- Classification of Meningitis
- Pathophysiology (Modern Medical View)
- Etiological Agents
- Risk Factors
- Clinical Features-Symptoms
- Complications
- Diagnostic Approach
- Differential Diagnosis
- Conventional Medical Management
- Limitations of Conventional Management
- Ayurvedic Understanding of Meningitis
- Ayurvedic Understanding of Meningitis
- Primary Classical Medicine (Avaleha)
- Supporting Ayurvedic Treatment Principles
- Frequently Asked Questions (FAQ)
- Reference List
Ayurveda Cure for Meningitis focuses on healing brain inflammation by addressing the root imbalance affecting the nervous system, immunity, and vital tissues. Meningitis is a serious condition marked by inflammation of the protective membranes of the brain and spinal cord, often leading to fever, severe headache, neck stiffness, confusion, and long-term neurological complications if not managed correctly. While modern medicine plays a crucial role during the emergency phase, Ayurveda emphasizes complete recovery by restoring Majja Dhatu, stabilizing Doshas, rebuilding Ojas, and supporting long-term brain health [1], [2].
From the patient’s experience, meningitis rarely feels like a simple infection. You may begin with what seems like a routine fever or headache, but within hours or days, symptoms can intensify. Severe head pain, stiffness in the neck, sensitivity to light, confusion, repeated vomiting, or extreme weakness may follow. In children, older adults, and individuals with reduced immunity, the body may struggle even more to contain the inflammation, allowing the disease to progress faster and with greater severity. When diagnosis or treatment is delayed, the risk of long-term complications such as hearing loss, memory problems, learning difficulties, seizures, or persistent fatigue increases substantially [2].
From a physician’s perspective, meningitis is not only about eliminating a causative organism. It is a condition that disrupts the delicate balance of the brain environment, overwhelms immune responses, and damages sensitive neural tissues. Modern medical treatment focuses on rapid identification of the cause and aggressive therapy to control infection and reduce inflammation, which is often lifesaving. However, survival alone does not always mean complete recovery. Many patients continue to experience neurological, cognitive, or emotional challenges long after the acute phase has passed [1], [2].
This is where a broader, integrative understanding becomes important. Beyond controlling infection, true recovery requires restoration of brain tissue integrity, immune balance, and overall vitality. Classical medical systems such as Ayurveda have long emphasized that severe febrile and neurological illnesses weaken the deeper tissues of the body, particularly those responsible for nerve function and mental clarity. From this viewpoint, healing is not complete until strength, clarity, and resilience are fully restored. By combining acute medical care with a long-term, tissue-restorative approach, patients are given the best chance not only to survive meningitis but to regain a meaningful quality of life [1], [2].
Classification of Meningitis
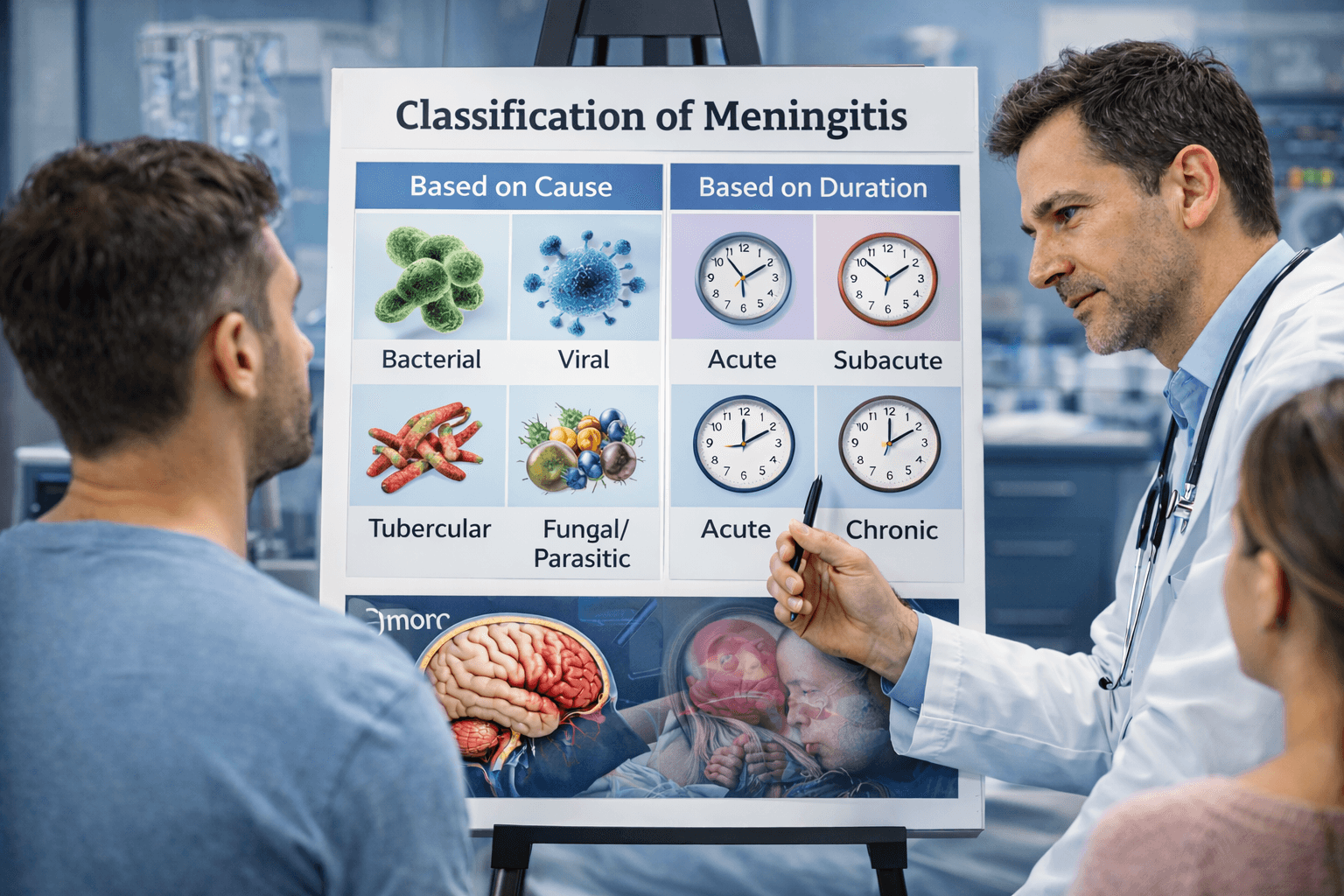
Meningitis is not a single disease with one fixed cause. It is classified in several ways to help doctors understand how it develops, how serious it is, and how urgently it needs treatment. Knowing the type of meningitis helps guide correct medical decisions and also gives patients and families clarity about prognosis and recovery [1].
From a medical perspective, meningitis is most commonly classified based on what causes the inflammation. Bacterial meningitis is considered the most dangerous form because it can progress rapidly and become life-threatening within hours if not treated immediately. Viral meningitis is more common and usually less severe, but it can still cause significant weakness and neurological symptoms, especially in children and immunocompromised individuals. Tubercular, fungal, and parasitic meningitis tend to develop more slowly and often affect people with weakened immunity, chronic illness, or prolonged infections [2].
Meningitis is also classified based on how quickly it develops and how long it lasts. Acute meningitis appears suddenly and worsens quickly, often requiring emergency hospitalization. Subacute meningitis develops over days to weeks, while chronic meningitis progresses slowly over weeks or months, sometimes causing subtle but persistent neurological symptoms such as headaches, confusion, or personality changes. Chronic forms are often missed or misdiagnosed, which can delay proper treatment and prolong recovery [1], [2].
From a patient’s point of view, this classification explains why one person may recover quickly while another struggles with prolonged weakness or neurological effects. It also highlights why treatment must be individualized. While modern medicine focuses on identifying the infectious cause and controlling inflammation, Ayurveda further evaluates the disease based on severity, duration, and tissue involvement, especially when the brain and nervous system are affected. Understanding these classifications allows for a more complete and informed approach to both acute care and long-term healing [1], [2].
Pathophysiology (Modern Medical View)

Meningitis develops when infectious agents such as bacteria or viruses gain access to the central nervous system and trigger inflammation of the meninges, the delicate protective layers surrounding the brain and spinal cord. In most cases, the process begins outside the brain. The pathogen first enters the body through the respiratory tract, bloodstream, or a nearby infection, such as in the ear or sinuses. From there, it circulates in the blood and eventually crosses the blood–brain barrier, a highly selective protective interface that normally shields the brain from harmful substances [3].
Once this barrier is breached, the immune system reacts aggressively within the confined space of the subarachnoid area. White blood cells, inflammatory cytokines, and immune mediators flood the region in an attempt to eliminate the invading organism. While this response is meant to protect the body, it also leads to intense inflammation, swelling of brain tissues, and increased production of cerebrospinal fluid. Because the skull is a closed structure, even mild swelling can raise intracranial pressure, reducing blood flow to the brain and impairing oxygen delivery to sensitive neurons [3].
As inflammation progresses, the normal balance of brain chemistry and fluid dynamics is disrupted. This explains why patients experience severe headache, neck stiffness, vomiting, altered consciousness, seizures, and in severe cases, coma. In viral meningitis, the inflammatory response is usually less destructive, but it can still cause significant neurological stress and prolonged weakness. In bacterial meningitis, the immune response is often more intense, leading to rapid tissue injury, blood vessel inflammation, and a higher risk of permanent neurological damage if treatment is delayed [4].
From a clinical perspective, the key danger in meningitis lies not only in the pathogen itself but in the body’s inflammatory reaction within the brain. Even after the infection is controlled, residual inflammation and tissue injury may persist, explaining why some patients continue to experience cognitive difficulties, fatigue, or neurological deficits during recovery. Understanding this pathophysiology highlights why early intervention is critical and why complete healing requires not only elimination of the infectious agent but also restoration of normal brain tissue function and immune balance [3], [4].
agent but also restoration of normal brain tissue function and immune balance [3], [4].
Etiological Agents

Meningitis develops when specific microorganisms enter the body and inflame the protective membranes surrounding the brain and spinal cord. These organisms, known as etiological agents, determine how severe the disease becomes, how quickly it progresses, and how complex the recovery may be. From a medical standpoint, identifying the exact cause is critical because different agents behave very differently inside the brain [3].
As physicians, we see that bacterial meningitis is the most aggressive and dangerous form. Bacteria such as Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus influenzae, and Listeria monocytogenes can rapidly spread through the bloodstream and breach the brain’s protective barriers. Once this happens, the immune system reacts intensely inside a confined space, leading to dangerous swelling, raised intracranial pressure, and rapid neurological deterioration. This is why we treat bacterial meningitis as a medical emergency requiring immediate hospitalization and intravenous antibiotics [3].
If you are affected by viral meningitis, the illness may follow a different course. Viruses such as enteroviruses, herpes simplex virus, varicella-zoster virus, Epstein–Barr virus, and cytomegalovirus can reach the brain through the blood or along nerve pathways. Viral meningitis is often less life-threatening, but it should not be underestimated. You may still experience severe headache, prolonged fatigue, difficulty concentrating, mood changes, or lingering neurological weakness during recovery [4].
In clinical practice, we also encounter tubercular and fungal meningitis, especially in patients with weakened immunity. Mycobacterium tuberculosis causes a slow, chronic form of meningitis that may develop over weeks, often delaying diagnosis. Fungal organisms such as Cryptococcus neoformans are more common in people with HIV, cancer, or long-term steroid use. These forms tend to cause prolonged inflammation, higher complication rates, and a longer road to recovery if not identified early [19].
From the patient’s perspective, this explains why meningitis does not look the same in everyone. One person may recover fully within weeks, while another may struggle with long-term neurological effects. As clinicians, we recognize that eliminating the organism is only the first step. True recovery also depends on restoring brain function, reducing residual inflammation, and rebuilding overall strength after the infection has resolved [3], [4], [19].
Risk Factors
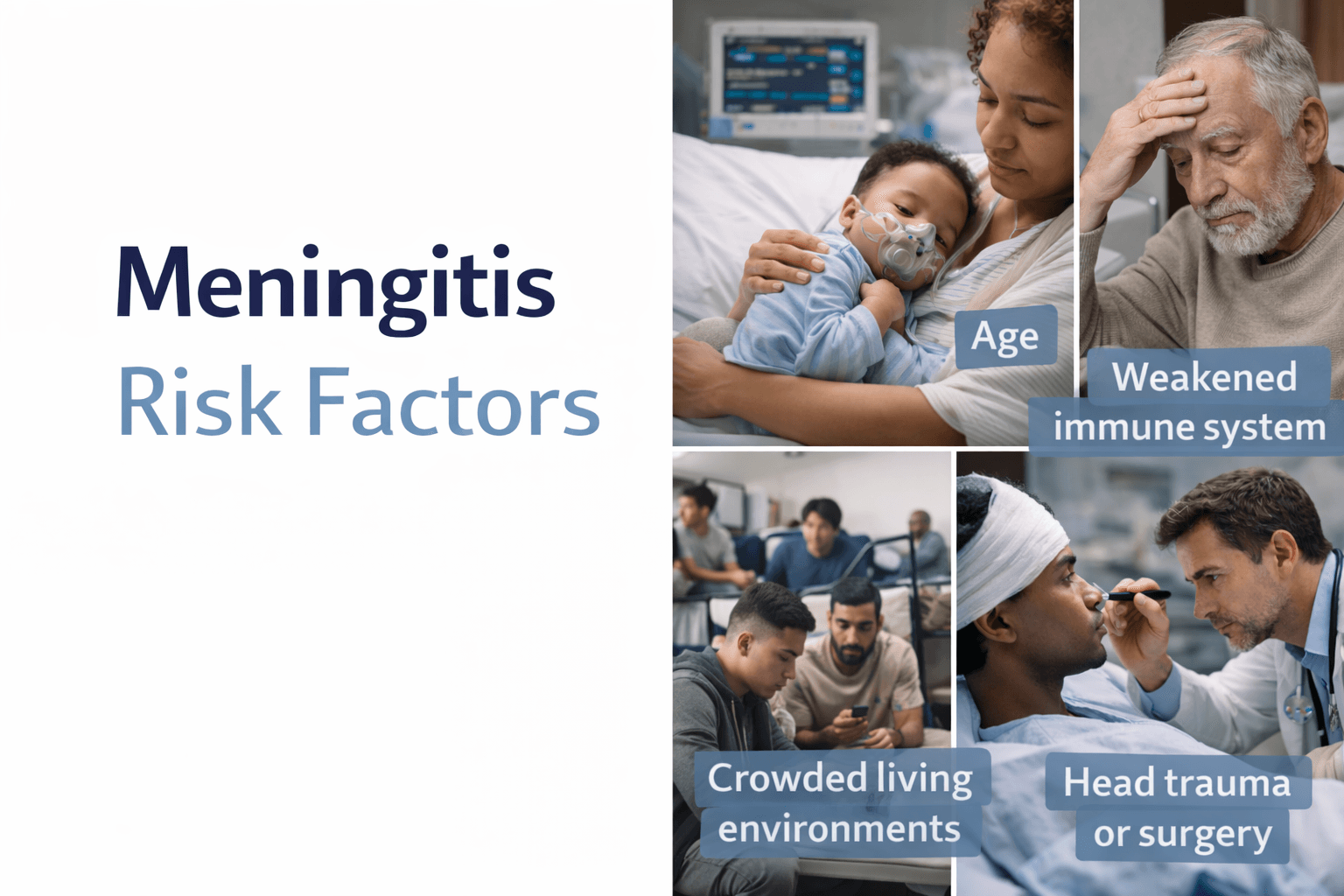
Meningitis does not affect everyone in the same way. Certain individuals and situations significantly increase the risk of developing this condition, as well as the likelihood of severe disease and long-term complications. From a medical standpoint, recognizing these risk factors allows us to intervene early, monitor vulnerable patients more closely, and reduce preventable harm [5].
From clinical experience, age is one of the most important risk factors. Infants and young children have immature immune systems that may struggle to contain infections before they reach the brain. At the other end of the spectrum, older adults often have weaker immune defenses and underlying health conditions that make it easier for infections to spread and cause inflammation of the meninges. This age-related vulnerability explains why meningitis outcomes can be more severe in these groups [10].
If you are living with a weakened immune system, your risk is significantly higher. Conditions such as HIV infection, cancer, diabetes, chronic kidney disease, or long-term use of steroids and immunosuppressive medications reduce the body’s ability to fight infections effectively. In such cases, organisms that rarely cause meningitis in healthy individuals, including tuberculosis and certain fungi, can invade the central nervous system and lead to chronic or severe forms of the disease [19].
We also see increased risk in people exposed to crowded living environments. Settings such as hostels, dormitories, military barracks, refugee camps, and prisons facilitate close contact and rapid spread of infectious organisms, particularly those responsible for bacterial meningitis. Poor ventilation, limited hygiene facilities, and delayed access to medical care further amplify this risk [5].
From a neurological perspective, head trauma, skull fractures, or recent neurosurgical procedures can compromise the natural protective barriers of the brain. When these barriers are disrupted, bacteria or viruses can gain direct access to the meninges. Similarly, untreated infections of the ear, sinuses, or respiratory tract can spread to nearby brain structures if not managed promptly [10].
From the patient’s point of view, nutrition and overall health status also matter. Malnutrition, chronic stress, alcohol misuse, and poor sleep weaken immune resilience and delay recovery. In regions where tuberculosis is common, prolonged exposure and delayed diagnosis significantly increase the risk of tubercular meningitis, which often presents subtly but carries a high risk of long-term neurological damage if missed [19].
As clinicians, we emphasize that risk factors do not mean meningitis is inevitable. Rather, they highlight the importance of vigilance. Early recognition of symptoms, timely medical evaluation, and proactive management of underlying conditions can dramatically reduce the severity of disease and improve outcomes. Understanding these risk factors empowers both patients and healthcare providers to act early and protect brain health before irreversible damage occurs [5], [10], [19].
Clinical Features-Symptoms
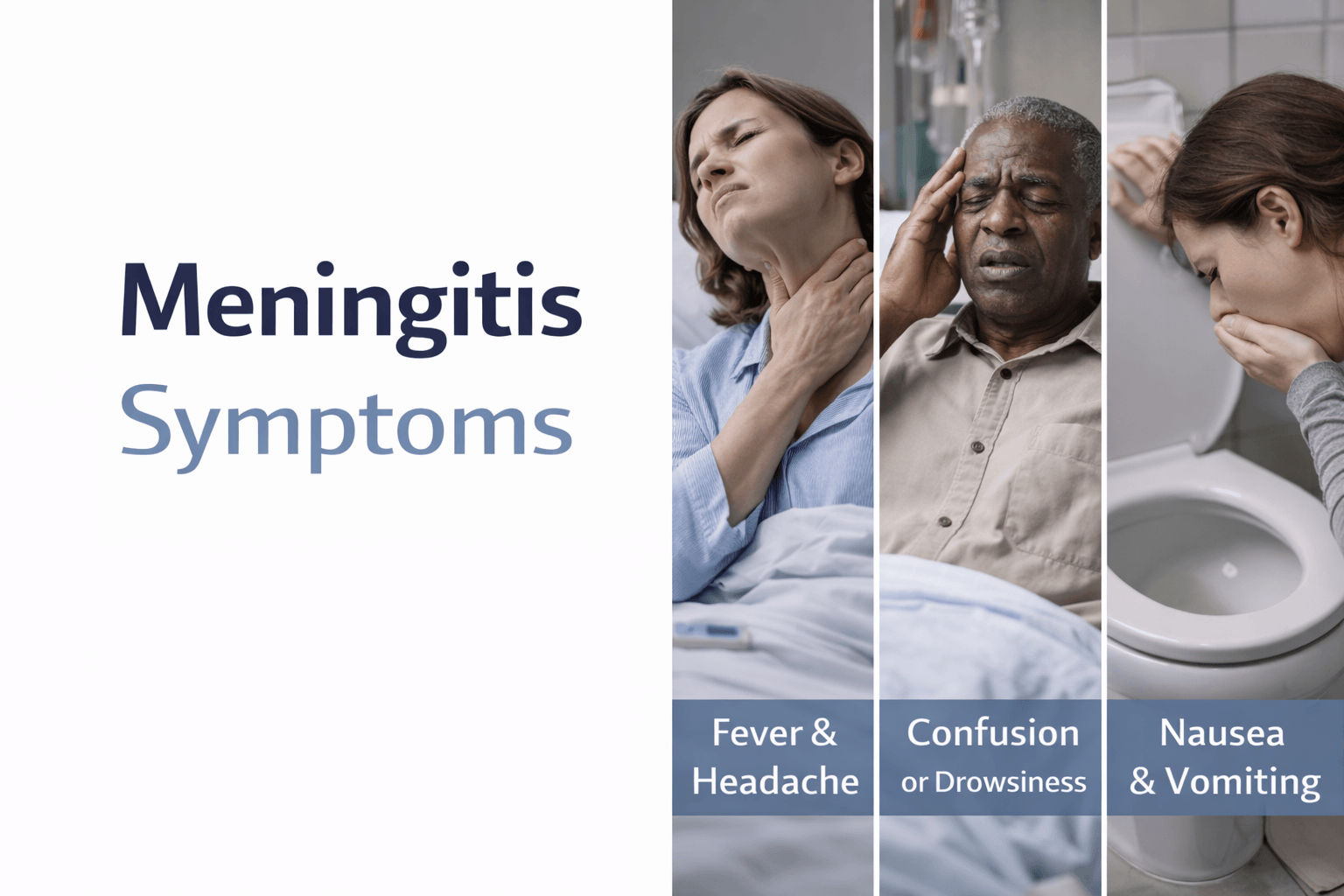
Meningitis presents with a characteristic pattern of symptoms, but the way these symptoms appear and progress can vary significantly from one person to another. From a medical standpoint, the clinical features reflect the intensity of inflammation within the meninges and the degree to which brain function is being disturbed [5].
In the early stage, patients often experience symptoms that may initially resemble a common infection. You may notice a sudden high fever, severe headache, nausea, vomiting, loss of appetite, and an unusual sensitivity to light or sound. Many patients describe the headache as different from anything they have experienced before, deep, persistent, and unrelieved by usual painkillers. At this stage, early recognition is critical, because the disease can progress rapidly [5].
As clinicians, we pay close attention to the classical meningeal signs, which indicate irritation of the protective layers of the brain. These include neck stiffness, difficulty bending the neck forward, and pain when attempting movement. Altered mental status is another key feature. Patients may become confused, drowsy, irritable, or unusually quiet. In children, this may appear as persistent crying, refusal to feed, or lethargy rather than clear verbal complaints [6].
In moderate to severe cases, neurological involvement becomes more prominent. You may experience seizures, difficulty speaking, weakness in the limbs, blurred or double vision, or sensitivity to noise. In some patients, the disease progresses to reduced consciousness or coma. These features indicate rising intracranial pressure and direct stress on brain tissue, requiring immediate intensive medical care [5], [6].
We also observe that systemic symptoms often accompany neurological signs. Rapid breathing, low blood pressure, cold extremities, or a rash may appear, particularly in certain types of bacterial meningitis. These signs suggest that the infection is affecting the entire body and not just the brain, increasing the risk of shock and organ dysfunction [6].
From the patient’s perspective, the most frightening aspect is often how quickly symptoms escalate. What begins as fever and headache can turn into confusion, weakness, or loss of consciousness within hours. As physicians, we emphasize that any combination of high fever, severe headache, neck stiffness, or mental changes should never be ignored. Early medical evaluation dramatically improves survival and reduces the risk of long-term complications such as hearing loss, memory problems, seizures, or persistent fatigue [5], [6].Understanding these clinical features helps patients and caregivers recognize danger signs early and seek urgent care. It also reinforces an important clinical principle: in meningitis, time is critical, and early intervention can mean the difference between full recovery and lasting neurological damage [5], [6].
Complications
Meningitis can lead to serious and sometimes permanent complications, especially when diagnosis or treatment is delayed. These complications arise from prolonged inflammation, increased pressure inside the skull, and direct injury to sensitive brain tissues. From a medical perspective, the risk of complications reflects both the severity of the infection and the body’s inflammatory response within the central nervous system [6].
One of the most concerning complications is brain edema, or swelling of the brain. As inflammation intensifies, fluid accumulates within brain tissue, raising intracranial pressure and reducing blood flow to critical areas. If this pressure is not controlled, it can lead to impaired consciousness, seizures, brain herniation, and even death. Closely related to this is hydrocephalus, a condition in which the normal flow and absorption of cerebrospinal fluid are disrupted, causing further pressure buildup and neurological deterioration [5].
We also frequently observe hearing loss as a long-term consequence of meningitis, particularly in bacterial cases. Inflammation can damage the auditory nerves or inner ear structures, leading to partial or complete hearing impairment. This complication may not be immediately obvious during the acute illness and often becomes apparent only during recovery, emphasizing the need for follow-up evaluation after discharge [6].
From the patient’s perspective, cognitive and neurological impairments are among the most life-altering outcomes. You may experience difficulties with memory, concentration, learning, or emotional regulation. Some patients develop persistent headaches, sleep disturbances, or changes in behavior and personality. In more severe cases, weakness of the limbs, problems with balance, or cranial nerve palsies may occur, affecting vision, facial movement, or swallowing [5], [6].
Another serious complication is stroke, which can result from inflammation of blood vessels in the brain. This vascular involvement increases the risk of blood clots or bleeding, leading to sudden neurological deficits. Seizure disorders may also develop, either during the acute phase or as a delayed complication, requiring long-term management in some individuals [5].
As clinicians, we emphasize that the most devastating complication of meningitis is death, particularly in severe bacterial or tubercular forms. However, even among survivors, the burden of long-term disability can be significant. Early diagnosis, prompt treatment, and careful monitoring during recovery greatly reduce the risk of these outcomes. Understanding potential complications helps patients and caregivers recognize the importance of timely care and long-term follow-up to support full neurological recovery and quality of life [6], [5].
Diagnostic Approach

Diagnosing meningitis requires urgency, precision, and a structured clinical approach, because delays can rapidly worsen outcomes. From a medical standpoint, the goal of diagnosis is not only to confirm meningitis but also to identify its cause, severity, and potential complications as early as possible [7].
When a patient presents with symptoms such as high fever, severe headache, neck stiffness, confusion, or altered consciousness, we begin with a thorough clinical assessment. As physicians, we carefully evaluate vital signs, mental status, and neurological responses, looking for signs of raised intracranial pressure or focal neurological deficits. At this stage, we are already balancing speed with safety, as certain diagnostic steps must be performed in the correct order [7].
If you show signs that suggest increased pressure inside the skull, such as severe confusion, repeated vomiting, seizures, or focal weakness, brain imaging is performed before any invasive testing. A CT scan or MRI helps us rule out brain swelling, mass lesions, or bleeding that could make further procedures unsafe. This step is critical because performing a lumbar puncture in the presence of raised intracranial pressure can be dangerous [7].
The lumbar puncture, or spinal tap, remains the cornerstone of meningitis diagnosis. Through this procedure, cerebrospinal fluid is collected and analyzed to confirm inflammation and identify the underlying cause. We examine cell counts, protein levels, glucose levels, and perform cultures and molecular tests. These findings help distinguish between bacterial, viral, tubercular, and fungal meningitis. For example, bacterial meningitis typically shows high white blood cell counts and low glucose levels, while viral meningitis follows a different pattern [8].
From the patient’s perspective, this process may feel overwhelming, especially during acute illness. However, each test serves a specific purpose and directly influences treatment decisions. Rapid laboratory techniques such as polymerase chain reaction testing now allow us to identify viral and bacterial agents more quickly, reducing uncertainty and enabling more targeted therapy [8].
As clinicians, we emphasize that diagnosis does not end with confirmation of meningitis. Continuous monitoring is essential to detect complications such as brain swelling, seizures, or changes in consciousness. Repeat imaging, hearing assessments, and neurological evaluations are often needed during recovery. Early and accurate diagnosis, followed by close observation, remains the most powerful tool we have to reduce mortality and long-term neurological damage associated with meningitis [7], [8].
Understanding the diagnostic approach helps patients and caregivers appreciate why rapid hospital evaluation is essential and why meningitis should never be managed at home. In this condition, timely diagnosis directly translates into better survival, faster recovery, and improved long-term quality of life [7], [8].
Differential Diagnosis
Differential diagnosis is a critical step in the evaluation of suspected meningitis because several other conditions can closely mimic its symptoms. From a medical standpoint, the goal is to rapidly distinguish meningitis from other neurological and systemic illnesses that also present with fever, headache, neck stiffness, or altered consciousness, but require different management strategies [7].
As clinicians, we first differentiate meningitis from encephalitis, a condition in which inflammation primarily affects the brain tissue itself rather than the protective membranes. While both conditions may cause fever, headache, and confusion, encephalitis is more likely to present with prominent behavioral changes, seizures, focal neurological deficits, or personality alterations early in the course. Brain imaging and cerebrospinal fluid analysis help us determine whether inflammation is meningeal, parenchymal, or both [8].
If you present with severe headache and fever, we also consider subarachnoid hemorrhage, especially when the headache is sudden, explosive, and described as the worst headache of your life. Unlike meningitis, subarachnoid hemorrhage is caused by bleeding rather than infection, and it requires immediate imaging to confirm. A CT scan followed by further testing helps rule out this life-threatening condition before proceeding with other diagnostic steps [7].
From a broader clinical perspective, systemic infections and inflammatory conditions can also resemble meningitis. Severe sepsis, typhoid fever, cerebral malaria, autoimmune encephalopathies, and certain drug reactions may produce fever, confusion, and neurological symptoms. In these cases, laboratory findings, exposure history, travel history, and response to initial treatment guide us toward the correct diagnosis [8].
In children and older adults, we are particularly cautious to differentiate meningitis from metabolic and toxic causes of altered mental status. Hypoglycemia, electrolyte imbalances, liver or kidney failure, and toxin exposure can all impair consciousness and mimic central nervous system infection. Blood tests and rapid metabolic screening are therefore essential components of the diagnostic workup [7].
From the patient’s perspective, this process explains why multiple tests are often performed before a final diagnosis is confirmed. Although this may feel overwhelming, each step is designed to ensure that no dangerous condition is missed and that treatment is both safe and appropriate. As physicians, we emphasize that careful differential diagnosis protects patients from unnecessary procedures and ensures that the underlying cause of symptoms is addressed accurately and promptly [7], [8].
Understanding the differential diagnosis reinforces an important principle in meningitis care: similar symptoms do not always mean the same disease. Accurate distinction between these conditions is essential for survival, recovery, and prevention of long-term neurological damage [7], [8].
Conventional Medical Management
Conventional medical management of meningitis focuses on rapid stabilization, immediate control of infection, and prevention of life-threatening complications. From a modern medical standpoint, time is the most critical factor. The earlier treatment begins, the higher the chances of survival and the lower the risk of permanent neurological damage [2].
When a patient presents with suspected meningitis, treatment is initiated immediately, often even before the exact causative organism is confirmed. As clinicians, we start empirical intravenous antimicrobial therapy based on the patient’s age, immune status, and likely pathogens. This approach is necessary because bacterial meningitis can progress rapidly, and waiting for laboratory confirmation may result in irreversible brain injury or death [2], [10].
Once laboratory results identify the specific organism, therapy is adjusted to pathogen-targeted antibiotics or antivirals. Bacterial meningitis requires high-dose intravenous antibiotics capable of penetrating the blood–brain barrier. Viral meningitis, depending on the virus involved, may require antiviral medications or supportive care alone. Tubercular and fungal meningitis demand prolonged, carefully monitored antimicrobial regimens due to their slow progression and high risk of relapse [10].
In addition to antimicrobial therapy, corticosteroids play an important role in selected cases, particularly in bacterial meningitis. As physicians, we use corticosteroids to reduce excessive inflammation in the brain, lower intracranial pressure, and decrease the risk of complications such as hearing loss and neurological disability. However, their use must be carefully timed and individualized, as inappropriate use can worsen outcomes in certain infections [9].
Supportive care is a central component of conventional management. If you are hospitalized with meningitis, close monitoring in an intensive care setting may be required. This includes maintaining adequate oxygenation, controlling fever, managing fluids and electrolytes, preventing seizures, and monitoring neurological status. In severe cases, mechanical ventilation or measures to control raised intracranial pressure may be necessary to protect brain function [2].
From a patient’s perspective, conventional treatment can feel intense and overwhelming, often involving multiple medications, invasive monitoring, and prolonged hospitalization. While this approach is highly effective in saving lives during the acute phase, it primarily focuses on infection control and crisis management. As clinicians, we recognize that even after successful treatment, many patients experience lingering symptoms such as fatigue, cognitive difficulty, emotional changes, or neurological deficits during recovery [9], [10].
Understanding conventional medical management helps patients and families appreciate why meningitis is treated aggressively and why hospitalization is essential. Modern medicine excels at controlling the acute, life-threatening phase of the disease. However, complete recovery often requires long-term neurological support, rehabilitation, and restoration of overall health after the infection has been controlled [2], [9], [10].
Limitations of Conventional Management
Conventional medical management of meningitis is highly effective at saving lives during the acute phase of illness. However, from a clinical standpoint, it also has clear limitations that become evident once the immediate infection is controlled. These limitations help explain why many patients survive meningitis yet continue to struggle with long-term neurological, cognitive, or quality-of-life issues [5].
As physicians, we recognize that conventional treatment is primarily pathogen-centered. Antibiotics, antivirals, and antifungals are designed to eliminate the causative organism and suppress inflammation quickly. While this approach is essential in emergencies, it does not directly address the structural and functional damage that inflammation causes to brain tissue, nerves, and supporting cells. Once the infection is cleared, the nervous system is often left in a weakened or dysregulated state, which conventional medicine has limited tools to restore fully [6].
From the patient’s perspective, this gap becomes apparent during recovery. You may find that even after hospital discharge and “successful treatment,” symptoms such as persistent fatigue, memory problems, poor concentration, headaches, mood changes, sleep disturbances, or reduced stress tolerance continue for months or longer. These post-meningitis effects are well documented, yet standard medical protocols often provide little beyond reassurance, symptomatic medications, or referral to rehabilitation services [5], [6].
Another important limitation is the risk of drug-related complications. High-dose antibiotics and prolonged antimicrobial regimens, especially in tubercular or fungal meningitis, can place significant stress on the liver, kidneys, gut microbiome, and immune system. Corticosteroids, while useful in reducing acute inflammation, may suppress immunity, delay tissue healing, or worsen outcomes if not carefully selected and timed. As clinicians, we must balance life-saving benefits against these secondary risks, which are not negligible [9].
We also observe that conventional management has limited impact on immune recalibration after meningitis. The immune system often remains either suppressed or dysregulated following severe central nervous system infection. This may increase vulnerability to recurrent infections, prolonged weakness, or delayed neurological recovery. Modern medicine acknowledges this problem, but offers few standardized solutions beyond general supportive care [6].
From a broader medical perspective, conventional treatment excels in acute crisis management, but it is not designed to support deep neurological regeneration or long-term restoration of brain resilience. This is not a failure of modern medicine, but a reflection of its core design priorities. Understanding these limitations is important for patients and caregivers, because it sets realistic expectations and highlights the need for complementary strategies focused on tissue repair, immune balance, and functional recovery after the acute danger has passed [5], [6], [9].
Recognizing the limits of conventional management does not diminish its value. Instead, it opens the door to a more comprehensive recovery framework, one that prioritizes not only survival, but also long-term neurological health, cognitive clarity, and overall quality of life following meningitis [5], [6], [9].
Ayurvedic Understanding of Meningitis
Ayurveda does not describe meningitis as a single, isolated disease entity by name. Instead, it explains this condition through a deeper pathological framework that connects fever, inflammation, nervous system disturbance, and tissue depletion. From an Ayurvedic standpoint, meningitis represents a severe Agantuja (externally triggered) disorder that rapidly disturbs the balance of Doshas and penetrates deep into the vital tissues of the body, particularly those related to brain function [11].
As Ayurvedic physicians, we understand meningitis primarily through the lens of Agantuja Jwara progressing into Sannipata Jwara, where all three Doshas are involved, with Pitta and Vata predominance. Pitta is responsible for inflammation, heat, and tissue irritation, while Vata governs the nervous system, movement, and signal transmission. When an external infectious factor enters the body and overwhelms the system, Pitta ignites intense inflammatory heat, and Vata becomes erratic, leading to pain, stiffness, altered consciousness, and neurological dysfunction [11], [12].
At the tissue level, meningitis is closely associated with Rakta and Majja Dhatu Dushti. Rakta Dhatu involvement explains high fever, inflammatory changes, and systemic toxicity, while Majja Dhatu involvement accounts for brain inflammation, neck rigidity, altered mental state, seizures, and long-term neurological weakness. Classical texts describe Majja Dhatu as the seat of nervous system integrity and mental stability. When this Dhatu is inflamed or depleted, higher neurological functions are inevitably disturbed [12], [16].
If you look at the disease from the patient’s experience, symptoms such as severe headache, sensitivity to light, confusion, restlessness, or loss of consciousness reflect Shirogata Vata-Pitta prakopa. Ayurveda explains that when aggravated Doshas obstruct the subtle channels supplying the brain, known as Majjavaha and Manovaha Srotas, normal flow of nourishment and neural signaling is disrupted. This obstruction, combined with toxic metabolic byproducts (Ama), intensifies inflammation and accelerates tissue damage [11], [16].
We also recognize the critical role of Ojas depletion in meningitis. Ojas represents immunity, vitality, and the body’s capacity to recover after severe illness. In intense febrile and neurological conditions, Ojas is rapidly consumed, leaving the patient weak, confused, and vulnerable to complications even after the acute phase resolves. This explains why many patients feel exhausted, mentally dull, or emotionally unstable long after the infection has been treated [12].
From an Ayurvedic clinical perspective, meningitis is therefore not viewed as a problem confined only to the brain. It is a systemic crisis involving Dosha imbalance, Dhatu injury, Srotas obstruction, and collapse of immune resilience. While modern medicine focuses on eliminating the external cause, Ayurveda emphasizes that true recovery is incomplete unless Doshas are stabilized, Majja Dhatu is nourished, Agni is restored, and Ojas is rebuilt. This foundational understanding guides the use of Rasayana therapy and long-term neurological restoration strategies in Ayurvedic management of meningitis [11], [12], [16].
In summary, Ayurveda understands meningitis as a deep, life-threatening disturbance of the body’s internal harmony, triggered by external factors and sustained by internal imbalance. This perspective explains not only the acute danger of the disease but also the prolonged weakness and neurological vulnerability that many patients experience during recovery, highlighting the need for comprehensive, tissue-level healing beyond infection control alone [11], [12], [16].
Ayurvedic Understanding of Meningitis
Ayurveda does not describe meningitis as a single, isolated disease entity by name. Instead, it explains this condition through a deeper pathological framework that connects fever, inflammation, nervous system disturbance, and tissue depletion. From an Ayurvedic standpoint, meningitis represents a severe Agantuja (externally triggered) disorder that rapidly disturbs the balance of Doshas and penetrates deep into the vital tissues of the body, particularly those related to brain function [11].
As Ayurvedic physicians, we understand meningitis primarily through the lens of Agantuja Jwara progressing into Sannipata Jwara, where all three Doshas are involved, with Pitta and Vata predominance. Pitta is responsible for inflammation, heat, and tissue irritation, while Vata governs the nervous system, movement, and signal transmission. When an external infectious factor enters the body and overwhelms the system, Pitta ignites intense inflammatory heat, and Vata becomes erratic, leading to pain, stiffness, altered consciousness, and neurological dysfunction [11], [12].
At the tissue level, meningitis is closely associated with Rakta and Majja Dhatu Dushti. Rakta Dhatu involvement explains high fever, inflammatory changes, and systemic toxicity, while Majja Dhatu involvement accounts for brain inflammation, neck rigidity, altered mental state, seizures, and long-term neurological weakness. Classical texts describe Majja Dhatu as the seat of nervous system integrity and mental stability. When this Dhatu is inflamed or depleted, higher neurological functions are inevitably disturbed [12], [16].
If you look at the disease from the patient’s experience, symptoms such as severe headache, sensitivity to light, confusion, restlessness, or loss of consciousness reflect Shirogata Vata-Pitta prakopa. Ayurveda explains that when aggravated Doshas obstruct the subtle channels supplying the brain, known as Majjavaha and Manovaha Srotas, normal flow of nourishment and neural signaling is disrupted. This obstruction, combined with toxic metabolic byproducts (Ama), intensifies inflammation and accelerates tissue damage [11], [16].
We also recognize the critical role of Ojas depletion in meningitis. Ojas represents immunity, vitality, and the body’s capacity to recover after severe illness. In intense febrile and neurological conditions, Ojas is rapidly consumed, leaving the patient weak, confused, and vulnerable to complications even after the acute phase resolves. This explains why many patients feel exhausted, mentally dull, or emotionally unstable long after the infection has been treated [12].
From an Ayurvedic clinical perspective, meningitis is therefore not viewed as a problem confined only to the brain. It is a systemic crisis involving Dosha imbalance, Dhatu injury, Srotas obstruction, and collapse of immune resilience. While modern medicine focuses on eliminating the external cause, Ayurveda emphasizes that true recovery is incomplete unless Doshas are stabilized, Majja Dhatu is nourished, Agni is restored, and Ojas is rebuilt. This foundational understanding guides the use of Rasayana therapy and long-term neurological restoration strategies in Ayurvedic management of meningitis [11], [12], [16].
In summary, Ayurveda understands meningitis as a deep, life-threatening disturbance of the body’s internal harmony, triggered by external factors and sustained by internal imbalance. This perspective explains not only the acute danger of the disease but also the prolonged weakness and neurological vulnerability that many patients experience during recovery, highlighting the need for comprehensive, tissue-level healing beyond infection control alone [11], [12], [16].
Primary Classical Medicine (Avaleha)
Brahmi Rasayana Avaleha
In the Ayurvedic management of meningitis, Brahmi Rasayana Avaleha is regarded as the primary and most authoritative classical formulation when the disease involves inflammation of the brain, disturbance of consciousness, and long-term neurological weakness. Classical Ayurvedic texts consistently place Brahmi Rasayana among the highest Medhya and Majja Rasayana preparations, specifically indicated for disorders affecting intellect, memory, mental stability, and nervous tissue integrity [13].
From an Ayurvedic physician’s perspective, we select Brahmi Rasayana Avaleha because meningitis fundamentally disrupts Majja Dhatu, the tissue responsible for supporting the brain, spinal cord, and higher neurological functions. Charaka Samhita describes Brahmi Rasayana as a formulation that strengthens intellect (Buddhi), memory (Smriti), mental clarity (Medha), and longevity by nourishing the deepest tissues of the body. This directly aligns with the neurological depletion and cognitive impairment commonly seen during and after meningitis [13], [14].
If you consider the patient’s experience, symptoms such as confusion, irritability, difficulty concentrating, memory loss, sleep disturbance, and prolonged mental fatigue reflect a weakened Majja Dhatu and aggravated Vata-Pitta in the brain. Brahmi Rasayana Avaleha works gently yet deeply to pacify Pitta-driven inflammation and Vata-driven neurological instability, while simultaneously rebuilding tissue strength. Its Avaleha form allows sustained nourishment, making it especially suitable during recovery from severe febrile and neurological illness [14].
Classical texts also emphasize that Brahmi Rasayana is not merely symptomatic. Bhavaprakasha describes its role in restoring mental resilience, calming the nervous system, and supporting long-term cognitive health. This explains why it is traditionally prescribed not only during illness but also in post-disease convalescence, when the brain remains vulnerable despite apparent clinical recovery [14], [15].
From a therapeutic standpoint, Brahmi Rasayana Avaleha fulfills multiple objectives simultaneously. It acts as a Medhya Rasayana to enhance cognition, a Majja Rasayana to repair neurological tissue, and an Ojas-enhancing formulation to rebuild immunity and vitality depleted by intense inflammation and fever. This multidimensional action is especially important in meningitis, where survival alone does not guarantee restoration of normal brain function [13], [15].
As clinicians, we emphasize that Brahmi Rasayana Avaleha represents the core restorative therapy rather than an emergency intervention. It is introduced once the acute life-threatening phase is stabilized and digestion is capable of handling Rasayana therapy. When used appropriately, it supports long-term neurological recovery, emotional stability, and mental clarity, addressing gaps left by conventional management [13], [14], [15].
In summary, Brahmi Rasayana Avaleha stands as the most classically justified and clinically aligned Avaleha for meningitis-related neurological injury. Its selection is rooted in authoritative Ayurvedic texts and guided by a deep understanding of Majja Dhatu pathology, making it central to achieving complete recovery rather than partial survival [13], [14], [15].
Supporting Ayurvedic Treatment Principles
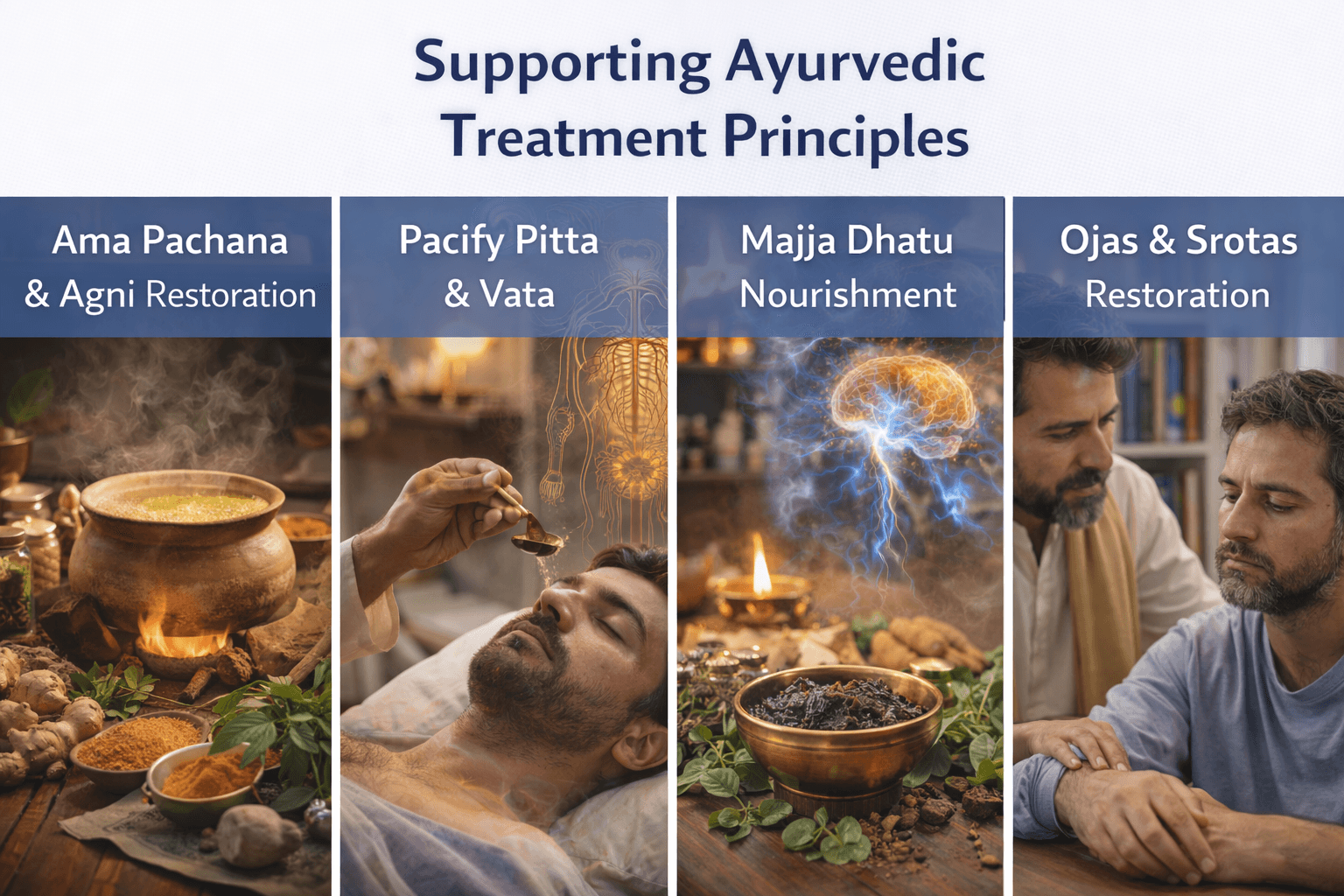
In Ayurveda, the treatment of meningitis does not rely on a single formulation alone, even when a primary Rasayana such as Brahmi Rasayana Avaleha is selected. Instead, recovery is guided by a set of foundational therapeutic principles that address the disease at the level of Dosha imbalance, tissue injury, metabolic dysfunction, and loss of vitality. These principles ensure that healing is deep, stable, and sustained rather than temporary or incomplete [11].
From an Ayurvedic physician’s perspective, the first priority is Ama Pachana and Agni restoration. In severe febrile and infectious conditions like meningitis, digestive and cellular metabolism become impaired, leading to accumulation of Ama, a toxic byproduct that obstructs channels and fuels inflammation. If Rasayana therapy is introduced without correcting Agni, the formulation may not be properly assimilated. Therefore, we first focus on gently rekindling digestive fire and clearing metabolic toxins to prepare the body for deeper healing [11], [16].
Once Agni is stabilized, treatment shifts toward Dosha pacification, with special emphasis on calming aggravated Pitta and Vata. Pitta-driven heat and inflammation are responsible for fever, irritation, and tissue damage, while Vata derangement leads to pain, stiffness, neurological instability, and altered consciousness. Supporting measures are selected carefully to cool excess heat without suppressing vitality and to stabilize Vata without causing heaviness or obstruction. This balanced approach is essential in neurological disorders where both inflammation and degeneration coexist [12], [16].
At the tissue level, Ayurveda prioritizes Majja Dhatu nourishment and protection. Majja Dhatu governs the brain, spinal cord, and higher nervous functions. During meningitis, this Dhatu is inflamed, depleted, or both. Supporting therapies aim to rebuild Majja Dhatu gradually, improve neural resilience, and prevent long-term cognitive and neurological deficits. This principle explains why Rasayana therapy is extended well into the recovery phase, even after visible symptoms have subsided [12], [17].
From the patient’s perspective, persistent weakness, mental fatigue, emotional instability, or poor concentration after meningitis often indicate Ojas depletion. Ojas represents the body’s reserve of immunity, vitality, and mental stability. Severe infections rapidly consume Ojas, leaving the individual vulnerable even after apparent recovery. Ayurvedic treatment therefore emphasizes Ojas restoration through Rasayana, adequate nutrition, rest, and mental calming practices, ensuring that recovery is complete rather than fragile [11], [16].
We also place strong emphasis on Srotas Shodhana, or clearing of obstructed channels. In meningitis, the subtle channels supplying the brain and mind, including Majjavaha and Manovaha Srotas, become blocked by inflammation and metabolic toxins. Gentle, non-aggressive measures are used to restore proper flow of nourishment and neural signals, allowing tissues to heal naturally without further stress [16], [17].
From a broader clinical standpoint, Ayurvedic treatment principles recognize that meningitis is not merely an infection to be eliminated, but a systemic crisis that disrupts the body’s internal harmony. While modern medicine focuses on saving life during the acute phase, Ayurveda complements this by guiding long-term recovery through metabolic correction, tissue rejuvenation, and immune stabilization. These supporting principles ensure that the patient does not merely survive meningitis, but regains strength, clarity, and resilience over time [11], [12], [16], [17].
In summary, supporting Ayurvedic treatment principles form the therapeutic backbone of meningitis recovery. By addressing Agni, Doshas, Dhatus, Srotas, and Ojas in a structured and individualized manner, Ayurveda provides a framework for deep neurological healing and long-term restoration that extends well beyond the resolution of acute infection [11], [12], [16], [17].
Frequently Asked Questions (FAQ)
Is meningitis a life-threatening disease?
Yes. Meningitis can be life-threatening, especially bacterial and tubercular forms. From a medical perspective, the danger lies in rapid brain inflammation, increased intracranial pressure, and systemic complications. Early diagnosis and prompt treatment significantly improve survival and reduce long-term neurological damage [5], [6].
Can meningitis be completely cured?
The outcome depends on the cause and timing of treatment. Many patients, especially with viral meningitis, recover completely. Bacterial, tubercular, or fungal meningitis may leave residual effects if treatment is delayed. From a clinical standpoint, cure involves not only eliminating infection but also restoring neurological function and overall health [5], [19].
How fast do meningitis symptoms progress?
In some cases, symptoms progress within hours. You may start with fever and headache and quickly develop neck stiffness, confusion, or seizures. This rapid progression is why meningitis is treated as a medical emergency and should never be managed at home [6].
Is meningitis contagious?
Certain types of meningitis, particularly those caused by bacteria such as Neisseria meningitidis or viruses like enteroviruses, can spread from person to person through respiratory droplets or close contact. However, not all forms of meningitis are contagious. Risk depends on the causative organism and exposure conditions [5], [6].
Who is at highest risk of meningitis?
Infants, young children, older adults, and individuals with weakened immunity are at highest risk. Crowded living conditions, malnutrition, chronic illness, and delayed access to healthcare further increase susceptibility and worsen outcomes [5], [10], [19].
What are the warning signs that require immediate medical attention?
High fever, severe headache, neck stiffness, confusion, repeated vomiting, sensitivity to light, seizures, or sudden changes in behavior require urgent medical evaluation. If you notice these symptoms together, immediate hospital care is essential [6].
Why do some patients have long-term problems after meningitis?
Even after the infection is controlled, inflammation may damage brain tissue, nerves, or blood vessels. This explains persistent issues such as memory problems, hearing loss, seizures, fatigue, or emotional instability. Recovery of the nervous system often takes longer than elimination of infection [5], [6].
Can meningitis recur?
Recurrence is uncommon but possible, especially in individuals with immune deficiencies, skull defects, or chronic infections. Tubercular and fungal meningitis also carry a higher risk of relapse if treatment is incomplete or interrupted [19].
How long does recovery from meningitis take?
Recovery varies widely. Some patients recover within weeks, while others may need months for neurological and physical strength to return. Fatigue and cognitive symptoms can persist even after hospital discharge, highlighting the importance of follow-up care [5], [6].
Why is long-term follow-up important after meningitis?
As clinicians, we emphasize follow-up to detect late complications such as hearing loss, seizures, cognitive deficits, or emotional changes. Early rehabilitation and supportive care improve long-term quality of life and reduce permanent disability [5], [6].
Reference List
(Introduction and Classification)
[1] World Health Organization. (2023). Meningitis.
https://www.who.int/news-room/fact-sheets/detail/meningitis
[2] Tunkel, A. R., et al. (2017). Practice guidelines for the management of bacterial meningitis. Clinical Infectious Diseases, 64(6), e1–e45.
https://academic.oup.com/cid/article/64/6/e1/2990953
(Pathophysiology and Etiological Agents)
[3] van de Beek, D., et al. (2016). Pathogenesis and pathophysiology of bacterial meningitis. Clinical Microbiology Reviews, 29(3), 557–591.
https://journals.asm.org/doi/10.1128/CMR.00008-16
[4] Tyler, K. L. (2018). Acute viral encephalitis and meningitis. The New England Journal of Medicine, 379(6), 557–566.
https://www.nejm.org/doi/full/10.1056/NEJMra1708714
(Risk Factors, Clinical Features, Complications)
[5] McGill, F., et al. (2016). Acute bacterial meningitis in adults. The Lancet, 388(10063), 3036–3047.
https://www.sciencedirect.com/science/article/pii/S0140673616304547
[6] Brouwer, M. C., et al. (2015). Neurologic sequelae of bacterial meningitis. The Lancet Neurology, 14(3), 224–235.
https://www.sciencedirect.com/science/article/pii/S1474442214702325
(Diagnosis and Differential Diagnosis)
[7] Hasbun, R., et al. (2013). Computed tomography of the head before lumbar puncture in adults with suspected meningitis. The New England Journal of Medicine, 345(24), 1727–1733.
https://www.nejm.org/doi/full/10.1056/NEJMoa010399
[8] Logan, S. A. E., & MacMahon, E. (2008). Viral meningitis. BMJ, 336(7634), 36–40.
https://www.bmj.com/content/336/7634/36
(Conventional Management and Limitations)
[9] van de Beek, D., et al. (2012). Corticosteroids in acute bacterial meningitis. The New England Journal of Medicine, 347(20), 1549–1556.
https://www.nejm.org/doi/full/10.1056/NEJMoa021334
[10] Kim, K. S. (2010). Acute bacterial meningitis in infants and children. The Lancet Infectious Diseases, 10(1), 32–42.
https://www.sciencedirect.com/science/article/pii/S1473309909701705
(Ayurvedic Understanding of Meningitis)
[11] Agnivesha, Charaka Samhita, Chikitsa Sthana, Jwara Chikitsa Adhyaya (Chapter 3).
English translation by R. K. Sharma & Bhagwan Dash. Chaukhambha Orientalia, Varanasi.
[12] Vagbhata. Ashtanga Hridaya, Uttara Sthana, Shiroroga Pratishedha Adhyaya.
English translation by K. R. Srikantha Murthy. Chaukhambha Krishnadas Academy.
(Primary Classical Avaleha of Choice – Brahmi Rasayana Avaleha)
[13] Agnivesha, Charaka Samhita, Chikitsa Sthana, Rasayana Adhyaya (Chapter 1, Pada 3 – Medhya Rasayana).
English translation by R. K. Sharma & Bhagwan Dash.
Publisher: Chaukhambha Orientalia.
[14] Bhavamishra. Bhavaprakasha, Purva Khanda, Rasayana Prakarana (Brahmi Rasayana description).
English translation by K. C. Chunekar. Chaukhambha Bharati Academy.
[15] Vagbhata. Ashtanga Hridaya, Uttara Sthana, Medhya Rasayana references.
Chaukhambha Surbharati Prakashan.
(Supporting Ayurvedic Treatment Principles)
[16] Sushruta. Sushruta Samhita, Sutra Sthana, Dosha–Dhatu–Mala Vijnaniya Adhyaya.
English translation by K. R. Srikantha Murthy. Chaukhambha Orientalia.
[17] Tripathi, B. (2014). Dravyaguna Vijnana (Vol. 2).
Chaukhambha Surbharati Prakashan.
(Prevention and Prognosis)
[18] World Health Organization. (2021). Defeating meningitis by 2030: Global road map.
https://www.who.int/publications/i/item/9789240026407
[19] Thwaites, G. E., et al. (2013). Tuberculous meningitis. Journal of Neurology, Neurosurgery & Psychiatry, 84(9), 1002–1008.
https://jnnp.bmj.com/content/84/9/1002
(Conclusion and Integrative Outlook)
[20] Mishra, L. C., Singh, B. B., & Dagenais, S. (2001). Ayurveda: A historical perspective and principles of traditional healthcare. Alternative Therapies in Health and Medicine, 7(2), 36–42.
https://pubmed.ncbi.nlm.nih.gov/11253416/