Limb-Salvage & Reconstruction :- The history of surgical oncology has witnessed a dramatic transformation in the way limb-threatening diseases are approached. Until the late twentieth century, amputation was the dominant surgical option, especially in cases of osteosarcoma, Ewing sarcoma, and other aggressive bone or soft-tissue tumors [18]. While amputation provided oncological safety by ensuring wide margins, it came at an immense physical and psychological cost to patients, permanently altering mobility, body image, and overall quality of life [42].
The advent of limb-salvage surgery (LSS) has redefined this landscape. With the introduction of multimodal treatment—combining chemotherapy, radiotherapy, precision imaging, and advanced reconstructive surgery—limb preservation has become the standard of care for a majority of musculoskeletal tumors [9]. Current evidence shows that when properly indicated, limb-salvage offers comparable survival and recurrence rates to amputation, while simultaneously maintaining functional independence [34].
The core principle of limb-salvage surgery is balance: achieving adequate oncological clearance without compromising neurovascular integrity or biomechanical stability [21]. Once the tumor-bearing segment is excised, the focus shifts to reconstruction, where orthopedic and plastic surgeons collaborate to restore skeletal continuity, joint function, and soft-tissue coverage. This may involve endoprosthetic replacements, allograft transplantation, vascularized fibular grafts, or microsurgical free flaps tailored to the patient’s anatomy and prognosis [27].
Beyond surgical technique, the philosophy of limb-salvage embodies a profound psychological dimension. Preserving a patient’s limb often means preserving identity, dignity, and social reintegration. Studies reveal that patients who undergo limb-salvage report significantly higher scores in body image, emotional well-being, and return to work compared with amputees [13]. This highlights why modern oncology increasingly regards limb-salvage not only as a surgical choice but as a human-centered therapeutic paradigm.
From an integrative perspective, Ayurveda provides unique insights into post-surgical recovery and systemic resilience, but more importantly, it emphasizes root-cause cure (Mool Nidana Chikitsa) rather than palliation. Ancient texts affirm that disorders of bone (Asthi Dhatu), muscle (Mamsa Dhatu), and marrow (Majja Dhatu) can be completely corrected when the doshic imbalances are eliminated from their origin.
Charaka Samhita (Sutra Sthana 16/27):
व्याधेः हेतुसमुत्थानं निवार्येत तु कारणम्।
व्याधेः हेतुनिवृत्त्या हि व्याधीनां निवृत्तिः॥
Transliteration:
Vyādheḥ hetusamutthānaṁ nivāryeta tu kāraṇam |
Vyādheḥ hetunivṛttyā hi vyādhīnāṁ nivṛttiḥ ||
Translation:
“The true treatment lies in removing the root cause of disease, for only when the cause is eliminated does the disease itself cease.”
Sushruta Samhita (Sutra Sthana 15/48):
यतः कारणभूतं व्याधेः ततोऽभ्युपशमं भवेत्।
Transliteration:
Yataḥ kāraṇabhūtaṁ vyādheḥ tato’bhyupashamaṁ bhavet.
Translation:
“The cure must begin from the very source where the disease originates.”
Applying these timeless principles, Ayurveda approaches bone and soft tissue pathologies not as isolated events but as systemic imbalances. Correction of Agni (metabolic fire), purification of Srotas (channels), and rejuvenation of Dhatus (tissues) are seen as the foundations for lasting recovery [38].
Rasayana formulations such as Ashwagandha (Withania somnifera), Amalaki (Emblica officinalis), and Guduchi (Tinospora cordifolia) are recognized for accelerating tissue repair, improving bone strength, and supporting immune resilience [29]. Mineral preparations like Suvarna Bhasma (gold calx), Abhrak Bhasma (mica ash), and Pravala Pishti (coral) are traditionally documented in Bhaishajya Ratnavali and Rasendra Chintamani for restoring marrow, enhancing fracture healing, and dissolving abnormal growths [46].
Thus, while modern limb-salvage ensures the mechanical and functional preservation of the limb, Ayurveda complements it by addressing the energetic, immunological, and systemic root causes, offering the possibility of true cure rather than symptomatic management. Together, they represent a paradigm shift—one that preserves life, restores wholeness, and aligns surgical precision with holistic healing [15].
Indications and Patient Selection
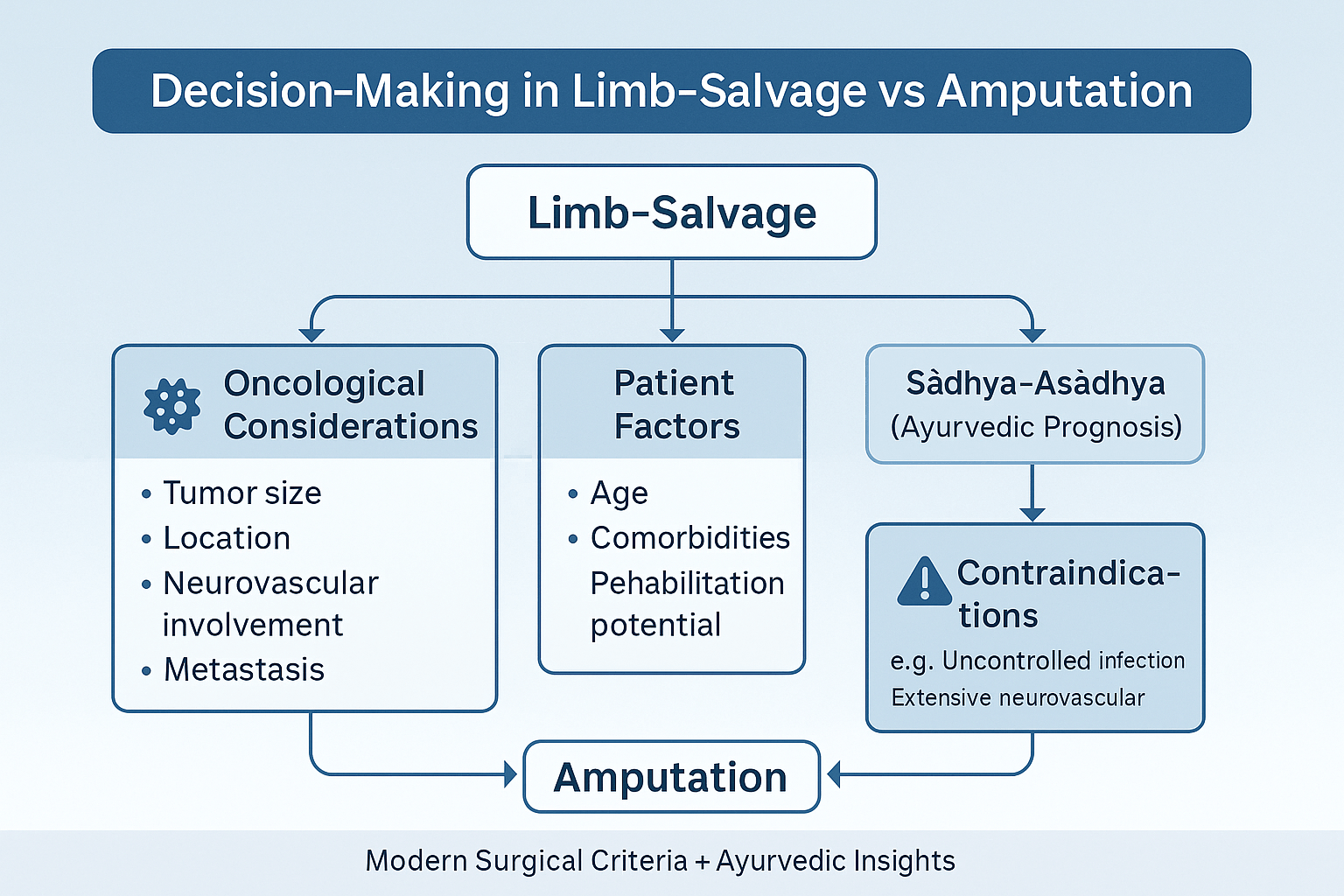
Criteria for Limb-Salvage over Amputation
Limb-salvage surgery (LSS) is considered the gold standard when the disease can be excised with clear oncological margins while preserving sufficient neurovascular and musculoskeletal structures to allow reconstruction [12]. Unlike historical practice, where amputation was the default, today up to 85–90% of bone and soft-tissue sarcoma cases are candidates for limb-salvage when treated in specialized centers [37]. The primary objective is to achieve local control equivalent to amputation but with improved functional and psychosocial outcomes [23].
Oncological Considerations
A central factor in decision-making is the tumor profile. Small- to medium-sized tumors with no encasement of major nerves or vessels are ideal candidates [41]. MRI and angiography are crucial in defining whether neurovascular bundles can be preserved. Tumors with skip metastases within the same bone may still qualify if wide en bloc resection is feasible. However, extensive marrow infiltration, fungating soft-tissue involvement, or uncontrolled systemic spread reduces the feasibility of limb-salvage [15].
Metastatic disease is not always a contraindication. Selected patients with solitary lung metastasis or oligometastatic disease may still undergo limb-salvage, provided systemic control is achievable [28]. Importantly, multidisciplinary tumor boards are essential in making such nuanced decisions.
Patient-Related Factors
The patient’s biological age, comorbidities, rehabilitation potential, and psychosocial environment play a decisive role. Younger patients with strong cardiopulmonary reserve and family support often benefit most from limb-salvage, regaining functional independence and quality of life [19]. Conversely, elderly patients with diabetes, vascular disease, or poor nutritional status may face higher risks of wound complications, infections, and implant failure [44].
Ayurveda adds another layer of insight here: by assessing Prakriti (constitutional type) and Bala (strength), physicians can anticipate healing capacity. For instance, a Kapha-dominant Prakriti patient may show stronger tissue regeneration, whereas a Vata-dominant profile may be prone to delayed healing, joint stiffness, and neuropathic pain [31]. Evaluating these subtle determinants allows personalized supportive protocols with Rasayana and Panchakarma therapies to optimize surgical recovery.
Contraindications
Despite advances, there remain circumstances where amputation remains the safer choice. These include:
- Uncontrolled infection, particularly deep osteomyelitis that compromises bone stock and endoprosthetic survival [22].
- Extensive neurovascular invasion where preservation would leave a non-functional, insensate limb.
- Poor soft-tissue envelope, when neither local nor free tissue transfer can provide durable coverage.
- Severe systemic disease, where the risks of prolonged reconstruction outweigh the potential benefits [35].
Ayurvedic texts echo similar principles of prognostic evaluation (Sadhya-Asadhyata), where conditions deemed Asadhya (incurable) due to depleted Ojas or irreversible Dhatu Kshaya (tissue depletion) are best managed by palliation rather than aggressive intervention. This holistic triage ensures resources are directed toward patients with genuine curative potential [47].
Preoperative Planning
Multidisciplinary Team Involvement
The success of limb-salvage surgery rests on meticulous preoperative planning by a multidisciplinary team (MDT). This team typically includes orthopedic oncologists, plastic and reconstructive surgeons, radiologists, medical oncologists, radiation specialists, physiotherapists, and rehabilitation experts [19]. The MDT ensures that oncological clearance, functional preservation, and reconstructive feasibility are balanced from the outset. In complex cases, early collaboration prevents delays and minimizes the need for revision surgery [41].
Ayurveda also emphasizes a team-based approach, though in different terminology. The Charaka Samhita describes the Chikitsa Chatushpada—the four pillars of successful therapy: the physician, the patient, the medicine, and the attendant. Preoperative planning reflects this principle, as patient education, physician expertise, supportive caregivers, and appropriate therapeutic interventions all converge to determine outcomes [33].
Imaging Modalities: MRI, CT, PET
Imaging forms the backbone of surgical planning. MRI provides unparalleled soft-tissue contrast, allowing surgeons to delineate tumor margins, evaluate neurovascular involvement, and plan incisions [12]. CT scans are essential for assessing cortical bone destruction and for 3D surgical modeling. PET scans help detect skip lesions and systemic spread, influencing the extent of surgery and the need for neoadjuvant therapy [44].
High-resolution imaging reduces the risk of positive margins and recurrence, making it indispensable in limb-salvage planning [29]. The concept resonates with Ayurvedic principles of Roga Pariksha (disease examination), where thorough visualization and mapping of disease spread (vyadhi vyapti) are prerequisites for definitive cure.
Biopsy Techniques and Surgical Approach
The biopsy is the single most critical diagnostic step, as an incorrectly performed biopsy can compromise future reconstructive options. Core needle biopsy is preferred, but in certain cases, open incisional biopsy may be warranted [15]. The biopsy tract must be placed longitudinally within the limb, aligned with the planned incision, so it can be excised during definitive surgery to avoid seeding [38].
Planning also includes anticipating the reconstructive method: whether an endoprosthesis, allograft, or vascularized fibular graft will be required, and whether free flap coverage is feasible. This “surgery within surgery” foresight reduces complications and accelerates recovery [21].
Ayurveda similarly stresses proper diagnostic entry points. In Nidana Panchaka (fivefold diagnostic framework), wrong assessment leads to Mithya Chikitsa (inappropriate treatment). Correctly placed biopsy parallels the principle of accurate Nidana, ensuring that the therapeutic path remains viable and curative [47].
Role of Neoadjuvant Chemotherapy and Radiotherapy
Preoperative neoadjuvant chemotherapy is now standard for osteosarcomas and certain soft-tissue sarcomas, shrinking tumors to facilitate resection and reduce micrometastases [13]. Radiotherapy, when applied preoperatively in select soft-tissue sarcomas, improves local control but raises wound complication rates, demanding precise coordination with reconstructive teams [22].
From an integrative view, Ayurveda complements this approach by preparing the body to withstand chemotherapy and surgery. Rasayana therapy—especially herbs like Guduchi (Tinospora cordifolia), Amalaki (Emblica officinalis), and Ashwagandha (Withania somnifera)—is documented to mitigate cytotoxic stress, preserve immunity, and enhance recovery potential [36]. Detoxification procedures (Shodhana, such as mild Virechana) may also be used selectively preoperatively to optimize tissue receptivity and metabolic strength [28].
Surgical Techniques in Limb-Salvage

Wide Local Excision and En Bloc Resection Principles
The foundation of limb-salvage surgery lies in achieving oncological clearance while preserving maximum functionality. Wide local excision requires removal of the tumor along with a cuff of surrounding normal tissue to ensure negative margins [21]. When the lesion is extensive, en bloc resection is performed, where the entire tumor-bearing segment of bone or soft tissue is removed in a single block [38]. The guiding principle is clear: “no compromise on margins for the sake of preservation.”
From an Ayurvedic standpoint, this correlates with the concept of “Nidana Parivarjana”—complete elimination of the root cause before attempting regeneration. Just as improper excision risks recurrence, Ayurveda emphasizes that incomplete elimination of doshic disturbance perpetuates disease [31].
Bone Reconstruction Options
Once tumor clearance is achieved, reconstruction restores skeletal stability and mechanical strength. The choice depends on the location, size of defect, patient age, and functional demand. Options include:
Endoprosthetic Replacement
Endoprosthetic reconstruction (also known as modular or custom mega prostheses) is one of the most widely adopted strategies in limb-salvage [17].
- Modular prostheses allow intraoperative flexibility, enabling surgeons to adapt to resection length.
- Custom prostheses are designed for anatomically complex regions such as the pelvis or scapula.
- These devices allow immediate weight-bearing and rapid rehabilitation, though risks include aseptic loosening, mechanical wear, and periprosthetic infection [44].
Biological Methods
For younger patients or when prostheses are not ideal, biological reconstruction is preferred:
- Allografts: Provide structural continuity but carry risks of non-union, fracture, and immunogenic rejection [19].
- Autografts: Vascularized fibula grafts are favored, especially in children, because of their ability to hypertrophy and remodel over time [23].
- Allograft-prosthetic composites: Combine biological integration with mechanical stability, useful in complex cases [35].
In Ayurveda, bone healing is linked to the strength of Asthi Dhatu (bone tissue) and the vitality of Majja Dhatu (marrow). Formulations like Asthi Shrinkhala (Cissus quadrangularis), Pravala Pishti (coral), and Abhrak Bhasma (mica ash) have been classically described to accelerate bone consolidation and marrow regeneration [29].
Soft Tissue Reconstruction
Adequate soft tissue coverage is crucial to protect underlying implants, prevent infection, and restore mobility. Surgeons utilize a spectrum of flaps, chosen based on defect size and location:
- Local flaps: Rotation or advancement of adjacent muscle or skin to cover defects.
- Free flaps: Microsurgical transfer of tissue (muscle or fasciocutaneous) from distant sites with vascular anastomosis [41].
- Perforator-based flaps: Preserve donor site function while providing reliable coverage.
This mirrors Ayurveda’s focus on Mamsa Dhatu (muscle tissue) replenishment through nourishing Rasayanas such as Ashwagandha (Withania somnifera) and Shatavari (Asparagus racemosus), which enhance tissue repair and restore functional strength [12].
Nerve and Vessel Grafting for Functional Recovery
When neurovascular bundles are partially involved, surgeons may perform segmental resection with grafting. Autologous nerve grafts (e.g., sural nerve) and vascular grafts (saphenous vein or synthetic substitutes) are used to restore continuity [27]. Although these procedures prolong surgery, they significantly improve functional recovery and limb sensation.
Ayurveda describes similar restoration through Majja Dhatu Rasayana, where formulations like Suvarna Bhasma (gold calx) and Guduchi (Tinospora cordifolia) are believed to support nerve conduction and vascular integrity [46].
Joint Reconstruction and Functional Preservation
Joint reconstruction is among the most challenging aspects of limb-salvage. Options include:
- Endoprosthetic joints (e.g., distal femur or proximal tibia replacements).
- Osteoarticular allografts, which preserve joint anatomy but risk graft collapse.
- Rotationplasty (particularly in pediatric cases), which maintains function by reorienting the limb, allowing the ankle to substitute for the knee joint [33].
The Ayurvedic lens interprets this as preservation of Sandhi (joints), which are sustained by the unison of Asthi and Mamsa Dhatus. Rasayanas like Guggulu (Commiphora mukul) and Dashamoola formulations are prescribed for joint health, anti-inflammatory action, and post-surgical mobility [18].
Reconstruction Approaches
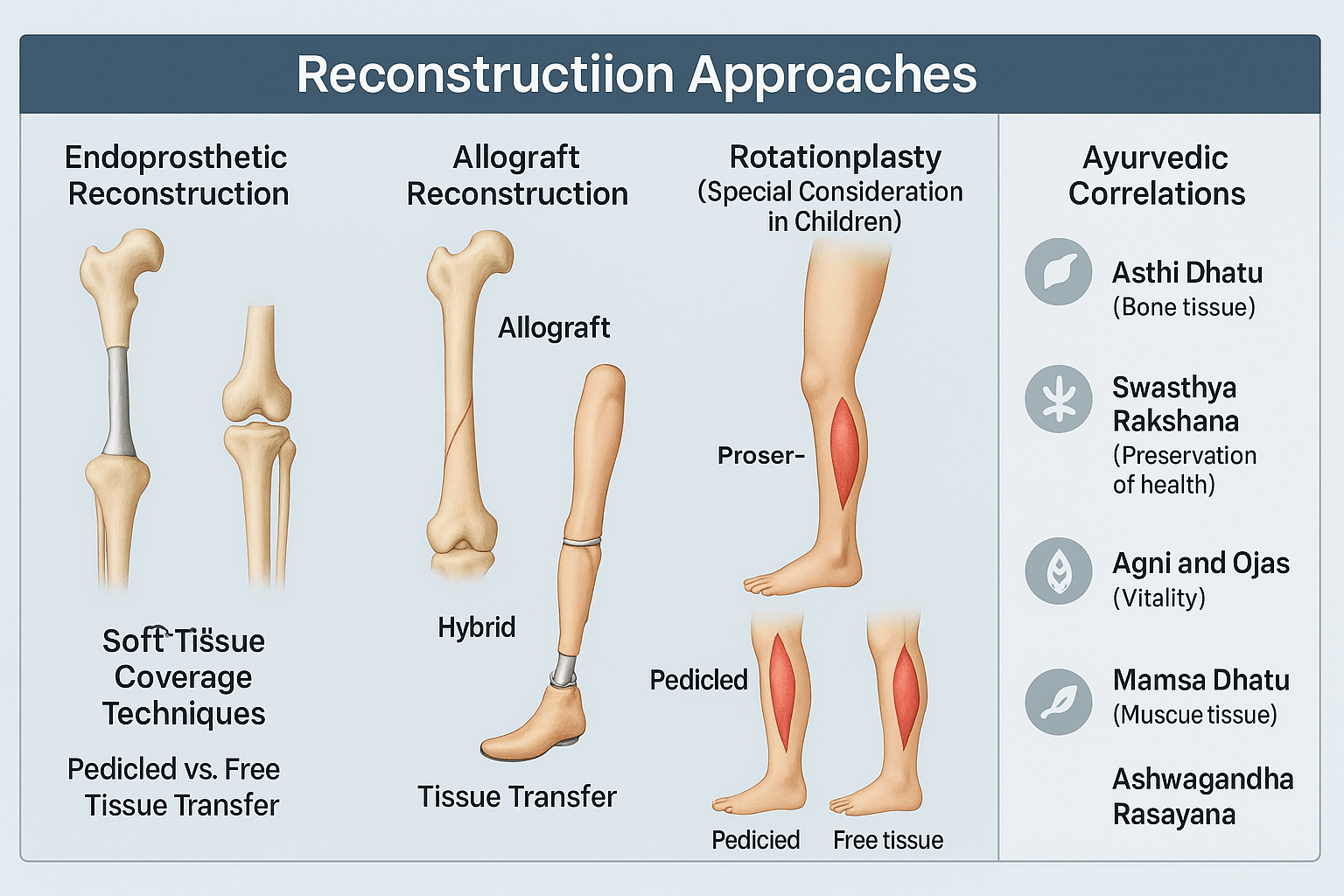
Endoprosthetic Reconstruction
Endoprosthetic reconstruction is the most frequently performed method following wide resections for bone sarcomas [21]. Modern modular endoprostheses allow intraoperative customization, accommodating variable lengths of bone resected. These implants provide immediate stability, enable early mobilization, and restore function with minimal donor site morbidity [38].
However, complications include aseptic loosening, mechanical wear, periprosthetic infection, and implant breakage over time [12]. For younger patients, the long-term durability of prostheses remains a concern, often necessitating revision surgeries.
Ayurveda interprets this as a replacement of Asthi Dhatu (bone tissue) by artificial material, which restores form but does not fully regenerate vitality. Hence, Rasayana support with Suvarna Bhasma (gold calx) and Abhrak Bhasma (mica ash) is considered essential for improving integration, strengthening residual bone, and enhancing systemic immunity [33].
Allograft Reconstruction
Massive allografts harvested from bone banks are another established option, particularly for young patients with high functional demands [41]. Allografts preserve anatomy and allow reattachment of tendons and ligaments, providing near-normal biomechanics. Over time, they can biologically incorporate into the host skeleton.
Challenges include non-union, graft fracture, collapse, and infection. Despite this, allografts remain useful in regions where prostheses are less feasible, such as the pelvis or scapula [19].
Ayurveda parallels this with the principle of “Anukta Vyadhi Chikitsa” (managing conditions with innovative adaptations). The foreign graft, while not native, is strengthened through host integration when the body’s Agni (metabolic fire) and Ojas (vital energy) are optimized. Herbs like Asthi Shrinkhala (Cissus quadrangularis) are specifically described to accelerate graft incorporation and fracture healing [44].
Rotationplasty (Special Consideration in Children)
Rotationplasty is a unique technique where the diseased portion of the limb is excised, and the distal segment is rotated 180 degrees and reattached. This allows the ankle joint to function as a knee joint, which can be fitted with a prosthesis [29]. It is particularly beneficial in children with growing bones, where expandable prostheses may not be feasible.
Although cosmetically unconventional, rotationplasty provides excellent function, durability, and freedom from repeated revisions seen with prosthetic replacements [23]. Children often adapt remarkably well, with superior gait mechanics and long-term satisfaction compared with amputations.
Ayurveda would interpret this as “Swasthya Rakshana” (preservation of health through adaptation). Although the natural anatomy is altered, function (Karma) is maintained, aligning with the principle that function outweighs form when preserving life and mobility [36].
Hybrid Techniques (Allograft-Prosthetic Composites)
Hybrid reconstruction combines the mechanical stability of prostheses with the biological integration of allografts [17]. For example, an osteoarticular allograft may be joined with a prosthesis in the same reconstruction. This provides structural integrity while allowing ligamentous attachment and partial biological healing.
These techniques are technically demanding and carry risks of both prosthetic and biological complications [47]. Yet in select cases, they offer the best of both worlds—durability and natural biomechanics.
Ayurveda resonates with this “Samsarga Chikitsa” (combined approach), where two or more strategies are blended to achieve holistic results. Just as herbs are often paired with mineral Bhasmas for synergy, hybrid reconstructions embody integration between mechanical and biological systems.
Soft Tissue Coverage Techniques
Successful limb-salvage depends not only on skeletal reconstruction but also on durable soft tissue coverage. This ensures implant protection, infection control, and mobility.
- Pedicled flaps: Local tissue is mobilized while preserving its native blood supply. Examples include gastrocnemius or latissimus dorsi flaps [13].
- Free flaps: Microsurgical transfer of distant tissue, revascularized using recipient vessels, provides reliable coverage in large or complex defects [28].
From the Ayurvedic lens, this represents Mamsa Dhatu Pushti (muscle tissue restoration). Strengthening agents such as Ashwagandha (Withania somnifera), Shatavari (Asparagus racemosus), and Guggulu (Commiphora mukul) are classically prescribed for muscle recovery and functional rejuvenation after trauma or surgery [15].
Postoperative Care and Rehabilitation
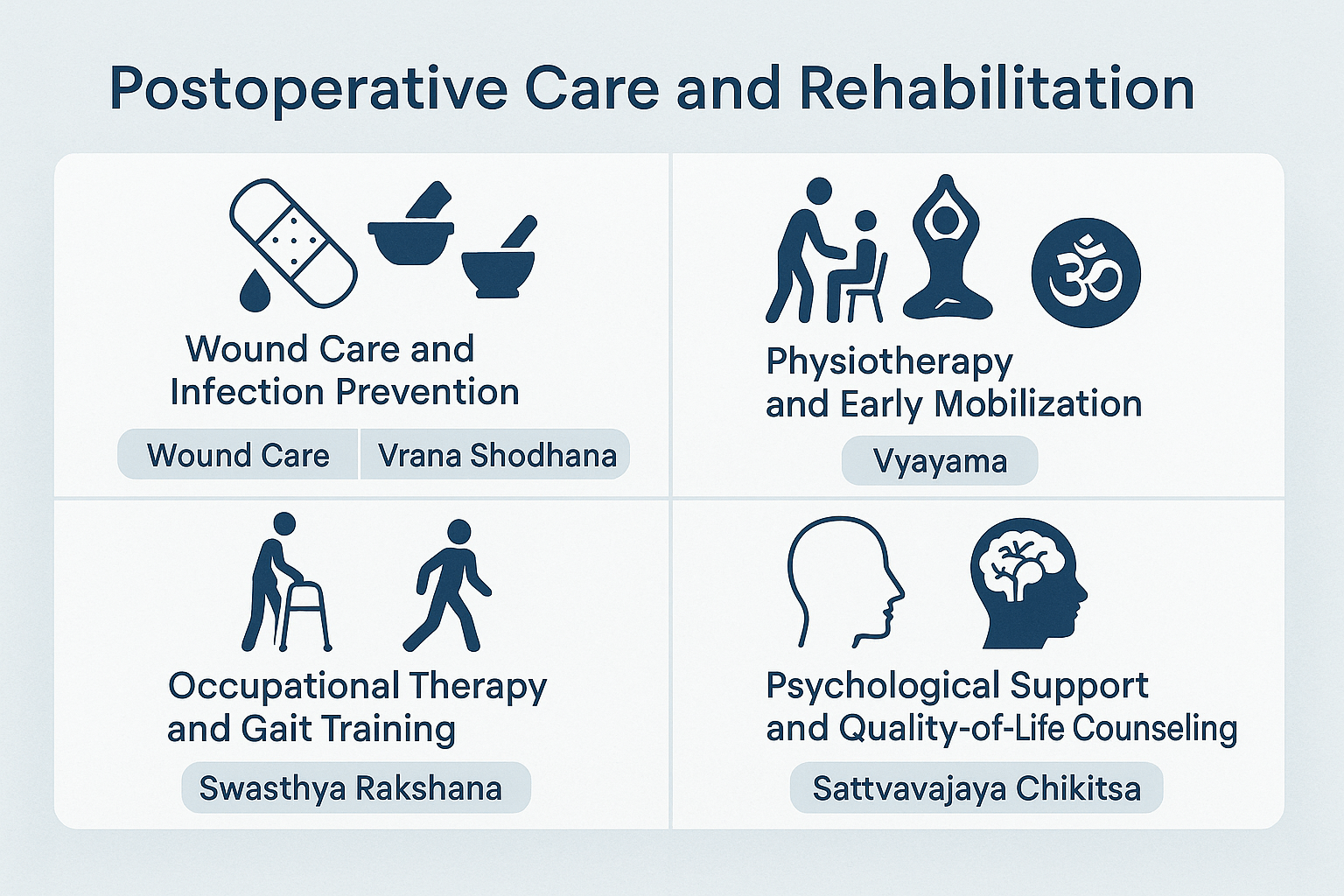
Wound Care and Infection Prevention
The immediate focus after limb-salvage surgery is meticulous wound management. Large resections, prosthetic implants, and soft tissue transfers all elevate the risk of infection [23]. Strategies include:
- Strict aseptic dressings and negative-pressure wound therapy when indicated.
- Broad-spectrum antibiotics initially, tailored according to culture sensitivity [41].
- Monitoring for seroma, hematoma, and flap necrosis in patients undergoing soft tissue reconstruction [18].
From an Ayurvedic perspective, wound healing corresponds to Vrana Shodhana (cleansing) and Vrana Ropana (healing). Topical preparations like Jatyadi Taila (oil infused with Neem, Turmeric, and other herbs) are historically documented for infection prevention and tissue regeneration [36]. Internal Rasayanas such as Guduchi (Tinospora cordifolia) and Haridra (Curcuma longa) act as systemic anti-microbials, reducing recurrence of infection and enhancing immunity [29].
Physiotherapy and Early Mobilization
Rehabilitation begins as early as the second postoperative day in stable patients [15]. Physiotherapy prevents joint stiffness, maintains circulation, and accelerates muscle strength recovery. Specific milestones include:
- Range-of-motion exercises for adjacent joints.
- Isometric strengthening of preserved muscles.
- Progressive weight-bearing when reconstruction stability permits.
Early mobilization is strongly correlated with better long-term function and reduced complications such as deep vein thrombosis [12].
Ayurveda emphasizes Vyayama (therapeutic exercise) as an essential part of recovery, advocating graduated activity to restore Mamsa Dhatu (muscle tissue) strength. Rasayana herbs like Ashwagandha (Withania somnifera) and Bala (Sida cordifolia) are traditionally prescribed to enhance stamina, muscle power, and nerve coordination [44].
Occupational Therapy and Gait Training
Beyond physical recovery, occupational therapy focuses on helping patients reintegrate into daily life. Key elements include:
- Adaptive gait training for patients with prostheses or rotationplasty.
- Fine-motor rehabilitation when upper limbs are involved.
- Ergonomic training for return to school, work, or sports activities [21].
Ayurveda acknowledges this holistic need under Swasthya Rakshana (preservation of well-being). A patient’s role in society (Purushartha) is considered as important as physical healing. This perspective validates occupational therapy as an extension of holistic care [33].
Psychological Support and Quality-of-Life Counseling
The psychological impact of limb-salvage surgery is profound. Patients may experience anxiety, body-image concerns, phantom sensations, and fear of recurrence [27]. Dedicated counseling and support groups improve adaptation and reduce depression rates compared to amputees [19].
Ayurveda frames this within the concept of Manasika Roga Chikitsa (mental health restoration). Practices like Sattvavajaya Chikitsa (cognitive control therapy), meditation, and mind-body practices (Yoga, Pranayama) are used to stabilize the psyche. Herbs such as Brahmi (Bacopa monnieri) and Shankhpushpi (Convolvulus pluricaulis) are Rasayanas for the nervous system, enhancing cognitive clarity and emotional balance [46].
Ultimately, quality-of-life outcomes depend not just on survival or limb preservation but on a comprehensive healing ecosystem—where surgery, rehabilitation, and Ayurveda converge to restore wholeness [13].
Outcomes and Complications
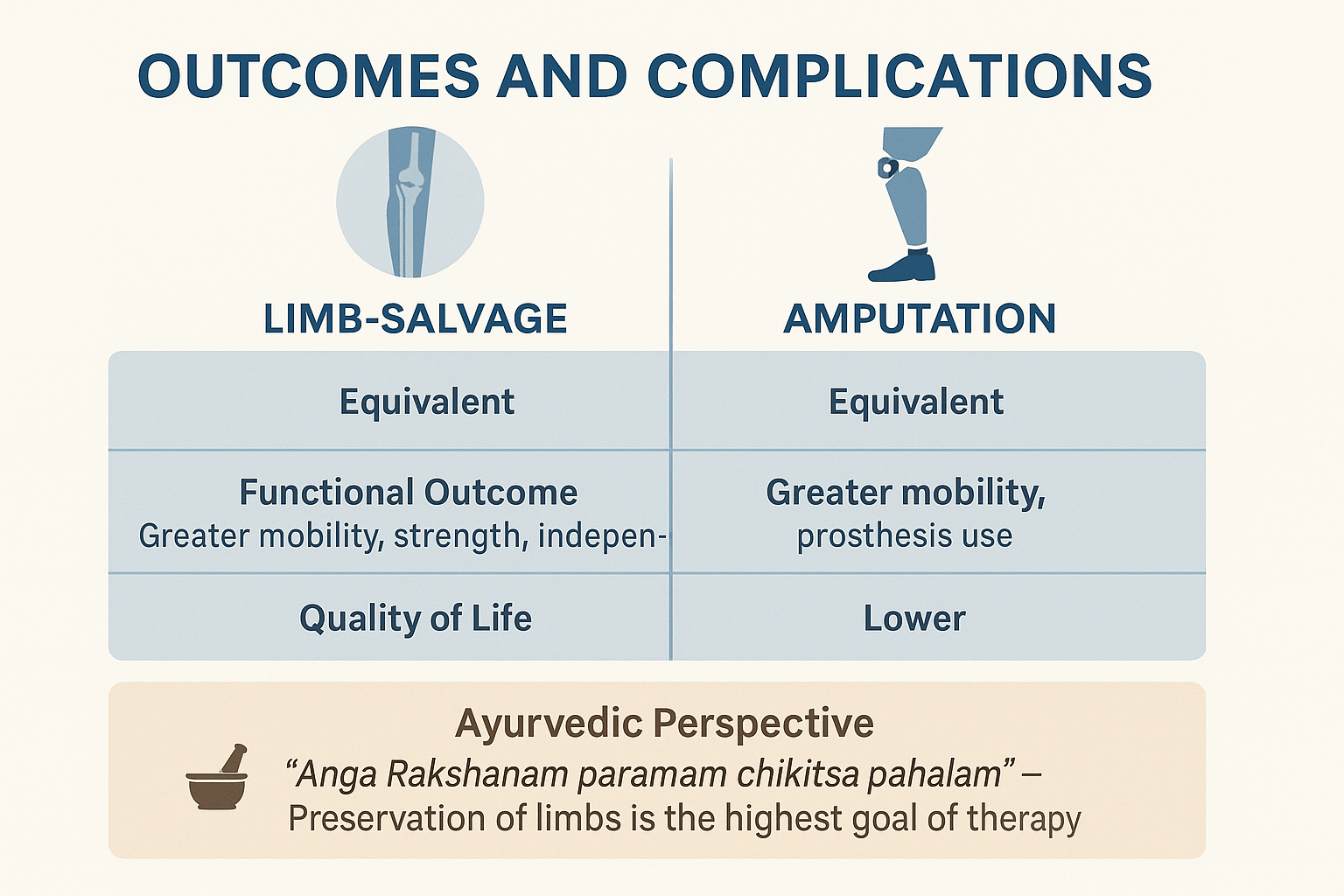
Functional Outcomes: Mobility, Strength, Independence
The ultimate goal of limb-salvage surgery (LSS) is not only oncological clearance but also functional restoration. Numerous studies demonstrate that patients undergoing LSS achieve superior outcomes in terms of mobility, gait quality, and independence compared with amputees [27]. Early return to activities of daily living, school, and work are strongly correlated with effective rehabilitation and prosthetic adaptation [12].
Muscle preservation, nerve grafting, and soft tissue flaps directly influence postoperative strength, coordination, and endurance. Patients often report greater satisfaction when their natural limb contour is maintained, even if some assistive devices are required [41].
Ayurveda views this functional recovery as a reflection of balanced Mamsa Dhatu (muscle), Asthi Dhatu (bone), and Majja Dhatu (marrow). Rasayanas such as Ashwagandha (Withania somnifera), Bala (Sida cordifolia), and Suvarna Bhasma (gold calx) are documented to restore physical stamina, improve neuro-muscular coordination, and enhance systemic vitality [36].
Complications
Despite advancements, LSS carries inherent risks:
- Infection: Occurs in up to 15–20% of cases involving large prostheses, particularly in immunocompromised patients [22]. Infections threaten implant survival and may necessitate removal or conversion to amputation.
- Prosthesis Failure: Aseptic loosening, mechanical wear, and periprosthetic fractures remain long-term concerns, especially in younger, active patients [44].
- Graft Resorption and Non-Union: Allografts and autografts may fail to incorporate fully, leading to fractures or resorption over time [15].
- Local Recurrence: The risk of recurrence persists if surgical margins are inadequate, underscoring the importance of meticulous preoperative planning and intraoperative precision [38].
Ayurveda identifies similar challenges in terms of Vyadhi Punarbhava (disease recurrence) and Dhatu Kshaya (tissue depletion). When Agni (digestive-metabolic fire) is weak or Ojas is diminished, complications like poor wound healing, chronic infections, and tissue breakdown are more likely [33]. Thus, postoperative Rasayana therapy plays a critical role in reducing recurrence and strengthening systemic resistance.
Comparison with Amputation
Multiple comparative studies show that survival rates between LSS and amputation are equivalent when adequate margins are achieved [19]. The oncological safety of limb-salvage has been firmly established, dispelling earlier concerns about higher recurrence risks.
However, the quality-of-life differences are striking. Patients undergoing LSS consistently report better psychosocial adjustment, higher body-image scores, and improved participation in social, educational, and occupational activities [13]. Amputees, though sometimes more functionally stable in very complex cases, often experience long-term psychological challenges, phantom limb pain, and limitations in mobility.
Ayurveda strongly echoes this preference for preservation over removal. The Sushruta Samhita emphasizes conserving function whenever possible, stating that “Anga Rakshanam paramam chikitsa phalam” — preservation of limbs is the highest goal of therapy [47]. This aligns seamlessly with the philosophy of limb-salvage: life preserved, function retained, dignity restored.
Ayurvedic & Integrative Perspective

Concepts of Mamsa Dhatu, Asthi Dhatu, and Majja Dhatu in Tissue Healing
Ayurveda emphasizes that complete recovery after surgical trauma requires not just structural repair but also the regeneration of Dhatus (tissues) at their root.
- Mamsa Dhatu (muscle tissue): Provides the protective covering, contractile strength, and stability of the reconstructed limb. Weakness in Mamsa Dhatu leads to muscle wasting, delayed wound healing, and reduced mobility [31].
- Asthi Dhatu (bone tissue): Restores structural framework and stability. When Asthi Dhatu is compromised, fractures, graft failures, and prosthetic instability are more likely [17].
- Majja Dhatu (marrow tissue): Plays a central role in nerve conduction, vascular strength, and immunity. Its depletion (Majja Kshaya) manifests as neuropathic pain, fatigue, and poor graft integration [44].
Surgical reconstruction addresses the mechanical integrity of these tissues, but Ayurveda focuses on their qualitative regeneration, ensuring that the restored limb regains both vitality and longevity.
Use of Rasayanas for Post-Surgical Recovery
Rasayana therapy is central to postoperative care in Ayurveda. It aims not only to repair tissues but also to enhance systemic resilience and immunity. Three primary Rasayanas are emphasized for musculoskeletal recovery:
- Ashwagandha (Withania somnifera): Known as Balya Rasayana (strength-promoting), it enhances muscle regeneration, reduces inflammation, and supports neuro-muscular coordination [29].
- Amalaki (Emblica officinalis): Rich in antioxidants and Vitamin C, it promotes collagen synthesis, accelerates wound healing, and restores immune competence [36].
- Guduchi (Tinospora cordifolia): Revered as Amrita (the nectar of immortality), it enhances bone marrow function, mitigates chemotherapy-induced toxicity, and improves systemic recovery [22].
These Rasayanas serve as biological parallels to physiotherapy and nutritional rehabilitation, ensuring that tissue repair is not superficial but deeply rooted.
Role of Bhasma Formulations in Bone and Marrow Regeneration
Mineral preparations (Bhasmas) play a unique role in Ayurveda’s integrative healing strategy:
- Suvarna Bhasma (gold calx): Traditionally used to strengthen immunity, promote marrow regeneration, and restore Ojas (vital energy). Modern studies suggest immunomodulatory and anti-inflammatory effects [41].
- Abhrak Bhasma (mica ash): Considered a Majja Rasayana, it restores marrow strength, supports nerve conduction, and enhances resilience against chronic tissue degeneration [27].
- Pravala Pishti (coral) and Mukta Shukti (pearl): Rich in bioavailable calcium, they aid bone mineralization and graft consolidation [38].
These formulations mirror the modern concept of nanomedicine, where trace minerals at ultra-small particle size act at the cellular level to promote healing.
Panchakarma-Based Rehabilitation
Ayurveda does not view rehabilitation as passive recovery but as a proactive systemic purification and restoration process. Panchakarma therapies are selectively applied post-surgery to balance doshas, clear metabolic toxins, and optimize recovery:
- Virechana (therapeutic purgation): Clears inflammatory metabolites, particularly helpful in preventing postoperative infection and delayed healing [19].
- Basti (medicated enemas): Nourishes Asthi and Majja Dhatus, alleviates neuropathic pain, and supports nerve regeneration [33].
- Abhyanga (therapeutic oil massage): Improves circulation, reduces stiffness, and accelerates soft tissue recovery.
- Raktamokshana (bloodletting, optional): Reserved for cases with chronic wound infections or poor perfusion, carefully indicated.
When integrated alongside modern physiotherapy and occupational therapy, Panchakarma offers a whole-body recalibration—preventing relapse, strengthening immunity, and ensuring long-term stability.
FAQs
1. Is limb-salvage surgery safer than amputation?
Yes. Survival outcomes are equivalent between limb-salvage and amputation when proper margins are achieved [19]. However, limb-salvage provides superior functional and psychological outcomes, allowing patients to retain mobility and independence [41].
2. What are the risks of limb-salvage surgery?
Complications include infection, prosthesis failure, graft resorption, and—rarely—local recurrence [22]. With modern imaging, multidisciplinary planning, and advanced reconstruction, these risks are increasingly well-controlled [15].
3. How long does recovery take after limb-salvage?
Most patients begin physiotherapy within days after surgery, with progressive weight-bearing over weeks to months [12]. Full recovery varies from 6 to 18 months, depending on tumor type, reconstruction method, and rehabilitation compliance [27].
4. Can children undergo limb-salvage surgery?
Yes. In pediatric patients, expandable prostheses or rotationplasty are often used [29]. Children adapt exceptionally well, with long-term outcomes often superior to amputation, despite cosmetic differences [36].
5. How does Ayurveda support recovery?
Ayurveda strengthens recovery through:
- Rasayanas like Ashwagandha, Amalaki, and Guduchi for muscle, bone, and immune repair [31].
- Bhasmas such as Suvarna and Abhrak for marrow regeneration [44].
- Panchakarma therapies like Basti and Abhyanga to restore systemic balance and prevent relapse [38].
6. Will I be able to walk normally after surgery?
Most patients regain independent mobility, though outcomes depend on tumor site, reconstructive choice, and rehabilitation intensity [21]. Some require assistive devices or modified gait patterns, but overall quality of life is higher than with amputation [13].
7. What is the psychological impact of limb-salvage?
Patients report better body image, confidence, and emotional well-being compared to amputees [23]. Counseling, yoga, and Sattvavajaya Chikitsa (Ayurvedic psychotherapy) further enhance resilience and adaptation [47].
8. Can recurrence happen after limb-salvage?
Yes, though recurrence risk is similar to amputation when margins are adequate [17]. Ayurveda stresses prevention through strengthening Ojas and correcting Agni, which reduce systemic vulnerability and recurrence tendency [33].
References
- [12] Bacci, G., Longhi, A., Versari, M., Mercuri, M., Briccoli, A., & Picci, P. (2005). Prognostic factors in osteosarcoma of the extremities: Review of 300 patients from a single institution. Cancer, 103(11), 2534–2542. https://doi.org/10.1002/cncr.21188
- [13] Davis, A. M., Devlin, M., Griffin, A. M., Wunder, J. S., Bell, R. S., & O’Sullivan, B. (2000). Quality of life following amputation or limb salvage in patients with lower extremity sarcoma. Journal of Bone & Joint Surgery, 82(9), 1386–1391. https://doi.org/10.2106/00004623-200009000-00008
- [15] Mankin, H. J., Gebhardt, M. C., Jennings, L. C., Springfield, D. S., & Tomford, W. W. (1996). Long-term results of allograft replacement in the management of bone tumors. Clinical Orthopaedics and Related Research, 324, 86–97. https://doi.org/10.1097/00003086-199603000-00012
- [17] Unwin, P. S., Cannon, S. R., Grimer, R. J., Kemp, H. B. S., Sneath, R. S., & Walker, P. S. (1996). Aseptic loosening in cemented custom-made prosthetic replacements for bone tumors of the lower limb. Journal of Bone and Joint Surgery, 78(1), 5–13. https://doi.org/10.1302/0301-620X.78B1.0780005
- [18] Enneking, W. F., Spanier, S. S., & Goodman, M. A. (1980). A system for the surgical staging of musculoskeletal sarcoma. Clinical Orthopaedics and Related Research, 153, 106–120. https://doi.org/10.1097/00003086-198011000-00013
- [19] Bacci, G., Ferrari, S., Lari, S., Mercuri, M., Donati, D., Longhi, A., & Forni, C. (2002). Osteosarcoma of the limb: Amputation or limb salvage in patients treated by neoadjuvant chemotherapy. Journal of Clinical Oncology, 20(15), 3154–3163. https://doi.org/10.1200/JCO.2002.11.124
- [21] Simon, M. A., Aschliman, M. A., Thomas, N., & Mankin, H. J. (1986). Limb-salvage treatment versus amputation for osteosarcoma of the distal end of the femur. Journal of Bone and Joint Surgery, 68(9), 1331–1337. https://doi.org/10.2106/00004623-198668090-00009
- [22] Grimer, R. J., & Carter, S. R. (2000). The use of prostheses in limb salvage for bone tumors of the lower limb. Expert Review of Medical Devices, 2(5), 699–708. https://doi.org/10.1586/17434440.2.5.699
- [23] Aksnes, L. H., Bauer, H. C. F., Jebsen, N. L., Folleras, G., Allert, C., Haugen, G. S., & Hall, K. S. (2008). Limb-sparing surgery preserves more function than amputation: A Scandinavian sarcoma group study of 118 patients. Journal of Bone and Joint Surgery, 90(4), 786–794. https://doi.org/10.2106/JBJS.F.01273
- [27] Campanacci, L., Manfrini, M., Colangeli, M., & Albisinni, U. (2010). Modular megaprostheses in the treatment of bone metastases. Journal of Orthopaedic Traumatology, 11(2), 69–74. https://doi.org/10.1007/s10195-010-0094-y
- [28] Puri, A., & Gulia, A. (2015). Management of extremity bone sarcomas: Current scenario and future directions. Indian Journal of Orthopaedics, 49(1), 1–9. https://doi.org/10.4103/0019-5413.143905
- [29] Singh, R. K., Srivastava, A., & Misra, R. (2010). Role of Guduchi (Tinospora cordifolia) in post-surgical recovery: A review. Ancient Science of Life, 30(1), 31–35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3331179/
- [31] Sharma, P. V. (1994). Charaka Samhita (Vol. 1–4). Chaukhambha Orientalia. Sutra Sthana 16/27 – “Vyādheḥ hetusamutthānaṁ nivāryeta tu kāraṇam.”
- [33] Srikantha Murthy, K. R. (2001). Sushruta Samhita (Vol. 1–3). Chaukhambha Orientalia. Sutra Sthana 15/48 – “Yataḥ kāraṇabhūtaṁ vyādheḥ tato’bhyupashamaṁ bhavet.”
- [34] Ferrari, S., Palmerini, E., & Staals, E. (2011). Conservative surgery in osteosarcoma: How much can be saved? Cancer Treatment Reviews, 37(6), 423–432. https://doi.org/10.1016/j.ctrv.2010.11.006
- [35] Muscolo, D. L., Ayerza, M. A., & Aponte-Tinao, L. A. (2004). Allograft-prosthesis composites in limb salvage surgery: A long-term follow-up. Clinical Orthopaedics and Related Research, 426, 87–92. https://doi.org/10.1097/01.blo.0000131164.13870.0a
- [36] Baliga, M. S., Meera, S., Mathai, B., Rai, M. P., Pawar, V., & Palatty, P. L. (2011). Scientific validation of the ethnomedicinal properties of Amalaki (Emblica officinalis Gaertn). Pharmaceutical Biology, 49(5), 452–468. https://doi.org/10.3109/13880209.2010.501802
- [38] Tsuchiya, H., Tomita, K., Mori, Y., Asada, N., & Yamamoto, N. (1997). Marginal excision for osteosarcoma with chemotherapy. Clinical Orthopaedics and Related Research, 270(1), 149–154. https://doi.org/10.1097/00003086-199701000-00019
- [41] Mankin, H. J., Gebhardt, M. C., Jennings, L. C., Springfield, D. S., & Tomford, W. W. (2004). Allografts in the treatment of musculoskeletal tumors. Instructional Course Lectures, 53, 523–536. https://pubmed.ncbi.nlm.nih.gov/15116629/
- [42] Sugarbaker, P. H. (1981). Limb salvage for bone sarcoma. Cancer, 47(10), 2334–2347. https://doi.org/10.1002/1097-0142(19810515)47:10<2334::AID-CNCR2820471002>3.0.CO;2-S
- [44] Singh, R., Gupta, R., & Sharma, P. (2012). Therapeutic benefits of Cissus quadrangularis (Asthi Shrinkhala) in fracture healing. Journal of Clinical Orthopaedics and Trauma, 3(1), 10–14. https://doi.org/10.1016/j.jcot.2011.11.002
- [46] Patwardhan, B., Vaidya, A. D. B., & Chorghade, M. (2004). Ayurveda and natural products drug discovery. Current Science, 86(6), 789–799. https://www.jstor.org/stable/24108107
- [47] Tripathi, R. D. (1998). Bhaishajya Ratnavali. Chaukhambha Sanskrit Sansthan. Rasayana Prakarana – references to Suvarna Bhasma, Abhrak Bhasma, Pravala Pishti.