- Causes of Anemia – Modern and Ayurvedic
- The Modern Medical View
- The Ayurvedic View- Understanding Panduroga
- Comparing the Two Perspectives
- Complete Symptomatology- Typical and Atypical Presentations
- The Common Symptoms Most Recognized
- Systemic Symptoms Across Body Systems
- Ayurvedic Description of Symptoms
- Compounding Factors
- A Holistic View of Symptoms
- Diseases and Complications Arising from or Mimicking Anemia
- Diseases That Develop as a Result of Anemia
- Rare or Atypical Disease Associations
- Conditions That Mimic Anemia
- Ayurvedic Interpretation of Complications and Mimics
- Why Recognizing These Associations Matters
- Diagnostic Approaches in Modern and Ayurvedic Medicine
- Confirming Anemia: The Role of the Complete Blood Count
- Microscopic Clues- Peripheral Blood Smear
- Iron Studies and Nutritional Testing
- Specialized Tests for Complex Cases
- The Ayurvedic – Observing the Body’s Signs
- Visual Examination of the Body
- Pulse Diagnosis: Nadi Pariksha
- The Tenfold Evaluation: Dashavidha Pariksha
- Observing Natural Wastes: Mala and Mutra Pariksha
- Ayurvedic Treatment Strategies
- Shodhana (Purification Therapy)- Clearing the Pathways
- Shamana (Pacification Therapy)- Restoring Balance and Nourishment
- Rasayana (Rejuvenative Therapy)-Strengthening the Foundation
- Dietary Recommendations (Ahara)
- Lifestyle Guidelines (Vihara)
- A Personalized, Layered Approach
- Modern Medical Treatment
- Iron Therapy: The Cornerstone of Iron Deficiency Anemia
- Vitamin and Mineral Supplementation
- Erythropoiesis-Stimulating Agents
- Blood Transfusion – Immediate but Temporary Correction
- Disease-Specific Treatments: Addressing the Root Cause
- Integrative Considerations
- Where Modern Medicine Meets Ayurveda
- References
Anemia is far more than just “low iron” or “feeling tired.” It represents a complex, systemic condition in which the body’s ability to transport oxygen is impaired due to a deficiency in either the number or quality of red blood cells or their hemoglobin content. Affecting over 1.6 billion people worldwide, anemia is considered one of the most common and widespread nutritional deficiencies globally. While it may seem simple—a low hemoglobin level confirmed by a blood test—the underlying causes, manifestations, and consequences of anemia are diverse and profound.
In developed countries like the United States and Europe, anemia often lurks undetected for years, causing vague symptoms such as fatigue, weakness, and reduced cognitive performance that are frequently misattributed to stress, aging, or other medical conditions. In low-resource settings, anemia can have devastating impacts—leading to maternal deaths, impaired childhood development, poor academic performance, and increased susceptibility to infections.
From the perspective of modern medicine, anemia is usually approached through laboratory evaluation, identifying the deficiency or dysfunction, and correcting it with iron, vitamin B12, folate, or transfusions. However, this approach sometimes overlooks the holistic terrain that allowed anemia to develop in the first place.
Ayurveda—the ancient medical science of India—describes anemia as Panduroga, a condition characterized not merely by pallor but by a fundamental imbalance in digestion (Agni), metabolism, tissue nourishment (Dhatu Poshana), and the harmonious interplay of bodily energies (Doshas). It identifies anemia as an indicator of deeper systemic disharmony, not just a biochemical deficiency.
This integrative guide aims to bridge the wisdom of Ayurveda with the precision of modern medicine. By doing so, it seeks to offer a comprehensive roadmap for understanding anemia’s causes, symptoms, atypical manifestations, complications, and holistic treatment options. Whether you are a patient searching for answers, a practitioner seeking integrative insights, or a health enthusiast eager to understand this condition, this guide will provide a detailed, research-backed foundation.
In the article that follow, we will explore:
- How modern medicine classifies anemia
- How Ayurveda conceptualizes Panduroga
- The wide array of symptoms—both typical and unusual—that anemia can cause
- Diseases that mimic anemia or are caused by it
- Diagnostic strategies from both paradigms
- Treatment options from iron pills to Ayurvedic Rasayanas
- Prevention strategies at individual and public health levels
- Cutting-edge research linking Ayurvedic treatments with scientific validation
By the end, you will understand anemia not merely as a lab value but as a dynamic health signal, requiring a multifaceted response that addresses both the root cause and the symptomatic burden.
Causes of Anemia – Modern and Ayurvedic
The Modern Medical View
In modern medicine, anemia arises from one or more fundamental mechanisms: either the body is losing blood, failing to produce enough red blood cells, or destroying them faster than they can be replaced.
Blood loss is a common cause, especially in women with heavy menstrual bleeding, individuals with gastrointestinal ulcers or cancers, or those experiencing slow, chronic bleeding from hemorrhoids or inflammatory bowel disease. Acute trauma or surgical bleeding can also rapidly deplete red blood cells.
In some cases, the problem lies in underproduction. Conditions like iron deficiency, vitamin B12 or folate deficiency, chronic kidney disease, or bone marrow disorders such as aplastic anemia or leukemia can impair the body’s ability to manufacture new red cells. Here, the bone marrow is either starved of the raw materials it needs or is damaged and unable to function properly.
Other individuals experience increased destruction of red blood cells—a process known as hemolysis. This can occur in autoimmune conditions where the immune system mistakenly attacks red blood cells, or in hereditary disorders such as sickle cell anemia or thalassemia. Certain infections like malaria, exposure to toxic substances, or even mechanical factors such as artificial heart valves can also cause premature red cell breakdown.
Beyond these primary categories, modern life introduces additional factors. Long-term use of proton pump inhibitors can reduce iron absorption from food. Individuals following strict vegan diets may lack vitamin B12, which is found primarily in animal products. Excessive tea or coffee intake, gastric bypass surgeries, and malabsorption syndromes like celiac disease can also impair nutrient absorption and contribute to anemia.
In each of these pathways, the end result is the same: a reduction in the body’s ability to carry oxygen to tissues, leading to fatigue, weakness, and systemic dysfunction.
The Ayurvedic View- Understanding Panduroga
Ayurveda approaches anemia through a broader lens. Known as Panduroga—literally “pale disease”—anemia in Ayurveda is described as a disorder of Rakta Dhatu (the blood tissue) arising from vitiation of Pitta Dosha and weakened Agni (digestive fire).
Rather than focusing solely on iron deficiency or cell counts, Ayurveda sees anemia as a failure in the chain of nourishment: from digestion, to absorption, to assimilation, to the final transformation of food into healthy blood. If any step in this chain is impaired, even an iron-rich diet may fail to nourish the tissues properly.
The classical Ayurvedic texts, including Charaka Samhita (Chikitsa Sthana 16), describe various causes of Panduroga. An improper diet, heavy in sour, salty, oily, or fermented foods, can aggravate Pitta and impair digestion. Chronic emotional stress, suppression of natural urges, or overuse of purgative therapies can disturb the internal balance necessary for healthy tissue formation. Blood loss from hemorrhoids, ulcers, or parasites is another recognized cause, as are infestations of intestinal worms (Krimi).
In Ayurveda, digestion plays a central role. Weak digestive fire—Agni Mandya—leads to the accumulation of undigested food toxins (Ama), which obstructs the nourishing channels (Srotas). This blockage prevents the proper transformation of food into blood, resulting in the pallor and weakness characteristic of anemia.
Unlike modern medicine, which often localizes the problem to the blood itself, Ayurveda views anemia as a systemic disorder reflecting broader imbalances in digestion, metabolism, and tissue formation.
Comparing the Two Perspectives
The difference between modern and Ayurvedic understanding of anemia lies not in contradiction but in focus. Modern medicine emphasizes measurable deficiencies—iron, vitamin B12, folate—or observable pathology in the bone marrow or immune system. Ayurveda, by contrast, emphasizes functional digestion, metabolic integrity, and the harmonious flow of nutrients through the body’s channels.
In modern clinical settings, treatment typically centers on replacing what’s missing: prescribing iron tablets, vitamin injections, or transfusions. Ayurveda, while also using mineral and herbal preparations rich in iron, aims first to restore digestive strength, clear metabolic obstructions, and enable the body to process and integrate nutrients effectively.
Thus, Ayurveda teaches a critical insight: the mere presence of iron is not enough; the body’s capacity to digest, absorb, and transform iron into healthy blood is equally vital. This insight explains why some patients fail to respond to iron supplements until deeper digestive imbalances are corrected.
By integrating both paradigms, we gain a richer, more holistic understanding of anemia—not just as a biochemical deficiency but as a reflection of deeper physiological harmony or disturbance.
Complete Symptomatology- Typical and Atypical Presentations
Anemia can be a master of disguise. Its symptoms range from subtle fatigue to profound weakness, from cognitive fog to life-threatening heart strain. Some individuals remain unaware of their condition for years, while others suffer from debilitating manifestations that impair daily life. Understanding the full spectrum of anemia’s symptoms is crucial, not only for diagnosis but also to recognize the hidden burden it imposes.
The Common Symptoms Most Recognized
Fatigue is the most universal complaint among anemic patients. People often describe a deep, persistent tiredness that sleep does not relieve. This fatigue is more than feeling worn out after a long day—it is a fundamental lack of cellular energy due to reduced oxygen delivery to tissues.
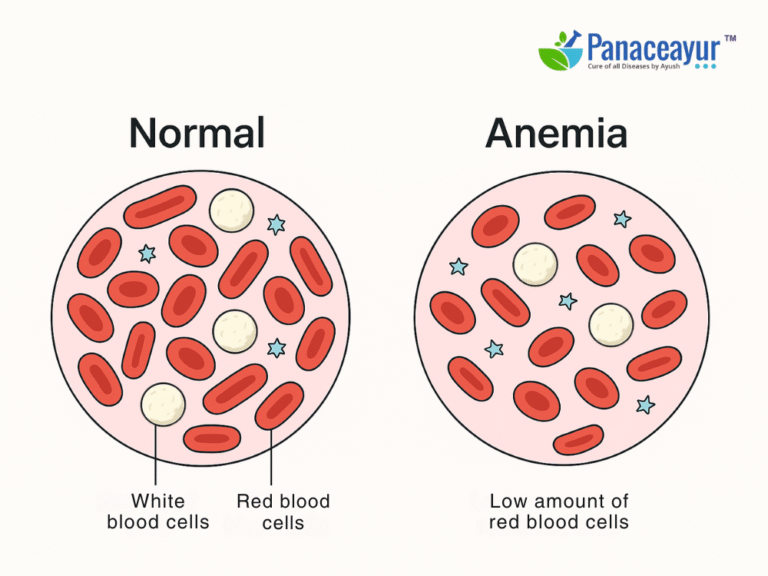
Pallor is another hallmark sign. In mild cases, it may only be noticeable in the conjunctiva (the inner lining of the lower eyelid) or mucous membranes of the mouth. In more severe anemia, the entire skin appears pale or even yellowish.
Shortness of breath, especially with exertion, is a key symptom that many patients initially ignore or attribute to aging or being “out of shape.” The reduced oxygen-carrying capacity of blood forces the heart and lungs to work harder to meet the body’s needs.
Other common symptoms include dizziness, lightheadedness, headaches, and palpitations. Some individuals report feeling their heart “pounding” or racing even with minor activity.
Cold intolerance is another frequent but often overlooked complaint. With anemia, the extremities—hands and feet—may feel persistently cold or numb due to poor oxygenation.
Systemic Symptoms Across Body Systems
Anemia affects every organ system, though the manifestations may differ depending on severity, duration, and underlying cause.
In the cardiovascular system, the heart compensates for anemia by pumping faster and harder. This results in tachycardia (increased heart rate), a bounding or forceful pulse, and sometimes a systolic heart murmur detectable on examination. In elderly individuals or those with preexisting heart disease, anemia can precipitate angina or heart failure.
In the nervous system, anemia may cause irritability, difficulty concentrating, memory problems, and even mood swings. In vitamin B12 deficiency anemia, neurological symptoms are particularly prominent, including numbness, tingling in the hands and feet, loss of balance, or an unsteady gait. Left untreated, B12 deficiency can lead to irreversible nerve damage.
The gastrointestinal system also reveals signs. Patients may develop a smooth, reddened tongue (glossitis), painful cracks at the corners of the mouth (angular cheilitis), or even difficulty swallowing due to esophageal webs—a triad of findings characteristic of Plummer-Vinson syndrome in iron deficiency anemia.
The skin and nails provide important visual clues. Spoon-shaped nails (koilonychia), brittle or ridged nails, pale nail beds, and dry, flaky skin are frequent findings. Some individuals develop hair thinning or hair loss as a consequence of chronic anemia.
The immune system may be compromised in anemias involving bone marrow failure (such as aplastic anemia), leading to frequent infections and slow wound healing.
Ayurvedic Description of Symptoms
Ayurvedic texts provide a rich and nuanced description of anemia’s manifestations under the term Panduroga. The classical signs include:
- Twak Panduta – paleness of the skin
- Daurbalya – generalized weakness or debility
- Shwasa – breathlessness, especially on exertion
- Hriddrava – palpitations or a sense of heart fluttering
- Aruchi – loss of appetite or disinterest in food
- Shirogourava – heaviness in the head or mental fog
- Pandutva – a pale-yellowish hue of the skin and sclera
- Swedadhikya – excessive sweating without exertion
The Charaka Samhita emphasizes that these symptoms result not merely from a blood deficiency but from deeper disruptions in digestion, metabolism, and tissue nourishment.
Atypical and Rare Presentations
Beyond these typical symptoms, anemia can sometimes manifest in unusual or indirect ways, leading to delayed diagnosis or misattribution to other conditions.
One such example is pica—an abnormal craving for non-nutritive substances like ice, clay, dirt, or starch. This peculiar symptom is strongly associated with iron deficiency anemia, though its mechanism remains unclear. Individuals may compulsively chew ice (pagophagia), a behavior that paradoxically relieves oral inflammation but signals an underlying deficiency.
Another underrecognized symptom is restless leg syndrome, characterized by an irresistible urge to move the legs, particularly at night. Iron deficiency is implicated in the brain’s dopamine metabolism, linking it to this neurologic disorder.
Certain manifestations are more visible in severe or chronic anemias. Splenomegaly (enlarged spleen) and bone deformities occur in thalassemia major, as the body attempts to compensate by expanding bone marrow and increasing extramedullary hematopoiesis. Individuals with sickle cell anemia may develop recurrent painful leg ulcers, jaundice, or episodes of acute chest pain.
Skin hyperpigmentation may be a clue in hereditary hemochromatosis, where iron overload rather than deficiency becomes the issue. Patients with lead poisoning may exhibit a bluish line on the gums (Burton’s line) and neurological deficits alongside anemia.
In some cases, anemia masks itself beneath other disorders. For example, a patient with profound fatigue, pallor, and weakness may initially be evaluated for hypothyroidism or chronic fatigue syndrome, delaying the diagnosis of anemia. Similarly, unexplained anemia in an elderly patient may be the first sign of hidden gastrointestinal cancer or bone marrow disease.
Compounding Factors
The degree to which anemia manifests symptoms depends not only on its severity but also on how rapidly it develops. Acute blood loss from trauma may cause sudden dizziness, cold sweats, and low blood pressure. In contrast, slowly progressive anemia allows the body to adapt, masking symptoms until the hemoglobin drops dangerously low.
Age, gender, underlying health status, and comorbidities also influence symptom expression. A young, healthy individual with a hemoglobin of 10 g/dL may tolerate anemia better than an elderly person with coronary artery disease.
A Holistic View of Symptoms
By integrating the insights of modern and Ayurvedic medicine, we gain a fuller appreciation of anemia’s diverse manifestations. It is not merely pallor and fatigue—it is a multi-system disorder affecting the heart, brain, skin, immune system, and beyond.
Understanding these signs, both typical and atypical, empowers patients and practitioners to detect anemia early, recognize its systemic impact, and investigate the deeper causes underlying its presence.
Diseases and Complications Arising from or Mimicking Anemia
Anemia is not an isolated issue confined to the bloodstream. It ripples outward, affecting multiple organs, altering physiology, and sometimes leading to complications that may overshadow the anemia itself. Beyond its direct symptoms, anemia may also signal—or be mistaken for—other serious diseases. Understanding these connections is vital for accurate diagnosis and holistic care.
Diseases That Develop as a Result of Anemia
When anemia persists, the body must adapt to the reduced oxygen-carrying capacity of the blood. These adaptations, while protective in the short term, can eventually lead to further health problems.
One of the most concerning complications is high-output heart failure. As anemia worsens, the heart works harder to pump more blood per minute in an attempt to deliver sufficient oxygen to the tissues. Over time, this increased workload can enlarge the heart and weaken its pumping efficiency, leading to shortness of breath, swelling of the legs, and fluid buildup in the lungs.
Pregnant women with anemia face increased risks of preterm labor, low birth weight, and postpartum hemorrhage. Severe maternal anemia impairs oxygen delivery to the fetus, raising the chance of developmental delays or stillbirth. These risks are particularly high in low-resource settings where anemia often goes untreated during pregnancy.
In individuals with chronic anemias such as sickle cell disease, the consequences extend beyond fatigue. Recurrent episodes of vaso-occlusive crises can cause severe bone pain, strokes, pulmonary hypertension, and organ damage over time. Repeated blood transfusions in these patients may lead to iron overload (secondary hemochromatosis), damaging the liver, heart, and endocrine glands.
Neurological complications also arise, especially in vitamin B12 deficiency anemia. If left untreated, the lack of B12 impairs the myelin sheath surrounding nerves, leading to numbness, tingling, loss of balance, memory loss, and in severe cases, dementia or psychosis. Unlike other anemias, neurological damage from B12 deficiency may not be reversible even after treatment.
In conditions like thalassemia major, the bone marrow expands in an attempt to produce more red cells. This expansion leads to skeletal deformities, particularly in the face and skull, and increased bone fragility. Additionally, extramedullary hematopoiesis (blood cell production occurring outside the bone marrow) may cause splenomegaly or hepatomegaly, further complicating management.
Rare or Atypical Disease Associations
Certain conditions are uniquely associated with specific types of anemia and may be unfamiliar to the general public. For instance, Plummer-Vinson syndrome—a triad of iron deficiency anemia, difficulty swallowing (dysphagia), and esophageal webs—can present in middle-aged women and carries an increased risk of esophageal cancer.
In autoimmune hemolytic anemia, the immune system attacks its own red blood cells, leading to jaundice, dark urine, and splenomegaly. Similarly, paroxysmal nocturnal hemoglobinuria (PNH) may cause sudden episodes of reddish-brown urine in the morning, along with anemia and increased risk of life-threatening blood clots.
Patients with hereditary hemochromatosis accumulate excess iron over decades, leading to skin hyperpigmentation (“bronze diabetes”), joint pain, liver cirrhosis, and diabetes mellitus. Iron overload may paradoxically coexist with anemia in conditions requiring repeated transfusions or ineffective erythropoiesis.
Conditions That Mimic Anemia
Several diseases can masquerade as anemia due to overlapping symptoms such as fatigue, pallor, or weakness. For example, hypothyroidism often presents with sluggishness, cold intolerance, and dry skin—symptoms that overlap with anemia, especially when mild.
Chronic kidney disease reduces the production of erythropoietin, the hormone stimulating red blood cell production. Patients may develop normocytic, normochromic anemia, often without obvious signs of bleeding or nutritional deficiency.
Leukemia and other bone marrow disorders may initially be misdiagnosed as simple anemia. Patients may present with fatigue and pallor, but also experience unexplained bruising, recurrent infections, or bone pain. Blood tests showing pancytopenia (low counts of red cells, white cells, and platelets) warrant further investigation with a bone marrow biopsy.
Other mimics include malabsorption syndromes such as celiac disease or Crohn’s disease, which impair iron, B12, and folate absorption, leading to anemia despite adequate dietary intake.
In elderly individuals, anemia of chronic inflammation may develop secondary to long-standing infections, autoimmune diseases, or cancers. This anemia is often mild but persistent, and correcting it requires addressing the underlying chronic disease rather than simply prescribing iron.
Ayurvedic Interpretation of Complications and Mimics
Ayurveda views these downstream effects of anemia as manifestations of deep-seated imbalances in tissue nutrition (Dhatu Kshaya) and bodily energies (Dosha Vikriti). The progression from simple Panduroga to heart dysfunction, neurological deficits, or immune collapse reflects worsening depletion of vitality (Ojas Kshaya) and blockage of channels (Srotorodha).
For example, cardiac strain from chronic anemia corresponds to Hridaya Daurbalya (weakness of the heart) in Ayurvedic terminology, often requiring rejuvenative therapies (Hridya Rasayana) in addition to correcting anemia itself. Neurological complications parallel Majja Dhatu Kshaya (bone marrow and nerve tissue depletion), demanding deeper restorative interventions.
Conditions mimicking anemia are similarly framed within Ayurvedic diagnostics as diseases arising from digestive failure (Agni Mandya) or toxin accumulation (Ama Sanchaya), requiring purification (Shodhana) before replenishment (Brimhana).
Why Recognizing These Associations Matters
Failing to recognize anemia’s complications or underlying causes can delay life-saving treatments. For instance, simply prescribing iron tablets in a patient with hidden gastrointestinal bleeding from colon cancer risks missing an early-stage malignancy. Similarly, treating vitamin B12 deficiency anemia without identifying accompanying neurological symptoms risks irreversible nerve damage.
A holistic approach considers anemia not as an isolated laboratory finding but as a signal of deeper imbalances or diseases needing attention. Whether viewed through the lens of modern hematology or Ayurvedic pathology, anemia deserves investigation beyond its superficial appearance.
Diagnostic Approaches in Modern and Ayurvedic Medicine
Diagnosing anemia requires more than simply confirming low hemoglobin; it demands a deeper investigation into the type, cause, and systemic context of the deficiency. Both modern medicine and Ayurveda provide valuable frameworks for diagnosing anemia, though they approach it from different angles—one rooted in laboratory analysis, the other in observation of functional and constitutional signs.
Confirming Anemia: The Role of the Complete Blood Count
In modern medicine, diagnosis begins with the complete blood count (CBC). This essential blood test measures hemoglobin levels, hematocrit (the proportion of blood occupied by red cells), and red blood cell indices such as mean corpuscular volume (MCV) and mean corpuscular hemoglobin (MCH). A hemoglobin reading below 13 grams per deciliter in men or 12 grams per deciliter in women typically confirms anemia.
The CBC also provides clues about the nature of the anemia. A low MCV suggests small, iron-deficient red cells, while a high MCV indicates large cells, commonly seen in vitamin B12 or folate deficiency. Elevated red cell distribution width (RDW) may signal a mixed nutritional deficiency or evolving disease.
Microscopic Clues- Peripheral Blood Smear
Beyond numeric values, visual examination of blood under a microscope offers critical insight. A peripheral blood smear can reveal abnormally shaped cells, such as sickle-shaped cells in sickle cell anemia or fragmented cells (schistocytes) in hemolytic anemia. The presence of nucleated or immature red cells may indicate marrow stress or infiltration. These visual markers can point directly to certain types of anemia even before additional tests are performed.
Iron Studies and Nutritional Testing
When iron deficiency is suspected, modern diagnostics assess serum ferritin to estimate iron stores, along with serum iron, total iron-binding capacity (TIBC), and transferrin saturation to evaluate circulating iron levels and transport capacity. These tests help distinguish between iron deficiency anemia and anemia of chronic inflammation, where iron stores may appear normal but utilization is impaired.
For macrocytic anemias, measuring vitamin B12 and folate levels is essential to uncover deficiencies impairing DNA synthesis. Without correcting these deficiencies, red blood cell production remains ineffective despite supplementation with iron.
Specialized Tests for Complex Cases
Certain anemias require more advanced diagnostics. A Coombs test helps detect autoimmune hemolytic anemia, while hemoglobin electrophoresis identifies inherited disorders like thalassemia or sickle cell disease. In patients with unexplained anemia or abnormal blood counts, a bone marrow biopsy may be necessary to evaluate marrow function or detect leukemia.
When gastrointestinal bleeding is suspected as a hidden cause, clinicians may order a stool occult blood test to check for microscopic blood loss. In cases of environmental or occupational exposure, blood lead levels are measured to detect lead poisoning contributing to anemia.
Through this combination of laboratory and microscopic analysis, modern medicine maps out anemia’s physiological cause, enabling a targeted treatment plan.
The Ayurvedic – Observing the Body’s Signs
While modern diagnostics focus on laboratory values, Ayurveda emphasizes direct observation, tactile assessment, and functional evaluation. An Ayurvedic physician seeks to understand the visible and subtle signs that reflect the state of the blood tissue (Rakta Dhatu) and the digestive fire (Agni).
Visual Examination of the Body
In Ayurveda, pale conjunctiva or tongue indicates depletion of blood tissue, while a yellowish tint suggests an imbalance in Pitta Dosha affecting the blood. The appearance of the skin—whether pale, dry, or yellowish—provides further confirmation. Nails are inspected for brittleness, ridging, or spoon-shaped deformities, signaling poor nourishment at the tissue level.
Pulse Diagnosis: Nadi Pariksha
An Ayurvedic physician also assesses the pulse (Nadi Pariksha) to identify the dominant dosha imbalance contributing to anemia. A bounding, rapid pulse may reflect excess heat and Pitta, while a weak, irregular pulse suggests Vata dominance impairing circulation and tissue nourishment.
The Tenfold Evaluation: Dashavidha Pariksha
Diagnosis in Ayurveda is holistic and individualized. The Dashavidha Pariksha, or tenfold examination, considers constitution (Prakriti), pathology (Vikriti), tissue quality (Sara), body build (Samhanana), body measurements (Pramana), adaptability (Satmya), mental strength (Satva), digestive power (Ahara Shakti), exercise capacity (Vyayama Shakti), and age (Vaya). Each factor helps personalize diagnosis and treatment, revealing deeper causes behind the anemia.
Observing Natural Wastes: Mala and Mutra Pariksha
The examination extends to natural wastes. Pale or scanty urine (Mutra), light-colored stools (Mala), or the presence of undigested food particles point to impaired digestion and absorption. Sweat abnormalities (Sweda)—whether excessive or absent—signal disturbances in bodily channels (Srotas) affecting blood nourishment.
Integrating Both Diagnostic Systems
When viewed side by side, modern and Ayurvedic diagnostics each offer unique insights. Modern medicine measures deficiencies in iron, B12, or folate with laboratory precision, while Ayurveda interprets functional imbalances through clinical observation. Neither system is complete on its own; together they form a comprehensive map.
A patient may have low hemoglobin on a blood test, but if digestive fire is weak (Agni Mandya), simply providing iron supplements may not resolve the anemia. The Ayurvedic approach helps identify why the nutrients are not being properly assimilated or transformed into healthy tissue.
By integrating laboratory testing with Ayurvedic assessment, healthcare practitioners can move beyond simply correcting lab numbers and address anemia as a systemic imbalance requiring both biochemical and functional restoration. This integrative model promotes not just symptom relief but long-term resilience and vitality.
Ayurvedic Treatment Strategies
Treatment of anemia in Ayurveda goes beyond simply replacing iron or nutrients. It focuses on restoring the body’s digestive fire (Agni), clearing metabolic waste (Ama), rejuvenating tissue (Dhatu Poshana), and correcting the imbalance of doshas—particularly Pitta and Rakta vitiation. Ayurvedic treatment is both systemic and personalized, designed to address root causes and nourish the entire body.
Shodhana (Purification Therapy)- Clearing the Pathways
For patients showing signs of toxin accumulation (Ama) or excessive Pitta, Ayurveda recommends Shodhana Chikitsa, or purification therapy, as a first step. Purification clears obstructions in the body’s channels (Srotas) and prepares the system to better absorb nutrients.
Among purification methods, Virechana (therapeutic purgation) is the primary choice for anemia with Pitta dominance. By eliminating excess Pitta from the liver and gastrointestinal tract, Virechana supports healthier blood formation. In cases with coexisting worm infestation (Krimi), deworming therapies using herbal antiparasitic formulations may be recommended before nutrient replenishment.
Purification is not necessary for every patient. It is typically prescribed when digestive toxins, sluggish metabolism, or inflammatory signs accompany anemia. For milder cases or those with weak constitutions, purification is avoided in favor of gentle nourishing therapies.
Shamana (Pacification Therapy)- Restoring Balance and Nourishment
Once purification is completed—or in cases where it is not required—Shamana Chikitsa aims to pacify dosha imbalances and directly nourish blood tissue. This is achieved through specific herbal-mineral formulations known for their hematinic and tissue-restorative properties.
Among the most widely used is Mandura Bhasma, a purified iron oxide preparation created through elaborate Ayurvedic processing (Shodhana and Marana). Mandura Bhasma enhances iron absorption, stimulates hematopoiesis, and improves liver function. It is often prescribed alongside other herbs to enhance its bioavailability and tolerability.
Another key formulation is Punarnava Mandura, a classical compound containing Mandura Bhasma, Punarnava (Boerhaavia diffusa), Triphala, Trikatu, and other supportive herbs. Punarnava Mandura not only replenishes iron but also acts as a mild diuretic, liver protector, and digestive stimulant—making it ideal in anemia linked with edema, sluggish digestion, or mild hepatic dysfunction.
Navayasa Churna is a traditional powder combining nine iron-rich substances, prescribed for similar indications. Its gentle action makes it suitable for younger patients or those with weaker digestion.
Liquid preparations such as Lohasava (a fermented iron tonic) and Draksharishta (grape-based digestive tonic) are often prescribed to enhance appetite, aid digestion, and improve iron assimilation in individuals with poor gastrointestinal function.
Rasayana (Rejuvenative Therapy)-Strengthening the Foundation
Beyond direct iron supplementation, Ayurveda incorporates Rasayana therapy, or rejuvenative treatment, to fortify vitality (Ojas), improve immunity, and enhance tissue nourishment at a deeper level. Rasayanas nourish not only the blood but also the supportive tissues that maintain its quality and quantity.
Herbs like Amalaki (Emblica officinalis), Haritaki (Terminalia chebula), and Guduchi (Tinospora cordifolia) are used as Rasayana agents to promote tissue regeneration, balance metabolism, and protect against oxidative stress.
For individuals experiencing fatigue, cognitive fog, or poor endurance along with anemia, Rasayana therapy improves both quantity (hemoglobin) and quality (tissue function) of the blood.
Dietary Recommendations (Ahara)
Diet plays a pivotal role in anemia recovery. Ayurveda emphasizes foods that nourish Rakta Dhatu while avoiding those that aggravate Pitta or impair digestion.
Iron-rich foods recommended include black sesame seeds, jaggery (unrefined cane sugar), black raisins, dates, pomegranate, spinach, and beetroot. These are ideally consumed with digestive spices such as cumin, coriander, or fennel to enhance assimilation.
Warm, cooked meals are preferred over raw or cold foods to support digestive fire. Patients are advised to avoid excessive intake of sour, salty, fermented, oily, or processed foods, as these can increase Pitta and weaken Agni. Curd, cold drinks, and night-time heavy meals are discouraged.
Cooking food in iron cookware, a time-tested Ayurvedic practice, can naturally enrich meals with trace iron.
In cases where digestion is weak, small frequent meals with digestive teas (jeera, ajwain, ginger) may be recommended to gradually rebuild Agni.
Lifestyle Guidelines (Vihara)
Recovery from anemia is not solely dependent on medication and diet. Ayurveda integrates lifestyle modifications (Vihara) to optimize blood production and energy restoration.
Patients are advised to avoid daytime sleeping, which may further slow digestion and metabolism. Light physical activity, such as gentle yoga or walking, is encouraged to stimulate circulation without overexertion. Excessive physical strain, late-night work, and stress-inducing activities are discouraged during the recovery period.
Practices such as Nasya (nasal oil application) using medicated oils may be prescribed to nourish the brain and nervous system, especially in cases where anemia presents with cognitive or neurological symptoms linked to B12 deficiency.
Mindful breathing practices and stress-reduction techniques align with Ayurveda’s recognition of the mind-body connection in hematopoiesis.
A Personalized, Layered Approach
Ayurvedic treatment of anemia is neither uniform nor solely symptom-focused. It adapts therapy to the patient’s constitution (Prakriti), digestive strength, dosha imbalance, and severity of tissue depletion. Some patients may require only dietary guidance and gentle herbal tonics; others may need purification, mineral supplementation, and long-term rejuvenative therapies.
This layered, holistic approach seeks not just to correct hemoglobin levels but to rebuild vitality, strengthen digestion, improve tissue resilience, and prevent recurrence. By nourishing the foundation, Ayurveda aspires toward sustainable recovery rather than temporary correction.
Modern Medical Treatment
In modern medicine, the treatment of anemia is tailored according to its underlying cause, severity, and associated health conditions. While the goal is to restore normal hemoglobin levels, treatment also aims to address any factors contributing to the deficiency, whether nutritional, genetic, inflammatory, or pathological.
Iron Therapy: The Cornerstone of Iron Deficiency Anemia
For individuals diagnosed with iron deficiency anemia, oral iron supplementation remains the first-line therapy. Iron is typically administered as ferrous sulfate, ferrous gluconate, or ferrous fumarate, each providing different elemental iron concentrations. A standard dose may range from 60 to 200 milligrams of elemental iron per day.
Iron supplements are best absorbed on an empty stomach or with vitamin C, which enhances absorption. However, many patients experience gastrointestinal side effects such as nausea, abdominal discomfort, constipation, or diarrhea. To improve tolerance, iron may be taken with food, although absorption is reduced.
In cases where oral iron is poorly tolerated, ineffective, or contraindicated—such as patients with inflammatory bowel disease, malabsorption syndromes, or those undergoing dialysis—intravenous iron therapy is prescribed. Modern intravenous preparations like iron sucrose, ferric carboxymaltose, or iron dextran provide higher doses with faster replenishment, though they require monitoring for allergic reactions or iron overload.
Iron therapy typically continues for several months, even after hemoglobin normalizes, to replenish depleted iron stores and prevent relapse.
Vitamin and Mineral Supplementation
In patients with macrocytic anemia, caused by vitamin B12 or folate deficiency, treatment focuses on replacing the missing nutrients. Vitamin B12 is administered as intramuscular injections (cyanocobalamin or hydroxocobalamin), usually starting with daily or weekly injections followed by monthly maintenance.
For individuals with dietary deficiency or malabsorption, lifelong supplementation may be required. Oral vitamin B12 may be used in mild cases or in individuals without intrinsic factor deficiency.
Folic acid supplementation is given orally in doses of 1 to 5 mg per day, depending on the severity of deficiency and underlying causes.
It is critical to correct vitamin B12 deficiency before or along with folate in combined deficiencies to prevent worsening of neurological complications.
In certain anemias involving other trace mineral deficiencies, such as copper or zinc imbalance, targeted supplementation may also be included.
Erythropoiesis-Stimulating Agents
In patients with anemia secondary to chronic kidney disease, chemotherapy, or bone marrow suppression, erythropoiesis-stimulating agents (ESAs) are used to stimulate red blood cell production. Recombinant erythropoietin (epoetin alfa) or darbepoetin alfa can reduce the need for transfusions and improve quality of life.
These agents are typically administered subcutaneously or intravenously and require close monitoring to avoid excessive hemoglobin correction, which increases the risk of thrombosis or cardiovascular events.
Iron supplementation is often co-administered with ESAs to support optimal response.
Blood Transfusion – Immediate but Temporary Correction
For patients with severe anemia or symptomatic anemia requiring urgent correction, packed red blood cell transfusions provide immediate restoration of oxygen-carrying capacity. Transfusions are commonly indicated when hemoglobin falls below 7 to 8 g/dL in stable patients, or higher thresholds in individuals with active bleeding, cardiovascular disease, or symptomatic hypoxia.
While transfusions are lifesaving in acute situations, they carry risks such as allergic reactions, febrile non-hemolytic reactions, hemolytic reactions, transfusion-related infections, and iron overload with repeated transfusions. Therefore, transfusions are used judiciously, often as a bridge until definitive treatment takes effect.
Disease-Specific Treatments: Addressing the Root Cause
In some forms of anemia, treatment must target the underlying disease process. For example:
- In autoimmune hemolytic anemia, corticosteroids or immunosuppressive therapies are administered to reduce red cell destruction.
- In aplastic anemia, immunosuppressive therapy or bone marrow transplantation may be required to restore marrow function.
- In thalassemia major or sickle cell disease, chronic transfusions, iron chelation therapy, and emerging gene therapies are integral to management.
- In anemia of chronic inflammation, treating the primary inflammatory disease (e.g., rheumatoid arthritis, infections) is necessary for anemia improvement.
Monitoring Treatment Response and Complications
Throughout treatment, regular monitoring of hemoglobin, hematocrit, reticulocyte count, ferritin, and iron studies is essential to assess progress and avoid complications like iron overload.
Patients receiving long-term iron or transfusion therapy are monitored for liver function, cardiac health, and endocrine complications associated with iron accumulation.
In individuals treated with erythropoiesis-stimulating agents, monitoring blood pressure and thrombotic risk is equally important.
Integrative Considerations
Modern treatment of anemia is highly effective in correcting measurable deficiencies. However, some patients report lingering fatigue, poor energy, or recurrent anemia despite normalized lab values. In such cases, integrative strategies—such as incorporating dietary optimization, gastrointestinal health evaluation, or stress management—can play a complementary role alongside medical treatment.
By understanding both the biochemical correction and systemic context of anemia, practitioners can tailor care beyond mere lab normalization, supporting long-term vitality and resilience.
Where Modern Medicine Meets Ayurveda
Anemia occupies a unique place in healthcare, sitting at the crossroads of nutrition, digestion, systemic disease, and tissue health. Both modern medicine and Ayurveda offer valuable, evidence-based perspectives, yet they approach anemia from fundamentally different starting points. Integrating these approaches allows for a more comprehensive, patient-centered path to healing.
Modern medicine excels in its diagnostic precision and targeted correction of deficiencies. Through laboratory measurements of hemoglobin, hematocrit, iron studies, vitamin B12, and folate levels, clinicians can rapidly identify specific nutritional gaps or pathological processes impairing red blood cell production. The treatments—whether iron supplements, vitamin injections, erythropoiesis-stimulating agents, or transfusions—are effective at restoring hemoglobin values and addressing acute physiological deficits. For patients with chronic kidney disease, chemotherapy-induced anemia, or genetic blood disorders, these interventions can be life-saving.
Yet despite this precision, many patients treated for anemia find their recovery incomplete. Fatigue lingers; immunity remains compromised; vitality does not fully return. The laboratory numbers may normalize, but the person behind them feels only partially restored. Here lies a gap where Ayurveda provides complementary depth.
Ayurveda views anemia (Panduroga) not only as a numerical deficiency but as a breakdown in digestion, tissue transformation, and systemic balance. It recognizes that iron or nutrients must not only be consumed but properly digested, absorbed, metabolized, and integrated into healthy blood tissue. If the digestive fire (Agni) is weak or the body’s metabolic channels (Srotas) are obstructed, simply adding more iron will not correct the problem. This insight explains why some individuals fail to respond to iron therapy until deeper digestive imbalances are addressed.
The concept of strengthening Agni—through dietary adjustments, digestive spices, herbal formulations, and purification therapies—becomes central in an Ayurvedic anemia treatment plan. Likewise, rejuvenative therapies (Rasayanas) aim not merely to increase hemoglobin but to rebuild vitality (Ojas), restore cellular integrity, and nourish the tissues from within.
Scientific research increasingly supports some of these principles. Studies on traditional iron preparations like Mandura Bhasma suggest comparable bioavailability to pharmaceutical iron, with potentially fewer gastrointestinal side effects. Polyherbal formulations like Punarnava Mandura and Lohasava show hepatoprotective, anti-inflammatory, and mild diuretic properties alongside their hematinic effects, offering a broader therapeutic action than simple iron replacement. Meanwhile, practices such as cooking in iron utensils—long recommended in Ayurveda—are now validated for their ability to increase dietary iron intake.
Beyond physical treatments, Ayurveda brings attention to the role of mental and emotional well-being in hematopoiesis. Chronic stress, grief, suppressed emotions, and lifestyle imbalance are viewed as contributing to poor digestion, weak tissue formation, and lowered immunity. Integrating stress-reducing practices like pranayama, mindfulness, or gentle yoga into anemia recovery adds a layer of holistic care often absent from purely biomedical models.
This integration does not imply replacing modern treatments with Ayurveda or vice versa. Rather, it invites a partnership: using modern diagnostics to identify specific deficiencies and monitor progress, while applying Ayurvedic principles to correct the deeper functional imbalances that allowed anemia to develop in the first place. For example, a patient recovering from iron deficiency anemia may benefit from iron supplements while simultaneously adopting an iron-rich Ayurvedic diet, improving digestive capacity, and using Rasayana herbs to rebuild energy reserves.
In chronic, relapsing anemias—whether due to inflammation, autoimmune disease, or malabsorption—Ayurvedic interventions aimed at clearing metabolic toxins (Ama), restoring digestive health, and pacifying dosha imbalances provide a complementary framework to conventional care. By supporting the body’s inner environment, these interventions may improve long-term response to medical treatments and reduce recurrence.
Ultimately, an integrative approach honors both the measurable and the experiential aspects of healing. It recognizes anemia not only as a depletion of red blood cells but as a signal of broader physiological, nutritional, and emotional imbalance. It seeks not merely to normalize a lab value but to restore the person’s strength, vitality, and resilience.
For Western readers accustomed to viewing anemia as a number on a blood test, the Ayurvedic lens expands the horizon—inviting a deeper understanding of the body’s innate wisdom, the interconnectedness of systems, and the profound role of digestion, mind, and spirit in sustaining health.
References
Appeal:
If any reference link does not open due to technical issues or future webpage updates, you are encouraged to search by the researcher’s name, article title, or copy and paste the reference into a search engine or scientific database. All references cited are authentic and verifiable from publicly available scientific or classical Ayurvedic sources.
- World Health Organization. (2020). Anaemia. Retrieved from https://www.who.int/health-topics/anaemia
- Pasricha, S. R., Tye-Din, J., Muckenthaler, M. U., & Swinkels, D. W. (2021). Iron deficiency. The Lancet, 397(10270), 233-248. https://doi.org/10.1016/S0140-6736(20)32594-0
- Bhishagratna, K. K. (Translator). (2006). Charaka Samhita (Chikitsa Sthana, Chapter 16: Panduroga Chikitsa). Varanasi: Chaukhamba Sanskrit Series Office.
- Gorde, P., Suryawanshi, S., & Mahajan, R. (2017). A review on Mandura Bhasma: Classical perspectives and modern validation. International Journal of Ayurveda Research, 8(1), 45-50. Retrieved from https://ijaronline.com/article.asp?issn=0974-7788;year=2017;volume=8;issue=1;spage=45;epage=50
- Beard, J. L. (2001). Iron biology in immune function, muscle metabolism and neuronal functioning. The Journal of Nutrition, 131(2), 568S-580S. https://doi.org/10.1093/jn/131.2.568S
- Kotecha, R. V., Patel, K. D., & Bhalodia, Y. (2014). Clinical evaluation of Punarnava Mandura in iron deficiency anemia: A double-blind study. AYU (An International Quarterly Journal of Research in Ayurveda), 35(1), 50-54. Retrieved from https://www.ayujournal.org/text.asp?2014/35/1/50/129060
- O’Connell, J., & Kraut, E. H. (2021). Vitamin B12 deficiency. Cleveland Clinic Journal of Medicine, 88(5), 295-301. https://doi.org/10.3949/ccjm.88a.ccc066
- Bopche, A. V., & Mishra, A. K. (2012). Impact of cooking in iron pots on the iron content of food and its role in reducing iron deficiency anemia: A review. Indian Journal of Public Health, 56(1), 49-54. https://doi.org/10.4103/0019-557X.96976











2 Responses
This has been so helpful thanks for sharing
Very informative guide! It clearly explains how anemia is diagnosed and the treatment options available. Helpful for anyone who wants to understand the condition better and manage it effectively.