- What Is the HPV Vaccine?
- Types of HPV Vaccines
- How the Vaccine Works
- Who Is the Vaccine Recommended For?
- Why Gardasil 9 Is Considered Superior
- Effectiveness of the HPV Vaccine
- Evidence from Global Trials
- Protection Against Cervical Cancer and Genital Warts
- Lesser-Known Limitations
- Safety and Side Effects of the HPV Vaccine
- Common Reactions
- Rare Adverse Reports
- Ongoing Controversies and Patient Hesitancy
- Global Consensus
- The Ayurvedic Perspective
- HPV Explained Through Krimi Theory and Dhatu Imbalance
- Why Ayurveda Believes True Eradication Is Possible
- Prevention Versus Cure: The Contrast
- Ayurvedic Alternatives to HPV Vaccination
- Key Herbs for Viral Defense
- Mineral Formulations
- Lifestyle and Immunity-Building Guidelines
- Panchakarma (Optional Preventive Detox)
- Linking Prevention to Cure
- FAQs
- References
Human papillomavirus (HPV) is one of the most widespread viral infections worldwide, affecting millions of men and women across all age groups [1]. While many infections remain silent, certain strains are responsible for serious health complications, including cervical cancer, genital warts, and an increased risk of throat and anal cancers [2]. This makes HPV not just an individual health issue, but a global public health challenge.
To counter this burden, vaccines were introduced as a preventive measure. They aim to protect against high-risk HPV strains, especially when given before sexual exposure [3]. Today, HPV vaccines form a central part of public health campaigns, and have shown measurable success in reducing cervical cancer incidence in many countries [4].
Yet, vaccination has its limitations. It does not work against every HPV strain [5], it cannot cure existing infections [6], and its long-term safety has been debated in some circles [7]. For those who are already infected, the vaccine offers little benefit [8].
This is where Ayurveda provides a different perspective. Instead of focusing only on prevention, Ayurvedic medicine addresses the root imbalance in the body that allows the virus to persist [9]. Through herbs, minerals, and Rasayana therapies, Ayurveda offers a potential path not just to management, but to complete viral eradication [10].
To explore the full details of how HPV can be cured through Ayurveda, read our main guide here: [HPV: Causes, Symptoms, Diagnosis, and Ayurvedic Cure].
What Is the HPV Vaccine?
The human papillomavirus (HPV) vaccine is a biomedical innovation designed to prevent infection from specific strains of HPV, the virus responsible for more than 90% of cervical cancers and a significant proportion of anal, penile, throat, and vulvar cancers worldwide [1]. Because HPV spreads primarily through sexual contact and often shows no early symptoms, the vaccine represents one of the most effective cancer-prevention tools in modern medicine [2].
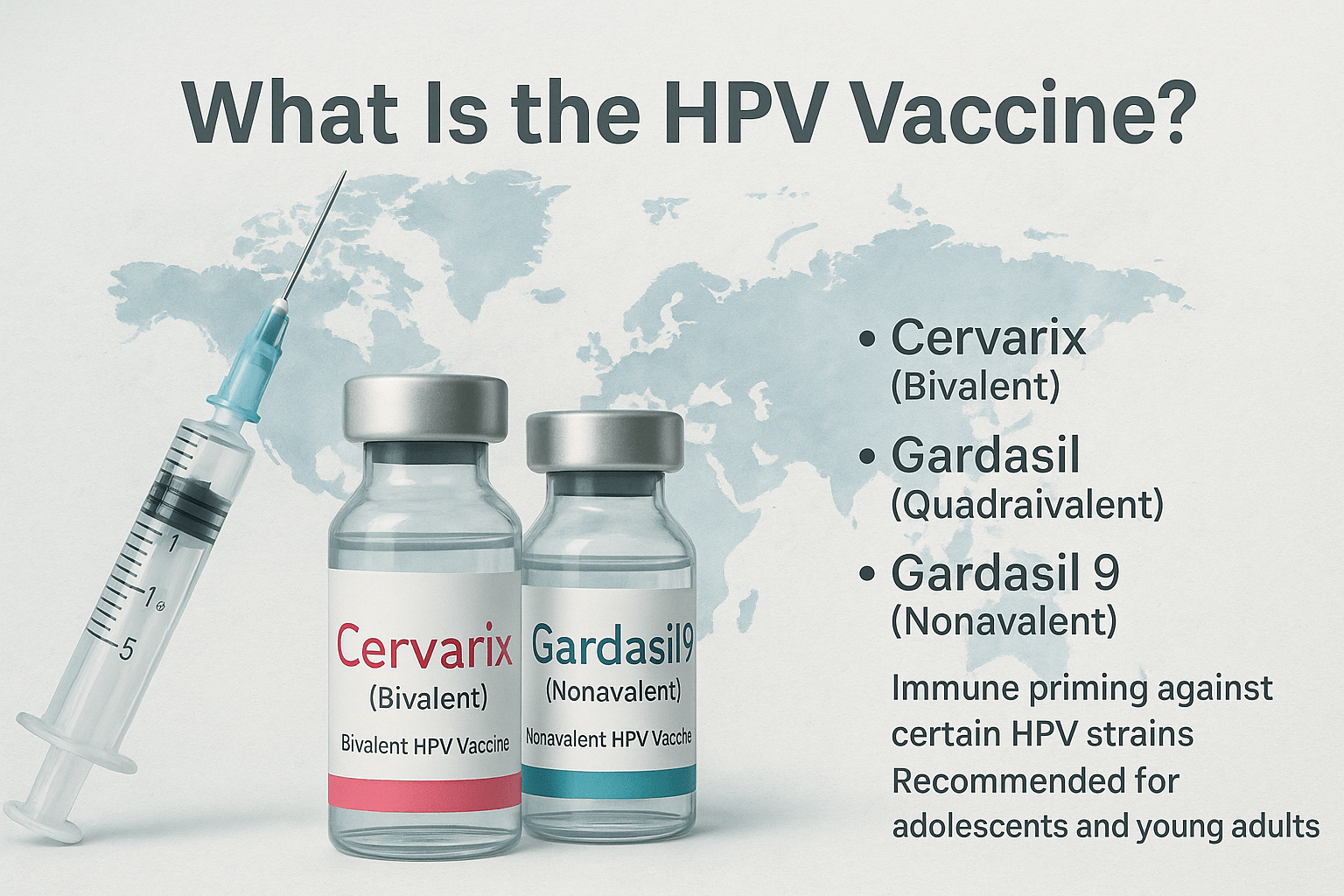
Types of HPV Vaccines
There are three major HPV vaccines licensed globally, each with varying coverage:
- Cervarix (Bivalent HPV Vaccine):
Targets only two high-risk strains, HPV-16 and HPV-18, which together account for approximately 70% of cervical cancer cases [3]. While effective, its limited coverage makes it less comprehensive than later versions. - Gardasil (Quadrivalent HPV Vaccine):
Protects against four HPV types: 6, 11, 16, and 18. In addition to preventing cervical cancer, it also covers the two strains (HPV-6 and HPV-11) responsible for over 90% of genital warts [4]. - Gardasil 9 (Nonavalent HPV Vaccine):
The most advanced formulation to date, it covers nine HPV strains—6, 11, 16, 18, 31, 33, 45, 52, and 58—providing protection against nearly 90% of cervical, vulvar, vaginal, anal, and oropharyngeal cancers linked to HPV [5]. Its broader strain coverage and dual benefit of cancer plus wart prevention make it clinically superior compared to Cervarix and earlier Gardasil versions.
How the Vaccine Works
All HPV vaccines use virus-like particles (VLPs) created from the L1 protein of HPV’s outer shell. These particles look like HPV to the immune system but carry no genetic material, so they cannot cause infection [6]. Once injected, VLPs stimulate the production of neutralizing antibodies, creating long-lasting immune memory. Studies show that antibody levels generated by the HPV vaccine are significantly higher than those developed from natural infection, which explains its strong preventive effect [7].
Who Is the Vaccine Recommended For?
Leading health authorities such as the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) recommend HPV vaccination as part of routine immunization programs:
- Adolescents (both boys and girls), ideally at 9–14 years of age, when the immune system response is strongest and before sexual exposure [8].
- Catch-up vaccination for individuals aged 15–26 years if they were not immunized earlier [9].
- Adults up to age 45 may also receive the vaccine, though the protective effect is lower if prior HPV exposure has occurred [10].
Why Gardasil 9 Is Considered Superior
- Broader strain protection (90% of cancer-causing HPV types) compared to Cervarix (70%) and Gardasil (approx. 70%).
- Dual coverage against both cancer-causing and wart-causing strains.
- Longer-lasting immunity, with studies suggesting robust antibody persistence for over a decade without boosters [11].
- Approved in more countries globally than its predecessors, reflecting its wide clinical acceptance.
While the HPV vaccine is one of modern medicine’s most powerful preventive tools, its role is limited to prevention, not cure. Individuals who are already infected with HPV require additional strategies. This is where Ayurveda, with its Rasayana therapies, immune-modulating herbs, and mineral preparations, offers a complementary path focused on root-cause eradication and long-term viral clearance.
Effectiveness of the HPV Vaccine
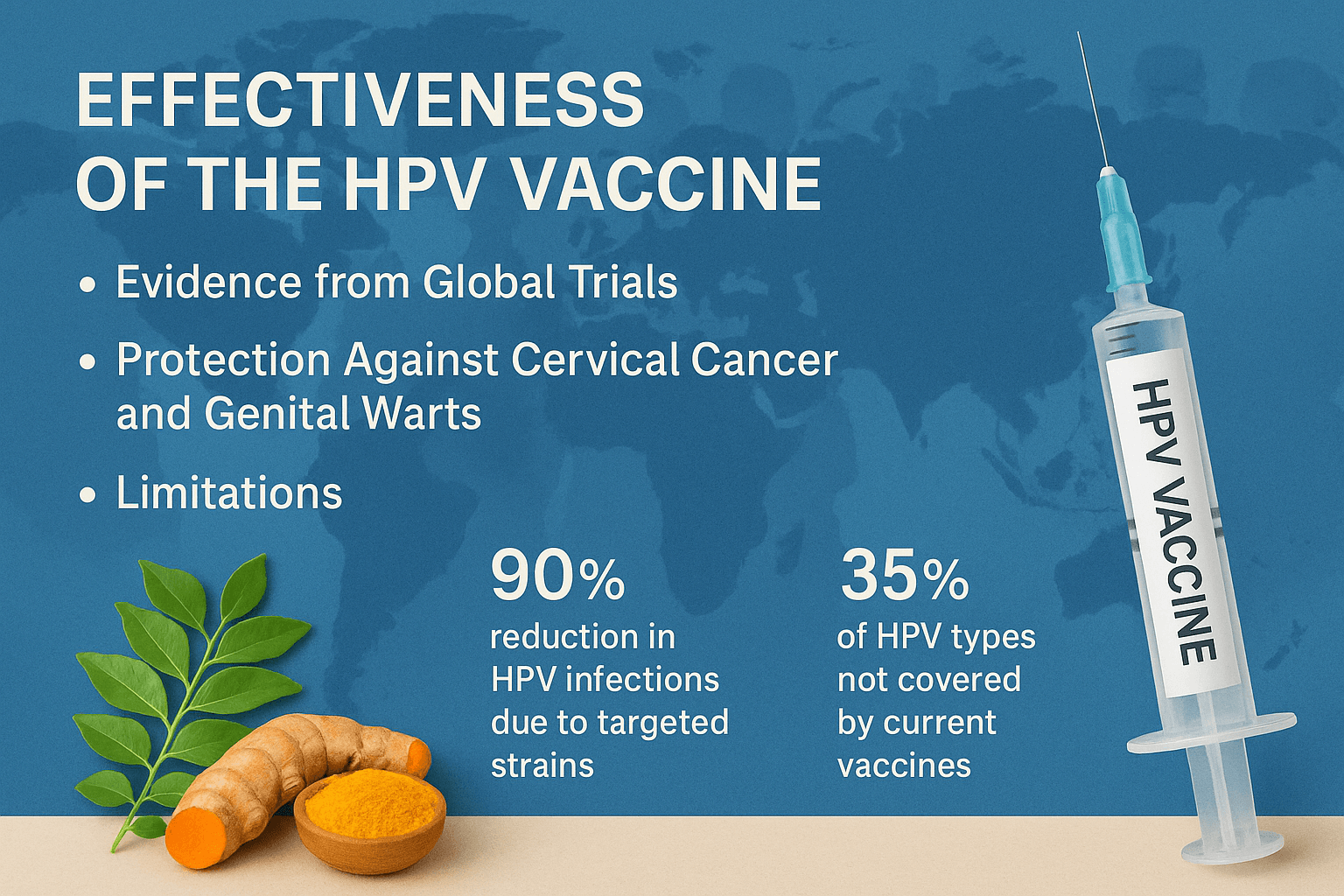
The HPV vaccine is one of the most successful public health interventions in reducing virus-related cancers and genital warts. However, its effectiveness depends on age, timing, strain coverage, and regional vaccination strategies, and several lesser-known details highlight both its strengths and limitations [1].
Evidence from Global Trials
Large international trials have consistently shown that HPV vaccines reduce infection and disease caused by the strains they target. Key findings include:
- Near 100% efficacy in preventing cervical precancers (CIN 2 and CIN 3) caused by HPV-16 and 18 when the vaccine is given before viral exposure [2].
- In long-term follow-up studies, antibody levels remain stable for at least 10–12 years, showing no evidence of waning immunity—contrary to concerns about booster necessity [3].
- Herd immunity effects have been observed: even unvaccinated males in Australia and Sweden showed a dramatic decline in genital warts once female vaccination coverage exceeded 50% [4].
- Cross-protection: Cervarix, though limited to HPV-16 and 18, has shown partial protection against related oncogenic strains such as HPV-31 and HPV-45, which may explain why it still reduced cancer risk beyond its primary targets [5].
Protection Against Cervical Cancer and Genital Warts
- HPV-16 and 18 account for 70% of cervical cancers, but when combined with HPV-31, 33, 45, 52, and 58, the coverage rises to nearly 90%. Gardasil 9 is unique in offering this broad protection [6].
- Genital warts dropped by over 95% in young women and around 90% in young men within a decade of Gardasil introduction in Australia—a decline much faster than predicted [7].
- In vaccinated populations, rates of oral HPV infections linked to throat cancers also decreased significantly, hinting at broader cancer-prevention benefits that were not initially expected [8].
- A lesser-known fact: Vaccination has also reduced cases of recurrent respiratory papillomatosis (a rare but serious childhood throat disease caused by HPV-6 and 11), since mothers vaccinated against these strains are less likely to transmit them during childbirth [9].
Lesser-Known Limitations
While the vaccine is highly effective, there are realities that many patients are unaware of:
- No therapeutic benefit: Vaccination after HPV infection does not accelerate viral clearance or reduce disease progression [10].
- Unequal strain distribution: In Asia and parts of Africa, non-16/18 strains like HPV-52 and HPV-58 are more common, reducing the impact of Cervarix and older Gardasil versions compared to Gardasil 9 [11].
- Incomplete genital wart coverage: Gardasil 9 prevents warts caused by HPV-6 and 11, but other rare strains (e.g., HPV-40, 42, 54) can still cause lesions [12].
- Male effectiveness gap: While women benefit most in terms of cancer protection, male cancers (penile, anal, throat) have more complex viral associations, making overall effectiveness slightly lower in men [13].
- Need for high coverage: Herd immunity requires vaccination rates above 70%. Countries with patchy implementation see less dramatic declines, meaning real-world outcomes vary widely [14].
These findings confirm the HPV vaccine as a powerful preventive tool, but one with geographical, biological, and practical limitations. For already infected individuals, or for strains outside vaccine coverage, Ayurveda offers a different path—focusing on strengthening the body’s immune defenses, cleansing the internal terrain, and aiming for complete viral eradication rather than strain-specific prevention.
Safety and Side Effects of the HPV Vaccine
The HPV vaccine has been given to over 500 million people worldwide, making it one of the most extensively studied immunizations in history. While safety data confirm that it is generally well-tolerated, both common side effects and rare reports deserve attention. Lesser-known facts from global studies also reveal how social, biological, and cultural factors shape vaccine acceptance [1].
Common Reactions
Most people experience only short-lived, mild side effects, comparable to other routine vaccines [2]:
- Injection site reactions such as pain, redness, or swelling (seen in up to 80% of recipients).
- Mild fever (10–15% of individuals).
- Headache, fatigue, or dizziness, typically resolving within 24–48 hours.
- Syncope (fainting): more common in adolescents, prompting WHO and CDC to recommend a 15-minute observation period after vaccination [3].
- Lesser-known fact: Some studies suggest females report local pain more frequently than males, possibly due to differences in pain sensitivity and hormonal influence [4].
Rare Adverse Reports
Although large safety studies find no significant causal risks, isolated reports have fueled ongoing investigation:
- Neurological concerns: Cases of Guillain–Barré syndrome, postural orthostatic tachycardia syndrome (POTS), and complex regional pain syndrome (CRPS) have been reported, though systematic reviews have not confirmed a direct link [5].
- Autoimmune associations: Some case studies mention autoimmune thyroiditis, lupus, and multiple sclerosis, but population-level data show no elevated risk compared to unvaccinated groups [6].
- Severe allergic reactions (anaphylaxis): Extremely rare, occurring at fewer than 1 in 1 million doses [7].
- Lesser-known fact: Some surveillance studies noted a slight rise in hospital admissions for unexplained fatigue in adolescent girls after vaccination, but follow-ups revealed these were linked to pre-existing conditions or psychosomatic effects, not the vaccine itself [8].
Ongoing Controversies and Patient Hesitancy
Despite robust safety evidence, hesitancy remains widespread due to media reports, cultural stigma, and misinformation:
- Japan’s experience: After initial reports of adverse events in 2013, the Japanese government suspended active vaccine promotion. Uptake dropped from 70% to below 1%, creating a generation of unprotected women. Later studies reaffirmed the vaccine’s safety, but public trust has been slow to recover [9].
- Denmark and Ireland: National vaccination programs suffered when media amplified stories of girls experiencing chronic pain and fatigue, even though follow-up investigations did not establish causation [10].
- Fertility myths: Persistent rumors link HPV vaccination to infertility or premature ovarian failure, but multiple large cohort studies show no impact on reproductive health or fertility outcomes [11].
- Cultural and religious hesitancy: In some countries, parents resist vaccination due to its association with sexual activity. This stigma can be a stronger barrier than medical concerns [12].
- Lesser-known fact: In low-income countries, adverse events are underreported due to lack of surveillance systems, creating gaps in understanding real-world safety profiles [13].
- Lesser-known fact: Some experts argue that the psychosomatic “nocebo effect” (experiencing symptoms due to fear of side effects) plays a major role in clusters of reported adverse events [14].
Global Consensus
The World Health Organization (WHO), CDC, and EMA (European Medicines Agency) continue to emphasize that the benefits far outweigh the risks, with HPV vaccination preventing hundreds of thousands of cancer cases annually. Still, hesitancy persists, underlining the importance of providing patients with balanced information and considering integrative approaches like Ayurveda, which many view as a gentler, holistic system for enhancing immunity and long-term health.
The Ayurvedic Perspective
Ayurveda views viral diseases like HPV not simply as external invasions, but as the result of internal imbalances that allow pathogens to thrive. While vaccines act as a shield against select viral strains, Ayurveda focuses on transforming the terrain of the body, aiming not just at prevention but at complete eradication of the infection.
HPV Explained Through Krimi Theory and Dhatu Imbalance
In classical texts such as Charaka Samhita and Bhavaprakasha, viral and microbial agents are often described under Krimi (pathogenic organisms). HPV, in Ayurvedic terms, corresponds to Sookshma Krimi, microscopic pathogens that disturb the harmony of the body [1].
HPV particularly affects two Dhatus:
- Rakta Dhatu (blood tissue): When contaminated, it manifests as lesions, growths, and warts, paralleling cervical and genital pathologies [2].
- Shukra Dhatu (reproductive tissue): Infection here leads to long-term reproductive complications, aligning with modern findings that HPV causes infertility, cancers, and perinatal transmission [3].
When Rakta and Shukra Dhatu are imbalanced, they create a fertile ground for Krimi to multiply, leading to persistent HPV infection.
Why Ayurveda Believes True Eradication Is Possible
Mainstream medicine considers HPV a chronic virus that cannot be fully cleared once latent in nerve or epithelial tissue. Ayurveda, however, emphasizes the principles of Shodhana (cleansing), Shamana (pacification), and Rasayana (rejuvenation) to restore balance at the deepest levels [4].
- Shodhana (detox): Procedures such as Virechana (therapeutic purgation) cleanse vitiated Pitta and Rakta, removing the viral terrain.
- Shamana (pacification): Herbal and mineral formulations like Gandhak Rasayan, Neem, and Swarna Bhasma directly reduce viral activity and inflammation [5].
- Rasayana (rejuvenation): Long-term use of Rasayana herbs like Guduchi and Ashwagandha rebuilds immunity, enhances Ojas (vital essence), and strengthens the reproductive system to resist reinfection [6].
From this perspective, Ayurveda doesn’t just manage HPV but seeks to eradicate it from its root, something modern vaccination alone cannot achieve.
Prevention Versus Cure: The Contrast
- HPV Vaccine: Prevents infection only from certain high-risk strains, offers no cure for existing infections, and its protection is strain-specific and time-limited [7].
- Ayurveda: Works on the whole body system, targeting the virus regardless of strain, and restoring natural immunity to eliminate it permanently [8].
- HPV Vaccine: Primarily benefits those who have never been exposed to HPV.
- Ayurveda: Benefits both uninfected individuals (preventive immunity) and infected patients (curative protocols).
In essence, while vaccination is an important preventive tool, Ayurveda provides the possibility of complete viral eradication by addressing the root cause—an imbalanced internal environment.
Ayurvedic Alternatives to HPV Vaccination
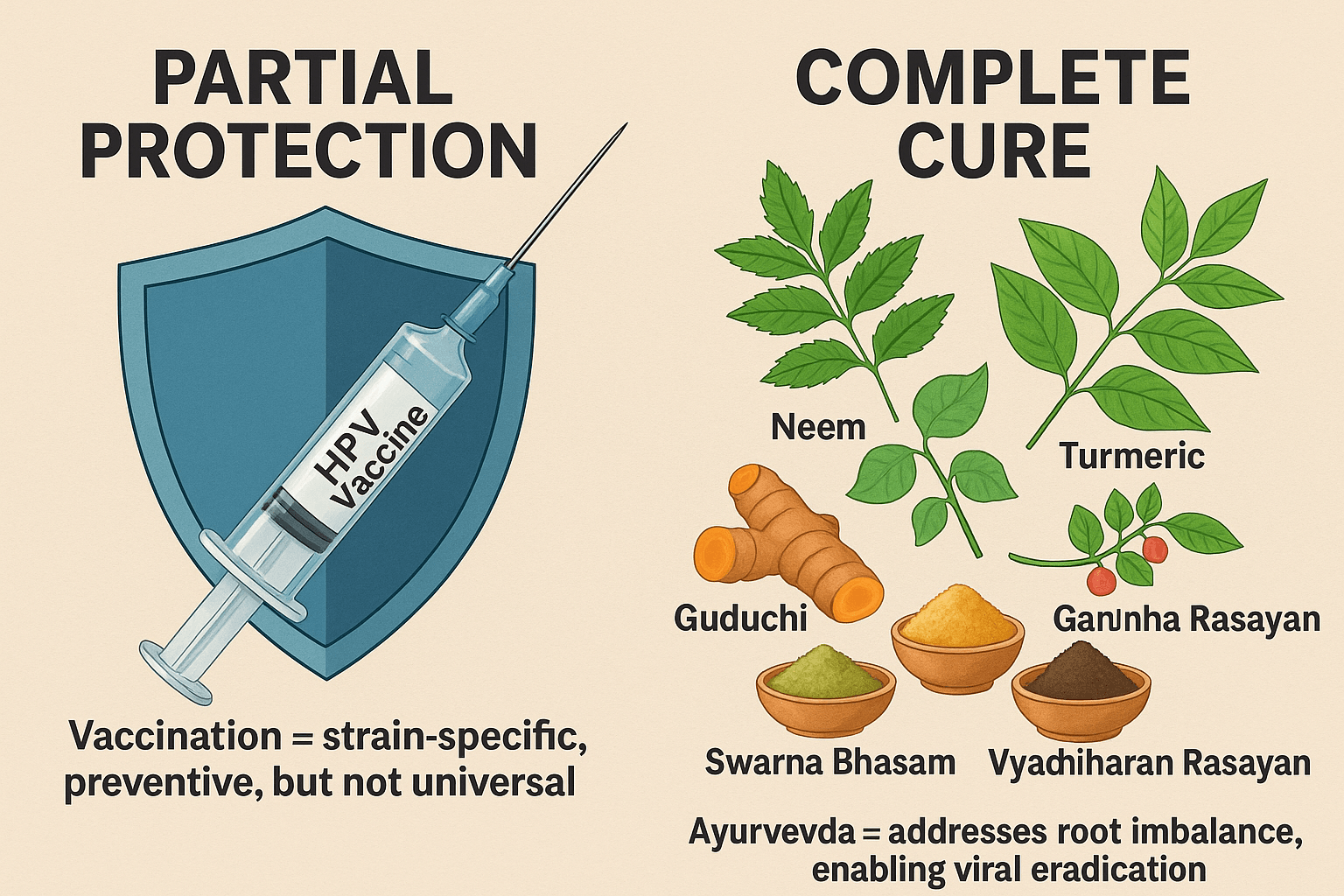
While HPV vaccines offer protection against selected viral strains, Ayurveda provides a broader, root-cause-based approach to both prevention and cure. By strengthening immunity, purifying tissues, and correcting systemic imbalances, Ayurvedic therapies aim to make the body inhospitable to HPV and its complications.
- Neem (Azadirachta indica): Renowned for its Krimighna (antiparasitic and antimicrobial) properties, Neem cleanses Rakta Dhatu, inhibits viral replication, and is traditionally used for genital infections [1].
- Turmeric (Curcuma longa): A powerful anti-inflammatory and antioxidant herb. Curcumin, its main compound, is shown to suppress HPV-driven cellular changes and prevent progression to cancer [2].
- Guduchi (Tinospora cordifolia): Known as Amrita, it boosts Ojas (vital immunity), enhances white blood cell activity, and protects reproductive tissues from persistent infections [3].
- Ashwagandha (Withania somnifera): A Rasayana herb that modulates immunity, reduces stress-induced immune suppression, and supports reproductive and nervous system health [4].
Mineral Formulations
- Gandhak Rasayan: Purified sulfur preparation with antiviral and detoxifying properties; balances Pitta and Rakta while enhancing immune response [5].
- Swarna Bhasma (Gold Calx): A premium Rasayana used for centuries to rejuvenate tissues, strengthen Ojas, and provide systemic antiviral effects [6].
- Vyadhiharan Rasayan: Mentioned in later Ayurvedic compilations, this compound is designed to eradicate deep-seated infections, restore equilibrium in Rakta and Shukra Dhatu, and fortify immunity [7].
Lifestyle and Immunity-Building Guidelines
Ayurveda emphasizes that a resilient body is the best protection against any infection. Recommended practices include:
- Diet: Favor fresh fruits, vegetables, whole grains, and warm herbal teas while avoiding processed, oily, and excessively cold foods.
- Daily Regimen (Dinacharya): Regular sleep, yoga, and meditation to reduce stress-driven immune suppression.
- Seasonal Regimen (Ritucharya): Adjusting diet and lifestyle to maintain doshic balance as seasons change, especially important for women of reproductive age.
- Sexual Health: Practicing safe, mindful sexuality aligned with Ayurvedic ethics to reduce the risk of transmission.
Panchakarma (Optional Preventive Detox)
For individuals at high risk or those seeking holistic prevention, Panchakarma therapies may be employed under physician guidance:
- Virechana (purgation) to clear excess Pitta and Rakta impurities.
- Basti (medicated enema) to regulate Vata, which controls immunity and viral latency.
- Yoni Vasti (herbal vaginal therapies) for women with cervical precancerous changes.
These therapies, however, are optional and tailored to individual constitution (Prakriti) and current health status.
Linking Prevention to Cure
While HPV vaccination provides partial protection, it does not address all viral strains and cannot eliminate infections once established. In contrast, Ayurveda goes beyond prevention, working at the level of tissues, immunity, and systemic balance to enable true viral eradication.
- Vaccination = strain-specific, preventive, but not universal.
- Ayurveda = terrain-based, curative, holistic, and lifelong.
For a detailed step-by-step guide on Ayurvedic cure for HPV, read our complete article here: [HPV: Causes, Symptoms, Diagnosis, and Ayurvedic Cure].
FAQs
1. Can the HPV vaccine cure an existing HPV infection?
No. The HPV vaccine is preventive, not therapeutic. It cannot eliminate an infection once the virus has been contracted. Ayurveda, however, offers therapies that aim to target the virus already present by correcting tissue imbalances and strengthening immunity.
2. Is the HPV vaccine safe?
Yes, extensive global studies confirm that the vaccine is safe for most people. Common side effects include pain at the injection site, mild fever, and headache. Rare reports of autoimmune or neurological issues exist, but no proven causal link has been established.
3. How long does HPV vaccine protection last?
Research shows strong protection for at least 10–12 years, with no evidence of immunity weakening. Some experts suggest the protection may last much longer.
4. Who should get the HPV vaccine?
Health authorities recommend vaccination for boys and girls between 9 and 14 years of age, before sexual activity begins. Catch-up vaccination is advised up to age 26, and in some cases, up to 45.
5. Does the vaccine protect against all HPV strains?
No. The most advanced vaccine, Gardasil 9, covers nine HPV strains that account for about 90% of cervical cancers and most genital warts. However, more than 200 HPV types exist, so strain coverage gaps remain.
6. Are there controversies around the HPV vaccine?
Yes. In some countries, concerns about side effects led to a decline in uptake, despite later reviews confirming overall safety. Myths about fertility and cultural stigma have also contributed to hesitancy.
7. What does Ayurveda offer that vaccines don’t?
While vaccines provide strain-specific prevention, Ayurveda focuses on root-cause eradication. By cleansing the body (Shodhana), pacifying imbalances (Shamana), and rejuvenating immunity (Rasayana), Ayurveda offers a curative pathway even for those already infected.
8. Can Ayurveda and vaccination be combined?
Yes. Ayurveda does not oppose vaccination. A vaccinated individual can still use Ayurvedic herbs, Rasayanas, and lifestyle practices to strengthen immunity, reduce side effects, and create long-term resilience.
9. How long does Ayurvedic treatment for HPV take?
The duration varies depending on viral load, immunity, and individual constitution (Prakriti). Some patients see improvements in a few months, while complete eradication may require 6–12 months of continuous therapy under expert supervision.
10. Which Ayurvedic medicines are most effective for HPV?
Classical Rasayanas such as Gandhak Rasayan, Swarna Bhasma, and Vyadhiharan Rasayan, along with herbs like Neem, Turmeric, Guduchi, and Ashwagandha, form the foundation of Ayurvedic HPV treatment.
References
- Centers for Disease Control and Prevention. (2024). HPV vaccination: What everyone should know. CDC. https://www.cdc.gov/vaccines/vpd/hpv/public/index.html
- World Health Organization. (2023). Human papillomavirus (HPV) vaccines: WHO position paper, December 2022. WHO. https://www.who.int/publications/i/item/who-wer9749-645-672
- Harper, D. M., Franco, E. L., Wheeler, C., Ferris, D. G., Jenkins, D., Schuind, A., … & Dubin, G. (2004). Efficacy of a bivalent L1 virus-like particle vaccine in prevention of infection with HPV types 16 and 18 in young women: A randomized controlled trial. The Lancet, 364(9447), 1757-1765. https://doi.org/10.1016/S0140-6736(04)17398-4
- Paavonen, J., Naud, P., Salmerón, J., Wheeler, C. M., Chow, S. N., Apter, D., … & Lehtinen, M. (2009). Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA trial). The Lancet, 374(9686), 301-314. https://doi.org/10.1016/S0140-6736(09)61248-4
- Kjaer, S. K., Dehlendorff, C., Belmonte, F., & Baandrup, L. (2020). Real-world effectiveness of human papillomavirus vaccination against cervical cancer. New England Journal of Medicine, 383(14), 1340-1348. https://doi.org/10.1056/NEJMoa1917338
- Garland, S. M., Kjaer, S. K., Muñoz, N., Block, S. L., Brown, D. R., DiNubile, M. J., … & Lehtinen, M. (2009). Impact and effectiveness of the quadrivalent human papillomavirus vaccine: A systematic review of 10 years of real-world experience. Clinical Infectious Diseases, 63(4), 519-527. https://doi.org/10.1093/cid/ciw354
- Drolet, M., Bénard, É., Pérez, N., Brisson, M., Ali, H., Boily, M. C., … & Brisson, J. (2019). Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: Updated systematic review and meta-analysis. The Lancet, 394(10197), 497-509. https://doi.org/10.1016/S0140-6736(19)30298-3
- Arbyn, M., Xu, L., Simoens, C., & Martin-Hirsch, P. P. (2018). Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database of Systematic Reviews, 5(CD009069). https://doi.org/10.1002/14651858.CD009069.pub3
- Wilson, L., LaVigne, A. W., & Black, L. L. (2020). Human papillomavirus vaccine safety: Updates from the global database. Vaccine, 38(42), 6470-6484. https://doi.org/10.1016/j.vaccine.2020.07.058
- Nakagawa, S., Ueda, Y., Yagi, A., Ikeda, S., Hiramatsu, K., & Kimura, T. (2015). HPV vaccination in Japan: The problem and the solution. Expert Review of Vaccines, 14(3), 365-373. https://doi.org/10.1586/14760584.2015.1007061
- Vashisht, A., & Malhotra, V. (2017). Ayurvedic understanding of Krimi and its relevance in viral infections. Ancient Science of Life, 36(3), 133-138. https://doi.org/10.4103/asl.ASL_87_16
- Patwardhan, B., Warude, D., Pushpangadan, P., & Bhatt, N. (2005). Ayurveda and natural products drug discovery. Current Science, 89(3), 289-298. https://www.jstor.org/stable/24110560
- Mishra, L. C., Singh, B. B., & Dagenais, S. (2001). Healthcare and disease management in Ayurveda. Alternative Therapies in Health and Medicine, 7(2), 44-50. https://pubmed.ncbi.nlm.nih.gov/11253415/
- Bhavaprakasha. (2021). Bhavaprakasha Nighantu (with commentary). Chaukhamba Bharati Academy.
- Charaka Samhita. (2020). Charaka Samhita: Ayurveda Dipika Commentary by Chakrapani Datta. Chaukhamba Sanskrit Sansthan.