Best Medicines to Cure Herpes
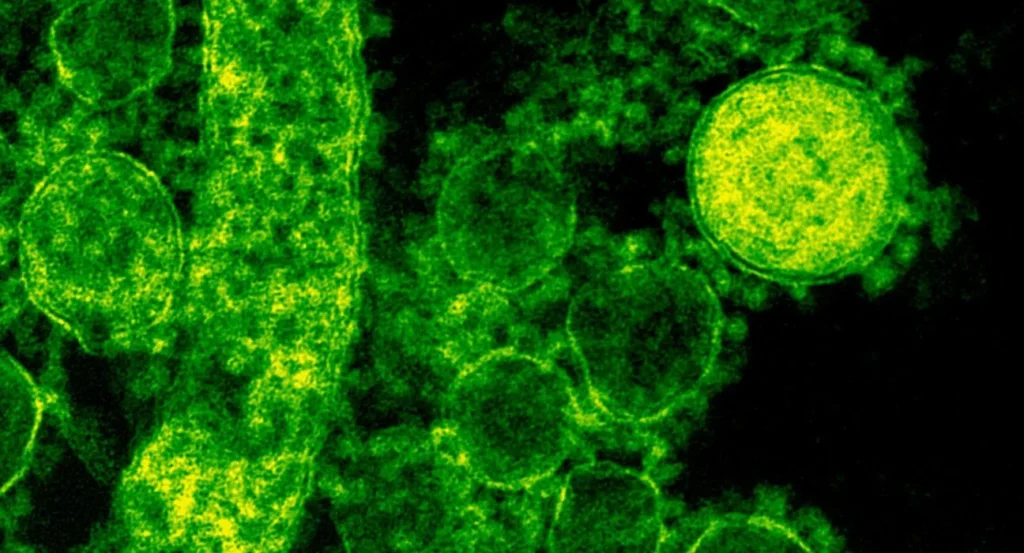
The herpes family of viruses, known scientifically as Herpesviridae, comprises a large group of viruses that cause various diseases in humans and animals. This viral family includes well-known members like herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2), which cause oral and genital herpes, respectively. Other significant members include the varicella-zoster virus (VZV), which causes chickenpox and shingles, the Epstein-Barr virus (EBV), responsible for infectious mononucleosis, and the cytomegalovirus (CMV), which can lead to serious infections in immunocompromised individuals. Herpesviruses: A Detailed Exploration of HSV-1, HSV-2, CMV, and EBV Herpesviruses are a significant family of DNA viruses known to cause a wide range of diseases in humans. Among these, Herpes Simplex Virus Type 1 (HSV-1), Herpes Simplex Virus Type 2 (HSV-2), Cytomegalovirus (CMV), and Epstein-Barr Virus (EBV) are the most clinically significant. Each virus has unique characteristics, modes of transmission, associated symptoms, and health implications. Understanding these viruses in detail is crucial for managing and mitigating their impact on global health. HSV-1: Herpes Simplex Virus Type 1 Overview and Prevalence Herpes Simplex Virus Type 1 (HSV-1) is one of the most common viruses in the world. It is primarily associated with oral herpes, which typically manifests as cold sores or fever blisters around the mouth and lips. However, HSV-1 can also cause genital herpes through oral-genital contact, highlighting its versatility in transmission. According to the World Health Organization (WHO), approximately 67% of the global population under the age of 50 is infected with HSV-1. This makes it one of the most widespread viral infections, with significant public health implications. The virus is highly contagious and spreads through direct contact with infected saliva, skin, or mucous membranes. Transmission and Lifecycle HSV-1 is primarily transmitted through direct contact with infected bodily fluids or lesions. Common methods of transmission include kissing, sharing eating utensils, and engaging in oral sex. Once the virus enters the body, it travels along the nerve cells to the trigeminal ganglion, where it establishes latency. During this latent phase, the virus remains dormant and does not cause symptoms. However, various triggers such as stress, illness, or a weakened immune system can reactivate the virus, leading to recurrent outbreaks. These outbreaks typically manifest as cold sores or fever blisters, which are painful and can take several days to heal. During an outbreak, the virus becomes active and can be shed through the skin, even if no visible sores are present. Symptoms and Complications The primary symptom of HSV-1 infection is the development of cold sores or fever blisters around the mouth. These sores are usually preceded by a tingling or itching sensation at the site of infection. Other symptoms may include: Swollen lymph nodes Fever Sore throat Headache Fatigue In rare cases, HSV-1 can cause more severe complications, such as herpetic encephalitis, which is an inflammation of the brain. This condition is life-threatening and requires immediate medical attention. Additionally, HSV-1 can cause ocular herpes, leading to corneal infections and potential vision loss if not treated promptly. Treatment and Management There is currently no cure for HSV-1, but antiviral medications can help manage the symptoms and reduce the frequency of outbreaks. Common antiviral drugs used to treat HSV-1 include acyclovir, valacyclovir, and famciclovir. These medications can be taken during an outbreak to shorten its duration or as a daily suppressive therapy to reduce the likelihood of future outbreaks. Preventive measures, such as avoiding close contact with infected individuals during an active outbreak and practicing good hygiene, are also essential in managing HSV-1. Additionally, individuals with frequent outbreaks may benefit from lifestyle changes that reduce stress and strengthen the immune system. HSV-2: Herpes Simplex Virus Type 2 Overview and Prevalence Herpes Simplex Virus Type 2 (HSV-2) is primarily associated with genital herpes, a sexually transmitted infection (STI) that affects millions of people worldwide. HSV-2 is less common than HSV-1, but it is more likely to cause recurrent and severe genital infections. The Centers for Disease Control and Prevention (CDC) estimate that approximately 12% of adults in the United States are infected with HSV-2. Women are more frequently affected than men, likely due to biological factors that make them more susceptible to infection. Transmission and Lifecycle HSV-2 is primarily transmitted through sexual contact, including vaginal, anal, and oral sex. The virus is most contagious during active outbreaks when visible sores are present. However, like HSV-1, HSV-2 can also be transmitted through asymptomatic shedding, meaning the virus can spread even when no symptoms are apparent. Once HSV-2 enters the body, it travels to the sacral ganglia, a cluster of nerve cells near the base of the spine, where it establishes latency. The virus can reactivate periodically, leading to recurrent genital sores, which are often painful and can cause significant discomfort. Symptoms and Complications The primary symptom of HSV-2 infection is the development of painful blisters or sores in the genital and anal regions. These sores may be accompanied by: Itching or burning sensations Swollen lymph nodes in the groin Painful urination Flu-like symptoms, such as fever and body aches Recurrent outbreaks of HSV-2 are common, particularly in the first year after infection. Over time, the frequency and severity of outbreaks may decrease, but the virus remains in the body for life. In addition to physical symptoms, HSV-2 can have significant psychosocial impacts, including anxiety, depression, and stigma. The fear of transmitting the virus to a partner can also affect sexual relationships and overall quality of life. Treatment and Management As with HSV-1, there is no cure for HSV-2. However, antiviral medications can help manage the symptoms, reduce the frequency of outbreaks, and lower the risk of transmission. Daily suppressive therapy with antivirals is particularly beneficial for individuals with frequent outbreaks or those in relationships where one partner is uninfected. Education and counseling are essential components of HSV-2 management, helping individuals understand their condition, reduce the risk of transmission, and cope with the emotional aspects of living with the virus. Safe sex practices, such as using condoms and dental dams, are also crucial in preventing the