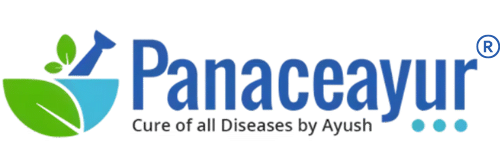
Endometriosis is a chronic, progressive gynecological disorder characterized by the growth of endometrial-like tissue outside the uterine cavity. This tissue behaves much like the normal endometrium—thickening, breaking down, and bleeding with each menstrual cycle—but since it is located outside the uterus, the blood has no way to exit the body. This results in inflammation, scar tissue formation, and the development of painful adhesions [1].
The condition affects an estimated 10% of women in their reproductive years worldwide, making it one of the most common causes of chronic pelvic pain and infertility in women of childbearing age [2]. Despite its prevalence, awareness remains low, and the average delay in diagnosis can range from 7 to 10 years after the first onset of symptoms. This delay often worsens disease progression and has a profound effect on quality of life [3].
Women with endometriosis often experience severe menstrual pain, heavy bleeding, pain during sexual intercourse, and fatigue, but the spectrum of symptoms can vary widely. Some women may remain asymptomatic, while others face debilitating pain and infertility. Beyond physical health, the condition has significant psychological and social impacts, including anxiety, depression, and reduced work productivity [4].
From an Ayurvedic perspective, endometriosis can be understood through the lens of Udavarta Yonivyapad (a disorder caused by the upward or reverse flow of menstrual blood due to vitiated Vata) and Artava Dushti (abnormalities in menstrual flow and quality). These classical descriptions emphasize the importance of balanced Apana Vata—the downward-moving force responsible for menstruation and elimination. When Apana Vata is disturbed, along with Pitta dosha (inflammation) and Kapha dosha (excess growth and adhesions), the menstrual process becomes impaired [5].
Additionally, the role of digestive imbalance (Agnimandya) and toxin accumulation (Aama) is central in Ayurveda. Improper diet, stress, and lifestyle contribute to the formation of Aama, which circulates through the body and lodges in the reproductive channels (Artavavaha Srotas), creating blockages (Srotorodha). This obstructs normal flow, causes inflammation, and manifests as painful and irregular menstruation [6].
Thus, while modern medicine describes endometriosis in terms of misplaced tissue, immune dysfunction, and hormonal imbalances, Ayurveda offers a holistic framework linking digestion, toxins, and the subtle balance of energies in the body. This integrative understanding not only addresses symptoms but also the root causes, giving a broader approach to both treatment and prevention [7].
Causes and Risk Factors
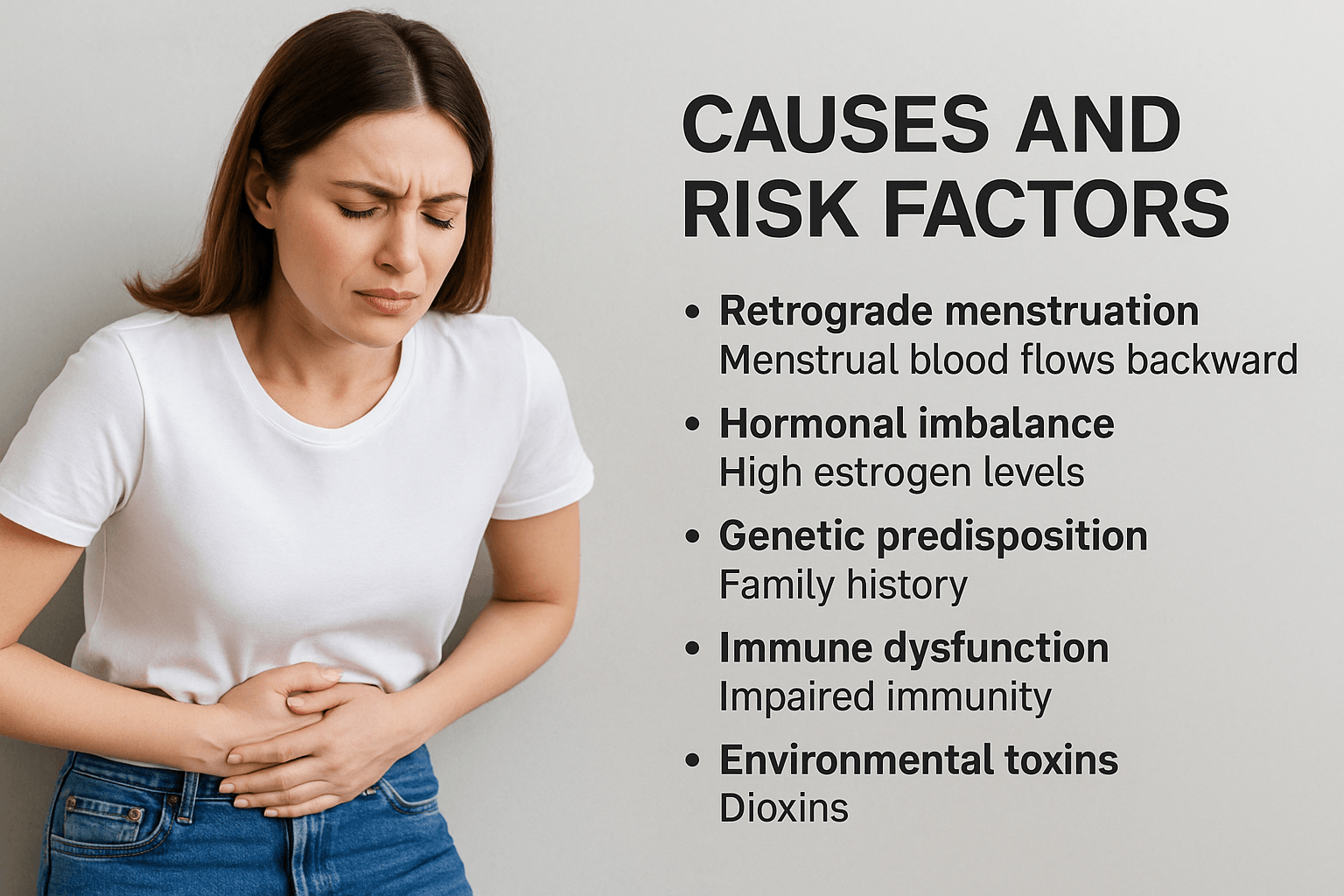
Although endometriosis has been studied for decades, its exact cause remains elusive. Current research suggests it is a multifactorial condition involving retrograde menstruation, hormonal influences, immune system dysfunction, and environmental triggers. Ayurveda provides additional insights, linking the disorder to imbalances in digestion, toxins, and reproductive channels.
Retrograde menstruation
One of the most widely accepted theories is retrograde menstruation, where menstrual blood containing endometrial cells flows backward through the fallopian tubes into the pelvic cavity rather than leaving the body. These displaced cells can implant onto pelvic organs, grow, and bleed with each cycle, causing inflammation and scarring [1]. However, not all women with retrograde flow develop endometriosis, which means other mechanisms also play a role.
Hormonal imbalance
Endometriosis is an estrogen-dependent condition. Elevated estrogen levels promote the survival and growth of endometrial-like tissue outside the uterus. Estrogen enhances angiogenesis (blood vessel growth) and stimulates local inflammation, which sustains lesions and adhesions [2]. Progesterone resistance—where endometrial tissue does not respond properly to progesterone—also worsens the imbalance.
Genetic predisposition
Family and twin studies show a strong hereditary component. Women with a mother or sister diagnosed with endometriosis are at higher risk of developing the condition themselves [3]. Researchers have identified genetic variations linked to immune response, estrogen metabolism, and inflammation pathways, all of which may contribute to susceptibility.
Immune dysfunction
Normally, the immune system identifies and destroys misplaced endometrial cells. In endometriosis, however, this defense mechanism is impaired. Dysfunctional immune responses allow endometrial implants to survive and spread. Studies show increased inflammatory cytokines, defective natural killer cells, and abnormal T-cell activity in women with endometriosis [4]. This chronic immune imbalance perpetuates pain and tissue damage.
Environmental toxins
Exposure to certain chemicals has been linked to endometriosis risk. Dioxins, PCBs, and other endocrine-disrupting pollutants can mimic estrogen and interfere with hormonal signaling. These toxins promote oxidative stress and chronic inflammation, creating an environment favorable for endometrial lesion growth [5]. Modern studies suggest that women with higher levels of such toxins may experience more severe disease.
Ayurvedic perspective
Ayurveda views endometriosis as a disorder rooted in dosha imbalance. The primary culprits are Vata and Pitta. Disturbed Apana Vata (the downward-moving energy governing menstruation) causes irregular or painful flow, while aggravated Pitta fuels inflammation and abnormal tissue growth. Kapha contributes by stabilizing adhesions and cystic masses.
Underlying this process is Agnimandya (weak digestive fire), which leads to the formation of Aama (metabolic toxins). Aama circulates in the bloodstream, contaminating the reproductive tissues (Artavavaha Srotas). This results in Rakta Dushti (impure blood) and Srotorodha (blockage of microchannels), which mirror the modern concepts of immune dysfunction and adhesions [6].
Ayurvedic texts emphasize that improper diet, sedentary lifestyle, stress, and suppressed natural urges worsen these imbalances. In this way, both ancient wisdom and modern science agree: endometriosis is not caused by a single factor, but by a complex interplay of genetics, immunity, hormones, environment, and lifestyle.
Symptoms
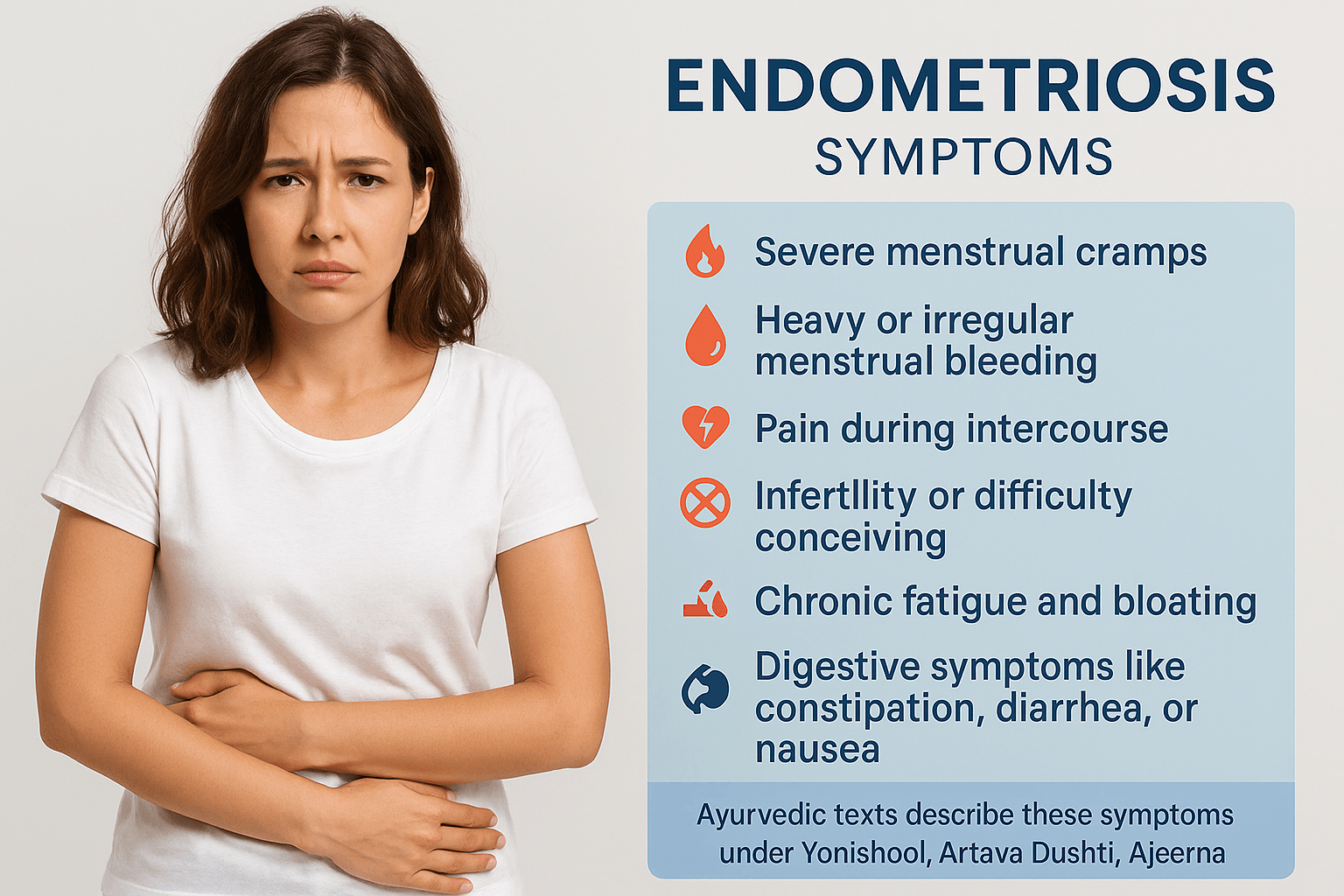
Endometriosis is often called a “silent disruptor” because it manifests differently in every woman. While some experience debilitating symptoms, others remain asymptomatic and only discover the condition when facing fertility challenges. This diversity makes endometriosis a complex and frequently misdiagnosed disease [1].
Severe Menstrual Cramps (Kashta Artava)
One of the hallmark features of endometriosis is intense menstrual pain, far beyond what most women experience during a normal cycle. This pain often begins a few days before menstruation, peaks during the period, and can persist afterward. It may radiate to the lower back, pelvis, and thighs, sometimes strong enough to interfere with daily activities or even cause missed school or work days [2].
In Ayurveda, this pain is recognized as Kashta Artava, linked to aggravated Apana Vata. Disturbed Vata dosha disrupts the smooth downward flow of menstrual blood, leading to spasmodic pain and irregular flow.
Heavy or Irregular Menstrual Bleeding (Artava Dushti)
Many women with endometriosis suffer from heavy menstrual bleeding (menorrhagia) or irregular cycles. Periods may last longer than a week and involve large clots. In some cases, spotting occurs between cycles. This excessive blood loss can lead to secondary conditions such as iron-deficiency anemia, fatigue, and pallor [3].
Ayurveda categorizes this as Artava Dushti, a state of vitiated menstrual flow arising from Pitta aggravation (inflammation, heat) and Rakta Dushti (impurity in blood).
Pain During Intercourse (Dyspareunia)
Endometriotic lesions located behind the uterus, near the vagina, or in the recto-vaginal pouch can cause deep pelvic pain during or after sexual intercourse. This pain, known as dyspareunia, is not only physically distressing but also has emotional and relational consequences, often leading to anxiety about intimacy and strained partnerships [4].
Ayurvedic interpretation associates this with Yonishool (pelvic pain disorders) caused by imbalances in Vata and Kapha, which obstruct natural lubrication and cause tissue tenderness.
Infertility or Difficulty Conceiving
Endometriosis is one of the leading causes of infertility, affecting up to 30–50% of women with the condition. Adhesions and scar tissue may distort pelvic anatomy, block fallopian tubes, or interfere with egg release from the ovaries. Additionally, inflammation and altered immune activity create a hostile environment that impairs fertilization and implantation [5].
Ayurveda describes this as Beeja Dushti (defects in reproductive tissue) and Srotorodha (obstruction in reproductive channels). Long-term presence of Aama (toxins) and Rakta Dushti can further damage the delicate balance required for conception.
Chronic Fatigue and Bloating
The systemic inflammatory response of endometriosis does not remain confined to the pelvic cavity. Women often report persistent fatigue, low energy, and abdominal bloating, especially before and during menstruation. This bloating, often called “endo belly,” can cause visible abdominal distension, discomfort, and body image concerns [6].
From an Ayurvedic lens, this is due to disturbed Agni (digestive fire) and accumulation of Aama, which circulate through the channels and cause heaviness, lethargy, and swelling.
Digestive Symptoms
Endometriosis often involves the intestines, particularly in cases of deep infiltrating disease. As a result, women may experience constipation, diarrhea, nausea, abdominal cramps, and even painful bowel movements around menstruation. These gastrointestinal symptoms frequently lead to misdiagnosis as irritable bowel syndrome (IBS) [7].
Ayurvedic texts equate this to Ajeerna (indigestion) and Grahani dosha, where Vata and Pitta imbalance disrupts normal digestion and elimination.
Psychological and Emotional Symptoms
Beyond the physical manifestations, endometriosis exerts a heavy emotional toll. Chronic pain, fertility struggles, fatigue, and unpredictable flares contribute to anxiety, depression, mood swings, and social withdrawal. Studies confirm that women with endometriosis often have a lower quality of life compared to those with other chronic conditions [8].
Ayurveda emphasizes the role of Manasika doshas (Rajas and Tamas) in worsening perception of pain and emotional instability. Strengthening Sattva (clarity, calmness) through meditation, yoga, and supportive therapies is considered essential for comprehensive healing.
In summary, the symptoms of endometriosis span across gynecological, gastrointestinal, systemic, and psychological domains, making it a truly multidimensional disorder. Both modern science and Ayurveda agree that the burden of symptoms arises not from a single factor but from a complex interplay of inflammation, hormonal imbalance, immune dysfunction, and lifestyle-related disturbances.
Diagnosis
Diagnosing endometriosis is often a complex and delayed process, as its symptoms overlap with conditions like irritable bowel syndrome, pelvic inflammatory disease, or ovarian cysts. Many women face years of uncertainty before receiving a definitive diagnosis [1]. Both modern medicine and Ayurveda provide frameworks for identifying the disease, though their methods differ in approach.
Ultrasound and MRI
Modern non-invasive imaging techniques have become essential tools in the evaluation of endometriosis. Transvaginal ultrasound is particularly helpful in detecting ovarian cysts known as endometriomas, although it is less effective for identifying smaller or superficial lesions. Magnetic resonance imaging (MRI) provides a more detailed picture, especially for deep infiltrating endometriosis involving pelvic organs such as the rectum and bladder. These imaging modalities are often used together to help map the disease before surgical treatment [2].
Laparoscopy
For decades, laparoscopy has been regarded as the gold standard in diagnosing endometriosis. It allows direct visualization of lesions and adhesions in the pelvic cavity, while biopsies taken during surgery provide histological confirmation. However, newer guidelines recognize that diagnosis can often be made using a combination of symptoms and imaging, with laparoscopy reserved for severe or uncertain cases. This shift helps reduce unnecessary invasive procedures while still ensuring accuracy [3].
Blood Markers
Researchers continue to explore the possibility of using blood-based markers for non-invasive diagnosis. The most studied protein, CA-125, may be elevated in women with endometriosis, but its lack of sensitivity and specificity limits its reliability. Elevated levels are also found in ovarian cancer, pelvic infections, or fibroids. Emerging research on cytokines, microRNAs, and genetic markers offers hope, but none have yet replaced imaging or surgical confirmation as the primary diagnostic tools [4].
Ayurvedic Diagnosis through Nidan Panchaka
Ayurveda approaches diagnosis using the Nidan Panchaka system, a fivefold framework that looks beyond physical lesions to identify the root causes of disease.
- Hetu (Causes): Ayurveda emphasizes lifestyle, dietary patterns, and stress as key contributors. Habits such as irregular eating, excessive consumption of heavy or spicy foods, and suppression of natural urges aggravate Vata and Pitta doshas, setting the stage for disease.
- Linga (Signs and Symptoms): Pelvic pain, painful menstruation, heavy or irregular flow, bloating, fatigue, and digestive upsets are considered central clinical features.
- Samprapti (Pathogenesis): Endometriosis is understood as the result of disturbed Apana Vata (responsible for downward flow) combined with Agnimandya (weak digestion) and accumulation of Aama (toxins). These factors lead to Rakta Dushti (impure blood) and Srotorodha (blockage of channels).
- Upashaya (Therapeutic Response): Relief observed from herbal medicines, detoxification (Shodhana), and dietary modifications further confirms the diagnosis.
- Pratyaya (Confirmation): Integration of these findings provides a holistic confirmation, highlighting both symptomatic patterns and underlying imbalances.
By blending modern imaging and laboratory tools with Ayurvedic root-cause analysis, a more comprehensive diagnosis can be achieved. Modern medicine identifies the structural extent of endometriosis, while Ayurveda highlights the systemic imbalances that perpetuate the condition. Together, they create a balanced, patient-centered diagnostic approach.
Complications if Untreated
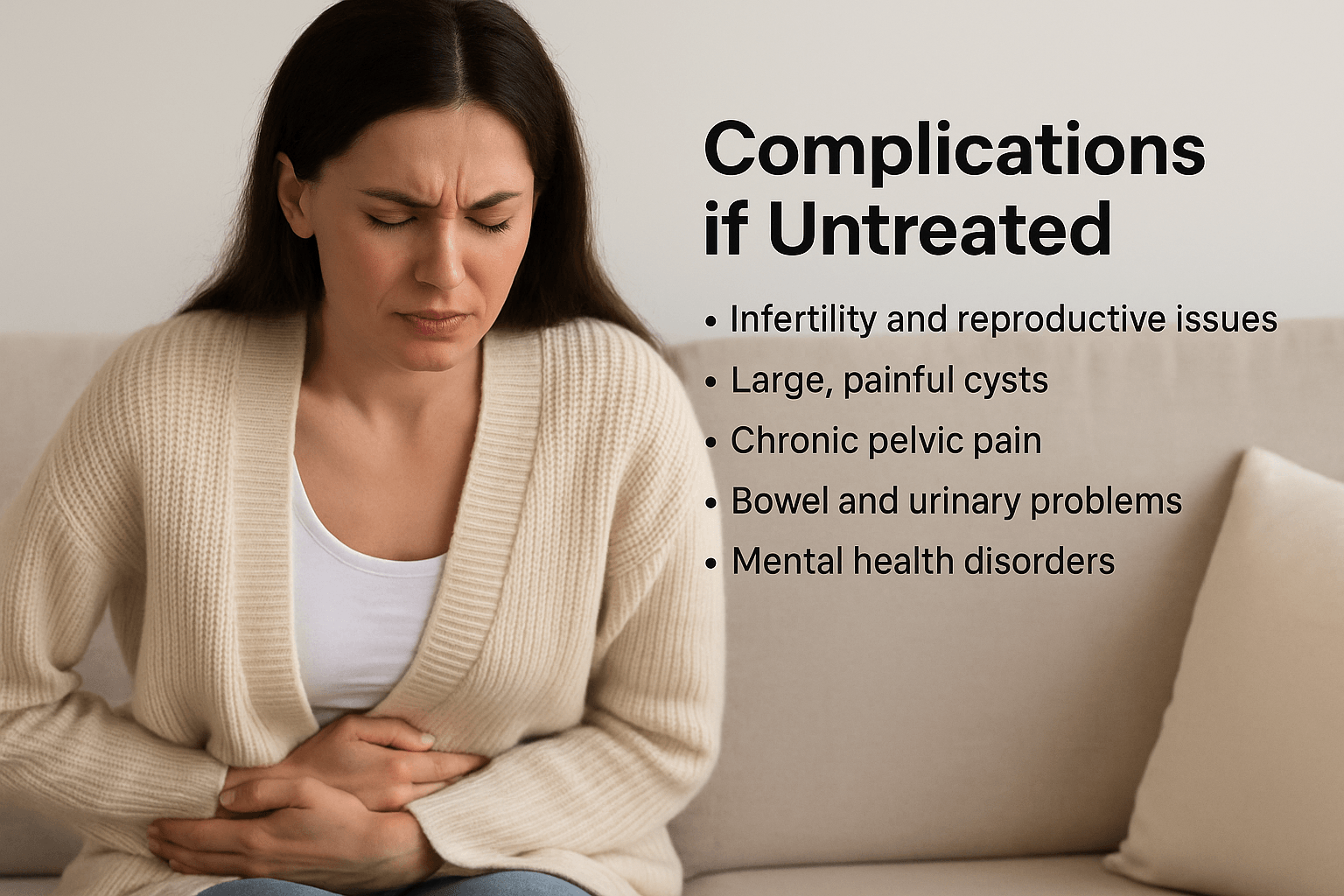
When endometriosis is left untreated, it does not remain a simple gynecological issue. Instead, it evolves into a multi-system disorder that can compromise fertility, pelvic health, immunity, digestion, and emotional well-being. The complications extend far beyond the reproductive system, influencing almost every aspect of a woman’s life.
Infertility and Subfertility
One of the most well-recognized complications is infertility, which affects up to 50% of women with advanced disease. Adhesions and scar tissue may distort the uterus, ovaries, and fallopian tubes, preventing the normal meeting of egg and sperm. Chronic inflammation within the pelvis creates an environment that is hostile to fertilization and embryo implantation. Even in cases where conception occurs, the risk of miscarriage, ectopic pregnancy, or implantation failure is higher than average [1].
From an Ayurvedic perspective, untreated endometriosis represents long-term Beeja Dushti (defective reproductive tissue) and Srotorodha (blockage of reproductive channels). The accumulation of Aama (toxins) and disturbed Apana Vata weakens the quality of ovum and the receptivity of the uterus.
Large Cyst Formation (Endometriomas)
A common progression is the formation of endometriomas, sometimes called “chocolate cysts” due to their dark, thick fluid content. These cysts can grow large, rupture, or twist the ovary (torsion), causing acute emergencies. Long-standing endometriomas also reduce ovarian reserve, leading to premature ovarian insufficiency and diminishing natural fertility [2].
In Ayurveda, these cysts mirror Granthi (tumor-like growths) within the Artavavaha Srotas (reproductive channels), aggravated by vitiated Kapha and Rakta.
Chronic Pelvic Pain and Adhesions
Untreated endometriosis often results in progressive scarring and adhesions. These fibrous bands bind pelvic organs together, leading to restricted mobility of the uterus, ovaries, and intestines. Women experience non-cyclic pelvic pain that persists beyond menstruation, worsening with bowel movements, urination, or intercourse. Over time, this leads to a chronic pain syndrome, severely impairing mobility, productivity, and intimacy [3].
Ayurveda describes this as Yonishool (persistent pelvic pain) caused by obstruction of channels (Srotorodha) and imbalance of Vata. If unresolved, it evolves into Asadhya Avastha (difficult-to-cure stage).
Digestive and Urinary Complications
When lesions spread to the intestines or bladder, women may face bowel obstruction, rectal bleeding, painful bowel movements, diarrhea, constipation, or painful urination. In severe cases, endometriotic nodules can perforate the bowel or obstruct ureters, causing hydronephrosis and kidney damage if untreated [4].
In Ayurveda, this reflects the extension of Aama and Rakta Dushti into neighboring systems, disturbing Purishavaha Srotas (intestinal channels) and Mutravaha Srotas (urinary channels).
Impact on Pregnancy and Obstetric Outcomes
Women with untreated endometriosis face higher risks of complications during pregnancy, including ectopic pregnancy, placental abnormalities, preterm birth, and increased need for cesarean delivery [5]. These risks add to the emotional burden of infertility and recurrent pregnancy loss.
Risk of Malignancy
Although rare, long-term endometriosis increases the risk of certain cancers, particularly ovarian clear cell carcinoma and endometrioid carcinoma. The lifetime risk is small, but higher compared to women without endometriosis. This highlights the importance of timely diagnosis and management [6].
Immune Dysfunction and Systemic Inflammation
Endometriosis is increasingly recognized as a systemic inflammatory disease, not just a localized pelvic condition. Untreated disease perpetuates chronic immune activation, increasing susceptibility to autoimmune disorders such as thyroid disease, lupus, and rheumatoid arthritis [7]. Persistent inflammation also contributes to fatigue and reduced resilience.
Ayurveda explains this as prolonged Agnimandya and Ojas kshaya (depletion of vital immunity), leading to vulnerability against multiple disorders.
Mental Health and Emotional Well-being
Living with untreated endometriosis has profound psychological consequences. Chronic pain, infertility, fatigue, and unpredictable flare-ups create emotional distress, often leading to anxiety, depression, poor body image, and relationship strain. Quality of life studies show women with endometriosis often report lower well-being scores than those with diabetes or asthma [8].
Ayurveda attributes this to disturbances in Manasika doshas (Rajas and Tamas), which amplify pain perception and emotional instability. Restoring Sattva (clarity and calmness) through meditation, yoga, and mind-body balance is therefore essential.
In-Short
If left untreated, endometriosis progresses beyond menstrual pain to cause infertility, organ damage, digestive and urinary complications, chronic inflammation, mental health challenges, and even cancer risks. Modern medicine emphasizes the structural and immune complications, while Ayurveda highlights the root imbalance of doshas, toxins, and channel obstructions. Together, they underscore why early diagnosis and treatment are vital to prevent irreversible complications.
Ayurvedic Cure and Management
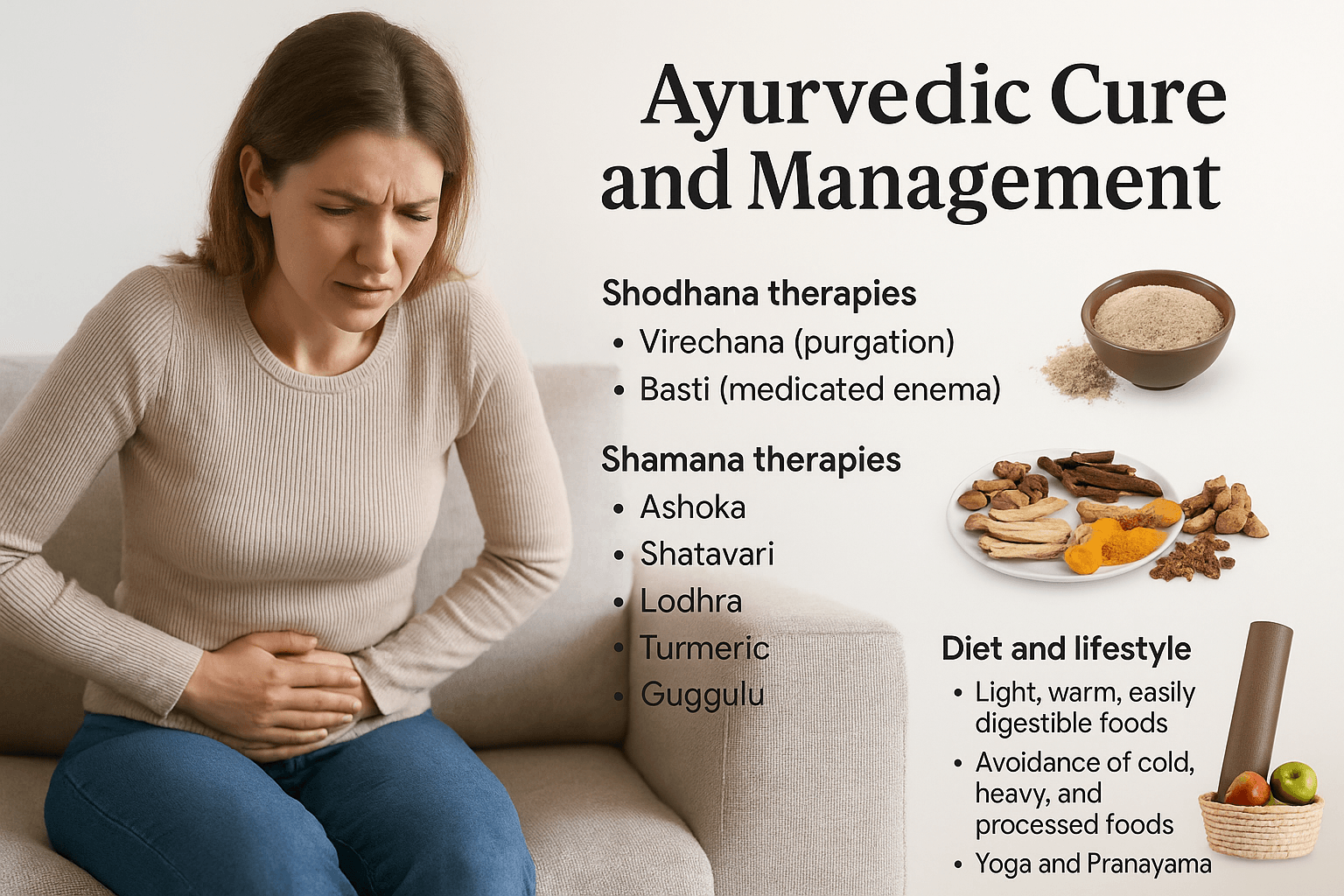
Ayurveda treats endometriosis by focusing on the root causes of dosha imbalance, toxin accumulation (Aama), and obstruction of reproductive channels (Srotorodha), rather than merely suppressing symptoms. Treatment integrates Shodhana (detoxification), Shamana (pacification), and Rasayana (rejuvenation) therapies, supported by potent herbal Rasayanas and mineral preparations documented in classical texts [1].
Shodhana (Detoxification Therapies)
Detoxification is essential to clear accumulated toxins and restore balance. Virechana (purgation therapy) pacifies excess Pitta and reduces inflammatory processes. Basti (medicated enema), particularly Yoni Vasti, regulates Apana Vata, the downward energy that governs menstruation and fertility. Oils like Dashmoola taila and decoctions such as Guduchi kwath are frequently used for cleansing the pelvic channels and relieving congestion [2].
Shamana (Pacification Therapies)
Potent Herbs
- Ashoka (Saraca asoca): Classical uterine tonic, regulates menstrual bleeding [3].
- Shatavari (Asparagus racemosus): Balances female hormones and enhances fertility [4].
- Lodhra (Symplocos racemosa): Reduces pelvic inflammation and swelling [5].
- Turmeric (Curcuma longa): Potent anti-inflammatory and antioxidant, useful in pelvic pain [6].
- Guggulu (Commiphora mukul): Breaks adhesions, reduces cystic and fibroid growth [7].
- Manjistha (Rubia cordifolia): Blood purifier, clears Aama [8].
- Kanchanar (Bauhinia variegata): Especially effective in abnormal tissue growths [9].
- Guduchi (Tinospora cordifolia): Immunomodulator, balances all three doshas [10].
Classical Polyherbal Preparations
- Kanchnar Guggulu: Used for fibroids, ovarian cysts, and endometriotic masses [11].
- Pushyanug Churna: Regulates heavy menstrual bleeding [12].
- Sootshekhar Ras: Restores digestive fire (Agni) and relieves menstrual pain [13].
- Ashokarishta and Dashmoolarishta: Strengthen the uterus and reduce inflammation [14].
Rasayana (Rejuvenation and Mineral Preparations)
For chronic and recurrent cases, Ayurveda recommends Rasa Shastra preparations, which rejuvenate tissues and restore hormonal balance.
Potent Mineral and Bhasma Preparations
- Swarna Bhasma (Gold calx): Rasayana for fertility and immunity [15].
- Rajata Bhasma (Silver calx): Cooling, balances Pitta [16].
- Abhrak Bhasma (Mica calx): Rejuvenative, strengthens reproductive health [17].
- Tamra Bhasma (Copper calx): Reduces Kapha and abnormal growths [18].
- Lauh Bhasma (Iron calx): Corrects anemia from heavy bleeding [19].
- Pravala Pishti (Coral): Pacifies Pitta, reduces excessive bleeding [20].
- Mukta Shukti Bhasma (Pearl oyster shell): Alkalinizing, relieves dysmenorrhea [21].
- Godanti Bhasma (Gypsum): Cooling, analgesic for pelvic inflammation [22].
- Gandhak Rasayan (Purified sulphur): Detoxifies blood, strengthens immunity [23].
- Trivanga Bhasma (Lead, zinc, tin compound): Improves reproductive function [24].
- Heerak Bhasma (Diamond): Supreme Rasayana for chronic, resistant gynecological disorders [25].
Diet and Lifestyle
Sustaining recovery requires dietary and lifestyle regulation. Women are advised to eat light, warm, easily digestible foods to support Agni and prevent Aama formation. Cold, heavy, and processed foods should be avoided as they aggravate Kapha and Aama. Yoga asanas such as Supta Baddha Konasana, Bhujangasana, and Paschimottanasana reduce pelvic congestion, while Pranayama calms stress and restores Vata balance. Ayurveda also emphasizes meditation, adequate sleep, and seasonal Rasayana therapy for long-term prevention [26].
Ayurveda provides a root-cause–oriented cure for endometriosis by cleansing toxins, pacifying doshas, and rejuvenating reproductive tissues. Herbs such as Ashoka, Shatavari, and Guggulu regulate menstrual health, while potent Bhasmas and Rasayanas like Swarna Bhasma, Abhrak Bhasma, and Gandhak Rasayan strengthen immunity, restore fertility, and prevent recurrence. This comprehensive approach not only relieves symptoms but also addresses the systemic imbalances underlying endometriosis [27].
Frequently Asked Questions (FAQ)
Q1. What exactly is endometriosis?
Endometriosis is a chronic gynecological condition where tissue similar to the uterine lining grows outside the uterus, causing pain, inflammation, cysts, and sometimes infertility [1].
Q2. Can endometriosis be cured completely?
Modern medicine currently offers only symptom management through hormonal therapy or surgery, but recurrence is common. Ayurveda, however, aims at root-cause correction by detoxifying the body, balancing doshas, and rejuvenating reproductive health with herbs and mineral Rasayanas [2].
Q3. How does Ayurveda explain endometriosis?
In Ayurveda, endometriosis correlates with Udavarta Yonivyapad and Artava Dushti. It is caused by disturbed Apana Vata, Pitta inflammation, and Kapha adhesions, combined with Agnimandya (weak digestion) and Aama (toxin accumulation). These lead to Rakta Dushti (impure blood) and Srotorodha (blockages in reproductive channels) [3].
Q4. What are the common symptoms I should look for?
Key symptoms include severe menstrual cramps, heavy or irregular bleeding, pain during intercourse, difficulty conceiving, fatigue, bloating, and digestive disturbances such as constipation or diarrhea around menstruation [4].
Q5. Which Ayurvedic herbs are useful for managing endometriosis?
Several herbs are well-documented in Ayurveda: Ashoka, Shatavari, Lodhra, Guggulu, Turmeric, Manjistha, and Guduchi. Classical formulations like Kanchnar Guggulu, Pushyanug Churna, and Ashokarishta are also commonly prescribed [5].
Q6. Are minerals (Bhasmas) used in Ayurvedic treatment of endometriosis?
Yes. Potent Rasayana preparations such as Swarna Bhasma (gold), Abhrak Bhasma (mica), Gandhak Rasayan (sulphur), Pravala Pishti (coral), and Mukta Shukti Bhasma (pearl oyster shell) are used to strengthen immunity, balance hormones, and prevent recurrence [6].
Q7. Can Ayurveda help with infertility due to endometriosis?
Yes. By reducing adhesions, improving uterine receptivity, and purifying blood (Rakta Shuddhi), Ayurvedic therapies enhance fertility. Herbs like Shatavari, Ashoka, and Guggulu combined with Rasayanas like Swarna Bhasma support ovum quality and conception potential [7].
Q8. How long does Ayurvedic treatment for endometriosis take?
The duration depends on severity, age, and fertility goals. Many women begin experiencing relief in 2–3 months, but complete rebalancing with Shodhana, Shamana, and Rasayana therapies usually takes 6–12 months under expert supervision [8].
Q9. Are there dietary restrictions in Ayurvedic management of endometriosis?
Yes. Ayurveda recommends a light, warm, easily digestible diet while avoiding cold, heavy, oily, and processed foods. Fresh vegetables, whole grains, ghee, and herbal teas support recovery. Lifestyle measures such as yoga, pranayama, and meditation are also essential [9].
Q10. Can endometriosis lead to cancer if untreated?
Although rare, women with long-standing untreated endometriosis have a slightly increased risk of ovarian cancer, particularly clear cell and endometrioid types. This is why timely diagnosis and management—whether modern or Ayurvedic—is crucial [10].
References
- World Health Organization. (2023). Endometriosis – Key facts. WHO. Retrieved from https://www.who.int/news-room/fact-sheets/detail/endometriosis
- Becker, C. M., Bokor, A., Heikinheimo, O., Horne, A., Jansen, F., Kiesel, L., … Vanhie, A. (2022). ESHRE guideline: Endometriosis. Human Reproduction Open, 2022(2), hoac009. https://doi.org/10.1093/hropen/hoac009
- National Institute for Health and Care Excellence. (2017, last updated 2025). Endometriosis: diagnosis and management (NICE guideline NG73). Retrieved from https://www.nice.org.uk/guidance/ng73
- Hirsch, M., Dhillon-Smith, R., Cutner, A., & Yap, C. (2016). The diagnostic accuracy of CA-125 for endometriosis: a systematic review and meta-analysis. BJOG: An International Journal of Obstetrics & Gynaecology, 123(11), 1761–1768. https://doi.org/10.1111/1471-0528.14055
- Yale Medicine. (2024). Endometriosis Fact Sheet. Retrieved from https://www.yalemedicine.org/conditions/endometriosis
- American College of Obstetricians and Gynecologists (ACOG). (2022). Endometriosis FAQs. Retrieved from https://www.acog.org/womens-health/faqs/endometriosis
- Hsu, A. L., Khachikyan, I., & Stratton, P. (2010). Invasive and non-invasive methods for diagnosis of endometriosis. Obstetrics and Gynecology International, 2010, 1–9. https://doi.org/10.1155/2010/504060
- Zondervan, K. T., Becker, C. M., Koga, K., Missmer, S. A., Taylor, R. N., & Vigano, P. (2018). Endometriosis. Nature Reviews Disease Primers, 4(1), 9. https://doi.org/10.1038/s41572-018-0008-5
- Giudice, L. C. (2010). Clinical practice: Endometriosis. The New England Journal of Medicine, 362(25), 2389–2398. https://doi.org/10.1056/NEJMcp1000274
- Chung, H. F., et al. (2025). Global pooled prevalence of endometriosis: Updated estimates from multi-country cohorts. Human Reproduction, 40(2), 321–333. https://doi.org/10.1093/humrep/deae312
- Charaka. (2022 reprint). Charaka Samhita – Chikitsa Sthana, Chapter 30 (Yonivyapad Chikitsa). Chaukhambha Sanskrit Pratishthan, Varanasi.
- Sushruta. (2021 reprint). Sushruta Samhita – Sharira Sthana, Chapter 2 (Artava Dushti). Chaukhambha Orientalia, Varanasi.
- Vagbhata. (2020 reprint). Ashtanga Hridaya – Nidana Sthana, Chapter 1–2. Chaukhambha Krishnadas Academy, Varanasi.
- Bhavamishra. (2021 reprint). Bhavaprakasha Nighantu – Guduchyadi Varga, on Ashoka, Shatavari, and Lodhra. Chaukhambha Bharati Academy, Varanasi.
- Sharma, P. V. (2017). Dravyaguna Vijnana, Vol II. Chaukhambha Bharati Academy. [Ashoka, Shatavari, Lodhra monographs]
- Singh, R. H. (2018). An Introduction to Ayurveda. Chaukhambha Sanskrit Series. [Concepts of Vata, Pitta, Kapha, and Artava Dushti]
- Patgiri, B., & Prajapati, P. K. (2015). Rasashastra-based herbo-mineral formulations in women’s health: Review. Ayu, 36(1), 5–11. https://doi.org/10.4103/0974-8520.169011
- Kesarwani, R., Gupta, A., & Watal, G. (2013). Nutritional and therapeutic potential of Rasayana herbs in female reproductive health. Journal of Ethnopharmacology, 150(3), 707–719. https://doi.org/10.1016/j.jep.2013.09.045
- Tripathi, Y. B., & Pandey, R. S. (2014). Therapeutic applications of Swarna Bhasma and other Ayurvedic Bhasmas in gynecological disorders. Ancient Science of Life, 33(4), 218–226. https://doi.org/10.4103/0257-7941.146986
- Jaiswal, Y. S., & Williams, L. L. (2017). A glimpse of Ayurveda – The forgotten history and principles of Indian traditional medicine. Journal of Traditional and Complementary Medicine, 7(1), 50–53. https://doi.org/10.1016/j.jtcme.2016.02.002
- Tiwari, P., & Dwivedi, S. (2019). Role of Kanchnar Guggulu and Pushyanug Churna in gynecological disorders: A classical review. International Journal of Ayurvedic Medicine, 10(3), 298–305. https://www.ijam.co.in/index.php/ijam/article/view/1322
- Aithal, V., & Rani, R. (2021). Pharmacological perspectives of Ashokarishta and Dashmoolarishta in gynecological health. Journal of Ayurveda and Integrative Medicine, 12(4), 567–573. https://doi.org/10.1016/j.jaim.2020.11.001
- Balekundri, A., & Mannur, V. (2020). Influence of Gandhak Rasayan and herbo-mineral Rasayana therapy in reproductive health. AYU, 41(2), 145–151. https://doi.org/10.4103/ayu.AYU_161_19
- Upadhyay, S., & Patel, V. (2016). Safety and efficacy of Bhasma formulations in chronic gynecological disorders. Journal of Ethnopharmacology, 188, 80–90. https://doi.org/10.1016/j.jep.2016.04.040
- Kotecha, R. (2016). Ayurvedic management of gynecological disorders through Rasayana therapy. International Journal of Ayurveda Research, 7(1), 1–8. https://doi.org/10.4103/0974-7788.173431