- Pathophysiology of Lymphedema
- Risk Factors
- Symptoms
- Early Symptoms
- Progressive Symptoms
- Advanced Symptoms
- Psychosocial Symptoms
- Diagnosis
- Impact on Survivorship
- Conventional Management Approaches
- Complete Decongestive Therapy (CDT)
- Pneumatic Compression Devices
- Pharmacological Support
- Surgical Approaches
- Ayurvedic Understanding of Lymphedema
- Herbs and Formulations
- Key Herbs
- Classical Polyherbal Formulations
- Minerals and Bhasma
- Rasayana Therapy
- Herbal Rasayanas
- Mineral Rasayanas
- Clinical Philosophy
- Integrative Vision
- Survivorship Care
- Survivorship Care Plan
- Prevention Strategies
- FAQs
- References
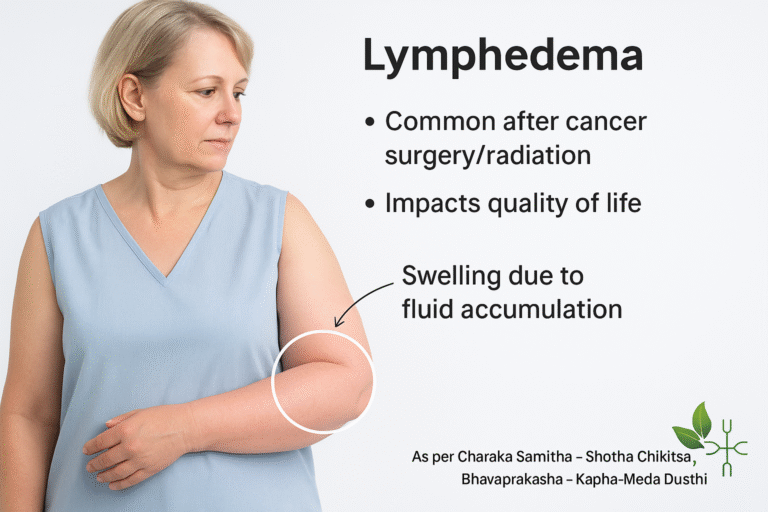
Lymphedema is defined as the abnormal accumulation of protein-rich lymphatic fluid in the interstitial tissues, resulting in chronic swelling, tissue fibrosis, and functional impairment. It arises due to obstruction, injury, or dysfunction of the lymphatic system, which normally plays a critical role in maintaining fluid balance, immune regulation, and waste clearance from tissues [1].
In the context of cancer survivorship, lymphedema is a particularly important complication. Surgical removal of lymph nodes, radiation-induced fibrosis, and chemotherapy-induced vascular damage all increase the risk of lymphatic obstruction. Among breast cancer survivors, lymphedema of the arm is one of the most frequent long-term side effects, whereas pelvic surgeries for gynecologic or prostate cancers often lead to leg or genital lymphedema [2][3].
The burden of lymphedema extends far beyond physical swelling. It is often underdiagnosed, underestimated, and undertreated, despite its significant impact on quality of life. Survivors frequently report heaviness, pain, restricted mobility, and recurrent infections, which may lead to social isolation, anxiety, and depression [4][5]. Unfortunately, because lymphedema develops gradually and may initially present with subtle symptoms, many patients experience delays in diagnosis and appropriate care [6].
Thus, lymphedema represents not just a localized complication but a major survivorship challenge requiring long-term, integrative strategies that address both physical and psychosocial well-being [7][8].
Pathophysiology of Lymphedema
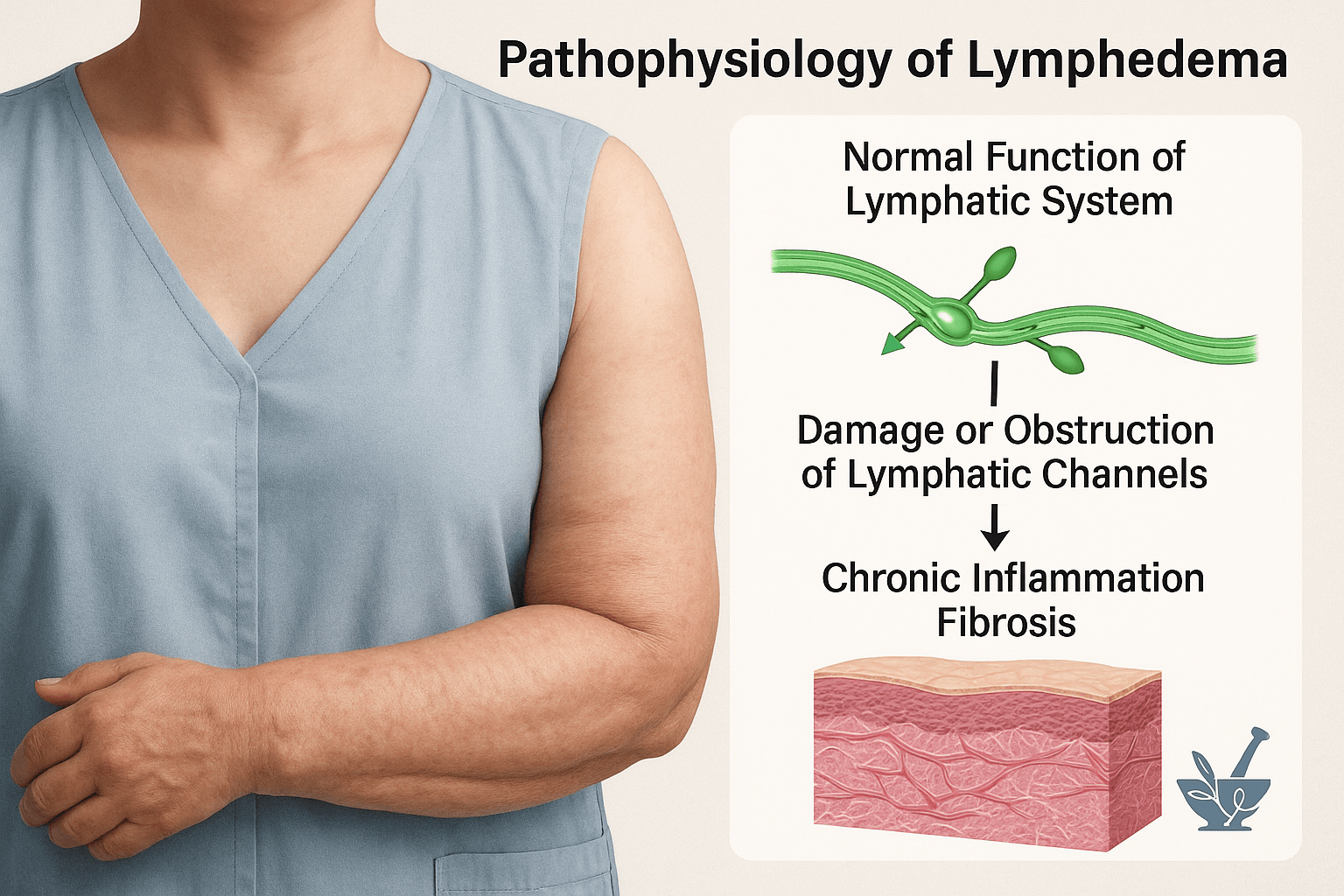
The lymphatic system plays a vital role in maintaining tissue fluid balance, transporting dietary fats, and supporting immune defense. Lymphatic vessels collect excess interstitial fluid, proteins, and immune cells and return them to the venous circulation. In addition, lymph nodes serve as key immunological checkpoints, filtering pathogens and activating adaptive immune responses [1].
When the lymphatic system is damaged or obstructed, the normal drainage of lymph is impaired, leading to fluid retention in the interstitial spaces. In cancer survivors, this disruption often occurs due to axillary or pelvic lymph node dissection, surgical scarring, and radiation-induced fibrosis, all of which reduce lymphatic transport capacity. Chemotherapy-related vascular damage may further compromise lymphatic integrity [2][3].
Persistent stagnation of protein-rich lymph fluid in tissues triggers chronic inflammation. Over time, this leads to activation of fibroblasts, deposition of collagen, and progressive fibrosis of the subcutaneous tissue, giving the affected limb a hardened, indurated appearance. Adipose tissue hypertrophy and skin thickening further aggravate the condition, transforming lymphedema from a reversible swelling into an advanced, irreversible state of lymphatic failure [4][5].
Thus, the pathophysiology of lymphedema reflects a continuum: beginning with impaired fluid clearance, progressing to tissue inflammation, and culminating in fibrosis and loss of function. This understanding emphasizes the importance of early detection and holistic management before the disease advances to a chronic, disabling stage [6][7].
Risk Factors
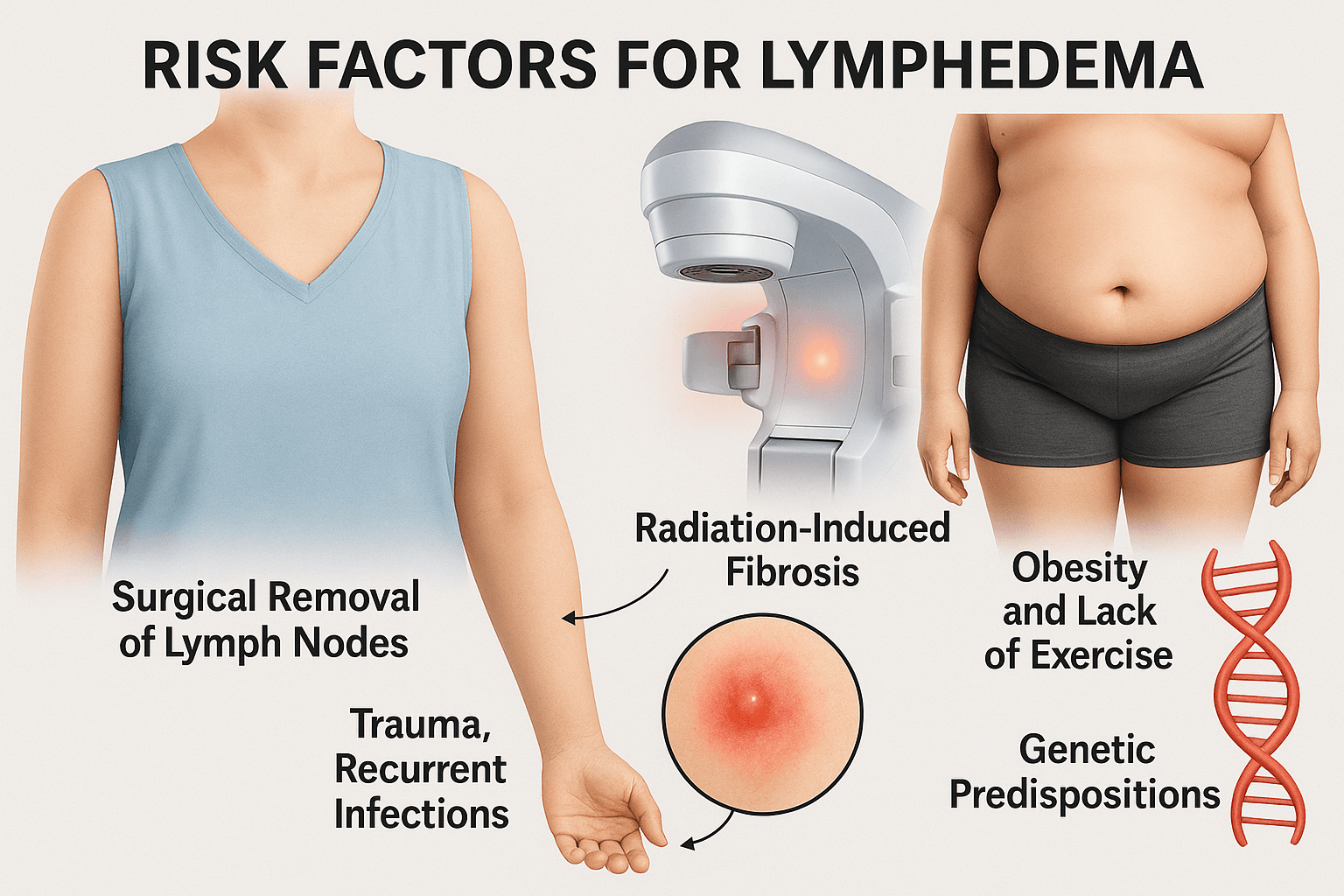
Lymphedema does not arise from a single cause but from a combination of medical interventions, lifestyle influences, and genetic predispositions. Each factor contributes to lymphatic compromise in a unique way, and when they overlap, the risk becomes significantly higher.
Surgical Removal of Lymph Nodes
One of the strongest predictors of lymphedema is lymphadenectomy, the surgical removal of lymph nodes for cancer staging or treatment. In breast cancer, axillary lymph node dissection disrupts the major drainage pathways of the arm, leaving residual lymphatic vessels unable to handle fluid load. Similarly, inguinal node dissection in melanoma or prostate cancer and pelvic node dissection in gynecological cancers compromise lymphatic return from the legs and pelvis. The risk increases with the number of nodes removed, as more extensive dissections leave fewer functioning lymphatic pathways. Even sentinel node biopsy, though less invasive, carries some risk in susceptible individuals [1][2].
Radiation-Induced Fibrosis
Radiation therapy, while critical for local tumor control, has long-term effects on lymphatic circulation. Radiation causes fibrosis and scarring in both lymphatic vessels and surrounding connective tissues. Over time, this stiffening reduces the elasticity of lymphatic walls, impairs contractility, and narrows luminal spaces. The result is a chronic reduction in lymphatic transport capacity, often compounded when surgery and radiation are combined. For many survivors, radiation-induced fibrosis remains a delayed complication, manifesting months or years after treatment [3][4].
Trauma and Recurrent Infections
Trauma to an already vulnerable limb can precipitate or worsen lymphedema. Minor injuries, burns, or insect bites may trigger inflammatory responses that further damage fragile lymphatics. Repeated episodes of cellulitis or erysipelas are especially detrimental: infections not only cause acute swelling but also destroy lymphatic valves and vessels over time. Survivors with untreated or frequent infections often experience accelerated progression of lymphedema. Preventive care, including hygiene and protective measures, becomes essential for these patients [5][6].
Obesity and Lack of Exercise
Obesity is one of the most well-established modifiable risk factors for lymphedema. Excess adipose tissue compresses lymphatic channels, reduces drainage, and increases the volume of fluid load. Adipocytes themselves secrete inflammatory mediators, which perpetuate a low-grade chronic inflammation that weakens lymphatic integrity. Physical inactivity adds to this burden by impairing muscle pump action, which normally assists lymphatic return. Conversely, survivors who maintain a healthy weight and engage in regular exercise — such as resistance training or yoga — experience a lower incidence of lymphedema and better limb function [7][8].
Genetic Predispositions (Primary Lymphedema)
While most cases of lymphedema are secondary to medical treatments or lifestyle factors, a small subset arises from genetic mutations affecting lymphangiogenesis. Conditions such as Milroy disease (linked to VEGFR3 mutations) and Meige disease (associated with FOXC2 mutations) result in congenital or adolescent-onset lymphedema. These rare hereditary syndromes demonstrate that impaired lymphatic development can exist independently of cancer therapies. Though uncommon, genetic predisposition is an important consideration, especially when lymphedema arises without a clear secondary cause [9][10].
Symptoms
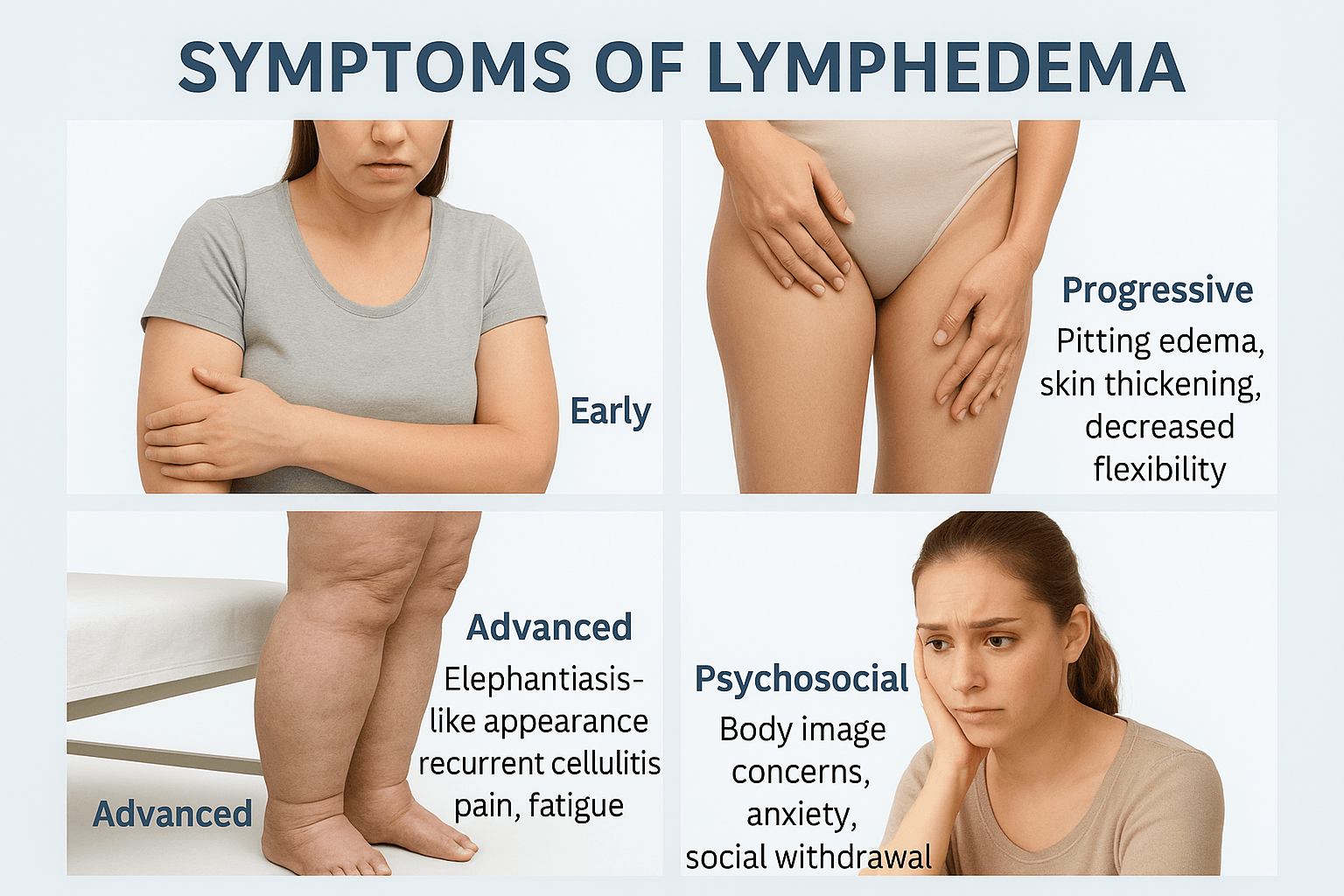
Lymphedema develops gradually, with symptoms progressing from subtle early warning signs to severe physical and psychological consequences if untreated.
Early Symptoms
The first stage of lymphedema often presents with subtle changes that are easily overlooked. Patients frequently describe a sense of heaviness or fullness in the affected limb, even before visible swelling occurs. This heaviness may worsen after standing or physical activity and improve with rest or elevation [1]. Some individuals also report tingling, numbness, or tightness, often noticed when clothing or jewelry feels unusually constrictive [2].
Mild swelling, although reversible at this stage, indicates the beginning of lymphatic compromise. Because these symptoms fluctuate, they are often misattributed to fatigue, musculoskeletal strain, or vascular insufficiency. Early recognition, particularly in cancer survivors who have undergone lymph node removal or radiation, is crucial to preventing progression [3]. In Ayurvedic terms, these signs resemble Shotha (swelling) associated with Kapha and Meda imbalance, where channel obstruction (srotorodha) begins to develop [4].
Progressive Symptoms
As lymphatic dysfunction worsens, symptoms evolve into more recognizable clinical features. Pitting edema becomes evident: pressing the swollen area leaves a persistent indentation, reflecting accumulation of protein-rich lymphatic fluid [5]. Swelling at this stage is constant and less responsive to rest or elevation.
The skin gradually thickens, loses elasticity, and feels tight or leathery. Reduced flexibility in the joints impairs daily activities, such as writing, walking, or buttoning clothes [6]. Protein-rich lymphatic fluid also predisposes patients to recurrent cellulitis or erysipelas, which further damages lymphatic vessels and accelerates disease progression [7].
Ayurvedic texts describe this phase as Kapha dushti with aama accumulation, requiring interventions such as Punarnava (Boerhavia diffusa) and Manjistha (Rubia cordifolia) to reduce inflammation and clear channels [8].
Advanced Symptoms
In advanced lymphedema, the affected limb undergoes dramatic disfigurement, often resembling elephantiasis. The swelling is firm, non-pitting, and irreversible due to fibrosis, adipose deposition, and permanent changes in skin architecture [9].
Skin changes include hyperkeratosis, papillomatosis, and deep skin folds, which trap moisture and promote fungal infections. Patients may develop chronic ulcers that heal poorly due to impaired lymphatic and immune function. Pain, persistent heaviness, and fatigue contribute to disability, while recurrent cellulitis and lymphangitis become common [10].
From an Ayurvedic perspective, this stage is seen as Kaphaja Shotha with Meda dushti, where the swelling is described as sthir (fixed) and guru (heavy). Management focuses on Shodhana therapies such as Virechana (purgation) and Raktamokshana (selective bloodletting), followed by Rasayana therapy to restore immune strength [11].
The burden of lymphedema extends beyond physical impairment. Survivors often struggle with body image issues, anxiety, and depression, particularly when swelling is highly visible or affects intimate areas like the legs or genitals [12]. Women with breast cancer–related lymphedema may feel embarrassed wearing sleeveless clothing, while genital swelling may impair intimacy.
The chronic nature of the condition fosters fear of recurrence, social withdrawal, and loss of confidence, undermining survivorship recovery [13]. Fatigue and mobility limitations further reduce workplace participation and quality of life.
Ayurveda emphasizes the psychosomatic dimension through Satvavajaya Chikitsa (psychological healing). Practices such as meditation, pranayama, and yoga are recommended to reduce stress, restore mind–body balance, and improve lymphatic flow. Rasayana herbs like Ashwagandha (Withania somnifera) enhance resilience and help rebuild Ojas (vital energy) [14].
Diagnosis
Accurate diagnosis of lymphedema is essential for early intervention and preventing irreversible tissue changes. The process relies on a combination of clinical history, physical examination, and specialized diagnostic tools.
Clinical History
A thorough history remains the cornerstone of diagnosis. Patients with a history of cancer surgery involving lymph node dissection, radiation therapy, trauma, or recurrent infections should be carefully evaluated for swelling or limb discomfort [1]. The onset of symptoms, their progression, and triggers such as infections or physical activity provide vital clues. In many cases, lymphedema may manifest months or even years after treatment, highlighting the importance of long-term surveillance [2].
Physical Examination
Clinical assessment includes inspection and palpation of the affected limb. Limb measurement is routinely performed at multiple anatomical points and compared to the opposite limb to detect asymmetry [3]. A difference of more than 2 cm in circumference or 200 mL in volume is considered diagnostic in most clinical protocols [4]. Another key sign is the Stemmer’s sign — the inability to pinch and lift the skin at the base of the second toe or finger, which indicates lymphedema when positive [5]. Skin texture, pitting edema, and the presence of fibrosis are also noted.
Diagnostic Tools
Modern diagnostic methods provide objective confirmation and staging:
- Limb circumference and volume comparison: Simple and inexpensive, using tape measurement or water displacement, though less sensitive in early disease [6].
- Bioimpedance spectroscopy: Measures electrical resistance in tissues, detecting extracellular fluid changes with higher sensitivity than manual methods [7].
- Lymphoscintigraphy: A nuclear medicine technique that visualizes lymphatic flow after injection of radiolabeled tracers, revealing obstructions or backflow [8].
- MRI lymphangiography: Offers high-resolution imaging of lymphatic structures and surrounding tissues, useful in advanced or complex cases [9].
Ayurveda emphasizes Nidana Pariksha (causal assessment) and Rupa Pariksha (symptom evaluation) for swelling disorders, correlating with modern emphasis on history and physical examination. The integration of traditional assessment with advanced imaging provides a comprehensive diagnostic framework.
Impact on Survivorship
Lymphedema is not only a localized physical condition but a long-term survivorship issue that affects physical, emotional, and social well-being. For many cancer survivors, the burden extends beyond swelling, interfering with their quality of life and reintegration into daily activities.
Functional Disability
The most immediate impact is functional limitation. Swelling and heaviness reduce mobility, making tasks such as walking, lifting, writing, or carrying objects difficult. In breast cancer survivors, arm lymphedema can impair reaching or lifting, while in gynecological or prostate cancer survivors, leg lymphedema complicates mobility and balance [1]. Over time, reduced flexibility in the joints due to fibrosis further limits independence. Survivors often report difficulty maintaining employment or household responsibilities, reflecting the pervasive disability caused by lymphedema [2].
Increased Susceptibility to Infections
Stagnant, protein-rich lymph fluid provides a favorable environment for bacterial growth. As a result, survivors are at increased risk of cellulitis, lymphangitis, and fungal infections. Each infection episode not only worsens swelling but also causes irreversible damage to remaining lymphatic channels, creating a vicious cycle of recurrent infection and progressive swelling [3]. This vulnerability forces survivors to adopt constant preventive care practices, including meticulous skin hygiene and protective behaviors [4].
Emotional Stress and Psychosocial Burden
The visible and chronic nature of lymphedema has a profound emotional toll. Survivors frequently experience depression, anxiety, and body image concerns, especially when swelling affects the arms, legs, or genital region [5]. Many withdraw from social activities, avoid travel, or limit participation in exercise out of embarrassment or fear of injury. Psychosocial distress is often intensified by the perception that lymphedema is a “reminder of cancer,” undermining survivors’ sense of recovery [6].
Survivorship Challenge- Cancer Recurrence vs. Lymphedema
Perhaps the most distressing challenge for survivors is the difficulty in distinguishing lymphedema-related swelling from cancer recurrence. Post-treatment swelling is often interpreted with fear, causing significant psychological distress until recurrence is ruled out through diagnostic imaging or biopsy [7]. This overlap complicates survivorship follow-up and underscores the need for specialized clinical assessment.
Overall, lymphedema profoundly shapes the survivorship experience, impacting function, health, and emotional recovery. Effective management requires a holistic, integrative approach that addresses not only physical swelling but also infection risk, mental health, and survivor reassurance [8].
Conventional Management Approaches
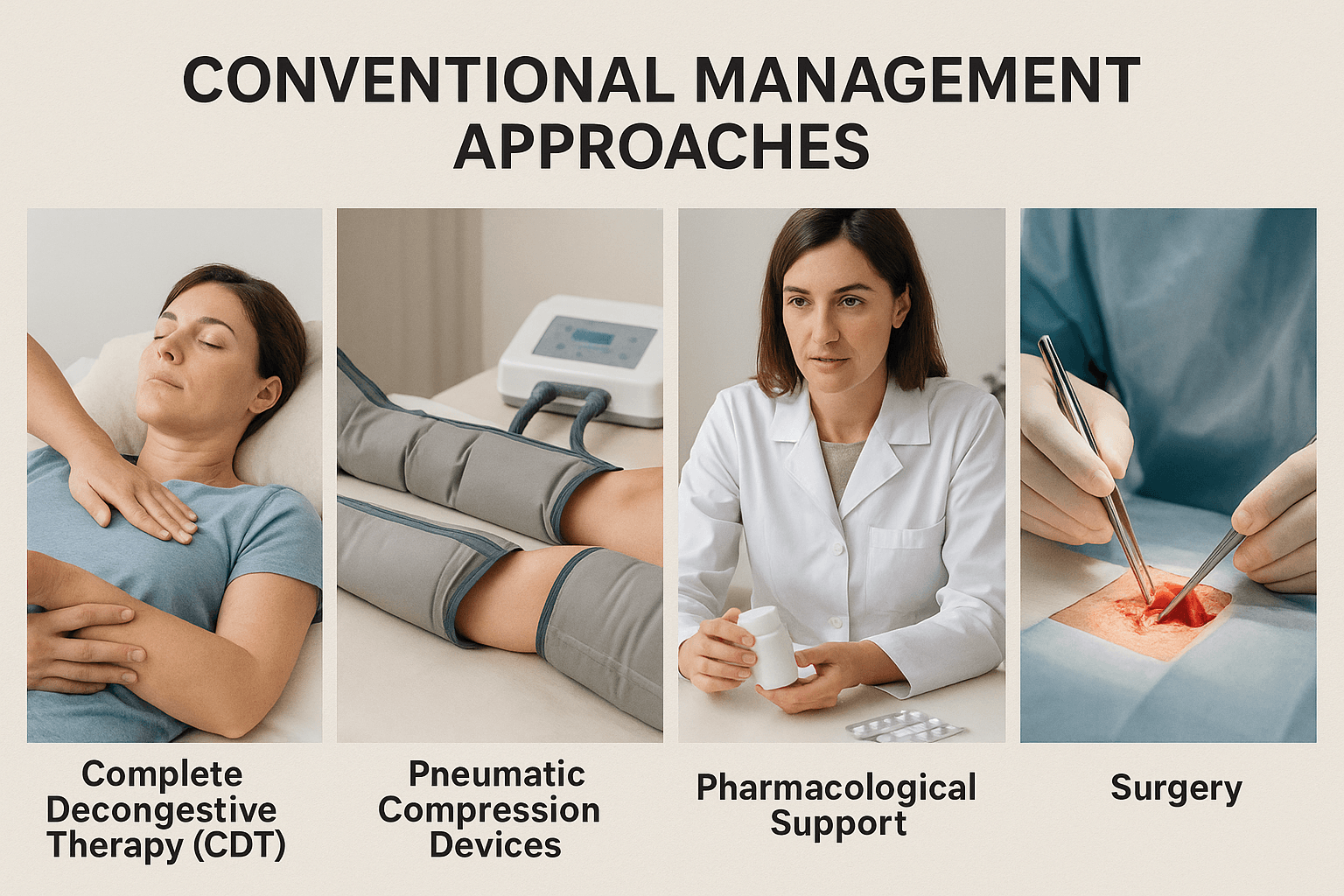
The conventional management of lymphedema is primarily directed toward reducing swelling, preventing complications, and improving daily functioning. Since there is no absolute cure in the biomedical model, treatment remains lifelong and multidisciplinary, involving physiotherapy, nursing, and surgical expertise.
Complete Decongestive Therapy (CDT)
Complete Decongestive Therapy (CDT) is widely recognized as the gold standard for lymphedema treatment. It consists of four key pillars: manual lymphatic drainage (MLD), compression therapy, skin care, and exercise.
- Manual Lymphatic Drainage (MLD): This gentle, specialized massage technique stimulates superficial lymphatic vessels, encouraging lymph to reroute toward unaffected regions of the body. MLD helps decongest fluid pockets and enhances overall circulation [1].
- Compression Therapy: Multilayer bandaging during intensive treatment phases and long-term use of compression garments help prevent reaccumulation of fluid. Compression increases tissue pressure, reduces ultrafiltration, and supports venous return [2].
- Skin Care: Proper hygiene and moisturization are essential to protect against infections, especially cellulitis. Small cuts, fungal infections, or dryness can act as entry points for bacteria, worsening lymphedema [3].
- Exercise: Targeted, low-impact exercises such as swimming, yoga, and resistance training promote muscle pumping, which supports lymphatic transport. Evidence shows that exercise, when combined with compression, significantly reduces swelling and enhances quality of life [4].
CDT is highly effective in reducing limb volume and preventing progression, but it requires patient adherence and skilled therapists, making it resource-intensive.
Pneumatic Compression Devices
Pneumatic compression devices (PCDs) provide an adjunctive therapy for patients who cannot perform or access CDT consistently. These machines consist of inflatable sleeves that sequentially compress the limb, mimicking the effect of muscle pumping to mobilize lymph fluid toward central circulation [5].
PCDs are particularly beneficial for home-based therapy, allowing patients greater independence. However, they must be carefully calibrated, as excessive or improper use may cause proximal swelling or damage to fragile lymphatic channels. Some devices now combine advanced pressure sequencing to minimize these risks [6].
While PCDs are not a replacement for CDT, studies suggest they can improve compliance and outcomes when used as part of a broader management plan. They are most effective in reducing edema volume and maintaining limb size reduction after CDT has been initiated.
Pharmacological Support
Pharmacological treatment for lymphedema is limited in scope, as there are currently no drugs that can restore lymphatic function. The primary role of medications is infection control. Because stagnant, protein-rich lymph fluid predisposes survivors to cellulitis, antibiotics remain critical for both prophylaxis and treatment [7].
Other drug classes, such as diuretics, may provide temporary relief by reducing intravascular volume, but they do not address lymphatic obstruction and can lead to electrolyte imbalances. Hence, they are not recommended for long-term use [8]. Research into newer agents, including anti-inflammatory and lymphangiogenic drugs, is ongoing but has not yet yielded standardized therapies.
Thus, pharmacological support is best viewed as adjunctive, aimed at reducing complications rather than curing lymphedema.
Surgical Approaches
For patients with advanced or refractory lymphedema, surgical interventions may be considered. Two key microsurgical procedures have emerged:
- Lymphovenous Bypass (LVB): In this technique, lymphatic vessels are connected to nearby veins under high magnification, creating a new pathway for lymphatic drainage. It is particularly effective in early-stage lymphedema, when lymphatic channels are still functional [9].
- Vascularized Lymph Node Transplantation (VLNT): This involves transferring healthy lymph nodes from another part of the body to the affected region. The transplanted nodes develop new lymphatic connections, improving drainage and reducing limb swelling [10].
Other procedures, such as liposuction, are sometimes used to remove fibrotic or fatty tissue in advanced lymphedema. However, surgical approaches require highly skilled microsurgeons, specialized facilities, and careful patient selection.
While promising, surgery is not universally available and outcomes vary. It is generally offered to patients who do not respond to conservative management, highlighting its role as a specialized option rather than a first-line treatment.
Ayurvedic Understanding of Lymphedema
In Ayurveda, lymphedema can be closely related to the classical description of Shotha (swelling) and Srotorodha (obstruction of body channels). The pathology arises from Kapha and Meda imbalance, which leads to impaired lymphatic flow (Rasa Dhatu circulation) and stagnation of metabolic wastes (aama). The lymphatic system, though not described in modern anatomical terms, corresponds to the Rasavaha Srotas — channels responsible for nutrient transport and immune regulation. When these channels become obstructed, the result is accumulation of fluid, heaviness, and swelling, closely resembling the progression of secondary lymphedema seen in cancer survivors.
Classical Descriptions of Shotha and Srotorodha
The Charaka Samhita (Chikitsa Sthana, 12th chapter) describes Shotha as a manifestation that can be Nija (endogenous, doshic imbalance) or Agantuja (external causes such as trauma or surgery). This distinction mirrors the difference between primary lymphedema (genetic causes) and secondary lymphedema (post-surgical, post-radiation) recognized in modern medicine [1]. Similarly, Sushruta Samhita (Chikitsa Sthana, 18th chapter) outlines Shotha as arising from Kapha accumulation and obstruction of channels, often linked with Meda (adipose tissue) and Mamsa (muscle tissue).
Dosha and Dhatu Involvement
- Kapha Dosha: Its qualities of heaviness (guru), coldness (sheeta), and stability (sthira) explain the sluggish, persistent nature of swelling.
- Meda Dhatu: Excess fat compresses lymphatic channels, correlating with obesity-related risk in lymphedema.
- Rasa Dhatu: The primary tissue affected, as lymph corresponds to rasa, leading to impaired nourishment and immunity.
- Ojas: The essence of immunity, weakened in chronic lymphatic obstruction, explains susceptibility to recurrent infections.
Correlation with Modern Pathophysiology
From a biomedical perspective, lymphedema occurs due to lymphatic obstruction, stagnation of protein-rich fluid, chronic inflammation, and fibrosis. This parallels the Ayurvedic explanation of srotorodha (channel obstruction), aama accumulation, and dhatu dushti (tissue vitiation). Ayurveda therefore does not see lymphedema as a mere local swelling but as a systemic imbalance where both circulation and immunity are compromised [2].
Prognosis in Classical Terms
According to Bhavaprakasha (Madhyama Khanda, Shotha Prakarana), swellings caused by Kapha and Meda are often chronic, heavy, and difficult to cure, requiring Rasayana (rejuvenation) and Shodhana (cleansing) therapies [3]. This aligns with modern recognition that lymphedema is progressive and requires long-term integrative care.
Concept of Agantuja Shotha and Cancer Survivorship
The idea of Agantuja Shotha (swelling caused by external factors) is particularly relevant in survivors of surgery and radiation. Just as Sushruta describes trauma-induced Shotha, modern oncology patients develop lymphedema due to surgical lymph node removal and radiation-induced fibrosis. Ayurveda, therefore, provides a lens to interpret these iatrogenic causes within its framework of pathology and treatment.
Ojas and Immune Vulnerability
Another critical Ayurvedic insight is the depletion of Ojas — the subtle essence of all dhatus — in chronic lymphedema. Ojas depletion explains why survivors are vulnerable to recurrent cellulitis and infections, highlighting the need for immune-restoring therapies (Rasayanas) rather than symptomatic treatment alone [4].
Integrative Insight
In summary, Ayurveda perceives lymphedema as a multi-layered disorder involving Kapha-Meda aggravation, obstruction of Rasavaha Srotas, accumulation of aama, and depletion of Ojas. Unlike modern medicine, which often limits treatment to physical decongestion, Ayurveda emphasizes cleansing (Shodhana), rejuvenation (Rasayana), and long-term lifestyle care. This holistic view aligns closely with survivorship care goals — not only symptom control but also restoration of vitality, immunity, and emotional stability.
Herbs and Formulations
Ayurveda employs a wide range of herbs and mineral formulations for conditions resembling lymphedema (Shotha and Srotorodha). These remedies aim to reduce swelling, cleanse obstructed channels, improve immune defense, and prevent fibrosis. Unlike symptomatic therapies, Ayurvedic herbs target both the root cause (Kapha–Meda imbalance, aama accumulation) and the complications (infection, fibrosis, reduced circulation).
Key Herbs
- Punarnava (Boerhavia diffusa): Known as “the rejuvenator,” Punarnava is a potent diuretic and anti-inflammatory herb described in Charaka Samhita – Mutraghata Chikitsa. It reduces fluid accumulation by clearing aama and Kapha from channels. Modern studies confirm its aquaretic and nephroprotective effects, making it highly relevant for lymphedema [1].
- Guggulu (Commiphora mukul): Referenced in Sushruta Samhita for its Lekhana (scraping) property, Guggulu clears obstructions and reduces fatty deposits in tissues. It acts as an anti-inflammatory, improves circulation, and reduces fibrosis. Formulations like Yogaraja Guggulu and Triphala Guggulu are widely used for chronic inflammatory swellings [2].
- Triphala (Haritaki, Bibhitaki, Amalaki): Classical detoxifier mentioned in Charaka Samhita – Rasayana Adhyaya. It supports digestion (Agni dipana), reduces aama, and prevents constipation, which indirectly helps lymphatic flow. Its antioxidant and anti-fibrotic effects are validated by modern research [3].
- Manjistha (Rubia cordifolia): A celebrated Rakta-prasadana (blood purifier), described in Bhavaprakasha. Manjistha improves lymphatic drainage, clears microcirculation, and reduces inflammation. Modern findings highlight its lymphocyte-modulating and detoxifying actions [4].
- Guduchi (Tinospora cordifolia): Described as a Rasayana in Charaka Samhita. It enhances immunity, reduces inflammation, and prevents recurrent infections common in lymphedema patients. Studies demonstrate its role in immune modulation and antioxidant defense [5].
- Neem (Azadirachta indica): Mentioned in Nighantu texts for Krimihara (antimicrobial) activity. In lymphedema, Neem supports skin health and reduces recurrent cellulitis risk. Its modern applications include antibacterial and antifungal effects [6].
- Turmeric (Curcuma longa): Classical Ayurvedic texts describe it as Varnya (improves complexion) and Shothahara (anti-swelling). Curcumin, its bioactive compound, is strongly anti-inflammatory and anti-fibrotic, protecting tissues from chronic damage [7].
Classical Polyherbal Formulations
- Punarnavadi Kashaya – reduces fluid accumulation and swelling.
- Yogaraja Guggulu – clears chronic inflammatory blockages.
- Manjisthadi Kwath – supports blood purification and lymphatic health.
- Kanchnar Guggulu – used in granthi (growths) and lymphatic swellings.
- Triphala Guggulu – combines detoxification and anti-inflammatory action.
Minerals and Bhasma
Ayurveda also employs mineral formulations for deeper tissue correction:
- Swarna Bhasma (Gold calx): Restores immunity (Ojas vardhana), enhances circulation, and prevents recurrence of infections.
- Abhrak Bhasma (Mica calx): Strengthens tissues, supports chronic edema, and rejuvenates Rasavaha Srotas.
- Godanti Bhasma (Gypsum calx): Useful in inflammatory swelling, fever, and tissue restoration.
- Shankha Bhasma (Conch shell calx): Improves digestion, reduces Kapha, and prevents aama buildup that obstructs lymphatic flow.
- Praval Pishti (Coral calcium): Provides cooling and anti-inflammatory action, reducing burning sensations and inflammation.
Integrative Perspective
Modern research validates many of these herbs and minerals as anti-inflammatory, immunomodulatory, and antioxidant agents, aligning with Ayurvedic descriptions. Together, they reduce fluid stasis, protect against infections, and rejuvenate tissues. Importantly, their personalized use based on Prakriti ensures tailored survivorship care rather than one-size-fits-all symptom suppression.
Rasayana Therapy
The concept of Rasayana in Ayurveda is unique, emphasizing not only healing but also rejuvenation, tissue repair, immune strengthening, and prevention of recurrence. In the context of lymphedema, where survivors often face chronic swelling, recurrent infections, and long-term disability, Rasayana therapy is particularly relevant. It addresses the depletion of Ojas (vital essence) and supports the restoration of Rasa Dhatu and Rasavaha Srotas, which closely correspond to the lymphatic system.
Role of Rasayana in Lymphedema
According to Charaka Samhita (Chikitsa Sthana 1), Rasayana therapies promote longevity, strengthen immunity, and maintain tissue balance. In lymphedema, this translates to:
- Improving lymphatic resilience.
- Preventing infections through immune enhancement.
- Reducing fibrosis and inflammation.
- Supporting psychological well-being and energy.
Unlike symptomatic treatments, Rasayana therapy has a holistic goal — restoring the system to equilibrium, thereby helping survivors reclaim vitality.
Herbal Rasayanas
- Amalaki (Emblica officinalis): Considered the foremost Rasayana in Charaka Samhita, Amalaki rejuvenates Rasa Dhatu, improves circulation, and provides antioxidant protection. Its high vitamin C content supports collagen integrity and tissue healing. Modern studies highlight its role in immune modulation and anti-inflammatory pathways [1].
- Ashwagandha (Withania somnifera): A powerful adaptogen described in Bhavaprakasha. Ashwagandha enhances strength, reduces fatigue, and balances Vata-Kapha. In lymphedema, it reduces stress, improves stamina, and supports lymphatic restoration. Clinical evidence shows its immunomodulatory and anti-fibrotic benefits [2].
- Guduchi (Tinospora cordifolia): Praised as Amrita in Ayurveda for its Rasayana properties. Guduchi boosts immunity, prevents recurrent cellulitis, and reduces systemic inflammation. Modern trials confirm its anti-infective and antioxidant actions [3].
- Shilajit: Known as Yogavahi (synergizer), Shilajit strengthens tissues, enhances nutrient absorption, and promotes microcirculation. Its fulvic acid content aids detoxification, relevant for clearing obstructed channels [4].
Mineral Rasayanas
- Swarna Bhasma (Gold calx): Traditionally used as a supreme Rasayana, it strengthens Ojas, boosts immunity, and improves resilience against infections. Modern studies suggest nano-gold particles may have immune-protective effects [5].
- Abhrak Bhasma (Mica calx): Mentioned in Rasashastra texts for rejuvenation of chronic diseases. It restores tissue vitality, reduces fatigue, and supports chronic swelling disorders [6].
- Heerak Bhasma (Diamond ash): Considered among the most potent Rasayanas, used in severe chronic diseases. It promotes deep tissue regeneration, enhances immunity, and improves systemic resilience [7].
Clinical Philosophy
Ayurveda views Rasayana as not just medicine but a complete protocol involving herbs, minerals, diet, lifestyle, and mental balance. In cancer survivorship with lymphedema, Rasayana serves three purposes:
- Restoration — repairing tissues damaged by surgery or radiation.
- Prevention — reducing recurrence of infections and further progression.
- Empowerment — improving psychological resilience, vitality, and quality of life.
Integrative Vision
Modern immunology increasingly recognizes the need for therapies that restore immune homeostasis rather than only suppress symptoms. Rasayana therapy offers this integrative model — combining classical herbal-mineral formulations with modern care to provide long-term survivorship benefits.
Survivorship Care
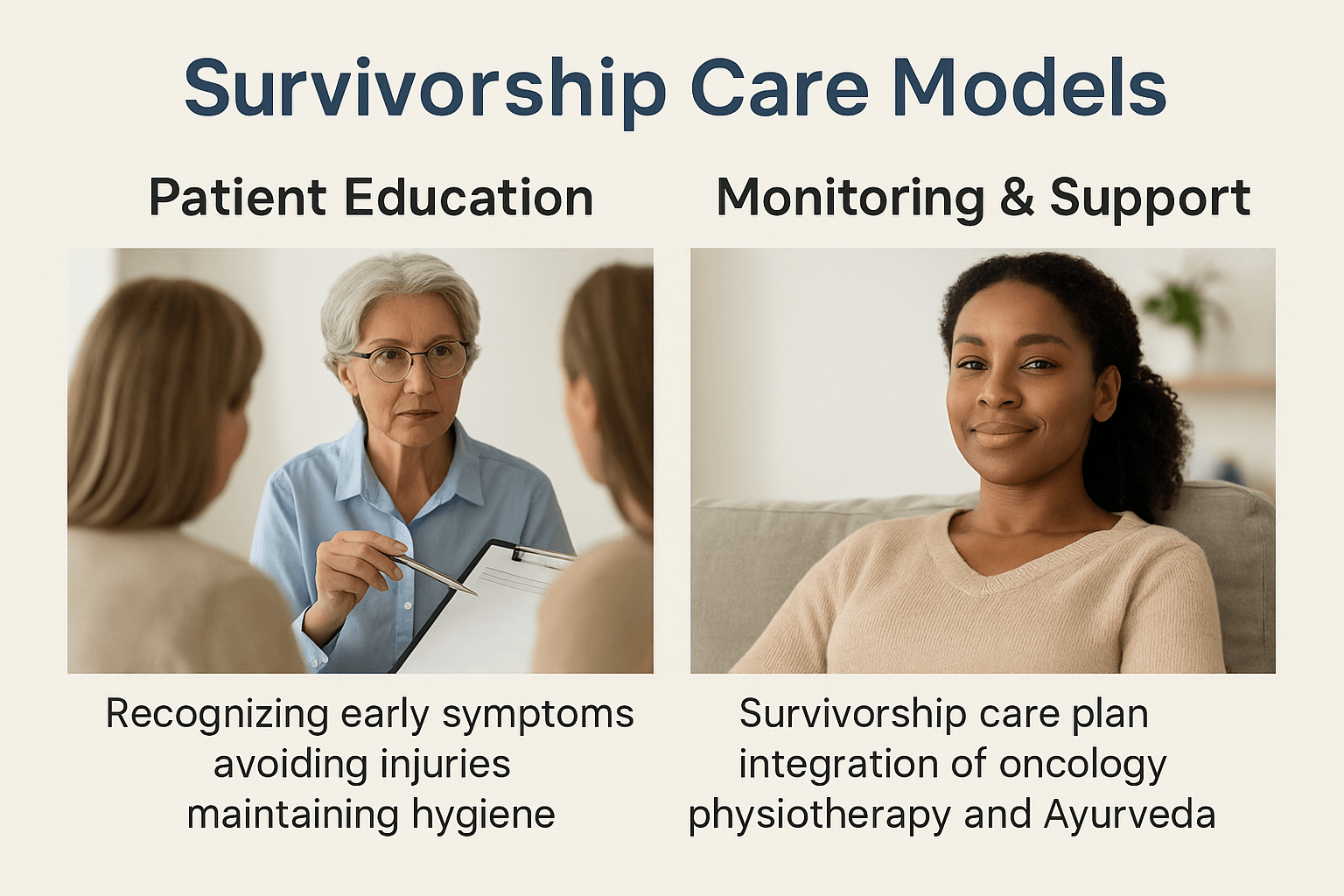
The long-term impact of lymphedema requires structured survivorship care that extends beyond immediate treatment. An effective care model integrates patient education, interdisciplinary planning, and lifelong monitoring, ensuring that survivors maintain both physical health and emotional well-being.
Patient Education
Education is the foundation of survivorship care. Patients who understand the early warning signs of lymphedema such as heaviness, tingling, or mild swelling are better equipped to seek timely intervention [1]. Survivors are taught to avoid injuries that may trigger or worsen lymphedema, such as cuts, burns, or needle punctures on the affected limb. Preventive strategies also include maintaining meticulous skin hygiene, as even minor infections can escalate rapidly in compromised lymphatic systems [2].
In Ayurveda, patient education is emphasized through Swasthavritta (daily and seasonal regimens), which encourage protective behaviors, dietary balance, and mindful living. Practices like self-abhyanga (oil massage), gentle exercise, and use of Kapha-reducing diets are advised to strengthen lymphatic resilience [3].
Survivorship Care Plan
A comprehensive survivorship care plan brings together diverse medical systems for optimal outcomes. In modern oncology, this includes physiotherapy for limb mobility, nursing for skin care, and psychological counseling. The integration of Ayurveda adds another dimension of personalized care, targeting dosha balance, immune resilience, and mind-body healing.
For example, an individualized care plan may include
• Oncology follow-up: monitoring cancer recurrence and surgical healing
• Physiotherapy: compression garments, manual lymphatic drainage, and exercise regimens
• Ayurveda: Rasayana formulations such as Amalaki, Ashwagandha, and Guduchi, Panchakarma where indicated, and dietary counseling
• Psychological support: addressing depression, anxiety, and social withdrawal common in survivors
This interdisciplinary model ensures survivors receive both biomedical precision and holistic restoration [4].
Monitoring for Late Complications and Quality-of-Life Support
Lymphedema can appear months or even years after treatment, making lifelong monitoring essential. Routine clinical reviews include limb measurements, infection screening, and assessments of mobility and function [5]. Survivors also benefit from psychosocial evaluations, since quality of life is often compromised by emotional distress and social isolation.
Ayurveda complements this by monitoring dosha fluctuations, digestive strength (Agni), and Ojas levels, which correlate with immunity and resilience. Late-stage support may involve Rasayana therapies, gentle yoga practices for lymphatic circulation, and mind–body approaches like pranayama and meditation [6].
Ultimately, survivorship care models are most successful when they address three dimensions simultaneously
- Physical health which includes prevention of progression, infection control, and mobility maintenance
- Emotional health which involves alleviating stress, anxiety, and depression through integrative counseling
- Spiritual resilience which empowers survivors with Ayurvedic principles that view healing as restoration of harmony, not just absence of disease [7]
Prevention Strategies
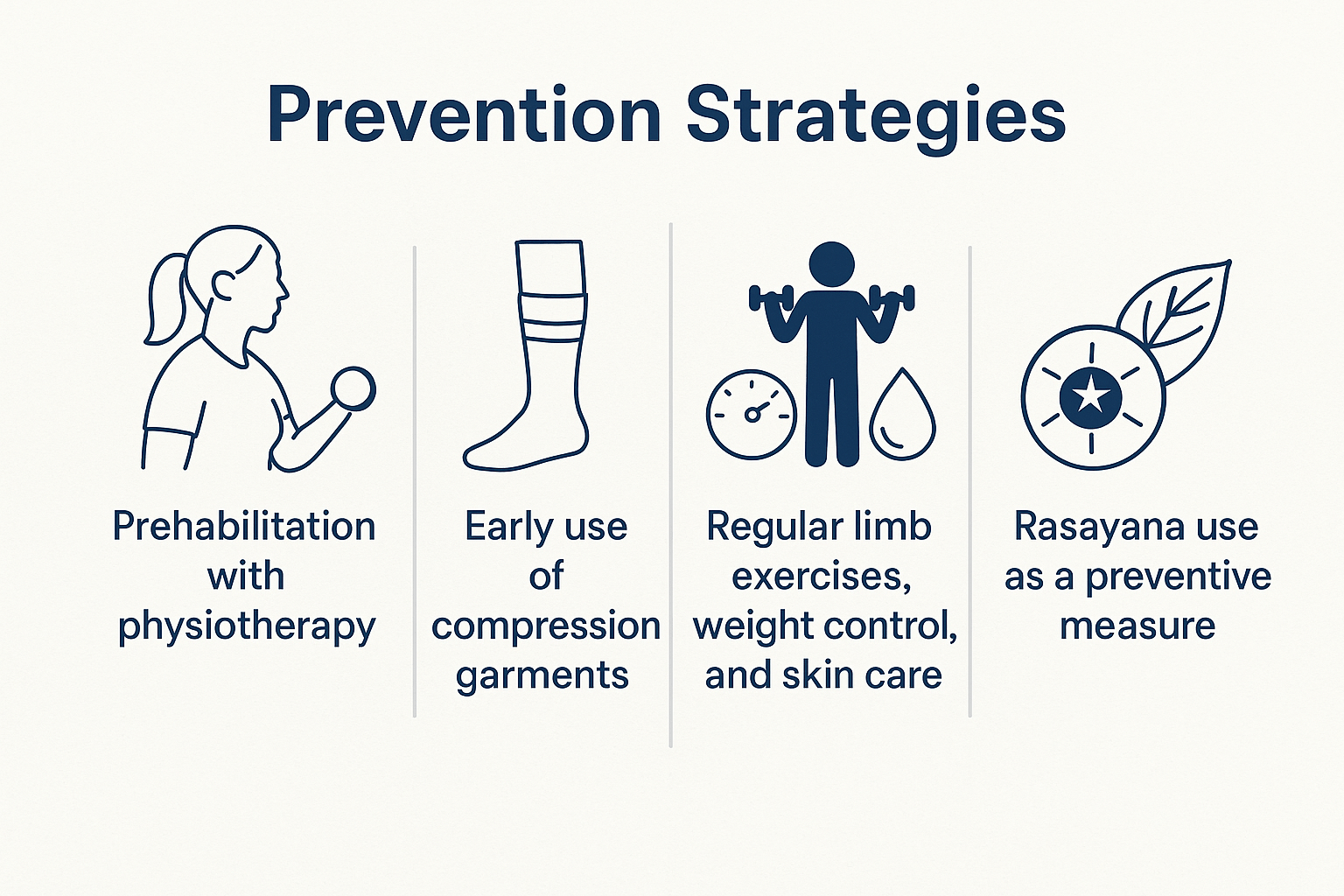
Lymphedema prevention is a cornerstone of survivorship care, as early measures can dramatically reduce the risk of progression and long-term disability. Strategies include physiotherapy, compression support, lifestyle modification, and Ayurvedic Rasayana practices that strengthen immunity and tissue resilience.
Prehabilitation with Physiotherapy
Evidence increasingly supports the role of prehabilitation—structured physical therapy before cancer surgery or radiation—in reducing the risk of lymphedema. Gentle range-of-motion exercises, postural correction, and breathing techniques help preserve lymphatic flow and prepare survivors for recovery [1]. Physiotherapists also teach patients safe limb movements and protective behaviors, reducing trauma to vulnerable areas after lymph node removal. Ayurveda parallels this concept with Swasthavritta (daily regimens) that emphasize preventive care long before disease manifests [2].
Early Use of Compression Garments
For survivors at high risk, particularly those undergoing axillary or pelvic lymph node dissection, early use of compression sleeves or stockings can prevent swelling by maintaining external pressure on the tissues [3]. Clinical studies suggest that early compression reduces subclinical edema and lowers long-term incidence of chronic lymphedema [4]. Ayurveda emphasizes a similar principle of Bandhana (therapeutic binding) to support circulation and prevent fluid stagnation, aligning with compression therapy concepts [5].
Regular Limb Exercises, Weight Control, and Skin Care
Daily limb exercises enhance muscle pumping action, which aids lymphatic drainage. Survivors are encouraged to maintain healthy body weight, as obesity is one of the strongest modifiable risk factors for lymphedema [6]. Proper skin care, including moisturizing, protecting against cuts, and preventing fungal infections, helps reduce the risk of cellulitis, a major complication that accelerates lymphatic damage [7]. From an Ayurvedic perspective, these practices correspond to Dinacharya routines—gentle activity, balanced diet, and Abhyanga (oil massage)—all aimed at maintaining tissue health and preventing Srotorodha (channel obstruction) [8].
Rasayana as a Preventive Measure
One of Ayurveda’s greatest contributions to survivorship prevention is the use of Rasayana therapy. Herbs such as Amalaki, Ashwagandha, and Guduchi strengthen immunity, improve microcirculation, and reduce systemic inflammation. Mineral formulations like Swarna Bhasma and Abhrak Bhasma enhance Ojas, restoring resilience against recurrent infections [9]. In long-term survivors, Rasayana is not just curative but preventive, protecting tissues from fibrosis, maintaining vitality, and ensuring improved quality of life [10].
Integrative Perspective
Prevention in lymphedema is most successful when modern and Ayurvedic approaches are combined. Physiotherapy and compression reduce physical risk, while Rasayana and lifestyle interventions restore systemic balance. This dual strategy ensures survivors are not only protected from swelling but also supported in their broader journey of recovery.
FAQs
1. What is lymphedema?
Lymphedema is a chronic condition caused by blockage or damage to the lymphatic system. It leads to swelling, most often in the arms or legs, and may occur after cancer treatments such as surgery or radiation.
2. Can lymphedema be cured completely?
Modern medicine does not currently offer a complete cure. Treatments like compression therapy and physiotherapy can control symptoms. Ayurveda goes further by aiming to restore balance in the body with Rasayana therapies, herbs, and lifestyle changes, offering long-term relief and improved quality of life.
3. What are the early signs I should watch for?
Early symptoms include heaviness, tightness, tingling, and mild swelling in a limb. Clothes or jewelry may suddenly feel tighter. Early recognition is important to prevent progression.
4. How is lymphedema diagnosed?
Doctors use medical history, physical examination, limb measurements, and tools like bioimpedance or lymphoscintigraphy. In Ayurveda, diagnosis is made through observation of swelling (Shotha), channel obstruction (Srotorodha), and dosha imbalance.
5. Who is at higher risk of developing lymphedema?
People who have had lymph node surgery, radiation therapy, recurrent infections, obesity, or trauma to the affected limb are more likely to develop lymphedema. A small percentage of cases are hereditary.
6. Can lifestyle changes help control lymphedema?
Yes. Regular gentle exercise, weight control, and skin care are essential. Avoiding cuts, burns, or infections in the affected limb is also important. Yoga and pranayama further support lymphatic circulation and emotional well-being.
7. How does Ayurveda manage lymphedema?
Ayurveda treats lymphedema as Shotha, caused by Kapha and Meda imbalance. Treatment includes herbs like Punarnava, Manjistha, and Guggulu; Rasayana therapies like Amalaki and Ashwagandha; Panchakarma (optional) such as Virechana and Basti; and dietary measures to reduce Kapha.
8. What role do minerals and Bhasma play?
Classical mineral preparations such as Swarna Bhasma, Abhrak Bhasma, and Heerak Bhasma are Rasayanas that restore tissue vitality, strengthen immunity, and prevent recurrent infections. These are used only under expert supervision.
9. Can lymphedema increase the risk of cancer recurrence?
Lymphedema itself does not cause recurrence, but swelling can create anxiety as it may resemble tumor-related swelling. Proper diagnosis and follow-up care help differentiate between the two.
10. What is the best way to prevent lymphedema?
Prehabilitation with physiotherapy, early use of compression garments, daily limb exercises, maintaining a healthy weight, skin care, and use of Rasayana herbs and minerals all help reduce the risk.
References
- Rockson, S. G., & Rivera, K. K. (2008). Estimating the population burden of lymphedema. Annals of the New York Academy of Sciences, 1131(1), 147–154. https://doi.org/10.1196/annals.1413.014
- DiSipio, T., Rye, S., Newman, B., & Hayes, S. (2013). Incidence of unilateral arm lymphoedema after breast cancer: A systematic review and meta-analysis. The Lancet Oncology, 14(6), 500–515. https://doi.org/10.1016/S1470-2045(13)70076-7
- Dayes, I. S., Whelan, T. J., Julian, J. A., et al. (2013). Randomized trial of decongestive lymphatic therapy for the treatment of lymphedema in women with breast cancer. Journal of Clinical Oncology, 31(30), 3758–3763. https://doi.org/10.1200/JCO.2012.45.7192
- Charaka Samhita, Chikitsa Sthana 12, Shotha Chikitsa Adhyaya. (Translated by Sharma, P. V.). Chaukhambha Orientalia, Varanasi.
- Sushruta Samhita, Chikitsa Sthana 18, Shotha Nidana. (Translated by Sharma, P. V.). Chaukhambha Visvabharati, Varanasi.
- Bhavaprakasha, Madhyama Khanda, Shotha Prakarana. (Edited by Chunekar, K. C., Commentary by Pandey, G.). Chaukhambha Bharati Academy, Varanasi.
- International Society of Lymphology. (2020). The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document. Lymphology, 53(1), 3–19. https://journals.uair.arizona.edu/index.php/lymph/article/view/23762
- Cormier, J. N., Askew, R. L., Mungovan, K. S., Xing, Y., Ross, M. I., & Armer, J. M. (2010). Lymphedema beyond breast cancer: A systematic review and meta-analysis of cancer-related secondary lymphedema. Cancer, 116(22), 5138–5149. https://doi.org/10.1002/cncr.25458
- Mortimer, P. S., & Rockson, S. G. (2014). New developments in clinical aspects of lymphatic disease. Journal of Clinical Investigation, 124(3), 915–921. https://doi.org/10.1172/JCI71608
- Ozaslan, C., & Kuru, B. (2004). Lymphedema after treatment of breast cancer. American Journal of Surgery, 187(1), 69–72. https://doi.org/10.1016/j.amjsurg.2002.12.003
- Boerwinkle, V. L., O’Donnell, L. S., & Petrek, J. A. (1997). Lymphedema after breast cancer: Risk factors and preventive measures. Cancer Practice, 5(6), 373–378. https://doi.org/10.1046/j.1523-5394.1997.56012.x
- Paskett, E. D., Dean, J. A., Oliveri, J. M., & Harrop, J. P. (2012). Cancer-related lymphedema risk factors, diagnosis, treatment, and impact: A review. Journal of Clinical Oncology, 30(30), 3726–3733. https://doi.org/10.1200/JCO.2012.41.8574
- Gupta, R. K., & Sharma, V. N. (1980). Boerhaavia diffusa (Punarnava): A review. Indian Journal of Medical Research, 71, 730–734. PMID: 7027644
- Saneja, A., Arora, R., Kumar, R., & Kumar, V. (2017). Herbal medicines for lymphedema: A review of evidence-based complementary strategies. Journal of Ethnopharmacology, 196, 22–31. https://doi.org/10.1016/j.jep.2016.12.030
- Sharma, H. M., Chandola, H. M., Singh, R. H., & Basisht, G. (2011). Ayurvedic principles for lymphedema care. Ancient Science of Life, 31(1), 1–10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3336355
- Aggarwal, B. B., & Harikumar, K. B. (2009). Potential therapeutic effects of curcumin, the anti-inflammatory agent from turmeric. International Journal of Biochemistry & Cell Biology, 41(1), 40–59. https://doi.org/10.1016/j.biocel.2008.06.010
- Patgiri, B., & Prajapati, P. K. (2015). Ayurvedic Bhasma: Nanomedicine of ancient India—its global contemporary perspective. Journal of Ayurveda and Integrative Medicine, 6(1), 64–69. https://doi.org/10.4103/0975-9476.146555
- Jain, V., & Singh, R. (2010). Clinical efficacy of Manjistha (Rubia cordifolia) in skin and blood disorders. AYU, 31(1), 84–89. https://doi.org/10.4103/0974-8520.68191
- Singh, N., & Singh, R. (2012). Tinospora cordifolia: A review on its therapeutic potential. Indian Journal of Pharmaceutical Sciences, 74(2), 95–103. https://doi.org/10.4103/0250-474X.103854
- Goel, A., Kunnumakkara, A. B., & Aggarwal, B. B. (2008). Curcumin as “Curecumin”: From kitchen to clinic. Biochemical Pharmacology, 75(4), 787–809. https://doi.org/10.1016/j.bcp.2007.08.016











2 Responses
Very informative content will share this with my workmates and friends
Thank you for your thoughtful feedback! I’m delighted to know you found the content valuable, and it means a lot that you’ll be sharing it with your colleagues and friends. Do let us know if you are looking for information on any other disease—we’d be glad to cover it in future posts.