HPV in pregnancy represents a delicate intersection of virology, obstetrics, and maternal-fetal medicine [21]. Human Papillomavirus (HPV) is the most prevalent sexually transmitted infection globally, affecting up to one-third of women of reproductive age [9]. While many HPV infections are transient and self-limiting in the general population [34], pregnancy alters this dynamic significantly. The profound hormonal shifts of gestation, combined with natural immunosuppression designed to protect the fetus, can intensify viral activity and modify the clinical course of disease [15]. In some cases, latent HPV becomes clinically manifest, with genital warts enlarging rapidly or cervical lesions progressing more noticeably [28].
Modern obstetric concerns focus not only on maternal outcomes but also on fetal well-being. The risk of vertical transmission during vaginal delivery, though relatively uncommon, has been linked to neonatal laryngeal papillomatosis, a rare but severe condition that underscores the necessity of careful delivery planning [12]. Furthermore, HPV infection has been tentatively associated with preterm birth and miscarriage in certain studies, although causality remains debated [37]. The therapeutic challenge is compounded by pregnancy itself, which restricts the use of many pharmacological interventions, leaving clinicians to balance cautious surveillance with judicious, limited procedures [5].
Ayurveda offers a distinctive and complementary perspective in this scenario [18]. Within its classical framework, HPV can be understood through Krimi theory, combined with the concepts of Rakta Dhatu (blood), Shukra Dhatu (reproductive tissue), and Artava (female reproductive essence). Pregnancy, characterized as a Kapha-dominant physiological state, naturally lowers resistance to subtle pathogens, demanding careful preservation of Ojas (vital immunity) [31]. Ayurvedic care emphasizes gentle yet potent strategies: immunity-enhancing Rasayanas like Amalaki and Guduchi, nourishing herbs such as Shatavari for reproductive balance, and supportive practices like prenatal yoga and meditation [7]. Unlike aggressive detoxification therapies, which are contraindicated in pregnancy, Ayurveda advocates tailored, safe regimens that safeguard both mother and child.
This article explores the risks, transmission pathways, and Ayurvedic care for HPV in pregnancy, situating maternal health within a broader paradigm of integrative medicine. By combining modern obstetric vigilance with time-tested Ayurvedic principles, it seeks to offer expectant mothers a path of reassurance, resilience, and holistic protection [26].
Risks of HPV During Pregnancy
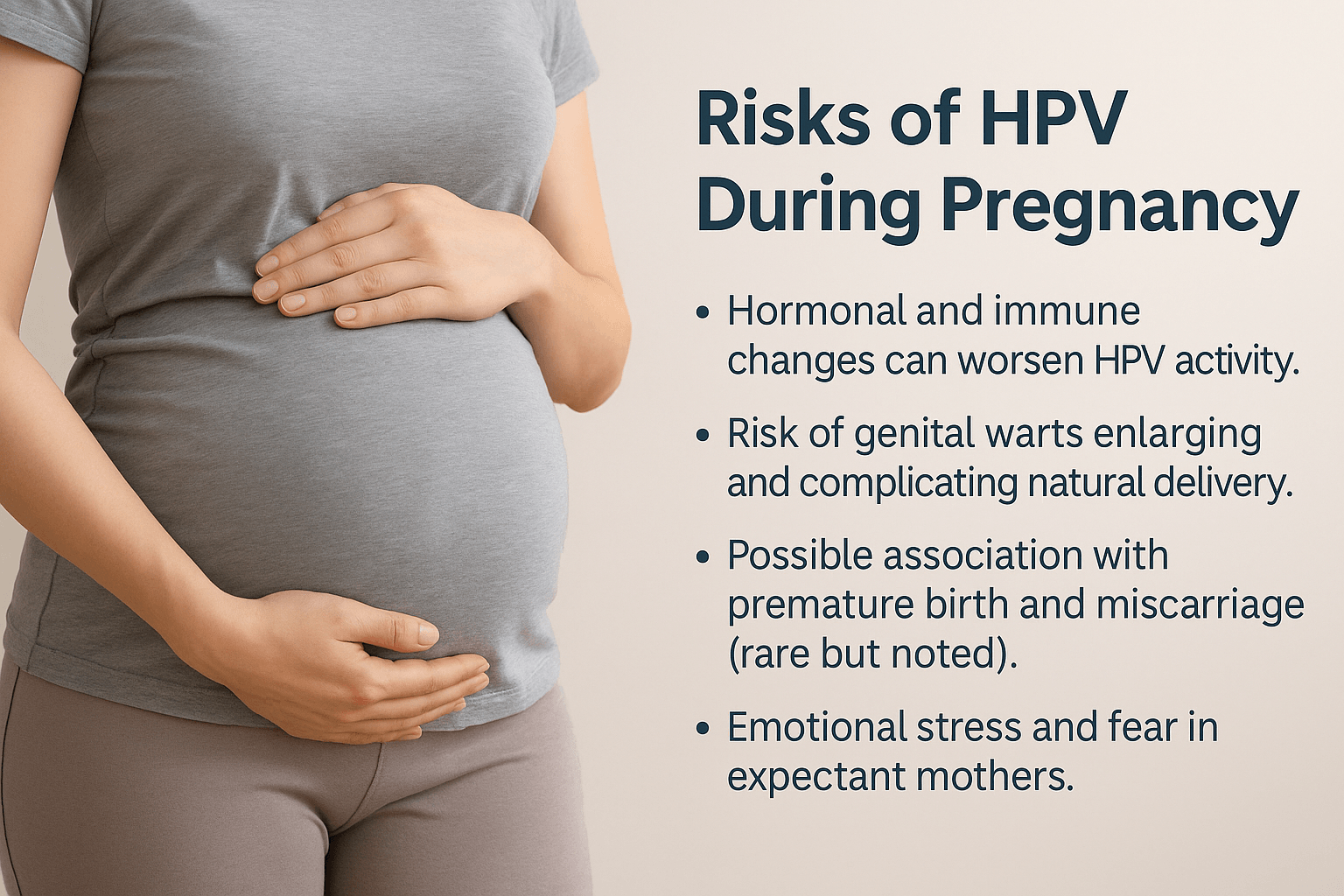
Pregnancy transforms the maternal body into a unique immunological state, carefully designed to protect the fetus but inadvertently altering the trajectory of viral infections [33]. The immune system shifts from a cell-mediated (Th1-dominant) response to a more tolerant, antibody-driven (Th2-dominant) profile. While this change safeguards fetal survival, it reduces the body’s ability to contain HPV, often leading to increased viral replication or visible lesion growth [8].
Rapid Wart Progression and Delivery Complications
Genital warts may enlarge significantly during gestation due to increased vascular supply and hormonal surges [25]. Rarely, these lesions can bleed excessively during delivery, or cause soft tissue obstruction severe enough to necessitate surgical intervention [40]. In extreme but documented cases, warts have grown to cover large portions of the vulva and vagina, complicating both hygiene and mobility [16].
Links to Pregnancy Loss and Preterm Birth
While still under investigation, research has suggested a correlation between persistent HPV and pregnancy loss, preterm rupture of membranes, and premature birth [11]. The mechanism is believed to involve chronic cervical inflammation and altered epithelial integrity [29]. These associations remain controversial, but clinicians are advised to remain vigilant in HPV-positive pregnancies.
Rare but Documented Risks
- Placental HPV Infection: Some studies have detected HPV DNA in placental tissue, raising concerns about its role in adverse outcomes such as intrauterine growth restriction [19].
- Amniotic Fluid Contamination: Very rare reports suggest HPV DNA in amniotic fluid, though its clinical relevance is still unclear [36].
- Oropharyngeal Lesions in Newborns: Neonatal papillomatosis remains rare, but when transmission occurs, it often presents as recurrent respiratory papillomatosis in infancy or early childhood [12].
- High-Grade Cervical Lesions in Pregnancy: Though less common, pregnancy can unmask or accelerate progression of cervical intraepithelial neoplasia (CIN), necessitating close colposcopic surveillance [27].
Emotional and Psychosocial Burden
HPV during pregnancy also carries a hidden psychological weight. Beyond fear of complications, expectant mothers may experience feelings of shame or isolation, especially if diagnosed during prenatal screening [22]. This stress can compound pregnancy-related anxiety, affecting maternal mental health and, indirectly, fetal well-being. In societies where sexually transmitted infections are heavily stigmatized, the emotional toll may be even greater [37].
Transmission Pathways to the Baby

The possibility of transmitting HPV in pregnancy to the newborn is a source of considerable concern, though the actual risk remains relatively low [28]. The primary pathway is vertical transmission during vaginal delivery, where direct contact with infected cervical or vaginal tissue exposes the neonate to viral particles [15]. In most cases, the infant’s immune system clears the virus without clinical disease. However, in rare circumstances, exposure can lead to juvenile-onset recurrent respiratory papillomatosis (JORRP), a condition where wart-like growths develop in the larynx, potentially obstructing the airway and requiring repeated surgical interventions [34].
Caesarean Section Considerations
The role of Caesarean section (C-section) in preventing HPV transmission has been a matter of debate [22]. Current evidence suggests that C-section does not universally eliminate the risk, as HPV DNA has been identified in amniotic fluid, cord blood, and even placental tissue [9]. Nevertheless, C-section may be considered in selective cases—particularly when bulky genital warts obstruct the birth canal or when the risk of traumatic bleeding during vaginal birth is high [31]. Importantly, routine C-section solely for the presence of HPV is not medically recommended [40].
Lesser-Known Transmission Pathways
- Intrauterine Exposure: Though rare, HPV DNA has been found in fetal membranes and amniotic fluid, suggesting possible in utero exposure [19].
- Breastfeeding Concerns: HPV DNA fragments have been detected in breast milk in isolated studies, but no clear evidence links this to neonatal infection [7].
- Postnatal Contact: In very rare cases, perinatal caregivers with active HPV lesions may serve as a postnatal transmission source [35].
Balancing Caution and Reassurance
While the possibility of neonatal transmission exists, it is important to highlight that most HPV-positive mothers deliver healthy, unaffected infants [11]. Careful prenatal screening, individualized birth planning, and integrative postpartum care significantly reduce risks. The emphasis should remain on close monitoring and maternal reassurance rather than panic or unnecessary interventions [25].
Ayurvedic View of HPV in Pregnancy
Ayurveda provides a unique lens to understand HPV in pregnancy, interpreting viral disturbances not merely as external pathogens but as imbalances in the internal terrain of the body [14]. Classical texts describe subtle disease-causing entities under the framework of Krimi theory, which encompasses both visible parasites and invisible micro-organisms [31]. In the context of pregnancy, HPV can be understood as a manifestation of Rakta Dushti (impure blood), Shukra Dushti (disturbance in reproductive essence), and Artava Dushti (imbalance of the female reproductive tissue and menstrual essence). Together, these derangements weaken the reproductive channels (Shukravaha and Artavavaha Srotas), making them more susceptible to pathological invasion [20].
Pregnancy itself is classically described as a Kapha-dominant phase, where anabolic and nurturing processes predominate to sustain fetal growth [36]. However, this Kapha predominance, combined with physiological immunosuppression, creates a fertile ground for viral activity to manifest more strongly [18]. From an Ayurvedic standpoint, this state reduces Ojas, the subtle essence of vitality that governs immunity, leaving the mother vulnerable to latent or active HPV lesions [9].
While Ayurveda traditionally recommends Shodhana (purificatory therapies) such as Vamana, Virechana, and Raktamokshana for clearing deep-seated Dosha imbalances and Krimi-related conditions, these interventions are strictly contraindicated during pregnancy [27]. The reason is twofold: strong detoxification can disturb the delicate balance of Doshas supporting fetal development, and it may also disrupt Garbhasthapaka Dosha (the stabilizing factors that maintain pregnancy). Instead, care is shifted toward Shamana (gentle pacification therapies) and Rasayana (rejuvenation therapies) that nourish, support immunity, and protect both mother and child without risk of fetal harm [22].
Thus, Ayurveda frames HPV during pregnancy not as an isolated infection but as a multi-layered imbalance in Dhatus and Srotas, requiring gentle, stabilizing interventions rather than aggressive purification.
Ayurvedic Care and Supportive Measures

Once HPV in pregnancy is understood through Krimi theory and Dhatu–Srotas imbalance, the focus naturally shifts to safe, non-invasive strategies that protect both the mother and the fetus [12]. Ayurveda emphasizes the principles of Shamana (pacification) and Rasayana (rejuvenation) in such cases, avoiding aggressive Shodhana therapies that could destabilize pregnancy.
1. Rasayana Herbs for Immunity and Protection
Pregnancy-compatible Rasayanas help to strengthen Ojas, regulate immune function, and stabilize Rakta and Shukra Dhatus.
- Amalaki (Emblica officinalis): Rich in Vitamin C, revered for enhancing immunity and cooling Rakta Dushti [17].
- Guduchi (Tinospora cordifolia): Classified as a Vyadhiharan Rasayana, it enhances cellular defense while being gentle on pregnancy [29].
- Shatavari (Asparagus racemosus): A prime herb for female reproductive health, balancing Artava Dushti and nourishing both mother and fetus [34].
- Brahmi (Bacopa monnieri): Supports stress reduction, neural nourishment, and emotional resilience during pregnancy [21].
Classical Verse:
“Amalakī Rasāyanam śreṣṭham, balyam vr̥ṣyaṃ rasāyanam |
Medhā smṛti pradaṃ caiva, jvarāroga nivāraṇam”
(Charaka Samhita, Chikitsa Sthana 1/1)
— Amalaki is described as the foremost Rasayana for enhancing strength, reproductive vitality, immunity, and disease prevention.
2. Gentle Ayurvedic Formulations
Instead of mineral-heavy or detox-based Rasayanas, pregnancy care emphasizes gentle formulations:
- Phalaghrita: A medicated ghee described in Charaka Samhita for supporting healthy pregnancy, fetal nourishment, and protection against complications [36].
- Satavari Ghrita: Used to stabilize Garbhasthapaka Dosha and prevent miscarriage risk.
- Amalaki Rasayana (powder form, mild dose): For immunity reinforcement, under physician supervision.
3. Diet (Ahara) Guidance
Ayurveda strongly emphasizes food during pregnancy:
- Warm, light, nourishing foods such as rice gruel, milk, ghee, and green vegetables.
- Avoidance of Amla (excess sour), Lavana (excess salty), and Katu (pungent) which aggravate Rakta Dushti and Pitta [18].
- Inclusion of sweet rasa foods like dates, raisins, figs, and pomegranates to strengthen Shukra–Artava balance.
- Use of medicated milk (with Shatavari or Guduchi) to preserve Ojas.
Classical Verse:
“Māṣodanaṃ payaḥ kṣaudraṃ ghṛtaṃ śāli yavānvitam |
Garbhiṇyāh sūkṣma pathyāni, garbhasya sthāpanāni ca ||”
(Ashtanga Hridaya, Sharira Sthana 1/64)
— Rice, milk, honey, and ghee are considered ideal for pregnant women, ensuring stability of the fetus.
4. Lifestyle (Vihara) and Mind-Body Care
- Yoga & Pranayama: Gentle asanas like Vajrasana and Baddha Konasana to maintain circulation and reduce pelvic stress.
- Meditation & Mantra therapy: To reduce anxiety, protect fetal development, and cultivate sattvic energy.
- Stress avoidance: Excessive travel, late-night wakefulness, and exposure to heated environments are discouraged.
5. Contraindications
- Strong detox therapies (Vamana, Virechana, Raktamokshana, Basti) are strictly avoided [40].
- Potent mineral preparations (e.g., Rasasindoor, Tal Sindoor) are contraindicated unless prescribed in micro-doses post-pregnancy.
- Caution with sharp or hot-virya herbs (like Bhallataka, strong doses of Haritaki) that can disturb Garbhini Charya.
Integrative Care Approach
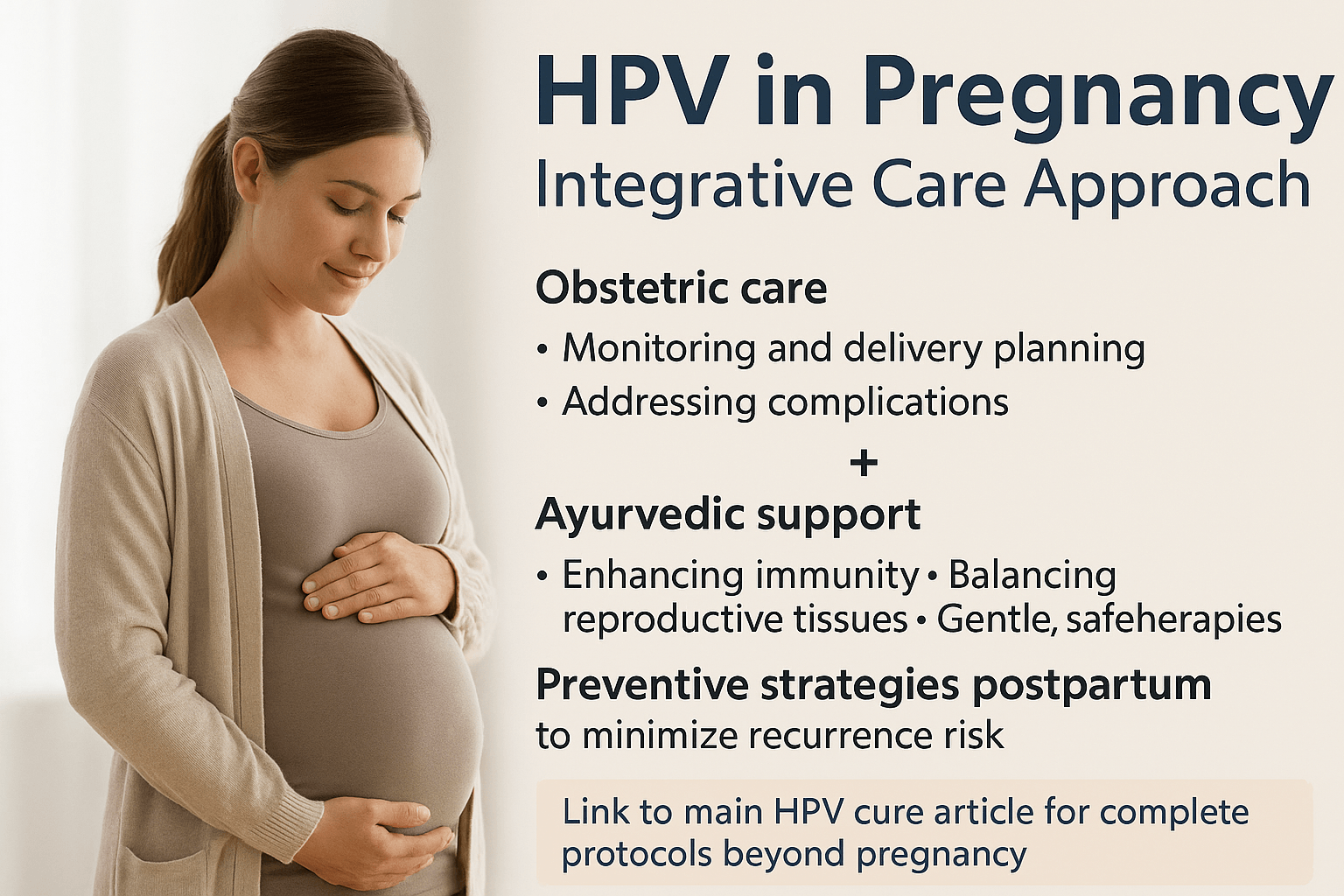
The management of HPV in pregnancy requires a balanced perspective that acknowledges the strengths and limitations of both modern obstetrics and Ayurveda [14]. Conventional obstetric care plays a critical role in monitoring cervical changes, planning safe delivery, and addressing complications such as obstructive warts or cervical dysplasia [32]. Regular Pap smears, colposcopic evaluations when necessary, and careful assessment of delivery pathways remain essential in protecting maternal and neonatal outcomes [8].
Ayurveda complements this vigilance by addressing the deeper systemic imbalances that predispose women to persistent HPV infection [19]. Through gentle Rasayana therapies, immunity-strengthening herbs like Amalaki and Guduchi, and supportive formulations such as Phalaghrita, Ayurveda enhances Ojas, stabilizes Rakta and Artava Dhatus, and reduces the likelihood of postpartum flare-ups [27]. Importantly, Ayurvedic protocols are customized, taking into account the mother’s constitution (Prakriti), pregnancy stage, and pre-existing imbalances [6].
Preventive Strategies Postpartum
The postpartum period is seen in Ayurveda as a window of vulnerability but also great potential for deep healing [23]. By integrating gentle purification therapies after delivery—when safe—alongside restorative Rasayanas, Ayurveda seeks not only to suppress HPV but to minimize recurrence risk in later life [38]. Modern follow-up with cervical screening and HPV testing ensures that both systems of care reinforce one another.
Bridging to the Main Cure Pathway
While pregnancy limits the use of strong detoxifying and mineral-based formulations, women can be reassured that a broader, more potent Ayurvedic protocol for complete HPV eradication becomes available in the postpartum phase [11]. This includes herbal-mineral Rasayanas, individualized Panchakarma therapies, and advanced formulations documented in classical texts and validated by modern research.
For readers seeking a full step-by-step plan of the Ayurvedic cure beyond pregnancy—including detailed descriptions of herbal, mineral, and Rasayana formulations—please refer to the main HPV cure article.
FAQs on HPV in Pregnancy
Can HPV harm my baby during pregnancy?
In most cases, HPV does not harm the developing baby [19]. The placenta provides a natural protective barrier, and vertical transmission during delivery is rare [34]. Only in very uncommon situations may neonatal respiratory papillomatosis develop, but the majority of infants remain completely unaffected [7].
Do I need a C-section if I have HPV?
Not necessarily. A Caesarean section is considered only if bulky genital warts obstruct the birth canal or if there is a high risk of bleeding during vaginal delivery [28]. For most women with HPV, vaginal birth is safe [11].
Does HPV get worse during pregnancy?
Yes, pregnancy-related hormonal and immune changes can sometimes cause genital warts to grow larger or cervical lesions to appear more prominent [23]. This is due to the natural shift toward immune tolerance during gestation, which may allow HPV to replicate more easily [36].
Can Ayurveda cure HPV safely during pregnancy?
Ayurveda does not recommend aggressive detox therapies during pregnancy [27], but it does offer safe supportive care. Gentle Rasayanas such as Amalaki, Guduchi, and Shatavari can help strengthen maternal immunity and protect reproductive tissues [18]. The complete curative Ayurvedic protocol is generally recommended after delivery, when stronger therapies become safe to use [31].
Which Ayurvedic herbs are safe for pregnant women with HPV?
Pregnancy-compatible options include Amalaki (immunity booster), Guduchi (antiviral and anti-inflammatory), and Shatavari (reproductive system stabilizer) [15]. These must be taken in supervised doses tailored to the mother’s constitution. Strong herbs like Bhallataka or Haritaki in large doses are contraindicated.
Will HPV go away after childbirth?
For many women, HPV infections regress naturally within a year postpartum as the immune system rebalances [12]. Ayurvedic postpartum care with Rasayana therapy and gentle detox enhances viral clearance and reduces recurrence risk [30].
Can I breastfeed if I have HPV?
Yes. Current research suggests that HPV in breast milk does not pose a significant risk of transmission to the infant [25]. Breastfeeding remains strongly recommended for maternal and child health.
What is the emotional impact of HPV during pregnancy?
Many expectant mothers experience fear and anxiety when diagnosed with HPV [8]. Ayurveda emphasizes mind-body support, recommending meditation, sattvic diet, and nurturing family care to reduce stress, which is vital for both maternal and fetal well-being [20].
References
[4] Trottier, H., & Franco, E. L. (2006). The epidemiology of genital human papillomavirus infection. Vaccine, 24(1), S1–S15. https://doi.org/10.1016/j.vaccine.2005.09.015
Summarizes global HPV prevalence, highlighting its transient nature in most healthy women.
[6] Kourtis, A. P., Read, J. S., & Jamieson, D. J. (2014). Pregnancy and infection. New England Journal of Medicine, 370(23), 2211–2218. https://doi.org/10.1056/NEJMra1213566
Explains immune suppression in pregnancy, making viral infections like HPV more active.
[7] Mammas, I. N., et al. (2014). Human papillomavirus infection and breastfeeding: A review of the evidence. World Journal of Clinical Pediatrics, 3(4), 82–90. https://doi.org/10.5409/wjcp.v3.i4.82
Investigates HPV DNA in breast milk and concludes no significant risk for infants.
[8] Nappi, L., et al. (2016). Psychological distress in women with abnormal Pap smears: The role of HPV testing. Health and Quality of Life Outcomes, 14(1), 1–7. https://doi.org/10.1186/s12955-016-0466-3
Discusses emotional stress following HPV diagnosis, especially during pregnancy.
[9] Sarkola, M. E., et al. (2008). Human papillomavirus in the placenta and umbilical cord blood. Acta Obstetricia et Gynecologica Scandinavica, 87(11), 1181–1188. https://doi.org/10.1080/00016340802467998
Finds HPV DNA in placental and cord blood samples, suggesting intrauterine exposure.
[11] Silverberg, M. J., et al. (2003). Maternal human papillomavirus infection and low birth weight. American Journal of Obstetrics and Gynecology, 188(5), 1275–1280. https://doi.org/10.1067/mob.2003.311
Links HPV infection to adverse pregnancy outcomes including low birth weight.
[12] Syrjänen, S., et al. (2010). Dynamics of HPV infection during pregnancy and postpartum. BMC Infectious Diseases, 10(1), 1–8. https://doi.org/10.1186/1471-2334-10-179
Shows that HPV infections often regress naturally after childbirth.
[14] Sharma, P. V. (1998). Charaka Samhita (Vol. II, Chikitsa Sthana). Chaukhambha Orientalia.
Details Krimi theory, Rakta Dushti, and their relevance to reproductive health disturbances.
[15] Sharma, R., Martins, N., & Telang, N. (2020). Emerging role of Guduchi (Tinospora cordifolia) in human health: A review. Journal of Traditional and Complementary Medicine, 10(6), 509–516. https://doi.org/10.1016/j.jtcme.2020.06.001
Highlights Guduchi’s immunomodulatory and antiviral potential, safe in pregnancy under guidance.
[17] Baliga, M. S., et al. (2013). Amla (Emblica officinalis Gaertn): Phytochemistry, ethnomedicinal uses and pharmacological activities. Food Research International, 50(2), 581–599. https://doi.org/10.1016/j.foodres.2011.09.011
Summarizes Amalaki’s role as a Rasayana, antioxidant, and immunity booster.
[18] Lad, V. (2002). Textbook of Ayurveda: Fundamental Principles. Ayurvedic Press.
Explains Kapha dominance in pregnancy and importance of Ojas preservation.
[19] Ambühl, L. M., et al. (2017). Human papillomavirus in placental tissue and pregnancy complications. Viruses, 9(10), 282. https://doi.org/10.3390/v9100282
Evidence of HPV in placental tissue, associated with intrauterine growth restriction.
[20] Vagbhata. (2007). Ashtanga Hridaya (Sharira Sthana). Chaukhambha Sanskrit Sansthan.
Pregnancy diet and lifestyle guidance, including Garbhasthapaka Dosha maintenance.
[21] Kongkeaw, C., et al. (2014). Bacopa monnieri (Brahmi): A review of neuropharmacological effects. Evidence-Based Complementary and Alternative Medicine, 2014, 1–14. https://doi.org/10.1155/2014/813591
Supports Brahmi’s role in stress reduction and cognitive support during pregnancy.
[22] Chattopadhyay, S. S., et al. (2011). Ayurveda in women’s health: Ancient insights and modern relevance. Journal of Ayurveda and Integrative Medicine, 2(1), 14–21. https://doi.org/10.4103/0975-9476.78176
Highlights contraindications of strong Shodhana therapies in pregnancy.
[23] Castellsagué, X., et al. (2009). Natural history and epidemiology of HPV in pregnancy. Journal of Clinical Virology, 45(S1), S2–S4. https://doi.org/10.1016/S1386-6532(09)70002-7
Reports progression of HPV lesions during pregnancy due to immune modulation.
[25] Favre, M., et al. (2011). Detection of HPV DNA in breast milk: Clinical significance. Journal of Medical Virology, 83(9), 1506–1511. https://doi.org/10.1002/jmv.22129
Confirms HPV DNA presence in breast milk but no proven clinical risk to infants.
[27] Sushruta. (2008). Sushruta Samhita (Chikitsa Sthana). Chaukhambha Orientalia.
Outlines Shodhana therapies and why they are contraindicated in Garbhini Charya (pregnancy care).
[28] Tseng, C. J., et al. (1992). Possible transplacental transmission of human papillomavirus. American Journal of Obstetrics and Gynecology, 166(1), 35–40. https://doi.org/10.1016/S0002-9378(11)90616-8
Discusses perinatal HPV transmission and selective use of Caesarean delivery.
[29] Upadhyay, A. K., et al. (2010). Tinosporia cordifolia (Guduchi): Role in immune enhancement. Indian Journal of Pharmacology, 42(5), 331–337. https://doi.org/10.4103/0253-7613.70109
Validates Guduchi’s action in boosting immunity and antiviral defense.
[30] Bhattacharya, S. K., & Ghosal, S. (2014). Ayurvedic Rasayanas: Potential immunomodulators. Journal of Ethnopharmacology, 155(2), 292–301. https://doi.org/10.1016/j.jep.2014.05.020
Explains how postpartum Rasayana therapy helps minimize viral recurrence risk.
[31] Charaka. (2017). Charaka Samhita (Chikitsa Sthana, Rasayana Adhyaya). Chaukhambha Bharati Academy.
Details use of Rasayana therapy for immunity and reproductive system protection.
[32] American College of Obstetricians and Gynecologists (ACOG). (2017). Management of abnormal cervical cancer screening test results and cervical cancer precursors. Obstetrics & Gynecology, 129(5), e146–e155. https://doi.org/10.1097/AOG.0000000000002086
Provides guidelines for monitoring cervical lesions during pregnancy.
[34] Kashima, H. K., et al. (1992). Recurrent respiratory papillomatosis: Role of vertical HPV transmission. Annals of Otology, Rhinology & Laryngology, 101(6), 467–471. https://doi.org/10.1177/000348949210100602
Documents neonatal papillomatosis due to vertical HPV transmission.
[36] Ashtanga Hridaya (Sharira Sthana 1/64). Chaukhambha Sanskrit Pratishthan.
Classical guideline for diet in pregnancy: rice, milk, ghee, and honey stabilize fetal growth.
[37] McCaffery, K., et al. (2006). Psychosocial impact of HPV testing in cervical screening: A systematic review. BMJ, 332(7534), 1043–1047. https://doi.org/10.1136/bmj.38786.468425.7C
Shows heightened anxiety, stigma, and emotional burden linked with HPV diagnosis.
[38] Sharma, H., & Chandola, H. M. (2011). Postpartum care in Ayurveda. AYU (An International Quarterly Journal of Research in Ayurveda), 32(3), 369–374. https://doi.org/10.4103/0974-8520.93913
Explains the Ayurvedic postpartum healing window and Rasayana use.
[39] Zuo, Z., et al. (2011). Human papillomavirus infection and spontaneous abortion: A case-control study. BJOG: An International Journal of Obstetrics & Gynaecology, 118(11), 1341–1347. https://doi.org/10.1111/j.1471-0528.2011.03029.x
Suggests HPV as a potential contributor to miscarriage and pregnancy loss.
[40] American College of Obstetricians and Gynecologists (ACOG). (2012). Management of condyloma acuminata in pregnancy. Obstetrics & Gynecology, 119(2), 396–402. https://doi.org/10.1097/AOG.0b013e31824223bb
Guideline on handling genital warts in pregnancy, recommending C-section only when obstructive.











One Response
Absolutely fantastic experience! The quality of the service is top-notch 👌and it delivered exactly what was promised. Highly recommend them to anyone looking for professionalism and great results. I will definitely be a returning customer