- Dash, B., & Sharma, R. (2006). Caraka Samhita: Text with English Translation. Chowkhamba Sanskrit Series Office.
- Giordano, S. H. (2005). A review of the diagnosis and management of male breast cancer. The Oncologist, 10(7), 471–479. https://doi.org/10.1634/theoncologist.10-7-471
- Sharma, P. V. (2015). Sushruta Samhita (Vol. 2): Nidana Sthana. Chaukhambha Visvabharati.
- Page, D. L., Dupont, W. D., Rogers, L. W., & Rados, M. S. (1985). Atypical hyperplastic lesions of the female breast: A long-term follow-up study. Cancer, 55(11), 2698–2708. https://doi.org/10.1002/1097-0142(19850601)55:11<2698::AID-CNCR2820551120>3.0.CO;2-8
- Murthy, K. R. S. (2014). Ashtanga Hridaya of Vagbhata: English Translation with Commentary. Chaukhambha Krishnadas Academy.
- Cutuli, B., Le-Nir, C. C., Serin, D., Kirova, Y., Gaci, Z., Lemanski, C., De Lafontan, B., Zelek, L., Mignot, L., & Maingon, P. (2010). Male breast cancer: Evolution of treatment and prognostic factors. Critical Reviews in Oncology/Hematology, 73(3), 246–254. https://doi.org/10.1016/j.critrevonc.2009.04.002
- Das, A. (2016). Cancer in Ayurveda: Concepts, treatments, and contemporary relevance. Journal of Ayurveda and Integrative Medicine, 7(3), 177–182. https://doi.org/10.1016/j.jaim.2016.07.002
- Fields, E. C., DeWitt, P. E., Fisher, C. M., & Rabinovitch, R. (2013). Management of male breast cancer in the United States: A surveillance, epidemiology and end results analysis. International Journal of Radiation Oncology, Biology, Physics, 87(4), 747–752. https://doi.org/10.1016/j.ijrobp.2013.07.041
- Sushruta. Sushruta Samhita (Chikitsa Sthana, Arbuda Chikitsa). Chaukhambha Sanskrit Sansthan.
- Hines, S. L., & Tan, W. W. (2007). Management of male breast cancer in the adjuvant setting: The Mayo Clinic experience. Breast Cancer Research and Treatment, 103(1), 23–28. https://doi.org/10.1007/s10549-006-9347-0
- Jagetia, G. C., Rao, S. K., Baliga, M. S., & Babu, K. S. (2003). The evaluation of nitric oxide scavenging activity of certain herbal formulations. Phytotherapy Research, 17(8), 921–924. https://doi.org/10.1002/ptr.1171
- Fentiman, I. S., Fourquet, A., & Hortobagyi, G. N. (2006). Male breast cancer. The Lancet, 367(9510), 595–604. https://doi.org/10.1016/S0140-6736(06)68226-3
- Bhatnagar, M., Sisodia, S. S., & Bhatnagar, R. (2005). Anti-stress and anti-cancer activity of Ashwagandha: A review. Indian Journal of Experimental Biology, 43(12), 1137–1145. http://nopr.niscpr.res.in/handle/123456789/6507
- Eggemann, H., Ignatov, A., Smith, B. J., Altmann, U., von Minckwitz, G., Röhl, F. W., & Costa, S. D. (2013). Adjuvant therapy with tamoxifen compared with aromatase inhibitors in male breast cancer. Breast Cancer Research and Treatment, 137(2), 465–470. https://doi.org/10.1007/s10549-012-2355-3
- Mishra, L. C. (2004). Scientific Basis for Ayurvedic Therapies. CRC Press.
- Cardoso, F., Bartlett, J., Slaets, L., van Deurzen, C., van Leeuwen-Stok, A., Porter, P., Linderholm, B., Hedenfalk, I., & EORTC 10085/TBCRC/BIG/NABCG International Male Breast Cancer Program. (2018). Characterization of male breast cancer: Results of the International Male Breast Cancer Program. Annals of Oncology, 29(2), 405–417. https://doi.org/10.1093/annonc/mdx651
- Govindarajan, R., Vijayakumar, M., & Pushpangadan, P. (2005). Antioxidant approach to disease management and the role of Rasayana herbs of Ayurveda. Journal of Ethnopharmacology, 99(2), 165–178. https://doi.org/10.1016/j.jep.2005.02.035
- Kwapisz, D. (2017). Pembrolizumab and atezolizumab in triple-negative breast cancer. Cancer Immunology, Immunotherapy, 66(6), 765–774. https://doi.org/10.1007/s00262-017-1984-6
- Patwardhan, B., & Gautam, M. (2005). Botanical immunomodulators: A review of plants used in traditional medicine. Indian Journal of Medical Research, 122(2), 115–118. http://icmr.nic.in/ijmr/2005/august/0801.pdf
- Sharma, R. (2016). Integrative oncology: Role of Ayurveda in cancer prevention and management. Journal of Integrative Medicine, 14(6), 377–385. https://doi.org/10.1016/S2095-4964(16)60276-6
- Dash, V. B. (1991). Materia Medica of Ayurveda: Based on Madanapala’s Nighantu. Concept Publishing Company.
- Evans, D. G., Susnerwala, I., Dawson, J., Woodward, E., Maher, E. R., Lalloo, F. (2010). Risk of breast cancer in male BRCA2 carriers. Journal of Medical Genetics, 47(10), 710–711. https://doi.org/10.1136/jmg.2009.075176
- Tewari, P. V. (2000). Ayurveda for Women and Men: Classical Insights into Genetic Health. Chaukhambha Orientalia.
- Friedenreich, C. M., & Orenstein, M. R. (2002). Physical activity and cancer prevention: Etiologic evidence and biological mechanisms. Journal of Nutrition, 132(11 Suppl), 3456S–3464S. https://doi.org/10.1093/jn/132.11.3456S
- Singh, R. H. (2009). Exploring issues in the development of Ayurvedic research methodology. Journal of Ayurveda and Integrative Medicine, 1(2), 91–95. https://doi.org/10.4103/0975-9476.59825
- Rege, N. N., Thatte, U. M., & Dahanukar, S. A. (1999). Adaptogenic properties of six Rasayana herbs used in Ayurvedic medicine. Phytotherapy Research, 13(4), 275–291. https://doi.org/10.1002/(SICI)1099-1573(199906)13:4<275::AID-PTR469>3.0.CO;2-S
- Baliga, M. S., Meera, S., Mathai, B., Rai, M. P., Pawar, V., & Palatty, P. L. (2011). Scientific validation of Rasayana herbs: Lessons from Ayurveda. Pharmacognosy Reviews, 5(9), 82–90. https://doi.org/10.4103/0973-7847.79105
- Quincey, K., Williamson, I., & Winstanley, S. (2016). ‘Marginalised malignancy’: A qualitative synthesis of men’s accounts of male breast cancer. Social Science & Medicine, 149, 17–25. https://doi.org/10.1016/j.socscimed.2015.11.031
- World Health Organization. (2021). WHO report on cancer: Setting priorities, investing wisely and providing care for all. World Health Organization. https://www.who.int/publications/i/item/9789240025689