Fatty liver, medically known as hepatic steatosis, is a condition in which excess fat accumulates inside the liver cells, interfering with normal metabolism and detoxification processes (1, 3). Under healthy circumstances, the liver contains a small amount of fat, but when this fat exceeds 5–10% of the liver’s total weight, it is termed a fatty liver.
Modern hepatology divides the disease into two major types: non-alcoholic fatty liver disease (NAFLD), now reclassified as metabolic dysfunction-associated steatotic liver disease (MASLD), and alcohol-related fatty liver disease (AFLD). NAFLD or MASLD occurs in individuals who consume little to no alcohol, and its rise parallels the global epidemic of obesity, diabetes, and metabolic syndrome (1, 2, 3). Alcohol-related fatty liver, on the other hand, results from chronic alcohol intake that overwhelms hepatic metabolism and causes fat retention in hepatocytes.
Recent global studies show that one in three adults may have some degree of fatty liver, making it one of the most widespread lifestyle-related liver conditions of the modern era (1, 2). Because the liver has remarkable regenerative capacity, early fatty liver disease is often silent and produces few or no symptoms until the condition progresses to inflammation or fibrosis. By that stage, many patients experience fatigue, heaviness, or mild right upper abdominal discomfort, which are usually mistaken for digestive disturbances rather than liver pathology (3).
In Ayurveda, fatty liver is understood through the lens of Yakrit Vriddhi (enlargement or dysfunction of the liver) and Medoroga (disorders of fat metabolism), arising from imbalance in Rasa Dhatu (plasma) and Meda Dhatu (fat tissue) (5, 7, 9, 11). The root cause begins with weakened digestive fire (Agni Mandya), which leads to the formation of metabolic toxins (Ama). These toxins block microchannels (Srotas) of the liver, resulting in stagnation of unprocessed nutrients and excessive fat deposition within hepatic tissues.
Emotional and psychological factors also play a role. Chronic stress, anxiety, and irregular eating patterns aggravate Pitta and Vata doshas, impairing digestion and bile secretion, thus contributing to liver overload (7, 18). In Ayurvedic physiology, harmony between Agni (digestive fire), Pitta (metabolic energy), and Ojas (vital essence) maintains liver health. When this equilibrium is disturbed, metabolic waste begins to accumulate—manifesting clinically as fatty liver disease (5, 7, 9).
How the Liver Works
The liver serves as the body’s natural detoxification plant and primary energy regulator. It processes food nutrients, neutralizes toxins, and maintains internal chemical balance (4). Modern physiology explains that the liver regulates blood sugar, synthesizes proteins, and manages fat metabolism. It converts glucose to glycogen for energy storage, produces essential plasma proteins such as albumin, and manufactures bile, which helps digest fats and remove waste from the body (4).
According to Ayurveda, the liver is the seat of Pitta Dosha and the home of Ranjaka Pitta, which governs blood formation, coloration, and metabolic purification (5, 7, 9). Ranjaka Pitta functions within the Yakrit (liver) and Pleeha (spleen), supporting transformation of food essence into nourishing blood, closely resembling the modern concept of hepatic and hemopoietic activity. When Pitta remains balanced, digestion and metabolism proceed efficiently, but when aggravated or weakened, it leads to disorders such as Yakrit Vriddhi and Meda Dushti (5, 9).
Ayurvedic texts emphasize the deep connection between the liver and the body’s overall vitality. The liver influences Rasa Dhatu (nutritive plasma) and Rakta Dhatu (blood), determining the health of the skin, digestion, and emotional stability. When the liver becomes weak or overloaded, unprocessed metabolic toxins (Ama) circulate through the bloodstream, causing fatigue, heaviness, loss of appetite, and a dull appearance (7, 11, 18). Modern research supports this by showing that hepatic dysfunction and oxidative stress can alter neurotransmitter balance, influencing both mood and energy levels (4, 6).
Both Ayurveda and modern medicine agree that the liver is not merely an organ of detoxification but a master controller of vitality, metabolism, and mental well-being, serving as the energetic bridge between the body and mind.
What Happens Inside the Liver
Inside the liver, millions of microscopic cells called hepatocytes work constantly to maintain the body’s internal balance. These cells store energy, process nutrients, and filter out toxins that enter the bloodstream. The liver acts as a central hub for detoxification, metabolism, and nutrient transformation, ensuring that every tissue receives clean, usable energy (4, 6).
From a modern medical perspective, the liver plays multiple essential roles. It converts glucose to glycogen for storage and releases it when energy is required. It synthesizes proteins, regulates lipid metabolism, and produces bile, which helps digest fats and eliminate waste products (4, 6). When the liver’s natural metabolic functions are disrupted—by alcohol, poor diet, toxins, or chronic stress fat begins to accumulate in hepatocytes, resulting in fatty liver disease. Over time, this excess fat triggers inflammation and oxidative stress, which damage the delicate liver cells and impair their ability to detoxify and regenerate (6, 8).
Ayurveda describes the same process in philosophical and functional terms. The liver is considered the home of Pitta Dosha, and particularly of Ranjaka Pitta, the sub-type responsible for blood purification and transformation of food essence into energy (5, 7, 9). When Agni (digestive fire) is weak, food is not properly digested, leading to the formation of Ama—toxic residues that circulate through the Rasavaha and Raktavaha Srotas (nutrient and blood channels). These toxins accumulate in the Yakrit (liver), blocking microchannels and producing metabolic stagnation (7, 9, 11).
This blockage is known as Srotorodha in Ayurveda and directly parallels the modern concept of impaired lipid oxidation and mitochondrial dysfunction in hepatic steatosis (6, 7). Once the balance of Pitta and Meda Dhatu (fat tissue) is disturbed, excess fat begins to infiltrate the liver, while inflammation arises from oxidative injury. Both systems agree that restoring liver fire and clearing blockages are key to reversing this process.
When the liver becomes weak, unprocessed metabolic waste and Ama remain in circulation, causing fatigue, mental fog, and dull skin tone. The disturbed Ranjaka Pitta fails to maintain the vibrancy of Rakta Dhatu, resulting in reduced vitality and poor digestion. This is why Ayurveda connects liver health not only with digestion but also with mood and mental clarity (7, 11, 18).
Stages of Fatty Liver

Fatty liver disease evolves through specific stages that mark how fat, inflammation, and scarring develop inside the liver over time. Each stage reflects the balance between liver damage and regeneration, and understanding these changes helps guide treatment both in modern medicine and in Ayurveda.
1. Simple Steatosis (Fatty Liver) – corresponds to Grade 1–2
In this early phase, small droplets of fat accumulate inside the hepatocytes, but the liver still functions normally. Fat infiltration is mild (Grade 1) when less than one-third of liver cells are affected and moderate (Grade 2) when up to two-thirds are involved. This stage usually causes no pain or visible symptoms, although patients may notice bloating, heaviness, or mild fatigue.
According to Ayurveda, this corresponds to the early stage of Meda Vriddhi (increased fat tissue) and Agni Mandya (sluggish metabolism). Weak digestive fire produces Ama (toxic waste), which blocks Rasavaha Srotas (nutrient channels) and the Yakrit (liver). Simple steatosis is completely reversible through correction of diet, detoxification (Virechana), and use of herbs such as Katuki (Picrorhiza kurroa), Kalmegh (Andrographis paniculata), and Punarnava (Boerhaavia diffusa) (5, 6, 7, 8, 9, 11, 19).
2. Steatohepatitis (NASH or MASH) – inflammation and hepatocyte injury (can include Grade 2–3)
If fat accumulation continues, it leads to inflammation and oxidative stress within liver cells, producing a condition known as Steatohepatitis. Here, the liver becomes enlarged, tender, and develops microscopic ballooning of hepatocytes (Grade 3). This inflammation is the body’s attempt to defend itself but ultimately causes damage.
In Ayurveda, this stage reflects aggravated Pitta Dosha interacting with Meda Dhatu and Ama, resulting in heat and inflammation inside the liver, described as Yakrit Dushti (liver vitiation). The metabolic fire becomes erratic, leading to incomplete fat processing and tissue injury. If left untreated, this stage can advance into fibrosis (6, 8, 10, 11, 14, 15).
3. Fibrosis – scar tissue formation around veins and lobules
Persistent inflammation causes the body to form fibrous connective tissue in an attempt to repair damaged liver cells. This scar tissue surrounds blood vessels and lobules, reducing oxygen supply and disturbing bile flow. Fibrosis marks the transition from a reversible to a potentially chronic stage of the disease.
Ayurvedically, this corresponds to partial obstruction of Srotas (microchannels), reducing nutrient flow and oxygenation to the Yakrit. The condition parallels Granthi formation—a nodular hardening described in texts when Ama and Meda stagnate due to chronic Pitta-Kapha imbalance (8, 14, 15, 19).
4. Cirrhosis – complete architectural distortion and loss of function
Over years of fibrosis, the healthy architecture of the liver collapses, forming thick scar tissue and regenerative nodules. This leads to cirrhosis, where liver function is severely compromised. The organ becomes shrunken, hard, and unable to filter blood or synthesize proteins efficiently. Patients may experience jaundice, ascites (fluid accumulation), weakness, and mental confusion due to toxins entering the bloodstream (8, 35).
In Ayurveda, this final stage aligns with Yakrit Shotha (swollen liver) and Kumbhakamala (obstructive jaundice). It represents depletion of Ojas (vital energy) and destruction of Agni, leading to multisystem failure. The Charaka Samhita explains that untreated Yakrit Vikara at this stage results in irreversible degeneration (32).
Both Ayurveda and modern hepatology agree that early recognition and treatment during Simple Steatosis or Steatohepatitis can prevent irreversible damage. Once fibrosis develops, therapies must focus on rejuvenation (Rasayana), enhancing Agni, and restoring Dhatu Samya (tissue balance) using mineral and herbal formulations that rebuild hepatocyte function and detoxify the system (19, 24).
Main Causes
Fatty liver disease develops when the balance between fat production and fat utilization inside the liver becomes disturbed. Instead of being broken down or exported, fat begins to accumulate within liver cells. This imbalance can result from multiple metabolic, dietary, hormonal, and lifestyle factors, often coexisting and amplifying each other.
1. Overnutrition and Poor Diet
Excessive consumption of refined carbohydrates, trans fats, and fructose-rich foods is one of the most prominent causes of fatty liver disease. When the diet contains more energy than the body can utilize, the liver begins converting this surplus into triglycerides. Over time, these fats accumulate in liver cells, leading to hepatocellular stress and metabolic dysfunction (10, 11, 29). Highly processed foods, deep-fried snacks, bakery items, sweetened beverages, and packaged juices disrupt insulin signaling, suppressing the liver’s ability to oxidize fat efficiently. In addition, fructose from soft drinks and high-fructose corn syrup directly increases hepatic de novo lipogenesis—the conversion of sugars into fats. Ayurveda parallels this understanding by attributing excessive Madhura Rasa (sweet taste) and Snigdha Ahara (oily, heavy foods) as causes of Meda Dhatu Vriddhi (fat tissue overgrowth) and Ama accumulation. Overeating, especially before previous meals are digested, further weakens Agni (digestive fire) and blocks Rasavaha Srotas (nutrient channels). Modern and Ayurvedic evidence thus converge on the same conclusion: improper dietary habits are the most critical factor driving fatty liver disease.
2. Obesity and Insulin Resistance
Obesity creates a biochemical environment of chronic low-grade inflammation that disrupts fat metabolism. When the body’s tissues become resistant to insulin, glucose uptake decreases, forcing the liver to convert excess sugar into fat. This mechanism—known as insulin resistance—is central to the development of non-alcoholic fatty liver disease. Adipose tissue releases inflammatory cytokines such as TNF-alpha and interleukins, which impair mitochondrial function in hepatocytes and increase oxidative stress (8, 10). Over time, this leads to hepatic steatosis, inflammation, and fibrosis. Ayurveda explains this through the concept of Meda Vriddhi (fat tissue accumulation) and Kapha-Pitta Dushti (dual dosha imbalance). Obese individuals, particularly those with a Kapha-Pitta Prakriti, are predisposed to sluggish metabolism, weak Agni, and accumulation of Ama in the Yakrit (liver). The resulting Srotorodha (microchannel blockage) mirrors the modern understanding of disrupted lipid transport and insulin signaling. Early lifestyle correction—balanced diet, physical activity, and digestive-strengthening herbs such as Trikatu and Guduchi—can prevent the progression from simple steatosis to steatohepatitis. Both systems affirm that reversing insulin resistance is crucial for restoring normal hepatic metabolism.
3. Alcohol Consumption
Alcohol metabolism overwhelms liver enzymes, producing toxic intermediates like acetaldehyde and reactive oxygen species (ROS). These compounds directly damage hepatocyte membranes, impair mitochondrial function, and cause inflammation. Even moderate drinking over long periods can reduce hepatic fatty acid oxidation and promote triglyceride accumulation (6, 8). Chronic intake also increases gut permeability, allowing endotoxins to enter the bloodstream, which further stimulates liver inflammation. From an Ayurvedic standpoint, Madyapana (excessive alcohol consumption) is classified as a major Aharaja Nidana (dietary cause) for Yakrit Vikara (liver disorders). Alcohol aggravates Pitta Dosha, producing internal heat and dryness, which burns Ojas (vital essence) and impairs Agni (digestive fire). The result is toxic accumulation (Ama Janya Pitta Dushti) that damages Rasa and Rakta Dhatus (nutrient and blood tissues). Ayurveda also warns that long-term alcohol consumption leads to Kumbhakamala (obstructive jaundice) and Yakrit Shotha (liver swelling). Both disciplines agree that abstaining from alcohol is the most effective measure to prevent progression to cirrhosis. Clinical evidence supports that alcohol cessation can reverse steatosis within weeks, provided fibrosis has not yet developed.
4. Sedentary Lifestyle
Physical inactivity slows down metabolism and reduces the body’s capacity to burn fat. A sedentary lifestyle diminishes insulin sensitivity, increases triglyceride synthesis, and leads to weight gain—all risk factors for fatty liver (10, 25). Prolonged sitting, lack of exercise, and erratic sleep patterns also contribute to metabolic inflexibility, where the body can no longer efficiently switch between burning carbohydrates and fats for energy. Regular aerobic activity, yoga, and resistance training have been proven to decrease hepatic fat content by improving mitochondrial function and insulin response. Ayurveda emphasizes Vihara Nidana (lifestyle causes) as equally important as diet in the pathogenesis of Meda Roga (fat-related diseases). Daytime sleeping, lack of movement, suppression of natural urges, and irregular eating habits weaken Agni and promote Kapha Dosha accumulation, causing heaviness, sluggishness, and fatty deposition in the Yakrit (7, 9, 11). Classical texts recommend daily Vyayama (exercise), Abhyanga (oil massage), and Ushnodaka Pana (warm water drinking) to prevent stagnation of metabolic waste. Thus, both modern and Ayurvedic medicine highlight that movement and metabolic activation are essential for preventing fatty liver.
5. Diabetes and Metabolic Syndrome
Type 2 diabetes, hypertension, and hyperlipidemia often coexist as part of metabolic syndrome—a cluster of conditions that profoundly affects liver health. Insulin resistance, central obesity, and dyslipidemia increase the liver’s exposure to free fatty acids and inflammatory cytokines. Over time, this promotes steatosis, inflammation, and fibrosis, even in non-alcoholic individuals (10, 11, 15). Modern studies show that nearly 70% of diabetic patients have some form of fatty liver disease. Ayurveda interprets this as Madhumeha Janya Yakrit Dushti—liver dysfunction secondary to deranged sugar metabolism. In this state, Pitta and Kapha aggravation lead to excessive Kleda (moist metabolic waste) and Ama production, obstructing the Rasavaha Srotas and reducing liver efficiency (5, 7, 9, 11). Uncontrolled diabetes also weakens Ojas and Agni, leading to fatigue and poor digestion. Ayurvedic management focuses on restoring Agni and balancing Kapha through herbs like Gudmar (Gymnema sylvestre) and Triphala. Modern management emphasizes glycemic control and lifestyle modification, showing the complementary alignment of both systems.
6. Hormonal and Genetic Factors
Hormonal imbalances significantly influence liver metabolism. Polycystic ovary syndrome (PCOS), thyroid disorders, and menopause alter lipid regulation and promote hepatic fat storage (10, 11, 15). In PCOS, insulin resistance and elevated androgen levels trigger fat accumulation, while hypothyroidism slows metabolism, leading to sluggish bile secretion and poor fat digestion. Genetic variations such as the PNPLA3 and TM6SF2 polymorphisms further increase susceptibility to fatty liver disease, even in individuals with normal body weight. Ayurveda recognizes Beeja Dosha (genetic predisposition) and Prakriti (constitutional body type) as key determinants of disease vulnerability. Individuals with Kapha-Pitta Prakriti are more prone to Meda Vriddhi and Yakrit Dushti due to their natural tendency toward fat retention and stronger internal heat. Hormonal imbalance in women is interpreted as disturbed Rasa Dhatu flow, leading to stagnation and metabolic blockages. Ayurvedic treatment emphasizes restoring endocrine balance through Rasayana herbs such as Ashoka, Shatavari, and Guduchi, along with lifestyle measures for hormonal regulation.
7. Medications and Toxins
Long-term use of certain drugs can contribute to fatty liver. Corticosteroids, tamoxifen, methotrexate, amiodarone, and antiviral agents interfere with mitochondrial beta-oxidation, leading to fat buildup inside hepatocytes. Industrial solvents, pesticides, and heavy metals like mercury and lead further impair hepatic detoxification enzymes, worsening fat retention (10, 11). These substances also induce oxidative stress, causing inflammation and fibrosis. Ayurveda identifies similar causative agents under Dravya Dushti substances that disturb Agni and generate Ama. Exposure to synthetic chemicals and heavy metals is said to aggravate Pitta Dosha and damage Rakta Dhatu (blood tissue), mirroring hepatotoxicity in modern science (5, 7, 9, 11, 18). Purification therapies such as Virechana (therapeutic purgation), Nasya (nasal detox), and use of Rasayana herbs help eliminate these toxins from the system. Modern medicine and Ayurveda thus converge on detoxification as a cornerstone for reversing drug induced hepatic steatosis. Preventive monitoring, clean diet, and awareness of medication side effects are vital to avoid chronic liver injury.
Common Symptoms You Should Not Ignore
Fatty liver disease often develops silently, showing few obvious signs until the condition becomes advanced. Recognizing early symptoms can help prevent severe liver damage and systemic complications. The manifestations are both physical and emotional, reflecting the deep connection between the liver, metabolism, and mental state in both modern medicine and Ayurveda.
Early Symptoms:
At the beginning, symptoms are subtle and easily overlooked. Patients may experience abdominal bloating, heaviness after meals, dull skin, tiredness, or brain fog. These signs indicate that the liver is struggling to metabolize nutrients and detoxify waste efficiently. The accumulation of fat within liver cells leads to mild inflammation and reduced energy conversion, which manifests as fatigue and sluggishness (6, 8, 10, 11).
Moderate Symptoms:
As the disease progresses, symptoms become more noticeable. Pain or discomfort in the right upper abdomen, nausea, loss of appetite, and a coated tongue may develop. Ayurveda interprets this stage as Mandagni (weak digestive fire) and Ama Utpatti (toxin formation), where metabolic residues begin circulating through the body, affecting digestion, skin, and mood (5, 7, 9, 11).
Severe Symptoms:
Advanced stages present with jaundice (yellowish eyes), fluid accumulation in the abdomen (ascites), persistent itching, and sometimes confusion or sleep disturbance due to toxin buildup in the brain. These correspond to Yakrit Shotha (liver swelling) and Kumbhakamala (obstructive jaundice) in Ayurveda (7, 9, 11, 32).
Ayurvedic Descriptions:
Ayurveda identifies symptoms such as Arochaka (loss of taste), Klama (fatigue), Mandagni (weak digestion), and Anga Gaurava (heaviness). These arise from an imbalance of Pitta and Kapha Doshas, leading to congestion in the Yakrit and poor circulation of Rasa Dhatu (nutrient plasma) (5, 7, 9, 11).
Emotional Link:
The liver is deeply tied to emotional health. Excess liver heat (Pitta aggravation) manifests as irritability, frustration, anger, or mood swings. In chronic stages, patients may experience apathy or depression due to energy stagnation. Balancing Pitta through calming herbs like Bhringraj, Aloe Vera, and Guduchi, along with relaxation practices, helps restore emotional equilibrium (7, 9, 18).
Diagnosis
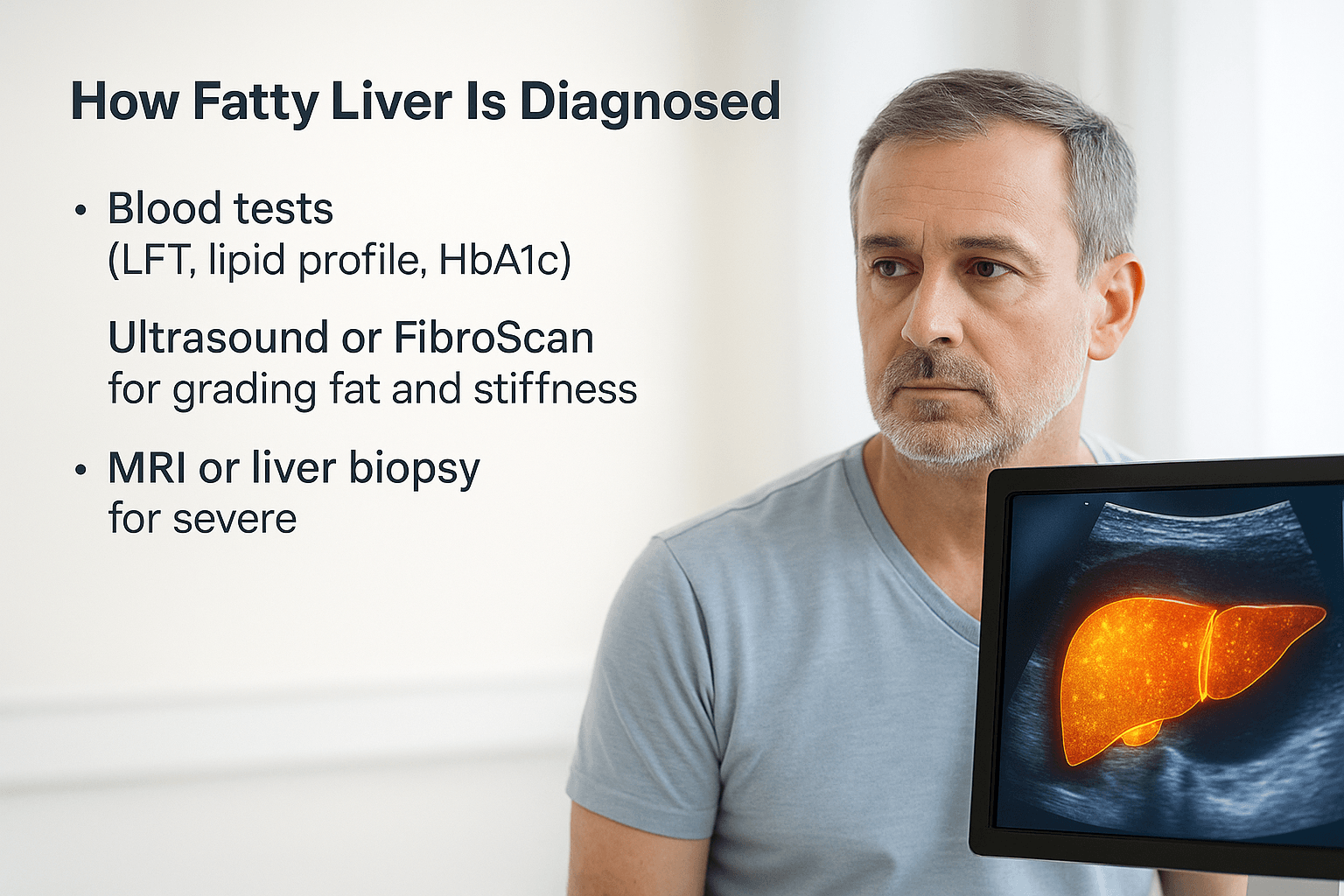
Fatty liver is often detected incidentally during routine health checkups because the early stages usually produce no clear symptoms. Modern diagnostic methods combine blood investigations, imaging techniques, and tissue analysis to confirm fat accumulation, inflammation, and liver stiffness. Ayurveda, meanwhile, assesses the condition through detailed evaluation of Agni, Dosha, Dhatu, and Srotas to understand the metabolic imbalance underlying the disease.
Blood Tests
The first step in evaluation involves basic liver function tests (LFT), which measure enzymes such as ALT (Alanine Transaminase) and AST (Aspartate Transaminase). Elevated levels of these enzymes suggest liver cell stress or inflammation. The lipid profile test helps determine cholesterol and triglyceride levels, which are often raised in fatty liver. Additionally, fasting blood sugar and HbA1c levels indicate insulin resistance, a common contributing factor. A complete blood count (CBC) and tests for viral hepatitis may also be performed to rule out other causes (6, 8, 10, 11, 15).
Ultrasound and FibroScan
Ultrasonography remains the most accessible and non-invasive tool to detect hepatic steatosis. It reveals a bright, echogenic liver texture compared to the kidneys, indicating fat infiltration. FibroScan (Transient Elastography) is a more advanced test that measures liver stiffness and quantifies fat content using controlled vibration waves. It helps grade the condition from mild fatty infiltration to advanced fibrosis or cirrhosis (8, 10, 14, 15).
MRI and Liver Biopsy
Magnetic Resonance Imaging (MRI) provides a highly accurate quantification of hepatic fat and can differentiate between simple steatosis and inflammation. When imaging and blood tests cannot determine the exact cause or stage, a liver biopsy may be performed. This involves taking a small tissue sample to assess cellular fat, inflammation, and fibrosis under the microscope. Although invasive, it remains the gold standard for definitive diagnosis and staging (8, 10, 15, 19).
In Ayurveda, diagnosis does not rely on machines but on comprehensive examination—Darshana (observation), Sparshana (palpation), and Prashna (patient inquiry). The physician assesses digestive strength (Agni), fat metabolism (Meda Dhatu), and signs of Ama accumulation such as coated tongue, heaviness, or altered taste perception. Pulse analysis (Nadi Pariksha) and eye inspection (Netra Pariksha) are also used to identify underlying Pitta-Kapha imbalance. Thus, while modern tests confirm the structural damage, Ayurvedic evaluation reveals the root metabolic disorder that must be corrected for true healing.
Ayurvedic Cure: Cleansing and Healing the Liver
Ayurveda approaches fatty liver not by suppressing symptoms but by eliminating the underlying cause metabolic toxins (Ama), weak digestive fire (Agni Mandya), and deranged Pitta and Kapha Doshas. The treatment aims to cleanse, restore, and rejuvenate the liver through a sequence of therapies known as Shodhana (detoxification), Shamana (pacification), and Rasayana (rejuvenation).
A. Detox (Shodhana Therapy)
Detoxification is the first and most essential step in Ayurvedic liver management. Virechana (therapeutic purgation) is the primary procedure to expel aggravated Pitta and Ama from the liver and intestines. It is carried out after preparatory therapies such as Snehapana (internal oleation) and Swedana (sudation). In obese or Kapha-dominant individuals, Vamana (therapeutic emesis) is performed to clear excess fat and mucus from the Medovaha Srotas (fat channels). Basti (medicated enema) is used to purify the lower channels, supporting fat metabolism and improving bile flow. In patients with elevated bilirubin or yellow eyes, Raktamokshana (bloodletting) may be administered selectively to relieve Pitta congestion and detoxify the blood (5, 7, 9, 11).
B. Herbal Medicines and Formulations
Herbal hepatoprotective medicines form the backbone of Ayurvedic liver care. Katuki (Picrorhiza kurroa) acts as a powerful bile regulator and liver stimulant, while Kalmegh (Andrographis paniculata) shields hepatocytes from oxidative damage. Punarnava (Boerhaavia diffusa) reduces inflammation and water retention, and Bhumyamalaki (Phyllanthus niruri) aids toxin removal and regeneration. Triphala and Guggulu optimize fat metabolism, improve digestion, and clear metabolic waste. These herbs are often combined in decoctions, powders, or Avaleha (herbal jam) forms to deliver synergistic results. Their collective actions rejuvenate Agni, cleanse Meda Dhatu, and normalize liver function, validated by both classical texts and modern hepatology research (6, 8, 10, 11, 15, 19, 24).
C. Rasayana (Rejuvenation Therapy)
After detoxification, Rasayana therapy nourishes and rebuilds liver cells. The Liver Rasayana Avaleha, prepared with Katuki, Punarnava, Kalmegh, and Bhumyamalaki, is prescribed in doses of 15 g twice daily for 30 days. This preparation revitalizes Agni, repairs hepatic tissues, and restores metabolic intelligence. Abhrak Bhasma and Tamra Bhasma support bile secretion and detoxification, while Swarna Makshik Bhasma improves enzyme balance and enhances immunity. In cases of advanced fibrosis or cirrhosis, Heerak Bhasma (Diamond ash) may be cautiously included under expert supervision. Each formulation is customized according to Prakriti (body constitution) and disease stage. Ayurveda also prescribes diet regulation, yoga, and meditation to sustain liver vitality and prevent recurrence (5, 7, 9, 11, 15, 19, 24).
Liver Rasayana Avaleha (Main Medicine To Cure)
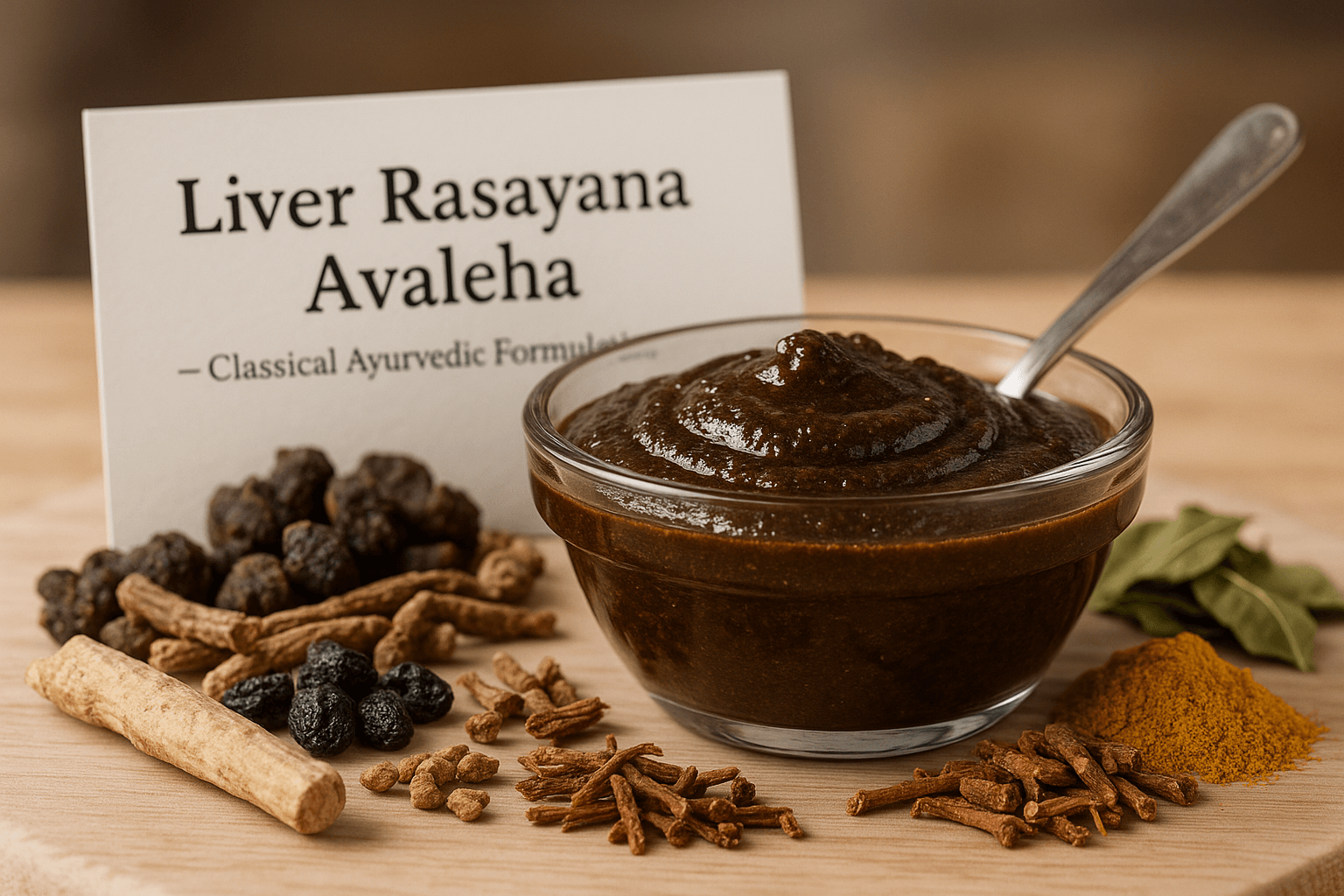
The Liver Rasayana Avaleha is a classical polyherbal and herbo-mineral preparation derived from Charaka Samhita (Chikitsa Sthana 1/1–4), Rasendra Sara Sangraha (Yakrit Rogadhikara), and Bhavaprakasha Nighantu (Rasayana Adhyaya). It is specially formulated to purify Rasavaha and Raktavaha Srotas, dissolve excess Meda Dhatu, enhance Pitta balance, and restore liver metabolism. This powerful Rasayana acts as a complete solution for Yakrit Vriddhi, Meda Roga, Kumbhakamala, and Yakrit Shotha (fatty liver, inflammation, or fibrosis).
Ingredients and Weight (for 30 Days Course)
Katuki (Picrorhiza kurroa) – 200 g
Punarnava (Boerhaavia diffusa) – 150 g
Kalmegh (Andrographis paniculata) – 150 g
Bhumyamalaki (Phyllanthus niruri) – 150 g
Triphala (Haritaki, Bibhitaki, Amalaki) – 200 g
Guggulu (Commiphora mukul) – 100 g
Guduchi (Tinospora cordifolia) – 100 g
Daruharidra (Berberis aristata) – 100 g
Yashtimadhu (Glycyrrhiza glabra) – 100 g
Mandur Bhasma (Iron oxide calx) – 10 g
Abhrak Bhasma (Purified mica calx) – 5 g
Tamra Bhasma (Copper calx) – 5 g
Swarna Makshik Bhasma (Gold-copper-iron pyrite calx) – 3 g
Heerak Bhasma (Diamond ash, optional for advanced fibrosis) – 1 g
Shilajit (Asphaltum purified) – 20 g
Nimbapatra Churna (Azadirachta indica) – 50 g
Kutki Satva (concentrate) – 20 g
Trikatu (Pippali, Maricha, Shunthi) – 50 g
Pippalimula (Piper longum root) – 30 g
Aloe vera pulp (Kumari Ras) – 100 ml
Bhavana Dravya (liquid medium) – Decoction of Punarnava, Katuki, and Guduchi – 1.5 liters
Base – Jaggery – 1 kg
Ghee – 200 g
Honey – 100 g (added post cooling)
Preparation Method
Kwatha (decoction) Coarsely powder the crude herbs (Katuki, Punarnava, Kalmegh, Bhumyamalaki, Guduchi, Daruharidra) and boil in water equal to ~8× total herb weight. Reduce to 1/4 and filter warm to obtain a clear kwatha.
Base and Avaleha paka Melt jaggery separately, then combine with the filtered kwatha and cook on gentle heat, stirring continuously. Add ghee during this concentration step. Continue till Avaleha paka (thick, jam-like) is reached as per classical tests (tantu-pāka/thread test). Take off heat.
Mandatory cooling before adding actives Allow the hot Avaleha to cool naturally to 40 °C (lukewarm). Use a food-grade thermometer. Do not add any bhasma or honey above 40 °C.
Addition of powders at ≤40 °C At 40 °C, add the fine churna of Triphala, Trikatu, Pippalimula, Guggulu and the standardized extracts (e.g., Kutki satva). Mix thoroughly.
Incorporation of herbo-mineral actives at ≤40 °C At 38–40 °C, add Mandur Bhasma, Abhrak Bhasma, Tamra Bhasma, Swarna Makshik Bhasma, and (only when clearly indicated) Heerak Bhasma. Fold in slowly to avoid lumping and to preserve intended pharmaceutics per rasa-shastra norms. Dissolve purified Shilajit at the same temperature.
Bhavana (trituration) Give 3–7 bhavana cycles with Punarnava-Katuki-Guduchi kwatha (room-temperature), each cycle 20–30 minutes, to ensure uniform dispersion and potentiation without raising temperature above 40 °C.
Dosage and Duration
Take 15 grams twice daily (morning and evening) after meals with lukewarm water or honey for 30 days. For chronic conditions, treatment may be extended under medical supervision.
Therapeutic Actions
This Avaleha works as a Yakrit Rasayana enhancing bile secretion, restoring enzymatic function, and dissolving accumulated fat and toxins. Katuki and Kalmegh regulate Pitta and improve bile flow; Punarnava and Bhumyamalaki detoxify and rejuvenate liver cells; Mandur, Tamra, and Swarna Makshik Bhasma correct anemia, stimulate metabolism, and strengthen hepatocytes. Abhrak and Shilajit act as adaptogens, restoring vitality, while Triphala, Guggulu, and Trikatu enhance fat digestion and remove Ama.
Precaution and Warning
The formulation may vary based on multiple factors such as age, gender, body constitution (Prakriti), health condition, metabolic strength (Agni), severity and stage of liver disease (steatosis, fibrosis, or cirrhosis), presence of comorbidities like diabetes or hypertension, and response to detox therapy. The ratio of herbs and minerals may be modified by a qualified Ayurvedic physician accordingly.
- Patients with severe hepatic failure, pregnancy, lactation, or advanced cirrhosis should use this under strict medical supervision.
- Avoid spicy, oily, and fermented foods, as well as alcohol and late-night eating.
- Maintain regular physical activity, hydration, and timely meals.
- Ghee and mineral dosages must be reduced in high Kapha or obese patients and increased slightly in Vata-Pitta individuals with low body weight.
- In cases of chronic jaundice or fibrosis, Heerak Bhasma and Tamra Bhasma may be added cautiously.
Mode of Action (Ayurvedic and Modern View)
This formulation enhances Agni, purifies the blood, rejuvenates Rasa and Rakta Dhatus, and clears blockages in Medovaha and Rasavaha Srotas. On a modern level, it supports hepatocellular regeneration, enhances bile flow, regulates lipid metabolism, reduces inflammation, and provides antioxidant protection against free radicals.
Clinical Benefit
Improves liver enzyme profile, reduces fatty infiltration, enhances digestion, relieves heaviness, normalizes appetite, and restores overall vitality within 30 days of continuous use.
References: Charaka Samhita – Chikitsa Sthana 1/1–4; Bhavaprakasha Nighantu – Rasayana Adhyaya; Rasendra Sara Sangraha – Yakrit Rogadhikara; Rasatarangini – Taranga 24; Bhaishajya Ratnavali – Yakrit Rogadhikara; Journal of Ethnopharmacology (2020); AYU Journal (2017); Ancient Science of Life (2020).
Frequently Asked Questions
1. What exactly is fatty liver disease?
Fatty liver disease occurs when excess fat builds up inside the liver cells, affecting how the organ detoxifies, digests, and regulates metabolism. When more than 5% of liver tissue contains fat, it is termed hepatic steatosis. It may occur in people who do not drink alcohol (non-alcoholic fatty liver disease, NAFLD) or those who consume excessive alcohol (alcoholic fatty liver disease, AFLD).
2. Can fatty liver happen without alcohol?
Yes. Non-alcoholic fatty liver disease (NAFLD) is now one of the world’s fastest-growing metabolic disorders, often linked with poor diet, obesity, and insulin resistance. It can affect even non-drinkers with sedentary lifestyles or high-sugar diets.
3. How does Ayurveda explain fatty liver?
Ayurveda recognizes fatty liver as Yakrit Vriddhi and Medoroga, conditions where excess fat and toxins accumulate due to weak digestive fire (Agni Mandya) and imbalanced Pitta and Kapha Doshas. It describes liver congestion as a result of Ama (metabolic waste) blocking Rasa and Rakta Dhatus, leading to sluggish metabolism and dullness.
4. What are the early signs of fatty liver?
Most early stages are silent. Subtle symptoms like bloating, heaviness after meals, fatigue, dull skin, and mental fog may appear. Ayurveda also lists Arochaka (loss of taste), Klama (fatigue), Mandagni (weak digestion), and Anga Gaurava (heaviness in limbs) as early warning signs.
5. Is fatty liver reversible?
Yes, in most cases, fatty liver is completely reversible through detoxification, diet correction, herbal Rasayana therapy, and lifestyle changes. Ayurveda focuses on removing toxins, improving liver metabolism, and regenerating hepatic tissue naturally.
6. How does stress affect the liver?
Stress increases cortisol and adrenaline, which alter glucose and fat metabolism. This leads to increased fat deposition in the liver. In Ayurvedic understanding, mental stress aggravates Pitta and Vata, disturbing Ranjaka Pitta (the metabolic energy in the liver).
7. How common is fatty liver worldwide?
It is estimated that nearly one in three adults globally have some form of fatty liver. The condition is rapidly increasing among young adults due to processed foods, alcohol, lack of sleep, and exposure to synthetic chemicals.
8. Can people with normal weight get fatty liver?
Yes, lean individuals can also develop fatty liver if they have poor digestion, high sugar intake, or stress-induced hormonal imbalance. Ayurveda explains this as Meda Dushti without obesity — where internal fat metabolism is disturbed even if the external body weight appears normal.
9. How does Ayurveda treat fatty liver?
Ayurveda treats fatty liver through three stages: Shodhana (cleansing through Virechana, Vamana, and Basti), Shamana (balancing Doshas with herbal medicines), and Rasayana (rejuvenation using formulations like Liver Rasayana Avaleha). The treatment restores Agni, removes Ama, and repairs liver tissue.
10. Is fatty liver dangerous if untreated?
If ignored, fatty liver can progress to non-alcoholic steatohepatitis (NASH), fibrosis, and eventually cirrhosis or liver cancer. Early intervention with herbal detox, dietary control, and lifestyle balance can prevent this progression and restore complete liver health.