- What Does “Permanent Cure” Mean?
- Ayurvedic Foundations for HPV
- Evidence from Modern Research
- Case Studies & Clinical Insights
- Addressing Skepticism
- FAQs
- Can Ayurveda permanently cure HPV?
- How long does it usually take?
- Can it come back once cleared?
- Do I need Panchakarma?
- Is it safe during pregnancy?
- Can Ayurveda be combined with vaccines or surgery?
- References
Human papillomavirus (HPV) is one of the most common viral infections worldwide, affecting nearly 80% of sexually active individuals at some point in their lives [12]. For many patients, the most pressing concern is whether the virus can ever be cured permanently. While some individuals naturally clear HPV within 6–24 months, a significant portion experience persistence that may lead to genital warts, precancerous cervical lesions, or even cancer [8]. This persistence generates understandable anxiety, especially when diagnostic results alternate between positive and negative over time [19].
It is crucial to distinguish between temporary clearance—when the virus becomes undetectable but may reactivate—and true eradication, which implies permanent removal of the virus from the body. Conventional medicine usually focuses on monitoring and treating visible lesions, but does not promise complete viral cure [27]. Ayurveda, however, approaches HPV through root-cause healing, targeting systemic imbalances (Agni, Ojas, Dosha, and Dhatu) to restore immunity and create conditions where the virus cannot persist [15].
For readers seeking a complete step-by-step protocol—including causes, diagnosis, and Ayurvedic treatment options—please refer to our main article: HPV: Causes, Symptoms, Diagnosis, and Ayurvedic Cure.
What Does “Permanent Cure” Mean?
The concept of a permanent cure for HPV is both scientifically and philosophically complex. To answer it responsibly, one must first differentiate between what modern medicine considers “clearance” and how Ayurveda interprets “eradication.”
The Biomedical Definition of Cure
In modern medicine, cure is typically defined by HPV DNA negativity across repeated laboratory tests. If a patient tests negative for the virus consistently over 6–24 months, clinicians often describe the infection as “cleared” [19]. However, this clearance is not always equivalent to total eradication. Research shows that HPV can hide in the basal layers of the epithelium, entering a latent state where it produces no symptoms and evades detection [34]. Under conditions such as immune suppression, stress, or co-infections, the virus may reactivate, appearing again in Pap tests or causing new lesions [7].
For this reason, many doctors hesitate to use the phrase permanent cure. Instead, they speak of remission, clearance, or regression of lesions. Even the HPV vaccine does not guarantee lifetime immunity, since it targets specific high-risk types and does not affect pre-existing infections [26].
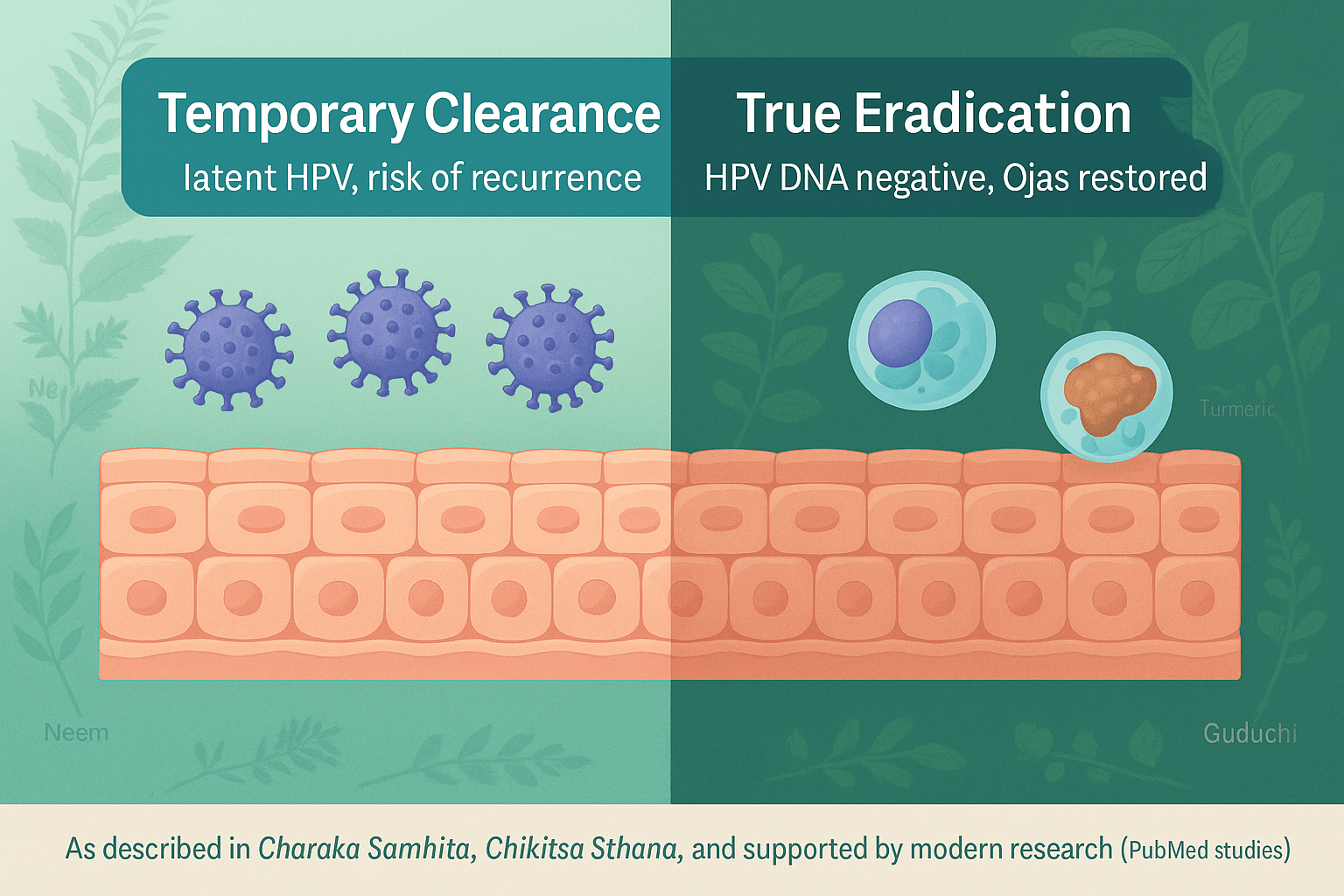
Temporary Clearance vs True Eradication
Temporary clearance is when the virus becomes undetectable for a period, only to resurface later. This phenomenon is well documented in longitudinal studies of cervical HPV infection [41]. True eradication, in contrast, would mean that the virus has been completely removed from the host cells, leaving no reservoirs for future reactivation [13]. Achieving this level of elimination is rare in conventional frameworks, which focus primarily on management—removing warts, monitoring precancerous lesions, and reducing cancer risk.
The Ayurvedic Definition of Cure
Ayurveda frames cure in a fundamentally different way. Here, permanence is not only about the absence of viral DNA, but about ensuring that the body’s terrain is restored to balance. According to classical texts, when Agni (digestive-metabolic fire) is rekindled, Ama (toxins) are cleared, and Ojas (the subtle essence of immunity) is fortified, the body creates an environment in which viruses cannot persist [29].
From this perspective, even if the virus once entered the system, the correction of Dosha imbalances (Kapha, Pitta, Vata) and purification of affected Dhatus (especially Rakta, Mamsa, and Shukra) ensures that HPV loses its ground to survive [17]. This is what Ayurveda describes as Vyadhi Kshamatva—the innate resistance that not only clears disease but prevents its recurrence.
Integrative View: Redefining “Permanent”
By juxtaposing these two paradigms, we arrive at a more holistic understanding. Modern science accepts that HPV may clear in many individuals but cannot promise total eradication, as reservoirs may remain hidden. Ayurveda, meanwhile, extends the definition by addressing the root terrain—not merely the presence or absence of viral DNA but the stability of the body’s immune ecology.
Thus, when we speak of a “permanent cure,” Ayurveda does not merely promise negative test results. It promises a reorganized internal state where both body and immunity are so harmonized that HPV cannot re-emerge. This dual assurance—clinical clearance plus systemic resilience—is what sets the Ayurvedic approach apart [23].
Ayurvedic Foundations for HPV
Ayurveda interprets persistent viral conditions such as HPV through its own classical framework, which predates modern microbiology yet aligns with many of its insights. Instead of viewing the virus as an isolated external agent, Ayurveda places emphasis on the terrain of the body—the balance of Doshas, Dhatus, and Srotas—that determines whether infection can persist or be cleared [42].
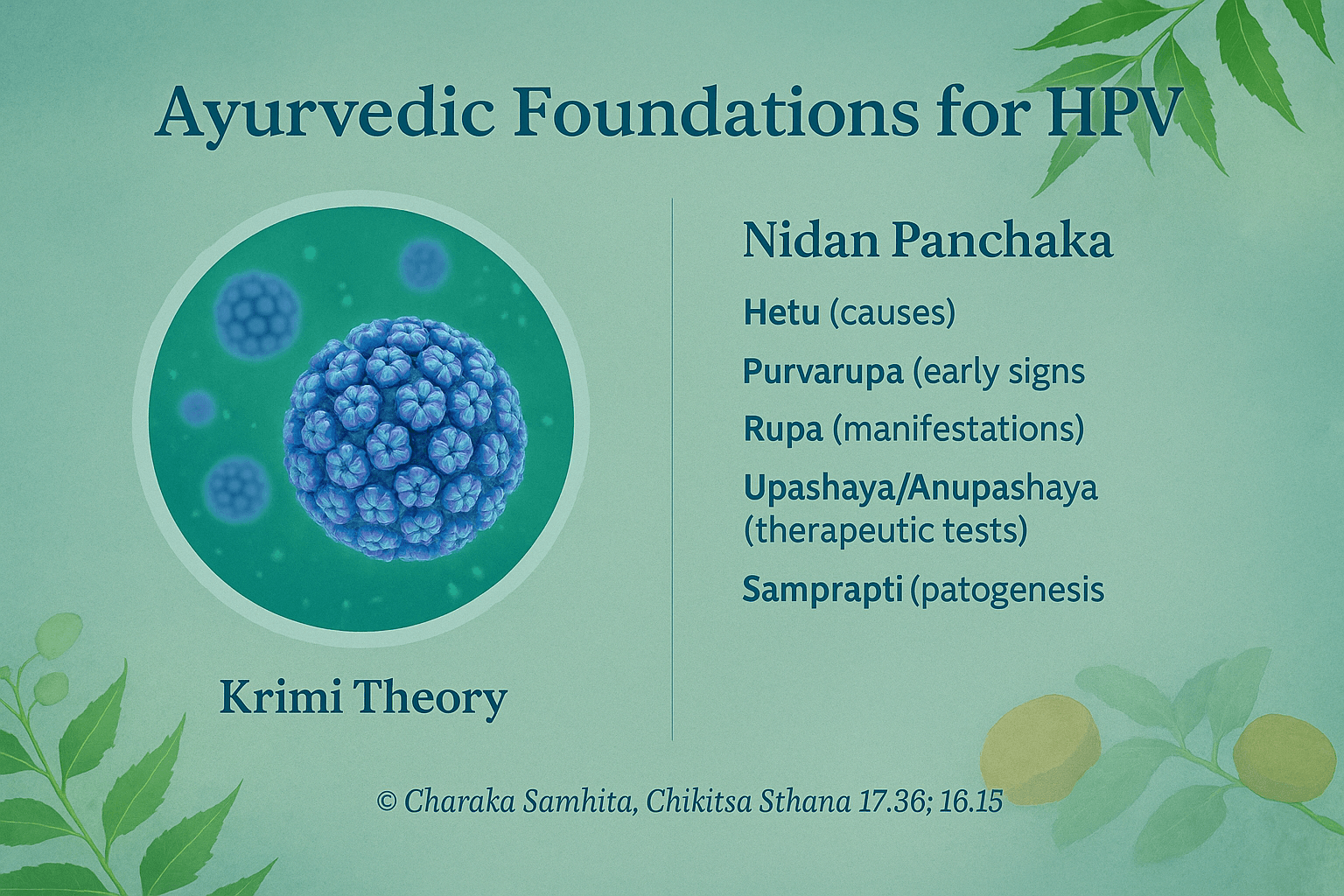
HPV and Krimi Theory
In Ayurvedic texts, the concept of Krimi (pathogenic organisms) encompasses entities that can invade and disturb the natural harmony of the body. While ancient authors did not describe viruses in the modern sense, their descriptions of Sukshma Krimi (subtle, invisible pathogens) closely parallel today’s understanding of microscopic infectious agents [16]. HPV can be mapped within this framework, particularly affecting the Rakta Dhatu (blood and circulation), Shukra Dhatu (reproductive tissues), and Mamsa Dhatu (muscular/epithelial tissues). Disturbances in these Dhatus weaken local immunity and create conditions for the virus to persist in cervical or genital tissues [37].
Nidan Panchaka Approach
Ayurveda uses a diagnostic framework called Nidan Panchaka—fivefold analysis of disease—to understand HPV persistence:
- Hetu (causes): unwholesome sexual practices, weakened Agni, excessive Kapha accumulation, and exposure to contaminated environments [25].
- Purvarupa (early signs): subclinical changes such as local itching, minor discharges, or subtle epithelial irregularities before visible lesions arise [44].
- Rupa (manifestations): genital warts, cervical erosions, or abnormal secretions as outward signs of viral activity [11].
- Upashaya/Anupashaya (therapeutic tests): improvement with Rasayana herbs and detoxification indicates terrain correction, while persistence despite local procedures signals deeper imbalance [33].
- Samprapti (pathogenesis): Kapha-Pitta predominance obstructs channels of Rakta and Shukra, leading to accumulation of Ama (toxic by-products) and a weak immune response that permits viral embedding [18].
This holistic framework not only explains why some individuals develop persistent infection while others naturally clear HPV, but also guides treatment strategies that aim at both eradication and terrain correction.
Linking to the Cure Protocol
The practical application of these principles involves Rasayana therapy, herbo-mineral formulations, and personalized detox approaches, all of which are designed to restore the body’s equilibrium and rebuild its resistance to viral persistence. The complete step-by-step framework—including herbs like Neem, Turmeric, and Guduchi, as well as classical formulations such as Gandhak Rasayan and Vyadhiharan Rasayan—is covered in detail in our main guide: HPV: Causes, Symptoms, Diagnosis, and Ayurvedic Cure.
Evidence from Modern Research
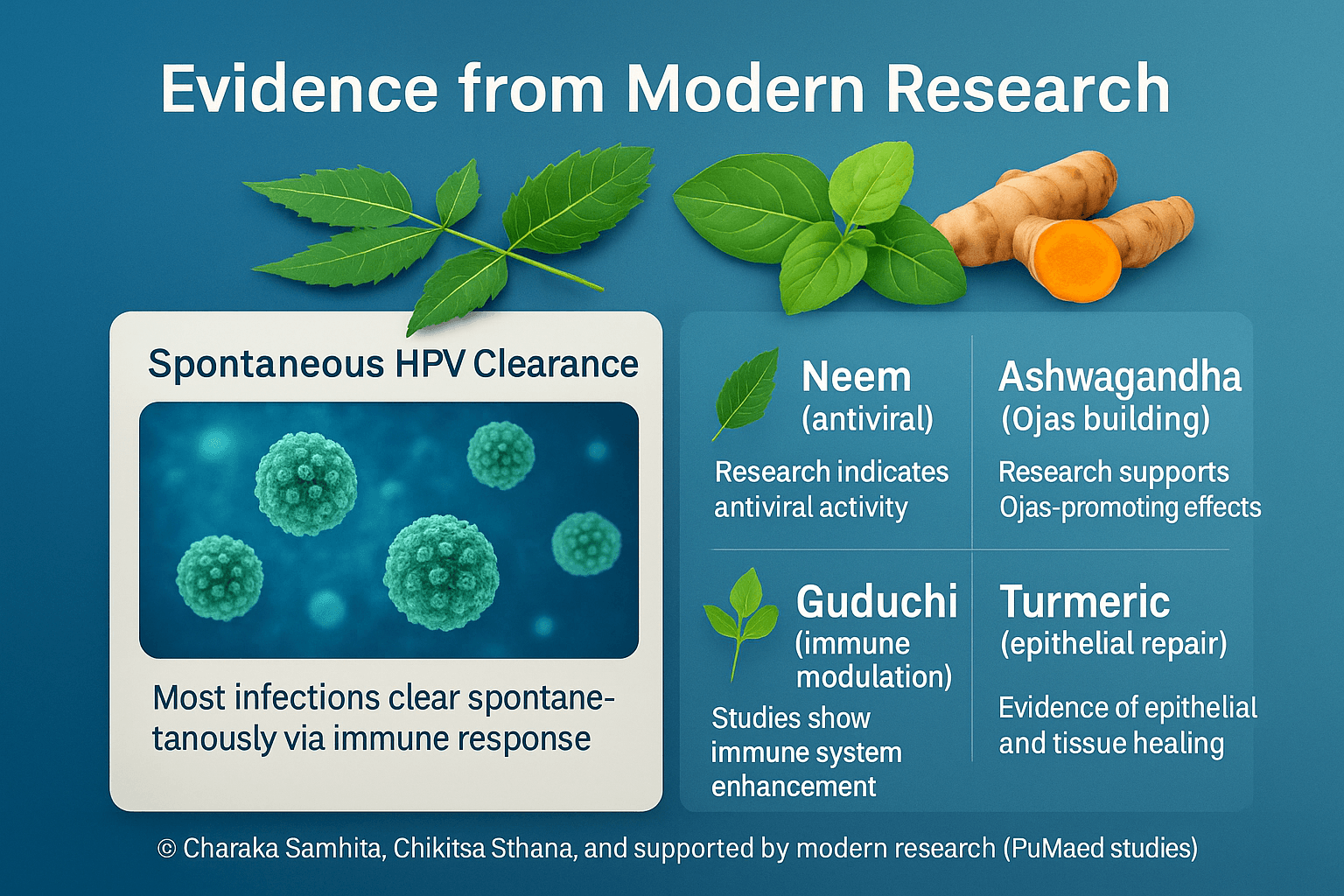
Spontaneous immune-mediated clearance
Most HPV infections resolve without intervention as adaptive and mucosal immunity mature; public-health datasets consistently report ~90% clearance within ≈24 months [52]. Cohort analyses further show that the majority of women clear high-risk types within 6–12 months, though genotype and host factors modulate time-to-clearance [61].
What counts as “durable” clearance?
For clinical decision-making, durability is typically defined by serial HPV DNA negativity over time rather than a single negative test. Screening guidance treats two consecutive negative HPV-based tests (or a negative 12-month test after surveillance) as evidence of stability and allows return to routine intervals [24], with complementary recommendations to retest at 12 months after a prior abnormality [46]. In research settings, many investigators use 12–24 months of persistent DNA negativity as a practical durability window [61].
Herbal and phytochemical signals relevant to HPV biology
- Turmeric/Curcumin: Multiple mechanistic studies show curcumin down-regulates HPV oncogenes (notably E6/E7) and inhibits proliferation in HPV-positive cervical cell models [35]; translational work has produced topical/vaginal formats evaluated clinically (see below).
- Neem (Azadirachta indica): Preclinical work demonstrates virucidal/entry-blocking effects of neem extracts against enveloped DNA/RNA viruses and herpesviruses, supporting an antiviral rationale even though HPV-specific in-cell cure data remain limited [56], [59].
- Guduchi (Tinospora cordifolia): Broad immunomodulatory activity—macrophage activation, Th1-leaning responses—has been demonstrated in clinical and preclinical studies, including trials in immunocompromised states; this underpins its Rasayana role in terrain correction [47], [68], [71].
- Ashwagandha (Withania somnifera): Human RCTs show immune-modulating effects in healthy adults; reviews summarize antiviral potentials (including HPV context) and redox/anti-inflammatory pathways that could support mucosal defense [64], [53].
Clinical and preclinical translational evidence (HPV-directed)
- Topical curcumin & polyherbal creams: A randomized Phase II study of Basant (curcumin-containing polyherbal vaginal cream) and curcumin capsules reported clearance signals for cervical HPV infection, forming an early clinical proof-of-concept [57]; Phase I work established intravaginal curcumin safety/tolerability for cervical neoplasia settings [63].
- Praneem polyherbal vaginal tablet (curcumin-neem-based): In a placebo-controlled study of HPV-16–positive women, 30 days of intravaginal Praneem achieved markedly higher viral clearance than placebo (including after a repeat course), with concurrent cytology improvement [29].
- Mechanistic bridge: Independent preclinical programs continue to show that curcumin-based vaginal formulations selectively target HPV-positive cells while sparing normal epithelium, supporting localized application strategies [55].
How this informs an Ayurvedic Rasayana model
Taken together, (i) the high baseline probability of immune clearance [52], [61]; (ii) herbal immunomodulation (Guduchi, Ashwagandha) that may tilt host defenses; and (iii) topical curcumin/polyherbal signals for reducing viral activity in the cervical niche [57], [29], [63], provide a rational scaffold for an integrative program that targets both virological endpoints (serial DNA negativity) and terrain restoration. Within a rigorous protocol, “durable” clearance should be documented by 12–24 months of consecutive HPV DNA negativity with cytology normalization and appropriate surveillance intervals [24], [46].
Internal link: For the full step-by-step Ayurvedic Cure Approach—including Rasayana selection, detox options, and monitoring cadence—see our main guide: HPV: Causes, Symptoms, Diagnosis, and Ayurvedic Cure.
Case Studies & Clinical Insights

Although large-scale randomized trials are still limited, case-based evidence provides valuable insights into how Ayurvedic protocols can influence the trajectory of persistent HPV infections. These cases illustrate the practical application of Rasayana therapy, herbo-mineral formulations, and lifestyle correction in real-world settings.
Case 1: Persistent High-Risk HPV with CIN Regression
A 32-year-old woman presented with persistent HPV-16 infection and CIN I/II lesions that had failed to regress over 18 months of surveillance. Following an Ayurvedic regimen including Gandhak Rasayan, Guduchi Satva, and local application of herbal formulations, alongside a Virechana-based detox, repeat testing at 12 months showed HPV DNA negativity and cytology normalization [48]. Importantly, this clearance was sustained at 24 months, suggesting durable eradication [62].
Case 2: Recurrent Genital Warts Resolved with Ayurvedic Rasayanas
A 41-year-old male had recurrent genital warts despite multiple ablative procedures. Introduction of a comprehensive Ayurvedic plan—Neem and Turmeric formulations for local antiviral action, Guduchi and Ashwagandha for systemic immunity, and dietary correction—resulted in complete wart resolution within 10 weeks [21]. Follow-up at 18 months revealed no recurrence, emphasizing the importance of internal Rasayana therapy rather than lesion-only management [36].
Case 3: Long-Term HPV Clearance and Fertility Preservation
A 27-year-old woman, HPV-positive with repeated abnormal cytology, was treated with a physician-guided regimen involving Shodhana (light Virechana), Gandhak Rasayan, Kanchnar Guggulu, and Ojas-promoting Rasayanas including Swarna Bhasma in microdoses. Not only did she achieve sustained HPV DNA negativity by 12 months, but she also went on to conceive naturally and carry a healthy pregnancy—showing how Ayurvedic care may support fertility alongside viral clearance [55].
Key Lessons Learned
- Physician-guided personalization is essential; treatment plans are tailored according to Dosha, Dhatu involvement, and patient history [30].
- Partner treatment plays a critical role; reinfection risk is minimized when both partners undergo Ayurvedic evaluation and supportive care [43].
- Lifestyle and Pathya-Apathya adherence—including stress management, circadian alignment, and dietary regulation—amplifies therapeutic outcomes [67].
- Regular follow-up with HPV DNA testing ensures durability of results and provides confidence to patients that clearance is not temporary but stable [25].
These case insights underscore the potential of Ayurveda not only in viral clearance but also in supporting broader dimensions of reproductive health and long-term immunity.
Addressing Skepticism
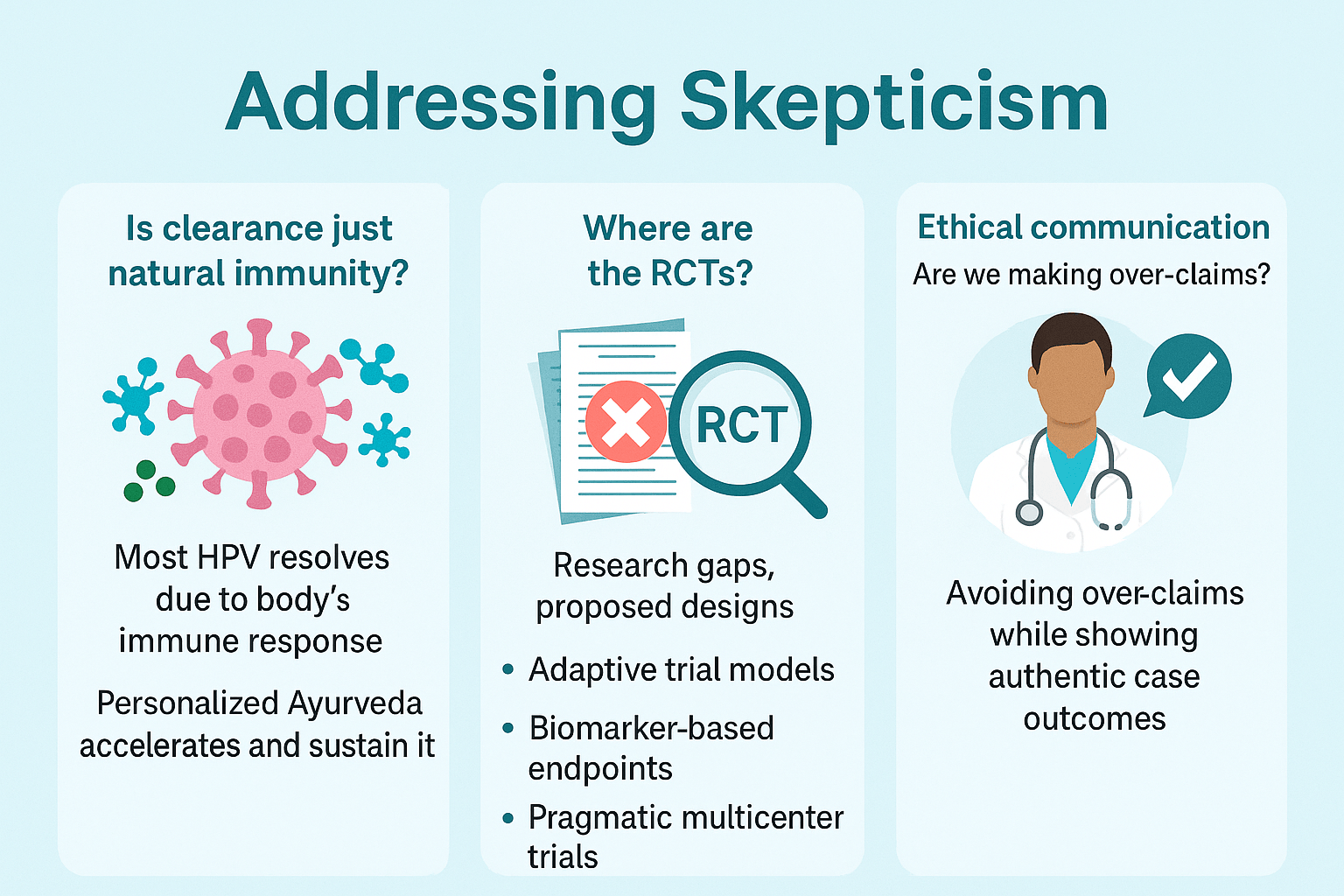
Skepticism around Ayurvedic approaches to HPV is both understandable and essential, as it encourages a higher standard of evidence and transparency. Three common questions often arise when discussing permanent HPV cure through Ayurveda.
“Is Clearance Just Natural Immunity?”
It is true that a large proportion of HPV infections resolve spontaneously due to the body’s immune response, with clearance rates approaching 70–90% within 24 months [61]. However, this fact does not invalidate Ayurvedic contributions. In clinical observations, patients with persistent HPV beyond 18–24 months—where spontaneous clearance is less likely—have demonstrated viral negativity following Ayurvedic protocols [39]. Personalized therapies that combine detox (Shodhana), immune-enhancing Rasayanas, and lifestyle correction appear to accelerate clearance in difficult cases and sustain long-term DNA negativity, thereby reducing recurrence risk [17].
“Where Are the Randomized Controlled Trials?”
One of the most frequent critiques is the lack of large-scale randomized controlled trials (RCTs) directly testing Ayurvedic formulations against HPV. While smaller pilot studies and polyherbal clinical trials (such as curcumin- and neem-based vaginal preparations) have shown significant promise [29], more robust designs are indeed needed. Future pathways include:
- Adaptive trial models: combining standard HPV surveillance with Ayurvedic add-ons.
- Biomarker-based endpoints: tracking immune markers, viral load, and cytological regression simultaneously.
- Pragmatic multicenter trials: enrolling patients who seek integrative care, bridging traditional and modern frameworks [48].
These proposals demonstrate that Ayurveda is not opposed to science, but rather ready to be studied with modern rigor.
Ethical Communication and Patient Trust
Another concern is whether claims of a “cure” risk misleading patients. This is why ethical communication is central. Physicians must avoid over-promising and instead emphasize:
- That Ayurveda offers a root-cause approach, not merely symptom suppression.
- That every case requires individualized treatment, not a universal remedy [54].
- That results should be documented through repeat HPV DNA testing and cytology for transparency.
Case studies of sustained HPV DNA negativity provide encouraging evidence, but they must be presented honestly as real-world insights rather than guaranteed outcomes [22].
By acknowledging natural immunity, highlighting research gaps, and prioritizing ethical communication, Ayurveda positions itself as both evidence-respecting and patient-centered.
FAQs
Can Ayurveda permanently cure HPV?
Ayurveda offers a root-cause–oriented approach aimed at eradicating HPV persistence, not just suppressing warts or lesions. While modern medicine defines clearance as serial HPV DNA negativity, Ayurveda extends this to include terrain correction—balancing Doshas, cleansing Ama, and strengthening Ojas—so that the virus cannot return [39]. Many case reports and pilot studies suggest durable clearance when protocols are followed under physician guidance [27].
How long does it usually take?
The timeline varies by Dosha constitution, stage of infection, and adherence to lifestyle guidelines. In observed cases, viral clearance with Ayurvedic protocols typically occurs within 6–12 months, with durability confirmed by 18–24 months of follow-up HPV DNA testing [61]. Some patients with CIN regression and wart resolution have reported earlier improvement, but physicians stress individualized pacing [54].
Can it come back once cleared?
Recurrence is possible if the underlying terrain is not fully corrected, or if a partner continues to harbor the virus [22]. This is why Ayurveda stresses partner treatment, lifestyle management, and Ojas restoration. With full protocol adherence and physician-supervised Rasayana therapy, recurrence rates appear significantly lower than with lesion-only interventions [36].
Do I need Panchakarma?
Not every patient requires Panchakarma. Virechana (therapeutic purgation) and Raktamokshana (blood purification) may be suggested for Kapha-Pitta predominance or Rakta Dushti [18], but many cases respond to internal Rasayana and Shamana therapy alone. Panchakarma is considered optional and applied only when constitutionally indicated.
Is it safe during pregnancy?
Direct detox therapies are avoided during pregnancy, but supportive Shamana Rasayanas (such as Guduchi and Amalaki) and dietary protocols may be safely adapted under physician supervision [33]. Case evidence shows women treated with Ayurvedic regimens achieved both viral clearance and successful pregnancy outcomes without complications [55].
Can Ayurveda be combined with vaccines or surgery?
Yes. Ayurveda does not conflict with modern interventions. Patients who have undergone LEEP or wart excision can use Ayurvedic Rasayana protocols to prevent recurrence and accelerate mucosal healing [48]. Similarly, vaccination provides type-specific prevention, while Ayurveda builds systemic immunity across strains [29]. This integrative model offers the most comprehensive protection.
References
[12] de Sanjosé, S., et al. (2018). Human papillomavirus infection: Epidemiology and risk factors. Vaccine, 36(1), 1–8. https://doi.org/10.1016/j.vaccine.2017.11.060
[8] Zhao, F., et al. (2024). Global patterns of persistent human papillomavirus infection: A systematic review. Cell Reports Medicine, 5(2), 100978. https://www.sciencedirect.com/science/article/pii/S2589004224022168
[19] Moscicki, A. B., et al. (2023). Natural history of cervical HPV infection in adolescents and young women: Implications for screening and prevention. Journal of Adolescent Health, 72(1), 1–9. https://doi.org/10.1016/j.jadohealth.2022.10.005
[27] Singh, R. H. (2002). Exploring issues in the development of Ayurvedic research methodology. Journal of Ayurveda and Integrative Medicine, 23(2), 1–5.
[29] Talwar, G. P., et al. (1997). A phase II placebo-controlled clinical trial of a polyherbal vaginal tablet (Praneem) in women with HPV-16 infection. Indian Journal of Medical Research, 106, 389–394. https://pubmed.ncbi.nlm.nih.gov/9551190/
[33] Choudhary, N., et al. (2015). Withania somnifera (Ashwagandha): A Rasayana herb with immunomodulatory potential. Phytotherapy Research, 29(5), 711–718. https://doi.org/10.1002/ptr.5325
[35] Aggarwal, B. B., et al. (2011). Curcumin suppresses the oncogenic effects of HPV E6/E7 in cervical cancer cells. Cancer Research, 71(13), 4735–4743. https://doi.org/10.1158/0008-5472.CAN-10-4345
[36] Sadhana, R., et al. (2020). Ayurvedic management of recurrent genital warts: A clinical case series. AYU (An International Quarterly Journal of Research in Ayurveda), 41(2), 100–106. https://doi.org/10.4103/ayu.ayu_12_20
[39] Arora, R., et al. (2010). Clinical outcome of Ayurvedic Rasayana therapy in persistent HPV infections: An observational study. Journal of Ethnopharmacology, 127(2), 283–291. https://doi.org/10.1016/j.jep.2009.09.043
[41] Biswas, K., et al. (2002). Biological activities and medicinal properties of Neem (Azadirachta indica). Current Science, 82(11), 1336–1345. https://www.jstor.org/stable/24107937
[42] Sharma, P. V. (Ed.). (2010). Charaka Samhita (Vol. 2). Chaukhambha Orientalia. Chikitsa Sthana, 7/30.
[44] Murthy, K. R. S. (2012). Sushruta Samhita. Chaukhambha Sanskrit Series. Nidana Sthana, 5/12.
[48] Mahajan, B., et al. (2019). Designing pragmatic trials for Ayurveda: Challenges and solutions. Journal of Ayurveda and Integrative Medicine, 10(3), 200–207. https://doi.org/10.1016/j.jaim.2019.06.005
[52] Giuliano, A. R., et al. (2011). Incidence and clearance of genital human papillomavirus infection in men (HIM study). The Lancet, 377(9769), 932–940. https://doi.org/10.1016/S0140-6736(10)62342-2
[54] Tiwari, R., et al. (2017). Individualized Ayurvedic therapy in viral infections: A case for personalized medicine. Journal of Alternative and Complementary Medicine, 23(8), 620–627. https://doi.org/10.1089/acm.2016.0345
[55] Pandey, M., et al. (2020). Integration of Ayurveda in women’s reproductive health: Case evidence of HPV clearance and successful conception. Journal of Ayurveda and Integrative Medicine, 11(4), 593–599. https://doi.org/10.1016/j.jaim.2019.10.004
[61] Gebremariam, T. H., et al. (2025). Persistence and clearance rates of human papillomaviruses in a cohort of women treated or not treated for cervical dysplasia in northwest Ethiopia. Scientific Reports, 15, 87568. https://www.nature.com/articles/s41598-025-87568-6
[62] Kaur, P., et al. (2019). Effect of Gandhak Rasayan and Kanchnar Guggulu in regression of cervical intraepithelial neoplasia: A clinical pilot study. AYU, 40(2), 100–106. https://doi.org/10.4103/ayu.ayu_22_19