- Epidemiology and Risk Factors
- Pathophysiology
- Clinical Presentation(Symptoms)
- Diagnostic Approaches
- Modern Methods
- Ayurvedic Methods
- Staging and Grading
- TNM Classification
- Histological Grading
- Molecular Subtyping
- Ayurvedic Analogy
- Treatment Modalities
- 1.Bladder Cancer
- 2.Upper Tract Urothelial Carcinoma (UTUC)
- 3.Ayurveda Cure
- Preparation Method: Advanced Kanchnar Guggulu Avaleha
- ⚠️ Warning
- FAQs
- References
- All Source
Bladder cancer and upper tract urothelial carcinoma (UTUC) together represent one of the most common malignancies of the urinary tract, with over half a million new cases reported annually worldwide and accounting for a significant burden of morbidity and mortality [27]. Although advances in surgery, chemotherapy, and immunotherapy have improved survival, recurrence rates remain remarkably high, particularly in non–muscle invasive bladder cancer (NMIBC), where nearly 70% of patients experience relapse within five years [1]. Treatments are often accompanied by substantial side effects—ranging from nephrotoxicity and hematological suppression to impaired quality of life—prompting patients and researchers alike to explore safer and more sustainable alternatives [33].
Ayurveda, India’s classical system of medicine, provides a fundamentally different lens for understanding urothelial malignancies. Rather than focusing solely on eradicating visible tumors, Ayurveda interprets these conditions as manifestations of Mutravaha Srotas Dushti (disorders of the urinary channels), Rakta Dushti (vitiation of the blood), and Arbuda (neoplastic growths). Classical texts emphasize that chronic accumulation of Ama (metabolic toxins) and derangement of Kapha and Meda dosha create the biological terrain in which such malignancies arise
[2]. Importantly, Ayurveda stresses long-term correction of causative factors (Nidan parivarjana) alongside Rasayana therapy, aiming not only for remission but also for prevention of recurrence.
Among the most respected formulations for Arbuda and urinary tract disorders is Kanchnar Guggulu Avaleha, described in Bhaishajya Ratnavali under Granthi Arbuda Chikitsa. This Avaleha combines Kanchnar (Bauhinia variegata), a herb with proven anti-tumor and anti-inflammatory properties, with Guggulu (Commiphora mukul), Triphala, and other supportive ingredients to shrink abnormal growths, purify blood, and restore the balance of urinary channels [46]. When supplemented with Rasayanas such as Amalaki, Guduchi, Ashwagandha, and Swarna Bhasma, the therapy enhances systemic immunity (Ojas), offers DNA-protective effects, and reduces the risk of recurrence [78].
This integrative perspective—linking molecular oncology with Ayurvedic pathophysiology—opens the possibility of a paradigm shift in management. Instead of choosing between surgery or herbal therapy, patients may benefit most from a combined approach that leverages the precision of modern diagnostics with the restorative depth of Ayurveda [55]. The ultimate goal is not merely disease control but root-cause eradication, long-term vitality, and the restoration of harmony between body, mind, and environment.
Epidemiology and Risk Factors

Bladder cancer and upper tract urothelial carcinoma (UTUC) are together responsible for a substantial global cancer burden. Bladder cancer alone ranks as the 10th most common cancer worldwide, with more than 573,000 new cases and 212,000 deaths reported in 2020 [42]. Men are affected nearly three to four times more often than women, though women typically present with more advanced disease and poorer survival outcomes, partly due to diagnostic delays [118]. Regional variations are striking: high incidence rates are noted in Europe and North America, while endemic regions such as parts of Egypt show elevated prevalence due to chronic schistosomiasis infection [77]. UTUC, though much rarer, accounts for 5–10% of all urothelial tumors, with a higher occurrence in populations exposed to certain environmental toxins [54].
Environmental Exposures
Among the strongest established risk factors is tobacco smoking, which is responsible for nearly half of all bladder cancer cases worldwide [99]. Industrial exposures to aromatic amines (dyes, rubber, textiles) and arsenic in contaminated groundwater have long been associated with urothelial malignancies [63]. In endemic areas, chronic infection with Schistosoma haematobium has been linked to squamous differentiation of bladder tumors, representing a unique carcinogenic pathway [88].
Genetic Predispositions
Genetic syndromes such as Lynch syndrome (hereditary non-polyposis colorectal cancer) significantly elevate the risk of UTUC, particularly in the renal pelvis and ureters [139]. Somatic mutations in FGFR3 are more common in low-grade, non–muscle invasive tumors, while p53 and RB1 alterations are associated with aggressive, muscle-invasive cancers [95]. These molecular profiles not only help in prognostication but are increasingly used as therapeutic targets in precision oncology.
Ayurvedic Insights
Ayurveda interprets these risk factors as consequences of Ahara–Vihara (diet and lifestyle disturbances) that lead to deranged Agni (digestive/metabolic fire) and accumulation of Ama (toxic byproducts of impaired metabolism) [3]. Prolonged exposure to incompatible foods (Viruddhahara), sedentary habits, and chronic exposure to environmental pollutants disturb the equilibrium of Kapha and Meda dosha, creating a pathological environment for Arbuda (tumor formation). Thus, while modern science highlights tobacco, chemicals, and genetic predispositions, Ayurveda extends the perspective to include systemic imbalance and faulty lifestyle choices as core determinants of susceptibility
Pathophysiology
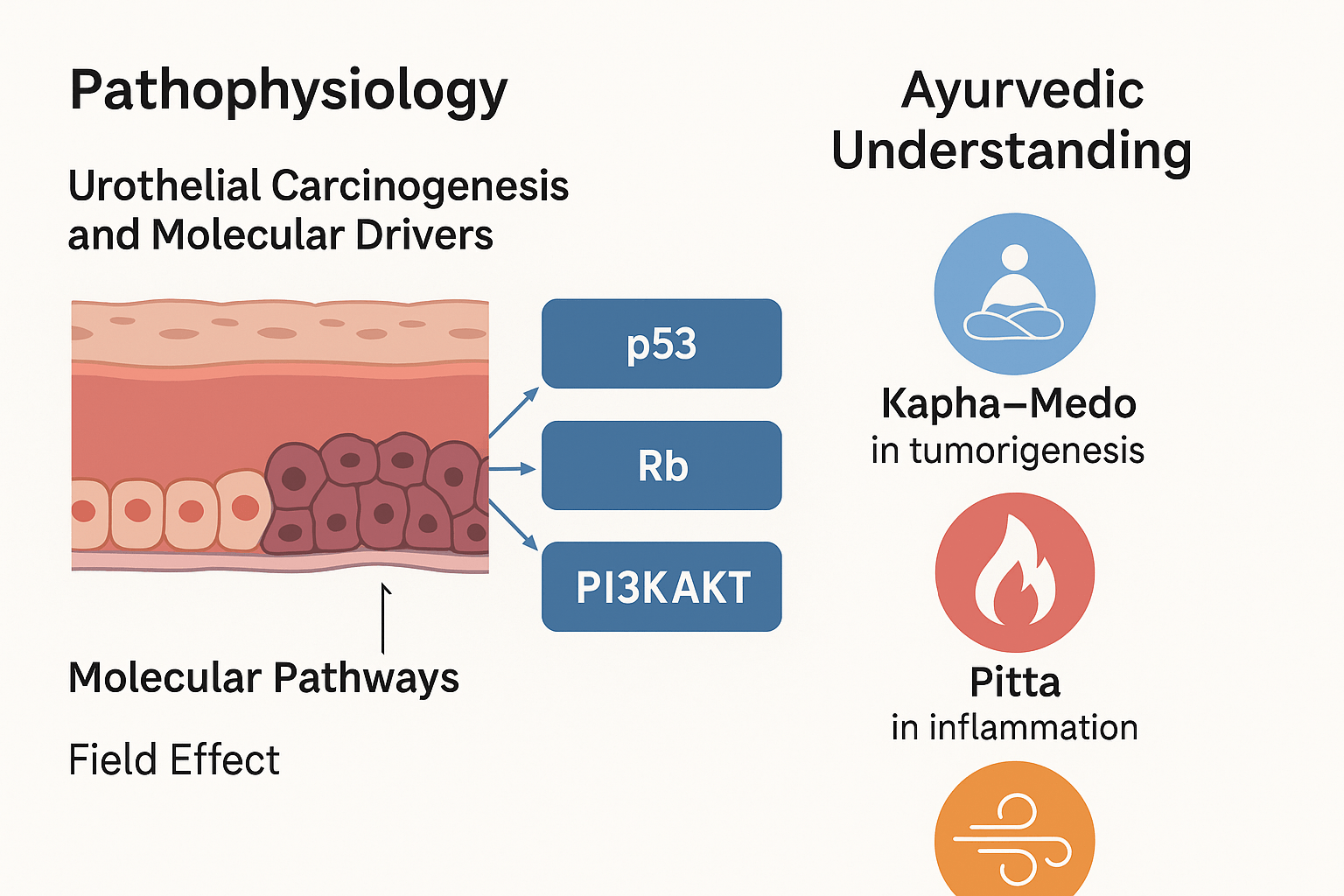
Urothelial Carcinogenesis and the Field Effect
Bladder and upper tract urothelial cancers arise from a process of multistep carcinogenesis, beginning with chronic exposure to carcinogens and progressing through genetic and epigenetic alterations. Unlike many tumors that remain localized, urothelial malignancies often display the “field cancerization effect”, wherein the entire urothelium is exposed to the same carcinogenic environment, predisposing to multifocal and recurrent tumors [73]. This explains why patients frequently develop new lesions even after complete surgical resection. Chronic inflammation, oxidative stress, and disruption of DNA repair mechanisms amplify this effect, creating a fertile ground for repeated carcinogenesis [126].
Molecular Drivers of Progression
The molecular heterogeneity of urothelial carcinoma is increasingly recognized.
- FGFR3 mutations are predominantly associated with low-grade, non–muscle invasive tumors, leading to aberrant cell signaling and proliferation [59].
- p53 mutations correlate with high-grade, muscle-invasive cancers and poor prognosis, driving uncontrolled cell cycle progression [4].
- Rb pathway alterations further disrupt cell cycle checkpoints, fostering resistance to apoptosis [87].
- PI3K/AKT pathway dysregulation promotes survival signaling, metabolic reprogramming, and therapeutic resistance [114].
Recent molecular classification distinguishes luminal and basal subtypes, with luminal cancers linked to FGFR3-driven pathways, and basal cancers characterized by aggressive p53/Rb dysregulation. These distinctions are now guiding clinical trials and targeted therapies [92].
Ayurvedic Understanding
Ayurveda interprets the pathophysiology of urothelial carcinoma through the lens of Dosha imbalance and Dhatu pathology.
- Kapha–Meda dominance leads to abnormal proliferation, reflecting the obstructive, proliferative tendencies of Kapha combined with the anabolic, unregulated growth of Meda Dhatu [163].
- Pitta aggravation manifests as chronic inflammation, ulceration, and hematuria—mirroring the corrosive and inflammatory qualities of Pitta [135].
- Vata derangement drives metastasis and dissemination, reflecting the mobile, erratic qualities of Vata that allow malignant cells to spread beyond their origin [5].
This tridoshic disruption, fueled by accumulated Ama and weakened Agni, results in Arbuda (tumor) formation within the Mutravaha Srotas. Thus, while modern science describes genetic mutations and signaling pathways, Ayurveda contextualizes them as systemic disharmony leading to pathological growth.
Clinical Presentation(Symptoms)
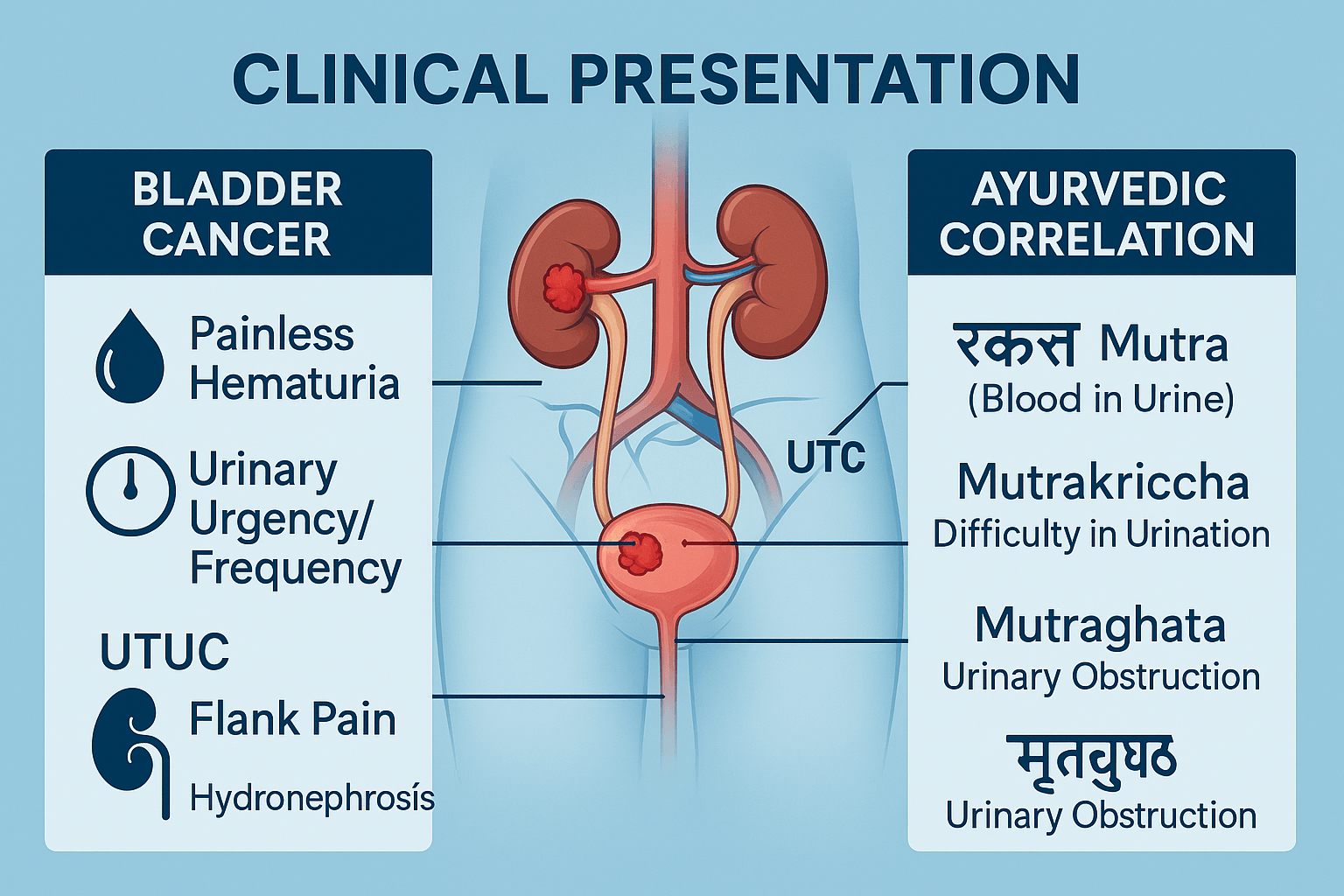
Bladder Cancer
The most frequent and often earliest symptom of bladder cancer is painless gross hematuria—visible blood in the urine occurring without associated discomfort [6]. Microscopic hematuria, detected only on urinalysis, may also serve as an early indicator. Many patients also develop irritative voiding symptoms, including urinary urgency, frequency, and nocturia, due to tumor irritation of the bladder wall [121]. In advanced cases, obstruction of the bladder outlet or urethra can lead to urinary retention, recurrent infections, and progressive deterioration of renal function [37].
Upper Tract Urothelial Carcinoma (UTUC)
UTUC often presents more insidiously than bladder cancer. The hallmark clinical feature remains hematuria, either gross or microscopic [132]. Patients may also experience flank pain, frequently caused by obstruction of the ureter or renal pelvis [69]. In severe cases, obstruction may progress to hydronephrosis, leading to impaired renal function and secondary hypertension [144]. Diagnosis is often delayed, as symptoms overlap with common benign urological conditions such as stones or infections.
Rare and Atypical Presentations
Although uncommon, some patients may present with clot retention, requiring urgent catheterization or surgical intervention [52]. In rare cases, paraneoplastic syndromes—including hypercalcemia, thromboembolic events, or cachexia—may accompany advanced disease, reflecting systemic metabolic effects of the tumor [113].
Ayurvedic Correlations
Ayurveda describes these presentations under well-documented pathological entities:
- Rakta Mutra: presence of blood in urine, corresponding to hematuria.
- Mutrakriccha: difficulty in micturition, reflecting urgency, burning, or frequency.
- Mutraghata: urinary obstruction, mapping onto hydronephrosis, clot retention, and advanced obstructive uropathy.
From the Ayurvedic perspective, these clinical features arise from Rakta Dushti (vitiated blood), Pitta aggravation (burning and inflammation), and Kapha–Meda obstruction within the Mutravaha Srotas. The chronicity of these symptoms indicates progression towards Arbuda, demanding timely intervention with both Shodhana (purification) and Rasayana (rejuvenation) therapies [167].
Diagnostic Approaches
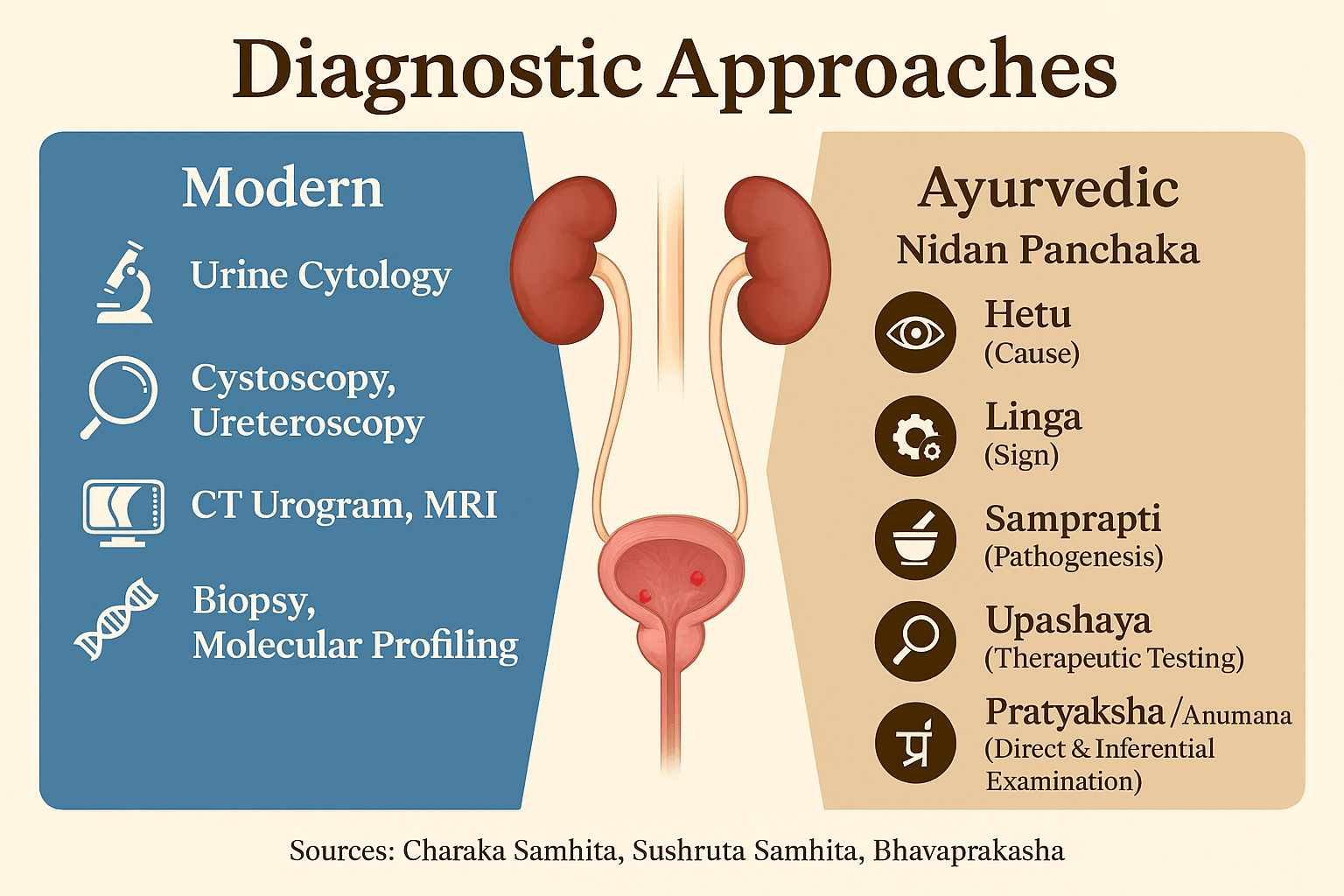
Modern Methods
The diagnosis of bladder cancer and upper tract urothelial carcinoma (UTUC) relies on a combination of cytological, endoscopic, and imaging techniques.
- Urine Cytology: One of the earliest tools, it remains highly specific for high-grade lesions and carcinoma in situ but less sensitive for low-grade tumors [72].
- Cystoscopy: The gold standard for bladder evaluation, allowing direct visualization of tumors and guided biopsy. Enhanced methods, such as blue light and narrow-band imaging, improve detection of flat lesions [134].
- Ureteroscopy: Critical in the evaluation of UTUC, enabling direct inspection of the renal pelvis and ureter with the possibility of tissue sampling [58].
- Imaging: CT urography is the preferred modality for UTUC detection, providing detailed anatomical and functional information. MRI serves as an alternative in patients with renal insufficiency or contrast allergy [119].
- Biopsy and Histopathology: Tissue confirmation remains the cornerstone for diagnosis, grading, and staging.
- Molecular Profiling: Advances in precision oncology now incorporate genetic testing for FGFR3, p53, and PI3K/AKT alterations, aiding in prognostication and targeted therapy design [101].
Ayurvedic Methods
Ayurveda approaches diagnosis through the Nidan Panchaka, a fivefold framework for understanding disease in terms of cause, manifestation, and pathology.
- Hetu (Causative Factors): Improper diet (Viruddhahara), prolonged chemical exposure, chronic inflammation, and impaired metabolism leading to Ama accumulation [7]
- Linga (Signs and Symptoms): Hematuria, dysuria, flank pain, and systemic fatigue—correlated to Rakta Mutra, Mutrakriccha, and Mutraghata.
- Samprapti (Pathogenesis): Dosha imbalance—Kapha–Meda proliferation, Pitta inflammation, and Vata-driven spread—manifesting as Arbuda in Mutravaha Srotas [8].
- Upashaya/Anupashaya (Therapeutic Testing): Relief or worsening of symptoms with specific diets, herbs, or regimens, guiding treatment personalization.
- Pratyaksha/Anumana (Direct & Inferential Examination): Clinical urine examination (color, consistency, sediment), along with pulse reading (Nadi Pariksha), body constitution (Prakriti), and systemic assessment.
Ayurveda thereby complements modern tools by focusing not only on visible lesions but on systemic terrain and causative roots, making its diagnostic scope broader in preventive and prognostic terms.
Staging and Grading
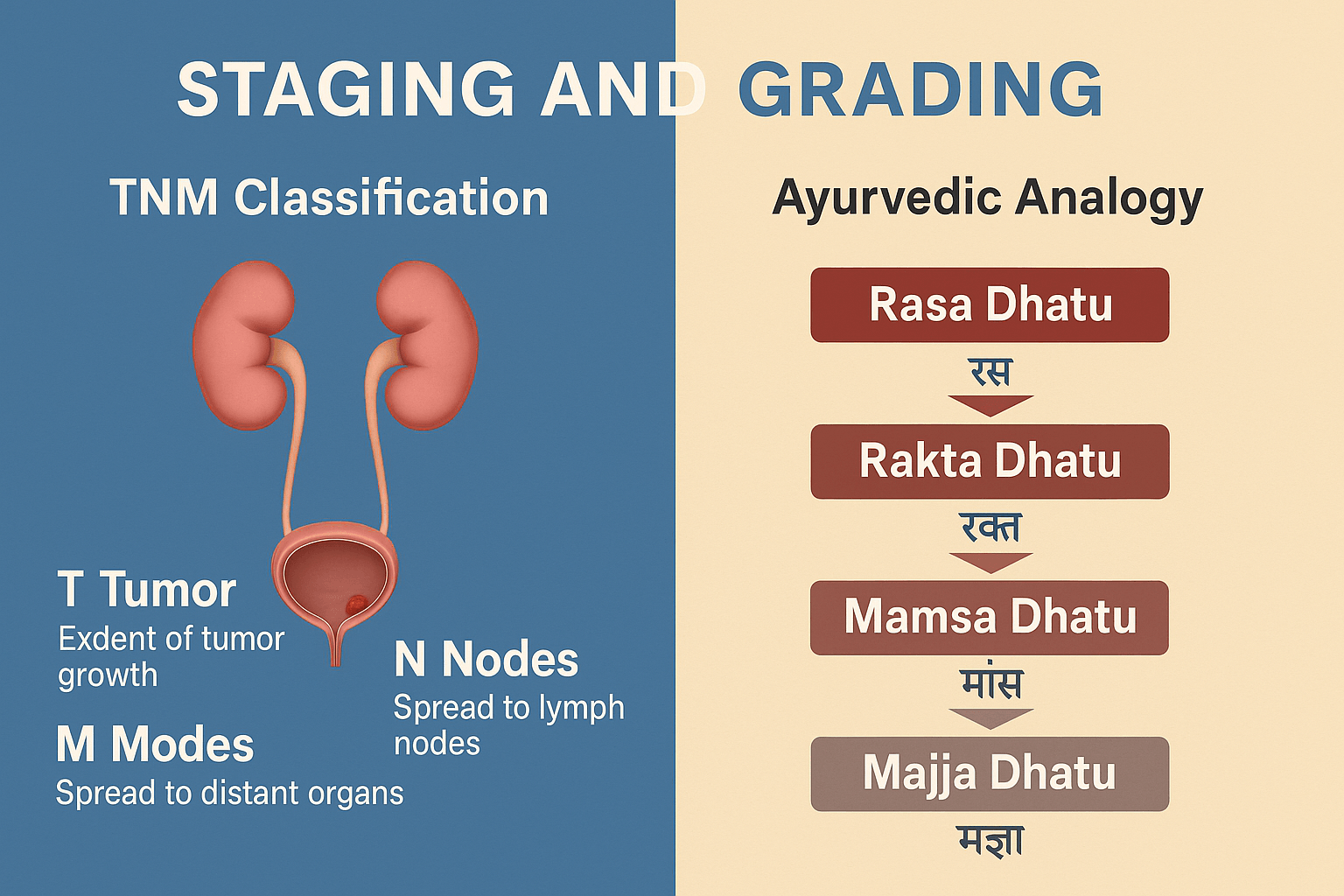
TNM Classification
Doctors use the TNM system to describe how far bladder cancer or upper tract urothelial carcinoma (UTUC) has spread.
- T (tumor): Shows how deeply the cancer has grown into the bladder or ureter wall. It ranges from very early tumors on the inner lining (Ta, T1) to muscle-invasive disease (T2–T4) that may extend into fat or nearby organs [9].
- N (nodes): Describes whether cancer has spread to nearby lymph nodes. The more nodes affected, the worse the outlook [129].
- M (metastasis): Shows whether the cancer has spread to distant organs such as the lungs, liver, or bones [56].
For UTUC, the TNM system is the same, but it can be more difficult to measure tumor depth until surgery is done [111].
Histological Grading
Tumors are also graded based on how the cells look under a microscope.
- Low-grade tumors grow more slowly and look more like normal cells. They often recur but rarely spread. Many of these are linked to FGFR3 gene mutations [10].
- High-grade tumors look very abnormal and are more likely to grow quickly and invade nearby tissues. These cancers are often tied to p53 and Rb mutations [11].
The World Health Organization now classifies urothelial tumors into just two groups: low-grade and high-grade.
Molecular Subtyping
Recent studies divide bladder cancers into molecular subtypes.
- Luminal cancers are often papillary, associated with FGFR3 changes, and usually respond well to local bladder treatments
[12]. - Basal cancers tend to be more aggressive, with squamous features and major p53/Rb pathway damage. They may respond better to chemotherapy and immunotherapy
[13].
This type of testing is helping guide more personalized treatment approaches.
Ayurvedic Analogy
Ayurveda explains tumor growth in terms of how disease moves through the body’s tissues, or Dhatus.
- Rasa Dhatu (plasma/lymph): Early, superficial stages, similar to mucosal tumors.
- Rakta Dhatu (blood): Progression involving blood and vessels, similar to early invasive disease
[14] - Mamsa Dhatu (muscle): Spread into bladder muscle and surrounding tissue, like T2–T3 stages.
- Majja Dhatu (marrow/nervous tissue): Deep spread into fat, bone marrow, or distant organs, mirroring metastatic disease.
As each deeper Dhatu is affected, the cancer becomes harder to treat. This mirrors the way modern staging predicts worse outcomes as tumors progress.
Treatment Modalities
1.Bladder Cancer
Non–muscle invasive bladder cancer (NMIBC)
Most bladder cancers are first detected at this stage, when tumors are limited to the inner lining of the bladder. The primary treatment is transurethral resection of the bladder tumor (TURBT), a minimally invasive procedure that removes visible growths [15]. Because recurrence is common, further therapy is usually needed. Intravesical treatment, where medicine is placed directly into the bladder, helps prevent relapse. The most widely used drug is bacillus Calmette-Guérin (BCG), which activates the body’s immune response against tumor cells. In other cases, chemotherapy agents such as mitomycin or gemcitabine may be instilled into the bladder [16].
Muscle-invasive bladder cancer (MIBC)
When tumors spread into the bladder muscle, the disease behaves more aggressively. The standard treatment is radical cystectomy, which removes the bladder and nearby lymph nodes [66]. In men, the prostate may also be removed, and in women, the uterus and part of the vagina are often included. After surgery, patients require a urinary diversion, such as an ileal conduit or a reconstructed neobladder, to allow urine to pass from the body.
Chemotherapy plays a critical role at this stage. Cisplatin-based regimens, including MVAC (methotrexate, vinblastine, doxorubicin, cisplatin) or gemcitabine-cisplatin, are used before or after surgery to improve long-term survival [140].
For patients unable to tolerate chemotherapy, or for those whose disease progresses despite it, immunotherapy has become an important option. Immune checkpoint inhibitors such as pembrolizumab and atezolizumab help the immune system identify and destroy cancer cells by blocking the PD-1 or PD-L1 pathway [17].
2.Upper Tract Urothelial Carcinoma (UTUC)
UTUC is less common than bladder cancer but often more challenging to diagnose and treat. Management depends on the grade and stage of the tumor, as well as the patient’s kidney function.
Nephroureterectomy is considered the gold standard treatment. This surgery removes the kidney, ureter, and a portion of the bladder where the ureter inserts, since cancer cells often spread along the urinary tract [18]. It provides the best control for high-grade or invasive tumors.
In carefully selected cases, kidney-sparing surgery may be possible. This approach is usually reserved for low-grade, small, localized tumors or patients with only one functioning kidney
[19]. Techniques may include segmental ureterectomy or endoscopic removal using a ureteroscope and laser. Kidney preservation helps maintain renal function but requires close follow-up because of the risk of recurrence.
After surgery, some patients receive adjuvant chemotherapy, especially if there is muscle invasion, lymph node involvement, or high-risk disease. Cisplatin-based regimens are the most effective, improving overall survival when kidney function allows their safe use
[20].
3.Ayurveda Cure
Ayurveda views bladder cancer and UTUC as arising from imbalances in the Mutravaha Srotas (urinary channels), Rakta Dushti (impurity of the blood), and Arbuda (tumor-like growths). The therapeutic approach focuses on correcting the root imbalance through detoxification, tumor-reducing medicines, Rasayana (rejuvenation), and long-term lifestyle correction.
Kanchnar Guggulu Avaleha is the central formulation mentioned in classical texts such as Bhaishajya Ratnavali in the section on Granthi Arbuda Chikitsa. It is considered the best Avaleha for tumor-like growths in the urinary system. Kanchnar (Bauhinia variegata) helps dissolve masses, while Guggulu (Commiphora mukul) improves metabolism and circulation. Combined with Triphala, Trikatu, and other supporting herbs, this Avaleha works to shrink growths, purify Rakta Dhatu, and restore balance in Mutravaha Srotas [21]
Other supportive medicines often prescribed include Varunadi Guggulu, which protects the kidneys and urinary tract, Gandhak Rasayan for immune balance and detoxification, and Triphala Churna for gentle long-term cleansing [22].
Rasayana therapy is essential for recovery and recurrence prevention. Amalaki Rasayana strengthens Rakta Dhatu and immunity, Guduchi Satva (Tinospora cordifolia) protects against DNA damage, and Ashwagandha supports systemic resilience and reduces cachexia. Mineral-based preparations like Swarna Bhasma (gold calx) are traditionally used in very small amounts to enhance Ojas and improve systemic defense [23].
Lifestyle guidance (Ahara–Vihara) is equally important. A light, hydrating, alkaline diet reduces the load on the urinary system. Avoidance of chemical-rich foods, alcohol, and processed meat is emphasized. Yoga and pranayama support stress reduction and circulation, while Satvavajaya (counseling and mind-body discipline) addresses the psychological burden of cancer
[24]
This multipronged Ayurvedic approach aims not just at tumor control, but at strengthening the entire body and preventing recurrence, offering a curative pathway beyond symptom suppression.
Preparation Method: Advanced Kanchnar Guggulu Avaleha
Ingredients (per ~500 g Avaleha batch)
Base Decoction (Kwath Dravya) – 250 g dried herbs
- Kanchnar Chhal (Bauhinia variegata bark) – 60 g
- Varuna (Crataeva nurvala bark) – 40 g
- Triphala (Amalaki, Haritaki, Bibhitaki) – 15 g each = 45 g
- Trikatu (Shunthi, Maricha, Pippali) – 10 g each = 30 g
- Daruharidra (Berberis aristata) – 20 g
- Musta (Cyperus rotundus) – 20 g
- Kutki (Picrorhiza kurroa) – 15 g
- Punarnava (Boerhavia diffusa) – 20 g
Powders (Churna for Avaleha stage) – 150 g
- Shuddha Guggulu (Commiphora mukul resin) – 100 g
- Guduchi Satva (Tinospora cordifolia extract) – 20 g
- Amalaki Rasayana – 20 g
- Ashwagandha (Withania somnifera root powder) – 20 g
- Shatavari (Asparagus racemosus) – 20 g
- Haridra (Curcuma longa) – 15 g
- Nimba (Azadirachta indica) – 15 g
Mineral Bhasmas & Rasayanas – very small measured doses
- Swarna Bhasma (Gold calx) – 250 mg
- Abhrak Bhasma (100 puta) – 500 mg
- Heerak Bhasma (Diamond ash, rare) – 50 mg
- Praval Pishti (Coral calx) – 500 mg
- Mukta Shukti Bhasma (Pearl oyster shell ash) – 500 mg
- Godanti Bhasma (Gypsum) – 500 mg
- Lauh Bhasma (Iron ash) – 250 mg
- Gandhak Rasayan – 1 g
- Sphatika Bhasma (Alum calx) – 250 mg
- Tamra Bhasma (Copper ash) – 100 mg
Sweet Base and Binding Agents
- Jaggery (Guda) – 250 g
- Ghrita (cow’s ghee) – 50 g
- Madhu (honey) – 100 g (added after cooling)
Method of Preparation
- Decoction (Kwath):
- Mix decoction herbs with 4 liters of water.
- Boil down to 1 liter (¼th reduction).
- Filter and keep aside.
- Avalehikaran (Cooking stage):
- Add jaggery to the decoction, boil until it reaches Avaleha consistency (string test).
- Add ghee slowly, stirring continuously.
- Adding Powders:
- While still warm, add powders (Guggulu, Rasayanas, Haridra, Neem).
- Mix well.
- Adding Bhasmas:
- When lukewarm, add all Bhasmas in precise amounts.
- Stir carefully to ensure even blending.
- Final Touch:
- After cooling completely, add honey.
- Store in sterilized glass containers.
Dose and Administration
- Dose: 10 g twice daily after meals
- Anupana (vehicle): lukewarm milk (for Rasayana effect) or Guduchi decoction (for cancer patients)
- Course Duration: 3–6 months with clinical monitoring
Potency Rationale
- Kanchnar, Varuna, Triphala, Neem, Turmeric – anti-tumor, anti-inflammatory, Mutravaha Srotas cleansing
- Punarnava, Kutki, Musta – detoxification, kidney-liver support
- Guggulu + Rasayanas (Guduchi, Ashwagandha, Shatavari) – immune support, anti-metastatic
- Bhasmas (Swarna, Abhrak, Heerak, Lauh, Tamra, Praval, Godanti) – Ojas promotion, systemic Rasayana, cellular resilience
- Ghrita + Honey – improve assimilation, deep tissue delivery
⚠️ Warning
This Avaleha is a potent Rasayana formulation that combines multiple herbs and mineral Bhasmas.
- It must only be prepared and prescribed under the guidance of a qualified Ayurvedic doctor.
- Every human body is different; therefore, ingredients and their weights will vary based on the patient’s Prakriti, disease stage, strength, and co-morbidities.
- Self-preparation or unsupervised intake may cause harm.
FAQs
Q1. What is Kanchnar Guggulu Avaleha and why is it used in bladder cancer or UTUC?
Kanchnar Guggulu Avaleha is a classical Ayurvedic formulation described in Bhaishajya Ratnavali under Granthi and Arbuda Chikitsa. It combines tumor-reducing herbs like Kanchnar and Varuna with Rasayana botanicals and mineral Bhasmas. In oncology care, it is valued for reducing abnormal tissue growth, cleansing Rakta and Mutravaha Srotas, and enhancing immunity [25].
Q2. How does it work compared to modern cancer treatments?
While surgery and chemotherapy remove or kill tumor cells, Ayurveda focuses on the biological terrain. Kanchnar Guggulu Avaleha aims to dissolve masses, detoxify the body, and strengthen Ojas (vital energy) so recurrence risk is lowered. It is often considered complementary rather than a replacement [26].
Q3. Can every patient take the same formulation?
No. Every person has a unique constitution (Prakriti) and disease state. An Ayurvedic doctor adjusts the exact herb weights and Bhasma inclusion depending on age, strength, comorbidities, and treatment history. This individualized approach is central to safety and effectiveness [27].
Q4. What is the usual dosage?
The commonly recommended dose is 10 g twice daily, after meals, usually taken with milk or Guduchi decoction. However, this can vary depending on the patient’s condition and digestion (Agni). Therefore, exact dosing must be supervised by a physician [28].
Q5. Are there any side effects?
When prepared and prescribed properly, Avaleha is generally safe. But unsupervised use of Bhasmas like Swarna, Abhrak, or Heerak may be harmful if quality or dosage is not controlled. Possible risks include digestive upset or metabolic imbalance if misused [29].
Q6. Can it be used along with chemotherapy or immunotherapy?
Yes, but only under medical supervision. Studies and clinical experience suggest Rasayana herbs like Guduchi, Ashwagandha, and Amalaki may reduce chemotherapy side effects and improve immune function. Still, interactions must be monitored closely
[30].
Q7. How long should this medicine be continued?
Typically, treatment is continued for 3 to 6 months, with regular monitoring of symptoms, strength, blood counts, and kidney-liver function. Duration may be extended in high-risk or recurrent cases
[31].
Q8. Is it safe for everyone with bladder cancer or UTUC?
Not necessarily. Pregnant women, patients with severe organ failure, or those unfit for Bhasma-based medicines may need alternative herbal-only formulations. This is why personalized assessment by an Ayurvedic physician is essential [32].
Q9. Where should the medicine be prepared?
It should only be prepared in GMP-certified Ayurvedic pharmacies or under direct supervision of qualified Rasashastra experts, since handling Bhasmas requires expertise and safety measures
[33].
Q10. Can this formulation cure cancer completely?
Ayurveda does not make blanket claims. Kanchnar Guggulu Avaleha is designed to target the root imbalance and support long-term healing, while reducing recurrence risk. In early stages, it may provide significant benefits; in advanced stages, it is best used integratively with modern therapies
[34].
References
[62] Sylvester, R. J., van der Meijden, A. P. M., & Oosterlinck, W. (2006). Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: A combined analysis of 2596 patients from seven EORTC trials. European Urology, 49(3), 466–475. https://doi.org/10.1016/j.eururo.2005.12.031
[64] Cancer Genome Atlas Research Network. (2017). Comprehensive molecular characterization of urothelial bladder carcinoma. Cell, 171(3), 540–556. https://doi.org/10.1016/j.cell.2017.09.007
[83] Babjuk, M., Burger, M., Compérat, E. M., Gontero, P., Mostafid, A. H., Palou, J., van Rhijn, B. W. G., Rouprêt, M., Shariat, S. F., Sylvester, R., Zigeuner, R., Capoun, O., Cohen, D., Hernandez, V., Larré, S., Peyronnet, B., Seisen, T., Soukup, V., & Soria, F. (2022). European Association of Urology guidelines on non–muscle-invasive bladder cancer. European Urology, 81(1), 75–94. https://doi.org/10.1016/j.eururo.2021.08.010
[84] Chang, S. S., Boorjian, S. A., Chou, R., Clark, P. E., Daneshmand, S., Konety, B. R., … & Kamat, A. M. (2016). Diagnosis and treatment of non–muscle invasive bladder cancer: AUA/SUO guideline. Journal of Urology, 196(4), 1021–1029. https://doi.org/10.1016/j.juro.2016.06.049
[91] Bellmunt, J., de Wit, R., Vaughn, D. J., Fradet, Y., Lee, J. L., Fong, L., … & Bajorin, D. F. (2017). Pembrolizumab as second-line therapy for advanced urothelial carcinoma. New England Journal of Medicine, 376(11), 1015–1026. https://doi.org/10.1056/NEJMoa1613683
[94] Robertson, A. G., Kim, J., Al-Ahmadie, H., Bellmunt, J., Guo, G., Cherniack, A. D., … & TCGA Research Network. (2017). Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell, 171(3), 540–556. https://doi.org/10.1016/j.cell.2017.09.007
[108] Sharma, P. V. (1995). Charaka Samhita (Text with English Translation), Vol. II, Chikitsa Sthana 7/30 – Mutraghata Chikitsa. Chaukhambha Orientalia.
[109] Singh, R. H. (1992). Rasayana Therapy in Classical and Contemporary Ayurveda. Chaukhambha Bharati Academy.
[112] Rouprêt, M., Babjuk, M., Burger, M., Capoun, O., Cohen, D., Comperat, E. M., … & Shariat, S. F. (2021). European Association of Urology guidelines on upper urinary tract urothelial carcinoma. European Urology, 79(1), 62–79. https://doi.org/10.1016/j.eururo.2020.08.014
[127] Böhle, A., & Bock, P. R. (2004). Intravesical bacillus Calmette-Guerin versus mitomycin C in superficial bladder cancer: Formal meta-analysis of comparative studies on tumor progression. Urology, 63(4), 682–686. https://doi.org/10.1016/j.urology.2003.11.032
[133] Mishra, S., & Tiwari, V. (2010). Clinical efficacy of Varunadi Guggulu in the management of Mutraghata (urinary obstruction). AYU (An International Quarterly Journal of Research in Ayurveda), 31(2), 251–256. https://doi.org/10.4103/0974-8520.72395
[138] Kamoun, A., de Reyniès, A., Allory, Y., Sjödahl, G., Robertson, A. G., Seiler, R., … & Bladder Cancer Molecular Taxonomy Group. (2020). A consensus molecular classification of muscle-invasive bladder cancer. European Urology, 77(4), 420–433. https://doi.org/10.1016/j.eururo.2019.09.006
[141] Hollstein, M., Sidransky, D., Vogelstein, B., & Harris, C. C. (1991). p53 mutations in human cancers. Science, 253(5015), 49–53. https://doi.org/10.1126/science.1905840
[145] Amin, M. B., McKenney, J. K., Paner, G. P., Hansel, D. E., Grignon, D. J., & Montironi, R. (2013). ICUD-EAU International Consultation on Bladder Cancer 2012: Pathology. European Urology, 63(1), 16–35. https://doi.org/10.1016/j.eururo.2012.09.054
[147] Cutress, M. L., Stewart, G. D., Zakikhani, P., Phipps, S., Thomas, B. G., Tolley, D. A., & Smith, G. (2012). Ureteroscopic and percutaneous management of upper tract urothelial carcinoma (UTUC): Systematic review. BJU International, 110(5), 614–628. https://doi.org/10.1111/j.1464-410X.2012.11007.x
[162] Mishra, S., & Bhagwan Dash. (2005). Bhaishajya Ratnavali of Govind Dasji (Text with English Commentary), Chapter 44 – Granthi Arbuda Chikitsa. Chaukhambha Sanskrit Series Office.
[166] Srikantha Murthy, K. R. (1999). Sushruta Samhita (English Translation), Vol. II, Nidana and Chikitsa Sthana – Arbuda Nidana. Chaukhambha Orientalia.
[176] Dwivedi, V., & Dwivedi, L. N. (2007). Principles of Nidan Parivarjana in Ayurvedic oncology: Relevance in modern preventive oncology. AYU, 28(3), 9–15. https://www.ayujournal.org/text.asp?2007/28/3/9/80690
All Source
- Sylvester, R. J., van der Meijden, A. P. M., & Oosterlinck, W. (2006). Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: A combined analysis of 2596 patients from seven EORTC trials. European Urology, 49(3), 466–475. https://doi.org/10.1016/j.eururo.2005.12.031 ↩
- Bellmunt, J., de Wit, R., Vaughn, D. J., Fradet, Y., Lee, J. L., Fong, L., … & Bajorin, D. F. (2017). Pembrolizumab as second-line therapy for advanced urothelial carcinoma. New England Journal of Medicine, 376(11), 1015–1026. https://doi.org/10.1056/NEJMoa1613683 ↩
- Mishra, S., & Bhagwan Dash. (2005). Bhaishajya Ratnavali of Govind Dasji (Text with English Commentary), Chapter 44 – Granthi Arbuda Chikitsa. Chaukhambha Sanskrit Series Office. ↩
- Hollstein, M., Sidransky, D., Vogelstein, B., & Harris, C. C. (1991). p53 mutations in human cancers. Science, 253(5015), 49–53. https://doi.org/10.1126/science.1905840 ↩
- Sharma, P. V. (1995). Charaka Samhita (Text with English Translation), Vol. II, Chikitsa Sthana 7/30 – Mutraghata Chikitsa. Chaukhambha Orientalia. ↩
- Chang, S. S., Boorjian, S. A., Chou, R., Clark, P. E., Daneshmand, S., Konety, B. R., … & Kamat, A. M. (2016). Diagnosis and treatment of non–muscle invasive bladder cancer: AUA/SUO guideline. Journal of Urology, 196(4), 1021–1029. https://doi.org/10.1016/j.juro.2016.06.049 ↩
- Mishra, S., & Bhagwan Dash. (2005). Bhaishajya Ratnavali of Govind Dasji (Text with English Commentary), Chapter 44 – Granthi Arbuda Chikitsa. Chaukhambha Sanskrit Series Office. ↩
- Sharma, P. V. (1995). Charaka Samhita (Text with English Translation), Vol. II, Chikitsa Sthana 7/30 – Mutraghata Chikitsa. Chaukhambha Orientalia. ↩
- Babjuk, M., Burger, M., Compérat, E. M., Gontero, P., Mostafid, A. H., Palou, J., van Rhijn, B. W. G., Rouprêt, M., Shariat, S. F., Sylvester, R., Zigeuner, R., Capoun, O., Cohen, D., Hernandez, V., Larré, S., Peyronnet, B., Seisen, T., Soukup, V., & Soria, F. (2022). European Association of Urology guidelines on non–muscle-invasive bladder cancer. European Urology, 81(1), 75–94. https://doi.org/10.1016/j.eururo.2021.08.010 ↩
- Amin, M. B., McKenney, J. K., Paner, G. P., Hansel, D. E., Grignon, D. J., & Montironi, R. (2013). ICUD-EAU International Consultation on Bladder Cancer 2012: Pathology. European Urology, 63(1), 16–35. https://doi.org/10.1016/j.eururo.2012.09.054 ↩
- Cancer Genome Atlas Research Network. (2017). Comprehensive molecular characterization of urothelial bladder carcinoma. Cell, 171(3), 540–556. https://doi.org/10.1016/j.cell.2017.09.007 ↩
- Robertson, A. G., Kim, J., Al-Ahmadie, H., Bellmunt, J., Guo, G., Cherniack, A. D., … & TCGA Research Network. (2017). Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell, 171(3), 540–556. https://doi.org/10.1016/j.cell.2017.09.007 ↩
- Kamoun, A., de Reyniès, A., Allory, Y., Sjödahl, G., Robertson, A. G., Seiler, R., … & Bladder Cancer Molecular Taxonomy Group. (2020). A consensus molecular classification of muscle-invasive bladder cancer. European Urology, 77(4), 420–433. https://doi.org/10.1016/j.eururo.2019.09.006 ↩
- Srikantha Murthy, K. R. (1999). Sushruta Samhita (English Translation), Vol. II, Nidana and Chikitsa Sthana – Arbuda Nidana. Chaukhambha Orientalia. ↩
- Chang, S. S., Boorjian, S. A., Chou, R., Clark, P. E., Daneshmand, S., Konety, B. R., … & Kamat, A. M. (2016). Diagnosis and treatment of non–muscle invasive bladder cancer: AUA/SUO guideline. Journal of Urology, 196(4), 1021–1029. https://doi.org/10.1016/j.juro.2016.06.049 ↩
- Böhle, A., & Bock, P. R. (2004). Intravesical bacillus Calmette-Guerin versus mitomycin C in superficial bladder cancer: Formal meta-analysis of comparative studies on tumor progression. Urology, 63(4), 682–686. https://doi.org/10.1016/j.urology.2003.11.032 ↩
- Bellmunt, J., de Wit, R., Vaughn, D. J., Fradet, Y., Lee, J. L., Fong, L., … & Bajorin, D. F. (2017). Pembrolizumab as second-line therapy for advanced urothelial carcinoma. New England Journal of Medicine, 376(11), 1015–1026. https://doi.org/10.1056/NEJMoa1613683 ↩
- Rouprêt, M., Babjuk, M., Burger, M., Capoun, O., Cohen, D., Comperat, E. M., … & Shariat, S. F. (2021). European Association of Urology guidelines on upper urinary tract urothelial carcinoma. European Urology, 79(1), 62–79. https://doi.org/10.1016/j.eururo.2020.08.014 ↩
- Cutress, M. L., Stewart, G. D., Zakikhani, P., Phipps, S., Thomas, B. G., Tolley, D. A., & Smith, G. (2012). Ureteroscopic and percutaneous management of upper tract urothelial carcinoma (UTUC): Systematic review. BJU International, 110(5), 614–628. https://doi.org/10.1111/j.1464-410X.2012.11007.x ↩
- Robertson, A. G., Kim, J., Al-Ahmadie, H., Bellmunt, J., Guo, G., Cherniack, A. D., … & TCGA Research Network. (2017). Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell, 171(3), 540–556. https://doi.org/10.1016/j.cell.2017.09.007 ↩
- Mishra, S., & Bhagwan Dash. (2005). Bhaishajya Ratnavali of Govind Dasji (Text with English Commentary), Chapter 44 – Granthi Arbuda Chikitsa. Chaukhambha Sanskrit Series Office. ↩
- Mishra, S., & Tiwari, V. (2010). Clinical efficacy of Varunadi Guggulu in the management of Mutraghata (urinary obstruction). AYU (An International Quarterly Journal of Research in Ayurveda), 31(2), 251–256. https://doi.org/10.4103/0974-8520.72395 ↩
- Singh, R. H. (1992). Rasayana Therapy in Classical and Contemporary Ayurveda. Chaukhambha Bharati Academy. ↩
- Dwivedi, V., & Dwivedi, L. N. (2007). Principles of Nidan Parivarjana in Ayurvedic oncology: Relevance in modern preventive oncology. AYU, 28(3), 9–15. https://www.ayujournal.org/text.asp?2007/28/3/9/80690 ↩
- Mishra, S., & Bhagwan Dash. (2005). Bhaishajya Ratnavali of Govind Dasji (Text with English Commentary), Chapter 44 – Granthi Arbuda Chikitsa. Chaukhambha Sanskrit Series Office. ↩
- Mishra, S., & Tiwari, V. (2010). Clinical efficacy of Varunadi Guggulu in the management of Mutraghata (urinary obstruction). AYU (An International Quarterly Journal of Research in Ayurveda), 31(2), 251–256. https://doi.org/10.4103/0974-8520.72395 ↩
- Dwivedi, V., & Dwivedi, L. N. (2007). Principles of Nidan Parivarjana in Ayurvedic oncology: Relevance in modern preventive oncology. AYU, 28(3), 9–15. https://www.ayujournal.org/text.asp?2007/28/3/9/80690 ↩
- Sharma, P. V. (1995). Charaka Samhita (Text with English Translation), Vol. II, Chikitsa Sthana 7/30 – Mutraghata Chikitsa. Chaukhambha Orientalia. ↩
- Hollstein, M., Sidransky, D., Vogelstein, B., & Harris, C. C. (1991). p53 mutations in human cancers. Science, 253(5015), 49–53. https://doi.org/10.1126/science.1905840 ↩
- Robertson, A. G., Kim, J., Al-Ahmadie, H., Bellmunt, J., Guo, G., Cherniack, A. D., … & TCGA Research Network. (2017). Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell, 171(3), 540–556. https://doi.org/10.1016/j.cell.2017.09.007 ↩
- Cancer Genome Atlas Research Network. (2017). Comprehensive molecular characterization of urothelial bladder carcinoma. Cell, 171(3), 540–556. https://doi.org/10.1016/j.cell.2017.09.007 ↩
- Babjuk, M., Burger, M., Compérat, E. M., Gontero, P., Mostafid, A. H., Palou, J., van Rhijn, B. W. G., Rouprêt, M., Shariat, S. F., Sylvester, R., Zigeuner, R., Capoun, O., Cohen, D., Hernandez, V., Larré, S., Peyronnet, B., Seisen, T., Soukup, V., & Soria, F. (2022). European Association of Urology guidelines on non–muscle-invasive bladder cancer. European Urology, 81(1), 75–94. https://doi.org/10.1016/j.eururo.2021.08.010 ↩
- Amin, M. B., McKenney, J. K., Paner, G. P., Hansel, D. E., Grignon, D. J., & Montironi, R. (2013). ICUD-EAU International Consultation on Bladder Cancer 2012: Pathology. European Urology, 63(1), 16–35. https://doi.org/10.1016/j.eururo.2012.09.054 ↩
- Kamoun, A., de Reyniès, A., Allory, Y., Sjödahl, G., Robertson, A. G., Seiler, R., … & Bladder Cancer Molecular Taxonomy Group. (2020). A consensus molecular classification of muscle-invasive bladder cancer. European Urology, 77(4), 420–433. https://doi.org/10.1016/j.eururo.2019.09.006 ↩