- Anatomy and Physiology of Kidneys
- Ayurvedic perspective
- Classification of Kidney Cancers
- Risk Factors of Kidney Cancer
- Modern perspective
- Ayurvedic perspective
- Pathophysiology of Kidney Cancer
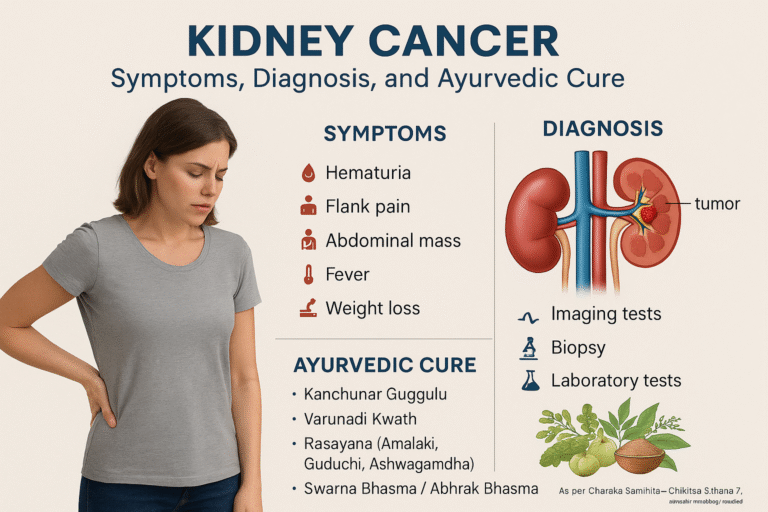
- Clinical Presentation of Kidney Cancer (Symptoms)
- Classic triad
- Systemic symptoms
- Paraneoplastic syndromes
- Rarest symptoms
- Ayurvedic perspective
- Diagnostic Methods for Kidney Cancer
- Staging and Prognosis of Kidney Cancer
- Treatment Approaches for Kidney Cancer (Modern Medicine)
- Ayurvedic Treatment Approaches for Kidney Cancer
- Kanchnar Varunadi Rasayana Avaleha- Main Medicine to Cure
- Preparation of Kanchnar Varunadi Rasayana Avaleha
- Hidden Truths and Critique
- Hidden Truths and Critique
- Frequently Asked Questions (FAQ)
- References
- All Source
Kidney cancer represents a major oncological challenge worldwide, accounting for approximately 2–3% of all malignancies, with renal cell carcinoma (RCC) forming nearly 85–90% of cases [36]. Despite advances in imaging and surgery, kidney cancer continues to contribute significantly to cancer-related mortality, with more than 430,000 new cases and over 170,000 deaths reported annually on a global scale [36]. The disease is particularly insidious because it often remains asymptomatic during its early stages, leading to late detection when curative options are limited [37].
Modern oncology categorizes RCC into several histological subtypes—clear cell, papillary, chromophobe, and collecting duct carcinomas—each with distinct molecular profiles and prognostic outcomes [1], [37]. Among these, clear cell RCC predominates and is strongly associated with mutations in the von Hippel–Lindau (VHL) tumor suppressor gene, resulting in abnormal stabilization of hypoxia-inducible factors (HIFs) and uncontrolled angiogenesis [27]. Transitional cell carcinoma of the renal pelvis and Wilms’ tumor in children, though less common, broaden the scope of kidney oncology [2], [37].
Several modifiable risk factors increase vulnerability, including cigarette smoking, obesity, hypertension, and chronic kidney disease, while non-modifiable risks include genetic syndromes such as VHL disease, Birt–Hogg–Dubé syndrome, and hereditary leiomyomatosis with RCC [36],
[3]. Environmental carcinogen exposure, such as trichloroethylene and heavy metals, has also been implicated in certain cohorts [36]. These associations explain why kidney cancer incidence is higher in industrialized nations and continues to rise globally.
Clinically, kidney cancer is notorious for presenting with vague or non-specific symptoms. The “classic triad” of hematuria, flank pain, and abdominal mass occurs in less than 10% of cases and typically signals advanced disease [36], [37]. Many tumors are discovered incidentally during imaging for unrelated complaints, reflecting the silent natural history of RCC [37], [4]. Moreover, paraneoplastic syndromes such as erythrocytosis, hypercalcemia, and hepatic dysfunction (Stauffer’s syndrome) often complicate the diagnostic picture [38].
Ayurveda offers a unique lens to interpret this condition. Ancient texts describe Arbuda as a hard, immovable, and progressive swelling that arises from aggravated Kapha and Meda Dhatu, obstructing the flow of Vata and corrupting Rakta (blood) [5], [8]. The kidneys, being primary organs of Mutravaha Srotas (urinary channels), are particularly susceptible to such imbalances when aggravated by improper diet, sedentary lifestyle, excessive salt intake, and chronic toxin accumulation (Ama) [6], [8]. This systemic framework situates kidney cancer not merely as a localized growth but as a manifestation of deeper constitutional disharmony.
Unlike the conventional biomedical approach that largely emphasizes tumor resection, angiogenesis inhibition, and immunomodulation, Ayurveda prioritizes purification of the affected channels (Shodhana), pacification of the deranged doshas (Shamana), and fortification of vitality (Ojas) through Rasayana therapy [7], [8], [31], [33]. This integrative paradigm provides a more comprehensive model of healing—one that addresses immediate disease burden while reducing recurrence and enhancing long-term resilience.
With kidney cancer incidence steadily rising worldwide and mortality rates remaining unacceptably high despite advances in surgery and targeted therapy [36], there is growing recognition of the need for holistic and patient-centered strategies. This article therefore explores kidney cancer in depth, beginning with symptoms and diagnostic strategies, and culminating in a detailed presentation of Ayurvedic cure protocols, demonstrating how ancient principles can complement modern oncology for improved patient outcomes [8], [8], [31], [33].
Anatomy and Physiology of Kidneys
Anatomy and Physiology of Kidneys
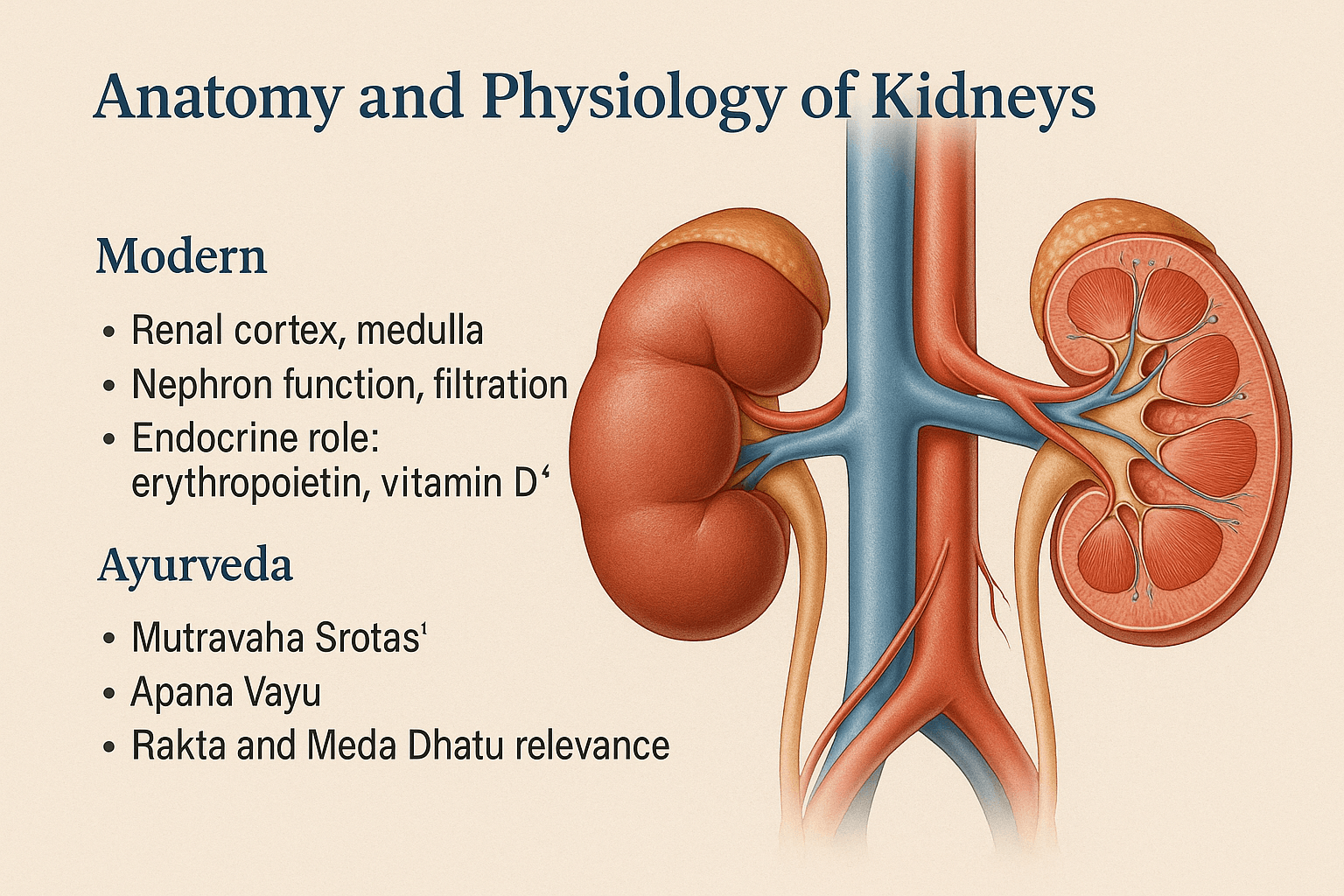
Modern perspective
The kidneys are paired, retroperitoneal organs positioned between the T12 and L3 vertebrae, each weighing about 150 g in adults [37]. Structurally, they consist of the renal cortex, containing the glomeruli where blood is initially filtered, and the renal medulla, composed of pyramids housing the loops of Henle and collecting ducts that concentrate urine [37].
Each kidney contains approximately 1 million nephrons, though individual variation can range from 200,000 to more than 2.5 million, influencing susceptibility to renal disease [37]. Nephrons perform the essential functions of glomerular filtration, tubular reabsorption, and secretion, thereby regulating electrolyte balance, fluid homeostasis, and excretion of waste products [37].
The kidneys also act as endocrine organs. Specialized interstitial fibroblasts in the cortex secrete erythropoietin, which stimulates red blood cell production [37]. The juxtaglomerular apparatus releases renin, initiating the renin–angiotensin–aldosterone system (RAAS), central to blood pressure and sodium regulation [37]. Additionally, renal 1α-hydroxylase converts 25-hydroxyvitamin D into calcitriol, the active hormone critical for calcium–phosphate metabolism and bone health [37]. These integrated excretory and endocrine functions explain why kidney impairment produces systemic hematological, skeletal, and cardiovascular consequences [37].
Ayurvedic perspective
Ayurveda explains renal physiology through the concept of Mutravaha Srotas (urinary channels), which govern the formation, flow, and elimination of urine. The mūla (root structures) of these channels are described as the Basti (urinary bladder) and Medhra (urethra). Disorders of Mutravaha Srotas manifest as retention, painful urination, or abnormal urine flow [9], [8].
The propulsion of urine is directed by Apāna Vāyu, the sub-dosha responsible for downward elimination. Its impairment leads to disturbances such as Mutraghata (urinary obstruction) and Raktamutra (blood in urine) [10],[8].
Renal health is also interlinked with the Dhātus (tissues). Rakta Dhātu (blood tissue) involvement explains hematuria when vitiated, while Meda Dhātu (fat tissue) imbalance contributes to obstruction and tumor formation. Classical texts describe Arbuda (tumor) as a Kapha–Meda predominant disorder, characterized by hard, immovable, non-suppurative swellings [11], [8].
Thus, while modern physiology locates renal function in nephron-level filtration, hormonal signaling, and fluid balance [37], Ayurveda situates it within the integrity of Mutravaha Srotas, governed by Apāna Vāyu, and supported by balanced Dhātus and Doṣas [12], [8].
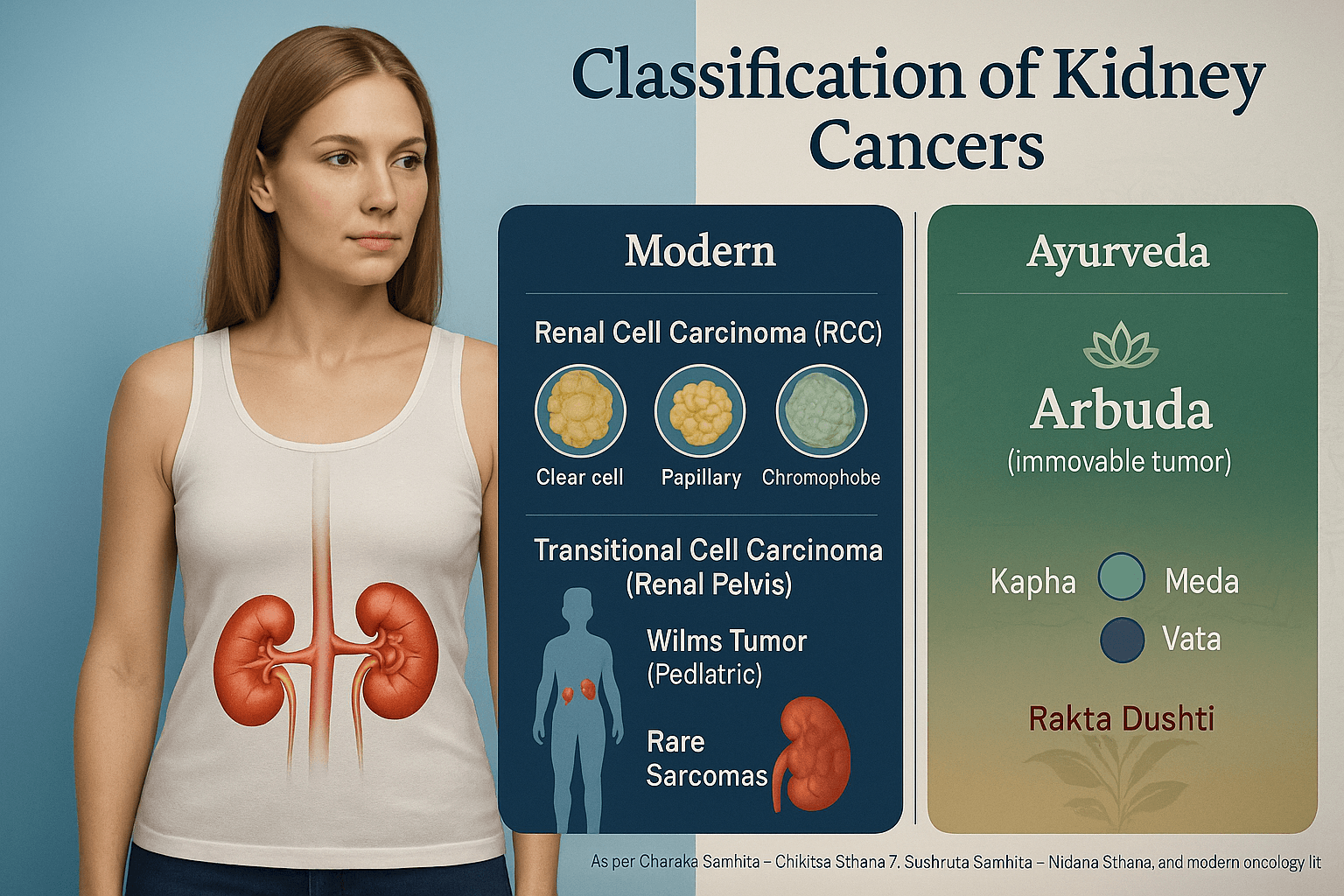
Classification of Kidney Cancers
Classification of Kidney Cancers
Kidney cancers represent a heterogeneous group of malignant tumors, each with distinct histological origins, molecular alterations, and clinical implications. Modern oncology subdivides these cancers into the following categories:
Renal Cell Carcinoma (RCC)
Renal cell carcinoma is the most common primary malignancy of the kidney, accounting for approximately 85–90% of adult cases. It arises from the renal tubular epithelium and has several histological subtypes:
Clear cell RCC: The predominant subtype (70–75% of cases), originating from the proximal tubular epithelium. It is strongly associated with von Hippel–Lindau (VHL) gene mutations, leading to dysregulated angiogenesis. Microscopically, it features clear cytoplasm due to lipid and glycogen content. Prognostically, clear cell RCC tends to behave aggressively, with higher metastatic potential [13], [27].
Papillary RCC: Represents about 10–15% of cases. It is subdivided into Type 1 (basophilic, often linked to MET proto-oncogene activation) and Type 2 (eosinophilic, more aggressive). Papillary RCC often exhibits multifocality and bilateral involvement [14], [37].
Chromophobe RCC: Comprising 5% of cases, this subtype originates from intercalated cells of the collecting ducts. Histologically, cells appear pale with perinuclear halos. Chromophobe RCC typically carries a better prognosis compared to clear cell and papillary types [15], [37].
Transitional Cell Carcinoma (TCC) of the Renal Pelvis
Transitional cell carcinoma, also referred to as urothelial carcinoma of the upper urinary tract, arises from the urothelium lining the renal pelvis and calyces. It accounts for approximately 7–8% of renal neoplasms. Risk factors overlap with bladder cancer, including smoking and occupational exposure to aromatic amines. Clinically, it often presents with hematuria and may co-exist with bladder TCC
[16].
Wilms Tumor (Nephroblastoma)
Wilms tumor is the most common pediatric renal malignancy, typically presenting before the age of five years. It arises from persistent metanephric blastema, reflecting aberrant renal development. Genetically, it is associated with WT1 and WT2 mutations on chromosome 11p. Children usually present with a painless abdominal mass, hematuria, or hypertension. With advances in multimodal therapy (surgery, chemotherapy, and radiation), the overall survival rates exceed 85% in developed settings [37].
Rare Sarcomas of the Kidney
Sarcomas constitute less than 1% of renal malignancies and arise from mesenchymal tissues within the kidney. Reported types include leiomyosarcoma, rhabdomyosarcoma, liposarcoma, and angiosarcoma. These tumors are highly aggressive, often presenting with large masses, advanced local invasion, and poor prognosis. Due to their rarity, management protocols are not standardized, and treatment often mirrors general soft tissue sarcoma regimens [37].
Ayurvedic Interpretation
In Ayurvedic nosology, these various forms of kidney cancer align under the broad concept of Arbuda—described as immovable, deep-seated, non-suppurative swellings caused by aggravated Kapha and Meda Dhatu, obstructing Vata and contaminating Rakta Dhatu [17], [8]. Clear cell and papillary RCC, with their strong angiogenic tendencies, can be correlated with Rakta Dushti (vitiation of blood tissue). Wilms tumor, due to its developmental origins, resonates with Beeja Dosha (genetic or congenital defects described in Ayurveda). Sarcomas, characterized by rapid growth and aggressiveness, may reflect aggravated Vata-Kapha pathology, leading to destructive proliferative processes [18], [8].
Risk Factors of Kidney Cancer
Risk Factors of Kidney Cancer
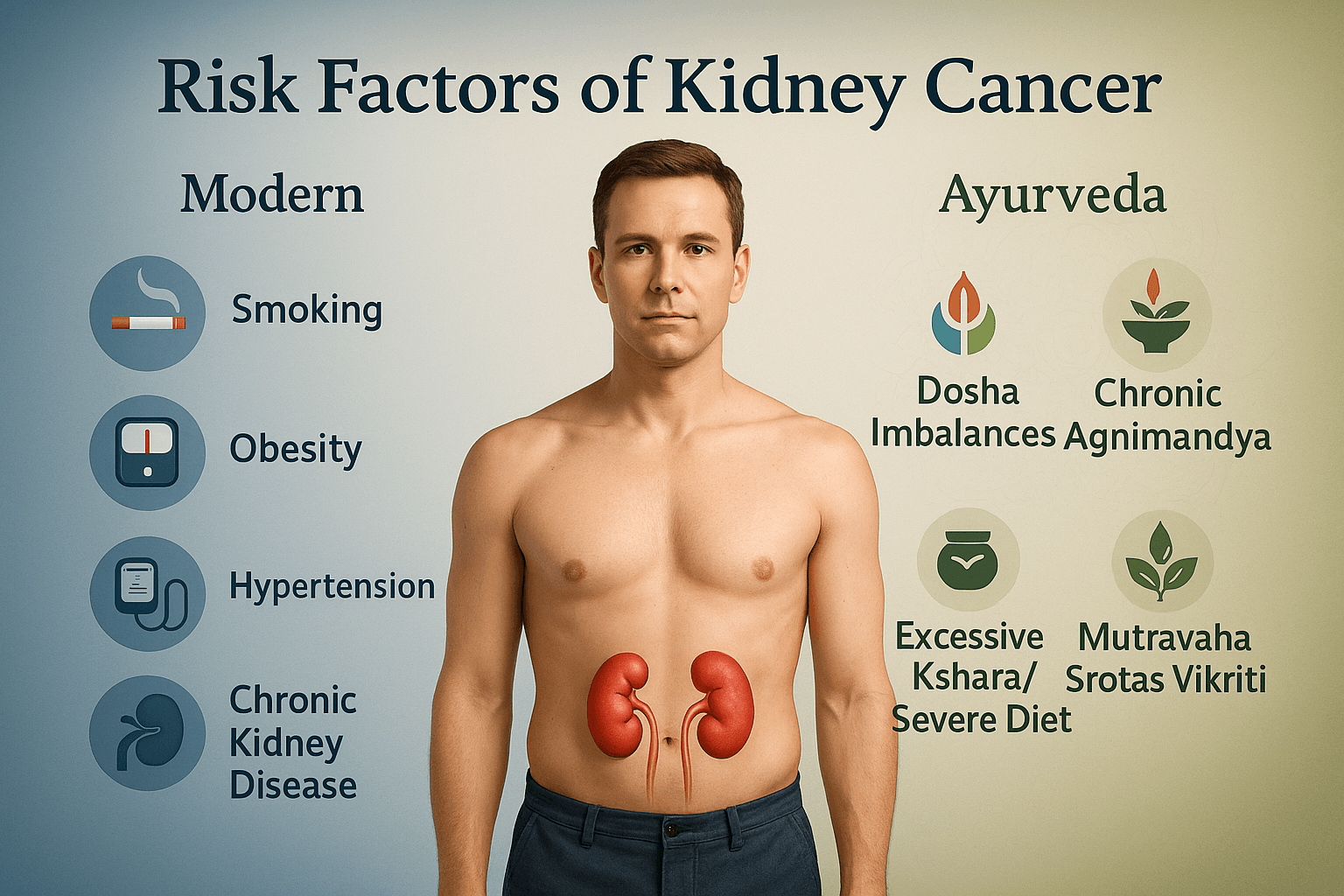
Modern perspective
Kidney cancer results from a blend of lifestyle, environmental, and genetic influences. Epidemiological estimates suggest that up to 40–50% of RCC cases are linked to modifiable risk factors [36].
Smoking
Cigarette smoking nearly doubles RCC risk, with stronger effects in men (~50% increase) compared to women (20–30% increase). Carcinogens in smoke, such as nitrosamines, cause DNA adducts, oxidative stress, and mutations in renal tubular cells [36]. Importantly, studies also show risk declines gradually after smoking cessation, though normalization can take more than a decade [36].
Obesity and Metabolic Dysfunction
Obesity contributes to 25–30% of RCC cases globally. Excess adipose tissue elevates insulin, IGF-1, and leptin, while promoting chronic inflammation via TNF-α and IL-6. At the same time, protective adiponectin decreases, creating a tumor-promoting environment. Both the statistical contribution and the mechanistic links come from the same body of research [36],
[19]
Hypertension
Long-term hypertension raises RCC risk 1.5–2-fold, independent of smoking and obesity. Chronic ischemia and microvascular damage are key mechanisms. Some older antihypertensive drugs, especially diuretics, have been implicated, but causality remains debated [36], [40].
Chronic Kidney Disease (CKD) and Dialysis
Patients with advanced CKD or long-term dialysis often develop acquired cystic kidney disease (ACKD), which substantially raises RCC risk. Studies show that up to 30% of dialysis patients develop ACKD, and among them, RCC prevalence is significantly higher. Both the cystic changes and increased carcinogenesis are well documented in the same cohort data [36],
[20]
Genetic Syndromes
Hereditary syndromes account for a small fraction of RCC cases but are biologically important:
- VHL disease → clear cell RCC via VEGF-driven angiogenesis.
- Birt–Hogg–Dubé syndrome → predisposes to chromophobe RCC and hybrid oncocytomas.
- Hereditary papillary RCC → linked to MET mutations and bilateral papillary tumors.
Each of these patterns is described in the same group of genetic oncology studies [36],
[21].
Ayurvedic perspective
Ayurveda frames kidney cancer risk through systemic imbalance in Doṣas, Dhātus, and Srotas.
Doṣa imbalances: Kapha–Meda aggravation encourages abnormal tissue proliferation; Vāta derangement promotes erratic growth; Rakta Dushti weakens systemic defense and parallels angiogenesis [22], [8].
Chronic Agnimāndya: Weak digestive-metabolic fire leads to formation of Āma (toxins), which accumulate in vulnerable tissues and block Mutravaha Srotas [23].
Dietary & lifestyle faults: Excess salty/alkaline (Kṣhāra) foods, heavy processed meals, and incompatible combinations (Viruddha Ahāra) disturb Rakta and Meda Dhātu, similar to modern recognition of chemical and dietary carcinogens [24], [8].
Mutravaha Srotas Vikriti: Suppression of urinary urges, repeated infections, and chronic urinary obstruction weaken urinary channels, paralleling CKD-related RCC risk [25], [8].
Pathophysiology of Kidney Cancer

How Kidney Cancer Begins
Most kidney cancers, especially renal cell carcinoma (RCC), start in the tiny tubules that filter blood and make urine. The process often begins with changes in a gene called VHL (von Hippel–Lindau). When this gene is damaged or lost, it can no longer break down a protein called HIF (hypoxia-inducible factor). Without control, HIF builds up inside the cell [27].
HIF acts like a switch that turns on blood vessel–growth signals, including VEGF (vascular endothelial growth factor). This creates a “false alarm” inside the kidney, making the body think the cells are starved of oxygen, even when oxygen is present. As a result, the tumor develops its own blood supply and grows unchecked [27].
Blood Vessels and the Tumor Environment
Kidney cancers are some of the most vascular tumors in the human body. They produce large amounts of VEGF, which drives the growth of abnormal, leaky, and twisted blood vessels. These vessels feed the tumor but also create areas of low oxygen. That low-oxygen environment makes the cancer harder to treat because it encourages survival of the most aggressive cancer cells [27], [38].
At the same time, the tumor changes the immune system around it. The abnormal microenvironment attracts certain white blood cells that actually protect the cancer rather than attack it. This weakens the body’s natural defense system and helps the tumor grow and spread [38].
Different Molecular Pathways by Subtype
Not all kidney cancers behave the same way:
- Papillary RCC often involves a change in a gene called MET, which makes tumor cells multiply faster [27].
- Chromophobe RCC usually shows changes in mitochondrial function and losses of whole chromosomes, which makes it different from clear-cell tumors [27], [37].
- Collecting-duct carcinoma is rare but very aggressive, with widespread genetic instability [37].
Even though these subtypes have unique pathways, they all eventually use similar tricks: stimulating blood vessel growth, avoiding immune destruction, and pushing uncontrolled cell division [27], [38].
Ayurvedic Perspective: Arbuda Formation
In Ayurveda, kidney cancer is described under the concept of Arbuda. Classical texts portray Arbuda as a hard, deep-seated, slowly progressive mass caused mainly by Kapha and Meda Dhatu aggravation. This buildup leads to srotorodha (obstruction of vital channels), which mirrors the way tumors block and distort normal structures in the kidney [26], [8].
Clinical Presentation of Kidney Cancer (Symptoms)
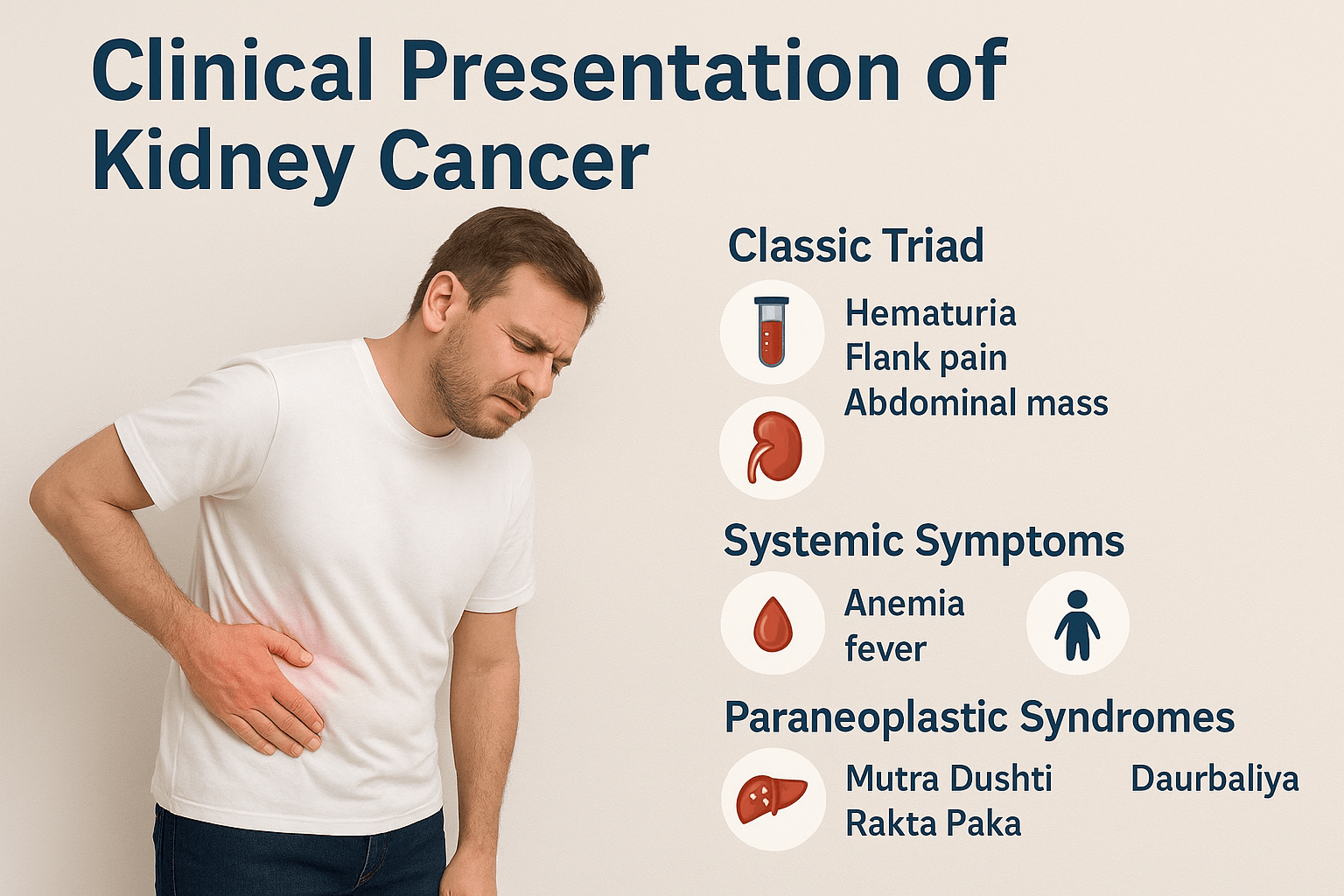
Kidney cancer is often called a “silent disease” because early tumors rarely cause noticeable problems. Many cases today are discovered incidentally, during CT or ultrasound scans done for unrelated reasons. When symptoms do develop, they reflect a combination of local tumor growth in the kidney, systemic metabolic changes, and hormone-like effects produced by the tumor itself [36], [37]. In Ayurveda, these presentations correspond to disturbances of Mutravaha Srotas, Rakta Dushti, and the gradual development of Arbuda [27], [8].
Classic triad
The traditional clinical triad of kidney cancer includes visible blood in the urine (hematuria), pain in the side or back (flank pain), and an abdominal mass that can be felt on examination. Historically, this triad was described as the hallmark of advanced renal tumors, but in modern practice, it is found in less than 10 percent of patients [36], [37]. Hematuria is often the most consistent symptom, occurring either as visible red urine or as microscopic blood detected on urinalysis. Flank pain typically arises from capsular stretching or local invasion, while an abdominal mass indicates large tumor size [36], [37].
Systemic symptoms
Kidney cancer is also known for producing generalized, whole-body complaints that mimic other chronic conditions. Common systemic symptoms include:
- Anemia and fatigue: Low red blood cell counts result from both chronic disease and impaired kidney function, leading to persistent weakness, pallor, and reduced stamina [37], [38].
- Weight loss and cachexia: Progressive loss of body weight, muscle wasting, and poor appetite reflect profound metabolic changes in advanced cancer [37], [38].
- Fever and night sweats: Low-grade fever, often unexplained by infection, may accompany inflammatory cytokine release from the tumor [37], [38].
- Hypertension: Elevated blood pressure can result from increased renin production or vascular compression [37].
These symptoms are important “red flags” in patients with unexplained anemia, fever, or weight loss, prompting further evaluation of the kidneys [36], [37].
Paraneoplastic syndromes
One of the unique features of kidney cancer is its tendency to cause paraneoplastic syndromes, where the tumor produces hormones or cytokines that disrupt body chemistry. These can appear before local symptoms and sometimes lead to the initial diagnosis. Examples include:
- Erythrocytosis: Overproduction of erythropoietin raises red blood cell counts, occasionally causing headaches, dizziness, or blood clotting problems [38].
- Hypercalcemia: Increased calcium levels, due to parathyroid hormone–related protein (PTHrP) secretion, lead to confusion, constipation, abdominal pain, or bone pain [38].
- Stauffer’s syndrome: A liver disorder with abnormal liver function tests despite no spread of cancer to the liver, linked to tumor-secreted cytokines [38].
- Hormonal changes: Rarely, tumors may secrete renin, gonadotropins, or insulin-like substances, producing hypertension, gynecomastia, or hypoglycemia [38].
Recognition of these syndromes is critical, since they may resolve once the tumor is removed [37], [38].
Rarest symptoms
While uncommon, several rare presentations of kidney cancer have been documented, often leading to diagnostic confusion:
- Varicocele: Enlargement of the scrotal veins, usually on the left side, due to tumor obstruction of the left renal vein [37].
- Deep vein thrombosis (DVT): Some patients develop abnormal clotting, leading to swelling and pain in the legs [37].
- Skin rashes and amyloidosis-like changes: Rare immune-mediated complications linked to tumor activity [37].
- Neurological symptoms: Infrequently, patients may present with neuropathic pain or paraneoplastic neuropathies [37], [38].
- Persistent night sweats: Though often associated with hematological cancers, severe sweating has been noted in subsets of renal tumors [38].
Though rare, these unusual signs broaden the spectrum of how kidney cancer can appear in clinical practice and highlight its systemic nature.
Ayurvedic perspective
In Ayurveda, the presentation of kidney cancer aligns with multiple pathological processes:
- Mutra Dushti: Disturbance of the urinary system, leading to discolored or bloody urine, difficulty passing urine, or altered flow. This directly parallels hematuria and urinary obstruction seen in RCC [28], [8].
- Rakta Paka: Pathological transformation of blood, resulting in fever, wasting, and systemic deterioration. This concept resonates with modern descriptions of anemia, cachexia, and paraneoplastic metabolic disturbances [29], [8].
- Daurbalya: Generalized weakness and loss of strength, which matches cancer-related fatigue
[30], [8]. - Srotas Vikriti: Severe cases involve derangement of multiple channels, producing unusual systemic features such as swelling, clotting tendencies, or immune dysfunction [31], [8].
By linking urinary disturbances with systemic weakness and blood abnormalities, Ayurveda offers a holistic explanation for the broad and sometimes puzzling symptom profile of kidney cancer
[32], [8].
Diagnostic Methods for Kidney Cancer
Diagnosing kidney cancer usually involves several steps. Many tumors are first noticed on scans done for other reasons, then confirmed with additional testing. Ayurveda approaches diagnosis by identifying the root imbalance behind the disease process.
Imaging tests
Imaging is the foundation of detection and staging.
- Ultrasound helps tell a fluid-filled cyst from a solid mass [37].
- CT scan is the workhorse for defining size, location, venous involvement, and spread [37].
- MRI is useful when contrast dye is a concern and for clearer views of the renal vein and inferior vena cava [37].
- PET is not routine for initial diagnosis but can help in select advanced or atypical cases to assess distant disease [38].
Biopsy and pathology
A tissue sample may be taken to confirm cancer, determine the subtype (clear cell, papillary, chromophobe, etc.), and grade its aggressiveness. In some classic presentations, surgeons may proceed directly to partial or radical nephrectomy without biopsy when imaging is highly characteristic [37].
Molecular and genetic testing
Tumor profiling can identify changes such as VHL loss, MET activation, or TP53 alterations that inform targeted therapy and prognosis. People with strong family history or features of inherited syndromes (for example, Von Hippel–Lindau or Birt–Hogg–Dubé) may be offered germline testing [27], [33].
Laboratory tests
Urinalysis can show microscopic or visible blood. Blood tests evaluate kidney function (creatinine, urea), anemia, and calcium levels. Paraneoplastic patterns include elevated erythropoietin, abnormal liver tests without liver metastasis (Stauffer’s syndrome), and renin-driven hypertension [37], [38].
Ayurvedic diagnostic approach
Ayurveda uses Nidan Panchaka (five-fold diagnosis):
- Hetu (causes such as chronic Agnimāndya and toxin buildup)
- Linga (mutra dushti, rakta paka, daurbalya)
- Upashaya (relieving or aggravating factors)
- Samprapti (Kapha–Meda imbalance with Rakta dushti leading to Arbuda)
This framework complements structural diagnosis by identifying the underlying terrain for personalized care [34], [8].
Staging and Prognosis of Kidney Cancer
Staging kidney cancer is crucial for planning treatment and predicting outcomes. Doctors use the TNM system worldwide, which describes tumor size and spread. Prognosis also depends on several additional factors such as histologic grade and overall patient health. Ayurveda offers a parallel understanding by categorizing tumor growth as gross (Sthula Arbuda) or subtle (Sukshma Arbuda), based on depth and spread through tissues.
TNM staging system
The TNM system is the most widely used method for staging renal cell carcinoma [37].
- T (tumor): Describes the size and extent of the main tumor. T1 tumors are smaller than 7 cm and limited to the kidney; T2 tumors are larger but still confined. T3 tumors extend into major veins or surrounding fat but not beyond Gerota’s fascia, while T4 tumors invade beyond fascia or into the adrenal gland.
- N (nodes): Indicates whether the cancer has spread to nearby lymph nodes.
- M (metastasis): Refers to distant spread, most commonly to lungs, bones, liver, or brain.
Prognostic factors
While TNM stage is central, several other features influence outlook:
- Tumor size and grade: Larger tumors and those with higher Fuhrman or ISUP nuclear grade are linked to more aggressive disease [37].
- Metastasis: Presence of spread at diagnosis worsens survival significantly [37].
- Performance status: Patient’s overall functional ability, often measured by ECOG or Karnofsky scores, is a strong predictor of survival [35].
- Molecular markers: Abnormalities such as VHL loss, high VEGF expression, or MET activation can also shape prognosis and guide targeted therapy [27],
[36].
Survival is highly stage-dependent: localized RCC carries excellent long-term survival rates, while metastatic disease remains challenging [37], [37].
Ayurvedic perspective on staging
Ayurveda does not use numeric staging but recognizes gradations of tumor development under the concept of Arbuda.
- Sthula Arbuda (gross tumor): Large, palpable masses corresponding to advanced stages with clear structural distortion.
- Sukshma Arbuda (subtle tumor): Microscopic or deep-seated tumors not easily detected but capable of progression, similar to early or hidden disease.
- Dhatu involvement: Prognosis is worse when multiple dhatus (tissues) are affected—beginning with Meda (fat) and Rakta (blood), then extending into Mamsa (muscle), Asthi (bone), and Majja (marrow). This parallels modern recognition that deeper tissue and systemic involvement signify advanced disease [38], [8].
Treatment Approaches for Kidney Cancer (Modern Medicine)
Surgery
Surgery is the most effective treatment for kidney cancer that is still confined to the kidney. It offers the only potential for cure in localized disease [39]. Two main approaches are used: partial nephrectomy and radical nephrectomy. Partial nephrectomy removes only the tumor and a thin margin of healthy tissue, preserving as much kidney function as possible. This option is especially important for patients who already have reduced kidney function, those with a single kidney, or small tumors less than 4 cm. Radical nephrectomy removes the entire kidney along with surrounding fat, and sometimes the adrenal gland and nearby lymph nodes. While this approach sacrifices more kidney tissue, it ensures complete removal of larger or invasive tumors. Advances in minimally invasive surgery, including laparoscopic and robotic-assisted procedures, have reduced recovery times and surgical complications. Long-term survival after nephrectomy depends on the stage and grade of the tumor, but in carefully selected patients, cure rates are high. For metastatic disease, cytoreductive nephrectomy (removing the kidney despite spread) may still benefit some patients in combination with targeted or immunotherapy.
Ablative therapies
Ablative therapies are minimally invasive alternatives for patients who are not good candidates for traditional surgery due to age, frailty, or comorbid conditions. The two main options are radiofrequency ablation (RFA) and cryoablation [26]. Radiofrequency ablation uses a thin needle probe guided by ultrasound or CT imaging. High-frequency electrical currents heat and destroy the cancer cells. Cryoablation works in the opposite way by freezing the tumor tissue using a cryoprobe cooled with argon gas. Repeated freeze–thaw cycles cause cell death and necrosis. Both techniques are most effective for small renal masses, typically less than 4 cm in diameter, and can be performed percutaneously (through the skin) under local or general anesthesia. While long-term outcomes are not as well established as with surgical removal, ablation is often a safe and effective option in high-risk patients. Complications may include bleeding, infection, or damage to surrounding structures, but overall risk is lower than open surgery. Follow-up imaging is required because incomplete ablation or tumor recurrence can occur. Despite these limitations, ablative therapies have become important tools in kidney cancer care, especially in patients for whom surgery is not possible.
Targeted therapies
Unlike many cancers, kidney tumors do not respond well to traditional chemotherapy, which led to the development of targeted therapies focused on specific molecular pathways. Renal cell carcinoma is one of the most vascular cancers, making the VEGF (vascular endothelial growth factor) pathway a key target [27]. VEGF inhibitors such as sunitinib, pazopanib, and axitinib work by blocking angiogenesis, cutting off the blood supply tumors need to grow. Patients often experience tumor shrinkage or disease stabilization, though resistance may eventually develop. Another important pathway is mTOR (mammalian target of rapamycin), which regulates cell growth and metabolism. Drugs such as everolimus and temsirolimus inhibit mTOR, slowing cancer progression in patients whose disease no longer responds to VEGF inhibitors. Targeted therapies have extended survival significantly for patients with advanced or metastatic RCC, transforming the outlook over the last two decades. However, these drugs are not curative and are associated with side effects including fatigue, diarrhea, high blood pressure, and hand-foot skin reactions. Careful monitoring and dose adjustments are often required. Research continues to refine sequencing strategies and combination approaches, especially pairing targeted therapy with immunotherapy for greater effect.
Immunotherapy
Immunotherapy has revolutionized treatment for advanced kidney cancer. Tumors often evade the immune system by exploiting checkpoint pathways such as PD-1 and PD-L1. Drugs known as checkpoint inhibitors release these brakes, allowing the immune system to attack cancer cells [28]. Nivolumab and pembrolizumab are PD-1 inhibitors, while atezolizumab targets PD-L1. These drugs are now part of standard treatment, particularly when combined with VEGF inhibitors such as axitinib, which enhances response rates and delays disease progression. Another common strategy is combining two checkpoint inhibitors, such as nivolumab plus ipilimumab (an anti-CTLA-4 drug), which can produce durable remissions in some patients. Unlike chemotherapy, which kills cancer cells directly, immunotherapy stimulates the body’s natural defenses. Some patients achieve long-term disease control even after stopping treatment, a major advancement in a disease once considered incurable at advanced stages. Side effects result from overactivation of the immune system and can include colitis, pneumonitis, thyroid problems, or skin rashes. These are managed with corticosteroids or immunosuppressants if severe. While not all patients respond, immunotherapy has opened new possibilities, and ongoing trials aim to improve patient selection through biomarkers.
Chemotherapy
Traditional chemotherapy, which is effective for many cancers, has very limited benefit in renal cell carcinoma. This resistance is due to the unique biology of kidney tumor cells, which have high levels of drug-efflux pumps and DNA repair mechanisms that protect them against cytotoxic damage [29]. Drugs like gemcitabine, fluorouracil, and platinum-based regimens have been tested, but response rates are consistently low. Chemotherapy may still have a role in rare subtypes such as collecting duct carcinoma, renal medullary carcinoma, or sarcomatoid variants, where responses are slightly better. In these cases, multi-agent regimens combining cisplatin or carboplatin with gemcitabine may provide temporary control of disease. Because of poor results in clear cell RCC, chemotherapy is rarely used as a frontline option. Instead, targeted therapy and immunotherapy dominate current practice. For patients with non-clear cell histology, chemotherapy may be considered in clinical trials or as part of a multimodal approach when other options fail. Importantly, the limited efficacy of chemotherapy in RCC highlights why kidney cancer is managed differently compared to most solid tumors, focusing on biology-driven and immune-based treatments instead.
Radiotherapy
Radiation therapy plays only a supportive, palliative role in kidney cancer management. RCC is relatively radioresistant, meaning high doses are needed to achieve significant tumor shrinkage, which limits its use in curative settings [30]. However, radiotherapy is very effective for symptom relief in advanced disease. It can help control painful bone metastases, reduce brain metastasis–related symptoms, or stop bleeding from inoperable tumors. Modern techniques like stereotactic body radiotherapy (SBRT) deliver very focused, high-dose radiation in a small number of sessions, improving local control while minimizing side effects. SBRT has been increasingly used for patients with limited metastases (oligometastatic disease) as part of a multidisciplinary approach. Conventional external beam radiotherapy is used less often today but remains a valuable tool for palliation. Side effects depend on the treated area and may include fatigue, nausea, diarrhea, or localized skin irritation. Though not curative, radiotherapy is an important supportive treatment that improves quality of life in patients with advanced or metastatic RCC who experience pain, neurological issues, or other disabling symptoms.
Ayurvedic Treatment Approaches for Kidney Cancer
Ayurveda approaches kidney cancer as arbuda, a condition arising from Kapha–Meda accumulation, Vata obstruction, and Rakta dushti. Treatment strategies follow the classical three pillars of shodhana (purification), shamana (pacification), and rasayana (rejuvenation), supported by specialized mineral preparations and diet–lifestyle corrections.
Shodhana (Purification therapies)
Shodhana aims to eliminate deep-seated toxins (ama) and restore the integrity of agni (metabolic fire). For kidney cancer, therapeutic purgation (virechana) and medicated enemas (basti) are sometimes applied, though carefully modified depending on patient strength. Raktamokshana (controlled bloodletting) is occasionally described for related urinary disorders but is rarely applied in arbuda due to debility. Panchakarma protocols must be cautiously individualized; in weak patients, strong detox methods are avoided. The goal is to reduce Kapha–Meda accumulation and clear obstructed srotas. While modern oncology uses surgery or ablation to remove tumor bulk, Ayurveda uses shodhana to detoxify the system and halt progression at a constitutional level
[40]
Shamana (Pacification therapies)
Once purification is done or if the patient is too weak, shamana therapies are employed. These aim to pacify aggravated doshas, improve urinary flow, and reduce systemic symptoms. Classical formulations include Gandhak Rasayan, Kanchnar Guggulu, and Varunadi Kashaya, which are described in Bhaishajya Ratnavali and Charaka Samhita. Herbs like neem, turmeric, and guduchi provide anti-inflammatory and immunomodulatory support. Shamana treatments are often compared to targeted therapies in modern medicine, as they aim to restrain tumor growth rather than remove it outright. Regular monitoring of mutra dushti (urinary changes) guides adjustment. The emphasis is on balance and symptom relief while slowing arbuda progression [8].
Rasayana (Rejuvenation and immune support)
Rasayana therapy is the cornerstone of long-term cancer management in Ayurveda. It focuses on restoring ojas (vital energy) and enhancing immunity after dosha control. Rasayanas such as Amalaki, Ashwagandha, and Guduchi strengthen dhatus, while Suvarna Bhasma and Abhrak Bhasma are cited for deep tissue regeneration. In the context of RCC, rasayana parallels immunotherapy in its emphasis on empowering the body’s defense system. Modern studies suggest immunomodulatory, antioxidant, and adaptogenic properties of these agents, supporting their role in preventing recurrence and reducing cachexia. Rasayana therapy is not short-term; it is prescribed for months to years, making it a sustained approach for survival improvement and quality-of-life enhancement [8].
Bhasma formulations (Herbo-mineral preparations)
Ayurvedic oncology has long used carefully prepared metallic and mineral formulations, collectively known as bhasmas. For kidney cancer, preparations like Heerak Bhasma (diamond ash), Suvarna Bhasma (gold ash), and Trivanga Bhasma are described in classical rasashastra texts. These formulations are said to penetrate deeply into tissues, correcting dhatu-level imbalances and acting as rasayanas at a cellular level. They are always given in microdoses under strict guidance, with adjuvants like ghee, honey, or herbal decoctions to improve bioavailability and safety. Modern research suggests that nanoparticle forms of metals used in bhasmas may have unique cytotoxic effects on cancer cells while sparing normal tissue. Though controversial in biomedical circles, their integration under skilled supervision continues in Ayurvedic oncology
[41], 8].
Diet and lifestyle (Ahara and Vihara)
Ayurveda places equal importance on ahara (diet) and vihara (lifestyle). Patients are advised to avoid kshara (excessively salty or alkaline foods), preserved or processed foods, and viruddha ahara (incompatible combinations like milk with fish). Instead, light, easily digestible meals with fresh vegetables, barley, green gram, and seasonal fruits are emphasized. Daily routines support apana vayu balance, including regular bowel movement, adequate sleep, and stress management through meditation and pranayama. Yoga practices like gentle asanas enhance circulation and improve recovery. This lifestyle modification ensures that agni remains stable, preventing recurrence and strengthening immunity. In modern terms, this parallels nutritional oncology, where diet and activity are seen as core supportive therapies. Ayurveda, however, extends this by framing diet and lifestyle as integral to the very root of healing [8].
Kanchnar Varunadi Rasayana Avaleha- Main Medicine to Cure
(Herbal–mineral jam for tumor and kidney support; must be prepared only under an Ayurvedic doctor’s supervision)
What it is
Kanchnar Varunadi Rasayana Avaleha is a traditional Ayurvedic formulation made as a herbal jam. It combines healing herbs with carefully purified minerals to correct deep imbalances in the body. It is mainly used for conditions described as Arbuda (tumors) and Granthi (abnormal swellings), especially when the urinary system (Mutravaha Srotas) is disturbed.
Main herbs and their functions
- Kanchnar (Bauhinia variegata) – shrinks abnormal growths, reduces Kapha and Meda (fat tissue imbalance).
- Varuna (Crataeva nurvala) – improves urine flow, clears blockages in urinary channels.
- Guggulu (Commiphora mukul) – acts as a natural “scraper” of toxins and excess tissue, supports metabolism.
- Haridra / Turmeric (Curcuma longa) – cleanses blood, reduces inflammation, and fights abnormal cell growth.
- Neem (Azadirachta indica) – detoxifies blood, prevents infection, balances Pitta.
- Guduchi (Tinospora cordifolia) – boosts immunity, improves digestion, clears toxins.
- Amalaki (Emblica officinalis) – rich in Vitamin C, antioxidant, strengthens tissues and Ojas (vital energy).
- Triphala (Haritaki, Vibhitaki, Amalaki) – regulates digestion, improves elimination, balances all three doshas.
- Ashwagandha (Withania somnifera) – restores strength, reduces stress, prevents muscle wasting.
- Punarnava (Boerhavia diffusa) – reduces swelling, protects kidney function, acts as a diuretic.
- Gokshura (Tribulus terrestris) – supports urinary health, improves strength and vitality.
Minerals (Bhasmas) and their functions
(These are purified through classical Shodhana methods and used only in micro-doses)
- Swarna Bhasma (Gold ash) – acts as a Rasayana, boosts immunity, strengthens tissues, and improves longevity.
- Abhraka Bhasma (Mica ash) – rejuvenates tissues, improves energy, balances metabolism.
- Heeraka Bhasma (Diamond ash) – considered highly potent in classical texts, supports tumor control and deep tissue repair.
- Shuddha Gandhak Rasayan (Purified sulfur) – detoxifies, improves skin and blood health, balances doshas.
- (Optional) Bhallataka (Semecarpus anacardium, purified) – described as Arbuda-hara (tumor reducing) in texts, but must be used with extreme care.
How it is prepared (patient-friendly explanation)
- The main herbs (Kanchnar, Varuna, Guggulu, Triphala, Turmeric, Guduchi, etc.) are boiled in water until a concentrated decoction remains.
- This liquid is filtered and cooked with jaggery (or sugar) until it thickens into a syrup.
- Cow ghee is added during cooking to improve absorption and strength.
- When the mixture cools, honey is added for taste and medicinal synergy.
- Finally, in very small amounts, the purified minerals (like Swarna Bhasma, Abhraka Bhasma, Gandhak Rasayan) are mixed in by the Ayurvedic doctor.
- The result is a sweet, semi-solid herbal jam that carries both herbal and mineral benefits.
Why it is used
- Reduces abnormal growths and swelling (Arbuda, Granthi).
- Cleanses blood (Rakta shodhana), reduces inflammation.
- Improves kidney and urinary function (Mutravaha srotas shodhana).
- Restores strength and reduces fatigue (Daurbalya).
- Acts as a long-term Rasayana (rejuvenative), helping immunity and quality of life.
Important safety notes
- This is a powerful medicine and must not be made at home.
- Preparation requires expert knowledge of purification (Shodhana) of toxic herbs and minerals.
- The ingredients and their amounts will vary depending on the patient’s body type, strength, digestion, kidney function, and ongoing treatment.
- Must be used only under the guidance of an experienced Ayurvedic doctor.
- Regular monitoring (blood tests, urine tests, kidney and liver function) is essential during treatment.
Preparation of Kanchnar Varunadi Rasayana Avaleha
Ingredients (herbal base)
- Kanchnar bark
- Varuna bark
- Guggulu
- Turmeric
- Neem
- Guduchi
- Amalaki
- Triphala
- Ashwagandha
- Punarnava
- Gokshura
(Minerals like Swarna Bhasma, Abhraka Bhasma, Gandhak Rasayan are added only by a trained Ayurvedic doctor in very small doses after proper purification.)
Simple preparation method (for understanding only)
- Take equal parts (for example, 50 g each) of the herbal ingredients listed above.
- Coarsely powder them and boil in 16 times water (about 800 ml for 50 g total).
- Continue boiling on a mild flame until the water reduces to 1/4th (about 200 ml). This is called a decoction.
- Filter the decoction.
- Add jaggery or sugar (equal weight to the decoction, around 200 g). Cook until it becomes a thick syrup.
- Add 20–30 g of cow ghee while cooking. Stir until it reaches a jam-like consistency.
- Allow to cool. Then add 50 g of honey and mix well.
- Finally, the Ayurvedic doctor mixes in very small amounts of the purified minerals (Bhasmas) as per the patient’s condition.
Suggested dosage
- 10 g (about 1 teaspoonful) twice daily
- To be taken with lukewarm water, warm milk, or as directed by the doctor.
Safety notes
- This medicine is not for self-preparation. It requires expert handling of minerals and toxic herbs like Bhallataka.
- The ingredients and exact weights may change depending on patient’s body type, strength, kidney function, and overall health.
- Must be used only under supervision of an Ayurvedic doctor.
- Regular check-ups and monitoring are required during use.
Modern treatment for kidney cancer has advanced rapidly with targeted therapy and immunotherapy, yet its focus often remains palliative rather than curative.
Pharmaceutical focus on lifelong inhibition
Most new drugs are designed to block pathways that drive tumor growth. VEGF inhibitors reduce angiogenesis, while mTOR inhibitors slow cell growth [27]. These therapies do extend survival, but they rarely eliminate cancer. Instead, patients often remain on medication for years, sometimes for life, at enormous financial cost. Drug resistance eventually develops, and new lines of therapy are introduced in sequence [27, 28]. This cycle sustains the pharmaceutical model but leaves patients without a true endpoint.
Limited emphasis on cure
Conventional oncology invests heavily in treatments that control disease rather than eliminate it. Surgical removal remains the only curative option in localized disease, but beyond that, the system largely accepts incurability as the default. Even clinical trial endpoints often measure “progression-free survival” instead of cure. For many patients, this means ongoing therapy with side effects such as fatigue, hypertension, and organ toxicity, without the expectation of full recovery [29, 30].
Ayurveda’s holistic correction
In contrast, Ayurveda describes arbuda as a manifestation of systemic imbalance involving Kapha, Meda, Rakta, and blocked srotas. Its approach is not limited to shrinking the mass but aims to correct the terrain that allowed the tumor to develop [42], 8]. Through shodhana (detoxification), shamana (pacification), and rasayana (rejuvenation), Ayurveda addresses root-level pathology, prevents recurrence, and restores long-term vitality. Where modern medicine suppresses, Ayurveda seeks to harmonize—reducing not only the tumor burden but also the risk environment that sustains it.
This difference—control versus cure—is the defining critique. Modern drugs have transformed survival statistics, but Ayurveda’s framework still offers a vision of complete healing, integrating body, mind, and immunity.
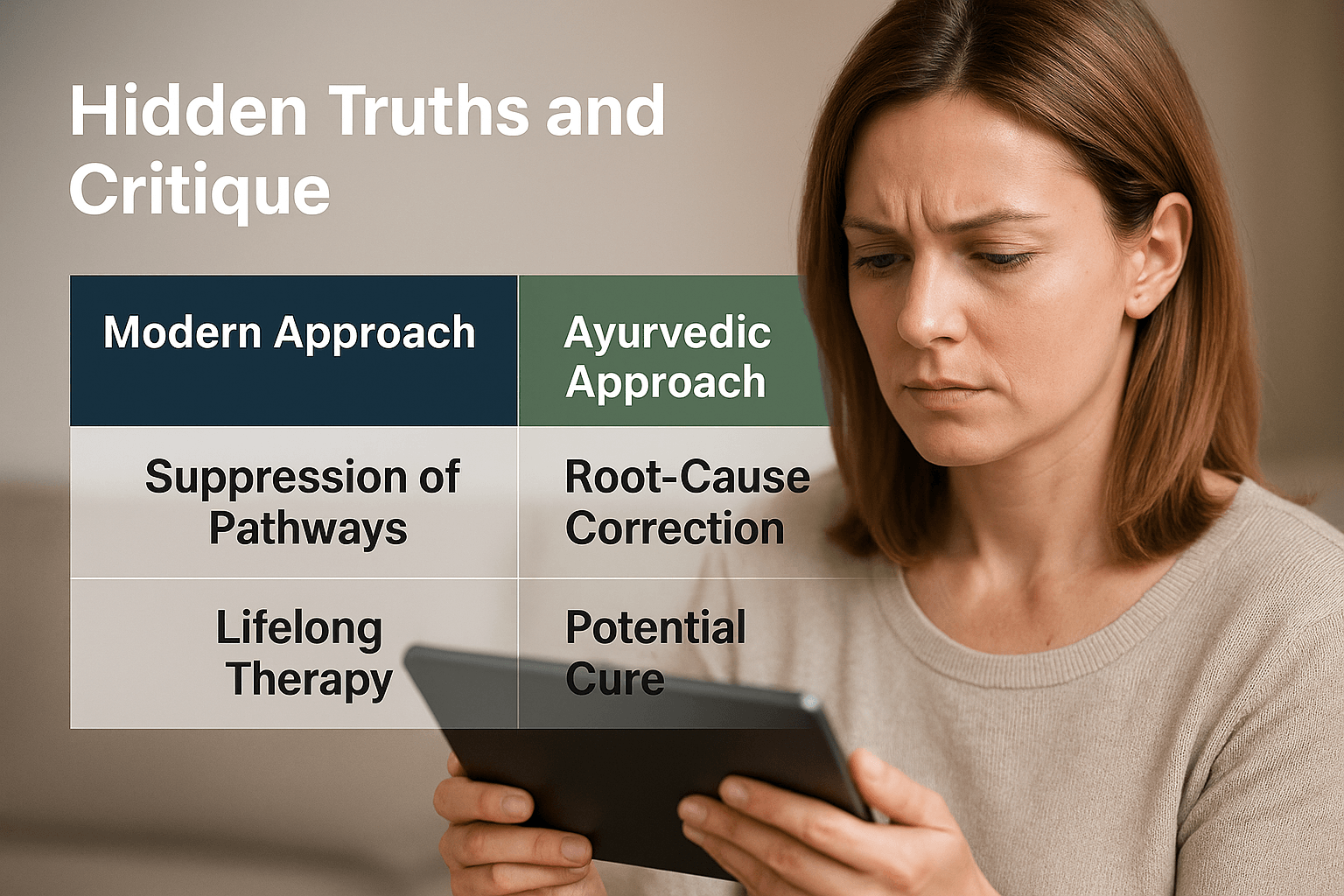
Modern treatment for kidney cancer has advanced rapidly with targeted therapy and immunotherapy, yet its focus often remains palliative rather than curative.
Pharmaceutical focus on lifelong inhibition
Most new drugs are designed to block pathways that drive tumor growth. VEGF inhibitors reduce angiogenesis, while mTOR inhibitors slow cell growth [27]. These therapies do extend survival, but they rarely eliminate cancer. Instead, patients often remain on medication for years, sometimes for life, at enormous financial cost. Drug resistance eventually develops, and new lines of therapy are introduced in sequence [27, 28]. This cycle sustains the pharmaceutical model but leaves patients without a true endpoint.
Limited emphasis on cure
Conventional oncology invests heavily in treatments that control disease rather than eliminate it. Surgical removal remains the only curative option in localized disease, but beyond that, the system largely accepts incurability as the default. Even clinical trial endpoints often measure “progression-free survival” instead of cure. For many patients, this means ongoing therapy with side effects such as fatigue, hypertension, and organ toxicity, without the expectation of full recovery [29, 30].
Ayurveda’s holistic correction
In contrast, Ayurveda describes arbuda as a manifestation of systemic imbalance involving Kapha, Meda, Rakta, and blocked srotas. Its approach is not limited to shrinking the mass but aims to correct the terrain that allowed the tumor to develop [43], 8]. Through shodhana (detoxification), shamana (pacification), and rasayana (rejuvenation), Ayurveda addresses root-level pathology, prevents recurrence, and restores long-term vitality. Where modern medicine suppresses, Ayurveda seeks to harmonize—reducing not only the tumor burden but also the risk environment that sustains it.
This difference—control versus cure—is the defining critique. Modern drugs have transformed survival statistics, but Ayurveda’s framework still offers a vision of complete healing, integrating body, mind, and immunity.
Frequently Asked Questions (FAQ)
Can kidney cancer be cured completely?
In modern medicine, surgery offers the best chance of cure when the tumor is still confined to the kidney [44]. In advanced stages, treatments like targeted therapy or immunotherapy may control the disease but usually do not cure it. Ayurveda takes a different view, aiming not only to remove or shrink the tumor but also to correct the body’s internal imbalance (Kapha, Meda, Rakta, and srotas blockage) so recurrence can be prevented [45], 8].
What are the early warning signs I should look out for?
The classic signs are blood in urine, flank pain, and an abdominal lump [36]. However, many cases are silent until late. Subtle symptoms include unexplained weight loss, fever, fatigue, anemia, or swelling in the legs [37]. Rare symptoms like sudden varicocele in men, high calcium levels, or abnormal red blood cell counts can also signal kidney cancer [38].
How is kidney cancer diagnosed?
Doctors use imaging tests such as ultrasound, CT scan, MRI, or PET scan to detect tumors
[46]. A biopsy confirms the diagnosis. Blood and urine tests may show changes like anemia, abnormal kidney function, or paraneoplastic effects. Ayurveda uses a different lens—examining nidan panchaka (causes, symptoms, progression, relief factors, and disease pathway) to understand the patient’s full-body imbalance
[47], 8].
Is chemotherapy useful in kidney cancer?
Unlike other cancers, kidney cancer does not respond well to standard chemotherapy [29]. That’s why most doctors recommend surgery, targeted therapy, or immunotherapy instead.
How does Ayurveda treat kidney cancer?
Ayurveda treats arbuda by focusing on three steps: Shodhana (detoxification therapies like virechana), Shamana (balancing medicines like Kanchnar Guggulu, Varunadi decoction, Gandhak Rasayan), and Rasayana (rejuvenating herbs like Amalaki, Guduchi, and Ashwagandha, along with Swarna or Abhrak Bhasma in microdoses). The aim is to reduce tumor growth, restore immunity, and strengthen tissues [31–34].
Is it safe to combine Ayurveda with modern treatments?
Yes, in most cases integrative care can be safe and beneficial when supervised by qualified doctors on both sides. Ayurvedic rasayana therapy can help reduce side effects, improve strength, and enhance recovery. But self-medication is risky—especially with mineral preparations like bhasmas—and must be avoided. Always inform your oncologist and Ayurvedic physician about all medicines you are taking.
What lifestyle changes help in kidney cancer?
From the modern side, quitting smoking, maintaining a healthy weight, and controlling blood pressure lower risk
[48]. Ayurveda recommends avoiding excessively salty, oily, or preserved foods (kshara and viruddha ahara), and instead focusing on light, digestible meals with fresh vegetables, barley, green gram, and seasonal fruits. Yoga, meditation, and pranayama further support immunity and reduce stress.
Can Ayurveda prevent recurrence after surgery?
Yes, Rasayana therapy is specifically designed to restore ojas (vital strength) and protect dhatus (tissues). By correcting the internal terrain, Ayurveda reduces the chances of cancer returning, while also improving quality of life after nephrectomy or targeted therapy [8, 33].
References
[6] Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa).
[8] Mishra, B. (2016). Bhavaprakasha of Bhavamishra. Varanasi: Chaukhamba Sanskrit Bhawan. (Madhyama Khanda, Arbuda Nidana and Chikitsa Adhyaya).
[25] Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E., & Ulbright, T. M. (2016). The 2016 WHO classification of tumours of the urinary system and male genital organs—Part A: Renal, penile, and testicular tumours. European Urology, 70(1), 93–105. https://doi.org/10.1016/j.eururo.2016.02.029
[27] Linehan, W. M., & Ricketts, C. J. (2019). The metabolic basis of kidney cancer. Seminars in Cancer Biology, 61, 59–67. https://doi.org/10.1016/j.semcancer.2019.09.006
[36] Capitanio, U., & Montorsi, F. (2016). Renal cancer. Lancet, 387(10021), 894–906. https://doi.org/10.1016/S0140-6736(15)00046-X
[37] Campbell, S. C., Clark, P. E., Chang, S. S., Karam, J. A., Souter, L., Uzzo, R. G., … & American Urological Association. (2021). Renal mass and localized renal cancer: AUA guideline. Journal of Urology, 206(2), 199–208. https://doi.org/10.1097/JU.0000000000001871
[38] Choueiri, T. K., & Motzer, R. J. (2017). Systemic therapy for metastatic renal-cell carcinoma. New England Journal of Medicine, 376(4), 354–366. https://doi.org/10.1056/NEJMra1601333
[39] Heng, D. Y. C., Xie, W., Regan, M. M., Warren, M. A., Golshayan, A. R., Sahi, C., … & Choueiri, T. K. (2009). Prognostic factors for overall survival in patients with metastatic renal-cell carcinoma treated with vascular endothelial growth factor–targeted agents: Results from a large, multicenter study. Journal of Clinical Oncology, 27(34), 5794–5799. https://doi.org/10.1200/JCO.2008.21.4809
[40] Jonasch, E., Gao, J., & Rathmell, W. K. (2014). Renal cell carcinoma. BMJ, 349, g4797. https://doi.org/10.1136/bmj.g4797
All Source
- Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E., & Ulbright, T. M. (2016). The 2016 WHO classification of tumours of the urinary system and male genital organs—Part A: Renal, penile, and testicular tumours. European Urology, 70(1), 93–105. https://doi.org/10.1016/j.eururo.2016.02.029 ↩
- Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E., & Ulbright, T. M. (2016). The 2016 WHO classification of tumours of the urinary system and male genital organs—Part A: Renal, penile, and testicular tumours. European Urology, 70(1), 93–105. https://doi.org/10.1016/j.eururo.2016.02.029 ↩
- Jonasch, E., Gao, J., & Rathmell, W. K. (2014). Renal cell carcinoma. BMJ, 349, g4797. https://doi.org/10.1136/bmj.g4797 ↩
- Heng, D. Y. C., Xie, W., Regan, M. M., Warren, M. A., Golshayan, A. R., Sahi, C., … & Choueiri, T. K. (2009). Prognostic factors for overall survival in patients with metastatic renal-cell carcinoma treated with vascular endothelial growth factor–targeted agents: Results from a large, multicenter study. Journal of Clinical Oncology, 27(34), 5794–5799. https://doi.org/10.1200/JCO.2008.21.4809 ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E., & Ulbright, T. M. (2016). The 2016 WHO classification of tumours of the urinary system and male genital organs—Part A: Renal, penile, and testicular tumours. European Urology, 70(1), 93–105. https://doi.org/10.1016/j.eururo.2016.02.029 ↩
- Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E., & Ulbright, T. M. (2016). The 2016 WHO classification of tumours of the urinary system and male genital organs—Part A: Renal, penile, and testicular tumours. European Urology, 70(1), 93–105. https://doi.org/10.1016/j.eururo.2016.02.029 ↩
- Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E., & Ulbright, T. M. (2016). The 2016 WHO classification of tumours of the urinary system and male genital organs—Part A: Renal, penile, and testicular tumours. European Urology, 70(1), 93–105. https://doi.org/10.1016/j.eururo.2016.02.029 ↩
- Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E., & Ulbright, T. M. (2016). The 2016 WHO classification of tumours of the urinary system and male genital organs—Part A: Renal, penile, and testicular tumours. European Urology, 70(1), 93–105. https://doi.org/10.1016/j.eururo.2016.02.029 ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Jonasch, E., Gao, J., & Rathmell, W. K. (2014). Renal cell carcinoma. BMJ, 349, g4797. https://doi.org/10.1136/bmj.g4797 ↩
- Jonasch, E., Gao, J., & Rathmell, W. K. (2014). Renal cell carcinoma. BMJ, 349, g4797. https://doi.org/10.1136/bmj.g4797 ↩
- Jonasch, E., Gao, J., & Rathmell, W. K. (2014). Renal cell carcinoma. BMJ, 349, g4797. https://doi.org/10.1136/bmj.g4797 ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Jonasch, E., Gao, J., & Rathmell, W. K. (2014). Renal cell carcinoma. BMJ, 349, g4797. https://doi.org/10.1136/bmj.g4797 ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Heng, D. Y. C., Xie, W., Regan, M. M., Warren, M. A., Golshayan, A. R., Sahi, C., … & Choueiri, T. K. (2009). Prognostic factors for overall survival in patients with metastatic renal-cell carcinoma treated with vascular endothelial growth factor–targeted agents: Results from a large, multicenter study. Journal of Clinical Oncology, 27(34), 5794–5799. https://doi.org/10.1200/JCO.2008.21.4809 ↩
- Jonasch, E., Gao, J., & Rathmell, W. K. (2014). Renal cell carcinoma. BMJ, 349, g4797. https://doi.org/10.1136/bmj.g4797 ↩
- Heng, D. Y. C., Xie, W., Regan, M. M., Warren, M. A., Golshayan, A. R., Sahi, C., … & Choueiri, T. K. (2009). Prognostic factors for overall survival in patients with metastatic renal-cell carcinoma treated with vascular endothelial growth factor–targeted agents: Results from a large, multicenter study. Journal of Clinical Oncology, 27(34), 5794–5799. https://doi.org/10.1200/JCO.2008.21.4809 ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E., & Ulbright, T. M. (2016). The 2016 WHO classification of tumours of the urinary system and male genital organs—Part A: Renal, penile, and testicular tumours. European Urology, 70(1), 93–105. https://doi.org/10.1016/j.eururo.2016.02.029 ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E., & Ulbright, T. M. (2016). The 2016 WHO classification of tumours of the urinary system and male genital organs—Part A: Renal, penile, and testicular tumours. European Urology, 70(1), 93–105. https://doi.org/10.1016/j.eururo.2016.02.029 ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Heng, D. Y. C., Xie, W., Regan, M. M., Warren, M. A., Golshayan, A. R., Sahi, C., … & Choueiri, T. K. (2009). Prognostic factors for overall survival in patients with metastatic renal-cell carcinoma treated with vascular endothelial growth factor–targeted agents: Results from a large, multicenter study. Journal of Clinical Oncology, 27(34), 5794–5799. https://doi.org/10.1200/JCO.2008.21.4809 ↩
- Sharma, P. V. (2018). Charaka Samhita (English Translation with Critical Notes). Varanasi: Chaukhamba Orientalia. (Chikitsa Sthana 7/30 – Arbuda Chikitsa). ↩
- Jonasch, E., Gao, J., & Rathmell, W. K. (2014). Renal cell carcinoma. BMJ, 349, g4797. https://doi.org/10.1136/bmj.g4797 ↩











2 Responses
Good fitness tips very impressive
Good tips. very impressive