- What is HPV and why it is often silent
- Symptoms of HPV
- HPV-Associated Disorders: Common, Less Common, and Rare Conditions
- Less Common but Clinically Important HPV-Associated Conditions
- Rare but Clinically Significant HPV-Associated Conditions
- Immune Suppression, STDs, Viral Co-Infections, Microbiome, and Their Role in HPV Persistence
- Why Treating HPV Requires More Than Wart Removal
- How Ayurveda Clears HPV at the Root Level
- Why Ayurvedic Treatment Prevents Recurrence
- Why This Approach Takes Time but Leads to Stability
- Diagnosis of HPV
- Why HPV Persists in Some People Despite Normal Screening
- Clinical Implications for Patients
- Why modern medicine cannot fully “cure” HPV
- Ayurvedic Cure for HPV- The complete root-cause framework
- The four pillars of Ayurvedic HPV care
- Bhallataka Rasayana Avaleha (central Rasayana medicine)
- How to Take It (Dosage)
- Critical Patient Safety Warning About Avaleha Medicines
- Why Market-Bought Avaleha Will Not Work
- Integrative Care Reminder
- FAQs
- References
HPV is a very common virus that often clears naturally, but some high-risk types can persist and cause cervical and other cancers. Modern medicine prevents HPV through vaccination and reduces risk through screening, but it does not directly “erase” an existing infection. Ayurveda approaches HPV by correcting the internal terrain through digestion, immunity (Ojas), blood and tissue purification (Rakta Dhatu), and Rasayana therapy, with the goal of supporting long-term clearance and recurrence prevention. Screening and follow-up remain essential.
What is HPV and why it is often silent
Human Papillomavirus (HPV) refers to a large group of viruses. Many HPV infections produce no symptoms and may clear on their own within 1 to 2 years, especially in people with healthy immune function. The concern arises when HPV persists, particularly high-risk types that can cause precancerous cellular changes and cancers. HPV is the primary cause of cervical cancer, and HPV-related cancers can also affect the anus, penis, vulva, vagina, and oropharynx.
Human Papillomavirus (HPV) is a group of more than 200 related viruses. Around 40 of these strains infect the genital tract, mouth, and throat. According to the World Health Organization, over 80% of sexually active men and women will contract HPV at some point in their lives [1].
Most HPV infections do not cause symptoms and are cleared naturally within one to two years. However, some strains can persist in the body and lead to serious health issues.
Global risk and why Western countries still see serious HPV harm
HPV is the most common viral sexually transmitted infection (STI) worldwide. High-risk HPV types, particularly HPV-16 and HPV-18, are responsible for nearly 70% of cervical cancer cases across the globe [2]. Cervical cancer is currently the fourth most common cancer in women, with over 600,000 new cases and 340,000 deaths annually [3].
Even in advanced health systems, HPV causes harm because early changes are often silent and people skip screening. Countries such as the UK, USA, Canada, and Australia have strong prevention programs, but gaps in screening participation and follow-up still leave room for preventable disease.
Low-risk strains, like HPV-6 and HPV-11, do not cause cancer but are responsible for about 90% of genital warts [4]. HPV is also linked to other cancers, including anal, penile, vulvar, vaginal, and oropharyngeal cancers, affecting both men and women [5].
Limitations of Modern Prevention
Vaccines such as Gardasil and Cervarix are highly effective in preventing infection with certain high-risk HPV strains. Still, they have some limitations:
- They do not protect against all HPV types.
- They work best when given before sexual activity begins.
- They do not treat existing infections.
- Accessibility remains limited in low- and middle-income countries, where the highest burden of cervical cancer occurs [6].
The Ayurvedic Perspective
Ayurveda interprets HPV through three core concepts:
- Krimi (microorganisms) – representing the viral invasion.
- Dushta Rakta (impure blood) – indicating a disturbed internal environment.
- Doshic imbalance (Pitta and Kapha aggravation) – making the body more vulnerable.
From an Ayurvedic lens, persistent HPV infection develops when Ojas (vital immunity) is weakened due to factors like poor diet, stress, and unhealthy lifestyle choices.
How Ayurveda Approaches HPV
Ayurveda doesn’t just focus on removing warts or suppressing abnormal cells. Instead, it aims at restoring complete balance:
- Shodhana (Detoxification): Therapies like Virechana (purgation) and Raktamokshana (bloodletting) help cleanse toxins.
- Shamana (Pacification): Herbs and mineral preparations balance disturbed doshas and strengthen Rakta Dhatu (blood tissue).
- Rasayana (Rejuvenation): Immune-boosting formulations such as Guduchi, Neem, Ashwagandha, and Swarna Bhasma restore Ojas and prevent recurrence.
This holistic framework highlights Ayurveda’s root-cause approach. Rather than just suppressing symptoms, it works to strengthen the immune system, balance internal energies, and prevent long-term risks like precancerous changes or cancer development [7].
Clinical disclaimer
This article is for education only and does not replace medical diagnosis or treatment. HPV can require screening and follow-up using Pap tests, HPV DNA testing, colposcopy, and biopsy when indicated. Ayurvedic care can be supportive and integrative, but it should be used responsibly and alongside appropriate medical supervision, especially if there are abnormal screening results or suspected precancer or cancer.
Safety and supervision notice for Ayurveda
Some classical Ayurvedic medicines discussed here, including Bhallataka Rasayana Avaleha and mineral Rasayana preparations, are potent and require correct purification and expert dosing. Self-medication and home preparation without supervision are not advised. Your safety depends on quality-controlled preparation, correct assessment, and monitoring.
Symptoms of HPV

Human Papillomavirus (HPV) is often called a “silent infection” because the majority of cases do not produce noticeable symptoms. In most healthy individuals, the immune system clears the virus within one to two years [1]. However, when HPV persists or involves high-risk strains, symptoms can appear in diverse ways — ranging from benign warts to precancerous lesions and cancers.
Common Symptoms
Genital Warts
- Caused mainly by HPV-6 and HPV-11.
- Appear as soft bumps or clusters around the vulva, vagina, cervix, penis, scrotum, or anus.
- Can be raised, flat, or cauliflower-like in shape.
- May cause itching or mild irritation [2].
Oral and Throat Lesions
- HPV can infect the oral cavity, tonsils, and throat.
- Symptoms include warts inside the mouth, persistent sore throat, or hoarseness.
- In some cases, oral HPV can progress to oropharyngeal cancers [3].
Cervical Cell Changes
- High-risk HPV types (especially 16 and 18) cause silent alterations in cervical cells.
- These changes are typically detected only by Pap smears or HPV DNA tests.
- If untreated, they may progress to cervical intraepithelial neoplasia (CIN) or cervical cancer [4].
Cancer Risks
Persistent infection with oncogenic HPV is a major cause of:
- Cervical cancer (responsible for 70% of cases)
- Anal cancer
- Penile cancer
- Vulvar and vaginal cancers
- Oropharyngeal cancers [5]
Rare Symptoms
Recurrent Respiratory Papillomatosis (RRP)
- Benign but potentially dangerous wart growths in the larynx or trachea.
- Causes hoarseness, chronic cough, and sometimes life-threatening airway obstruction [6].
Conjunctival Papillomas
- Noncancerous growths on the eye surface.
- Can cause eye irritation, redness, or blurred vision [7].
HPV-Related Nail Lesions
- Warts around or under fingernails and toenails (periungual or subungual).
- Sometimes misdiagnosed as fungal infection or melanoma [8].
Persistent Ulcers and Painful Lesions
- Some individuals develop chronic ulcers in the genital or oral regions.
- These are slow-healing and may mimic precancerous or cancerous lesions [9].
Systemic Symptoms in Immunocompromised Patients
- In HIV-positive individuals or those with suppressed immunity, HPV may cause widespread, aggressive wart growths.
- Higher likelihood of malignant transformation [10].
Overlooked or Special Situations
Pregnancy-Related Changes
- Genital warts may enlarge rapidly due to hormonal shifts and increased blood flow.
- In rare cases, large warts may obstruct the birth canal.
- Transmission during childbirth can cause juvenile-onset recurrent respiratory papillomatosis (JORRP) in newborns [11].
Impact on Fertility
- While HPV itself does not directly cause infertility, it may reduce sperm quality in men or cause cervical narrowing after treatment in women.
- These indirect effects can hinder conception [12].
Non-Genital Skin Warts
- Certain HPV strains (types 1, 2, 4) cause common warts on hands, feet, and other skin areas.
- Plantar warts can be painful, especially in athletes or barefoot workers [13].
Subclinical Infections
- Many HPV infections remain invisible.
- Special tests like acetic acid application during colposcopy reveal faint white lesions (acetowhite epithelium) [14].
Psychological Impact
- Diagnosis of HPV or genital warts often triggers anxiety, shame, or depression.
- Psychosocial symptoms are clinically significant but frequently overlooked [15].
HPV-Associated Disorders: Common, Less Common, and Rare Conditions

Human Papillomavirus is not a single disease but a group of viruses capable of affecting multiple epithelial surfaces of the body. Depending on viral type, duration of infection, immune response, and tissue involved, HPV can lead to benign lesions, precancerous changes, or invasive malignancies. These outcomes are interconnected and represent a spectrum rather than isolated conditions.
Commonly Recognised HPV-Related Disorders
These conditions are the most widely recognised and form the foundation of modern screening and prevention programs.
Genital warts
Genital warts are usually caused by low-risk HPV types such as HPV-6 and HPV-11. They can appear on the vulva, vagina, cervix, penis, scrotum, perianal region, or anus. Although non-cancerous, genital warts often recur after removal by cauterisation, cryotherapy, or topical agents. Recurrence occurs because local treatments eliminate visible lesions but do not necessarily clear underlying viral persistence or restore immune surveillance.
Cervical intraepithelial neoplasia
Cervical intraepithelial neoplasia refers to abnormal cellular changes in the cervical epithelium detected through Pap smear cytology or HPV DNA testing. CIN represents a continuum of dysplasia, from mild changes to high-grade lesions. While CIN is not cancer, persistent high-grade CIN significantly increases the risk of progression if not appropriately monitored or treated.
Cervical cancer
Cervical cancer is the most extensively studied outcome of persistent high-risk HPV infection, particularly HPV-16 and HPV-18. It usually develops slowly over many years and often remains asymptomatic in early stages. This prolonged silent phase is what makes regular screening effective in preventing invasive disease when follow-up is timely.
Other anogenital cancers
HPV is also causally linked to cancers of the anus, penis, vulva, and vagina. These cancers are less common than cervical cancer but are clinically significant and increasingly recognised. Persistent high-risk HPV infection plays a central role, especially in individuals with immune suppression, smoking history, or delayed diagnosis.
Precancerous HPV-Related Disorders Beyond the Cervix
HPV-associated precancer is not limited to the cervix. Several other epithelial sites may develop intraepithelial neoplasia that carries long-term risk.
Anal intraepithelial neoplasia
Anal intraepithelial neoplasia involves precancerous changes in the anal canal epithelium linked to high-risk HPV, most commonly HPV-16. It is more frequently observed in certain risk groups and can progress if high-grade lesions persist without detection.
Vulvar intraepithelial neoplasia
Vulvar intraepithelial neoplasia includes HPV-associated forms that may present with itching, burning, discoloration, or subtle skin changes. Symptoms may be mild or absent, which can delay diagnosis and increase persistence risk.
Penile and vaginal intraepithelial neoplasia
HPV can also cause precancerous lesions in penile and vaginal tissues. These conditions are uncommon but clinically relevant, particularly in individuals with long-standing infection or reduced immune competence.
Bowenoid papulosis
Bowenoid papulosis is a high-grade squamous intraepithelial condition associated with high-risk HPV. It may resemble benign genital papules but represents significant dysplasia and requires careful clinical evaluation rather than reassurance alone.
HPV-Related Disorders Outside the Genital Tract
HPV does not exclusively affect the reproductive system. Several non-genital manifestations are clinically important.
Cutaneous warts
Many HPV types infect the skin rather than mucosal surfaces. These can cause common warts on the hands, flat warts on the face or limbs, and plantar warts on the soles. While usually benign, widespread or persistent cutaneous warts may reflect broader susceptibility or immune imbalance.
Oral and oropharyngeal HPV involvement
HPV can infect the oral cavity and oropharynx, including the tonsils and base of the tongue. In some cases, this leads to visible papillomas, while in others it remains silent but contributes to cancer risk over time. HPV-related oropharyngeal cancer has become an increasingly recognised clinical entity.
Less Common but Clinically Important HPV-Associated Conditions

In addition to well-recognised genital warts and cervical disease, HPV is associated with a range of less frequently discussed conditions that are often overlooked in routine patient education. These conditions may not always present with obvious findings on standard screening, yet they can significantly affect long-term health, immune stability, and quality of life.
Oropharyngeal HPV infections
HPV can infect the mucosal tissues of the throat, tonsils, and base of the tongue. In many cases, these infections remain silent for long periods and may present only with subtle symptoms such as persistent throat discomfort, voice changes, a sensation of a lump in the throat, or recurrent sore throat without clear cause. Because routine HPV screening does not include the oropharyngeal region, these infections are often detected late or only after symptoms progress.
Recurrent respiratory papillomatosis
Recurrent respiratory papillomatosis is a rare but clinically significant condition in which wart-like growths develop in the larynx or other parts of the airway. These growths can cause hoarseness, chronic cough, breathing difficulty, or voice fatigue. The condition is known for frequent recurrence and may require repeated medical or surgical intervention. Its chronic nature reflects persistent viral activity combined with local immune vulnerability.
Chronic inflammatory genital mucosal changes
HPV may contribute to ongoing inflammatory changes in the genital mucosa that are not cancerous and may not meet criteria for dysplasia. These changes can manifest as persistent irritation, burning, abnormal discharge, tissue sensitivity, or discomfort during sexual activity. Such symptoms are often dismissed or attributed to non-specific causes, yet they may reflect ongoing viral presence and immune imbalance at the tissue level.
HPV-associated dysplasia in immunocompromised individuals
In individuals with immune suppression, whether due to medical conditions, medications, or chronic viral co-infections, HPV behaves differently. Dysplastic changes may develop more rapidly, persist longer, or recur despite treatment. Viral clearance is often slower, and the risk of progression is higher even when lesions are detected early. This group requires closer monitoring and a broader therapeutic perspective.
Psychological and sexual health impact
Beyond physical manifestations, HPV carries a substantial psychological and sexual health burden. Many individuals experience anxiety related to cancer risk, fear of transmission to partners, shame or stigma, relationship strain, and reduced sexual confidence. These effects are increasingly recognised as integral components of HPV-related disease, influencing overall wellbeing and adherence to follow-up care.
Ayurvedic Interpretation of These Presentations
From an Ayurvedic perspective, these varied and seemingly unrelated presentations are not viewed as isolated surface disorders. They are understood as expressions of deep-seated Rakta Dhatu involvement, persistent Krimi influence, and gradual depletion of Ojas. When immune vitality is compromised and tissue nourishment is weakened, HPV is able to manifest across different anatomical sites and clinical forms.
This understanding explains why local or symptom-based interventions alone often fail to provide lasting resolution and why systemic, immunity-focused strategies are emphasised in Ayurvedic management.
Rare but Clinically Significant HPV-Associated Conditions
Although uncommon, these conditions are important because they are often missed or misdiagnosed.
Recurrent respiratory papillomatosis
Recurrent respiratory papillomatosis involves wart-like growths in the larynx or respiratory tract. It may cause hoarseness, voice changes, or breathing difficulty and can require repeated interventions due to recurrence.
Giant condyloma
Giant condyloma is a rare, locally aggressive anogenital tumour most often associated with low-risk HPV types. It differs from typical genital warts by its size, invasive behavior, and potential for significant tissue destruction.
Epidermodysplasia verruciformis
Epidermodysplasia verruciformis is a rare condition characterised by heightened susceptibility to certain HPV types, leading to widespread skin lesions and an increased risk of skin malignancy over time. It highlights the role of host immunity in HPV expression.
Country-Specific Screening Implications
Across the United Kingdom, United States, Canada, and Australia, organised screening programs focus primarily on cervical cancer prevention through HPV testing and cytology. Routine population screening for anal, penile, vulvar, vaginal, or oropharyngeal HPV-related disease is not widely implemented.
In the United Kingdom, NHS cervical screening relies on primary HPV testing with cytology follow-up, but non-cervical HPV-related conditions are evaluated based on symptoms or risk factors.
In the United States, screening guidelines emphasise cervical testing, while other HPV-associated sites are managed through symptom-based assessment and risk-based clinical judgement.
In Canada, cervical screening programs are transitioning toward HPV DNA testing, with similar limitations for non-cervical disease surveillance.
In Australia, despite advanced HPV vaccination and screening programs, routine screening remains cervix-focused, and other HPV-related conditions require proactive clinical evaluation when symptoms arise.
Across all these regions, a key clinical reality remains. Screening detects cellular risk and disease progression, not viral clearance. This explains why patients with normal screening results may still experience recurrence, persistence, or related disorders and why long-term immune-focused strategies are increasingly discussed alongside routine screening.
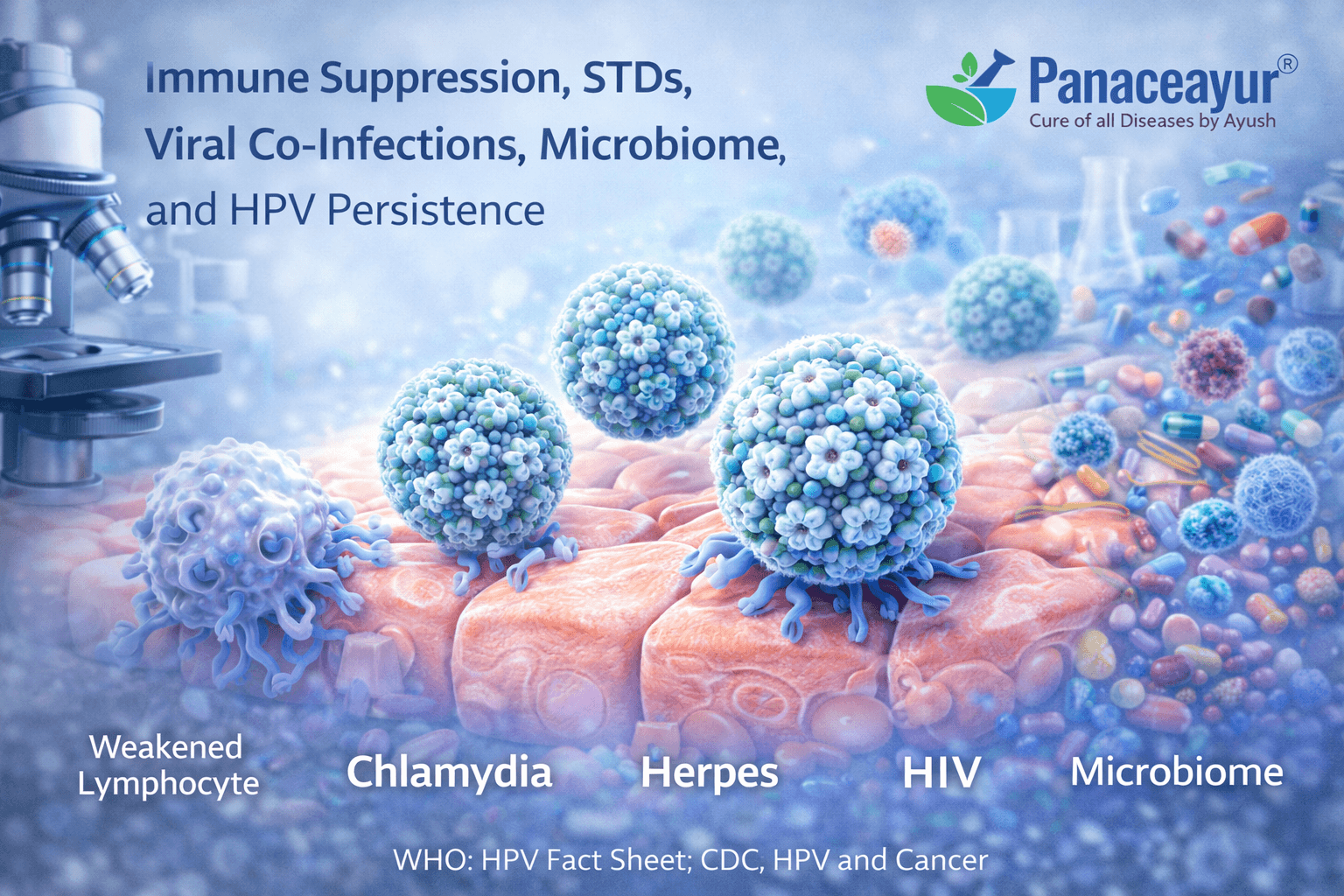
HPV persistence is rarely the result of HPV alone. In a significant number of individuals, long-term HPV infection reflects a deeper interaction between immune suppression, sexually transmitted infections, chronic viral co-infections, and disruption of the local microbiome. When these factors coexist, HPV is more likely to persist silently, reactivate intermittently, or recur despite normal screening results.
Immune Suppression as the Central Driver of Persistence
Clearance of HPV depends primarily on effective cell-mediated immunity. When immune surveillance is weakened, HPV-infected cells may not be recognised or eliminated efficiently. Immune suppression may be caused by chronic psychological stress, poor sleep, nutritional deficiencies, smoking, alcohol excess, metabolic disease, autoimmune disorders, advancing age, or prolonged inflammation.
Medical causes of immune suppression include HIV infection, long-term corticosteroid use, chemotherapy, biologic immune-modulating drugs, and post-transplant medications. In these settings, HPV often behaves more aggressively, with higher rates of persistence, recurrence of warts, and progression to precancerous lesions even when screening intervals are followed.
Role of Sexually Transmitted Infections in Sustaining HPV
Sexually transmitted infections significantly influence HPV behaviour by damaging mucosal barriers and maintaining chronic inflammation. Infections such as Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, Mycoplasma genitalium, syphilis, and HIV alter epithelial integrity and immune signalling at the genital and anal mucosa.
Even when these infections are asymptomatic or partially treated, they may create a permissive tissue environment that allows HPV to persist. This explains why individuals with a history of recurrent STIs often experience prolonged HPV positivity or repeated wart formation despite normal cytology.
Herpesvirus Co-Infections and Immune Exhaustion
Beyond classic STDs, herpesviruses play a critical but under-recognised role in HPV persistence. Herpes simplex virus types 1 and 2 can cause repeated mucosal inflammation and epithelial micro-injury, weakening local antiviral defences. Recurrent herpes outbreaks exhaust immune resources and may facilitate HPV persistence at the same anatomical sites.
Cytomegalovirus and Epstein–Barr virus are widespread latent infections that continuously modulate immune function. Although often clinically silent, they exert chronic immune pressure and are associated with immune dysregulation, especially under stress or illness. In such conditions, immune prioritisation may shift away from HPV clearance.
Human herpesvirus-6 and human herpesvirus-7 are known to infect immune cells and influence cytokine signalling. Their reactivation can contribute to immune suppression and altered antiviral responses, indirectly supporting HPV persistence.
Human herpesvirus-8, although less common, is associated with immune compromise and oncogenic processes. In individuals with immune suppression, co-existence of HPV and HHV-8 reflects a broader failure of immune containment rather than isolated viral behaviour.
Rubella and Immune Memory Disruption
Rubella infection or immune memory alterations related to viral exposure can influence immune regulation, particularly in women of reproductive age. Although rubella is not directly oncogenic, immune activation or dysregulation associated with viral exposure may affect how the immune system responds to other persistent viruses such as HPV.
This interaction becomes clinically relevant when multiple viral exposures coexist and immune balance is already compromised.
Microbiome Disruption and Viral Survival
The genital, anal, and oral microbiome plays a crucial role in mucosal immunity. Healthy microbial communities support epithelial integrity, regulate inflammation, and assist immune recognition of pathogens. Sexually transmitted infections, repeated antibiotic use, poor hygiene practices, and chronic inflammation disrupt this balance.
Loss of protective Lactobacillus species in the vaginal microbiome, recurrent bacterial vaginosis, or dysbiosis of the anal and oral microbiome creates conditions favourable for HPV persistence. Microbiome disruption also amplifies the effects of viral co-infections, compounding immune exhaustion.
Combined Viral Load and Immune Overload
When HPV exists alongside HSV, CMV, EBV, HHV-6, HHV-7, or HHV-8, the immune system is required to manage multiple latent and active infections simultaneously. This cumulative viral burden can overwhelm immune surveillance, allowing HPV to persist at low levels without producing abnormal screening results.
This explains why some individuals experience fluctuating HPV test results, recurrent lesions, or long-term anxiety despite adherence to screening guidelines.
Why Screening Does Not Capture These Interactions
Cervical screening programs are designed to detect cellular abnormalities and high-risk HPV types at specific sites. They do not evaluate immune competence, latent viral co-infections, microbiome health, or systemic viral burden. As a result, HPV may persist in the presence of untreated STIs or latent herpesvirus infections even when screening reports are normal.
This limitation is consistent across healthcare systems in the United Kingdom, United States, Canada, and Australia, where screening remains cervix-focused and symptom-driven for other HPV-related sites.
Clinical Implications for Long-Term HPV Resolution
Persistent HPV should prompt a broader clinical perspective that includes immune status, STD and viral co-infection burden, microbiome health, and lifestyle factors. Addressing HPV in isolation, without recognising the influence of herpesviruses, chronic viral latency, and repeated STI exposure, often results in incomplete resolution and recurrence.
This integrated understanding explains why long-term HPV management increasingly emphasises immune restoration, treatment of co-infections, and stabilisation of the tissue environment alongside responsible screening and follow-up.
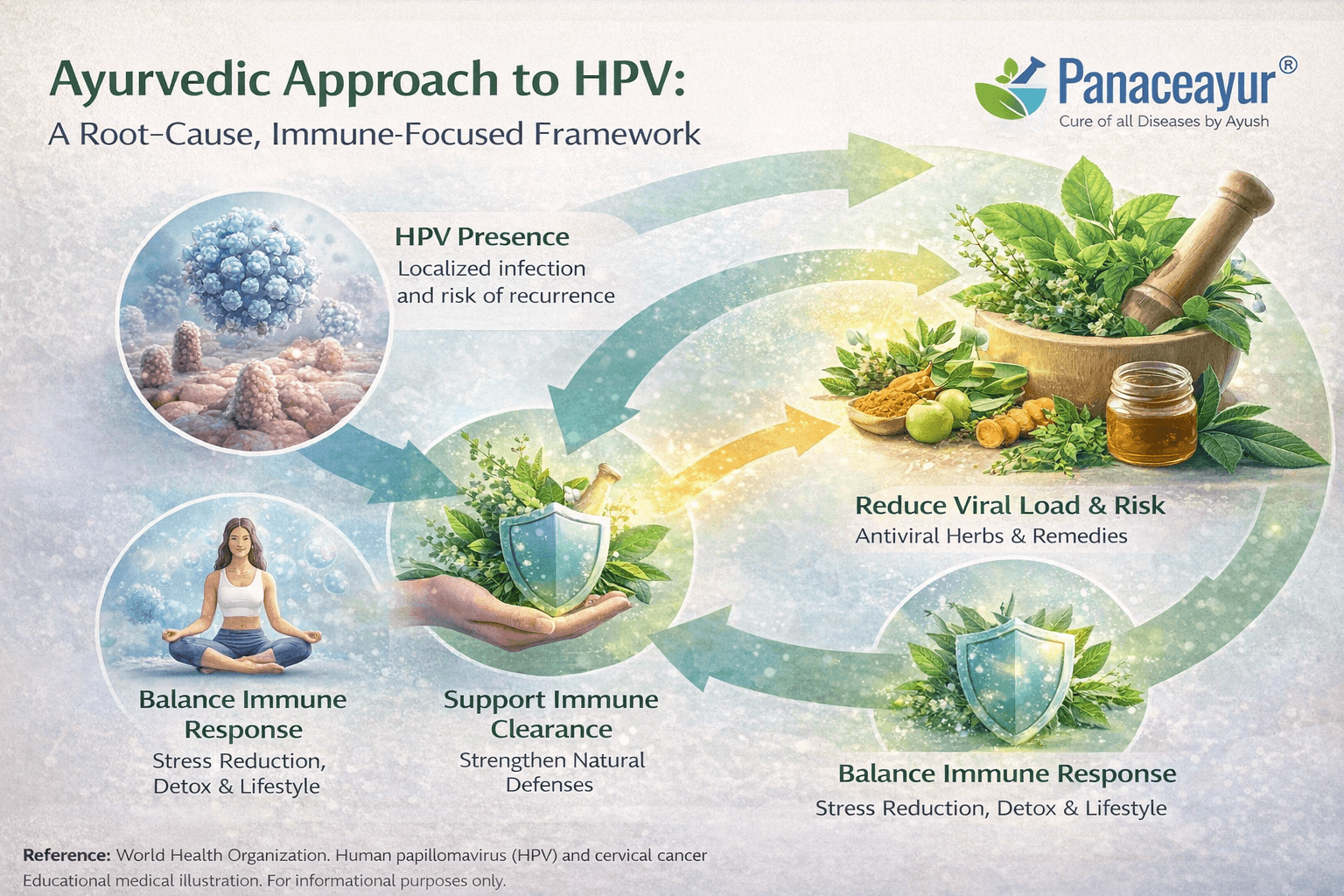
Why Treating HPV Requires More Than Wart Removal
Visible warts or abnormal tissue changes are often mistaken for the disease itself. In reality, both modern medicine and Ayurveda recognise that these visible findings are only surface manifestations of a deeper viral and immune process.
Procedures such as cauterisation, cryotherapy, laser ablation, or surgical excision remove affected tissue but do not directly address the presence of HPV within surrounding cells or deeper epithelial layers. As a result, removal of lesions does not confirm that the virus has been eliminated, that immune control has been restored, or that the risk of recurrence has been resolved.
This limitation explains why many individuals experience repeated episodes of warts or abnormal cellular changes despite undergoing multiple procedures over time. The virus may persist in a latent or low-level state, remaining undetected by routine screening while retaining the ability to reactivate under immune stress.
From a clinical perspective, wart removal is a local intervention, while HPV is a systemic and immune-mediated condition. Treating only the visible lesion without addressing immune resilience, tissue environment, and co-existing factors leaves the underlying cause untouched.
From an Ayurvedic standpoint, HPV is not limited to the skin or mucosa. It represents a deeper disturbance involving Rakta Dhatu, Mamsa Dhatu, immune intelligence, and chronic Krimi persistence. When treatment focuses only on removing visible growths, the underlying terrain that allowed the virus to establish itself remains unchanged. This is why warts often return even after repeated procedures.
Ayurveda recognises that viral clearance depends on restoring the body’s internal environment so that the virus can no longer survive or replicate. This process is not cosmetic or purely local. It is systemic, gradual, and immune-centred.
How Ayurveda Clears HPV at the Root Level
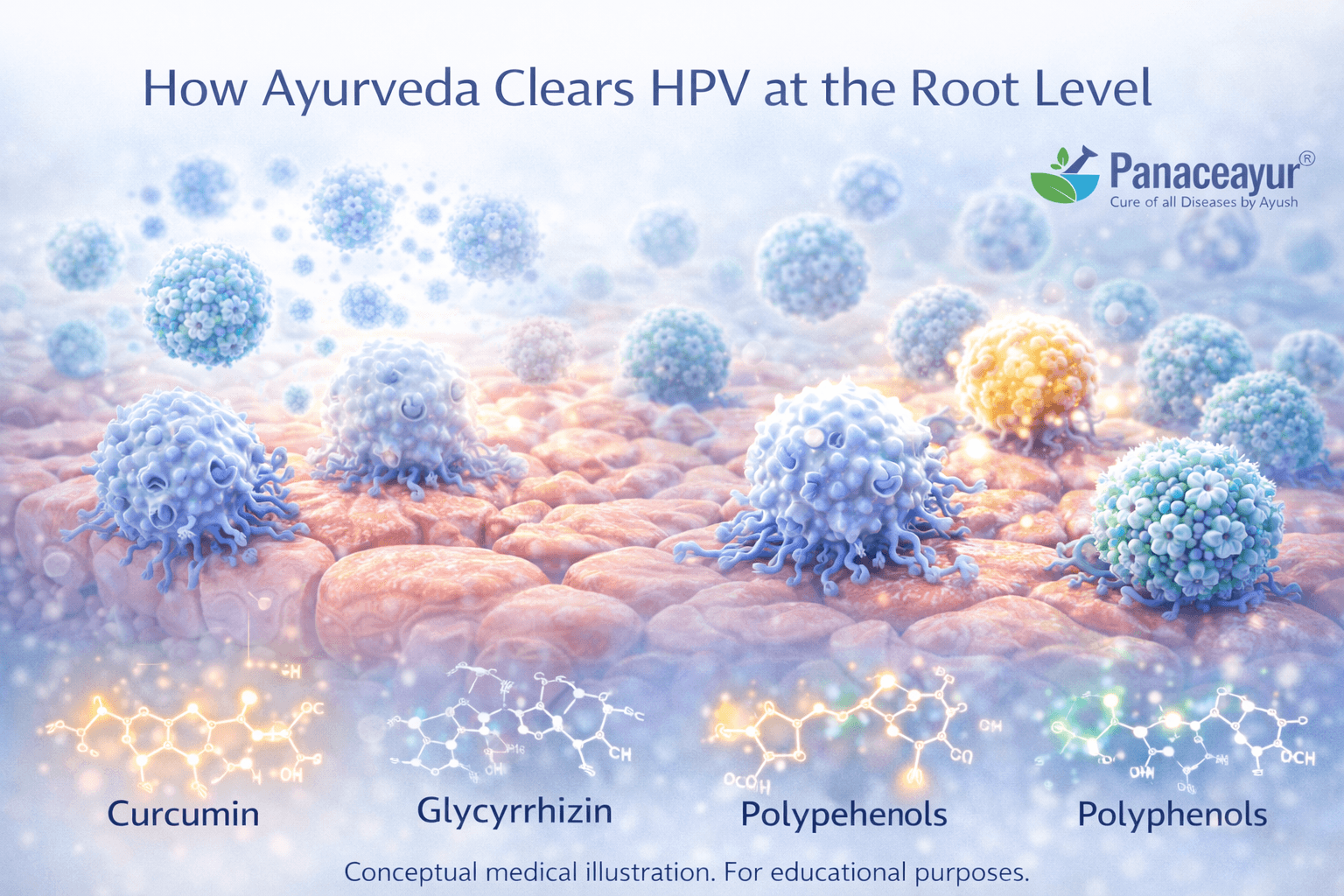
Ayurveda approaches HPV through correction of the internal terrain rather than attacking the virus directly. The goal is to make the body inhospitable to viral persistence.
The first focus is on Rakta Dhatu purification. Rakta Dhatu governs tissue vitality, immunity, and resistance to infection. When Rakta is vitiated, viral conditions become chronic and recurrent. Ayurvedic therapies and formulations aim to detoxify and stabilise Rakta so that abnormal tissue changes gradually regress.
The second focus is Krimi management. Classical Ayurvedic texts describe Krimi not only as worms but as persistent pathogenic entities that reside deep within tissues and evade superficial treatment. HPV fits this description closely. Ayurvedic formulations are designed to disrupt this deep-seated persistence rather than merely suppress symptoms.
The third pillar is restoration of Ojas. Ojas represents immune strength, tissue resilience, and recovery capacity. HPV persistence is consistently associated with depleted Ojas due to stress, chronic infections, poor digestion, and lifestyle strain. Rasayana therapy is used to rebuild Ojas so the immune system can recognise and clear virally infected cells over time.
Why Ayurvedic Treatment Prevents Recurrence
Unlike local procedures, Ayurveda does not aim for immediate removal of visible lesions alone. As internal correction progresses, warts may shrink, soften, dry, or resolve naturally. More importantly, the tendency for recurrence reduces because the viral environment is no longer supported.
Ayurvedic treatment also addresses Agni, the digestive and metabolic fire. Impaired Agni leads to Ama accumulation, which weakens immunity and sustains chronic disease. By correcting digestion and metabolism, Ayurveda removes the internal conditions that allow HPV to persist silently.
Lifestyle and dietary regulation further support viral clearance by reducing inflammation, stabilising hormones, and protecting mucosal tissues. These measures are not supportive add-ons but integral to long-term viral resolution.
Why This Approach Takes Time but Leads to Stability
Ayurvedic viral clearance is not instantaneous because it mirrors the body’s natural immune processes. Just as HPV establishes itself gradually, its elimination occurs in stages as immune strength returns and tissue health normalises.
This explains why Ayurveda emphasises patience, consistency, and personalised treatment rather than quick removal. The objective is not temporary suppression but long-term stability where the virus loses its ability to reactivate.
Clinical Relevance for Patients
Patients who undergo repeated wart removal without systemic correction often experience frustration, anxiety, and loss of confidence in treatment. Ayurveda offers a different therapeutic goal. Instead of asking how quickly a wart can be removed, it asks why the body allowed it to form and how to correct that internal state.
By focusing on Rakta Dhatu purification, Krimi resolution, Ojas restoration, Agni correction, and immune resilience, Ayurveda aims to clear HPV at its root and reduce the likelihood of recurrence, rather than chasing surface manifestations.
Diagnosis of HPV
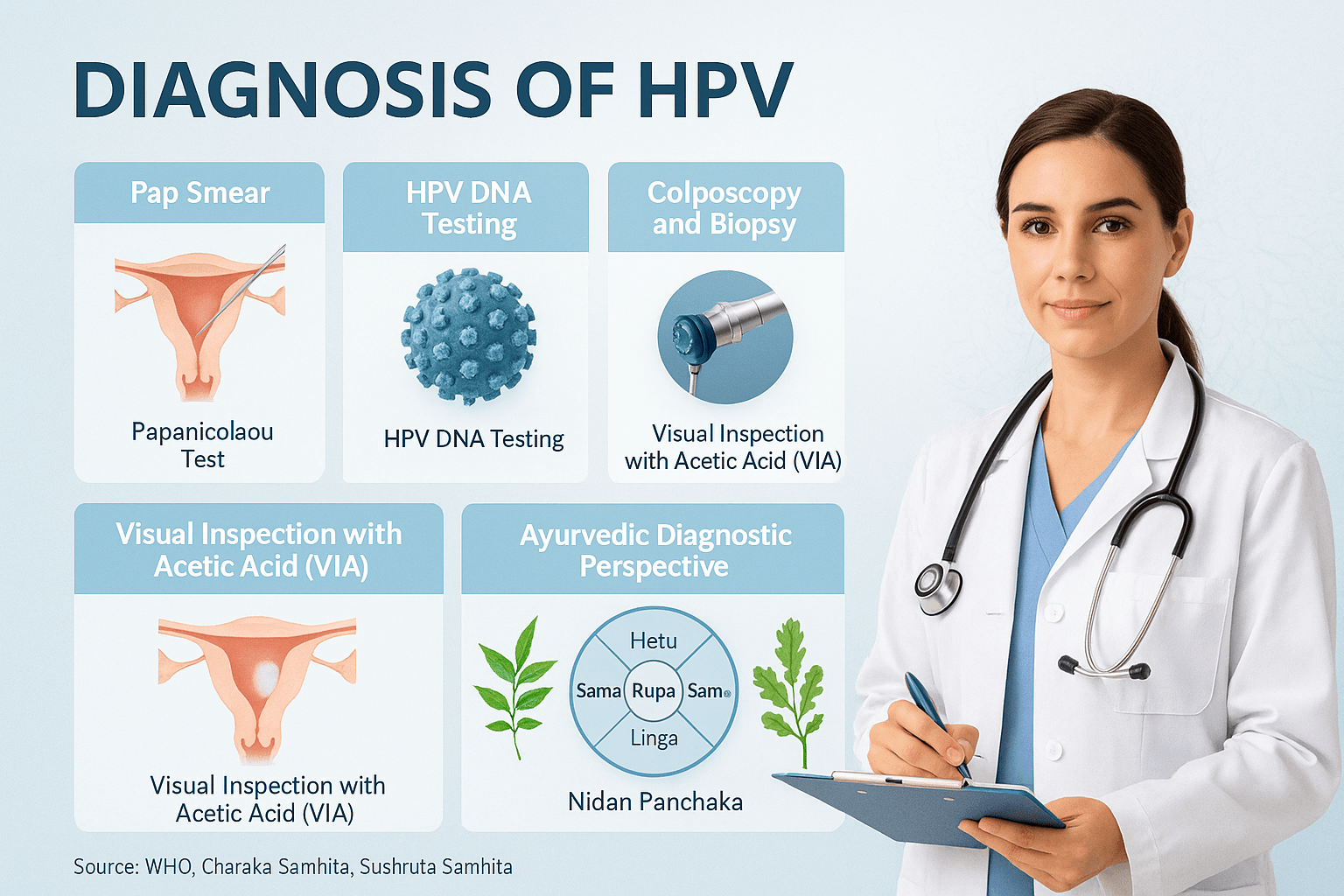
HPV is often symptomless, making diagnostic testing essential for early detection and prevention of complications such as cervical cancer. Diagnosis methods combine modern medical screening with supportive Ayurvedic diagnostic approaches.
Pap Smear (Papanicolaou Test)
- The Pap smear is the most common test for detecting cervical abnormalities caused by HPV.
- It involves collecting cervical cells and examining them under a microscope.
- Detects precancerous changes known as cervical intraepithelial neoplasia (CIN) before they develop into cancer [1].
HPV DNA Testing
- Modern HPV DNA tests detect the genetic material of high-risk HPV types such as HPV-16 and HPV-18.
- Can be performed alongside Pap smear (co-testing).
- Provides higher sensitivity in identifying women at risk for cervical cancer [2].
Colposcopy and Biopsy
- If abnormal cells are detected, a colposcopy is performed using a magnifying device to examine the cervix closely.
- A biopsy may be taken from suspicious areas for histopathological confirmation [3].
Visual Inspection with Acetic Acid (VIA)
- A low-cost alternative widely used in resource-limited settings.
- The cervix is swabbed with 3–5% acetic acid; HPV-infected areas turn white (acetowhite lesions).
- Offers immediate results but requires trained personnel [4].
Anal, Oral, and Penile HPV Testing
- Anal Pap tests may be used for high-risk groups, such as men who have sex with men (MSM) and HIV-positive individuals.
- Oral HPV testing and penile swabs can detect viral presence in non-cervical sites, though these are less routinely used [5].
Subclinical Infections
- Many HPV cases remain subclinical (invisible).
- Detection relies on DNA-based tests, colposcopy, or immunohistochemistry, as physical symptoms may not appear [6].
Ayurvedic Diagnostic Perspective (Nidan Panchaka)
Ayurveda approaches HPV diagnosis through Nidan Panchaka (fivefold diagnostic method):
- Hetu (causes): Unprotected sex, low immunity, improper lifestyle.
- Linga (symptoms): Warts, ulcers, Rakta Dushti (impure blood signs).
- Rupa (clinical picture): Localized or systemic spread depending on dosha involvement (Pitta-Kapha predominance).
- Samprapti (pathogenesis): Viral lodgment in Rakta and Shukra Dhatus, leading to Krimi manifestation.
- Upashaya (therapeutic test): Relief through Shodhana (detox), Rasayana (immunity), and Krimighna herbs (antiviral action) confirms diagnosis [7].
When to Get Tested
- Women aged 21–29: Pap smear every 3 years.
- Women aged 30–65: Pap smear + HPV DNA co-test every 5 years.
- High-risk individuals (HIV-positive, multiple partners, immunocompromised) should undergo more frequent screening [8].
When to get tested (UK & USA )
Screening intervals vary by country and guideline updates, but these are commonly referenced standards.
USA (USPSTF)
Ages 21 to 29: Pap test every 3 years.
Ages 30 to 65: Pap every 3 years, or high-risk HPV testing every 5 years, or co-testing every 5 years.
UK (NHS)
Invitations are generally every 5 years from age 25 to 64, with shorter intervals in some higher-risk cases or based on results.
This article keeps the focus on education. Readers should follow local clinical advice and the most recent personal screening recommendations.
Why HPV Persists in Some People Despite Normal Screening

Many individuals are reassured by normal screening results yet continue to experience HPV-related symptoms, recurrence of lesions, or ongoing anxiety. This situation is common and does not indicate a failure of screening. It reflects the biological behavior of HPV and the specific purpose and limitations of screening tools.
What Normal Screening Actually Indicates
Cervical screening tests such as Pap smears and HPV DNA testing are designed to detect abnormal cellular changes or the presence of high-risk HPV types in sampled tissue, most commonly the cervix. A normal result means that no significant abnormalities were identified at the time of testing and that high-risk HPV was not detected in that specific sample. It does not confirm that the virus has been fully eliminated from the body, nor does it rule out HPV presence in other anatomical sites.
HPV Latency and Undetectable Infection
HPV has the ability to remain latent within epithelial tissues. During latency, viral activity is minimal and may not produce detectable cellular changes. Viral DNA levels can fall below detection thresholds, resulting in normal screening reports. Latent HPV may reactivate years later if immune balance is disrupted, which explains delayed recurrence despite earlier normal tests.
Screening Is Site-Specific, Not Whole-Body Surveillance
Organised screening programs primarily assess cervical tissue. HPV can persist in other regions such as the vulva, vagina, anus, penis, oropharynx, and adjacent skin. A normal cervical screening result does not evaluate these sites, which explains why some individuals experience genital warts, anal symptoms, or oral HPV-related conditions despite consistently normal cervical tests.
Role of the Immune System in HPV Clearance
HPV clearance depends largely on effective immune surveillance rather than medical intervention. Factors such as chronic stress, inadequate sleep, nutritional deficiencies, smoking, alcohol excess, recurrent infections, or immune suppression due to illness or medication can weaken immune function. When immune resilience is reduced, HPV may persist silently without causing abnormal screening findings.
Local Inflammation and Tissue Vulnerability
Chronic local inflammation can create a tissue environment that supports HPV persistence even when dysplasia is not present. Recurrent genital infections, microbiome imbalance, hormonal fluctuations, or repeated mechanical irritation can increase tissue vulnerability. These factors may not trigger abnormal cytology but can influence long-term viral behavior.
HPV Type and Viral Load Influence Detection
High-risk HPV screening focuses on cancer-associated types and does not routinely include low-risk HPV types that cause warts. As a result, individuals may have visible wart disease while high-risk HPV tests remain negative. Additionally, very low viral loads may escape detection, particularly during early infection or latent phases.
Screening Intervals and Time Gaps
In countries such as the United Kingdom, Canada, and Australia, screening intervals may extend up to five years. In the United States, intervals vary depending on age and testing method. During these intervals, HPV status may change independently of scheduled testing, contributing to situations where symptoms arise despite recent normal results.
Clinical Implications for Patients
Normal screening results are reassuring but should not be interpreted as proof of complete viral clearance. Persistent symptoms, recurrent lesions, or unexplained genital or oral changes warrant clinical evaluation even when screening reports are normal. This explains why many individuals seek approaches that focus on immune resilience, tissue health, and long-term stability alongside routine screening and follow-up.
If you want, I can next integrate this section seamlessly with the Ayurvedic interpretation of immunity, Rakta Dhatu, and Ojas, or move forward with the section on HPV in men and missed diagnosis pathways.
Why modern medicine cannot fully “cure” HPV
Modern prevention and care are highly valuable, but they have limits.
Vaccines prevent many HPV infections, especially when given before exposure, but they do not treat existing infections. Screening detects risk early, and procedures remove abnormal tissue or warts, but none of these approaches guarantee complete eradication of an established infection in every person.
This is why many people search for “HPV cure” even after receiving good conventional care. The unmet need is long-term recurrence prevention, immune restoration, and tissue resilience.
Modern HPV prevention- what works and what it cannot do
HPV vaccination remains one of the strongest public health tools. It is routinely recommended for adolescents, with catch-up schedules and some shared decision options for adults depending on local policy.
Prevention is still incomplete because:
Some people are vaccinated after exposure, some miss screening, and some have immune conditions that increase persistence risk.
Ayurvedic Cure for HPV- The complete root-cause framework
Ayurvedic understanding of HPV (Charmakeela, Rakta Dushti, Krimi)
Ayurveda interprets HPV-like conditions through a combined lens of:
Krimi involvement (pathogenic invasion), Rakta Dushti (disturbed blood and tissue environment), and Dosha imbalance, commonly Pitta and Kapha patterns. In this view, persistence is more likely when digestion is weak (Agni impairment), metabolic toxins accumulate (Ama), and Ojas declines, reducing immune stability.
For this purpose, Ayurveda prescribes special Rasayana Avalehas (herbal confections) that combine deep detoxification, blood purification, and immunity-boosting actions.
The four pillars of Ayurvedic HPV care
Ayurvedic HPV care becomes effective when it follows a complete sequence rather than a single medicine.
1) Correct the terrain that supports persistence
This includes diet, digestion, stress reduction, sleep, and avoiding repeated irritation.
2) Purify blood and reproductive tissues
Ayurveda focuses on Rakta Dhatu and Shukra Dhatu support, because persistent genital conditions often reflect deeper tissue imbalance. Human Papillomavirus (HPV)-Symptoms
3) Strengthen immune surveillance and tissue repair
Rasayana therapy aims to rebuild Ojas and long-term resilience, not temporary suppression. Human Papillomavirus (HPV)-Symp…
4) Prevent recurrence with long-term Rasayana
HPV recurrence is a major fear. Ayurveda addresses recurrence by rebuilding resistance and stabilising dosha patterns over months.
| Topic | Modern approach | Ayurvedic approach |
| Main goal | Prevention, screening, lesion control | Root-cause correction, immune restoration, and long-term recurrence prevention |
| Virus clearance | Often occurs naturally in some individuals, not guaranteed by treatment | Supports immune-led viral clearance, Dhatu strengthening, and tissue resilience |
| Wart management | Physical removal methods, cauterization, topical cytotoxic or immune-modulating agents | Lekhana therapy, Krimighna herbs, Rasayana support, and gradual tissue healing |
| Personalisation | Guideline-based, largely uniform protocols | Individualized based on Prakriti, Dosha imbalance, Agni, and immune status |
| Monitoring | Pap smear, HPV DNA testing, clinical follow-up; treatment does not replace monitoring | Clinical symptom tracking, recurrence observation, immune response assessment; modern screening is encouraged alongside Ayurvedic care |
Bhallataka Rasayana Avaleha (central Rasayana medicine)
Bhallataka (Semecarpus anacardium), after proper purif sical Ayurvedic sources as a potent Rasayana used in stubborn conditions involving abnormal growth patterns and deep-seated disease tendencies. Your document correctly positions Bhallataka Rasayana Avaleha as the core Avaleha for HPV-type persistence and recurrence patterns
Bhallataka Rasayana Avaleha(Jam Based Medicine)-As per Ayurveda texts
- Mentioned in Charaka Samhita (Chikitsa Sthana – Rasayana Adhyaya) and further explained in Bhavaprakasha Nighantu, Bhallataka (Semecarpus anacardium) is described as a potent Rasayana for stubborn diseases like Granthi, Arbuda, Kushta, and Krimi [1,2].
- Its action is Lekhana (scraping), Krimighna (antiviral/antiparasitic), and Rasayana (rejuvenating).
- Classical commentators highlight that when Bhallataka is properly purified (Śodhana), it becomes a strong immunity enhancer and disease-destroyer.
Why This Avaleha for HPV?
- Shrinks warts and growths: Bhallataka’s scraping action helps in clearing Charmakeela (HPV warts).
- Destroys viral persistence: When fortified with Vyadhiharan Rasayan (a mineral Rasayana described in Rasashastra for chronic, incurable diseases), it directly targets hidden viral reservoirs [3].
- Purifies blood and tissues: Herbs like Guduchi, Neem, Triphala, Turmeric, and Bhumyamalaki clean the blood and prevent malignant transformation [4–6].
- Strengthens immunity (Ojas): Swarna Bhasma (Gold), Abhraka Bhasma (Mica), and Yashada Bhasma (Zinc) rebuild cellular immunity and protect mucosal tissue [7].
Key Herbs and Their Role
- Bhallataka (Semecarpus anacardium): Main ingredient; has lekhana (scraping) action to remove warts and krimighna (antiviral) effect. Used in Granthi, Arbuda, Kushta [1].
- Triphala (Amalaki, Haritaki, Bibhitaki): Detoxifies and rejuvenates tissues. Prevents abnormal cell growth, purifies Rakta Dhatu [2].
- Guduchi (Tinospora cordifolia): Enhances disease resistance (Vyadhi-kshamatva). Modern research shows strong immunomodulatory action [3].
- Neem (Azadirachta indica): Powerful blood purifier; induces apoptosis in HPV-infected cervical cells. Traditionally used in Krimi and Kushta [4].
- Turmeric (Curcuma longa): Curcumin suppresses HPV E6/E7 oncogenes, prevents malignant transformation [5].
- Vidanga (Embelia ribes): Krimighna (destroys hidden viral/microbial factors). Helps in cleansing the gut and immune system [6].
- Bhumyamalaki (Phyllanthus niruri): Famous antiviral; inhibits viral replication and supports the liver [7].
- Shatavari (Asparagus racemosus): Rasayana for the reproductive system, balances hormones, and supports cervical tissue healing [8].
- Manjishtha (Rubia cordifolia): Potent Rakta-shodhaka (blood purifier), reduces inflammation and discoloration [9].
- Ashwagandha (Withania somnifera): Adaptogen and Ojas booster; reduces stress-induced immune suppression [10].
Key Minerals and Their Role
- Swarna Bhasma (Gold): Supreme Rasayana; enhances immunity, improves T-cell and macrophage response, prevents recurrence [11].
- Rajata Bhasma (Silver): Cooling and antiviral; soothes inflamed genital and oral mucosa [12].
- Yashada Bhasma (Zinc): Strong antiviral and skin-healing; modern medicine also uses zinc for wart regression [13].
- Tamra Bhasma (Copper): Scraping action on abnormal growths; improves liver function and immunity [14].
- Abhraka Bhasma (Mica): Strengthens all Dhatus (tissues), rejuvenates Majja (bone marrow), prevents recurrence [15].
- Lauh Bhasma (Iron): Corrects Rakta-duṣṭi, builds healthy blood, supports immunity [16].
- Pravala Pishti (Coral): Cooling, anti-Pitta; heals ulcers, reduces burning sensations [17].
- Mukta Shukti (Pearl/Oyster Shell): Balances acid–alkali, calms inflamed tissues, promotes healing [18].
- Godanti Bhasma (Gypsum): Cooling, reduces fever-like inflammatory states, stabilizes Rakta [19].
- Sphatika Bhasma (Alum): Antiviral, antiseptic, and wart-shrinking [20].
- Hiraka Bhasma (Diamond): Rare Rasayana; promotes deep tissue rejuvenation and cellular repair [21].
- Swarna Makshik Bhasma (Chalcopyrite): Improves Pitta–Kapha balance, strengthens digestion and immunity [22].
- Trivanga Bhasma (Lead–Tin–Zinc): Useful for genito-urinary health; improves tissue resistance [23].
- Nag Bhasma (Lead): Cautiously used after purification; effective in Kapha disorders with warts [24].
- Gandhaka Rasayan (Sulphur compound): Antiviral, Rasayana for skin and immunity [25].
- Vyadhiharan Rasayan: Kupipakwa mineral preparation (mercury–sulphur–arsenical base) described for chronic, stubborn, and “incurable” diseases. Strong antiviral and disease-eliminating effect [26].
Preparation (Under-Supervision of Qualified Doctor) Strictly
- Purification: Bhallataka kernels purified in buttermilk/cow’s urine for 7 days [2].
- Decoction: Bhallataka + Triphala decoction prepared.
- Avaleha Base: Decoction cooked with jaggery until jam-like; cooled, then mixed with ghee and honey.
- Fortification: Herbal powders and mineral Bhasmas are added in prescribed micro-doses.
- Final Step: Vyadhiharan Rasayan is added in tiny quantity to complete the fortified Avaleha.
How to Take It (Dosage)
- Dose: ½–1 teaspoon (≈3–6 g) once or twice daily.
- With (Anupāna): Warm milk (Rasayana effect), honey (wart regression), Guduchi decoction (blood purification).
- Course: 3–6 months under supervision.
- Pathya (Diet): Light, sattvic food; avoid spicy, sour, fermented foods; include amla, turmeric, leafy vegetables.
Critical Patient Safety Warning About Avaleha Medicines

Do Not Buy Bhallataka Rasayana Avaleha From the Open Market
Patients must clearly understand that purchasing Avaleha or Rasayana medicines from the open market is unsafe and ineffective in chronic viral conditions such as HPV. These conditions require precise formulation, purification, and medical supervision. Market-available products do not meet these requirements.
Even when a product label claims to be “classical,” “authentic,” or “as per Ayurvedic texts,” it often fails to deliver therapeutic benefit and may carry safety risks.
Why Market-Bought Avaleha Will Not Work
Market-available Bhallataka Rasayana Avaleha commonly fails due to multiple hidden and critical factors.
One of the most serious issues is incorrect or incomplete Shodhana of Bhallataka. Classical Ayurvedic texts clearly state that Bhallataka must undergo mandatory purification before use. Improperly purified Bhallataka can be ineffective or harmful.
Another major limitation is the absence or incorrect proportion of Vyadhiharan Rasayan. This component is essential for chronic, deep-seated, and recurrent conditions. Generic market formulations often omit it entirely or include it in sub-therapeutic amounts.
Market products are not customised. They are prepared as one-size-fits-all formulas without considering the patient’s Prakriti, Dosha imbalance, disease stage, recurrence pattern, digestive strength, or immune status. Chronic viral conditions do not respond to generic formulations.
Raw material quality is another concern. Many commercial preparations use low-grade, aged, or adulterated herbs that lack the potency required for Rasayana action.
Processing errors are also common. Incorrect cooking temperature, improper duration, or mechanical preparation methods alter the pharmacological behavior of the Avaleha and reduce its Rasayana effect.
Anupana selection is usually ignored. In Ayurveda, the vehicle used to administer a medicine determines its tissue penetration and action. Market products cannot account for this because they are sold without clinical evaluation.
Associated disorders are not assessed. Conditions such as Pitta aggravation, weak digestion, Ama accumulation, immune depletion, or co-existing infections strongly influence outcomes. Market products are dispensed without evaluating these factors.
There is no monitoring or follow-up. Dose adjustments, tolerance assessment, and response tracking are essential in Rasayana therapy. Market products offer none of this.
Because of these reasons, patients often conclude that Ayurveda does not work, when in reality the medicine was never correctly prepared, prescribed, or supervised.
Absolute Rule: Never Prepare or Consume This Medicine Without Medical Supervision
Bhallataka Rasayana Avaleha and mineral-based Rasayanas must never be prepared or consumed without the supervision of a qualified Ayurvedic physician. This is not optional.
Bhallataka is a highly potent substance. Improper purification, incorrect dosage, or unsuitable patient selection can cause irritation, burning sensations, digestive distress, or worsening of symptoms.
Mineral Rasayanas require precise pharmaceutical processing and micro-dosing. Even small deviations can alter safety and efficacy.
Patient-specific factors such as digestive capacity, tissue strength, heat tolerance, metabolic state, and immune condition must be assessed before initiation. These factors cannot be determined without clinical evaluation.
Incorrect use can aggravate disease, create new complications, or suppress symptoms while the underlying pathology continues unchecked.
Ayurveda is a structured medical science. It is not a home-remedy system, and complex viral conditions like HPV must never be self-treated or managed with over-the-counter Rasayana products.
Integrative Care Reminder
Ayurvedic treatment does not replace medical screening or diagnostic evaluation. Chronic viral conditions such as HPV require responsible monitoring to detect cellular changes early and to guide timely medical decisions.
Patients must continue with recommended Pap smears and HPV DNA testing as advised by national screening programs. When indicated, colposcopy or biopsy should be undertaken without delay. Regular follow-up with qualified healthcare providers remains essential, even when symptoms improve or lesions resolve.
Ayurveda works best as a root-cause-focused, immune-supportive medical system that complements modern diagnostics. Its role is to strengthen immunity, stabilise tissue health, and reduce viral persistence while screening ensures early detection of risk. Used together, both systems provide safer, more comprehensive care than either approach used in isolation.
FAQs
Can HPV be cured permanently?
Some HPV infections clear naturally, but persistence can occur. Modern care prevents and detects risk, while Ayurveda aims to support immune-led clearance and reduce recurrence. Screening and follow-up remain essential
Does HPV always lead to cancer?
No. Many HPV infections clear naturally. Cancer risk is mainly linked to persistent high-risk HPV types and lack of screening follow-up.
Why does HPV come back after treatment?
Recurrence can happen if the virus persists silently, immunity is weakened, or reinfection occurs. This is why long-term immune support and preventive habits matter.
Can Ayurveda help clear HPV?
Yes. Ayurveda aims for complete cure rather than symptom control. Bhallataka Rasayana Avaleha helps by purifying the blood, boosting immunity, and removing the virus from its root.
Can I take Ayurvedic treatment with the HPV vaccine or medical procedures?
Ayurvedic support can be complementary, but decisions should be made with a clinician, especially if there are abnormal results or procedures planned.
- What is Bhallataka Rasayana Avaleha?
It is a classical Ayurvedic herbal jam prepared from purified Bhallataka, Triphala, ghee, honey, and jaggery. When fortified with Vyadhiharan Rasayan and mineral Bhasmas, it becomes a powerful medicine for HPV. - How does this Avaleha work against HPV?
- Removes warts with Bhallataka’s scraping action
- Destroys hidden virus through Vyadhiharan Rasayan
- Purifies blood with Guduchi, Neem, and Triphala
- Boosts immunity with Swarna Bhasma and Abhraka Bhasma
- Prevents recurrence as a Vyadhi-hara Rasayana
- Is Bhallataka Rasayana Avaleha safe?
Yes, when prescribed by an Ayurvedic doctor. Bhallataka is purified before use and minerals are processed safely. Raw Bhallataka should never be taken without proper purification. - How long does it take to see results?
Most patients see improvement within three to six months of regular use. Chronic or severe HPV cases may need a longer course. - Can this Avaleha prevent cervical cancer caused by HPV?
Yes. Turmeric and Neem have been shown to suppress HPV-related changes, while Rasayana therapy protects tissues from precancerous or cancerous transformation. - What diet should I follow during treatment?
Avoid spicy, sour, and fermented foods. Favor fresh vegetables, green leafy vegetables, Amla, and turmeric. Good sexual hygiene is important to prevent reinfection. - Can men also use Bhallataka Rasayana Avaleha?
Yes. The formulation works for both men and women with HPV, whether it affects the genital, anal, or throat region. - Can this medicine be taken with HPV vaccines or modern treatments?
Yes. It can be combined with vaccination or medical procedures. Ayurveda complements modern approaches by strengthening immunity and preventing recurrence. - Who should avoid this Avaleha?
Pregnant women, those with ulcers or strong Pitta imbalance, people allergic to the cashew family (Anacardiaceae), and anyone using it without medical supervision.
References
- Charaka Samhita. (2024). Rasayana chapter – Ayurvedic rejuvenation therapy.
https://www.carakasamhitaonline.com/index.php/Rasayana_Adhyaya - Charaka Samhita. (2024). Chikitsa Sthana (treatment section).
https://www.carakasamhitaonline.com/index.php/Chikitsa_Sthana - Ministry of AYUSH. (2006). The Ayurvedic Pharmacopoeia of India, Part-I, Vol. 2 – Bhallataka monograph.
https://www.ayurveda.hu/api/API-Vol-2.pdf - Ministry of AYUSH. (2016). The Ayurvedic Pharmacopoeia of India, Part-I, Vol. 6 – monographs.
https://dravyagunatvpm.files.wordpress.com/2019/10/api-part-1-vol-6-monographs.pdf - Savrikar, S. S., & Ravishankar, B. (2010). Bhaishajya Kalpanaa – The Ayurvedic pharmaceutics (Avaleha concept). Ayu, 31(1), 74–80.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3025621/ - Sharma, S. (Ed.). (1982). Rasatarangini – Classical Rasashastra text (24th Taranga: purification).
https://www.ijooar.com/PDFUpload/V7_I2_A128.pdf - Ayurpharm Review. (2014). Rasatarangini overview (Shodhana methods).
https://www.ayurpharm.com/imagesuser/ayurpharm351.pdf - Sharma, M. B., Zala, U. V., & Paneliya, A. M. (2023). Purification of Bhallataka: A pharmaceutical study. IJISRT, 8(3).
https://ijisrt.com/assets/upload/files/IJISRT23MAR2012.pdf - Deshpande, P. R. (2016). Vyadhiharana Rasayan: Kupipakwa formulation, dose and clinical use. AyurPub, 1(3), 108–113.
https://ayurpub.com/wp-content/uploads/2016/08/vyadiharana-rasa.-prakash.pdf - IAMJ Resource. (n.d.). Kupipakwa Rasayana overview (including Vyadhiharana Rasa).
https://iamj.in/RASASHASTRA_BHAISHAJYA/images/upload/kupi_pakwa_Rasayana.pdf - Joglekar, A. A., et al. (2024). Ayurvedic health-care approaches in cancer management. International Journal of Ayurveda Research.
https://journals.lww.com/ijar/fulltext/2024/05030/ayurvedic_health_care_arenas_in_the_management_of.5.aspx - Kantak, S., et al. (2023). Abhraka (mica) bhasma shows nano features. Journal of Ayurveda and Integrative Medicine.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7527821/ - Chaudhari, S. Y., et al. (2016). Safety of Tamra Bhasma in acute and sub-chronic use. Journal of Ayurveda and Integrative Medicine, 7(1), 23–29.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4910297/ - Chaudhari, S. Y., et al. (2013). Review of research on Tamra Bhasma. AYU, 34(3), 290–293.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3764875/ - Saini, S., Sharma, P., Bansal, R., & Kumar, P. (2023). Swarna Bhasma increases T-cell responses in vitro. Frontiers in Immunology, 14, 1138246.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10123016/ - Bhaskaran, J. K., et al. (2021). Immunomodulatory effect of Swarna-prashana in infants. Ancient Science of Life, 40(4), 242–252.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8078605/ - Al-Gurairi, F. T., et al. (2002). Oral zinc sulfate for resistant viral warts: clinical trial. Clinical and Experimental Dermatology, 27(8), 651–654.
https://pubmed.ncbi.nlm.nih.gov/11952542/ - Wang, C.-C., et al. (2025). Oral zinc sulfate reduces wart recurrence: meta-analysis. PLOS ONE, 20(5), e0323051.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0323051 - ClinicalTrials.gov. (Ongoing). Zinc sulfate for HPV clearance (NCT03404310).
https://clinicaltrials.gov/study/NCT03404310 - Maher, D. M., et al. (2011). Curcumin suppresses HPV-16 oncogenes and restores tumor suppressor pathways. International Journal of Oncology, 39(1), 111–118.
https://pubmed.ncbi.nlm.nih.gov/21061268/ - Zhao, X., et al. (2024). Curcumin directly targets HPV E6 in cervical cells. Phytotherapy Research, 38(10), 4967–4981.
https://pubmed.ncbi.nlm.nih.gov/37157900/ - Kumar, S., et al. (2022). Neem bark extract induces apoptosis in cervical cancer cells. BMC Complementary Medicine and Therapies, 22, 239.
https://bmccomplementmedtherapies.biomedcentral.com/articles/10.1186/s12906-022-03718-7 - Batra, N., et al. (2022). Neem in oncology: review of therapeutic potential. Integrative Cancer Therapies, 21, 1–17.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9358515/ - Yates, C. R., et al. (2022). Immunomodulatory review of Tinospora cordifolia. Planta Medica, 88(17), 1508–1523.
https://pubmed.ncbi.nlm.nih.gov/33480818/ - Singh, J., et al. (2024). Giloy (Tinospora) immunomodulatory properties: scoping review. Journal of Food Science and Technology.
https://pmc.ncbi.nlm.nih.gov/articles/PMC11699423/ - Lee, N. Y., et al. (2016). Pharmacological potential of Phyllanthus niruri. Genetics and Molecular Research, 15(2).
https://europepmc.org/article/med/27283048 - Venkateswaran, P. S., et al. (1987). Phyllanthus niruri inhibits hepatitis B virus polymerase. The Lancet, 330(8553), 764–766.
https://europepmc.org/article/pmc/pmc304186 - Tan, W.-C., et al. (2013). Antiviral activity of Phyllanthus species. Evidence-Based Complementary and Alternative Medicine, 2013.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3856372/ - Namburi, U. R. S., & Sreelatha, T. K. (2011). Ayurvedic management of warts (Charmakeela): review. Ayu, 32(3), 372–375.
https://journals.lww.com/aayu/fulltext/2011/32010/a_review_on_management_of_warts_in_ayurveda.19.aspx - JAIMS Review Board. (2020). Comprehensive review of Bhallataka in Ayurveda. Journal of Ayurveda and Integrated Medical Sciences.
https://jaims.in/jaims/article/download/847/864/ - Easy Ayurveda. (2015). Charaka Chikitsa 1.1 – Abhaya-Amalakiya Rasayana (chapter guide).
https://www.easyayurveda.com/2015/07/02/charaka-chikitsa-1-1-abhaya-amalakeeya-rasayana/ - Easy Ayurveda. (2024). Charaka Samhita – All chapter reference links.
https://www.easyayurveda.com/2024/04/25/charaka-samhita-all-chapters-reference-links/ - Kantak, S., et al. (2020). Abhraka bhasma characterization: PubMed record. Journal of Ayurveda and Integrative Medicine.
https://pubmed.ncbi.nlm.nih.gov/30826258/ - Rathi, B., et al. (2023). Pravala Bhasma formulations in Bhaishajya Ratnavali. Journal of Integrative Standard Medicine, 11(2).
https://journals.lww.com/jism/fulltext/2023/11020/pravala_bhasma_formulations_in_bhaishajya.4.aspx - Khanorkar, T. V., et al. (2022). Avaleha preparation methods – literature review. Ayuscript, 1(3).
https://ayuscript.com/submission/ad_54433.pdf